Joint effects 2011 - An update of the involvement - 18 Weeks
Joint effects 2011 - An update of the involvement - 18 Weeks
Joint effects 2011 - An update of the involvement - 18 Weeks
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
<strong>Joint</strong> <strong>effects</strong> <strong>2011</strong><br />
<strong>An</strong> <strong>update</strong> <strong>of</strong> <strong>the</strong> <strong>involvement</strong> <strong>of</strong><br />
Allied Health Pr<strong>of</strong>essionals in orthopaedic<br />
and musculoskeletal services in Scotland<br />
mskscoping<strong>2011</strong>-rs.indd 1 03/11/<strong>2011</strong> 11:01
<strong>Joint</strong> <strong>effects</strong> <strong>2011</strong><br />
Acknowledgements<br />
The National MSK Redesign Programme benefits from a wide range <strong>of</strong> continuing<br />
support. Many thanks to all our contributors in Scotland: users <strong>of</strong> our MSK services<br />
and <strong>the</strong>ir representatives, AHPs at all levels, <strong>the</strong> Programme Board, a multidisciplinary<br />
expert panel, o<strong>the</strong>rs from service delivery, policy, academia and those supporting<br />
employment initiatives. Also to <strong>the</strong> many clinical staff who participated in <strong>the</strong> <strong>2011</strong><br />
scoping exercise, Fraser Ferguson, Michael McMenemy and Susan Parroy for<br />
co-ordinating it and producing <strong>the</strong> final publications.<br />
Our UK partners in particular: The Arthritis and Musculoskeletal Alliance, Sue<br />
Greenhalgh, Consultant Physio<strong>the</strong>rapist with Bolton PCT’s Musculoskeletal Service, for<br />
expert input on red flags, and Dr Jonathan Hill and <strong>the</strong> STarT team at Keele University.<br />
© Scottish Government Health Directorates <strong>2011</strong><br />
Design and editorial platform1design.com<br />
2<br />
mskscoping<strong>2011</strong>-rs.indd 2 03/11/<strong>2011</strong> 11:01
<strong>Joint</strong> <strong>effects</strong> <strong>2011</strong><br />
NHSScotland has a clear vision for achieving sustainable quality in<br />
Scotland’s healthcare.<br />
The National Musculoskeletal (MSK) Redesign Programme is designed to contribute<br />
towards achieving this aim and will bring about significant and sustainable service<br />
improvements for patients across Scotland in terms <strong>of</strong> better access, better advice and<br />
information, more targeted management and better patient outcomes, whilst at <strong>the</strong><br />
same time ensuring we use our resources efficiently.<br />
This scoping report provides a landscape <strong>of</strong> current practice across Scotland, updating<br />
a similar exercise, <strong>Joint</strong> <strong>effects</strong> 2005. It clearly demonstrates that health boards have<br />
developed MSK services to improve patient experience and outcome.<br />
What is clear from <strong>the</strong>se examples is that <strong>the</strong>re is innovation in services across<br />
Scotland and much we can learn from each o<strong>the</strong>r. The information in this report is<br />
intended to support local service clinical leaders and staff in developing <strong>the</strong>ir MSK<br />
services fur<strong>the</strong>r and to help realise <strong>the</strong> ambition we all have for <strong>the</strong>se services in<br />
Scotland. It is intended to help to inform staff, develop networks, and share <strong>the</strong><br />
learning and experience <strong>of</strong> MSK services.<br />
I firmly believe that we now have <strong>the</strong> opportunity to turn <strong>the</strong> vision into a reality and<br />
make a real difference to <strong>the</strong> many hundreds <strong>of</strong> thousands <strong>of</strong> people in Scotland who<br />
suffer from MSK problems.<br />
John Turner<br />
Chair National Musculoskeletal Programme Board<br />
Chief Executive, NHS 24<br />
The programme we are undertaking to transform musculoskeletal (MSK)<br />
services in NHSScotland is exciting and tremendously important.<br />
In 2007 service users said <strong>the</strong>y wanted easy access and a single point <strong>of</strong> referral,<br />
which we agreed to test out using NHS 24, and The Delivery Framework for Adult<br />
Rehabilitation 2007 still underpins all our work.<br />
We want to ensure all musculoskeletal practitioners, heads <strong>of</strong> service and AHP<br />
directors are actively engaged in this innovative and crucial area. It is our shared<br />
responsibility to work toge<strong>the</strong>r and make this happen.<br />
It is clear from <strong>Joint</strong> Effects <strong>2011</strong> that allied health pr<strong>of</strong>essionals are actively engaged<br />
and committed to <strong>the</strong> improvement agenda. The many examples you will read<br />
about show this. There is still more we can do to reduce variation in our practice<br />
by adopting, spreading and embedding best practice before we achieve truly<br />
transformational change.<br />
We have a real opportunity to use <strong>the</strong> information in this scoping report to continue<br />
to transform our MSK services. We must measure and demonstrate not only <strong>the</strong><br />
health impact but also <strong>the</strong> wider socio-economic impact that AHPs are having. We<br />
need to ensure that our practice is person centred and evidence based. I am confident<br />
that AHPs across Scotland will rise to both <strong>the</strong> opportunity and challenge.<br />
I look forward to working with you all as we deliver better services and better<br />
outcomes for patients in Scotland.<br />
Jacqui Lunday<br />
Chief Health Pr<strong>of</strong>essions Officer<br />
Scottish Government<br />
3<br />
mskscoping<strong>2011</strong>-rs.indd 3 03/11/<strong>2011</strong> 11:01
<strong>Joint</strong> <strong>effects</strong> <strong>2011</strong><br />
<strong>Joint</strong> <strong>effects</strong> <strong>2011</strong> provides an important insight into <strong>the</strong> role <strong>of</strong> allied health<br />
pr<strong>of</strong>essionals in delivering care to musculoskeletal patients in Scotland.<br />
Since <strong>the</strong> scoping in 2005, a great deal <strong>of</strong> progress has been made in improving care<br />
for patients including improved patient <strong>involvement</strong> schemes, self referral processes<br />
and <strong>the</strong> development <strong>of</strong> outcome measures for musculoskeletal conditions. However<br />
as our own recent research has found, <strong>the</strong> quality <strong>of</strong> musculoskeletal services in<br />
Scotland continues to vary between different health boards. It will thus be important<br />
that <strong>the</strong> good practice identified in this work is spread widely across individual boards.<br />
Ros Meek<br />
Director<br />
Arthritis and Musculoskeletal Alliance<br />
We at Keele University are delighted to be working toge<strong>the</strong>r with <strong>the</strong> MSK<br />
redesign team in Scotland to pilot <strong>the</strong> suitability <strong>of</strong> <strong>the</strong> STarT MSK tool which<br />
is a modification <strong>of</strong> <strong>the</strong> hugely successful STarT Back tool.<br />
This work takes forward recent primary care research demonstrating <strong>the</strong> benefit <strong>of</strong><br />
stratified models <strong>of</strong> care for low back pain problems, recently published in The Lancet.<br />
This project seeks to build on this proven decision aid and will expand this approach to<br />
individuals with a range <strong>of</strong> musculoskeletal conditions. In collaboration with <strong>the</strong> MSK<br />
redesign team in Scotland we will ensure that <strong>the</strong> new risk stratification approach<br />
can safely assist <strong>the</strong> selection <strong>of</strong> <strong>the</strong> large group <strong>of</strong> low-risk patients who are unlikely<br />
to benefit from additional interventions beyond minimal packages <strong>of</strong> reassurance<br />
and information. We also anticipate that our stratified approach will help to facilitate<br />
patient access to treatment resources for those who really need <strong>the</strong>m in a timely and<br />
cost-effective manner.<br />
I would like to congratulate this team for trail blazing an exciting path that is likely to<br />
have substantial benefits for MSK patients in Scotland. Well done!<br />
Dr Jonathan Hill<br />
Arthritis Research UK Lecturer in Physio<strong>the</strong>rapy<br />
Keele University<br />
4<br />
mskscoping<strong>2011</strong>-rs.indd 4 03/11/<strong>2011</strong> 11:01
<strong>Joint</strong> <strong>effects</strong> <strong>2011</strong><br />
Contents<br />
The policy context 6<br />
The musculoskeletal umbrella 6<br />
Person-centred, safe and effective 7<br />
The National Musculoskeletal Redesign Programme 8<br />
Multi-pr<strong>of</strong>essional MSK care pathways 8<br />
The National Advice and Triage Service 8<br />
Working Health Services Scotland 11<br />
The <strong>2011</strong> Scottish AHP MSK scoping 12<br />
Wider aims 12<br />
Method 12<br />
Findings 12<br />
Conclusion 13<br />
Summary <strong>of</strong> MSK services 15<br />
Overview 16<br />
Service descriptions 20<br />
Glossary 47<br />
5<br />
mskscoping<strong>2011</strong>-rs.indd 5 03/11/<strong>2011</strong> 11:01
<strong>Joint</strong> <strong>effects</strong> <strong>2011</strong><br />
The policy context<br />
In 2007 <strong>the</strong> need for musculoskeletal (MSK) service redesign was signalled by <strong>the</strong><br />
Scottish Government Health Directorates (SGHD) Co-ordinated, integrated and fit<br />
for purpose – The delivery framework for adult rehabilitation. The aim is to create a<br />
modern, effective, multi-disciplinary, multi-agency approach to rehabilitation services<br />
that are flexible and responsive, using <strong>the</strong> best that technology can <strong>of</strong>fer.<br />
Its most recent publication, Achieving sustainable quality: A 20:20 Vision (<strong>2011</strong>)<br />
recognises <strong>the</strong> challenges healthcare will have in <strong>the</strong> future and <strong>the</strong> need for services<br />
to be radically different.<br />
Some problems affect specific parts <strong>of</strong> <strong>the</strong> body, o<strong>the</strong>rs cause widespread muscular<br />
pain and fatigue. Autoimmune response conditions such as rheumatoid arthritis and<br />
ankylosing spondylitis are <strong>of</strong>ten progressive and are not related to age.<br />
The key role <strong>of</strong> <strong>the</strong> allied health pr<strong>of</strong>essionals (AHPs) in delivering a sophisticated<br />
and integrated approach to health, life and work in relation to MSK conditions is<br />
recognised by <strong>the</strong> Scottish Government. Since <strong>the</strong> publication <strong>of</strong> <strong>Joint</strong> <strong>effects</strong> 2005<br />
<strong>the</strong>re have been significant developments in both policy and front-line service delivery<br />
to support this.<br />
All Scottish Health Boards are now involved in <strong>the</strong> National Musculoskeletal Redesign<br />
Programme. The SGHD is supporting a major redesign <strong>of</strong> patient musculoskeletal<br />
pathways to improve services for patients, introduce more responsive and appropriate<br />
pathways, and support greater cost effectiveness across <strong>the</strong> system.<br />
The musculoskeletal umbrella<br />
Musculoskeletal conditions is a broad term encompassing around 200 different<br />
problems affecting <strong>the</strong> muscles, joints and skeleton. These conditions result in 9.5<br />
million lost working days, and currently cost <strong>the</strong> UK economy £7.4 billion a year. In<br />
Scotland back and neck pain are in <strong>the</strong> top 10 most frequent conditions seen by GPs.<br />
Forty-eight percent <strong>of</strong> work-related illness in Scotland is <strong>of</strong> MSK origin. One in four<br />
patients, over a million people in Scotland consulted <strong>the</strong>ir GP for a MSK condition<br />
last year.<br />
Disorders such as osteoarthritis and osteoporosis are becoming increasingly common<br />
as a result <strong>of</strong> an ageing population. The number <strong>of</strong> people in Scotland having hip<br />
and knee joint replacements has grown from 7,000 to 15,000 in <strong>the</strong> last 10 years.<br />
The cost in Scotland for orthopaedics has risen from £<strong>18</strong>0 million 1999/2000 to £360<br />
million in 2007/8.<br />
6<br />
mskscoping<strong>2011</strong>-rs.indd 6 03/11/<strong>2011</strong> 11:01
<strong>Joint</strong> <strong>effects</strong> <strong>2011</strong><br />
Person-centred, safe and effective<br />
The three national quality ambitions for NHSScotland clearly state that all services will<br />
be person-centred, safe and effective. Alongside this, a wide ranging and evidencebased<br />
work programme underpins <strong>the</strong> National Musculoskeletal Redesign Programme.<br />
● ● 2005 AHPs do count. The AHP Census Day demonstrated that neuro-MSK and<br />
orthopaedic patients represent 65% <strong>of</strong> <strong>the</strong> caseload <strong>of</strong> occupational <strong>the</strong>rapists,<br />
physio<strong>the</strong>rapists and podiatrists.<br />
●●<br />
●●<br />
●●<br />
2006 to 2009 National work and publications on patient self referral<br />
(www.selfreferralphysioinfo.com).<br />
2007 Co-ordinated, integrated and fit for purpose – <strong>the</strong> delivery framework for<br />
adult rehabilitation (SGHD).<br />
2009 NHS Quality Improvement Scotland (NHS QIS) published a systematic review<br />
on service delivery organisation for acute low back pain recommending that <strong>the</strong><br />
physio<strong>the</strong>rapy management <strong>of</strong> low back pain (LBP) should take account <strong>of</strong> existing<br />
evidence-based guidelines.<br />
● ● 2009 Health works, The SGHD’s Fit for Work Service will allow workers to access<br />
rapid diagnosis and referral to services for common physical and mental health<br />
conditions in a bid to reduce <strong>the</strong>ir time out <strong>of</strong> work.<br />
●●<br />
●●<br />
2009 National physio<strong>the</strong>rapy low back pain audit – Improving back care in<br />
Scotland (NHS QIS) identified that over 55,000 people each year are referred<br />
to physio<strong>the</strong>rapy with back pain. Audit cycles demonstrated improvement in<br />
recording <strong>of</strong> red and yellow flags, improving patient safety and treatment in line<br />
with best guidance.<br />
2010 Scottish backs (www.scottishbacks.co.uk) a web-based relaunch <strong>of</strong> <strong>the</strong><br />
award-winning Working Backs Scotland.<br />
●●<br />
●●<br />
●●<br />
●●<br />
●●<br />
●●<br />
2010 A national dataset <strong>of</strong> clinical outcome measures for MSK conditions. Nine<br />
measures were agreed, based on a review <strong>of</strong> <strong>the</strong> literature and pr<strong>of</strong>essional<br />
consensus. These measures will be used across Scotland.<br />
2010 The healthcare quality strategy provided reinforcement that services need to<br />
have a direct and positive impact in supporting everyone in Scotland to live longer<br />
healthier lives and to participate more productively both economically and socially.<br />
Increased effectiveness, efficiency and productivity <strong>of</strong> <strong>the</strong> health sector in Scotland<br />
will make a significant and direct contribution to economic growth. It focuses on<br />
three quality ambitions: safety, effectiveness and person centredness.<br />
2010 Realising potential, an action plan for AHPs in mental health reflected <strong>the</strong><br />
key role <strong>of</strong> rehabilitation within mental health services. This rehabilitation-focused<br />
initiative builds on <strong>the</strong> understanding that both physical health and mental<br />
wellbeing are integral to all AHP services and future healthcare provision.<br />
2010 The Evaluation report <strong>of</strong> Lothian and NHS 24’s telephone physio<strong>the</strong>rapy self<br />
referral pilot identified benefits for patients in being able to access physio<strong>the</strong>rapy<br />
via <strong>the</strong> telephone. However, in terms <strong>of</strong> sustainability and cost effectiveness, <strong>the</strong><br />
evidence for that particular operating model was less convincing.<br />
<strong>2011</strong> From strength to strength: Celebrating 10 years <strong>of</strong> <strong>the</strong> AHPs in Scotland<br />
