Annual General Meeting of the Irish Thoracic Society - IJMS | Irish ...
Annual General Meeting of the Irish Thoracic Society - IJMS | Irish ...
Annual General Meeting of the Irish Thoracic Society - IJMS | Irish ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
31<br />
1<br />
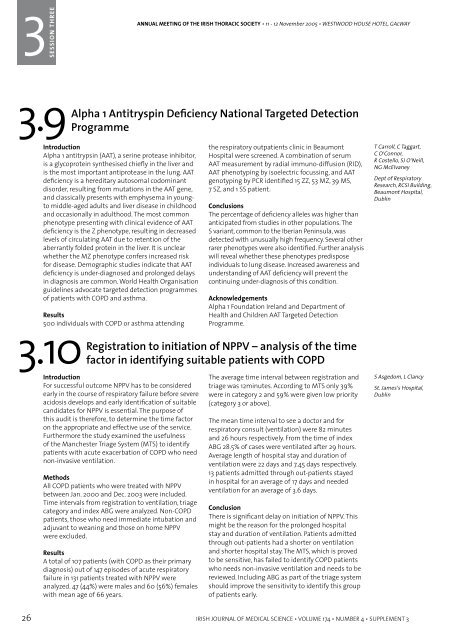
SESSION THREE ONE<br />
ANNUAL MEETING OF THE IRISH THORACIC SOCIETY • 11 - 12 November 2005 • WESTWOOD HOUSE HOTEL, GALWAY<br />
ANNUAL MEETING OF THE IRISH THORACIC SOCIETY • 11 - 12 November 2005 • WESTWOOD HOUSE HOTEL, GALWAY<br />
3<br />
SESSION<br />
SESSION THREE ONE<br />
3.9<br />
Alpha 1 Antitryspin Deficiency National Targeted Detection<br />
Programme<br />
Introduction<br />
Alpha 1 antitrypsin (AAT), a serine protease inhibitor,<br />
is a glycoprotein syn<strong>the</strong>sised chiefly in <strong>the</strong> liver and<br />
is <strong>the</strong> most important antiprotease in <strong>the</strong> lung. AAT<br />
deficiency is a hereditary autosomal codominant<br />
disorder, resulting from mutations in <strong>the</strong> AAT gene,<br />
and classically presents with emphysema in youngto<br />
middle-aged adults and liver disease in childhood<br />
and occasionally in adulthood. The most common<br />
phenotype presenting with clinical evidence <strong>of</strong> AAT<br />
deficiency is <strong>the</strong> Z phenotype, resulting in decreased<br />
levels <strong>of</strong> circulating AAT due to retention <strong>of</strong> <strong>the</strong><br />
aberrantly folded protein in <strong>the</strong> liver. It is unclear<br />
whe<strong>the</strong>r <strong>the</strong> MZ phenotype confers increased risk<br />
for disease. Demographic studies indicate that AAT<br />
deficiency is under-diagnosed and prolonged delays<br />
in diagnosis are common. World Health Organisation<br />
guidelines advocate targeted detection programmes<br />
<strong>of</strong> patients with COPD and asthma.<br />
Results<br />
500 individuals with COPD or asthma attending<br />
3.10<br />
<strong>the</strong> respiratory outpatients clinic in Beaumont<br />
Hospital were screened. A combination <strong>of</strong> serum<br />
AAT measurement by radial immuno-diffusion (RID),<br />
AAT phenotyping by isoelectric focussing, and AAT<br />
genotyping by PCR identified 15 ZZ, 53 MZ, 39 MS,<br />
7 SZ, and 1 SS patient.<br />
Conclusions<br />
The percentage <strong>of</strong> deficiency alleles was higher than<br />
anticipated from studies in o<strong>the</strong>r populations. The<br />
S variant, common to <strong>the</strong> Iberian Peninsula, was<br />
detected with unusually high frequency. Several o<strong>the</strong>r<br />
rarer phenotypes were also identified. Fur<strong>the</strong>r analysis<br />
will reveal whe<strong>the</strong>r <strong>the</strong>se phenotypes predispose<br />
individuals to lung disease. Increased awareness and<br />
understanding <strong>of</strong> AAT deficiency will prevent <strong>the</strong><br />
continuing under-diagnosis <strong>of</strong> this condition.<br />
Acknowledgements<br />
Alpha 1 Foundation Ireland and Department <strong>of</strong><br />
Health and Children AAT Targeted Detection<br />
Programme.<br />
Registration to initiation <strong>of</strong> NPPV – analysis <strong>of</strong> <strong>the</strong> time<br />
factor in identifying suitable patients with COPD<br />
T Carroll, C Taggart,<br />
C O’Connor,<br />
R Costello, SJ O’Neill,<br />
NG McElvaney<br />
Dept <strong>of</strong> Respiratory<br />
Research, RCSI Building,<br />
Beaumont Hospital,<br />
Dublin<br />
3.11<br />
Audit on non-invasive ventilation (NIV) and its<br />
effectiveness in an exacerbation <strong>of</strong> chronic obstructive<br />
pulmonary disease (COPD)<br />
