Havva Dashtdar, Hussin A. Rothan, Terence Tay, Raja Elina Ahmad ...
Havva Dashtdar, Hussin A. Rothan, Terence Tay, Raja Elina Ahmad ...
Havva Dashtdar, Hussin A. Rothan, Terence Tay, Raja Elina Ahmad ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
A Preliminary Study Comparing the Use of Allogenic ChondrogenicPre-Differentiated and Undifferentiated Mesenchymal Stem Cells forthe Repair of Full Thickness Articular Cartilage Defects in Rabbits<strong>Havva</strong> <strong>Dashtdar</strong>, <strong>Hussin</strong> A. <strong>Rothan</strong>, <strong>Terence</strong> <strong>Tay</strong>, <strong>Raja</strong> <strong>Elina</strong> <strong>Ahmad</strong>, Razif Ali, Liang Xin <strong>Tay</strong>, Pan Pan Chong, Tunku KamarulTissue Engineering Group, NOCERAL, Faculty of Medicine, Department of Orthopaedic Surgery, University of Malaya, Kuala Lumpur, MalaysiaReceived 21 December 2010; accepted 28 February 2011Published online 28 March 2011 in Wiley Online Library (wileyonlinelibrary.com). DOI 10.1002/jor.21413ABSTRACT: Chondrogenic differentiated mesenchymal stem cells (CMSCs) have been shown to produce superior chondrogenic expressionmarkers in vitro. However, the use of these cells in vivo has not been fully explored. In this study, in vivo assessment of cartilagerepair potential between allogenic-derived chondrogenic pre-differentiated mesenchymal stem cells and undifferentiated MSCs (MSCs)were compared. Bilateral full thickness cartilage defects were created on the medial femoral condyles of 12 rabbits (n ¼ 12). Rabbitswere divided into two groups. In one group, the defects in the right knees were repaired using alginate encapsulated MSCs while in thesecond group, CMSCs were used. The animals were sacrificed and the repaired and control knees were assessed at 3 and 6 months afterimplantation. Quantitative analysis was performed by measuring the Glycosaminoglycans (GAGs)/total protein content. The meanBrittberg score was higher in the transplanted knees as compared to the untreated knee at 6 months (p < 0.05). Quantitative analysisof GAGs was consistent with these results. Histological and immunohistochemical analysis demonstrated hyaline-like cartilage regenerationin the transplanted sites. Significant differences between the histological scores based on O’Driscoll histological grading wereobserved between contralateral knees at both 3 and 6 months (p < 0.05). No significant differences were observed between the Britberg,O’Driscoll scores, and GAGs/total protein content when comparing defect sites treated with MSC and CMSC (p > 0.05). This studydemonstrates that the use of either MSC or CMSC produced superior healing when compared to cartilage defects that were untreated.However, both cells produced comparable treatment outcomes. ß 2011 Orthopaedic Research Society. Published by Wiley Periodicals,Inc. J Orthop Res 29:1336–1342, 2011Keywords:mesenchymal stem cell; chondrogenic differentiation; cartilage repairDamage to cartilage tissue as the result or trauma ordisease conditions are becoming increasingly common.The poor vascular properties of cartilage tissue makeshealing extremely difficult especially in the presenceof full thickness articular cartilage defects. Cellulartherapy has been considered a successful treatmentoption and has demonstrated to produce superior tissuerepair quality as compared to conventional surgeryin many studies. 1–6Autologous chondrocyte implantation (ACI) hasbeen used in many clinical trials and has beenreported to produce good outcomes in previous literatures.7 However, the use of ACI has several limitations.These include donor site morbidity, cellulardedifferentiation when cultured in vitro and thereduced ability to maintain good long-term tissuerepair. 8 To overcome these issues, mesenchymal stemcells (MSCs) have emerged as an alternative cellsource. One of the main characteristics of MSCs is itsmultipotency; that is, MSCs do not de-differentiateduring in vitro cell culture and will continue to be aprogenitor for other cell types despite being removedfrom its original environment. 9Through previous studies, allogenic or autologousbone marrow (BM) derived MSCs have been encapsulatedinto different scaffolds with or without theaddition of growth factors to treat cartilage defects invarious animal models. 