(SGHD) identified significant developments in <strong>the</strong> MSK AHP workforce in terms <strong>of</strong><br />
<strong>the</strong>ir extended roles in diagnostics, prescribing and advanced treatments.<br />
<strong>2011</strong> Achieving sustainable quality: A 20:20 vision, most recently published by <strong>the</strong><br />
Scottish Government, clearly articulates <strong>the</strong> need for services to play <strong>the</strong>ir part in<br />
achieving sustainable quality. It also recognises <strong>the</strong> challenges healthcare will have<br />
into <strong>the</strong> future and <strong>the</strong> need for <strong>the</strong>m to be radically different. It calls on health<br />
services to be bold enough to be able to meet <strong>the</strong>se future demands in a way that<br />
is sustainable by making changes to turn vision into reality.<br />
7<br />
mskscoping<strong>2011</strong>-rs.indd 7 03/11/<strong>2011</strong> 11:01
<strong>Joint</strong> <strong>effects</strong> <strong>2011</strong><br />
The National Musculoskeletal Redesign Programme<br />
2010 – 2013: Allied Health Pr<strong>of</strong>essional <strong>involvement</strong><br />
The need for redesign was signalled within <strong>the</strong> Delivery framework for adult<br />
rehabilitation published in 2007. The framework identified that considerable<br />
improvements could be made for patients in both <strong>the</strong>ir outcome and experience <strong>of</strong><br />
Scotland’s MSK services. In particular by:<br />
●●<br />
improving access to services<br />
●●<br />
providing consistent and high quality information about <strong>the</strong>ir condition<br />
as early as possible<br />
●●<br />
providing information and advice to support self-management<br />
●●<br />
shortening waiting times<br />
●●<br />
adopting evidence-based treatment plans<br />
●●<br />
enabling people to stay in or return to work<br />
●●<br />
ensuring an equal, high quality <strong>of</strong> care across Scotland<br />
●●<br />
achieving sustainability and efficiencies to reinvest in better MSK services.<br />
There are three key work areas:<br />
1 Multi-pr<strong>of</strong>essional MSK care pathways<br />
2 A pilot using NHS 24 telephony to provide a National Advice and Triage Service to<br />
signpost to information and local MSK services.<br />
3 Embedding Working Health Services Scotland in all MSK pathways<br />
Multi-pr<strong>of</strong>essional MSK care pathways<br />
AHPs within health boards across Scotland are working as part <strong>of</strong> multidisciplinary<br />
teams, developing and introducing a range <strong>of</strong> MSK care pathways.<br />
This MSK scoping exercise demonstrates a lot <strong>of</strong> ‘pathway activity’. More is planned.<br />
Business redesign approaches are being used to modernise services and ensure<br />
patients have access to high quality, consistent information about <strong>the</strong>ir condition as<br />
soon as possible.<br />
Pathfinder Boards have focused on pathways that are based around <strong>the</strong> highest<br />
patient activity, i.e. low back pain, hip and knee problems. They have adopted a<br />
multidisciplinary approach and take a ‘patient-eye view’ <strong>of</strong> <strong>the</strong> existing service on<br />
<strong>of</strong>fer, asking <strong>the</strong> question “why” at each step <strong>of</strong> <strong>the</strong> patient journey.<br />
The aim is to reduce duplication and take steps out, so people can access <strong>the</strong> most<br />
appropriate healthcare option quickly, easily and safely.<br />
There are many more AHPs practicing in new ways, e.g. referring patients for, and<br />
acting on, diagnostic tests, prescribing medication and undertaking injections avoiding<br />
<strong>the</strong> need for ano<strong>the</strong>r GP referral. The MSK pathway programme is being supported<br />
by dedicated project management support with training for new roles and advanced<br />
practice provided through NHS Education for Scotland (NES).<br />
The National Advice and Triage Service<br />
NHS 24 is leading on <strong>the</strong> development <strong>of</strong> <strong>the</strong> national point <strong>of</strong> access to MSK services<br />
using <strong>the</strong>ir established telephony platform. The NHS 24 pilot will go live in two early<br />
adopter sites between December and January. The project will be evaluated and is due<br />
to report in early Summer 2012.<br />
The service will operate Monday to Friday, 9.00 am to 8.00 pm. Patients and those<br />
wanting access to advice and information will be encouraged to call a national<br />
number. The first person a caller will talk to will be a call operator. They will be taken<br />
through a series <strong>of</strong> questions about <strong>the</strong>ir MSK problem, covering demographic details,<br />
key safety and problem-specific questions, risk indicators and employment. Call<br />
operators follow protocols developed by MSK experts, have extensive training and<br />
clinical supervision on hand at all times.<br />
The protocol has been developed and endorsed by a national expert panel including<br />
service users and is based on <strong>the</strong> NHS 24 operating model where patient safety<br />
8<br />
mskscoping<strong>2011</strong>-rs.indd 8 03/11/<strong>2011</strong> 11:01
<strong>Joint</strong> <strong>effects</strong> <strong>2011</strong><br />
comes first. It also includes <strong>the</strong> STarT MSK screening tool under development at<br />
Current referral pathway<br />
Keele University. This assists in identifying people at low, medium or high risk <strong>of</strong><br />
experiencing persistent problems.<br />
It is anticipated that by using this approach, NHS 24 will be able to manage a<br />
proportion <strong>of</strong> callers on behalf <strong>of</strong> local AHP services, free up much needed frontline<br />
<strong>18</strong> (0) days<br />
20 (2) days<br />
68 (50) days<br />
capacity and avoid many GP appointments.<br />
Low-risk callers<br />
Advice and information resources available on<br />
<strong>the</strong> web, via digital TV and even through a smart<br />
phone application. Encouraged to call <strong>the</strong> NHS 24<br />
service back after two weeks if <strong>the</strong>ir symptoms<br />
don’t improve.<br />
Medium or high-risk callers Will be referred directly to local MSK services<br />
as well as being provided with advice and<br />
information resources.<br />
Callers with work-related issues Working Health Services and local employability<br />
services, where appropriate.<br />
Patient visits<br />
GP 1.8 times GP completes<br />
on average written or<br />
Referral<br />
before being electronic<br />
received<br />
referred to referral<br />
by local<br />
AHP service or patient<br />
AHP service,<br />
self-refers<br />
put onto<br />
waiting list<br />
Proposed referral pathway<br />
5 days<br />
Patient<br />
contacted and<br />
<strong>of</strong>fered an<br />
appointment<br />
78 (60) days<br />
Patient attends<br />
GPs will be encouraged to direct <strong>the</strong>ir patients to <strong>the</strong> new MSK line but will still<br />
Less than 40 days<br />
be able to refer directly into local services if <strong>the</strong>y feel <strong>the</strong> new phone service is not<br />
appropriate for some patients.<br />
Callers will have quick and easy access to high quality advice and information about<br />
how to manage <strong>the</strong>ir condition from Day 1 and direct referral if needed into local<br />
MSK services. This contrasts sharply with current practice. Currently, patients may<br />
need to visit a GP on more than one occasion before being referred to a local MSK<br />
service and <strong>the</strong>n face a long wait (can be around nine weeks in many services) before<br />
receiving advice or <strong>the</strong> required treatment.<br />
Patient calls<br />
NATs, is triaged<br />
and referral<br />
sent on to<br />
local MSK<br />
service<br />
Patient<br />
contacted and<br />
<strong>of</strong>fered an<br />
appointment<br />
Patient attends<br />
9<br />
mskscoping<strong>2011</strong>-rs.indd 9 03/11/<strong>2011</strong> 11:01
<strong>Joint</strong> <strong>effects</strong> <strong>2011</strong><br />
Promotional material for use by <strong>the</strong> pilot health boards Lothian and Lanarkshire<br />
10<br />
mskscoping<strong>2011</strong>-rs.indd 10 03/11/<strong>2011</strong> 11:01
<strong>Joint</strong> <strong>effects</strong> <strong>2011</strong><br />
Planned evaluation<br />
1 Safety for patients<br />
2 Acceptability to user and clinicians<br />
3 Reliability <strong>of</strong> clinical pathways and system<br />
4 Impact on GP and AHP services, costs and patient experience and outcome<br />
5 Value as a national model for o<strong>the</strong>r AHP pr<strong>of</strong>essions and morbidities<br />
Working Health Services Scotland<br />
Working Health Services Scotland (WHSS) is a Government-funded pilot scheme to<br />
treat people who are <strong>of</strong>f, or struggling to stay in, work and are employed by small and<br />
medium companies <strong>of</strong> less than 250 people. It aims to help employees remain in, or<br />
return to, work quickly after a period <strong>of</strong> absence. People can self-refer, calling 0800<br />
019 2211, and referrals are welcome from GPs, o<strong>the</strong>r health pr<strong>of</strong>essionals and partner<br />
organisations.<br />
This service will be embedded in <strong>the</strong> new MSK pathways in every health board and its<br />
impact evaluated. Opportunities to raise <strong>the</strong> pr<strong>of</strong>ile <strong>of</strong> work-related health issues and<br />
signpost people who may benefit will be part <strong>of</strong> <strong>the</strong> MSK pathway process.<br />
The programme is based on telephone-case-managed support for employees. It<br />
includes fast access to a range <strong>of</strong> <strong>the</strong>rapies and counselling services based on <strong>the</strong><br />
individuals’ needs.<br />
11<br />
mskscoping<strong>2011</strong>-rs.indd 11 03/11/<strong>2011</strong> 11:01
<strong>Joint</strong> <strong>effects</strong> <strong>2011</strong><br />
The <strong>2011</strong> Scottish AHP MSK scoping<br />
In 2005, a scoping study <strong>of</strong> <strong>the</strong> <strong>involvement</strong> <strong>of</strong> allied health pr<strong>of</strong>essions in<br />
musculoskeletal services was undertaken at <strong>the</strong> request <strong>of</strong> <strong>the</strong> Chief Pr<strong>of</strong>essions<br />
Officer <strong>of</strong> <strong>the</strong> SGHD to identify productive and creative models and used to share and<br />
learn from <strong>the</strong>se experiences. There were two publications: AHP activities in Scottish<br />
MSK services 2005 and <strong>Joint</strong> <strong>effects</strong> 2005. <strong>An</strong> <strong>update</strong> <strong>of</strong> this work was commissioned<br />
to support <strong>the</strong> National Musculoskeletal Redesign Programme. As in 2005, this work<br />
has focused primarily on <strong>the</strong> activities <strong>of</strong> three pr<strong>of</strong>essional groups and <strong>the</strong>ir support<br />
teams: occupational <strong>the</strong>rapists, physio<strong>the</strong>rapists and podiatrists although some<br />
examples from o<strong>the</strong>r AHPs have been provided and are included.<br />
Wider aims<br />
●●<br />
To promote and share practice between services and pr<strong>of</strong>essions.<br />
●●<br />
To enable <strong>the</strong> exchange <strong>of</strong> useful resources available to <strong>the</strong> public, patients<br />
and clinicians.<br />
●●<br />
To demonstrate to a wider audience <strong>the</strong> important input and impact AHPs have on<br />
MSK services in Scotland.<br />
●●<br />
To <strong>update</strong> AHP activities in Scottish MSK services 2005 to represent a snapshot <strong>of</strong><br />
AHP MSK activity in Scotland in <strong>2011</strong>.<br />
Method<br />
The <strong>update</strong> was undertaken between January <strong>2011</strong> and September <strong>2011</strong>. A database<br />
<strong>of</strong> AHP contacts was developed and all AHP directors in every board were notified<br />
by email and at <strong>the</strong>ir monthly meetings. A template was developed and circulated<br />
widely by email. Summaries for publication were agreed and recirculated. There were<br />
a few, but not many, follow-up phone interviews for clarification. AHP directors were<br />
circulated twice with <strong>the</strong> full database reports in confidence.<br />
Findings<br />
As to be expected, <strong>the</strong>re have been considerable developments in both services<br />
and practice. Boards have clearly been using <strong>the</strong> three quality ambitions to drive<br />
improvements. Developments have been found in a range <strong>of</strong> areas, notably:<br />
Patient <strong>involvement</strong> in service development and quality assessment is much more<br />
common. Patient focus groups, video diaries and feedback and even <strong>the</strong> use <strong>of</strong> a<br />
patient postbox have made it easier to listen to patients’ views on AHP services.<br />
Self referral is widely available and in some health boards <strong>the</strong>re is nearly 100%<br />
coverage for community AHP services. In o<strong>the</strong>r boards it is patchier. However it<br />
is still disappointing that only a few services really market this to patients. With<br />
some exceptions, finding information on Scotland’s AHP MSK services requires an<br />
understanding <strong>of</strong> <strong>the</strong> structure <strong>of</strong> healthcare and quite complex use <strong>of</strong> web search<br />
engines. Self referral forms can be found but it is not always easy.<br />
Drop-in clinics and a wide range <strong>of</strong> appointment times with evening clinics are<br />
<strong>of</strong>fered by a number <strong>of</strong> services. Some more specialised services have moved out into<br />
<strong>the</strong> community.<br />
Patient pre-assessment forms, self completion questionnaires and screening<br />
tools are clearly being used more. Follow-up is also common, ei<strong>the</strong>r by use <strong>of</strong> a<br />
phone call post discharge, or a postal questionnaire including a range <strong>of</strong> outcome<br />
measures.<br />
National agreement for MSK clinical outcome measures achieved in 2010 should<br />
lead to increased use <strong>of</strong> validated measures. However, converting individual patient<br />
clinical outcome measures (PROMs and PREMs) more widely to demonstrate wholeservice<br />
impacts and improvements is still quite unusual.<br />
12<br />
mskscoping<strong>2011</strong>-rs.indd 12 03/11/<strong>2011</strong> 11:01
<strong>Joint</strong> <strong>effects</strong> <strong>2011</strong><br />
There is much greater standardisation <strong>of</strong> assessment and referral forms across<br />
many health boards and more patient information provided although <strong>the</strong> extent and<br />
content varies.<br />
There has been a lot <strong>of</strong> pathway and redesign development, which continues as<br />
part <strong>of</strong> <strong>the</strong> current National MSK Redesign Programme.<br />
The regular use <strong>of</strong> systems and technology to support patient care still remains<br />
highly variable. Some services have, and make good use <strong>of</strong>, legacy systems. O<strong>the</strong>rs<br />
have built <strong>the</strong>ir own databases to support quality improvements but <strong>the</strong>re are still<br />
many services that are dependent on paper for <strong>the</strong> retrieval <strong>of</strong> patient outcomes.<br />
Many but not all have access to e-GP referrals and some specialised services are using<br />
e-vetting very successfully.<br />
The lack <strong>of</strong> systems and diary management can only hamper flexible and adaptable<br />
service development, however some services have effectively used <strong>of</strong>f-<strong>the</strong>-shelf<br />
products as an interim measure.<br />
Advanced AHP practice in partnership with o<strong>the</strong>r clinicians forms <strong>the</strong> basis for many<br />
services. Most services are delivered within community settings, health centres and<br />
community hospitals. Ensuring advanced practice is integrated into normal services<br />
and not seen a ‘stand-alone’ is clearly a current development in some boards. The<br />
