- Page 1 and 2: METHODS IN MOLECULAR BIOLOGY 333 T
- Page 3 and 4: M E T H O D S I N M O L E C U L A R
- Page 5 and 6: © 2006 Humana Press Inc. 999 River
- Page 8 and 9: Contents Preface ..................
- Page 10 and 11: Contributors PAUL J. R. BARTON •
- Page 12 and 13: Current Status of Renal Transplanta
- Page 14 and 15: Current Status of Renal Transplanta
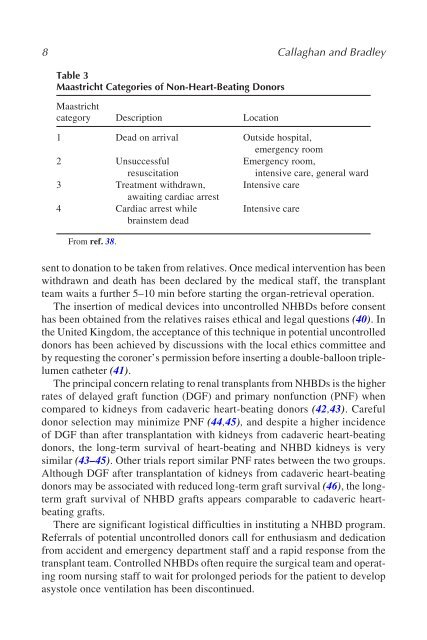
- Page 16 and 17: Current Status of Renal Transplanta
- Page 20 and 21: Current Status of Renal Transplanta
- Page 22 and 23: Current Status of Renal Transplanta
- Page 24 and 25: Current Status of Renal Transplanta
- Page 26 and 27: Current Status of Renal Transplanta
- Page 28 and 29: Current Status of Renal Transplanta
- Page 30 and 31: Current Status of Renal Transplanta
- Page 32 and 33: Current Status of Renal Transplanta
- Page 34 and 35: Current Status of Renal Transplanta
- Page 36 and 37: Current Status of Renal Transplanta
- Page 38: Current Status of Renal Transplanta
- Page 41 and 42: METHODS IN MOLECULAR BIOLOGY 333 T
- Page 43 and 44: 30 Friend and Imber meaningful surv
- Page 45 and 46: 32 Friend and Imber the most urgent
- Page 47 and 48: 34 Friend and Imber ent population
- Page 49 and 50: 36 Friend and Imber inotrope use, c
- Page 51 and 52: 38 Friend and Imber very experience
- Page 53 and 54: 40 Friend and Imber 14. Auxiliary L
- Page 55 and 56: 42 Friend and Imber subsequent isol
- Page 57 and 58: 44 Friend and Imber 21. Heffron, T.
- Page 59 and 60: 46 Friend and Imber 53. Saudubray,
- Page 61 and 62: 48 Lakey et al. There are an estima
- Page 63 and 64: 50 Lakey et al. diabetic to burn su
- Page 65 and 66: 52 Lakey et al. ber 31, 2000, less
- Page 67 and 68: 54 Lakey et al. Fig. 1. Schematic v
- Page 69 and 70:
56 Lakey et al. Table 1 Effect of I
- Page 71 and 72:
58 Lakey et al. from suitable donor
- Page 73 and 74:
60 Lakey et al. mined by high-perfo
- Page 75 and 76:
62 Lakey et al. Fig. 3. (A) Mean po
- Page 77 and 78:
64 Lakey et al. Fig. 5. HbA1c at 3-
- Page 79 and 80:
66 Lakey et al. All patients enjoy
- Page 81 and 82:
68 Lakey et al. 6. Sirolimus-based
- Page 83 and 84:
70 Lakey et al. Fig. 7. Two-layer (
- Page 85 and 86:
72 Table 2 Human Islet Transplantat
- Page 87 and 88:
74 Lakey et al. 3.4. Single-Donor I
- Page 89 and 90:
76 Lakey et al. difficult to isolat
- Page 91 and 92:
78 Lakey et al. 4.2. Islet Transpla
- Page 93 and 94:
80 Lakey et al. Table 3 Major Targe
- Page 95 and 96:
82 Lakey et al. CD40L (anti-CD154)
- Page 97 and 98:
84 Lakey et al. as kidney, heart, o
- Page 99 and 100:
86 Lakey et al. 14. Despres, J. P.,
- Page 101 and 102:
88 Lakey et al. tion despite a weak
- Page 103 and 104:
90 Lakey et al. 77. Maffi, P., Bert
- Page 105 and 106:
92 Lakey et al. 108. Idezuki, Y., G
- Page 107 and 108:
94 Lakey et al. 138. http://www.imm
- Page 109 and 110:
96 Lakey et al. tory reaction trigg
- Page 111 and 112:
98 Lakey et al. 198. O’Neil, J. J
- Page 113 and 114:
100 Lakey et al. 232. Delves, P. J.
- Page 115 and 116:
102 Lakey et al. 259. Grewal, I. S.
- Page 118 and 119:
Status of Lung Transplantation 105
- Page 120 and 121:
Status of Lung Transplantation 107
- Page 122 and 123:
Status of Lung Transplantation 109
- Page 124 and 125:
Status of Lung Transplantation 111
- Page 126 and 127:
Status of Lung Transplantation 113
- Page 128 and 129:
Status of Lung Transplantation 115
- Page 130 and 131:
Status of Lung Transplantation 117
- Page 132 and 133:
Status of Lung Transplantation 119
- Page 134 and 135:
Status of Lung Transplantation 121
- Page 136 and 137:
Status of Lung Transplantation 123
- Page 138 and 139:
Status of Lung Transplantation 125
- Page 140 and 141:
Status of Lung Transplantation 127
- Page 142 and 143:
Status of Lung Transplantation 129
- Page 144 and 145:
Chronic Rejection in the Heart 131
- Page 146 and 147:
Chronic Rejection in the Heart 133
- Page 148 and 149:
Chronic Rejection in the Heart 135
- Page 150 and 151:
Chronic Rejection in the Heart 137
- Page 152 and 153:
Chronic Rejection in the Heart 139
- Page 154 and 155:
Chronic Rejection in the Heart 141
- Page 156 and 157:
Chronic Rejection in the Heart 143
- Page 158 and 159:
Direct and Indirect Allorecognition
- Page 160 and 161:
Direct and Indirect Allorecognition
- Page 162 and 163:
Direct and Indirect Allorecognition
- Page 164 and 165:
Direct and Indirect Allorecognition
- Page 166 and 167:
Direct and Indirect Allorecognition
- Page 168 and 169:
Direct and Indirect Allorecognition
- Page 170 and 171:
HLA Typing and Organ Transplantatio
- Page 172 and 173:
HLA Typing and Organ Transplantatio
- Page 174 and 175:
HLA Typing and Organ Transplantatio
- Page 176 and 177:
HLA Typing and Organ Transplantatio
- Page 178 and 179:
HLA Typing and Organ Transplantatio
- Page 180 and 181:
HLA Typing and Organ Transplantatio
- Page 182 and 183:
HLA Typing and Organ Transplantatio
- Page 184 and 185:
HLA Typing and Organ Transplantatio
- Page 186 and 187:
HLA Typing and Organ Transplantatio
- Page 188 and 189:
Gene Transfer to Solid Organs 175 8
- Page 190 and 191:
Gene Transfer to Solid Organs 177 t
- Page 192 and 193:
Gene Transfer to Solid Organs 179 5
- Page 194 and 195:
Gene Transfer to Solid Organs 181
- Page 196 and 197:
183 Adenovirs (Ad) Nonenveloped vir
- Page 198 and 199:
Gene Transfer to Solid Organs 185 t
- Page 200 and 201:
Gene Transfer to Solid Organs 187 A
- Page 202 and 203:
Gene Transfer to Solid Organs 189 c
- Page 204 and 205:
Gene Transfer to Solid Organs 191 2
- Page 206 and 207:
Gene Transfer to Solid Organs 193 5
- Page 208 and 209:
Gene Transfer to Solid Organs 195 8
- Page 210 and 211:
Gene Transfer to Solid Organs 197 1
- Page 212 and 213:
Gene Transfer to Solid Organs 199 1
- Page 214 and 215:
202 Collins Table 1 Advantages and
- Page 216 and 217:
204 Collins The advantage of these
- Page 218 and 219:
206 Collins have used liposomal del
- Page 220 and 221:
208 Table 2 Ligands Used for Recept
- Page 222 and 223:
210 Collins It must not be forgotte
- Page 224 and 225:
212 Collins Fig. 3. Receptor-mediat
- Page 226 and 227:
214 Collins Receptor-mediated polyl
- Page 228 and 229:
216 Collins there are, to date, mor
- Page 230 and 231:
218 Collins 29. Niculescu-Duvaz, D.
- Page 232 and 233:
220 Collins 59. Wolfert, M. A. and
- Page 234 and 235:
222 Collins 91. Simoes, S., Slepush
- Page 236 and 237:
224 Collins 122. Hart, S. L., Harbo
- Page 239 and 240:
Antibody Relevance After Transplant
- Page 241 and 242:
Antibody Relevance After Transplant
- Page 243 and 244:
Antibody Relevance After Transplant
- Page 245 and 246:
Antibody Relevance After Transplant
- Page 247 and 248:
Antibody Relevance After Transplant
- Page 249 and 250:
Antibody Relevance After Transplant
- Page 251 and 252:
Antibody Relevance After Transplant
- Page 253 and 254:
Antibody Relevance After Transplant
- Page 255 and 256:
Antibody Relevance After Transplant
- Page 257:
Antibody Relevance After Transplant
- Page 260 and 261:
248 Graca and Waldmann 2. The Use o
- Page 262 and 263:
250 Graca and Waldmann Fig. 1. Indu
- Page 264 and 265:
252 Graca and Waldmann Despite this
- Page 266 and 267:
254 Graca and Waldmann transforming
- Page 268 and 269:
256 Graca and Waldmann The role of
- Page 270 and 271:
258 Graca and Waldmann Fig. 5. A re
- Page 272 and 273:
260 Graca and Waldmann 4. Kahan, B.
- Page 274 and 275:
262 Graca and Waldmann 35. Powrie,
- Page 276 and 277:
264 Graca and Waldmann 67. Annacker
- Page 278 and 279:
266 Graca and Waldmann 96. Bommired
- Page 280 and 281:
Immune Monitoring in Transplantatio
- Page 282 and 283:
Immune Monitoring in Transplantatio
- Page 284 and 285:
Immune Monitoring in Transplantatio
- Page 286 and 287:
Immune Monitoring in Transplantatio
- Page 288 and 289:
Immune Monitoring in Transplantatio
- Page 290 and 291:
Immune Monitoring in Transplantatio
- Page 292 and 293:
Immune Monitoring in Transplantatio
- Page 294 and 295:
283 Table 1 Current and Potential F
- Page 296 and 297:
Immune Monitoring in Transplantatio
- Page 298 and 299:
Immune Monitoring in Transplantatio
- Page 300 and 301:
Immune Monitoring in Transplantatio
- Page 302 and 303:
Proteomics and Laser Microdissectio
- Page 304 and 305:
Proteomics and Laser Microdissectio
- Page 306 and 307:
Proteomics and Laser Microdissectio
- Page 308 and 309:
Proteomics and Laser Microdissectio
- Page 310 and 311:
Proteomics and Laser Microdissectio
- Page 312 and 313:
Proteomics and Laser Microdissectio
- Page 314 and 315:
Proteomics and Laser Microdissectio
- Page 316 and 317:
Real-Time PCR 305 14 Real-Time Quan
- Page 318 and 319:
Real-Time PCR 307 Table 1 Real-Time
- Page 320 and 321:
Real-Time PCR 309 Fig. 2. Determina
- Page 322 and 323:
Real-Time PCR 311 such as Applied B
- Page 324 and 325:
Real-Time PCR 313 Table 2 Compariso
- Page 326 and 327:
315 Fig. 4. Quantification of RNA u
- Page 328 and 329:
Real-Time PCR 317 correlate directl
- Page 330 and 331:
319 Table 4 Common Internal Control
- Page 332 and 333:
321 Table 5 Examples of Single-Nucl
- Page 334 and 335:
Real-Time PCR 323 3.2. Real-Time PC
- Page 336 and 337:
Real-Time PCR 325 3.3.2. Sources of
- Page 338 and 339:
Real-Time PCR 327 9. Barton, P. J.