10–14 It has been reported thatCorrespondence to: Tunku Kamarul (T: þ60-3-7949-2061; F: þ60-3-7949-4642; E-mail: tkzrea@yahoo.com)ß 2011 Orthopaedic Research Society. Published by Wiley Periodicals, Inc.the transplantation of BM-derived MSCs in cartilagedefects provide good repair outcomes. 3 However, invivo assessments of chondrogenic pre-differentiatedMSCs (CSMCs) to repair full thickness cartilage defecthave not been previously demonstrated and thereforewarrants further investigations. This is importantconsidering that lineage committed cells have shownto produce superior chondrogenic expression markersthan those of undifferentiated MSCs. 15 In this study,alginate gel encapsulated MSCs supplemented withtransforming growth factor-b3 (TGF-b3) and fibroblastgrowth factor-basic (BFGF) to produce CMSCs wereimplanted in cartilage defects and compared to undifferentiatedMSCs.The objective of this study was to evaluate therepair outcomes of full thickness cartilage defect usingMSCs and CMSCs in rabbit knees at 3 and 6 months.MATERIAL AND METHODSFourteen New Zealand White male rabbits (15- to 16-weekold, 2–3 kg) used in this study was in accordance with theguidelines of the Animal Care and Use Committee and,institutional review board in University of Malaya (Referencenumber: OS/10/11/2008/HD(R).Isolation and Culture of Bone Marrow-Derived MesenchymalStem CellsTwo of these rabbits were sacrificed for BM harvesting duringthe MSC isolation stage. BM was harvested in sterile conditionsfrom the femur, tibia, and humerus using a bone cutterand an aspirator. Two milliliters of BM was mixedthoroughly with the same amount of phosphate buffer saline(PBS, pH 7.2) supplemented with 1% penicillin/streptomycin1336 JOURNAL OF ORTHOPAEDIC RESEARCH SEPTEMBER 2011
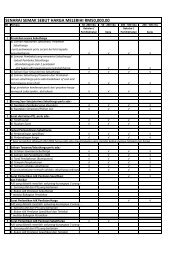
CHONDROGENIC PRE-DIFFERENTIATED AND UNDIFFERENTIATED MSCs IN CARTILAGE REPAIR 1337(Invitrogen, Carlsbad, CA). The diluted BM was layered onto3 ml of Ficol Paque (Amersham Biosciences, Uppsala, Sweden)in 15 ml centrifuge tubes and centrifugated at 2,500 rpmfor 25 min. The buffy coat was extracted and washed usingDMEM low glucose supplemented with 1% penicillin/streptomycinand 1% L-glutamine by spinning at 1,600 rpm for10 min. The resulting pellet (mononuclear cells) was suspendedin growth medium DMEM-LG supplemented with10% fetal bovine serum (FBS) and cultured in 75 cm 2 tissueculture flasks (Nunc, Rockside, Denmark). Cell culturemedium was changed every 3 days and the cells were culturedand expanded until passage 3 (P3) in a humidified incubatorat 378C, 5% CO 2 . Cell viability was verified at each passageusing Trypan blue exclusion dye method prior to cell counting.All MSCs used for transplantation were at passage 3.MSCs Seeding in Alginate BeadsMSCs were harvested using TrypLE TM Express at P3 andsuspended in 1.2% sterile alginate solution (Sigma–Aldrich,St. Louis, MO) in 0.15 M sodium chloride at cells densities of1 10 6 cells/ml. The cell suspension was dropped into a102 mM calcium chloride solution using a syringe. Theresulting beads were washed with 0.15 M sodium chlorideafter 10 min of polymerization and transferred into 2 ml ofgrowth medium (DMEM supplemented with 10% FBS). MSCalginate constructs in growth medium were prepared justbefore being transplanted into the knee defects (Group 1). Toprepare CMSCs, the mesenchymal cells were cultured at P3in defined medium containing 40 mg/ml Ascorbate-2-Phosphate(Sigma–Aldrich, St. Louis, MO), 1 mM sodium pyruvate,40 mg/ml proline (Sigma–Aldrich), 0.003 M dexamethasone(Sigma–Aldrich), 1 insulin–transferrin–selenium, 10 ng/mlTGF-b3, and 10 ng/ml BFGF. The cells were maintained incell culture incubator at 378C and 5% CO 2 for 3 weeks(Group 2). Characterization of MSCs and CMSCs wereassessed as described in previous studies. 