Hordeolum and chalazion treatment The full gamut
Hordeolum and chalazion treatment The full gamut
Hordeolum and chalazion treatment The full gamut
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
Leonid Skorin Jr, OD, DO, FAAO, FAOCO<br />
<strong>Hordeolum</strong> <strong>and</strong> <strong>chalazion</strong> <strong>treatment</strong><br />
<strong>The</strong> <strong>full</strong> <strong>gamut</strong><br />
Hordeola <strong>and</strong> chalazia are some of the most<br />
common inflammatory eyelid disorders<br />
encountered in optometric practice. Many<br />
patients try to treat these lesions conservatively<br />
using home remedies or over-the-counter<br />
medication. Often, such <strong>treatment</strong> is efficacious<br />
<strong>and</strong> the lesion resolves as intended. In those<br />
individuals where the condition persists, the<br />
optometrist may be consulted for more definitive<br />
care.<br />
Internal hordeolum<br />
Signs <strong>and</strong> symptoms<br />
An internal hordeolum (meibomian stye) is a<br />
small abscess caused by an acute staphylococcal<br />
infection of the meibomian gl<strong>and</strong>s of the tarsus<br />
(Figure 1) 1 . <strong>The</strong>se lesions may occur in<br />
conjunction with acute or chronic blepharitis.<br />
<strong>The</strong>y point posteriorly <strong>and</strong> often rupture<br />
spontaneously <strong>and</strong> drain through the<br />
conjunctival surface 2 . A specific change in<br />
meibomian gl<strong>and</strong> secretion has been linked to<br />
internal hordeolum formation 3 .<br />
Figure 1 Internal hordeolum<br />
scrubs with a mild shampoo also helps to remove<br />
any debris, which may have accumulated on the<br />
eyelid margin surface, <strong>and</strong> in those patients with<br />
blepharitis. Because staphylococcus species are<br />
usually the underlying causes of the infection,<br />
primary medical therapy should consist of a<br />
penicillinase-resistant penicillin such as<br />
dicloxacillin. Dosages of 125mg to 250mg every<br />
six hours, usually result in prompt resolution of<br />
the infection 5 . Patients who are allergic to<br />
penicillin can try oral erythromycin,<br />
chloramphenicol or the aminoglycosides 2 . Finally,<br />
in cases which resist medical therapy, incision<br />
<strong>and</strong> drainage using a sterile needle or blade may<br />
be necessary 5 .<br />
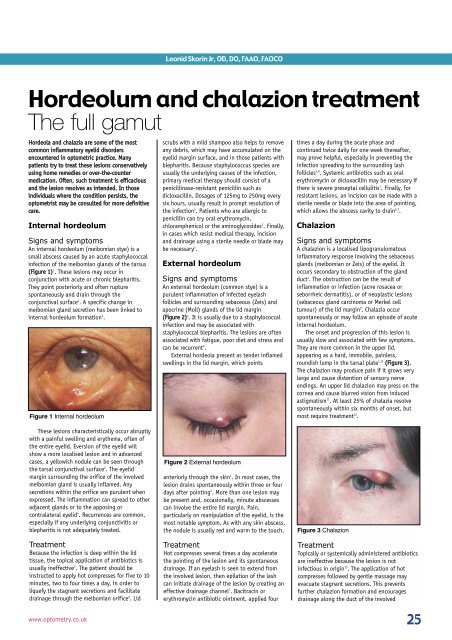
External hordeolum<br />
Signs <strong>and</strong> symptoms<br />
An external hordeolum (common stye) is a<br />
purulent inflammation of infected eyelash<br />
follicles <strong>and</strong> surrounding sebaceous (Zeis) <strong>and</strong><br />
apocrine (Moll) gl<strong>and</strong>s of the lid margin<br />
(Figure 2) 4 . It is usually due to a staphylococcal<br />
infection <strong>and</strong> may be associated with<br />
staphylococcal blepharitis. <strong>The</strong> lesions are often<br />
associated with fatigue, poor diet <strong>and</strong> stress <strong>and</strong><br />
can be recurrent 6 .<br />
External hordeola present as tender inflamed<br />
swellings in the lid margin, which points<br />
times a day during the acute phase <strong>and</strong><br />
continued twice daily for one week thereafter,<br />
may prove helpful, especially in preventing the<br />
infection spreading to the surrounding lash<br />
follicles 5,8 . Systemic antibiotics such as oral<br />
erythromycin or dicloxacillin may be necessary if<br />
there is severe preseptal cellulitis 1 . Finally, for<br />
resistant lesions, an incision can be made with a<br />
