Simulation Today Autumn 2019
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
Volume 1 No. 1<br />
<strong>Autumn</strong> <strong>2019</strong><br />
<strong>Simulation</strong> <strong>Today</strong><br />
A resource for all involved in the teaching and practice of simulation<br />
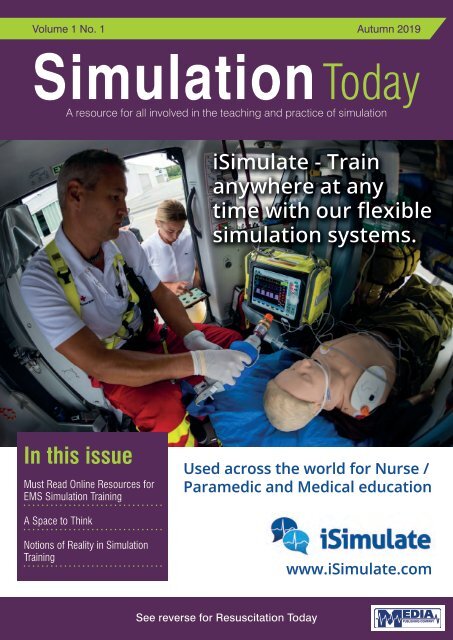
iSimulate - Train<br />
anywhere at any<br />
time with our flexible<br />
simulation systems.<br />
In this issue<br />
Must Read Online Resources for<br />
EMS <strong>Simulation</strong> Training<br />
Used across the world for Nurse /<br />
Paramedic and Medical education<br />
A Space to Think<br />
Notions of Reality in <strong>Simulation</strong><br />
Training<br />
www.iSimulate.com<br />
See reverse for Resuscitation <strong>Today</strong>
CONTENTS<br />
CONTENTS<br />
<strong>Simulation</strong> <strong>Today</strong><br />
4 EDITORS COMMENT<br />
6 FEATURE Must Read Online Resources for EMS <strong>Simulation</strong><br />
Training Program Success<br />
9 FEATURE A Space to Think<br />
15 FEATURE Notions of reality in simulation training<br />
17 FEATURE Focused nurse-defibrillation training: A simple and<br />
cost-effective strategy to improve survival from<br />
in-hospital cardiac arrest<br />
21 COMPANY NEWS<br />
This issue edited by:<br />
David Halliwell MSc<br />
c/o Media Publishing Company<br />
Media House<br />
48 High Street<br />
SWANLEY, Kent BR8 8BQ<br />
ADVERTISING & CIRCULATION:<br />
Media Publishing Company<br />
Media House, 48 High Street<br />
SWANLEY, Kent, BR8 8BQ<br />
Tel: 01322 660434 Fax: 01322 666539<br />
E: info@mediapublishingcompany.com<br />
www.MediaPublishingCompany.com<br />
PUBLISHED:<br />
Spring, Summer and <strong>Autumn</strong><br />
COPYRIGHT:<br />
Media Publishing Company<br />
Media House<br />
48 High Street<br />
SWANLEY, Kent, BR8 8BQ<br />
COVER STORY<br />
iSimulate provides smart simulation solutions that are used by clinical<br />
education organizations across the world. Our mantra is simple – we use the<br />
best of current mobile technology (iPads etc) to create products that are more<br />
realistic, cost effective and simpler to use than traditional simulation solutions.<br />
The latest version - REALITi360 is a modular simulation ecosystem<br />
incorporating a patient simulator, CPR feedback and video capture in a single<br />
simulation system.<br />
Please contact us for further information:<br />
Info@isimulate.com<br />
www.isimulate.com<br />
PUBLISHERS STATEMENT:<br />
The views and opinions expressed in<br />
this issue are not necessarily those of<br />
the Publisher, the Editors or Media<br />
Publishing Company.<br />
Next Issue Spring 2020<br />
Subscription Information – <strong>Autumn</strong> <strong>2019</strong><br />
<strong>Simulation</strong> <strong>Today</strong> is a tri-annual publication<br />
published in the months of March and<br />
September. The subscription rates are as<br />
follows:-<br />
UK:<br />
Individuals - £12.00 inc. postage<br />
Commercial Organisations - £30.00 inc. postage<br />
Rest of the World:<br />
Individuals - £60.00 inc. postage<br />
Commercial Organisations - £72.00 inc. postage<br />
We are also able to process your<br />
subscriptions via most major credit<br />
cards. Please ask for details.<br />
Cheques should be made<br />
payable to MEDIA PUBLISHING.<br />
Designed in the UK by me&you creative<br />
SIMULATION TODAY - AUTUMN <strong>2019</strong><br />
3
EDITORS COMMENT<br />
EDITORS COMMENT<br />
<strong>Simulation</strong> is an educational tool or technique which is dramatically changing as<br />
our students embrace new ways of learning and teaching.<br />
SIMULATION TODAY - AUTUMN <strong>2019</strong><br />
“3D printing<br />
and scanning<br />
are becoming<br />
common in<br />
hospitals as<br />
we develop<br />
new lifelike<br />
education<br />
tools, and the<br />
“make your<br />
own” teaching<br />
tool community<br />
continues to<br />
gain traction.”<br />
Historically our thoughts were shaped by a few key individuals, whose interest in undertaking<br />
medical simulation were driven by a desire to improve a technique or promote a particular<br />
method of clinical practice. (An example of which is the ‘Resuscitation Annie’ – developed by<br />
Laerdal, which was specifically developed to promote participation as the global desire to teach<br />
resuscitation came into the public consciousness.)<br />
But <strong>Simulation</strong> in the 21st century is very different to that of the last century. As educators we<br />
have new tools at our disposal, we have access to cheap Augmented Reality, Mixed Reality,<br />
Virtual Reality, all of which are being used to enhance Medical and Nursing / Paramedical AHP<br />
education.<br />
3D printing and scanning are becoming common in hospitals as we develop new lifelike<br />
education tools, and the “make your own” teaching tool community continues to gain traction.<br />
This Journal will feature many of the leading thinkers in Healthcare <strong>Simulation</strong>, and will share ideas<br />
from the worlds of Human Factors, Education and Educational Equipment.<br />
We will be sharing individual experiences, and showcasing leading products and engaging with<br />
key thinkers from around the world.<br />
We hope that this journal will be seen as a resource and is packed with sufficient information to<br />
make it useful as a reference point for the reader.<br />
Best Wishes<br />
David Halliwell MSc<br />
David Halliwell is a Senior Teaching Fellow at 2 x UK Universities, leading modules in healthcare<br />
<strong>Simulation</strong>.<br />
A senior NHS clinician and manager for many years, David developed many educational<br />
programmes and learning strategies, most recently he began developing his own education<br />
tools. Lecturing internationally – he recently won the “Best Overall Presentation” at the Simghosts<br />
conference in Miami.<br />
4
HPSN UK<br />
December 3-4<br />
Nottingham Gateway<br />
HPSN UK <strong>2019</strong> is an international conference focused on advancing the practice and<br />
innovation of healthcare simulation for educators, technologists, technicians, nurses,<br />
doctors, midwives, allied health, patient safety leads and other healthcare professionals.<br />
Make valuable connections, experience exciting keynotes and attend special events.<br />
Call for Sessions<br />
Share your expertise in a workshop,<br />
presentation or poster. Abstract submissions<br />
until October 30th at hpsn.com<br />
Register Now<br />
Don’t miss out as space is limited for this<br />
free event.<br />
Register at hpsn.com<br />
Your worldwide<br />
training partner<br />
of choice
FEATURE<br />
MUST READ ONLINE RESOURCES<br />
FOR EMS SIMULATION TRAINING<br />
PROGRAM SUCCESS<br />
Lance Baily BA, EMT-B (https://www.linkedin.com/in/lancebaily/)<br />
Founder of Healthy<strong>Simulation</strong>.com & SimGHOSTS.org<br />
Lance@Healthy<strong>Simulation</strong>.com<br />
SIMULATION TODAY - AUTUMN <strong>2019</strong><br />
In the United States, a National Association for EMS Educators<br />
(NAEMSE) supported research article entitled “<strong>Simulation</strong> Use in<br />
Paramedic Education Research (SUPER): A Descriptive Study” reported<br />
on the utilization of medical simulation in EMS programs across the<br />
Country. The publication found some shocking results, in that had some<br />
shocking findings, in that:<br />
“Paramedic programs reported they have or have access to a wide<br />
range of simulation resources” but that “<strong>Simulation</strong> equipment (of any<br />
type) reportedly sits idle and unused in (31%) of programs” due to “lack<br />
of training”.<br />
With the methodology of medical simulation following behind the<br />
advances in healthcare simulation technology, combined with the<br />
inability of programs to invest beyond equipment into instructor training<br />
-- it is no wonder clinical simulation in EMS is slow to adopt. That’s<br />
why administrators and EMS Training program directors must carefully<br />
consider the need to train and educate instructors as a true cost of<br />
providing simulation training, beyond the shiny new toys of medical<br />
simulators.<br />
Finding key resources is half the battle, so here below are a brief<br />
breakdown of the 5 Top Medical <strong>Simulation</strong> resource articles available<br />
for free on Healthy<strong>Simulation</strong>.com to help EMS programs across the UK<br />
jump start or expand their simulation programs.<br />
Healthy<strong>Simulation</strong>.com is the leading online medical simulation<br />
resource website providing the latest news, conference highlights,<br />
research updates, job listings, product demos and more!<br />
1. <strong>Simulation</strong> Use in Paramedic Education Research (SUPER):<br />
A Descriptive Study<br />
(https://www.healthysimulation.com/7081/simulation-use-inparamedic-education-research-super-a-descriptive-study/).<br />
The purpose of this research was to characterize the use of<br />
simulation in initial paramedic education programs in order to assist<br />
stakeholders’ efforts to target educational initiatives and resources.<br />
This group sought to provide a snapshot of what simulation<br />
resources programs have or have access to and how they are<br />
used; faculty perceptions about simulation; whether program<br />
characteristics, resources, or faculty training influence simulation<br />
use; and if simulation resources are uniform for patients of all ages.<br />
2. JEMS: Standardization of EMS <strong>Simulation</strong> Activities<br />
Improves the Learning Experience<br />
(https://www.healthysimulation.com/16618/jemsstandardization-of-ems-simulation-activities-improves-thelearning-experience/):<br />
A recent JEMS publication by Aaron<br />
Dix, NRP, MBA, CHSE, NCEE, CP-C , Jennifer McCarthy, MAS,<br />
NRP, MICP, CHSE , and Andrew E. Spain, MA, NCEE, EMT-P<br />
entitled “Standardization of EMS <strong>Simulation</strong> Activities Improves<br />
the Learning Experience” concluded that “Standardization is<br />
an essential consideration for any simulation activity” and that<br />
“the level of standardization must be specifically chosen and<br />