use <strong>of</strong> injection <strong>the</strong>rapy is now widespread throughout physio<strong>the</strong>rapy and podiatry in<br />
Scotland and in some places available within every service.<br />
Increasing links to exercise and better integration <strong>of</strong> work, health and leisure are<br />
evident; some boards lead <strong>the</strong> way in this. Staff skill mix has been adjusted to include<br />
exercise and fitness pr<strong>of</strong>essionals within <strong>the</strong> traditional healthcare team. There are also<br />
examples <strong>of</strong> exercise classes being targeted at particular populations and links with<br />
<strong>the</strong> voluntary sector to deliver patient-led group activity.<br />
In <strong>the</strong> hospital sector <strong>the</strong> use <strong>of</strong> education classes in preparation for planned joint<br />
replacement surgery is becoming widespread.<br />
Conclusion<br />
Scotland has led <strong>the</strong> world in permitting and promoting self referral to AHP services,<br />
this approach now underpins Scottish Government Policy, but many AHP services are<br />
still quite difficult to find on <strong>the</strong> internet. How patients and <strong>the</strong> public learn about self<br />
referral is also difficult to judge. The NHS 24 pilot may assist with this.<br />
AHPs are in a unique position to support and promote Scottish policies on working<br />
health, and assist as many people to stay at work, or return to work as soon as<br />
possible. More needs to be done to establish links with leisure services and to be<br />
effective advocates for physical activity and public health.<br />
Services will have to demonstrate <strong>the</strong>y are not only effective and efficient but that<br />
<strong>the</strong>y add value. The national approach to consistent outcome measurement will<br />
support this.<br />
There continues to be variation in <strong>the</strong> delivery and management <strong>of</strong> musculoskeletal<br />
services between and within individual health boards in Scotland. This is also<br />
confirmed by The Arthritis and Musculoskeletal Alliance (ARMA)’s Musculoskeletal<br />
Map <strong>of</strong> Scotland due for publication later this year.<br />
It will be important that <strong>the</strong> good practice identified in this report and <strong>the</strong><br />
opportunities <strong>of</strong>fered by <strong>the</strong> National MSK Redesign Programme are used<br />
to reduce variation and continue to drive improvements in <strong>the</strong> quality <strong>of</strong><br />
musculoskeletal services for <strong>the</strong> people <strong>of</strong> Scotland.<br />
13<br />
mskscoping<strong>2011</strong>-rs.indd 13 03/11/<strong>2011</strong> 11:01
<strong>Joint</strong> <strong>effects</strong> <strong>2011</strong><br />
14<br />
mskscoping<strong>2011</strong>-rs.indd 14 03/11/<strong>2011</strong> 11:01
<strong>Joint</strong> <strong>effects</strong> <strong>2011</strong><br />
13<br />
Summary <strong>of</strong> MSK services<br />
All entries have been submitted and agreed by contributors. They are backed up<br />
by more detailed information which will be released as a PDF file to AHP managers<br />
and contributors. Many services have <strong>of</strong>fered to share <strong>the</strong>ir existing resources. The<br />
overview table is to help you find your way around <strong>the</strong> entries and to prompt <strong>the</strong><br />
sharing <strong>of</strong> ideas and existing resources.<br />
1 NHS Ayrshire and Arran 20<br />
12<br />
2 NHS Borders 22<br />
3 NHS Dumfries and Galloway 23<br />
4 NHS Fife 25<br />
15<br />
5 NHS Forth Valley 27<br />
8<br />
6<br />
6 NHS Grampian 29<br />
7 NHS Greater Glasgow and Clyde 31<br />
8 NHS Highland 35<br />
9 NHS Lanarkshire 36<br />
5<br />
14<br />
4<br />
10 NHS Lothian 38<br />
11 NHS National Waiting Times Centre 39<br />
11<br />
1<br />
7<br />
3<br />
9<br />
10<br />
2<br />
12 NHS Orkney 40<br />
13 NHS Shetland 42<br />
14 NHS Tayside 42<br />
15 NHS Western Isles 45<br />
15<br />
mskscoping<strong>2011</strong>-rs.indd 15 03/11/<strong>2011</strong> 11:01
<strong>Joint</strong> <strong>effects</strong> <strong>2011</strong><br />
Overview<br />
NHS Ayrshire and Arran<br />
Patient <strong>involvement</strong><br />
Access: evening, one stop<br />
Self referral<br />
Pathways and redesign<br />
Systems and technology<br />
Advanced practice<br />
Injection<br />
Outcomes<br />
Demonstrate value<br />
Exercise, work and health<br />
Pre-assesment, screening and follow up<br />
AHP Board Lead on MSK Redesign ● ● ● ● ● ● judith.reid@aapct.scot.nhs.uk<br />
AHP Electronic Diary Management ● billy.mcclean@nhs.net<br />
AHP Low Back Pain Pathway ● ● ● ● ● ● ● ● judith.reid@aapct.scot.nhs.uk<br />
AHP Orthopaedic Services ● ● carol.kirk@aaaht.scot.nhs.uk<br />
AHP Pain Services ● ● arlene.sloan@aapct.scot.nhs.uk<br />
Counterweight Programme ● ● ● carolyn.paton@aapct.scot.nhs.uk<br />
Occupational Therapy Hand Service ● gillian.cowan@aaaht.scot.nhs.uk<br />
Physio<strong>the</strong>rapy Service ● ● billy.mcclean@nhs.net<br />
Podiatry Service ● ● ● ● ● ● helen.jackson@aapct.scot.nhs.uk<br />
Service Redesign in Orthotics ● ● ● colin.keith@aapct.scot.nhs.uk<br />
NHS Borders<br />
Musculoskeletal Physio<strong>the</strong>rapy in 13 locations ● ● ● ● maggie.stobie@borders.scot.nhs.uk<br />
Podiatry Service ● ● pamela.gordon@borders.scot.nhs.net<br />
NHS Dumfries and Galloway<br />
Back Pain Service ● ● ● ● ● ann.grant@nhs.net<br />
Dumfries and Galloway Royal Infirmary Physio<strong>the</strong>rapy Department ● sherylreason@nhs.net<br />
Dumfries and Galloway-East Physio<strong>the</strong>rapy ● ● ● amanda.hall@nhs.net<br />
Electronic Triage <strong>of</strong> orthopaedic GP referrals by lead podiatrist helps waiting times ● ● neil.malcolm@nhs.net<br />
NHS Fife<br />
Fife Physio<strong>the</strong>rapy Service ● ● ● ● ● ● ● ● grant.syme1@nhs.net<br />
Fife Podiatric Learning Disability Service ● ● ● karen.hutt@nhs.net<br />
Hand Therapy Team ● sheilamclellan@nhs.net<br />
Integrated Pain Management Service ● ● melanie.hutchison@nhs.net<br />
16<br />
mskscoping<strong>2011</strong>-rs.indd 16 03/11/<strong>2011</strong> 11:01
Patient <strong>involvement</strong><br />
Access: evening, one stop<br />
Self referral<br />
Pathways and redesign<br />
Systems and technology<br />
Pre-assesment, screening and follow up<br />
Advanced practice<br />
Injection<br />
Outcomes<br />
Demonstrate value<br />
Exercise, work and health<br />
Orthopaedic Foot and <strong>An</strong>kle Service ● ● carolyntodd@nhs.net<br />
Podiatry Musculoskeletal (Biomechanics) Service ● ● ● ● ● ● ● ● carolyntodd@nhs.net<br />
Rheumatology Podiatry ● ● ● adele.osborne@nhs.net<br />
Rheumatology ● ● janet.harkess@nhs.net<br />
NHS Forth Valley<br />
Extended Scope Practitioner Clinics in Orthopaedics ● ● ● ● ● lesleydawson@nhs.net<br />
Forth Valley Back Pain Service and Exercise Classes ● ● ● ● ● ● nturvill@nhs.net<br />
Forth Valley Physio<strong>the</strong>rapy ● ● ● ● ● catriona.phin@nhs.net<br />
Occupational Therapy for In-patients ● rosina.mcguire@nhs.net<br />
Orthotic Services (Open Referral) ● ● ● lynne.rowley@nhs.net<br />
Podiatry Service ● ● ● gordon.mclay@nhs.net<br />
Rheumatology ESP Clinics ● ● anitacarr@nhs.net<br />
Rheumatology Occupational Therapy ● rosina.mcguire@nhs.net<br />
NHS Grampian<br />
Elective Orthopaedics Occupational Therapy ● ● ● eve.cruickshank@nhs.net<br />
Grampian Physio<strong>the</strong>rapy Services ● ● ● ● ● ● lynn.morrison @nhs.net<br />
Moray Occupational Therapy ● ● ● judith.fairburn@nhs.net<br />
<strong>Joint</strong> <strong>effects</strong> <strong>2011</strong><br />
Orthopaedic Rehabilitation Unit<br />
eve.cruickshank@nhs.net<br />
Orthotics Services ● ● steven.lindsay@nhs.net<br />
Rheumatology ● f.mccurdy@nhs.net<br />
Supported Discharge Service Stroke and Trauma Orthopaedics ● ● ● beththomson@nhs.net<br />
NHS Greater Glasgow and Clyde<br />
Call Centre Access and evening clinics popular with patients ● ● ● paul.higgins@ggc.scot.nhs.uk<br />
Community Physio<strong>the</strong>rapy Services. Out-patient musculoskeletal services – Renfrewshire CHP ● ● ● ● elizabeth.lightbody@ggc.scot.nhs.uk<br />
ESP Orthopaedic Foot and <strong>An</strong>kle Triage Service ● ● ● paul.higgins@ggc.scot.nhs.uk<br />
MSK Physio<strong>the</strong>rapy Service Review ● ● ● ● hea<strong>the</strong>r.cameron@ggc.scot.nhs.uk<br />
MSK Outcome Measure Pr<strong>of</strong>orma ● ● karen.glass@ggc.scot.nhs.uk<br />
17<br />
mskscoping<strong>2011</strong>-rs.indd 17 03/11/<strong>2011</strong> 11:01
<strong>Joint</strong> <strong>effects</strong> <strong>2011</strong><br />
Patient <strong>involvement</strong><br />
Access: evening, one stop<br />
Self referral<br />
Pathways and redesign<br />
Systems and technology<br />
Advanced practice<br />
Injection<br />
Outcomes<br />
Demonstrate value<br />
Exercise, work and health<br />
Pre-assesment, screening and follow up<br />
One Stop Rheumatology Foot Service – a partnership with Glasgow Caledonian University. ● ● ● ● ● mhairi.brandon@ggc.scot.nhs.uk<br />
Pain Services ● aline.williams@ggc.scot.nhs.uk<br />
Practice Development: laser, <strong>the</strong>rapy, dry needling, deep enucleation, surgery<br />
and steroid injections<br />
● ● ● ● paul.higgins@ggc.scot.nhs.uk<br />
Practice Innovations: patient stories, videos, phone follow up and <strong>the</strong> CARE measure ● ● karen.glass@ggc.scot.nhs.uk<br />
Rehabilitation Service – Glasgow City Community Health ● ● ● ● paul.higgins@ggc.scot.nhs.uk<br />
Training for Financial Inclusion and Employability ● ● hea<strong>the</strong>r.cameron@ggc.scot.nhs.uk<br />
NHS Highland<br />
Easter Ross Orthopaedic Triage Pilot ● ● ● ● sue.king6@nhs.net<br />
Hand Therapy and Splinting Service ● karen.tolmie@nhs.net<br />
Hand Therapy for Orthopaedics ● lindacurrie@nhs.net<br />
Mid CHP Podiatry ● roderick.wells@nhs.net<br />
South East Highland CHP Podiatry Service ● michael.gates@nhs.net<br />
NHS Lanarkshire<br />
Extended Scope Practitioner Service in Orthopaedic Out-patients ● ● ● ● ● janie.thomson@lanarkshire.scot.nhs.uk<br />
Low Back Pain Physio<strong>the</strong>rapy Pathway ● ● ● ● ● christine.mccallum@lanarkshire.scot.nhs.uk<br />
Physio<strong>the</strong>rapy Assessment Line ● ● ● ● ● ● ruth.currie@lanarkshire.scot.nhs.uk<br />
Podiatry Biomechanics Service ● ● ● jim.logan@lanarkshire.scot.nhs.uk<br />
NHS Lothian<br />
East and Midlothian Physio<strong>the</strong>rapy Service ● ● ● ● ● brian.brockie@nhslothian.scot.nhs.uk<br />
Edinburgh Community Physio<strong>the</strong>rapy Service ● ● ● ● ● eddie.balfour@nhslothian.scot.nhs.uk<br />
Foot and <strong>An</strong>kle, Orthopaedic Clinic ● ● ● ● ● colin.thomson@luht.scot.nhs.uk<br />
Podiatry Biomechanics Clinic (Edinburgh, East Lothian and Midlothian) ● ● william.mcmurrich@nhslothian.scot.nhs.uk<br />
Spinal Practitioner Support to Orthopaedic Spinal Service ● ● vivienne.boyd@luht.scot.nhs.uk<br />
West Lothian Musculoskeletal Service ● ● ● ● orla.crummey@nhslothian.scot.nhs.uk<br />
NHS National Waiting Times Centre<br />
Innovations in Orthopaedics ● birgit.clark@gjnh.scot.nhs.uk<br />
MSK Physio<strong>the</strong>rapist in Occupational Health and Orthopaedic Out-patients ● ● ● ● kathryn.macpherson@gjnh.scot.nhs.uk<br />
<strong>18</strong><br />
mskscoping<strong>2011</strong>-rs.indd <strong>18</strong> 03/11/<strong>2011</strong> 11:01
Patient <strong>involvement</strong><br />
Access: evening, one stop<br />
Self referral<br />
Pathways and redesign<br />
Systems and technology<br />
Pre-assesment, screening and follow up<br />
Advanced practice<br />
Injection<br />
Outcomes<br />
Demonstrate value<br />
Exercise, work and health<br />
Elective Orthopaedic Surgery ● ● ● ● birgit.clark@gjnh.scot.nhs.uk<br />
NHS Orkney<br />
MSK Orthopaedic Triage Service ● ● paula.hemsley@nhs.net<br />
Musculoskeletal Pathways, Balfour Hospital ● ● peter.mackellar@nhs.net<br />
Occupational Health, pre-employment assessment and return to work ● ● lesley.platford@nhs.net<br />
Rheumatology Telemedicine Link Clinic ● ● lesley.platford@nhs.net<br />
Video Capture Gait <strong>An</strong>alysis ● ● richard.bailey2@nhs.net<br />
NHS Shetland<br />
Musculoskeletal Podiatry Service ● ● ● ● ● ● bruce.mcculloch@nhs.net<br />
Occupational Therapy Service ● ● ● duty.ot@shetland.gov.uk<br />
NHS Tayside<br />
Advanced Physio<strong>the</strong>rapy Practitioner and GPwSi, MSK Primary Care Triage Service ● ● ● ● janice.mcnee@nhs.net<br />
Injection Therapy Expansion ● ● ● ● ● ● janice.mcnee@nhs.net<br />
Musculoskeletal Out-patient Services – General ● ● ● ● ● angelamurphy@nhs.net<br />
Lower Limb Biomechanics Clinic ● ● mikeblack@nhs.net<br />
Orthopaedic Screening in Secondary care ● ● ● janice.mcnee@nhs.net<br />
Rheumatology ● ● ● ● ● alisonknight@nhs.net<br />
Trauma and Elective Hand Clinics ● ● ● sarah.dalgleish@nhs.net<br />
Virtual Ward (Community Rehabilitation) ● ● ● denise.connon@nhs.net<br />
Working Health Services ● ● ● ● ● ● cathy.grieve@nhs.net<br />
NHS Western Isles<br />
Musculoskeletal Physio<strong>the</strong>rapy, class-based exercise groups ● ● ● ● sheila.nicolson@nhs.net<br />
Self Referral Clinic at <strong>the</strong> Physio<strong>the</strong>rapy Department ● ● ● nico.groenendijk@nhs.net<br />
Physio<strong>the</strong>rapy Services across Western Isles ● ● ● ● ● ● ● ● nico.groenendijk@nhs.net<br />
Podiatry Musculoskeletal Service – Western Isles ● ● smacphee1@nhs.net<br />
<strong>Joint</strong> <strong>effects</strong> <strong>2011</strong><br />
19<br />
mskscoping<strong>2011</strong>-rs.indd 19 03/11/<strong>2011</strong> 11:01
<strong>Joint</strong> <strong>effects</strong> <strong>2011</strong><br />
Service descriptions<br />
NHS Ayrshire and Arran<br />
AHP Board Lead on MSK Redesign<br />
Judith Reid<br />
judith.reid@aapct.scot.nhs.uk<br />
AHP Electronic Diary Management<br />
Billy McClean<br />
billy.mcclean@nhs.net<br />
01563 827197<br />
AHP Low Back Pain Pathway<br />
Judith Reid<br />
judith.reid@aapct.scot.nhs.uk<br />
AHP Orthopaedic Services<br />
Carol Kirk<br />
carol.kirk@aaaht.scot.nhs.uk<br />
01563 827126<br />
The MSK redesign board was established in October 2010. Phase 1, low back pain pathway<br />
was successfully implemented in April <strong>2011</strong>, with hand pathway going live in November <strong>2011</strong><br />
and o<strong>the</strong>r pathways (hip, knee, shoulder and foot/ankle) through 2012. In line with <strong>the</strong> quality<br />
strategy, several measures will capture effectiveness, safety and patient centredness. EQ5D5L<br />
is being used as a continuous measure for all MSK conditions. The STarT tools help inform <strong>the</strong><br />
management approach, with o<strong>the</strong>r measures, e.g. HADS, informing exit routes. Survey and<br />
focus group evaluation <strong>of</strong> both staff and patient perception is in place with snapshot evaluation<br />
using CARE measure. Project documents are available.<br />
Centralised management <strong>of</strong> MS Outlook diaries has been introduced across Physio<strong>the</strong>rapy<br />
as a stepping stone to a bespoke electronic patient management system. This has improved<br />
efficiency and productivity with a reduction <strong>of</strong> unfilled slots and reduction in assistant and<br />
clinical time used to manage diaries across peripheral sites. Trackcare PMS will be used to<br />
manage diaries centrally across AHP MSK services once <strong>the</strong> redesign is complete and IT solutions<br />
have been implemented.<br />
The low back pain pathway was implemented in April <strong>2011</strong> as <strong>the</strong> first pathway within <strong>the</strong><br />
overarching MSK redesign in line with <strong>the</strong> Government vision. GPs refer electronically through a<br />
single point <strong>of</strong> contact to access community-based AHP services. A robust process <strong>of</strong> escalation<br />
utilises community-based MSK ESPs (who also work in orthopaedics) to access diagnostic<br />
investigations and refer directly to secondary care as required.<br />
OT and Physio<strong>the</strong>rapy provide services to those undergoing elective and trauma orthopaedic<br />
surgery. Elective THJR patients have a pre-admission visit by <strong>the</strong> orthopaedic TI and are reviewed<br />
by <strong>the</strong> TI on <strong>the</strong> ward post surgery. TKJR patients attend a pre-op joint school (Crosshouse only)<br />
as part <strong>of</strong> <strong>the</strong> Rapid Recovery Programme. The MDT ensure timely and safe discharge home.<br />
