Georgia Nursing - July 2022
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
Page 12 • <strong>Georgia</strong> <strong>Nursing</strong> <strong>July</strong>, August, September <strong>2022</strong><br />
Advancing Health Equity in <strong>Georgia</strong> continued from page 11<br />
Care” describes the disturbing health care experiences<br />
of individuals from underrepresented groups and<br />
the impact of racial, ethnic, and other forms of<br />
discrimination have on quality of health care. Little<br />
sustained change has occurred in reducing health<br />
disparities since this report 19 years ago.<br />
Social, economic, and environmental inequities,<br />
and psychosocial trauma, and residential segregation<br />
have been examined and provide pathways to<br />
understanding the interconnectedness of structural<br />
racism and poor health (Bailey et al, 2017; Yearby,<br />
2020). Although these issues are complex, they<br />
add a contextual framework in understanding the<br />
relationships among these concepts and help to<br />
organize approaches to achieve health equity.<br />
To address health inequities imposed by the<br />
social determinants of health and other barriers it is<br />
important to have some common evidence supported<br />
definitions (see Table 1). Additionally, it is important to<br />
engage people across multiple disciplines and sectors.<br />
One important sector is nursing. <strong>Nursing</strong> has been<br />
recognized as a key player not only in the health care<br />
workforce, but also for the central role nurses play in<br />
building healthier communities and achieving health<br />
equity where everyone has a fair opportunity for<br />
quality health care (Robert Wood Johnson Foundation,<br />
2020). The National League of <strong>Nursing</strong> (2019)<br />
highlights the impact Social Determinants of Health<br />
(SDOH) has on health equity, social justice, and health<br />
outcomes, and recommends that SDOH integration in<br />
nursing education curricula is critical to advance the<br />
health of national and global communities. American<br />
Association of Colleges of <strong>Nursing</strong>’s (AACN) newly<br />
released Essentials for professional nursing education<br />
calls for competencies that reflect an understanding<br />
of the interrelatedness of SDOH, systemic racism, bias,<br />
and health equity (AACN, 2021). AACN acknowledges<br />
how imperative it is for a prepared nursing workforce<br />
to address the persistent and pervasive health<br />
inequities in urban and rural areas where there are<br />
unequal distribution of resources and access to<br />
healthcare services (AACN, 2021).<br />
Although, there are many drivers of health<br />
disparities and the magnitude and complexity of<br />
these problems cannot rely on one discipline alone for<br />
solutions, nursing is key to any organized health system<br />
approach to advance health equity among <strong>Georgia</strong>ns.<br />
For 20 consecutive years the Gallup Poll reports<br />
nurses rated highest among a list of professionals in<br />
honesty and ethics (Saad, <strong>2022</strong>). The first principle in<br />
the American Nurses Association (ANA) Code of Ethics<br />
for Nurses reads that, “the nurse, in all professional<br />
relationships, practices with compassion and respect<br />
for the inherent dignity, worth, and uniqueness of<br />
every individual unrestricted by consideration of social<br />
or economic status, personal attributes, or the nature<br />
of the health problems.” p.1.<br />
The Healthy People 2020 declaration placed an<br />
emphasis on eliminating health disparities as cited:<br />
Health disparities adversely affect groups of people<br />
who have systematically experienced greater social or<br />
To access electronic copies of<br />
<strong>Georgia</strong> <strong>Nursing</strong>, please visit<br />
http://www.<strong>Nursing</strong>ALD.com/publications<br />
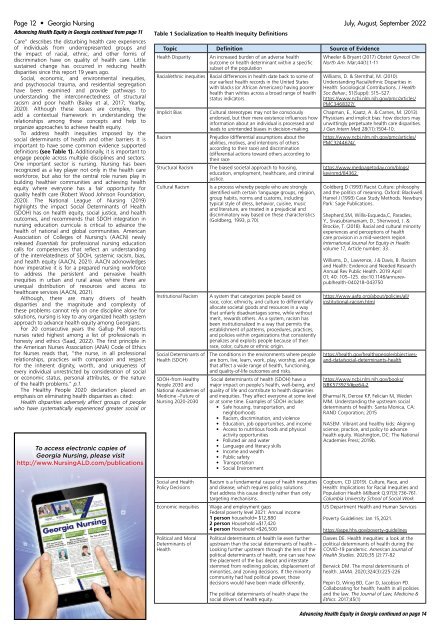
Table 1 Socialization to Health Inequity Definitions<br />
Topic Definition Source of Evidence<br />
Health Disparity<br />
Racial/ethnic inequities<br />
Implicit Bias<br />
Racism<br />
Structural Racism<br />
Cultural Racism<br />
Institutional Racism<br />
Social Determinants of<br />
Health (SDOH)<br />
SDOH-from Healthy<br />
People 2030 and<br />
National Academies of<br />
Medicine –Future of<br />
<strong>Nursing</strong> 2020-2030<br />
An increased burden of an adverse health<br />
outcome or health determinant within a specific<br />
subset of the population<br />
Racial differences in health date back to some of<br />
our earliest health records in the United States<br />
with blacks (or African Americans) having poorer<br />
health than whites across a broad range of health<br />
status indicators.<br />
Cultural stereotypes may not be consciously<br />
endorsed, but their mere existence influences how<br />
information about an individual is processed and<br />
leads to unintended biases in decision-making.<br />
Prejudice (differential assumptions about the<br />
abilities, motives, and intentions of others<br />
according to their race) and discrimination<br />
(differential actions toward others according to<br />
their race<br />
The biased societal approach to housing,<br />
education, employment, healthcare, and criminal<br />
justice.<br />
Is a process whereby people who are strongly<br />
identified with certain ‘language groups, religion,<br />
