Eyelid misdirection and its management
Eyelid misdirection and its management
Eyelid misdirection and its management
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
ot<br />
Leonid Skorin Jr, OD, DO, FAAO, FAOCO<br />
<strong>Eyelid</strong> <strong>misdirection</strong> <strong>and</strong> <strong>its</strong> <strong>management</strong><br />
Misdirected eyelashes may result<br />
from various causes, but it is<br />
important to identify the exact<br />
mechanism or anatomical deviation<br />
for the <strong>misdirection</strong> to adequately<br />
address treatment. The goal of<br />
treatment is to remove or redirect<br />
the offending eyelashes.<br />
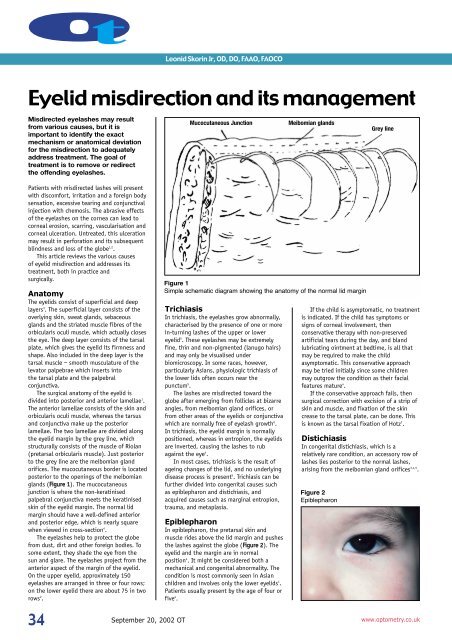
Mucocutaneous Junction<br />
Meibomian gl<strong>and</strong>s<br />
Grey line<br />
Patients with misdirected lashes will present<br />
with discomfort, irritation <strong>and</strong> a foreign body<br />
sensation, excessive tearing <strong>and</strong> conjunctival<br />
injection with chemosis. The abrasive effects<br />
of the eyelashes on the cornea can lead to<br />
corneal erosion, scarring, vascularisation <strong>and</strong><br />
corneal ulceration. Untreated, this ulceration<br />
may result in perforation <strong>and</strong> <strong>its</strong> subsequent<br />
blindness <strong>and</strong> loss of the globe 1,2 .<br />
This article reviews the various causes<br />
of eyelid <strong>misdirection</strong> <strong>and</strong> addresses <strong>its</strong><br />
treatment, both in practice <strong>and</strong><br />
surgically.<br />
Anatomy<br />
The eyelids consist of superficial <strong>and</strong> deep<br />
layers 3 . The superficial layer consists of the<br />
overlying skin, sweat gl<strong>and</strong>s, sebaceous<br />
gl<strong>and</strong>s <strong>and</strong> the striated muscle fibres of the<br />
orbicularis oculi muscle, which actually closes<br />
the eye. The deep layer consists of the tarsal<br />
plate, which gives the eyelid <strong>its</strong> firmness <strong>and</strong><br />
shape. Also included in the deep layer is the<br />
tarsal muscle – smooth musculature of the<br />
levator palpebrae which inserts into<br />
the tarsal plate <strong>and</strong> the palpebral<br />
conjunctiva.<br />
The surgical anatomy of the eyelid is<br />
divided into posterior <strong>and</strong> anterior lamellae 1 .<br />
The anterior lamellae consists of the skin <strong>and</strong><br />
orbicularis oculi muscle, whereas the tarsus<br />
<strong>and</strong> conjunctiva make up the posterior<br />
lamellae. The two lamellae are divided along<br />
the eyelid margin by the grey line, which<br />
structurally consists of the muscle of Riolan<br />
(pretarsal orbicularis muscle). Just posterior<br />
to the grey line are the meibomian gl<strong>and</strong><br />
orifices. The mucocutaneous border is located<br />
posterior to the openings of the meibomian<br />
gl<strong>and</strong>s (Figure 1). The mucocutaneous<br />
junction is where the non-keratinised<br />
palpebral conjunctiva meets the keratinised<br />
skin of the eyelid margin. The normal lid<br />
margin should have a well-defined anterior<br />
<strong>and</strong> posterior edge, which is nearly square<br />
when viewed in cross-section 4 .<br />
The eyelashes help to protect the globe<br />
from dust, dirt <strong>and</strong> other foreign bodies. To<br />
some extent, they shade the eye from the<br />
sun <strong>and</strong> glare. The eyelashes project from the<br />
anterior aspect of the margin of the eyelid.<br />
On the upper eyelid, approximately 150<br />
eyelashes are arranged in three or four rows;<br />
on the lower eyelid there are about 75 in two<br />
rows 2 .<br />
Figure 1<br />