16 CMSCs used fortransplantations were at passage 3.Creation of Cartilage DefectTwelve (n ¼ 12) rabbits were equally divided into twogroups. Each animal underwent surgery to create fullthickness cartilage defects on the articular surface of theweight-bearing medial femoral condyle of both knees (hindlegs). The defects were created using a custom-made cylindricalchondrotome (Fig. 1A), and standardized according to thefollowing dimensions: 5 mm diameter and approximately1 mm depth (or until cartilage tissue were completelyremoved, as observed under 5 magnification). Care wastaken to not violate the subchondral bone. Total removal ofcartilage tissue was confirmed using observations madeunder the aid of a microsurgical microscope.Transplantation of Cell Alginate ConstructsTransplantations of the MSC and CMSC constructs into thedefective areas (i.e., right knee in each respective group)were conducted approximately 3–4 weeks following theinitial defect creation procedure. The transplanted cells wereobtained only from rabbits of the same litter. The left kneewas left untouched until the end of the experiment,representing the control group of the study. A periosteal flapwas used to hold the alginate beads at the defect area usingmicrosurgical sutures (Nylon 9-0) and fibrin glue.Post-operatively, antibiotics and analgesia were administeredfor 3 consecutive days. No wound infection wasFigure 1. Gross morphology. (A) Defect was created in the medial chondyle of the knee. (B) Right knee (treatment) 3 months afterCMSCs implantation. (C) Left knee (control) defect with an irregular surface observed at 3 months. (D) Right and left knees of CMSCstreated rabbits 6 months after implantation. In the right knee, repair tissue appears smoother and homogenous than the left.JOURNAL OF ORTHOPAEDIC RESEARCH SEPTEMBER 2011
1338 DASHTDAR ET AL.observed in any of the rabbits. The rabbits moved freelywithin their cages and were sacrificed at 3 and 6 monthsafter transplantation.Morphological AnalysisThe quality of cartilage tissues in both knees were comparedby two independent observer, in accordance to the Brittberg/International Cartilage Research Society (ICRS) morphologicalscore and general histological evaluation. 17,18Histology and Immunohistology ApplicationThe distal femur was cut and the medial condyle was dividedinto two equal parts using a saw. Half of the sample used forhistology. These samples were fixed in 10% buffered formalinfor 48–72 h, and decalcified in 10% formic acid. The specimenswere processed for histological slides, embedded in paraffin,and cut into 5 mm sections. The slides were stained usinghematoxylin and eosin (H&E), Safranin O Fast green andimmunohistochemical staining for collagen type II. Immunohistochemistryfor collagen type II was performed usingprimary antibody anticollagen type II (mouse-anti-rabbit;Merck, Darmstadt, Germany) in 1:100 dilution and accordingto the company protocol (DakoCytomation, Glostrup, Denmark).The histology images were analyzed using O’Driscollhistological scoring as previously described. 19Biochemical AnalysisProtein and glycosaminoglycan (GAGs) were determinedusing Bio-Rad DC protein assay kit (Bio-Rad Laboratories,Richmond, CA) and Blyscan sulfated Glycosaminoglycanassay kit (Biocolor Ltd., Country Antrim, UK) according topreviously established methods 20 or based on the manufacturer’sprotocols. Spectrophotometer absorbance measurementswere performed at 750 and 656 nm for protein andGAG assays, respectively. GAG content was normalizedaccording to the protein contents (mg GAG/mg protein).Statistical AnalysisGrading scores obtained from the Brittberg, O’Driscollmeasures and GAGs contents were statistically analyzedusing Wilcoxon signed-rank test available on the statisticalsoftware package SPSS (version 17.0). To compare thesignificant differences of values between the two experimentgroups and, between treatment and control groups, Mann–Whitney tests were conducted accordingly.RESULTSMorphological ObservationThe gross morphological appearances of the regeneratedcartilage tissues filling in the defects (Fig. 1A) at3 months post-transplantation are shown (Fig. 1B andC). The Brittberg’s scores for the MSC and CMSCgroups were significantly higher than their respectivecontrols (8.17 1.83 vs. 7.00 2.28 for MSC andCMSC, respectively; p < 0.05). There were significantdifferences in the Brittberg Score of transplantedknees in both groups treated with MSCs at 6 months(7.50 1.38 points) to that of the untreated knees(4.50 1.38 points). CMSC-treated knees demonstratedbetter result as compared to MSCs group(9.00 2.00 vs. 7.33 1.53). However, these differenceswere not statistically significant (Table 1).Figure 1D illustrates the gross appearance of theregenerated tissue between the MSC-treated and theuntreated defect at 6 months