web_vol47 4.pdf - International Hospital Federation
web_vol47 4.pdf - International Hospital Federation
web_vol47 4.pdf - International Hospital Federation
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
Policy: China<br />
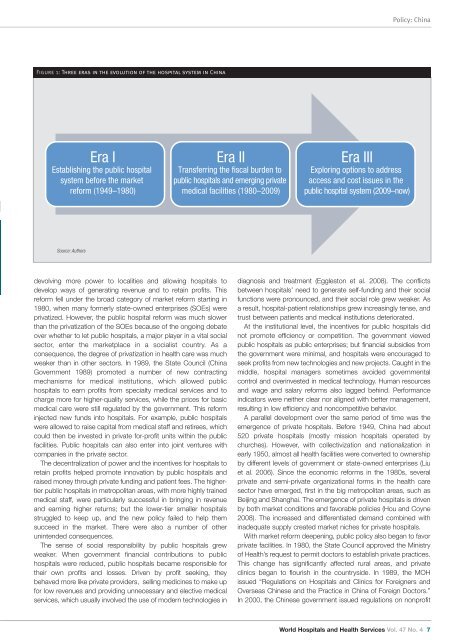
Figure 1: Three eras in the evolution of the hospital system in China<br />
Era I<br />
Establishing the public hospital<br />
system before the market<br />
reform (1949–1980)<br />
Era II<br />
Transferring the fiscal burden to<br />
public hospitals and emerging private<br />
medical facilities (1980–2009)<br />
Era III<br />
Exploring options to address<br />
access and cost issues in the<br />
public hospital system (2009–now)<br />
Source: Authors<br />
devolving more power to localities and allowing hospitals to<br />
develop ways of generating revenue and to retain profits. This<br />
reform fell under the broad category of market reform starting in<br />
1980, when many formerly state-owned enterprises (SOEs) were<br />
privatized. However, the public hospital reform was much slower<br />
than the privatization of the SOEs because of the ongoing debate<br />
over whether to let public hospitals, a major player in a vital social<br />
sector, enter the marketplace in a socialist country. As a<br />
consequence, the degree of privatization in health care was much<br />
weaker than in other sectors. In 1989, the State Council (China<br />
Government 1989) promoted a number of new contracting<br />
mechanisms for medical institutions, which allowed public<br />
hospitals to earn profits from specialty medical services and to<br />
charge more for higher-quality services, while the prices for basic<br />
medical care were still regulated by the government. This reform<br />
injected new funds into hospitals. For example, public hospitals<br />
were allowed to raise capital from medical staff and retirees, which<br />
could then be invested in private for-profit units within the public<br />
facilities. Public hospitals can also enter into joint ventures with<br />
companies in the private sector.<br />
The decentralization of power and the incentives for hospitals to<br />
retain profits helped promote innovation by public hospitals and<br />
raised money through private funding and patient fees. The highertier<br />
public hospitals in metropolitan areas, with more highly trained<br />
medical staff, were particularly successful in bringing in revenue<br />
and earning higher returns; but the lower-tier smaller hospitals<br />
struggled to keep up, and the new policy failed to help them<br />
succeed in the market. There were also a number of other<br />
unintended consequences.<br />
The sense of social responsibility by public hospitals grew<br />
weaker. When government financial contributions to public<br />
hospitals were reduced, public hospitals became responsible for<br />
their own profits and losses. Driven by profit seeking, they<br />
behaved more like private providers, selling medicines to make up<br />
for low revenues and providing unnecessary and elective medical<br />
services, which usually involved the use of modern technologies in<br />
diagnosis and treatment (Eggleston et al. 2008). The conflicts<br />
between hospitals’ need to generate self-funding and their social<br />
functions were pronounced, and their social role grew weaker. As<br />
a result, hospital-patient relationships grew increasingly tense, and<br />
trust between patients and medical institutions deteriorated.<br />
At the institutional level, the incentives for public hospitals did<br />
not promote efficiency or competition. The government viewed<br />
public hospitals as public enterprises; but financial subsidies from<br />
the government were minimal, and hospitals were encouraged to<br />
seek profits from new technologies and new projects. Caught in the<br />
middle, hospital managers sometimes avoided governmental<br />
control and overinvested in medical technology. Human resources<br />
and wage and salary reforms also lagged behind. Performance<br />
indicators were neither clear nor aligned with better management,<br />
resulting in low efficiency and noncompetitive behavior.<br />
A parallel development over the same period of time was the<br />
emergence of private hospitals. Before 1949, China had about<br />
520 private hospitals (mostly mission hospitals operated by<br />
churches). However, with collectivization and nationalization in<br />
early 1950, almost all health facilities were converted to ownership<br />
by different levels of government or state-owned enterprises (Liu<br />
et al. 2006). Since the economic reforms in the 1980s, several<br />
private and semi-private organizational forms in the health care<br />
sector have emerged, first in the big metropolitan areas, such as<br />
Beijing and Shanghai. The emergence of private hospitals is driven<br />
by both market conditions and favorable policies (Hou and Coyne<br />
2008). The increased and differentiated demand combined with<br />
inadequate supply created market niches for private hospitals.<br />
With market reform deepening, public policy also began to favor<br />
private facilities. In 1980, the State Council approved the Ministry<br />
of Health’s request to permit doctors to establish private practices.<br />
This change has significantly affected rural areas, and private<br />
clinics began to flourish in the countryside. In 1989, the MOH<br />
issued “Regulations on <strong>Hospital</strong>s and Clinics for Foreigners and<br />
Overseas Chinese and the Practice in China of Foreign Doctors.”<br />
In 2000, the Chinese government issued regulations on nonprofit<br />
World <strong>Hospital</strong>s and Health Services Vol. 47 No. 4 7