Simple schematic diagram showing the anatomy of the normal lid margin<br />
Trichiasis<br />
In trichiasis, the eyelashes grow abnormally,<br />
characterised by the presence of one or more<br />
in-turning lashes of the upper or lower<br />
eyelid 5 . These eyelashes may be extremely<br />
fine, thin <strong>and</strong> non-pigmented (lanugo hairs)<br />
<strong>and</strong> may only be visualised under<br />
biomicroscopy. In some races, however,<br />
particularly Asians, physiologic trichiasis of<br />
the lower lids often occurs near the<br />
punctum 5 .<br />
The lashes are misdirected toward the<br />
globe after emerging from follicles at bizarre<br />
angles, from meibomian gl<strong>and</strong> orifices, or<br />
from other areas of the eyelids or conjunctiva<br />
which are normally free of eyelash growth 6 .<br />
In trichiasis, the eyelid margin is normally<br />
positioned, whereas in entropion, the eyelids<br />
are inverted, causing the lashes to rub<br />
against the eye 4 .<br />
In most cases, trichiasis is the result of<br />
ageing changes of the lid, <strong>and</strong> no underlying<br />
disease process is present 5 . Trichiasis can be<br />
further divided into congenital causes such<br />
as epiblepharon <strong>and</strong> distichiasis, <strong>and</strong><br />
acquired causes such as marginal entropion,<br />
trauma, <strong>and</strong> metaplasia.<br />
Epiblepharon<br />
In epiblepharon, the pretarsal skin <strong>and</strong><br />
muscle rides above the lid margin <strong>and</strong> pushes<br />
the lashes against the globe (Figure 2). The<br />
eyelid <strong>and</strong> the margin are in normal<br />
position 4 . It might be considered both a<br />
mechanical <strong>and</strong> congenital abnormality. The<br />
condition is most commonly seen in Asian<br />
children <strong>and</strong> involves only the lower eyelids 1 .<br />
Patients usually present by the age of four or<br />
five 4 .<br />
If the child is asymptomatic, no treatment<br />
is indicated. If the child has symptoms or<br />
signs of corneal involvement, then<br />
conservative therapy with non-preserved<br />
artificial tears during the day, <strong>and</strong> bl<strong>and</strong><br />
lubricating ointment at bedtime, is all that<br />
may be required to make the child<br />
asymptomatic. This conservative approach<br />
may be tried initially since some children<br />
may outgrow the condition as their facial<br />
features mature 4 .<br />
If the conservative approach fails, then<br />
surgical correction with excision of a strip of<br />
skin <strong>and</strong> muscle, <strong>and</strong> fixation of the skin<br />
crease to the tarsal plate, can be done. This<br />
is known as the tarsal fixation of Hotz 7 .<br />
Distichiasis<br />
In congenital distichiasis, which is a<br />
relatively rare condition, an accessory row of<br />
lashes lies posterior to the normal lashes,<br />
arising from the meibomian gl<strong>and</strong> orifices 3,4,5 .<br />
Figure 2<br />
Epiblepharon<br />
34<br />
September 20, 2002 OT www.optometry.co.uk
Figure 3<br />
Involutional entropion with preseptal<br />
muscle override causing in-turning of lid<br />
margin <strong>and</strong> eyelashes rubbing the globe<br />
Figure 4<br />
Involutional entropion causing untoward<br />
corneal <strong>and</strong> conjunctival changes<br />
The meibomian gl<strong>and</strong>s themselves may be<br />
rudimentary, atrophic or normal 8 . Often this<br />
extra row of lashes is incomplete. Although<br />
the lashes in trichiasis are typically of normal<br />
calibre, the aberrant hairs in distichiasis are<br />
often softer, shorter, less pigmented <strong>and</strong><br />
finer 9 . It has been associated with<br />
