Resus Today Summer 2021
Resus Today Summer 2021
Resus Today Summer 2021
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
Volume 8 No. 2<br />
<strong>Summer</strong> <strong>2021</strong><br />
<strong>Resus</strong>citation <strong>Today</strong><br />
A Resource for all involved in the Teaching and Practice of <strong>Resus</strong>citation<br />
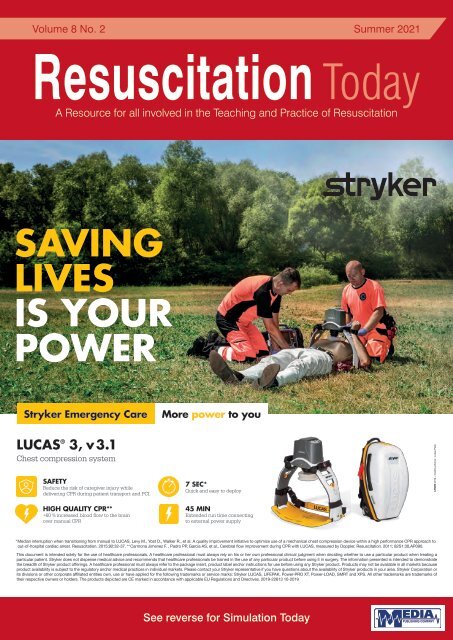
SAVING<br />
LIVES<br />
IS YOUR<br />
POWER<br />
Stryker Emergency Care<br />
More power to you<br />
LUCAS ® 3, v 3.1<br />
Chest compression system<br />
SAFETY<br />
Reduce the risk of caregiver injury while<br />
delivering CPR during patient transport and PCI.<br />
HIGH QUALITY CPR**<br />
+60 % increased blood flow to the brain<br />
over manual CPR<br />
7 SEC*<br />
Quick and easy to deploy<br />
45 MIN<br />
Extended run time connecting<br />
to external power supply<br />
2019 – Crédits photos : Lukas Palik<br />
* Median interruption when transitioning from manual to LUCAS, Levy M., Yost D., Walker R., et al. A quality improvement initiative to optimize use of a mechanical chest compression device within a high performance CPR approach to<br />
out-of-hospital cardiac arrest. <strong>Resus</strong>citation. 2015;92:32-37. ** Carmona Jimenez F. , Padro PP, Garcia AS, et al., Cerebral flow improvement during CPR with LUCAS, measured by Doppler. <strong>Resus</strong>citation. 2011; 82S1:30,AP090.<br />
This document is intended solely for the use of healthcare professionals. A healthcare professional must always rely on his or her own professional clinical judgment when deciding whether to use a particular product when treating a<br />
particular patient. Stryker does not dispense medical advice and recommends that healthcare professionals be trained in the use of any particular product before using it in surgery. The information presented is intended to demonstrate<br />
the breadth of Stryker product offerings. A healthcare professional must always refer to the package insert, product label and/or instructions for use before using any Stryker product. Products may not be available in all markets because<br />
product availability is subject to the regulatory and/or medical practices in individual markets. Please contact your Stryker representative if you have questions about the availability of Stryker products in your area. Stryker Corporation or<br />
its divisions or other corporate affiliated entities own, use or have applied for the following trademarks or service marks: Stryker LUCAS, LIFEPAK, Power-PRO XT, Power-LOAD, SMRT and XPS. All other trademarks are trademarks of<br />
their respective owners or holders. The products depicted are CE marked in accordance with applicable EU Regulations and Directives. 2019-22613 10-2019<br />
See reverse for Simulation <strong>Today</strong>
THE RIGHT ARM<br />
IN THE CATH LAB<br />
MECHANICAL CPR<br />
The unique single arm design enables unrivalled access to the thorax with<br />
no restrictions regarding the patient’s weight and breadth of thorax.<br />
Made from radiolucent<br />
materials; the corpuls cpr<br />
provides exceptional<br />
visibility under X–ray.<br />
The intuitive user-friendly<br />
design allows a single<br />
person to set up and<br />
operate in matter of<br />
seconds.<br />
Want to learn more?<br />
Watch this video:<br />
Scan the QR code with your<br />
phone camera and click the link.<br />
Or visit: uqr.to/cpr-arm<br />
www.theortusgroup.com<br />
knowledge.theortusgroup.com<br />
E: hello@theortusgroup.com<br />
T: +44 (0)845 4594705
CONTENTS<br />
CONTENTS<br />
<strong>Resus</strong>citation <strong>Today</strong><br />
4 EDITORS COMMENT<br />
6 FEATURE Drowning<br />
10 FEATURE The Future of Point of Care Ultrasound (POCUS)<br />
Training<br />
13 FEATURE New technologies and Artificial Intelligence in<br />
Emergency Medicine: tools to improve Cardio-<br />
Pulmonary <strong>Resus</strong>citation (CPR)<br />
This issue edited by:<br />
David Halliwell<br />
MSc Paramedic<br />
c/o Media Publishing Company<br />
Greenoaks<br />
Lockhill<br />
Upper Sapey, Worcester, WR6 6XR<br />
ADVERTISING & CIRCULATION:<br />
Media Publishing Company<br />
Greenoaks, Lockhill<br />
Upper Sapey, Worcester, WR6 6XR<br />
Tel: 01886 853715<br />
E: info@mediapublishingcompany.com<br />
www.MediaPublishingCompany.com<br />
PUBLISHED:<br />
Spring, <strong>Summer</strong> and Autumn<br />
WHY NOT WRITE FOR US?<br />
<strong>Resus</strong>citation <strong>Today</strong> welcomes<br />
the submission of clinical papers,<br />
case reports and articles that you<br />
feel will be of interest to your<br />
colleagues.<br />
The publication is mailed to all resuscitation,<br />
A&E and anaesthetic departments plus all<br />
intensive care, critical care, coronary care and<br />
cardiology units.<br />
All submissions should be forwarded to<br />
info@mediapublishingcompany.com<br />
If you have any queries please contact the<br />
publisher Terry Gardner via:<br />
info@mediapublishingcompany.com<br />
COPYRIGHT:<br />
Media Publishing Company<br />
Greenoaks<br />
Lockhill<br />
Upper Sapey, Worcester, WR6 6XR<br />
PUBLISHERS STATEMENT:<br />
The views and opinions expressed in<br />
this issue are not necessarily those of<br />
the Publisher, the Editors or Media<br />
Publishing Company.<br />
Next Issue Autumn <strong>2021</strong><br />
Subscription Information – <strong>Summer</strong> <strong>2021</strong><br />
<strong>Resus</strong>citation <strong>Today</strong> is a tri-annual publication<br />
published in the months of March, June and<br />
September. The subscription rates are as<br />
follows:-<br />
UK:<br />
Individuals - £12.00 inc. postage<br />
Commercial Organisations - £30.00 inc. postage<br />
Rest of the World:<br />
Individuals - £60.00 inc. postage<br />
Commercial Organisations - £72.00 inc. postage<br />
We are also able to process your<br />
subscriptions via most major credit<br />
cards. Please ask for details.<br />
Cheques should be made<br />
payable to MEDIA PUBLISHING.<br />
Designed in the UK by me&you creative<br />
RESUSCITATION TODAY - SUMMER <strong>2021</strong><br />
3
EDITORS COMMENT<br />
EDITORS COMMENT<br />