incorporated into the design to ensure that each simulation is<br />
appropriate and useful.” Furthermore, the research found that<br />
“Standardization within simulation activities improves quality and<br />
the experience for learners [and] also enhances the efforts of<br />
proper simulation design, execution and debriefing making the<br />
effort of evidence-based practice worth it.”<br />
3. About Ambulance Simulators<br />
(https://www.healthysimulation.com/ambulance-simulator/):<br />
Providing EMS students and professionals with realistic<br />
training is crucial to their success in the field. By providing<br />
EMS learners with the opportunity to train in the most realistic<br />
way possible, clinical educators can reduce costs associated<br />
with medical errors while improving provider performance.<br />
Ambulance Simulators enable Emergency Medical Service (EMS)<br />
professionals to realistically train for the unique challenges<br />
of patient care within a confined and mobile space. Ranging<br />
from simple environmental wallpaper coverings for static sim<br />
lab rooms to fully immersive simulated ambulances on moving<br />
hydraulic presses with realistic lights and sirens, ambulance<br />
simulation has quickly become a key component in educating<br />
and training EMS providers.<br />
4. <strong>Simulation</strong> Technician Entry Level Job Description<br />
Downloadable Template<br />
(https://www.healthysimulation.com/18426/medicalsimulation-technician-job-description)<br />
A <strong>Simulation</strong> Technician/<br />
Technologist works in the field of healthcare simulation<br />
supporting the many technical aspects of medical simulation.<br />
Here, we take a look at the general entry level requirements of a<br />
Sim Tech position and provide a downloadable template for your<br />
program to use as a starting point. Additional articles related to<br />
6
FEATURE<br />
simulation staffing of Sim Techs and other positions can be found<br />
on our Medical <strong>Simulation</strong> Jobs page, including where to find<br />
Sim Techs, how to train them, and what to pay them!<br />
5. How Vassar College Built Their Own Ambulance Simulator<br />
(https://www.healthysimulation.com/16238/jems-covershow-vassar-college-built-their-own-ambulance-simulator/)<br />
Ambulance <strong>Simulation</strong> for EMS students is an important aspect<br />
of training that may be difficult to reproduce repeatedly. Not many<br />
programs have available access to a contemporary ambulance<br />
due to obvious cost or scheduled “active duty” cycles. Enter<br />
Vassar College who empowered an EMT student with set building<br />
experience to help build them their “Simbulance”, a confined but<br />
open air ambulance simulator design with attached viewing deck!<br />
The Simbulance project came about from the desire to provide a<br />
more realistic simulated experience—one that includes lifting and<br />
moving a patient to an ambulance, performing skills in the back of<br />
an ambulance, calling in reports to the hospital and, finally, taking<br />
the patient out of the ambulance and bringing them to the next<br />
point of care in the ED.<br />
Do not have space for<br />
traditional patient<br />
simulators?<br />
Try VERA, your<br />
standardised patient,<br />
a VR solution that<br />
allows patient<br />
communication via<br />
VR Headset, computer<br />
browser or mobile device.<br />
Looking to Attend a <strong>Simulation</strong><br />
Conference?<br />
<strong>Simulation</strong> Champions across the UK should consider attending<br />
the annual Association for Simulated Practice in Healthcare (ASPiH)<br />
event. Learn more at https://aspih.org.uk/<br />
Ask us for a demo<br />
www.simulaids.eu.com/vera<br />
info@simulaids.eu.com 01530 512425<br />
VERA – exclusively available in the UK from Simulaids Ltd<br />
WHY NOT WRITE FOR US?<br />
<strong>Simulation</strong> <strong>Today</strong> welcomes the submission of clinical<br />
papers, case reports and articles that you<br />
feel will be of interest to your colleagues.<br />
The publication is mailed to all resuscitation, A&E and anaesthetic departments<br />
plus all intensive care, critical care, coronary care and cardiology units plus<br />
Universities and Schools of Midwifery that teach <strong>Simulation</strong>.<br />
All submissions should be forwarded to info@mediapublishingcompany.com<br />
If you have any queries please contact the publisher Terry Gardner via:<br />
info@mediapublishingcompany.com<br />
SIMULATION TODAY - AUTUMN <strong>2019</strong><br />
7
iSimulate - Train anywhere at any time<br />
with our flexible simulation systems.<br />
Used across the world for Nurse / Paramedic<br />
and Medical education<br />
www.iSimulate.com
FEATURE<br />
A SPACE TO THINK<br />
How can recent advances in cognitive load theory inform<br />
practice in simulation-based healthcare education?<br />
Dr Lewis Moore BSc MBBS PGCert; Student No. – 17834412<br />
Module – MDM148 Principles and Practice of <strong>Simulation</strong>.<br />
Introduction<br />
<strong>Simulation</strong> is becoming a central modality in medical education with<br />
recent evidence of educational benefit and improved patient outcomes<br />
(1, 2). <strong>Simulation</strong> has traditionally taken its theoretical underpinning from<br />
experiential learning (3) and constructivism (4), but the last ten years<br />
have seen an explosion of publications attempting to use cognitive load<br />
theory to improve simulation-based education (SBE)(5-9).<br />
Cognitive Load Theory<br />
Cognitive load theory (CLT) is based on the neuropsychological<br />
observation that the human working memory is severely limited in both<br />
capacity and time (10, 11), and states that if its limits are exceeded,<br />
errors will be made and learning will be impaired (12). The long-term<br />
memory, however, is effectively unlimited, information in the long-term<br />
memory is stored in organised schema, and may be usefully accessed<br />
with only minimal cognitive effort. CLT attempts to minimise the risk of<br />
cognitive overload and maximise learning (13).<br />
CLT splits cognitive workload into three types; intrinsic load which is<br />
related to the complexity of the problem to be solved, extraneous load<br />
which distracts from the problem and wastes cognitive resources, and<br />
germane load (sometimes conceptualised as a sub-type of intrinsic<br />
load) which represents cognition used to organise or categorise<br />
information, and is thought to be a source of learning (14).<br />
Intrinsic load is seen as highest when a problem has a high degree<br />
of element interactivity, where many factors must be considered<br />
simultaneously to produce a ‘correct’ answer (think long multiplication<br />
or complex grammar). Medical care and procedures, simulated or<br />
otherwise, are such problems; learners must assess many body<br />
systems simultaneously using different modalities (history, examination,<br />
imaging, bloods) while communicating effectively with a patient and<br />
members of the team (5). The same is true in the simulation lab, and<br />
we must be mindful that complex tasks may leave minimal cognitive<br />
space for learning, and that small amounts of extraneous load may lead<br />
to cognitive overload, expressed as frustration and poor performance.<br />
The principles of CLT state that we should adjust the intrinsic load to<br />
be appropriate to the learner, while minimising the extraneous load and<br />
introducing or improving the germane load to maximise learning. This is<br />
demonstrated in Figure 1.<br />
Outline of this Essay<br />
This essay will initially explore the design principles that were taken<br />
from the wider education community and applied to medical education<br />
- more specifically, to SBE. It will then explore the science of measuring<br />
cognitive load (CL), the effect of emotion on CL, and finally will<br />
examine studies which have used CLT principles to design educational<br />
interventions and test their efficacy.<br />
Cognitive Load Theory in <strong>Simulation</strong>-Based<br />
Education<br />
Fraser et al. adapted the primary CLT literature (12) derived from the<br />
classroom setting in disciplines such as mathematics and engineering,<br />
and previous attempts to make CLT relevant to medical education (5)<br />
for use in medical SBE, making many practical recommendations (7) as<br />
explored below.<br />
Figure 1 – Graphical representation of cognitive limits and different<br />
states of optimisation. (Adapted from Sweller J, Van Merrienboer JJ,<br />
Paas FG. Cognitive architecture and instructional design. Educational<br />
psychology review. 1998;10(3):251-6)<br />
Minimising Extraneous Load<br />
Extraneous load (EL) is the enemy in CLT; neither relevant to the task<br />
at hand nor educationally useful, making its reduction a core goal in<br />
educational design. EL is primarily conceptualised as deriving from<br />
information that is presented to the learner sub-optimally, and the<br />
strategies for minimising EL therefore focus on this.<br />
The split attention effect is the observation that the requirement to<br />
obtain information from multiple sources simultaneously, and to usefully<br />
integrate these, produces more CL than if the information was in a single<br />
source. A large body of evidence in the CL literature outside medicine<br />
(15) demonstrates that if all information is presented in a single form or<br />
location, then learning is enhanced via reduction of extraneous load.<br />
Summarising all relevant information on a card would reduce CL but<br />
impair realism, clearly there is a balance to be struck depending on the<br />
SIMULATION TODAY - AUTUMN <strong>2019</strong><br />
9
FEATURE<br />
SIMULATION TODAY - AUTUMN <strong>2019</strong><br />
expertise of the learner and the desired realism of the scenario. With this<br />
principle in mind, educators can make this a conscious choice and even<br />
produce different versions of the same scenario with different levels of<br />
realism and visuospatial cognitive demand.<br />
Contrary to this, the expertise reversal effect (14) describes how the<br />
opposite may be true for expert learners who may feel alienated if they<br />
