Resus Today Autumn 2020
Resus Today Autumn 2020
Resus Today Autumn 2020
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
Volume 7 No. 2<br />
<strong>Autumn</strong> <strong>2020</strong><br />
<strong>Resus</strong>citation <strong>Today</strong><br />
A Resource for all involved in the Teaching and Practice of <strong>Resus</strong>citation<br />
See reverse for Simulation <strong>Today</strong>
Just breathe<br />
PENTHROX 99.9%, 3 ml inhalation vapour, liquid: Please refer<br />
to the Summary of Product Characteristics (SmPC) before<br />
prescribing. Abbreviated Prescribing Information.<br />
Presentation: Each bottle of PENTHROX contains 3 ml of<br />
methoxyflurane 99.9%, a clear, almost colourless, volatile liquid,<br />
with a characteristic fruity odour. Each PENTHROX combination<br />
pack consists of one bottle of 3 ml PENTHROX, one PENTHROX<br />
Inhaler and one Activated Carbon (AC) chamber. Indications:<br />
Emergency relief of moderate to severe pain in conscious adult<br />
patients with trauma and associated pain. Dosage and<br />
administration: PENTHROX should be self-administered under<br />
supervision of a person trained in its administration, using the<br />
hand held PENTHROX Inhaler. It is inhaled through the custombuilt<br />
PENTHROX inhaler. Adults: One bottle of 3 ml PENTHROX<br />
as a single dose, administered using the device provided. A<br />
second bottle should only be used where needed. The frequency<br />
at which PENTHROX can be safely used is not established. The<br />
following administration schedule is recommended: no more than<br />
6 ml in a single day, administration on consecutive days is not<br />
recommended and the total dose to a patient in a week should<br />
not exceed 15 ml. Onset of pain relief is rapid and occurs after<br />
6-10 inhalations. Patients are able to titrate the amount of<br />
PENTHROX inhaled and should be instructed to inhale<br />
intermittently to achieve adequate analgesia. Continuous<br />
inhalation of a bottle containing 3 ml provides analgesic relief for<br />
up to 25-30 minutes; intermittent inhalation may provide longer<br />
analgesic relief. Patients should be advised to use the lowest<br />
possible dose to achieve pain relief. Renal impairment:<br />
Methoxyflurane may cause renal failure if the recommended dose<br />
is exceeded. Caution should be exercised for patients diagnosed<br />
with clinical conditions that would pre-dispose to renal injury.<br />
Hepatic impairment: Cautious clinical judgement should be<br />
exercised when PENTHROX is to be used more frequently than<br />
on one occasion every 3 months. Paediatric population:<br />
PENTHROX should not be used in children and adolescents under<br />
18 years. For detailed information on the method of administration<br />
refer to the SmPC. Contraindications: Use as an anaesthetic<br />
agent. Hypersensitivity to methoxyflurane, any fluorinated<br />
anaesthetic or to any of the excipients. Patients who are known<br />
to be genetically susceptible to malignant hyperthermia. Patients<br />
or patients with a known family history of severe adverse reactions<br />
after being administered with inhaled anaesthetics. Patients who<br />
have a history of showing signs of liver damage after previous<br />
methoxyflurane use or halogenated hydrocarbon anaesthesia.<br />
Clinically significant renal impairment. Altered level of<br />
MAT-PEN-UK-000310 Date of preparation: October <strong>2020</strong><br />
Look familiar?<br />
It’s TIME for change...<br />
71 MINUTES FASTER DISCHARGE 1 ON AVERAGE &<br />
SUPERIOR PAIN RELIEF 2,3 FOR MODERATE TO SEVERE<br />
TRAUMA PAIN WITH PENTHROX VS SAT *<br />
Penthrox is indicated for the emergency relief of moderate to severe pain in conscious adult patients with trauma and associated pain. 4<br />
consciousness due to any cause including head injury, drugs or<br />
alcohol. Clinically evident cardiovascular instability. Clinically<br />
evident respiratory depression. Warnings and Precautions: To<br />
ensure the safe use of PENTHROX as an analgesic the lowest<br />
effective dose to control pain should be used and it should be<br />
used with caution in the elderly or other patients with known risk<br />
factors for renal disease, and in patients diagnosed with clinical<br />
conditions which may pre-dispose to renal injury. Methoxyflurane<br />
causes significant nephrotoxicity at high doses. Nephrotoxicity is<br />
thought to be associated with inorganic fluoride ions, a metabolic<br />
breakdown product. When administered as instructed for the<br />
analgesic indication, a single dose of 3 ml methoxyflurane<br />
produces serum levels of inorganic fluoride ions below 10<br />
micromol/l. In the past when used as an anaesthetic agent,<br />
methoxyflurane at high doses caused significant nephrotoxicity,<br />
which was determined to occur at serum levels of inorganic<br />
fluoride ions greater than 40 micromol/l. Nephrotoxicity is also<br />
related to the rate of metabolism. Factors that increase the rate<br />
of metabolism such as drugs that induce hepatic enzymes can<br />
increase the risk of toxicity with methoxyflurane as well as subgroups<br />
of people with genetic variations that may result in fast<br />
metaboliser status. Methoxyflurane is metabolised in the liver,<br />
therefore increased exposures in patients with hepatic impairment<br />
can cause toxicity. PENTHROX should be used with care in patients<br />
with underlying hepatic conditions or with risks for hepatic<br />
dysfunction. Previous exposure to halogenated hydrocarbon<br />
anaesthetics (including methoxyflurane when used as an<br />
anaesthetic agent), especially if the interval is less than 3 months,<br />
may increase the potential for hepatic injury. Potential effects on<br />
blood pressure and heart rate are known class-effects of high-dose<br />
methoxyflurane used in anaesthesia and other anaesthetics.<br />
Caution is required with use in the elderly due to possible<br />
reduction in blood pressure. Potential CNS effects such as<br />
sedation, euphoria, amnesia, ability to concentrate, altered<br />
sensorimotor co-ordination and change in mood are known classeffects.<br />
The possibility of CNS effects may be seen as a risk factor<br />
for potential abuse, however reports are very rare in postmarketing<br />
use. PENTHROX is not appropriate for providing relief<br />
of break-through pain/exacerbations in chronic pain conditions<br />
or for the relief of trauma related pain in closely repeated episodes<br />
for the same patient. PENTHROX contains the excipient, butylated<br />
hydroxytoluene (E321) which may cause local skin reactions (e.g.<br />
contact dermatitis), or irritation to the eyes and mucous<br />
membranes. To reduce occupational exposure to methoxyflurane,<br />
the PENTHROX Inhaler should always be used with the AC<br />
Chamber which adsorbs exhaled methoxyflurane. Multiple use of<br />
PENTHROX Inhaler without the AC Chamber creates additional<br />
risk. Elevation of liver enzymes, blood urea nitrogen and serum<br />
uric acid have been reported in exposed maternity ward staff<br />
when methoxyflurane was used in the past at the time of labour<br />
and delivery. Interactions: There are no reported drug interactions<br />
when used at the analgesic dosage (3 – 6 ml). Methoxyflurane is<br />
metabolised by the CYP 450 enzymes, particularly CYP 2E1 and<br />
to some extent CYP 2A6. It is possible that enzyme inducers (such<br />
as alcohol or isoniazid for CYP 2E1 and phenobarbital or rifampicin<br />
for CYP 2A6) which increase the rate of methoxyflurane<br />
metabolism might increase its potential toxicity and they should<br />
be avoided concomitantly with methoxyflurane. Concomitant use<br />
of methoxyflurane with medicines (e.g. contrast agents and some<br />
antibiotics) which are known to have a nephrotoxic effect should<br />
be avoided as there may be an additive effect on nephrotoxicity;<br />
tetracycline, gentamicin, colistin, polymyxin B and amphotericin<br />
B have known nephrotoxic potential. Sevoflurane anaesthesia<br />
should be avoided following methoxyflurane analgesia, as<br />
sevoflurane increases serum fluoride levels and methoxyflurane<br />
nephrotoxicity is associated with raised serum fluoride.<br />
Concomitant use of PENTHROX with CNS depressants, such as<br />
opioids, sedatives or hypnotics, general anaesthetics,<br />
phenothiazines, tranquillisers, skeletal muscle relaxants, sedating<br />
antihistamines and alcohol may produce additive depressant<br />
effects. If opioids are given concomitantly with PENTHROX, the<br />
patient should be observed closely. When methoxyflurane was<br />
used for anaesthesia at the higher doses of 40–60 ml, there were<br />
reports of drug interaction with hepatic enzyme inducers (e.g.<br />
barbiturates) increasing metabolism of methoxyflurane and<br />
resulting in a few reported cases of nephrotoxicity; reduction of<br />
renal blood flow and hence anticipated enhanced renal effect<br />
when used in combination with drugs (e.g. barbiturates) reducing<br />
cardiac output; and class effect on cardiac depression, which may<br />
be enhanced by other cardiac depressant drugs, e.g. intravenous<br />
practolol during cardiac surgery. Fertility, pregnancy and<br />
lactation: No clinical data on effects of methoxyflurane on fertility<br />
are available. As with all medicines care should be exercised when<br />
administered during pregnancy especially the first trimester. There<br />
is insufficient information on the excretion of methoxyflurane in<br />
human milk. Caution should be exercised when methoxyflurane<br />
is administered to a nursing mother. Effects on ability to drive<br />
and use machines: Methoxyflurane may have a minor influence<br />
on the ability to drive and use machines. Patients should be<br />
advised not to drive or operate machinery if they are feeling<br />
Before administering PENTHROX, make sure you have read and fully understood the SmPC and educational materials, which provide important information about how to safely use the device to minimise risk of serious side effects.<br />
PENTHROX educational materials and training on its administration are available from Galen on request.<br />
*SAT = Standard Analgesic Treatment: In the St. Mary’s Hospital service evaluation, SAT consisted of IV opioids or procedural sedation in the majority of cases. 1 In the MEDITA trial, SAT consisted of IV paracetamol (1 g) or IV ketoprofen<br />
(100 mg) for moderate pain and IV morphine (0.1 mg/kg) for severe pain, 2 and in the InMEDIATE trial, SAT varied among sites but most frequently comprised of NSAIDs for moderate pain and IV locally approved opioid and non-opioid<br />
analgesics for severe pain. 3<br />
drowsy or dizzy. Undesirable effects: The common non-serious<br />
reactions are CNS type reactions such as dizziness and somnolence<br />
and are generally easily reversible. Serious dose-related<br />
nephrotoxicity has only been associated with methoxyflurane<br />
when used in large doses over prolonged periods during general<br />
anaesthesia. The following adverse drug reactions have either<br />
been observed in PENTHROX clinical trials in analgesia, with<br />
analgesic use of methoxyflurane following post-marketing<br />
experience or are linked to methoxyflurane use in analgesia found<br />
in post-marketing experience and in scientific literature (refer to<br />
the SmPC for further details): Very Common (≥1/10): dizziness;<br />
common (≥1/100 to
CONTENTS • Incurved face seal<br />
4 EDITORS COMMENT<br />
6 FEATURE COVID-19 pandemic patient’s preparation: ears using simulation<br />
