Resus Today Summer 2019
Resus Today Summer 2019
Resus Today Summer 2019
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
Volume 6 No. 2<br />
<strong>Summer</strong> <strong>2019</strong><br />
<strong>Resus</strong>citation <strong>Today</strong><br />
A Resource for all involved in the Teaching and Practice of <strong>Resus</strong>citation<br />
Illuminating<br />
Infant CPR<br />
Illuminating<br />
Seeing is<br />
Infant CPR<br />
believing<br />
Seeing is<br />
believing<br />
CONTACT US TO FIND OUT MORE<br />
Tel: 01252 344007 |<br />
braydenbaby@welmedical.com<br />
www.welmedical.com<br />
CONTACT US TO FIND OUT MORE<br />
Tel: 01252 344007 |<br />
braydenbaby@welmedical.com<br />
www.welmedical.com
CONTENTS<br />
CONTENTS<br />
<strong>Resus</strong>citation <strong>Today</strong><br />
4 EDITORS COMMENT<br />
6 CLINICAL PAPER Airway Management in the Emergency<br />
Department (The OcEAN-Study) -<br />
a prospective single centre observational<br />
cohort study<br />
17 CLINICAL PAPER Repeated vital sign measurements in<br />
the emergency department predict<br />
patient deterioration within 72 hours:<br />
a prospective observational study<br />
This issue edited by:<br />
Paul Jones (MRes; BSc; fHEA; Paramedic)<br />
c/o Media Publishing Company<br />
Media House<br />
48 High Street<br />
SWANLEY, Kent BR8 8BQ<br />
ADVERTISING & CIRCULATION:<br />
Media Publishing Company<br />
Media House, 48 High Street<br />
SWANLEY, Kent, BR8 8BQ<br />
Tel: 01322 660434 Fax: 01322 666539<br />
E: info@mediapublishingcompany.com<br />
www.MediaPublishingCompany.com<br />
PUBLISHED:<br />
Spring, <strong>Summer</strong> and Autumn<br />
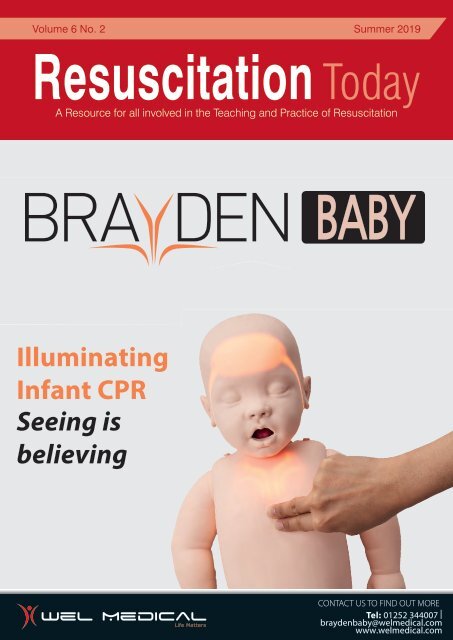
COVER STORY<br />
Dear Friends and Colleagues,<br />
We are delighted to announce the much-anticipated arrival of Brayden Baby,<br />
the new member of our Brayden family. This is truly a unique baby, having<br />
The First<br />
been created and developed by a highly skilled design team with help from<br />
Illuminating<br />
leading European experts in the field of resuscitation.<br />
Infant CPR<br />
Brayden Baby illuminating infant CPR has been designed to be an ideal<br />
teaching manikin for Paediatric BLS, EPALS and EPILS.<br />
<strong>Resus</strong>citation professionals are praising it for its many innovative features –<br />
read more about these in this issue.<br />
We have more great news for you!<br />
'Here's<br />
looking at<br />
you, Baby!'<br />
Manikin<br />
CONTACT US TO FIND OUT MORE<br />
Tel: 01252 344007 | paul.mulvey@welmedical.com<br />
www.welmedical.com<br />
COPYRIGHT:<br />
Media Publishing Company<br />
Media House<br />
48 High Street<br />
SWANLEY, Kent, BR8 8BQ<br />
PUBLISHERS STATEMENT:<br />
The views and opinions expressed in<br />
this issue are not necessarily those of<br />
the Publisher, the Editors or Media<br />
Publishing Company.<br />
Next Issue Autumn <strong>2019</strong><br />
Subscription Information – <strong>Summer</strong> <strong>2019</strong><br />
<strong>Resus</strong>citation <strong>Today</strong> is a tri-annual publication<br />
published in the months of March and<br />
September. The subscription rates are as<br />
follows:-<br />
UK:<br />
Individuals - £12.00 inc. postage<br />
Commercial Organisations - £30.00 inc. postage<br />
Rest of the World:<br />
Individuals - £60.00 inc. postage<br />
Commercial Organisations - £72.00 inc. postage<br />
There are lots more Brayden Babies looking for good homes and if you would like<br />
to see this little genius in action, please email paul.mulvey@welmedical.com to<br />
arrange an informal demonstration.<br />
Best wishes<br />
Brayden<br />
P.S Please take a look at a short overview of Brayden Baby ‘in action’ on<br />
www.welmedical.com/baby-brayden-advanced<br />
We are also able to process your<br />
subscriptions via most major credit<br />
cards. Please ask for details.<br />
Cheques should be made<br />
payable to MEDIA PUBLISHING.<br />
Designed in the UK by me&you creative<br />
RESUSCITATION TODAY - SUMMER <strong>2019</strong><br />
3
EDITORS COMMENT<br />
EDITORS COMMENT<br />
It’s interesting that this season’s edition relates to both the management of<br />
the patient’s airway in the Emergency Department, and the recognition of<br />
deterioration in the most serious of patients in the first place. Failure to manage a<br />
patient’s airway appropriately is always going to lead to poor prognoses and the<br />
observation of vital signs is… well, vital. Both of these issues are contentious and<br />
evolving, considered and developing. They professionally divide colleagues and<br />
create professional discussion – as well as offering the opportunity for high quality<br />
studies to develop even higher quality patient care.<br />
RESUSCITATION TODAY - SUMMER <strong>2019</strong><br />
“Resources<br />
for managing<br />
patients in an<br />
emergency<br />
setting are<br />
becoming<br />
more effective,<br />
and technology<br />
continues to<br />
improve patient<br />
outcomes,<br />
we find<br />
ourselves at a<br />
crossroads…”<br />
As resources for managing patients in an emergency setting become more effective (when<br />
they are used well), and technology continues to improve patient outcomes, I suggest we find<br />
ourselves at a crossroads. There are options – but what direction should we go? Is it towards<br />
the high-tech intervention that continues to perfuse but offers little hope of positive long-term<br />
outcome? Do we aim for a back-to-basics approach of doing the simple things well and accept<br />
that if they are not effective then it was not to be? Is it about taking a true moral and ethical<br />
approach, with the individual at the centre of all of the decisions we make? Or, should we be<br />
looking at a combination of all of the above: a resuscitation road-map which allows high quality<br />
basic care, accompanied by modern technology that can assist with identifying arrest causation,<br />
but based on real-time, patient-focused decision-making?<br />
There are so many more aspects of resuscitation to be considered: causes; prevention;<br />
recognition; management; and decision-making to name but a few. And there are so many<br />
possibilities within those aspects too: the education; the skills; the tools; the people; the effects;<br />
the outcomes. Quite rightly, the time is upon us to break the taboo and talk about such topics as<br />
applying patient choice and dignity in dying alongside the more professionally concerning areas<br />
of legal and regulatory care.<br />
<strong>Resus</strong>citation <strong>Today</strong> offers the opportunity to consider all of these aspects and more; and you<br />
are welcome to submit your own work for publication – I look forward to receiving submissions<br />
for review that range from ‘simple’ position-pieces to ‘complex’ analytical research papers. From<br />
novices who may be experimenting with their investigative genes, to experts in the field who can<br />
offer academic challenge to the ‘norm’.<br />
Get in touch, submit comments and work at: info@mediapublishingcompany.com<br />
Paul Jones (MRes; BSc; fHEA; Paramedic)<br />
4
<strong>Resus</strong>citation<br />
and Emergency<br />
Care<br />
A full range of products for<br />
use in an emergency and<br />
resuscitation situation.<br />
• Bag-Valve-Mask (BVM)<br />
• Pocket <strong>Resus</strong>citation Mask<br />
• Airway Management Devices<br />
• Video Laryngoscopy<br />
• Oxygen Therapy Masks<br />
The complete solution from<br />
the respiratory care specialists<br />
To view the full range visit<br />
www.intersurgical.co.uk/info/emergency<br />
lnteract with us<br />
Quality, innovation and choice<br />
www.intersurgical.co.uk
CLINICAL PAPER<br />
AIRWAY MANAGEMENT IN THE EMERGENCY<br />
DEPARTMENT (THE OCEAN-STUDY) - A PROSPECTIVE<br />
SINGLE CENTRE OBSERVATIONAL COHORT STUDY<br />
Michael Bernhard 1,2,3† , Sönke Nils Bax 2,7*† , Thomas Hartwig 2 , Maryam Yahiaoui-Doktor 4 , Sirak Petros 5 , Sven<br />
Bercker 6 , Alexandra Ramshorn-Zimmer 2 and André Gries 2<br />
Reproduced with permission from the Scandinavian Journal of Trauma, <strong>Resus</strong>citation and Emergency Medicine. (<strong>2019</strong>) 27:20 doi: 10.1186/s13049-019-0599-1<br />
Abstract<br />
Background<br />
Emergency airway management (AM) is a major key for successful<br />
resuscitation of critically ill non-traumatic (CINT) patients. Details of<br />
the AM of these patients in German emergency departments (ED) are<br />
unknown. This observational study describes epidemiology, airway<br />
techniques, success rates and complications of AM in CINT ED patients<br />
in the resuscitation room (RR).<br />
Methods<br />
Data was collected prospectively on adult CINT patients admitted to<br />
the RR of a single German university ED September 2014 to August<br />
2015. Patient characteristics, out-of-hospital and in-hospital RR AM,<br />
complications and success rates were recorded using a self-developed<br />
airway registry form.<br />
Results<br />
During the study period 34,303 patients were admitted to the ED,<br />
out of those 21,074 patients for non-trauma emergencies. Suffering<br />
from severe acute life-threatening problems, 532 CINT patients were<br />
admitted to the RR. 150 (28.2%) CINT patients had received out-ofhospital<br />
AM. In 16 of these cases (10.7%) the inserted airway needed to<br />
be changed after RR admission (unrecognized oesophageal intubation:<br />
n = 2, laryngeal tube exchange: n = 14). 136 (25.6%) CINT patients<br />
without out-of-hospital AM received RR AM immediately after admission.<br />
The first-pass and overall success rate in the RR were 71 and 100%,<br />
respectively, and multiple intubation attempts were necessary in<br />
29%. A lower Cormack/Lehane (C/L) grade was associated with less<br />
intubation attempts (C/L1/2 vs. 3/4: 1.2 ± 0.5 vs. 1.8 ± 1.2, p = 0.0002).<br />
Complication rate was 43%.<br />
Conclusions<br />
OcEAN demonstrates the challenges of AM in CINT patients in a<br />
German ED RR. We propose a nation-wide ED airway registry to better<br />
track outcomes in the future.<br />
Keywords<br />
Airway management, Emergency department, <strong>Resus</strong>citation room, Firstpass<br />
success, Complications<br />
Background<br />
Methods<br />
RESUSCITATION TODAY - SUMMER <strong>2019</strong><br />
Critically ill patients frequently require airway management in the field<br />
or in the Emergency Department (ED) [1]. Several investigations have<br />
shown that emergency airway management in the field and in the ED<br />
is associated with adverse events and complications (e.g., hypoxemia,<br />
oesophageal intubation, hypotension) [2, 3]. However, inadequate<br />
oxygenation and ventilation will lead to wrong outcome and therefore<br />
emergency airway management is of priority in resuscitation of critically<br />
ill patients [4, 5].<br />
Studies have demonstrated that the number of intubation attempts<br />
is associated with increasing complication rates, therefore, the “firstpass<br />
intubation success” is an important concept in emergency airway<br />
management [6, 7]. ED Airway registries exist in some countries (e.g.,<br />
Australia [8], North America [9, 10], Korea [11], Japan [12]), however<br />
data on emergency airway management in German EDs are still<br />
missing.<br />
The aim of this study is to evaluate airway management in critically<br />
ill patients in the resuscitation room (RR) of a German ED in order to<br />
describe incidence, devices, techniques, success and complication<br />
rates.<br />
Study design<br />
This prospective single centre observational cohort [Observation of<br />
airway management in Emergency Department (OcEAN)] study was<br />
carried out from 1 September 2014 to 31 August 2015 in the ED of<br />
the University Hospital of Leipzig, Germany. The OcEAN study was<br />
approved by the ethical committee of the Medical Faculty of the<br />
University of Leipzig, Germany (265–14-25,082,014).<br />
Setting<br />
More than 34,000 patients are managed annually in the ED of the<br />
University Hospital of Leipzig, a level 1 trauma centre. However,<br />
about 50% of patients suffering from non-traumatic acute problems<br />
or emergencies. The out-of-hospital emergency care is provided by<br />
an EMS system staffed with paramedics and EMS physicians. In our<br />
institution, all non-traumatic critically ill patients in the RR are treated<br />
by a team of two nurses, one resident and one senior physician with<br />
emergency and intensive care competency. Patients fulfilling the nontrauma<br />
RR activation criteria according to Additional file 1: Table S1<br />
(in the Supplemental material) are admitted to the RR, the others are<br />
treated in other regions of the ED as the observation unit or one of the<br />
single cabins.<br />
6
CLINICAL PAPER<br />
Study definition and data collection<br />
All adult non-traumatic critically ill patients needing airway management<br />
in the ED RR were consecutively included. Paediatric and trauma<br />
patients were excluded. For further analysis, data were documented<br />
in a self-developed and implemented airway registry form. The airway<br />
registry form included the “Utstein airway core variables” established<br />
