- Page 1 and 2:
Textbook of Patient Safety and Clin
- Page 3 and 4:
Liam Donaldson • Walter Ricciardi
- Page 5 and 6:
Foreword As a member of the 17th le
- Page 7 and 8:
Preface Despite the extensive atten
- Page 9 and 10:
Acknowledgements The volume editors
- Page 11 and 12:
xii Contents 11 Adverse Event Inves
- Page 13 and 14:
Part I Introduction
- Page 15 and 16:
4 explain how to prepare and update
- Page 17 and 18:
6 considered preventable) [11]. Fur
- Page 19 and 20:
8 W. Ricciardi and F. Cascini the l
- Page 21 and 22:
10 W. Ricciardi and F. Cascini inte
- Page 23 and 24:
12 maximized or perhaps even realiz
- Page 25 and 26:
14 steps in obtaining, managing, an
- Page 27 and 28:
16 quality improvement methodologie
- Page 29 and 30:
18 99. Morciano C, et al. Policies
- Page 31 and 32:
20 Reason travelled the world makin
- Page 33 and 34:
22 For each hospital unit, other do
- Page 35 and 36:
24 As head of clinical risk managem
- Page 37 and 38:
26 R. Tartaglia Table 2.1 Differenc
- Page 39 and 40:
28 R. Tartaglia Open Access This ch
- Page 41 and 42:
30 otherwise efficient brains lead
- Page 43 and 44:
32 • A routine violation is basic
- Page 45 and 46:
34 Table 3.1 Framework of contribut
- Page 47 and 48:
36 H. Higham and C. Vincent The con
- Page 49 and 50:
38 H. Higham and C. Vincent recogni
- Page 51 and 52:
40 H. Higham and C. Vincent Table 3
- Page 53 and 54:
42 assessment and prevention was no
- Page 55 and 56:
44 of human error, 2nd: 1983: Bella
- Page 57 and 58:
46 ment of theories on how to deliv
- Page 59 and 60:
48 all times, not only when there i
- Page 61 and 62:
50 healthcare, pursued by enthusias
- Page 63 and 64:
52 15. National Academies of Scienc
- Page 65 and 66:
54 In this chapter, I will reflect
- Page 67 and 68:
56 hospital, there may be 50 indivi
- Page 69 and 70:
58 medicals, these are part of the
- Page 71 and 72:
60 facility and could therefore bec
- Page 73 and 74:
62 health. It is hoped that the Che
- Page 75 and 76:
64 Medication Without Harm, invites
- Page 77 and 78:
66 21. World Alliance for Patient S
- Page 79 and 80:
68 death of my late husband, Pat, f
- Page 81 and 82:
70 S. Sheridan et al. test. A separ
- Page 83 and 84:
72 enced some kind of harm due to h
- Page 85 and 86:
74 S. Sheridan et al. member of The
- Page 87 and 88:
76 6.7.1 Example: Canada 6.7.1.1 Wo
- Page 89 and 90:
78 All stakeholders must accept, va
- Page 91 and 92:
Human Factors and Ergonomics in Hea
- Page 93 and 94:
7 Human Factors and Ergonomics in H
- Page 95 and 96:
7 Human Factors and Ergonomics in H
- Page 97 and 98:
7 Human Factors and Ergonomics in H
- Page 99 and 100:
7 Human Factors and Ergonomics in H
- Page 101 and 102:
Patient Safety in the World Neelam
- Page 103 and 104:
8 Patient Safety in the World 95 8.
- Page 105 and 106:
8 Patient Safety in the World adopt
- Page 107 and 108:
Infection Prevention and Control An
- Page 109 and 110:
9 Infection Prevention and Control
- Page 111 and 112:
9 Infection Prevention and Control
- Page 113 and 114:
9 Infection Prevention and Control
- Page 115 and 116:
9 Infection Prevention and Control
- Page 117 and 118:
9 Infection Prevention and Control
- Page 119 and 120:
9 Infection Prevention and Control
- Page 121 and 122:
9 Infection Prevention and Control
- Page 123 and 124:
9 Infection Prevention and Control
- Page 125 and 126:
The Patient Journey Elena Beleffi,
- Page 127 and 128:
10 The Patient Journey 119 End of e
- Page 129 and 130:
10 The Patient Journey 121 Fig. 10.
- Page 131 and 132:
10 The Patient Journey advocates) i
- Page 133 and 134:
10 The Patient Journey Table 10.2 T
- Page 135 and 136:
10 The Patient Journey 7. Internati
- Page 137 and 138:
130 from these interactions that pe
- Page 139 and 140:
132 Data integration is certainly t
- Page 141 and 142:
134 organizational processes, such
- Page 143 and 144:
136 Table 11.3 Scheme of contributo
- Page 145 and 146:
138 tocol requires one or more exte
- Page 147 and 148:
140 system failure. Quantification
- Page 149 and 150:
142 8. Carayon P, editor. Handbook
- Page 151 and 152:
144 similar industries, in terms of
- Page 153 and 154:
146 (2002) argue is a more effectiv
- Page 155 and 156:
148 for research in patient safety
- Page 157 and 158:
150 hospital in Kenya with focus on
- Page 159 and 160:
152 Haines et al. (2002) proposed a
- Page 161 and 162:
154 G. Dagliana et al. Fast Track -
- Page 163 and 164:
156 G. Dagliana et al. 11. Jha AK,
- Page 165 and 166:
Part III Patient Safety in the Main
- Page 167 and 168:
162 development of new receptor ant
- Page 169 and 170:
164 Physician burnout and the psych
- Page 171 and 172:
166 S. Damiani et al. Fig. 13.1 In
- Page 173 and 174:
168 mortality and has rapidly becom
- Page 175 and 176:
170 ing to patient safety and share
- Page 177 and 178:
172 ability to cope with the workin
- Page 179 and 180:
174 2. Vlayen A, Verelst S, Bekkeri
- Page 181 and 182:
Safe Surgery Saves Lives Francesco
- Page 183 and 184:
14 Safe Surgery Saves Lives manner
- Page 185 and 186:
14 Safe Surgery Saves Lives not yet
- Page 187 and 188:
14 Safe Surgery Saves Lives In a su
- Page 189 and 190: 14 Safe Surgery Saves Lives 14.15.1
- Page 191 and 192: 14 Safe Surgery Saves Lives • Tea
- Page 193 and 194: Emergency Department Clinical Risk
- Page 195 and 196: 15 Emergency Department Clinical Ri
- Page 197 and 198: 15 Emergency Department Clinical Ri
- Page 199 and 200: 15 Emergency Department Clinical Ri
- Page 201 and 202: 15 Emergency Department Clinical Ri
- Page 203 and 204: 15 Emergency Department Clinical Ri
- Page 205 and 206: 15 Emergency Department Clinical Ri
- Page 207 and 208: 15 Emergency Department Clinical Ri
- Page 209 and 210: 206 • Pragmatic: in a healthcare
- Page 211 and 212: 208 Risks associated with pregravid
- Page 213 and 214: 210 Table 16.1 Common and Recurrent
- Page 215 and 216: 212 improved clinical surveillance
- Page 217 and 218: 214 (only IM wards or all medical w
- Page 219 and 220: 216 M. L. Regina et al. Table 17.1
- Page 221 and 222: 218 Table 17.2 Types and preventabi
- Page 223 and 224: 220 nicians were certain resulted w
- Page 225 and 226: 222 M. L. Regina et al. Table 17.5
- Page 227 and 228: 224 Table 17.6 “Debiasing questio
- Page 229 and 230: 226 in care. At a minimum, medicati
- Page 231 and 232: 228 cation rates there substantiall
- Page 233 and 234: 230 well-structured, concise, focus
- Page 235 and 236: 232 M. L. Regina et al. Fig. 17.3 W
- Page 237 and 238: 234 M. L. Regina et al. Table 17.12
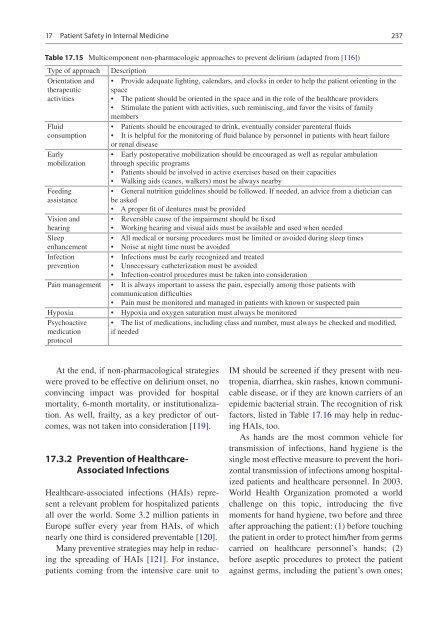
- Page 239: 236 Table 17.14 Risk factors for as