post-transplantation. Inthe MSC-treated knee, the regenerated cartilagetissues exhibited smooth glistening surface with lessdistinct demarcation of the defect border peripherally.In contrast, the regenerated tissues in the untreatedknee had rough surface and very distinct woundmargins.Histological and Histochemical AnalysisO’Driscoll histological scores of the post-implantationrepair tissue was significantly (p < 0.05) higher in thetransplanted sites when compared to the control sitesat 3 months (10.5 1.38 vs. 7.67 0.82) and 6 monthsTable 1. Summary of the Results Comparing the Treated (Right Knee) and Untreated (Left Knee) Groups , andComparing the MSC- and CMSC-Treated GroupsLeft Knee(Untreated)Knee Sidep-Value Cell Type Used (Comparing Right Knee)(WilcoxonSigned-RankTest)ComparingRight Knee(Treated)Left–RightKneesMSC CMSCp-Value(Mann–WhitneyU Signed-RankTest) ComparingMSC- andCMSC-TreatedKnees3 monthsBrittberg 7.00 2.28 8.17 1.83 0.336 7.33 1.53 9.00 2.00 0.317O’Driscoll 7.67 0.82 10.5 1.38 0.042 10.0 1.00 11.0 1.73 1.000GAG/protein 0.82 0.34 1.23 0.84 0.600 0.77 0.09 0.82 0.18 0.2756 monthsBrittberg 4.50 1.38 7.50 1.38 0.024 7.67 1.00 7.33 1.73 1.000O’Driscoll 8.67 1.86 11.8 1.47 0.026 11.6 2.08 12.0 1.00 0.655GAG/protein 0.82 0.10 1.36 0.16 0.046 1.67 0.14 1.29 0.38 0.052Data presented are mean values 1 SD. Statistical significant values (p < 0.05).JOURNAL OF ORTHOPAEDIC RESEARCH SEPTEMBER 2011
CHONDROGENIC PRE-DIFFERENTIATED AND UNDIFFERENTIATED MSCs IN CARTILAGE REPAIR 1339(11.8 1.47 vs. 8.67 1.86). However, there were nosignificant differences in these scores between theMSC and CMSC groups at 3 and 6 months (Table 1).The histology of the repaired sites obtained fromthe MSCs group after 3 months demonstrated a thinlayer of neocartilage forming and contained clusteredcells within the immature tissue (Fig. 2A). Therepaired tissue from CMSCs group at 6 months containedboth fibrocartilage and hyaline cartilage(Fig. 2C). In the control sites, the defects did notappear to undergo any repair process (Fig. 2B) or wereonly filled with fibrous tissue (Fig. 2B). Some sitesdemonstrated incomplete repair with hyaline like cartilage,but there were no vertical integration of thistissue with the subchondral bone. In some parts, thedefect was filled with bone (Fig. 3B). This repair tissueat 6 months demonstrated early signs of degenerationwith the presences of vertical fissures in the neocartilage(Fig. 3D). Immunohsitochemical staining showedhigher concentration of type II collagen in the transplantedtissues in both MSC and CMS than those inthe control sites (Fig. 3).The GAG content of the repaired tissue was verifiedqualitatively using Safranin O Fast green staining. Inthe transplanted groups, the repaired tissue stainedmore intensely for GAG within the intermediate anddeep zones as compared to that of the control sites(Fig. 4).Sulfated Glycoaminoglycans (GAG) AnalysisThe results of GAG quantitative analysis are summarizedin Table 1. Consistent with the morphological andhistological scores, the mean levels of GAG/proteinwere higher in the treated knees as compared to thecontrol knees at 3 and 6 months post-transplantation,Figure 2. Histology of the defect site of the rabbit’s knee inMSC-treated group (A,B) and CMSC-treated group (C,D) after 3and 6 months, respectively (H&E 10): Arrows point therepaired tissue in the right knees after 3 and 6 month ofimplantation.with no significant differences noted between the 2MSC groups at 3 months post-transplantation. Interestinglyhowever, there was a trend towards a higherGAG/protein level in the MSC group (1.67 0.14)compared to the CMSC groups (1.29 0.38), with thedifference being marginally close but did not reach thesignificance threshold (p ¼ 0.052).DISCUSSIONMesenchymal stem cells exhibit a stable phenotype invitro and have multilineage potential of differentiatinginto the adipocytes, chondrocytes, or osteocytes. 21 Invitro studies have suggested that the induction ofadult stem cells into chondrogenic lineage could beachieved via the introduction of soluble, biophysical,and 3D culturing environment factors. 22 The characteristicsof CMSCs were described in previous studies,which demonstrates an up-regulation of chondrogenicgenes, which included Sox9, COMP, as well as theexpression of GAG and type II collagen. 