are given physiological data written down, and cannot see, for instance,<br />
individual waveforms on the monitor which they may usually rely on.<br />
The worked example effect suggests that being shown how to complete<br />
a task carries more educational value, or is at least much more efficient<br />
than solving the problem independently(16). In simulation this is<br />
conceptualised in several ways; for instance a skilled assistant may<br />
interpret blood gas or ultrasound images. If these skills are not explicit<br />
learning objectives and cannot be performed ‘automatically’ by the<br />
learner, then they can reasonably be outsourced to help prevent overload.<br />
Another implementation of this principle would be to allow learners<br />
to retry a scenario they had struggled with after some reflection and<br />
feedback (17). This mirrors Kolb’s experiential learning (3) cycling<br />
between action and reflection.<br />
Adjusting Intrinsic Load<br />
As learners gain expertise, they develop schemas allowing them to<br />
organise and simplify information, making a task such as assessing<br />
a patient with chest pain daunting or difficult (high intrinsic CL) for<br />
a medical student but very simple (minimal intrinsic CL) for even a<br />
relatively-junior paramedic or emergency medicine physician. Because<br />
of this, we must carefully design tasks to ensure that the intrinsic load is<br />
are neither inherently too complex nor too mundane for the learner, as<br />
this would impair learning.<br />
The pretraining effect (18) encourages that we prepare students<br />
adequately for a simulated experience; showing them the monitoring<br />
equipment, where they might find pulses on the Laedral SimMan 3G,<br />
the location of drugs and equipment, and the format in which they can<br />
expect briefing and assistance. Providing this information will prevent<br />
these otherwise small questions from building into an overwhelming fog<br />
of uncertainty.<br />
Germane Load<br />
Reduction and optimisation of other forms of CL theoretically allow us<br />
to leave some of the learner’s working memory to learn or to structure<br />
the task (19). Some suggestions regarding how this can be done are<br />
to introduce structural assessments like ABCDE, 4 H’s and 4T’s or to<br />
ask the learner to explain their thought process as they go along. While<br />
adding another simultaneous task will necessarily improve cognitive<br />
workload, this approach is thought to guide the learner towards the<br />
most important ideas and information, and improve outcomes. If the<br />
learner asks themselves these questions in a similar ‘real-life’ situation,<br />
their outcomes should theoretically be better.<br />
What Does it Add?<br />
As a purveyor, organiser and consumer of medical education on<br />
nearly a daily basis, the author has become increasingly aware of<br />
the prevalence of disparity between the difficulty of an educational<br />
intervention and the needs and abilities of the learners. While it may<br />
seem like common sense to teach at the right level of detail, this<br />
is often not the case, or is made very challenging by large gaps in<br />
seniority between the learner and educator (and therefore assumed<br />
knowledge) or by the wide range of ability in a cohort of learners. The<br />
above principles allow or indeed encourage simulationists and other<br />
educators to identify the needs and abilities of the learner, and adjust<br />
the intervention accordingly. They may help us not to deliver SBE badly,<br />
but can they lead us to excellence? While these tools may be useful for<br />
some, they seem undeserving of the hype that CLT has generated in the<br />
recent years.<br />
A summary of CLT-based recommendations for SBE can be found in<br />
Appendix 1.<br />
Measuring Cognitive Load<br />
The scientific method suggests that if CL indeed exists, then there<br />
should be a way to measure it (20) and observe its effects. Only if CL<br />
can be measured reliably can we draw meaningful conclusions about<br />
its effects.<br />
How is CL Measured?<br />
As a cognitive phenomenon, the obvious method to measure CL is<br />
self-reporting. Paas (21) pioneered this in the educational psychology<br />
domain and his validated CL scale (1 – very very low to 9 – very<br />
very high) is widely used in medical education. NASA created their<br />
own tool, NASA-TLX, for assessing mental workload (22), which is a<br />
distinct concept but widely thought to be analogous to cognitive load.<br />
Problems associated with self-reporting include the intrusive nature<br />
of the sampling, the disruptive nature of pausing a task for a learner<br />
to complete a questionnaire (itself adding to CL), or the reporting<br />
happening after the exercise, introducing recall bias. CL is sometimes<br />
inferred from surrogate physiological measurements such as heart<br />
rate (23), EEG (24) or pupillary tracking or dilation (25). Physiological<br />
measurements give little indication as to absolute CL, but indicate<br />
fluctuations over time (8). The final way that CL is measured is by asking<br />
learners to perform a secondary task alongside the main intervention,<br />
such as pressing a button when a vibrating stimulus is applied to<br />
their arm (26). The response time (or other performance measure) is<br />
hypothesised to indicate the CL engaged in the primary task.<br />
Validity of CL Measurements<br />
Naismith and Cavalcanti produced a systematic review (8) of the SBE<br />
literature correlating cognitive load measurements and educational<br />
outcomes or task performance. Included studies were rated out of 5<br />
for the validity of their measurement techniques, using a tool previously<br />
created by Cook et al. (27). Of the 35 studies compared across all<br />
domains, 6 showed that higher cognitive load was associated with<br />
better learning or performance outcomes (positive association), 8<br />
showed a negative association and 14 were neutral. In the studies from<br />
the medical education literature, there were no studies with positive<br />
association, 5 negative, and 7 neutral. The studies showing negative<br />
association between CL and performance came from studies with a<br />
higher mean validity score (See Figure 2).<br />
The overarching message of this review is that the scientific community<br />
does not have an agreed- upon standard for how to measure cognitive<br />
10
FEATURE<br />
load. Many studies modify the Paas or NASA-TLX instruments, or create<br />
their own with little or no attempt to validate them before using them<br />
to draw conclusions. Physiology or even observer rating is also used<br />
without any solid evidence of validity. The literature does not compare<br />
‘like with like’ and therefore, the heterogeneity of these results is<br />
unsurprising.<br />
CL as Meta-Examination<br />
Aldekhyl et al. (28) used an ultrasound-based simulation to assess<br />
sonographic competence of 29 clinicians of varying seniority. CL<br />
was approximated by tracking eye movements while the participants<br />
attempted to obtain suitable images. It was found that higher gaze-shift<br />
rate, indicating higher cognitive load was negatively associated with<br />
performance. The more experienced clinicians, having consolidated<br />
their knowledge, find it easier to obtain the images, and therefore CL<br />
is low, whereas those with less experience can perform the task, but at<br />
greater cognitive expense. This observation is profoundly striking as it<br />
opens a new door for assessment of clinical competence; we would<br />
clearly prefer to employ an anaesthetist who could calmly complete a<br />
crossword while delivering a safe anaesthetic than one who nervously<br />
watched the monitor throughout. This does however seem somewhat<br />
perverse and intrusive; as a profession, we are used to being assessed<br />
and examined, but wearing a heart rate monitor and eye-tracking<br />
equipment during a clinical station would seem very dystopian at a job<br />
interview.<br />
Summary<br />
The ability to reliably measure a variable is a prerequisite to<br />
understanding its importance. It has been demonstrated that while<br />
many studies have purportedly measured ‘cognitive load’ they have<br />
measured a wide variety of different things. A consensus on how CL is<br />
to be measured, and its experimental validation, must be made a priority<br />
by the research community for the quality of evidence to improve.<br />
Emotion and Cognitive Load<br />
Cognitive load theorists have attempted to integrate emotion into CLT,<br />
with emotion being classified as intrinsic load in, for instance, a breaking<br />
bad news scenario (7), and extrinsic when general ‘stress’ appears to<br />
shrink the size of the usable working memory (31).<br />
In an observational study, Fraser et al. asked 84 undergraduate<br />
medical students to rate their emotional state and cognitive load in<br />
an SBE scenario (32), finding that students with a higher perceived ‘<br />
invigoration’ also experienced higher CL, and were significantly less<br />
likely to correctly identify clinical signs (regression coefficient 0.63, 95%<br />
CI 0.28–0.99; p = 0.001).<br />
The same authors decided to use CLT to attempt to answer an ongoing<br />
debate in SBE: should the mannikin die during sim scenarios (33)?<br />
While death of the mannikin is necessary for practicing cardiac arrest<br />
management, it is sometimes used as feedback for poor performance,<br />
and while some see this as highly realistic and motivating feedback,<br />
others feel that it is a potentially damaging violation of the safe learning<br />
environment that simulation attempts to provide (34). The study in<br />
question (35) used a randomised controlled trial to assess the effect<br />
of unexpected manikin death on emotion, cognitive load, and distant<br />
learning outcomes. 112 undergraduate medical students undertook a<br />
simulation scenario involving salicylate poisoning. They were randomly<br />
assigned to 2 groups whose scenarios differed only in the last 3<br />
minutes; one group with a good patient outcome and the second with<br />
