use of tumor markers in testicular, prostate, colorectal, breast, and ...
use of tumor markers in testicular, prostate, colorectal, breast, and ...
use of tumor markers in testicular, prostate, colorectal, breast, and ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
6 Use <strong>of</strong> Tumor Markers <strong>in</strong> Testicular, Prostate, Colorectal, Breast, <strong>and</strong> Ovarian Cancers<br />
TUMOR MARKERS IN TESTICULAR<br />
CANCER: NACB RECOMMENDATIONS<br />
Table 2 presents a summary <strong>of</strong> recommendations from representative<br />
guidel<strong>in</strong>es published on the <strong>use</strong> <strong>of</strong> <strong>tumor</strong> <strong>markers</strong> <strong>in</strong> <strong>testicular</strong><br />
cancer. This Table also summarizes the NACB guidel<strong>in</strong>es<br />
for the <strong>use</strong> <strong>of</strong> <strong>markers</strong> <strong>in</strong> this malignancy. A number <strong>of</strong> groups<br />
have made detailed recommendations regard<strong>in</strong>g the management<br />
<strong>of</strong> <strong>testicular</strong> cancer (13-21), with some <strong>of</strong> those relat<strong>in</strong>g to <strong>tumor</strong><br />
marker <strong>use</strong> summarized <strong>in</strong> Table 3. Table 4 summarizes the<br />
prognostic significance <strong>of</strong> serum <strong>tumor</strong> <strong>markers</strong> <strong>in</strong> metastatic<br />
<strong>testicular</strong> cancer, accord<strong>in</strong>g to the consensus statement <strong>of</strong> the<br />
International Germ Cell Consensus Classification (IGCCC),<br />
which rema<strong>in</strong>s the cornerstone for diagnosis <strong>and</strong> treatment <strong>of</strong><br />
<strong>testicular</strong> germ cell <strong>tumor</strong>s. Below, we briefly review the histological<br />
types <strong>of</strong> <strong>testicular</strong> cancer <strong>and</strong> present a more detailed discussion<br />
on the <strong>markers</strong> listed <strong>in</strong> these Tables.<br />
HISTOLOGICAL TYPES OF TESTICULAR<br />
CANCER<br />
In the most recent WHO-Most<strong>of</strong>i classification (8, 22), <strong>testicular</strong><br />
cancers are subdivided <strong>in</strong>to two major types, sem<strong>in</strong>omas <strong>and</strong><br />
NSGCT, which differ with respect to both marker expression <strong>and</strong><br />
treatment. The <strong>in</strong>cidence <strong>of</strong> sem<strong>in</strong>oma peaks <strong>in</strong> the fourth decade<br />
<strong>of</strong> life <strong>and</strong> that <strong>of</strong> NSGCT <strong>in</strong> the third. Sem<strong>in</strong>omas can be either<br />
pure sem<strong>in</strong>omas or the rare spermatocytic sem<strong>in</strong>omas that occur<br />
<strong>in</strong> older age groups. Most NSGCTs are a mixture <strong>of</strong> histological<br />
types (ie, embryonal carc<strong>in</strong>omas, choriocarc<strong>in</strong>omas, teratomas,<br />
<strong>and</strong> yolk sac <strong>tumor</strong>s). About 10% to 20% <strong>of</strong> the nonsem<strong>in</strong>omas<br />
also conta<strong>in</strong> a sem<strong>in</strong>oma component. These are classified as comb<strong>in</strong>ed<br />
<strong>tumor</strong>s accord<strong>in</strong>g to the British classification (23), but as<br />
nonsem<strong>in</strong>omas accord<strong>in</strong>g to the WHO classification system (22).<br />
Teratomas are further subdivided as mature or immature. Somatic<br />
cancers <strong>of</strong> various types occasionally develop from a teratoma<br />
<strong>and</strong> are classified as non-germ cell malignancies. Metastases may<br />
conta<strong>in</strong> any component occurr<strong>in</strong>g <strong>in</strong> the primary <strong>tumor</strong> <strong>and</strong> occasionally<br />
components not detected <strong>in</strong> the primary <strong>tumor</strong> (22).<br />
Fewer than 10% <strong>of</strong> NSGCT conta<strong>in</strong> a s<strong>in</strong>gle tissue type <strong>and</strong> all<br />