for systems-based learning to prepare the largest<br />
healthcare workforce and system in Canada<br />
18 FEATURE Penthrox Can Outperform Morphine<br />
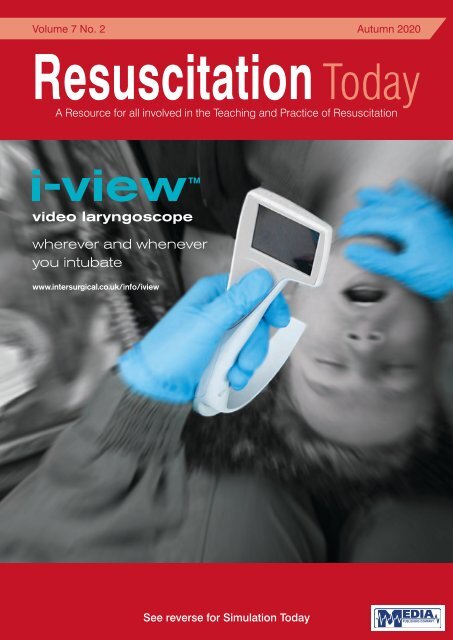
COVER STORY<br />
Quality, innovation and choice<br />
Intersurgical i-view video laryngoscope, tracheal intubation and COVID-19<br />
lnteract with us<br />
The use of the i-view video laryngoscope for tracheal intubation in the context of Covid-19<br />
is investigated in a new blog post by our Airway Group Product Manager, David Chapman.<br />
www.intersurgical.co.uk<br />
The article looks at the latest guidelines regarding airway management, the potential<br />
benefits of single use devices in the context of infection control and what advantages<br />
videolaryngoscopy may have to offer over direct laryngoscopy for tracheal intubation.<br />
AMBULANCE_UK_Half_Page_FiltaMask_<strong>2020</strong>_07.indd 1<br />
The i-view video laryngoscope is a single use, fully disposable video laryngoscope,<br />
providing the option of video laryngoscopy wherever you might need to intubate.<br />
By incorporating a Macintosh blade, i-view can also be used for direct laryngoscopy<br />
and the technique for insertion is more familiar and instinctive than for devices with a<br />
hyper-angulated blade. Its ergonomic design ensures i-view is easy to use, and the<br />
integral LCD screen provides an optimal view in a variety of light conditions.<br />
By combining all the advantages of a fully integrated video laryngoscope in a single use,<br />
disposable product, i-view is also ideal for use where there are concerns regarding<br />
infection control, providing a cost-effective solution that is ready to use seconds after<br />
removing from the packaging.<br />
Visit our dedicated website page www.intersurgical.com/info/iview to view the video,<br />
download the information sheet or make an enquiry.<br />
Access to the article can be found on the Dave Airways blog: https://daveairways.<br />
Subscription Information – <strong>Autumn</strong> <strong>2020</strong><br />
<strong>Resus</strong>citation <strong>Today</strong> is a tri-annual publication<br />
published in the months of March, June and<br />
September. The subscription rates are as<br />
follows:-<br />
wordpress.com/<strong>2020</strong>/06/21/the-i-view-videolaryngoscopy-and-tracheal-intubationfor-patients-with-suspected-or-confirmed-covid-19/<br />
Or through the ‘Interact with us’ section of the i-gel ® supraglottic airway website:<br />
https://www.intersurgical.com/info/igel-interact<br />
Contact information:<br />
Intersurgical<br />
Crane House<br />
Molly Millars Lane<br />
Wokingham<br />
Berkshire RG41 2RZ<br />
England<br />
Tel: 0118 9656 300<br />
Email: info@intersurgical.com<br />
Website: www.intersurgical.com<br />
respiratory infections who may be<br />
a source of aerosolised infectious<br />
pathogens and who also require<br />
supplementary oxygen.<br />
Combining an oxygen delivery<br />
system with a filter media<br />
covering the exhalation ports,<br />
it is designed to reduce the risk<br />
to paramedics, hospital staff<br />
and visitors.<br />
providing improved level of<br />
fit and comfort<br />
• On-chin positioning<br />
providing a better fit to a wider<br />
range of face shapes<br />
• Low elastic position<br />
eliminating trauma to the<br />
The complete solution from<br />
the respiratory care specialists<br />
View our full Infection Control range:<br />
www.intersurgical.co.uk/info/InfectionControl<br />
AMBULANCE_UK_Half_Page_FiltaMask_<strong>2020</strong>_07.indd 1 24/07/<strong>2020</strong> 14:55<br />
This issue edited by:<br />
David Halliwell<br />
MSc Paramedic<br />
c/o Media Publishing Company<br />
Media House<br />
48 High Street<br />
SWANLEY, Kent BR8 8BQ<br />
CONTENTS<br />
<strong>Resus</strong>citation <strong>Today</strong><br />
ADVERTISING & CIRCULATION:<br />
Media Publishing Company<br />
Media House, 48 High Street<br />
SWANLEY, Kent, BR8 8BQ<br />
Tel: 01322 660434 Fax: 01322 666539<br />
E: info@mediapublishingcompany.com<br />
www.MediaPublishingCompany.com<br />
PUBLISHED:<br />
Spring, Summer and <strong>Autumn</strong><br />
COPYRIGHT:<br />
Media Publishing Company<br />
Media House<br />
48 High Street<br />
SWANLEY, Kent, BR8 8BQ<br />
PUBLISHERS STATEMENT:<br />
The views and opinions expressed in<br />
this issue are not necessarily those of<br />
the Publisher, the Editors or Media<br />
Publishing Company.<br />
Next Issue Spring 2021<br />
UK:<br />
Individuals - £12.00 inc. postage<br />
Commercial Organisations - £30.00 inc. postage<br />
Rest of the World:<br />
Individuals - £60.00 inc. postage<br />
Commercial Organisations - £72.00 inc. postage<br />
We are also able to process your<br />
subscriptions via most major credit<br />
cards. Please ask for details.<br />
Cheques should be made<br />
payable to MEDIA PUBLISHING.<br />
Designed in the UK by me&you creative<br />
RESUSCITATION TODAY - AUTUMN <strong>2020</strong><br />
3
EDITORS COMMENT<br />
EDITORS COMMENT<br />
With the focus for so many of us having been Covid 19 for many many months<br />
we decided to maintain the Covid 19 theme here in the <strong>Autumn</strong> edition of<br />
<strong>Resus</strong>citation <strong>Today</strong>.<br />
We have some new scientific articles, including a fascinating article from Professor Sir Keith Porter<br />
who discusses penthrox.<br />
“...it has been<br />
fascinating to<br />
share experiences<br />
and best practices<br />
with practitioners<br />
from around the<br />
world during these<br />
Both the American Heart Association and the ERC are set to release new resuscitation guidelines<br />
in the new year and have been asking for comments on the scientific advice before it is provided<br />
to us via the <strong>Resus</strong>citation Council UK.<br />
There have been many “on line resuscitation congresses”, in both Adult and Child <strong>Resus</strong>citation<br />
and it has been fascinating to share experiences and best practices with practitioners from<br />
around the world during these events.<br />
If you have interesting articles you would like to put forwards for publication in this journal during<br />
2021 please send them to info@mediapublishingcompany.com<br />
Monivent Ad - MDT/Lifecast A4 June <strong>2020</strong> David a..pdf:Layout Halliwell 1 12/6/20 14:05 Page 1<br />
events.”<br />
MSc Paramedic<br />
MEET A FEW OF OUR GROWING FAMILY<br />
RESUSCITATION TODAY - AUTUMN <strong>2020</strong><br />
For further information or to arrange a demonstration, please contact:<br />
Lifecast Body Simulation Ltd, Workshop 6, Elstree TV & Film Studios, London WD6 1JG<br />
4<br />
Enquiries: 01202 823 175 or 01202 8324 2376<br />
E-mail: info@lifecastbodysim.com www.lifecastbodysim.com
i-view <br />
<br />
<br />
<br />
<br />
Single-use<br />
No reusable components<br />
Fully disposable<br />
No reprocessing<br />
Minimises the risk<br />
of cross contamination<br />
i-view<br />
video laryngoscopy<br />
wherever and whenever you intubate<br />
www.intersurgical.co.uk/info/iview<br />
lnteract with us<br />
Quality, innovation and choice<br />
www.intersurgical.co.uk
FEATURE<br />
COVID-19 PANDEMIC PREPARATION: USING<br />
SIMULATION FOR SYSTEMS-BASED LEARNING<br />
TO PREPARE THE LARGEST HEALTHCARE<br />
WORKFORCE AND SYSTEM IN CANADA<br />
Mirette Dubé 1* , Alyshah Kaba 1,2 , Theresa Cronin 1 , Sue Barnes 1 , Tara Fuselli 1 and Vincent Grant 1,3,4<br />
Dubé et al. Advances in Simulation (<strong>2020</strong>) 5:22 https://doi.org/10.1186/s41077-020-00138-w © The Author(s). <strong>2020</strong><br />
Abstract<br />
Healthcare resources have been strained to previously unforeseeable<br />
limits as a result of the COVID-19 pandemic of <strong>2020</strong>. This has prompted<br />
the emergence of critical just-in-time COVID-19 education, including<br />
rapid simulation preparedness, evaluation and training across all<br />
healthcare sectors. Simulation has been proven to be pivotal for both<br />
healthcare provider learning and systems integration in the context<br />
of testing and integrating new processes, workflows, and rapid<br />
changes to practice (e.g., new cognitive aids, checklists, protocols)<br />
and changes to the delivery of clinical care. The individual, team,<br />
and systems learnings generated from proactive simulation training<br />
is occurring at unprecedented volume and speed in our healthcare<br />
system. Establishing a clear process to collect and report simulation<br />
outcomes has never been more important for staff and patient safety<br />
to reduce preventable harm. Our provincial simulation program in the<br />
province of Alberta, Canada (population = 4.37 million; geographic<br />
area = 661,848 km 2 ), has rapidly responded to this need by leading<br />
the intake, design, development, planning, and co-facilitation of<br />
over 400 acute care simulations across our province in both urban<br />
and rural Emergency Departments, Intensive Care Units, Operating<br />
Rooms, Labor and Delivery Units, Urgent Care Centers, Diagnostic<br />
Imaging and In-patient Units over a 5-week period to an estimated<br />
30,000 learners of real frontline team members. Unfortunately, the<br />
speed at which the COVID-19 pandemic has emerged in Canada may<br />
prevent healthcare sectors in both urban and rural settings to have<br />
an opportunity for healthcare teams to participate in just-in-time in<br />
situ simulation-based learning prior to a potential surge of COVID-19<br />
patients. Our coordinated approach and infrastructure have enabled<br />
organizational learnings and the ability to theme and categorize a mass<br />
volume of simulation outcome data, primarily from acute care settings<br />
to help all sectors further anticipate and plan. The goal of this paper<br />
is to share the unique features and advantages of using a centralized<br />
provincial simulation response team, preparedness using learning and<br />
systems integration methods, and to share the highest risk and highest<br />
frequency outcomes from analyzing a mass volume of COVID-19<br />
simulation data across the largest health authority in Canada.<br />
Keywords: Simulation, COVID-19; debriefing, Systems integration,<br />
Pandemic preparation, Quality, Safety, Organizational learning<br />
Introduction<br />
RESUSCITATION TODAY - AUTUMN <strong>2020</strong><br />
With the emergence of the COVID-19 pandemic of <strong>2020</strong>, healthcare<br />
resources have been strained to unforeseeable capacities, promoting<br />
the need for rapid, effective, and efficient preparedness. This has<br />
prompted the emergence of just-in-time preparedness strategies,<br />
including simulation for systems evaluation and healthcare provider<br />
(HCP) learning to support planning across healthcare sectors [1–9].<br />
Simulation has been pivotal for systems testing and integrating new<br />
and improved components such as novel workflows, protocols, and<br />
cognitive aids with rapid changes to practice and care delivery. Finding<br />
clear approaches to rapidly collect and report what is working well and<br />
what needs to change is urgently required for HCP and patient safety to<br />
ultimately reduce preventable harm.<br />
The provincial simulation program, named eSIM (educate, simulate,<br />
innovate, motivate) in the province of Alberta, Canada (population<br />
= 4.37 million; geographic area = 661,848 km2, [10]), has rapidly<br />
responded to preparedness training by establishing a central eSIM<br />
provincial COVID response team (similar to an emergency command<br />
center operations team for simulation) to facilitate a large-scale<br />
