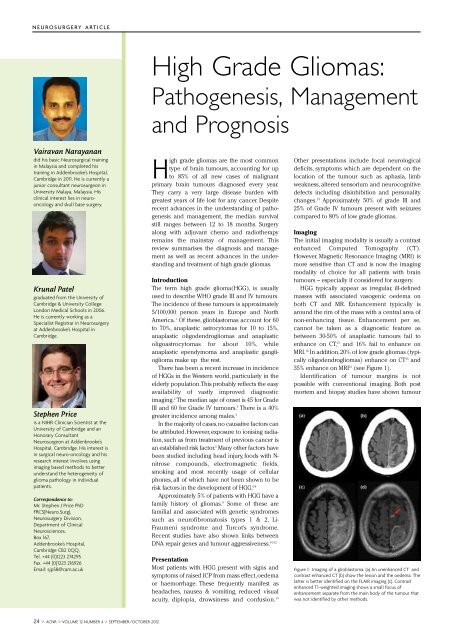
N E U RO S U RG E RY A RT I C L EVairavan Narayan<strong>and</strong>id his basic Neurosurgical tra<strong>in</strong><strong>in</strong>g<strong>in</strong> Malaysia <strong>and</strong> completed histra<strong>in</strong><strong>in</strong>g <strong>in</strong> Addenbrooke’s Hospital,Cambridge <strong>in</strong> 2011. He is currently ajunior consultant neurosurgeon <strong>in</strong>University Malaya, Malaysia. Hiscl<strong>in</strong>ical <strong>in</strong>terest lies <strong>in</strong> neurooncology<strong>and</strong> skull base surgery.Krunal Patelgraduated from the University ofCambridge & University CollegeLondon Medical Schools <strong>in</strong> 2006.He is currently work<strong>in</strong>g as aSpecialist Registrar <strong>in</strong> Neurosurgeryat Addenbrooke’s Hospital <strong>in</strong>Cambridge.Stephen Priceis a NIHR Cl<strong>in</strong>ician Scientist at theUniversity of Cambridge <strong>and</strong> anHonorary ConsultantNeurosurgeon at Addenbrooke’sHospital, Cambridge. His <strong>in</strong>terest is<strong>in</strong> surgical neuro-oncology <strong>and</strong> hisresearch <strong>in</strong>terest <strong>in</strong>volves us<strong>in</strong>gimag<strong>in</strong>g based methods to betterunderst<strong>and</strong> the heterogeneity ofglioma pathology <strong>in</strong> <strong>in</strong>dividualpatients.Correspondence to:Mr. Stephen J Price PhDFRCS(Neuro.Surg),Neurosurgery Division,Department of Cl<strong>in</strong>ical<strong>Neuroscience</strong>s,Box 167,Addenbrooke’s Hospital,Cambridge CB2 0QQ,Tel. +44 (0)1223 274295Fax. +44 (0)1223 216926Email: sjp58@cam.ac.ukHigh Grade Gliomas:Pathogenesis, Management<strong>and</strong> PrognosisHigh grade gliomas are the most commontype of bra<strong>in</strong> tumours, account<strong>in</strong>g for upto 85% of all new cases of malignantprimary bra<strong>in</strong> tumours diagnosed every year.They carry a very large disease burden withgreatest years of life lost for any cancer. Despiterecent advances <strong>in</strong> the underst<strong>and</strong><strong>in</strong>g of pathogenesis<strong>and</strong> management, the median survivalstill ranges between 12 to 18 months. Surgeryalong with adjuvant chemo <strong>and</strong> radiotherapyrema<strong>in</strong>s the ma<strong>in</strong>stay of management. Thisreview summarises the diagnosis <strong>and</strong> managementas well as recent advances <strong>in</strong> the underst<strong>and</strong><strong>in</strong>g<strong>and</strong> treatment of high grade gliomas.IntroductionThe term high grade glioma(HGG), is usuallyused to describe WHO grade III <strong>and</strong> IV tumours.The <strong>in</strong>cidence of these tumours is approximately5/100,000 person years <strong>in</strong> Europe <strong>and</strong> NorthAmerica. 1 Of these, glioblastomas account for 60to 70%, anaplastic astrocytomas for 10 to 15%,anaplastic oligodendrogliomas <strong>and</strong> anaplasticoligoastrocytomas for about 10%, whileanaplastic ependymoma <strong>and</strong> anaplastic gangliogliomamake up the rest.There has been a recent <strong>in</strong>crease <strong>in</strong> <strong>in</strong>cidenceof HGGs <strong>in</strong> the Western world, particularly <strong>in</strong> theelderly population. This probably reflects the easyavailability of vastly improved diagnosticimag<strong>in</strong>g. 2 The median age of onset is 45 for GradeIII <strong>and</strong> 60 for Grade IV tumours. 3 There is a 40%greater <strong>in</strong>cidence among males. 4In the majority of cases, no causative factors canbe attributed. However, exposure to ionis<strong>in</strong>g radiation,such as from treatment of previous cancer isan established risk factor. 