NBE CME programme for DNB consultants - National Board Of ...
NBE CME programme for DNB consultants - National Board Of ...
NBE CME programme for DNB consultants - National Board Of ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
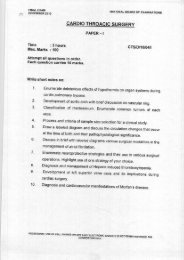
<strong>NBE</strong> <strong>CME</strong> <strong>programme</strong> <strong>for</strong> <strong>DNB</strong> <strong>consultants</strong>Cerebral PalsyHistory - The candidates should be very clear about the duration of the illness – present illness; Apatient with recurrent episodes of almost identical illnesses with symptom free intervals – the lastepisode to be described in full and others included under the heading of past illness; All events(including treatment) should be described in the chronological order - as the disease developsDescribing each symptom separately is not desirable; Illnesses which have origins in the neonatalperiod to be described from birth e.g. birth asphyxia with seizures leading to Cerebral palsy;Describe in detail only relevant history. Discredit <strong>for</strong> spending too much time on irrelevant history;All aspects of history to be discussed and documented. At postgraduate level they must knowwhich is relevant and which is irrelevant; At the end of history the candidate should be able to drawsome conclusions regarding the problem e.g. Degenerative diseases of brain -Intracranial spaceoccupying lesion, Chronic liver diseasePhysical Examination - General physical examination - Observation about general appearance,Diagnostic clues – positive and negative; Growth - Detailed measurements only in growth problems;Development - Details only in cases of developmental delay; System involved - Give all details;Other systems - Positive findings only.Summary - The candidates should summarize the case in 4 or 5 sentences – only relevant history,positive findings and important negative findingsDiagnosis - Complete diagnosis to be given; Substantiate the diagnosis based on history, findingsand course of the disease – both positive and negative; Differential diagnosis only if there arevalid reasons; Candidates should state why the DD is suggestedInvestigations - Relevant investigations only; The candidates should know why he is suggestinga particular investigation.Treatment - Essential treatment only; Rationale of treatment should be explained.Coma/Altered SensoriumHistory- When? How? Under what circumstances? How long? Who were there? Witness shouldbe questioned. History of fever - CNS infection, febrile encephalopathy(cerebral malaria, Dengueencephalopathy, leptospirosis with aseptic meningitis etc) ; History of Headache, vomiting – increasein ICP; History of seizures; If known seizure disorder – whether omission/over dosage of AED;History of fall/head trauma – concussion, intracranial injury; History of drug intake – suspicion isvery misleading – family members on drugs; History of Pica – Lead poisoning; Similar episodesbe<strong>for</strong>e – lethargy, vomiting, Coma – Inborn error of metabolism; Underlying chronic medicalconditions – CRF, hepatic encephalopathy etcClinical Examination-ABC; Glasgow Coma Scale; Pulse – bradycardia - ‘! ICT; Temp. – Febrileseizures, CNS infection, febrile encephalopathy; Respiration – ef<strong>for</strong>tless tachypnea-metabolicacidosis, DKA -slow breathing – respiratory depression, ataxic breathing – cerebellar herniatino;BP – HT, hypertensive encephalopathy, increased ICP; Pupils – asymmetry – unilateral dilatedfixed pupil – Tentorial herniation-Pinpoint – OPC, barbiturates, Dilated, fixed – postictal, atropineetc.Differential Diagnosis- Metabolic; Trauma, Tumour, Toxins; CNS infection; Vascular; Demyelination;Postictal; HIE; Persistent vegetative stateManagement -Non Surgical - ABC; Draw blood fro biochemistry/drug/toxin; 25% dextrose ifhypoglycemia; IV mannitol if increase in ICP; IV antibniotics if suspicion of meningitis; IVanticonvulsants, seixures; Sublingual nifedipine if hypertensive; Antidotes <strong>for</strong> poisoning; Investigatethe cause and manage accordinglySurgical - Extradural/subdural tap; Cerebral abscess – drainage; Tumous with obstructivehydrocephalus – VP shuntAny other - Water & electrolyte balance – look <strong>for</strong> SIADH/central diabetes insipidus; Nutrition;146