Outreach domiciliary visits are carried out where necessary. <strong>An</strong> OA knee pathway delivers OT<br />
and physio<strong>the</strong>rapy rehabilitation to avoid surgical intervention. These services will be reviewed<br />
as part <strong>of</strong> <strong>the</strong> MSK redesign.<br />
20<br />
mskscoping<strong>2011</strong>-rs.indd 20 03/11/<strong>2011</strong> 11:01
<strong>Joint</strong> <strong>effects</strong> <strong>2011</strong><br />
AHP Pain Services<br />
Arlene Sloan<br />
arlene.Sloan@aapct.scot.nhs.uk<br />
Counterweight Programme<br />
Carolyn Paton<br />
carolyn.paton@aapct.scot.nhs.uk<br />
Occupational Therapy Hand Service<br />
Gillian Cowan<br />
gillian.cowan@aaaht.scot.nhs.uk<br />
01563 827126<br />
Physio<strong>the</strong>rapy Service<br />
Billy McClean<br />
billy.mcclean@nhs.net<br />
01563 827197<br />
Chronic Pain services across Ayrshire are managed through anaes<strong>the</strong>tics. <strong>An</strong> MCN is being<br />
established as part <strong>of</strong> <strong>the</strong> MSK redesign. Work has begun on development <strong>of</strong> a physio<strong>the</strong>rapyled<br />
Level 1 pain management programme. <strong>An</strong> initial programme <strong>of</strong> staff education is underway<br />
with delivery <strong>of</strong> service scheduled from April 2012. Collaborative working with Working Health<br />
Services, Mental Health and Leisure Services is ongoing and will fur<strong>the</strong>r enhance management<br />
options.<br />
Dietetics provide support, education and advice to patients and clinicians through <strong>the</strong> Ayrshire<br />
wide Counterweight programme. The programme provides weight-loss support and nutritional<br />
advice to those who are overweight. This approach is embedded within <strong>the</strong> OA knee and spinal<br />
pathways and will be extended as part <strong>of</strong> <strong>the</strong> MSK redesign.<br />
Hand <strong>the</strong>rapy (Crosshouse only) is provided to in/out-patients following trauma/elective<br />
surgery. <strong>An</strong> Extended Role Hand Clinic is held by <strong>the</strong> Senior Occupational Therapist to review<br />
patients post operatively. Hand <strong>the</strong>rapy is also provided one evening per week. OT also<br />
provides a service for Rheumatology patients at Ayr & Crosshouse and attend a ‘one stop’<br />
Multidisciplinary Inflammatory <strong>Joint</strong> Disease Clinic held at Heathfield Clinic and Ayrshire Central<br />
Hospital.<br />
Physio<strong>the</strong>rapy services across primary and secondary care, with specialist services in<br />
rheumatology, hands, hydro<strong>the</strong>rapy and extended scope roles in orthopaedics. Referral systems<br />
in place from physio<strong>the</strong>rapy to orthopaedic services. Injection <strong>the</strong>rapy provided throughout<br />
<strong>the</strong> physio<strong>the</strong>rapy service and combined clinics (ESP’s and clinical specialists) enabling fur<strong>the</strong>r<br />
investigation as required. Core contributor to low back pain pathway.<br />
21<br />
mskscoping<strong>2011</strong>-rs.indd 21 03/11/<strong>2011</strong> 11:01
<strong>Joint</strong> <strong>effects</strong> <strong>2011</strong><br />
Podiatry Service<br />
Helen Jackson<br />
helen.jackson@aapct.scot.nhs.uk<br />
MSK Podiatry Service accepts self referrals, GP, physio, consultant and o<strong>the</strong>r AHP referrals.<br />
A team <strong>of</strong> specialists provide assessment, diagnosis and treatment for children and adults<br />
presenting with MSK conditions. Three team members carry out foot and ankle steroid<br />
injections and a fur<strong>the</strong>r three staff input to <strong>the</strong> multidisciplinary inflammatory joint disease<br />
clinics. Special provision is made for diabetic patients who require ‘<strong>of</strong>f-loading’ bespoke devices.<br />
Functional orthoses, both bespoke and <strong>of</strong>f <strong>the</strong> shelf, are provided by clinicians with technical<br />
support. A foot and ankle MSK pathway is currently being developed which it is hoped will<br />
improve access to imaging, bloods and orthopaedics.<br />
Outcome measures: audit, VAS. Plan to start using <strong>the</strong> Manchester and Oxford foot pain scale.<br />
Service Redesign in Orthotics<br />
Colin Keith<br />
colin.keith@aapct.scot.nhs.uk<br />
NHS Borders<br />
Musculoskeletal Physio<strong>the</strong>rapy in 13 locations<br />
Maggie Stobie and May Sharp<br />
maggie.stobie@borders.scot.nhs.uk<br />
may.sharp@borders.scot.nhs.uk<br />
0<strong>18</strong>96 826545<br />
Orthotics provide services across Ayrshire but currently can only be accessed through<br />
Orthopaedics. Referral pathways to Orthotics are being reviewed as part <strong>of</strong> <strong>the</strong> MSK redesign to<br />
allow direct access for GPs and o<strong>the</strong>r AHPs and an email triage system set up. Over 60% <strong>of</strong> <strong>the</strong><br />
service caseload involves treatment <strong>of</strong> foot and ankle conditions. <strong>Joint</strong> working with Podiatry in<br />
treatment <strong>of</strong> diabetic and rheumatoid conditions has been established toge<strong>the</strong>r with ongoing<br />
clinics in Paediatrics and LDS with Physio<strong>the</strong>rapy.<br />
Physio<strong>the</strong>rapy is delivered at 13 locations and all accept self referral. The orthopaedic ESP<br />
includes a multidisciplinary team providing effective assessment <strong>of</strong> <strong>the</strong> routine orthopaedic<br />
out-patient waiting list at <strong>the</strong> Borders General Hospital and creates effective management <strong>of</strong><br />
non-surgical cases. The patient pathway through triage has run since 2008 with future plans to<br />
introduce <strong>the</strong> service into primary care settings.<br />
The Physio<strong>the</strong>rapy Spinal Service has implemented evidence-based guidelines for both primary<br />
and secondary care. They treat and manage complex spinal patients and those triaged from<br />
<strong>the</strong> orthopaedic waiting list. The recently launched hip and knee school is part <strong>of</strong> <strong>the</strong> enhanced<br />
recovery programme, set up to reduce patient length <strong>of</strong> stay in hospital. Patients are seen before<br />
<strong>the</strong>ir operation for an hour-long education and exercise class, <strong>the</strong> classes are run jointly with<br />
occupational <strong>the</strong>rapy, enabling home requirements to be assessed and relevant equipment<br />
delivered prior to <strong>the</strong>ir operation.<br />
22<br />
mskscoping<strong>2011</strong>-rs.indd 22 03/11/<strong>2011</strong> 11:01
<strong>Joint</strong> <strong>effects</strong> <strong>2011</strong><br />
Musculoskeletal Physio<strong>the</strong>rapy in 13 locations<br />
Continued<br />
Podiatry Service<br />
Pamela Gordon<br />
pamela.gordon@borders.scot.nhs.net<br />
NHS Dumfries and Galloway<br />
Back Pain Service<br />
<strong>An</strong>n Grant<br />
ann.grant@nhs.net<br />
O<strong>the</strong>r services include dedicated physio<strong>the</strong>rapy time for MSK referrals from <strong>the</strong> Occupational<br />
Health Service and a multidisciplinary Rheumatology team working across primary and<br />
secondary care. MSK patients also have access to hydro<strong>the</strong>rapy. The chronic pain management<br />
team includes OT and Physio<strong>the</strong>rapy working on assessment and management <strong>of</strong> patients<br />
including education and self-management programmes.<br />
The Podiatry Service aims to deliver care to patients as near to <strong>the</strong>ir home as possible through<br />
basing staff in local health centres and all accept self referral. NHS Borders covers a large<br />
geographical area and provides a range <strong>of</strong> primary and secondary care and mental health<br />
services to a population <strong>of</strong> 107,000. The rurality <strong>of</strong> <strong>the</strong> area and <strong>the</strong> dispersed nature <strong>of</strong> <strong>the</strong><br />
population are key issues in <strong>the</strong> delivery <strong>of</strong> healthcare. There is an MSK podiatry service and<br />
orthopaedic triage service based at Borders General Hospital five days per week. This service<br />
sees patients on referral from GPs, consultants and o<strong>the</strong>r healthcare pr<strong>of</strong>essionals.<br />
The service was implemented to triage all patients referred to Orthopaedics with neck, thoracic<br />
and low back pain, directing <strong>the</strong>m for appropriate treatment and investigations and providing<br />
GPs with options for future management <strong>of</strong> symptoms. The team is also working with Pain<br />
Association Scotland to establish a service for those with chronic pain. A knee pathway is under<br />
development.<br />
Improvements: reduction in requests for MRI for back problems and those referred for surgical<br />
intervention.<br />
Outcome measures: Oswestry Disability Index,VAS HAD scores and self-efficacy questionnaire,<br />
DAPOS.<br />
Dumfries and Galloway Royal Infirmary Physio<strong>the</strong>rapy Department<br />
Sheryl Reason<br />
sherylreason@nhs.net<br />
Assessment and treatment <strong>of</strong> all out-patients with orthopaedic pre- and post-operative<br />
conditions. Patients are referred via consultants, GPs or through self referral. Rheumatology<br />
conditions are assessed and treated in a one-stop multidisciplinary clinic. A joint podiatry and<br />
physio<strong>the</strong>rapy clinic is held for those with biomechanical problems. MSK rehabilitation is carried<br />
out in a gym setting.<br />
23<br />
mskscoping<strong>2011</strong>-rs.indd 23 03/11/<strong>2011</strong> 11:01
<strong>Joint</strong> <strong>effects</strong> <strong>2011</strong><br />
Dumfries and Galloway-East Physio<strong>the</strong>rapy<br />
Amanda Hall<br />
amanda.hall@nhs.net<br />
01387 244402<br />
Accept GP, consultant and self referrals. <strong>Joint</strong> injection service provided by PT at three sites.<br />
Involved in shoulder pathway project. Services are co-located with GPs with well established<br />
partnership working, e.g. PTs attend weekly meetings with GPs at Lockerbie Health Centre.<br />
Links with sport and leisure services in parts <strong>of</strong> region – exercise referral scheme.<br />
4,812 new patients were seen last year and <strong>the</strong>re has been a change in skill mix to provide an<br />
increase in administrative support in order to release clinicians’ time.<br />
Electronic Triage <strong>of</strong> orthopaedic GP referrals by lead podiatrist<br />
helps waiting times<br />
Neil Malcolm<br />
neil.malcolm@nhs.net<br />
01387 244414<br />
The Podiatry Department provides a region-wide lower limb musculoskeletal service in a variety<br />
<strong>of</strong> settings and is staffed by a lead MSK podiatrist and three part-time specialist podiatrists.<br />
Assessment and treatment is provided as near people’s home as possible.<br />
All podiatrists carry out basic biomechanical assessments and insole manufacture, and have to<br />
access <strong>the</strong> PACS imaging system.<br />
The service accepts referrals from all healthcare pr<strong>of</strong>essionals but does not accept self referrals<br />
at this time. <strong>Joint</strong> assessments with paediatric and adult physio<strong>the</strong>rapists are available when<br />
necessary.<br />
The lead MSK podiatrist is able to triage orthopaedic referrals from GPs electronically. Patients<br />
see <strong>the</strong> appropriate clinician first time which helps to reduce orthopaedic waiting times.<br />
Treatments <strong>of</strong>fered include advice, exercises, orthotic <strong>the</strong>rapy and injection <strong>the</strong>rapy. The majority<br />
<strong>of</strong> orthoses supplied to patients are manufactured in-house with a small number receiving<br />
preformed devices.<br />
24<br />
mskscoping<strong>2011</strong>-rs.indd 24 03/11/<strong>2011</strong> 11:01
<strong>Joint</strong> <strong>effects</strong> <strong>2011</strong><br />
NHS Fife<br />
Fife Physio<strong>the</strong>rapy Service<br />
Grant Syme<br />
grant.syme1@nhs.net<br />
01592 717828<br />
The service operates across <strong>the</strong> two District General Hospitals and <strong>the</strong> three Community Health<br />
Partnerships. The musculoskeletal service is provided through consultant and GP referrals,<br />
both in hospital and in community locations throughout Fife. Whilst <strong>the</strong>re are four discrete<br />
management units, <strong>the</strong> service aims to provide people with seamless access to physio<strong>the</strong>rapy.<br />
Self referral is available at one site. Back Pain Redesign reduced costs and found that 90% <strong>of</strong><br />
patients could be independently managed by <strong>the</strong> consultant physio<strong>the</strong>rapist in <strong>the</strong> first instance.<br />
Outcomes in use: EUROQOL, Oswestry Pain Disability Index, Patient Satisfaction, Visual<br />
<strong>An</strong>alogue Pain Scale, Global Change Patient Rating.<br />
Fife Podiatric Learning Disability Service<br />
Karen Hutt and Dorothy Hathaway<br />
karen.hutt@nhs.net<br />
01383 565307<br />
The service provides a comprehensive MSK service to all patients with a learning disability who<br />
have a biomechanical need. This includes biomechanical assessment, gait analysis and recording,<br />
physical <strong>the</strong>rapy treatments including laser and acupuncture, footwear assessments and referral<br />
to Orthopaedic as required, casting and supplying <strong>of</strong> appropriate orthotics. Carers are advised<br />
on exercise regimes and postural management. <strong>Joint</strong> team working is undertaken with <strong>the</strong><br />
learning disciplinary team, in particular joint clinics with physio<strong>the</strong>rapy. There is a specific service<br />
for people with Down’s syndrome.<br />
All people with Down’s syndrome in Fife are <strong>of</strong>fered an assessment at <strong>the</strong> clinic where<br />
representatives from <strong>the</strong> multidisciplinary team assess <strong>the</strong>ir needs. The team consists <strong>of</strong> podiatry,<br />
physio<strong>the</strong>rapy, occupation <strong>the</strong>rapy, nursing, psychology, speech and language <strong>the</strong>rapy and<br />
dietetics. Currently all individuals seen at <strong>the</strong> clinic with a podiatry biomechanical need have<br />
been supplied an appropriate orthotic device and are followed up as required.<br />
25<br />
mskscoping<strong>2011</strong>-rs.indd 25 03/11/<strong>2011</strong> 11:01
<strong>Joint</strong> <strong>effects</strong> <strong>2011</strong><br />
Hand Therapy Team<br />
Sheila McLellan<br />
sheilamclellan@nhs.net<br />
01592 643355 ext. 23690<br />
Integrated Pain Management Service<br />
Melanie Hutchison<br />
melanie.hutchison@nhs.net<br />
01383 623623<br />
Orthopaedic Foot and <strong>An</strong>kle Service<br />
Carolyn Todd<br />
carolyntodd@nhs.net<br />
Podiatry Musculoskeletal (Biomechanics) Service<br />
Carolyn Todd<br />
carolyntodd@nhs.net<br />
01592 6452<strong>18</strong><br />
The Hand Therapy Team consists <strong>of</strong> two specialist nurses, one full-time Advanced Occupational<br />
Therapist, one part-time specialist OT and one full-time orthopaedic physio<strong>the</strong>rapy practitioner.<br />
The team provides an out-patient service in both Queen Margaret Hospital (Dunfermline) and<br />
The Victoria Hospital (Kirkcaldy). Assessment, intervention and rehabilitation is provided for<br />
people who have ei<strong>the</strong>r sustained hand/upper limb trauma, undergone hand/upper limb elective<br />
surgery or who have a hand/upper limb condition. Referrals are accepted from AHP colleagues,<br />
GPs and consultants. Services <strong>of</strong>fered include <strong>the</strong>rmoplastic static and dynamic splinting, sensory<br />
assessment/re-education, injection <strong>the</strong>rapy, wound management, functional assessment and<br />
rehabilitation, streng<strong>the</strong>ning programmes and pain management advice.<br />
The Occupational Therapy Service provides assessment, intervention, rehabilitation and complex<br />
case management for clients referred and triaged to <strong>the</strong> secondary care aspect <strong>of</strong> Fife Integrated<br />
Pain Management Service. The services are in a variety <strong>of</strong> settings throughout Fife including: <strong>the</strong><br />