5 Many other factors havebeen studied <strong>in</strong>clud<strong>in</strong>g head <strong>in</strong>jury, foods with N-nitrose compounds, electromagnetic fields,smok<strong>in</strong>g <strong>and</strong> most recently usage of cellularphones, all of which have not been shown to berisk factors <strong>in</strong> the development of HGG. 6-8Approximately 5% of patients with HGG have afamily history of gliomas. 9 Some of these arefamilial <strong>and</strong> associated with genetic syndromessuch as neurofibromatosis types 1 & 2, Li-Fraumeni syndrome <strong>and</strong> Turcot’s syndrome.Recent studies have also shown l<strong>in</strong>ks betweenDNA repair genes <strong>and</strong> tumour aggressiveness. 10-12PresentationMost patients with HGG present with signs <strong>and</strong>symptoms of raised ICP from mass effect, oedemaor haemorrhage. These frequently manifest asheadaches, nausea & vomit<strong>in</strong>g, reduced visualacuity, diplopia, drows<strong>in</strong>ess <strong>and</strong> confusion. 13Other presentations <strong>in</strong>clude focal neurologicaldeficits, symptoms which are dependent on thelocation of the tumour such as aphasia, limbweakness, altered sensorium <strong>and</strong> neurocognitivedefects <strong>in</strong>clud<strong>in</strong>g dis<strong>in</strong>hibition <strong>and</strong> personalitychanges. 14 Approximately 50% of grade III <strong>and</strong>25% of Grade IV tumours present with seizurescompared to 80% of low grade gliomas.Imag<strong>in</strong>gThe <strong>in</strong>itial imag<strong>in</strong>g modality is usually a contrastenhanced Computed Tomography (CT).However, Magnetic Resonance Imag<strong>in</strong>g (MRI) ismore sensitive than CT <strong>and</strong> is now the imag<strong>in</strong>gmodality of choice for all patients with bra<strong>in</strong>tumours – especially if considered for surgery.HGG typically appear as irregular, ill-def<strong>in</strong>edmasses with associated vasogenic oedema onboth CT <strong>and</strong> MR. Enhancement typically isaround the rim of the mass with a central area ofnon-enhanc<strong>in</strong>g tissue. Enhancement per se,cannot be taken as a diagnostic feature asbetween 30-50% of anaplastic tumours fail toenhance on CT, 15 <strong>and</strong> 16% fail to enhance onMRI. 16 In addition, 20% of low grade gliomas (typicallyoligodendrogliomas) enhance on CT 15 <strong>and</strong>35% enhance on MRI 16 (see Figure 1).Identification of tumour marg<strong>in</strong>s is notpossible with conventional imag<strong>in</strong>g. Both postmortem <strong>and</strong> biopsy studies have shown tumourFigure 1: Imag<strong>in</strong>g of a glioblastoma. (a) An unenhanced CT <strong>and</strong>contrast enhanced CT (b) show the lesion <strong>and</strong> the oedema. Thelatter is better identified on the FLAIR imag<strong>in</strong>g (c). Contrastenhanced T1-weighted imag<strong>in</strong>g shows a small focus ofenhancement separate from the ma<strong>in</strong> body of the tumour thatwas not identified by other methods.24 > ACNR > VOLUME 12 NUMBER 4 > SEPTEMBER/OCTOBER 2012
N E U RO S U RG E RY A RT I C L Emultiple sites for mutation have been identifiedmak<strong>in</strong>g this marker difficult to assess. Inaddition, the results are semi-quantitative withno clear cut off to def<strong>in</strong>e positive or negativestatus, result<strong>in</strong>g <strong>in</strong> non-st<strong>and</strong>ard <strong>in</strong>terpretationof test results.Figure 2: Histology of a glioblastoma. (a) shows the microvascular proliferation <strong>and</strong> (b) shows evidence of tumour necrosis –the presence of either of these factors <strong>in</strong> an astrocytic tumour is sufficient