RESidENcy PROGRAM Scholarly and Community Medicine Projects
RESidENcy PROGRAM Scholarly and Community Medicine Projects
RESidENcy PROGRAM Scholarly and Community Medicine Projects
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
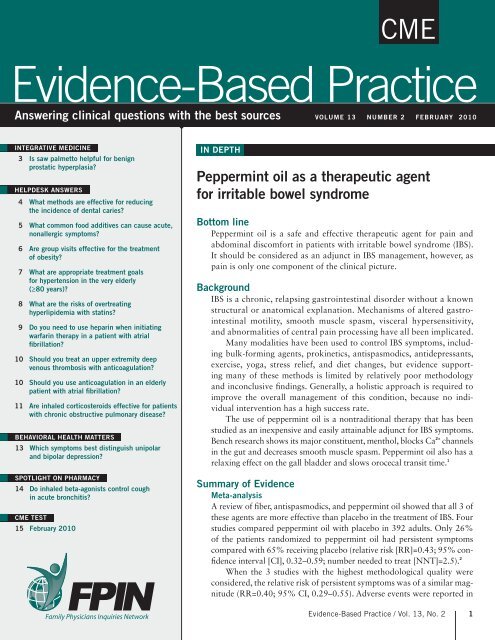
CME<br />
Evidence-Based Practice<br />
Answering clinical questions with the best sources VOLUME 13 NUMBER 2 FEBRUARY 2010<br />
INTEGRATIVE MEDICINE IN DEPTH<br />
3 Is saw palmetto helpful for benign<br />
prostatic hyperplasia?<br />
HELPDESK ANSWERS<br />
4 What methods are effective for reducing<br />
the incidence of dental caries?<br />
5 What common food additives can cause acute,<br />
nonallergic symptoms?<br />
6 Are group visits effective for the treatment<br />
of obesity?<br />
7 What are appropriate treatment goals<br />
for hypertension in the very elderly<br />
(≥80 years)?<br />
8 What are the risks of overtreating<br />
hyperlipidemia with statins?<br />
9 Do you need to use heparin when initiating<br />
warfarin therapy in a patient with atrial<br />
fibrillation?<br />
10 Should you treat an upper extremity deep<br />
venous thrombosis with anticoagulation?<br />
10 Should you use anticoagulation in an elderly<br />
patient with atrial fibrillation?<br />
11 Are inhaled corticosteroids effective for patients<br />
with chronic obstructive pulmonary disease?<br />
BEHAVIORAL HEALTH MATTERS<br />
13 Which symptoms best distinguish unipolar<br />
<strong>and</strong> bipolar depression?<br />
SPOTLIGHT ON PHARMACY<br />
14 Do inhaled beta-agonists control cough<br />
in acute bronchitis?<br />
CME TEST<br />
15 February 2010<br />
Peppermint oil as a therapeutic agent<br />
for irritable bowel syndrome<br />
Bottom line<br />
Peppermint oil is a safe <strong>and</strong> effective therapeutic agent for pain <strong>and</strong><br />
abdominal discomfort in patients with irritable bowel syndrome (IBS).<br />
It should be considered as an adjunct in IBS management, however, as<br />
pain is only one component of the clinical picture.<br />
Background<br />
IBS is a chronic, relapsing gastrointestinal disorder without a known<br />
structural or anatomical explanation. Mechanisms of altered gastrointestinal<br />
motility, smooth muscle spasm, visceral hypersensitivity,<br />
<strong>and</strong> abnormalities of central pain processing have all been implicated.<br />
Many modalities have been used to control IBS symptoms, including<br />
bulk-forming agents, prokinetics, antispasmodics, antidepressants,<br />
exercise, yoga, stress relief, <strong>and</strong> diet changes, but evidence supporting<br />
many of these methods is limited by relatively poor methodology<br />
<strong>and</strong> inconclusive findings. Generally, a holistic approach is required to<br />
improve the overall management of this condition, because no individual<br />
intervention has a high success rate.<br />
The use of peppermint oil is a nontraditional therapy that has been<br />
studied as an inexpensive <strong>and</strong> easily attainable adjunct for IBS symptoms.<br />
Bench research shows its major constituent, menthol, blocks Ca 2+ channels<br />
in the gut <strong>and</strong> decreases smooth muscle spasm. Peppermint oil also has a<br />
relaxing effect on the gall bladder <strong>and</strong> slows orocecal transit time. 1<br />
Summary of Evidence<br />
Meta-analysis<br />
A review of fiber, antispasmodics, <strong>and</strong> peppermint oil showed that all 3 of<br />
these agents are more effective than placebo in the treatment of IBS. Four<br />
studies compared peppermint oil with placebo in 392 adults. Only 26%<br />
of the patients r<strong>and</strong>omized to peppermint oil had persistent symptoms<br />
compared with 65% receiving placebo (relative risk [RR]=0.43; 95% confidence<br />
interval [CI], 0.32–0.59; number needed to treat [NNT]=2.5). 2<br />
When the 3 studies with the highest methodological quality were<br />
considered, the relative risk of persistent symptoms was of a similar magnitude<br />
(RR=0.40; 95% CI, 0.29–0.55). Adverse events were reported in<br />
Evidence-Based Practice / Vol. 13, No. 2 1