specialist out-patient unit in Queen Margaret Hospital, Victoria Hospital and Whyteman’s Brae<br />
Hospital in Kirkcaldy, clients’ homes and workplaces, and local community health clinics.<br />
The Foot and <strong>An</strong>kle Team consists <strong>of</strong> two orthopaedic consultants, two registrars, two<br />
podiatrists (one Extended Scope) and one orthotist. Referrals are received electronically from<br />
GPs and triaged to <strong>the</strong> appropriate team member. There is access to diagnostic investigations<br />
and imaging. Treatments can include biomechanical assessment +/– orthotic management,<br />
insole management and footwear, exercises, steroid injections, acupuncture, onward referral to<br />
physio<strong>the</strong>rapy and pain services, and where appropriate surgical intervention.<br />
The Podiatry Department provides a comprehensive Fife-wide lower limb musculoskeletal<br />
service. This is delivered by specialists who provide <strong>the</strong> assessment, diagnosis and treatment <strong>of</strong><br />
children and adults presenting with complex MSK conditions. There are combined clinics with<br />
physio<strong>the</strong>rapists and late clinics to accommodate working patients. Direct access to orthotist<br />
services has shortened <strong>the</strong> journey for patients who need footwear or modifications, with<br />
bespoke and <strong>of</strong>f-<strong>the</strong>-shelf orthoses being an integral part <strong>of</strong> providing <strong>the</strong> service. Work is<br />
ongoing to introduce skill mix.<br />
Improvements and outcomes: audit, patient survey, VAS Care Aims with mean VAS scores<br />
improving following intervention.<br />
26<br />
mskscoping<strong>2011</strong>-rs.indd 26 03/11/<strong>2011</strong> 11:01
<strong>Joint</strong> <strong>effects</strong> <strong>2011</strong><br />
Rheumatology podiatry<br />
Adele Osborne<br />
adele.osborne@nhs.net<br />
01383 722911<br />
The Rheumatology Podiatry Department provides a comprehensive Fife-wide lower limb<br />
musculoskeletal service which also includes acupuncture and steroid injections. This is delivered<br />
by specialists who provide <strong>the</strong> assessment, diagnosis and treatment <strong>of</strong> adults presenting with<br />
inflammatory conditions. There are late clinics to accommodate working patients. Work is<br />
ongoing to introduce skill mix.<br />
Improvements and outcomes: audit, patient satisfaction survey, VAS, Care Aims with mean VAS<br />
scores improving following podiatry interventions.<br />
Rheumatology<br />
Janet Harkess<br />
janetharkess@nhs.net<br />
01383 623623<br />
The service provides an OT assessment, intervention and rehabilitation service for individuals<br />
with rheumatological conditions, in clinics or patients’ own homes.<br />
NHS Forth Valley<br />
Extended Scope Practitioner Clinics in Orthopaedics<br />
Lesley Dawson<br />
lesleydawson@nhs.net<br />
01786 434061<br />
These clinics have played a significant role in reducing waiting times in NHS FV over <strong>the</strong> last<br />
eight years. They assess and treat 50% <strong>of</strong> all elective orthopaedic patients, with just over<br />
half <strong>of</strong> <strong>the</strong>se being discharged at <strong>the</strong>ir first appointment, requiring only advice or referral to<br />
physio<strong>the</strong>rapy or appliances.<br />
All referrals are triaged to ensure appropriate streaming to ESP or consultant clinics. ESP see on<br />
average seven new patients per clinic and onward referral rates are low at less than 5%.<br />
A recent audit showed that only 2.8% <strong>of</strong> patients discharged from ESP clinics in 2009 were<br />
re-referred back into <strong>the</strong> system and seen by an orthopaedic consultant within twelve months <strong>of</strong><br />
discharge.<br />
Outcomes measured: discharge rates and a patient satisfaction survey.<br />
27<br />
mskscoping<strong>2011</strong>-rs.indd 27 03/11/<strong>2011</strong> 11:01
<strong>Joint</strong> <strong>effects</strong> <strong>2011</strong><br />
Forth Valley Back Pain Service and Exercise Classes<br />
Norma Turvill<br />
nturvill@nhs.net<br />
The strength <strong>of</strong> <strong>the</strong> service lies in its capacity to direct patients to <strong>the</strong> part <strong>of</strong> <strong>the</strong> service that<br />
can help <strong>the</strong>m <strong>the</strong> most. Patients can refer <strong>the</strong>mselves to <strong>the</strong> Physio<strong>the</strong>rapy Department where<br />
<strong>the</strong>y will be thoroughly examined and talked through a treatment plan. Exercise is an essential<br />
part <strong>of</strong> back care and Forth Valley has classes to suit all abilities, <strong>the</strong>se can be accessed by<br />
self referral or referral by <strong>the</strong> physio<strong>the</strong>rapist. A pain management programme is in place for<br />
patients with longer term problems and <strong>the</strong> service can also give advice about workplace issues.<br />
Patients who require a second opinion or fur<strong>the</strong>r investigation can meet with an extended scope<br />
physio<strong>the</strong>rapist practitioner who specialises in back pain via <strong>the</strong> Orthopaedic Department.<br />
Improvements measured: outcomes from <strong>the</strong> orthopaedic clinic are recorded, e.g. discharged,<br />
exercise programme, pain management, investigations, onward referral, physio<strong>the</strong>rapy.<br />
Outcomes measured: before and after treatment by pain management programme – TSK,<br />
coping skills inventory, exercise programme – VAS, exercise options taken up.<br />
Forth Valley Physio<strong>the</strong>rapy<br />
Catriona Phin<br />
catriona.phin@nhs.net<br />
01786 434061<br />
Occupational Therapy for In-patients<br />
Rosina McGuire<br />
rosina.mcguire@nhs.net<br />
01324 567435<br />
Orthotic Services (Open Referral)<br />
Lynne Rowley<br />
lynne.rowley@nhs.net<br />
01324 616084<br />
This Forth-Valley-wide service includes a staff physio<strong>the</strong>rapy service, injection clinics, specialists<br />
in hands, paediatrics and women’s health. Close links with local GPs and orthopaedic clinics<br />
with ESP physio<strong>the</strong>rapists working in orthopaedic and rheumatology clinics<br />
Outcomes measured: WOMAC, KOOS, Roland and Morris, HAD, TSK, VAS, DASH, MYMOP,<br />
although outcomes not recorded with all patients.<br />
The OTs perform an assessment and <strong>the</strong>n <strong>the</strong> rehabilitation <strong>of</strong> acute trauma and elective<br />
patients to enable a safe and effective discharge home.<br />
The service has an open-access referral system with clinics held in hospitals and health centres<br />
with ward cover at weekends when required.<br />
Improvements measured: audit <strong>of</strong> referral-to-treatment dates compared to standard orthopaedic<br />
pathway.<br />
Outcomes measured: <strong>the</strong> foot function index and pain scale being recorded before and after<br />
treatment where possible.<br />
28<br />
mskscoping<strong>2011</strong>-rs.indd 28 03/11/<strong>2011</strong> 11:01
<strong>Joint</strong> <strong>effects</strong> <strong>2011</strong><br />
Podiatry Service<br />
Gordon Mclay<br />
gordon.mclay@nhs.net<br />
01786 431133<br />
Rheumatology ESP Clinics<br />
<strong>An</strong>ita Carr<br />
anitacarr@nhs.net<br />
01786 434061<br />
Rheumatology Occupational Therapy<br />
Rosina McGuire<br />
rosina.mcguire@nhs.net<br />
01324 567435<br />
The service operates throughout <strong>the</strong> Forth Valley in a number <strong>of</strong> settings. Patients can be<br />
referred by any healthcare pr<strong>of</strong>essional, and receive a full podiatry and medical assessment to<br />
determine <strong>the</strong> appropriate course <strong>of</strong> action. The services provided include:<br />
Acupuncture, Rheumatology, <strong>Joint</strong> podiatry/physio<strong>the</strong>rapy (paediatric and adult), Occupational<br />
Health, Biomechanical specialist service and a podiatry technician orthotic manufacturing<br />
service. The Occupational Health podiatry service has had an immense uptake with demand<br />
outstripping supply and provides a more local service to members <strong>of</strong> staff. The amount <strong>of</strong> days<br />
saved to <strong>the</strong> organisation in absence figures cannot be calculated.<br />
Fast access self referral clinics for patients already within <strong>the</strong> rheumatology service, requiring<br />
assessment for injection. Initial screening by phone <strong>the</strong>n assessed in clinic and fur<strong>the</strong>r<br />
investigations / onward referral completed if required.<br />
The team provides assessment and intervention for people with rheumatological conditions<br />
this includes giving advice, splinting, obtaining any necessary equipment, and supporting <strong>the</strong>m<br />
within <strong>the</strong>ir employment.<br />
NHS Grampian<br />
Elective Orthopaedics Occupational Therapy<br />
Eve Cruickshank<br />
eve.cruickshank@nhs.net<br />
01224 556044<br />
This OT service provides input at a pre-admission clinic in order to prepare patients for surgery<br />
and allow liaison with community OT colleagues to deliver necessary equipment. It also provides<br />
assessment, treatment and additional advice once <strong>the</strong> patient is admitted to hospital and after<br />
<strong>the</strong>ir surgery including rehabilitation following hip/knee replacements or back surgery.<br />
Outcomes measured: goal setting before and after treatment.<br />
29<br />
mskscoping<strong>2011</strong>-rs.indd 29 03/11/<strong>2011</strong> 11:01
<strong>Joint</strong> <strong>effects</strong> <strong>2011</strong><br />
Grampian Physio<strong>the</strong>rapy Services<br />
Lynn Morrison<br />
lynn.morrison@nhs.net<br />
01224 555466<br />
Musculoskeletal services are provided at several different settings – GP practice, Community<br />
hospital, District General hospital and Acute hospital. Self referral is available at some but not<br />
all sites. There are plans in place to make self referral into MSK physio<strong>the</strong>rapy services available<br />
throughout Grampian in May <strong>2011</strong>.<br />
Staff work as a team across a locality, providing sickness and annual leave cover. Triage issued<br />
and based on knowledge <strong>of</strong> demand and capacity. There is a pilot <strong>of</strong> different assessment times<br />
(20/30/40 minutes) and local research funding has been obtained for this.<br />
Moray Occupational Therapy<br />
Judy Fairburn<br />
judith.fairburn@nhs.net<br />
01343 567245/559461<br />
Orthopaedic Rehabilitation Unit<br />
Eve Cruickshank<br />
eve.cruickshank@nhs.net<br />
01224 556044<br />
<strong>An</strong> integrated OT service between NHS and Council. Moray Occupational Therapy has a duty<br />
system for all new referrals. There is an open referral system – self referral or anyone else<br />
representing <strong>the</strong> patient. <strong>An</strong>yone can access <strong>the</strong> service by telephone, email or letter.<br />
The unit provides a service to patients from 16 onwards with orthopaedic trauma or elective<br />
orthopaedic conditions who require specialist in-patient rehabilitation. The unit also takes<br />
patients who have had amputation following orthopaedic surgery.<br />
Improvements measured: patient satisfaction questionnaire.<br />
Outcomes measured: goal setting takes place throughout treatment.<br />
Orthotics Services<br />
Steven Lindsay<br />
steven.lindsay@nhs.net<br />
01224 556843<br />
Orthotics clinical and technical services are provided in Woodend Hospital and in some<br />
satellite clinics within Grampian. Currently, initial referral can be made by any medical or AHP<br />
pr<strong>of</strong>essional, with self referral available for existing patients. The orthotic service along with<br />
<strong>the</strong> pros<strong>the</strong>tics and wheelchair services are ‘housed’ in <strong>the</strong> primary care setting, although a<br />
significant volume <strong>of</strong> work takes place within secondary care.<br />
30<br />
mskscoping<strong>2011</strong>-rs.indd 30 03/11/<strong>2011</strong> 11:01
<strong>Joint</strong> <strong>effects</strong> <strong>2011</strong><br />
Rheumatology<br />
Fiona McCurdy<br />
f.mccurdy@nhs.net<br />
01224 554751<br />
Supported Discharge Service Stroke and Trauma Orthopaedics<br />
Beth Thomson<br />
beththomson@nhs.net<br />
01224 556401<br />
NHS Greater Glasgow and Clyde<br />
Call Centre Access and evening clinics popular with patients<br />
Paul Higgins<br />
paul.higgins@ggc.scot.nhs.uk<br />
0141 211 142<br />
Community Physio<strong>the</strong>rapy Services. Out-patient musculoskeletal<br />
services – Renfrewshire CHP<br />
Elizabeth Lightbody<br />
elizabeth.lightbody@ggc.scot.nhs.uk<br />
01505 821621<br />
The service provides specialist assessment and intervention to both in- and out-patients. The<br />
occupational <strong>the</strong>rapy team has input into <strong>the</strong> Rheumatoid Arthritis Management Programme<br />
(RAMP) as well as <strong>the</strong> Adolescent Transition Service, to assist patients as <strong>the</strong>y move from<br />
paediatric to adult services. The service is part <strong>of</strong> a multidisciplinary team, it <strong>of</strong>fers an<br />
education programme for chronic fatigue management and provides specialist information<br />
for OTs working in community rehabilitation services. The service’s consultant uses a range <strong>of</strong><br />
standardised measures.<br />
The service provides rehabilitation from OTs, physio<strong>the</strong>rapists and SLT within <strong>the</strong> patient’s<br />
own home for up to six weeks after early discharge from acute or specialist rehabilitation or<br />
intermediate care.<br />
Outcomes measured: individual pr<strong>of</strong>essional measures, goal setting, service users rating own<br />
achievements.<br />
All podiatry primary and community care services use self referral or referral by ano<strong>the</strong>r<br />
healthcare pr<strong>of</strong>essional. All new patients referrals are by telephone using a single call centre.<br />
This operates daily from 9.00 am to 5.00 pm in <strong>the</strong> old Glasgow area (and some areas <strong>of</strong> Clyde).<br />
The model is used in some places for return patient appointments. It has proved to be popular<br />
with patients and was highlighted at a recent patient feedback day as top priority. This cannot<br />
be rolled out across <strong>the</strong> board area at <strong>the</strong> moment due to IM&T capability and capacity issues at<br />
<strong>the</strong> call centre. Evening clinics are also available where <strong>the</strong> DNA rates are close to zero. Access<br />
to services will be fur<strong>the</strong>r simplified as part <strong>of</strong> a general AHP redesign.<br />
This service covers 30 GP practices and <strong>of</strong>fers out-patients physio<strong>the</strong>rapy for most postsurgical<br />
and musculoskeletal problems. Patients are referred via <strong>the</strong>ir GP or o<strong>the</strong>r healthcare<br />
pr<strong>of</strong>essionals.<br />
Outcomes measured: EMS, Tinetti. Record before and after completion <strong>of</strong> treatment in<br />
domicilary service. MSK use VAS etc. Injection-service-specific pr<strong>of</strong>orma and outcome.<br />
31<br />
mskscoping<strong>2011</strong>-rs.indd 31 03/11/<strong>2011</strong> 11:01
<strong>Joint</strong> <strong>effects</strong> <strong>2011</strong><br />
ESP Orthopaedic Foot and <strong>An</strong>kle Triage Service<br />
Paul Higgins<br />
paul.higgins@ggc.scot.nhs.uk<br />
0141 211 1425<br />
MSK Physio<strong>the</strong>rapy Service Review<br />
Hea<strong>the</strong>r Cameron<br />
hea<strong>the</strong>r.cameron@ggc.scot.nhs.uk<br />
0141 211 8562<br />
ESP orthopaedic foot and ankle triage services were set up in <strong>the</strong> community in 2004.<br />
Orthopaedic waiting times were around <strong>18</strong> months and <strong>the</strong> surgical conversion rate averaged<br />
30%. The service received <strong>the</strong> national AHP award for best innovative service in 2007.<br />
The service continues with a surgical conversion rate for foot and ankle patients <strong>of</strong> 90 – 95%.<br />
Permanent funding for <strong>the</strong> two whole time equivalent (wte) posts was secured in 2008. Patients<br />