project managing the initiation, planning, execution, and performance/<br />
monitoring of a provincial COVID-19 simulation response [11]. Over just<br />
5 weeks, this response team enabled a harmonized intake process,<br />
design, and development of a robust COVID-19 simulation curriculum,<br />
mobilized a data collection/outcome reporting team, and a response<br />
plan to facilitate over 400 acute care simulation session requests across<br />
Alberta’s broad geographical zones. This coordinated approach and<br />
infrastructure enabled an integrated provincial multi-site simulation<br />
response, allowing the ability to rapidly theme and categorize a mass<br />
number of simulation findings (over 2,500 systems issues) from over<br />
30,000 learners (HCP) on the frontline. The simulation “command<br />
center” served to disseminate the outcomes across a large single health<br />
authority to further support ongoing planning, develop and refine the<br />
curriculum, and remain a specialized contact team of simulation experts<br />
for all health sectors (primarily acute care; urban and rural).<br />
The goal of this paper is to share the unique features and advantages of<br />
using a centralized provincial simulation response team, preparedness<br />
using learning and systems integration methods, and to share the<br />
6<br />
*<br />
Correspondence: mirette.dube@ahs.ca<br />
1<br />
eSIM Provincial Simulation Program, Alberta Health Services, Alberta Health Services, 1403 29th Street NW, Calgary, Alberta T2N 2 T9, Canada<br />
Full list of author information is available at the end of the article
FEATURE<br />
highest risk and highest frequency outcomes from analyzing a mass<br />
volume of COVID-19 simulation data across the largest health authority<br />
in Canada.<br />
Background<br />
Alberta Health Services: largest integrated healthcare system in<br />
Canada<br />
Alberta Health Services (AHS) has a centralized approach to its<br />
leadership and core operational functions (e.g., human resources<br />
and information technology) and provides medical care at over 650<br />
facilities across the province, including 106 acute care hospitals and<br />
25,653 continuing care beds/spaces, five stand-alone psychiatric<br />
facilities, 2723 addiction and mental health beds and 243 community<br />
palliative and hospice beds. AHS has over 125,000 employees and<br />
over 10,000 physicians and service accountability zones are divided<br />
into five geographical areas: North, Edmonton, Central, Calgary,<br />
and South [10]. There are few organizations in the world, which are<br />
comparable to AHS’ integrated healthcare system relative to its size<br />
and capacity [12], making it a unique opportunity to glean insights and<br />
lessons learned from COVID-19 pandemic preparedness.<br />
Pandemic preparedness and planning: role of simulation for<br />
team training and systems integration<br />
While disaster planning has become core content within some training<br />
curricula, the majority of health professionals remain ill prepared to<br />
deal with large scale disasters and will not encounter these critical<br />
scenarios in practice [13, 14]. Simulation is one method that has been<br />
identified to improve readiness and preparedness in times of disaster<br />
through deliberate practice and exposure to rare situations [15–18].<br />
Simulation-based learning has historically focused on individual and<br />
team training of practicing HCPs [19–25], although it has evolved to<br />
include just-in-time in situ training within the actual clinical environment<br />
[26–28] including simulation for systems integration (SIS), targeting<br />
the testing and integration of systems and processes (e.g., workflows,<br />
care pathways) that are uniquely important to disaster preparedness<br />
[29–32].<br />
the literature [8, 9, 26–28]. Pandemics place high demands on clinical<br />
care and potential risk of contamination for HCP, which increases<br />
the fear of spread to others [1, 36, 37]. Deliberate practice through<br />
simulation can reduce the cognitive load of HCP involved in direct<br />
frontline patient care, potentially mitigating latent safety threats (LSTs)<br />
(e.g., errors in design, organization, and/or training that may have a<br />
significant impact on patient safety) in times of extended pressure,<br />
exhaustion, and burnout [38].<br />
As recently illustrated in both Italy [2] and Singapore [3], simulation is<br />
key to preparedness by optimizing work flow structures, developing<br />
new processes, managing staffing levels, procuring equipment, bed<br />
management, and enforcing consistency of medical management of<br />
patients. In those ways, simulation can be used as both a learning and<br />
evaluation tool (e.g., SIS/SFD) [32]. Diekmann et al. also described<br />
the potential of using simulation to improve hospital responses to the<br />
COVID-19 crisis [6]. Recently published COVID-19 simulation papers<br />
[8, 9] share lessons learned in an attempt to support organizations<br />
that may seek to use simulation for diagnosing, testing, and<br />
embedding these approaches within pandemic constraints. While<br />
these papers do not provide specific outcomes from their system<br />
simulations, they share practical tips, tools, scenarios, debriefing<br />
questions, and resources which can be used to analyze the current<br />
needs and responses to potentially mitigate the negative impacts<br />
of the COVID-19 crisis. Similarly, Chan and Nickson [7], published<br />
an example of practical considerations for organizations in the<br />
development for just-in-time simulation training, including the scenario<br />
development, prebriefing, and debriefing, using system and process<br />
simulation for the testing of airway management for suspected/<br />
confirmed cases of COVID-19. While many of the findings in the<br />
emergent literature above glean insights into the use of simulation<br />
as both a learning and evaluation tool to prepare for COVID-19, a<br />
key gap identified is that many of these outcomes are unique to the<br />
experience of one specific site or one unique institution, which limit<br />
the generalizability and scalability of the findings. This is especially<br />
important when using simulation for pandemic preparedness to rapidly<br />
test systems and processes and prepare frontline teams to care for<br />
potential COVID-19 patients.<br />
The eSIM COVID-19 response team has been involved in pioneering<br />
work in SIS [11, 32, 33] systems integration, an engineering term<br />
defined as bringing many subsystems together into one better<br />
functioning system, has the potential to improve the safety and<br />
quality of care through re-engineering of the processes and systems<br />
in which HCP work [34]. The system engineering initiative for patient<br />
safety (SEIPS) 2.0 model provides a framework outlining how the<br />
work system components (e.g., tools/technology, tasks, environment,<br />
people/teams) provide a matrix for thematically categorizing system<br />
focused debriefing (SFD) outcomes in a complex adaptive healthcare<br />
system [35]. SIS/SFD allows testing of new processes within<br />
healthcare systems to inform design and utility, and to identify system<br />
issues proactively to prevent harm [15, 19–21].<br />
The rapid onset of the COVID-19 crisis is having a profound impact<br />
on global health, increasing demand, and risks on healthcare systems<br />
due to rapidly changing and unpredictable circumstances. The use<br />
of in situ simulation as a proactive risk mitigation strategy to prepare<br />
healthcare organizations for pandemic planning is well supported in<br />
Therefore, an identified need in the literature is the ability to proactively<br />
identify systems issues, while testing new pandemic processes in real<br />
time, and sharing these organizational learnings and system-level<br />
outcomes on a mass scale to both anticipate and plan for COVID-19.<br />
This is an invaluable opportunity to support healthcare organizations’<br />
preparedness during a global pandemic.<br />
COVID-19 simulation project approach<br />
Our provincial simulation program rapidly mobilized to respond to<br />
our organization’s need by establishing a central simulation COVID<br />
response team and a large-scale evaluation project to manage the<br />
initiation, planning, execution, and performance/monitoring for all<br />
simulation-based requests. The following sections will summarize our<br />
project evaluation approach based on common project phases [39]:<br />
(A) project initiation and planning; (B) project execution; (C) project<br />
performance and monitoring; (D) organizational learning; and (E)<br />
reporting of outcomes.<br />
RESUSCITATION TODAY - AUTUMN <strong>2020</strong><br />
7
FEATURE<br />
Project initiation and planning<br />
Rapidly designating the eSIM COVID-19 response team allowed<br />
a centralized contact and triage system across the province for all<br />
simulation-based requests coming from hundreds of centers, allowing<br />
coordination, planning, and resource oversight for simulation training.<br />
Team members included a team lead, geographically dispersed<br />
eSIM consultants (clinicians whose workplace role is to lead the<br />
design, delivery, faculty development, and evaluation of simulation<br />
methodologies and projects at AHS) and a designated data and<br />
outcomes team solely responsible for theming and categorizing<br />
thousands of simulation data points from COVID-19 simulations.<br />
The simulation infrastructure in place in AHS prior to COVID-19 (e.g.,<br />
eSIM consultants positioned in every zone (rural, urban, and mobile<br />
program) and > 1300 eSIM-trained simulation educators across<br />
AHS) ensured every geographical zone was supported. The intake<br />
process was maintained through a central spreadsheet accessible to<br />
the entire provincial team and a needs assessment facilitated by an<br />
eSIM consultant (Additional file 1 intake form) to ensure the needs and<br />
objectives aligned with established simulation-based methodologies<br />
and capacity. Requests were prioritized as they were processed and<br />
whenever possible, prior relationships with simulation-trained educators<br />
comfortable with the use of simulation-based methods were leveraged<br />
to help facilitate the large number of sessions. eSIM consultants either<br />
fully led the sessions, initiated sessions while mentoring others to<br />
replicate delivery on an on-going basis (especially when large numbers<br />
of HCP were involved), and/or shared resources with faculty who had<br />
the capacity and experience to lead sessions independently.<br />
The first wave of intake requests (and patients) in Alberta, organically<br />
flooded from Emergency Departments, followed by Intensive Care<br />
Units, Operating Rooms, Labor and Delivery Units, and Neonatal<br />
ICUs in Calgary. Simulations were triaged for COVID-19 training and<br />
preparedness for the highest risk locations and activities across acute<br />
care. A second wave of requests included diagnostic imaging and<br />
inpatient medical units (including newly created inpatient units for<br />
COVID-19, among others). A similar pattern of requests followed from all<br />
of the five geographic zones in Alberta in concordance with the number<br />
of COVID-19 cases starting to move through the system. Daily response<br />
team meetings ensured strategic planning with eSIM consultants to then<br />
specifically target and reach out to acute care sites with no simulation<br />
