SIMULATION CASEBOOK - MyCourses
SIMULATION CASEBOOK - MyCourses
SIMULATION CASEBOOK - MyCourses
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
Gilbert Program in Medical Simulation<br />
Simulation Casebook<br />
Harvard Medical School Draft of the 1 st edition (2011), updated 3/2/12<br />
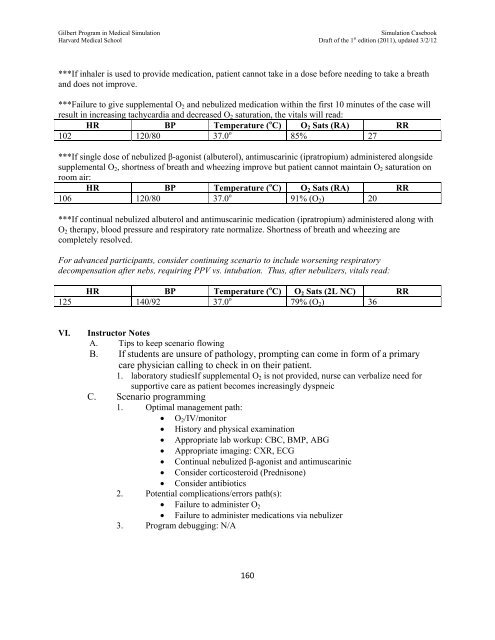
***If inhaler is used to provide medication, patient cannot take in a dose before needing to take a breath<br />
and does not improve.<br />
***Failure to give supplemental O 2 and nebulized medication within the first 10 minutes of the case will<br />
result in increasing tachycardia and decreased O 2 saturation, the vitals will read:<br />
HR BP Temperature ( o C) O 2 Sats (RA) RR<br />
102 120/80 37.0 o 85% 27<br />
***If single dose of nebulized β-agonist (albuterol), antimuscarinic (ipratropium) administered alongside<br />
supplemental O 2 , shortness of breath and wheezing improve but patient cannot maintain O 2 saturation on<br />
room air:<br />
HR BP Temperature ( o C) O 2 Sats (RA) RR<br />
106 120/80 37.0 o 91% (O 2 ) 20<br />
***If continual nebulized albuterol and antimuscarinic medication (ipratropium) administered along with<br />
O 2 therapy, blood pressure and respiratory rate normalize. Shortness of breath and wheezing are<br />
completely resolved.<br />
For advanced participants, consider continuing scenario to include worsening respiratory<br />
decompensation after nebs, requiring PPV vs. intubation. Thus, after nebulizers, vitals read:<br />
HR BP Temperature ( o C) O 2 Sats (2L NC) RR<br />
125 140/92 37.0 o 79% (O 2 ) 36<br />
VI.<br />
Instructor Notes<br />
A. Tips to keep scenario flowing<br />
B. If students are unsure of pathology, prompting can come in form of a primary<br />
care physician calling to check in on their patient.<br />
1. laboratory studiesIf supplemental O 2 is not provided, nurse can verbalize need for<br />
supportive care as patient becomes increasingly dyspneic<br />
C. Scenario programming<br />
1. Optimal management path:<br />
O 2 /IV/monitor<br />
History and physical examination<br />
Appropriate lab workup: CBC, BMP, ABG<br />
Appropriate imaging: CXR, ECG<br />
Continual nebulized β-agonist and antimuscarinic<br />
Consider corticosteroid (Prednisone)<br />
Consider antibiotics<br />
2. Potential complications/errors path(s):<br />
Failure to administer O 2<br />
Failure to administer medications via nebulizer<br />
3. Program debugging: N/A<br />
160