Annals of Diagnostic Paediatric Pathology
Annals of Diagnostic Paediatric Pathology
Annals of Diagnostic Paediatric Pathology
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
80<br />
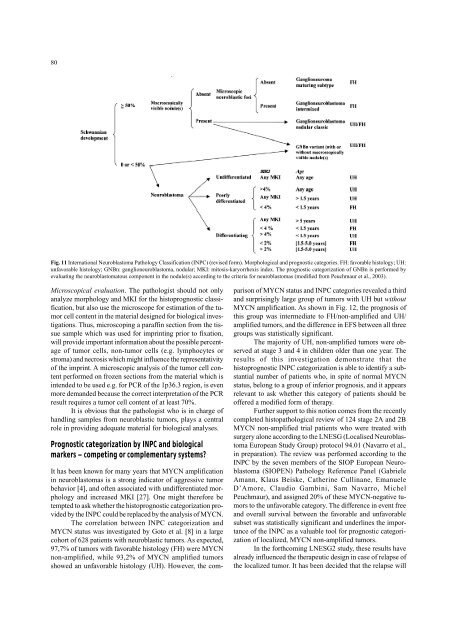
Fig. 11 International Neuroblastoma <strong>Pathology</strong> Classification (INPC) (revised form). Morphological and prognostic categories. FH: favorable histology; UH:<br />
unfavorable histology; GNBn: ganglioneuroblastoma, nodular; MKI: mitosis-karyorrhexis index. The prognostic categorization <strong>of</strong> GNBn is performed by<br />
evaluating the neuroblastomatous component in the nodule(s) according to the criteria for neuroblastomas (modified from Peuchmaur et al., 2003).<br />
Microscopical evaluation. The pathologist should not only<br />
analyze morphology and MKI for the histoprognostic classification,<br />
but also use the microscope for estimation <strong>of</strong> the tumor<br />
cell content in the material designed for biological investigations.<br />
Thus, microscoping a paraffin section from the tissue<br />
sample which was used for imprinting prior to fixation,<br />
will provide important information about the possible percentage<br />
<strong>of</strong> tumor cells, non-tumor cells (e.g. lymphocytes or<br />
stroma) and necrosis which might influence the representativity<br />
<strong>of</strong> the imprint. A microscopic analysis <strong>of</strong> the tumor cell content<br />
performed on frozen sections from the material which is<br />
intended to be used e.g. for PCR <strong>of</strong> the 1p36.3 region, is even<br />
more demanded because the correct interpretation <strong>of</strong> the PCR<br />
result requires a tumor cell content <strong>of</strong> at least 70%.<br />
It is obvious that the pathologist who is in charge <strong>of</strong><br />
handling samples from neuroblastic tumors, plays a central<br />
role in providing adequate material for biological analyses.<br />
Prognostic categorization by INPC and biological<br />
markers – competing or complementary systems<br />
It has been known for many years that MYCN amplification<br />
in neuroblastomas is a strong indicator <strong>of</strong> aggressive tumor<br />
behavior [4], and <strong>of</strong>ten associated with undifferentiated morphology<br />
and increased MKI [27]. One might therefore be<br />
tempted to ask whether the histoprognostic categorization provided<br />
by the INPC could be replaced by the analysis <strong>of</strong> MYCN.<br />
The correlation between INPC categorization and<br />
MYCN status was investigated by Goto et al. [8] in a large<br />
cohort <strong>of</strong> 628 patients with neuroblastic tumors. As expected,<br />
97,7% <strong>of</strong> tumors with favorable histology (FH) were MYCN<br />
non-amplified, while 93,2% <strong>of</strong> MYCN amplified tumors<br />
showed an unfavorable histology (UH). However, the comparison<br />
<strong>of</strong> MYCN status and INPC categories revealed a third<br />
and surprisingly large group <strong>of</strong> tumors with UH but without<br />
MYCN amplification. As shown in Fig. 12, the prognosis <strong>of</strong><br />
this group was intermediate to FH/non-amplified and UH/<br />
amplified tumors, and the difference in EFS between all three<br />
groups was statistically significant.<br />
The majority <strong>of</strong> UH, non-amplified tumors were observed<br />
at stage 3 and 4 in children older than one year. The<br />
results <strong>of</strong> this investigation demonstrate that the<br />
histoprognostic INPC categorization is able to identify a substantial<br />
number <strong>of</strong> patients who, in spite <strong>of</strong> normal MYCN<br />
status, belong to a group <strong>of</strong> inferior prognosis, and it appears<br />
relevant to ask whether this category <strong>of</strong> patients should be<br />
<strong>of</strong>fered a modified form <strong>of</strong> therapy.<br />
Further support to this notion comes from the recently<br />
completed histopathological review <strong>of</strong> 124 stage 2A and 2B<br />
MYCN non-amplified trial patients who were treated with<br />
surgery alone according to the LNESG (Localised Neuroblastoma<br />
European Study Group) protocol 94.01 (Navarro et al.,<br />
in preparation). The review was performed according to the<br />
INPC by the seven members <strong>of</strong> the SIOP European Neuroblastoma<br />
(SIOPEN) <strong>Pathology</strong> Reference Panel (Gabriele<br />
Amann, Klaus Beiske, Catherine Cullinane, Emanuele<br />
D’Amore, Claudio Gambini, Sam Navarro, Michel<br />
Peuchmaur), and assigned 20% <strong>of</strong> these MYCN-negative tumors<br />
to the unfavorable category. The difference in event free<br />
and overall survival between the favorable and unfavorable<br />
subset was statistically significant and underlines the importance<br />
<strong>of</strong> the INPC as a valuable tool for prognostic categorization<br />
<strong>of</strong> localized, MYCN non-amplified tumors.<br />
In the forthcoming LNESG2 study, these results have<br />
already influenced the therapeutic design in case <strong>of</strong> relapse <strong>of</strong><br />
the localized tumor. It has been decided that the relapse will