- Page 243 and 244: 240 In patients with kidney disease
- Page 245 and 246: 242 Table 17.19 Clinical response t
- Page 247 and 248: 244 stones. Giordano’s test posit
- Page 249 and 250: 246 in practice. Swiss Med Wkly. 20
- Page 251 and 252: 248 procedures done by general inte
- Page 253 and 254: 250 tion: a systematic review and m
- Page 255 and 256: 252 162. Improvement IfH. What is a
- Page 257 and 258: 254 and therapeutic strategies, all
- Page 259 and 260: 256 direct effect of radiotherapy o
- Page 261 and 262: 258 obtaining treatment consent and
- Page 263 and 264: 260 A. Marcolongo et al. Table 18.1
- Page 265 and 266: 262 A. Marcolongo et al. Toxicities
- Page 267 and 268: 264 nies that are aimed at building
- Page 269 and 270: 266 A. Marcolongo et al. tissues. B
- Page 271 and 272: 268 and breast cancer) and can be r
- Page 273 and 274: 270 happened during the first three
- Page 275 and 276: 272 40. World Health Organization (
- Page 277 and 278: Patient Safety in Orthopedics and T
- Page 279 and 280: 19 Patient Safety in Orthopedics an
- Page 281 and 282: 19 Patient Safety in Orthopedics an
- Page 283 and 284: 19 Patient Safety in Orthopedics an
- Page 285 and 286: 19 Patient Safety in Orthopedics an
- Page 287 and 288: 19 Patient Safety in Orthopedics an
- Page 289 and 290: Patient Safety and Risk Management
- Page 291 and 292:
20 Patient Safety and Risk Manageme
- Page 293 and 294:
20 Patient Safety and Risk Manageme
- Page 295 and 296:
20 Patient Safety and Risk Manageme
- Page 297 and 298:
20 Patient Safety and Risk Manageme
- Page 299 and 300:
20 Patient Safety and Risk Manageme
- Page 301 and 302:
Patient Safety in Pediatrics Sara A
- Page 303 and 304:
21 Patient Safety in Pediatrics eve
- Page 305 and 306:
21 Patient Safety in Pediatrics of
- Page 307 and 308:
21 Patient Safety in Pediatrics Cri
- Page 309 and 310:
21 Patient Safety in Pediatrics of
- Page 311 and 312:
Patient Safety in Radiology Mahdieh
- Page 313 and 314:
22 Patient Safety in Radiology The
- Page 315 and 316:
22 Patient Safety in Radiology indu
- Page 317 and 318:
22 Patient Safety in Radiology CA a
- Page 319 and 320:
22 Patient Safety in Radiology Refe
- Page 321 and 322:
Organ Donor Risk Stratification in
- Page 323 and 324:
23 Organ Donor Risk Stratification
- Page 325 and 326:
23 Organ Donor Risk Stratification
- Page 327 and 328:
326 M. Plebani et al. Fig. 24.1 The
- Page 329 and 330:
328 ical laboratory and the definit
- Page 331 and 332:
330 • Findings of external accred
- Page 333 and 334:
332 M. Plebani et al. Fig. 24.2 Mod
- Page 335 and 336:
334 laboratory medicine professiona
- Page 337 and 338:
336 (WHO) website on the incidence
- Page 339 and 340:
338 54. Magnezi R, Hemi A, Hemi R.
- Page 341 and 342:
340 In 2010 this condition represen
- Page 343 and 344:
342 which should be slightly smalle
- Page 345 and 346:
344 needed by the pulse waveform to
- Page 347 and 348:
346 washed properly prior to steril
- Page 349 and 350:
348 ocular reaction without infecti
- Page 351 and 352:
350 large retrospective cohort stud
- Page 353 and 354:
352 • Lack of appropriate skills.
