You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
Volume 35 No. 5<br />
<strong>October</strong> <strong>2020</strong><br />
DEDICATED TO THE AMBULANCE SERVICE AND ITS SUPPLIERS<br />
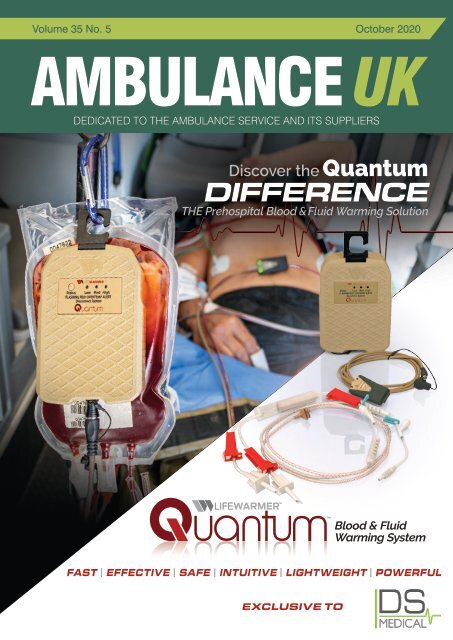
Discover the Quantum<br />
DIFFERENCE<br />
THE Prehospital Blood & Fluid Warming Solution<br />
<br />
<br />
Blood & Fluid<br />
Warming System<br />
FAST | EFFECTIVE | SAFE | INTUITIVE | LIGHTWEIGHT | POWERFUL<br />
EXCLUSIVE TO
THE NEXT GENERATION OF CORPULS3<br />
4G modem, WLAN,<br />
LAN port<br />
Intuitive operating<br />
concept with JogDial<br />
Large, transflective<br />
8.4” colour display,<br />
optional with<br />
touchscreen<br />
Softkeys and<br />
function buttons (in<br />
addition to touchscreen)<br />
Combined<br />
operational<br />
weight under<br />
9kg<br />
Shock Protection<br />
THE FUTURE AT YOUR FINGERTIPS<br />
Monitoring Unit<br />
Patient Box<br />
Defibrillator/Pacer<br />
The newest and most dynamic of the corpuls generation is the brand new<br />
C3T. This unique design is the very first pre hospital touch screen modular<br />
defib / monitor unit to be introduced to the emergency services market.<br />
Our engineers have worked hard to combine the exceptional features of the<br />
already established corpuls3, and the new requirements/demands from the<br />
emergency services, creating the latest generation of defib / monitor unit, C3T.<br />
www.theortusgroup.com T: +44 (0)845 459 4706
CONTENTS<br />
CONTENTS<br />
<strong>Ambulance</strong> <strong>UK</strong><br />
141 EDITOR’S COMMENT<br />
142 FEATURES<br />
142 Clinical Skills for Police Officers in Specialist Role:<br />
An Audit of Patient Report Forms in 2019<br />
146 Why a simple blood test could identify those most<br />
at risk of Covid-19 complications<br />
148 NEWSLINE<br />
166 COMPANY NEWS<br />
This issue edited by:<br />
Sam English<br />
c/o Media Publishing Company<br />
48 High Street<br />
SWANLEY BR8 8BQ<br />
ADVERTISING:<br />
Terry Gardner, Samantha Marsh<br />
CIRCULATION:<br />
Media Publishing Company<br />
Media House, 48 High Street<br />
SWANLEY, Kent, BR8 8BQ<br />
Tel: 01322 660434 Fax: 01322 666539<br />
E: info@mediapublishingcompany.com<br />
www.ambulanceukonline.com<br />
COVER STORY<br />
The Quantum Solution<br />
The Quantum from Lifewarmer is the most technologically advanced blood and fluid<br />
warming device to enter the <strong>UK</strong> market.<br />
PUBLISHED BI-MONTHLY:<br />
February, April, June, August,<br />
<strong>October</strong>, December<br />
COPYRIGHT:<br />
Media Publishing Company<br />
Media House<br />
48 High Street<br />
SWANLEY, Kent, BR8 8BQ<br />
DS Medical are honoured to have been appointed sole distributor for the <strong>UK</strong> and Ireland<br />
market.<br />
The device exceeds all healthcare and logistical requirements for the delivery of warmed<br />
blood or fluids across the defined spectrum of care.<br />
The system consists of unique thermal administration sets that incorporate sensing<br />
elements with an integrated heating system that does not disrupt the fluid path. With<br />
advanced intelligence throughout the system, the lightweight Controller modulates and<br />
moderates the energy flow to the integrated heating elements to ensure consistent<br />
normothermic fluid delivery to the casualty.<br />
The battery is the smallest in category, able to rapidly adjust power distribution based<br />
on the temperature and flow rate of the input fluid. This creates a highly efficient system<br />
capable of previously unrealized performance optimizations.<br />
The Quantum system has an operational weight of just 624 grams yet can deliver one<br />
litre of 4°C Whole Blood (WB) at 100mL/min with an output temperature of 38°C+/- 2°C<br />
with only a 24 second warm-up period.<br />
The Quantum Blood and Fluid Warmer provides the Health Care Professional with<br />
significant technological advantage in the fight to eliminate preventable death.<br />
DS Medical would welcome the opportunity to discuss Quantum in greater detail.<br />
PUBLISHERS STATEMENT:<br />
The views and opinions expressed in<br />
this issue are not necessarily those of<br />
the Publisher, the Editors or Media<br />
Publishing Company.<br />
Next Issue December <strong>2020</strong><br />
Subscription Information – <strong>October</strong> <strong>2020</strong><br />
<strong>Ambulance</strong> <strong>UK</strong> is available through<br />
a personal, company or institutional<br />
subscription in both the <strong>UK</strong> and overseas.<br />
<strong>UK</strong>:<br />
Individuals - £24.00 (inc postage)<br />
Companies - £60.00 (inc postage)<br />
Rest of the World:<br />
£60.00 (inc. surface postage)<br />
£84.00 (airmail)<br />
We are also able to process your<br />
subscriptions via most major credit<br />
cards. Please ask for details.<br />
Cheques should be made<br />
payable to MEDIA PUBLISHING.<br />
Designed in the <strong>UK</strong> by me&you creative<br />
AMBULANCE <strong>UK</strong> - OCTOBER<br />
Do you have anything you would like to add or include? Please contact us and let us know.<br />
139
Basic<br />
<strong>Ambulance</strong> and Emergency Blood Testing<br />
Lactate, Hemoglobin, Hematocrit, Glucose, and Ketone<br />
for early patient assessment and treatment<br />
Fingerstick capillary sample, no blood draws<br />
Results as fast as 6 seconds with laboratory-quality results<br />
Rapid detection of sepsis, hypo- and hyperglycemia, and DKA<br />
Evaluation of trauma, hemorrhage, acute coronary syndrome<br />
novabiomedical.com<br />
Scan to learn more or<br />
visit https://www2.novabio.us/ukemsbasic
EDITOR’S COMMENT<br />
EDITOR’S COMMENT<br />
Welcome to this issue of A<strong>UK</strong><br />
So here we are in <strong>October</strong> still haunted by the ghost of Christmas future, the other big ‘C’, and reeling from a<br />
summer not of whoa but woe. I don’t know about anyone else but sometimes I find writing somewhat cathartic<br />
so sitting here writing this I thought I might reflect on the year thus far in the fond hope I can find something<br />
positive.<br />
“Surprise,<br />
surprise,<br />
numbers<br />
began to<br />
increase and<br />
the strategy<br />
seemed<br />
obvious.<br />
A little like<br />
watching<br />
numbers<br />
fly up the<br />
tube in the<br />
National<br />
Lottery,<br />
area by area<br />
‘hot spots’<br />
were closed<br />
down.”<br />
Let’s begin with last Christmas when everyone I knew had a weird flu-like illness, my GP friend told me it had<br />
even surprised him in its “different to the normal”presentation, lo and behold, enter stage left a brand new<br />
coronavirus. Now I’m not really into politics but come mid February it was, I think, obvious to everyone that<br />
things were not looking good. My parents boarded themselves into the house and haven’t been out since, Then<br />
mid March the politicians started listening to “science” and convinced the nation to close its doors…that worked!<br />
…I can remember working in my day job on the last weekend in March when our demand hit 100% increase on<br />
normal and thinking well this is going to need some creative thinking, this just isn’t working the way they said it<br />
would. I’ve found a positive ! The weather over Spring made working from home a distinct pleasure but then I’m<br />
lucky to work for the health service, thousands of others lost their jobs, their lives and their sanity so really not a<br />
positive, just a sobering reminder that sometimes the cure creates more issues than the disease.<br />
Everyone looks forward to Summer, so as restrictions eased and bars re-opened, I think most people breathed<br />
a sigh of relief. Surprise, surprise, numbers began to increase and the strategy seemed obvious. A little like<br />
watching numbers fly up the tube in the National Lottery, area by area ‘hot spots’ were closed down. I’m<br />
cynical, with a third of the country now ‘closed’ again, I’m not convinced that was successful, however, putting<br />
the cynicism to the side let’s consider my favourite intervention, the mask! So now everyone has a little piece<br />
of cloth that comes in and out of their pocket every two minutes, can be worn under the nose or chin, can be<br />
hung on the car mirror so it isn’t forgotten next time at the shops and protects others even though the rules<br />
that probably did protect people, hand washing and distance are pretty much obsolete because of the power<br />
of the mask and the psychological confidence it brings. Worse still, the fomitic things are all over the place, I’m<br />
just waiting for a dolphin to end up with one wrapped round its snout.<br />
Time for the second wave. What on earth did they think would happen when the kids got back to school.<br />
History perhaps might have given them a clue, since kids are the flu season super spreaders every single<br />
year. I’m not sure how many students there are in the <strong>UK</strong> but again not entirely surprising when you send<br />
them all over the country for the first time with a full grant and no parental oversight that within a fortnight every<br />
university had hundreds of new cases…now wasn’t that a surprise!<br />
And here we are, you just know its bad when the supermarkets are putting Easter eggs on their shelves, no<br />
family Christmas this year, although I suppose technically if you cremate the Turkey like my wife does each<br />
year you could get a few people round for its funeral.<br />
Did I say this was a cathartic exercise, it isn’t really, it just makes me sad to think of the people who have lost a<br />
year of their lives, the kids who should be enjoying life, the families who had their lives ruined, the people who<br />
have died not only of the disease but of fear to have that ‘lump’, that ‘weakness’, that ‘chest pain’ investigated.<br />
Those who have had operations cancelled, those that cannot see their grandchildren or grandparents. The<br />
vulnerable who might as well have been imprisoned for perhaps one of their last remaining years. And finally,<br />
let’s not forget the perhaps irreparable damage to the <strong>UK</strong> economy, the unemployment, the lost businesses<br />
and the debt that will probably have to be repaid for the next century, the next budget will be interesting. Will<br />
we look back when this is all over, if it ever is, they’ve never cured another coronavirus, the common cold, and<br />
say “I’m not sure our scientific decisions were that great.”<br />
Stay safe, stay distance, stay hygienic and of course, don’t leave the house without your shield of invincibility…<br />
Sam English, Co-Editor <strong>Ambulance</strong> <strong>UK</strong><br />
AMBULANCE <strong>UK</strong> - OCTOBER<br />
For the latest <strong>Ambulance</strong> Service News visit: www.ambulancenewsdesk.com<br />
141
FEATURE<br />
CLINICAL SKILLS FOR POLICE OFFICERS IN<br />
SPECIALIST ROLE: AN AUDIT OF PATIENT<br />
REPORT FORMS IN 2019<br />
Abstract<br />
officers in specialist roles (referred to as officers in this report) are<br />
particularly proficient. It also evaluates components of the form itself.<br />
AMBULANCE <strong>UK</strong> - OCTOBER<br />
Some specialist police officers, predominantly from firearms units, are<br />
trained in pre-hospital medicine to a national standard curriculum initially<br />
developed in 2009. The incidents are recorded in Patient Report Forms,<br />
which are subsequently reviewed by their clinical governance oversight<br />
to quality assure the treatment given and to inform future training or<br />
curriculum development. This is a retrospective review of 298 Patient<br />
Report Forms from 2019 from five police forces covering a mixture<br />
of metropolitan and semi-rural areas. Patients were predominantly<br />
male and the mechanisms of injury were mainly stabbings, road traffic<br />
collisions or alcohol/ drug-related. There were 42 (14%) medical callouts<br />
which were mostly cardiac in nature. Other non-trauma incidents<br />
included mental health problems. The most frequent injuries sustained<br />
by patients were lacerations, stab wounds and abrasions and 116 (31%)<br />
patients were reported as being in pain. 55 (18%) patients required<br />
airway support. Cardiopulmonary resuscitation (CPR) was required in<br />
40 (13%) patients with a Return of Spontaneous Circulation (ROSC)<br />
on scene achieved in 17 patients (43%). More focus on medical<br />
emergencies and mental health in training could be valuable. Airway<br />
management has improved compared to previous audits and there<br />
is potential for supraglottic airways to be used more frequently. The<br />
relatively high numbers of ROSC on scene is commendable. These<br />
officers are well-trained and serial audits show a steady increase in use<br />
of skills, which makes them an important medical resource, although it<br />
is important to remember that they are police officers first.<br />
Introduction<br />
The year 2019 saw a 7% increase in knife & sharp object offences in<br />
England and Wales 1 ; the highest on record (however, this figure does not<br />
include statistics from Greater Manchester). There were 6060 incidents<br />
involving firearms and a terrorist attack on London Bridge 1 . It is, therefore,<br />
more important than ever for the police officers responding to such<br />
incidents to have a high degree of medical capability. In 2010, firearms<br />
police officers began training to a national curriculum in basic but essential<br />
life-saving skills. ‘Clinical Skills for Police Officers in Specialist Role’ is a<br />
module (previously named D-13), which involves the assessment and<br />
treatment of casualties using the ABCDE paradigm 2 .<br />
Patient Report Forms (PFRs) record details of the care provided each<br />
time an officer is called to a patient. They are reviewed by a registered<br />
medical professional for assurance of the treatment given and are<br />
used to inform future training for the continual quality improvement of<br />
medical care. This audit aims to examine the PRFs completed in 2019<br />
and compare the data to previous years using earlier audits. It will look<br />
for emerging trends, identify areas for improvement and where police<br />
Method<br />
This is a retrospective audit of 298 PRFs completed by predominantly<br />
police firearms officers in 2019. The PRFs are from five police forces<br />
in England, all under the same clinical governance structure 3 , covering<br />
a mixture of urban and semi-rural areas. Anonymised data was<br />
categorised into the mechanisms of injury, types of injuries, sex of the<br />
patient, observations recorded and interventions provided by officers.<br />
Results<br />
There were 217 male patients, accounting for 73% of PRFs. There were<br />
51 firearms deployments, making up 18% of PRFs. 16 PRFs did not<br />
record whether the incident was a firearms operation or not. Officers<br />
spent an average of 51 minutes on scene.<br />
Mechanism of Injury<br />
The three most common mechanisms of injury were stabbing, alcohol/<br />
drug-related, or road traffic collisions (RTCs) (Figure 1). While there were<br />
11 incidents (4% of PRFs) where the mechanism of injury was alcohol<br />
or drugs alone, 66 incidents (22% of all call-outs) involved drugs or<br />
alcohol, including 13 self-harm/ parasuicides (59%) and 13 stabbings<br />
(19%). The ‘other’ category included three patients with hypothermia,<br />
Number of Patients<br />
70<br />
60<br />
50<br />
40<br />
30<br />
20<br />
10<br />
0<br />
Mechanism of Injury<br />
Alcohol/ drug-related<br />
Not alcohol/ drug-related<br />
Figure 1: Number of most commonly reported mechanisms of injury,<br />
including the proportion of incidents in each category where alcohol/<br />
drugs were also reported in the PRF.<br />
142<br />
For further recruitment vacancies visit: www.ambulanceukonline.com
FEATURE<br />
Number of Patients<br />
12<br />
11<br />
10<br />
9<br />
8<br />
7<br />
6<br />
5<br />
4<br />
3<br />
2<br />
1<br />
0<br />
Pain<br />
116 patients (39%) suffered from pain. The analgesic Methoxyflurane<br />
(Penthrox) was used in 23 patients (8% of all patients), mainly in<br />
RTC (seven patients) or assault (seven patients). 83% of the patients<br />
(19) were given only one dose. Before administration of Penthrox,<br />
the majority of these patients reported ‘severe pain,’ which is rated<br />
at 8-10/10, and mostly reduced to ‘moderate pain’ (rated at 4-7/10),<br />
although one patient reported no change in pain levels. Two patients<br />
were identified as candidates for Penthrox but refused it or their care<br />
was taken over by paramedics.<br />
Number of Patients<br />
Medical Incidents<br />
Figure 2: The number of patients reported for each medical incident.<br />
Assessment<br />
- Catastrophic haemorrhage:<br />
137 patients (47%) had an external bleed, which was mainly treated with<br />
direct pressure. On one occasion, where a man had a heavily bleeding<br />
head wound after an assault, the application of a pressure bandage<br />
was commended by the Emergency Department. 12% of those who had<br />
an external bleed had a tourniquet applied (16 patients). One man had<br />
three fractures (two wrists and one hip), two completed suicides, two<br />
a catastrophic bleed from a deep laceration on his forearm which was<br />
12minor cuts, two welfare concerns, someone who was pushed through a<br />
treated with a tourniquet on his upper arm, stemming the bleed. The<br />
11<br />
window, one industrial accident, a fall from a horse and a casualty from<br />
10<br />
patient was identified as very unwell as a result of blood loss (confusion,<br />
9a police operation. Six incidents were unspecified.<br />
8<br />
pale complexion) and the two officers were complimented on the<br />
7<br />
application of a tourniquet by the Helimed doctor taking over care.<br />
642 PRFs (14%) were medical call-outs (this excludes mental health). The<br />
5<br />
As the first responders, their quick assessment and decision-making<br />
Amputation<br />
4majority of these incidents involved cardiac arrest or patients with chest<br />
0.9%<br />
markedly improved the outcome for this patient.<br />
3<br />
pain (Figure 2). Mental health problems were noted explicitly in the free-<br />
of 10 PRFs (3%), although the true number of incidents where mental<br />
2<br />
1text<br />
0<br />
Abrasion Burns A - Airway:<br />
health played a part is likely to be much higher, considering 14.8% that the 0.3%<br />
Abrasion<br />
55 patients (18%) had obstructed airways, which were often managed<br />
total number of suicides, para-suicides, missing persons and domestic<br />
Burns<br />
using a combination of manoeuvres (Table 1). Positioning the patient<br />
incidents was 35 (which would Laceration make it involved in 15% of PRFs).<br />
Bruising<br />
31.1%<br />
on their side or turning the patient was commonly used to manage<br />
Bruising<br />
Open Fracture<br />
Medical Incidents<br />
obstruction. All patients with a reported initial AVPU Score (Alert, Verbal,<br />
11.3%<br />
Injuries<br />
Closed Fracture<br />
Pain, Unresponsive Puncture Score) of Pain or Unresponsive (74 patients) were<br />
The most frequently reported injuries were lacerations, stab wounds and Open given airway support where required. 24 (8%) patients had suspected<br />
abrasions (Figure 3). 46 patients (11%) sustained fractures and three Fracture<br />
Stab Wound<br />
