Eyelid and Eyelid Margin disorders - Optometry Today
Eyelid and Eyelid Margin disorders - Optometry Today
Eyelid and Eyelid Margin disorders - Optometry Today
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
CET CONTINUING<br />
EDUCATION<br />
& TRAINING<br />
2 FREE CET POINTS<br />
OT CET content supports <strong>Optometry</strong> Giving Sight<br />
4 4 4 4<br />
Approved for: Optometrists AS Points SP Points IP Points “How do I complete this exam?” Go to www.optometrytoday.tv/FAQ<br />
34<br />
17/09/10 CET<br />
Management Options for UK Optometrists Part 3<br />
<strong>Eyelid</strong> <strong>and</strong> <strong>Eyelid</strong> <strong>Margin</strong><br />
Disorders<br />
Course code: C-14374 O/AS/SP/IP<br />
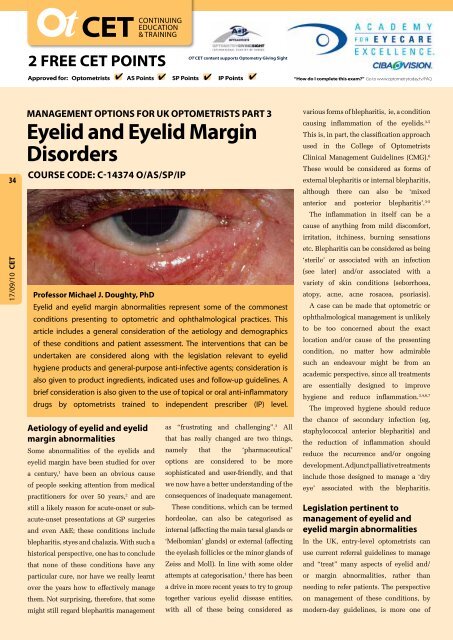
Professor Michael J. Doughty, PhD<br />
<strong>Eyelid</strong> <strong>and</strong> eyelid margin abnormalities represent some of the commonest<br />
conditions presenting to optometric <strong>and</strong> ophthalmological practices. This<br />
article includes a general consideration of the aetiology <strong>and</strong> demographics<br />
of these conditions <strong>and</strong> patient assessment. The interventions that can be<br />
undertaken are considered along with the legislation relevant to eyelid<br />
hygiene products <strong>and</strong> general-purpose anti-infective agents; consideration is<br />
also given to product ingredients, indicated uses <strong>and</strong> follow-up guidelines. A<br />
brief consideration is also given to the use of topical or oral anti-inflammatory<br />
drugs by optometrists trained to independent prescriber (IP) level.<br />
Aetiology of eyelid <strong>and</strong> eyelid<br />
margin abnormalities<br />
Some abnormalities of the eyelids <strong>and</strong><br />
eyelid margin have been studied for over<br />
a century, 1 have been an obvious cause<br />
of people seeking attention from medical<br />
practitioners for over 50 years, 2 <strong>and</strong> are<br />
still a likely reason for acute-onset or subacute-onset<br />
presentations at GP surgeries<br />
<strong>and</strong> even A&E; these conditions include<br />
blepharitis, styes <strong>and</strong> chalazia. With such a<br />
historical perspective, one has to conclude<br />
that none of these conditions have any<br />
particular cure, nor have we really learnt<br />
over the years how to effectively manage<br />
them. Not surprising, therefore, that some<br />
might still regard blepharitis management<br />
as “frustrating <strong>and</strong> challenging”. 3 All<br />
that has really changed are two things,<br />
namely that the ‘pharmaceutical’<br />
options are considered to be more<br />
sophisticated <strong>and</strong> user-friendly, <strong>and</strong> that<br />
we now have a better underst<strong>and</strong>ing of the<br />
consequences of inadequate management.<br />
These conditions, which can be termed<br />
hordeolae, can also be categorised as<br />
internal (affecting the main tarsal gl<strong>and</strong>s or<br />
‘Meibomian’ gl<strong>and</strong>s) or external (affecting<br />
the eyelash follicles or the minor gl<strong>and</strong>s of<br />
Zeiss <strong>and</strong> Moll). In line with some older<br />
attempts at categorisation, 1 there has been<br />
a drive in more recent years to try to group<br />
together various eyelid disease entities,<br />
with all of these being considered as<br />
various forms of blepharitis, ie, a condition<br />
causing inflammation of the eyelids. 3-5<br />
This is, in part, the classification approach<br />
used in the College of Optometrists<br />
Clinical Management Guidelines (CMG). 6<br />
These would be considered as forms of<br />
external blepharitis or internal blepharitis,<br />
although there can also be ‘mixed<br />
anterior <strong>and</strong> posterior blepharitis’. 3-5<br />
The inflammation in itself can be a<br />
cause of anything from mild discomfort,<br />
irritation, itchiness, burning sensations<br />
etc. Blepharitis can be considered as being<br />
‘sterile’ or associated with an infection<br />
(see later) <strong>and</strong>/or associated with a<br />
variety of skin conditions (seborrhoea,<br />
atopy, acne, acne rosacea, psoriasis).<br />
A case can be made that optometric or<br />
ophthalmological management is unlikely<br />
to be too concerned about the exact<br />
location <strong>and</strong>/or cause of the presenting<br />
condition, no matter how admirable<br />
such an endeavour might be from an<br />
academic perspective, since all treatments<br />
are essentially designed to improve<br />
hygiene <strong>and</strong> reduce inflammation. 3,4,6,7<br />
The improved hygiene should reduce<br />
the chance of secondary infection (eg,<br />
staphylococcal anterior blepharitis) <strong>and</strong><br />
the reduction of inflammation should<br />
reduce the recurrence <strong>and</strong>/or ongoing<br />
development. Adjunct palliative treatments<br />
include those designed to manage a ‘dry<br />
eye’ associated with the blepharitis.<br />
Legislation pertinent to<br />
management of eyelid <strong>and</strong><br />
eyelid margin abnormalities<br />
In the UK, entry-level optometrists can<br />
use current referral guidelines to manage<br />
<strong>and</strong> “treat” many aspects of eyelid <strong>and</strong>/<br />
or margin abnormalities, rather than<br />
needing to refer patients. The perspective<br />
on management of these conditions, by<br />
modern-day guidelines, is more one of
preventative care, ie, to reduce the<br />
chance of presenting acute- or sub-acute<br />
conditions requiring (from a patient’s<br />
perspective) urgent intervention.<br />
For the majority of commonly<br />
presenting conditions, management<br />
is with either non-medicinal products<br />
(CE marked, MD, SL, GSL) or products<br />
designated as P Medicines. All of these<br />
can be accessed (including by way of<br />
wholesale trading), supplied <strong>and</strong> sold<br />
on (at recommended retail price) to<br />
patients by all optometrists, as well<br />
as being available via the Internet. A<br />
few conditions may present as severe,<br />
as they have developed over many<br />
months prior to their being seen by the<br />
optometrist, <strong>and</strong> may respond to these<br />
types of treatments but really need more<br />
substantial medical (or even surgical)<br />
intervention. Notwithst<strong>and</strong>ing, the<br />
optometrist is in an excellent position to<br />
