McNair Research Journal - University of St. Thomas
McNair Research Journal - University of St. Thomas
McNair Research Journal - University of St. Thomas
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
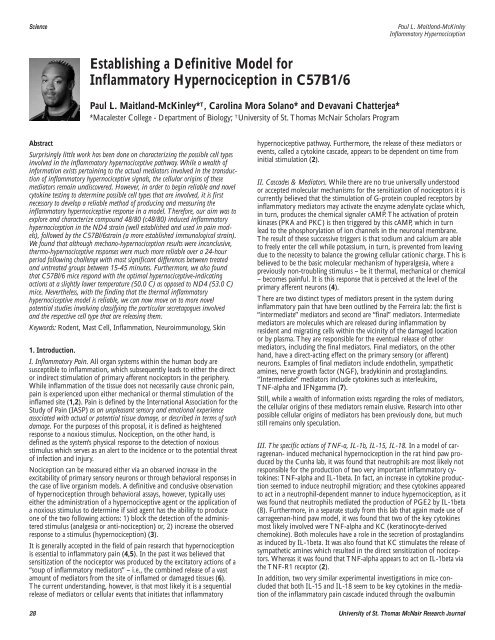
Science<br />
Establishing a Definitive Model for<br />
Inflammatory Hypernociception in C57B1/6<br />
Paul L. Maitland-McKinley* T , Carolina Mora Solano* and Devavani Chatterjea*<br />
*Macalester College - Department <strong>of</strong> Biology; T <strong>University</strong> <strong>of</strong> <strong>St</strong>. <strong>Thomas</strong> <strong>McNair</strong> Scholars Program<br />
Abstract<br />
Surprisingly little work has been done on characterizing the possible cell types<br />
involved in the inflammatory hypernociceptive pathway. While a wealth <strong>of</strong><br />
information exists pertaining to the actual mediators involved in the transduction<br />
<strong>of</strong> inflammatory hypernociceptive signals, the cellular origins <strong>of</strong> these<br />
mediators remain undiscovered. However, in order to begin reliable and novel<br />
cytokine testing to determine possible cell types that are involved, it is first<br />
necessary to develop a reliable method <strong>of</strong> producing and measuring the<br />
inflammatory hypernociceptive response in a model. Therefore, our aim was to<br />
explore and characterize compound 48/80 (c48/80) induced inflammatory<br />
hypernociception in the ND4 strain (well established and used in pain models),<br />
followed by the C57Bl/6strain (a more established immunological strain).<br />
We found that although mechano-hypernociception results were inconclusive,<br />
thermo-hypernociceptive responses were much more reliable over a 24-hour<br />
period following challenge with most significant differences between treated<br />
and untreated groups between 15-45 minutes. Furthermore, we also found<br />
that C57Bl/6 mice respond with the optimal hypernociceptive-indicating<br />
actions at a slightly lower temperature (50.0 C) as opposed to ND4 (53.0 C)<br />
mice. Nevertheless, with the finding that the thermal inflammatory<br />
hypernociceptive model is reliable, we can now move on to more novel<br />
potential studies involving classifying the particular secretagogues involved<br />
and the respective cell type that are releasing them.<br />
Keywords: Rodent, Mast Cell, Inflammation, Neuroimmunology, Skin<br />
1. Introduction.<br />
I. Inflammatory Pain. All organ systems within the human body are<br />
susceptible to inflammation, which subsequently leads to either the direct<br />
or indirect stimulation <strong>of</strong> primary afferent nociceptors in the periphery.<br />
While inflammation <strong>of</strong> the tissue does not necessarily cause chronic pain,<br />
pain is experienced upon either mechanical or thermal stimulation <strong>of</strong> the<br />
inflamed site (1,2). Pain is defined by the International Association for the<br />
<strong>St</strong>udy <strong>of</strong> Pain (IASP) as an unpleasant sensory and emotional experience<br />
associated with actual or potential tissue damage, or described in terms <strong>of</strong> such<br />
damage. For the purposes <strong>of</strong> this proposal, it is defined as heightened<br />
response to a noxious stimulus. Nociception, on the other hand, is<br />
defined as the system’s physical response to the detection <strong>of</strong> noxious<br />
stimulus which serves as an alert to the incidence or to the potential threat<br />
<strong>of</strong> infection and injury.<br />
Nociception can be measured either via an observed increase in the<br />
excitability <strong>of</strong> primary sensory neurons or through behavioral responses in<br />
the case <strong>of</strong> live organism models. A definitive and conclusive observation<br />
<strong>of</strong> hypernociception through behavioral assays, however, typically uses<br />
either the administration <strong>of</strong> a hypernociceptive agent or the application <strong>of</strong><br />
a noxious stimulus to determine if said agent has the ability to produce<br />
one <strong>of</strong> the two following actions: 1) block the detection <strong>of</strong> the administered<br />
stimulus (analgesia or anti-nociception) or, 2) increase the observed<br />
response to a stimulus (hypernociception) (3).<br />
It is generally accepted in the field <strong>of</strong> pain research that hypernociception<br />
is essential to inflammatory pain (4,5). In the past it was believed that<br />
sensitization <strong>of</strong> the nociceptor was produced by the excitatory actions <strong>of</strong> a<br />
“soup <strong>of</strong> inflammatory mediators” – i.e., the combined release <strong>of</strong> a vast<br />