5,16 In thisstudy, the results demonstrated that CMSCs producedgood quality cartilage tissue as compared to theuntreated knees. Despite the ability of CMSCs to producebetter histological repair outcomes than MSCs,these differences were not significant. It may havebeen the case that the use of alginate gel for transplantingMSCs may have induced chondrogenic differentiation.It has been previously demonstrated thatalginate can independently induce chondrogenesis inBM stromal cells without the need of other stimulatingfactors. 23 The ideal microenvironment provided by thealginate gels has been shown to increase the cell–matrix signaling, which initiates and promotes the cellulardifferentiation process. 24 Because both cells typeswere encapsulated in alginate gel, the 3D environmentprovided by the alginate gel may have maintained therounded cell shape, thereby promoting chonrogenesis.22 It has been shown that the differentiation ofMSCs into a chondrogenic phenotype requires the cellsto maintain a rounded shape, which can be achievedthrough pellet encapsulation within a semi-solidmaterial, such as that provided by the alginate gel. 25The round nuclear shape of MSCs obtained in thisenvironment has been associated with a high level ofexpression of the chondrogenesis molecular markers. 15In addition, alginate gel encapsulating MSCs werepreviously shown to be associated with an increaseexpression of type II collagen and aggrecan genes andnot of collagen type I. However, it is interesting to notethat an increase in GAG/protein in both MSC- andCMSC-treated knees almost demonstrated a significantdifference between the two treatment groups at6 months with a p-value of only 0.052. There appearsto be a remarkable increase in GAG/protein for theMSC-treated group, exceeding that of the CMSC groupwhen cells are left in vivo for 6 months duration. Itmay have been the case that prolonged chondrogenicdifferentiation in vitro may have resulted in the lost ofJOURNAL OF ORTHOPAEDIC RESEARCH SEPTEMBER 2011
1340 DASHTDAR ET AL.Figure 3. Immunohistochemistry for collagen type II for MSC-treated group (A,B), CMSC-treated group (C,D), and normal cartilage(E,F) 10. (A) The defect of the left knee after 6 months, the repaired cartilage has no vertical integration with subchondral bone, itcontains scarce amount of collagen type II. (B) Collagen type II is deposited (stained brown) in the repaired cartilage. (C) Repairedtissue of the left knee shows an irregular immature cartilage mass with clustered cells and low amount of collagen type II, a part of thedefect has been replaced by bone (arrow). (D) The repaired tissue of the right knee contains a great amount of collagen type II especiallyat superficial layer (arrow). (E) Normal cartilage negative control (stained without collagen type II antibody). (F) Normal cartilagepositive control type II collagen is more abundant in superficial and deep zones.the MSC’s chondrogenic potential when transplantationwas performed in rabbits. Nevertheless, thisissue remains speculative and warrants furtherinvestigation.In the present study, the gross morphologicalappearances of smoother and more homogenous regeneratedcartilage tissues in the MSCs-treated knee indicateda superior tissue repair following MSCtreatment compared those left untreated. This findingwas consistent with previous reports demonstratingsatisfactory repair of damaged cartilage with the useof MSC, even in conditions involving osteochondraldefects. 1–4 The question however remains as towhether the observed enhanced cartilage repair was adirect result of the transplanted MSCs or merely aconsequence of augmented expansion of the surroundingcells, for example, chondrocytes/progenitor cells orextracellular matrix, contributing to the healing process.20,26 To the best of our knowledge, this issue hasnot been specifically addressed in any previouspublications.The histological analyses of the present study identifiedclear differences between the MSC-treated anduntreated knees. The MSC treatment appeared toinduce a greater amount of type II collagen formation.In contrast, the repaired tissue of the untreated kneeshowed an irregular immature cartilage mass withclustered cells and low amount of collagen type II. Inaddition, the repaired tissue treated with MSCscontained a vast amount of GAG in the intermediateand deep zones, whereas the untreated regeneratedtissue showed only scarce amount of GAG. Similarobservations were reported in previous studies, demonstratingthat cartilage treated with MSCs had extracellularmatrix that primarily consisted of a hyalineand fibro-cartilage mixture, while the untreated cartilagedefects were composed of merely a thin layer offibrous tissue. 