in the out-of-hospital airway management, as well as parameters<br />
implemented in out-of-hospital and ED airway registries in North<br />
America and Austria, as well as other out-of-hospital studies from<br />
Germany [4, 5, 8, 9, 13-16].<br />
The OcEAN airway registry form was completed in the RR, any missing<br />
data were followed up through interviews with the staff involved or from<br />
the medical records.<br />
The OcEAN airway registry form included the patient’s characteristics<br />
(age, gender, weight, high, body mass index), out-of-hospital triage score<br />
using American Society of Anesthesiology (ASA) score [17] at hospital<br />
admission and National Advisory Committee of Aeronautics (NACA) score<br />
in order to stratify the patient cohort [18], as well as the chief complaint<br />
leading to ED admission [cardiac arrest, unconsciousness (Glasgow<br />
coma scale [19] < 9), respiratory failure, shock].<br />
The out-of-hospital airway management records were reviewed by the<br />
main investigator [airway management technique performed by EMS<br />
physicians including endotracheal intubation, supraglottic airway device<br />
(SAD), cricothyroidotomy, success of airway management, use of<br />
capnography].<br />
The ED airway management was recorded, including patient position<br />
[back-up head elevated (BUHE [20]) or supine position], immobilization,<br />
and airway device [Macintosh blade, video laryngoscope, SAD<br />
(laryngeal tube, laryngeal mask airway), cricothyroidotomy, tracheotomy<br />
tube]. The number of intubation attempts per patient was also recorded.<br />
An airway management attempt was defined as the insertion of the<br />
airway device in the mouth (i.e., single passage of a laryngoscopy<br />
blade behind the lips, insertion of SAD). Multiple intubation attempts<br />
were defined as more than one insertion attempt. Per our institutional<br />
safety protocol, physicians had to handover the airway procedure to<br />
another physician after a second failed attempt at airway management.<br />
Difficult airway characteristics were described using parameters of the<br />
LEMON law (look external, evaluate 3–3-2 rule, Mallampati score [21],<br />
obstruction, immobilisation). Degree of visualization of the vocal cords<br />
was described using Cormack/Lehane (C/L) grade [22, 23] as assessed<br />
by direct or video laryngoscopy. The intubations’ difficulty scale (IDS)<br />
RESUSCITATION TODAY - SUMMER <strong>2019</strong><br />
Fig. 1 Study cohort: ED = emergency department, CINT = critically ill non-traumatic, RR = resuscitation room<br />
7
CLINICAL PAPER<br />
Table 1 Patient’s characteristics<br />
out-of-hospital airway management (n = 150) ED airway management (n = 136) p<br />
Epidemiology<br />
age (years), MV ± SD, 66 ± 16 65 ± 18 0.730<br />
Median, min-max 69, 18–94 71, 20–89<br />
Weight (kg), MV ± SD, 83 ± 27 81 ± 22 0.403<br />
Median, min-max 80, 42–180 80, 40–150<br />
Hight (cm), MV ± SD, 170 ± 32 170 ± 9 0.992<br />
Median, min-max 170, 150–190 170, 140–190<br />
BMI (kg/m 2 ), MV ± SD, 28 ± 8 28 ± 7 0.419<br />
Median, min-max 28, 15–58 26, 16–59<br />
Male Gender [n, (%)] 86 (57.3%) 82 (60.2%) 0.611<br />
NACA (points), MV ± SD, 5.3 ± 0.8 4.8 ± 0.7 0.001<br />
Median, min-max 5.5, 3–6 5, 3–6<br />
ASA (points), MV ± SD, 3.5 ± 1.3 3.2 ± 0.9 0.007<br />
Median, min-max 4, 1–6 3, 1–5<br />
Reason for airway management<br />
Cardiac arrest [n, (%)] 74 (49.3%) 9 (6.6%) < 0.001<br />
Unconsciousness [n, (%)] 50 (33.3%) 58 (42.6%) 0.105<br />
Respiratory failure [n, (%)] 18 (12.0%) 50 (36.8%) < 0.001<br />
Hemodynamic instability [n, (%)] 8 (5.3%) 19 (14.0%) 0.01<br />
RESUSCITATION TODAY - SUMMER <strong>2019</strong><br />
was calculated for each patient [24]. A difficult intubation was defined as<br />
one that requires more than two attempts or an IDS ≥5 points [24].<br />
For ED airway management, intubation conditions (very good = glottis<br />
open, good = glottis open and less combative patient, poor = glottis<br />
nearly closed and combative patient, very bad = glottis closed) were<br />
recorded. Moreover, any complication during RR airway management<br />
was documented. Complications (e.g. oxygen desaturation,<br />
hypotension) were defined in accordance to Sakles et al. [6].<br />
Statistical analysis<br />
Data were entered into Microsoft Excel 2014 (Microsoft, Germany) and<br />
analysed using SPSS (IBM-Statistics, Version 20, IBM Inc., Armonk, NY,<br />
USA). Descriptive statistics included number or percentages, mean<br />
(SD), median and minimal to maximal value. Ch i2 -test or, as appropriate,<br />
Fisher’s exact test were used to compare groups of binary data and<br />
to test for trends. For all analyses, actual P-values were reported<br />
and all tests were two-tailed. Statistically significant differences were<br />
considered at p < 0.05 level.<br />
Results<br />
During the 12-month study period, 34,303 patients were admitted to the<br />
ED. 13,229 patients with 592 treated in the RR were excluded due to<br />
trauma as leading cause of admission. 21,074 patients were admitted<br />
for non-traumatic emergencies, with 537 patients directly admitted to<br />
the RR (2.54%). After excluding five patients due to incomplete datasets,<br />
286 critically ill non-traumatic patients receiving airway management in<br />
the RR were further investigated (53.8%).<br />
In 150 (52.4%) patients, airway management was performed by EMS<br />
before and in 136 (47.6%) patients by ED staff after admission to the RR<br />
(Fig. 1). In 11 (7.3%) patients of the EMS group, the airway was secured<br />
with a laryngeal tube by paramedics. In 7 out of these 11 (63.6%) cases,<br />
an EMS physician had changed the airway device into an endotracheal<br />
tube in the out-of-hospital setting. In 16 (10.7%) patients of the EMS<br />
group, the airway device had to be changed after RR admission due<br />
to various reasons. The patient characteristics in the EMS and the RR<br />
management group were comparable (Table 1). However, according<br />
to the out-of-hospital triage score, patients with out-of-hospital airway<br />
management had a higher NACA (5.3 ± 0.8 vs. 4.8 ± 0.7, p = 0.001) and<br />
ASA score (3.5 ± 1.3 vs. 3.2 ± 0.9, p = 0.007) in comparison to patients<br />
with in-hospital airway management in the RR. The leading indication<br />
for airway management in the field and the RR setting differ significantly,<br />
with cardiac arrest in the out-of-hospital setting and unconsciousness as<br />
well as respiratory failure in the RR setting (Table 1).<br />
Patients with out-of-hospital airway management in the<br />
resuscitation room<br />
Patients who received airway management by EMS physicians (n = 150)<br />
underwent endotracheal intubation or laryngeal tube insertion in 90.7%<br />
(n = 136) and 9.3% (n = 14), respectively. Out of hospital capnography<br />
was used in 82.7%. Oesophageal intubation was detected in two cases<br />
(1.5%) of the out-of-hospital intubation group. In one of these patients<br />
capnography had not been used in the field or during transport. Both<br />
patients were admitted with on-going cardiopulmonary resuscitation and<br />
ED physicians secured the airway within the first intubation attempt using<br />
direct laryngoscopy (each C/L grade 1). In both cases, there were no<br />
predicted or occurred difficult airways using LEMON law and IDS score.<br />
8
CLINICAL PAPER<br />
In the 14 patients with out-of-hospital inserted laryngeal tubes, we<br />
observed insufficient ventilation (e.g. airway leakage) in 8 cases<br />
(57.1%), in 75% without out-of-hospital use of capnography. During<br />
the RR period, all 14 patients with laryngeal tube were successfully<br />
intubated using direct vs. video laryngoscopy (42.9%, n = 6 vs. 57.1%,<br />
n = 8) within 1.3 ± 0.5 (Median: 1, min-max 1–2) vs. 1.9 ± 1.4 attempts<br />
(Median: 1.5, min-max 1–5), respectively. We did not observe a<br />
significant difference according to LEMON law (0.7 ± 0.5 vs. 0.6 ± 0.5<br />
points) or IDS score (2.7 ± 0.5 vs. 2.0 ± 1.9) comparing direct vs. video<br />
laryngoscopy, while C/L grades were significantly different (2.3 ± 1.0 vs.<br />
1.4 ± 0.5, p = 0.04).<br />
RR patients without out-of-hospital airway management<br />
In 136 patients, airway management was initiated first after RR<br />
admission. A tracheotomy tube change was necessary in 2 cases, both<br />
successful at the first attempt. The other patient had been intubated<br />
with first-pass, second-pass, and third-pass intubation success rates<br />
of 70.9% (n = 95), 14.9% (n = 20), and 0.8% (n = 1), respectively.<br />
Overall, 100% of the intubations were successful in mean after 1.3 ± 0.8<br />
intubation attempts (Median: 1, min-max: 1–6). Multiple intubation<br />
attempts were needed in 39 cases (29.1%). The intubation procedure<br />
was handed over to another physician in 14 cases (10.4%), as required<br />
by the institutional ED safety protocol. In the cases handed over,<br />
1.2 ± 0.4 intubations attempts were required for successful intubation by<br />
the next provider (Median 1, min-max: 1–2).<br />
Table 2 Difficult airway characteristics (n = 136)<br />
[n, (%)]<br />
anticipated difficult airway 32 (23.5%)<br />
Table 2 Difficult airway characteristics (n = 136)<br />
LEMON<br />
[n, (%)]<br />
0 points 85 (62.5%)<br />
anticipated difficult airway 32 (23.5%)<br />
LEMON ≥1 point 51 (37.5%)<br />
LEMON<br />
IDS<br />
0 points 85 (62.5%)<br />
0 points 39 (28.8%)<br />
LEMON ≥1 point 51 (37.5%)<br />
1–5 points 81 (59.6%)<br />
IDS<br />
≥ 5 points 16 (11.6%)<br />
0 points 39 (28.8%)<br />
Cormack/Lehane I 59 (43.4%)<br />
1–5 points 81 (59.6%)<br />
II 40 (29.4%)<br />
≥ 5 points 16 (11.6%)<br />
III 23 (16.9%)<br />
Cormack/Lehane I 59 (43.4%)<br />
IV 4 (2.9%)<br />
II 40 (29.4%)<br />
not documented 10 (7.4%)*<br />
III 23 (16.9%)<br />
*including 2 patients with tracheotomy tube exchange<br />
IV 4 (2.9%)<br />
not documented 10 (7.4%)*<br />
desaturation *including 2 (9.3%) patients(Table with tracheotomy 4). The overall tube exchange complication rate was 42.6%.<br />
The complication rates (and mean number of intubations attempts)<br />
increased according to the C/L grade 1, 2, 3 and 4 as following 24%<br />
(1.2 ± 0.5), 25% (1.2 ± 0.4), 24% (1.6 ± 0.8), and 75% (3.3 ± 2.2).<br />
Direct laryngoscopy and video laryngoscopy was used in 69.9%<br />
(n = 94) and 30.1% (n = 40), respectively. Overall, the needed mean<br />
number of intubation attempts in the direct (macintosh blade) and video<br />
laryngoscopy (macintosh-like blade) group with 1.2 ± 0.5 vs. 1.2 ± 0.4<br />
were comparable (p = 0.887).<br />
The percentage of anticipated difficult airways estimated by the acting<br />
physician was 23.5%. The prediction of difficult airways according to<br />
patients with at least one positive LEMON criterion and with an IDS ≥5<br />
points was 37.5 and 11.6%. The difficult airway characteristics of the<br />
patients are presented in Table 2, and the difficulties contributed to<br />
problems during RR intubation procedures were shown in Table 3.<br />
BUHE and supine, as patient positioning for endotracheal intubation,<br />
were used in 50.7% (n = 68) and 44.8% (n = 60), respectively. In order<br />
to optimize the first intubation attempt, stylets, NBA, Jackson’s position,<br />
BURP, and suction units were used in 91.0% (n = 122), 82.1% (n = 110),<br />
70.9% (n = 95), 26.9% (n = 36), and 14.2% (n = 19).<br />
The mean number of needed intubation attempts correlated with the<br />
intubation condition categories “very good/good” and “bad/very bad” with<br />
1.2 ± 0.5 vs. 2.2 ± 1.4 (p = 0.0001) and C/L grade 1/2 and 3/4 (1.2 ± 0.5<br />
vs. 1.8 ± 1.2, p = 0.0002) (Fig. 2). First-pass success was associated with<br />
C/L 1, 2, 3 and 4 with 79.5, 77.5, 56.5, and 25.0%, respectively. Patient<br />
positioning in BUHE or supine did not affect the C/L grade (BUHE vs.<br />
supine: C/L grade 1/2: 78.1 vs. 79.3%; C/L grade 3/4: 21.9 vs. 20.7,<br />
p = 0.873). Direct laryngoscopy compared with video laryngoscopy did<br />
not lead to better C/L grade 1/2 (81.3 vs. 73.9%, p = 0.334).<br />
Complications and adverse events were documented in 129 out of<br />
136 patients (94.9%). The most common complications and adverse<br />
events during RR airway management were hypotension (20.4%) and<br />
Discussion<br />
This prospective single centre study evaluated the out-of-hospital and<br />
ED initiated airway management in adult non-traumatic critically ill<br />
patients in an academic German ED during a one-year observational<br />
period. The primary goal was to evaluate the out-of-hospital airway<br />
management performed by EMS physicians at hospital arrival and to<br />
document the airway management in the RR setting in the ED in order to<br />
describe incidence, airway technique, success and complication rates.<br />
Several ED airway registries exist worldwide (e.g., Australia [8], North<br />
America Table[9, 3 Difficulties 10], Korea [11], contributed Japan [12]), to problems however during data on emergency<br />
resuscitation room intubation procedures (n = 129)<br />
[n, (%)]<br />
Table Secretion/blood 3 Difficulties contributed to problems during 21 (16.3%)<br />