to make a diagnosis of glioblastoma. (Picture courtesyof Dr Kieren All<strong>in</strong>son, Addenbrooke’s Hospital, Cambridge).extends beyond the marg<strong>in</strong> on CT, 17-20 contrastenhancedT1-weighted MRI 20-21 <strong>and</strong> T2-weighted MR. 20-23 These techniques cannotdeterm<strong>in</strong>e the marg<strong>in</strong> or the <strong>in</strong>vasiveness ofthese tumours. Advanced imag<strong>in</strong>g methodshave been developed for assessment of thesetumours. These are be<strong>in</strong>g used <strong>in</strong> cl<strong>in</strong>ical practice<strong>and</strong> are summarised elsewhere. 24Post-operative MRI is the only method ofobjectively assess<strong>in</strong>g the extent of resection.Studies have shown it identifies more cases of<strong>in</strong>complete resection compared to the judgementof the surgeon. 25 Imag<strong>in</strong>g with<strong>in</strong> 72 hoursavoids the post-operative changes that occurlater.HistologyHigh grade gliomas arise from support<strong>in</strong>g glialcells <strong>in</strong> the bra<strong>in</strong>. The predom<strong>in</strong>ant cell typedeterm<strong>in</strong>es the pathological classification.Tumours are graded accord<strong>in</strong>g to the WorldHealth Organisation (WHO) grad<strong>in</strong>g system(Grade I to IV). 26 HGGs comprise of WHOgrade III <strong>and</strong> IV tumours. Multiple subtypeshave been identified which may alterresponse to treatment <strong>and</strong> prognosis. These<strong>in</strong>clude subtype III which comprisesanaplastic astrocytoma, oligoastrocytoma,anaplastic oligoastrocytoma as well assubtype IV which <strong>in</strong>cludes glioblastoma,glioblastoma with oligodendrocyte component<strong>and</strong> gliosarcoma. 27Grade III tumours are diffusely <strong>in</strong>filtrat<strong>in</strong>gastrocytomas with focal or dispersedanaplasia <strong>and</strong> a marked proliferative potentialwith <strong>in</strong>creased cellularity, dist<strong>in</strong>ct nuclearatypia <strong>and</strong> high mitotic activity while Grade IVtumours show cellular polymorphism, nuclearatypia, brisk mitotic activity, vascular thrombosis,microvascular proliferation <strong>and</strong> necrosis(see Figure 2).Grad<strong>in</strong>g is determ<strong>in</strong>ed by the most malignantpart of tumour, which makes it essentialfor adequate sampl<strong>in</strong>g to determ<strong>in</strong>e theproper grade, especially <strong>in</strong> biopsy procedures.Molecular markers <strong>and</strong> their significanceOne of the biggest advances <strong>in</strong> high gradeglioma management has come <strong>in</strong> the form ofmolecular markers. Three particular markershave been well studied over the past fewyears.Figure 3: Methylation of MGMT <strong>in</strong>hibits repair of DNAdamaged by both radiotherapy <strong>and</strong> chemotherapy drugs.1. MGMT Methylation StatusThe MGMT gene encodes O-6-methylguan<strong>in</strong>e-DNA methyltransferase enzyme – a DNA repairenzyme that removes alkyl groups from the O-6 position of guan<strong>in</strong>e, an important site of DNAalkylation. MGMT methylation status has beenused to prognosticate response to alkylat<strong>in</strong>gchemotherapeutic agents like Temozolomide.In the methylated form, it is non-functional(i.e. the enzyme is not produced) thus limit<strong>in</strong>gDNA repair, cf. Figure 3). Two recent retrospectivestudies by Hegi et al 28 <strong>and</strong> Stupp et al 29analysed this particular molecular marker <strong>and</strong>found the methylation phenomenon present<strong>in</strong> up to 45% of cases of GBM. Further, <strong>in</strong> thepresence of methylation, median survival forradiotherapy with Temozolomide