The latest <strong>Resus</strong>citation guidelines have been released, new slide sets for<br />
courses, new books / manuals and an ever growing evidence base. This has<br />
been welcomed by the <strong>Resus</strong> community and we will plan to review the teaching<br />
materials in the next edition of this journal.<br />
As a community we are seeing a shift towards “high quality“ resuscitation, through the use of CPR<br />
feedback devices, controlling rate and depth of human (manual) CPR.<br />
RESUSCITATION TODAY - SUMMER <strong>2021</strong><br />
“As a<br />
community we<br />
are seeing a<br />
shift towards<br />
“high quality“<br />
resuscitation,<br />
through the<br />
use of CPR<br />
feedback<br />
devices,<br />
controlling<br />
rate and depth<br />
of human<br />
(manual)<br />
CPR.”<br />
We are seeing a continued growth of mechanical CPR - especially since covid19 - and now we<br />
are seeing an increased interest in Ventilation Monitoring - controlling Volume and Rate of CPR to<br />
reduce Hyperventilation.<br />
In this edition of the journal Dr Abdo Koury shares his insight into the EOlife device and its<br />
use of Artificial Intelligence to support Improved Ventilation and reduce death by “Rescuer<br />
Hyperventilation” - ventilation monitoring appears to be a huge area for us to consider in <strong>2021</strong>.<br />
Adam Gent has provided this journal with a review of the science of drowning for this journal - at<br />
the time of writing there have been 14 deaths by drowning in the past week in the U.K. and we are<br />
grateful to Adam for this opportunity to review our drowning science knowledge.<br />
David Halliwell<br />
MSc Paramedic<br />
4
<strong>Resus</strong>citation<br />
and Emergency<br />
Care<br />
A full range of products for<br />
use in an emergency and<br />
resuscitation situation<br />
• Bag-Valve-Mask (BVM)<br />
resuscitators<br />
• Pocket resuscitation masks<br />
• Supraglottic airways<br />
• Video laryngoscope<br />
• Oxygen therapy masks<br />
The complete solution from<br />
the respiratory care specialists<br />
To view the full range visit<br />
www.intersurgical.co.uk/info/emergency<br />
lnteract with us<br />
Quality, innovation and choice<br />
www.intersurgical.co.uk
FEATURE<br />
DROWNING<br />
Adam Gent<br />
20th January <strong>2021</strong><br />
To begin with, lets just forget “near-drowning”, “dry drowning”, “wet<br />
drowning”, “freshwater drowning”, “saltwater drowning” and “secondary<br />
drowning”. (1)<br />
These terms are outdated and no longer accepted by The World<br />
Health Organization (2), the United Kingdom <strong>Resus</strong>citation Council (3),<br />
International Liaison Committee on <strong>Resus</strong>citation (4) , the Wilderness<br />
Medical Society (5) , the International Lifesaving Federation (6), the<br />
American Heart Association (7) who all discourage the use of these<br />
terms.<br />
Unfortunately, these terms still slip past the editors of major medical<br />
journals, allowing their use to be perpetuated. These terms are most<br />
pervasive in the nonmedical press and social media to add an illusion of<br />
gravitas, where the term drowning seems to be synonymous with death.<br />
The currently accepted definition of drowning from the World Congress<br />
on Drowning (8) is:<br />
“Drowning is the process of experiencing respiratory impairment from<br />
submersion or immersion in a liquid.”<br />
Key to this are:<br />
Sudden immersion in cold water causes an immediate fall in skin<br />
temperature which triggers several body reflexes (9) collectively (and<br />
annoyingly) known as the “cold-shock” response, and they last for<br />
just the first few minutes after falling in.<br />
The “cold-shock” responses include:<br />
1) instantaneous gasping for air<br />
2) sudden increase in breathing rate<br />
3) sudden increase in heart rate<br />
4) sudden increase in blood pressure<br />
5) dramatic decrease in breath-holding time (from around 60<br />
seconds to just 20-25 seconds (10).<br />
A combination of gasping and a decreased ability to hold ones<br />
breath causes the casualty to inhale water. And this is the<br />
fundamental cause of drowning – respiratory distress.<br />
Inhaling water appears to cause laryngospasm in the first instance<br />
(although this is debated) but real problem occur when water enters<br />
the lower airway, in particular the alveoli; only a small amount of<br />
water is required to cause significant problems – less than 4ml/kg<br />
(11, 12).<br />
RESUSCITATION TODAY - SUMMER <strong>2021</strong><br />
• Drowning is a process, not the end result. The definition of drowning<br />
does not include death.<br />
• There must be respiratory impairment. If a casualty is rescued from<br />
the water with no respiratory distress, they did not drown or ‘near<br />
drowned’, they were simply rescued.<br />
• Submersion occurs where the whole body is submersed, including<br />
the airway. Immersion is where the body is within a liquid but not<br />
covering the airway.<br />
• Drowning is limited to liquids. Casualties submersed in powders<br />
(which behave as free flowing fluids) are asphyxiated.<br />
Once it is determined a drowning incident has occurred, there are 3<br />
possible outcomes:<br />
• Mortality (death)<br />
• Morbity (illness or injury)<br />
• No morbidity<br />
Drowned casualties either die as a result of respiratory impairment, are<br />
rescued with consequential illness or injury following their respiratory<br />
impairment or have no lasting illness or injury.<br />
The Process of drowning<br />
Stage 1: Cold water Immersion Response (0-2 minutes):<br />
• Regardless of the salinity of the water, the inflammatory response<br />
leads to increased permeability of alveoli capillary membrane and<br />
exacerbates fluid, plasma and electrolyte shifts into the alveoli<br />
resulting in pulmonary oedema leading to decreased oxygen and<br />
carbon dioxide exchange and some bronchospasm.<br />
• Water in the alveoli also causes surfactant washout and<br />
dysfunction and leading to reduced lung compliance and alveoli<br />