2.2% bony GSW injuries Entry to the face, mainly from falls over six feet or from RTCs.<br />
patients had amputations (one hand, one finger and one foot). Closed One Fracture patient<br />
GSW Exit<br />
12.3%<br />
A supraglottic GSW Exit airway was used on one occasion for a child in cardiac<br />
suffered self-inflicted 0.9% disembowelment, where officers sealed large wounds<br />
arrest. Laceration In two patients who had substantial facial trauma and were<br />
with clingfilm. The GSW doctors Entry and surgeons at the hospital were grateful for<br />
Stab Wound Wound<br />
unresponsive, Amputation<br />
3.8%<br />
the ambulance crews replaced oropharyngeal airways<br />
their resourceful actions, which helped to 16.0% save the young Puncture man’s life.<br />
6.3%<br />
that had been placed by police with supraglottic airways.<br />
GSW Exit<br />
0.9%<br />
GSW Entry<br />
3.8%<br />
Laceration<br />
31.1%<br />
Amputation<br />
0.9%<br />
Stab Wound Wound<br />
16.0%<br />
Abrasion<br />
14.8%<br />
Puncture<br />
6.3%<br />
Burns<br />
0.3%<br />
Bruising<br />
11.3%<br />
Closed Fracture<br />
12.3%<br />
Open<br />
Fracture<br />
2.2%<br />
Abrasion<br />
Burns<br />
Bruising<br />
Open Fracture<br />
Closed Fracture<br />
Puncture<br />
Stab Wound<br />
GSW Entry<br />
GSW Exit<br />
Laceration<br />
Amputation<br />
Figure 3: The proportions of injuries, out of all injuries sustained by<br />
patients reported in the PRFs. (N.B. patients may have had more than<br />
one injury).<br />
B - Breathing:<br />
Table 1: Number of times officers used<br />
each airway manoeuvre.<br />
Airway Management Frequency<br />
Repositioning patient 28<br />
Suction 10<br />
Chin lift 15<br />
Jaw thrust 20<br />
Nasopharyngeal airway 15<br />
Oropharyngeal airway 16<br />
Supraglottic airway 1<br />
The respiratory rate was recorded in 265 (89%) PRFs. 33 (11%) patients<br />
had chest seals (vented or non-vented) and only one had a suspected<br />
flail chest. 121 patients were treated with oxygen (40% of patients). 39<br />
patients had breathing recorded as ‘not normal’ but were not given<br />
oxygen by police. This was mainly because it was refused, not available,<br />
AMBULANCE <strong>UK</strong> - OCTOBER<br />
Do you have anything you would like to add or include in Features? Please contact us and let us know.<br />
143
FEATURE<br />
or given by the ambulance or fire service, so was not recorded. In three<br />
RTC patients with abnormal breathing and in two patients who had been<br />
stabbed and had chest seals applied, oxygen was not given.<br />
C - Circulation:<br />
141 (47%) PRFs had an exact heart rate filled in rather than only indicating<br />
the presence or absence of a pulse. CPR was required in 40 patients<br />
(13%) and 75% of those patients had an Automated External Defibrillator<br />
(AED) applied. ROSC on scene was achieved in 17 patients (43%).<br />
Pre-hospital oxygen treatment is mandatory in all major trauma; shock;<br />
cardiac arrest; convulsions; smoke inhalation; carbon monoxoide<br />
poisoning and in unwell paediatric patients 2 . Audits from 2010-15 and<br />
2017 indicate that oxygen delivery was generally lower than expected 4,9 .<br />
Data from this audit suggests that officers are very capable of identifying<br />
which patients require oxygen, but its use can be limited by the situation<br />
on scene. Oxygen delivery may be impractical, the patient may refuse it,<br />
or other emergency services may provide it. Considering that excessive<br />
oxygen can be detrimental to patient outcome 10 , its use in 2019<br />
generally seems appropriate.<br />
AMBULANCE <strong>UK</strong> - OCTOBER<br />
Discussion<br />
Airway Management<br />
The airway ladder used to protect the airway begins with repositioning the<br />
patient, using a chin lift or a jaw thrust, then progressing to airway adjuncts 2 .<br />
Often, simple manoeuvres such as positioning the patient on their side<br />
provided an adequate airway in the patients included in this audit.<br />
An audit in 2017 found some PRFs involving unresponsive casualties<br />
had the ‘Airway’ section of the form left blank. The report stressed<br />
that a patient’s reduced consciousness should always lead to prompt<br />
airway protection 4 . As in the manual, airway obstruction in unconscious<br />
patients is most commonly caused by the tongue and early, often<br />
simple actions can re-open the airway 2 . In 2019, all unresponsive<br />
patients’ airways were assessed and the majority were successfully<br />
managed with positional support or an adjunct. This indicates an<br />
improvement in airway management across all forces.<br />
There was only one occasion in which a supraglottic airway was used<br />
by an officer, although they were used by ambulance staff in two<br />
patients with major facial injuries. The low usage of these airways may<br />
be explained by the effectiveness of the commonly used adjuncts<br />
paired with careful patient positioning which protects the airway in<br />
the short-term before paramedics arrive. However, there may be an<br />
argument for using supraglottic airways more during CPR. In out of<br />
hospital cardiac arrest, there is evidence that asynchronous CPR has<br />
an improved outcome compared to conventional compressions and<br />
ventilation in a 30:2 ratio when CPR is not performed by an emergency<br />
medical service (EMS) professional 5, 6, 7 . In the context of these officers,<br />
it may be appropriate to use bag-valve-masks and supraglottic airways<br />
for asynchronous CPR in cardiac arrest. The technique is also useful if<br />
the number of responders is limited, as the airway can be maintained<br />
and good ventilation provided by only one person, whilst the other can<br />
deliver compressions. This is suitable for officers in specialist roles<br />
who may be alone or medically unsupported in more rural locations. If<br />
not frequently used, it may be a difficult skill to keep current. However,<br />
considering the number of cardiac arrests officers attend compared<br />
to some other incidents, it would become fairly common if used in<br />
most cardiac arrests. Certainly, those officers in specialist roles may<br />
benefit from this training. In the context of the Covid-19 pandemic,<br />
first responders should be wearing aerosol-generating procedure<br />
(AGP) personal protective equipment (PPE) if carrying out AGPs 8 . In<br />
light of this, it is unlikely that officers have adequate PPE to perform<br />
safe asynchronous CPR currently. This may mean that for the time<br />
being, officers get limited opportunities to use supraglottic airways and<br />
improve this skill.<br />
Non-Trauma Incidents<br />
There was an increased proportion of medical incidents in 2019<br />
compared to previous years 4,9 . 19 (8%) PRFs filled in between 2010-15<br />
were medical in nature, compared to 42 (14%) incidents in 2019. The<br />
types of medical problems encountered are comparable to previous<br />
years: mainly cardiac arrest or chest pain. Officers are trained in basic<br />
life support so are competent at managing medical cardiac arrests.<br />
However, 12 patients (29% of patients with medical problems) had<br />
(non-traumatic) chest pain, which is not covered to the same extent in<br />
training. This represents more than the combined number of patients with<br />
burns, found hanging or who had fallen from a height of greater than six<br />
feet (a combined total of 11 patients), and almost equals the number of<br />
shootings attended (14 patients). Although police officers are generally<br />
more likely to be called to trauma incidents, it is interesting that the most<br />
common medical emergencies are more frequent than some types of<br />
trauma. Perhaps this should be acknowledged more in training.<br />
There was a comparative increase in incidents related to drugs or<br />
alcohol. Between 2010-15, 31 PRFs (13%) reported alcohol/ drugs<br />
as the mechanism of injury 9 . Based on audits in 2017, 24 PRFs were<br />
in this category, 4,11 which made up 11% of incidents. In 2019 it rose<br />
to 67 PRFs (22%). However, alcohol/ drug use among patients may<br />
be underreported as, where it is not the main mechanism of injury, it<br />
may not be detailed in the PRF. The PRFs, which are specific to the<br />
patients, may not reflect the use of alcohol/ drugs in some situations.<br />
For example, in assaults, the victim may not be under the influence, but<br />
others involved may be.<br />
Pain<br />
Pain was very frequently reported in PRFs. However, the number is likely<br />
to be inaccurate, as it is clear that some injuries which would have been<br />
painful did not have pain recorded in the PRF, as noted in a 2017 audit 11 .<br />
Penthrox was only introduced in 2017 and it is difficult to compare<br />
trends due to differences in forms. In 2018, it was used in 10 (6%) patients<br />
compared to 23 (8%) in 2019. Generally, it appears to be effective in<br />
reducing pain score from severe to moderate, but its use by officers is<br />
currently limited by strict protocols. An audit of the use of Penthrox in<br />
these five forces 12 (Franklin, Elford et al, in preparation) looks at whether<br />
these protocols might be safely loosened to improve availability.<br />
Return of Spontaneous Circulation on Scene<br />
A report into out of hospital cardiac arrests 13 found that ROSC was<br />
achieved in 29.8% of all cases and in 41.8% of those who arrested in the<br />
presence of EMS. This indicates that the rate of 43% ROSC achieved by<br />
officers on scene is in line with the national standard. However, this is not<br />
directly comparable because the national report included all out of hospital<br />
cardiac arrest ROSCs rather than just ROSC on scene. Considering that<br />
144<br />
For more news visit: www.ambulanceukonline.com
FEATURE<br />
these officers often deliver CPR in challenging circumstances, in a prehospital<br />
environment without the kit of an ambulance, it is a credit to their<br />
training and abilities that the rate is so high.<br />
Improvements to the PRF<br />
It is a pity that the comparability of PRFs is limited by subtle differences<br />
in the forms between forces. It would be easier to audit data if there was<br />
a national standard of form. Better still, an online version would reduce<br />
errors in audits and save time. That said, the difficulty of agreeing on a<br />
national form has previously been documented 4 . It is more likely that a<br />
national reporting template might be used to inform the development of<br />
PRFs toward a standard format.<br />
The components of the PRF could also be improved. The respiratory<br />
rate was almost always recorded, but less than half of PRFs recorded<br />
an exact heart rate. Perhaps if the form had tick box categories for heart<br />
rate, as it does currently for respiratory rate, it could improve the number<br />
filled out. Although it is less important than recording a respiratory<br />
rate, heart rate of over 120 beats per minute is currently part of the<br />
exclusion criteria for use of Penthrox, so it would be useful if this was<br />
incorporated in the PRF.<br />
The PRFs included in this audit may not reflect all of the medical care<br />
given by the units in 2019. For instance, some forms were not filled<br />
in completely. Many of the incomplete observations, examinations or<br />
interventions were carried out by other members of the emergency<br />
services (as often noted in the free-text). Adding a tick-box to indicate<br />
when this was the case would avoid care appearing insufficient and<br />
would highlight the admirable teamwork between police and medical<br />
practitioners on scene.<br />
The free text section is a valuable part of the form that to some degree<br />
bypasses the problems with the form itself. The level of detail in the freetext<br />
section of the PRFs is often high and also acknowledges the PRF as a<br />
feedback mechanism to improve on care given. However, in some PRFs,<br />
the free text contradicted the boxes ticked, which leads to flawed reporting.<br />
This audit reveals a substantial number of incidents involving mental<br />
health, but this is based on analysis of the free-text material and clinical<br />
judgement of the incidents. Unfortunately, as there is no standard way of<br />
reporting mental health incidents on the PRFs, it is difficult to compare<br />
this to previous years but it could be an interesting component of future<br />
audits. An important addition would be a tick-box option for mental<br />
health, to enable a more reliable audit of these cases.<br />
Conclusion<br />
highlights the importance of medical and mental health training.<br />
There is no doubt that the skill of these officers saves lives and the<br />
quality of care given is commendable.<br />
References<br />
1. Ons.gov.uk. <strong>2020</strong>. Crime In England And Wales - Office For National Statistics. [online]<br />
Available at: https://www.ons.gov.uk/peoplepopulationandcommunity/crimeandjustice/<br />
bulletins/crimeinenglandandwales/yearendingdecember2019 [Accessed 02 May <strong>2020</strong>].<br />
2. Faculty of Pre-Hospital Care. Clinical material for police officers in specialist role,<br />
D13.2019.<br />
3. Williams, C., 2010. Police Clinical Governance. South Wales Police. Version 3.0<br />
4. Serebriakoff, P., Hartley, F., Hall, J. and Porter, K., 2019. An update on firearm police<br />
medical response. Trauma, 22(1), pp.76-77.<br />
5. Sanson, G., Ristagno, G., Caggegi, G., Patsoura, A., Xu, V., Zambon, M., Montalbano,<br />
D., Vukanovic, S. and Antonaglia, V., 2019. Impact of ‘synchronous’ and ‘asynchronous’<br />
CPR modality on quality bundles and outcome in out-of-hospital cardiac arrest<br />
patients. Internal and Emergency Medicine, 14(7), pp.1129-1137. Available at: https://<br />
europepmc.org/article/med/31273676 [Accessed: 25 May <strong>2020</strong>].<br />
6. Zhan, L., Yang, L., Huang, Y., He, Q. and Liu, G., 2017. Continuous chest compression<br />
versus interrupted chest compression for cardiopulmonary resuscitation of nonasphyxial<br />
out-of-hospital cardiac arrest. Cochrane Database of Systematic Reviews.<br />
27(3). Available at: https://www.cochrane.org/CD010134/EMERG_continuous-chestcompression-versus-interrupted-chest-compression-cardiopulmonary-resuscitation-cpr<br />
[Accessed: 25 May <strong>2020</strong>].<br />
7. Hüpfl, M., Selig, H. and Nagele, P., 2010. Chest-compression-only versus standard<br />
cardiopulmonary resuscitation: a meta-analysis. The Lancet, 376(9752), pp.1552-<br />
1557. Available at: https://www.thelancet.com/journals/lancet/article/PIIS0140-<br />
6736(10)61454-7/fulltext [Accessed: 25 May <strong>2020</strong>].<br />
8. Fphc.rcsed.ac.uk. <strong>2020</strong>. Statement From The FPHC Regarding Resuscitation During<br />
The COVID Pandemic - The Faculty Of Pre-Hospital Care. [online] Available at: https://<br />
fphc.rcsed.ac.uk/about/about-us/news/<strong>2020</strong>/statement-from-the-fphc-regardingresuscitation-during-the-covid-pandemic<br />
https://fphc.rcsed.ac.uk/my-fphc/about-us/<br />
news/<strong>2020</strong>/statement-from-the-fphc-regarding-resuscitation-during-the-covidpandemic.<br />
[Accessed 03 June <strong>2020</strong>].<br />
9. Hartley, F., Howells, A., Thurgood, A., Hall, F. and Porter, K., 2017. Medical training for<br />
police officers in specialist role (D13): A retrospective review of patient report forms<br />
from 2010–2015. Trauma, 20(1), pp.20-24.<br />
10. O’Driscoll, B., Howard, L., Earis, J., et al. British Thoracic Society Guideline for oxygen<br />
use in adults in healthcare and emergency settings . BMJ Open Resp Res 2017;4<br />
11. Rhimes, P., Williams, S., Hall, J., Porter, K, <strong>2020</strong>. Retrospective Audit of Patient Report<br />
Forms (PRFs) from semi rural specialist police firearms units January to December<br />
2017. Faculty Published Resources - The Faculty of Pre-Hospital Care. Available at:<br />
https://fphc.rcsed.ac.uk/media/2883/retrospective-audit-of-patient-report-forms-prfsfrom-semi-rural-specialist-police.pdf<br />
[Accessed: 30 June <strong>2020</strong>].<br />
12. Franklin, M., Elford, J. Hall, J., Porter, K., <strong>2020</strong>. Penthrox Audit <strong>2020</strong>. Due for<br />
publication. Available at: https://fphc.rcsed.ac.uk/media/2898/administration-ofmethoxyflurane-penthrox-as-a-pre-hospital-analgesic-by-specialist-police-officers-aretrospective-audit-of-patient-report-forms.pdf<br />
13. Out-of-Hospital Cardiac Arrest Outcomes Registry Epidemiology Report, 2018. English<br />
<strong>Ambulance</strong> Services. [online] Available at: https://warwick.ac.uk/fac/sci/med/research/<br />
ctu/trials/ohcao/publications/epidemiologyreports/ohcao_epidemiology_report_2018_<br />
published.pdf [Accessed: 25 May <strong>2020</strong>].<br />
PRFs recording the management of patients are essential tools for<br />
governing their clinical activities, aiding the training of specialist<br />
officers and enabling quality improvement of the care they provide.<br />
Simple modifications to the forms could enable police officers to<br />
more accurately and reliably record information. Officers showed<br />
improvements in airway management compared to previous years<br />
and there is possibly scope for increased use of supraglottic airway<br />
devices, primarily for asynchronous CPR. Generally, oxygen was used<br />
appropriately and the frequency of ROSC achieved demonstrates sound<br />
resuscitation skills. Incidents are frequently not trauma-related, which<br />
Authors<br />
Corresponding author<br />
Dr Jane Elford MBChB BSc (Hons), Foundation Year 1 Doctor, Ysbyty<br />
Gwynedd, Bangor. jane.elford@doctors.org.uk<br />
Miss Maggie Franklin, Medical Student, University of Liverpool.<br />
Miss Amy Elford BSc (Hons), University of Durham.<br />
Dr J Hall MBE, Hon Secretary FPHC RCS Ed.<br />
Prof. Sir K Porter, Professor of Clinical Traumatology, University Hospital<br />
Birmingham.<br />
AMBULANCE <strong>UK</strong> - OCTOBER<br />
Do you have anything you would like to add or include in Features? Please contact us and let us know.<br />
145
FEATURE<br />
WHY A SIMPLE BLOOD TEST COULD<br />
IDENTIFY THOSE MOST AT RISK OF<br />
COVID-19 COMPLICATIONS<br />
AMBULANCE <strong>UK</strong> - OCTOBER<br />
Abstract<br />
One of the biggest challenges facing medical teams treating Covid-19 patients<br />
is identifying which ones are likely to suffer the most extreme responses to the<br />
virus. Knowing this would make it possible to direct resources more efficiently<br />
and begin potentially life-saving treatment earlier.<br />
A large proportion of Covid-19 patients recover without a serious illness, and<br />
while certain factors such as age, diabetes or obesity are known to increase<br />
the chances that a patient will have more serious complications, these alone<br />
do not give a clear prediction of how the disease will progress.<br />
Now scientists believe they have an answer: a simple, affordable well<br />
established blood test which essentially measures the thickness of blood<br />
and makes it possible to separate the patients that are mildly affected, on the<br />
road to recovery or who are likely to deteriorate.<br />
The test in question is clinical viscosity. Scientists have been measuring<br />
viscosity for over 100 years and easy to use analysers have been available<br />