Introduction<br />
The British <strong>Thoracic</strong> <strong>Society</strong> (BTS) published guidelines<br />
on <strong>the</strong> use <strong>of</strong> (NIV) in 2002 (Thorax 2002: 57: 192-211).<br />
On introducing this service in June 2004, we wished<br />
to determine its effectiveness <strong>of</strong> <strong>the</strong> Harmony Bipap<br />
machine (Respironics Inc), and <strong>the</strong> compatibility <strong>of</strong> our<br />
service with <strong>the</strong> BTS guidelines.<br />
Method<br />
We preformed an audit on all patients that received<br />
NIV from June 04 to May 05, using <strong>the</strong> NIV audit sheet<br />
from <strong>the</strong> BTS guidelines.<br />
Results<br />
Number <strong>of</strong> patients treated were fifteen, with two<br />
requiring a second application <strong>of</strong> NIV, (F=4,M=11).<br />
Diagnosis; 80% had COPD, 6% had COPD and asthma<br />
and 6% had COPD and obesity. Number <strong>of</strong> chest<br />
x-rays preformed prior to initiation = (Yes-16 + No-<br />
1).Arterial blood gases (ABG) prior to initiation = (Y-17<br />
+ N-0).ABG’s preformed pre-discharge = (Y-12 + N-5).<br />
Spirometery preformed pre-discharge = (Y-6 + No-11).<br />
Documentation <strong>of</strong> informed consent and action to<br />
taken if NIV fails = (Y-6 + No-11). Average length <strong>of</strong><br />
stay <strong>of</strong> those treated with NIV = 12.5 days, and those<br />
receiving conservative treatment prior to <strong>the</strong> NIV<br />
service = 18.3 days. Benefits <strong>of</strong> NIV = (Y-13 + No-4).<br />
Final outcome was fourteen were discharged home,<br />
one was a bridge to mechanical ventilation and two<br />
died a few days later. Follow up as an outpatient = (Y-6<br />
+ No-9).<br />
Conclusions<br />
Marked improvements for patients treated with<br />
NIV. Reduced hospital stay and morbidity. Less need<br />
for intubations and it proved cost effective. Some<br />
<strong>of</strong> <strong>the</strong> recommendations made are; Proper written<br />
documentation regarding consent, prognosis<br />
and options if NIV fails. Early initiation <strong>of</strong> NIV. All<br />
patients followed up at outpatients. A new pr<strong>of</strong>orma<br />
based on <strong>the</strong> BTS guidelines. Induction for all new<br />
Junior Doctors on NIV and <strong>the</strong> use <strong>of</strong> <strong>the</strong> Harmony<br />
machine.12 monthly updates on NIV for all nurses and<br />
physio’s on medical ward. Changes to be considered;<br />
Dedicated respiratory beds with specialised nursing<br />
staff. An ABG analyser for medical ward. Domiciliary<br />
NIV service to be considered for <strong>the</strong> future<br />
TA Howe, JR Williams,<br />
G Shivashanker,<br />
M Jadoon, F Hardoo<br />
Medical ward, Erne<br />
Hospital, Enniskillen,<br />
Co Fermanagh<br />
Introduction<br />
For successful outcome NPPV has to be considered<br />
early in <strong>the</strong> course <strong>of</strong> respiratory failure before severe<br />
acidosis develops and early identification <strong>of</strong> suitable<br />
candidates for NPPV is essential. The purpose <strong>of</strong><br />
this audit is <strong>the</strong>refore, to determine <strong>the</strong> time factor<br />
on <strong>the</strong> appropriate and effective use <strong>of</strong> <strong>the</strong> service.<br />
Fur<strong>the</strong>rmore <strong>the</strong> study examined <strong>the</strong> usefulness<br />
<strong>of</strong> <strong>the</strong> Manchester Triage System (MTS) to identify<br />
patients with acute exacerbation <strong>of</strong> COPD who need<br />
non-invasive ventilation.<br />
Methods<br />
All COPD patients who were treated with NPPV<br />