either co-manage these conditions with a<br />
patient’s GP (for access to certain topical<br />
or oral prescription-only medicines)<br />
or to facilitate assessment by an<br />
ophthalmologist at their local hospital.<br />
<strong>Eyelid</strong> margin hygiene<br />
products – options, use <strong>and</strong><br />
patient assessments<br />
The cause of many common eyelid <strong>and</strong><br />
margin problems is poor ocular hygiene.<br />
Whereas it was once acceptable to simply<br />
encourage facial <strong>and</strong> peri-ocular hygiene<br />
by use of a face flannel, energetically<br />
rubbed around <strong>and</strong> along the eyelids, such<br />
practices have all too often been resigned<br />
to history <strong>and</strong> alternatives introduced<br />
that focus (sic) on the site of the problem.<br />
Inspection of the eyelid marginal zone,<br />
unaided or especially by biomicroscopy,<br />
will reveal that it is rarely ‘squeaky’<br />
clean, but that particulate <strong>and</strong>/or oily<br />
debris can be present around the bases<br />
of the eyelashes <strong>and</strong> across the orifices<br />
of the adjacent Meibomian gl<strong>and</strong>s. Some<br />
oily material is normal <strong>and</strong> the amount<br />
of ‘meibum’ across the marginal zone<br />
can be assessed 5,8 using a meibometer<br />
(not commercially available in UK). 5 This<br />
narrow oily zone serves as a limiting barrier<br />
to the edge of the proximal tear meniscus<br />
(lacrimal lake) so as to stop tears normally<br />
overflowing across the eyelid margin. 5,9<br />
Its normal presence <strong>and</strong> function should<br />
be a reminder that excessive cleansing<br />
of the eyelid margin is not beneficial.<br />
However, excess non-cleansed meibum<br />
will mix with material that causes eyelid<br />
margin problems to slowly develop. Even<br />
for an eyelid that appears to be clean,<br />
impression cytology (where small filter<br />
disc is pressed against the eyelid marginal<br />
zone) can be used to show that this zone<br />
is covered with dead cells (Figure 1).<br />
Such cell material <strong>and</strong> debris, mixed with<br />
denatured meibum, can accumulate if not<br />
regularly removed. With each eyeblink,<br />
this material will likely be compressed<br />
against the bases of the eyelashes, congeal<br />
<strong>and</strong> dry out; the patient now presents<br />
with an obvious anterior blepharitis.<br />
<strong>Eyelid</strong> hygiene for blepharitis is<br />
important <strong>and</strong> has long been recognised<br />
with recommendations for application<br />
of natural plant extract (eg, chamomile)<br />
infusions, 1 or lotions of boric acid, 2 <strong>and</strong><br />
these can still be useful in certain cases,<br />
eg, for seborrhoeic blepharitis. 4 The use of<br />
sodium bicarbonate solutions also dates<br />
back at least 50 years, 1 <strong>and</strong> persist in some<br />
current day guidelines, 3,6 despite there<br />
being almost no information available as<br />
to what constitutes a satisfactory sodium<br />
bicarbonate solution for wiping the lid<br />
margins. More aggressive treatments have<br />
also included cleaning the eyelid margins<br />
with a 1:5000 solution of benzalkonium<br />
chloride, 10 noted for its ‘valuable<br />
detergent action’, or the application of<br />
a 2% solution of silver nitrate. 11 Where<br />
the blepharitis is associated with a scalp<br />
condition (eg, seborrhoeic blepharitis<br />
with uncomplicated chronic d<strong>and</strong>ruff),<br />
treatment of the hair <strong>and</strong> scalp is likely<br />
an essential part of management (eg, with<br />
daily use of shampoos containing anti-<br />
‘mould’/fungus/yeast compounds such<br />
as selenium sulphide or ketoconazole).<br />
The ocular use in the 1950’s of<br />
Selsun ophthalmic ointment (selenium<br />
sulphide 2.5% with 17% surfactant), 12<br />
is no longer recommended simply<br />
because it is too toxic for the delicate<br />
mucous membrane of the conjunctiva<br />
The once or twice-daily application<br />
of ophthalmic ointments containing 3%<br />
ammoniated mercury, 11 or 1% yellow<br />
mercuric oxide, 13 have also suffered the<br />
same fate after regulatory authorities<br />
decided that the possible adverse effects<br />
of chronic use of mercurial compounds<br />
outweighed the potential benefits.<br />
More recent times have seen the<br />
introduction of eyelid hygiene products,<br />
perhaps also more widely known by as<br />
Figure 1<br />
Material obtained by impression cytology from<br />
across the human eyelid margin zone stained with<br />
rose bengal (in vivo) <strong>and</strong> with Giemsa (ex vivo) to<br />
show large <strong>and</strong> sometimes anucleate squamous<br />
cells (some of which are stained crimson)<br />
35<br />
17/09/10 CET
CET CONTINUING<br />
EDUCATION<br />
& TRAINING<br />
2 FREE CET POINTS<br />
OT CET content supports <strong>Optometry</strong> Giving Sight<br />
4 4 4 4<br />
Approved for: Optometrists AS Points SP Points IP Points “How do I complete this exam?” Go to www.optometrytoday.tv/FAQ<br />
36<br />
17/09/10 CET<br />
‘lid scrubs’, <strong>and</strong> referred to as ‘dedicated<br />
cleaning solutions’ by the CMG. 6 A<br />
limited number of commercial products<br />
were introduced in North America in<br />
the 1980’s, <strong>and</strong> designed to replace the<br />
home remedy <strong>and</strong> unlabelled use of a<br />
proprietary baby shampoo for eyelid<br />
hygiene. 14 Notwithst<strong>and</strong>ing, the advice<br />
<strong>and</strong> recommendations for the use of baby<br />
shampoo have persisted well beyond<br />
the commercialisation of ‘lid scrubs’. 4,8,15<br />
Perhaps rather ironically, baby shampoo<br />
may be used as the referent treatment for<br />
evaluation of new products. 15,16 <strong>Eyelid</strong><br />
hygiene products have now become<br />
increasingly popular, with most finding<br />
their way into pharmacy product listings<br />
(eg, Chemist <strong>and</strong> Druggist Monthly)<br />
<strong>and</strong> even some over-the-counter (OTC)<br />
directories. These products are not<br />
routinely listed in a MIMS or BNF,<br />
because they are non-medicinal <strong>and</strong>,<br />
at least as yet, not considered true<br />
treatments for a common condition.<br />
The contemporary eyelid hygiene<br />
products are designed to gently cleanaway<br />
accumulated material, preferably<br />