strabismus, ptosis, cleft palate, congenital<br />
ear defects, trisomy 18, <strong>and</strong> m<strong>and</strong>ibulofacial<br />
dystosis 4,5 .<br />
Acquired distichiasis happens when<br />
normal, non-hair producing meibomian<br />
gl<strong>and</strong>s (sebaceous) of the tarsal plate are<br />
transformed into hair follicles (pilosebaceous<br />
un<strong>its</strong>) by mechanical or chemical stimuli 10 .<br />
These stimuli include chronic inflammation<br />
such as blepharitis <strong>and</strong> meibomitis,<br />
cicatricial conditions of the mucosa such as<br />
Stevens-Johnson syndrome, ocular<br />
pemphigoid <strong>and</strong> severe chemical burns, <strong>and</strong><br />
metaplastic triggering process such as<br />
mechanical or surgical trauma to the<br />
meibomian gl<strong>and</strong>s 5 .<br />
The goal of treatment is to destroy the<br />
distichiatic lashes while retaining the normal<br />
ones. This is best accomplished by<br />
performing a lid-splitting procedure<br />
combined with cryotherapy. This is done by<br />
splitting the lid into the anterior <strong>and</strong><br />
posterior lamellae along the grey line.<br />
Cryotherapy is then applied to the posterior<br />
lamellae using a double freeze-thaw<br />
technique. This procedure avoids the risk of<br />
damage to the normal lashes <strong>and</strong><br />
www.optometry.co.uk<br />
depigmentation of the skin. To prevent postoperative<br />
cicatricial entropion, the anterior<br />
lamellae is recessed during reconstruction 11 .<br />
If there are only one or two distichiatic<br />
lashes, then direct surgical excision<br />
performed with the aid of an operating<br />
microscope can be done. Each abnormal cilia<br />
is located <strong>and</strong> excised through the<br />
conjunctival surface of the lid 12 .<br />
The application of lubricants or a soft<br />
b<strong>and</strong>age contact lens or, in severe cases,<br />
topical antibiotics may be indicated before<br />
surgical intervention 5,13 .<br />
Marginal entropion<br />
Marginal entropion occurs when only the<br />
posterior eyelid margin becomes rounded,<br />
physically causing inversion through the<br />
posterior pulling of the posterior lamellae<br />
structures. This causes the lashes to become<br />
misdirected as the mucocutaneous junction<br />
migrates anteriorly <strong>and</strong> the keratinised<br />
portion of the lid is pulled posteriorly 4 .<br />
Marginal entropion can be considered a mild<br />
form of cicatricial entropion 1 . Marginal<br />
entropion is the most common cause of<br />
trichiasis in adults 1,14 .<br />
Entropion<br />
Entropion is a condition in which the eyelid<br />
margin turns inward against the globe 14 . It<br />
can be classified as congenital, spastic,<br />
involutional (senile) or cicatricial 15 .<br />
Involutional entropion is the most<br />
common cause of entropion in elderly<br />
patients. It affects mainly the lower eyelid<br />
because the upper lid has a wider tarsal<br />
plate <strong>and</strong> is more stable. Ageing changes<br />
create a relative excess of skin <strong>and</strong> anterior<br />
lamellae of the eyelid. This causes overriding<br />
of the preseptal orbicularis muscle over the<br />
pretarsal muscle during lid closure, which<br />
tends to move the lower border of the tarsal<br />
plate away from the globe <strong>and</strong> the upper<br />
border towards the globe 14 (Figure 3).<br />
Persistent rubbing by in-turned eyelashes<br />
against the conjunctiva <strong>and</strong> cornea leads to<br />
conjunctival chemosis <strong>and</strong> injection,<br />
superficial punctate keratopathy <strong>and</strong><br />
eventual corneal ulceration (Figure 4).<br />
Continued stretching of the orbicularis<br />