for 50 years. Interest in and demand for clinical viscometers has increased<br />
following the discovery that severe Covid-19 patients have very significantly<br />
raised plasma and serum viscosity levels.<br />
This is reported in the publication of a paper in the Lancet on 25 May <strong>2020</strong> by<br />
Cheryl Maier from Emory University, Georgia, Atlanta which demonstrated a<br />
dramatic rise of blood viscosity in severe Covid-19 patients. The sickest patients<br />
had the highest plasma viscosity levels, more than double normal values, and<br />
were also more likely to have a blood clot.<br />
Despite having prescribed medications, known as blood thinners, to prevent<br />
blood clots in Covid-19 patients, clotting unusually still occurred. Although<br />
referred to as blood thinners, these medications would normally block factors<br />
involved in the clotting process as opposed to thinning the blood. As a result<br />
of this, it is believed that there is more to investigate within the coagulation<br />
process. Hyperviscosity may be an important piece of the puzzle in linking<br />
inflammation to clotting. Cheryl Maier said: “One thing that stood out was the<br />
extremely high levels of fibrinogen, a big sticky protein that increases with<br />
inflammation and is a key building block for making blood clots.”<br />
Performing plasma viscosity measurements is a simple procedure when<br />
using viscometers specifically designed for clinical analysis. However, it<br />
appears that in north America, (USA and Canada) the majority of clinical<br />
laboratories are having to use viscometers that are designed for commercial<br />
use or for whole blood analysis. Many publications on clinical viscosity<br />
from north America actually report a “relative” viscosity rather than a true<br />
viscosity. This is because the analysers in use have not been designed to be<br />
calibrated, to standardised international values, SI units.<br />
The advantage of reporting an absolute viscosity value rather than a<br />
relative viscosity, is that absolute viscosities are scientifically a true value,<br />
independent of testing method and removes the potential for errors due to<br />
contamination of the water standard or the requirement to specify type of<br />
water used; e.g. tap water, distilled water, sterile water, de-ionised water etc.<br />
Results are then capable of being expressed in an internationally agreed<br />
standard format of Pascals second (Pa-s).<br />
The main advantage of using a viscosity system which has been designed,<br />
calibrated and controlled for clinical analysis, compared to an adapted<br />
industrial viscometer is that a clinical viscometer has increased precision<br />
and sensitivity in the clinical relevant range of 1.2 to 10 mPa-s. Commercial<br />
viscometers tend to have an operating range of between 10 and 100,000 Pa-s.<br />
Introducing clinical viscometers to pathology laboratories will enable<br />
clinicians to rapidly obtain results which can be easily interpreted for both<br />
plasma and serum viscosity, which for covid-19 patients will allow a simple<br />
rapid decision on which patients require more intensive therapy.<br />
Further advantages include:<br />
• Systems designed for closed vial sampling to reduce biohazard risk to<br />
operators<br />
• Systems designed for high sample throughput by fully automated<br />
sampling and cleaning<br />
• Automated cleaning designed to remove sample contamination and carry over<br />
• Software designed to highlight clinically abnormal/significant results<br />
• Systems designed to analyse small sample volumes under 0.5ml<br />
• As only 50µl is used per test, repeat tests can be carried out on 0.5ml sample<br />
• Integration to clinical laboratory Information Management Systems (LIMS)<br />
standard<br />
• Systems designed to be compliant with clinical laboratory regulatory<br />
requirements such as ISO:151489<br />
How can a combined plasma and serum viscosity be used and<br />
interpreted?<br />
The key to predicting how a patient’s illness is progressing lies in comparing two<br />
different viscosity measurements, blood plasma and blood serum both of which<br />
can be carried out on modern clinical viscometers.<br />
Plasma viscosity is mainly determined by the level of a blood clotting protein<br />
called fibrinogen and antibody concentrations produced by the body’s<br />
immune system, when it detects and neutralises harmful substances.<br />
Dr.Cheryl Maier’s Covid-19 patients had fibrinogen levels of up to five times<br />
the normal value.<br />
Serum is a clear fluid released from blood when blood clots. There is no<br />
fibrinogen in serum as this is all used in the production of the clot. Serum<br />
viscosity levels are mainly dependent upon the number of antibodies, the<br />
‘fighting proteins’ present. So, an increased serum viscosity can indicate a<br />
strong antibody response to Covid-19.<br />
If both plasma and serum results are normal and the patient has a diagnosis of<br />
Covid-19, they are probably asymptomatic, an infected patient who does not<br />
present with serious symptoms but is possibly a carrier.<br />
If only the serum viscosity is raised, this indicates increased antibody<br />
production and may indicate a recovering patient.<br />
If the plasma and serum viscosity analysis reveals that both results are<br />
raised, then the patient has raised antibody levels, and may also have a<br />
raised fibrinogen level. These patients should have their fibrinogen monitored<br />
to see if it is rising or falling.<br />
A raised plasma viscosity with normal serum viscosity indicates raised<br />
fibrinogen with no antibody response. These patients are probably<br />
deteriorating and will therefore be more likely to require intensive therapy.<br />
146<br />
For further recruitment vacancies visit: www.ambulanceukonline.com
Discover the Quantum FEATURE<br />
DIFFERENCE<br />
THE Prehospital Blood & Fluid Warming Solution<br />
<br />
<br />
Blood & Fluid<br />
Warming System<br />
CAPABILITIES:<br />
u Delivery of 1000mL of 4°C Whole Blood at 100ml/min with an<br />
output temperature of 38°C+/-2°C on a single battery charge<br />
u Warm-up time 24 seconds.<br />
Lightweight & Portable 624gms total weight<br />
FAST | EFFECTIVE | SAFE | INTUITIVE | LIGHTWEIGHT | POWERFUL<br />
AMBULANCE <strong>UK</strong> - OCTOBER<br />
Exclusive to www.dsmedical.co.uk Contact DS Medical: 01329 311451<br />
147<br />
Do you have anything you would like to add or include in Features? Please contact us and let us know.
NEWSLINE<br />
Just brew-ti-ful:<br />
firefighter<br />
entrepreneurs serve<br />
up 20,000 cups of<br />
coffee to Covid-19<br />
key workers<br />
Two firefighter entrepreneurs<br />
handed out over 20,000 cups<br />
of coffee to frontline key<br />
workers, including <strong>Ambulance</strong><br />
staff, during the peak of the<br />
coronavirus in the <strong>UK</strong> as they<br />
gear up for a second spike in<br />
the pandemic.<br />
Matt Broxton, 28, and Tom Taylor,<br />
28, decided to set up an online<br />
coffee company because the<br />
instant coffee at the fire stations<br />
they both worked at was ‘terrible’<br />
and ‘tasted like tarmac’.<br />
The pair has sold 4741.25kg of<br />
coffee so far which at 7g a cup<br />
is the equivalent of 677,321 cups<br />
of coffee with 20,000 of those<br />
going direct to the frontline for<br />
free during the <strong>UK</strong> lockdown in<br />
the spring.<br />
Frontline Coffee aims to support<br />
frontline charities ‘one coffee bean<br />
at a time’ and has so far raised<br />
over £17,000 with donations<br />
made to NHS Charities Together,<br />
the RNLI (Royal National Lifeboat<br />
Institution), TASC (The <strong>Ambulance</strong><br />
Staff Charity) and The Firefighters<br />
Charity.<br />
Matt said: “Our emergency and<br />
health services are the best in<br />
the world, but they are only the<br />
best because of the people that<br />
make them up. We strive to be<br />
a company that supports these<br />
amazing people.<br />
“In the fire service after you’ve<br />
been out on a ‘shout’ to a house<br />
fire or had to deal with a difficult<br />
situation, it’s a typically British<br />
thing to do to have a coffee or<br />
cup of tea.<br />
“When lockdown happened and<br />
key workers were having to deal<br />
with the enormity of Covid-19,<br />
we felt these people would be in<br />
even more need of a good cup of<br />
coffee when they finally sat down<br />
for a break.<br />
“That is why we made it our<br />
mission to get good coffee to key<br />
workers working exceptionally<br />
hard during these troubling times<br />
in hospitals, police, fire and<br />
ambulance stations during the <strong>UK</strong><br />
lockdown.<br />
“Our soul mission is also to raise<br />
awareness about the great work<br />
They felt all key workers involved<br />
in dealing with the Covid-19<br />
pandemic ‘deserved a decent cup<br />
of coffee’. The young founders set<br />
up Frontline Coffee with its profits<br />
donated to emergency service<br />
and health charities.<br />
“Me and Tom both have a passion<br />
for real coffee so we always<br />
used to joke about how terrible<br />
the instant coffee was at the fire<br />
station and how it used to taste<br />
like tarmac.<br />
our frontline services do and<br />
raise money for their respective<br />
charities. We’re absolutely<br />
delighted to have raised more<br />
than £17,000 so far.”<br />
Frontline Coffee has taken off so<br />
rapidly that Matt has left his job<br />
as a firefighter with the London<br />
Fire Brigade to focus on their<br />
social enterprise full-time. Tom,<br />
meanwhile, still works for the<br />
Devon and Somerset fire service.<br />
AMBULANCE <strong>UK</strong> - OCTOBER<br />
148<br />
For more news visit: www.ambulanceukonline.com
NEWSLINE<br />
i-view <br />
Matt and Tom’s collection<br />
includes a blend for each<br />
emergency service such as First<br />
Response supporting TASC, the<br />
Bevan Blend for NHS Charities<br />
Together named after its creator,<br />
Aneurin Bevan and The Thin Red<br />
Line for Firefighter Charity and<br />
more. Frontline Coffee also sell<br />
grinders, brewing kits, specialist<br />
tea and merchandise.<br />
The pair got started with one<br />
second hand industrial roaster<br />
and it is now manufactured<br />
on a grand scale in the south<br />
west of England. Matt and<br />
Tom hand-picked the coffee<br />
beans to match the exact taste<br />
the pair were looking for. They<br />
hand-pack orders themselves<br />
before arranging deliveries to<br />
customers.<br />
Tom said: “We never expected<br />
Frontline Coffee to take off like<br />
this but it grew legs so we had to<br />
make a decision that one of us<br />
would have to take it on full-time.<br />
We decided that Matt would be<br />
better pushing it further on a dayto-day<br />
basis as he had created<br />
the website and runs all of our<br />
social media.<br />
“We didn’t want to look back in<br />
10 years’ time and say ‘what if?’.<br />
We had spoken quite a few times<br />
about setting up something for<br />
charity and giving something<br />
back. The sudden arrival of<br />
Covid-19 brought Frontline Coffee<br />
forward quicker than either of us<br />
ever imagined. It has just been an<br />
amazing journey so far.”<br />
Working in the Frontline services<br />
clearly runs in both families. Matt’s<br />
mum, Jannette was a nurse, and<br />
his Dad, Gary and uncle, Ron,<br />
were both in the Royal Navy, while<br />
girlfriend Rosie, who is Tom’s<br />
cousin, is also a nurse. Tom’s<br />
wife, Kirsty, meanwhile, is a police<br />
detective.<br />
Matt added: “Both mine and<br />
Tom’s families both have a history<br />
of working for frontline services so<br />
I guess we all have it in our blood<br />
to help people. Now more than<br />
ever, we aim to support our key<br />
workers through this next set of<br />
challenging times.”<br />
<br />
Single-use<br />
No reusable components<br />
Fully disposable<br />
No reprocessing<br />
Minimises the risk<br />
of cross contamination<br />
i-view<br />
video laryngoscopy<br />
wherever and whenever you intubate<br />
www.intersurgical.co.uk/info/iview<br />
Quality, innovation and choice<br />
lnteract with us<br />
AMBULANCE <strong>UK</strong> - OCTOBER<br />
www.intersurgical.co.uk<br />
149
NEWSLINE<br />
WMAS<br />
<strong>Ambulance</strong>: Code<br />
Red, the new<br />
documentary on<br />
paramedics<br />
The first episode of the new<br />
documentary on paramedics<br />
“<strong>Ambulance</strong>: Code Red” went<br />
on air on Channel 5. The<br />
EMS protagonist is the West<br />
Midlands <strong>Ambulance</strong> Service.<br />
Critical care paramedic Tom<br />
Waters speaks about his<br />
experience as a paramedic on<br />
the ambulance, but also about his<br />
experience on stage. Indeed, he<br />
starred in this new documentary<br />
series on paramedics and<br />
ambulance life.<br />
In 2015, Tom alongside Dr Dave<br />
Cooper was involved in the rescue<br />
and treatment of 18-year-old Leah<br />
Washington and 20-year-old Vicky<br />
Cooper during the Alton Towers<br />
rollercoaster crash. Together they<br />
climbed 40ft to treat Leah and<br />
Vicky, who both had to have part<br />
of their legs amputated following<br />
the horrific accident. They were<br />
given a national award for their<br />
efforts.<br />
In this new series, Tom will<br />
appears with specially trained<br />
paramedics battling at the<br />
roadside to save a 13-year-old<br />
boy left with suspected brain<br />
injuries following a road accident.<br />
Time is ticking for the patient<br />
and the critical care paramedics<br />
will have to use their diagnostic<br />
and life-saving skills to prioritise<br />
treatment so he can make it to the<br />
hospital.<br />
Without giving further spoilers,<br />
the chief executive of West<br />
Midlands <strong>Ambulance</strong> Service,<br />
Anthony Marsh, reported that “the<br />
programme gives a real insight<br />
into the support that critical-care<br />
paramedics and doctors provided<br />
by the air ambulance charity<br />
can give to its own ambulance<br />
crews who are dealing with some<br />
of the most complex patients.<br />
It demonstrates how they work<br />
with the crews on scene to use<br />
their enhanced skills to benefit<br />
patients. Without the work of the<br />
staff on scene, the teams wouldn’t<br />
be able to use those skills, so it<br />
really is all about working together.<br />
The teams provide critical care<br />
at the scene that saves lives,<br />
brains and limbs, including prehospital<br />
surgery and pre-hospital<br />
anaesthesia.”<br />
EEAST<br />
<strong>Ambulance</strong> service<br />
strikes back<br />
with hard-hitting<br />
campaign against<br />
abuse<br />
The EAST of England<br />
<strong>Ambulance</strong> Service NHS Trust<br />
has responded to increased<br />
assaults and abuse against<br />
staff with a tough publicity<br />
campaign that spells out the<br />
impact that abuse has on<br />
crews – and their ability to do<br />
their job.<br />
The Choose Respect!<br />
campaign features shocking<br />
images of ambulance crew<br />
members – accompanied by<br />
text describing being violently<br />
or sexually assaulted while on<br />
duty, along with facts about how<br />
it affected their ability to work.<br />
Alex, 27, is an Emergency<br />
Medical Technician, working out<br />
of Thetford, who volunteered to<br />
feature in the campaign.<br />
He was assaulted on Boxing<br />
Day 2019 by a violent drunk,<br />
causing him to be off work for<br />
more than a week. He said:<br />
assistance, and the police took<br />
him away.<br />
“There was no major damage,<br />
but I was off work for a week<br />
and a half as I couldn’t drive<br />
because of headaches. And<br />
I had a black eye for three<br />
weeks.<br />
“I’m more hesitant now about<br />
going into situations that are<br />
flagged as potentially violent…<br />
instead of going in and seeing<br />
what the situation is, I’ll wait<br />
until the Police arrive.”<br />
Chief Executive Dorothy<br />
Hosein said the campaign was<br />
intended to make people aware<br />
that assaults against staff were<br />
not without consequences:<br />
“We are seeing a steady<br />
increase in assaults and abuse,<br />
year-on-year from just over<br />
1,000 incidents in 2015-16 to<br />
over 1,300 in 2018-19.<br />
“This has to stop. There were<br />
250 incidents between March 1<br />
and June 11 this year alone.<br />
Not only does this cause<br />
terrible long-term physical<br />
and psychological harm to our<br />
“We had taken our patient to<br />
West Suffolk Hospital, when<br />
there was a problem with<br />
another patient being admitted<br />
in front of us. The patient<br />
became aggressive to the duty<br />
sister and the students, and<br />
when I went over to him, he<br />
punched my colleague.<br />
employees, but clinicians and<br />
other essential staff needing<br />
time off work because of<br />
assaults or abuse affects our<br />
capacity to serve the public<br />
during the pandemic.<br />
“No-one deserves to be abused<br />
at work, but we will not tolerate<br />
our staff – who are only ever<br />
AMBULANCE <strong>UK</strong> - OCTOBER<br />
“I managed to push him out the<br />
of door, where he began to try<br />
and break into the back of an<br />
ambulance before he returned<br />
and tried to hit me.<br />
“I dodged the punch, but didn’t<br />
expect the head-butt. The<br />
security team and two passing<br />
prison guards came to my<br />
there to help people – being<br />
abused and left unable to work,<br />
at a time when the public really<br />
needs them.<br />
“We will always support our<br />
staff and work with the police<br />
to secure convictions and the<br />
strongest penalties wherever<br />
appropriate.”<br />
150<br />
For further recruitment vacancies visit: www.ambulanceukonline.com
www.theortusgroup.com T: +44 (0)845 459 4706<br />
NEWSLINE<br />
xxx<br />
xxx<br />
corpuls simulation<br />
xxx<br />
REALITY . SIMULATED<br />
xxx<br />
Typical xxx training methods focus on learning<br />
a technique xxx though repetition, but there is<br />
often a large gap between theoretical scenarios<br />
and the actual ‘fight’ for a human life.<br />
xxx<br />
corpuls<br />
xxx<br />
simulation brings realistic scenarios<br />
to your training and ensures the paramedic is<br />
prepared xxx to overcome unforseen situations.<br />
This, xxxas well as the exact replication of all<br />
corpuls defibrillators, creates an incomparably<br />
realisic training situation - the result being<br />
xxx<br />
that<br />
xxxthe team is optimally prepared for every<br />
scenario and therefore, a significantly better<br />
quality of care for the patient.<br />
FOUR IN ONE<br />
With corpuls simulation, you can simulate all four corpuls defibrillators in one system using<br />
the same hardware:<br />
corpuls aed corpuls 1<br />
corpuls 3<br />
12.9” iPad as Touchscreen Monitor Realistic parameters and curves<br />
Scenario Editior<br />
Bluetooth connection to corpuls cpr<br />
Simulation consumables<br />
All the functions of the original device<br />
When coming to terms with the ‘new normal’,<br />
we knew we needed to adapt our business to<br />
ensure continued communication and engagement<br />
with our customers and partners.<br />