before it gets too compacted <strong>and</strong> dried<br />
out. The ingredients include a range of<br />
mild surfactants (detergents) <strong>and</strong> soothing<br />
agents (Table 1). The overall formulations,<br />
drawing on experience with cosmetics, are<br />
generally designed to be hypoallergenic<br />
The synthetic surfactants are numerous<br />
(Table 1) <strong>and</strong> include a range of anionic<br />
<strong>and</strong>/or non-ionic surfactants with (tri)<br />
glyceride or glycol side chains that should<br />
help disperse oily materials. 14 Other<br />
ingredients are partly based on very old<br />
concepts where certain natural plant<br />
<strong>and</strong> flower extracts (eg, Hamamelis) are<br />
considered to have astringent properties<br />
as well as being generally soothing. Other<br />
natural ingredients provide soothing effects<br />
but may not provide any extra cleansing<br />
PRODUCT NAME SURFACTANT /<br />
CLEANSING<br />
INGREDIENTS<br />
LID CARE<br />
(PADS)<br />
SUPRANETTES<br />
(PADS)<br />
BLEPHACLEAN<br />
(PADS)<br />
BLEPHASOL<br />
(SOLUTION)<br />
STERILID<br />
(FOAM)<br />
(sodium)<br />
lauroamphodiacetate,<br />
(sodium) trideceth<br />
sulphate,<br />
hexylene glycol, propylene<br />
glycol, PEG-20 sorbitan<br />
monolaurate,<br />
PEG, polysorbate 80, citric<br />
acid<br />
PEG-8, poloxamer 184,<br />
polysorbate 20, capryloyl<br />
glycine,<br />
propylene glycol<br />
PEG-8, poloxamer 184,<br />
polysorbate 20, capryloyl<br />
glycine,<br />
propylene glycol, caprylic<br />
/ capric<br />
glycerides<br />
No sPEG-80, sorbitol<br />
laurate,<br />
Sodium<br />
lauroamphoacetate,<br />
sodium trieth sulphate,<br />
cocamidopropyl betaine,<br />
cocamidopropl PGdimonium<br />
NATURAL<br />
CLEANSING<br />
(ASTRINGENT),<br />
SOOTHING <strong>and</strong><br />
OTHER NATURAL<br />
INGREDIENTS<br />
none listed<br />
Hamamelis<br />
virginiana extracts, 1<br />
Calendula<br />
officianalis<br />
extracts, 2<br />
zinc sulphate,<br />
Centella Asiatica<br />
extracts, Iris<br />
florentina extracts,<br />
retinyl palmitate<br />
zinc sulphate,<br />
Centella Asiatica<br />
extracts, Iris<br />
florentina extracts,<br />
retinyl palmitate<br />
allantoin, linalool<br />
oils, tea tree oil,<br />
panthenol<br />
BUFFERING AGENTS<br />
STABILIZER<br />
PRESERVATIVES<br />
boric acid<br />
EDTA<br />
Phosphate<br />
methyl & propyl<br />
parabens 3<br />
phosphate<br />
phosphate<br />
boric acid<br />
EDTA<br />
sodium<br />
perborate 4<br />
Table 1<br />
<strong>Eyelid</strong> hygiene products <strong>and</strong> their ingredients. PEG = polyethylene glycol; 1 also known as witch hazel; 2 also<br />
known as pot marigold; 3 conventional preservatives; 4 oxidative preservative<br />
action, eg, Calendula extracts, allantoin,<br />
or natural oils. There is current interest<br />
in the (mild) antibacterial effects of fairly<br />
large amounts or concentrated solutions<br />
of tea tree oils, 16 or linalool oil mixtures. 17<br />
The extent of the blepharitis can be<br />
graded (eg, 0 to 4 scale) <strong>and</strong> the patient<br />
reassessed periodically (every few weeks)
to see how well they are managing with lid<br />
are excreted <strong>and</strong> so contribute to a normal<br />
hygiene. Management of blepharitis may<br />
thickness lipid layer on the tear film. 21<br />
take many weeks or months to resolve.<br />
An alternative to warm compresses is the<br />
The eyelid margin (at least by unaided<br />
vision or even close-up photography)<br />
may not appear that different before <strong>and</strong><br />
after routine preventative eyelid hygiene<br />
measures. 15,18 This is an important point,<br />
since by current day perspectives one<br />
should really not be able to see that the<br />
eyelid margins have been ‘scrubbed’<br />
ie, the cleansing, in itself, should not<br />
redden <strong>and</strong> inflame the lid margin!<br />
The way in which ‘lid scrubs’ are used<br />
is so important for effective management<br />
of chronic blepharitis, <strong>and</strong> it is perhaps<br />
unfortunate that we have to largely rely on<br />
anecdotal accounts rather than organised<br />
clinical trials. One needs to consider<br />
how the ingredients are actually brought<br />
into contact with the eyelid margin,<br />
how often the procedure is undertaken<br />
<strong>and</strong> how long the treatment should last.<br />
<strong>Eyelid</strong> <strong>Margin</strong> Hygiene Technique<br />
The technique of eyelid hygiene should<br />
be selected according to the extent of the<br />
presenting signs, <strong>and</strong> a practitioner needs<br />
to take time to evaluate their patients<br />
<strong>and</strong> instruct them on the principles. If<br />
dominated by a greasy/oily appearance,<br />
perhaps with ‘foam’ along lateral<br />
aspects of the eyelid margin (which<br />
are also indicative of Meibomian gl<strong>and</strong><br />
dysfunction – MGD), then logically the<br />
eyelid margin really only needs to be<br />
gently wiped with a surfactant mixture to<br />
facilitate removal of such material. Some<br />
of these current products are cotton gauze<br />
pads soaked with the ingredients. These<br />
Figure 2<br />
Scanning electron microscopy of an upper eyelid<br />
margin of a rabbit presenting with mild blepharitis.<br />
The bases of the eyelashes (top of image) are<br />
largely obscured by large quantities of compacted<br />
dead cells <strong>and</strong>, most notably, the distal edge of this<br />
‘garbage zone’ is clearly colonised with numerous<br />
rod-shaped bacteria<br />
minimum requirements for any special<br />
manual dexterity, 15 even in children. 19<br />
Some practical trials on the efficacy of<br />
lid scrubbing have used six cycles of<br />
back-<strong>and</strong>-forth rubbing, 16 or even ten<br />
cycles. 20 However, a few wipes approach<br />
can likely be continued for as long as<br />
a problem is apparent. If oily/greasy<br />
material predominates <strong>and</strong> there are just<br />
some slight signs of MGD, then promoting<br />
normal meibum excretion onto the eyelid<br />
marginal zone might be achieved with the<br />
daily use of warm (wet) compresses. This<br />
also is a time honoured remedy, 10 but likely<br />
needs to be applied for several minutes to<br />
be effective, eg, 5 to 10 minutes of warm<br />
compress with a cotton ball, gauze pads<br />
or even the clean facial flannel, which is<br />