sterile needle or blade into the area of pointing,<br />
which allows the abscess cavity to drain 6,7 .<br />
Chalazion<br />
Signs <strong>and</strong> symptoms<br />
A <strong>chalazion</strong> is a localised lipogranulomatous<br />
inflammatory response involving the sebaceous<br />
gl<strong>and</strong>s (meibomian or Zeis) of the eyelid. It<br />
occurs secondary to obstruction of the gl<strong>and</strong><br />
duct 4 . <strong>The</strong> obstruction can be the result of<br />
inflammation or infection (acne rosacea or<br />
seborrheic dermatitis), or of neoplastic lesions<br />
(sebaceous gl<strong>and</strong> carcinoma or Merkel cell<br />
tumour) of the lid margin 9 . Chalazia occur<br />
spontaneously or may follow an episode of acute<br />
internal hordeolum.<br />
<strong>The</strong> onset <strong>and</strong> progression of this lesion is<br />
usually slow <strong>and</strong> associated with few symptoms.<br />
<strong>The</strong>y are more common in the upper lid,<br />
appearing as a hard, immobile, painless,<br />
roundish lump in the tarsal plate 1,10 (Figure 3).<br />
<strong>The</strong> <strong>chalazion</strong> may produce pain if it grows very<br />
large <strong>and</strong> cause distention of sensory nerve<br />
endings. An upper lid <strong>chalazion</strong> may press on the<br />
cornea <strong>and</strong> cause blurred vision from induced<br />
astigmatism 11 . At least 25% of chalazia resolve<br />
spontaneously within six months of onset, but<br />
most require <strong>treatment</strong> 12 .<br />
<strong>The</strong>se lesions characteristically occur abruptly<br />
with a painful swelling <strong>and</strong> erythema, often of<br />
the entire eyelid. Eversion of the eyelid will<br />
show a more localised lesion <strong>and</strong> in advanced<br />
cases, a yellowish nodule can be seen through<br />
the tarsal conjunctival surface 2 . <strong>The</strong> eyelid<br />
margin surrounding the orifice of the involved<br />
meibomian gl<strong>and</strong> is usually inflamed. Any<br />
secretions within the orifice are purulent when<br />
expressed. <strong>The</strong> inflammation can spread to other<br />
adjacent gl<strong>and</strong>s or to the apposing or<br />
contralateral eyelid 4 . Recurrences are common,<br />
especially if any underlying conjunctivitis or<br />
blepharitis is not adequately treated.<br />
Treatment<br />
Because the infection is deep within the lid<br />
tissue, the topical application of antibiotics is<br />
usually ineffective 5 . <strong>The</strong> patient should be<br />
instructed to apply hot compresses for five to 10<br />
minutes, two to four times a day, in order to<br />
liquefy the stagnant secretions <strong>and</strong> facilitate<br />
drainage through the meibomian orifice 2 . Lid<br />
www.optometry.co.uk<br />
Figure 2 External hordeolum<br />
anteriorly through the skin 1 . In most cases, the<br />
lesion drains spontaneously within three or four<br />
days after pointing 5 . More than one lesion may<br />
be present <strong>and</strong>, occasionally, minute abscesses<br />
can involve the entire lid margin. Pain,<br />
particularly on manipulation of the eyelid, is the<br />
most notable symptom. As with any skin abscess,<br />
the nodule is usually red <strong>and</strong> warm to the touch.<br />
Treatment<br />
Hot compresses several times a day accelerate<br />
the pointing of the lesion <strong>and</strong> its spontaneous<br />
drainage. If an eyelash is seen to extend from<br />
the involved lesion, then epilation of the lash<br />
can initiate drainage of the lesion by creating an<br />