trained champion, those who had not made any requests, and to ensure<br />
simulation support and curriculum resources were shared across all<br />
zones.<br />
Curriculum development<br />
A novel part of our approach was the creation of a robust, centrally<br />
located simulation curriculum, which was rapidly developed and<br />
mobilized over a 10-day period at the onset of the COVID-19 simulation<br />
response. Curriculum content was vetted through medical experts,<br />
clinical leaders, Infection Prevention and Control consultants, and<br />
the organization’s Emergency Command Center to ensure accuracy,<br />
alignment, and validity before application. New emerging curriculum<br />
resources for COVID-19 were reviewed daily to ensure the most relevant<br />
up-to-date information was reflected within current best practice<br />
recommendations. The curriculum included COVID-19 simulation<br />
scenarios for all sectors, and included a prebriefing script, debriefing<br />
tools [32], cognitive aids, “how-to” guides and shared webinars.<br />
Curricular materials were shared over the 5-week period with over 600<br />
teams across AHS.<br />
Objectives for the COVID-19 simulation scenarios were based on the<br />
highest risk and highest impact system issues identified and prioritized<br />
by integrated interprofessional teams of clinicians, managers, and<br />
educators—based on their units/departments greatest needs. Table<br />
1 provides samples of frequently used scenario objectives across all<br />
simulations and their related work system categories [35].<br />
Project execution<br />
Central to our unique approach was the planning and execution of<br />
three common simulation-based methods to prepare teams and the<br />
healthcare system during COVID-19 preparedness (Table 2). These<br />
methods include (1) surge planning and table top debriefing;<br />
RESUSCITATION TODAY - AUTUMN <strong>2020</strong><br />
Table 1 Sample COVID-19 simulation scenario objectives (highest risk and highest frequency)<br />
Examples of some COVID-19 scenario objectives (pre-determined to be highest risk and highest frequency)<br />
Equipment: Implement creation of carts for personal protective equipment/intubation<br />
Cognitive aids: Apply airway pause with COVID-19 additions<br />
Paging systems: Assess addition of “COVID-19” stem to pages to ensure HCP safety and priority response<br />
Task complexity: Prepare smaller specialized teams for intubation (e.g., airway response team)<br />
Prepare smaller teams to anticipate and prepare for any aerosol-generating medical procedure<br />
Designate and prepare personal protective equipment (PPE) coach for donning and doffing<br />
Organize clean runner role to help with cognitive overload<br />
Signage: Evaluate plan for new areas for COVID-19 vs non-COVID-19 patients (surge specific phases)<br />
Transport routes: Assess, plan, testing of dedicated hallways and elevators<br />
Assess staffing during day and night with Intensive Care Unit surge bed plans and escalating to 2 patients per room<br />
Site capacity and triggers: Evaluate pandemic surge exercises identifying triggers, bed capacity, flow restrictions, and<br />
continuity across the site<br />
Communication pathways: Apply testing of handover tools and new alerts<br />
Workflow: Identify appropriate number staff/roles caring for patient(s)<br />
Policies (testing of new or existing): Appraise any unnecessary and preventable delays in care and/or process<br />
System issue categories<br />
[35]<br />
Tools and technology<br />
People and tasks<br />
Environment<br />
Organization<br />
Processes<br />
8
FEATURE<br />
Table 2 Method, objective, and examples of intake requests<br />
Method Objective(s) Sample of intake requests<br />
Table top exercises<br />
Process walk-through/<br />
environmental scan<br />
with debriefing<br />
Rapid cycle simulation<br />
and debriefing<br />
• Surge planning<br />
• Bed capacity allocation<br />
• Identify LSTs, new workflows, new processes, using a<br />
systems approach to debriefing<br />
• Training small groups of interprofessional teams in rapid<br />
cycle simulation training and debriefing (once processes<br />
are established). Most often 20-min simulations followed<br />
by 20-min debriefings.<br />
• Assess a hospital’s emergency response operational plan<br />
related to current bed capacity and pandemic surge<br />
planning phases 1 through 4.<br />
• Align organizational pandemic policies with current local<br />
current state resources to bridge expectations of front line<br />
staff and pandemic policy makers.<br />
• Determine new processes for a COVID stroke patient from<br />
CT (computed tomography) scan to emergency intubation<br />
to angiography.<br />
• Determine workflow process from the emergency room<br />
triage through to an isolation room for a team COVID-19 intubation<br />
process.<br />
• Determine the environmental layout and associated<br />
workflows, including LSTs when ventilating two patients in<br />
one Intensive Care Unit room (new processes, staffing<br />
ratios), testing of IT-related issues and central alarm bank.<br />
• Determining new and unique processes and educational<br />
needs within indigenous health centers and communities<br />
to ensure safety of vulnerable populations and ensuring<br />
preparedness.<br />
• Apply new processes of patient flow from triage to isolation<br />
room including intubation, safe PPE processes for all<br />
emergency departments in Calgary over 2 days (4 adult<br />
sites). a<br />
• Apply COVID-19 medical management to a complex medical<br />
scenario.<br />
a Approximately 250 interprofessional team members per site (including physicians, nurses, respiratory therapists, infection prevention and control (IPAC) staff,<br />
environmental services, clinical leaders, and other non-clinical team members such as protective services)<br />
(2) process walkthrough and environmental scans; and (3) rapid cycle<br />
simulation and debriefing. Both learnerfocused and system-focused<br />
debriefing approaches were used across these three methods [22, 32].<br />
Surge planning and table top debriefing<br />
In some instances, eSIM consultants and human factors (HF)<br />
specialists led the co-facilitation and debriefing of table top surge<br />
planning exercises. These exercises allowed for proactive pandemic<br />
surge planning assessment of facility, departments, programs,<br />
and services related to COVID-19 patient flow. eSIM and HF were<br />
then utilized for designing decision algorithms, observation of new<br />
work processes and work environments, and identifying further<br />
improvement opportunities.<br />
Rapid cycle simulation and debriefing<br />
Once final COVID-19 processes and workflows were established,<br />
departments/clinical areas progressed to rapid cycle simulation training<br />
followed by debriefing [41]. This involved rapid training sessions<br />
(average 20-min scenario duration followed by 20-min debriefings) to<br />
ensure small groups of interprofessional team members were able to<br />
apply new processes in the live clinical environment prior to use with<br />
actual patients. All questions related to medical management, infection,<br />
prevention and control (IPAC) and process were also debriefed during<br />
these sessions.<br />
Project performance and monitoring<br />
Process walkthrough and environmental scans<br />
Early preparatory work focused on using a systems approach to<br />
co-design new COVID-19 processes and spaces. These physical<br />
walkthrough simulations were based on day-to-day movement,<br />
case-specific patient presentations, and workflows that would be<br />
impacted by COVID-19. They were also used to train multiple HCPs<br />
to orientate them to the new COVID-19 response for their areas (see<br />
Additional file 2 for key points to consider in a process walkthrough<br />
environmental scan planning exercise). The primary focus was on<br />
identifying LSTs prior to the first patient experience which allowed for<br />
application of a new processes in a plan, do, study, act (PDSA) cycle<br />
[40]. The team moved through a department/clinical area, doing an<br />
environmental scan for barriers, identification of missing equipment,<br />
testing of communication pathways, and identification of new tasks/<br />
roles/responsibilities. Any changes to the space and processes were<br />
actioned to leadership.<br />
Data collection and analysis<br />
A data outcomes team was designated to rapidly process and analyze<br />
data collected from all provincial COVID-19 simulations. Figure 1<br />
outlines a systematic iterative process developed for intake and entry of<br />
data. An initial coding scheme for categorization of data was created.<br />
Data analysis included the theming of system-focused debriefing<br />
outcomes [32] based on the SEIPS 2.0 system categories (e.g., tools/<br />
technology, tasks, environment, people/teams) [35]. All outcome data<br />
were analyzed to determine convergence of themes and repeated<br />
expression of reoccurring constructs. Discrepancies in the codes and<br />
labeling of themes were discussed by the core project team regularly<br />
and resolved; with themes simplified and altered accordingly until<br />
complete agreement was reached. Saturation of emergent themes was<br />
reached across > 400 simulation sessions provincially. The number<br />
of learners/participants and simulation sessions was collected using a<br />
standardized intake spreadsheet and was collated biweekly.<br />
RESUSCITATION TODAY - AUTUMN <strong>2020</strong><br />
9
FEATURE<br />
Fig. 1 Systematic process for intake and entry of data<br />
Organizational learning<br />
Fig. 1 Systematic process for intake and entry of data<br />
When using a simulation for systems integration approach, the<br />
collection and sharing of systems issues and learnings is key to<br />
informing a parent organization. The eSIM program’s infrastructure and<br />
approach was critical in a pandemic situation, as the information and<br />
learnings from the SIS were used to iteratively make improvements<br />
and help teams across the organization anticipate and plan for issue<br />
mitigation and process improvement. The timely analysis of large<br />
volumes of data that was being collated and themed in real time by the<br />
eSIM response team proactively informed and enabled scaling up of<br />
quality improvement activities across sites, departments, and zones.<br />
Our organizational learning included broad sharing of weekly dashboard<br />
updates of key outcomes, webinars (local and international webinars<br />
shared across the entire AHS organization and beyond resulting in over<br />
4000 unique views; recording shared with > 100, 000 email addresses)<br />
[4, 42], and key COVID-19 resources developed for simulation.<br />
COVID-19 simulation project key outcomes<br />
Highest impact and highest frequency outcomes<br />
The provincial eSIM COVID-19 simulation response team facilitated<br />
simulation session requests by leading the intake, design, development,<br />
planning, and facilitation of over 400 acute care simulation sessions<br />
across all sectors of our provincial health program. In under a 5-week<br />
period, an estimated 30,000 learners participated in simulation in both<br />
rural (17%) and urban (83%) centers across the province (Fig. 2).<br />
There was a wide variance in the number of sessions/learners per<br />
request ranging from 1-3 days of simulation training and 10-400<br />
people requiring training per request. Well over 2500 systems issues,<br />
