SIMULATION CASEBOOK - MyCourses
SIMULATION CASEBOOK - MyCourses
SIMULATION CASEBOOK - MyCourses
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
Gilbert Program in Medical Simulation<br />
Simulation Casebook<br />
Harvard Medical School Draft of the 1 st edition (2011), updated 3/2/12<br />
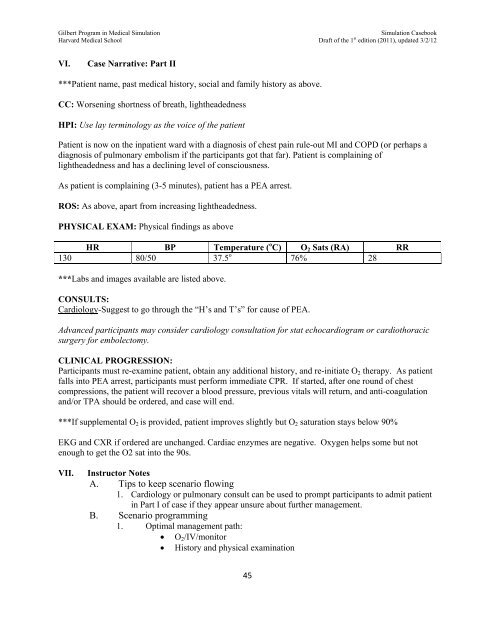
VI.<br />
Case Narrative: Part II<br />
***Patient name, past medical history, social and family history as above.<br />
CC: Worsening shortness of breath, lightheadedness<br />
HPI: Use lay terminology as the voice of the patient<br />
Patient is now on the inpatient ward with a diagnosis of chest pain rule-out MI and COPD (or perhaps a<br />
diagnosis of pulmonary embolism if the participants got that far). Patient is complaining of<br />
lightheadedness and has a declining level of consciousness.<br />
As patient is complaining (3-5 minutes), patient has a PEA arrest.<br />
ROS: As above, apart from increasing lightheadedness.<br />
PHYSICAL EXAM: Physical findings as above<br />
HR BP Temperature ( o C) O 2 Sats (RA) RR<br />
130 80/50 37.5 o 76% 28<br />
***Labs and images available are listed above.<br />
CONSULTS:<br />
Cardiology-Suggest to go through the “H’s and T’s” for cause of PEA.<br />
Advanced participants may consider cardiology consultation for stat echocardiogram or cardiothoracic<br />
surgery for embolectomy.<br />
CLINICAL PROGRESSION:<br />
Participants must re-examine patient, obtain any additional history, and re-initiate O 2 therapy. As patient<br />
falls into PEA arrest, participants must perform immediate CPR. If started, after one round of chest<br />
compressions, the patient will recover a blood pressure, previous vitals will return, and anti-coagulation<br />
and/or TPA should be ordered, and case will end.<br />
***If supplemental O 2 is provided, patient improves slightly but O 2 saturation stays below 90%<br />
EKG and CXR if ordered are unchanged. Cardiac enzymes are negative. Oxygen helps some but not<br />
enough to get the O2 sat into the 90s.<br />
VII.<br />
Instructor Notes<br />
A. Tips to keep scenario flowing<br />
1. Cardiology or pulmonary consult can be used to prompt participants to admit patient<br />
in Part I of case if they appear unsure about further management.<br />
B. Scenario programming<br />
1. Optimal management path:<br />
O 2 /IV/monitor<br />
History and physical examination<br />
45