Full Clinical Guidelines - Community First Health Plans.
Full Clinical Guidelines - Community First Health Plans.
Full Clinical Guidelines - Community First Health Plans.
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
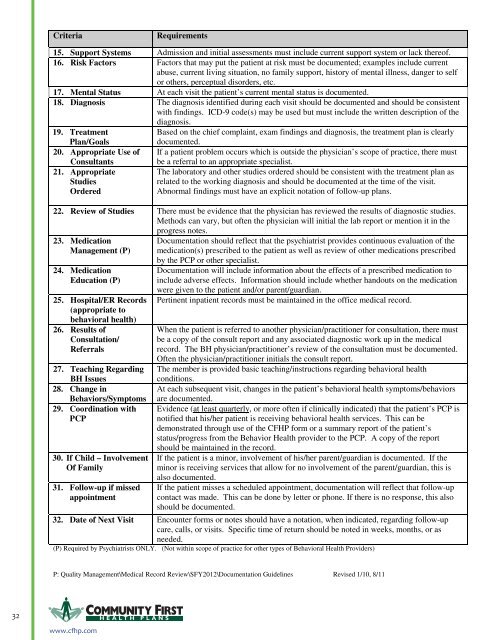
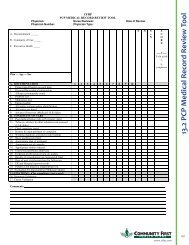
Criteria<br />
Requirements<br />
15. Support Systems Admission and initial assessments must include current support system or lack thereof.<br />
16. Risk Factors Factors that may put the patient at risk must be documented; examples include current<br />
abuse, current living situation, no family support, history of mental illness, danger to self<br />
or others, perceptual disorders, etc.<br />
17. Mental Status At each visit the patient’s current mental status is documented.<br />
18. Diagnosis The diagnosis identified during each visit should be documented and should be consistent<br />
with findings. ICD-9 code(s) may be used but must include the written description of the<br />
diagnosis.<br />
19. Treatment<br />
Based on the chief complaint, exam findings and diagnosis, the treatment plan is clearly<br />
Plan/Goals<br />
documented.<br />
20. Appropriate Use of If a patient problem occurs which is outside the physician’s scope of practice, there must<br />
Consultants<br />
21. Appropriate<br />
Studies<br />
Ordered<br />
be a referral to an appropriate specialist.<br />
The laboratory and other studies ordered should be consistent with the treatment plan as<br />
related to the working diagnosis and should be documented at the time of the visit.<br />
Abnormal findings must have an explicit notation of follow-up plans.<br />
22. Review of Studies There must be evidence that the physician has reviewed the results of diagnostic studies.<br />
Methods can vary, but often the physician will initial the lab report or mention it in the<br />
progress notes.<br />
23. Medication<br />
Management (P)<br />
24. Medication<br />
Education (P)<br />
25. Hospital/ER Records<br />
(appropriate to<br />
behavioral health)<br />
26. Results of<br />
Consultation/<br />
Referrals<br />
27. Teaching Regarding<br />
BH Issues<br />
28. Change in<br />
Behaviors/Symptoms<br />
29. Coordination with<br />
PCP<br />
30. If Child – Involvement<br />
Of Family<br />
31. Follow-up if missed<br />
appointment<br />
Documentation should reflect that the psychiatrist provides continuous evaluation of the<br />
medication(s) prescribed to the patient as well as review of other medications prescribed<br />
by the PCP or other specialist.<br />
Documentation will include information about the effects of a prescribed medication to<br />
include adverse effects. Information should include whether handouts on the medication<br />
were given to the patient and/or parent/guardian.<br />
Pertinent inpatient records must be maintained in the office medical record.<br />
When the patient is referred to another physician/practitioner for consultation, there must<br />
be a copy of the consult report and any associated diagnostic work up in the medical<br />
record. The BH physician/practitioner’s review of the consultation must be documented.<br />
Often the physician/practitioner initials the consult report.<br />
The member is provided basic teaching/instructions regarding behavioral health<br />
conditions.<br />
At each subsequent visit, changes in the patient’s behavioral health symptoms/behaviors<br />
are documented.<br />
Evidence (at least quarterly, or more often if clinically indicated) that the patient’s PCP is<br />
notified that his/her patient is receiving behavioral health services. This can be<br />
demonstrated through use of the CFHP form or a summary report of the patient’s<br />
status/progress from the Behavior <strong>Health</strong> provider to the PCP. A copy of the report<br />
should be maintained in the record.<br />
If the patient is a minor, involvement of his/her parent/guardian is documented. If the<br />
minor is receiving services that allow for no involvement of the parent/guardian, this is<br />
also documented.<br />
If the patient misses a scheduled appointment, documentation will reflect that follow-up<br />
contact was made. This can be done by letter or phone. If there is no response, this also<br />
should be documented.<br />
32. Date of Next Visit Encounter forms or notes should have a notation, when indicated, regarding follow-up<br />
care, calls, or visits. Specific time of return should be noted in weeks, months, or as<br />
needed.<br />
(P) Required by Psychiatrists ONLY. (Not within scope of practice for other types of Behavioral <strong>Health</strong> Providers)<br />
P: Quality Management\Medical Record Review\SFY2012\Documentation <strong>Guidelines</strong> Revised 1/10, 8/11<br />
32 H EALTH PLANS<br />
www.cfhp.com