collapse.<br />
The fundamental cause of death from drowning is hypoxia, leading to<br />
arrhythmias and cardiac arrest.<br />
It is or this very simple reason that lifejackets and PFD save lives by<br />
keeping the airway above the water during the first few minutes of<br />
uncontrolled breathing.<br />
Shallow Water Blackout<br />
A combination of inhaled water and hyperventilation might, at this<br />
stage cause shallow water blackout:<br />
Ordinarily as we hold our breath our oxygen levels are decreasing<br />
whilst our carbon dioxide levels are increasing. The desire to<br />
breathe is triggered by elevated CO2 levels which usually occurs<br />
before our O2 levels drop below a particular threshold at which point<br />
we go unconscious or ‘blackout’.<br />
6
FEATURE<br />
very cold water this can take over an hour to achieve. If the<br />
casualty was not wearing a life jacket of PFD, it is likely they died<br />
of drowning rather than hypothermia. If the casualty’s airway is<br />
protected by a life-jacket and they are breathing normally, they<br />
are not a Drowned casualty, they are a hypothermic casualty and<br />
should be treated as such.<br />
To rescue or not?<br />
National Operation Guidance decision tool (14) based on the work<br />
of Dr Mike Tipton (15) is a model is designed to give casualties<br />
every reasonable chance of rescue and resuscitation and is<br />
balanced against the risk of harm to responders when carrying out<br />
rescues.<br />
Image source: Wikipedia. CC BY-SA 4.0, File:Shallow water blackout<br />
diagram 1 revised.svg<br />
If the casualty has been hyperventilating, they have a normal amount<br />
of oxygen in their blood stream but vastly reduced CO2 levels. As<br />
they attempt to hold their breathe, they reach the low 02 threshold<br />
of blackout before their raising C02 levels have triggered a desire to<br />
breath.<br />
The length of time submerged and the temperature of the water are<br />
the two main factors determining survivability; generally, the longer<br />
a casualty is submerged and the warmer the water, the lower the<br />
chances of survival. Other factors affecting survivability include the<br />
age and/or size of the casualty, as smaller and/or younger people<br />
can survive longer than larger people or adults.<br />
1. Start The Clock<br />
The main factors are the length of time the casualty has been<br />
submerged and the water temperature. It is not possible to know<br />
for certain when a casualty became submerged, so the clock<br />
should start when the first attendance arrives on scene. It should<br />
not be assumed that the person has been submerged for longer<br />
than this.<br />
2. Risk Assess<br />
A risk assessment should balance the likelihood of casualty<br />
survival and the likelihood and severity of harm to rescuers.<br />
The decision will consider whether an immediate rescue can be<br />
started or if one should await specialist resources.<br />
Image source: Wikipedia. CC BY-SA 4.0 File:Shallow water blackout<br />
diagram 2 revised.svg<br />
3. At 30 minutes<br />
further Risk Assessment should be considered given the reduced<br />
likelihood of survival against the danger to rescuers which may<br />
be increased (darkness, cold, exposure, fatigue, changing tides<br />
or river levels).<br />
Stage 2: Functional Disability (2-30 minutes)<br />
If the casualty has survived the ‘cold-shock’, rapid cooling of the<br />
muscles reduces contractility preventing normal muscle movement;<br />
the casualty may be unable to swim or may have lost manual dexterity<br />
preventing them from grasping rescue lines or ordinarily climbing out.<br />
It is this loss of muscle control which is why drowning may not appear<br />
ass drowning:<br />
1. Except in rare circumstances, drowning people are physiologically<br />
unable to call out for help due to uncontrolled breathing.<br />
2. A drowning casualty may not wave for help, favouring suing their<br />
arms to keep their airway above the water.<br />
Stage 3: Hypothermia (> 30 minutes).<br />
After prolonged exposure, the casualty will become hypothermic.<br />
Unconsciousness can be expected around 30-32oc but even in<br />
If the water is ‘icy-cold’ (below 7oc) the casualty should be<br />
considered survivable, although the likelihood of survival reduces<br />
as time passes. If not, the operation should move to recovery of<br />
the body, if safe.<br />
4. At 60 minutes<br />
If rescue operations have continued at 60 minutes a further<br />
assessment should be made. If the water is ‘icy-cold’ and<br />
the casualty is known to be young and/or small they should<br />
be considered survivable, although again their chances are<br />
further reducing as time passes. The risk assessment should be<br />
revisited to decide if rescue should continue or if the incident<br />
should switch to body recovery.<br />
5. At 90 minutes<br />
After 90 the decision should be taken to switch to body recovery<br />
because the circumstances are regarded as no longer survivable.<br />
RESUSCITATION TODAY - SUMMER <strong>2021</strong><br />
7
FEATURE<br />
RESUSCITATION TODAY - SUMMER <strong>2021</strong><br />
Image source: National operational Guidance: Water Rescue and Flooding”. National Central Programme Office.<br />
https://www.ukfrs.com/pdf/print/node%3A20802 Accessed on 9th January <strong>2021</strong><br />
8
FEATURE<br />
Rescue<br />
• Avoid entry into the water whenever possible. If entry into the water is<br />
essential, use a buoyant rescue aid or flotation device.<br />
• Remove the victim from the water and start resuscitation as quickly<br />
and safely as possible.<br />
• Cervical spine injury is uncommon in drowning victims (approximately<br />
0.5%). Spinal immobilisation is difficult in the water and delays<br />
removal from the water and adequate resuscitation of the victim.<br />
• Consider cervical spine immobilisation if there is a history of diving,<br />
water slide use, signs of severe injury, or signs of alcohol intoxication.<br />
• Despite potential spinal injury, if the victim is pulseless and apnoeic<br />