wait a maximum <strong>of</strong> six weeks from referral to being seen. The service contributes to reduced<br />
orthopaedic waiting times, frees up consultant time, ensures patients are seen by <strong>the</strong> best<br />
person and provides a local service to <strong>the</strong> community.<br />
Over 72,500 patients are seen each year in <strong>the</strong> NHS Greater Glasgow and Clyde (NHS GG&C)<br />
physio<strong>the</strong>rapy musculoskeletal services. Currently delivered in 30 community sites and nine<br />
acute sites including clinics, health centres, hospitals, leisure centres, and o<strong>the</strong>r community<br />
centres throughout NHS GG&C. The MSK physio service employs 154.4 wte physio<strong>the</strong>rapy staff<br />
(75.19 wte in CH(C)PS and 79.21 wte in acute sector).<br />
A redesign <strong>of</strong> MSK services is currently underway, due for implementation early 2012 which will<br />
streamline services and improve accessibility and efficiency.<br />
Patients can access physio<strong>the</strong>rapy via a number <strong>of</strong> routes: self, GP or consultant referral. The<br />
majority <strong>of</strong> sites <strong>of</strong>fer self referral – most patients use <strong>the</strong> telephone but some sites also <strong>of</strong>fer<br />
drop-in sessions.<br />
Extended Scope Physio<strong>the</strong>rapists (ESPs) work across GG&C in acute hospital settings; <strong>the</strong> ESPs<br />
triage orthopaedic referrals and have a key role in patients pathways, ordering investigations<br />
and listing for surgery where appropriate.<br />
Glasgow Back Pain Service (GBPS) has a well established pathway for people with low back pain<br />
providing speedy access for those who may require it to specialist physio<strong>the</strong>rapy advice and/ or<br />
investigation / onward referral. This service has also recently been extended to include Clyde.<br />
32<br />
mskscoping<strong>2011</strong>-rs.indd 32 03/11/<strong>2011</strong> 11:01
<strong>Joint</strong> <strong>effects</strong> <strong>2011</strong><br />
MSK Outcome Measure Pr<strong>of</strong>orma<br />
Karen Glass<br />
karen.glass@ggc.scot.nhs.uk<br />
Many MSK clinicians were only recording VAS pain scales as an outcome measure. Impact <strong>of</strong> <strong>the</strong><br />
service on service users in any improvement in function, work or physical activity could not be<br />
demonstrated.<br />
Validated outcomes <strong>of</strong> pain VAS and function (from ‘patient functional scale’) were combined<br />
with non-validated outcomes related to work status and medication consumption and a record<br />
was kept <strong>of</strong> health improvement discussions: physical activity, alcohol intake, smoking and<br />
weight.<br />
Outcomes were recorded in discussion with <strong>the</strong> patient ra<strong>the</strong>r than strictly patient reported or<br />
<strong>the</strong>rapist reported. The ‘new’ MSK outcomes pr<strong>of</strong>orma was piloted in February 2010 and with<br />
minor changes rolled out and audited in October 2010. The Clinical Governance Support Unit is<br />
processing <strong>the</strong> data and a draft report is now available.<br />
One Stop Rheumatology Foot Service – a partnership with Glasgow<br />
Caledonian University<br />
Mhairi Brandon<br />
mhairi.brandon@ggc.scot.nhs.uk<br />
The MDT foot clinic coordinates rapid investigations such as diagnostic ultrasound and gait<br />
analysis to facilitate treatment planning and evaluation. This clinic has been developed as a onestop<br />
shop, specifically for <strong>the</strong> management <strong>of</strong> patients with complex lower limb problems. The<br />
MDT foot clinic is linked with <strong>the</strong> Foot and <strong>An</strong>kle Research Group based at Glasgow Caledonian<br />
University and provides <strong>the</strong> opportunity to undertake audit and facilitate research. The specialist<br />
experience gained by running this type <strong>of</strong> clinic will also provide <strong>the</strong> opportunity to develop<br />
capacity and capability in ultrasound imaging, injection <strong>the</strong>rapy and research for AHPs.<br />
This one-stop approach resulted in 75% <strong>of</strong> patients not requiring any fur<strong>the</strong>r input AHP<br />
input following that episode <strong>of</strong> care, 5% were fast tracked to Orthopaedics for a surgical<br />
intervention and 20% were sent for additional medical management relating to <strong>the</strong>ir ongoing<br />
rheumatological condition.<br />
Pain Services<br />
Aline Williams and Linda Sparks<br />
aline.williams@ggc.scot.nhs.uk<br />
Specialist physio<strong>the</strong>rapists work within <strong>the</strong> pain services in <strong>the</strong> acute division as part <strong>of</strong> a<br />
multidisciplinary team. In addition to providing specialist advice to patients <strong>the</strong>y also deliver<br />
training and education to o<strong>the</strong>r MSK physio<strong>the</strong>rapists. A multidisciplinary pain management<br />
programme has been established.<br />
33<br />
mskscoping<strong>2011</strong>-rs.indd 33 03/11/<strong>2011</strong> 11:01
<strong>Joint</strong> <strong>effects</strong> <strong>2011</strong><br />
Practice Development: laser, <strong>the</strong>rapy, dry needling, deep enucleation,<br />
surgery and steroid injections<br />
Paul Higgins<br />
paul.higgins@ggc.scot.nhs.uk<br />
0141 211 1425<br />
Practice Innovations: patient stories, videos, phone follow up<br />
and <strong>the</strong> CARE measure<br />
Karen Glass<br />
karen.glass@ggc.scot.nhs.uk<br />
Orthopaedic Foot and <strong>An</strong>kle Triage provides an alternative care pathway within <strong>the</strong> community<br />
for patients historically referred to hospital out-patient services.<br />
Dry needling is used as an adjunct to treatment for a wide range <strong>of</strong> painful foot conditions<br />
such as Hallux Limitus, heel pain, painful diabetic neuropathy, Plantar digital neuritis and Plantar<br />
Fasciitis. Particular benefit has been reported for those patients with podiatric conditions that<br />
have proved difficult to progress or resolve using traditional treatment methods. There are now<br />
26 podiatrists across NHSGGC trained in steroid injection <strong>the</strong>rapy.<br />
The impact <strong>of</strong> projects using qualitative feedback from service users. Video, patient stories and<br />
telephone feedback <strong>of</strong> patient experience <strong>of</strong> self referral.<br />
Video and patient stories: patients were interviewed in <strong>the</strong>ir own home at a convenient time by<br />
<strong>the</strong> practice development physio<strong>the</strong>rapist and one <strong>of</strong> <strong>the</strong> service managers. Footage was edited<br />
down to approximately six minutes. This is a powerful tool for improvements but especially in<br />
explaining AHP services to non-clinicians and board members.<br />
Telephone feedback: a practical, relatively inexpensive way to get good quality qualitative<br />
feedback on a service.<br />
CARE: clinicians attended NES funded training on ‘empathy and engagement’. Following this<br />
300 measures were analysised. <strong>An</strong> opportunity arose to take part in a national reliability study <strong>of</strong><br />
<strong>the</strong> CARE measure for AHPs led by <strong>the</strong> NMAHP Research Unit at Stirling University. 80 clinicians<br />
from <strong>the</strong> community are currently collecting CARE measures.<br />
Rehabilitation Service – Glasgow City Community Health<br />
Paul Higgins<br />
paul.higgins@ggc.scot.nhs.uk<br />
0141 211 1425<br />
The team was established in May <strong>2011</strong> and provides various aspects <strong>of</strong> MSK care via podiatrists,<br />
physio<strong>the</strong>rapists and OT staff. The rehabilitation teams were established to support integration<br />
<strong>of</strong> <strong>the</strong> current range <strong>of</strong> rehabilitation services. The team will provide a full co-ordinated<br />
assessment within <strong>the</strong> hospital or community. Treatment plans and reviews will take place within<br />
a patient’s own home, or o<strong>the</strong>r appropriate community or workplace setting.<br />
The aim is a single point <strong>of</strong> access, better pathways, local provision and patients seeing <strong>the</strong><br />
right person first time. The service will deal with all levels <strong>of</strong> need, complexity and vulnerability,<br />
promoting self management and vocational rehabilitation. This will be underpinned by a full<br />
understanding <strong>of</strong> <strong>the</strong> inequalities and discrimination faced by patients and <strong>the</strong> wider public.<br />
34<br />
mskscoping<strong>2011</strong>-rs.indd 34 03/11/<strong>2011</strong> 11:01
<strong>Joint</strong> <strong>effects</strong> <strong>2011</strong><br />
Training for Financial Inclusion and Employability<br />
Hea<strong>the</strong>r Cameron<br />
hea<strong>the</strong>r.cameron@ggc.scot.nhs.uk<br />
0141 211 8562<br />
Bespoke training was developed to assist AHP development and support staff working within<br />
acute MSK to signpost patients to appropriate services. The training aimed to:<br />
1 identify at assessment, people’s aspirations to stay in work, return to work or access<br />
employment<br />
2 develop a new focus on enabling <strong>the</strong> individual to achieve <strong>the</strong>ir employability goals<br />
3 effectively refer vocational rehabilitation and employability services.<br />
On evaluation, <strong>the</strong> training was well received with staff reporting increased confidence in<br />
<strong>the</strong>ir knowledge and skills. A resource manual was also developed to support sustainability <strong>of</strong><br />
learning.<br />
NHS Highland<br />
Easter Ross Orthopaedic Triage Pilot<br />
Sue King<br />
sue.king6@nhs.net<br />
01349 852496 ext. 7398<br />
Easter Ross Orthopaedic Triage Pilot has been successful in meeting <strong>the</strong> original aims <strong>of</strong> <strong>the</strong><br />
project: Improving compliance with <strong>the</strong> orthopaedic referral pathways and demonstration <strong>of</strong> a<br />
sustainable reduction in orthopaedic referrals from <strong>the</strong> GP practices.<br />
Funding to continue <strong>the</strong> Easter Ross Orthopaedic Triage service for a fur<strong>the</strong>r six months was<br />
granted whilst Mid Highland CHP considers <strong>the</strong> long-term future <strong>of</strong> this pilot locally and its<br />
potential as a sustainable solution across <strong>the</strong> rest <strong>of</strong> Highland is evaluated.<br />
O<strong>the</strong>r strands to <strong>the</strong> work were triage, Teach and Treat Clinic and patient-focused booking for<br />
physio<strong>the</strong>rapy. Project reports available on request.<br />
Hand Therapy and Splinting Service<br />
Karen Tolmie<br />
karen.tolmie@nhs.net<br />
01463 704293<br />
The Occupational Therapy Department, Raigmore Hospital in Inverness <strong>of</strong>fers a hand <strong>the</strong>rapy<br />
and splinting service to both in- and out-patients from throughout <strong>the</strong> Highlands. Patients are<br />
referred primarily by medical or allied health pr<strong>of</strong>essionals. A range <strong>of</strong> conditions impairing hand<br />
function are treated including post elective or traumatic surgery and neurological conditions.<br />
Patients who are known to <strong>the</strong> service may initiate re-referral. The service <strong>of</strong>fers specialist advice<br />
for AHP colleagues working elsewhere in Highland.<br />
35<br />
mskscoping<strong>2011</strong>-rs.indd 35 03/11/<strong>2011</strong> 11:01
<strong>Joint</strong> <strong>effects</strong> <strong>2011</strong><br />
Hand Therapy for Orthopaedics<br />
Linda Currie<br />
lindacurrie@nhs.net<br />
01631 788971<br />
Mid CHP Podiatry<br />
Roddy Wells<br />
roderick.wells@nhs.net<br />
01397 709800<br />
South East Highland CHP Podiatry Service<br />
Michael Gates<br />
michael.gates@nhs.net<br />
01463 723250<br />
Provision <strong>of</strong> Occupational Therapy Hand<strong>the</strong>rapy Services for orthopaedic clinic (LIH) and postsurgical<br />
<strong>the</strong>rapy for patients discharged from NHS Greater Glasgow and Clyde Hospitals.<br />
Mid CHP Podiatry delivers services in nine locations. All referrals are accepted. There is a<br />
PEAK system for patient appointments and no electronic patient records. A New Activity and<br />
Waiting Times data collection system in place since February <strong>2011</strong> across all AHP disciplines. No<br />
recognised MSK specialist for Mid Highland CHP, but part-time post currently awaiting clearance<br />
by vacancy panel. All staff expected to carry out routine MSK assessments and treatments.<br />
MSK referrals continue to increase. 94% <strong>of</strong> new patients were seen within eight weeks <strong>of</strong><br />
<strong>the</strong>ir initial referral. Most staff are trained in acupuncture and two staff to undertake foot and<br />
ankle steroid injections. There are plans to train staff up on x-ray interpretation as well as blood<br />
and biochemistry results. All staff have access to results reporting and PACs imaging systems.<br />
Functional orthoses are manufactured by clinicians on site and staff can refer on to <strong>the</strong> local<br />
Orthotic Department for footwear and <strong>the</strong> more palliative type <strong>of</strong> orthotic devices. All staff are<br />
able to refer directly to X-ray and Orthopaedics accept referrals.<br />
The plans for a dedicated MSK triage referral service are underway across Highland. At <strong>the</strong><br />
moment South East Highland CHP is <strong>the</strong> only CHP without a recognised podiatric biomechanical<br />
/ MSK specialist. O<strong>the</strong>r CHPs within Highland ei<strong>the</strong>r have an individual already in place or have<br />
funding to put someone in place.<br />
NHS Lanarkshire<br />
Extended Scope Practitioner Service in Orthopaedic Out-patients<br />
Janie Thomson<br />
Janie.thomson@lanarkshire.scot.nhs.uk<br />
01355 585447<br />
A team <strong>of</strong> six physio ESPs, a podiatry ESP and one consultant physio provide assessment clinics<br />
for general MSK conditions which are unlikely to require surgery. These clinicians are able to<br />
request necessary investigations and are also qualified in injection <strong>the</strong>rapy which can be <strong>of</strong>fered<br />
as a treatment in both ortho and physio<strong>the</strong>rapy clinics. The same team provide complex case<br />
clinical reasoning clinics across Lanarkshire and also provide training and support on a one-toone<br />
basis with difficult physio/podiatry cases.<br />
Improvements measured: reduction in number <strong>of</strong> back pain cases seen in ortho clinics, reduction<br />
in ortho ESP waits, reduction in radiology requesting.<br />
36<br />
mskscoping<strong>2011</strong>-rs.indd 36 03/11/<strong>2011</strong> 11:01
<strong>Joint</strong> <strong>effects</strong> <strong>2011</strong><br />
Low Back Pain Physio<strong>the</strong>rapy Pathway<br />
Christine McCallum<br />
christine.mccallum@lanarkshire.scot.nhs.uk<br />
01698 242615<br />
The lower back pain pathway was introduced in July 2010. All patients with LBP are ei<strong>the</strong>r self<br />
referred or GP referred, <strong>the</strong>y are assessed and treated according to an evidence-based, managed<br />
clinical pathway. There is a clear escalation policy for patients identified requiring fur<strong>the</strong>r<br />
investigation or have complex needs. <strong>An</strong> orthopaedic spinal clinic run jointly by an ESP and an<br />
orthopaedic surgeon reviews all patients with more complex outcomes or who have had an MRI<br />
in order to provide a single point <strong>of</strong> exit from NHSL for surgical opinion if required. Exit routes<br />
to o<strong>the</strong>r services such as WHSS, pain clinic, and exercise classes are available with outcome<br />
measures assigned to each in order to evaluate <strong>the</strong> pathway and inform future service provision.<br />
Improvements measured: measurable reduction in inappropriate referrals to ESP ortho vetting<br />
system and reduction in waits. Resources were shifted to support <strong>the</strong> service through savings<br />
made.<br />
Outcomes measured: at present VAS, and clinical subjective and objective markers. STarT Back<br />
