FINAL PROGRAM 6TH EDITION - EuroMediCom
FINAL PROGRAM 6TH EDITION - EuroMediCom
FINAL PROGRAM 6TH EDITION - EuroMediCom
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
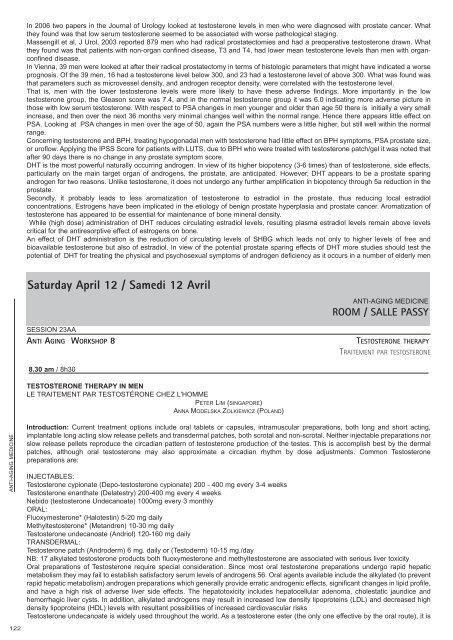
In 2006 two papers in the Journal of Urology looked at testosterone levels in men who were diagnosed with prostate cancer. Whatthey found was that low serum testosterone seemed to be associated with worse pathological staging.Massengill et al, J Urol, 2003 reported 879 men who had radical prostatectomies and had a preoperative testosterone drawn. Whatthey found was that patients with non-organ confined disease, T3 and T4, had lower mean testosterone levels than men with organconfineddisease.In Vienna, 39 men were looked at after their radical prostatectomy in terms of histologic parameters that might have indicated a worseprognosis. Of the 39 men, 16 had a testosterone level below 300, and 23 had a testosterone level of above 300. What was found wasthat parameters such as microvessel density, and androgen receptor density, were correlated with the testosterone level.That is, men with the lower testosterone levels were more likely to have these adverse findings. More importantly in the lowtestosterone group, the Gleason score was 7.4, and in the normal testosterone group it was 6.0 indicating more adverse picture inthose with low serum testosterone. With respect to PSA changes in men younger and older than age 50 there is initially a very smallincrease, and then over the next 36 months very minimal changes well within the normal range. Hence there appears little effect onPSA. Looking at PSA changes in men over the age of 50, again the PSA numbers were a little higher, but still well within the normalrange.Concerning testosterone and BPH, treating hypogonadal men with testosterone had little effect on BPH symptoms, PSA prostate size,or uroflow. Applying the IPSS Score for patients with LUTS, due to BPH who were treated with testosterone patch/gel it was noted thatafter 90 days there is no change in any prostate symptom score.DHT is the most powerful naturally occurring androgen. In view of its higher biopotency (3-6 times) than of testosterone, side effects,particularly on the main target organ of androgens, the prostate, are anticipated. However, DHT appears to be a prostate sparingandrogen for two reasons. Unlike testosterone, it does not undergo any further amplification in biopotency through 5a reduction in theprostate.Secondly, it probably leads to less aromatization of testosterone to estradiol in the prostate, thus reducing local estradiolconcentrations. Estrogens have been implicated in the etiology of benign prostate hyperplasia and prostate cancer. Aromatization oftestosterone has appeared to be essential for maintenance of bone mineral density.While (high dose) administration of DHT reduces circulating estradiol levels, resulting plasma estradiol levels remain above levelscritical for the antiresorptive effect of estrogens on bone.An effect of DHT administration is the reduction of circulating levels of SHBG which leads not only to higher levels of free andbioavailable testosterone but also of estradiol. In view of the potential prostate sparing effects of DHT more studies should test thepotential of DHT for treating the physical and psychosexual symptoms of androgen deficiency as it occurs in a number of elderly menSaturday April 12 / Samedi 12 AvrilSESSION 23AAANTI AGING WORKSHOP 8 TESTOSTERONE THERAPY8.30 am / 8h30TESTOSTERONE THERAPY IN MENLE TRAITEMENT PAR TESTOSTÉRONE CHEZ L'HOMMEPETER LIM (SINGAPORE)ANNA MODELSKA ZOLKIEWICZ (POLAND)ANTI-AGING MEDICINEROOM / SALLE PASSYTRAITEMENT PAR TESTOSTERONEANTI-AGING MEDICINEIntroduction: Current treatment options include oral tablets or capsules, intramuscular preparations, both long and short acting,implantable long acting slow release pellets and transdermal patches, both scrotal and non-scrotal. Neither injectable preparations norslow release pellets reproduce the circadian pattern of testosterone production of the testes. This is accomplish best by the dermalpatches, although oral testosterone may also approximate a circadian rhythm by dose adjustments. Common Testosteronepreparations are:INJECTABLES:Testosterone cypionate (Depo-testosterone cypionate) 200 - 400 mg every 3-4 weeksTestosterone enanthate (Delatestry) 200-400 mg every 4 weeksNebido (testosterone Undecanoate) 1000mg every 3 monthlyORAL:Fluoxymesterone* (Halotestin) 5-20 mg dailyMethyltestosterone* (Metandren) 10-30 mg dailyTestosterone undecanoate (Andriol) 120-160 mg dailyTRANSDERMAL:Testosterone patch (Androderm) 6 mg. daily or (Testoderm) 10-15 mg./dayNB: 17 alkylated testosterone products both fluoxymesterone and methyltestosterone are associated with serious liver toxicityOral preparations of Testosterone require special consideration. Since most oral testosterone preparations undergo rapid hepaticmetabolism they may fail to establish satisfactory serum levels of androgens 56. Oral agents available include the alkylated (to preventrapid hepatic metabolism) androgen preparations which generally provide erratic androgenic effects, significant changes in lipid profile,and have a high risk of adverse liver side effects. The hepatotoxicity includes hepatocellular adenoma, cholestatic jaundice andhemorrhagic liver cysts. In addition, alkylated androgens may result in increased low density lipoproteins (LDL) and decreased highdensity lipoproteins (HDL) levels with resultant possibilities of increased cardiovascular risksTestosterone undecanoate is widely used throughout the world. As a testosterone ester (the only one effective by the oral route), it is122