resuscitation room intubation procedures (n = 129)<br />
Reduced mouth opening 12 (9.3%)<br />
[n, (%)]<br />
Short neck 9 (8.5%)<br />
Secretion/blood 21 (16.3%)<br />
Immobilisation 7 (5.4%)<br />
Reduced mouth opening 12 (9.3%)<br />
Untrained personal 7 (5.4%)<br />
Short neck 9 (8.5%)<br />
Retrognathy 4 (3.1%)<br />
Immobilisation 7 (5.4%)<br />
Patient positioning 3 (2.3%)<br />
Untrained personal 7 (5.4%)<br />
Anatomy pharynx/larynx 3 (2.3%)<br />
Retrognathy 4 (3.1%)<br />
Foreign body 1 (1.6%)<br />
Patient positioning 3 (2.3%)<br />
Anatomy neck 0 (0.0%)<br />
Anatomy pharynx/larynx 3 (2.3%)<br />
Malfunction equipment 0 (0.0%)<br />
Foreign body 1 (1.6%)<br />
Anatomy neck 0 (0.0%)<br />
Malfunction equipment 0 (0.0%)<br />
RESUSCITATION TODAY - SUMMER <strong>2019</strong><br />
9
CLINICAL PAPER<br />
Fig. 2 Number of mean intubations attempts according to intubations conditions and Cormack/Lehane grade. MV = mean value,<br />
SD = standard deviation<br />
Fig. 2 Number of mean intubations attempts according to intubations conditions and Cormack/Lehane grade. MV = mean value,<br />
SD = standard deviation<br />
airway management in German EDs are still missing. Thereby, the<br />
introduction of an airway registry is an important issue for quality<br />
assurance [25]. To our knowledge, this is the first study investigating RR<br />
airway management in non- traumatic patients in a German ED setting.<br />
As described in the study protocol only critically ill non-traumatic<br />
patients were investigated in this study and patients with trauma were<br />
excluded. However, this study population may restrict the comparability<br />
of our results to other airway registries [8, 10, 32, 33].<br />
RESUSCITATION TODAY - SUMMER <strong>2019</strong><br />
In patients with out-of-hospital airway management admitted to the RR we<br />
found a low incidence of oesophageal intubation with 1.5% in comparison<br />
to other studies that reported a rate of 5.1–6.7% in German physicianstaffed<br />
EMS [26, 27]. Interestingly, 9.3% of the admitted patients were<br />
treated with a laryngeal tube. According to institutional policy all 14<br />
patients with SADs were intubated immediately after RR admission. In<br />
57% of these SAD patients ventilation was insufficient at RR admission.<br />
Comparable complications and adverse events rates after out-of-hospital<br />
laryngeal tube insertion were also reported elsewhere [28, 29, 30]. One of<br />
the major concerns is that only 82.7% of patients received capnography<br />
in the out-of-hospital setting. Oesophageal intubations, as well as<br />
insufficient ventilation after insertion of a laryngeal tube would likely be<br />
recognized during the out-of-hospital airway management if capnography<br />
would solely have been used [28, 31].<br />
Table 4 Complications during airway management in<br />
resuscitation room (n = 129)<br />
Hypotension (decrease in SBP to < 90 mmHg) 26 (20.2%)<br />
Table 4 Complications during airway management in<br />
desaturation (decrease in oxygen saturation ≥ 10%) 12 (9.3%)<br />
resuscitation room (n = 129)<br />
Hypotension<br />
oesphageal<br />
(decrease<br />
intubation<br />
in SBP to < 90 mmHg) 26<br />
7<br />
(20.2%)<br />
(5.4%)<br />
desaturation aspiration (decrease in oxygen saturation ≥ 10%) 124 (9.3%) (3.1%)<br />
oesphageal endobronchial intubation intubation 7 (5.4%) 2 (1.6%)<br />
aspiration cardiac arrest 4 (3.1%) 4 (3.1%)<br />
endobronchial complicationsintubation 2 (1.6%) 55 (42.6%)<br />
SBP systolic blood pressure<br />
cardiac arrest 4 (3.1%)<br />
complications 55 (42.6%)<br />
SBP systolic blood pressure<br />
In the second part of this investigation, the observed sample size of<br />
136 ED initiated airway procedures in our ED is comparable with those<br />
in other large ED airway registries (including 50–90 cases per year)<br />
[10, 34]. In addition, we investigated RR patients with out-of-hospital<br />
airway management already performed by EMS physicians. However,<br />
16 of theses cases with insufficient ventilation and oxygenation needed<br />
immediate airway management after hospital arrival. The observed<br />
first-pass success rate of the 134 patients receiving invasive airway<br />
management after RR admission was 70.9%. These findings were in<br />
line with previous analysis of ED airway registry reporting a first-pass<br />
success range of 61–94% [7, 8, 10, 33, 34, 35]. However, the first-pass<br />
success rate in this study was lower than in the meta-analysis by Park<br />
et al. [36] founded 84% as an ED benchmark. The aim of improving<br />
first-pass success should be paramount since it is well known that<br />
multiple intubation attempts are associated with significant increases<br />
in complications [6, 7, 12]. The overall airway management success in<br />
this investigation was 100% and comparable with the results of other<br />
airway registries and ED studies [7, 10, 32, 34]. Overall, the airway<br />
of all patients was secured using endotracheal intubation, excluding<br />
two patients with tracheostomy tube change (1.5%). Contrary to other<br />
investigations [10, 25, 32], fiberoptic intubation and cricothyroidotomy<br />
was not performed during the study period. However, with an<br />
anticipated incidence of cricothyroidotomy of 0.3%, it is likely only a<br />
question of time for this procedure to also be seen in our institution.<br />
The intubation procedure was performed in two-thirds of cases using<br />
direct laryngoscopy with Macintosh blades, and less often using C-MAC<br />
video laryngoscopes with Macintosh-like blades. Other investigations<br />
found a comparable rate of video laryngoscopy use in 39–48% [8, 34].<br />
10
CLINICAL PAPER<br />
It is anticipated that the incidence of video laryngoscopy assisted<br />
intubation will increase in the upcoming years [10, 33].<br />
A difficult airway was anticipated in 23.5% of patients receiving RR<br />
airway management. One-third of airways were predicted as difficult<br />
per LEMON law, and a moderate to severe intubation situation was<br />
observed in 11.6% per IDS. These findings were in the range with<br />
data reported from other airway registries [33]. In line with previous<br />
investigations, problems associated with difficulties during ED airway<br />
management were most often secretion or blood in the pharynx,<br />
reduced mouth opening, short neck and immobilization [4]. In<br />
contrast to Khandelwal et al. [20] and Turner et al. [37], we did not<br />
find an association between C/L grade and BUHE or supine position<br />
in ED airway management. Hossfeld et al. [38] reported an improved<br />
visualization using video laryngoscopes (with Macintosh-like blade)<br />
compared to standard Macintosh laryngoscopes. However, in line<br />
with some investigations [39], we found similar C/L grade 1/2 using<br />
video laryngoscopes in comparison to direct laryngoscopy with<br />
standard Macintosh blade.<br />
Complications associated with the intubation procedures were<br />
observed in 42.6%. Other studies reported complication rates<br />
between 10 and 29% [8, 32, 33, 34]. Differences in the reported<br />
complication rates are at least in part due to varying definitions<br />
of complications in other airway registries. Hypotension was the<br />
most common reported complication with 20%, which is in line with<br />
other investigations reporting an incidence of 7–18% [40, 41]. The<br />
incidence of immediately detected and corrected oesophageal<br />
intubations in 5.4% was in line with other ED studies [8, 34].<br />
Immediate recognition of oesophageal intubation using capnography<br />
is imperative to prevent hypoxemia [31]. In the RR, we used<br />
capnography without exception. Desaturation occurred in this study<br />
with 9.3% and which is comparable to other out-of-hospital and ED<br />
airway registries (11–16%) [8, 33, 42].<br />
Our study suffers from several limitations. At first, this study was<br />
carried out at a single institution and so the results cannot be taken<br />
to be representative of all EDs in Germany, or other places in the<br />
world. Nevertheless, this study provided detailed information about<br />
German RR airway management in critically ill non-traumatic patients<br />
for the very first time. Furthermore, the study was observational in<br />
nature, neither randomized nor controlled. The team leader was<br />
required to complete the airway registry form. Reporter bias is difficult<br />
to exclude, and there may be a tendency to document an improved<br />
glottis visualisation and underreport complications. The self-developed<br />
emergency airway registry form was combined with the information<br />
of medical charts, which has been reported to be beneficial [45]. The<br />
team leaders were instructed repeatedly and attempts to improve<br />
accuracy were made by interviewing the ED physicians and by<br />
reviewing the medical record.<br />
Due to the fact that in Germany a multi-centre airway registry does not<br />
exist, we suggest that this should be initiated in order to analyse the<br />
situation countrywide. Studies identified more than eleven emergency<br />
airway registries that sometimes widely differed concerning inclusion<br />
period, inclusion criteria, definition of complications and application of<br />
newer methods of emergency airway management [47]. Comparability<br />
of the reported results and first-pass-success rates is only possible<br />
to a limited extent. Therefore, standardised reporting forms should<br />
be used in order to make the results comparable. Using the data,<br />
benchmarking would be possible, with systematic investigation on<br />
first-pass success, techniques, complications and adverse events.<br />
Moreover, the effect of new techniques in the ED setting concerning<br />
emergency airway management over the years will be detectable as<br />
described by Brown et al. [34]. Using these data, procedural and<br />
structural optimisation of this important field will be possible.<br />
Conclusions<br />
As a limitation of this study, we need to mention that we performed<br />
but did not document specific procedures for preoxygenation<br />
(e.g., delayed sequence intubation using non-invasive ventilation<br />
for preoxygenation [43]) or apnoeic oxygenation [44]. Including<br />
these procedures to further study protocols seems to be necessary.<br />
Moreover, the kind of laryngoscopy (video vs. direct laryngoscopy)<br />
should be documented in further studies. Cardiac arrest as a major<br />
complication during ED airway management occurred in the present<br />
investigation at a rate of 3.1%, which was comparable to other outof-hospital<br />
and ED investigations with a reported range between<br />
1.5–4.4% [8, 34, 45].<br />
Rapid sequence induction using neuromuscular blocking agents was<br />
performed in 87.5% in the RR setting. These findings are in line with<br />
other data from ED airway registries described percentages between<br />
73 and 92% [10, 25, 32, 34]. However, there are other data from<br />
a Japanese ED airway registry stated a lower rate of RSI use with<br />
only 20% [35]. Comparable with other investigations [34], the most<br />
frequent used neuromuscular blocking agent was rocuronium in 85%.<br />
Taking together, the game changer in out-of-hospital airway<br />
management are preoxygenation (e.g. delayed sequence intubation),<br />
using of video laryngoscopy and muscle relaxation [43, 46].<br />
In conclusion, RR airway management of critically ill non-traumatic<br />
patients has substantial challenges. Our study results confirm that<br />
RR airway management is a high-risk procedure. We propose a<br />
nation-wide airway registry to better track outcomes of RR airway<br />
management in the future.<br />
Abbreviations<br />
AM: Airway management; ASA: American Society of Anaesthesiology;<br />
BUHE: Back-up head elevated or supine position; C/L: Cormack/<br />
Lehane score; CINT: Critically ill non-traumatic patients; ED:<br />
Emergency department; EMS: Emergency medical service (in<br />
Germany with emergency doctors and emergency paramedics); IDS:<br />
Intubations’ difficulty scale; LEMON: Look external, evaluate 3–2-2<br />
rule, Malampati score, obstruction, immobilisation; NACA: National<br />
Advisory Committee of Aeronautics; OcEAN: Observation of airway<br />
management in Emergency Department; RR: <strong>Resus</strong>citation room;<br />
SAD: Supraglottic airway device<br />
Acknowledgements<br />
Not applicable<br />
Funding<br />
This study was funded solely by departmental resources.<br />
RESUSCITATION TODAY - SUMMER <strong>2019</strong><br />
11
CLINICAL PAPER<br />
RESUSCITATION TODAY - SUMMER <strong>2019</strong><br />
Availability of data and materials<br />
The datasets used and/or analysed during the current study are<br />
available from the corresponding author on reasonable request.<br />
Authors’ contributions<br />
MB and SNB contributed equally to the manuscript. MB, SNB, TH,<br />
AG and ARZ conceived the study, collected the data, and performed<br />
first and subsequent drafts. MB, SNB, MYD, AG, ARZ performed the<br />
statistical analysis of the data. SP reviewed and constructively criticised<br />