tool in use. Will shortly be using <strong>the</strong> EQ5D, Roland and Morris and HADS.<br />
Physio<strong>the</strong>rapy Assessment Line<br />
Ruth Currie<br />
ruth.currie@lanarkshire.scot.nhs.uk<br />
01698 723246<br />
The Physio<strong>the</strong>rapy Assessment Line (PAL) is a single-access telephone triage service for all<br />
adults living within NHS Lanarkshire with an MSK condition for which Physio<strong>the</strong>rapy advice or<br />
intervention may be <strong>of</strong> benefit. More than 60 experienced MSK clinicians have been trained and<br />
handle calls, with <strong>the</strong> service manned by up to 10 physio<strong>the</strong>rapists each morning. Calls last on<br />
average 15 minutes with <strong>the</strong> patient being thoroughly questioned and <strong>the</strong>n managed in line<br />
with evidence-based treatment and local service pathways such as routine appointment, urgent<br />
appointment and emergency referral.<br />
Improvements measured: call data outcomes available from our database and telephone system.<br />
Outcomes measured: numerous outcomes are recorded including <strong>the</strong> call outcomes as<br />
mentioned above, <strong>the</strong> percentage <strong>of</strong> back pain referrals made, <strong>the</strong> percentage <strong>of</strong> patients asked<br />
to self manage, presenting conditions and demographics. A 22% increase in demand has been<br />
addressed with <strong>the</strong> same resource.<br />
37<br />
mskscoping<strong>2011</strong>-rs.indd 37 03/11/<strong>2011</strong> 11:01
<strong>Joint</strong> <strong>effects</strong> <strong>2011</strong><br />
Podiatry Biomechanics Service<br />
Jim Logan<br />
jim.logan@lanarkshire.scot.nhs.uk<br />
01355 585447<br />
NHS Lothian<br />
East and Midlothian Physio<strong>the</strong>rapy Service<br />
Brian Brockie<br />
brian.brockie@nhslothian.scot.nhs.uk<br />
0131 536 8430<br />
2,500 new patients last year accessed <strong>the</strong> service by referral from GPs, Physio<strong>the</strong>rapy, Podiatry<br />
or o<strong>the</strong>r healthcare providers. No self referral. Patients are able to initiate a re-referral back<br />
into <strong>the</strong> system for an existing condition providing it is within an agreed timescale. Preassessment<br />
questionnaires are sent out prior to patients first visit. There are currently ten<br />
podiatrists providing biomechanics service across NHSL. A MSK foot and ankle pathway is under<br />
development and will provide direct links into orthopaedic services in NHSL. A change in stock<br />
procurement resulted in a 20% saving on <strong>the</strong> cost <strong>of</strong> orthotic devices.<br />
Provide a skilled, accessible and equitable musculoskeletal and rehabilitation service for <strong>the</strong><br />
population <strong>of</strong> East and Mid Lothian, in a variety <strong>of</strong> settings. Provide users with timely and<br />
clinically effective care, including assessment, treatment and advice to elevate pain, maximise<br />
function and promote self management. Provide clinical education and specialist teaching to<br />
undergraduates and post graduates.<br />
Contributes to a hospital-based consultant out-patient clinic based in Roodlands by way <strong>of</strong><br />
extended scope physio<strong>the</strong>rapy practitioners being part <strong>of</strong> a hospital multidisciplinary team<br />
consisting <strong>of</strong> orthopaedic surgeons, rheumatologist and MSK GPwSI to provide expert<br />
assessment and treatment.<br />
Edinburgh Community Physio<strong>the</strong>rapy Service<br />
Eddie Balfour<br />
eddie.balfour@nhslothian.scot.nhs.uk<br />
0131 536 9732<br />
Foot and <strong>An</strong>kle, Orthopaedic Clinic<br />
Colin Thomson<br />
colin.thomson@luht.scot.nhs.uk<br />
Provide a skilled, accessible and equitable musculoskeletal and rehabilitation service for <strong>the</strong><br />
population <strong>of</strong> <strong>the</strong> City <strong>of</strong> Edinburgh, in a variety <strong>of</strong> out-patient settings. To provide users with<br />
timely, individualised and clinically effective care, including screening, assessment, treatment and<br />
advice to alleviate pain, maximise function and promote self-management. To provide clinical<br />
education and specialist teaching to undergraduate and post-graduate physio<strong>the</strong>rapists and<br />
o<strong>the</strong>r healthcare pr<strong>of</strong>essionals.<br />
This multi-pr<strong>of</strong>essional clinic has access to diagnostic facilities including ultrasound, x-ray, MRI<br />
and bloods. Treatment may include exercises, referral for orthotic <strong>the</strong>rapy or injection <strong>the</strong>rapy.<br />
Some patients may require surgery. Manchester and Oxford foot pain questionnaire is used<br />
before surgery.<br />
38<br />
mskscoping<strong>2011</strong>-rs.indd 38 03/11/<strong>2011</strong> 11:01
<strong>Joint</strong> <strong>effects</strong> <strong>2011</strong><br />
Podiatry Biomechanics Clinic (Edinburgh, East Lothian and Midlothian)<br />
William McMurrich<br />
william.mcmurrich@nhslothian.scot.nhs.uk<br />
0131 537 7463<br />
Spinal Practitioner Support to Orthopaedic Spinal Service<br />
Vivienne Boyd<br />
vivienne.boyd@luht.scot.nhs.uk<br />
0131 242 1946<br />
West Lothian Musculoskeletal Service<br />
Orla Crummey<br />
orla.crummey@nhslothian.scot.nhs.uk<br />
01506 522063/522057<br />
NHS National Waiting Times Centre<br />
Innovations in Orthopaedics<br />
Birgit Clark<br />
birgit.clark@gjnh.scot.nhs.uk<br />
0141 951 5193<br />
The podiatry service operates throughout Edinburgh, East and Mid Lothian CHPs. Patients<br />
may self refer or be referred by any healthcare pr<strong>of</strong>essional. Initial assessment and treatment<br />
(including supplying orthoses) is provided in community settings. Fur<strong>the</strong>r gait analysis, orthotics<br />
and injection <strong>the</strong>rapy may be obtained from <strong>the</strong> in-house MSK/Biomechanics clinic. Orthotics<br />
are manufactured on site using Podiatry Department laboratory technicians.<br />
The spinal practitioner post supports <strong>the</strong> Orthopaedic Spinal Service by performing exactly <strong>the</strong><br />
same tasks as <strong>the</strong> surgeon, providing <strong>the</strong> appropriate screening i.e. taking a history, clinical<br />
examination, ordering <strong>the</strong> appropriate investigations, making a diagnosis and arranging <strong>the</strong><br />
appropriate management including putting <strong>the</strong> patient on to <strong>the</strong> surgical waiting list.<br />
This service incorporates a large physio<strong>the</strong>rapy department based in St John’s hospital at<br />
Livingston and physio<strong>the</strong>rapy centres in 12 outlying clinics in primary care (many <strong>of</strong> <strong>the</strong>se are<br />
part-time clinics). St John’s <strong>of</strong>fers hydro<strong>the</strong>rapy and a large rehab gym as well as one-to-one<br />
treatments. Two <strong>of</strong> <strong>the</strong> new-build health centres have larger departments with gym facilities.<br />
The service receives approx 12,000 new referrals a year and services a growing population <strong>of</strong><br />
172,800. The population is increasing year on year (10% in <strong>the</strong> past 10 years). Referrals are<br />
from consultants, GPs and o<strong>the</strong>r health pr<strong>of</strong>essionals. Self referral is possible in most centres.<br />
The patient caseload includes post-surgical, chronic pain, rheumatological, general MSK, A&E,<br />
and ENT (dizziness and TMJ) patients.<br />
The NHS National Waiting Times Centre in Clydebank is an NHS special health board which<br />
manages <strong>the</strong> Golden Jubilee National Hospital, <strong>the</strong> Beardmore Hotel and Conference Centre<br />
and <strong>the</strong> new Beardmore Centre for Health Science. It provides an elective service to help<br />
local NHS Boards meet <strong>the</strong>ir waiting time targets in key specialties. This service is available to<br />
patients across Scotland. The orthopaedic programme continues to grow year on year. From<br />
30 operations in 2002 <strong>the</strong> hospital performs 300 per month. The GJNH does 15% <strong>of</strong> all joint<br />
replacements in Scotland. It takes a lead in pioneering new techniques, e.g. computer-assisted<br />
orthopaedic surgery (CAOS) and The CALEDonian Technique (enhanced recovery) leading to<br />
four days length <strong>of</strong> stay following joint replacement surgery.<br />
39<br />
mskscoping<strong>2011</strong>-rs.indd 39 03/11/<strong>2011</strong> 11:01
<strong>Joint</strong> <strong>effects</strong> <strong>2011</strong><br />
MSK Physio<strong>the</strong>rapist in Occupational Health and Orthopaedic<br />
Out-patients<br />
Kathryn Macpherson<br />
kathryn.macpherson@gjnh.scot.nhs.uk<br />
0141 951 5121<br />
Elective Orthopaedic Surgery<br />
Birgit Clark<br />
birgit.clark@gjnh.scot.nhs.uk<br />
0141 951 5193<br />
This is a split post between MSK physio<strong>the</strong>rapy in Occupational Health (90%) and Orthopaedic<br />
(10%) out-patients. It <strong>of</strong>fers a dedicated musculoskeletal physio<strong>the</strong>rapy service and vocational<br />
rehabilitation for staff working at <strong>the</strong> GJNH and Beardmore. Staff can be referred or self-refer to<br />
<strong>the</strong> service. Staff who have <strong>the</strong>ir surgery at <strong>the</strong> GJNH can be referred through <strong>the</strong>ir consultant or<br />
GJNH physio.<br />
This is an elective orthopaedic service, based at <strong>the</strong> Golden Jubilee National Hospital (GJNH)<br />
managed by NHS National Waiting Times Centre, <strong>of</strong>fering hip and knee replacements, some<br />
spinal surgeries and minor surgeries including ACL repairs, arthroscopies, meniscectomies, hand<br />
surgeries and foot surgeries. The Rehabilitation Department consisting <strong>of</strong> physio<strong>the</strong>rapists and<br />
OTs, supported by generic rehabilitation assistants provide pre- and post-operative intervention.<br />
Very few patients require referrals for out-patient physio<strong>the</strong>rapy, by following strict criteria.<br />
Patients are <strong>of</strong>fered follow-up physio<strong>the</strong>rapy at GJNH or will be referred to a facility accessible<br />
closer to home.<br />
All patients are reviewed by <strong>the</strong> Arthroplasty Outcomes Team for <strong>the</strong>ir post-operative check up<br />
at six weeks or three months dependent on type <strong>of</strong> surgery, one year, five years and 10 years.<br />
The enhanced recovery programme known in-house as CALEDonian Technique encourages early<br />
mobility <strong>of</strong> patients post-surgery and improved length <strong>of</strong> stay.<br />
Improvements measured by internal audit.<br />
Outcomes used: pain scores, Oxford knee/hip scores, range <strong>of</strong> movement, day <strong>of</strong> mobilization,<br />
referral rates for out-patient care.<br />
NHS Orkney<br />
MSK Orthopaedic Triage Service<br />
Paula Hemsley<br />
paula.hemsley@nhs.net<br />
This was set up in January 2008 and modelled on <strong>the</strong> Raigmor service which <strong>of</strong>fered training<br />
and <strong>the</strong>ir existing clinical pathways. It took some time to embed but is now fully accepted and<br />
has recently been extended to reviewing all <strong>the</strong> post-op total hip replacements. It freed up<br />
consultation time and improved surgical conversion rates. Triage is now embedded in <strong>the</strong> core<br />
service as <strong>of</strong> March 2010 at 12.5 hours per week.<br />
40<br />
mskscoping<strong>2011</strong>-rs.indd 40 03/11/<strong>2011</strong> 11:01
<strong>Joint</strong> <strong>effects</strong> <strong>2011</strong><br />
Musculoskeletal Pathways, Balfour Hospital<br />
Peter Mackellar<br />
peter.mackellar@nhs.net<br />
Occupational Health, pre employment assesment and return to work<br />
Lesley Platford<br />
lesley.platford@nhs.net<br />
Rheumatology Telemedicine Link Clinic<br />
Lesley Platford<br />
lesley.platford@nhs.net<br />
The Physio<strong>the</strong>rapy Service is wide ranging: General MSK Outpatients ,Woman’s and Men’s<br />
health. Cardiac rehab and <strong>the</strong> telephone based follow up road to recovery programme for<br />
patients that wish to carry out <strong>the</strong>ir programme at home, Pulmonary rehab ,Rheumatology,<br />
Occupational health, Orthopaedic triage, Fracture clinic. Consultant lead orthopaedic clinics.<br />
Lead by out moving moving and handling <strong>the</strong>rapist who is in an excellent position to advise staff<br />
<strong>of</strong> preventative and back saving advice. Staff identified with MSK injury are <strong>of</strong>fered same day<br />
physio<strong>the</strong>rapy or at <strong>the</strong>ir earliest convenience. Regular <strong>update</strong>s are given to occupational health.<br />
O<strong>the</strong>r Occupational Health Services <strong>of</strong>fered are:<br />
1 pre-employment occupational health assessments<br />
2 ergonomic work station assessments<br />
3 return-to-work programmes.<br />
Since July 2010 <strong>the</strong>re has been a rheumatology video link service with <strong>the</strong> consultant in<br />
Aberdeen. It is run once an month by a senior MSK physio<strong>the</strong>rapist. Additional training in<br />
injection will extend <strong>the</strong> service. The patients are seen jointly by <strong>the</strong> <strong>the</strong>rapist and consultant<br />
and booked for fur<strong>the</strong>r treatment at this clinic and given exercise advice at <strong>the</strong> time <strong>of</strong> <strong>the</strong><br />
consultation.<br />
Publication <strong>of</strong> <strong>the</strong> results <strong>of</strong> this model <strong>of</strong> care is awaited.<br />
Video Capture Gait <strong>An</strong>alysis<br />
Richard Bailey<br />
richard.bailey2@nhs.net<br />
0<strong>18</strong>56 888231<br />
A gait analysis assessment procedure is currently being developed. Using a video camera to<br />
cache to a memory stick all <strong>the</strong> patient assessments done on a treadmill. Using pre- and posttreatment<br />
gait analysis as an audit tool to assess objectively <strong>the</strong> effectiveness <strong>of</strong> treatment. This<br />
information can also be sent to o<strong>the</strong>r practitioners who may be involved in <strong>the</strong>ir care, giving<br />
an excellent visual account <strong>of</strong> <strong>the</strong> patient’s problems. Data can be re-examined via slow motion<br />
replay in order to help augment appropriate treatment plan.<br />
Gait analysis is <strong>of</strong>fered as part <strong>of</strong> routine physio<strong>the</strong>rapy assessment.<br />
41<br />
mskscoping<strong>2011</strong>-rs.indd 41 03/11/<strong>2011</strong> 11:01
<strong>Joint</strong> <strong>effects</strong> <strong>2011</strong><br />
NHS Shetland<br />
Musculoskeletal Podiatry Service<br />
Bruce McCulloch<br />
bruce.mcculloch@nhs.net<br />
01595 743202<br />
This service is based on a joint approach to patient care with physio<strong>the</strong>rapy, orthotics and<br />
medical imaging. Clinics take place in an out-patient physio<strong>the</strong>rapy department with access<br />
to plain x-ray to support diagnosis via direct referral to medical imaging. Our practitioners are<br />
qualified to prescribe appropriate medication for patients using <strong>the</strong> service.<br />
Improvements measured: suggestion made about <strong>the</strong> language used in <strong>the</strong> original leaflet and<br />
subsequent changes were made and approved.<br />
Outcomes measured: number <strong>of</strong> processes in <strong>the</strong> patient journey following <strong>the</strong> LEAN method,<br />
and a time and cost analysis.<br />
Occupational Therapy Service<br />
Occupational Therapy Service<br />
duty.ot@shetland.gov.uk<br />
01595 744319<br />
This service evolved when services were merged in 2009 because <strong>of</strong> lengthy waiting lists and<br />
duplication <strong>of</strong> processes. It operates an open referral system for patients suffering any condition<br />
resulting in a functional difficulty with performing daily living activities.<br />
NHS Tayside<br />
Advanced Physio<strong>the</strong>rapy Practitioner and GPwSI, MSK Primary Care<br />
Triage Service<br />
Janice McNee<br />
janice.mcnee@nhs.net<br />
01382 425668<br />
This service <strong>of</strong>fers a twice-weekly clinic which can accommodate up to 15% <strong>of</strong> all patients<br />