sudden deterioration and death. The students’ self-rated emotions were<br />
significantly poorer and subjective cognitive load significantly higher<br />
in the unexpected death cohort (see Figure 3). Three months after<br />
the simulation, the students faced the same scenario in a summative<br />
objective structured clinical examination (OSCE). Those that were in<br />
the mannikin death group were significantly less likely (70.9% vs 86.9%:<br />
OR of 0.37, 95% CI, 0.14-0.95; P = 0.04) to be rated as competent by<br />
the examiner and pass the station (see Figure 3). While it may seem<br />
appropriate for some for the mannikin to die, this study gives strong<br />
evidence to support the view that the emotional impact of this outcome<br />
will impair learning, and therefore should not be routinely used in<br />
simulation practice.<br />
In the broader psychological literature, the relationship between emotion<br />
and learning has been studied extensively, and certain principles are<br />
held to be true. Positive emotions can stimulate motivation, enhance<br />
creativity, and improve learning outcomes (7, 29), while negative<br />
emotions affect learning unpredictably, sometimes acting to heighten<br />
the relevance and therefore recall of a memory, and other times thought<br />
to overwhelm the ability to learn (30).<br />
Figure 2 – The studies that identify a negative relationship between<br />
cognitive load and learning outcomes used, on average, the more valid<br />
measurement tools. (Taken from Naismith LM, Cavalcanti RB. Validity<br />
of cognitive load measures in simulation-based training: a systematic<br />
review. Academic Medicine. 2015;90(11):S24-S35)<br />
Cognitive Load in Practice<br />
Educational Intervention Designed using CLT Principles<br />
Andersen et al. tested CLT-based design in a small randomised<br />
controlled trial to teach surgical skills in a virtual reality (VR) simulation<br />
(36). Eighteen medical students underwent an hour of training in<br />
performing mastoidectomy on a freely available VR training package<br />
(See Figure 4).<br />
Half trained using traditional instructions, and half trained using CLTdesigned<br />
instructions, comprised of worked examples and partially<br />
completed procedures. Students were then assessed by expert<br />
examiners for competence in performing this procedure. Students who<br />
studied worked examples reported higher CL (52% vs 41%, p = 0.02),<br />
and performed less well in examination (13.0 vs 15.4, p < 0.005) than<br />
those studying with traditional instructions.<br />
This study adds to the evidence that higher cognitive load impairs<br />
learning. The study detracts, however, from the suggestion that worked<br />
SIMULATION TODAY - AUTUMN <strong>2019</strong><br />
11
FEATURE<br />
Figure 3<br />
examples provide lower CL and improved outcomes. It is important not<br />
to draw too many conclusions from a small study, and to appreciate<br />
that there are many factors involved in cognitive load and learning<br />
outcomes. Perhaps the worked examples were difficult to navigate in<br />
the software interface, or perhaps there were too many sections to get<br />
through in the allotted hour? The study highlights the use of including<br />
CL analysis when assessing the usefulness of a training intervention.<br />
CL Analysis of Other SBE Interventions<br />
Other authors have used CL solely as an adjunct in their analysis of<br />
an education intervention. Dankbaar et al. tested a computer-based<br />
simulation game against other interventions for the acquisition of<br />
emergency care and resuscitation skills (37). All 61 students were<br />
trained using an e- learning module and were then randomised into<br />
three groups to receive either a) no further training, b) 2 hours of paperbased<br />
practice cases, or c) 2 hours of computer-based simulation,<br />
and were later tested in a manikin-based simulation. The clinical<br />
competence of control, paper, and simulation groups were scored<br />
at 7.5, 7.9 and 7.2 respectively (p= 0.12); adding a further 2 hours<br />
of different forms of study did not significantly improve the students’<br />
resuscitation skills, and cognitive load was not reported significantly<br />
differently between the groups.<br />
The author included a CL questionnaire as part of the analysis;<br />
interestingly, the questionnaire has subsections for intrinsic cognitive<br />
load (‘’the content of the e-module was very complex’’), extraneous<br />
cognitive load (‘’the explanations were very unclear’’), and germane<br />
cognitive load (“the e-module really enhanced my understanding of the<br />
problems that were discussed’’). The author cited Paas (38) and stated<br />
that the scale was previously validated, but appears to have missed<br />
the point entirely: the cited article makes no reference to the ability of<br />
learners to be able to self-assess subtypes of CL, and the questions<br />
indicate a general misunderstanding of CL theory. As discussed in the<br />
section on measurement of CL, authors appear unaware of the need to<br />
use validated instruments, and feel it appropriate to modify or design<br />
their own questionnaires without any validation. Aside from this, it seems<br />
highly appropriate to use CL measurements as part of the assessment<br />
of simulation or other interventions in medical education. If learning<br />
outcomes are poor, then cognitive overload is one possible explanation,<br />
and should be easily picked up on a post-course questionnaire.<br />
Conclusion<br />
There has been a large amount of publication activity concerning CLT<br />
in the SBE literature in the last 5 years. The initial recommendations<br />
from the wider literature have been adapted and applied practically<br />
to healthcare SBE to some effect. While there have been some efforts<br />
to standardise measurement of CL, authors often design their own<br />
unvalidated instruments, which is a clear weakness of the current body<br />
of literature, requiring further research. CLT can help us to understand<br />
certain specific questions in simulation practice (Should we allow<br />
manikins to die?) and may provide an intermediary for the link between<br />
emotion and educational attainment. CLT is not panacea for educational<br />
design, but is a tool that can help us to avoid cognitive overload, which<br />
is one of several potential reasons for poor outcomes from educational<br />
interventions.<br />
References<br />
1. Cook DA, Hatala R, Brydges R, Zendejas B, Szostek JH, Wang<br />
AT, et al. Technology-enhanced simulation for health professions<br />
education: a systematic review and meta-analysis. Jama.<br />
2011;306(9):978-88.<br />
SIMULATION TODAY - AUTUMN <strong>2019</strong><br />
Figure 4 – A virtual reality training software for performing mastoidectomy.<br />
(Taken from Andersen SAW, Mikkelsen PT, Konge L, Cayé-Thomasen P,<br />
Sørensen MS. The effect of implementing cognitive load theory-based<br />
design principles in virtual reality simulation training of surgical skills: a<br />
randomized controlled trial. Advances in <strong>Simulation</strong>. 2016;1(1):20)<br />
2. McGaghie WC, Issenberg SB, Barsuk JH, Wayne DB. A critical<br />
review of simulation-based mastery learning with translational<br />
outcomes. Medical education. 2014;48(4):375-85.<br />
3. Kolb D. Experiential learning as the science of learning and<br />
development. Englewood Cliffs, NJ: Prentice Hall; 1984.<br />
4. Yoders S. Constructivism Theory and Use from 21 st Century<br />
Perspective. Journal of Applied Learning Technology. 2014;4(3).<br />
5. Van Merriënboer JJ, Sweller J. Cognitive load theory in health<br />
professional education: design principles and strategies. Medical<br />
education. 2010;44(1):85-93.<br />
6. Young JQ, Van Merrienboer J, Durning S, Ten Cate O. Cognitive<br />
load theory: Implications for medical education: AMEE guide no.<br />
86. Medical teacher. 2014;36(5):371-84.<br />
12
FEATURE<br />
7. Fraser KL, Ayres P, Sweller J. Cognitive load theory for the design of<br />
medical simulations. <strong>Simulation</strong> in Healthcare. 2015;10(5):295-307.<br />
8. Naismith LM, Cavalcanti RB. Validity of cognitive load measures<br />
in simulation-based training: a systematic review. Academic<br />
Medicine. 2015;90(11):S24-S35.<br />
9. Cao CG, Zhou M, Jones DB, Schwaitzberg SD. Can surgeons<br />
think and operate with haptics at the same time? Journal of<br />
Gastrointestinal Surgery. 2007;11(11):1564-9.<br />
10. Miller GA. The magical number seven, plus or minus two: Some<br />
limits on our capacity for processing information. Psychological<br />
review. 1956;63(2):81.<br />
11. Peterson L, Peterson MJ. Short-term retention of individual verbal<br />
items. Journal of experimental psychology. 1959;58(3):193.<br />
12. Sweller J. Cognitive load during problem solving: Effects on<br />
learning. Cognitive science. 1988;12(2):257-85.<br />
13. Sweller J. Cognitive load theory. Psychology of learning and<br />
motivation. 55: Elsevier; 2011. p. 37-76.<br />
14. Kalyuga S. Cognitive load theory: How many types of load does it<br />
really need? Educational Psychology Review. 2011;23(1):1-19.<br />
15. Ginns P. Integrating information: A meta-analysis of the spatial<br />
contiguity and temporal contiguity effects. Learning and<br />
Instruction. 2006;16(6):511-25.<br />
16. Clark RC, Nguyen F, Sweller J. Efficiency in learning: Evidence-based<br />
guidelines to manage cognitive load: John Wiley & Sons; 2011.<br />
17. Zigmont JJ, Kappus LJ, Sudikoff SN, editors. Theoretical<br />
foundations of learning through simulation. Seminars in<br />
perinatology; 2011: Elsevier.<br />
18. Mayer RE, Moreno R. Nine ways to reduce cognitive load in<br />
multimedia learning. Educational psychologist. 2003;38(1):43-52.<br />
19. Paas F, Van Gog T. Optimising worked example instruction:<br />
Different ways to increase germane cognitive load. Elsevier; 2006.<br />
20. Horton M. In defence of Francis Bacon: A criticism of the critics<br />
of the inductive method. Studies in History and Philosophy of<br />
Science Part A. 1973;4(3):241-78.<br />
training. Engineering in Medicine and Biology Society (EMBC),<br />