effective drainage channel 7 . Bacitracin or<br />
erythromycin antibiotic ointment, applied four<br />
Figure 3 Chalazion<br />
Treatment<br />
Topically or systemically administered antibiotics<br />
are ineffective because the lesion is not<br />
infectious in origin 13 . <strong>The</strong> application of hot<br />
compresses followed by gentle massage may<br />
evacuate stagnant secretions. This prevents<br />
further <strong>chalazion</strong> formation <strong>and</strong> encourages<br />
drainage along the duct of the involved<br />
25
ot<br />
gl<strong>and</strong> – which may be of benefit if the lesion is<br />
small 2 . Vigorous massage can cause further<br />
extravasation of the meibomian secretions into<br />
the surrounding tissue, spreading the<br />
granulomatous inflammation 2 . Regrettably, this<br />
<strong>treatment</strong> is not very effective, resolving only<br />
around 40% of these lesions 13,14 .<br />
Chalazia which fail to resolve with<br />
conservative management may be treated with an<br />
intralesional injection of steroid 14 . This technique<br />
increases the resolution rate to 80%, while<br />
combining the conservative therapy with steroid<br />
injection increases the resolution rate to 90% 14 .<br />
Since the <strong>chalazion</strong> is encapsulated by<br />
connective tissue, there is little room for<br />
space-occupying steroid medication. <strong>The</strong>refore,<br />
a steroid of increased concentration such as<br />
triamcinolone acetomide (Kenalog-40), a<br />
40mg/ml concentration works well since<br />
only a 0.10-0.20cc dose needs to be injected<br />
(Figure 4).<br />
<strong>The</strong> chalazia can be injected through the skin<br />
surface or the conjunctival side using a 1ml<br />
tuberculin syringe with a 27-gauge or 30-gauge<br />
needle. <strong>The</strong> steroid suspension should be<br />
injected into the centre of the lesion. If injection<br />
is performed from the conjunctival side, several<br />
drops of a topical anaesthetic to numb the<br />
puncture site <strong>and</strong> minimise blinking. Injection<br />
through the skin surface of the eyelid requires no<br />
anaesthesia. Some practitioners prefer to use a<br />
<strong>chalazion</strong> clamp, but this is not always necessary.<br />
Chalazia typically resolve within one or two weeks<br />
after a single injection, but larger chalazia may<br />
require a second injection.<br />
This technique is safe <strong>and</strong> effective. <strong>The</strong>re has<br />
been one reported case of a serious complication<br />
resulting in both retinal <strong>and</strong> choroidal vascular<br />
occlusion from embolisation of the injected<br />
steroid 15 . To minimise the chances of this<br />
occurring, practitioners should aspirate for blood<br />
before injecting, take care to inject slowly, <strong>and</strong><br />
avoid heavy digital pressure during <strong>and</strong> after<br />
injection 16 . Other less serious complications<br />
include pain on injection, depigmentation of the<br />
eyelid at the injection site, temporary skin<br />
atrophy <strong>and</strong> subcutaneous white (steroid)<br />
deposits (Figure 5) 5 .<br />
Figure 5<br />
Subcutaneous white (steroid) deposits<br />
after intralesional triamcinolone injection<br />
<strong>The</strong> most reliable therapy involves surgical<br />
excision of the affected meibomian gl<strong>and</strong><br />
(Figures 6-9). <strong>The</strong> surrounding eyelid tissue<br />
needs to be injected with the anaesthetic<br />
Figure 9<br />
Forceps pointing to excised gl<strong>and</strong><br />
after it has been cleaned of debris<br />