- Page 340 and 341:
Real-Time PCR 329 40. Primer expres
- Page 342 and 343:
Organ Preservation 331 15 Organ Pre
- Page 344 and 345:
Organ Preservation 333 2. Managemen
- Page 346 and 347:
Organ Preservation 335 tal observat
- Page 348 and 349:
Organ Preservation 337 donors, depe
- Page 350 and 351:
Organ Preservation 339 Table 1 Lung
- Page 352 and 353:
Organ Preservation 341 obtained wit
- Page 354 and 355:
Organ Preservation 343 Fig. 2. Acti
- Page 356 and 357:
Organ Preservation 345 Fig. 3. Outl
- Page 358 and 359:
Organ Preservation 347 and related
- Page 360 and 361:
Organ Preservation 349 mic, ischemi
- Page 362 and 363:
Organ Preservation 351 While these
- Page 364 and 365:
Organ Preservation 353 experimental
- Page 366 and 367:
Organ Preservation 355 with inhaled
- Page 368 and 369:
Organ Preservation 357 cellular sol
- Page 370 and 371:
Organ Preservation 359 4. Rosengard
- Page 372 and 373:
Organ Preservation 361 35. Powner,
- Page 374 and 375:
Organ Preservation 363 64. Hendry,
- Page 376 and 377:
Organ Preservation 365 factor-media
- Page 378 and 379:
Organ Preservation 367 120. Bonser,
- Page 380 and 381:
Organ Preservation 369 150. Macdona
- Page 382 and 383:
Organ Preservation 371 180. Carbogn
- Page 384:
209. Szabo, G., Soos, P., Bahrle, S
- Page 387 and 388:
376 Hopkins the extent of cold isch
- Page 389 and 390:
378 Hopkins or sequential administr
- Page 391 and 392:
380 Hopkins Table 2 Current Availab
- Page 393 and 394:
382 Hopkins 2. Renal failure: acute
- Page 395 and 396:
384 Table 4 Comparison of Azathiopr
- Page 397 and 398:
386 Hopkins Table 6 Side-Effect Pro
- Page 399 and 400:
388 Hopkins baseline immunosuppress
- Page 401 and 402:
390 Hopkins supplement to maintenan
- Page 403 and 404:
392 Hopkins 3. Kauppinen, H., Soots
- Page 405 and 406:
394 Hopkins uline versus no inducti
- Page 407 and 408:
396 Hopkins 62. Mycophenolate Mofet
- Page 409 and 410:
398 Hopkins 89. Mentzer, R. M., Jah
- Page 412 and 413:
Experimental Models of Graft Arteri
- Page 414 and 415:
Experimental Models of Graft Arteri
- Page 416 and 417:
405 Fig. 1. Variation in GA severit
- Page 418 and 419:
Experimental Models of Graft Arteri
- Page 420 and 421:
Experimental Models of Graft Arteri
- Page 422 and 423:
Experimental Models of Graft Arteri
- Page 424 and 425:
Experimental Models of Graft Arteri
- Page 426 and 427:
Experimental Models of Graft Arteri
- Page 428 and 429:
Experimental Models of Graft Arteri
- Page 430 and 431:
Experimental Models of Graft Arteri
- Page 432 and 433:
Experimental Models of Graft Arteri
- Page 434:
Experimental Models of Graft Arteri










![SISTEM SENSORY [Compatibility Mode].pdf](https://img.yumpu.com/20667975/1/190x245/sistem-sensory-compatibility-modepdf.jpg?quality=85)