2012 Annual International Conference of the IEEE; 2012: IEEE.<br />
25. Reiner M, Gelfeld TM. Estimating mental workload through eventrelated<br />
fluctuations of pupil area during a task in a virtual world.<br />
International Journal of Psychophysiology. 2014;93(1):38- 44.<br />
26. Davis D, Oliver M, Byrne A. A novel method of measuring the<br />
mental workload of anaesthetists during simulated practice. British<br />
journal of anaesthesia. 2009;103(5):665-9.<br />
27. Cook DA, Zendejas B, Hamstra SJ, Hatala R, Brydges R. What<br />
counts as validity evidence? Examples and prevalence in a<br />
systematic review of simulation-based assessment. Advances in<br />
Health Sciences Education. 2014;19(2):233-50.<br />
28. Aldekhyl S, Cavalcanti RB, Naismith LM. Cognitive load predicts<br />
point-of-care ultrasound simulator performance. Perspectives on<br />
medical education. 2018;7(1):23-32.<br />
29. Bower GH, Forgas JP. Mood and social memory. 2001.<br />
30. Pekrun R. The impact of emotions on learning and achievement:<br />
Towards a theory of cognitive/motivational mediators. Applied<br />
Psychology. 1992;41(4):359-76.<br />
31. Beilock SL, Kulp CA, Holt LE, Carr TH. More on the fragility<br />
of performance: choking under pressure in mathematical<br />
problem solving. Journal of Experimental Psychology: General.<br />
2004;133(4):584.<br />
32. Fraser K, Ma I, Teteris E, Baxter H, Wright B, McLaughlin K.<br />
Emotion, cognitive load and learning outcomes during simulation<br />
training. Medical education. 2012;46(11):1055-62.<br />
33. Corvetto MA, Taekman JM. To die or not to die? A review of<br />
simulated death. <strong>Simulation</strong> in Healthcare. 2013;8(1):8-12.<br />
34. Rudolph JW, Raemer DB, Simon R. Establishing a safe container<br />
for learning in simulation: the role of the presimulation briefing.<br />
<strong>Simulation</strong> in Healthcare. 2014;9(6):339-49.<br />
35. Fraser K, Huffman J, Ma I, Sobczak M, McIlwrick J, Wright<br />
B, et al. The emotional and cognitive impact of unexpected<br />
simulated patient death: a randomized controlled trial. Chest.<br />
2014;145(5):958-63.<br />
21. Paas FG. Training strategies for attaining transfer of problemsolving<br />
skill in statistics: A cognitive-load approach. Journal of<br />
educational psychology. 1992;84(4):429.<br />
22. Hart SG, Staveland LE. Development of NASA-TLX (Task Load<br />
Index): Results of empirical and theoretical research. Advances in<br />
psychology. 52: Elsevier; 1988. p. 139-83.<br />
23. Yuviler-Gavish N, Yechiam E, Kallai A. Learning in multimodal<br />
training: Visual guidance can be both appealing and<br />
disadvantageous in spatial tasks. International journal of humancomputer<br />
studies. 2011;69(3):113-22.<br />
24. Soussou W, Rooksby M, Forty C, Weatherhead J, Marshall S,<br />
editors. EEG and eye-tracking based measures for enhanced<br />
36. Andersen SAW, Mikkelsen PT, Konge L, Cayé-Thomasen P,<br />
Sørensen MS. The effect of implementing cognitive load theorybased<br />
design principles in virtual reality simulation training<br />
of surgical skills: a randomized controlled trial. Advances in<br />
<strong>Simulation</strong>. 2016;1(1):20.<br />
37. Dankbaar ME, Alsma J, Jansen EE, van Merrienboer JJ, van<br />
Saase JL, Schuit SC. An experimental study on the effects<br />
of a simulation game on students’ clinical cognitive skills<br />
and motivation. Advances in Health Sciences Education.<br />
2016;21(3):505-21.<br />
38. Paas F, Tuovinen JE, Tabbers H, Van Gerven PW. Cognitive load<br />
measurement as a means to advance cognitive load theory.<br />
Educational psychologist. 2003;38(1):63-71.<br />
SIMULATION TODAY - AUTUMN <strong>2019</strong><br />
13
FEATURE<br />
Appendix 1 – Summary of CLT Principles for SBE Design<br />
SIMULATION TODAY - AUTUMN <strong>2019</strong><br />
(Taken from Fraser KL, Ayres P, Sweller J. Cognitive load theory for the design of medical simulations. <strong>Simulation</strong> in Healthcare. 2015;10(5):295-307.)<br />
14
FEATURE<br />
NOTIONS OF REALITY IN<br />
SIMULATION TRAINING<br />
Mike Davis PhD MEd DASE Cert Ed FAcadMEd<br />
Freelance consultant in continuing medical education, Blackpool UK<br />
Introduction<br />
Have you ever felt emotional about a seriously ill or traumatised<br />
patient, especially when you thought that you or your team were not<br />
managing as well as you might? Have you, on the death of the patient<br />
– maybe a 2 year old caught up in something totally unexpected and<br />
suddenly deteriorating in spite of you all doing everything you can – felt<br />
distressed, tearful, ashamed, that you were not able to save a life?<br />
I saw this happen in a large-scale simulation event (Davis et al 2008)<br />
conducted as part of preparation for deployment to the British military<br />
hospital in Afghanistan. A mannikin 2-year old with multiple blast injuries<br />
died under the care of a paediatric trauma specialist and her team.<br />
You might wonder why that would happen. Or you may have<br />
experienced that sense of reality that can emerge from a wellconstructed<br />
and presented simulation. This paper intends to explore<br />
why a plastic dummy can generate those responses, by exploring the<br />
nature of reality that a simulation can create.<br />
Aspects of reality<br />
The question we need to address is: to what extent does the physical<br />
reality contribute significantly to the simulated experience? For the<br />
military, this is an important component, but only accounts for 2 of the<br />
9 criteria for judging the potential impact of the HOSPEX simulation<br />
environment.<br />
Sociological reality<br />
The vast majority of professional life is conducted in multi-professional<br />
teams but simulation can become somewhat of a silo-endorsing<br />
activity by virtue of its success and subsequent adoption as part<br />
of undergraduate and postgraduate study in single professional<br />
groups. It is not uncommon, therefore, to find groups of, say medical<br />
or paramedic students fulfilling multiple roles in the management of<br />
a clinical case in a sim suite. Sociological reality is more likely to be<br />
manifested in in situ simulations, where HCPs experience a clinical case<br />
in their own, multi-disciplinary environment.<br />
Sociological reality in simulation is a product of deliberate efforts to<br />
ensure that people experiencing the event are doing so by playing<br />
themselves in role, and that the roles reflects the variety of contribution<br />
to that event. This serves the purpose of reinforcing the nature of the<br />
role and keeps participants in their comfort zone, by virtue of the fact<br />
that they are either:<br />
There is widespread acceptance that there are three types of reality that<br />
we experience in the simulated environment:<br />
playing themselves in a familiar situation (i.e. one designed to reinforce<br />
good practice and support others’ learning<br />
• physical<br />
• sociological, and<br />
• psychological<br />
and I am going to explore these in turn and then examine the ways in<br />
which they can combine to recreate what we loosely call “real life”.<br />
Physical reality<br />
There are increasingly sophisticated attempt to replicate a human being<br />
by virtue not only of the appearance, but also of the ways in which that<br />
can be enhanced by the manifestation of appropriate clinical features:<br />
sounds, discharges, words etc. Mannekins range in sophistication from<br />
simple plastic dolls with limited capacity for movement and no sounds,<br />
to chillingly realistic representations of human life, like the recent release<br />
of the geriatric patient by Simulaids, described in their literature as<br />
having:<br />
“realistic patient positioning, flexibility and superior range of motion<br />
[… capable of simulating] over 35 nursing and medical procedures”<br />
(simulaids.eu.com; [accessed 5th July <strong>2019</strong>])<br />
or<br />
playing themselves in an unfamiliar situation (i.e. but one that they could<br />
reasonably be expected to face)<br />
In either case, the sociological reality reinforces the team nature and<br />
the multiple responsibilities within the simulated case being managed,<br />
thereby making the simulation more life-like.<br />
Psychological reality<br />
This is a bi-product of every aspect of the way in which simulation is<br />
created and has been neatly summarised by GP and medical educator<br />
Lizzie Norris as “a busy brain”. Interestingly, it is just as likely to arise<br />
from an almost equipment free, small group simulation as it is from<br />
something taking place with the most sophisticated simulation suite.<br />
Among the early ambitions of the designers of the European Trauma<br />
Course (ETC), for example, was the capacity to arrive in a setting<br />
with minimal equipment and personnel and still teach a team-based<br />
approach to trauma management, by virtue of creating an intellectual<br />
SIMULATION TODAY - AUTUMN <strong>2019</strong><br />
15
FEATURE<br />
and emotional environment within which participants could explore their<br />
competence at their limits of prior experience.<br />
While physical and sociological reality arise from the environment and<br />
the invited participants, psychological reality is the product of the nature<br />
of the experience as it unfolds and this depends significantly on the<br />
extent to which information flow is realistic and timely.<br />
Information flow<br />
Information flow is the shorthand depiction of all of the sensory data that<br />
arise from a clinical case. In the case of the human patient being treated<br />
in resus, for example, this would be all of the information that is evident<br />
from receiving the patient, taking an SBAR handover from paramedics,<br />
to the outcomes of investigations arising from an A to E primary survey.<br />
This would include what the patient says (if they are talking), as well as<br />
any visual signs (bleeding, etc) and the results of any interventions like<br />
blood test results, CT scans, X` rays.<br />
The key difference between the mannikin and a patient is that in the<br />
