June 09-41-2.indd - Kma.org.kw
June 09-41-2.indd - Kma.org.kw
June 09-41-2.indd - Kma.org.kw
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
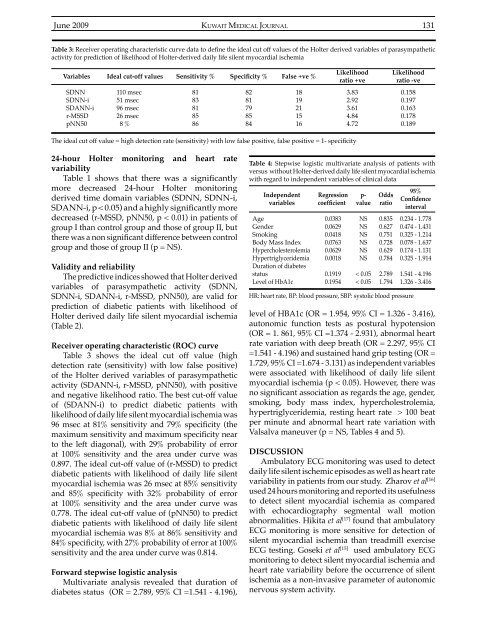
<strong>June</strong> 20<strong>09</strong>KUWAIT MEDICAL JOURNAL 131Table 3: Receiver operating characteristic curve data to define the ideal cut off values of the Holter derived variables of parasympatheticactivity for prediction of likelihood of Holter-derived daily life silent myocardial ischemiaVariables Ideal cut-off values Sensitivity % Specificity % False +ve %SDNNSDNN-iSDANN-ir-MSSDpNN50110 msec51 msec96 msec26 msec8 %8183818586828179858<strong>41</strong>819211516Likelihoodratio +ve3.832.923.614.844.72Likelihoodratio -ve0.1580.1970.1630.1780.189The ideal cut off value = high detection rate (sensitivity) with low false positive, false positive = 1- specificity24-hour Holter monitoring and heart ratevariabilityTable 1 shows that there was a significantlymore decreased 24-hour Holter monitoringderived time domain variables (SDNN, SDNN-i,SDANN-i, p < 0.05) and a highly significantly moredecreased (r-MSSD, pNN50, p < 0.01) in patients ofgroup I than control group and those of group II, butthere was a non significant difference between controlgroup and those of group II (p = NS).Validity and reliabilityThe predictive indices showed that Holter derivedvariables of parasympathetic activity (SDNN,SDNN-i, SDANN-i, r-MSSD, pNN50), are valid forprediction of diabetic patients with likelihood ofHolter derived daily life silent myocardial ischemia(Table 2).Receiver operating characteristic (ROC) curveTable 3 shows the ideal cut off value (highdetection rate (sensitivity) with low false positive)of the Holter derived variables of parasympatheticactivity (SDANN-i, r-MSSD, pNN50), with positiveand negative likelihood ratio. The best cut-off valueof (SDANN-i) to predict diabetic patients withlikelihood of daily life silent myocardial ischemia was96 msec at 81% sensitivity and 79% specificity (themaximum sensitivity and maximum specificity nearto the left diagonal), with 29% probability of errorat 100% sensitivity and the area under curve was0.897. The ideal cut-off value of (r-MSSD) to predictdiabetic patients with likelihood of daily life silentmyocardial ischemia was 26 msec at 85% sensitivityand 85% specificity with 32% probability of errorat 100% sensitivity and the area under curve was0.778. The ideal cut-off value of (pNN50) to predictdiabetic patients with likelihood of daily life silentmyocardial ischemia was 8% at 86% sensitivity and84% specificity, with 27% probability of error at 100%sensitivity and the area under curve was 0.814.Forward stepwise logistic analysisMultivariate analysis revealed that duration ofdiabetes status (OR = 2.789, 95% CI =1.5<strong>41</strong> - 4.196),Table 4: Stepwise logistic multivariate analysis of patients withversus without Holter-derived daily life silent myocardial ischemiawith regard to independent variables of clinical dataIndependentvariablesAgeGenderSmokingBody Mass IndexHypercholesterolemiaHypertriglyceridemiaDuration of diabetesstatusLevel of HbA1cRegressioncoefficient0.03830.06290.0<strong>41</strong>80.07630.06290.00180.19190.1954p-valueNSNSNSNSNSNS< 0.05< 0.05Oddsratio0.8350.6270.7510.7280.6290.7842.7891.794HR: heart rate, BP: blood pressure, SBP: systolic blood pressure95%Confidenceinterval0.234 - 1.7780.474 - 1.4310.325 - 1.2140.078 - 1.6370.174 - 1.1310.325 - 1.91<strong>41</strong>.5<strong>41</strong> - 4.1961.326 - 3.<strong>41</strong>6level of HBA1c (OR = 1.954, 95% CI = 1.326 - 3.<strong>41</strong>6),autonomic function tests as postural hypotension(OR = 1. 861, 95% CI =1.374 - 2.931), abnormal heartrate variation with deep breath (OR = 2.297, 95% CI=1.5<strong>41</strong> - 4.196) and sustained hand grip testing (OR =1.729, 95% CI =1.674 - 3.131) as independent variableswere associated with likelihood of daily life silentmyocardial ischemia (p < 0.05). However, there wasno significant association as regards the age, gender,smoking, body mass index, hypercholestrolemia,hypertriglyceridemia, resting heart rate > 100 beatper minute and abnormal heart rate variation withValsalva maneuver (p = NS, Tables 4 and 5).DISCUSSIONAmbulatory ECG monitoring was used to detectdaily life silent ischemic episodes as well as heart ratevariability in patients from our study. Zharov et al [16]used 24 hours monitoring and reported its usefulnessto detect silent myocardial ischemia as comparedwith echocardiography segmental wall motionabnormalities. Hikita et al [17] found that ambulatoryECG monitoring is more sensitive for detection ofsilent myocardial ischemia than treadmill exerciseECG testing. Goseki et al [15] used ambulatory ECGmonitoring to detect silent myocardial ischemia andheart rate variability before the occurrence of silentischemia as a non-invasive parameter of autonomicnervous system activity.