23,26There are a number of limitations in the study thatare worth highlighting. The present study utilized onlya limited numbers of animals as a consequence offinancial constraints. This prohibits the use of parametricstatistical analyses, which would in effect, producemore convincing results, and thereby strengthenthe conclusions derived from the analyses. In addition,the constraints related to the availability of resourcesallowed assessment of cartilage repair only at 2 timepoints, that is, 3 months and 6 months post-surgery. Alarger number of observational time points that shouldideally be performed would provide further informationregarding the temporal evolution of the repairprocess, providing a better insight into the actualeffect of MSC on the long-term outcome of cartilagerepair. The present study did not specifically distinguishthe contributing effect of alginate on the cartilageregeneration. Improvement to the study designby introducing another treatment arm involving theuse of alginate without cells would be desirable toJOURNAL OF ORTHOPAEDIC RESEARCH SEPTEMBER 2011
CHONDROGENIC PRE-DIFFERENTIATED AND UNDIFFERENTIATED MSCs IN CARTILAGE REPAIR 1341Figure 4. Safranin-O Fast green staining for MSC-treated group (A,B) and CMSC-treated group (C,D) observed at 6 months andnormal cartilage (E) 10. (A) Cutting edge of the defect in the left knee after 6 months, arrow shows the cluster of cells at the border ofthe defect. (B) Repaired tissue in the right knee shows glycosaminoglycans in the intermediate and deep zones. (C) Repaired tissue ofthe left knee shows no or scarce mount of glycosaminoglycans. (D) The arrow points repaired tissue of the right knee contains highamounts of glycosaminoglycans in the intermediate and deep zones. (E) Normal cartilage stains maroon especially in the intermediateand deep zones, bone stains green.specifically address the issues regarding the potentialrole of alginate in allowing better regeneration of thenative chondrocytes, without the introduction ofMSCs. It was not possible to identify the percentage ofMSCs that underwent chondrogenic transformationdue to the technical complexities involved. In additionthis meant that the homogenicity of the CMSCs usedin the present study was also not verified. However,the characterization of CMSCs has provided strongevidences to support that chondrogenic transformationin vitro has occurred to a large degree as demonstratedby the strong positive staining of GAG and collagentype II. 5,16 Lastly, the present study onlyinvestigated the anatomical profiles of the regeneratedcartilage as well as its extracellular matrix biochemicalprofiles. The introduction of more sophisticatedinvestigative modalities such as proteomic andgene expression analyses would provide more precisemolecular markers of the regenerate cartilage tissue,thus providing a global depiction of the healing processwith and without MSC treatment.In conclusion, this study demonstrates that thetransplantation of MSCs for repair of full thicknessarticular cartilage defects produced superior healingcompared to the intrinsic repair of the untreatedcartilage defects, irrespective of their state ofdifferentiation. This has a clinical implication on wideruse of the undifferentiated MSC for cell-based transplantationtherapy for articular cartilage repair, asthis option is associated with more simplified laboratoryprocessing that would not impose on additionalresources and financial burden.ACKNOWLEDGMENTSWe thank Nor Azeera Bakar and Balqis Mariapee Sarinahfor the animal handling. This research was funded byUniversity of Malaya Vote-f research grant (Grant No:PS169/2008C) and The Ministry of Science, Technology andInnovation Malaysia (MOSTI) under the Technofundscheme.REFERENCES1. Wakitani S, Gto T, Pineda SJ, et al. 1994. Mesenchymal cellbaserepair of large full-thickness defects of articular cartilage.J Bone Joint Surg Am 76:579–592.2. Wakitani S, Imoto K, Yamamoto T, et al. 2002. Humanautologous culture expanded bone marrow mesenchymal celltransplantation for repair of cartilage defects in osteoarthriticknees. Osteoarthritis Cartilage 10:199–206.3. Brittberg M, Lindahl A, Nilsson A, et al. 1994. Treatment ofdeep cartilage defect in the knee with autologous chondrocytetransplantation. N Engl J Med 331:889–895.JOURNAL OF ORTHOPAEDIC RESEARCH SEPTEMBER 2011