the manuscript. All authors read and approved the final manuscript.<br />
Ethics approval and consent to participate<br />
The OcEAN study was approved by the ethical committee of the<br />
Medical Faculty of the University of Leipzig, Germany (265–14-<br />
25,082,014).<br />
Consent for publication<br />
Not applicable.<br />
Competing interests<br />
The authors declare that they have no competing interests.<br />
Publisher’s Note<br />
Springer Nature remains neutral with regard to jurisdictional claims in<br />
published maps and institutional affiliations.<br />
Author details<br />
†<br />
Michael Bernhard and Sönke N. Bax contributed equally to the<br />
manuscript.. * Correspondence: soenke@bax-se.de; soenke.bax@<br />
paracelsus-kliniken.de. 1 Emergency Department, University Hospital of<br />
Düsseldorf, Düsseldorf, Germany. 2 Emergency Department, University<br />
Hospital of Leipzig, Leipzig, Germany. 3 Working group “Trauma and<br />
<strong>Resus</strong>citation Room Management“, Task Force Emergency Medicine,<br />
German Society of Anaesthesiology and Intensiv care Medizin,<br />
Nürnberg, Germany. 4 Institute for Medical Informatics, Statistics and<br />
Epidemiology (IMISE), University of Leipzig, Leipzig, Germany. 5 Medical<br />
Intensive Care Unit, University Hospital of Leipzig, Leipzig, Germany.<br />
6<br />
Department of Anaesthesiology and Intensive Care Medicine, University<br />
Hospital of Leipzig, Leipzig, Germany. 7 Emergency Department,<br />
Paracelsus Hospital of Henstedt-Ulzburg, Wilstedter Straße 134,<br />
D-24558 Henstedt-Ulzburg, Germany.<br />
References<br />
1. Cook TM, Woodall N, Harper J, Benger J. Fourth National Audit<br />
Project. Major complications of airway management in the UK:<br />
results of the fourth National Audit Project of the Royal College of<br />
Anaesthetists and the difficult airway society. Part 2: intensive care<br />
and emergency departments. Br J Anaesth. 2011;106:632–42.<br />
2. Cook TM, MacDouglas-Davis SR. Complications and failure of<br />
airway management. BJA. 2013;109(Suppl 1):I68–85.<br />
3. Cook TM, Behringer EC, Benger J. Airway management outside the<br />
operating room: hazardous and incompletely studied. Curr Opin<br />
Anesthesiol. 2012;25:461–9.<br />
4. Bernhard M, Mohr S, Weigand MA, Martin E, Walther A. Developing<br />
the skill of endotracheal intubation: implication for emergency<br />
medicine. Acta Anaesthesiol Scand. 2012;56:164–71.<br />
5. Mohr S, Weigand MA, Hofer S, Martin E, Gries A, Walther A,<br />
Bernhard M. Developing the skill of laryngeal mask insertion - a<br />
prospective single center study. Anaesthesist. 2013;62:447–52.<br />
6. Sakles JC, Chiu S, Mosier J, Walker C, Stolz U. The importance of<br />
the first pass success when performing orotracheal intubation in the<br />
emergency department. Acad Emerg Med. 2013;20:71–8.<br />
7. Bernhard M, Becker TK, Gries A, Knapp J, Wenzel V. The first shot<br />
is often the best shot: first-pass intubation success in emergency<br />
airway management. Anesth Analg. 2015;121(5):1389–93.<br />
8. Fogg T, Annesley N, Hitos K, Vassiliadis J. Prospective observational<br />
study of the practice of endotracheal intubation in the emergency<br />
department of a tertiary hospital in Sydney, Australia. Emerg Med<br />
Ausstalas. 2012;24:617–24.<br />
9. Bair AE, Filbin MR, Kulkarni RG, Walls RM. The failed intubation<br />
attempt in the emergency department: analysis of the prevalence,<br />
rescue techniques, and personnel. J Emerg Med. 2002;23(2):131–40.<br />
10. Sagarin MJ, Barton ED, Chng YM, Walls RM on behalf of the<br />
National Emergency Airway Registry (NEAR) Investigators. Airway<br />
management in the US and Canadian emergency medicine<br />
residents: a multicenter analysis of more than 6000 endotracheal<br />
intubations attempts. Ann Emerg Med. 2005;46:328–36.<br />
11. Cho J, Cho YS, You JS, Lee HS, Kim H, Chung HS. Current status<br />
of emergency airway management for elderly patients in Korea:<br />
multicentre study using the Korean emergency airway management<br />
registry. Emerg Med Australas. 2013;25:439–44.<br />
12. Hasegawa K, Shigemitsu K, Hagiwara Y, Chiba T, Watase H, Brown<br />
CA, Brwon DF. Japanese emergency medicine research Alliance<br />
investigators. Association between repeated intubations attempts<br />
and adverse events in emergency department: an analysis of a<br />
multicenter prospective observationsal study. Ann Emerg Med.<br />
2012;60:749–54.<br />
13. Breckwoldt J, Klemstein S, Brunne B, Schnitzer L, Arnzt HR,<br />
Mochmann HC. Expertise in prehospital endotracheal intubation<br />
by emergency medicine physicians – comparing “proficient<br />
performers” and “experts”. <strong>Resus</strong>citation. 2012;83:434–9.<br />
14. Davis DP. The need for standardized data reporting for prehospital<br />
airway management. Crit Care. 2011;15:133.<br />
15. Lossius HM, Sollid SJM, Rehn M, Lockey DJ. Revisiting the value<br />
of pre-hospital tracheal intubation: an all time systematic literature<br />
review extracting the Utstein airway core variables. Crit Care.<br />
2011;15:R26.<br />
16. Sollid SJM, Lockey D. Lossius HM and pre-hospital advanced<br />
airway management expert group: a consensus-based template<br />
for uniform reporting of data from pre-hospital advanced airway<br />
management. Scand J Trauma <strong>Resus</strong> Emeg Med. 2009;17:58.<br />
17. Saklad M. Grading of patients for surgical procedures.<br />
Anesthesiology. 1941;2:281–4.<br />
18. Tryba M, Brüggemann H, Echtermeyer V. Klassifizierung von<br />
Erkrankungen und Verletzungen im Notarztrettungssystemen.<br />
Notfallmedizin. 1980;6:725–7.<br />
19. Teasdale G, Jennet B. Assessment of coma and impaired<br />
consiousness. A practical scale. Lancet. 1974;2:81–4.<br />
20. Khandelwal N, Khorsand S, Mitchell SH, Joffe AM. Head-elevated<br />
patient positioning decreases complications of emergent tracheal<br />
intubation in the Ward and Intensive care unit. Anesth Analg.<br />
2016;122:1101–7.<br />
21. Mallampati SR, Gatt SP, Gugino LD, Desai SP, Waraksa B, Freiberger<br />
D, Liu PL. A clinical sign to predict difficult tracheal intubation: a<br />
prospective study. Can Anaesth Soc J. 1985;32:429–34.<br />
22. Cormack RS, Lehane J. Difficult tracheal intubation in obstetrics.<br />
Anaesthesia. 1984;39:1105–011.<br />
23. Samsoon GL, Young JR. Diffcult tracheal intubation: a retrospective<br />
study. Anaesthesia. 1987;42:487–90.<br />
24. Adnet F, Borron SW, Racine SX, Clemessy JL, Fournier JL, Plaisance<br />
P, Lapandry C. The intubation difficulty scale (IDS). Anesthesiology.<br />
1997;87:1290–7.<br />
12
CLINICAL PAPER<br />
25. Phelan MP, Glauser J, Yuen HW, Sturges-Smith E, Schrump SE.<br />
Airway registry: a performance improvement surveillance project<br />
of emergency department airway management. Am J Med Qual.<br />
2010;25:346–50.<br />
26. Gries A, Sikinger M, Hainer C, et al. Time in care of trauma patients<br />
in the air rescue service: implications for disposition? Anaesthesist.<br />
2008;57:562–70.<br />
27. Timmermann A, Russo SG, Eich C, et al. The out-of-hospital<br />
esophageal and endobronchial intubations performed by<br />
emergency physicians. Anesth Analg. 2007;104:619–23.<br />
28. Bernhard M, Beres W, Timmermann A, Stepan R, Greim CA, Kaisers<br />
UX, Gries A. Prehospital airway management usingthe laryngeal<br />
tube. An emergency department point of view. Anaesthesist.<br />
2014;63:589–96.<br />
29. Bernhard M, Hossfeld B, Kumle B, Becker TK, Böttiger BW, Birkholz<br />
T. Don’t forget to ventilate during cardiopulmonary resuscitation<br />
with mechanical chest compression devices. Eur J Anaesthesiol.<br />
2016;33:553–6.<br />
30. Schalk R, Seeger FH, Mutlak H, et al. Complications associated with<br />
the prehospital use of laryngeal tubes – a systematic analysis of risk<br />
factors and strategies for prevention. <strong>Resus</strong>citation. 2014;85:1629–32.<br />
31. Von Goedecke A, Herff H, Paal P, Dörges V, Wenzel V. Field airway<br />
management disasters. Anesth Analg. 2007;104:481–3.<br />
32. Walls RM, et al. Emergency airway management: a multi-center<br />
report of 8937 emergency department intubations. J Emerg Med.<br />
2011;41:347–54.<br />
33. Fogg T, Alkhouri H, Vassiliadis J. The Royal North Shore Hospital<br />
Emergency Department airway registry: closing the audit loop.<br />
Emerg Med Australisia. 2016;28:27–33.<br />
34. Brown CA, et al. Techniques, success and adverse events of<br />
emergency department adult intubations. Ann Emerg Med.<br />
2015;65:363–70.<br />
35. Hasegawa K, et al. Emergency airway management in Japan:<br />
interim analysis of a multi-center prospective observational study.<br />
<strong>Resus</strong>citation. 2012;83:428–33.<br />
36. Park L, Zeng I, Brainard A. Systematic review and meta-analysis<br />
of first-pass success rate in emergency department intubation:<br />
creating a benchmark for emergency airway care. Emerg Med<br />
Austral. 2017;29:40–8.<br />
37. Turner JS, Ellender TJ, Okonkwo ER, et al. Feasibility of upright<br />
patient positioning and intubation success rates at two academic<br />
emergency departments. Am J Emerg Med. 2017;35:986–92.<br />
38. Hossfeld B, Frey K, Doerges V, Lampl L, Helm M. Improvement in<br />
glottic visualisation by using the C-MAC PM video laryngoscope as<br />
a first-line device for out-of-hospital emergency tracheal intubation.<br />
Eur J Anaesthesiol. 2015;32:425–31.<br />
39. Carlson JN, Crofts J, Walls RM, Brown CA. Direct vs. video<br />
laryngoscopy for intubating adult patients with gastrointestinal<br />
bleeding. West J Emerg Med. 2015;16:1052–6.<br />
40. Newton A, Ratchford A, Khan I. Incidence of adverse events during<br />
prehospital rapid sequence intubation: a review of one year on<br />
the London helicopter emergency medical service. J Trauma.<br />
2008;64:487–92.<br />
41. Rognas L, Hansen TM, Kirkegaard H, Tonnesen E. Pre-hospital<br />
advanced airway management by experienced anaesthesiologists:<br />
a prospective descriptive study. Scand J Trauma <strong>Resus</strong>c Emerg<br />
Med. 2013;21:58.<br />
42. Helm M, Kremers G, Lampl L, Hossfeld B. Incidence of transient<br />
hypoxia during pre-hospital rapid sequence intubation by<br />
anaesthesiologists. Acta Anaesthesiol Scand. 2013;57:199–205.<br />
43. Weingart SD, Trueger S, Wong N, Scofi J, Singh N, Rudolph SS.<br />
Delayed sequence intubation: a prospective observational study.<br />
Ann Emerg Med. 2015;65:349–55.<br />
44. Oliveira LE, Silva L, Cabrera D, Barrionuevo P, et al. Effectiveness<br />
of apneic oxygenation during intubation: a systematic review and<br />
meta-analysis. Ann Emerg Med. 2017;70:483–94.<br />
45. Bloomer R, Burns BJ, Ware S. Improving documentation in<br />
prehospital rapid sequence induction: investigating the use of a<br />
dedicated airway registry form. Emerg Med J. 2013;30:324–6.<br />
46. Hossfeld B, Bein B, Böttiger BW, Bohn A, Fischer M, Gräsner JT,<br />
Hinkelbein J, Kill C, Lott C, Popp E, Rössler M, Schaumberg A,<br />
Wenzel A, Bernhard M. Recommended practice for out-of-hospital<br />
emergency anaesthesia in adults. Statement from the out-of-hospital<br />
emergency Anaesthesia working Group of the Emergency Medicine<br />
Research Group of the German Society of Anaesthesiology and<br />
Intensive Care. Eur J Anaesthesiol. 2016;33:881–97.<br />
47. Girrbach FF, Hilbig F, Michael M, Bernhard M. Systematic analysis of<br />
airway registries in emergency medicine. Anaesthesist. 2018;67:664–73.<br />
WHY NOT WRITE FOR US?<br />
<strong>Resus</strong>citation <strong>Today</strong> welcomes the submission of<br />
clinical papers, case reports and articles that you<br />
feel will be of interest to your colleagues.<br />
The publication is mailed to all resuscitation, A&E and anaesthetic departments<br />
plus all intensive care, critical care, coronary care and cardiology units.<br />
All submissions should be forwarded to info@mediapublishingcompany.com<br />
If you have any queries please contact the publisher Terry Gardner via:<br />
info@mediapublishingcompany.com<br />
RESUSCITATION TODAY - SUMMER <strong>2019</strong><br />
13
The new corpuls cpr has redefined the standard for the next generation<br />
of chest compression devices used by the emergency services and<br />
hospitals.<br />
PROTECT YOUR AMBULANCE CREW<br />
USER FRIENDLY<br />
The corpuls cpr has the capability of being able to<br />
supply fully automated chest compressions, ensuring less<br />
strain on rescue workers, particularly when performed in<br />
a moving vehicle. The corpuls cpr is able to check its<br />
position of the compression pad after each ventilation<br />
break or 100 compressions (in continuous mode) to<br />
compensate for any impact cpr has on the patient’s<br />
thorax.<br />
The corpuls cpr comes with clearly visible colour<br />
display and easy to access control panel buttons.<br />
The compression depth and/or rate, can be manually<br />
adjusted when required.<br />
LOW RUNNING COSTS<br />
REUSABLE COMPRESSION PADS<br />
The compression pads come in two sizes and can be disinfected with all common agents, keeping running costs to a<br />
minimum. This ensures that the corpuls cpr can be deployed on every CPR job without financial impact.