Our solution...<br />
For the latest <strong>Ambulance</strong> Service News visit: www.ambulancenewsdesk.com<br />
We aim to support, engage, and debate all<br />
things medical. From product tutorials, to interviews<br />
with key industry professionals, we are<br />
here to keep you up-to-date with everything<br />
you need to know, when you need to know it.<br />
Scan the QR code to sign up<br />
for further details on the<br />
launch. As a thank you for<br />
signing up, you’ll be entered<br />
into our free draw to win a<br />
£100 Amazon Gift Voucher.<br />
AMBULANCE <strong>UK</strong> - OCTOBER<br />
151
NEWSLINE<br />
AMBULANCE <strong>UK</strong> - OCTOBER<br />
Statement in<br />
response to CQC<br />
inspection report<br />
Today’s Care Quality<br />
Commission report is<br />
clear that the Trust has<br />
not addressed some longstanding<br />
concerns around<br />
culture, leadership and<br />
governance. The Trust’s<br />
executive team absolutely<br />
recognise the seriousness<br />
of the concerns raised by<br />
the CQC, and have set out to<br />
improve the organisation’s<br />
culture, strengthen<br />
safeguarding, and tackle<br />
inappropriate behaviour, as<br />
urgent priorities.<br />
Since the inspection during June<br />
and July this summer, the Trust<br />
has:<br />
• updated safeguarding policies;<br />
now using new procedures<br />
to record, manage and audit<br />
concerns<br />
• increased support and<br />
mentoring for staff raising<br />
concerns and clearer routes<br />
for mental health support<br />
identified;<br />
• introduced more robust<br />
complaints procedures to<br />
ensure effective investigations<br />
and lessons are learned<br />
systematically.<br />
During the next month the Trust<br />
will:<br />
• increase the visibility of the<br />
Freedom to Speak Up Guardian<br />
and encourage staff to speak<br />
up<br />
• introduce campaigns to<br />
encourage positive cultural<br />
change and behaviour<br />
• survey all staff on their<br />
experience of the Trust’s<br />
culture including inappropriate<br />
behaviour.<br />
The Chair of the East of England<br />
<strong>Ambulance</strong> Service, Nicola<br />
Scrivings said:<br />
“Today’s report calls out where<br />
we need to improve and we will<br />
now do everything possible, as<br />
fast as possible, to make the<br />
improvements required.<br />
“We are working closely with the<br />
CQC, NHS colleagues and other<br />
partners to take action right now<br />
to address these concerns and<br />
put this right for the long-term.<br />
“The trust aims to provide<br />
outstanding quality of care and<br />
performance for patients and be<br />
an exceptional place to work,<br />
volunteer and learn. In a message<br />
to staff today, the executive<br />
team has again reinforced its<br />
commitment to listen to and<br />
support anyone who raises<br />
concerns.<br />
“It is clear from the CQC staff<br />
survey that the majority of staff<br />
at the Trust are proud to work for<br />
EEAST. The role of the leaders<br />
is to make sure every member<br />
of the team feels that pride, with<br />
the support and culture they<br />
deserve.”<br />
SECAMB<br />
<strong>Ambulance</strong> crews<br />
return to improved<br />
and modernised<br />
Sheppey station<br />
South East Coast <strong>Ambulance</strong><br />
Service (SECAmb) staff have<br />
returned to Sheppey <strong>Ambulance</strong><br />
Station following a six-month<br />
major refurbishment project.<br />
The station modernisation forms<br />
part of the Trust’s ongoing work<br />
to convert all of its estate to its<br />
Make Ready system – a vehicle<br />
preparation system which sees<br />
specialist teams of staff employed<br />
to clean, restock and maintain<br />
vehicles, meaning staff, who<br />
previously undertook these tasks,<br />
can spend more time treating<br />
patients.<br />
The improvement work at the<br />
Main Road site in Queenborough<br />
means the station now boasts<br />
modern rest, educational and<br />
training facilities including a<br />
training room including named<br />
in memory of Rhod Prosser, a<br />
SECAmb paramedic who sadly<br />
died following a battle with cancer<br />
earlier this year.<br />
<strong>Ambulance</strong> crews, who<br />
temporarily began shifts in<br />
Sittingbourne while the works<br />
took place, and responded<br />
from response posts including<br />
Sheppey Fire Station, will now<br />
start their shifts at the new base<br />
before being posted to respond<br />
from a number of <strong>Ambulance</strong><br />
Community Response Posts<br />
across the region.<br />
As part of wider improvements<br />
in the area, and as announced<br />
last month, ambulance crews<br />
starting and ending their shifts<br />
at Medway and Sittingbourne<br />
ambulance stations will, instead,<br />
start and finish at a new facility<br />
in Gillingham, which expected to<br />
become operational in 2022.<br />
The new centre will house a<br />
Make Ready Centre as well as<br />
999 and 111 operations centres.<br />
Sheppey vehicles will feed into<br />
the Gillingham centre regularly<br />
for restocking, cleaning and<br />
maintenance.<br />
SECAmb Operating Unit Manager<br />
for Dartford and Medway, Will<br />
Bellamy, said: “It’s been great to<br />
welcome crews back to the muchimproved<br />
station. Our staff, and in<br />
turn our patients, will benefit from<br />
this development which ensures<br />
our site on the island is modern<br />
and provides us with a building<br />
and facilities which are fit for the<br />
future.<br />
“I would like to thank staff for their<br />
patience while the work took place<br />
and also Kent Fire and Rescue for<br />
their continued support which has<br />
included us using their premises<br />
as a rest point for crews.”<br />
SECAMB<br />
Trust achieves<br />
gold award for<br />
commitment to<br />
equality and diversity<br />
South East Coast <strong>Ambulance</strong><br />
Service NHS Foundation Trust<br />
(SECAmb) is pleased to have<br />
achieved a gold award from<br />
enei (Employers Network for<br />
Equality and Inclusion).<br />
The TIDE (Talent Inclusion and<br />
Diversity Evaluation) gold award is<br />
the third year in a row SECAmb has<br />
been recognised by the organisation<br />
following two silver awards.<br />
SECAmb is the only ambulance<br />
trust in a record 98 entries from<br />
organisations from across 26<br />
sectors. A total of 51 achieved an<br />
award with SECAmb among 13<br />
achieving the highly-coveted gold<br />
award.<br />
Other gold winners include IBM<br />
<strong>UK</strong> ltd, the Ministry of Justice and<br />
fellow NHS organisation, North East<br />
London NHS Foundation Trust.<br />
SECAmb will use the benchmark<br />
report to implement further<br />
improvements in how diversity<br />
and inclusion is thoroughly<br />
embedded throughout the<br />
whole organisation and a part of<br />
everything it does.<br />
SECAmb Executive Director of<br />
HR & Organisation Development,<br />
Ali Mohammed said: “I’m really<br />
pleased that our approach to<br />
diversity and inclusion has once<br />
again been recognised, this year<br />
with an enei gold benchmark.<br />
We know that we must do lots<br />
more to ensure this is embedded<br />
throughout the whole organisation<br />
but it’s great to see our continued<br />
progress recognised in this way.”<br />
152<br />
For more news visit: www.ambulanceukonline.com
Solution Sheet<br />
HEXAGON INTRODUCES ASSISTIVE AI TECHNOLOGY FOR<br />
PUBLIC SAFETY AGENCIES<br />
Insights from next-generation tools<br />
Next-generation (NG9-1-1 / 112) technologies open new<br />
In today’s world, headline-grabbing emergencies are happening<br />
more communications frequently in more channels places. (e.g., It is hard texting to watch and messaging<br />
television, listen<br />
to apps) the radio, between or read the a news public article and without public safety learning answering about another<br />
incident points impacting (PSAPs). And communities because in PSAPs both the are short the and first long link term. in<br />
the public safety chain, many next-generation solutions<br />
Unfortunately, are designed those with responding call-takers to complex in mind. emergencies often have very<br />
little lead time and real-time information, making complex emergencies<br />
even When more integrated challenging within and disruptive. a PSAP’s Whether data-rich it is an computer-aided<br />
explosion, terrorist<br />
attack, dispatch or smaller (CAD) events system, like coordinated for example, thefts AI across and ML a city, can there help is<br />
a fill need operational for clear, immediate blind spots insights with that assistive can inform insights, swift and effective helping<br />
action. avoid seeking The impacts faster to public from build safety large, agencies safer, rapid on-set can smarter detect incidents. and respond cities And to<br />
complex because events, those the insights better they are can based contain on the the effects. organization’s<br />
data, Once it considered promotes confident a futuristic decision-making.<br />
science fiction concept,<br />
Hexagon’s artificial Safety intelligence & Infrastructure (AI) division plays identified critical this roles gap in and developed<br />
a Another society<br />
new AI-powered benefit today.<br />
product,<br />
From of NG9-1-1 HxGN<br />
smartphones<br />
OnCall / 112 ® technologies Dispatch<br />
and computers<br />
| Smart include Advisor, a to fill it.<br />
caller’s to infrastructure ability to quickly and government share photos operations, and videos AI with is<br />
Why call-takers. do public safety agencies need assistive AI?<br />
pervasive and PSAPs utilized with remote in countless access ways. to cameras A recent can IDC<br />
leverage report described AI to quickly AI as and “inescapable,” accurately identify and predicted potential 90%<br />
When complex emergencies occur, anyone working in a public safety<br />
suspects, of new enterprise suspect vehicles, apps will unsafe have embedded incident scenes, AI by 2025. or a<br />
agency knows relevant information trickles in. Crucial insights can be<br />
suspicious package. And passing images and video to the<br />
hidden in the noise or spread across systems and departments. Even<br />
field But what gives is first it, responders exactly? The invaluable National information.<br />
Institute of Justice<br />
members of the same team may hold different fragments of information.<br />
describes AI as a machine’s ability to independently<br />
These fragments need to be filtered and pieced together to understand<br />
Organizations perceive and respond commonly to tasks utilize that AI in would other typically ways,<br />
the magnitude and nature of what is happening, but it’s often impossible<br />
from<br />
to<br />
require gunshot<br />
see the big<br />
human detection<br />
picture<br />
intelligence systems<br />
until it’s too late<br />
and<br />
to act.<br />
decision-making. to evidence analysis AI,<br />
and along processing. with machine Genetic learning testing (ML), utilizes works AI behind and ML the<br />
to<br />
A scenes uncover<br />
sad example to enhance patterns<br />
of this is the the in DNA<br />
2019 execution that solve<br />
Christchurch of shootings tasks crimes like and<br />
in New<br />
Zealand identify transcribing that perpetrators.<br />
were audio over in less and than video, 20 minutes. blocking It is unwanted<br />
those types of<br />
situations emails, that preventing are keeping banking agency supervisors fraud, and even directors diagnosing up at night.<br />
medical conditions.<br />
Many agencies have analytics solutions that mine data and give clarity<br />
to How past AI events processes in order data to prepare varies for because the future. it A can recent be survey autonomous of<br />
public (i.e., safety applied professionals across an in the entire US found business 81 percent process) of respondents or<br />
said assistive AI somewhat, (i.e., applied very, or extremely in specific important stages). to their IDC organisations.*<br />
describes<br />
these processes as producing insights, assessing<br />
Agencies options, that and use taking AI on a regular actions. basis The are processes already familiar help with these<br />
benefits:<br />
organizations determine which steps are best handled<br />
by AI, and which by people.<br />
• Efficiency: Streamlined workflows between control rooms and the field<br />
Ready to try AI?<br />
At all levels of a public safety organization, AI-enabled<br />
• Feedback: Operational data provides insights into where process<br />
solutions improvements support can be continual, made autonomous assessment<br />
that is more efficient, effective, and scalable than<br />
What manual has monitoring been missing of in video, the field alarms, however and is quick common access to<br />
crucial operating information pictures to understand alone. what is happening in the here and<br />
now. In complex, fast-moving situations, even a single timely insight<br />
can Assistive be a game-changer. AI doesn’t automate That pressing decision-making, need for timely but insights is<br />
what instead drove equips the creation decision-makers of Smart Advisor. with additional relevant<br />
information. The right AI solution can be a critically<br />
What assistive HxGN tool OnCall for organizations Dispatch | Smart working Advisor? to build safer,<br />
smarter cities today and for generations to come.<br />
Smart Advisor uses assistive AI, advanced statistics, and machine<br />
learning HxGN Benefits OnCall® (ML) to for continually Dispatch public analyse safety | Smart operational Advisor leverages data in real-time AI to<br />
fill and operational ML to identify blind spots, similarities enabling and responders patterns to act in sooner and<br />
be operational<br />
AI is quickly emerging<br />
better informed. data and<br />
as<br />
alert<br />
a key<br />
PSAPs<br />
technology<br />
in real<br />
for<br />
time.<br />
public<br />
It<br />
safety<br />
uncovers<br />
organizations<br />
connections<br />
seeking to<br />
to<br />
build<br />
detect<br />
safer,<br />
emerging,<br />
smarter communities.<br />
complex<br />
For emergencies<br />
A survey example, of when public<br />
sooner it detects safety<br />
and similarities shares<br />
professionals<br />
findings and anomalies found<br />
for immediate<br />
81% across of<br />
calls action.<br />
respondents for service, By filling<br />
said it alerts operational<br />
AI is agencies somewhat,<br />
blind to the very,<br />
spots, potential or extremely<br />
Smart onset Advisor of complex<br />
emergencies, helps<br />
important<br />
PSAPs<br />
to from mitigate<br />
their large, organizations. rapid-onset detrimental events Agencies<br />
impacts to smaller that<br />
on<br />
use linked AI on a<br />
incidents.<br />
communities,<br />
regular basis By detecting are<br />
levels<br />
already patterns<br />
of service,<br />
familiar and<br />
and<br />
connections with<br />
staff<br />
these<br />
well-being.<br />
sooner, benefits: agencies<br />
can act faster and coordinate smarter to reduce the impact on<br />
communities, Learn<br />
• Efficiency:<br />
more resources, about<br />
Streamlined<br />
how and Hexagon’s staff. workflows<br />
first-to-market<br />
from the PSAP<br />
solution<br />
to the<br />
can<br />
field<br />
help your organization see the unseen.<br />
How • does Forecasting: it work? Evidence-based insights into crime<br />
trends promotes effective policing<br />
Smart Advisor works within Hexagon’s industry-leading, nextgeneration<br />
• Awareness: computer-aided Data mining dispatch tools (CAD) uncover solutions patterns, to deliver<br />
continual, similarities, autonomous and assessments linked incidents across the entire pool of<br />
Artificial Intelligence a Critical Public Safety Tool<br />
Next-generation technology offers assistive, real-time insights for organizations<br />
live • and Worker recent events. well-being: It works Automated behind the scenes processes and only reduce alerts<br />
the user when a situation is detected. That makes working with<br />
staff stress and turnover and allow personnel to<br />
Smart Advisor more efficient, effective, and scalable than manual<br />
focus on high-level tasks<br />
monitoring of videos, alarms, and common operating pictures alone<br />
and • reduces Transparency: overreliance Surveillance on contextual and searches. data collection<br />
Additionally,<br />
it reduces methods the burden (e.g., on facial staff by and acting license as a plate second recognition,<br />
set of eyes<br />
during evolving, sonar-based high pressure imaging) situations. promote opportunities to build<br />
public trust and improve accountability<br />
Most importantly, with Smart Advisor, the user is always in control;<br />
• Feedback: Operational data provides insights into<br />
no decision or action is automated. When notified, users can<br />
where process improvements can be made<br />
assess the alert and decide whether to act on, share, or dismiss<br />
Assistive AI doesn’t automate decision-making,<br />
but instead equips decision-makers with additional<br />
relevant information. The right AI solution can be a<br />
critically assistive tool for organizations working to build<br />
safer, smarter cities today and for generations to come.<br />
• Forecasting: Evidence-based insights into patterns in calls for service it. By detecting more crucial connections sooner, public safety<br />
by time of day, day of the week, season, and location<br />
agencies are better equipped to create safer, more resilient<br />
communities for citizens.<br />
• Awareness: Data mining tools uncover similarities linked incidents,<br />
and information on previous interactions with a caller<br />
For more information, visit http://hxgn.biz/SmartAdvisor-<strong>UK</strong><br />
• Worker well-being: Automated processes reduce staff stress and turnover<br />
by avoiding overload and allowing personnel to focus on high-level tasks *http://hxgn.biz/technology-<strong>UK</strong><br />
Hexagon is a global leader in sensor, software and autonomous technologies. We are putting data to work to boost efficiency, productivity and quality<br />
across industrial, manufacturing, infrastructure, safety and mobility applications. Our technologies are shaping urban and production ecosystems to
NEWSLINE<br />
a helipad so close to our highly<br />
Patients were previously flown to<br />
Measuring 30 metres by 30<br />
£600,000 helipad<br />
operational at Hull<br />
Royal Infirmary<br />
Helicopters are now able to fly<br />
critically ill and injured patients<br />
directly to Hull Royal Infirmary<br />
after its new £600,000 helipad<br />
was declared operational.<br />
Hull University Teaching Hospitals<br />
NHS Trust has completed the<br />
major construction project<br />
so patients seriously hurt in<br />
accidents across East and North<br />
Yorkshire and parts of Lincolnshire<br />
can be flown into the hospital<br />
grounds, the Major Trauma Centre<br />
(MTC) for the area.<br />
The helipad, behind Hull Royal<br />
Infirmary’s £12m Emergency<br />
Department (ED), had been<br />
funded entirely by the HELP<br />
Appeal, the only charity in the<br />
country dedicated to funding NHS<br />
hospital helipads.<br />
Trust Chief Executive Chris<br />
Long said: “We are deeply<br />