muscle, as well as both medial <strong>and</strong> lateral<br />
canthal tendons, causes a horizontal lid<br />
laxity. This lid laxity is aggravated by any<br />
orbital fat atrophy or enophthalmos 14<br />
(Figure 5). All these factors help contribute<br />
to the destabilisation of the eyelid.<br />
Management of entropion requires<br />
surgical reconstruction. If there is no or<br />
minimal horizontal lid laxity, a base-down<br />
triangle tarsal resection may be indicated<br />
(Figure 6). If there is horizontal lid laxity,<br />
then a combination of lateral canthal<br />
strengthening <strong>and</strong> tightening of the lower<br />
lid retractors increases the pull of the lower<br />
lid retractors, <strong>and</strong> also creates a barrier<br />
between the preseptal <strong>and</strong> pretarsal<br />
orbicularis muscles (Figure 7).<br />
Figure 5<br />
Insufficient support for prosthesis resulting<br />
in enophthalmic appearance <strong>and</strong> in-turning<br />
of superior <strong>and</strong> inferior eyelids. This<br />
simulates severe trichiasis<br />
Figure 6<br />
Base-down triangle resection. Sutures are<br />
in place prior to tightening<br />
Figure 7<br />
Forceps are holding the inferior lid<br />
retractors. Tightening them <strong>and</strong><br />
strengthening the lateral canthus corrects<br />
entropion<br />
Metaplasia<br />
Cicatricial lash problems result from acute or<br />
chronic inflammation. Subtle scarring of the<br />
posterior lamellae pulls the eyelashes<br />
toward the eye. This same inflammation can<br />
result in metaplasia of the meibomian<br />
gl<strong>and</strong>s resulting in the production of hair<br />
follicles <strong>and</strong> the consequent aberrant<br />
lashes 4 .<br />
The most common acute inflammatory<br />
causes include viral infection (herpes zoster,<br />
herpes simplex, vaccinia); chemical burns,<br />
especially alkali; trauma; radiation; <strong>and</strong><br />
surgery or cryotherapy. The most common<br />
chronic inflammatory causes include<br />
blepharitis (Staphylococcus, seborrhea,<br />
35
ot<br />
Figure 8<br />
ProLectro ophthalmic epilator<br />
Figure 9<br />
<strong>Eyelid</strong> with trichiasis being anaesthetised<br />
with a subcutaneous injection<br />
Figure 10<br />
Electrolysis microstylet wire inserted<br />
adjacent to aberrant eyelash<br />
rosacea); trachoma; chronic viral infection;<br />
conjunctival shrinkage (ocular cicatricial<br />
pemphigoid, Stevens-Johnson syndrome) or<br />
use of topical medication (drug-related<br />
pseudopemphigoid) 16 .<br />
Many ocular medications, including<br />
topical ophthalmic idoxuridine, demecarium,<br />
epinephrine, timolol, pilocarpine,<br />
echothiophate <strong>and</strong> dipivefrin, are associated<br />
with a pemphigoid-like syndrome 17-19 . When a<br />
patient who is taking a glaucoma medication<br />
topically develops pemphigoid-like changes,<br />
a conjunctival biopsy should be done <strong>and</strong><br />
the medication discontinued. In many cases,<br />
the cicatricial changes will arrest 2 . A<br />
different class of glaucoma agent or<br />
glaucoma surgery should be tried.<br />
Treatment of trichiasis<br />
The treatment approach depends on the<br />
extent of lid involvement. Epilation of<br />
multiple lashes can be inappropriate because<br />
often, lashes grow back rapidly in a more<br />
aberrant fashion <strong>and</strong> thicker in diameter 10 .<br />
Very fine, thin eyelashes (lanugo hairs) may<br />
be difficult to see <strong>and</strong> grasp with forceps.<br />
If mechanical removal is indicated (there<br />
are only one or two misdirected lashes),<br />
then simple epilation with jewellers’ forceps<br />