former case, the facilitator of the simulation has to provide timely<br />
feedback as to the features that would emerge from a human patient.<br />
This might emerge, in a sophisticated mannikin as a consequence of a<br />
technical intervention; in a basic mannikin, it would be announced in a<br />
timely way by the facilitator. The key ingredient here is “timely”, providing<br />
the lead clinician running the scenario with information that was a<br />
product of the leader’s interventions, e.g.<br />
responsible for developing language skills in teenage pupils. We were<br />
looking for ways to develop linguistic competence in pupils by engaging<br />
them in challenging linguistic environments and we came across an<br />
activity called “Bafa Bafa”, which involved learners exploring significant<br />
cultural diversity. While BafaBafa created a fictional world, it was one<br />
that was negotiated using complex linguistic skills that students,<br />
functioning slightly beyond their comfort zones, had to negotiate, both<br />
in the activity of the game itself, but also in the debrief that followed.<br />
Those pupils demonstrated amazing commitment to being an Alpha or<br />
a Beta and subjected their experience in those roles to critical scrutiny in<br />
the debrief that followed. Their confidence and competence in a range<br />
of complex linguistic skills flourished as they lived out the reality that the<br />
game demanded of them. That reality, however, had no equipment and<br />
the sociological reality was the “real” reality of their community. The buy<br />
in, however, was the product of “the busy brain”.<br />
References<br />
Davis M, Driscoll P, Hanson J, Wieteska S (2008), The Advanced Life<br />
Support Group’s View of HOSPEX. JR Army Med Corps 154(3): 206-208<br />
Dr Mike Davis is a freelance consultant in continuing medical education<br />
based in Blackpool. He works predominantly in the life support<br />
community and has educator roles with Generic Instructor Course<br />
(ALGS/RC(UK)), ATLS and ETC.<br />
He is one of the authors (with Jacky Hanson, Mike Dickinson,<br />
Lorna Lees and Mark Pimblett) of “How to teach using simulation in<br />
healthcare”, published by Wiley-Blackwell in 2017.<br />
SIMULATION TODAY - AUTUMN <strong>2019</strong><br />
Team leader: (to circulation team member) Could you take the blood<br />
pressure, please?<br />
Circulation: (putting on and inflating cuff)<br />
Facilitator (after appropriate pause): It’s 90 over 40.<br />
etc<br />
The key issue in offering a simulation in this way is that learners<br />
managing the clinical case are expected to undertake tasks in an<br />
appropriate sequence, taking an appropriate amount of time, and<br />
eliciting (in a low fidelity setting), appropriate clinical signs from the<br />
facilitator of the event, or, in a more sophisticated environment, picking<br />
up those signs from the mannikin or a monitor.<br />
Integrating realities<br />
Whatever is offered in terms of physical and sociological reality, the<br />
success or otherwise of a simulation is dependent on the extent to<br />
which the learners engage in the psychological reality of the simulation:<br />
they enter into what the 19th century poet, Samuel Taylor Coleridge,<br />
called “the willing suspension of disbelief”. This psychological state<br />
capitalising to a greater or lesser extent on the physical and social<br />
manifestations of the simulation, lays the foundations for the buy-in: it is<br />
real because it feels real and there is sufficient demand being made on<br />
the participants’ minds that they have sufficient but not overwhelming<br />
cognitive load for them to maintain their focus on the unfolding story<br />
instead of thinking “This is a plastic mannikin”.<br />
I first got involved in simulation training as an English teacher<br />
HELLO, MY<br />
NAME IS<br />
I am the<br />
first Patient<br />
Communication<br />
Simulator (PCS).<br />
Ask us for a demo<br />
www.simulaids.eu.com/alex<br />
info@simulaids.eu.com 01530 512425<br />
ALEX – exclusively available in the UK from Simulaids Ltd<br />
16
FEATURE<br />
FOCUSED NURSE-DEFIBRILLATION TRAINING:<br />
A SIMPLE AND COST-EFFECTIVE STRATEGY TO IMPROVE<br />
SURVIVAL FROM IN-HOSPITAL CARDIAC ARREST<br />
John A Stewart<br />
Scandinavian Journal of Trauma, Resuscitation and Emergency Medicine 2010 18:42 https://doi:10.1186/1757-7241-18-42 © 2010 Stewart<br />
Reproduced with permission from the Scandinavian Journal of Trauma, Resuscitation and Emergency Medicine<br />
Abstract<br />
Time to first defibrillation is widely accepted to correlate closely with<br />
survival and recovery of neurological function after cardiac arrest due<br />
to ventricular fibrillation or ventricular tachycardia. Focused training of<br />
a cadre of nurses to defibrillate on their own initiative may significantly<br />
decrease time to first defibrillation in cases of in-hospital cardiac arrest<br />
outside of critical care units. Such a program may be the best single<br />
strategy to improve in-hospital survival, simply and at reasonable cost.<br />
Introduction<br />
Survival from in-hospital cardiac arrest has not improved over the halfcentury<br />
since the advent of basic cardiopulmonary resuscitation (CPR)<br />
and defibrillation [1,2]. Survival rates remain about 18% at best, and<br />
survival is lower on general units than in critical-care areas [3].<br />
Explanations for this lack of progress often invoke co-morbidity, [2]<br />
and proposals for change have frequently focused on preventing<br />
presumably futile resuscitation attempts by means of do-not-resuscitate<br />
orders [4]. Medical emergency teams have increasingly been<br />
implemented to respond to early signs of deterioration and prevent<br />
progression to cardiac arrest [5]. But tachyarrythmic arrests (ventricular<br />
fibrillation (VF) and ventricular tachycardia (VT)) are typically sudden,<br />
and this subset of arrests comprises the cases with a real chance of<br />
survival--if defibrillation is accomplished quickly. The most important<br />
change in out-of-hospital resuscitation over the past quarter-century has<br />
been the renewed focus on early defibrillation by first responders, and<br />
the best approach to improving in-hospital survival may be simply to<br />
bring effective early defibrillation into the hospital [6].<br />
Organizing and delivering the full range of advanced cardiovascular life<br />
support (ACLS) treatments with code teams is an expensive, complex,<br />
and daunting undertaking [7] that has little relation to outcomes--<br />
because survival for presenting rhythms other than VF and VT is dismal,<br />
both outside and inside the hospital. A program focused on saving lives<br />
would look much different: it would devote resources to treatments with<br />
proven effectiveness (primarily early defibrillation), up to the point of<br />
clearly diminishing returns. To improve survival from in-hospital arrests,<br />
a more effective approach to in-hospital defibrillation is needed.<br />
Discussion<br />
A defibrillator originally was a large and cumbersome device which had<br />
to be moved from the critical care unit to arrests in other areas of the<br />
hospital. Trained emergency personnel were usually at the scene of<br />
an arrest by the time the defibrillator arrived. During the 1970s and<br />
1980s there was a trend toward greater numbers of more portable<br />
defibrillators in hospitals, and a defibrillator on every nursing unit is<br />
now the norm. But training did not keep pace with availability: In the<br />
mid-1980s this author brought the problem of delayed in-hospital<br />
defibrillation to the attention of several people active in the American<br />
Heart Association’s (AHA) Emergency Cardiac Care programs, and in<br />
1992 published a description of a nurse-defibrillation training program<br />
using manual defibrillators [8]. Later, those AHA-affiliated authors<br />
began addressing the issue but linked nurse defibrillation closely with<br />
the purchase and use of automated external defibrillators (AEDs)<br />
[9]. The American Heart Association/International Liaison Committee<br />
on Resuscitation’s stance continues to be that AEDs are the key to<br />
achieving early defibrillation in hospitals [10].<br />
The AHA’s promotion of AEDs for in-hospital use is not well supported<br />
by present evidence [11]. A large recent study from Detroit, the best to<br />
date, showed no improvement in time to defibrillation or survival after<br />
hospital-wide introduction of AED-capable defibrillators, at a cost of<br />
$2 million [12]. In addition, serious concerns have been raised about<br />
AED technology in the past few years, centering on the requirement<br />
for a “hands-off” period for rhythm analysis that has been shown to<br />
decrease survival [6].<br />
Inaccurate time data presents another impediment to implementation<br />
of nurse-defibrillation programs because the true extent of the<br />
delayed-defibrillation problem is obscured. Studies based on data<br />
from the National Registry of Cardiopulmonary Resuscitation (NRCPR)<br />
report median times of 0 minutes [1]. These time intervals, based<br />
on handwritten code records, are unrealistically short [13]. NRCPR<br />
researchers have recognized this, [14] but inaccurate time data<br />
continue to be reported with little or no reservation [15]--though the<br />
problem could be solved fairly simply [16].<br />
Several factors, then-limitations of AED technology, unrealistically short<br />
time-interval data, and of course cost [13]--serve to impede hospitals<br />
in addressing the problem of delayed defibrillation. A recent article<br />
provided some counterbalance to these factors: the investigators<br />
reported that delayed in-hospital defibrillation was a relatively frequent<br />
problem and that it lowered survival, although again the extent of<br />
the problem was obscured by use of NRCPR data [17]. (A main<br />
recommendation in the accompanying editorial was to buy more AEDs<br />
[18].)<br />
In recent years, there has been much interest in the 3-phase model of<br />
VF arrest proposed by Weisfeldt and Becker, which posits that after<br />