a little above normal body temperature;<br />
repeated re-warming of the material is<br />
thus essential (eg, by re-dipping into a<br />
bowl of moderately warm water). Recent<br />
similarly long duration (10 to 15 minute)<br />
use of a heated eye mask or eye bag. 22<br />
If the oily detritus appears a little more<br />
resistant to the wiping action of a gauze<br />
pad, then there are liquid products that<br />
can be used instead. These can be applied<br />
onto separate cotton gauze pads <strong>and</strong><br />
used in the same way as described or<br />
can be transferred to a sterile cotton bud<br />
applicator. The pre-packed individual<br />
sachets, once opened, may have enough<br />
liquid associated with the pad to<br />
adequately wet a cotton bud, which can<br />
then be systematically worked along the<br />
eyelid margin <strong>and</strong> bases of the eyelashes<br />
with gentle pressure. It will be up to the<br />
individual whether this is a rubbing back<br />
<strong>and</strong> forth action or simply one in which<br />
the cotton bud is slowly moved fairly<br />
firmly along the lid margin allowing for the<br />
solution to soak into the skin <strong>and</strong> eyelash<br />
bases. After a minute or so, a gauze pad can<br />
then be used to wipe away the dispersed<br />
material. One of the newer products<br />
comes in the form of a dispenser <strong>and</strong> the<br />
emergent foam is to be applied along the<br />
eyelid margin with the fingers, with the<br />
patient being advised that good h<strong>and</strong><br />
hygiene with a non-irritating soap product<br />
is an essential part of such a procedure.<br />
According to the severity of the<br />
presenting condition, cleansing can be<br />
done once a day (eg, before retiring to bed)<br />
or twice-a-day (morning <strong>and</strong> night), with<br />
the patient advised that regular gentle<br />
cleansing is likely the most effective way<br />
37<br />
17/09/10 CET<br />
are designed to be simply wiped back-<strong>and</strong>-<br />
research has established that not only<br />
of achieving a good result <strong>and</strong> to avoid too<br />
forth along the outer edge of the eyelid<br />
does the temperature need to be slightly<br />
aggressive ‘scrubbing’. Patients were once<br />
margin, with the procedure perhaps being<br />
higher than normal body temperature<br />
advised to undertake the procedure before<br />
repeated two or three times before the<br />
(ie, at 40 o C to 45 o C), but that this can<br />
retiring to bed ‘in order that the erythema<br />
pad is discarded. This can be done with<br />
improve the amount of normal oils that<br />
produced can subside during the night’. 12
CET CONTINUING<br />
EDUCATION<br />
& TRAINING<br />
2 FREE CET POINTS<br />
OT CET content supports <strong>Optometry</strong> Giving Sight<br />
4 4 4 4<br />
Approved for: Optometrists AS Points SP Points IP Points “How do I complete this exam?” Go to www.optometrytoday.tv/FAQ<br />
38<br />
17/09/10 CET<br />
The inclusion of soothing agents in<br />
contemporary products hopefully<br />
serves to emphasise that lid hygiene is<br />
not meant to be a traumatic procedure. 3<br />
Similarly, too aggressive ‘scrubbing’ (eg,<br />
excess warm/hot compresses, excess<br />
application of cleansing pads or even<br />
Meibomian gl<strong>and</strong> expression) can lead to<br />
at least temporary focal loss of eyelashes; 2<br />
this is hopefully avoidable. There is no<br />
efficacy data as to why the eyelid hygiene<br />
should be done before retiring to bed, <strong>and</strong><br />
one could likely find equal arguments as<br />
to whether female patients would prefer<br />
to undertake eyelid hygiene at the same<br />
time as removal of facial cosmetics or<br />
as a separate activity in the morning<br />
(prior to application of cosmetics).<br />
The issue of cosmetics use <strong>and</strong> the<br />
development of ‘blepharitis’ remains<br />
unclear, despite sporadic attention to<br />
the issue over the years. 23 A patient may<br />
present with mascara forming a liberal<br />
coating over a few or several Meibomian<br />
orifices, yet it is entirely possible that this<br />
will be removed as a result of effective<br />
use of surfactant-containing make up<br />
remover. However, for some patients,<br />
the efficacy of their cosmetics removal<br />
may need to be reviewed. A male patient<br />
might be expected to carry out lid hygiene<br />
Figure 3<br />
Clinical presentation of a likely infection of a eyelash<br />
follicle or accessory sebaceous gl<strong>and</strong> associated<br />
with the eyelashes (a ‘stye’)<br />
prior to a fresh start in the morning with a<br />
shave etc., which might produce a more<br />
useful result in the long-term management.<br />
The consequences of poor<br />
eyelid hygiene - the eyelashes<br />
<strong>and</strong> associated gl<strong>and</strong>s <strong>and</strong> its<br />
management<br />
If eyelid <strong>and</strong> peri-ocular hygiene is poor,<br />
then one can expect a progressive buildup<br />
of dead cells <strong>and</strong> meibum along the<br />
eyelid marginal zone. Electron microscopy<br />
studies on laboratory animals with<br />
obvious signs of blepharitis (Figure 2)<br />
show how substantial this material can<br />
be. 24 An almost inevitable consequence<br />
is colonisation of the eyelid margin zone<br />
with substantial numbers of bacteria.<br />
Most commonly this will result in a<br />
staphylococcal blepharitis, 1,12 since S.<br />
Aureus or S. epidermidis are common<br />
rod-shaped bacilli found on the normal<br />
lid margin. Other bacteria can also cause<br />
an infectious blepharitis, 11 notably those<br />
associated with acne-like conditions<br />
(eg, Propionobacterium acnes). 3,4<br />
For such infective blepharitis, a slightly<br />
more aggressive approach is likely needed<br />
for eyelid hygiene. The blepharitis, likely<br />
to now be of a recurrent <strong>and</strong> chronic<br />
nature, presents with signs of drying of the<br />
cellular <strong>and</strong> oily detritus, notably forming<br />
collarettes around the eyelash bases, or<br />
‘skuff’ that even extends quite a way<br />
along the eyelashes. This material needs<br />
to be moistened <strong>and</strong> softened before it can<br />
then be gently removed. Whether using<br />
a gauze pad or especially a cotton bud<br />
applicator, the idea should be to ‘daub’<br />
the eyelid margin with the cleansing<br />