grateful to the HELP Appeal for<br />
its £600,000 donation which<br />
has allowed us to construct<br />
the helipad directly behind our<br />
Emergency Department.<br />
skilled major trauma team means<br />
we will be able to save more lives<br />
in situations where every second<br />
counts.”<br />
Robert Bertram, Chief Executive<br />
of the HELP Appeal, said:<br />
“As the Major Trauma Centre<br />
for the whole region, funding<br />
a helipad outside ED was<br />
essential. Everyone is aware of<br />
the vital roles that hospitals and<br />
air ambulances play in treating<br />
a critically ill patient but having<br />
a helipad outside the ED can<br />
play a significant part in saving<br />
vital minutes when transporting<br />
a patient to the expert care they<br />
need to save lives.<br />
“As the only charity in the country<br />
funding live-saving helipads, we<br />
are pleased to be able to cover<br />
the entire cost of the helipad.<br />
We know the difference having a<br />
ground-level helipad right outside<br />
ED would make.<br />
“With the support of the air<br />
ambulances and the excellent<br />
emergency care team at Hull<br />
Royal Infirmary, this unique mix of<br />
helicopters, helipad and hospital<br />
medical staff will make a huge<br />
difference to those people who<br />
may need life-saving treatment<br />
the helipad on the other side of<br />
the hospital car park on Argyle<br />
Street and had to be transferred<br />
to Hull Royal in an ambulance<br />
along Anlaby Road, one of the<br />
busiest roads in the city centre.<br />
Intensive Care Consultant Dr<br />
Tom Cowlam, the trust’s clinical<br />
lead for the MTC, said: “The new<br />
helipad will shorten the journey<br />
by a quarter of an hour and<br />
remove the need for the patient<br />
to be transferred in a second<br />
ambulance to the Emergency<br />
Department.<br />
“It will make the transfer quicker<br />
and more seamless for the trauma<br />
patient.<br />
“When you have a really poorly<br />
person, this might be the<br />
difference between life and death<br />
because this could be the time<br />
when they are having surgery or a<br />
massive blood transfusion to save<br />
them.”<br />
Duncan Taylor, Director of Estates,<br />
Facilities and Development, said<br />
the trust funded the demolition<br />
of the Haughton building among<br />
others and clearance of the site<br />
before main contractor Unico<br />
Construction could begin work on<br />
metres, 900 tonnes of concrete<br />
were brought onto the hospital<br />
site, over the course of one day.<br />
An access road for fire engines<br />
and service vehicles has been<br />
built alongside a second<br />
pedestrian route where patients<br />
will be carried out of the air<br />
ambulance and rushed into the<br />
ED.<br />
Special double fences have been<br />
erected around the helipad as<br />
“baffles” to reduce noise pollution,<br />
provide security and the majority<br />
of the site has been turfed with<br />
pinned grass covered with mesh<br />
overlay to act as a “soakaway” to<br />
remove water from the helipad.<br />
Lights have been imported<br />
from Holland to be set into<br />
the concrete, now covered in<br />
specialist paint.<br />
Hull is one of the country’s 27<br />
Major Trauma Centres (MTCs),<br />
credited with saving an additional<br />
1,600 people’s lives since they<br />
were established in 2012.<br />
Lincs and Nott Air <strong>Ambulance</strong><br />
use the Hull helipad most often,<br />
with Yorkshire Air <strong>Ambulance</strong><br />
and Derbyshire, Leicester and<br />
Rutland Air <strong>Ambulance</strong> also flying<br />
casualties to the city.<br />
“There is no doubt that having<br />
urgently.”<br />
the helipad.<br />
The Search and Rescue<br />
helicopter, based at Humberside<br />
Airport, also lands in Hull with<br />
people winched off mountains or<br />
those injured on oil rigs or out at<br />
sea.<br />
AMBULANCE <strong>UK</strong> - OCTOBER<br />
The helipad will also be used by<br />
the Children’s Air <strong>Ambulance</strong>,<br />
which can fly specialist medical<br />
teams into Hull to treat seriously<br />
ill children as well as fly children<br />
from here to hospital with<br />
specialist paediatric services.<br />
To support the HELP Appeal<br />
please call the donation helpline<br />
on 0800 389 8999 or text HPAD22<br />
plus the amount and send to<br />
70070.<br />
154<br />
For further recruitment vacancies visit: www.ambulanceukonline.com
NEWSLINE<br />
The event dedicated to transforming<br />
our emergency services<br />
Be part of The Emergency Services Show 2021 to demonstrate what the future<br />
holds for the emergency services industry. Sell to the buyers and specifiers at the<br />
<strong>UK</strong>’s leading annual showcase of the blue light sector.<br />
> 10,000+<br />
VISITORS<br />
Use The Emergency Services Show to:<br />
> Meet buyers and specifiers of equipment<br />
and services<br />
> Network with the market<br />
> Launch new products<br />
> Maintain your brand awareness<br />
> Keep ahead of your competitors<br />
> Collaborate with other suppliers<br />
and services<br />
> Raise your profile in the industry<br />
> 450+<br />
LEADING SUPPLIERS<br />
> 15th<br />
SHOW<br />
Meet visitors with active buying requirements for:<br />
> Fire safety equipment<br />
> Medical and first aid<br />
> PPE, protective clothing and uniforms<br />
> Training and training equipment<br />
> Vehicles and ancillary kit<br />
> ICT<br />
> Road safety services and kit<br />
> Infection control<br />
> Control rooms<br />
> Facilities<br />
> Health & safety<br />
> Emergency planning/resilience<br />
> Recruitment<br />
NEW FOR 2021<br />
“<br />
It’s the best show that I can recall<br />
coming to. There’s a buzz about<br />
the show and a lot of energy.<br />
The quality of the people who have<br />
come and who are genuinely<br />
interested in what we are doing,<br />
we can offer them a genuine benefit.<br />
It’s been a real roaring success.<br />
Colin Hanna, Head of National Sales,<br />
St John <strong>Ambulance</strong><br />
GET INVOLVED NOW WWW.EMERGENCY<strong>UK</strong>.COM<br />
”<br />
AMBULANCE <strong>UK</strong> - OCTOBER<br />
Do you have anything you would like to add or include in Newsline? Please contact us and let us know.<br />
155
NEWSLINE<br />
LAS<br />
Service introduces<br />
new measures<br />
to help lead to<br />
tougher staff assault<br />
sentences<br />
We have recruited two Violence<br />
Reduction Officers as part of our<br />
ongoing work to protect staff.<br />
The officers will work closely with<br />
the Met Police as they support<br />
victims who want to take their<br />
cases to court.<br />
Louise Murray is one of the new<br />
Violence Reduction Officers and<br />
also works as an emergency<br />
medical technician out of Bromley<br />
<strong>Ambulance</strong> Station.<br />
She said: “Aggression against our<br />
staff can leave them in fear, it can<br />
lead to PTSD and cause all sorts<br />
of mental health problems.<br />
“I’ve seen the increase in assaults<br />
and know the impact it can have –<br />
I’ve been assaulted myself. That’s<br />
why I’m so passionate about<br />
what we are doing – making sure<br />
people have the support they<br />
need and also getting as much<br />
evidence as we can so we can<br />
push for prosecutions.”<br />
“We will do everything to support<br />
someone who has been attacked<br />
and that includes trying to ensure<br />
the attacker is prosecuted.”<br />
<strong>Ambulance</strong> crews in London were<br />
physically attacked 59 times in<br />
August alone.<br />
New figures from the Service<br />
show assaults dropped during<br />
March and April but as lockdown<br />
restrictions began easing,<br />
physical abuse has been on<br />
the rise with an average of two<br />
attacks a day.<br />
There have been 260 violent<br />
incidents since April – usually<br />
patients or their families attacking<br />
the ambulance crews who are<br />
there to help.<br />
Attacks include kicking, punching,<br />
head-butting and biting and there<br />
have also been nine assaults with<br />
weapons.<br />
There were 625 reported physical<br />
attacks last year and a further<br />
713 non-physical assaults, which<br />
include threats and verbal abuse.<br />
Managers fear the true scale of<br />
the problem could be worse as<br />
incidents are often not reported –<br />
despite a campaign to encourage<br />
staff to report all abuse.<br />
Chief Executive Garrett Emmerson<br />
said: “Protecting our people and<br />
ensuring they are safe while they<br />
are working is a highest priority.<br />
“Our crews and call handlers<br />
have made huge sacrifices to<br />
care for patients with courage<br />
and compassion – it is absolutely<br />
disgusting for them to be attacked<br />
while doing so and should not be<br />
seen as something which goes<br />
with the job.<br />
“We will push for the prosecution<br />
of anyone who attacks our staff.”<br />
saying exactly where you are can<br />
be challenging. Emergencies<br />
can happen anywhere, from<br />
Northumberland countryside to<br />
heritage North East beaches;<br />
these all present a challenge to<br />
locate patients in rural areas for<br />
NEAS.<br />
Explaining where you are can<br />
be difficult over the phone and<br />
landmark-based descriptions<br />
are prone to errors and GPS<br />
coordinates are long and difficult<br />
to communicate. Finding your<br />
location quickly can mean the<br />
difference between life and<br />
death in some cases. In winter<br />
especially, if you are not found<br />
quick enough outside you can<br />
suffer from hypothermia, which is<br />
a series condition when your body<br />
temperature drops dangerously<br />
low.<br />
The what3words platform has<br />
AMBULANCE <strong>UK</strong> - OCTOBER<br />
Violence Reduction Officer Louise<br />
Violence Reduction Officer Andrew<br />
NEAS<br />
3 words can save<br />
lives<br />
The North East <strong>Ambulance</strong><br />
Service (NEAS) has invested<br />
in new technology to increase<br />
its response time to patients in<br />
hard to reach locations.<br />
‘Where’s the emergency?’ is<br />
one of the first questions you<br />
are asked when calling 999 but<br />
divided coordinates of the world<br />
into a grid of 3m x 3m squares. It<br />
has given each square a unique<br />
combination of three words - a<br />
what3words address, which will<br />
take you to a precise location.<br />
After it was used successfully<br />
used elsewhere in the region<br />
by neighbouring emergency<br />
services, NEAS now joins over 90<br />
emergency services across Great<br />
Britain who are doing the same.<br />
156<br />
For more news visit: www.ambulanceukonline.com
NEWSLINE<br />
The new app has been<br />
streamlined within the ambulance<br />
service’s Emergency Operations<br />
Centre by integrating the platform<br />
into its system where emergency<br />
calls are taken. Once the three<br />
words have been provided to the<br />
call handler, they will then input<br />
these into the app and track your<br />
location. Emergency help can<br />
then be directed to you.<br />
Systems and resilience dispatch<br />
officer Mark Hagan has been the<br />
lead for NEAS on installing the<br />
what3words app into its system.<br />
He said, “A 999 call could be<br />
one of the worst times of your<br />
life. You might be on your own in<br />
immediate danger, possibly in a<br />
lot of pain or feeling very unwell.<br />
It’s the job of our health advisors<br />
to find where you are as quickly<br />
as possible. As every minute is<br />
delayed getting our frontline crew<br />
to you, the more your condition<br />
will deteriorate.<br />
“It is often assumed that our<br />
call handlers know your location<br />
based on phone signals, but they<br />
don’t and it can be very stressful<br />
at times trying to find the location<br />
of a patient who needs urgent<br />
help.<br />
“Before the new technology, we<br />
relied on people trying to identify<br />
landmarks, shops or junctions<br />
and this often proved difficult. If<br />
people were from outside of the<br />
area this was an added challenge<br />
as they weren’t familiar with where<br />
they were.<br />
“In the week we have been using<br />
what3words, it has been used five<br />
times so far to locate patients and<br />
we anticipate it will be used more<br />
frequently.<br />
“We also rely on resources from<br />
neighbouring partners such as the<br />
Coastguard and Mountain Rescue<br />
Service to locate a patient, but<br />
this app will really cut down on<br />
the time it will take to respond to<br />
patients and potentially save more<br />
lives.”<br />
The app is free to download for<br />
both iOS and Android and works<br />
entirely offline – making it ideal for<br />
use in areas of the <strong>UK</strong>, even with<br />
an unreliable data connection.<br />
What3words can also be used via<br />
the online map at:<br />
https://what3words.com and<br />
the technology is available in over<br />
40 languages, as well as being<br />
accessible anywhere in the world.<br />
Remember, if you are in an<br />
emergency and unable to tell the<br />
call handler of your exact location,<br />
follow these instructions on how<br />
to use what3words:<br />
1. Find the three-word address<br />
for your current location on the<br />
what3words app.<br />
2. Share your three-word address<br />
over the phone to the call<br />
handler.<br />
3. The emergency service can<br />
then coordinate a response<br />
directly to the exact location<br />
where help is needed.<br />
From horse riders, kayakers and<br />
rural walkers to mountain bikers,<br />
car crashes and sailors; the list<br />
is endless for reasons why you<br />
should download the what3words<br />
app as you never know when you<br />
might be in an emergency and it<br />
might just save your life.<br />
SECAMB<br />
Trust appoints new<br />
Non-Executive<br />
Director<br />
1 <strong>October</strong>, subject to the usual<br />
employment checks.<br />
Tom is a passionate supporter of<br />
the NHS. A nurse, he has spent<br />
four decades in healthcare and<br />
has experience in both hospital<br />
and pre-hospital care. Now a<br />
senior academic the majority<br />
of his research has focused on<br />
improving outcomes for patients<br />
under ambulance care.<br />
Tom has a long-standing<br />
relationship with SECAmb and<br />
has previously served as a<br />
SECAmb governor while at the<br />
University of Surrey. He holds a<br />
number of volunteer roles locally<br />
including being Clinical Director<br />
of HeartStart Farnham Lions and<br />
nationally as a Trustee of British<br />
Association for Immediate Care.<br />
He is a Fellow of the Royal<br />
College of Nursing, European<br />
Society of Cardiology, American<br />
Heart Association and American<br />
College of Cardiology. His<br />
contribution to patient care was<br />
recognised in 2019 by election as<br />
an honorary Fellow of the College<br />
of Paramedics.<br />
SECAmb Chairman, David Astley<br />
said: “I am pleased we have<br />
been able to appoint Tom and I<br />
look forward to working closely<br />
with him. I know SECAmb will<br />
benefit from his extensive clinical<br />
experience and his long-standing<br />
relationship with the Trust and<br />
other local partners.”<br />
Tom added: “As a patient I have<br />
South East Coast <strong>Ambulance</strong><br />
Service NHS Foundation<br />
Trust (SECAmb) is pleased to<br />
announce the appointment of a<br />
new Non-Executive Director.<br />
The Trust’s Council of Governors<br />
recently passed a resolution to<br />
appoint Professor Tom Quinn to<br />
the role. Tom, who works at St<br />
George’s, University of London<br />
and Kingston University, will begin<br />
a three-year term of office on<br />
first-hand experienced calling<br />
999, receiving expert care from<br />
call handlers and the ambulance<br />
crew who came to my aid. This<br />
interaction confirmed the highly<br />
professional and compassionate<br />
care which I already knew<br />
SECAmb delivered day-in, dayout.<br />
I am looking forward to taking<br />
up this new role and working<br />
with everyone across the whole<br />
organisation for the benefit of<br />
patients.”<br />
AMBULANCE <strong>UK</strong> - OCTOBER<br />
For the latest <strong>Ambulance</strong> Service News visit: www.ambulancenewsdesk.com<br />
157
NEWSLINE<br />
AMBULANCE <strong>UK</strong> - OCTOBER<br />
Health Scholars<br />
and the American<br />
Academy of<br />
Pediatrics Partner<br />
to Develop Pediatric<br />
Emergency Virtual<br />
Reality (VR)<br />
Simulation Training<br />
for First Responders<br />
The new VR applications will<br />
provide a remote, scalable<br />
way for first responders to<br />
practice properly assessing<br />
and providing care during a<br />
pediatric emergency.<br />
Health Scholars, the company<br />
recognized for voice-directed VR<br />
simulations including advanced<br />
cardiovascular life support (ACLS)<br />
training for first responders and<br />
clinicians, and the American<br />
Academy of Pediatrics (AAP),<br />
the 67,000-member organization<br />
dedicated to the optimal health<br />
and well-being for all infants,<br />
children, adolescents and young<br />
adults, are pleased to announce<br />
a partnership to co-develop VR<br />
training applications to equip<br />
first responders with skills vital to<br />
assessing and treating pediatric<br />
medical emergencies.<br />
“Health Scholars is proud to<br />
partner with AAP to bring a truly<br />
meaningful innovation to market,”<br />
noted Cole Sandau, CEO, Health<br />
Scholars. “The partnership will<br />
provide highly differentiated<br />
training to help first responders<br />
better prepare for pediatric<br />
emergency situations.”<br />
The goal of the partnership is to<br />
leverage VR technology to deliver<br />
more active and impactful training<br />
opportunities for first responders.<br />
As a result, EMS providers will<br />
have the first-ever capability to<br />
continuously train on real-to-life<br />
pediatric emergency encounters<br />
using deliberate practice. The use<br />
of VR makes rich, experiencebased<br />
training highly accessible<br />
to all first responders in a low<br />
cost/high yield model. “During the<br />
time of COVID, we need to design<br />
innovative educational methods<br />
that deliver critical content and<br />
skills, while recognizing that<br />
in-person training is not always<br />
feasible,” said AAP member<br />
Sarah Denny, MD, FAAP who<br />
reviewed and provided feedback<br />
to the VR scenarios. “Through this<br />
collaboration, EMS professionals<br />
can participate in distance<br />
learning using virtual reality and<br />
simulation to practice the critical<br />
hands-on skills that are necessary<br />
to treat pediatric emergencies in<br />
the field.”<br />
The two co-developed VR<br />
applications, “Pediatric<br />
Emergency Assessment” and<br />
“Pediatric Emergency Care,” are<br />
the first VR simulations dedicated<br />
to pediatric emergencies for EMS<br />
professionals. Recognizing severe<br />
illness in infants and children<br />
is challenging, and it’s further<br />
compounded by limited exposure<br />
to pediatric emergencies.<br />
Unless providers are practicing<br />
frequently, the nuanced critical<br />