including LSTs, have been proactively identified and mitigated through<br />
> 400 simulation sessions. Systems issues across all sessions were<br />
categorized into processes (61%), tools and technology (14%), persons<br />
and tasks (14%), environment (7%), and organization (4%).<br />
RESUSCITATION TODAY - AUTUMN <strong>2020</strong><br />
Fig. 2 Estimated number of participants in COVID-19 preparedness simulation by department<br />
Fig. 2 Estimated number of participants in COVID-19 preparedness simulation by department<br />
10
FEATURE<br />
Table 3 highlights the highest priority themes discussed in the<br />
debriefings (impact) and the highest reported outcomes (frequency)<br />
that emerged from all COVID-19 simulations.<br />
In analyzing the nine themes, it is clear that the rapid knowledge<br />
translation of best practices, new guidelines, and processes<br />
following system simulation events can potentially serve other<br />
organizations that may seek to learn from our centralized,<br />
coordinated approach to using system integration simulation for<br />
pandemic planning and preparedness.<br />
In synthesizing the learnings from the highest impact and highest<br />
frequency outcomes of the 9 themes reported in Table 3, there are<br />
several reasons on why these salient themes came together based on<br />
our unique context and organizational level approach to SIS. Each of<br />
these themes informed our organization as to what was working well<br />
at one site, department, and zone and what needed to be improved<br />
and scaled up across the organization. For example, although we<br />
had an IPAC team, and multiple related resources and cognitive aids<br />
designed to support IPAC processes; it became clear, as identified<br />
by the frontline through simulation, that more needed to be done to<br />
address the nuances and unique clinical practices of IPAC specific<br />
to the pandemic. While hundreds of learners continued to struggle<br />
with safe doffing, simulation was able to inform the development of<br />
emerging best practices surrounding 1:1 doffing, what questions were<br />
repeatedly being discussed; why breaches were happening; and<br />
ensuring one person guided and supported individuals during doffing.<br />
Observing the trending of process-related systems issues enabled<br />
our team to share this finding broadly and focus our simulation tools<br />
and approaches to further address systems issues that impacted<br />
not just one unit, site or department enabling the learnings identified<br />
through simulation to be scaffolded and shared across the entire<br />
province. This led to further development of a systemsbased process<br />
walk through approach, with debriefing, to ensure a systematic<br />
identification of process issues.<br />
Repeated SIS debriefings where frontline team members asked<br />
about personal items such as watches, earrings, and identification<br />
badges in COVID rooms allowed us to share rapidly evolving<br />
strategies to address proper maintenance of isolation environments<br />
and the prevention of contamination. For teams who were struggling<br />
with effective ways to communicate outside of COVID rooms, we<br />
were able to rapidly share innovations on a large scale to any other<br />
teams who were in the same position in preparing their unit and<br />
staff to respond to the evolving nature of the global pandemic. This<br />
involved designing, through simulation, innovative approaches<br />
necessary to keep staff and patients safe by communicating using<br />
dry erase markers on glass between rooms, as one example. As<br />
protected COVID-19 intubations were identified as a high anxiety<br />
and high-risk time for healthcare workers, as shown by repeated<br />
simulation requests from healthcare staff targeting these objectives,<br />
having the ability to test these processes in simulation and refine a<br />
critical care medicine cognitive aid for pre-intubation and then share<br />
these findings on such a large scale was essential to successful<br />
preparation and safety of staff. As a result of multiple simulations<br />
on intubation, a COVID-19 cognitive aid was developed, which was<br />
then contextualized for rural sites and then broadly shared across the<br />
province using our coordinated system.<br />
Discussion<br />
Our use of simulation for systems integration involved taking a project<br />
approach to the initiation, planning, execution, and reporting [39] (e.g.,<br />
shared learnings) to enable proactive improvement work for safer, more<br />
efficient, and reliable care processes for patients and healthcare teams<br />
[43–50]. This paper adds to the emerging literature on using simulation<br />
for pandemic planning and preparedness [8, 9] as it describes a<br />
highly coordinated COVID-19 pandemic simulation response using a<br />
centralized team, robust valid curriculum, and data outcomes team to<br />
analyze and rapidly share an unprecedented volume of simulation data<br />
for a large-scale SIS project across the largest single health authority in<br />
Canada.<br />
Unfortunately, the speed at which the COVID-19 pandemic has emerged<br />
in Canada may prevent every acute care center in both urban and<br />
rural settings in having healthcare teams participate in “just-in-time”<br />
in situ simulation-based learning and systems/process. The ability to<br />
test new pandemic processes, and share organizational learnings to<br />
be disseminated on a mass scale has been pivotal in preparing our<br />
healthcare system to respond to the emergent threat of COVID-19.<br />
The importance of using simulation as a “first choice” strategy for<br />
ensuring individual, team, and system readiness in times of crisis is<br />
supported by multiple publications in the literature [5, 51–53], and<br />
highlights that a sustained investment in simulation programs will<br />
have immeasurable impacts across healthcare systems following<br />
the pandemic. Many of these papers [3, 6–9] indicate a single site or<br />
unit approach to pandemic preparation, although do not specifically<br />
highlight using a coordinated and centralized simulation team,<br />
development of robust valid curriculum, and real time data analysis<br />
of emerging themes from hundreds of simulations. Although “more”<br />
may not necessarily always be better, we advocate that during times of<br />
pandemic where time sensitivity and reliable information are of utmost<br />
importance, a coordinated organizational-wide simulation response<br />
approach allows for broader and faster sharing, scalability, and<br />
generalizability of the findings. The validation of these 9 themes from<br />
simulations across multiple sites and teams outweighs the findings at<br />
only one.<br />
One of the emerging findings that differed our project from other<br />
COVID-19 system simulations experiences both nationally and globally<br />
in using simulation as both a learning and evaluation tool to prepare [3,<br />
6–9], was recognizing the critical importance of embedding simulation<br />
as a central part of the organizational learning, and the overall pandemic<br />
preparedness strategy. Similar to an operational “Emergency Command<br />
Center,” simulation programs (regardless of the size) need to situate<br />
themselves to be members “at the table” with key programs informing<br />
decision-making, and influencing organizational planning and pandemic<br />
preparedness from the beginning. Many factors influence the ability of<br />
simulation programs to “take this seat” including how the program is<br />
established prior to pandemic and how well it may be recognized by<br />
hospital administration staff in informing the organization of the needs<br />
and challenges coming directly from the frontline care providers. We<br />
situated ourselves as key informants to leaders and the organization’s<br />
administration, through planning and executing a large-scale simulation<br />
for systems integration project. Our outcomes, which identified over<br />
2500 systems issues, including LSTs, had meaning to the organization<br />
RESUSCITATION TODAY - AUTUMN <strong>2020</strong><br />
11
FEATURE<br />
RESUSCITATION TODAY - AUTUMN <strong>2020</strong><br />
Table 3 Highest impact and highest frequency outcomes<br />
Key themes and qualitative outcomes (highest impact and highest frequency) identified in simulation<br />
Systems categories<br />
1. Theme: Safe doffing (removal of PPE safely and in correct order) People/teams/tasks;<br />
Key outcomes<br />
Tools/technology<br />
Cross monitor team members during doffing<br />
Use and IPAC poster as a cognitive aid<br />
Ensure “1 to 1” doffing to avoid breaches observed when too many doffing at once (e.g., getting ahead or behind in<br />
doffing sequence)<br />
Consistent role of a “PPE Coach” to support safe doffing-ensure focus and intention with every step<br />
Implement “just-in-time” review of safe doffing to reduce cognitive load during long stressful periods in PPE.<br />
2. Theme: Conducting environmental scans of care areas is crucial in anticipating, planning ahead, and<br />
developing area processes<br />
Key outcomes<br />
Remove visitor chairs, extra equipment and linens from room to avoid waste, and additional cleaning<br />
between patients<br />
Keep transport routes<br />
Post signage for direction and decrease of clutter<br />
Creation of supply restocking checklist white this<br />
Creation of COVID-19 specific cart of required supplies<br />
Creation of small, labeled packages of specific supplies, or medications for fast grab and go<br />
Ensure team members are aware of the responsibilities required to maintain the space<br />
Ensure cleaning processes for removal of equipment leaving COVID-19 rooms (e.g., stretchers, wheelchairs)<br />
3. Theme: Conduct inter-departmental/inter-hospital transport routes to establish communication and process<br />
between departments and professions<br />
Key outcomes<br />
Test and walk through the route<br />
Use signage if COVID-19 routes differ from the usual process<br />
Clean hallways of clutter and reduce traffic if possible<br />
Consider dedicating elevator banks for COVID-19 patients, staff and carts<br />
Establish a designated clean person on transports to ensure surfaces are cleaned (e.g., floors, elevator buttons, stretchers,<br />
and wheel chairs)<br />
Emergency medical services should use a common Stem in communication and pages: This line is supposed to be with<br />
the one below to read: "Emergency medical services should<br />
“Possible/Confirmed COVID-19 patient” this goes afte the word "pages" in line above<br />
Upon arrival of out of external hospital emergency medical services, ensure transport is ready and routes are prepared.<br />
white this Should read; Upon arrival of externa;l hospital emergency medical services, ensure transport is ready and routes<br />
are prepared.<br />
Environment;<br />
Tools/technology;<br />
People/Teams/Tasks<br />
People/teams/tasks;<br />
Environment;<br />
Tools/technology<br />
4. Theme: Maintenance of isolation environment/prevention of contamination Tools/technology;<br />
Key outcomes<br />
People/teams/tasks<br />
Removal of stethoscopes, phones, ID badges, lanyards, watches, and earrings from person prior to donning.<br />
When items are on person, reinforce learnings re: do not reach below gown for ID badge/pager/mobile phone; or under<br />
visor to adjust goggles/mask.<br />
Creation of bins on an external cart in donning area for dropping items into<br />
Keep numbers of staff in the room low when possible<br />