agent <strong>and</strong> leave it for a few minutes. 2,4 In<br />
uncommon cases, the personal hygiene<br />
of a patient is likely to be so poor that the<br />
eyelashes (as well as other hair follicles)<br />
can become colonised with lice or<br />
mites, 3 eg, Demodex sp. 16 Any collarettes<br />
that appear to be particularly resistant to<br />
softening <strong>and</strong> wiping should be examined<br />
more carefully (eg, with biomicroscopy)<br />
for any signs of ‘macro’-organisms.<br />
When eyelid <strong>and</strong> personal hygiene is<br />
poor, another inevitable consequence is the<br />
development of a focal infection of either<br />
an eyelash follicle or accessory gl<strong>and</strong>s of<br />
the eyelashes. This results in an acute-onset<br />
focal swelling, a stye (Figure 3). These can<br />
be quite painful <strong>and</strong> result in swelling of the<br />
entire eyelid so that it presents closed. The<br />
key to successful management is to get the<br />
infection site to ‘point’ <strong>and</strong> the pus contents<br />
to be released so as to relieve the discomfort.<br />
By current perspectives, this is best done<br />
with the application of a warm compress<br />
(for 10 to 15 minutes) over the affected<br />
region, followed by carefully wiping <strong>and</strong><br />
cleansing with clean soft cotton or an eyelid<br />
hygiene pad. The procedure should be<br />
repeated a few hours later until resolution,<br />
with it being emphasised to the patient that<br />
keeping the area clean is important. Patients<br />
should also be advised that it is not generally<br />
a good idea for them to attempt to forcibly<br />
puncture the stye with a sharp object<br />
(although this might be done in extreme<br />
cases, under suitably clean conditions with<br />
a sterile lance by a health care professional).<br />
Home remedies such as using a sharpended<br />
cocktail stick or toothpick, dipped<br />
in phenol, 2 are no longer appropriate.<br />
When a stye develops, or is in the<br />
process of being pointed, the personal<br />
hygiene may be supplemented with the<br />
use of a topical anti-bacterial agent applied<br />
after the eyelid cleansing procedure.<br />
The ideal agent currently available are<br />
preparations containing diamidines,<br />
notably dibromopropamidine; Golden<br />
Eye Ointment <strong>and</strong> Brolene Eye Ointment<br />
are both available in small 5g tubes as P<br />
Medicines. These chemical anti-infectives
work to reduce the replication of common<br />
of the eyelid margin outwards <strong>and</strong> exert<br />
bacteria that affect the eyelid margin,<br />
sufficient pressure to expel the contents<br />
ie, they are bacteriostatic. 25 Twice daily<br />
of the gl<strong>and</strong>s in that region. 27,28 The<br />
application of the ointment along <strong>and</strong><br />
digital pressure may need to be exerted<br />
across the eyelid margins where the stye(s)<br />
for 30 seconds or more. A patient can<br />
is present should reduce the chance of<br />
be carefully instructed to do the same.<br />
cross infection of adjacent eyelashes. For<br />
most cases, the use of an antibiotic is not<br />
considered necessary, although some<br />
may opt for the use of chloramphenicol<br />
eye ointment, 6 or fusidic acid viscous<br />
eyedrops; 26 the use of fusidic acid might<br />
be considered as an acceptable but<br />
‘unlabeled’ use. 6 Both antibiotics are<br />
available as POMs (eg, Chloromycetin<br />
Eye Ointment <strong>and</strong> Fucithalmic) <strong>and</strong> the<br />
former is also now widely available as<br />
P Medicines (eg, Optrex Infected Eyes<br />
antibiotic drops, GoldenEye antibiotic<br />
ointment <strong>and</strong> Brochlor antibiotic<br />
ointment). All these anti-infective <strong>and</strong><br />
antibiotic preparations are available to<br />
entry-level <strong>and</strong> AS level optometrists.<br />
The combined consequences<br />
of poor eyelid hygiene <strong>and</strong><br />
an inflammatory response –<br />
Meibomian gl<strong>and</strong> dysfunction<br />
<strong>and</strong> its management<br />
The normal organisation <strong>and</strong> functioning<br />
of the Meibomian gl<strong>and</strong>s involves a<br />
holcrine secretory mechanism whereby<br />
the fatty contents of the gl<strong>and</strong>s undergo<br />
a transition to an oily fluid which is then<br />
expressed out of a patent orifice with<br />
every eyeblink. The orifices are lined<br />
with a stratified epithelium that can show<br />
various degrees of keratinisation. 3-5 If<br />
eyelid hygiene is poor, then the orifices<br />
can become blocked with dead cells <strong>and</strong><br />
a slow progressive process of stenosis<br />
develops. The gl<strong>and</strong>ular orifices can<br />
lose their characteristic ring-shaped<br />
appearance to be replaced by small domes<br />
Figure 4<br />
Clinical presentation of an individual with moderate<br />
plugging of the Meibomian gl<strong>and</strong> orifices. The<br />
lissamine green (<strong>and</strong> NaFl) staining reveals<br />
irregularity of Marx’s line but it is still located<br />
posteriorly to the Meibomian gl<strong>and</strong> orifices.<br />
respects, be considered to look like small<br />
styes, they are usually posteriorly located<br />
to the eyelashes. Plugged orifices usually<br />
cause little discomfort <strong>and</strong> are unlikely<br />
to be infected (unless there is substantial<br />
concurrent infectious anterior blepharitis).<br />
Such plugged orifices, even at early<br />
stages, cannot normally function to<br />
express the oils onto the eyelid margin,<br />
<strong>and</strong> so the patient may well present with<br />
symptomology suggestive of tear film<br />
deficiency, ie, dryness, scratchiness of<br />
the eyes, simply because the tear film is<br />
unstable. For early stage presentations,<br />
simply restoring normal gl<strong>and</strong>ular<br />
secretion should be the goal. The routine of<br />
regular eyelid hygiene is appropriate, with<br />
the combined effect of cleaning <strong>and</strong> gentle<br />
rubbing or massage of the eyelid margins<br />
adequate to restore patency to the gl<strong>and</strong>s.<br />
A practitioner may elect to carefully<br />
assess whether a gl<strong>and</strong> orifice is actually<br />
patent by applying pressure in the vicinity<br />
of the blocked orifices. In line with the<br />
perspective that eyelid hygiene is not meant<br />