Xylocaine (lidocaine). <strong>The</strong> eyelid is everted <strong>and</strong> a<br />
traction suture is placed through the eyelid<br />
margin. <strong>The</strong>n a <strong>chalazion</strong> clamp is positioned<br />
over the lesion. This helps stabilise the eyelid<br />
<strong>and</strong> assists in hemostasis. A surgical #11 or #15<br />
straight blade or a circular trephine blade is<br />
used to incise the involved meibomian gl<strong>and</strong><br />
through the conjunctival surface. A curette is<br />
then used to scrape out the chronic<br />
granulomatous debris.<br />
<strong>The</strong> <strong>chalazion</strong> clamp <strong>and</strong> traction suture are<br />
removed <strong>and</strong> the eyelid is repositioned. Digital<br />
pressure is applied until all the bleeding has<br />
stopped. <strong>The</strong> eye is treated with antibiotic<br />
ointment, which the patient should continue to<br />
use two times a day for five to seven days. <strong>The</strong><br />
patient should be re-evaluated after about two<br />
weeks.<br />
<strong>The</strong>re are usually few complications from this<br />
surgery. <strong>The</strong> eyelid may be swollen <strong>and</strong><br />
discoloured after the surgery for several days to<br />
one week. Occasionally, a subconjunctival<br />
haemorrhage can also develop, but this will<br />
resolve without incident (Figure 10). On rare<br />
occasions, the <strong>chalazion</strong> may recur if the<br />
surgical excision was incomplete.<br />
Figure 6<br />
Injection of eyelid with the anaesthetic,<br />
Xylocaine (lidocaine)<br />
Figure 4<br />
Setup for steroid injection for chalazia<br />
Locally injected steroid suspension works<br />
because a <strong>chalazion</strong> is composed of steroidsensitive<br />
histocytes, multi-nucleated giant cells,<br />
lymphocytes, plasma cells, polymorphonuclear<br />
leukocytes, <strong>and</strong> eosinophils 4 . <strong>The</strong> injected steroid<br />
suppresses additional inflammatory cells <strong>and</strong><br />
impedes chronic fibrosis.<br />
Figure 7<br />
Chalazion clamp <strong>and</strong> traction suture in place<br />
Figure 8<br />
Currette adjacent to granulomatous debris<br />
scraped from inside the meibomian gl<strong>and</strong><br />
Figure 10<br />
Child with eyelid ecchymosis <strong>and</strong><br />
subconjunctival haemorrhage after surgical<br />
excision of <strong>chalazion</strong><br />
Pyogenic granuloma<br />
Signs <strong>and</strong> symptoms<br />
A pyogenic granuloma may be seen after trauma<br />
or surgery, or may form over inflammatory<br />
lesions, such as chalazia. <strong>The</strong>se nodules occur<br />
rarely in the anophthalmic socket following<br />
enucleation of the eye <strong>and</strong> at the margin of<br />
corneal transplants 17 .<br />
<strong>The</strong>se lesions occur on the conjunctival side<br />
of the eyelid <strong>and</strong> are fleshy, red, usually sessile<br />
with a palpable rigid either non-tender or<br />
moderately tender presentation (Figure 11).<br />
Microscopically, a pyogenic granuloma is<br />
26<br />
June 28, 2002 OT<br />
www.optometry.co.uk
Figure 11<br />
Pyogenic granuloma<br />
composed of granulation tissue with chronic<br />
inflammatory cells, fibroblasts, <strong>and</strong> endothelial<br />
cells of budding capillaries. <strong>The</strong> term pyogenic<br />
granuloma is actually a misnomer since the<br />
lesion is neither pyogenic nor granulomatous 18 .<br />
Treatment<br />
Treatment consists of complete excision <strong>and</strong><br />
curettement of any underlying inflammatory<br />