skill sets needed to effectively<br />
treat infants and children decline<br />
over time, leading to significant<br />
readiness challenges.<br />
AAP and Health Scholars<br />
recognized a substantive<br />
gap in preparing for pediatric<br />
emergencies and see VR as<br />
a solution for increasing the<br />
frequency of training in realto-life<br />
scenarios. The new<br />
applications represent an<br />
industry breakthrough in using<br />
converged VR technologies<br />
to address critical outcomes.<br />
The applications use artificial<br />
intelligence (AI-enabled) voice<br />
technology to replicate real-world<br />
interaction and to create highly<br />
sophisticated, self-directed<br />
learning experiences that adapt<br />
to the providers’ proficiency<br />
level to optimize learning gains.<br />
This innovative approach to<br />
learner assessment captures<br />
rich information about individual<br />
learner competencies and the<br />
overall readiness of departments<br />
or regional/national organizations.<br />
The combination of all these<br />
elements creates one of the most<br />
sophisticated and consequential<br />
training platforms in the market.<br />
“Limited exposure to severely<br />
ill infants and children in the<br />
prehospital setting presents a<br />
challenge in terms of training.<br />
Providers need continuous<br />
deliberate practice for pediatric<br />
emergencies in order to maintain<br />
readiness for the subtle symptoms<br />
which severely ill infants and<br />
children often manifest and to<br />
promptly initiate high-quality<br />
resuscitative care. VR enables the<br />
delivery of this training to large<br />
learner populations,” said Brian<br />
Gillett, President & Chief Medical<br />
Officer, Health Scholars.<br />
“Pediatric Emergency<br />
Assessment” is available for<br />
immediate use, and “Pediatric<br />
Emergency Care” is available for<br />
pre-sale. For more information,<br />
visit https://healthscholars.com/<br />
solutions/first-responders/<br />
About Health Scholars<br />
Our mission is to advance<br />
healthcare education through<br />
virtualization, making experiencebased<br />
training scalable,<br />
accessible and affordable to<br />
both Healthcare and Public<br />
Safety providers. Our VR platform<br />
provides management, delivery<br />
and performance analysis<br />
of VR training and our AIenabled<br />
VR simulations deliver<br />
scenarios for resuscitation,<br />
perioperative, obstetrical, and<br />
public emergencies, providing<br />
a risk-free environment for<br />
repeated deliberate practice.<br />
For more information, visit www.<br />
HealthScholars.com.<br />
About the American Academy of<br />
Pediatrics<br />
The American Academy of<br />
Pediatrics is an organization of<br />
67,000 primary care pediatricians,<br />
pediatric medical subspecialists<br />
and pediatric surgical specialists<br />
dedicated to the optimal health<br />
and well-being for all infants,<br />
children, adolescents and young<br />
adults. For more information, visit<br />
www.aap.org.<br />
NEAS<br />
Supporting BAME<br />
communities thanks<br />
to NHS Charities<br />
Together donation<br />
North East <strong>Ambulance</strong> Service<br />
has received a grant of £50,000<br />
from NHS Charities Together to<br />
progress its work with Black,<br />
Asian and minority ethnic<br />
(BAME) communities and<br />
develop initiatives to support<br />
BAME staff in the workplace.<br />
The money will be used to support<br />
a community positive action officer<br />
to raise awareness of the services<br />
we provide and how to access<br />
them. The officer will also help to<br />
set up a community ambassador<br />
scheme working with local BAME<br />
community organisations and<br />
individuals and promote ourselves<br />
as an inclusive employer.<br />
Money for some smaller scale<br />
projects to improve BAME employee<br />
experience in the workplace is also<br />
included in this grant.<br />
Karen O’Brien, director of people<br />
and development, said “This<br />
money will be used to fund a post<br />
to improve our engagement with<br />
BAME people in the region.<br />
“This is especially important at<br />
this time due to the increased risk<br />
of COVID on BAME communities.<br />
It is important we improve our<br />
engagement and communication<br />
and it also gives us an opportunity<br />
to promote the many employment<br />
and volunteering opportunities<br />
available in the Trust.”<br />
158<br />
For more news visit: www.ambulanceukonline.com
NEWSLINE<br />
EEAST<br />
East of England<br />
<strong>Ambulance</strong> Service<br />
celebrate graduation<br />
of first apprentices<br />
The East of England<br />
<strong>Ambulance</strong> Service (EEAST) is<br />
celebrating after its first group<br />
of apprentices passed their<br />
courses to become qualified<br />
emergency medical technicians.<br />
A national programme, the level 4<br />
associate ambulance practitioner<br />
apprenticeship offers an<br />
innovative way to gain a higherlevel<br />
qualification in emergency<br />
care by combining a full-time job<br />
with study. Apprentices benefit<br />
from earning whilst they study and<br />
having their fees paid for by the<br />
Trust.<br />
The four apprentices – Sarah<br />
Batchelor, Sam Eaton, Mark Jones<br />
and Sarah Pym – passed their<br />
apprenticeship in August and will<br />
now go on to work as emergency<br />
medical technicians as part of<br />
a two-person ambulance crew<br />
responding to emergency (999)<br />
and urgent calls.<br />
required to achieve a level 3<br />
award in emergency response<br />
driving and a level 4 associate<br />
ambulance practitioner (QCF)<br />
diploma.<br />
The apprenticeship opens the<br />
door to higher education and the<br />
opportunity to gain paramedic<br />
qualifications. An apprenticeship<br />
pathway to become a paramedic<br />
is set to be introduced at EEAST<br />
next year, with all four newly<br />
qualified emergency medical<br />
technicians interested in following<br />
that route.<br />
Mark Stead, education manager<br />
at EEAST, said: “We are delighted<br />
to have our first four apprentices<br />
successfully complete their<br />
end point assessment. The<br />
four apprentices have worked<br />
incredibly hard and their<br />
dedication has been recognised<br />
with two merits and two distinction<br />
grades being awarded.<br />
“Many congratulations to Sarah,<br />
Sam, Mark and Sarah and<br />
to everyone in the Trust who<br />
supported them on their learning<br />
journey. We wish them a long and<br />
successful career at the East of<br />
England <strong>Ambulance</strong> Service.”<br />
been with EEAST for four years<br />
and took up the apprenticeship to<br />
progress his career.<br />
“I jumped at the chance of the<br />
apprenticeship to further my<br />
career with the ambulance service<br />
and see it as a stepping stone to<br />
becoming a paramedic,” he said.<br />
“I would say that dedication and<br />
a willingness to learn is crucial to<br />
completing the course, as there is<br />
lot to take in, but there is extensive<br />
support to help you throughout.”<br />
Sarah Pym, 42, was a support<br />
teacher at a SEN (special<br />
educational needs) school before<br />
starting the apprenticeship and<br />
is based at Harlow <strong>Ambulance</strong><br />
Station.<br />
She said: “I learnt so much in<br />
a short space of time in the<br />
apprenticeship programme and<br />
the support we received from<br />
Kevin Cowan [training centre<br />
and quality assurance manager<br />
at Welwyn Garden City] and the<br />
tutors was amazing. I had such a<br />
positive experience from training<br />
to operations and am glad I took<br />
the opportunity to change my<br />
career.<br />
“I have been<br />
interested in<br />
working for<br />
the ambulance<br />
service for<br />
a long time,<br />
but I wasn’t<br />
in a position<br />
to pursue it<br />
until I saw the<br />
advert for the<br />
apprenticeship.”<br />
a paramedic and longer term,<br />
given my background in teaching,<br />
would like to be involved in<br />
training.”<br />
Sam Eaton, 29, who works out of<br />
Potters Bar <strong>Ambulance</strong> Station,<br />
said: “The tutors were excellent<br />
in guiding us through the course<br />
and I would definitely recommend<br />
the apprenticeship to people<br />
looking to further their career with<br />
the ambulance service.”<br />
The course takes 18 months to<br />
complete, with the apprentices<br />
Mark Jones, 25, who is based at<br />
Thurrock <strong>Ambulance</strong> Station, has<br />
“In the future I would like to<br />
undertake the training to become<br />
Sarah Batchelor, 46, who works<br />
out of Huntingdon <strong>Ambulance</strong><br />
Station, said: “I have been<br />
interested in working for the<br />
ambulance service for a long<br />
time, but I wasn’t in a position to<br />
pursue it until I saw the advert for<br />
the apprenticeship.<br />
From left to right: Sarah Batchelor (top), Sam Eaton, Sarah Pym and Mark Jones<br />
“As someone who has come<br />
back to the classroom after an<br />
absence, the course was a bit of<br />
a shock to the system to start off<br />
with but everyone at the training<br />
centre was so supportive and it<br />
was a positive experience.”<br />
If you would like to find out<br />
more about becoming an<br />
apprentice at East of England<br />
<strong>Ambulance</strong> Service, please email<br />
apprenticeships@eastamb.nhs.uk<br />
AMBULANCE <strong>UK</strong> - OCTOBER<br />
For the latest <strong>Ambulance</strong> Service News visit: www.ambulancenewsdesk.com<br />
159
NEWSLINE<br />
AMBULANCE <strong>UK</strong> - OCTOBER<br />
SECAMB<br />
New combined<br />
ambulance and 111<br />
centre for Medway<br />
given planning go<br />
ahead<br />
Plans to develop a new multipurpose<br />
ambulance centre in<br />
Gillingham have been given the<br />
green light by planners.<br />
In a first for South East Coast<br />
<strong>Ambulance</strong> Service NHS<br />
Foundation Trust, (SECAmb), the<br />
development at Bredgar Road<br />
would comprise of a new Make<br />
Ready Centre for the Medway<br />
region, as well as 999 and NHS<br />
111 operations centres relocated<br />
from Coxheath and Ashford in<br />
Kent respectively.<br />
Following the approval by Medway<br />
Council planners, and subject to<br />
full business case approval from<br />
SECAmb’s Trust Board, building<br />
work is expected to begin at the<br />
site early next year ahead of it<br />
becoming fully operational in 2022.<br />
The development will be funded<br />
with a previously announced £6.52<br />
million of government capital<br />
funding.<br />
The Trust’s Make Ready system,<br />
which is already in place across<br />
much of SECAmb’s region, is a<br />
vehicle preparation system which<br />
sees specialist teams of staff<br />
employed to clean, restock and<br />
maintain the Trust’s fleet.<br />
<strong>Ambulance</strong> crews currently starting<br />
and ending their shifts at Medway<br />
and Sittingbourne ambulance<br />
stations will, instead, start and<br />
finish at the new centre. They will<br />
then respond from ambulance<br />
community response posts across<br />
the region with suitable rest<br />
facilities for crews between calls<br />
and when on a break.<br />
Staff based in Sheppey will<br />
continue to start and end their<br />
shifts from the ambulance station<br />
on the island which is currently<br />
undergoing a major refurbishment<br />
and upgrade to provide new<br />
educational and training facilities.<br />
The plans would see the new<br />
Make Ready facility in Gillingham<br />
housed on the two lower floors of<br />
the new centre while staff currently<br />
based at the Trust’s East 999<br />
Emergency Operations Centre<br />
(EOC) in Coxheath will benefit<br />
from a modern open plan office<br />
above. The Trust’s NHS 111 staff,<br />
currently based in Ashford, Kent,<br />
will occupy the top floor.<br />
Bringing the 999 and 111<br />
services under one roof will<br />
allow for greater support for<br />
each service, with the modern<br />
facilities matching the Trust’s West<br />
Emergency Operations Centre,<br />
based in Crawley, which opened<br />
in 2017, and reflects the ambitions<br />
of the Trust to deliver new<br />
integrated urgent care services<br />
over a wider area.<br />
Having both of these services<br />
housed in the same building will<br />
facilitate greater sharing of best<br />
practice and, where feasible,<br />
will enable the Trust to optimise<br />
functions between the two.<br />
An integrated region-wide<br />
approach will provide clearer<br />
pathways for patients and a more<br />
efficient and resilient emergency<br />
and urgent care response service.<br />
The development also provides<br />
SECAmb with greater capacity,<br />
allows it to improve the ratio of<br />
999 call taking across its two<br />
Emergency Operations Centres<br />
and will bring local recruitment<br />
opportunities for people across<br />
both 999 and 111 services.<br />
SECAmb currently operates eight<br />
Make Ready Centres across its<br />
region with the latest set to open<br />
in Brighton in the coming months.<br />
SECAmb Associate Director of<br />
Contact Centres and Integrated<br />
Care, John J O’Sullivan said:<br />
“I’m really pleased the project<br />
has been given the go-ahead by<br />
planners. Our current Emergency<br />
Operations Centre for the East<br />
of our region is outdated, lacks<br />
space and is no longer fit for<br />
purpose. In addition, bringing our<br />
999 and 111 operations under<br />
one roof provides us with greater<br />
resilience and enables the two<br />
services to work more closely<br />
together to benefit patients across<br />
our whole region.”<br />
SECAmb Operating Unit Manager<br />
for Dartford & Medway, Will<br />
Bellamy added: “This latest<br />
stage in the roll-out of our Make<br />
Ready system is an important<br />
step in the development of the<br />
service we are able to provide<br />
our patients locally. The system<br />
is more efficient and also means<br />
ambulance crews have access<br />
to improved modern facilities for<br />
training.<br />
“We understand that changes like<br />
this have an impact on staff and<br />
we will fully engage with all those<br />
the development affects ahead of<br />
go live in 2022.”<br />
What is Make Ready?<br />
• The Make Ready initiative<br />
significantly enhances and<br />
improves the service SECAmb<br />
provides to the community.<br />
• It minimises the risk of crossinfection,<br />
frees up front-line<br />
staff - who traditionally cleaned<br />
and re-stocked ambulances<br />
- to spend more time treating<br />
patients, and keeps vehicles on<br />
the road for longer.<br />
• The initiative ensures that<br />
specially-trained operatives<br />
regularly deep-clean, restock<br />
and check vehicles for<br />
mechanical faults.<br />
• Make Ready Centres are<br />
supported by a network<br />
of <strong>Ambulance</strong> Community<br />
Responses Posts (ACRPs)<br />
across the area with staff<br />
beginning and ending their<br />
shifts at the new centre.<br />
• During their shifts, staff will<br />
respond from the ACRPs which<br />
will provide facilities for staff.<br />
These are located based on<br />
patient demand.<br />
• Crews continue to respond<br />
from the same towns under the<br />
system but begin and end their<br />
shifts at staggered times with a<br />
vehicle that is fully prepared for<br />
them.<br />
• The system ensures crews have<br />
access to improved training<br />
facilities and opportunities<br />
and increased support from<br />
managers.<br />
NHS hospital<br />
helipads see 15,500<br />
landings<br />
The HELP Appeal, which<br />
improves helicopter emergency<br />
medical services (HEMS) by<br />
funding the construction of<br />
new or upgraded hospital and<br />
air ambulance helipads, has<br />
announced there have been<br />
15,500 landings on the NHS<br />
hospital helipads it has funded<br />
across the country.<br />
Since the charity’s creation in<br />
2009, it has donated £20 million<br />
towards 39 new or upgraded<br />
helipads, of which 32 have been<br />
NHS hospital helipads - including<br />
17 based at Major Trauma<br />
Centres - and six air ambulance<br />
helipads. The cost of planned<br />
helipad projects equates to<br />
£50.75 million so far.<br />
This year alone, despite the<br />
pandemic, new helipads funded<br />
by the charity opened at the Royal<br />
Devon and Exeter Hospital, Hull<br />
Royal Infirmary and Hereford<br />
County Hospital.<br />
160<br />
For further recruitment vacancies visit: www.ambulanceukonline.com
NEWSLINE<br />
New helipads at the Royal Sussex<br />
County Hospital, Brighton;<br />
Manchester University NHS<br />
Foundation Trust; Airedale<br />
General Hospital, Keighley;<br />
Campbeltown Hospital, Worcester<br />
Hospital, Luton & Dunstable<br />
Hospital and Sheffield Children’s<br />
Hospital are planned to open<br />
within the next year or two.<br />
The charity is also currently<br />
funding improvements to existing<br />
helipads at University Hospital<br />
Coventry; University Hospital<br />
Crosshouse, Kilmarnock; Carlise<br />
Hospital, and Peterborough City<br />
Hospital, which will open this year.<br />
The HELP Appeal expanded into<br />
Scotland in 2015, to fund nine<br />
hospital helipads including the<br />
Queen Elizabeth University Hospital<br />
in Glasgow and Edinburgh Royal<br />
Infirmary, and Raigmore Hospital,<br />
Inverness with another three in the<br />
pipeline. It also provided £200,000<br />
over a four-year period to the<br />
Scottish Air <strong>Ambulance</strong> Service<br />
to fund replacement secondary<br />
landing sites throughout Scotland.<br />
The charity pioneered the<br />
introduction and funding of Deck<br />
Integrated Fire Fighting System<br />
(DIFFS) on five rooftop helipads<br />
across the country including<br />
King’s College Hospital and St<br />
George’s hospital, with three more<br />
planned, which save each NHS<br />
hospital around £250,000 every<br />
year in firefighting costs.<br />
It has also funded helipads at<br />
brand new air bases for several<br />
air ambulances, including the<br />
Scotland’s Charity Air <strong>Ambulance</strong>;<br />
Midlands Air <strong>Ambulance</strong> Charity;<br />
Wiltshire Air <strong>Ambulance</strong>; Great<br />
Western Air <strong>Ambulance</strong>; Kent,<br />
Surrey & Sussex Air <strong>Ambulance</strong><br />
and London Air <strong>Ambulance</strong>; and<br />
is funding helipads for Lincs &<br />
Notts Air <strong>Ambulance</strong> in <strong>2020</strong> and<br />
Great North Air <strong>Ambulance</strong>.<br />
The HELP Appeal also funded<br />
lifesaving equipment for the<br />
Midlands Air <strong>Ambulance</strong> Charity<br />
(MAAC) and two Critical Care<br />
Cars in partnership with MAAC,<br />
with a third car launching in <strong>2020</strong>.<br />
It has also provided life-saving<br />
funding for the British Association<br />
for Immediate Care (BASICS)<br />
annually since 2019.<br />
Robert Bertram, Chief Executive<br />
of the HELP Appeal says: “Over<br />
10 years ago, hospital helipad<br />
facilities were severely lacking,<br />
yet finance for hospitals was tight.<br />
There was little doubt that if we<br />
