Evaluating the “Good Death” Concept from Iranian Bereaved Family
Evaluating the “Good Death” Concept from Iranian Bereaved Family
Evaluating the “Good Death” Concept from Iranian Bereaved Family
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
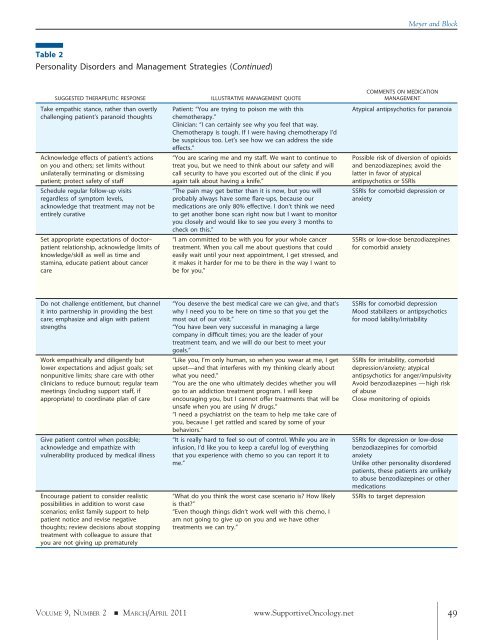
Table 2<br />
Personality Disorders and Management Strategies (Continued)<br />
SUGGESTED THERAPEUTIC RESPONSE ILLUSTRATIVE MANAGEMENT QUOTE<br />
Take empathic stance, ra<strong>the</strong>r than overtly<br />
challenging patient’s paranoid thoughts<br />
Acknowledge effects of patient’s actions<br />
on you and o<strong>the</strong>rs; set limits without<br />
unilaterally terminating or dismissing<br />
patient; protect safety of staff<br />
Schedule regular follow-up visits<br />
regardless of symptom levels,<br />
acknowledge that treatment may not be<br />
entirely curative<br />
Set appropriate expectations of doctor–<br />
patient relationship, acknowledge limits of<br />
knowledge/skill as well as time and<br />
stamina, educate patient about cancer<br />
care<br />
Do not challenge entitlement, but channel<br />
it into partnership in providing <strong>the</strong> best<br />
care; emphasize and align with patient<br />
strengths<br />
Work empathically and diligently but<br />
lower expectations and adjust goals; set<br />
nonpunitive limits; share care with o<strong>the</strong>r<br />
clinicians to reduce burnout; regular team<br />
meetings (including support staff, if<br />
appropriate) to coordinate plan of care<br />
Give patient control when possible;<br />
acknowledge and empathize with<br />
vulnerability produced by medical illness<br />
Encourage patient to consider realistic<br />
possibilities in addition to worst case<br />
scenarios; enlist family support to help<br />
patient notice and revise negative<br />
thoughts; review decisions about stopping<br />
treatment with colleague to assure that<br />
you are not giving up prematurely<br />
Patient: “You are trying to poison me with this<br />
chemo<strong>the</strong>rapy.”<br />
Clinician: “I can certainly see why you feel that way.<br />
Chemo<strong>the</strong>rapy is tough. If I were having chemo<strong>the</strong>rapy I’d<br />
be suspicious too. Let’s see how we can address <strong>the</strong> side<br />
effects.”<br />
“You are scaring me and my staff. We want to continue to<br />
treat you, but we need to think about our safety and will<br />
call security to have you escorted out of <strong>the</strong> clinic if you<br />
again talk about having a knife.”<br />
“The pain may get better than it is now, but you will<br />
probably always have some flare-ups, because our<br />
medications are only 80% effective. I don’t think we need<br />
to get ano<strong>the</strong>r bone scan right now but I want to monitor<br />
you closely and would like to see you every 3 months to<br />
check on this.”<br />
“I am committed to be with you for your whole cancer<br />
treatment. When you call me about questions that could<br />
easily wait until your next appointment, I get stressed, and<br />
it makes it harder for me to be <strong>the</strong>re in <strong>the</strong> way I want to<br />
be for you.”<br />
“You deserve <strong>the</strong> best medical care we can give, and that’s<br />
why I need you to be here on time so that you get <strong>the</strong><br />
most out of our visit.”<br />
“You have been very successful in managing a large<br />
company in difficult times; you are <strong>the</strong> leader of your<br />
treatment team, and we will do our best to meet your<br />
goals.”<br />
“Like you, I’m only human, so when you swear at me, I get<br />
upset—and that interferes with my thinking clearly about<br />
what you need.”<br />
“You are <strong>the</strong> one who ultimately decides whe<strong>the</strong>r you will<br />
go to an addiction treatment program. I will keep<br />
encouraging you, but I cannot offer treatments that will be<br />
unsafe when you are using IV drugs.”<br />
“I need a psychiatrist on <strong>the</strong> team to help me take care of<br />
you, because I get rattled and scared by some of your<br />
behaviors.”<br />
“It is really hard to feel so out of control. While you are in<br />
infusion, I’d like you to keep a careful log of everything<br />
that you experience with chemo so you can report it to<br />
me.”<br />
“What do you think <strong>the</strong> worst case scenario is? How likely<br />
is that?”<br />
“Even though things didn’t work well with this chemo, I<br />
am not going to give up on you and we have o<strong>the</strong>r<br />
treatments we can try.”<br />
COMMENTS ON MEDICATION<br />
MANAGEMENT<br />
Atypical antipsychotics for paranoia<br />
Possible risk of diversion of opioids<br />
and benzodiazepines; avoid <strong>the</strong><br />
latter in favor of atypical<br />
antipsychotics or SSRIs<br />
SSRIs for comorbid depression or<br />
anxiety<br />
SSRIs or low-dose benzodiazepines<br />
for comorbid anxiety<br />
SSRIs for comorbid depression<br />
Mood stabilizers or antipsychotics<br />
for mood lability/irritability<br />
SSRIs for irritability, comorbid<br />
depression/anxiety; atypical<br />
antipsychotics for anger/impulsivity<br />
Avoid benzodiazepines —high risk<br />
of abuse<br />
Close monitoring of opioids<br />
SSRIs for depression or low-dose<br />
benzodiazepines for comorbid<br />
anxiety<br />
Unlike o<strong>the</strong>r personality disordered<br />
patients, <strong>the</strong>se patients are unlikely<br />
to abuse benzodiazepines or o<strong>the</strong>r<br />
medications<br />
SSRIs to target depression<br />
Meyer and Block<br />
VOLUME 9, NUMBER 2 � MARCH/APRIL 2011 www.SupportiveOncology.net 49