- Page 355 and 356:
354 scription [126]. Furthermore, a
- Page 357 and 358:
356 time and knowledge to young doc
- Page 359 and 360:
358 48. Barry P, Gettinby G, Lees F
- Page 361 and 362:
360 implant versus intravitreal ant
- Page 363 and 364:
Part IV Healthcare Organization
- Page 365 and 366:
366 causes of safety incidents and
- Page 367 and 368:
368 • Human factors such as teamw
- Page 369 and 370:
370 access to the Emergency Room. F
- Page 371 and 372:
372 that many doctors simply choose
- Page 373 and 374:
374 E. Alti and A. Mereu Open Acces
- Page 375 and 376:
376 components (people, technology,
- Page 377 and 378:
378 J. Braithwaite et al. Hence, cl
- Page 379 and 380:
380 stakeholders to figure out how
- Page 381 and 382:
382 J. Braithwaite et al. Clinician
- Page 383 and 384:
384 27.5.3 Social Networks in a War
- Page 385 and 386:
386 J. Braithwaite et al. Fig. 27.9
- Page 387 and 388:
388 representations the essential l
- Page 389 and 390:
390 21. Pomare C, Churruca K, Ellis
- Page 391 and 392:
Measuring Clinical Workflow to Impr
- Page 393 and 394:
28 Measuring Clinical Workflow to I
- Page 395 and 396:
28 Measuring Clinical Workflow to I
- Page 397 and 398:
28 Measuring Clinical Workflow to I
- Page 399 and 400:
28 Measuring Clinical Workflow to I
- Page 401 and 402:
Shiftwork Organization Giovanni Cos
- Page 403 and 404:
29 Shiftwork Organization influenci
- Page 405 and 406:
29 Shiftwork Organization Many epid
- Page 407 and 408:
29 Shiftwork Organization quences o
- Page 409 and 410:
29 Shiftwork Organization in shift
- Page 411 and 412:
Non-technical Skills in Healthcare
- Page 413 and 414:
30 Non-technical Skills in Healthca
- Page 415 and 416:
30 Non-technical Skills in Healthca
- Page 417 and 418:
30 Non-technical Skills in Healthca
- Page 419 and 420:
30 Non-technical Skills in Healthca
- Page 421 and 422:
30 Non-technical Skills in Healthca
- Page 423 and 424:
30 Non-technical Skills in Healthca
- Page 425 and 426:
30 Non-technical Skills in Healthca
- Page 427 and 428:
30 Non-technical Skills in Healthca
- Page 429 and 430:
30 Non-technical Skills in Healthca
- Page 431 and 432:
30 Non-technical Skills in Healthca
- Page 433 and 434:
Medication Safety Hooi Cheng Soon,
- Page 435 and 436:
31 Medication Safety • Be familia
- Page 437 and 438:
31 Medication Safety 439 Table 31.1
- Page 439 and 440:
31 Medication Safety to be made bet
- Page 441 and 442:
31 Medication Safety medication reg
- Page 443 and 444:
31 Medication Safety and contexts,
- Page 445 and 446:
31 Medication Safety quently when m
- Page 447 and 448:
31 Medication Safety 31.5 Final Rec
- Page 449 and 450:
31 Medication Safety 451 ity and im
- Page 451 and 452:
31 Medication Safety 453 Open Acces
- Page 453 and 454:
456 studies in recent years have hi
- Page 455 and 456:
458 F. Ranzani and O. Parlangeli in
- Page 457 and 458:
460 Any difficulty encountered by t
- Page 459 and 460:
462 32.4.2 The Usability Assessment
- Page 461 and 462:
464 23. Parlangeli O, Mengoni G, Gu
- Page 463 and 464:
466 S. Ushiro et al. No-fault compe
- Page 465 and 466:
468 33.2 The Meaning of “No-Fault
- Page 467 and 468:
470 S. Ushiro et al. figure of 2.3
- Page 469 and 470:
472 S. Ushiro et al. Childbirth fac
- Page 471 and 472:
474 • When cerebral palsy is caus
- Page 473 and 474:
476 (c) (d) (e) (f) (g) (h) (i) (j)
- Page 475 and 476:
478 115 bpm to 80 bpm and complete
- Page 477 and 478:
480 • It is desirable that system
- Page 479 and 480:
482 cific monitoring procedures (1)
- Page 481 and 482:
484 Res. 2019;45(3):493-513. https:
- Page 483 and 484:
486 19. In the most severe cases, t
- Page 485 and 486:
488 Phases 3 and 4, strong emphasis
- Page 487 and 488:
490 Phases 5 and 6 focus is on the
- Page 489 and 490:
492 during a pandemic to promote tr
- Page 491 and 492:
494 M. Tanzini et al. the mother, p
- Page 493:
496 All four abilities are necessar