about 4 minutes treatment may be improved by a period of basic CPR<br />
SIMULATION TODAY - AUTUMN <strong>2019</strong><br />
Correspondence: jastewart325@gmail.com<br />
17
FEATURE<br />
before defibrillation [19]. The model has no relevance for in-hospital<br />
defibrillation because 1) the goal should be to defibrillate in less<br />
than 4 minutes (the AHA has established a benchmark of less than 3<br />
minutes for all in-hospital arrests [20]), and 2) with multiple rescuers<br />
typically available, all hospital protocols call for basic CPR while the<br />
defibrillator is being brought to the scene. Therefore, defibrillation<br />
at the earliest possible moment remains the best approach for inhospital<br />
tachyarrythmic arrests.<br />
Doing anything in the first moments of a code is emotionally<br />
difficult, but defibrillation is no more difficult than other tasks<br />
nurses are expected to perform in codes; certainly it is easier than<br />
performing effective basic CPR. The main rationale for AED use--<br />
the presumed need for advanced rhythm identification skills with<br />
manual defibrillators--is without foundation: the basic distinction,<br />
between an organized monitor rhythm and a chaotic pattern, is easily<br />
learned [21]. Another barrier to rapid defibrillation is the presumed<br />
danger to caregivers in administering a shock. However, dangers<br />
of defibrillation have long been overstated (no documented deaths<br />
or serious injuries in over 50 years) and safety has been further<br />
improved by the use of hands-free pads [22]. The basic procedure of<br />
defibrillation, whether with manual defibrillators or AEDs, is both easy<br />
and safe.<br />
In-hospital defibrillation training programs will have the capability to<br />
conduct unannounced drills for practice and performance testing.<br />
Many hospitals use “mock codes” to practice all aspects of code<br />
response; these are fairly complex productions involving a good<br />
deal of planning and disruption of daily work routines. Drills for<br />
defibrillation training can be conducted much more simply--one<br />
learner at a time--and preserve the element of unexpectedness<br />
that is a critical condition of performance. Such drills should prove<br />
valuable, both as a stimulus for learning and as an evaluation<br />
tool. Each learner could be required to perform competently in a<br />
surprise simulation 2 to 4 weeks after training, thereby providing<br />
a more valid test, and the participants’ general foreknowledge of<br />
the surprise testing should reinforce the training by encouraging<br />
continued mental rehearsal.<br />
The procedural skill of defibrillation can be taught primarily by<br />
repeated physical simulation, but the training program should also<br />
include a didactic component. This component will emphasize the<br />
extreme time-dependence of defibrillation and will aim to counter<br />
misconceptions about defibrillation, particularly regarding safety<br />
issues for caregivers and patients [23]. This component can likely<br />
be mastered through self-study, with a text or computer-based<br />
tutorial.<br />
SIMULATION TODAY - AUTUMN <strong>2019</strong><br />
The real problem comes not from the inherent difficulty of the task,<br />
but from the conditions of performance. Defibrillation is necessarily<br />
performed in a life-threatening situation, without warning and under<br />
intense time pressure [23]. Such stressors, in combination with the<br />
rarity of the event for a particular caregiver, can cause a significant<br />
decrease in skill. Demonstrating mastery in a single simulation in a<br />
classroom setting is not sufficient to ensure adequate retention and<br />
competent performance in an actual code. Clinical competence in<br />
defibrillation calls for overtraining: requiring practice well beyond<br />
the first competent performance by repeated performance in<br />
simulations and to a higher standard than may be required in an<br />
actual code. This is analogous to aspects of military training (e.g.,<br />
disassembling and reassembling a rifle while blindfolded). Two- to<br />
three-hour sessions with four to five trainees in each session should<br />
be sufficient for this component of the training.<br />
Affective aspects of defibrillation training also make it advisable<br />
to select a group of highly motivated learners. Participants in an<br />
in-hospital defibrillation program will be committing themselves to<br />
training intensively and maintaining competence for long periods of<br />
time without actually using the skill--but when called upon they will<br />
be expected to perform quickly and competently under very stressful<br />
conditions [23]. This level of personal commitment should not--and<br />
indeed, cannot--be expected of all nurses. But it is unnecessary to<br />
train all nurses in a facility, and indeed it is inadvisable to do so: a<br />
select group of nurses can be trained that their first responsibility<br />
in a code is to initiate monitoring and defibrillation while other<br />
staff do CPR, thus avoiding the role confusion that is known to<br />
be a significant problem with code team performance [24]. It may<br />
be possible to rely mainly on volunteers, thereby increasing the<br />
probability that training will succeed. The inherent emotional appeal<br />
of defibrillation--the very real prospect of restoring a patient’s life<br />
quickly, cleanly, and dramatically--can act as an inducement for<br />
volunteers as well as a powerful source of motivation during training.<br />
A study of the training program’s effectiveness should be preceded<br />
by a period for gathering baseline data on times to first monitoring<br />
and first defibrillation, [16] in order to gauge any Hawthorne<br />
effect in the subsequent study. A prospective, controlled study<br />
can be conducted by recruiting trainees to achieve randomization<br />
across shifts and units, so that any given unit will be staffed with<br />
a trained nurse approximately half of the time. If mean times to<br />
defibrillation are shortened in the experimental group (arrests with<br />
a defibrillation-trained nurse on the unit), survival can be tracked<br />
in a longer and/or larger study. The proportion of successful<br />
defibrillations should increase, and the number of shockable<br />
rhythms should also increase due to earlier monitoring--before<br />
deterioration to asystole [25].<br />
If the program proves effective, hospital-wide implementation can<br />
be accomplished by training perhaps one-fourth to one-third of<br />
nurses. Full coverage can be ensured with a backup system if the<br />
hospital pages codes overhead or if all defibrillation-trained nurses<br />
carry code pagers, thus allowing them to respond to code calls on<br />
adjoining units (and leave if coverage is already in place). Likewise,<br />
defibrillation-trained nurses can be instructed to return to their<br />
routine duties after the code team arrives.<br />
Conclusions<br />
The link between early defibrillation and survival is beyond<br />
dispute. A program focused on early defibrillation by nurses can<br />
be relatively easy to implement and cost-effective, and holds the<br />
promise of saving many lives.<br />
Competing interests<br />
The author declares that he has no competing interests.<br />
18
FEATURE<br />
References<br />
resuscitation. Resuscitation. 2005;65:285–290. doi: 10.1016/j.<br />
resuscitation.2004.12.020.<br />
1. Peberdy MA, Kaye W, Ornato JP. for the NRCPR Investigators.<br />
Cardiopulmonary resuscitation of adults in the hospital: A<br />
report of 14720 cardiac arrests from the National Registry of<br />
Cardiopulmonary Resuscitation. Resuscitation. 2003;58:297–308.<br />
doi: 10.1016/S0300-9572(03)00215-6.<br />
2. Ehlenbach WJ, Barnato AE, Curtis JR. Epidemiologic study of inhospital<br />
cardiopulmonary resuscitation in the elderly. N Engl J Med.<br />
2009;361(1):22–31. doi: 10.1056/NEJMoa0810245.<br />
3. Andréasson AC, Herlitz J, Bång A. Characteristics and<br />
outcome among patients with a suspected in-hospital cardiac<br />
arrest. Resuscitation. 1998;39(1):23–31. doi: 10.1016/S0300-<br />
9572(98)00120-8.<br />
4. Burns JP, Edwards J, Johnson J. Do-not-resuscitate order after<br />
25 years. Crit Care Med. 2003;31:1543–1550. doi: 10.1097/01.<br />
CCM.0000064743.44696.49.<br />
5. Hillman K, Parr M, Flabouris A, Bishop G, Stewart A. Redefining<br />
in-hospital resuscitation: The concept of the medical emergency<br />
team. Resuscitation. 2001;48(2):105–110. doi: 10.1016/S0300-<br />
9572(00)00334-8.<br />
6. American Heart Association. 2005 American Heart Association<br />
Guidelines for Cardiopulmonary Resuscitation and Emergency<br />
Cardiovascular Care. Part 7.2: Management of cardiac<br />
arrest. Circulation. 2005;112:IV-58–IV-66. doi: 10.1161/<br />
CIRCULATIONAHA.105.166557.<br />
7. Lee KH, Angus DC, Abramson NS. Cardiopulmonary resuscitation:<br />
What cost to cheat death? Crit Care Med. 1996;24:2046–2052. doi:<br />
10.1097/00003246-199612000-00019.<br />
8. Stewart JA. Defibrillation training for general unit nurses. J Emerg<br />
Nurs. 1992;18:519–524.<br />
9. American Heart Association. Textbook of Advanced Cardiac Life<br />
Support. 2. Dallas: American Heart Association; 1994.<br />
10. American Heart Association. 2005 American Heart Association<br />
Guidelines for Cardiopulmonary Resuscitation and Emergency<br />
Cardiovascular Care. Part 5: Electrical Therapies: Automated<br />
External Defibrillators, Defibrillation, Cardioversion, and<br />
Pacing. Circulation. 2005;112:IV-35–IV-46. doi: 10.1161/<br />
CIRCULATIONAHA.105.166554.<br />
11. Kenward G, Castle N, Hodgetts TJ. Should ward nurses be using<br />
automatic external defibrillators as first responders to improve the<br />
outcome from cardiac arrest? A systematic review of the primary<br />
research. Resuscitation. 2002;52:31–37. doi: 10.1016/S0300-<br />
9572(01)00438-5.<br />
12. Forcina MS, Farhat AY, MD O’Neill WW. Cardiac arrest survival after<br />
implementation of automated external defibrillator technology in the<br />
in-hospital setting. Crit Care Med. 2009;37:1229–1236. doi: 10.1097/<br />
CCM.0b013e3181960ff3.<br />
