Gastroenterology Today Summer 2021
Gastroenterology Today Summer 2021
Gastroenterology Today Summer 2021
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
FEATURE<br />
simple, easy to use, hygienic FIT sample collection devices. However,<br />
bespoke instruction for use (IFU) leaflets have been hugely influential in<br />
increasing uptake and improving sample quality. Such IFU are based<br />
around core sampling requirements but adapted to suit the specific<br />
clinical pathway adopted by Trusts and Health Boards. With local<br />
contact numbers, bar-codes, and detailed pathway information, patients<br />
are made to feel included in the diagnostic process and are provided<br />
with the tools to complete the sample collection successfully or talk to a<br />
knowledgeable professional should they have any questions. IFU have<br />
evolved over time, after initially being used in primary care, FIT is now<br />
being used in a more diverse range of patients, 11 so the detail must be<br />
regularly reviewed to ensure suitability. Usability studies, consultation<br />
events, focus groups and feedback from cancer charities all could<br />
contribute to the design and production of these IFU to maximise the<br />
inclusivity of the process.<br />
The design and application of sample collection devices are suited<br />
to patient-based sampling and, although the attributes will not be<br />
discussed in detail here, research has been conducted on the efficacy<br />
of FIT in the hands of patients, 12,13 , proving them suitable for this<br />
application. Additionally, the IFU provide supporting information such<br />
as tips for collecting the faeces prior to using the device, which helps<br />
familiarise using faeces as a sample and helps break some of the<br />
barriers to the sampling process. It also helps reduce contamination risk<br />
in terms of the faecal sample, and the sample collection device.<br />
FIT for All<br />
The last, and possibly most critical, barrier to uptake, is ensuring the IFU<br />
are suitable for a range of patient groups. With FIT now being used in a<br />
diverse range of patients, the bespoke literature must be as inclusive as<br />
possible, ensuring patients can understand and follow the instructions.<br />
As discussed above, the use of simple colourful pictures or diagrams<br />
and text help those with visual impairments, or those for whom English<br />
is not a primary language, and the additional information provided, such<br />
as phone numbers, links to videos and websites, provide more routes<br />
for patients to access help should this be required. It is important to<br />
consider that a FIT device should not be simply handed to a patient with<br />
no advice: as part of the safety-netting process, FIT should be provided<br />
following a discussion with the patient.<br />
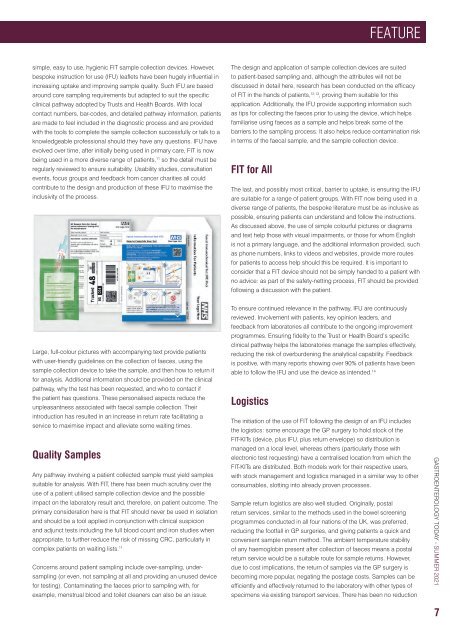
Large, full-colour pictures with accompanying text provide patients<br />
with user-friendly guidelines on the collection of faeces, using the<br />
sample collection device to take the sample, and then how to return it<br />
for analysis. Additional information should be provided on the clinical<br />
pathway, why the test has been requested, and who to contact if<br />
the patient has questions. These personalised aspects reduce the<br />
unpleasantness associated with faecal sample collection. Their<br />
introduction has resulted in an increase in return rate facilitating a<br />
service to maximise impact and alleviate some waiting times.<br />
Quality Samples<br />
Any pathway involving a patient collected sample must yield samples<br />
suitable for analysis. With FIT, there has been much scrutiny over the<br />
use of a patient utilised sample collection device and the possible<br />
impact on the laboratory result and, therefore, on patient outcome. The<br />
primary consideration here is that FIT should never be used in isolation<br />
and should be a tool applied in conjunction with clinical suspicion<br />
and adjunct tests including the full blood count and iron studies when<br />
appropriate, to further reduce the risk of missing CRC, particularly in<br />
complex patients on waiting lists. 11<br />
Concerns around patient sampling include over-sampling, undersampling<br />
(or even, not sampling at all and providing an unused device<br />
for testing). Contaminating the faeces prior to sampling with, for<br />
example, menstrual blood and toilet cleaners can also be an issue.<br />
To ensure continued relevance in the pathway, IFU are continuously<br />
reviewed. Involvement with patients, key opinion leaders, and<br />
feedback from laboratories all contribute to the ongoing improvement<br />
programmes. Ensuring fidelity to the Trust or Health Board’s specific<br />
clinical pathway helps the laboratories manage the samples effectively,<br />
reducing the risk of overburdening the analytical capability. Feedback<br />
is positive, with many reports showing over 90% of patients have been<br />
able to follow the IFU and use the device as intended. 14<br />
Logistics<br />
The initiation of the use of FIT following the design of an IFU includes<br />
the logistics: some encourage the GP surgery to hold stock of the<br />
FIT-KITs (device, plus IFU, plus return envelope) so distribution is<br />
managed on a local level, whereas others (particularly those with<br />
electronic test requesting) have a centralised location from which the<br />
FIT-KITs are distributed. Both models work for their respective users,<br />
with stock management and logistics managed in a similar way to other<br />
consumables, slotting into already proven processes.<br />
Sample return logistics are also well studied. Originally, postal<br />
return services, similar to the methods used in the bowel screening<br />
programmes conducted in all four nations of the UK, was preferred,<br />
reducing the footfall in GP surgeries, and giving patients a quick and<br />
convenient sample return method. The ambient temperature stability<br />
of any haemoglobin present after collection of faeces means a postal<br />
return service would be a suitable route for sample returns. However,<br />
due to cost implications, the return of samples via the GP surgery is<br />
becoming more popular, negating the postage costs. Samples can be<br />
efficiently and effectively returned to the laboratory with other types of<br />
specimens via existing transport services. There has been no reduction<br />
GASTROENTEROLOGY TODAY - SUMMER <strong>2021</strong><br />
7