The Tireless Arm that<br />
saves lives<br />
NEW CASE STUDIES AVAILABLE<br />
corpuls cpr compliant to current ERC/AHA guidelines.<br />
sales@theortusgroup.com www.theortusgroup.com T: +44 0845 4594705
Introducing<br />
The first infant manikin that helps you visualise the effects of CPR<br />
- both for compressions and ventilations.<br />
Illuminating<br />
Infant CPR<br />
Seeing is<br />
believing<br />
Developed with the help of<br />
European infant resuscitation<br />
experts. Brayden Baby is ideal for<br />
Paediatric BLS, EPALS and EPILS<br />
Launched at the <strong>2019</strong> European Paediatric <strong>Resus</strong>citation & Emergency<br />
Medicine Congress (PREM) in Ghent last month, Brayden Baby received a<br />
great deal of interest as it obviously fulfils and unmet need.<br />
There were queues to participate in the demonstration workshops over the<br />
two-day event, run by Liesje Andre, <strong>Resus</strong>citation Lead for Great Ormond<br />
Street Hospital for Children (to 2018) and Dr Jonathan Smart of Innosonian<br />
Europe.<br />
Ms Andre stated, ‘It was a privilege to be asked to help with the development<br />
of the Brayden Baby manikin. Having taught paediatric resuscitation in<br />
acute NHS hospitals for over 25 years, I wanted a manikin that could provide<br />
feedback for both effective chest compressions and ventilation. This new<br />
infant manikin does just that. It provides the student with intuitive lights to<br />
enable them to visualise the correct technique for quality chest compressions<br />
as well as ventilation… I do believe the Brayden Baby is a game changer for<br />
teaching good quality infant CPR’.<br />
Brayden Baby’s unique features include intuitive lights that provide real-time<br />
feedback for ventilation training. The lights indicate when ventilations are<br />
correctly delivered (volume and speed) and there is realistic chest rise. The<br />
lights also indicate when the value delivered is too large and delivered too<br />
quickly.<br />
In addition, the Brayden Baby has lights providing real-time feedback for<br />
chest compressions (depth, rate, recoil and finger/thumb position).<br />
The head positioning to open the airway in the correct neutral position,<br />
jaw thrust open and interconnected mouth and nose, and large occiput<br />
realistically mimic a baby. The Brayden Baby also has lights to indicate<br />
chest compression quality and work in the same way as the awardwinning<br />
Brayden adult manikin. Compression depth, rate, release and<br />
finger/thumb position are measured and when correct, the head quality<br />
light illuminates. Both sets of lights help guide the student to perform<br />
good quality infant CPR.<br />
In the UK, the response to Brayden Baby has been equally positive. Kevin<br />
Mackie, Lead Educator, <strong>Resus</strong>citation Council (UK), states, ‘In my opinion,<br />
the Brayden Baby manikin is the best infant BLS Manikin on the market today.<br />
CONTACT US TO FIND OUT MORE<br />
Tel: 01252 344007 |<br />
braydenbaby@welmedical.com<br />
www.welmedical.com<br />
From an educational perspective, the importance of objective feedback<br />
cannot be underestimated in improving performance of CPR.<br />
‘The Brayden Baby gives the usual visual feedback on compression rate, depth,<br />
position and recoil, but also now features additional lights that indicate rate<br />
and volume of ventilation. The ventilation resistance is the most realistic I have<br />
felt, and airway positioning is realistic and allows for jaw thrust to be added<br />
with ease. It is evident that a lot of thought has been put into the development<br />
of this manikin and it represents a significant contribution to the infant BLS<br />
training market.’<br />
Brayden Baby is now available across Europe and will demonstrated at<br />
various international educational workshops to help improve the quality<br />
of infant CPR.<br />
Jaw thrust manoeuvre<br />
For more information contact paul.mulvey@welmedical.com<br />
Correct Ventilation<br />
See the video at www.welmedical.com/baby-brayden-advanced
CLINICAL PAPER<br />
REPEATED VITAL SIGN MEASUREMENTS IN<br />
THE EMERGENCY DEPARTMENT PREDICT<br />
PATIENT DETERIORATION WITHIN 72 HOURS:<br />
A PROSPECTIVE OBSERVATIONAL STUDY<br />
Vincent M. Quinten 1* , Matijs van Meurs 2,3 , Tycho J. Olgers 1 , Judith M. Vonk 4 , Jack J. M. Ligtenberg 1<br />
and Jan C. ter Maaten 1<br />
Reproduced with permission from the Scandinavian Journal of Trauma, <strong>Resus</strong>citation and Emergency Medicine. (2018) 26:57 doi: 10.1186/s13049-018-0525-y<br />
Abstract<br />
Background<br />
More than one in five patients presenting to the emergency department<br />
(ED) with (suspected) infection or sepsis deteriorate within 72 h from<br />
admission. Surprisingly little is known about vital signs in relation<br />
to deterioration, especially in the ED. The aim of our study was to<br />
determine whether repeated vital sign measurements in the ED can<br />
differentiate between patients who will deteriorate within 72 h and<br />
patients who will not deteriorate.<br />
Methods<br />
We performed a prospective observational study in patients presenting<br />
with (suspected) infection or sepsis to the ED of our tertiary care<br />
teaching hospital. Vital signs (heart rate, mean arterial pressure (MAP),<br />
respiratory rate and body temperature) were measured in 30-min<br />
intervals during the first 3 h in the ED. Primary outcome was patient<br />
deterioration within 72 h from admission, defined as the development<br />
of acute kidney injury, liver failure, respiratory failure, intensive care unit<br />
admission or in-hospital mortality. We performed a logistic regression<br />
analysis using a base model including age, gender and comorbidities.<br />
Thereafter, we performed separate logistic regression analyses for each<br />
vital sign using the value at admission, the change over time and its<br />
variability. For each analysis, the odds ratios (OR) and area under the<br />
receiver operator curve (AUC) were calculated.<br />
Results<br />
In total 106 (29.5%) of the 359 patients deteriorated within 72 h from<br />
admission. Within this timeframe, 18.3% of the patients with infection and<br />
32.9% of the patients with sepsis at ED presentation deteriorated. Associated<br />
with deterioration were: age (OR: 1.02), history of diabetes (OR: 1.90), heart<br />
rate (OR: 1.01), MAP (OR: 0.96) and respiratory rate (OR: 1.05) at admission,<br />
changes over time of MAP (OR: 1.04) and respiratory rate (OR: 1.44) as well<br />
as the variability of the MAP (OR: 1.06). Repeated measurements of heart<br />
rate and body temperature were not associated with deterioration.<br />
Conclusions<br />
Repeated vital sign measurements in the ED are better at identifying<br />
patients at risk for deterioration within 72 h from admission than single<br />
vital sign measurements at ED admission.<br />
Keywords: Accident & emergency medicine; Patient deterioration;<br />
Sepsis; Vital signs<br />
Background<br />
More than one in five patients presenting to the emergency department<br />
(ED) with (suspected) infection or sepsis deteriorate within 72 h from<br />
admission, despite treatment [1]. Recent advances in research have<br />
improved our understanding of the pathophysiology of sepsis [2]. The<br />
adoption of surviving sepsis campaign (SSC) guidelines, increased<br />
awareness and early goal-directed therapy dramatically reduced sepsisrelated<br />
mortality over the past two decades [3, 4]. However, one of the<br />
main challenges for the physician in the ED remains to determine the<br />
risk of deterioration for the individual patient [2]. The numerous sepsisrelated<br />
biomarkers lack sensitivity and specificity for deterioration and<br />
are not readily available in the ED [5, 6, 7]. Despite the relative ease of<br />
measurement, surprisingly little is known about vital signs in relation<br />
to clinical outcomes, especially in the ED setting [8, 9, 10, 11]. There<br />
is limited evidence that oxygen saturation and consciousness level<br />
at ED arrival are associated with mortality, and that heart rate and<br />
Glasgow coma scale (GCS) are associated with intensive care unit<br />
(ICU) admission [9, 11]. For all other vital signs, insufficient evidence<br />
is available [9, 11]. The few available studies mostly studied vital<br />
signs used in triage systems or vital signs obtained at the time of ED<br />
admission [9, 12]. Almost one third of the medical patients who arrive at<br />
the ED with normal vital signs show signs of deterioration in vital signs<br />
within 24 h [13]. Our pilot study in the ED showed that vital signs change<br />
significantly during the patient’s stay in the ED [7]. However, surprisingly<br />
little is known on how to monitor and identify deteriorating patients in the<br />
emergency department [13]. The latest SSC guidelines recommend a<br />
thorough re-evaluation of routinely measured vital signs as parameter<br />
for response to treatment [4]. Therefore, the aim of the current study<br />
was to determine whether repeated vital sign measurements during<br />
the patient’s stay in the ED can distinguish between patients who will<br />
deteriorate within 72 h from admission and patients who will not.<br />
RESUSCITATION TODAY - SUMMER <strong>2019</strong><br />
17
CLINICAL PAPER<br />
Methods<br />
Study design and setting<br />
This study is a predefined prospective observational study, part of the<br />
Sepsis Clinical Pathway Database (SCPD) project in our emergency<br />
department (ED). The SCPD project is a prospective cohort study of<br />
medical patients presenting to the ED with fever and/or suspected<br />
infection or sepsis. Data was collected in the ED of the University<br />
Medical Center Groningen in The Netherlands, an academic tertiary<br />
care teaching hospital with over 30,000 ED visits annually.<br />
oxygen supplementation [7]. The protocol did not change during the<br />
inclusion period and was not influenced by the patient’s participation<br />
in the study. For patients arriving at the ED with EMS and (suspected)<br />
sepsis, treatment with fluid resuscitation and supplementary oxygen was<br />
started in the ambulance by EMS personnel according to the nationwide<br />
EMS guidelines for sepsis in The Netherlands [14]. The average time<br />
from EMS dispatch call to ED arrival is 40 min in The Netherlands, but<br />
actual dispatch times in this study were not measured [14]. Pre-hospital<br />
start of treatment was not influenced by the patient’s participation in the<br />
study.<br />
RESUSCITATION TODAY - SUMMER <strong>2019</strong><br />
This study was carried out in accordance with the Declaration of<br />
Helsinki, the Dutch Agreement on Medical Treatment Act and the<br />
Dutch Personal Data Protection Act. The Institutional Review Board of<br />
the University Medical Center Groningen ruled that the Dutch Medical<br />
Research Involving Human Subjects Act is not applicable for this study<br />
and granted a waiver (METc 2015/164). All participants provided written<br />
informed consent.<br />
Study population<br />
Data was collected between March 2016 and February 2017.<br />
Consecutive medical patients visiting the ED between 8 a.m. and 23<br />
p.m. were screened for eligibility. Inclusion criteria were: (1) age of 18<br />
years or older, (2) fever (> = 38 °C) or suspected infection or sepsis,<br />
(3) able to provide written informed consent. The clinical suspicion<br />
of infection or sepsis was judged by the coordinating internist acute<br />
medicine on duty. He/she handles all medical patient announcements<br />
from general practitioners or the emergency medical services (EMS),<br />
and medical patients that enter the ED without previous announcement.<br />
The judgement was based on information provided over the phone<br />
during the announcement, information obtained at triage and<br />
immediately after ED admission of the patient. Only patients with at least<br />
three repeated vital sign measurements during their first 3 h in the ED<br />
were included in the final analysis.<br />
Data collection<br />
The data collected in the SCPD project includes socio-demographic<br />
information, patient history, prescription drug usage, comorbidity,<br />
treatment parameters, results from routine blood analysis,<br />
questionnaires about activities of daily living, follow-up during the<br />
patient’s stay in the hospital and registration of various endpoints. The<br />
data was collected by trained members of our research staff during<br />
the patient’s stay in the ED and combined with data from the patient’s<br />
medical record for follow-up during the patient’s stay in the hospital.<br />
For the current study, next to the data collected for all patients included<br />
in the SCPD project, we repeatedly measured vital signs in 30-min<br />
intervals during the patient’s stay in de ED. These vital signs included<br />
heart rate, respiratory rate and blood pressure, measured using a<br />
Philips MP30 or MX550 bed-side patient monitor (Philips IntelliVue<br />
System with Multi-Measurement Module; Philips, Eindhoven, The<br />
Netherlands). Furthermore, the body temperature was measured using<br />
an electronic tympanic ear thermometer (Genius 2; Mountainside<br />
Medical Equipment, Marcy, New York, USA).<br />
All patients received treatment for infection or sepsis as per our<br />
hospital’s standardized protocol at the treating physician’s discretion.<br />
This protocol included intravenous antibiotics, fluid resuscitation and<br />
Endpoints and definitions<br />
The primary endpoint was patient deterioration within 72 h from ED<br />
admission. We defined patient deterioration as the development of<br />
organ dysfunction, ICU admission or death during the patient’s stay in<br />
the hospital. For organ dysfunction, we distinguished between acute<br />
kidney failure (AKI), liver failure and respiratory failure. AKI was defined<br />
using the Kidney Disease Improving Global Outcomes (KDIGO) criteria<br />
as an increase in serum creatinine by 26.5 μmol/L (0.3 mg/dL) within<br />
48 h or 1.5 times the baseline (known or presumed to have occurred<br />
within the prior 7 days) [15]. Liver failure was defined as total bilirubin<br />
level > 34.2 μmol/L (2.0 mg/dL) and either alkaline phosphatase or a<br />
transaminase level above twice the normal limit [16]. Respiratory failure<br />
was defined as the need for mechanical ventilation, or either hypoxemia<br />
(PaO 2<br />
< 8.0 kPa) or hypercapnia (PaCO 2<br />
> 6.5 kPa) in the arterial blood<br />