or epilating forceps can be attempted. A<br />
drop of topical anesthetic improves patient<br />
comfort <strong>and</strong> compliance. To avoid breakage,<br />
the lash should be grasped securely at <strong>its</strong><br />
base. A firm tug outward will remove the<br />
lash by <strong>its</strong> root 5 . Unfortunately, the<br />
eyelashes typically recur within three to six<br />
weeks 1 .<br />
Areas of recurrent trichiasis require more<br />
definitive treatment. These treatment<br />
modalities include electrolysis, laser<br />
photoablation, cryotherapy <strong>and</strong> surgical<br />
repair <strong>and</strong> reconstruction.<br />
Electrolysis<br />
This procedure is efficient when removing<br />
individual misdirected eyelashes. An easy<br />
<strong>and</strong> inexpensive method is with the use of<br />
the ProLectro electrolysis unit 5 . This is a<br />
small, h<strong>and</strong>-held unit which uses the basic<br />
principle of electrolysis. A mild, galvanic<br />
current is transmitted from the power source<br />
(a battery). The amount of current is<br />
regulated by a rheostat <strong>and</strong> gauge. The<br />
current passes through a connecting wire to<br />
the operator-held h<strong>and</strong>piece which contains<br />
the microstylet wire (Figure 8).<br />
The patient’s eyelid should first be<br />
anaesthetised with a subcutaneous injection<br />
of lidocaine 1% with 1:100,000 epinephrine<br />
(Figure 9). The patient is then seated behind<br />
the biomicroscope <strong>and</strong> instructed to hold<br />
the electrode (power source, rheostat,<br />
gauge) in their h<strong>and</strong> to complete the circuit.<br />
The clinician everts the lid <strong>and</strong> inserts the<br />
microstylet wire to a depth of 2mm<br />
immediately adjacent to the eyelash shaft<br />
into the hair follicle 1,5,10 . The wire must be<br />
positioned in the same direction in which<br />
the hair is growing 5 . When the wire is<br />
properly positioned, the switch which is<br />
located on the operator’s h<strong>and</strong>-piece is<br />
pressed <strong>and</strong> this starts the flow of current.<br />
The power is increased slowly until the tissue<br />
around the follicle coagulates 4 . This appears<br />
as frothy bubbling <strong>and</strong> can take anywhere<br />
from five to 10 seconds to be seen at the<br />
follicular orifice 10 (Figure 10).<br />
The eyelash usually slides out as the<br />
microstylet wire is removed. This indicates<br />
successful treatment. The lash can also be<br />
either wiped away with a cotton-tipped<br />
applicator or removed with epilating forceps.<br />
Any resistance to <strong>its</strong> removal indicates<br />
incomplete treatment <strong>and</strong> a second<br />
application should be done.<br />
Electrolysis can cause mild swelling or<br />
irritation in the immediate area of<br />
treatment 5 . Treatment of many lashes close<br />
together, or over-zealous use of electrolysis,<br />
can create scarring, notching <strong>and</strong> tendency<br />
toward cicatricial entropion 10,16 . Other<br />
disadvantages include the difficulty of<br />
making an accurate ‘blind’ insertion of the<br />
wire into the follicle, creating a false<br />
passage or not going deep enough, <strong>and</strong><br />
difficulty in treating small or lanugo<br />
lashes 16 .<br />
The failure rate by some authors has<br />
been stated to be as high as 50-70%,<br />
indicating recurrence of lashes 1,4 . Other<br />
sources state that only a low incidence of<br />
regrowth is seen, mostly with coarse or<br />
previously tweezed lashes 5 . Success rates can<br />
be increased by applying meticulous<br />
technique.<br />
Electrical current can be converted into<br />