to be painful or traumatic, an appropriate<br />
approach would be to gently position the<br />
affected part of the eyelid margin between<br />
thumb <strong>and</strong> forefinger <strong>and</strong> exert a gentle<br />
If assessed at the slit lamp, the<br />
appearance of clear (serous-like) or slightly<br />
cloudy (milky) liquid droplets indicates<br />
the orifice, whilst temporarily blocked, is<br />
at the end of a functioning gl<strong>and</strong>. One can<br />
attempt to do this along the length of the<br />
eyelid margin, noting that it is often rather<br />
more difficult to carry out towards the<br />
canthi <strong>and</strong> along the upper eyelid margin.<br />
If no exudate appears, the orifice is more<br />
substantially blocked, even keratinised.<br />
A practitioner can effect a little more<br />
focal pressure by attempting to squeeze<br />
the edge of the eyelid margin between<br />
either a clean cotton bud applicator tip<br />
<strong>and</strong> a forefinger, or between two cotton<br />
bud applicators; fluid droplets or more<br />
compacted (inspissated) contents are<br />
extruded. 8 In extreme cases, the pressure<br />
needed to express a gl<strong>and</strong> requires a<br />
force to be applied against a hard object<br />
such as a metal spatula tip, 1 <strong>and</strong> the<br />
extruded contents may appear to have the<br />
consistency of toothpaste <strong>and</strong> be opaque; a<br />
topical ocular anaesthetic should really be<br />
considered if such force is to be applied.<br />
Overall, however, in routine practice, such<br />
overzealous attempts to express the gl<strong>and</strong>s<br />
are likely to be most uncomfortable for the<br />
patient, 29 <strong>and</strong> it is likely better to adopt a<br />
slow <strong>and</strong> steady approach over many weeks<br />
with routine use of warm compresses<br />
<strong>and</strong> eyelid hygiene. The efficacy of all<br />
such measures can also be assessed by<br />
transillumination of the eyelid margin<br />
to assess whether a gl<strong>and</strong> has its normal<br />
elongated <strong>and</strong> uniform density or whether<br />
its contents are segmented, indicative of<br />
39<br />
17/09/10 CET<br />
(Figure 4). While these may, in some<br />
pinching motion to both direct the portion<br />
severe compaction of the contents. 3-5,28,30
CET CONTINUING<br />
EDUCATION<br />
& TRAINING<br />
2 FREE CET POINTS<br />
OT CET content supports <strong>Optometry</strong> Giving Sight<br />
4 4 4 4<br />
Approved for: Optometrists AS Points SP Points IP Points “How do I complete this exam?” Go to www.optometrytoday.tv/FAQ<br />
The consequences of not restoring<br />
or in others the apparent tear stability (as<br />
routine function of the Meibomian gl<strong>and</strong>s<br />
fluorescein tear break-up time measures)<br />
is now better understood <strong>and</strong> more easily<br />
may be normal, 38 even in acne rosacea.<br />
visualised (Figures 4 versus 5). Figure<br />
In some blepharitis cases (eg, atopic<br />
5 shows the upper eyelid margin of a<br />
eyelid disease/blepharitis with or<br />
40<br />
patient with a chronic history of recurrent<br />
staphylococcal blepharitis evident as<br />
collarettes along the eyelash bases <strong>and</strong><br />
without MGD), patient symptoms may<br />
be exacerbated by high temperatures or<br />
intake of hot spicy foods (both causing an<br />
17/09/10 CET<br />
chronic blockage (‘fall out’) of functioning<br />
Meibomian gl<strong>and</strong> orifices. The locations of<br />
the more anterior portions of the gl<strong>and</strong>s are<br />
evident as blotchy white regions that may<br />
or may not conceal partially functioning<br />
orifices. However, what is especially<br />
notable is the green staining line revealed<br />
with lissamine green that is clearly located<br />
anteriorly to the orifice regions; this is the<br />
anterior location of Marx’s line <strong>and</strong> with<br />
Figure 5<br />
Clinical presentation of an individual with moderate<br />
anterior blepharitis with almost complete<br />
obliteration of the Meibomian gl<strong>and</strong> orifices.<br />
The lissamine green staining not only reveals<br />
irregularity of Marx’s line but it is now partially<br />
located anteriorly to the Meibomian gl<strong>and</strong> orifices.<br />
From Doughty MJ et al. (2004) Ophthalmic Physiol.<br />
Opt. 24: 1-7. Copyright The College of Optometrists<br />
associated sweating). 4 For such patients, a<br />
little eyelid cleansing with lid wipes may<br />
serve to effectively augment routine facial<br />
hygiene <strong>and</strong> reduce symptoms. Associated<br />
reflex tearing may give rise to high values<br />
for tear secretion/volume assessments<br />
(Schirmer/tear meniscus height; see<br />
<strong>Optometry</strong> <strong>Today</strong>, August 13 2010). 35<br />
If staining <strong>and</strong> tear instability is apparent<br />
(eg, in seborrhoeic blepharitis), then the<br />
this configuration it has been argued that it<br />
especially if the patient is symptomatic.<br />
patient will likely benefit from the judicious<br />
is most unlikely that any gl<strong>and</strong> secretions<br />
Similarly, for an older patient being<br />
use of artificial tears, 4,6 <strong>and</strong> should be given<br />
will be able to serve a useful function. 9 This<br />
considered for cataract surgery, reduction<br />
instructions to use these just as if they had<br />
is because the oils will now be secreted<br />
or elimination of infectious blepharitis<br />
dry eye (see <strong>Optometry</strong> <strong>Today</strong>, August 13<br />
into the aqueous layer of the tear film rather<br />
than be extruded across the surface of the<br />
aqueous layer. In contrast, the lissamine<br />
green staining line in Figure 4, whilst<br />
somewhat irregular in width, is posteriorly<br />
located so that a functional secretion of the<br />
meibum can still occur. The same feature<br />
may be considered very beneficial. 3<br />
Some patients with chronic MGD,<br />
perhaps particularly those with acne<br />
rosacea, may show substantial signs<br />
of tear film deficiency as evidenced<br />
by rose bengal staining. In some cases<br />
of blepharitis, warm compress <strong>and</strong> lid<br />
2010). However, if staining is not evident<br />
then symptomatic relief may be provided<br />
with a comfort drop or moisturiser. This<br />
distinction could be important for a<br />