remove them from the water as quickly as possible (even if a back<br />
support device is not available) whilst attempting to limit neck flexion<br />
and extension.<br />
• Try to remove the victim from the water in a horizontal position to<br />
minimise the risks of post-immersion hypotension and cardiovascular<br />
collapse.<br />
Ventilation (3)<br />
• Prompt initiation of rescue breathing or positive pressure ventilation<br />
increases survival. If possible supplement ventilation with oxygen.<br />
• Give five initial ventilations as soon as possible.<br />
• Rescue breathing can be initiated whilst the victim is still in shallow<br />
water provided the safety of the rescuer is not compromised.<br />
• If the victim is in deep water, open their airway and if there is no<br />
spontaneous breathing start in-water rescue breathing if trained to do so.<br />
• In-water resuscitation is possible, but should ideally be performed<br />
with the support of a buoyant rescue aid.<br />
• If normal breathing does not start spontaneously, and the victim is <<br />
5 min from land, continue rescue breaths while towing. If more than<br />
an estimated 5 min from land, give rescue breaths over 1 min, then<br />
bring the victim to land as quickly as possible without further attempts<br />
at ventilation.<br />
Regurgitation (3)<br />
• Expect the casualty to vomit.<br />
• If regurgitation occurs, turn the victim’s mouth to the side and remove<br />
the regurgitated material<br />
• There is no need to clear the airway of aspirated water as this is<br />
absorbed rapidly into the central circulation.<br />
• Do not use abdominal thrusts or tip the victim head down to remove<br />
water from the lungs or stomach.<br />
Chest compressions (3)<br />
• As soon as the victim is removed from the water, check for breathing.<br />
If the victim is not breathing (or is making agonal gasps), start chest<br />
compressions immediately.<br />
• Continue CPR in a ratio of 30 compressions to 2 ventilations.<br />
• Most drowning victims will have sustained cardiac arrest secondary to<br />
hypoxia. In these patients, compression-only CPR is likely to be less<br />
effective and standard CPR should be used.<br />
Post Rescue Care<br />
After Drop<br />
A phenomena known as “After Drop” can occur as a result of aggressive<br />
rewarming; peripheral vasodilation can lead to a redistribution of blood<br />
and a drop in core temperature. This can occur during treatment or<br />
even after recovery. This can be prevented by moderated warming<br />
techniques; If the casualty has vital signs, is insulated and immobile,<br />
there is no rush to actively warm them.<br />
Curcum Rescue Collapse<br />
Particularly evident in immersion hypothermia casualties, ‘Curcum<br />
Rescue Collapse’ has been attributed to the aggressive repositioning<br />
of the casualty from a floating horizontal position to vertical as they<br />
were winched out of the sea using a hoist. Standing up quickly can<br />
cause orthostatic hypotension; a drop in blood pressure as the vascular<br />
system cannot constrict fast enough in the lower limbs and abdomen<br />
to squeeze oxygenated blood up to the brain; this is noticeable by the<br />
‘head rush’ or feeling of light-headedness as the brain is momentarily<br />
deprived of oxygen.<br />
Combined with the immediate loss of hydrostatic pressure which was<br />
being exerted on the body whilst the casualty was immersed, this<br />
drop in blood pressure can reduce cerebral perfusion to the point of<br />
unconsciousness and cardiac perfusion to the point of cardiac arrest.<br />
Both immersion and severely hypothermic casualties are now rescued<br />
horizontally and as such, should remain in this position until rescue.<br />
References<br />
1. Hawkings JC, Sempsrott J and Schmidt A (2016) “Drowning in a Sea of<br />
Misinformation: Dry Drowning and Secondary Drowning” Emergency medicine<br />
News. https://journals.lww.com/em-news/blog/BreakingNews/pages/post.<br />
aspx?PostID=377 Accessed 19th January <strong>2021</strong><br />
2. https://www.who.int/en/news-room/fact-sheets/detail/drowning<br />
3. UK <strong>Resus</strong>citation Council (2019) “Cardiac Arrest in Special Circumstances” in<br />
Advanced Life Support Guidelines. Ch 12. 113:142<br />
4. Idris AH, Berg RA, Bierens J, Bossaert L, Branche CM et al (2003)<br />
“Recommended Guidelines for Uniform Reporting of Data From Drowning”.<br />
Circulation. 108[20]:2565<br />
5. Schmidt AC, Sempsrott JR, Hawkins SC, Arastu AS, Cushing TA, Auerbach PS. (2016)<br />
“Wilderness Medical Society Practice Guidelines for the Prevention and Treatment of<br />
Drowning”. Wilderness and Environmental Medicine. June;27(2):236-51.<br />
6. Szpilman D, Pearn J, Queiroga AC (2019) “Medical Position Statement MPS<br />
22 – Research Needs for Drowning”. International Lifesaving Fderation Rescue<br />
Commission 28/08/2019. https://www.ilsf.org/wp-content/uploads/2020/01/<br />
MPS-22-2019-Research-Needs-for-Drowning.pdf Accessed 19th January <strong>2021</strong><br />
7. American Heart Association (2005) “Drowning”. Circulation. 112(2) Supp. 13.<br />
IV-133-IV-135.<br />
8. International Lifesaving (2015) “World Conference on Drowning Prevention 2015<br />
– Malaysia: Program and Proceedings”. ILS. https://www.ilsf.org/wp-content/<br />
uploads/2018/11/WCDP2015_ProgramProceedingsLR.pdf Accessed 19th<br />
January <strong>2021</strong><br />
9. Datta A and Tipton M (2006) “Respiratory responses to cold water immersion:<br />
neural pathways, interactions, and clinical consequences awake and asleep”.<br />
Journal of Applied Physiology. 100:6, 2057-2064<br />
10. Giesbrecht G. (2000) “Cold stress, near drowning and accidental hypothermia: A<br />
review”. Aviation, Space, and Environmental Medicine. 71. 733-52.<br />
11. Matthew JA. (2016) “Submersion and Diving-Related Illnesses”. In: David S.<br />
(eds) Clinical Pathways in Emergency Medicine. Springer, New Delhi.<br />
12. Schmidt AC, Sempsrott JR, Hawkins SC, Arastu AS, Cushing TA, Auerbach PS. (2016)<br />
“Wilderness Medical Society Practice Guidelines for the Prevention and Treatment of<br />
Drowning”. Wilderness and Environmental Medicine. Jun;27(2):236-51.<br />
