Dementia
gi2hff
gi2hff
- No tags were found...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
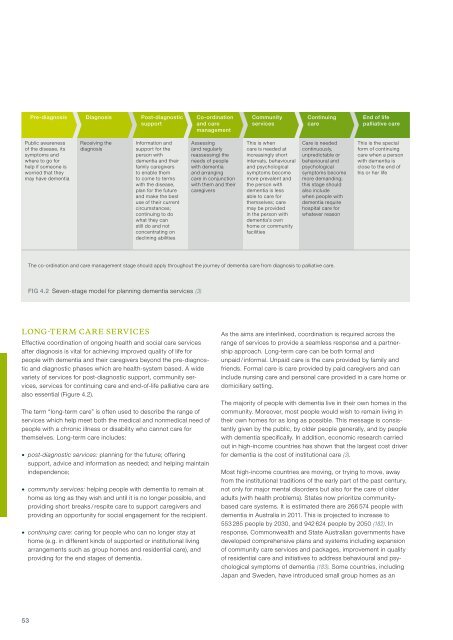
Pre-diagnosis Diagnosis Post-diagnostic<br />
support<br />
Co-ordination<br />
and care<br />
management<br />
Community<br />
services<br />
Continuing<br />
care<br />
End of life<br />
palliative care<br />
Public awareness<br />
of the disease, its<br />
symptoms and<br />
where to go for<br />
help if someone is<br />
worried that they<br />
may have dementia<br />
Receiving the<br />
diagnosis<br />
Information and<br />
support for the<br />
person with<br />
dementia and their<br />
family caregivers<br />
to enable them<br />
to come to terms<br />
with the disease,<br />
plan for the future<br />
and make the best<br />
use of their current<br />
circumstances;<br />
continuing to do<br />
what they can<br />
still do and not<br />
concentrating on<br />
declining abilities<br />
Assessing<br />
(and regularly<br />
reassessing) the<br />
needs of people<br />
with dementia<br />
and arranging<br />
care in conjunction<br />
with them and their<br />
caregivers<br />
This is when<br />
care is needed at<br />
increasingly short<br />
intervals, behavioural<br />
and psychological<br />
symptoms become<br />
more prevalent and<br />
the person with<br />
dementia is less<br />
able to care for<br />
themselves; care<br />
may be provided<br />
in the person with<br />
dementia’s own<br />
home or community<br />
facilities<br />
Care is needed<br />
continuously,<br />
unpredictable or<br />
behavioural and<br />
psychological<br />
symptoms become<br />
more demanding;<br />
this stage should<br />
also include<br />
when people with<br />
dementia require<br />
hospital care for<br />
whatever reason<br />
This is the special<br />
form of continuing<br />
care when a person<br />
with dementia is<br />
close to the end of<br />
his or her life<br />
The co-ordination and care management stage should apply throughout the journey of dementia care from diagnosis to palliative care.<br />
FIG 4.2 Seven-stage model for planning dementia services (3)<br />
Long-term care services<br />
Effective coordination of ongoing health and social care services<br />
after diagnosis is vital for achieving improved quality of life for<br />
people with dementia and their caregivers beyond the pre-diagnostic<br />
and diagnostic phases which are health-system based. A wide<br />
variety of services for post-diagnostic support, community services,<br />
services for continuing care and end-of-life palliative care are<br />
also essential (Figure 4.2).<br />
The term “long-term care” is often used to describe the range of<br />
services which help meet both the medical and nonmedical need of<br />
people with a chronic illness or disability who cannot care for<br />
themselves. Long-term care includes:<br />
• post-diagnostic services: planning for the future; offering<br />
support, advice and information as needed; and helping maintain<br />
independence;<br />
• community services: helping people with dementia to remain at<br />
home as long as they wish and until it is no longer possible, and<br />
providing short breaks / respite care to support caregivers and<br />
providing an opportunity for social engagement for the recipient.<br />
• continuing care: caring for people who can no longer stay at<br />
home (e.g. in different kinds of supported or institutional living<br />
arrangements such as group homes and residential care), and<br />
providing for the end stages of dementia.<br />
As the aims are interlinked, coordination is required across the<br />
range of services to provide a seamless response and a partnership<br />
approach. Long-term care can be both formal and<br />
unpaid / informal. Unpaid care is the care provided by family and<br />
friends. Formal care is care provided by paid caregivers and can<br />
include nursing care and personal care provided in a care home or<br />
domiciliary setting.<br />
The majority of people with dementia live in their own homes in the<br />
community. Moreover, most people would wish to remain living in<br />
their own homes for as long as possible. This message is consistently<br />
given by the public, by older people generally, and by people<br />
with dementia specifically. In addition, economic research carried<br />
out in high-income countries has shown that the largest cost driver<br />
for dementia is the cost of institutional care (3).<br />
Most high-income countries are moving, or trying to move, away<br />
from the institutional traditions of the early part of the past century,<br />
not only for major mental disorders but also for the care of older<br />
adults (with health problems). States now prioritize communitybased<br />
care systems. It is estimated there are 266 574 people with<br />
dementia in Australia in 2011. This is projected to increase to<br />
553 285 people by 2030, and 942 624 people by 2050 (182). In<br />
response, Commonwealth and State Australian governments have<br />
developed comprehensive plans and systems including expansion<br />
of community care services and packages, improvement in quality<br />
of residential care and initiatives to address behavioural and psychological<br />
symptoms of dementia (183). Some countries, including<br />
Japan and Sweden, have introduced small group homes as an<br />
53