eyelid lesion such as a <strong>chalazion</strong>. Pathologic<br />
evaluation is also recommended, since several<br />
other benign <strong>and</strong> malignant neoplasms, such as<br />
Kaposi’s sarcoma, may simulate pyogenic<br />
granuloma 17 .<br />
About the author<br />
Dr Leonid Skorin Jr is a licensed optometrist <strong>and</strong><br />
a board-certified ophthalmologist. He is<br />
fellowship trained in neuro-ophthalmology. He<br />
has numerous publications <strong>and</strong> has lectured<br />
internationally.<br />
References<br />
1. Kanski JJ (1991) Clinical Ophthalmology 4th<br />
ed. Butterworth-Heinemann, Boston,<br />
p. 12-14.<br />
2. Kaufman HE, Barron BA, McDonald MB,<br />
Kaufman SC (eds) (2000) Companion<br />
H<strong>and</strong>book to the Cornea 2nd ed.<br />
Butterworth-Heinemann, Boston, p. 29-33.<br />
3. Shine WE, McCulley JP (1996) Meibomian<br />
gl<strong>and</strong> triglyceride fatty acid differences in<br />
chronic blepharitis patients.<br />
Cornea 15: 340-346.<br />
4. Bertucci GM (2001) Periocular skin lesions<br />
<strong>and</strong> common eyelid tumors. In: Chen WP<br />
(ed) Oculoplastic Surgery: <strong>The</strong> Essentials.<br />
Thieme, New York, p. 225-241.<br />
5. Marren SE, Bartlett JD, Melore GG (2001)<br />
Diseases of the eyelids. In: Bartlett JD,<br />
Jaanus SD (eds) Clinical Ocular<br />
Pharmacology 4th ed. Butterworth-<br />
Heinemann, Boston, p. 485-522.<br />
6. Alex<strong>and</strong>er KL (1980) Some inflammations of<br />
the external eye <strong>and</strong> adnexa.<br />
J. Am. Optom. Assoc. 51: 142-146.<br />
7. Hudson RL (1981) Treatment of styes <strong>and</strong><br />
meibomian cysts. Practical procedures.<br />
Aust. Fam. Phys. 10: 714-717.<br />
8. Trevor-Roper PD (1974)Diseases of the<br />
eyelids. Int. Ophthalmol. Clin. 14: 362-393.<br />
9. Font RL (1986) Eyelids <strong>and</strong> lacrimal<br />
drainage system. In: Spencer WH (ed)<br />
Ophthalmic Pathology: An Atlas <strong>and</strong><br />
Textbook. WB Saunders, Philadelphia,<br />
p. 2141-2336.<br />
10. Gershen HJ (1985) Chalazion. In:<br />
Fraunfelder FT, Roy FH (eds) Current Ocular<br />
<strong>The</strong>rapy 2nd ed. WB Saunders, Philadelphia,<br />
p. 354-355.<br />
11. Nisted M, Hofstetter HW (1974) Effect of<br />
<strong>chalazion</strong> on astigmatism.<br />
Am. J. Optom. Physiol. Opt. 51: 579-582.<br />
12.Cottrell DG, Bosanquet RC, Fawcett IM<br />
(1983) Chalazions: the frequency of<br />
spontaneous resolution. BMJ<br />
1983; 287-1595.<br />
13.Bohigian GM (1979) Chalazion: a clinical<br />
evaluation. Am. Ophthalmol. 11:<br />
1397-1398.<br />
14. Garrett GW, Gillespie ME, Mannix BC (1988)<br />
Adrenocorticosteroid injection vs.<br />
conservative therapy in the <strong>treatment</strong> of<br />
chalazia. Am. Ophthalmol. 20:<br />
196-198.<br />
15.Thomas EL, Laborde RP (1986) Retinal <strong>and</strong><br />
choroidal vascular occlusion following<br />
intralesional corticosteroid injection of a<br />
<strong>chalazion</strong>. Ophthalmology 93: 405-407.<br />
16. Francis BA, Chang EL, Haik BG (1996)<br />
Particle size <strong>and</strong> drug interactions of<br />
injectable corticosteroids used in<br />
ophthalmic practice. Ophthalmology<br />
103: 1884-1888.<br />
17. Skorin L (2000) Corneal <strong>and</strong> eyelid<br />
anomalies. Consultant 40: 265-272.<br />
18.Griffith DG, Salasche SJ, Clemons DE (1987)<br />
Cutaneous Abnormalities of the Eyelid<br />
<strong>and</strong> Face: An Atlas With Histopathology.<br />
McGraw-Hill, New York, p. 136-137.<br />
www.optometry.co.uk<br />
27