13. Kobayashi L, Lindquist DG, Jenouri IM. Comparison of sudden<br />
cardiac arrest resuscitation performance data obtained from<br />
in-hospital incident chart review and in situ high-fidelity medical<br />
simulation. Resuscitation. 2010;81:463–71. doi: 10.1016/j.<br />
resuscitation.2010.01.003.<br />
14. Kaye W, Mancini ME, Lane-Truitt T. When minutes count--<br />
the fallacy of accurate time documentation during in-hospital<br />
15. Chan PS, Nichol G, Krumhotz HM. Hospital variation in time to<br />
defibrillation after in-hospital cardiac arrest. Arch Intern Med.<br />
2009;169:1265–73. doi: 10.1001/archinternmed.2009.196.<br />
16. Stewart JA. Determining accurate call-to-shock times is<br />
easy. Resuscitation. 2005;67(1):150–151. doi: 10.1016/j.<br />
resuscitation.2005.05.007.<br />
17. Chan PS, Krumholz HM, Nichol G. Delayed time to defibrillation after<br />
in-hospital cardiac arrest. N Engl J Med. 2008;358(1):9–17. doi:<br />
10.1056/NEJMoa0706467.<br />
18. Saxon LA. Survival after tachyarrhythmic arrest -- what are we<br />
waiting for? NEJM. 2008;358:77–79. doi: 10.1056/NEJMe0707823.<br />
19. Weisfeldt ML, Becker LB. Resuscitation after cardiac arrest: a<br />
3-phase time-sensitive model. JAMA. 2002;288:3035–8. doi:<br />
10.1001/jama.288.23.3035.<br />
20. NRCPR Science Advisory Board. Delayed time to defibrillation after<br />
in-hospital cardiac arrest. 2008. http://www.nrcpr.org/pdf/Time_to_<br />
Defibrillation.pdf<br />
21. Stewart AJ, Martin DL. Knowledge and attitude of nurses on medical<br />
wards to defibrillation. J Royal Coll Phys Lond. 1994;28:399–404.<br />
22. Lloyd MS, Heeke B, Walter PF, Langberg JJ. Hands-on<br />
defibrillation: an analysis of electrical current flow through<br />
rescuers in direct contact with patients during biphasic external<br />
defibrillation. Circulation. 2008;117:2510–2514. doi: 10.1161/<br />
CIRCULATIONAHA.107.763011.<br />
23. Mäkinen M, Niemi-Murola L, Kaila M, Castrén M. Nurses’ attitudes<br />
towards resuscitation and national resuscitation guidelines--Nurses<br />
hesitate to start CPR-D. Resuscitation. 2009;80:1399–1404. doi:<br />
10.1016/j.resuscitation.2009.08.025.<br />
24. Marsch SCU, Tschan F, Semmer N. Performance of first responders<br />
in simulated cardiac arrests. Crit Care Med. 2005;33:963–967. doi:<br />
10.1097/01.CCM.0000157750.43459.07.<br />
25. Weil MH. Rhythms and outcomes of cardiac arrest. Crit Care Med.<br />
2010;38:310. doi: 10.1097/CCM.0b013e3181b7825c.<br />
SIMULATION TODAY - AUTUMN <strong>2019</strong><br />
19
ADVERTORIAL FEATURE<br />
STANDARDIZED TRAINING OF PATIENT<br />
COMMUNICATION TECHNIQUES WITH<br />
ADVANCED SIMULATION TECHNOLOGY<br />
Balazs Moldovanyi, M.Sc. Computer Engineering, MBA; Ádám Helybély, M.Sc. Computer Engineering,<br />
MBA; Hugo Azevedo, BSc, Applied Mathematics, MS, Biomedical Engineering; Michelle Castleberry, BSc,<br />
Professional Communication<br />
The Patient Communication Simulator<br />
Summary Statement: As Healthcare <strong>Simulation</strong>ists we constantly<br />
ask ourselves, where do we start improving our training for the nurses,<br />
physicians, and allied healthcare professionals of 2050 through<br />
healthcare simulation today? Patient simulators needs both an ongoing<br />
evolution along the traditional dimensions or realism, dependability<br />
and affordability as well as a revolution to broaden the potential of<br />
simulation. Integrating Artificial Intelligence (AI) driven communication<br />
technologies into simulators for training healthcare professionals of the<br />
future will be revolutionary.<br />
A Patient Communication Simulator is a device that integrates<br />
verbal communication functionality into a traditional full-body patient<br />
simulator by merging physiology simulation and communication training<br />
modalities into a single scenario-driven instructor controlled experience.<br />
In this article, we are evaluating the first commercially available Patient<br />
Communication Simulator (PCS) and its future potential.<br />
Key Words: Communication, Speech Recognition, AI, Science Fiction<br />
How will the nurses, physicians, and allied healthcare professionals<br />
of 2050 differ from their peers fifty years earlier? Future healthcare<br />
professionals of 2050 will be making enhanced decisions. Enhanced<br />
decisions through collaborative consultation; think: increased<br />
telemedicine. Enhanced decisions with information at their fingertips;<br />
think: wearable computing. Enhanced Decisions supported by<br />
technology; think: AI & machine learning. Correspondingly, future<br />
healthcare professionals of 2050 will have escalated the human<br />
element, which will be proportionally more important for care of the<br />
future patient and success of future health care teams; thus, furthering<br />
efforts towards achieving the balance of ‘Art and Science of Medicine’.<br />
<strong>Simulation</strong> can be qualitatively better as a tool, by not only training<br />
to make triage decisions, but simultaneously allowing learners to<br />
understand the fundamentals in human-interactions. Training must<br />
improve for a stronger connection to the patient. <strong>Simulation</strong> must be<br />
more relatable. The time to start moving in that direction is now.<br />
Building on today’s needs with more advanced technology, The Patient<br />
Communication Simulator (PCS) is the first of its kind, infused with<br />
features and functions that a mere decade ago sounded like sciencefiction.<br />
ALEX is a revolutionary new product that integrates AV enhanced<br />
communication into a general purpose, full-body patient simulator, with<br />
the objective of aiding in the training of non-technical skills.<br />
SIMULATION TODAY - AUTUMN <strong>2019</strong><br />
<strong>Today</strong>, a significant portion of simulation-based training is for a<br />
healthcare system specializing in acute, curative, episodic issues.<br />
Learners are trained to make emergency, high pressure decisions in<br />
the fraction of a second. This skill will remain critical in healthcare; but<br />
the call to action is clear, it’s time to do more and do better than just a<br />
quantitative reformation.<br />
Patient simulators have been proven to be efficient and low-risk tools<br />
for several elements of the training of healthcare professionals, from<br />
procedural skill development to team communication.<br />
Simultaneously, trained standardized patients have introduced similar<br />
standardization and consistency in simulated patient-professional<br />
encounters, focusing on communication and physical interactions.<br />
The next generation of patient simulators are devices that can merge<br />
the benefits of these distinctly different approaches into a seamlessly<br />
integrated experience, further enhancing the realism of the simulation<br />
hence better facilitating its ultimate educational goals.<br />
Using pre-programmed scenarios to drive not only the physiological<br />
data but also the spoken responses and reactions of the patient, a<br />
previously unattainable level of learning and standardization, is possible<br />
across a larger number of dimensions of the simulation experience.<br />
Is this the revolution and evolution we’ve been waiting for? Does this<br />
balance art and science of medicine? Yes, it is the natural progression<br />
in technology to help train healthcare professionals for the future.<br />
simulaids.eu.com/alex | simulaids.eu.com/vera | http://blog.pcs.ai<br />
ALEX fuses today’s most impactful<br />
emerging technologies into a truly<br />
remarkable new teaching tool, opening<br />
an exciting new chapter in patient<br />
simulation. ALEX is a cloud connected<br />
patient simulator with an eye camera,<br />
and Speech Recognition capabilities.<br />
20
COMPANY NEWS<br />
CAE<br />
CAE Healthcare Introduces the CAE Luna<br />
infant patient simulator<br />
In <strong>2019</strong> CAE Healthcare officially released CAE<br />
Luna, an innovative infant simulator designed<br />
to fulfill clinical training requirements for<br />
neonatal and infant care for health conditions<br />
requiring expedient, life-saving team actions.<br />
CAE Luna can be configured for essential<br />
infant nursing skills or for more advanced<br />
international Pediatric Advanced Life<br />
Support (PALS) and Neonatal Resuscitation<br />
Program (NRP) and S.T.A.B.L.E. Program<br />
training requirements. The simulator<br />
includes Simulated Clinical Experiences<br />
(SCEs) for easy integration of simulationbased<br />
curriculum into clinical education for<br />
infant care.<br />
Discover true innovation in simulation with<br />
CAE Luna at https://caehealthcare.com/<br />
patient-simulation/luna/<br />
CAE Luna is the first completely wireless and<br />
tetherless baby simulator manufactured by<br />
CAE Healthcare. An advanced patient simulator<br />
offering physiological modeling that responds to<br />
clinical interventions just as an actual newborn<br />
child would, CAE Luna realistically represents a<br />
neonate from birth to 28 days after delivery.<br />
CAE Luna can be operated in hospitals or<br />
educational settings with a laptop, and without<br />
power cords or cables. The IV ports, peripheral<br />
arterial catheter site and umbilical cord allow<br />
professional caregivers to safely practice<br />
administering medications and fluids, while the<br />
advanced airway and tracheostomy site allows<br />
for repeated practice of delicate procedures<br />
without risk.<br />
WHY NOT WRITE FOR US?<br />
<strong>Simulation</strong> <strong>Today</strong> welcomes the submission of clinical<br />
papers, case reports and articles that you<br />
feel will be of interest to your colleagues.<br />
The publication is mailed to all resuscitation, A&E and anaesthetic departments<br />
plus all intensive care, critical care, coronary care and cardiology units plus<br />
Universities and Schools of Midwifery that teach <strong>Simulation</strong>.<br />
All submissions should be forwarded to info@mediapublishingcompany.com<br />
If you have any queries please contact the publisher Terry Gardner via:<br />
info@mediapublishingcompany.com<br />
SIMULATION TODAY - AUTUMN <strong>2019</strong><br />
21