Gastroenterology Today Summer 2021
Gastroenterology Today Summer 2021
Gastroenterology Today Summer 2021
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
CASE REPORT<br />
of toxicity. Clinical manifestations of lead toxicity are varied and can<br />
be non-specific. Acute toxicity often manifests as abdominal pain,<br />
constipation, body pains, decreased libido, headaches, memory<br />
problems and irritability. Chronic exposure can produce anaemia,<br />
reduced neuro-cognitive function, nephropathy, tremor, hearing loss<br />
and hypertension 2 .<br />
In the paediatric population lead toxicity risks significant and<br />
irreversible neurodevelopmental damage and should be investigated<br />
in any child presenting with an unexplained alteration in mental<br />
state and behavioral changes in the presence of risk factors for lead<br />
exposure 3 .<br />
An elevated blood lead level reflects recent exogenous exposure as<br />
well as release of endogenous lead from bone and soft tissue stores.<br />
Toxicity is thought to develop due to lead competing with calcium in<br />
several biological processes, inhibiting enzymes, and altering the<br />
permeability of the blood brain barrier.<br />
The mainstay of management is the separation of the patient from<br />
the source of the lead exposure. In patient with very elevated lead<br />
levels (>50 mcg/dL) or symptoms of acute toxicity chelation therapy<br />
can be considered under specialist guidance 4,5 . The two most<br />
commonly used chelating agents are DMSA (2,3-dimercaptosuccinic<br />
acid) or EDTA (calcium disodium ethylenediaminetetraacetic acid).<br />
Chelation should not be undertaken unless exposure to lead has<br />
been curtailed, as in the presence of ongoing lead exposure,<br />
chelation may lead to enhanced absorption of lead and therefore<br />
worsening toxicity.<br />
Regular and long-term monitoring of lead levels is required until<br />
normal levels are achieved, as lead can be stored in bone for several<br />
decades. Patients with established sequelae of lead toxicity such as<br />
cardiovascular disease, cognitive dysfunction and renal failure are<br />
unlikely to see reversibility of their symptoms over time even with<br />
chelation therapy.<br />
Conclusion<br />
Lead toxicity is an uncommon yet important differential in patients<br />
presenting with persistent abdominal pain. Prompt diagnosis and<br />
subsequent treatment is imperative in negating the potentially long-term<br />
damaging effects of lead on multiple organ systems. In these patients,<br />
a through social history is the most crucial, but often overlooked, step in<br />
reaching the diagnosis.<br />
References<br />
1. J. Route Reigart, British Medical Journal Best Practice<br />
Guidelines; Approach to Lead Toxicity. Updated 17th April <strong>2021</strong>.<br />
https://bestpractice.bmj.com/topics/en-gb/755/diagnosisapproach#referencePop27<br />
2. National Toxicology Program. Health effects of low-level lead<br />
evaluation. Research Triangle Park, NC: US Department of Health<br />
and Human Services; 2012. http://ntp.niehs.nih.gov/pubhealth/hat/<br />
noms/lead/index.html<br />
3. D. A. Gildow, Lead Toxicity, Occupational Medicine 2004;54:76–81<br />
DOI: 10.1093/occmed/kqh019<br />
4. Lin JL, Ho HH, Yu CC. Chelation therapy for patients with<br />
elevated body lead burden and progressive renal insufficiency. A<br />
randomized, controlled trial. Ann Intern Med 1999; 130:7.<br />
5. Association of Occupational and Environmental Clinics. Medical<br />
management guidelines for lead-exposed adults. April 2007. http://<br />
www.aoec.org<br />
6. Centres for Disease Control (CDC) and Prevention. Adult blood lead<br />
epidemiology and surveillance (ABLES). http://www.cdc.gov/niosh/<br />
topics/ables/description.html<br />
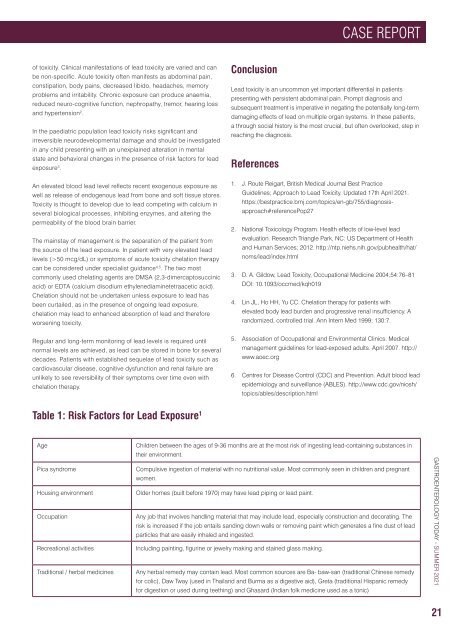
Table 1: Risk Factors for Lead Exposure 1<br />
Age<br />
Pica syndrome<br />
Housing environment<br />
Occupation<br />
Recreational activities<br />
Traditional / herbal medicines<br />
Children between the ages of 9-36 months are at the most risk of ingesting lead-containing substances in<br />
their environment.<br />
Compulsive ingestion of material with no nutritional value. Most commonly seen in children and pregnant<br />
women.<br />
Older homes (built before 1970) may have lead piping or lead paint.<br />
Any job that involves handling material that may include lead, especially construction and decorating. The<br />
risk is increased if the job entails sanding down walls or removing paint which generates a fine dust of lead<br />
particles that are easily inhaled and ingested.<br />
Including painting, figurine or jewelry making and stained glass making.<br />
Any herbal remedy may contain lead. Most common sources are Ba- baw-san (traditional Chinese remedy<br />
for colic), Daw Tway (used in Thailand and Burma as a digestive aid), Greta (traditional Hispanic remedy<br />
for digestion or used during teething) and Ghasard (Indian folk medicine used as a tonic)<br />
GASTROENTEROLOGY TODAY - SUMMER <strong>2021</strong><br />
21