didn’t offer non-repayable funds<br />
towards the cost of helipads,<br />
hospitals would struggle to ever<br />
have one, despite emergency<br />
medics saying they were<br />
desperately needed to save time<br />
and save lives.<br />
“Today, finance for hospitals<br />
remains tight, but the demand<br />
for our helipad grants continues<br />
to grow and we are recognised<br />
as the only charity in the country<br />
dedicated to funding hospital<br />
helipads.”<br />
Of the 15,500 landings, critically ill<br />
patients like 12-year-old George<br />
are alive and recovering well from<br />
their illness or injury, because<br />
the helipads they landed on<br />
were built beside the Emergency<br />
Department.<br />
George’s story<br />
George, who is 12 years old, was<br />
walking to school when he was<br />
hit by a motorbike at speed. He<br />
was flown to St George’s hospital<br />
helipad in 22 mins from Ashford in<br />
Surrey, a journey that would have<br />
taken one hour by road.<br />
Caroline, George’s mother, was<br />
at home when she received the<br />
news. She said: “George and I<br />
always walked to school together.<br />
This was the first time that he was<br />
going off by himself.<br />
“I was just waiting for my boys to<br />
come home, when I got a knock<br />
on the door. The lady said to<br />
me, your son has been in a road<br />
accident. As I walked round, I was<br />
so shocked. The road had been<br />
closed off, there were three police<br />
cars, an ambulance and George<br />
was in the middle of the road.”<br />
“When I went up to him at the<br />
scene, I didn’t know what to say<br />
to him. At the roadside, I just felt<br />
so guilty that he was on his own<br />
when this had happened to him.”<br />
HEMS doctor Sarah was at the<br />
scene: “If a fracture is open, like<br />
George’s was, that means that<br />
there’s also damage to the skin.<br />
If the fracture is displaced the<br />
bone may be facing in the wrong<br />
direction, which may affect blood<br />
supply, cause nerve damage and<br />
could be a lymph threatening<br />
injury.<br />
“It’s really important to reduce<br />
that risk, by putting it back into the<br />
position it was in before it broke.<br />
What we can provide is good<br />
pain relief, immediate reduction<br />
and emergency interventions, but<br />
what the patient actually needs<br />
is an orthopaedic surgeon and a<br />
theatre and it’s important we get<br />
the patient to this as quickly as<br />
possible. “<br />
This is why George was flown<br />
directly to St George’s hospital<br />
helipad which has immediate<br />
access to the Emergency<br />
Department.<br />
Caroline adds: “The helipad’s<br />
location made the process of<br />
getting to A&E as stress free as<br />
possible. This was important<br />
as it was a very stressful time<br />
for us. The alternative of landing<br />
anywhere else and being<br />
transported to hospital by vehicle<br />
would have taken longer and<br />
added to the strain.”<br />
St George’s orthopaedic registrar<br />
explains the danger behind<br />
George breaking his tibia (shin<br />
bone): “Children’s veins are<br />
different from adult’s veins. They<br />
have a weak spot and that’s the<br />
growth plate and it’s particularly<br />
vulnerable to injury. If the growth<br />
plate is damaged too much,<br />
the vein in that region will stop<br />
growing all together. This can<br />
result in lifelong disablement.”<br />
Caroline also adds: “With<br />
regards to George’s treatment<br />
the consultant said that it was<br />
important to get George to theatre<br />
as soon as possible.”<br />
Fortunately, surgeons were able<br />
to perform emergency surgery on<br />
George to repair his growth plate.<br />
He stayed in for two more nights<br />
as he was in a lot of pain and<br />
Caroline stayed by his side the<br />
whole time.<br />
Three months after the accident<br />
George says: “My legs feel<br />
good at the moment. It just felt<br />
good to start walking again. My<br />
mum is probably one of the most<br />
important people to me and I love<br />
her so much.”<br />
Caroline adds: “George has<br />
recovered well and is back to<br />
normal. The doctors are seeing<br />
him every six months to check for<br />
any growth plate issues.<br />
“Thank you to the air ambulance<br />
service for their help and support.<br />
He received first class treatment<br />
and for that we are extremely<br />
appreciative.<br />
“Also, having the helipad at<br />
the hospital made it possible<br />
for George to receive the best<br />
treatment in the quickest time<br />
possible. We will truly be forever<br />
grateful for this.”<br />
AMBULANCE <strong>UK</strong> - OCTOBER<br />
Do you have anything you would like to add or include in Newsline? Please contact us and let us know.<br />
161
NEWSLINE<br />
SECAMB<br />
Joint police and<br />
ambulance response<br />
service proving<br />
successful in Brighton<br />
Meet the police and ambulance<br />
Joint Response Unit (JRU)<br />
vehicle team which has been<br />
patrolling and responding to<br />
incidents in Brighton and Hove.<br />
National<br />
resuscitation<br />
organisation updates<br />
process to support<br />
conversations about<br />
an individual’s<br />
care and realistic<br />
treatment choices in<br />
a future emergency<br />
AMBULANCE <strong>UK</strong> - OCTOBER<br />
The vehicle which is staffed by<br />
Sussex Police and South East<br />
Coast <strong>Ambulance</strong> (SECAmb)<br />
allows a response police officer<br />
and a paramedic to work together<br />
to respond to incidents which<br />
require both services.<br />
The SECAmb vehicle, is kitted<br />
out with everything police<br />
need to tackle crime and<br />
medical equipment required by<br />
paramedics.<br />
Police officers working on the<br />
unit receive medical technique<br />
familiarisation and paramedics<br />
benefit from an input on conflict<br />
resolution.<br />
Assaults, collision and alcoholrelated<br />
incidents are the most<br />
common calls the JRU gets.<br />
The unit was started as a trial<br />
project in December 2019 and<br />
runs on Friday and Saturday<br />
twilight shifts from 6pm to 2am to<br />
meet the demands of the night<br />
time economy in the city.<br />
Both police and ambulance<br />
control are aware of the JRU and<br />
will actively seek to deploy the<br />
JRU to incidents that require a<br />
response from both services.<br />
Inspector Steve Hill said:<br />
“The Joint Response Unit is a<br />
worthwhile initiative which involves<br />
police officers and paramedics<br />
travelling together to incidents<br />
which may require both areas<br />
of expertise, resulting in a more<br />
effective and efficient service.<br />
“For example if there has been a<br />
fight and an arrested suspect has<br />
an injury, the medic could treat<br />
them then and there negating<br />
the need for officer to go and<br />
wait with them at hospital or call<br />
a double crewed ambulance.<br />
A cause for concern call could<br />
allow the officer to force entry<br />
to a premises to check and<br />
should a person be located there<br />
needing help, the medic is well<br />
placed to do so. Road collisions<br />
with injury are also an obvious<br />
incident where both services will<br />
be required.<br />
“The JRU also retains the ability<br />
to ‘self-deploy’ to an incident<br />
be it medical or police that they<br />
feel they could readily assist<br />
with. They can be proactively<br />
doing directed patrol activities,<br />
searching for missing people and<br />
if they are the closest unit to a<br />
category 1 medical emergency or<br />
a police assistance call they will<br />
attend.<br />
The unit has been responding<br />
to five or six incidents per shift<br />
and even during the Covid-19<br />
lockdown when the night time<br />
economy was closed, it still<br />
remained busy.<br />
During one shift last month, the<br />
team responded to a four calls in<br />
one Friday night shift including a<br />
man who had taken an overdose,<br />
a woman who was armed with<br />
two large kitchen knives and was<br />
self harming, a woman in distress<br />
on the edge of a cliff and a fight<br />
where a victim had been injured<br />
with a glass bottle.<br />
SECAmb operational team leader<br />
Tim Clark said: “Setting up the<br />
Joint Response Unit in the city of<br />
Brighton and Hove, and working<br />
so closely with the Sussex<br />
Police has been a celebration of<br />
collaborative working, enabling<br />
us to provide a more focused and<br />
specialised response to incidents<br />
requiring both ambulance and<br />
police attendance. While JRUs<br />
are not a new concept to the<br />
South East Coast <strong>Ambulance</strong><br />
Service, developing a joint<br />
working system within a busy and<br />
vibrant city such as Brighton and<br />
Hove presented a new challenge<br />
and the unit has proven to be<br />
an invaluable resource to both<br />
services.<br />
“It ensures a greater<br />
understanding of each services<br />
working practices, builds on<br />
our already robust collaborative<br />
relationship, reduces lost<br />
operational hours and, most<br />
importantly, provides the residents<br />
of Brighton and Hove with a more<br />
streamlined and tailored response<br />
to the varied and unique incidents<br />
we attend.”<br />
A second Sussex JRU is currently<br />
being trialled in Worthing.<br />
COVID-19 pandemic has drawn<br />
attention to importance of<br />
person-centred discussions<br />
when making decisions about<br />
cardiopulmonary resuscitation<br />
Resuscitation Council <strong>UK</strong><br />
has updated the ReSPECT<br />
(Recommended Summary<br />
Plan for Emergency Care and<br />
Treatment) process which<br />
supports person-centred<br />
conversations about care in<br />
a future emergency following<br />
feedback from professionals,<br />
patients and their families.<br />
As patients are often not able<br />
to make decisions about their<br />
priorities of care or treatment in an<br />
emergency, discussing what they<br />
would want to happen in advance<br />
is essential.<br />
The ReSPECT process is<br />
already widely used by health<br />
and social care organisations<br />
across England and in parts of<br />
Scotland to support them having<br />
important conversations with<br />
patients in advance about their<br />
emergency care, and whether<br />
cardiopulmonary resuscitation<br />
(CPR) should be attempted in a<br />
future emergency.<br />
The ReSPECT process is<br />
supported by a discussion<br />
guide and form and version 3<br />
is being introduced into clinical<br />
practice today. The form is used<br />
to document the discussion and<br />
any recommendations agreed, is<br />
signed by the clinician and can be<br />
162<br />
For further recruitment vacancies visit: www.ambulanceukonline.com
NEWSLINE<br />
signed by the patient/ their legal<br />
proxy or family member if they<br />
wish to do so.<br />
The changes made to the form<br />
have resulted in a more patientcentred<br />
form, with increased<br />
prompts for explicit clinical<br />
reasoning. It addresses areas<br />
where misunderstandings have<br />
been reported and includes more<br />
personable and clearer language.<br />
The COVID-19 pandemic has<br />
highlighted the importance of<br />
sensitive and well-structured<br />
conversations about someone’s<br />
realistic care choices and for<br />
there to be shared understanding<br />
between professionals, patients<br />
and their families.<br />
The ReSPECT process was first<br />
introduced by Resuscitation<br />
Council <strong>UK</strong> in 2016, with design<br />
expertise from the Helix Centre,<br />
Imperial College London,<br />
to support discussions and<br />
clinical recommendations<br />
about emergency care being<br />
made in advance. It was<br />
developed by experts and<br />
patient representatives keen to<br />
develop a process that supports<br />
professionals, patients and / or<br />
their families having a carefully<br />
constructed and person-centred<br />
conversation. It aims to develop<br />
a shared understanding between<br />
the healthcare professional and<br />
the patient of their condition,<br />
the outcomes the patient values<br />
and those they fear and then<br />
how realistic treatments and<br />
interventions, such as CPR, fit<br />
into this.<br />
The completed form stays<br />
with the patient and should be<br />
available immediately to health<br />
professionals called to help in an<br />
emergency, whether the patient<br />
is at home, in their community<br />
or in a healthcare setting.<br />
Professionals such as ambulance<br />
crews, out-of-hours doctors, care<br />
home staff and hospital staff will<br />
be better able to make quick<br />
decisions in an emergency about<br />
how best to help if key information<br />
has been recorded on the<br />
ReSPECT form.<br />
Sue Hampshire, Director of<br />
Clinical and Service Development<br />
at Resuscitation Council <strong>UK</strong> said:<br />
“We’re pleased to be introducing<br />
updated documentation to<br />
underpin the ReSPECT process<br />
today.<br />
“Communities in around 70%<br />
of counties in England and<br />
parts of Scotland are already<br />
using the ReSPECT process<br />
and the improvements we have<br />
introduced today are based on<br />
feedback from organisations who<br />
are already using the process as<br />
well as from patients and their<br />
families.<br />
“People have different views<br />
about the care or treatments they<br />
would want if they were suddenly<br />
ill and could not make decisions<br />
about their care or treatment.<br />
The new form will support better<br />
conversations and well-informed<br />
decision-making in advance, and<br />
we are happy to be introducing it<br />
for professionals and patients.”<br />
Dr Zoe Fritz, chair of the ReSPECT<br />
subcommittee, said: “We first<br />
developed the ReSPECT process<br />
to help professionals and<br />
patients or their families achieve<br />
better conversations and better<br />
recording of important treatment<br />
recommendations. The ReSPECT<br />
process encourages discussion<br />
about the individual’s condition,<br />
what’s important to them, what<br />
their realistic options are and<br />
what the likely potential health<br />
outcomes will be.<br />
“A number of misconceptions<br />
exist about CPR and when and<br />
how recommendations not to<br />
attempt CPR are made. So, it is<br />
crucial to have a person-centred<br />
approach and conversations<br />
that aim to ensure shared<br />
understanding between the<br />
professional and patient. By<br />
doing so, any misunderstandings<br />
can be addressed, and<br />
professionals can ensure that<br />
any recommendations made are<br />
based on what’s important to the<br />
patient.”<br />
When completed, the ReSPECT<br />
form provides a clinical<br />
record of agreed and realistic<br />
recommendations that come out<br />
of that conversation between a<br />
professional and the patient or<br />
their legal proxy or family member.<br />
A person’s ReSPECT form<br />
includes recommendations<br />
about emergency treatments<br />
that could be helpful and should<br />
be considered, as well as those<br />
not wanted by or that would not<br />
work for the patient. It includes a<br />
recommendation about CPR, but<br />
that may be a recommendation<br />
that CPR is attempted, or a<br />
recommendation that it is not<br />
attempted.<br />
For more information on the<br />
ReSPECT process, visit:<br />
www.resus.org.uk/respect<br />
WHY NOT WRITE FOR US?<br />
<strong>Ambulance</strong> <strong>UK</strong> welcomes the submission of clinical papers and case<br />
reports or news that you feel will be of interest to your colleagues.<br />
Material submitted will be seen by those working within the public and private sector<br />
of the <strong>Ambulance</strong> Service, Air <strong>Ambulance</strong> Operators, BASICS Doctors etc.<br />
All submissions should be forwarded to info@mediapublishingcompany.com<br />
If you have any queries please contact the publisher Terry Gardner via:<br />
info@mediapublishingcompany.com<br />
AMBULANCE <strong>UK</strong> - OCTOBER<br />
Do you have anything you would like to add or include in Newsline? Please contact us and let us know.<br />
163
NEWSLINE<br />
AMBULANCE <strong>UK</strong> - OCTOBER<br />
WAS<br />
Launch of the South<br />
Wales Trauma<br />
Network<br />
Monday 14 September saw<br />
the official launch of the South<br />
Wales Trauma Network, held at<br />
the new Major Trauma Centre at<br />
the University Hospital of Wales.<br />
Serving the population of South<br />
Wales, West Wales and South<br />
Powys, the network is made up<br />
of hospitals, emergency services<br />
and rehabilitation services<br />
across the region, working<br />
together to ensure patients with<br />
life-threatening or life-changing<br />
injuries receive the best possible<br />
treatment and care.<br />
The Welsh Government has<br />
provided £3.7 million capital<br />
and over £13 million recurrent<br />
revenue funding to support the<br />
pre-hospital, major trauma centre,<br />
specialist services and network<br />
elements of the programme<br />
business case.<br />
Its arrival marks a major step<br />
forward in the delivery of<br />
emergency care in Wales. Across<br />
the network more than 2,000<br />
patients a year are expected to be<br />
treated, and up to 70 lives saved<br />
over the next five years.<br />
Dr Dinendra Gill, Clinical Director<br />
for the South Wales Trauma<br />
Network, explains: “Today marks<br />
a significant milestone in planning<br />
for the network, and represents the<br />
culmination of extensive work by all<br />
NHS partners over many years.<br />
“Major trauma – which refers to<br />
multiple and serious injuries – is<br />
the leading cause of death in<br />
people under the age of 45 and<br />
a significant cause of disability or<br />
poor health. Patients with these type<br />
of injuries will have a better chance<br />
of survival if they are treated within a<br />
major trauma network.<br />
“As well as saving lives, the<br />
network will improve patient<br />
outcomes by preventing<br />
avoidable disability, returning<br />
more patients to their families, to<br />
work and to education.<br />
“I want to thank all those who<br />
have worked incredibly hard to<br />
open the service so that those<br />
who most need specialist care are<br />
able to benefit from it.”<br />
Officially opening the South Wales<br />
Trauma Network, Vaughan Gething<br />
MS, Minister for Health and<br />
Social Services – who attended<br />
the launch event virtually – said:<br />
“I am delighted to formally open<br />
the South Wales Trauma Network<br />
which will save lives and prevent<br />
avoidable disability for people<br />
involved in serious incidents.<br />
“While the new Major Trauma<br />
Centre at University Hospital of<br />
Wales is the setting for today’s<br />
launch event we celebrate the<br />
start of the Network which is a true<br />
collaboration of health services<br />
across the region with services<br />
in trauma units in each health<br />
board area and the major trauma<br />
desk within the Welsh <strong>Ambulance</strong><br />
Service.<br />
“This has been a long journey for<br />