Ensure cleaning process for roving items such as clipboards, ultrasound machines, etc.<br />
5. Theme: Roles and responsibilities People/teams/tasks;<br />
Key outcomes<br />
Environment<br />
A runner role is needed across multi areas: Operating Room, Emergency Department, Labor and Delivery Unit, Intensive<br />
Care Unit (team member to bring supplies between isolated COVID-19 care area and non-isolated area)<br />
Consider the involvement of HCAs and Unit Clerks to bring necessary equipment required for teams<br />
12
FEATURE<br />
Table 3 Highest impact and highest frequency outcomes (Continued)<br />
Key themes and qualitative outcomes (highest impact and highest frequency) identified in simulation<br />
Establish “clean” and “dirty” sides between rooms and within rooms by taping the floors for a visual cue<br />
Establish CODE COVID-19 team to attend to all rapid deteriorating patients<br />
because they were widespread and converged data from several sites<br />
including both urban and rural centers and across the continuum of<br />
care. In addition, we could equally share and reach all sites within<br />
our organizational structure for the new emerging themes we were<br />
uncovering in real time.<br />
We informed our organization on multiple levels through our webinars,<br />
dashboards, and relationships built across a large health authority.<br />
Queueing IPAC team members of ongoing concerns with best practices<br />
for safe doffing to enable targeted approaches; sharing weekly questions<br />
still arising from the frontline to the IPAC team; and then supporting<br />
the development of a “doffing buddy” program are a few examples.<br />
This example highlights that while the emerging literature on COVID-19<br />
simulations [3, 6-9] differ in their approach and scale of SIS, there is<br />
overlapping outcomes and triangulation of findings specific to IPAC<br />
across the different systems, countries, and jurisdictions. Essentially, this<br />
underlines the validity and robustness of the use of simulation for systems<br />
integration methodology for organizational learning.<br />
Systems categories<br />
6. Theme: Innovative approaches to communication Tools/technology;<br />
Key outcomes<br />
People/teams/tasks<br />
Use of dry erase markers on the shared glass wall of isolation to ante room<br />
Use of a laminated page that can be flipped back and forth<br />
Use of white boards to communicate key messages to outside team members<br />
Use of two-way radios (e.g., walkie talkies) and baby monitors<br />
Limit the use of negative pressure rooms and use ante rooms where available<br />
Use of speaker phone setting<br />
Use of tape on floor to communicate ‘clean versus dirty’ zones<br />
Check that monitors and speakers on phones (especially with PPE on) can be heard<br />
Include name/role tag stickers on outer PPE to ensure role clarity and effective communication<br />
Reduce noise and ensure use of closed-loop communication (additional communication challenges with PPE on)<br />
Use of trigger scripts on pagers to signal a priority response. Scripts like “COVID airway” or “COVID transport” to alert<br />
a team and get the right people and the right equipment to the right place.<br />
7. Theme: Psychological safety and speaking up People/teams/tasks<br />
Key outcomes<br />
Use critical language when breeches in PPE or when overcrowding in rooms occur<br />
Encourage all team members to speak up when they see breaches in safe PPE practices<br />
Removing hierarchical barriers can be challenging; promoting psychology safety is important for a cohesive team<br />
Go beyond your professional role to cross teach about PPE<br />
8. Theme: Critical care medicine pre-intubation cognitive aid People/teams/tasks;<br />
Key outcomes<br />
Tools/technology;<br />
Organization<br />
Communicate a plan ahead to ensure staff know their roles<br />
Double-check proper PPE during intubation<br />
Most experienced practitioner should perform the intubation<br />
Ensure the ventilator and video laryngoscopy device are in the room prior to start<br />
Consider back-up plan depending on available resources<br />
Ensure correct bagger filter is attached<br />
9. Theme: Use of cognitive aids and checklists Tools/technology<br />
Key outcomes<br />
Consider human factors science in the development of new COVID-19 cognitive aids and checklists<br />
Cognitive aids can be made into posters, use larger font, central point of reference white this<br />
They should be clear, easy to use adaptable to context, trained prior to implement, and pilot tested prior to use on a<br />
real patient<br />
Examples: COVID-19 airway pause checklist, checklists for buckets, and carts/bins, IPAC donning and doffing poster white this<br />
RESUSCITATION TODAY - AUTUMN <strong>2020</strong><br />
13
FEATURE<br />
RESUSCITATION TODAY - AUTUMN <strong>2020</strong><br />
We realized that process-related systems issues were widespread<br />
and the requests for environmental scans with debriefing prompted<br />
hundreds of teams to start redesigning their COVID care spaces after<br />
one of our “shared learnings” webinars. Seeing the rapid uptake of<br />
teams developing checklists and cognitive aids in isolation of each<br />
other, and with limited human factors experience, led us to establish<br />
collaborative human factors tools on how to develop an effective<br />
cognitive aid and principles of safe use. We believe all of these<br />
developments were the result of a swift and purposeful largescale<br />
centralized approach.<br />
Recognizing that not all health authorities have opportunity to coordinate<br />
or operationally support a centralized team and curriculum across sites;<br />
we recommend the explicit effort of simulation programs to align with<br />
other programs in meaningful ways to analyze and share emerging<br />
data in real-time to support validation for broader sharing and scalability<br />
when possible.<br />
The simulation methods and outcomes used in the COVID-19 response<br />
have had a profound impact on our teams, processes, and system<br />
functioning. Our experience offers other organizations’ learnings<br />
to glean and consider the importance of establishing a centralized<br />
simulation response team for scale, spread and speed of knowledge<br />
translation, implementation, and change management effectiveness.<br />
With on-going use of SIS sessions informing cycles of improvement,<br />
the simulation will continue to be a key organizational tool we will use<br />
to further manage this evolving crisis, as well as future needs of our<br />
healthcare organization. Our pandemic preparedness highlighted the<br />
essential use of simulation as both an evaluation tool capable of testing<br />
systems and processes, and identifying and mitigating LSTs, as well<br />
as an education tool capable of rapidly preparing frontline teams in<br />
terms of the changes identified above. This project has identified how<br />
the dissemination and broadcasting of curriculum and lessons learned<br />
(e.g., emerging themes, innovations, systems-based approaches) from<br />
simulation can rapidly help a large organization over a large geographic<br />
area be adequately prepared for an evolving situation like the COVID-19<br />
pandemic of <strong>2020</strong>.<br />
Supplementary information<br />
Supplementary information accompanies this paper at https://doi.<br />
org/10.1186/s41077-020-00138-w.<br />
Abbreviations<br />
AHS: Alberta Health Services; COVID: Coronavirus disease; COVID-19:<br />
Coronavirus disease 2019; eSIM: educate Simulate Innovate Motivate;<br />
HCA: Health care aides; HCP: Healthcare provider; HF: Human factors;<br />
ID: Identification badge; IPAC: Infection prevention and control; LST:<br />
Latent safety threat; PPE: Personal protective equipment; SEIPS: System<br />
engineering initiative for patient safety; SFD: System focused debriefing; SIS:<br />
Simulation for systems integration<br />
Acknowledgements<br />
The authors would like to recognize the many partnerships and people that<br />
enabled an impressive simulation response to the COVID-19 pandemic.<br />
This project, considering its scope and scale, would not have been possible<br />
without the efforts of many team members from the Alberta Health Services’<br />
eSIM Provincial Simulation Program, KidSIM Pediatric Simulation Program,<br />
and Covenant Health Authority. The authors would like to acknowledge the<br />
following people for their contributions to the project curriculum design,<br />
delivery, data entry, manuscript review, and input throughout the COVID-19<br />
simulation response project: Mark Allen, Ken Brisbin, Helen Catena, Jennifer<br />
Chatfield, Amy Cripps, Christina Eichorst, Andrea Faid, Monika Johnson,<br />
Erica Meunier, Annamaria Mundell, Albert Phung, Andrew Reid, Rob<br />
Ritchie, Jennifer Semaka, Cherie Serieska, Michael Sidra, Kristin Simard, Jill<br />
Soderstrom, Nadine Terpstra.<br />
The authors would also like to recognize Dan Duperron, Darren Steidl,<br />
and Sheneel Lal for biomedical engineering support; Juanita Clark for<br />
administrative support; AHS Design Lab Team (Ali Abid); AHS Infection<br />
Prevention and Control Team (Gwyneth Meyers); and the many simulation<br />
champions across the province of Alberta, including Drs. Gord McNeil,<br />
Jonathan Gaudet, Andrea Boone, Stuart Rose, Simon Ward, and Sharon<br />
Reece.<br />
Authors’ contributions<br />
MD, AK, TC, SB, TF, and VG were involved in the conceptualization, analysis,<br />
and interpretation of the data, drafting of the manuscript, and development of<br />
all figures and tables. The authors read and approved the final manuscript.<br />
Authors’ information<br />
MD is a Masters certified critical care Registered Respiratory Therapist with<br />
24 years of experience in healthcare. She has over thirteen years’ experience<br />
in simulation and debriefing; training hundreds of interprofessional teams,<br />
faculty development, simulation for systems integration and debriefing,<br />
undergraduate education, global health, human factors, design thinking,<br />
research, project and change management, former provincial Director of<br />
Quality and Patient Safety education, and leading provincial simulation<br />
and quality improvement projects. She is passionate about patient safety,<br />
improving healthcare systems, and has multiple peer-reviewed publications<br />
on interprofessional collaboration, team training, and using simulation and<br />
debriefing for systems improvement. During the COVID-19 pandemic of<br />
<strong>2020</strong>, MD was the eSIM Provincial Simulation Response Team Lead for the<br />
province of Alberta, Canada.<br />
Funding<br />
No funding was required for the development of this manuscript.<br />
Ethics approval and consent to participate<br />
No ethics approval or consent was needed for this manuscript.<br />
Consent for publication<br />
Not applicable<br />
Competing interests<br />
The authors declare that they have no competing interests.<br />
Author details<br />
1<br />
eSIM Provincial Simulation Program, Alberta Health Services, Alberta<br />
Health Services, 1403 29th Street NW, Calgary, Alberta T2N 2 T9, Canada.<br />
2<br />
Department of Community Health Sciences, Cumming School of Medicine,<br />
University of Calgary, Calgary, Canada. 3 Departments of Pediatrics and<br />
Emergency Medicine, Cumming School of Medicine, University of Calgary,<br />
Calgary, Canada. 4 KidSIM Pediatric Simulation Program, Alberta Children’s<br />
Hospital, 28 Oki Dr NW, Calgary, Alberta T3B 6A8, Canada.<br />
References<br />