gas analysis, or a peripheral oxygen saturation < 90% when breathing<br />
ambient air or < 95% with at least 2 L/min of oxygen supplementation<br />
[17]. In-hospital mortality was defined as all-cause mortality during the<br />
patient’s stay in the hospital. The Sepsis-2 criteria (2001 international<br />
sepsis definitions conference) were used to define sepsis, severe<br />
sepsis or septic shock, i.e. two or more systemic inflammatory response<br />
syndrome criteria and suspected/confirmed infection [18].<br />
Statistical analysis<br />
Continuous data were reported as median with interquartile range (IQR)<br />
and analysed using the Mann-Whitney U test. Categorical data were<br />
summarized as counts with percentages and analysed using the Chisquare<br />
test.<br />
For each vital sign and for each patient, we used the repeated<br />
measurements to estimate the linear change and variability over<br />
time. Linear change over time was estimated using individual linear<br />
regression analysis separately for each vital sign (heart rate, respiratory<br />
rate, mean arterial pressure and temperature) with the time of the<br />
measurement (in minutes) as independent variable. The resulting<br />
regression estimates for time, indicate the linear change per minute<br />
for each patient and each vital sign. The variability of each vital sign<br />
was calculated as the difference between the highest and lowest value<br />
during the first 3 h in the ED.<br />
To analyse the added value of the linear change and variability over time<br />
of each vital sign as predictors for patient deterioration within 72 h, we<br />
performed multiple logistic regression analysis. First, we constructed a<br />
base model containing age, gender and comorbidity. The added value<br />
of each vital sign to the base model was assessed using the following<br />
logistic regression analyses: (1) base model + vital sign value at<br />
admission, (2) base model + vital sign value at admission + change of<br />
the vital sign during the first 3 h in the ED and (3) base model + vital<br />
18
CLINICAL PAPER<br />
Fig. 1 Flow chart of patient recruitment. Consecutive adult medical patients visiting the emergency department of the University Medical Center<br />
Groningen between March 2016 and February 2017 were screened for eligibility<br />
sign value at admission + variability of the vital sign during the first 3 h<br />
in the ED. For each model, the area under the receiver operator curve<br />
(AUC) was calculated using the predicted probabilities.<br />
All statistical analyses were performed using IBM SPSS Statistics for<br />
Windows V.23.0 (IBM Corp, Armonk, New York, USA). A two-tailed<br />
p-value of < 0.05 was considered significant.<br />
Results<br />
Patient characteristics<br />
During the study period 366 patients met the inclusion criteria (Fig.<br />
1). Seven patients were excluded because they had less than three<br />
repeated vital sign measurements in the emergency department<br />
(ED) during the first 3 h from admission. The remaining 359 patients<br />
were included in the final analysis. Of the 359 patients, 106 (29,5%)<br />
patients deteriorated within 72 h from admission (Table 1). Patients<br />
with cardiac disease (p = 0.004), COPD (p = 0.047) or diabetes<br />
(p = 0.002), deteriorated more often compared to patients without these<br />
comorbidities. Malignancy (28.4%) and organ transplant (26.7%) were<br />
the most frequent comorbidities (Table 2).<br />
Patient deterioration<br />
Signs of organ failure were observed in 21.2% of the patients at ED<br />
admission (Table 3). An additional 6.1% of the patients deteriorated<br />
in the first 24 h after admission. The increase in respiratory failure<br />
(+ 4.2%) was the largest contributor to this deterioration. In the first 48<br />
h after admission, 3.1% of the patients deteriorated to multiple organ<br />
failure. Most deterioration took place within the first 72 h from admission<br />
(+ 8.3%), with only a small increase (+ 1.7%) during the rest of the<br />
hospitalization.<br />
RESUSCITATION TODAY - SUMMER <strong>2019</strong><br />
19
CLINICAL PAPER<br />
RESUSCITATION TODAY - SUMMER <strong>2019</strong><br />
Table 1 Patient characteristics<br />
Overall Not deteriorated Deteriorated p Value<br />
Number of patients [n (%)] 359 (100) 253 (70.5) 106 (29.5) –<br />
Demographics<br />
Age [median (IQR)] 63 (49; 71) 60 (47; 70) 66 (56; 74) .001*<br />
Male [n (% of the group)] 222 (61.8) 149 (58.9) 73 (68.9) .076<br />
Comorbidity<br />
Number of comorbidities [median (IQR)] 1 (0; 2) 1 (0; 2) 1 (1; 2) .001*<br />
Cardiac disease [n (% of the group)] 66 (18.4) 37 (14.6) 29 (27.4) .004*<br />
COPD [n (% of the group)] 23 (6.4) 12 (4.7) 11 (10.4) .047*<br />
Diabetes [n (%of the group)] 63 (17.5) 34 (13.4) 29 (27.4) .002*<br />
Chronic kidney disease [n (% of the group)] 43 (12.0) 26 (10.3) 17 (16.0) .125<br />
Chronic liver disease [n (% of the group)] 30 (8.4) 19 (7.5) 11 (10.4) .370<br />
Organ transplant [n (% of the group)] 96 (26.7) 64 (25.3) 32 (30.2) .339<br />
Malignancy [n (% of the group)] 102 (28.4) 77 (30.4) 25 (23.6) .189<br />
None of the above [n (% of the group)] 98 (27.3) 81 (32.0) 17 (16.0) .002*<br />
Disease severity<br />
Infection [n (% of overall)] 82 (22.8) 67 (81.7) 15 (18.3) .011*<br />
Sepsis [n (% of overall)] 277 (77.2) 186 (67.1) 91 (32.9) .011*<br />
Vital signs at ED admission<br />
Heart rate (bpm) [median (IQR)] 95 (83.0; 110.0) 95.0 (82.0; 110.0) 95.5 (83.0; 110.0) .262<br />
Mean arterial pressure (mmHg) [median (IQR)] 91.7 (83.3; 102.9) 94.3 (86.3; 103.3) 85.8 (73.4; 97.3)
CLINICAL PAPER<br />
Table 2 Study population comorbidity matrix<br />
N = 359 Cardiac disease COPD Diabetes Chronic Kidney Disease Chronic Liver Disease Organ Transplant Malignancy<br />
Cardiac disease 66 10 15 13 3 16 17<br />
Table COPD 2 Study population comorbidity matrix 23 3 1 1 4 5<br />
Diabetes N = 359 Cardiac disease COPD Diabetes 63 7Chronic Kidney Disease 9Chronic Liver Disease 17 Organ Transplant 11 Malignancy<br />
Chronic Cardiac disease Kidney Disease 66 10 15 43 13 23 29 16 417<br />
Chronic COPD Liver Disease 23 3 1 30 1 11 4 35<br />
Organ Diabetes Transplant 63 7 9 96 17 21 11<br />
Malignancy Chronic Kidney Disease 43 2 29 102 4<br />
Chronic Liver Disease 30 11 3<br />
Organ Transplant 96 21<br />
Age Malignancy and diabetes associated with higher risk of deterioration<br />
The logistic regression base model for patient deterioration including<br />
age, gender and comorbidities yielded an AUC of 0.679 (Table 4). A<br />
higher age (odds ratio (OR): 1.02 / year) and a history of diabetes (OR:<br />
of deterioration (Table 4, Fig. 2). A higher MAP at ED admission 102 was<br />
associated with a lower risk of deterioration (OR: 0.96/mmHg; model<br />
MAP-M1; AUC .746). The body temperature at ED admission was not<br />
independently associated with deterioration (model BT-M1; AUC .680).<br />
1.90) were associated with a higher risk of patient deterioration. Gender<br />
and comorbidities other than diabetes were not independent predictors<br />
of deterioration.<br />
Repeated vital sign measurements improve the prediction of<br />
deterioration<br />
Next to the vital signs at ED admission, the change and variability<br />
Vital signs at ED admission are associated with deterioration<br />
Patients who deteriorated had a lower MAP (p < 0.001) and a higher<br />
respiratory frequency (p = 0.03) at ED admission (Table 1). The base<br />
model extended with the patient’s vital signs at ED admission, showed<br />
that both a higher heart rate (OR: 1.01/beat per minute; model HRof<br />
the repeated vital signs measurements in the first 3 h in the<br />
ED were entered into the base model together with the vital signs<br />
at ED admission (Table 4, Fig. 2). An increase in MAP over time<br />
was associated with a lower risk of deterioration (OR: 0.873/unit<br />
increase; model MAP-M2; AUC .758). An increase in respiratory<br />
M1; AUC .683) and a higher respiratory rate (OR: 1.05/respiration per rate over time was associated with a higher risk of deterioration<br />
Table 3 Patient deterioration outcomes in different timeframes during the patient’s stay in-hospital and divided by infection and<br />
minute; model RR-M1; AUC .663) were associated with a higher risk (OR: 1.441/unit increase; model RR-M2; AUC .686). The changes in<br />
sepsis on emergency department presentation<br />
Acute Liver Respiratory Organ failure<br />
ICU Inhospital<br />
Deteriorated<br />
Kidney failure failure<br />
admission<br />
Single Multiple<br />
Table 3 Patient deterioration Injury outcomes in different timeframes during the patient’s stay in-hospital and divided mortality by infection and<br />
sepsis Total (N on = 359, emergency 100.0%) department presentation<br />
At ED admission Acute 45 (12.5%) Liver 21 (5.8%) 14 Respiratory (3.9%) 72 Organ (20.1%) failure 4 (1.1%) – ICU – Inhospital<br />
76 Deteriorated (21.2%)<br />
Kidney failure failure<br />
admission<br />
24 h after ED admission 51 (14.2%) 22 (6.1%) 29 (8.1%) 82<br />
Single<br />
(22.8%) 10<br />
Multiple<br />
Injury<br />
(2.8%) 16 (4.5%) 1 mortality (0.3%) 98 (27.3%)<br />
Total 48 (N h after = 359, ED100.0%)<br />
admission 57 (15.9%) 23 (6.4%) 33 (9.2%) 83 (23.1%) 15 (4.2%) 18 (5.0%) 1 (0.3%) 102 (28.4%)<br />
72 At ED h after admission ED admission 60 45 (16.7%) (12.5%) 23 21 (6.4%) (5.8%) 35 14 (9.7%) (3.9%) 87 72 (24.2%) (20.1%) 15 4 (1.1%) (4.2%) x – 18 (5.0%) – 3 (0.8%) 76 106 (21.2%) (29.5%)<br />
24 Until h after hospital ED admission discharge 51 70 (14.2%) (19.5%) 22 26 (6.1%) (7.2%) 29 43 (8.1%) (12.0%) 82 87 (22.8%) (24.2%) 10 24 (2.8%) (6.7%) xx 16 22 (4.5%) (6.1%) 12 (0.3%) (3.3%) 98 112 (27.3%) (31.2%)<br />
Infection 48 h after (N = ED82, admission 22.8%)<br />
72 At ED h after admission ED admission<br />
57 (15.9%)<br />
606 (7.3%) (16.7%)<br />
23 (6.4%)<br />
23 4 (4.9%) (6.4%)<br />
33 (9.2%)<br />
353 (3.7%) (9.7%)<br />
83 (23.1%)<br />
87 11 (24.2%) (13.4%)<br />
15 (4.2%)<br />
151 (1.2%) (4.2%) x 18 (5.0%)<br />
– 18 (5.0%)<br />
1 (0.3%)<br />
– 3 (0.8%)<br />
102 (28.4%)<br />
12 106 (14.6%) (29.5%)<br />
24 Until h after hospital ED admission discharge 70 (8.5%) (19.5%) 426 (4.9%) (7.2%) 43 (4.9%) (12.0%) 11 87 (13.4%) (24.2%) 24 (2.4%) (6.7%) xx 22 (2.4%) (6.1%) 012 (0.0%) (3.3%) 15 112 (18.3%) (31.2%)<br />
Infection 48 h after (N = ED82, admission 22.8%) 7 (8.5%) 4 (4.9%) 5 (6.1%) 12 (14.6%) 2 (2.4%) 2 (2.4%) 0 (0.0%) 15 (18.3%)<br />
72 At ED h after admission ED admission 76 (8.5%) (7.3%) 4 (4.9%) 53 (6.1%) (3.7%) 12 11 (14.6%) (13.4%) 21 (2.4%) (1.2%) 2 – (2.4%) 0 – (0.0%) 15 12 (18.3%) (14.6%)<br />
Until 24 h after hospital ED admission discharge 10 7 (8.5%) (12.2%) 64 (7.3%) (4.9%) 64 (7.3%) (4.9%) 14 11 (17.1%) (13.4%) 24 (2.4%) (4.9%) 23 (2.4%) (6.7%) 01 (0.0%) (1.2%) 15 18 (18.3%) (22.0%)<br />
Sepsis 48 h(N after = 277, ED 77.2%) admission<br />
At 72 ED h after admission ED admission<br />
7 (8.5%)<br />
739 (8.5%) (14.1%)<br />
4 (4.9%)<br />
417 (4.9%) (6.1%)<br />
5 (6.1%)<br />
511 (6.1%) (4.0%)<br />
12 (14.6%)<br />
12 61 (14.6%) (22.0%)<br />
2 (2.4%)<br />
23 (2.4%) (1.1%)<br />
2 (2.4%)<br />
– 2 (2.4%)<br />
0 (0.0%)<br />
– 0 (0.0%)<br />
15 (18.3%)<br />
64 15 (23.1%) (18.3%)<br />
24 Until h after hospital ED admission discharge 44 10 (15.9%) (12.2%) 18 6 (7.3%) (6.5%) 25 6 (7.3%) (9.0%) 71 14 (25.6%) (17.1%) 84 (2.9%) (4.9%) 14 3 (6.7%) (5.1%) 1 (0.4%) (1.2%) 83 18 (30.0%) (22.0%)<br />
Sepsis 48 h(N after = 277, ED 77.2%) admission 50 (18.1%) 19 (6.9%) 28 (10.1%) 71 (25.6%) 13 (4.7%) 16 (5.8%) 1 (0.4%) 87 (31.4%)<br />
72 At ED h after admission ED admission 53 39 (19.1%) (14.1%) 19 17 (6.9%) (6.1%) 30 11 (10.8%) (4.0%) 75 61 (27.1%) (22.0%) 13 3 (1.1%) (4.7%) x – 16 (5.8%) – 3 (1.1%) 64 91 (23.1%) (32.9%)<br />
24 Until h after hospital ED admission discharge 44 60 (15.9%) (21.7%) 18 20 (6.5%) (7.2%) 25 37 (9.0%) (13.4%) 71 73 (25.6%) (26.4%) 820 (2.9%) (7.2%) xx 14 19 (5.1%) (6.9%) 11 (0.4%) (4.0%) 83 94 (30.0%) (33.9%)<br />
ED: 48 emergency h after EDdepartment; admission x of which 50 (18.1%) one patient19 with (6.9%) all three organ 28 (10.1%) systems failing; 71 (25.6%) xx of which four 13 (4.7%) patient with all 16 three (5.8%) organ systems 1 (0.4%) failing 87 (31.4%)<br />
72 h after ED admission 53 (19.1%) 19 (6.9%) 30 (10.8%) 75 (27.1%) 13 (4.7%) x 16 (5.8%) 3 (1.1%) 91 (32.9%)<br />
Until hospital discharge 60 (21.7%) 20 (7.2%) 37 (13.4%) 73 (26.4%) 20 (7.2%) xx 19 (6.9%) 11 (4.0%) 94 (33.9%)<br />
ED: emergency department; x of which one patient with all three organ systems failing; xx of which four patient with all three organ systems failing<br />
RESUSCITATION TODAY - SUMMER <strong>2019</strong><br />
21
CLINICAL PAPER<br />
RESUSCITATION TODAY - SUMMER <strong>2019</strong><br />
Table 4 Logistic regression models for deterioration within 72 h from admission based on repeated vital sign measurements with a<br />
30-min interval during the first 3 h of ED admission<br />
heart rate and temperature were not independently associated with<br />
deterioration.<br />
Next to the vital signs at ED admission and change over time, a higher<br />
variability in MAP (i.e. a higher range) was significantly associated with a<br />
higher risk of deterioration (OR: 1.06/mmHg; model MAP-M3; AUC .800;<br />
Table 4, Fig. 2). The variability of the other vital signs was not associated<br />
with the risk of deterioration.<br />
Sig. Odds Ratio (95%<br />
CI)<br />
Discussion<br />
Model statistics<br />
Cox & Snell R 2 AUC (95% CI) N a<br />
Base model for deterioration within 72 h from admission .080 .679 (.619; .739) 359 (100%)<br />
Age .012* 1.022 (1.005; 1.039)<br />
Gender (0 = male, 1 = female) .502 0.839 (0.502; 1.402)<br />
Cardiac disease .158 1.544 (0.845; 2.820)<br />
COPD .159 1.906 (0.777; 4.676)<br />
Diabetes .035* 1.902 (1.048; 3.454)<br />
Chronic kidney disease .308 1.475 (0.699; 3.111)<br />
Chronic liver disease .345 1.493 (0.650; 3.429)<br />
Organ transplant .245 1.408 (0.791; 2.509)<br />
Malignancy .450 0.807 (0.463; 1.407)<br />
Base model with heart rate<br />
HR-M1. Heart rate at admission .042* 1.013 (1.000; 1.025) .091 .683 (.623; .742) 359 (100%)<br />
HR-M2. Heart rate at admission .035* 1.015 (1.001; 1.030) .091 .684 (.624; .743) 358 (99.7%)<br />
Heart rate change .463 1.039 (0.938; 1.151)<br />
HR-M3. Heart rate at admission .062 1.013 (0.999; 1.027) .091 .683 (.624; .743) 359 (100%)<br />
Heart rate variability .884 0.998 (0.977; 1.021)<br />
Base model with mean arterial pressure<br />
MAP-M1. MAP at admission
CLINICAL PAPER<br />
Fig. 2 Receiver operating curves of the logistic regression models for patient deterioration using various repeated vital sign measurements in 30-min<br />