patient, since it has long been noted that<br />
patients with blepharitis may particularly<br />
experience symptoms ‘during the use of<br />
will also likely stain with rose bengal. 31<br />
For the optometrist considering<br />
hygiene measures can reduce staining<br />
<strong>and</strong> improve tear stability, 34-36 but various<br />
near vision under artificial illumination’. 11<br />
The modern-day equivalent could be the<br />
management of more severe cases of<br />
studies indicate that one should not<br />
computer user with obstinate blepharitis.<br />
Meibomian gl<strong>and</strong> problems, whatever its<br />
expect to see any obvious (short-term?)<br />
In non-infectious blepharitis, for largely<br />
aetiology, consideration needs to be given<br />
improvement in the appearance of the<br />
unknown reasons, the non-extruded gl<strong>and</strong><br />
to the assessments that need to be made.<br />
Meibomian gl<strong>and</strong> orifices. It needs to be<br />
contents elicit a progressive inflammatory<br />
The optometrist also needs to decide when<br />
remembered that shortly after any eyelid<br />
response from inside the gl<strong>and</strong>s. In cases<br />
they really should rise to the challenge<br />
of dealing with blepharatis. For example,<br />
if observed in a contact lens wearer it is<br />
likely to be associated with other problems<br />
such as excessive spoilage of the lens. 32,33<br />
The continuing presence of the lens may<br />
hygiene that promotes Meibomian gl<strong>and</strong><br />
expression, tear film findings may be<br />
equivocal. 27 It is also possible that at some<br />
point in time (up to a few hours?) shortly<br />
after lid hygiene measures, there may be a<br />
more frothy discharge (‘foam’), especially<br />
of infectious blepharitis, it has been argued<br />
that enzymes (phospholipases) produced by<br />
the bacteria can alter the characteristics of<br />
the meibum to exacerbate this inflammatory<br />
reaction. One well-known consequence of<br />
this is the emergence of a focal inflammation<br />
actually exacerbate build-up of meibum<br />
<strong>and</strong> detritus along the lid margin. 29 The<br />
blepharitis really needs to be managed,<br />
if patients have been rubbing their eyes. 37<br />
In other cases, neither surface staining<br />
nor tear film instability may be apparent,<br />
of a Meibomian gl<strong>and</strong>, a posterior/interior<br />
hordeolum or chalazion (Figure 6).<br />
As long as the gl<strong>and</strong> orifice is blocked
<strong>and</strong> the production of meibum continues,<br />
the associated inflammation can result in<br />
single or multiple lumps along the eyelid<br />
margin. There is no immediate remedy<br />
but the application of warm compresses<br />
for 10 to 15 minutes several times a day<br />
will usually help to remedy the situation.<br />
This allows for a slow but progressive<br />
restoration of the gl<strong>and</strong>, <strong>and</strong> the swelling<br />
subsides. Application of gentle pressure<br />
<strong>and</strong> massage may assist this, but at this<br />
stage firm digital or other pressure to try<br />
to promote expression is only likely to<br />
lead to extreme discomfort. Routine eyelid<br />
hygiene remains important as a means<br />
of preventing any focal infection. Older<br />
remedies have included instructing the<br />
patient to apply an ophthalmic antibiotic<br />
ointment along the eyelid margins two to<br />
three times a day <strong>and</strong> then massage it in, 12<br />
but are no longer thought to be of significant<br />
benefit (but see below). If the chalazion fails<br />
to respond to external compresses <strong>and</strong> the<br />
contents really harden, then the patient will<br />
need to be referred to an ophthalmologist<br />
to have the chalazion excised. 39<br />
Special issues in the management of MGD<br />
Certain adjunct treatments can be<br />
beneficial, one of which is likely more<br />
appealing <strong>and</strong> available to the entry-level<br />
optometrist <strong>and</strong> the other accessible for<br />
the IP-trained optometrist. By current<br />
ideas, chronic MGD is thought to reflect<br />
an imbalance between certain types of<br />
essential fatty acids in the body, with<br />
omega-3 compounds likely the most<br />
common. 4,5 There has, therefore, emerged<br />
an idea that supplementing a patient’s<br />
normal oral intake of omega-3 fatty acids<br />
(eg, flaxseed oils) may improve MGD. 4<br />
While rather hard to prove, evidence has<br />
been presented that the consistency of<br />
expressed meibum can improve following<br />
use of such supplements, 13 along with<br />
Figure 6<br />
Clinical presentation of an individual with a<br />
recurrent history of Meibomian gl<strong>and</strong> dysfunction<br />
where the compaction <strong>and</strong> inflammation of the<br />
gl<strong>and</strong>ular contents leads to swelling (a chalazion)<br />
improvements in tear film quality. Longterm<br />
studies still need to be done to<br />
ascertain whether there is a sustained<br />
improvement as well as reduction in<br />
recurrence of MGD. Notwithst<strong>and</strong>ing, such<br />
supplements are now widely available as<br />
GSL or non-medicinal products, including<br />
over the Internet, <strong>and</strong> so available to entrylevel<br />
optometrists <strong>and</strong> patients alike.<br />
The second approach is to use orally<br />
administered antibiotics that have<br />
anti-inflammatory actions. These are<br />
the tetracycline group of antibiotics<br />
eg, chlortetracycline. It was once a<br />
recommended practice to ask a patient with<br />
blepharitis to apply chlortetracycline eye<br />
ointment (Aureomycin) two to three times<br />
per day, <strong>and</strong> this should be continued for<br />
a month before perhaps being reduced to<br />
one to two times per week over the ensuing<br />
months. 12 While no longer formally<br />
marketed, some NHS trusts may still<br />
list <strong>and</strong> produce an equivalent (generic)<br />
product which might be accessed by an<br />
IP optometrist or a hospital optometrist<br />
working under a patient group directive.<br />
Orally administered tetracyclines such<br />
as minocycline (not to be confused with<br />
other oral macrolide antibiotics such<br />
as erythromycin) can also be used in<br />
patients with recurrent MGD associated<br />
with conditions such as acne rosacea. 25<br />