many people and I thank all of<br />
those involved in what has been a<br />
truly collaborative effort to improve<br />
trauma services.”<br />
The University Hospital of Wales<br />
in Cardiff – which is Wales’<br />
only specialist neurosurgery<br />
hospital, and home of Noah’s Ark<br />
Children’s Hospital of Wales –<br />
becomes the region’s adult and<br />
children’s major trauma centre.<br />
As major trauma is relatively<br />
uncommon and complex to<br />
manage, services provided in<br />
the major trauma centre are<br />
highly specialised and available<br />
24 hours a day, seven days a<br />
week. The major trauma centre<br />
will collaborate with and support<br />
hospitals across the network.<br />
Establishing the network has led<br />
to enhanced roles for a number<br />
of other hospitals, including<br />
Morriston Hospital in Swansea,<br />
becoming a trauma unit with<br />
specialist services. Elsewhere, the<br />
network is supported by trauma<br />
units, rural trauma facilities and<br />
local emergency hospitals. The<br />
operational delivery network,<br />
which is hosted by Swansea<br />
Bay University Health Board, will<br />
oversee the running of the South<br />
Wales Trauma Network.<br />
Work to establish the network has<br />
been led by the NHS Wales Health<br />
Collaborative, in collaboration<br />
with health boards, the Welsh<br />
<strong>Ambulance</strong> Service NHS Trust, the<br />
Emergency Medical Retrieval and<br />
Transfer Service, Welsh Health<br />
Specialist Services Committee,<br />
Emergency <strong>Ambulance</strong> Service<br />
Committee, as well as third sector<br />
and community health councils.<br />
LAS<br />
Episode 2 of<br />
‘<strong>Ambulance</strong>’ to<br />
highlighted the<br />
contribution of<br />
voluntary Emergency<br />
Responders<br />
The second episode of the new<br />
series of the BBC documentary<br />
‘<strong>Ambulance</strong>’ highlighted the<br />
contribution of volunteer<br />
responders as London<br />
<strong>Ambulance</strong> Service (LAS) faced<br />
challenges from large protests<br />
and an IT system outage.<br />
The episode went behind the<br />
scenes of two busy weekend<br />
shifts where LAS faces the<br />
challenges of Extinction Rebellion<br />
protests and People’s Vote<br />
marches and an IT systems<br />
outage which meant the Service’s<br />
Emergency Operations Centre<br />
control room teams had to use<br />
pen and paper to take down<br />
information from 999 callers.<br />
Filmed in the autumn of 2019,<br />
viewers saw the variety of what a<br />
weekend day shift can bring for<br />
the country’s busiest ambulance<br />
service – from advanced paramedic<br />
Kevin responding to a cardiac<br />
arrest to crewmates Emily and<br />
Laura treating a 100-year-old who<br />
has fallen. All this while protests<br />
across central London posed the<br />
challenge of how crews can ensure<br />
they reach patients quickly.<br />
Viewers also saw Gary and Fabio –<br />
two of around 150 LAS Emergency<br />
Responders (ERs) - on shift. Retired<br />
police officer Gary and Fabio – who<br />
works in finance – volunteer their<br />
spare time responding to patients in<br />
the capital.<br />
ERs are LAS-trained volunteers<br />
who attend a range of emergency<br />
calls in Service uniform and in<br />
blue-light response cars.<br />
LAS Chief Executive Garrett<br />
Emmerson said:<br />
“This second episode again<br />
showed the breadth and variety of<br />
our Service and the commitment<br />
of all our staff and volunteers –<br />
as they faced challenges from<br />
protests and IT system outages,<br />
but still responded to those who<br />
needed us.<br />
“We were also delighted to see<br />
some of our volunteer Emergency<br />
Responders on the screen.<br />
Volunteers play a key role in our<br />
Service and this show highlights<br />
their commitment, professionalism<br />
and dedication.”<br />
164<br />
For more news visit: www.ambulanceukonline.com
NEWSLINE<br />
GNAAS<br />
The jet suit<br />
paramedic<br />
Mr. Mawson said the exercise had<br />
demonstrated the huge potential<br />
of utilising Jet Suits to deliver<br />
critical care services.<br />
The Lake District could become<br />
home to the world’s first Jet Suit<br />
paramedic, according to those<br />
behind the concept.<br />
A collaboration between Gravity<br />
Industries, which has developed<br />
and patented a 1050 brake<br />
horsepower Jet Suit, and the<br />
Great North Air <strong>Ambulance</strong><br />
Service (GNAAS), has resulted<br />
in a test flight in the heart of the<br />
Lakes.<br />
He added: “In a time in healthcare<br />
when we are exhausted with<br />
COVID and its effects, it’s<br />
important to still push the<br />
boundaries.<br />
“Our aircraft will remain a vital<br />
part of the emergency response<br />
in this terrain, as will the fantastic<br />
mountain rescue teams. But this<br />
is about looking at supplementing<br />
those resources with something<br />
completely new.<br />
The test at the Langdale Pikes<br />
saw Gravity Industries founder<br />
and Chief Test Pilot Richard<br />
Browning fly from the valley<br />
bottom to a simulated casualty<br />
site on The Band, near Bowfell.<br />
The simulated casualty site would<br />
take around 25 minutes to reach<br />
by foot. The Gravity Jet Suit is<br />
able to cover that distance in 90<br />
seconds, opening a range of<br />
possibilities in the emergency<br />
response arena.<br />
The ground-breaking exercise<br />
was the culmination of a year of<br />
discussion between GNAAS and<br />
Gravity Industries.<br />
Andy Mawson, director of<br />
operations and paramedic at<br />
GNAAS, identified the Lakes<br />
as a possible location for a Jet<br />
Suit paramedic after hearing of<br />
Mr. Browning’s work and then<br />
studying the charity’s own call-out<br />
data.<br />
“We think this technology could<br />
enable our team to reach some<br />
patients much quicker than ever<br />
before. In many cases this would<br />
ease the patient’s suffering. In some<br />
cases, it would save their lives.”<br />
Richard Browning added: “It was<br />
wonderful to be invited to explore<br />
the capabilities of the Gravity Jet<br />
Suit in an emergency response<br />
simulation and work alongside<br />
the team at GNAAS. We are just<br />
scratching the surface in terms<br />
of what is possible to achieve<br />
with our technology. Emergency<br />
response is one of the areas<br />
Gravity are actively pursuing,<br />
alongside launching a new<br />
commercial training location at<br />
the world-renowned Goodwood<br />
Estate.”<br />
With the test complete, GNAAS<br />
and Gravity Industries are now<br />
exploring the next steps in this<br />
collaboration.<br />
He said: “It showed dozens of<br />
patients every month within the<br />
complex but relatively small<br />
geographical footprint of the<br />
Lakes.<br />
“We could see the need. What<br />
we didn’t know for sure is how<br />
this would work in practice. Well<br />
we’ve seen it now and it is, quite<br />
honestly, awesome.”<br />
GNAAS and Gravity Industries<br />
would like to thank Langdale<br />
Mountain Rescue Team, the<br />
National Trust, Stool End Farm<br />
and Cumbria Police for their part<br />
in making the test possible.<br />
GNAAS is a charity and relies on<br />
donations to survive. To find out<br />
more please call 01325 487 263<br />
or visit gna.as/jet-suit<br />
AMBULANCE <strong>UK</strong> - OCTOBER<br />
For the latest <strong>Ambulance</strong> Service News visit: www.ambulancenewsdesk.com<br />
165
COMPANY NEWS<br />
significantly, safely and rapidly;<br />
preferably at the earliest possible<br />
intervention point of injury.<br />
Quantum is a Game-Changing<br />
innovation that has succeeded in<br />
closing a critical capability gap<br />
The Quantum<br />
Solution<br />
previously left exposed by other<br />
commercial off-the-shelf fluid<br />
warmers currently fielded.<br />
The Quantum exceeds all<br />
healthcare and logistical<br />
requirements for the delivery<br />
of warmed blood or fluids<br />
across the defined spectrum<br />
of care.<br />
With the Quantum, size, weight,<br />
performance, and ease of use are<br />
no longer collective barriers to<br />
the delivery of whole blood in far<br />
forward and Point of Injury (POI)<br />
casualty management.<br />
The system consists of unique<br />
thermal administration sets that<br />
incorporate sensing elements<br />
with an integrated heating system<br />
that does not disrupt the fluid<br />
path. With advanced intelligence<br />
throughout the system, the<br />
lightweight Controller modulates<br />
and moderates the energy flow to<br />
the integrated heating elements to<br />
ensure consistent normothermic<br />
fluid delivery to the casualty.<br />
The battery is the smallest in<br />
category, able to rapidly adjust<br />
power distribution based on<br />
the temperature and flow rate<br />
of the input fluid. This creates a<br />
highly efficient system capable of<br />
previously unrealized performance<br />
optimizations.<br />
The Quantum system has an<br />
operational weight of just 624<br />
grams yet can deliver one litre of<br />
4°C Whole Blood (WB) at 100mL/<br />
min with an output temperature<br />
of 38°C+/- 2°C with only a 24<br />
second warm-up period.<br />
The Quantum Blood and Fluid<br />
Warmer provides the Health<br />
Care Professional with significant<br />
technological advantage in the<br />
fight to eliminate preventable<br />
death.<br />
The Problem: Why Warm<br />
Infusion Fluids?<br />
Even a small decrease in body<br />
temperature of an injured patient<br />
starts a cascade of negative<br />
events significantly increasing<br />
morbidity and mortality. A core<br />
temperature of less than 35C<br />
(95F) is a poor prognostic<br />
indicator A core temperature<br />
of 32C (90F) is associated with<br />
100% mortality.<br />
Known as Secondary or<br />
Unintentional Hypothermia (UH).<br />
Once established, UH is very<br />
difficult to correct. Prevention<br />
measures starting from the<br />
earliest point of patient care is the<br />
most effective strategy.<br />
DS Medial have been appointed<br />
as <strong>UK</strong> & Ireland distributor please<br />
contact DS Medical on 01329<br />
311451 or alternatively email<br />
info@dsmedical.co.uk should<br />
you wish to discuss this in greater<br />
detail.<br />
Great Western Air<br />
<strong>Ambulance</strong> Charity<br />
unveil new critical<br />
care car<br />
Great Western Air <strong>Ambulance</strong><br />
Charity (GWAAC) have<br />
unveiled a new critical care<br />
car, which will allow them<br />
to reach more critically ill<br />
patients across the region.<br />
The charity’s critical care cars are<br />
operated alongside the helicopter,<br />
and carry the same equipment as<br />
the helicopter, bringing the crew<br />
and their lifesaving skills to the<br />
side of those in urgent need.<br />
AMBULANCE <strong>UK</strong> - OCTOBER<br />
166<br />
Administration of un-warmed<br />
IV fluids and cold stored blood<br />
products are an established risk<br />
factor for patients to develop<br />
UH. Particularly when initiated<br />
in the uncontrolled prehospital<br />
environment.<br />
Blood must be stored, refrigerated<br />
and kept very cold prior to<br />
transfusion. During transfusion,<br />
blood must be warmed<br />
For more news visit: www.ambulanceukonline.com<br />
The new model, a Skoda<br />
Kodiaq, which is used by South<br />
Western <strong>Ambulance</strong> Service<br />
NHS Foundation Trust, has been<br />
specially converted to meet the<br />
requirements of the Critical Care<br />
Team.<br />
The 720-litre boot has been<br />
redesigned to house essential<br />
lifesaving equipment, including<br />
ventilators, oxygen, controlled
COMPANY NEWS<br />
drugs and other specialist<br />
equipment the Critical Care<br />
Team carry. The front of the car<br />
has been adapted, with a 999<br />
response screen installed for the<br />
crew to receive details of call-outs<br />
and navigate to the location of<br />
the patient in need quickly and<br />
efficiently.<br />
The model has also been<br />
kitted out with additional power<br />
supplies, including split charging<br />
and mains shoreline capabilities<br />
to ensure that both the cars and<br />
the kit inside are constantly ready<br />
to respond.<br />
In 2019, GWAAC’s crew received<br />
over 2,000 call-outs, of which over<br />
two thirds were responded to by<br />
critical care car. The cars ensure<br />
that the crew are always ready<br />
to respond in any conditions, for<br />
example when the helicopter is<br />
unable to fly due to bad weather<br />
or maintenance, or when the<br />
location of a patient has limited<br />
safe landing sites nearby and is<br />
easier to access by road.<br />
Air Operations Officer at GWAAC,<br />
John Wood, said: “Having<br />
reliable, appropriate and fully<br />
equipped cars are essential for<br />
us to reach and treat patients in<br />
the most effective way. The new<br />
vehicles will enable our team to<br />
negotiate tougher terrain and<br />
drive safely in challenging weather<br />
conditions to reach patients<br />
quickly and safely, particularly in<br />
rural areas.”<br />
This new car will be one of three<br />
vehicles to join GWAAC’s fleet,<br />
updating the current models that<br />
the service uses, after the charity<br />
successfully bid for a one-off<br />
Government grant from the<br />
Department of Health and Social<br />
Care last year to purchase the<br />
much needed new cars.<br />
To find out more about GWAAC’s<br />
new critical care car, visit: www.<br />
gwaac.com/critical-care-cars<br />
South Central<br />
<strong>Ambulance</strong><br />
Service partners<br />
with GoodSAM to<br />
bring innovative<br />
video streaming<br />
technology into their<br />
Clinical Coordination<br />
Centre 999 Control<br />
Rooms<br />
South Central <strong>Ambulance</strong><br />
Service NHS Foundation Trust<br />
(SCAS) is launching a groundbreaking<br />
digital product -<br />
GoodSAM’s Instant On Scene -<br />
to enable the public to stream<br />
video directly from their<br />
smartphones into the SCAS<br />
999 Clinical Coordination<br />
Centres (CCC). The system<br />
is set to revolutionise triage<br />
for the <strong>Ambulance</strong> Service,<br />
ensuring medics can now see<br />
what the patient sees in just a<br />
few seconds.<br />
It will enable SCAS’s 999 CCC<br />
staff to send a text or email<br />
message to a caller containing<br />
a link which, when clicked on,<br />
enables video to be streamed<br />
live from the caller’s smartphone<br />
directly into the CCC. There’s<br />
nothing to download and no<br />
logins, the system works on any<br />
smartphone and on any network;<br />
its use is entirely voluntary. All<br />
data is securely transmitted with<br />
end-to-end encryption and no<br />
video is recorded, so members<br />
of the public can be absolutely<br />
confident that their information is<br />
safe.<br />
The 999 call continues while the<br />
video is streaming. Instant on<br />
Scene will help ensure patients<br />
are quickly assessed and<br />
given effective medical advice.<br />
It will support SCAS in better<br />
understanding the level of care<br />
or resources which may be<br />
required to deliver the best patient<br />
outcomes.<br />
Luci Stephens, Director of<br />
Operations (CCC) said: “This<br />
marks the start of an exciting new<br />
chapter in patient care by SCAS.<br />
We have previously been able<br />
to resolve patients’ healthcare<br />
issues, either by the dispatch<br />
of an emergency ambulance,<br />
by referring them to other areas<br />
of the NHS to receive ongoing<br />
care or by advising them over<br />
the telephone how to manage<br />
their symptoms at home. Using<br />
GoodSAM’s Instant On Scene<br />
brings an additional visual layer<br />
to our well-practiced processes<br />
and procedures and this will help<br />
to ensure that our patients get the<br />
right care, in the right place and<br />
at the right time. Patient safety<br />
remains at the heart of everything<br />
we do, and video consultations<br />
will provide exceptional support in<br />
allowing us to achieve this goal”.<br />
Ali Ghorbangoli, Technical Director<br />
and Co-Founder of GoodSAM<br />
said: “Developing a highly<br />
accessible and simple to use<br />
system is central to success. Our<br />
products are designed specifically<br />
for emergency situations - no<br />
apps, downloads or logins are<br />
required”.<br />
It is anticipated that the video<br />
solutions will translate into lifechanging<br />
outcomes, enabling<br />
SCAS to respond more rapidly<br />
and appropriately. Instant On<br />
Scene will also support major<br />
incidents and enable emergency<br />
services to share video streams in<br />
real-time.<br />
Medical Director and Co-Founder<br />
of GoodSAM, Professor Mark<br />
Wilson said: ‘In emergencies, time<br />
is vital in saving a person’s life<br />
or reducing long-term disability.<br />
Often <strong>Ambulance</strong> Services<br />
have limited information from<br />
bystanders about a patient’s, or<br />
multiple patients’, injuries to make<br />
decisions. Instantly being able to<br />
see the scene radically improves<br />
situational awareness. We are<br />
incredibly excited to be bringing<br />
this technology to SCAS, and<br />
we look forward to working with<br />
them in ensuring the GoodSAM<br />
system continues to save lives<br />
and further enhance patient care<br />
in the region’.<br />
GoodSAM’s Instant On Scene is<br />
being rolled out as part of SCAS’s<br />
Global Digital Exemplar (GDE)<br />
programme. This initiative is<br />
supported by NHS Digital and is<br />
designed to leverage technology<br />
to improve patient outcomes and<br />
staff working practices.<br />
“Developing<br />
a highly<br />
accessible<br />
and simple to<br />
use system<br />
is central<br />
to success.<br />
Our products<br />
are designed<br />
specifically<br />
for emergency<br />
situations<br />
- no apps,<br />
downloads<br />
or logins are<br />
required”.<br />
AMBULANCE <strong>UK</strong> - OCTOBER<br />
For the latest <strong>Ambulance</strong> Service News visit: www.ambulancenewsdesk.com<br />
167
INTRODUCING THE X SERIES ®<br />
ADVANCED:<br />
ADVANCE YOUR CARE FOR EVERY RESCUE<br />
Manage your patients more effectively than ever with ZOLL’s new<br />
X Series Advanced monitor/defibrillator. X Series Advanced offers<br />
two groundbreaking new features:<br />
Real BVM Help provides real-time clinical feedback on<br />
manual ventilation, including delivered tidal volume and<br />
rate, a ventilation quality indicator, and a countdown timer.<br />
TBI Dashboard enables care providers to effectively<br />
manage patients with traumatic brain injury. The<br />
dashboard combines trending of critical vital signs with<br />
real-time ventilation feedback in one comprehensive view.<br />
Interested to learn more? Request a demo and receive<br />
a free BVM: www.zoll.com/xseriesadvanced-uk<br />
© 2019 ZOLL Medical Corporation. All rights reserved. Real BVM Help, X Series Advanced and<br />
ZOLL are trademarks or registered trademarks of ZOLL Medical Corporation in the United States<br />
and/or other countries. All other trademarks are the property of their respective owners.<br />
MCN IP 1910 0295-05