13. Vittone M and Francesco A. (2006) “Drowning doesn’t look like drowning”.<br />
On Scene – the Journal of of U. S. Coast Guard Search and Rescue. Fall. P.14.<br />
https://mariovittone.com/wp-content/uploads/2010/05/OSFall06.pdf Accessed<br />
19th January <strong>2021</strong><br />
14. National operational Guidance: Water Rescue and Flooding”. National Central<br />
Programme Office. https://www.ukfrs.com/pdf/print/node%3A20802 Accessed<br />
on 9th January <strong>2021</strong><br />
15. Tipton MJ, Golden FS. (2011) “A proposed decision-making guide for the<br />
search, rescue and resuscitation of submersion (head under) victims based on<br />
expert opinion”. <strong>Resus</strong>citation. Jul;82(7):819-24<br />
RESUSCITATION TODAY - SUMMER <strong>2021</strong><br />
9
FEATURE<br />
THE FUTURE OF POINT OF CARE<br />
ULTRASOUND (POCUS) TRAINING<br />
Authors: Dr Andrew Tagg & Mr Benjamin Krynski<br />
About the authors: Dr Tagg is the Medical Director of Real Response, and an adult and paediatric emergency and retrieval<br />
specialist in Melbourne. Benjamin Krynski is an ALS paramedic in Sydney and Co-Founder of Real Response.<br />
Introduction<br />
The extended Focused Assessment with Sonography of Trauma<br />
(e-FAST) scan is a key part of the resuscitationists diagnostic toolkit<br />
(Kirkpatric et al. 2004). Rapid sonographic assessment of the chest for<br />
the presence of a pneumothorax can lead to life-saving interventions<br />
whilst the presence, or absence, of free fluid in the abdomen or pelvis<br />
can change the immediate disposition of the patient.<br />
RESUSCITATION TODAY - SUMMER <strong>2021</strong><br />
There are many opportunities for learning this core skill in the hospital<br />
environment. Repeat practice, guided by a skilled clinician, means that<br />
the skill of image acquisition can be taught to anyone. These images<br />
can then be reviewed remotely to facilitate making a diagnosis.<br />
The ability to perform a timely e-FAST scan degrades with time and<br />
there are concerns over the ability of any one practitioner to maintain<br />
their skills (Edgar et al. 2019). There is some evidence that visualizing<br />
a task can strengthen one’s ability to perform the task. The firing of<br />
bidirectional visuo-motor and motor-visual mirror neurons has been<br />
demonstrated in a number of sports including climbing (Boschker and<br />
Bakker, 2002), soccer (Horn, Williams, and Scott, 2002) and cricket<br />
(Breslin et al., 2005)<br />
We wanted to test the hypothesis that novices could obtain the visuomotor<br />
skill of e-FAST image acquisition using enhanced visualization<br />
through the medium of immersive virtual reality (IVR). If successful, it<br />
could lower the barrier of entry for POCUS education enhancing the<br />
number of trained staff who can perform an e-FAST assessment.<br />
The Model<br />
Using off the shelf hardware (Oculus Quest 2) as the delivery<br />
device the challenge was to create a virtual simulacrum of patient,<br />
pathology and ultrasound probes. Development and 3D modelling<br />
was completed with Unity, Marmoset toolbag and Substance<br />
painter, all commercially available platforms. Development was led<br />
by Real Response based in Melbourne, Australia and supported by<br />
Healthcare Australia.<br />
The Lumify POCUS was chosen for the device to be 3D rendered<br />
and embedded into the immersive virtual world and training scenario.<br />
The tablet, phased array, curvilinear and linear transducers were<br />
modelled.<br />
The Scenario<br />
The environment of an Australian Army MRH-90 Taipan helicopter<br />
was created and upon starting the scenario users are transported<br />
to the MedEvac bay where they receive a handover from a medic<br />
asking them to perform a e-FAST assessment on their patient to<br />
determine potential internal injury.<br />
The user is then expected to perform a e-FAST assessment using<br />
the Lumify ensuring they hold the transducer appropriately and in<br />
the correct location to acquire a high quality image and perform an<br />
interpretation. The user is assessed on their interpretation of the<br />
image acquired.<br />
10
FEATURE<br />
Instructor Guidance<br />
Instructors can remotely observe the user and offer real-time guidance<br />
and verbal direction. Through offering remote/virtual guidance by a<br />
skilled clinician, IVR for POCUS training may reduce the barrier of<br />
entry allowing a greater number of clinicians to become competent<br />
in the e-FAST assessment. These may include remote GP’s, nurses,<br />
paramedics, military medics and off-shore/industrial medics.<br />
The next stage of research will be to assess the ability and timeliness<br />
of a cohort of novices to acquire suitable images as compared to those<br />
learning passively from video.<br />
Summary<br />
The ability to perform and interpret an e-FAST scan is just one small<br />
part of the complex virtual simulation package that Real Response<br />
hopes to deliver. The post-COVID world poses a number of challenges<br />
to traditional face-to-face courses. With national and international travel<br />
curtailed we are becoming used to technology enhanced learning in the<br />
virtual Zoom classroom. Perhaps now is the right time to step into the<br />
virtual simulation space too?<br />
References:<br />
Boschker, M. S., and Bakker, F. C. (2002). Inexperienced sport climbers<br />
might perceive and utilize new opportunities for action by merely<br />
observing a model. Percept Mot Skills, 95(1), 3-9.<br />
Breslin, G., Hodges, N. J., Williams, A. M., Curran, W., and Kremer, J.<br />
(2005). Modelling relative motion to facilitate intra-limb coordination.<br />
Hum Mov Sci, 24(3), 446-463.<br />
Edgar, L., Fraccaro, L., Park, L., MacIsaac, J., Pageau, P., Ramnanan,<br />
C. and Woo, M., 2019. MP16: Which PoCUS skills are retained over<br />
time for medical students?. Canadian Journal of Emergency Medicine,<br />
21(S1), pp.S47-S48.<br />
Horn, R. R., Williams, A. M., & Scott, M. A. (2002). Learning from<br />