1. Adams JG, Walls RM. Supporting the health care workforce during the COVID-19 global<br />
epidemic. JAMA. <strong>2020</strong>;323(15):1439–40.<br />
2. Grasselli G, Pesenti A, Cecconi M. Critical care utilization for the COVID-19 outbreak in<br />
Lombardy, Italy: early experience and forecast during an emergency response. JAMA.<br />
<strong>2020</strong>;323(16):1545–6.<br />
3. Wong J, Goh QY, Tan Z, Lie SA, Tay YC, Ng SY, et al. Preparing for a COVID-19 pandemic: a<br />
review of operating room outbreak response measures in a large tertiary hospital in Singapore.<br />
Can J Anesth Can Anesth [Internet]. <strong>2020</strong> 11 [cited <strong>2020</strong> Apr 28]; Available from: https://doi.<br />
org/https://doi.org/10.1007/s12630-020-01620-9.<br />
4. Dube M, Boon A, Gaudet J, Linton K, Myers G, Grant V, et al. AHS e-Sim Webinar: COVID 19<br />
simulation shared learning and resource review [Internet]. [cited <strong>2020</strong> Jun 9]. Available from:<br />
https://www.youtube.com/watch?v=pTFT7k4fhO0&feature=youtu.be.<br />
5. Li L, Lin M, Wang X, Bao P, Li Y. Preparing and responding to 2019 novel coronavirus<br />
with simulation and technology-enhanced learning for healthcare professionals:<br />
challenges and opportunities in China. BMJ Simul Technol Enhanc Learn. <strong>2020</strong> Mar<br />
12;bmjstel-<strong>2020</strong>-000609.<br />
14
FEATURE<br />
6. Dieckmann P, Torgeirsen K, Qvindesland SA, Thomas L, Bushell V, Langli EH. The use of<br />
simulation to prepare and improve responses to infectious disease outbreaks like COVID-19:<br />
practical tips and resources from Norway, Denmark, and the UK. Adv Simul. <strong>2020</strong>;5(1):3.<br />
7. Chan A, Nickson C. COVID-19 airway management: better care through simulation • LITFL<br />
[Internet]. Life in the Fast Lane • LITFL • Medical Blog. <strong>2020</strong> [cited <strong>2020</strong> Apr 28]. Available<br />
from: https://litfl.com/covid19-airwaymanagement-better-care-through-simulation/.<br />
8. Brazil V, Lowe B, Ryan L, Bourke R, Scott C, Myers S, et al. Translational simulation for rapid<br />
transformation of health services, using the example of the COVID-19 pandemic preparation.<br />
Adv Simul. <strong>2020</strong>;5(1):9.<br />
9. Brydges R, Campbell DM, Beavers L, Khodadoust N, Iantomasi P, Sampson K, et al. Lessons<br />
learned in preparing for and responding to the early stages of the COVID-19 pandemic: one<br />
simulation’s program experience adapting to the new normal. Adv Simul. <strong>2020</strong> Jun 3;5(1):8.<br />
10. Dube M, Barnes S, Cronin T, Serieska C, Meunier E, Mundell A, et al. Our story: building the<br />
largest geographical provincial simulation program in Canada. Accepted article in Medical<br />
Training Magazine,. Medical Training Magazine [Internet]. 2019 Jul;(3). Available from: https://<br />
medicalsimulation.training/articles/largest-geographical-provincial-simulation-proram/.<br />
11. Dubé M, Shultz J, Barnes S, Pascal B, Kaba A. Goals, recommendations, and the how-to<br />
strategies for developing and facilitating patient safety and system integration simulations.<br />
HERD Health Environ Res Des J. <strong>2020</strong>;13(1): 94–105.<br />
12. Alberta Health Services A. About AHS | Alberta Health Services [Internet]. 2019. Available<br />
from: https://www.mmiwg-ffada.ca/wp-content/uploads/2019/05/5.-About-AHS-_-Alberta-<br />
Health-Services.pdf.<br />
13. Alexander AJ, Bandiera GW, Mazurik L. A multiphase disaster training exercise for emergency<br />
medicine residents: opportunity knocks. Acad Emerg Med. 2005;12(5):404–9.<br />
14. Myhre D, Bajaj S, Fehr L, Kapusta M, Woodley K, Nagji A. Precepting at the time of a natural<br />
disaster. Clin Teach. 2017;14(2):104–7.<br />
15. Kumar S, Purva M, Parameswari A. Impact of repeated simulation on learning curve<br />
characteristics of residents exposed to rare life threatening situations. BMJ Simul Technol<br />
Enhanc Learn. 2019 Dec 18;bmjstel-2019-000496.<br />
16. Gaba DM. Simulation as a critical resource in the response to ebola virus disease. Simul<br />
Healthc. 2014 Dec;9(6):337–8.<br />
17. Biddell EA, Vandersall BL, Bailes SA, Estephan SA, Ferrara LA, Nagy KM, et al. Use of<br />
simulation to gauge preparedness for ebola at a free-standing children’s hospital. Simul<br />
Healthc. 2016 Apr;11(2):94–9.<br />
18. Argintaru N, Li W, Hicks C, White K, McGowan M, Gray S, et al. An active shooter in your<br />
hospital: a novel method to develop a response policy using in situ simulation and video<br />
framework analysis. Disaster Med Public Health Prep. undefined/ed;1–9.<br />
19. Speirs C, Brazil V. See one, do one, teach one: is it enough? No: TRAINEE FOCUS. Emerg Med<br />
Australas. 2018;30(1):109–10.<br />
20. Cook DA, Andersen DK, Combes JR, Feldman DL, Sachdeva AK. The value proposition of<br />
simulation-based education. Surgery. 2018;163(4):944–9.<br />
21. Kaba A, Dube M, Charania I, Donahue M. Collaborative practice in action: building<br />
interprofessional competencies through simulation based education and novel approaches to<br />
team training. Health Edu Care. 2018;3.<br />
22. Eppich W, Cheng A. Promoting excellence and reflective learning in simulation (PEARLS):<br />
development and rationale for a blended approach to health care simulation debriefing. Simul<br />
Healthc. 2015;10(2):106.<br />
23. Patterson MD, Geis GL, Falcone RA, LeMaster T, Wears RL. In situ simulation: detection of<br />
safety threats and teamwork training in a high risk emergency department. BMJ Qual Saf.<br />
2013;22(6):468–77.<br />
24. Rosen MA, Hunt EA, Pronovost PJ, Federowicz MA, Weaver SJ. In situ simulation in<br />
continuing education for the health care professions: a systematic review. J Contin Educ Heal<br />
Prof. 2012;32(4):243–54.<br />
25. Posner GD, Clark ML, Grant VJ. Simulation in the clinical setting: towards a standard lexicon.<br />
Adv Simul [Internet]. 2017 20 [cited 2018 Sep 22];2. Available from: https://www.ncbi.nlm.<br />
nih.gov/pmc/articles/PMC5806315/.<br />
26. Brazil V, Purdy EI, Bajaj K. Connecting simulation and quality improvement: how can<br />
healthcare simulation really improve patient care? BMJ Qual Saf. 2019;28(11):862–5.<br />
27. Petrosoniak A, Brydges R, Nemoy L, Campbell DM. Adapting form to function: can simulation<br />
serve our healthcare system and educational needs? Adv Simul. 2018;3(1):8.<br />
28. Minor S, Green R, Jessula S. Crash testing the dummy: a review of in situ trauma simulation at a<br />
Canadian tertiary Centre. Can J Surg. 2019;62(4):243–8.<br />
29. Brazil V. Translational simulation: not ‘where?’ But ‘why?’ A functional view of in situ<br />
simulation. Adv Simul. 2017;2(1):20.<br />
30. Ajmi SC, Advani R, Fjetland L, Kurz KD, Lindner T, Qvindesland SA, et al. Reducing doorto-needle<br />
times in stroke thrombolysis to 13 min through protocol revision and simulation<br />
training: a quality improvement project in a Norwegian stroke Centre. BMJ Qual Saf.<br />
2019;28(11):939–48.<br />
31. Paige JT, Terry Fairbanks RJ, Gaba DM. Priorities related to improving healthcare safety<br />
through simulation. Simul Healthc. 2018;13(3S):S41.<br />
32. Dubé MM, Reid J, Kaba A, Cheng A, Eppich W, Grant V, et al. PEARLS for systems integration:<br />
a modified PEARLS framework for debriefing systemsfocused simulations. Simul Healthc<br />
J Soc Simul Healthc [Internet]. 2019 May [cited 2019 Jun 22]; Available from: http://<br />
europepmc.org/abstract/med/31135684.<br />
33. Kaba A, Barnes S. Commissioning simulations to test new healthcare facilities: a proactive and<br />
innovative approach to healthcare system safety. Adv Simul. 2019;4(1):17.<br />
34. Lopreiato, JO. Healthcare simulation dictionary. Rockville, MD: Agency for Healthcare<br />
Research and Quality.; 2016. Report No.: AHRQ Publication No. 16(17)-0043.<br />
35. Holden RJ, Carayon P, Gurses AP, Hoonakker P, Hundt AS, Ozok AA, et al. SEIPS 2.0: a human<br />
factors framework for studying and improving the work of healthcare professionals and<br />
patients. Ergonomics. 2013;56(11):1669–86.<br />
36. Semple S, Cherrie JW. Covid-19: protecting worker health. Ann Work Expo Health [Internet].<br />
[cited <strong>2020</strong> Apr 28]; Available from: https://academic.oup.com/annweh/advance-article/<br />
doi/10.1093/annweh/wxaa033/5810996.<br />
37. Alexander KA, Sanderson CE, Marathe M, Lewis BL, Rivers CM, Shaman J, et al. What factors<br />
might have led to the emergence of ebola in West Africa? PLoS Negl Trop Dis [Internet]. 2015<br />
4 [cited <strong>2020</strong> Apr 28];9(6). Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/<br />
PMC4456362/.<br />
38. Lavelle M, Reedy GB, Attoe C, Simpson T, Anderson JE. Beyond the clinical team: evaluating<br />
the human factors-oriented training of non-clinical professionals working in healthcare<br />
contexts. Adv Simul. 2019;4(1):11.<br />
39. Varkey P, Reller MK, Resar RK. Basics of quality improvement in health care. Mayo Clin Proc.<br />
2007;82(6):735–9.<br />
40. Taylor MJ, McNicholas C, Nicolay C, Darzi A, Bell D, Reed JE. Systematic review of the<br />
application of the plan–do–study–act method to improve quality in healthcare. BMJ Qual Saf.<br />
2014;23(4):290–8.<br />
41. Hunt EA, Duval-Arnould JM, Nelson-McMillan KL, Bradshaw JH, Diener-West M, Perretta<br />
JS, et al. Pediatric resident resuscitation skills improve after “rapid cycle deliberate practice”<br />
training. <strong>Resus</strong>citation. 2014;85(7):945–51.<br />
42. Dube M, Fusilli T. COVID 19 simulations [Internet]. Simulation Canada; <strong>2020</strong> [cited <strong>2020</strong> Jun<br />
9]. Available from: https://www.sim-one.ca/community/news/covid-19-simulations.<br />
43. Dieckmann P, Patterson M, Lahlou S, Mesman J, Nyström P, Krage R. Variation and adaptation:<br />
learning from success in patient safety-oriented simulation training. Adv Simul. 2017;2(1):21.<br />
44. Stone KP, Huang L, Reid JR, Deutsch ES. Systems integration, human factors, and simulation.<br />
In: Comprehensive Healthcare Simulation: Pediatrics [Internet]. Springer, Cham; 2016 [cited<br />
2018 May 18]. p. 67–75. (Comprehensive Healthcare Simulation). Available from: https://link.<br />
springer.com/chapter/10.1007/978-3-319-24187-6_6.<br />
45. Geis GL, Pio B, Pendergrass TL, Moyer MR, Patterson MD. Simulation to assess the safety of<br />
new healthcare teams and new facilities. Simul Healthc. 2011;6(3):125.<br />
46. Adler MD, Mobley BL, Eppich WJ, Lappe M, Green M, Mangold K. Use of simulation to test<br />
systems and prepare staff for a new hospital transition. J Patient Saf [Internet]. 2018 26<br />
[cited 2018 May 18];Publish Ahead of Print. Available from: https://journals.lww.com/<br />
journalpatientsafety/Abstract/publishahead/Use_of_Simulation_to_Test_Systems_and_<br />
Prepare.99648.aspx.<br />
47. Ventre KM, Barry JS, Davis D, Baiamonte AA, Wentworth AC, Pietras M, et al. Using in situ<br />
simulation to evaluate operational readiness of a children’s hospital-based obstetrics unit.<br />
Simul Healthc. 2014 Apr;9(2):102.<br />
48. Auerbach M, Kessler DO, Patterson M. The use of in situ simulation to detect latent safety<br />
threats in paediatrics: a cross-sectional survey. BMJ Simul Technol Enhanc Learn. 2015 Nov<br />
3;bmjstel-2015-000037.<br />
49. Carayon P, Hundt AS, Karsh B-T, Gurses AP, Alvarado CJ, Smith M, et al. Work system design<br />
for patient safety: the SEIPS model. BMJ Qual Saf. 2006; 15(suppl 1):i50–8.<br />
50. Hamman WR, Beaudin-Seiler BM, Beaubien JM, Gullickson AM, Gross AC, Orizondo-Korotko<br />
K, et al. Using in situ simulation to identify and resolve latent environmental threats to patient<br />