intervals during the first three hours of the patient’s stay in the emergency department. The base model includes age, gender and comorbidities.<br />
Model M1 contains the base model combined with the value of the vital sign at admission, model M2 contains model M1 combined with the change<br />
of the vital sign over time, model M3 contains model M1 combined with the variability of the vital. A) the ROC curve for the base model combined<br />
with heart rate (HR). B) the ROC curve for the base model combined with mean arterial pressure (MAP). C) the ROC curve for the base model<br />
combined with respiratory rate (RR). * Base model only including patients with respiratory rate at admission (AUC .638). D) the ROC curve for the base<br />
model combined with body temperature (BT)<br />
deterioration. Inclusion of repeated MAP measurements resulted in the<br />
largest AUC (.800), whereas repeated respiratory rate measurements<br />
only slightly improved the predictive capabilities of the logistic<br />
regression model over the base model. Repeated measurements of<br />
heart rate and body temperature were not associated with patient<br />
deterioration.<br />
associated with patient deterioration in ED patients with infection or<br />
sepsis. This suggests that keeping a close eye on the MAP during the<br />
patients stay in the ED is important. Our study shows that this not only<br />
applies to patients with septic shock (only 1.9% of our population), as<br />
recommended by the surviving sepsis campaign (SSC) guidelines, but<br />
for all patients with sepsis or infection [4].<br />
RESUSCITATION TODAY - SUMMER <strong>2019</strong><br />
Our results indicate that changes and variability of the MAP are<br />
Apart from our earlier pilot study, little is known about repeated vital<br />
23
CLINICAL PAPER<br />
RESUSCITATION TODAY - SUMMER <strong>2019</strong><br />
sign measurements in patients with infection or sepsis during their<br />
stay in the ED in relation to clinical outcomes, patient deterioration and<br />
(early) signs of organ failure. Our pilot study showed that vital signs<br />
changed significantly during the patient’s stay in the ED, but did not<br />
analyse patient deterioration [7]. Henriksen et al... retrospectively found<br />
a deterioration of vital signs from the normal to abnormal range within<br />
4–13 h after arrival in 31% of patients in the general ED population,<br />
leading to a four times higher 30-day mortality risk [13]. The available<br />
studies on vital signs in the ED mostly use only single measurements,<br />
mainly at triage [9, 12]. Furthermore, these were often retrospective<br />
studies in contrast to our study. Finally, they often included the general<br />
ED population and thus a more heterogeneous population. The<br />
endpoints and cut-off values differ from study to study, most studies<br />
used mortality endpoints, several studies had ICU admission as an<br />
endpoint and only a few studies included organ failure [8, 11, 13,<br />
19, 20, 21, 22]. The single measurements, heterogeneous patient<br />
populations and different endpoints make a direct comparison of those<br />
results with our study’s results impossible. Coslovsky et al aimed to<br />
develop a prediction model for in-hospital mortality using a model with<br />
age, prolonged capillary refill, blood pressure, mechanical ventilation,<br />
oxygen saturation index, GSC and the APACHEII diagnostic category<br />
in a cohort that contained 15% patients with infection among which<br />
7.3% with sepsis. Their model had an AUC of 0.92, although, it should<br />
be noted that their model was based on a heterogeneous patient<br />
population, single measurements and a combination of multiple vital<br />
signs [23]. Yamamoto et al. found an association between low body<br />
temperature (< 36 °C) at ED admission and higher 30 day in-hospital<br />
mortality risk in patients with suspected sepsis [24]. In our study, we did<br />
not find an association between body temperature and deterioration.<br />
Furthermore, it should be noted that the in-hospital mortality in our<br />
study (3.3%) is much lower than in the study of Yamamoto (9.6%). In<br />
summary, available studies did not specifically investigate ED patients<br />
with infection or sepsis, mostly used single vital sign measurements (at<br />
triage) and primarily had mortality or ICU admission endpoints.<br />
Early warning scores (EWS), like the national early warning score<br />
(NEWS) and many variants and related scores, are increasingly<br />
being used throughout healthcare. These EWS commonly contain<br />
a combination of various vital sign parameters, supplemented with<br />
laboratory values or other items, where each item is scored at certain<br />
thresholds. Early warning scores are mostly used as ‘track-and-trigger’<br />
systems to trigger the nurse to call the physician or a rapid response<br />
team, or to predict a high risk of mortality or ICU admission [25, 26].<br />
The many different EWS and patient populations, in which they have<br />
been validated, make it difficult to compare their performance. However,<br />
a recent review by Nannan Panday et al. showed that the NEWS score<br />
was the best to predict mortality or ICU admission in the general<br />
ED population and the modified early warning score was the best in<br />
patients with suspected infection or sepsis [25]. Their performance<br />
(AUC) was in the same range as we found for our repeated blood<br />
pressure measurements (MAP). However, it should be noted that<br />
we used only a single vital sign repeated measurement and had a<br />
composite outcome of patient deterioration, which included signs of<br />
organ dysfunction. Another recent study by Kivipuro et al. showed that<br />
the NEWS score was significantly higher before ICU admission when<br />
a patient was transferred from the ward to the ICU, compared to the<br />
NEWS score of the same patient at the ED [27]. In our hospital, modified<br />
early warning scores (MEWS) are taken at admission to the ward and<br />
thereafter three times per day. Deterioration of the MEWS score triggers<br />
an early response team. Further research is needed to clarify whether<br />
repeated vital sign measurements in combination with repeated early<br />
warning scores are useful in the detection of patient deterioration in<br />
patients with sepsis or infection.<br />
We have shown that almost 30% of the patients presenting to the ED<br />
with suspected infection or sepsis deteriorated within 72 h of admission<br />
and over 28% of the patients showed signs of (multiple) organ failure<br />
despite treatment. Our results show that 18.3% of the patients with<br />
infection, 32.9% of the patients with sepsis and in total 29.5% of the<br />
patients deteriorated within 72 h (Table 4). Glickman et al. showed<br />
that almost 23% of patients with uncomplicated sepsis progress<br />
to severe sepsis or septic shock within 72 h from admission [1].<br />
Although a direct comparison cannot be made because of a different<br />
population and different endpoints, these results clearly show that<br />
a large part of the patients with infection deteriorate in the first days<br />
in the hospital and develop (severe) sepsis. Therefore, we question<br />
whether the introduction of the recent Sepsis-3 definitions, in which<br />
infection or uncomplicated sepsis are no longer part of the sepsis<br />
severity spectrum, will lead to better patient care [28]. We would like to<br />
emphasise that it is important to properly monitor and treat all patients<br />
with infection or sepsis in the ED. Since sepsis-related mortality has<br />
dramatically reduced over the past two decades, we believe that early<br />
detection or prevention of organ failure is where the future focus of<br />
infection/sepsis research should be, since there is a lot to gain [29].<br />
The 30-min measurement interval in the current study was arbitrarily<br />
chosen, since there is no standard on how often vital signs should<br />
be measured in the ED and only little research has been conducted<br />
on this topic. Descriptive studies in the general ED population have<br />
shown that the time between two measurements is between 67 and<br />
130 min and that a higher illness severity results in more frequent<br />
measurements [10, 30]. We believe that these measurement intervals<br />
are not representative for patients with infection or sepsis, however,<br />
there are no specific guidelines on how often vital signs should be<br />
measured in these patients [13]. The 30-min measurement interval in<br />
our study was much more frequent than the median intervals reported<br />
by Johnson and Lambe [10, 30]. A higher measurement frequency<br />
might provide even more information about deterioration, although this<br />
might lead to a higher burden on the patient and staff. Therefore, we<br />
recommend continuous measurement of vital signs on a beat-to-beat<br />
level, preferably automated with the use of bed-side patients monitors<br />
or wearable devices [3]. Our next step, as a follow-up of this study,<br />
is to shorten the measurement interval to a beat-to-beat interval with<br />
heart rate variability (HRV) measured using bed-side patient monitors<br />
in the SepsiVit study [3]. As we have shown, a substantial number of<br />
patients deteriorate in the first days from admission. In the currently<br />
running SepsiVit study, we will extend the measurements beyond the<br />
boundaries of the ED towards the nursing wards during the first 48 h<br />
of hospitalization. During this period, we will investigate whether the<br />
combination of HRV with monitoring on the nursing wards can provide<br />
an early warning of patient deterioration. Such an early warning could<br />
provide a possible opportunity for intervention in the future.<br />
Strengths and limitations<br />
To the best of our knowledge this is the first study that prospectively<br />
investigated the relation between repeated vital sign measurements<br />
24
CLINICAL PAPER<br />
and patient deterioration in the ED in patients with infection or sepsis.<br />
We did not only use the common mortality and ICU admission<br />
endpoints, but also included signs of organ failure in our composite<br />
patient deterioration endpoint. Vital signs can be easily measured<br />
with equipment readily available in every ED. The repeated vital sign<br />
measurements in our study were obtained specifically by a trained<br />
member of our research staff, which minimized the amount of missing<br />
data. However, in spite of the prospective study design, 92 (25%)<br />
respiratory rate measurements were not recorded at triage by the<br />
triage nurse. It is well-known that respiratory rate is the most frequently<br />
missing vital sign, unfortunately our study is no exception [31]. These<br />
missing respiratory rate measurements at triage limit the power of our<br />
logistic regression models that include respiratory rate (RR-Mx; Table 4).<br />
Another limitation of our study is that it is a single centre study in an<br />
academic tertiary care teaching hospital. This may limit the generalizability<br />
to other patient populations, especially since our population contains<br />
a high number of patients with a history of organ transplantation (Table<br />
2). However, a history of organ transplantation was not independently<br />
associated with patient deterioration in our models (Table 4). Therefore,<br />
we believe that the specific patient population did not have a substantial<br />
influence on our results. We did not design the study to analyse<br />
combinations of multiple vital signs in our models, since we were<br />
interested in identifying which repeated vital sign measurements are<br />
helpful in predicting patient deterioration and not in the best combination<br />
of vital signs. We acknowledge that a combination of repeated vital<br />
signs may provide even more information in future studies, perhaps in<br />
combination with repeated early warning scores.<br />
Clinical implications<br />
We have shown that more than one in four patients presenting to the ED<br />
with suspected infection or sepsis deteriorated within 72 h of admission<br />
and showed signs of organ failure. These were not exclusively patients<br />
with sepsis at admission, but one in five patients that presented to the<br />
ED with infection only. Although the organ failure generally did not result<br />
in mortality, organ failure may even be preventable or treatable. Our<br />
results show that repeated vital sign measurements (especially blood<br />
pressure) at the ED is a predictor of patient deterioration and might<br />
result in a reduction of organ failure related morbidity. It is thus important<br />
to reassess patient at the ED frequently, including measurement of<br />
vital signs, as is done on the wards with early warning scores [29].<br />
Although it is known that patient deterioration is often preceded by<br />
changes in vital signs several hours before the event, these signs are<br />
frequently missed on general wards [25, 27, 32]. At this moment, we are<br />
conducting a subsequent study (SepsiVit study) with 48 h of continuous<br />
vital sign measurements at the ED and on the general wards to test the<br />
hypothesis that repeated vital sign measurements at the general ward<br />
(with high frequency) is better in the prediction of patient deterioration<br />
than the currently used systems [3]. Until this information from the<br />
SepsiVit study becomes available, we assess patients at the ED<br />
frequently, including repeated vital sign measurements.<br />
Conclusions<br />
Repeated measurement of vital signs in the ED are better at identifying<br />
patients at risk for deterioration within 72 h from admission than single<br />
vital sign measurements at ED admission. Repeated measurements of<br />
MAP and respiratory rate are associated with patient deterioration. Since<br />
almost one third of patients presenting with infection or sepsis to the ED<br />
deteriorate within 72 h, repeated vital sign measurements may be an<br />
important way to guarantee early identification of deterioration.<br />
Abbreviations<br />
AKI: Acute kidney injury; AUC: Area under the receiver operator curve;<br />
BT: Body temperature; COPD: Chronic obstructive pulmonary disease;<br />
ED: Emergency department; GCS: Glasgow coma score; HR: Heart<br />
rate; HRV: Heart rate variability; ICU: Intensive care unit; KDIGO: Kidney<br />
disease improving global outcomes; MAP: Mean arterial pressure;<br />
METc: Institutional review board; OR: Odds ratio; RR: Respiratory rate;<br />
