RN Idaho - May 2021
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
<strong>May</strong>, June, July <strong>2021</strong> <strong>RN</strong> <strong>Idaho</strong> • Page 5<br />
FEATURE<br />
Nursing Informatics: Use of the Mapping Medicare<br />
Disparities (MMD) Tool – A Starting Point for Examining<br />
Health Disparity Data in the United States<br />
Barbara McNeil PhD, <strong>RN</strong>-BC<br />
Adjunct graduate faculty, Gonzaga University<br />
mcneilb@gonzaga.edu<br />
The author has disclosed no potential conflicts of<br />
interest.<br />
As never before and during this pandemic, citizens and<br />
healthcare professionals have seen healthcare data upclose<br />
and embraced and valued it. Through daily analysis<br />
and visual representation of data and trends, the U.S.<br />
media and scientists have increased our understanding<br />
of the spread of COVID-19 across the globe. We are<br />
seeing how certain populations are more affected by<br />
COVID-19 and are developing an understanding of how<br />
social determinants of health influence health outcomes.<br />
The purpose of this paper is to examine the Centers<br />
for Medicare and Medicaid Services Office of Minority<br />
Health’s (CMS OMH) Mapping Medicare Disparities (MMD)<br />
tool (CMS OMH, 2020) and its usefulness for identifying<br />
health disparities across populations, informing the need<br />
for quality of care improvement.<br />
Health Disparities<br />
The term “health disparities” is commonly referred<br />
to as “ differences in health status or health outcomes,<br />
which may be difficult to attribute to individual<br />
providers” (Weissman, et al. 2012, p. 5). Examples of<br />
health disparities include gender, race/ethnicity, income,<br />
education level, sexual orientation, age, and geography.<br />
The concept of “health disparities” differs from<br />
“healthcare disparities” or “health utilization disparities.”<br />
Weissman et al. (2012, p. 5) utilized a National Institute<br />
of Health definition to clarify health disparities as “racial<br />
and ethnic differences in the quality of healthcare that<br />
are not due to access related factors or clinical needs,<br />
preferences, and appropriateness of intervention.” A<br />
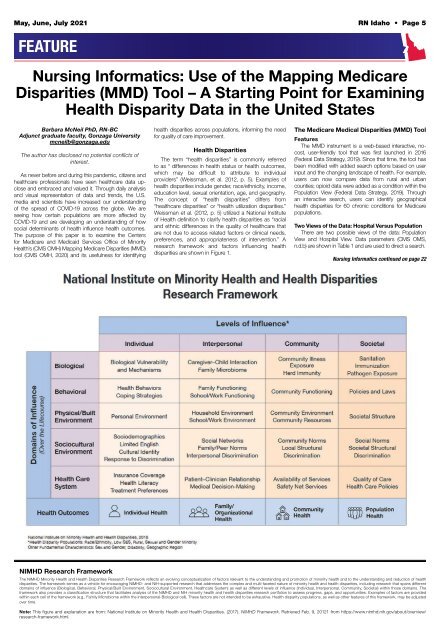
research framework and factors influencing health<br />
disparities are shown in Figure 1.<br />
The Medicare Medical Disparities (MMD) Tool<br />
Features<br />
The MMD instrument is a web-based interactive, nocost,<br />
user-friendly tool that was first launched in 2016<br />
(Federal Data Strategy, 2019). Since that time, the tool has<br />
been modified with added search options based on user<br />
input and the changing landscape of health. For example,<br />
users can now compare data from rural and urban<br />
counties; opioid data were added as a condition within the<br />
Population View (Federal Data Strategy, 2019). Through<br />
an interactive search, users can identify geographical<br />
health disparities for 60 chronic conditions for Medicare<br />
populations.<br />
Two Views of the Data: Hospital Versus Population<br />
There are two possible views of the data: Population<br />
View and Hospital View. Data parameters (CMS OMS,<br />
n.d.b) are shown in Table 1 and are used to direct a search.<br />
Nursing Informatics continued on page 22<br />
NIMHD Research Framework<br />
The NIMHD Minority Health and Health Disparities Research Framework reflects an evolving conceptualization of factors relevant to the understanding and promotion of minority health and to the understanding and reduction of health<br />
disparities. The framework serves as a vehicle for encouraging NIMHD- and NIH-supported research that addresses the complex and multi-faceted nature of minority health and health disparities, including research that spans different<br />
domains of influence (Biological, Behavioral, Physical/Built Environment, Sociocultural Environment, Healthcare System) as well as different levels of influence (Individual, Interpersonal, Community, Societal) within those domains. The<br />
framework also provides a classification structure that facilitates analysis of the NIMHD and NIH minority health and health disparities research portfolios to assess progress, gaps, and opportunities. Examples of factors are provided<br />
within each cell of the framework (e.g., Family Microbiome within the Interpersonal-Biological cell). These factors are not intended to be exhaustive. Health disparity populations, as well as other features of this framework, may be adjusted<br />
over time.<br />
Note: This figure and explanation are from: National Institute on Minority Health and Health Disparities. (2017). NIMHD Framework. Retrieved Feb. 9, 20121 from https://www.nimhd.nih.gov/about/overview/<br />
research-framework.html.