who are referred to <strong>the</strong> Physio<strong>the</strong>rapy Department. The clinic demonstrates a successful<br />
multidisciplinary approach in that APPs, podiatrists and GPwSI all share knowledge ensuring a<br />
cost-effective service with an improved patient journey. If patients require onward referral all<br />
investigations have already taken place, <strong>the</strong>refore waiting times are minimized. With <strong>the</strong> ability<br />
to order diagnostics o<strong>the</strong>r conditions, e.g. ovarian cysts and brain tumours, have been identified<br />
enabling patients to access <strong>the</strong> most effective management sooner.<br />
Improvements measured: reduction in orthopaedic waiting times, number <strong>of</strong> referrals to<br />
secondary care.<br />
Outcomes measured: survey in 2008 showed health outcomes improved measurably with 95%<br />
<strong>of</strong> patients assessed saying that <strong>the</strong>y had improved VAS recorded before and after completion <strong>of</strong><br />
treatment.<br />
42<br />
mskscoping<strong>2011</strong>-rs.indd 42 03/11/<strong>2011</strong> 11:01
<strong>Joint</strong> <strong>effects</strong> <strong>2011</strong><br />
Injection Therapy Expansion<br />
Janice McNee<br />
janice.mcnee@nhs.net<br />
01382 425668<br />
Injection <strong>the</strong>rapy has been used as a treatment option since 2001. The Patient Group Directive<br />
allows independent supply and administration <strong>of</strong> appropriate medication. Baseline information<br />
is recorded including medication name, dose and manufacturer’s number, and <strong>the</strong>n forwarded<br />
to <strong>the</strong> patient’s GP for information.<br />
Improvements measured: reduction in orthopaedic waiting times and number <strong>of</strong> referrals to<br />
secondary care.<br />
Outcomes measured: VAS, and patients’ perception <strong>of</strong> normality.<br />
Musculoskeletal Out-patient Services – General<br />
<strong>An</strong>gela Murphy<br />
angelamurphy@nhs.net<br />
01241 822514<br />
Lower Limb Biomechanics Clinic<br />
Mike Black<br />
mikeblack@nhs.net<br />
01382 425668<br />
Orthopaedic Screening in Secondary care<br />
Janice McNee<br />
janice.mcnee@nhs.net<br />
01382 425668<br />
Rheumatology<br />
Alison Knight<br />
alisonknight@nhs.net<br />
01382 425668<br />
General MSK out-patient services are provided across Tayside. Five departments in <strong>An</strong>gus (in<br />
each <strong>of</strong> <strong>the</strong> towns), two departments in Dundee (one in acute hospital and one in community<br />
health and care centre) and five departments in Perth and Kinross (in <strong>the</strong> city and towns). Each<br />
area accepts referrals from GPs, consultants, o<strong>the</strong>r healthcare pr<strong>of</strong>essionals, and self referral.<br />
Biomechanical clinics are staffed by a podiatrist and physio<strong>the</strong>rapist, combining <strong>the</strong> knowledge<br />
and skills <strong>of</strong> podiatry and physio<strong>the</strong>rapy to assess and treat patients with lower limb disorders<br />
associated with changes in <strong>the</strong> functional structure <strong>of</strong> <strong>the</strong> ankle/foot complex. The aim is to<br />
improve <strong>the</strong> patient journey and reduce waiting times for each discipline by providing a holistic<br />
package <strong>of</strong> care. This service is based in Dundee but accepts referrals from all Tayside.<br />
Physio<strong>the</strong>rapists screen referrals coming into <strong>the</strong> Orthopaedic Department, provide assessment,<br />
diagnosis and treatment <strong>of</strong> patients referred to Orthopaedics by Tayside GPs.<br />
A one-stop multidisciplinary inflammatory joint disease clinic where patients are immediately<br />
assessed and treated appropriately. Patients can be discharged by physio<strong>the</strong>rapists and OTs<br />
<strong>the</strong>reby reducing consultant waiting lists and improving patient care.<br />
Improvements measured: reduction in rheumatology waiting times.<br />
Outcomes measured: VAS recorded before and after completion <strong>of</strong> treatment.<br />
43<br />
mskscoping<strong>2011</strong>-rs.indd 43 03/11/<strong>2011</strong> 11:01
<strong>Joint</strong> <strong>effects</strong> <strong>2011</strong><br />
Trauma and Elective Hand Clinics<br />
Sarah Dalgleish<br />
sarah.dalgleish@nhs.net<br />
01382 425668<br />
These plastic surgery hand clinics are staffed by OTs and physio<strong>the</strong>rapists, who assess and treat<br />
patients appropriately and are <strong>the</strong>n able to discharge <strong>the</strong>m without consultant follow up. This<br />
enables waiting lists to be reduced and improves patient care.<br />
Improvements measured: reduction in plastic surgery waiting times.<br />
Outcomes measured: TAM scores, VAS recorded before and after completion <strong>of</strong> treatment.<br />
Virtual Ward (Community Rehabilitation)<br />
Denise Connon<br />
denise.connon@nhs.net<br />
01382 425665<br />
The aim <strong>of</strong> <strong>the</strong> virtual ward construct is to provide a co-ordinated, multidisciplinary approach<br />
to identifying people living with long-term conditions and to intervene earlier in <strong>the</strong>ir disease<br />
trajectory to improve quality <strong>of</strong> life and reduce use <strong>of</strong> unplanned health and social care services.<br />
The principles <strong>of</strong> <strong>the</strong> Virtual Ward have been prioritised in NHS Tayside through Steps to Better<br />
Health and recently aligned within new overarching Integrated Community Services (ICS) work<br />
streams in each CHP.<br />
Four Dundee and three Perth practices are involved in <strong>the</strong> first wave.<br />
Working Health Services<br />
Cathy Grieve<br />
cathy.grieve@nhs.net<br />
01382 825100<br />
This new NHS service was launched in 2008, it aims to assist employees (who live and/or work in<br />
NHS Tayside) <strong>of</strong> small to medium-sized enterprises (SMEs) to remain in or return to work quickly<br />
after a period <strong>of</strong> absence. SMEs are companies with less than 250 employees and most do not<br />
provide access to Occupational Health services. The service <strong>of</strong>fers access to a range <strong>of</strong> services<br />
including physio<strong>the</strong>rapy, case management, occupational <strong>the</strong>rapy and counselling.<br />
Outcomes measured include: COPM, EQ5D and HADS, assessments are completed at entry and<br />
discharge from <strong>the</strong> programme.<br />
44<br />
mskscoping<strong>2011</strong>-rs.indd 44 03/11/<strong>2011</strong> 11:01
<strong>Joint</strong> <strong>effects</strong> <strong>2011</strong><br />
NHS Western Isles<br />
Musculoskeletal Physio<strong>the</strong>rapy, class-based exercise groups<br />
Sheila Nicolson<br />
sheila.nicolson@nhs.net<br />
Self Referral Clinic at <strong>the</strong> Physio<strong>the</strong>rapy Department<br />
Sheila Nicolson and Nico Groenendijk<br />
sheila.nicolson@nhs.net<br />
nico.groenendijk@nhs.net<br />
0<strong>18</strong>51 708258<br />
Physio<strong>the</strong>rapy Services across Western Isles<br />
Nico Groenendijk<br />
nico.groenendijk@nhs.net<br />
0<strong>18</strong>51 704704 ext. 2258<br />
Following an audit <strong>of</strong> <strong>the</strong> type <strong>of</strong> condition referrals to OP MSK Physio<strong>the</strong>rapy, class-based<br />
exercise groups have been initiated in <strong>the</strong> Physio<strong>the</strong>rapy Department, Western Isles Hospital.<br />
A Back to Fitness class was commenced in June 2009 for clients with chronic low back pain. A<br />
Lower Limb class was commenced in July 2010. Both <strong>of</strong> <strong>the</strong>se classes are led by a physio<strong>the</strong>rapy<br />
clinical support worker. The classes are based on six weekly circuit classes, consisting <strong>of</strong> warmup,<br />
stretches, circuit-based exercise and relaxation. All clients are assessed prior to attending<br />
<strong>the</strong> classes, clients for <strong>the</strong> Back to Fitness class using <strong>the</strong> Roland-Morris Disability questionnaire,<br />
clients for <strong>the</strong> Lower Limb class, using both <strong>the</strong> KOOS knee survey or <strong>the</strong> Aggregated<br />
Locomotor Function (ALF) score. These classes are audited regularly and <strong>the</strong> outcome <strong>of</strong><br />
attendance assessed. Overall <strong>the</strong> outcomes and feedback are excellent.<br />
There is a weekly self referral clinic at <strong>the</strong> Physio<strong>the</strong>rapy Department, Western Isles Hospital,<br />
Stornoway. This commenced in September 2008. This drop-in clinic allows patients to self<br />
refer to Physio<strong>the</strong>rapy without having to attend <strong>the</strong>ir GP first. The DIC operates every Thursday<br />
afternoon, from 3.00 pm to 5.00 pm.<br />
By July <strong>2011</strong> approximately 3,000 attendees had self referred via this route. Ongoing patient<br />
satisfaction surveys <strong>of</strong> DIC clients indicate that this service is well received, feedback has been<br />
very positive.<br />
NHS Western Isles Physio<strong>the</strong>rapy Department employ an extended scope practitioner, who<br />
works in <strong>the</strong> orthopaedic clinic and fracture clinic. The ESP currently vets <strong>the</strong> orthopaedic<br />
waiting list and is able to assess and treat patients directly from this list. He is also able to list for<br />
surgery, administer cortico-steroid injections, refer onwards to o<strong>the</strong>r specialised centres, request<br />
plain x-ray, CT and MRI and ultrasound. The ESP routinely reviews all post-elective arthroplasty<br />
patients and post-operative hip fractures in <strong>the</strong> orthopaedic clinic. This service has helped to<br />
reduce orthopaedic waiting times and provides a more streamlined service.<br />
There are discussions taking place as to how <strong>the</strong> ESP post could support a remote rheumatology<br />
service to NHS Western Isles in <strong>the</strong> future.<br />
45<br />
mskscoping<strong>2011</strong>-rs.indd 45 03/11/<strong>2011</strong> 11:01
<strong>Joint</strong> <strong>effects</strong> <strong>2011</strong><br />
Podiatry Musculoskeletal Service – Western Isles<br />
Sarann Macphee<br />
smacphee1@nhs.net<br />
0<strong>18</strong>51 704704 ext. 2289<br />
Western Isles Podiatry Service <strong>of</strong>fers musculoskeletal services in a number <strong>of</strong> forms. The<br />
biomechanics clinic is based at <strong>the</strong> Western Isles Hospital and <strong>of</strong>fers a specialised assessment<br />
service and management for lower limb musculoskeletal pathologies or gait dysfunctions.<br />
Referrals for <strong>the</strong> clinic may originate from <strong>the</strong> areas <strong>of</strong> rheumatology, orthopaedics, paediatrics,<br />
fellow podiatrists, allied health pr<strong>of</strong>essionals, GPs and patient self referral. This clinic is<br />
conducted by <strong>the</strong> musculoskeletal specialist podiatrist. <strong>Joint</strong> consultations with fellow clinicians<br />
can be arranged to ease <strong>the</strong> burden <strong>of</strong> multiple visits on <strong>the</strong> individual and aim to improve<br />
clinical outcomes. This activity most frequently occurs with <strong>the</strong> paediatric physio<strong>the</strong>rapist.<br />
All clinicians in <strong>the</strong> department are specialist general practitioners as a minimum and as such are<br />
experienced in <strong>the</strong> management <strong>of</strong> general biomechanical and musculoskeletal complaints. This<br />
permits wide and frequent patient access through outreach clinics. There is a continuous audit<br />
cycle <strong>of</strong> orthotic provision and effectiveness.<br />
A specialised orthotic manufacturing laboratory is located at <strong>the</strong> Western Isles Hospital which<br />
allows clinicians to make, adjust or provide custom functional and accommodative or modified<br />
pre-made appliances, greatly aiding compliance, and <strong>the</strong> speed/ease <strong>of</strong> modification. This asset<br />
is also utilised by <strong>the</strong> visiting orthotist service.<br />
46<br />
mskscoping<strong>2011</strong>-rs.indd 46 03/11/<strong>2011</strong> 11:01
<strong>Joint</strong> <strong>effects</strong> <strong>2011</strong><br />
Glossary<br />
ACL<br />
<strong>An</strong>terior cruciate ligament<br />
MCN<br />
Managed Clinical Network<br />
AHP<br />
Allied health pr<strong>of</strong>essional – a who’s who can be found at<br />
MDT<br />
Multidisciplinary team<br />
www.scotland.gov.uk/Topics/Health/NHS-Scotland/chpo/whoareahps<br />
MRI<br />
Magnetic resonance imaging<br />
CARE<br />
CH(C)PS<br />
The Consultation and Relational Empathy (CARE) measure, an<br />
outcome measure supported by Scottish Government<br />
Community Health (and Care) Partnerships<br />
MSK<br />
MYMOP<br />
Musculoskeletal (to do with muscles, bones and joints)<br />
Measure your own outcome pr<strong>of</strong>ile – a patient-completed outcome<br />
measure<br />
CHP<br />
Community Health Partnership<br />
NMAHP<br />
Nursing, Midwifery and Allied Health Pr<strong>of</strong>essions<br />
COPM<br />
Canadian Occupational Performance Measure<br />
OA<br />
Osteoarthritis<br />
CT<br />
Computerised tomography scanner<br />
OT<br />
Occupational <strong>the</strong>rapist<br />
DAPOS<br />
DASH<br />
EMS<br />
ENT<br />
Questionnaire designed to measure depression, anxiety and positive<br />
outlook in people who suffer from pain<br />
A shoulder outcome measure<br />
Elderly Mobility Scale<br />
Ear nose and throat<br />
PACs<br />
PMS<br />
PT<br />
STarT Back<br />
Picture archiving and communication system<br />
Patient management system<br />
Physio<strong>the</strong>rapist<br />
Back pain specific screening tool developed by Keele University<br />
available at www.keele.ac.uk/sbst/<br />
EQ5D, EQ5D5L<br />
ESP<br />
GPwSI<br />
HADS<br />
IM&T<br />
IT<br />
KOOS<br />
LBP<br />
Standardised quality <strong>of</strong> life outcome measures available from <strong>the</strong><br />
EUROQOL group (www.euroqol.org)<br />
Extended scope practitioner<br />
Genereral practitioner with special interest<br />
The Hospital <strong>An</strong>xiety <strong>An</strong>d Depression Scale<br />
Information management and technology<br />
Information technology<br />
Knee and Osteoarthritis Outcome Score<br />
Low back pain<br />
STarT MSK<br />
TAM<br />
THJR<br />
TI<br />
TMJ<br />
TSK<br />
VAS<br />
WOMAC<br />
General MSK screening tool under development at Keele University<br />
Total active motion<br />
Total hip joint replacement<br />
Technical instructor<br />
Tempromandibular <strong>Joint</strong><br />
Tampa Scale <strong>of</strong> Kinesiophobia<br />
Visual <strong>An</strong>alogue Scale<br />
The WOMAC® Index s self-administered score and assesses <strong>the</strong><br />
three dimensions <strong>of</strong> pain, disability and joint stiffness in knee and<br />
LEAN<br />
A production practice that considers <strong>the</strong> expenditure <strong>of</strong> resources<br />
hip osteoarthritis using 24 questions.<br />
for any goal o<strong>the</strong>r than <strong>the</strong> creation <strong>of</strong> value for <strong>the</strong> end customer<br />
to be wasteful, and thus a target for elimination.<br />
47<br />
mskscoping<strong>2011</strong>-rs.indd 47 03/11/<strong>2011</strong> 11:01
over<br />
1 million<br />
people each<br />
year see <strong>the</strong>ir<br />
GP for an MSK<br />
condition<br />
15,000<br />
people had hip<br />
and knee replacement<br />
operations in 2010<br />
7,000 more than<br />
in 2000<br />
5.2<br />
million<br />
people live<br />
in Scotland<br />
Over half a<br />
million people<br />
see <strong>the</strong>ir GP<br />
for back pain<br />
each year<br />
over 400,000<br />
referrals into<br />
AHP MSK services<br />
each year<br />
mskscoping<strong>2011</strong>-rs.indd 48 03/11/<strong>2011</strong> 11:01




![Dr Matthew Checketts, NHS Tayside [PDF - 6Mb] - 18 Weeks](https://img.yumpu.com/49027155/1/190x143/dr-matthew-checketts-nhs-tayside-pdf-6mb-18-weeks.jpg?quality=85)


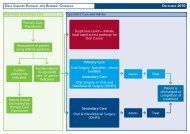


![Mark Sindall, NHS Dumfries and Galloway [PDF - 227Kb] - 18 Weeks](https://img.yumpu.com/30080335/1/190x143/mark-sindall-nhs-dumfries-and-galloway-pdf-227kb-18-weeks.jpg?quality=85)