controlled energy in the radiowave portion<br />
of the electromagnetic spectrum using a<br />
radiosurgical unit as an alternative method<br />
of treating localised trichiasis 1 . This<br />
radiosurgical epilating method uses an<br />
insulated electrocautery needle. Otherwise,<br />
the procedure is identical to the st<strong>and</strong>ard<br />
electrolysis surgical regimen. First treatment<br />
success rate has been reported to be as high<br />
as 67% 20 .<br />
Laser photoablation<br />
Argon laser photoablation can be used for<br />
treating focal, localised areas of trichiasis 21 .<br />
It is hoped that the pinpoint accuracy of the<br />
argon laser would allow destruction of the<br />
abnormal lash follicle with the least amount<br />
of damage to the surrounding structures,<br />
compared to other techniques such as<br />
cryotherapy or electrolysis 1 .<br />
Laser energy is delivered with a st<strong>and</strong>ard<br />
slit lamp. The eyelid is infiltrated with a<br />
local anaesthetic as used in electrolysis. A<br />
cotton-tipped applicator is used to orient<br />
the eyelid so that the lash follicle is parallel<br />
to the laser beam. Laser settings of 1.0<br />
watts to 2.5 watts, 0.2 seconds to 0.5<br />
seconds duration, 50 micron or 100 micron<br />
spot size, <strong>and</strong> blue-green colour are directed<br />
co-axially along the lash to a depth of 2mm<br />
giving the best results 1,2,4,10,16 . It usually<br />
takes from 15-30 burns per eyelash 1 .<br />
Non-pigmented lashes can be dyed with<br />
gentian violet for more efficient laser<br />
uptake 4 . The success rate ranges from<br />
50-90% 21 .<br />
Complications are typically rare but<br />
include eyelash recurrence, notching,<br />
scarring, depigmentation, <strong>and</strong> erythema 1 . As<br />
with electrolysis, only one lash follicle can<br />
be treated at a time 2 .<br />
36<br />
September 20, 2002 OT<br />
www.optometry.co.uk
Cryotherapy<br />
There is a graded sensitivity of tissues to the<br />
effects of freezing. Eyelash <strong>and</strong> hair follicles<br />
are more sensitive than epithelial cells <strong>and</strong><br />
connective tissue, but are less sensitive than<br />
pigment cells. Abnormal eyelashes can be<br />
destroyed by freezing the lash follicles to a<br />
temperature of -20˚C, whereas the<br />
surrounding eyelid tissue can withst<strong>and</strong><br />
temperatures of -40˚C 4,14 . Freezing to -20˚C<br />
will cause depigmentation which may or may<br />
not improve with time, therefore non-white<br />
patients may be better treated with a<br />
combination of electrolysis <strong>and</strong> surgery<br />
rather than cryotherapy 14 .<br />
Cryotherapy causes intracellular ice<br />
crystal formation, which results in cell<br />
membrane rupture. A change in the pH<br />
value of intracellular fluid results in protein<br />
desaturation. The cold injury to blood<br />
vessels causes thrombosis with secondary<br />
ischemia <strong>and</strong> infarction 10 .<br />
Cryotherapy uses an instrument called a<br />
cryoprobe <strong>and</strong> nitrous oxide as a heat sink.<br />
The eye should be protected with a plastic<br />
corneo-scleral guard. The eyelid is<br />
anaesthetised with lidocaine 1% with<br />
1:100,000 epinephrine injection. The<br />
vasoconstrictive effective of the epinephrine<br />
speeds freezing <strong>and</strong> slows thawing. The<br />
cryoprobe is placed on the lid skin adjacent<br />
to the misdirected lashes. The probe is<br />
placed for 30 seconds along the upper lid<br />
<strong>and</strong> for 25 seconds along the lower lid 4 .<br />
During the freezing portion of the<br />
procedure, ice crystals known as an ‘ice ball’<br />