histological types <strong>of</strong> tissue should be described (24).<br />
The precursor lesion <strong>of</strong> <strong>testicular</strong> sem<strong>in</strong>omas <strong>and</strong> nonsem<strong>in</strong>omas<br />
is carc<strong>in</strong>oma <strong>in</strong> situ (CIS) (25), also referred to as<br />
<strong>in</strong>tratubular germ cell neoplasia unclassified (ITGCNU) <strong>and</strong> <strong>testicular</strong><br />
<strong>in</strong>tratubular neoplasia (TIN). CIS cells are found with<strong>in</strong><br />
the spermatogonial niche <strong>of</strong> the sem<strong>in</strong>iferous tubule <strong>in</strong> the adult<br />
testis <strong>in</strong> close proximity to the Sertoli cells, the nurs<strong>in</strong>g cells <strong>of</strong><br />
spermatogenesis (26). The CIS cells can be detected <strong>in</strong> the adjacent<br />
parenchyma <strong>of</strong> most <strong>in</strong>vasive <strong>tumor</strong>s, <strong>and</strong> are more frequently<br />
associated with NSGCTs than with sem<strong>in</strong>omas (27).<br />
ITGCNU is considered to represent the pre-malignant counterpart<br />
<strong>of</strong> an embryonic germ cell, most likely a primordial germ<br />
cell or gonocyte. This theory is supported by multiple f<strong>in</strong>d<strong>in</strong>gs,<br />
<strong>in</strong>clud<strong>in</strong>g epidemiology, morphology, immunohistochemistry,<br />
<strong>and</strong> molecular characterization (28, 29).<br />
Recent data <strong>in</strong>dicate that <strong>in</strong>fertile men with bilateral<br />
microlithiasis have an <strong>in</strong>creased risk (up to 20%) <strong>of</strong> develop<strong>in</strong>g<br />
<strong>testicular</strong> sem<strong>in</strong>omas <strong>and</strong> NSGCTs (30). Surgical biopsy to assess<br />
the presence <strong>of</strong> ITGCNU (31) is <strong>in</strong>dicated <strong>in</strong> this condition.<br />
TISSUE MARKERS FOR TESTICULAR<br />
CANCER<br />
Genetic Aberrations<br />
A ga<strong>in</strong> <strong>of</strong> 12p is observed <strong>in</strong> germ cell <strong>tumor</strong>s both <strong>of</strong> <strong>testicular</strong><br />
<strong>and</strong> extragonadal orig<strong>in</strong>. This <strong>in</strong>dicates that ga<strong>in</strong> <strong>of</strong> 12p<br />
sequences may be <strong>of</strong> crucial importance for the development<br />
<strong>of</strong> this cancer <strong>and</strong>, <strong>in</strong>deed, this f<strong>in</strong>d<strong>in</strong>g is <strong>use</strong>d to diagnose germ<br />
cell <strong>tumor</strong>s at extragonadal sites (32). However, the expression<br />
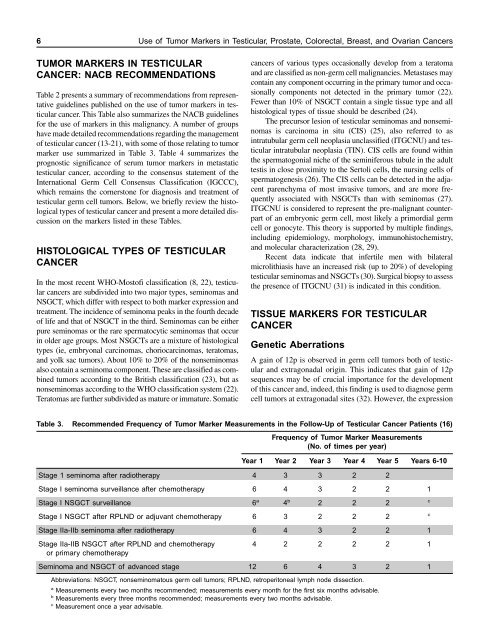
Table 3. Recommended Frequency <strong>of</strong> Tumor Marker Measurements <strong>in</strong> the Follow-Up <strong>of</strong> Testicular Cancer Patients (16)<br />
Frequency <strong>of</strong> Tumor Marker Measurements<br />
(No. <strong>of</strong> times per year)<br />
Year 1 Year 2 Year 3 Year 4 Year 5 Years 6-10<br />
Stage 1 sem<strong>in</strong>oma after radiotherapy 4 3 3 2 2<br />
Stage I sem<strong>in</strong>oma surveillance after chemotherapy 6 4 3 2 2 1<br />
Stage I NSGCT surveillance 6 a 4 b 2 2 2 c<br />
Stage I NSGCT after RPLND or adjuvant chemotherapy 6 3 2 2 2 c<br />
Stage IIa-IIb sem<strong>in</strong>oma after radiotherapy 6 4 3 2 2 1<br />
Stage IIa-IIB NSGCT after RPLND <strong>and</strong> chemotherapy 4 2 2 2 2 1<br />
or primary chemotherapy<br />
Sem<strong>in</strong>oma <strong>and</strong> NSGCT <strong>of</strong> advanced stage 12 6 4 3 2 1<br />
Abbreviations: NSGCT, nonsem<strong>in</strong>omatous germ cell <strong>tumor</strong>s; RPLND, retroperitoneal lymph node dissection.<br />
a Measurements every two months recommended; measurements every month for the first six months advisable.<br />
b Measurements every three months recommended; measurements every two months advisable.<br />
c Measurement once a year advisable.