demonstrations: the role of visual search during observational learning<br />
from video and point-light models. J Sports Sci, 20(3), 253-269.<br />
Kirkpatrick, A.W., Sirois, M., Laupland, K.B., Liu, D., Rowan, K., Ball,<br />
C.G., Hameed, S.M., Brown, R., Simons, R., Dulchavsky, S.A. and<br />
Hamiilton, D.R., 2004. Hand-held thoracic sonography for detecting<br />
post-traumatic pneumothoraces: the Extended Focused Assessment<br />
with Sonography for Trauma (EFAST). Journal of Trauma and Acute Care<br />
Surgery, 57(2), pp.288-295.<br />
Rodríguez, Á.L., Cheeran, B., Koch, G., Hortobágyi, T. and Fernandez-del-<br />
Olmo, M., 2014. The role of mirror neurons in observational motor learning: an<br />
integrative review. European Journal of Human Movement, (32), pp.82-103.<br />
Introducing the NEW EOlifeX ®<br />
- manual ventilation training made simple<br />
Hyperventilation risks are reduced by a<br />
factor of 10 with EOlife ®<br />
100%<br />
80%<br />
60%<br />
40%<br />
EOlifeX displays breath to breath Inspiratory Volume, Tidal Volume,<br />
Respiratory Rate, Mask Leakage and ensures life-saving ventilations<br />
are delivered in accordance with International <strong>Resus</strong>citation Guidelines.<br />
For further information please visit www.mdtglobalsolutions.com<br />
E-mail: sales@mdtglobalsolutions.com<br />
Visit us: Emergency Services Show, Sept 7/8 NEC - Stand 44<br />
20%<br />
0%<br />
Conventional<br />
ventilation<br />
with mask<br />
Ventilation<br />
with mask<br />
and EOlife<br />
Conventional<br />
ventilation with<br />
endotracheal<br />
tube<br />
Ventilation with<br />
endotracheal<br />
tube & EOlife<br />
Hypoventilation Adequate ventilation Hyperventilation<br />
RESUSCITATION TODAY - SUMMER <strong>2021</strong><br />
11
FEATURE<br />
North West resuscitation expert explains<br />
new <strong>2021</strong> <strong>Resus</strong>citation Guidelines<br />
The <strong>Resus</strong>citation Council<br />
(UK) (RCUK) has released its<br />
latest set of guidelines for<br />
the emergency treatment of<br />
critically unwell patients.<br />
The <strong>2021</strong> guidelines build on the<br />
2015 guidelines and the latest<br />
recommendations from the<br />
European <strong>Resus</strong>citation Council<br />
(ERC), providing the best up-todate<br />
evidence for clinical practice<br />
in the UK, including the use of escalating and high levels of energy.<br />
The guidelines also recognise that many cardiac arrests have<br />
premonitory signs and are preventable. Anthony Freestone, RCUK<br />
regional representative for the North West and advanced clinical<br />
practitioner at Blackpool Teaching Hospitals NHS Foundation Trust,<br />
explains: “The focus must always be on preventing cardiac arrest<br />
from occurring. Greater emphasis on recognising and treating the<br />
deteriorating patient should be every NHS Trust’s responsibility, in<br />
line with other Guidelines such as NICE (CG50).<br />
“With the growing recognition that many cardiac arrests can be<br />
identified in advance, it makes sense to employ comprehensive<br />
monitoring where possible to reduce mortality. Our defibrillator<br />
supplier builds precision monitoring into its defibrillators, to assist in<br />
peri and post arrest resuscitation stages.”<br />
On the latest defibrillation and cardioversion guidelines, Mr Freestone<br />
said: “Working in a Regional Cardiac Centre, with some of the best<br />
and most qualified staff within the field, I feel that energy plays a<br />
major part in resuscitation. In my experience for both defibrillation<br />
and cardioversion, using the highest possible energy level is a clinical<br />
necessity, a shock strategy re-enforced by both the RCUK and the<br />
ERC in certain situations. The guidelines call for an ‘initial synchronised<br />
shock at maximum defibrillator output’ to respond to atrial fibrillation,<br />
as this arrythmia often requires greater levels of energy to terminate.<br />
“Our Mindray defibrillators can rapidly charge and produce a biphasic<br />
shock at up to 360J in five seconds, so we are ideally equipped to<br />
meet this guideline.<br />
“For fixed high energy versus escalating shocks protocols, this is<br />
a very exciting time. The guidelines again highlight escalation of<br />
energy after a failed shock, and for patients where refibrillation has<br />
occurred, but now give us the option of starting within an energy<br />
range, empowering <strong>Resus</strong>citation Departments to think outside the<br />
box when it comes to defibrillation energy requirements.”<br />
The new guidelines clarify the RCUK’s position on capnography,<br />
requiring it be used to monitor the quality of CPR.<br />
“While defibrillation is important, we need to continue to push<br />
for high quality CPR, where the only recommendation is for<br />
capnography, which had previously always been more of a<br />
consideration. The technology does more than just tell the user<br />
to push harder, it’s an accurate display of how the resuscitation<br />
attempt is going and can provide a real insight into performance and<br />
feedback.” Mr Freestone comments.<br />
“Our Mindray devices provide up to 360J, capnography and a full<br />
range of peri and post arrest monitoring, which from a point of care<br />
perspective enables the patient to have the best possible chance of<br />
survival no matter the stage of resuscitation they are in.”<br />
RESUSCITATION TODAY - SUMMER <strong>2021</strong><br />
To find out more about Mindray’s<br />
D3 and D6 Platinum range<br />
defibrillators, just scan this QR code<br />
or visit www.mindrayuk.com.<br />
12
FEATURE<br />
NEW TECHNOLOGIES AND ARTIFICIAL INTELLIGENCE<br />
IN EMERGENCY MEDICINE: TOOLS TO IMPROVE<br />
CARDIO-PULMONARY RESUSCITATION (CPR)<br />
Abdo Khoury MD, MPH, MScDM<br />
Department of Emergency Medicine and Critical Care, Besancon University Hospital, France<br />
akhoury@chu-besancon.fr<br />
In the field of cardiopulmonary resuscitation (CPR), one might think<br />
that progress is more “laborious” than in other medical specialties,<br />
but the reality is more complex. Naturally, one would always wish that<br />