will form on the skin <strong>and</strong> should be allowed<br />
to exp<strong>and</strong> for 2mm or 3mm beyond the edge<br />
of the probe 4 . For larger areas of<br />
involvement, applications are made in an<br />
overlapping manner. The cryoprobe tip must<br />
be in firm contact with the tissue at the<br />
time of freezing without fluid between the<br />
two surfaces 16 .<br />
The thaw portion of the procedure<br />
typically takes 30 seconds <strong>and</strong> is considered<br />
complete when there is no evidence of ice<br />
crystals on the skin or conjunctiva 1 .<br />
Irrigation should not be used during the<br />
thaw. The maximum effect is achieved if the<br />
freeze is rapid, the thaw is slow, <strong>and</strong> the<br />
freeze-thaw cycle is repeated 14 . The<br />
lashes are then removed after the second<br />
cryo-treatment using forceps, <strong>and</strong> a<br />
steroid-antibiotic ointment is applied to the<br />
treated area three times a day for four days 1 .<br />
Significant inflammation, swelling, burning<br />
<strong>and</strong> pain occurs within the first 48 to 72<br />
hours post-operatively 10 . Systemic analgesics<br />
or narcotics can be prescribed.<br />
The double freeze-thaw technique using a<br />
cryoprobe has a success rate as high as<br />
84% 22 . This is because relatively large areas<br />
can be treated quickly <strong>and</strong> easily, small<br />
lashes which are difficult to epilate often<br />
respond well, <strong>and</strong> the procedure can be<br />
repeated as necessary 16 . Approximately 20%<br />
of patients do experience complications such<br />
www.optometry.co.uk<br />
as scarring, eyelid margin disruption, eyelid<br />
thinning, eyelash recurrence, loss of normal<br />
eyelashes, pigmentary skin changes,<br />
exacerbations of ocular cicatricial<br />
pemphigoid, <strong>and</strong> damage to the globe 1 .<br />
Although cryotherapy can be used to treat<br />
trichiasis in ocular cicatricial pemphigoid, it<br />
can cause further damage to the tear film<br />
<strong>and</strong> sometimes exacerbate the inflammatory<br />
response 2 . Cicatricial pemphigoid is a<br />
systemic autoimmune disorder characterised<br />
by inflammatory lesions of the mucous<br />
membranes which scar <strong>and</strong>, when the<br />
conjunctiva is involved, forms symblepharon<br />
<strong>and</strong> fornix shallowing <strong>and</strong> shortening.<br />
Surgery<br />
There are several surgical approaches used in<br />
the treatment of trichiasis. A simple<br />
pentagonal wedge resection can be used to<br />
treat localised trichiasis. When trichiasis is<br />
more diffuse, more elaborate techniques are<br />
necessary. These can include the tarsal<br />
fracture operation, terminal tarsal rotation<br />
operation or anterior lamellae recession if<br />
the upper eyelid is involved.<br />
About the author<br />
Leonid Skorin Jr is a licensed optometrist<br />
<strong>and</strong> board-certificated ophthalmologist. He is<br />
fellowship-trained in neuro-ophthalmology.<br />
He has written numerous publications <strong>and</strong><br />
has lectured internationally.<br />
Please note that this article is written in the<br />
context of optometry in the US.<br />
References<br />
1. Alford MA (2001) The <strong>management</strong> of<br />
trichiasis. In Focal Points: Clinical<br />
Modules for Ophthalmologists19; 4:<br />
1-10. American Academy of<br />
Ophthalmology, San Francisco, CA.<br />
2. Langford JD, Martin RT, Nunery WR<br />
(2000) Surgical treatment of trichiasis<br />
<strong>and</strong> distichiasis. In Mauriello JA (ed)<br />
Unfavorable Results of <strong>Eyelid</strong> <strong>and</strong><br />
Lacrimal Surgery: Prevention <strong>and</strong><br />