Current College of Optometrists CMG, 6<br />
indicate that it could be appropriate<br />
for an IP optometrist to be involved in<br />
the prescribing of the relevant PoMs.<br />
While the exact mechanisms whereby<br />
this might be realised for the optometrist<br />
are still to be resolved, the option of comanagement<br />
<strong>and</strong> asking a patient’s GP<br />
to provide the prescription would be<br />
appropriate, eg, Minocin MR at 2 x 100<br />
mg BDS for three months; one ought to<br />
consider, however, the risk of substantial<br />
gastrointestinal side effects. 3,34,35 Lower<br />
dosing (eg, 20 mg BDS) may be efficacious<br />
as a maintenance dose but it is unclear<br />
whether such an intervention would be<br />
adequate to reduce the severity; the use of<br />
lower doses should however reduce the<br />
risk of adverse reactions. Ocular rosacea<br />
may also be managed with judicious<br />
(unlabelled) use of a topical gel (for the<br />
skin) containing another antibacterial<br />
drug, metronidazole (PoM Rozex). 40<br />
Conclusion<br />
With eyelid <strong>and</strong> eyelid margin<br />
abnormalities being rather common<br />
conditions, optometrists are well placed<br />
to manage them. The most important<br />
aspect of this management relates to<br />
educating patients on ocular hygiene,<br />
but advice on palliative measures<br />
<strong>and</strong> the adjunct use of anti-infectives<br />
or antibiotics is appropriate as well.<br />
About the Author<br />
Professor Doughty has been teaching ocular<br />
pharmacology, as well as many aspects of<br />
ocular physiology <strong>and</strong> eye disease, for over<br />
25 years <strong>and</strong> authored books on the subject.<br />
He has held the post of research professor<br />
at Glasgow Caledonian University,<br />
Department of Vision Sciences since 1995.<br />
References<br />
See www.optometry.co.uk <strong>and</strong> search<br />
‘references’<br />
41<br />
17/09/10 CET
CET CONTINUING<br />
EDUCATION<br />
& TRAINING<br />
2 FREE CET POINTS<br />
OT CET content supports <strong>Optometry</strong> Giving Sight<br />
4 4 4 4<br />
Approved for: Optometrists AS Points SP Points IP Points “How do I complete this exam?” Go to www.optometrytoday.tv/FAQ<br />
Module questions<br />
Course code: C-14374 O/AS/SP/IP<br />
42<br />
17/09/10 CET<br />
1. Structures involved in the development of blepharitis include which of<br />
the following:<br />
(a) The eyelashes<br />
(b) The gl<strong>and</strong>s of Zeiss<br />
(c) Meibomian gl<strong>and</strong>s<br />
(d) All of the above<br />
2. Which of the following statements about eyelid cleansing <strong>and</strong> hygiene<br />
products is TRUE?<br />
(a) They are non-medicinal products<br />
(b) They are marketed as cosmetics<br />
(c) They will not be sold as medical devices<br />
(d) They are usually designated as P Medicines<br />
3. Past treatment options for blepharitis have included which of the<br />
following?<br />
(a) Regular applications of chlortetracycline ointments along the lid margins<br />
(b) Wiping the eyelid margin with benzalkonium chloride solutions<br />
(c) Application of phenol solutions to affected parts of the eyelids<br />
(d) All of the above<br />
4. Which of the following statements about modern-day treatment of<br />
non-infectious chronic blepharitis is TRUE?<br />
(a) It should routinely include the use of antibiotic eye ointments<br />
(b) It can be effectively achieved with regular use of dedicated cleaning solutions<br />
(c) It always needs to be supplemented with oral antibiotic <strong>and</strong> antiinflammatory<br />
drugs<br />
(d) It can likely be achieved with just the use of warm compresses or eye pads<br />
(masks)<br />
7. Which of the following statements about current perspectives for<br />
routine eyelid hygiene using a cleaning pad or cotton bud is TRUE?<br />
(a) It needs to be gently rubbed back <strong>and</strong> forth a few times<br />
(b) It should simply be wiped once along the eyelid margin <strong>and</strong> then discarded<br />
(c) It needs to be repeatedly used in a scrubbing motion along the eyelids many<br />
times<br />
(d) It is only really needed if there are signs of infection present<br />
8. Which of the following is an expected consequence of chronic<br />
Meibomian gl<strong>and</strong> dysfunction?<br />
(a) Development of collarettes around the eyelash bases<br />
(b) Oily excretions from the Meibomian gl<strong>and</strong>s<br />
(c) Focal loss of eyelashes<br />
(d) Development of single or multiple internal hordeola<br />
9. For a suspected case of staphylococcal blepharitis, which of the<br />
following products would be MOST appropriate after eyelid hygiene<br />
measures?<br />
(a) Oral Minocin MR (PoM)<br />
(b) Brolene Eye Ointment (P Medicine)<br />
(c) Aureomycin eye ointment (PoM)<br />
(d) Blephasol solution (SL)<br />
10. <strong>Eyelid</strong> transillumination is a procedure that might be used for what<br />
purpose?<br />
(a) Assessment of the extent of inspissation of the Meibomian gl<strong>and</strong>s<br />
(b) Checking to see if the eyelash follicles are intact<br />
(c) To assess the location (anterior or posterior) of Marx’s line<br />
(d) None of the above<br />
5. Which of the following is an example of a surfactant cleansing agent in<br />
an eyelid hygiene product?<br />
(a) Chamomile<br />
(b) Boric acid<br />
(c) Polysorbate<br />
(d) Sodium bicarbonate<br />
6. Which if the following can be considered as soothing agents included<br />
in contemporary eyelid hygiene products?<br />
(a) Boric acid<br />
(b) Calendula extracts<br />
(c) Lauroamphocetate extracts<br />
(d) Phosphate salts (buffer)<br />
11. Which of the following antibiotics can be useful as part of the<br />
management of some cases of blepharitis?<br />
(a) Chloramphenicol<br />
(b) Minocycline<br />
(c) Fusidic acid<br />
(d) All of the above<br />
12. Which eyelid feature should be more carefully examined by<br />
biomicroscopy if lice were the suspected cause of the blepharitis?<br />
(a) The outer canthus<br />
(b) The bases of the eyelashes<br />
(c) The shafts <strong>and</strong> tips of the eyelashes<br />
(d) The Meibomian gl<strong>and</strong> orifices<br />
PLEASE NOTE There is only one correct answer. All CET is now FREE. Enter online. Please complete online by midnight on October 20 2010 - You will be unable to submit<br />
exams after this date – answers to the module will be published on www.optometry.co.uk