SBP: Systolic blood pressure; SCPD: Sepsis clinical pathway database;<br />
SpO 2<br />
: Peripheral oxygen saturation; SSC: Surviving sepsis campaign;<br />
USA: United States of America<br />
Acknowledgements<br />
The authors thank the nurses and physicians in our emergency<br />
department for their assistance during the acquisition of the data. We<br />
thank the members of the Sepsis Research Team in our emergency<br />
department for their efforts in collecting the data.<br />
Availability of data and material<br />
The datasets used and/or analysed during the current study are<br />
available from the corresponding author on reasonable request.<br />
Funding<br />
This study is funded by the emergency department of the University<br />
Medical Center Groningen. VMQ received a MD-PhD scholarship from<br />
the University of Groningen, University Medical Center Groningen for his<br />
PhD research.<br />
Authors’ contributions<br />
VMQ drafted the study design, assisted with data acquisition, carried<br />
out data analysis and drafted the manuscript. MvM participated in the<br />
study design, assisted with data interpretation and critically revised<br />
the manuscript. TJO participated in the study design, assisted with<br />
data acquisition, and critically revised the manuscript. JMV carried out<br />
data analysis, assisted with data interpretation and critically revised the<br />
manuscript. JJML participated in the study design, assisted with data<br />
interpretation and critically revised the manuscript. JCtM participated in<br />
the study design, assisted with data interpretation, critically revised the<br />
manuscript and has given final approval of the version to be published.<br />
Ethics approval and consent to participate<br />
This study was carried out in accordance to the Declaration of Helsinki,<br />
the Dutch Agreement on Medical Treatment Act and the Dutch Personal<br />
Data Protection Act. The Institutional Review Board of the University<br />
Medical Center Groningen ruled that the Dutch Medical Research<br />
Involving Human Subjects Act is not applicable for this study and<br />
granted a waiver (METc 2015/164). All participants provided written<br />
informed consent.<br />
Consent for publication<br />
Not applicable.<br />
Competing interests<br />
The authors declare that they have no competing interests.<br />
RESUSCITATION TODAY - SUMMER <strong>2019</strong><br />
25
CLINICAL PAPER<br />
RESUSCITATION TODAY - SUMMER <strong>2019</strong><br />
Publisher’s Note<br />
Springer Nature remains neutral with regard to jurisdictional claims in<br />
published maps and institutional affiliations.<br />
Author details<br />
*<br />
Correspondence: v.m.quinten@umcg.nl 1 Department of Emergency<br />
Medicine, University of Groningen, University Medical Center Groningen,<br />
HPC TA10, PO Box 30001, 9700 RB Groningen, The Netherlands.<br />
2<br />
Department of Critical Care, University of Groningen, University<br />
Medical Center Groningen, Groningen, The Netherlands. 3 Department<br />
of Pathology and Medical Biology, Medical Biology section, University<br />
of Groningen, University Medical Center Groningen, Groningen, The<br />
Netherlands. 4 Department of Epidemiology, University of Groningen,<br />
University Medical Center Groningen, Groningen, The Netherlands.<br />
References<br />
1. Glickman SW, Cairns CB, Otero RM, Woods CW, Tsalik EL, Langley<br />
RJ, et al. Disease progression in hemodynamically stable patients<br />
presenting to the emergency department with sepsis. Acad Emerg<br />
Med Wiley Online Library. 2010;17:383–90.<br />
2. Buchan CA, Bravi A, Seely AJE. Variability analysis and the<br />
diagnosis, management, and treatment of sepsis. Curr Infect Dis<br />
Rep. 2012;14:512–21.<br />
3. Quinten VM, van Meurs M, Renes MH, Ligtenberg JJM, ter Maaten<br />
JC. Protocol of the SepsiVit study: a prospective observational study<br />
to determine whether continuous heart rate variability measurement<br />
during the first 48 hours of hospitalization provides an early warning<br />
for deterioration in patients presenting with infec. BMJ Open<br />
[Internet]. British Medical Journal Publishing Group; 2017 [cited<br />
2017 Nov 20];7:1–17. Available from: http://www.ncbi.nlm.nih.gov/<br />
pubmed/29151053<br />
4. Rhodes A, Evans LE, Alhazzani W, Levy MM, Antonelli M, Ferrer<br />
R, et al. Surviving Sepsis Campaign: International Guidelines for<br />
Management of Sepsis and Septic Shock: 2016. Intensive Care<br />
Med. [Internet]. Springer Berlin Heidelberg; 2017;43:304–377.<br />
Available from: https://link.springer.com/article/10.1007/s00134-017-<br />
4683-6<br />
5. Samraj RS, Zingarelli B, Wong HR. Role of biomarkers in sepsis<br />
care. Shock. Cincinnati. Ohio. 2013;40:358–65.<br />
6. Pierrakos C, Vincent J-L. Sepsis biomarkers: a review. Crit Care.<br />
2010;14:R15.<br />
7. Quinten VM, van Meurs M, Ter Maaten JC, Ligtenberg JJ. Trends<br />
in vital signs and routine biomarkers in patients with sepsis<br />
during resuscitation in the emergency department: a prospective<br />
observational pilot study. BMJ Open. 2016;6:9718.<br />
8. Ljunggren M, Castrén M, Nordberg M, Kurland L. The association<br />
between vital signs and mortality in a retrospective cohort study<br />
of an unselected emergency department population. Scand. J.<br />
Trauma. <strong>Resus</strong>c. Emerg. Med. [Internet]. BioMed Central; 2016<br />
[cited 2017 31];24:21. Available from: http://www.sjtrem.com/<br />
content/24/1/21<br />
9. Farrohknia N, Castrén M, Ehrenberg A, Lind L, Oredsson<br />
S, Jonsson H, et al. Emergency department triage scales<br />
and their components: a systematic review of the scientific<br />
evidence. Scand. J. Trauma. <strong>Resus</strong>c. Emerg. Med. [Internet].<br />
2011;19:42. Available from: http://sjtrem.biomedcentral.com/<br />
articles/10.1186/1757-7241-19-42<br />
10. Lambe KR, Currey JR, Considine J. Frequency of vital<br />
sign assessment and clinical deterioration in an Australian<br />
emergency department. Australas. Emerg. Nurs. J. [Internet].<br />
Elsevier; 2016 [cited 2017 Oct 16];19:217–222. Available<br />
from: http://www.sciencedirect.com/science/article/pii/<br />
S1574626716300398?via%3Dihub<br />
11. Hong W, Earnest A, Sultana P, Koh Z, Shahidah N, Ong MEH. How<br />
accurate are vital signs in predicting clinical outcomes in critically<br />
ill emergency department patients. Eur. J. Emerg. Med. [Internet].<br />
Lippincott Williams & Wilkins; 2013 [cited 2017 Oct 31];20:27–32.<br />
Available from: https://insights.ovid.com/pubmed?pmid=22198158<br />
12. Bleyer AJ, Vidya S, Russell GB, Jones CM, Sujata L, Daeihagh<br />
P, et al. Longitudinal analysis of one million vital signs in patients<br />
in an academic medical center. <strong>Resus</strong>citation [Internet].<br />
Elsevier; 2011 [cited 2017 Nov 2];82:1387–1392. Available<br />
from: http://www.sciencedirect.com/science/article/pii/<br />
S0300957211004096?via%3Dihub<br />
13. Henriksen DP, Brabrand M, Lassen AT. Prognosis and risk factors<br />
for deterioration in patients admitted to a medical emergency<br />
department. Cleary PR, editor. PLoS One [Internet]. Public Library of<br />
Science; 2014 [cited 2017 Oct 31];9:e94649. Available from: http://<br />
dx.plos.org/10.1371/journal.pone.0094649<br />
14. Alam N, Oskam E, Stassen PM, van EP, van de VPM, Haak HR, et<br />
al. Prehospital antibiotics in the ambulance for sepsis: a multicentre,<br />
open label, randomised trial. Lancet Respir. Med. [Internet].<br />
2017; Available from: http://linkinghub.elsevier.com/retrieve/pii/<br />
S2213260017304691<br />
15. Global Kidney Disease: Improving Outcomes (KDIGO) Acute Kidney<br />
Injury Work Group, Kellum J A, Lameire N, Aspelin P, Barsoum RS,<br />
Burdmann E A, et al. KDIGO clinical practice guideline for acute<br />
kidney injury. Kidney Inter. Suppl. [Internet]. 2012;2:1–138. Available<br />
from: http://www.kdigo.org/clinical_practice_guidelines/pdf/<br />
KDIGO%20AKI%20Guideline.pdf.<br />
16. Sands KE, Bates DW, Lanken PN, Graman PS, Hibberd PL,<br />
Kahn KL, et al. Epidemiology of Sepsis Syndrome in 8 Academic<br />
Medical Centers. JAMA [Internet]. American Medical Association.<br />
1997;278:234–40. Available from: http://jama.jamanetwork.com/<br />
article.aspx?doi=10.1001/jama.1997.03550030074038<br />
17. Burt CC, Arrowsmith JE. Respiratory failure. Surg. - Oxford Int. Ed.<br />
[Internet]. Elsevier; 2009;27:475–479. Available from: http://www.<br />
surgeryjournal.co.uk/article/S0263-9319(09)00195-1/fulltext.<br />
18. Levy MM, Fink MP, Marshall JC, Abraham E, Angus D, Cook D, et<br />
al. 2001 sccm/esicm/accp/ats/sis international sepsis definitions<br />
conference. Intensive Care Med. Springer. 2003;29:530–8.<br />
19. Kristensen AKB, Holler JG, Mikkelsen S, Hallas J, Lassen A.<br />
Systolic blood pressure and short-term mortality in the emergency<br />
department and prehospital setting: a hospital-based cohort<br />
study. Crit. Care [Internet]. BioMed Central; 2015 [cited 2017 Oct<br />
31];19:158. Available from: http://ccforum.com/content/19/1/158<br />
20. Barfod C, Lauritzen M, Danker J, Sölétormos G, Forberg J, Berlac<br />
P, et al. Abnormal vital signs are strong predictors for intensive<br />
care unit admission and in-hospital mortality in adults triaged in<br />
the emergency department - a prospective cohort study. Scand J<br />
Trauma <strong>Resus</strong>c Emerg Med [Internet]. BioMed Central; 2012 [cited<br />
2017 Oct 31];20:28. Available from: http://sjtrem.biomedcentral.<br />
com/articles/10.1186/1757-7241-20-28<br />
21. Walston J, Cabrera D, Bellew S, Olive M, Lohse C, Bellolio F. Vital<br />
signs predict rapid-response team activation within twelve hours of<br />
emergency Department Admission. West. J. Emerg. Med. [Internet].<br />
2016 [cited 2017 Oct 31];17:324–330. Available from: http://<br />
escholarship.org/uc/item/93r2v5j0<br />
26
CLINICAL PAPER<br />
22. Henning DJ, Oedorf K, Day DE, Redfield CS, Huguenel CJ, Roberts<br />
JC, et al. Derivation and validation of predictive factors for clinical<br />
deterioration after admission in emergency department patients<br />
presenting with abnormal vital signs without shock. West. J Emerg<br />
Med [Internet]. California Chapter of the American Academy of<br />
Emergency Medicine (Cal/AAEM); 2015 [cited 2017]<br />
23. Oct 31];16:1059–1066. Available from: http://www.ncbi.nlm.nih.gov/<br />
pubmed/26759655<br />
24. Coslovsky M, Takala J, Exadaktylos AK, Martinolli L, Merz TM. A<br />
clinical prediction model to identify patients at high risk of death<br />
in the emergency department. Intensive Care Med [Internet].<br />
Springer Berlin Heidelberg; 2015 [cited 2017 Oct 31];41:1029–1036.<br />
Available from: http://link.springer.com/10.1007/s00134-015-3737-x<br />
25. Yamamoto S, Yamazaki S, Shimizu T, Takeshima T, Fukuma S,<br />
Yamamoto Y, et al. Body temperature at the emergency department<br />
as a predictor of mortality in patients with bacterial infection. Med<br />
(Baltimore). [Internet] . 2016 [cited 2017 Oct 31];95:e3628. Available<br />
from: https://insights.ovid.com/pubmed?pmid=27227924.<br />
26. Nannan Panday RS, Minderhoud TC, Alam N, Nanayakkara<br />
PWB. Prognostic value of early warning scores in the emergency<br />
department (ED) and acute medical unit (AMU): A narrative review<br />
[Internet]. Eur. J. Intern. Med. Elsevier; 2017 [cited 2018 Jun 20].<br />
p. 20–31. Available from: https://www.sciencedirect.com/science/<br />
article/pii/S0953620517303758?via%3Dihub<br />
27. Kyriacos U, Jelsma J, Jordan S. Monitoring vital signs using early<br />
warning scoring systems: A review of the literature. J. Nurs. Manag.<br />
[Internet]. 2011 [cited 2017 Oct 12];19:311–330. Available from:<br />
http://doi.wiley.com/10.1111/j.1365-2834.2011.01246.x<br />
28. Kivipuro M, Tirkkonen J, Kontula T, Solin J, Kalliomäki J, Pauniaho<br />
SL, et al. National early warning score (NEWS) in a Finnish<br />
multidisciplinary emergency department and direct vs. late<br />
admission to intensive care. <strong>Resus</strong>citation [Internet]. Elsevier;<br />
2018;128:164–169. Available from: https://doi.org/10.1016/j.<br />
resuscitation.2018.05.020<br />
29. Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane<br />
D, Bauer M, et al. The third international consensus definitions for<br />
Sepsis and septic shock (Sepsis-3). JAMA [Internet]. American<br />
Medical Association; 2016 [cited 2017 Oct 5];315:801. Available<br />
from: http://www.ncbi.nlm.nih.gov/pubmed/26903338<br />
30. Quinten VM, van Meurs M, Ligtenberg JJM, Ter Maaten JC.<br />
Prehospital antibiotics for sepsis: beyond mortality? Lancet Resp Med<br />
[Internet]. 2018 [cited 2018 Feb 28];6. Available from: http://www.<br />
thelancet.com/pdfs/journals/lanres/PIIS2213-2600(18)30061-4.pdf.<br />
31. Johnson KD, Winkelman C, Burant CJ, Dolansky M, Totten V.<br />
The Factors that affect the frequency of vital sign monitoring<br />
in the emergency department. J. Emerg. Nurs. [Internet].<br />
Mosby; 2014 [cited 2017 Oct 31];40:27–35. Available<br />
from: http://www.sciencedirect.com/science/article/pii/<br />
S0099176712003923?via%3Dihub<br />
32. Cretikos MA, Bellomo R, Hillman K, Chen J, Finfer S, Flabouris<br />
A. Respiratory rate: the neglected vital sign. Med J Aust.<br />
2008;188:657–9.<br />
33. Fuhrmann L, Lippert A, Perner A, Østergaard D. Incidence, staff<br />
awareness and mortality of patients at risk on general wards.<br />
<strong>Resus</strong>citation [Internet]. Elsevier; 2008 [cited 2018 Jun 21];77:325–<br />
330. Available from: https://www.sciencedirect.com/science/article/<br />
pii/S030095720800052X?via%3Dihub<br />
RESUSCITATION TODAY - SUMMER <strong>2019</strong><br />
27
EMMA® Waveform Capnograph<br />
All Patient use<br />
Adult/Paediatric<br />
Infant/Neonate<br />
EtC02 & Respiratory rate<br />
End-tidal C0 2 and Respiratory<br />
Rate values + Waveform<br />
Tube Placement & ROSC<br />
Ensures efficacy of intubation<br />
Early detection of ROSC<br />
Effectiveness of CPR<br />
Feedback > effectiveness of<br />
chest compressions & CPR<br />
Optimised Power<br />
8 hrs. continuous use<br />
2 x AAA batteries<br />
Configurable Alarms<br />
High & Low EtC02, Apnoea<br />
Blocked airway, Battery status<br />
when every breath counts<br />
9 Application proven: pre-hospital, hospital, emergency, critical care & resuscitation<br />
9 Provides compliance to 2015 ERC/UK ALS, & NAP4 waveform capnography guidelines<br />
9 Monitoring of Intubated patients during recovery, transfers and transportation<br />
MEDACX LIMITED • ALEXANDER HOUSE • 60-62 STATION ROAD • HAYLING ISLAND • HAMPSHIRE • PO11 0EL<br />
02392 469737<br />
info@medacx.co.uk<br />
www.medacx.co.uk