things move faster, certainly, especially in the last few years. Because<br />
it is clear that we are facing a stagnation in the survival rate of patient<br />
in cardiorespiratory arrest (CA). Survival to discharge slightly improved<br />
from the seventies to reach 8.8% [1]. We must therefore remain patient<br />
and determined. No choice: we must innovate and we can!<br />
Recently, practitioners have, for example, thought to optimise chest<br />
compressions by focusing on two parameters: the depth of the<br />
compressions and their rhythm. Without forgetting to give time for<br />
thoracic relaxation. Having a bystander initiating prompt CPR has led to<br />
an increase in survival rate up to 11.3% [1]. All these optimisations have<br />
already proven to have a positive impact on the survival rate, which is<br />
our main objective. There is no doubt that the European <strong>Resus</strong>citation<br />
Council (ERC) Congress on Cardiac Arrest to be held in March <strong>2021</strong> (it<br />
should have been held in Manchester from 20 to 22 October) promises<br />
to be rich in new recommendations. The congress will certainly explore<br />
other avenues: improving ventilation is surely one of them, and in recent<br />
years many studies have been talking more and more about it.<br />
Proof of this is that things are “on the move”, these recommendations -<br />
or treatment protocols - are slowly but surely evolving. Although that to<br />
date, many of my colleagues would tend to consider them as optimal.<br />
The fact is that these international guidelines are relatively poorly<br />
applied, especially on ventilation [2] And this is where the problem lies:<br />
how to explain it?<br />
<strong>Today</strong>, the recommendations focus on chest compressions, recalling<br />
the uniformly accepted good practices: early warning, initiate chest<br />
compressions and ventilate if trained to do so... As for ventilation,<br />
which is of crucial importance, it has been proven long time ago, that<br />
hyperventilation of 30 times/minute reduces the chance of survival<br />
by a factor of 3 [3]. Hyperventilation increases the Mean Intrathoracic<br />
Pressure thus decreasing the venous return to the heart and decreasing<br />
the Coronary Arteries Perfusion Pressure (CPP) (fig 1). On the other<br />
hand, ventilating 12 times/minute multiplies survival by 3 folds...<br />
However, we still don’t know how to stick to the recommendations: the<br />
scientific knowledge is up to date, but putting it into practice remains...<br />
theoretical or even impossible.<br />
Moreover, in this field we are now seeing a return to the fundamentals,<br />
against a backdrop of specialist controversy: should we intubate or<br />
ventilate, taken up by the famous “intubate or not”? Two systems<br />
predominate: the Anglo-Saxon system based on mask ventilation with<br />
rapid transport to the nearest hospital where the doctors will perform<br />
advanced resuscitation, and the Franco-German system, with the<br />
Figure 1. Hemodynamic Study (n=9). Changes in mean intrathoracic<br />
pressure (MIP), coronary perfusion pressure (CPP), and right atrial<br />
diastolic pressure (RA diastolic) with different ventilation rates during<br />
resuscitation in a porcine model of cardiac arrest. Probability value<br />
FEATURE<br />
Figure 2. Percentage of hyperventilation (black), adequate ventilation<br />
(grey) and hypoventilation (light grey) for professional categories<br />
(n=280 tests for each ventilation technique).<br />
ETT, endotracheal tube [6].<br />
stability... In addition to this, there are other needs, very strong<br />
regulatory constraints and clinical trials that are more difficult to carry<br />
out in the field. Nevertheless, over the last twenty years, new fields of<br />
research (digital, miniaturisation …) have enlarged our perspectives and<br />
possibilities in healthcare innovations.<br />
Figure 3. Comparison of mean tidal volume (a) and mean ventilation<br />
rate (b) for each participant between conventional ventilation (O) and<br />
ventilation with VFD (X) for Basic Life Support (BLS) and Advanced<br />
Life Support (ALS) groups. n = 20 participants/group, ventilation was<br />
performed during 5 min/participant [8].<br />
become a reference in just a few years, has already inspired a number<br />
of manufacturers and, above all, generated new projects in research<br />
and development [9].<br />
It is in this context that applied artificial intelligence could well<br />
revolutionise practices, or at least shake them up. It seems to be<br />
present everywhere: robots, glasses, microscopes, radios... or almost.<br />
Indeed, it is far from having revealed its full potential in our branch,<br />
and would even be cruelly lacking. If it is not a question of replacing<br />
humans, but of “completing” them, of perfecting their gestures, then it<br />
has a bright future in emergency medicine and CPR [7].<br />
The time for breakthrough innovations may have come for emergency<br />
medicine. With solutions designed by and for practitioners, and<br />
validated by “field teams”. Significant progress which, besides relieving<br />
part of the extremely heavy burden of first aid to some extent, should<br />
save more lives. A real glimmer of hope in a particularly difficult context.<br />
Bibliography<br />
RESUSCITATION TODAY - SUMMER <strong>2021</strong><br />
We only seem to be at the dawn of these advances... And the<br />
applications are flourishing. For example, a team of engineers and I<br />
led a project to design a completely innovative ventilation assistance<br />
device. This small device, recently marketed by the French company<br />
Archeon, is attached to oxygen insufflators to measure the quality of<br />
ventilation during CPR: the right volume of air to be administered, the<br />
optimum ventilation frequency, and it analyses the different variables,<br />
depending on the patient’s profile [8]. Packed with electronics, its<br />
“intelligence” results from the interpretation of 56,000 ventilation cycles,<br />
with the aim of identifying a volume trend of optimal frequencies and to<br />