group habits, norms and customs, including<br />
typical style of dress, behavior, cuisine, music<br />
and literature, are treated in a prejudicial and<br />
discriminatory way based on these characteristics<br />
(Goldberg, 1993, p.70).<br />
A system that categorizes people based on<br />
race, color, ethnicity, and culture to differentially<br />
allocate societal goods and resources in a way<br />
that unfairly disadvantages some, while without<br />
merit, rewards others. As a system, racism has<br />
been institutionalized in a way that permits the<br />
establishment of patterns, procedures, practices,<br />
and policies within organizations that consistently<br />
penalizes and exploits people because of their<br />
race, color, culture or ethnic origin.<br />
The conditions in the environments where people<br />
are born, live, learn, work, play, worship, and age<br />
that affect a wide range of health, functioning,<br />
and quality-of-life outcomes and risks.<br />
Social determinants of health (SDOH) have a<br />
major impact on people’s health, well-being, and<br />
quality of life and contribute to health disparities<br />
and inequities. They affect everyone at some level<br />
or at some time. Examples of SDOH include:<br />
• Safe housing, transportation, and<br />
neighborhoods<br />
• Racism, discrimination, and violence<br />
• Education, job opportunities, and income<br />
• Access to nutritious foods and physical<br />
activity opportunities<br />
• Polluted air and water<br />
• Language and literacy skills<br />
• Income and wealth<br />
• Public safety<br />
• Transportation<br />
• Social Environment<br />
Wheeler & Bryant (2017) Obstet Gynecol Clin<br />
North Am. Mar;44(1):1-11<br />
Williams, D. & Sternthal, M. (2010).<br />
Understanding Racial/ethnic Disparities in<br />
Health: Sociological Contributions. J Health<br />
Soc Behav.; 51(Suppl): S15–S27.<br />
https://www.ncbi.nlm.nih.gov/pmc/articles/<br />
PMC3468327/<br />
Chapman, E., Kaatz, A. & Carnes, M. (2013).<br />
Physicians and implicit bias: how doctors may<br />
unwittingly perpetuate health care disparities.<br />
J Gen Intern Med 28(11):1504-10.<br />
https://www.ncbi.nlm.nih.gov/pmc/articles/<br />
PMC3244674/<br />
https://www.medpagetoday.com/blogs/<br />
kevinmd/84362<br />
Goldberg D (1993) Racist Culture: philosophy<br />
and the politics of meaning. Oxford: Blackwell.<br />
Hamel J (1993) Case Study Methods. Newbury<br />
Park: Sage Publications.<br />
Shepherd,SM, Willis-Esqueda,C, Paradies,<br />
Y., Sivasubramaniam, D., Sherwood, J. &<br />
Brockie, T. (2018). Racial and cultural minority<br />
experiences and perceptions of health<br />
care provision in a mid-western region.<br />
International Journal for Equity in Health<br />
volume 17, Article number: 33.<br />
https://www.aafp.org/about/policies/all/<br />
institutional-racism.html<br />
Williams, D., Lawrence, J & Davis, B. Racism<br />
and Health: Evidence and Needed Research<br />
Annual Rev Public Health. 2019 April<br />
01; 40: 105–125. doi:10.1146/annurevpublhealth-040218-043750<br />
https://health.gov/healthypeople/objectivesand-data/social-determinants-health<br />
https://www.ncbi.nlm.nih.gov/books/<br />
NBK573923/#pz64-2<br />
Bharmal N, Derose KP, Felician M, Weden<br />
MM. Understanding the upstream social<br />
determinants of health. Santa Monica, CA:<br />
RAND Corporation; 2015<br />
NASEM. Vibrant and healthy kids: Aligning<br />
science, practice, and policy to advance<br />
health equity. Washington, DC: The National<br />
Academies Press; 2019b.<br />
Social and Health<br />
Policy Decisions<br />
Economic inequities<br />
Political and Moral<br />
Determinants of<br />
Health<br />
Racism is a fundamental cause of health inequities<br />
and disease, which requires policy solutions<br />
that address this cause directly rather than only<br />
targeting mechanisms.<br />
Wage and employment gaps<br />
Federal poverty level 2021: Annual income<br />
1 person household= $12,880<br />
2 person Household =$17,420<br />
4 person Household =$26,500<br />
Political determinants of health lie even further<br />
upstream than the social determinants of health –<br />
Looking further upstream through the lens of the<br />
political determinants of health, one can see how<br />
the placement of the bus depot and interstate<br />
stemmed from redlining policies, displacement of<br />
minorities, and zoning decisions. If the minority<br />
community had had political power, those<br />
decisions would have been made differently.<br />
The political determinants of health shape the<br />
social drivers of health equity.<br />
Cogburn, CD (2019). Culture, Race, and<br />
Health: Implications for Racial Inequities and<br />
Population Health Milbank Q.97(3):736-761.<br />
Columbia University School of Social Work<br />
US Department Health and Human Services<br />
Poverty Guidelines: Jan 15,2021.<br />
https://aspe.hhs.gov/poverty-guidelines<br />
Dawes DE. Health inequities: a look at the<br />
political determinants of health during the<br />
COVID-19 pandemic. American Journal of<br />
Health Studies. 2020;35 (2):77-82<br />
Berwick DM. The moral determinants of<br />
health. JAMA. 2020;324(3):225-226<br />
Pepin D, Winig BD, Carr D, Jacobson PD.<br />
Collaborating for health: health in all policies<br />
and the law. The Journal of Law, Medicine &<br />
Ethics. 2017;45(1)<br />
Advancing Health Equity in <strong>Georgia</strong> continued on page 14