amount <strong>of</strong> mediators from the site <strong>of</strong> inflamed or damaged tissues (6).<br />
The current understanding, however, is that most likely it is a sequential<br />
release <strong>of</strong> mediators or cellular events that initiates that inflammatory<br />
Paul L. Maitland-McKinley<br />
Inflammatory Hypernociception<br />
hypernociceptive pathway. Furthermore, the release <strong>of</strong> these mediators or<br />
events, called a cytokine cascade, appears to be dependent on time from<br />
initial stimulation (2).<br />
II. Cascades & Mediators. While there are no true universally understood<br />
or accepted molecular mechanisms for the sensitization <strong>of</strong> nociceptors it is<br />
currently believed that the stimulation <strong>of</strong> G-protein coupled receptors by<br />
inflammatory mediators may activate the enzyme adenylate cyclase which,<br />
in turn, produces the chemical signaler cAMP. The activation <strong>of</strong> protein<br />
kinases (PKA and PKC) is then triggered by this cAMP, which in turn<br />
lead to the phosphorylation <strong>of</strong> ion channels in the neuronal membrane.<br />
The result <strong>of</strong> these successive triggers is that sodium and calcium are able<br />
to freely enter the cell while potassium, in turn, is prevented from leaving<br />
due to the necessity to balance the growing cellular cationic charge. This is<br />
believed to be the basic molecular mechanism <strong>of</strong> hyperalgesia, where a<br />
previously non-troubling stimulus – be it thermal, mechanical or chemical<br />
– becomes painful. It is this response that is perceived at the level <strong>of</strong> the<br />
primary afferent neurons (4).<br />
There are two distinct types <strong>of</strong> mediators present in the system during<br />
inflammatory pain that have been outlined by the Ferreira lab: the first is<br />
“intermediate” mediators and second are “final” mediators. Intermediate<br />
mediators are molecules which are released during inflammation by<br />
resident and migrating cells within the vicinity <strong>of</strong> the damaged location<br />
or by plasma. They are responsible for the eventual release <strong>of</strong> other<br />
mediators, including the final mediators. Final mediators, on the other<br />
hand, have a direct-acting effect on the primary sensory (or afferent)<br />
neurons. Examples <strong>of</strong> final mediators include endothelin, sympathetic<br />
amines, nerve growth factor (NGF), bradykinin and prostaglandins.<br />
“Intermediate” mediators include cytokines such as interleukins,<br />
TNF-alpha and IFNgamma (7).<br />
<strong>St</strong>ill, while a wealth <strong>of</strong> information exists regarding the roles <strong>of</strong> mediators,<br />
the cellular origins <strong>of</strong> these mediators remain elusive. <strong>Research</strong> into other<br />
possible cellular origins <strong>of</strong> mediators has been previously done, but much<br />
still remains only speculation.<br />
III. The specific actions <strong>of</strong> TNF-a, IL-1b, IL-15, IL-18. In a model <strong>of</strong> carrageenan-<br />
induced mechanical hypernociception in the rat hind paw produced<br />
by the Cunha lab, it was found that neutrophils are most likely not<br />
responsible for the production <strong>of</strong> two very important inflammatory cytokines:<br />
TNF-alpha and IL-1beta. In fact, an increase in cytokine production<br />
seemed to induce neutrophil migration; and these cytokines appeared<br />
to act in a neutrophil-dependent manner to induce hypernociception, as it<br />
was found that neutrophils mediated the production <strong>of</strong> PGE2 by IL-1beta<br />
(8). Furthermore, in a separate study from this lab that again made use <strong>of</strong><br />
carrageenan-hind paw model, it was found that two <strong>of</strong> the key cytokines<br />
most likely involved were TNF-alpha and KC (keratinocyte-derived<br />
chemokine). Both molecules have a role in the secretion <strong>of</strong> prostaglandins<br />
as induced by IL-1beta. It was also found that KC stimulates the release <strong>of</strong><br />
sympathetic amines which resulted in the direct sensitization <strong>of</strong> nociceptors.<br />
Whereas it was found that TNF-alpha appears to act on IL-1beta via<br />
the TNF-R1 receptor (2).<br />
In addition, two very similar experimental investigations in mice concluded<br />
that both IL-15 and IL-18 seem to be key cytokines in the mediation<br />
<strong>of</strong> the inflammatory pain cascade induced through the ovalbumin<br />
28 <strong>University</strong> <strong>of</strong> <strong>St</strong>. <strong>Thomas</strong> <strong>McNair</strong> <strong>Research</strong> <strong>Journal</strong>