tell, in real time, if we are within the standards. It starts to equip a large<br />
number of ambulances and emergency services across the world.<br />
EOlife ® Ventilation Feedback<br />
Device (VFD)<br />
We could just as easily mention the Lucas massage board, a real<br />
find, pure product of mechanical engineering. To automate and<br />
calibrate chest compressions gesture thanks to a machine, one had<br />
to think about it! An astonishing device that has opened up beautiful<br />
perspectives in terms of dealing with CPR. This system, which has<br />
1. Yan S, Gan Y, Jiang N, Wang R, Chen Y, Luo Z, et al. The global survival rate<br />
among adult out-of-hospital cardiac arrest patients who received cardiopulmonary<br />
resuscitation: a systematic review and meta-analysis. Crit Care 2020;24:61.<br />
2. Cordioli RL, Brochard L, Suppan L, Lyazidi A, Templier F, Khoury A, et al. How<br />
Ventilation Is Delivered During Cardiopulmonary <strong>Resus</strong>citation: An International<br />
Survey. Respir Care 2018;63:1293–301.<br />
3. Aufderheide TP, Sigurdsson G, Pirrallo RG, Yannopoulos D, McKnite S, von<br />
Briesen C, et al. Hyperventilation-induced hypotension during cardiopulmonary<br />
resuscitation. Circulation 2004;109:1960–5.<br />
4. Sinning C, Ahrens I, Cariou A, Beygui F, Lamhaut L, Halvorsen S, et al. The cardiac<br />
arrest centre for the treatment of sudden cardiac arrest due to presumed cardiac<br />
cause - aims, function and structure: Position paper of the Association for Acute<br />
CardioVascular Care of the European Society of Cardiology (AVCV), European<br />
Association of Percutaneous Coronary Interventions (EAPCI), European Heart<br />
Rhythm Association (EHRA), European <strong>Resus</strong>citation Council (ERC), European<br />
Society for Emergency Medicine (EUSEM) and European Society of Intensive Care<br />
Medicine (ESICM). Eur Heart J Acute Cardiovasc Care 2020;9:S193–202.<br />
5. Jabre P, Penaloza A, Pinero D, Duchateau F-X, Borron SW, Javaudin F, et al. Effect<br />
of Bag-Mask Ventilation vs Endotracheal Intubation During Cardiopulmonary<br />
<strong>Resus</strong>citation on Neurological Outcome After Out-of-Hospital Cardiorespiratory<br />
Arrest: A Randomized Clinical Trial. JAMA 2018;319:779–87.<br />
6. Sall FS, De Luca A, Pazart L, Pugin A, Capellier G, Khoury A. To intubate or not:<br />
ventilation is the question. A manikin-based observational study. BMJ Open Respir<br />
Res 2018;5:e000261.<br />
7. Jiang F, Jiang Y, Zhi H, Dong Y, Li H, Ma S, et al. Artificial intelligence in<br />
healthcare: past, present and future. Stroke Vasc Neurol 2017;2:230–43.<br />
8. Khoury A, De Luca A, Sall FS, Pazart L, Capellier G. Ventilation feedback device<br />
for manual ventilation in simulated respiratory arrest: a crossover manikin study.<br />
Scand J Trauma <strong>Resus</strong>c Emerg Med 2019;27:93.<br />
9. Strugo R, Wacht O, Kohn J. Mechanical CPR Devices: Where is the Science?<br />
JEMS. 2019.https://www.jems.com/exclusives/mechanical-cpr-devices-where-isthe-science/<br />
(accessed 10 Feb<strong>2021</strong>).<br />
14
FEATURE<br />
FREE EDUCATIONAL PODCASTS<br />
In the knowledge that conferences and exhibitions may be difficult to attend we are delighted to<br />
offer you the opportunity to listen to the following presentations listed on www.resustoday.com<br />
FREE OF CHARGE with further presentations being added on a regular basis (average Podcast<br />
time is 30 minutes):<br />
Management of Traumatic Cardiac Arrest - Richard Lyons<br />
The role of humour - Joel Symonds<br />
Assessment Treatment - Paddy Morgan<br />
Head Injuries - Dr Jonathan Hanson<br />
Drowning and cold water - Paddy Morgan<br />
Post <strong>Resus</strong>citation Care - Paul Rees<br />
The importance of sleep - Lisa Artist<br />
This unique section on our web site also gives you the opportunity to see the following products being<br />
demonstrated:<br />
• I-view(tm) video laryyngoscope<br />
• Water Rescue toddler<br />
• EOlife Ventillation Monitor<br />
• Quantum Life Warmer<br />
Visit www.resustoday.com<br />
We are also seeking further presentation/podcasts to add to this exciting new educational concept<br />
therefore if you have anything to submit that would interest those working in Pre Hospital Care,<br />
<strong>Resus</strong>citation and Simulation please forward it to info@mediapublishingcompany.com<br />
Volume 35 No. 5<br />
IT’S FREE - IT’S EDUCATIONAL - IT’S REWARDING<br />
WWW.RESUSTODAY.COM<br />
DEDICATED TO THE AMBULANCE SERVICE AND ITS SUPPLIERS<br />
October 2020<br />
Discover the Quantum<br />
DIFFERENCE<br />
THE Prehospital Blood &Fluid Warming Solution<br />
Volume 30 No. 4<br />
Winter 2020<br />
Gastroenterology <strong>Today</strong><br />
New Ways of Working<br />
within Endoscopy<br />
One of the impacts of Covid-19 is<br />
the way the NHS is accepting and<br />
encouraging new ways of working.<br />
But is this true in endoscopy?<br />
In this edition, we look at insourcing<br />
with 18 Week Support as a solution,<br />
the actual experience of our nurses<br />
and clinicians working on these<br />
short-term contracts and explore<br />
the differences in working life with<br />
18 Week Support compared to their<br />
day to day jobs in their home trusts.<br />
Volume 7 No. 2<br />
Autumn 2020<br />
<strong>Resus</strong>citation <strong>Today</strong><br />
A Resource for all involved in the Teaching and Practice of <strong>Resus</strong>citation<br />
Volume 2 No. 2<br />
Autumn 2020<br />
Simulation<strong>Today</strong><br />
A resource for all involved in the teaching and practice of simulation<br />
RESUSCITATION TODAY - SUMMER <strong>2021</strong><br />
Blood &<br />
Fl<br />
uid<br />
Wa<br />
rm<br />
in<br />
ng<br />
Sy<br />
ys<br />
te<br />
m<br />
ENHANCE PAEDIATRIC SIMULATION WITH REALITi<br />
Train critical skills required for your most vulnerable patients<br />
FAST | EFFECTIVE | SAFE | INTUITIVE | LIGHTWEIGHT | POWERFUL<br />
EXCLUSIVE TO<br />
See reverse for Simulation <strong>Today</strong><br />
See reverse for <strong>Resus</strong>citation <strong>Today</strong><br />
15