was significantlylonger than radiotherapy alone (21.7months, 95% CI 17.4-30.4 vs 15.3 months, 95%CI 13.0-20.9; P=0.007). In comparison, thedifference <strong>in</strong> survival <strong>in</strong> the unmethylatedgroup was <strong>in</strong>significant (11.8 months, 95% CI9.7-14.1 vs. 12.7 months, 95% CI 11.6-14.4). Asthe methylated group with radiotherapy alonehas better survival than either unmethylatedgroups, it suggests MGMT methylation functionsas a prognostic marker rather than apredictive marker. A prospective analysis byWeller et al shows an improvement <strong>in</strong> bothprogression free survival (7.5 months vs 6.3months) <strong>and</strong> overall survival (18.9 months vs11.1 months). 30 MGMT methylation statusassessment is not without its problems –2. IDH-1 MutationThe IDH-1 gene encodes the enzyme isocitratedehydrogenase (IDH-1) gene that convertsisocitrate to α-ketoglutarate with<strong>in</strong> the Krebscycle. This stage generates NADPH thatappears to be important <strong>in</strong> deal<strong>in</strong>g with cytotoxicoxidative stresses. Mutation of this generesults <strong>in</strong> an alternative metabolism of isocitrateto 2-hydroxyglutarate. Mutations cause a10 fold <strong>in</strong>crease <strong>in</strong> the production of 2-hydroxyglutarate.31 Accumulation of 2-hydroxyglutaratealso leads to the breakdown of HIF-1α, afactor important for generat<strong>in</strong>g a malignantcell phenotype.Mutation of IDH-1 gene was found <strong>in</strong> 12% ofGBM patients <strong>and</strong> seems to confer a bettermedian survival, (3.7 years vs 1.1years). 32Weller et al reconfirmed this via the GermanGlioma Network study which found IDH-1mutations <strong>in</strong> 16/286 patients (5.6%). They alsofound an improvement <strong>in</strong> both progressionfree survival (16.2 months vs 6.5 months) <strong>and</strong>overall survival (30.2 months vs 11.2months). 30 As with the MGMT mutation, IDH-1mutation is prognostic rather than predictive. 33Virtually all mutations (96%) are a po<strong>in</strong>t mutation<strong>in</strong>volv<strong>in</strong>g arg<strong>in</strong><strong>in</strong>e 132. This allows animmunohistochemistry test on paraff<strong>in</strong>embedded tissue.3. Chromosome 1p19q Loss <strong>in</strong>Oligodendroglial TumoursOne of the commonest chromosomal abnormalitiesseen <strong>in</strong> oligodendrogliomas is theconcurrent loss of part or all of the short armof chromosome 1 (1p) <strong>and</strong> the long arm ofchromosome 19 (19q). Cairncross et alshowed loss of 1p19q <strong>in</strong> 50-70% of anaplasticoligodendrogliomas. 34 This mutation had animproved survival with chemotherapy <strong>and</strong>was orig<strong>in</strong>ally thought to be predictive ofchemosensitivity. Results from a trial of radiotherapyvs chemoradiotherapy showed theradiotherapy only arm with 1p19q loss didbetter than the chemoradiotherapy armwithout loss of 1p19q suggest<strong>in</strong>g aga<strong>in</strong> theprognostic nature of these molecularmarkers. 35PathogenesisGlioblastomas develop either as primarytumours or arise from pre exist<strong>in</strong>g low gradegliomas (Table 1). These primary <strong>and</strong>secondary GBMs constitute separate <strong>and</strong>dist<strong>in</strong>ct disease entities. They affect differentepidemiological groups <strong>and</strong> carry differentprognoses.Primary gliomas usually are of a de novomanifestation <strong>in</strong>volv<strong>in</strong>g older patients with ashorter cl<strong>in</strong>ical history. On the other h<strong>and</strong>,secondary gliomas are usually part of a malignantprogression from low grade to high gradeACNR > VOLUME 12 NUMBER 4 > SEPTEMBER/OCTOBER 2012 > 25