Hospice of Emanuel - Emanuel Medical Center
Hospice of Emanuel - Emanuel Medical Center
Hospice of Emanuel - Emanuel Medical Center
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
SPRING 2008<br />
<strong>Hospice</strong> <strong>of</strong> <strong>Emanuel</strong> Helps Families at Life’s End<br />
(<strong>Hospice</strong>, Cont. from page 1)<br />
They slowed down a bit in 2003 when<br />
Bob’s mobility started to slip. But their<br />
days were still busy and happy, filled with<br />
family, friends and each other.<br />
In July 2007, life changed. MaryAnn was<br />
75 and very active – swimming laps,<br />
riding her bike – but all <strong>of</strong> sudden even a<br />
trip to the store would wear her out. Their<br />
family physician ran tests and didn’t like<br />
what we saw. He sent her to <strong>Emanuel</strong>’s<br />
cancer center, where doctors ran more<br />
tests. They, too, didn’t like what they saw.<br />
In November 2007, the Ranes learned that<br />
MaryAnn had pancreatic cancer that had<br />
migrated to her liver. Surgery, chemotherapy<br />
and radiation were long-shot options.<br />
“Doctors didn’t see much light at the end<br />
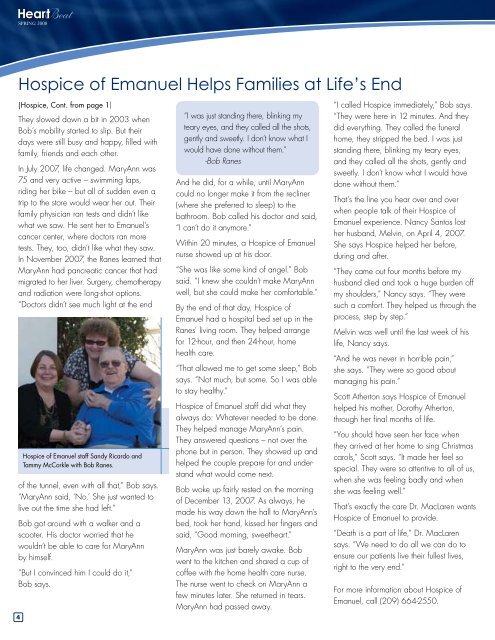
<strong>Hospice</strong> <strong>of</strong> <strong>Emanuel</strong> staff Sandy Ricardo and<br />
Tammy McCorkle with Bob Ranes.<br />
<strong>of</strong> the tunnel, even with all that,” Bob says.<br />
“MaryAnn said, ‘No.’ She just wanted to<br />
live out the time she had left.”<br />
Bob got around with a walker and a<br />
scooter. His doctor worried that he<br />
wouldn’t be able to care for MaryAnn<br />
by himself.<br />
“But I convinced him I could do it,”<br />
Bob says.<br />
“I was just standing there, blinking my<br />
teary eyes, and they called all the shots,<br />
gently and sweetly. I don’t know what I<br />
would have done without them.”<br />
-Bob Ranes<br />
And he did, for a while, until MaryAnn<br />
could no longer make it from the recliner<br />
(where she preferred to sleep) to the<br />
bathroom. Bob called his doctor and said,<br />
“I can’t do it anymore.”<br />
Within 20 minutes, a <strong>Hospice</strong> <strong>of</strong> <strong>Emanuel</strong><br />
nurse showed up at his door.<br />
“She was like some kind <strong>of</strong> angel.” Bob<br />
said. “I knew she couldn’t make MaryAnn<br />
well, but she could make her comfortable.”<br />
By the end <strong>of</strong> that day, <strong>Hospice</strong> <strong>of</strong><br />
<strong>Emanuel</strong> had a hospital bed set up in the<br />
Ranes’ living room. They helped arrange<br />
for 12-hour, and then 24-hour, home<br />
health care.<br />
“That allowed me to get some sleep,” Bob<br />
says. “Not much, but some. So I was able<br />
to stay healthy.”<br />
<strong>Hospice</strong> <strong>of</strong> <strong>Emanuel</strong> staff did what they<br />
always do: Whatever needed to be done.<br />
They helped manage MaryAnn’s pain.<br />
They answered questions – not over the<br />
phone but in person. They showed up and<br />
helped the couple prepare for and understand<br />
what would come next.<br />
Bob woke up fairly rested on the morning<br />
<strong>of</strong> December 13, 2007. As always, he<br />
made his way down the hall to MaryAnn’s<br />
bed, took her hand, kissed her fingers and<br />
said, “Good morning, sweetheart.”<br />
MaryAnn was just barely awake. Bob<br />
went to the kitchen and shared a cup <strong>of</strong><br />
c<strong>of</strong>fee with the home health care nurse.<br />
The nurse went to check on MaryAnn a<br />
few minutes later. She returned in tears.<br />
MaryAnn had passed away.<br />
“I called <strong>Hospice</strong> immediately,” Bob says.<br />
“They were here in 12 minutes. And they<br />
did everything. They called the funeral<br />
home, they stripped the bed. I was just<br />
standing there, blinking my teary eyes,<br />
and they called all the shots, gently and<br />
sweetly. I don’t know what I would have<br />
done without them.”<br />
That’s the line you hear over and over<br />
when people talk <strong>of</strong> their <strong>Hospice</strong> <strong>of</strong><br />
<strong>Emanuel</strong> experience. Nancy Santos lost<br />
her husband, Melvin, on April 4, 2007.<br />
She says <strong>Hospice</strong> helped her before,<br />
during and after.<br />
“They came out four months before my<br />
husband died and took a huge burden <strong>of</strong>f<br />
my shoulders,” Nancy says. “They were<br />
such a comfort. They helped us through the<br />
process, step by step.”<br />
Melvin was well until the last week <strong>of</strong> his<br />
life, Nancy says.<br />
“And he was never in horrible pain,”<br />
she says. “They were so good about<br />
managing his pain.”<br />
Scott Atherton says <strong>Hospice</strong> <strong>of</strong> <strong>Emanuel</strong><br />
helped his mother, Dorothy Atherton,<br />
through her final months <strong>of</strong> life.<br />
“You should have seen her face when<br />
they arrived at her home to sing Christmas<br />
carols,” Scott says. “It made her feel so<br />
special. They were so attentive to all <strong>of</strong> us,<br />
when she was feeling badly and when<br />
she was feeling well.”<br />
That’s exactly the care Dr. MacLaren wants<br />
<strong>Hospice</strong> <strong>of</strong> <strong>Emanuel</strong> to provide.<br />
“Death is a part <strong>of</strong> life,” Dr. MacLaren<br />
says. “We need to do all we can do to<br />
ensure our patients live their fullest lives,<br />
right to the very end.”<br />
For more information about <strong>Hospice</strong> <strong>of</strong><br />
<strong>Emanuel</strong>, call (209) 664-2550.