between Jan. 2000 and Dec. 2003 were included.<br />
Time intervals from registration to ventilation, triage<br />
category and index ABG were analyzed. Non-COPD<br />
patients, those who need immediate intubation and<br />
adjuvant to weaning and those on home NPPV<br />
were excluded.<br />
Results<br />
A total <strong>of</strong> 107 patients (with COPD as <strong>the</strong>ir primary<br />
diagnosis) out <strong>of</strong> 147 episodes <strong>of</strong> acute respiratory<br />
failure in 131 patients treated with NPPV were<br />
analyzed. 47 (44%) were males and 60 (56%) females<br />
with mean age <strong>of</strong> 66 years.<br />
The average time interval between registration and<br />
triage was 12minutes. According to MTS only 39%<br />
were in category 2 and 59% were given low priority<br />
(category 3 or above).<br />
The mean time interval to see a doctor and for<br />
respiratory consult (ventilation) were 82 minutes<br />
and 26 hours respectively. From <strong>the</strong> time <strong>of</strong> index<br />
ABG 28.5% <strong>of</strong> cases were ventilated after 29 hours.<br />
Average length <strong>of</strong> hospital stay and duration <strong>of</strong><br />
ventilation were 22 days and 7.45 days respectively.<br />
13 patients admitted through out-patients stayed<br />
in hospital for an average <strong>of</strong> 17 days and needed<br />
ventilation for an average <strong>of</strong> 3.6 days.<br />
Conclusion<br />
There is significant delay on initiation <strong>of</strong> NPPV. This<br />
might be <strong>the</strong> reason for <strong>the</strong> prolonged hospital<br />
stay and duration <strong>of</strong> ventilation. Patients admitted<br />
through out-patients had a shorter on ventilation<br />
and shorter hospital stay. The MTS, which is proved<br />
to be sensitive, has failed to identify COPD patients<br />
who needs non-invasive ventilation and needs to be<br />
reviewed. Including ABG as part <strong>of</strong> <strong>the</strong> triage system<br />
should improve <strong>the</strong> sensitivity to identify this group<br />
<strong>of</strong> patients early.<br />
S Asgedom, L Clancy<br />
St. James’s Hospital,<br />
Dublin<br />
3.12<br />
Results post initiation <strong>of</strong> an out-patient pulmonary<br />
rehabilitation programme<br />
Introduction<br />
Despite being proven worldwide, pulmonary<br />
rehabilitation programmes are still not widely<br />
available to COPD patients in Ireland. In 2004, <strong>the</strong><br />
Respiratory Assessment Unit launched a pulmonary<br />
rehabilitation programme.<br />
Method<br />
Patients attended twice weekly for eight weeks,<br />
for one hour <strong>of</strong> exercise, and an education talk. Pre<br />
and post programme individual out-patient assessments<br />
consisted <strong>of</strong> medical history, resting values<br />
<strong>of</strong> heart rate, respiratory rate, oxygen saturation,<br />
BORG breathlessness scale, medical research council<br />
dyspnoea scale (MRCD), and inhaler technique assessment.<br />
Patients performed a six-minute walk<br />
test, three-minute step test, and pulmonary function<br />
tests including inspiratory muscle strength testing.<br />
Patients completed a hospital anxiety and depression<br />
scale (HADS), and a St. Georges Respiratory Diseases<br />
Questionnaire (SGRQ). An anonymous patient satisfaction<br />
survey was returned at <strong>the</strong> end <strong>of</strong> <strong>the</strong> programme.<br />
Results<br />
Three classes enrolled to date (39 patients in total),<br />
with 32 patients (82.1%) completing <strong>the</strong> eight weeks.<br />
Analysis <strong>of</strong> results showed significant increases in<br />
6-minute walk test (p