safety: case study involving a labor and delivery ward. J Patient Saf. 2009;5(3):184.<br />
51. Halamek LP, Cady RAH, Sterling MR. Using briefing, simulation and debriefing to improve<br />
human and system performance. Semin Perinatol. 2019;43(8):151178.<br />
52. Taras J, Everett T. Rapid cycle deliberate practice in medical education - a systematic review.<br />
Cureus [Internet]. [cited <strong>2020</strong> 28];9(4). Available from: https://www.ncbi.nlm.nih.gov/pmc/<br />
articles/PMC5441688/.<br />
53. Dube M, Kessler D, Huang L, Petrosoniak A, Bajaj K. Considerations for psychological safety<br />
with system-focused debriefings. BMJ Simul Technol Enhanc Learn [Internet]. <strong>2020</strong>ay 1 [cited<br />
<strong>2020</strong> Apr 28];6(3). Available from: https://stel.bmj.com/content/6/3/132.<br />
Publisher’s Note<br />
Springer Nature remains neutral with regard to jurisdictional claims in<br />
published maps and institutional affiliations.<br />
RESUSCITATION TODAY - AUTUMN <strong>2020</strong><br />
15
PORTABLE MECHANICAL VENTILATION<br />
Especially designed for the Emergency Medical Services, Armed Forces and Hospitals<br />
MEDUVENT Standard<br />
MEDUMAT Standard 2<br />
• Works with or without an oxygen<br />
supply.<br />
• The innovative turbine-driven<br />
emergency ventilator maintains<br />
ventilation for approximately 8<br />
hours without requiring an external<br />
gas supply * .<br />
• Supplemental oxygen in<br />
concentrations from 21% to 100%<br />
can be delivered to the patient at<br />
any time using the universally<br />
compatible inhalation tube.<br />
• Space-saving, lightweight and simple<br />
to operate: One of the smallest<br />
turbine-driven ventilators in the<br />
world.<br />
• Immediate overview of major<br />
ventilation parameters in a large<br />
colour display and parallel<br />
presentation of up to three<br />
monitoring curves.<br />
• Differentiated ventilation modes for<br />
high-quality ventilation.<br />
• PRVC mode provides lungprotecting<br />
ventilation at trusted<br />
volume-controlled settings.<br />
• Ideal for non-invasive ventilation.<br />
• Intuitive user navigation.<br />
• Uninterrupted ventilation even<br />
while changing to a new oxygen<br />
source.<br />
* Assuming typical ventilation settings for an adult patient<br />
Available to purchase via the NHS Supply Chain Framework<br />
FAG000015628
Turbine Driven Ventilation<br />
MEDUVENT Standard<br />
Exclusively available to the UK market from the Ortus Group.<br />
Visit our website to find out more.<br />
www.theortusgroup.com<br />
E: sales@theortusgroup.com<br />
T: +44 (0)845 4594705
FEATURE<br />
PENTHROX CAN<br />
OUTPERFORM MORPHINE<br />
Unless you have had personal experience of using Penthrox this<br />
statement will come as a complete surprise. Two prospective<br />
studies, MEDITA (1) and InMEDIATE (2) , from Italy and Spain<br />
respectively and published in 2019 both reported the provision<br />
of better analgesia when Penthrox was compared with Standard<br />
Analgesic Treatment (SAT).<br />
The study reported that methoxyflurane was superior to SAT. The<br />
median time for onset of pain relief was 9 minutes in the methoxyflurane<br />
group and 15 minutes in the SAT group. Healthcare professionals in an<br />
overall assessment rated methoxyflurane good, very good or excellent in<br />
90.3% of cases compared with 64.4% in the SAT group. Methoxyflurane<br />
had no serious adverse effect on any of the patients.<br />
RESUSCITATION TODAY - AUTUMN <strong>2020</strong><br />
Penthrox is the trade name of methoxyflurane. As a handheld, selfadministered<br />
volatile inhalational analgesic it has had approximately<br />
7 million uses worldwide. Methoxyflurane was originally used as an<br />
anaesthetic agent but it was withdrawn because of reported cases<br />
of renal and liver toxicity. It was however observed that patients<br />
receiving methoxyflurane had excellent post-operative pain relief and<br />
it was therefore recognised in sub-anaesthetic dosage to have potent<br />
analgesic properties.<br />
Penthrox has a rapid onset, within 6-10 inhalations (3) and a rapid offset.<br />
Importantly, since its licensing in the UK in 2016 by the Medicines and<br />
Healthcare products Regulatory Agency (MHRA) for moderate to severe<br />
pain in adults due to trauma and related conditions, there have been<br />
no reported drug interactions and adverse events are usually mild and<br />
transient.<br />
Supplied in a 3ml vial, the device (often known as the green whistle)<br />
can be charged ready for use in under a minute and when used<br />
continuously will last 25-30 minutes. Most patients use it intermittently<br />
where it will last for approximately one hour. A second 3ml dose is<br />
permissible.<br />
Very importantly, Penthrox has minimal effect on the cardiovascular or<br />
respiratory system which makes it more suitable than opioids in certain<br />
patient groups (4) . Furthermore, it can be administered to patients with a<br />
potential pneumothorax, unlike nitrous oxide – oxygen gas. Whilst it can<br />
make some patients drowsy, they are fully rousable.<br />
The MEDITA study (Methoxyflurane versus Standard Analgesic<br />
Treatment for Acute Trauma Pain in the Emergency Setting) was a<br />
randomised, open label, active controlled multi-centre trial undertaken<br />
in Italy (1) involving 15 Emergency Medical Centres (both prehospital<br />
and ED settings). The study used a Visual Analogue Scale (VAS) to<br />
record changes in pain scores at baseline, 3, 5 and 10 minute intervals<br />
in patients receiving either methoxyflurane or Standard Analgesic<br />
Treatment (SAT). SAT was either intravenous paracetamol 1g or<br />
intravenous ketoprofen 100mg for moderate pain and morphine for<br />
severe pain.<br />
Two thirds of the patients had moderate pain where 80 patients received<br />
paracetamol and 11 received ketoprofen. Of the remaining third with<br />
severe pain 42 patients received morphine.<br />
At around the same time the InMEDIATE study (Inhaled Methoxyflurane<br />
Provides Greater Analgesia and Faster Onset of Action Versus Standard<br />
Analgesia in Patients with Trauma Pain) was taking place in Spain<br />
(2)<br />
. Once again this was a randomised controlled, open label, study<br />
comparing methoxyflurane with SAT. In this study standard analgesic<br />
treatment included intravenous, intramuscular and oral non-opioids,<br />
intravenous opioid and trans mucosal opioids. The study reported<br />
superior efficacy of methoxyflurane over SAT including better pain relief,<br />
speed of action (3.17 minutes methoxyflurane, 10 minutes SAT) and<br />
greater patient satisfaction (77% methoxyflurane, 38% SAT). In addition,<br />
patients prescribed methoxyflurane required less rescue medication<br />
(8.5% methoxyflurane, 12.1% SAT).<br />
A recent service evaluation at St Mary’s Hospital in London showed a 71<br />
minute mean reduction time is spent in the Emergency Department (ED) for<br />
patients receiving Penthrox compared to other analgesia and in particular<br />
for shoulder dislocations the mean reduction time was 183 minutes (5) .<br />
Specifically, to pre-hospital care there have been three ambulance service<br />
evaluations. When collated there were 155 patients where a significant<br />
reduction in pain scores was recorded. A more in-depth prospective study<br />
is due to report from the East Midlands Ambulance Service any time now.<br />
In relation to pre-hospital care Penthrox can provide fast, effective<br />
analgesia at the time of first patient contact avoiding the need for<br />
immediate cannulation and if necessary, it can be used as a bridging<br />
analgesia before the administration of an opioid. Its effectiveness in<br />
pre-hospital care is demonstrated in the paper by Forrest et al (6) where<br />
it has been used in a number of patients with multiple injuries.<br />
Like all drugs there are contraindications. The main ones are reduced<br />
level of consciousness, history of malignant hyperthermia and aged<br />
below 18 years (a requirement of the current product license) though<br />
it should be noted in the Republic of Ireland it is being used in the<br />
pre-hospital setting in children over the age of 5 years old. It should<br />
not be used in cases of severe cardiovascular instability, respiratory<br />
impairment, known clinically significant renal disease or liver impairment.<br />
There should be no concern about occupational exposure where a<br />
900-fold safety margin has been demonstrated (7) . Its sweet taste is<br />
detectable and Penthrox use should be discontinued prior to patient<br />
transportation by helicopter.<br />
18
FEATURE<br />
around the mouthpiece. Immediate deep inspiration could potentially<br />
initiate coughing.<br />
In summary, Penthrox may be considered a non-narcotic, easy to<br />
administer, safe and rapid acting first line alternative to currently<br />
available analgesic options for trauma related pain in both the prehospital<br />
and Emergency Department settings.<br />
References<br />
1. Mercandante S et al Adv Ther 2019 November; 36(11):3030-3046<br />
In terms of in-hospital use for fracture management it has favourable<br />
costings when combined with staffing costs for conscious sedation,<br />
intravenous anaesthesia and regional nerve blocks.<br />
Penthrox, is currently used by all hospitals and national pre-hospital<br />
services in Ireland and in the UK in 108 hospitals for ED usage with<br />
pending approval in 60 hospitals. It is used by the majority of Major<br />
Trauma Centres, approved for use in the military, used by a number of<br />
firearms units, St John Ambulance and sporting organisations including<br />
the Football Association (FA) and Rugby Football Union (RFU).<br />
Finally, under the current circumstances it is worth noting that the<br />
delivery of Penthrox is not by aerosol generation, it is a volatile liquid.<br />
Patients need coaching before its use and should be advised to initially<br />
take gentle breaths prior to breathing normally maintaining a good seal<br />
2. Borabia AM et al Ann Emerg Med<br />
https://doi.org/10.1016/j.annemergmed.2019.07.028<br />
3. Coffey F et al. Emerg Med J 2014; 31:613-618 doi: 10.1136/<br />
emermed-2013-202909.<br />
4. Oxer HF Jornal of military and veterans health 2016;24(2):14-20<br />
5. Young L et al ADV Ther.<strong>2020</strong> doi:10.1007\s1235-020-01294-1<br />
6. Forrest M et al Journal of Paramedic Practice 2019;11(2):54-60<br />
7. Frangos J et al Regul Toxicol Pharmacol.2016:80:210-25<br />
Professor Sir Keith Porter<br />
Professor of Clinical Traumatology<br />
Queen Elizabeth Hospital Birmingham<br />
OStJ, MD, MBBS, FRCS(Eng), FRCS(Ed), FIMC RCS(ED), FFSEM(Ed),<br />
FCEM, FRSA, FRCGP(Hon)<br />
<strong>Resus</strong>citation <strong>Today</strong><br />
Volume 7 No. 2<br />
<strong>Autumn</strong> <strong>2020</strong><br />
<strong>Resus</strong>citation <strong>Today</strong><br />
A Resource for all involved in the Teaching and Practice of <strong>Resus</strong>citation<br />
We trust you have enjoyed reading the<br />
latest edition of <strong>Resus</strong>citation <strong>Today</strong> and<br />
on the reverse side of this publication you<br />
will find Simulation <strong>Today</strong> which we hope<br />
will equally be of interest.<br />
When responding to advertisers please<br />
mention both publications.<br />
Should you wish to read previous issues<br />
online please visit:<br />
www.resustoday.com<br />
RESUSCITATION TODAY - AUTUMN <strong>2020</strong><br />
See reverse for Simulation <strong>Today</strong><br />
19