Management, 261-274. Butterworth<br />
Heinemann, Boston.<br />
3. Wagner P, Lang GK (2000) The eyelids. In<br />
Lang GK (ed) Ophthalmology: A Pocket<br />
Textbook Atlas, 17-47. Thieme, New York.<br />
4. Nerad JA, Chang A (2001) Trichiasis. In<br />
Chen WP (ed) Oculoplastic Surgery: The<br />
Essentials, 67-73. Thieme, New York.<br />
5. Marren SE, Bartlett JD, Melore GG (2001)<br />
Diseases of the eyelids. In Bartlett JD,<br />
Jaanus SD (eds) Clinical Ocular<br />
Pharmacology 4th ed, 485-522.<br />
Butterworth Heinemann, Boston.<br />
6. Karesh JW (2000) Evaluation <strong>and</strong><br />
<strong>management</strong> of entropion. In Mauriello<br />
JA (ed) Unfavorable Results of <strong>Eyelid</strong> <strong>and</strong><br />
Lacrimal Surgery: Prevention <strong>and</strong><br />
Management, 243-259. Butterworth<br />
Heinemann, Boston.<br />
7. Tyers AG, Collin JRO (2001) Colour Atlas<br />
of Ophthalmic Plastic Surgery 2nd ed,<br />
91-94. Butterworth Heinemann, Oxford.<br />
8. Frueh BR (1981) Treatment of<br />
distichiasis with cryotherapy.<br />
Ophthalmic. Surg. 12: 100-103.<br />
9. Byrnes GA, Wilson ME (1991) Congenital<br />
distichiasis. Arch. Ophthalmol. 109:<br />
1752-1753.<br />
10. Levine MR (1997) Trichiasis can be<br />
treated in different ways. Ocular. Surg.<br />
News 15: 58.<br />
11. Anderson RL, Harvey JT (1981) Lid<br />
splitting <strong>and</strong> posterior lamella<br />
cryosurgery for congenital <strong>and</strong> acquired<br />
distichiasis. Arch. Ophthalmol. 99:<br />
631-634.<br />
12. Wolfley D (1987) Excision of individual<br />
follicles for the <strong>management</strong> of<br />
congenital distichiasis <strong>and</strong> localized<br />
trichiasis. J. Pediatr. Ophthalmol.<br />
Strabismus 24: 22-26.<br />
13. Anderson RL, Holds JB (1995)<br />
Distichiasis. In Fraunfelder FT, Roy FH,<br />
Grove J (eds) Current Ocular Therapy,<br />
4th ed, 565. WB Saunders, Philadelphia.<br />
14. Colin JR (1984) Entropion <strong>and</strong> trichiasis.<br />
In Stewart WB (ed) Ophthalmic Plastic<br />
<strong>and</strong> Reconstructive Surgery, 131-142.<br />
American Academy of Ophthalmology,<br />
San Francisco, CA.<br />
15. Skorin L (2001) Entropion <strong>and</strong> <strong>its</strong><br />
<strong>management</strong>. OT (UK) 41: 35-36.<br />
16. Boynton JR (1993) Management of<br />
cicatricial entropion, trichiasis <strong>and</strong><br />
distichiasis. In Focal Points: Clinical<br />
Modules for Ophthalmologists 11; 12:<br />
1-9. American Academy of<br />
Ophthalmology, San Francisco, CA.<br />
17. Mondino BJ (1977) Bullous diseases of<br />
the skin <strong>and</strong> mucous membranes. In<br />
Tasman W, Jaeger EA (eds) Duane’s<br />
Clinical Ophthalmology Vol. 4, 1-19.<br />
Lippincott-Raven, Philadelphia.<br />
18. Foster CS (1977) The eye in skin <strong>and</strong><br />
mucous membrane disorders. In Tasman<br />
W, Jaeger EA (eds) Duane’s Clinical<br />
Ophthalmology Vol. 5, 1-41.<br />
Lippincott-Raven, Philadelphia.<br />
19. Fleming JC, Cape RC (1996) Surgical<br />
intervention in conjunction with medical<br />
treatment of cicatricial pemphigoid. In<br />
Bosniak S (ed) Principles <strong>and</strong> Practice of<br />
Ophthalmic Plastic <strong>and</strong> Reconstructive<br />
Surgery Vol. 1, 196-202. Saunders,<br />
Philadelphia.<br />
20. Kezirian GM (1993) Treatment of<br />
localized trichiasis with radiosurgery.<br />
Ophthal. Plast. Reconstr. Surg. 9:<br />
260-266.<br />
21. Bartley GB, Lowry JC (1992) Argon<br />
laser treatment of trichiasis.<br />
Am. J. Ophthalmol. 113: 71-74.<br />
22. Johnson RL, Collin JR (1985) Treatment<br />
of trichiasis with a lid cryoprobe.<br />
Br. J. Ophthalmol. 69: 267-270.<br />
37