web_vol47 4.pdf - International Hospital Federation
web_vol47 4.pdf - International Hospital Federation
web_vol47 4.pdf - International Hospital Federation
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
Policy: China<br />
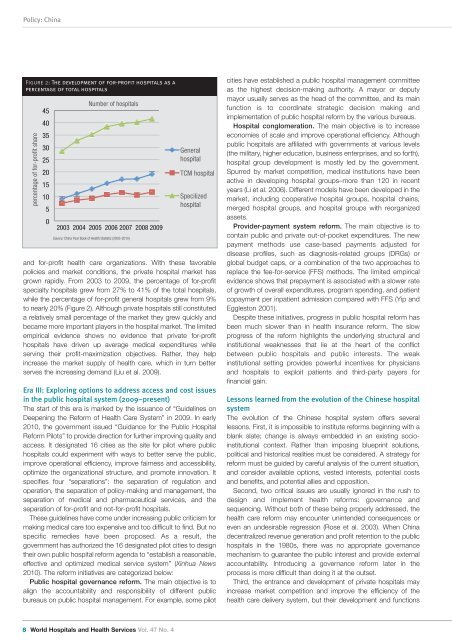
Figure 2: The development of for-profit hospitals as a<br />
percentage of total hospitals<br />
percentage of for-profit share<br />
45<br />
40<br />
35<br />
30<br />
25<br />
20<br />
15<br />
10<br />
5<br />
0<br />
Number of hospitals<br />
2003 2004 2005 2006 2007 2008 2009<br />
Source: China Year Book of Health Statistic (2003-2010)<br />
General<br />
hospital<br />
TCM hospital<br />
Specilized<br />
hospital<br />
and for-profit health care organizations. With these favorable<br />
policies and market conditions, the private hospital market has<br />
grown rapidly. From 2003 to 2009, the percentage of for-profit<br />
specialty hospitals grew from 27% to 41% of the total hospitals,<br />
while the percentage of for-profit general hospitals grew from 9%<br />
to nearly 20% (Figure 2). Although private hospitals still constituted<br />
a relatively small percentage of the market they grew quickly and<br />
became more important players in the hospital market. The limited<br />
empirical evidence shows no evidence that private for-profit<br />
hospitals have driven up average medical expenditures while<br />
serving their profit-maximization objectives. Rather, they help<br />
increase the market supply of health care, which in turn better<br />
serves the increasing demand (Liu et al. 2009).<br />
Era III: Exploring options to address access and cost issues<br />
in the public hospital system (2009–present)<br />
The start of this era is marked by the issuance of “Guidelines on<br />
Deepening the Reform of Health Care System” in 2009. In early<br />
2010, the government issued “Guidance for the Public <strong>Hospital</strong><br />
Reform Pilots” to provide direction for further improving quality and<br />
access. It designated 16 cities as the site for pilot where public<br />
hospitals could experiment with ways to better serve the public,<br />
improve operational efficiency, improve fairness and accessibility,<br />
optimize the organizational structure, and promote innovation. It<br />
specifies four “separations”: the separation of regulation and<br />
operation, the separation of policy-making and management, the<br />
separation of medical and pharmaceutical services, and the<br />
separation of for-profit and not-for-profit hospitals.<br />
These guidelines have come under increasing public criticism for<br />
making medical care too expensive and too difficult to find. But no<br />
specific remedies have been proposed. As a result, the<br />
government has authorized the 16 designated pilot cities to design<br />
their own public hospital reform agenda to “establish a reasonable,<br />
effective and optimized medical service system” (Xinhua News<br />
2010). The reform initiatives are categorized below:<br />
Public hospital governance reform. The main objective is to<br />
align the accountability and responsibility of different public<br />
bureaus on public hospital management. For example, some pilot<br />
cities have established a public hospital management committee<br />
as the highest decision-making authority. A mayor or deputy<br />
mayor usually serves as the head of the committee, and its main<br />
function is to coordinate strategic decision making and<br />
implementation of public hospital reform by the various bureaus.<br />
<strong>Hospital</strong> conglomeration. The main objective is to increase<br />
economies of scale and improve operational efficiency. Although<br />
public hospitals are affiliated with governments at various levels<br />
(the military, higher education, business enterprises, and so forth),<br />
hospital group development is mostly led by the government.<br />
Spurred by market competition, medical institutions have been<br />
active in developing hospital groups–more than 120 in recent<br />
years (Li et al. 2006). Different models have been developed in the<br />
market, including cooperative hospital groups, hospital chains,<br />
merged hospital groups, and hospital groups with reorganized<br />
assets.<br />
Provider-payment system reform. The main objective is to<br />
contain public and private out-of-pocket expenditures. The new<br />
payment methods use case-based payments adjusted for<br />
disease profiles, such as diagnosis-related groups (DRGs) or<br />
global budget caps, or a combination of the two approaches to<br />
replace the fee-for-service (FFS) methods. The limited empirical<br />
evidence shows that prepayment is associated with a slower rate<br />
of growth of overall expenditures, program spending, and patient<br />
copayment per inpatient admission compared with FFS (Yip and<br />
Eggleston 2001).<br />
Despite these initiatives, progress in public hospital reform has<br />
been much slower than in health insurance reform. The slow<br />
progress of the reform highlights the underlying structural and<br />
institutional weaknesses that lie at the heart of the conflict<br />
between public hospitals and public interests. The weak<br />
institutional setting provides powerful incentives for physicians<br />
and hospitals to exploit patients and third-party payers for<br />
financial gain.<br />
Lessons learned from the evolution of the Chinese hospital<br />
system<br />
The evolution of the Chinese hospital system offers several<br />
lessons. First, it is impossible to institute reforms beginning with a<br />
blank slate; change is always embedded in an existing socioinstitutional<br />
context. Rather than imposing blueprint solutions,<br />
political and historical realities must be considered. A strategy for<br />
reform must be guided by careful analysis of the current situation,<br />
and consider available options, vested interests, potential costs<br />
and benefits, and potential allies and opposition.<br />
Second, two critical issues are usually ignored in the rush to<br />
design and implement health reforms: governance and<br />
sequencing. Without both of these being properly addressed, the<br />
health care reform may encounter unintended consequences or<br />
even an undesirable regression (Rose et al. 2003). When China<br />
decentralized revenue generation and profit retention to the public<br />
hospitals in the 1980s, there was no appropriate governance<br />
mechanism to guarantee the public interest and provide external<br />
accountability. Introducing a governance reform later in the<br />
process is more difficult than doing it at the outset.<br />
Third, the entrance and development of private hospitals may<br />
increase market competition and improve the efficiency of the<br />
health care delivery system, but their development and functions<br />
8 World <strong>Hospital</strong>s and Health Services Vol. 47 No. 4