1342 DASHTDAR ET AL.4. Fragonas E, Valente M, Pozzi-Mucell M, et al. 2000.Articular cartilage repair in rabbits by using suspensions ofallogenic chondrocytes in alginate. Biomaterials 21:795–801.5. Kamarul T, Chong P, Selvaratnam L, et al. 2009. Quantitativereal-time PCR analysis for chondrogenic differentiationof human mesenchymal stem cell in alginate scaffolds. EurCells Mat 18(Suppl 1):44.6. Brittberg M. 2010. Cell carriers as the next generation of celltherapy for cartilage repair. A review of the matrix-inducedautologous chondrocyte implantation procedure. Am JSports Med 38:1259–1271.7. Grande DA, Pitman MI, Peterson L, et al. 1989. The repairof experimentally produced defects in rabbit articular cartilageby autologus chondrocyte transplantation. J Orthop Res7:208–218.8. Temenoff JS, Mikos AG. 2000. Review: tissue engineeringfor regeneration of articular cartilage. Biomaterials 21:431–440.9. Nejadnik H, Hui JH, Feng Choong EP, et al. 2010. Autologousbone marrow-derived mesenchymal stem cells versusautologous chondrocyte implantation: an observationalcohort study. Am J Sports Med 38:1110–1116.10. Gao J, Dennis JE, Solchaga LA, et al. 2002. Repair of osteochondraldefect with tissue-engineered two-phase compositematerial of injectable calcium phosphate and hyaluronansponge. Tissue Eng 8:827–837.11. Lee JW, Kim YH, Kim SH, et al. 2004. Chondrogenic differentiationof mesenchymal stem cells and its clinical applications.Yonsei Med J 45(Suppl):41–47.12. Kobayashi M, Chang YS, Oka M. 2005. A two year in vivostudy of polyvinyl alcohol-hydrogel (PVA_H) artificial meniscus.Biomaterials 26:3243–3248.13. Colman RM, Case ND, Guldberg RE. 2007. Hydrogel effectson bone marrow stromal cell response to chondrogenicgrowth factors. Giomaterials 28:2077–2086.14. Murphy JM, Kavalkavitch KW, Fink D, et al. 2000. Regenerationof meniscal tissue and protection of articular cartilageby an injection of mesenchymal stem cells. OsteoarthritisCartilage 8(Suppl B):S25.15. McBride SH, Knothe ML. 2008. Modulation of stem cellshape and fate A: the role of density and seeding protocol onnucleus shape and gene expression. Tissue Eng 14:1561–1572.16. Tan SL, Sulaiman S, Pingguan-Murphy B, et al. 2011.Human amnion as a novel cell delivery vehicle for chondrogenicmesenchymal stem cells. Cell Tissue Bank 12:59–70.17. Brittberg M. 2000. Evaluation of cartilage injuries andcartilage repair. Osteologie 9:17–25.18. ICRS Cartilage Evaluation package, 2000. http://www.cartilage.org/Evaluation_Package/ICRS_Evaluation.pdf(accessedAugust 6, 2002).19. O’Driscoll SW, Keeley FW, Salter RB. 1988. Durability ofregenerated articular cartilage produced by free autogenousperiosteal grafts in major full-thickness defects in jointsurfaces under the influence of continuous passive motion.J Bone Joint Surg Am 70:595–606.20. Kamarul T, Selvaratnam L, Masjuddin T, et al. 2008. Autologouschondrocyte transplantation in the repair of fullthicknessfocal cartilage damage in rabbits. J Orthop Surg16:230–236.21. Pittenger MF, Mackay AM, Beck SC, et al. 1999. Multilineagepotential of adult human mesenchymal stem cells.Science 284:143–147.22. Guilak F, Cohen D, Estes B, et al. 2009. Control of stem cellfate by physical interactions with the extracellular matrix.Cell Stem Cell 5:17–26.23. Diduch DR, Jordan CM, Mierisch CM, et al. 2000. Marrowstromal cells embedded in alginate for repair of osteochondraldefects. J Arthroscopic Relat Surg 16:571–577.24. Tuan RS, Boland G, Tuli R. 2003. Adult mesenchymal stemcells and cell-based tissue engineering. Arthritis Res Ther51:32–45.25. Hoben GM, Koay EJ, Athanasiou KA. 2008. Fibrochondrogenesisin two embryonic stem cell lines: effects of differentiationtimelines. Stem Cells 26:422–430.26. Pelttari K, Steck E, Richter W. 2008. The use of mesenchymalstem cells for chondrogenesis injury. Int J Care Inj39:58–65.JOURNAL OF ORTHOPAEDIC RESEARCH SEPTEMBER 2011