Annual General Meeting of the Irish Thoracic Society - IJMS | Irish ...
Annual General Meeting of the Irish Thoracic Society - IJMS | Irish ...
Annual General Meeting of the Irish Thoracic Society - IJMS | Irish ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
31<br />
1<br />
SESSION THREE ONE<br />
ANNUAL MEETING OF THE IRISH THORACIC SOCIETY • 11 - 12 November 2005 • WESTWOOD HOUSE HOTEL, GALWAY<br />
ANNUAL MEETING OF THE IRISH THORACIC SOCIETY • 11 - 12 November 2005 • WESTWOOD HOUSE HOTEL, GALWAY<br />
3<br />
SESSION<br />
SESSION THREE ONE<br />
Population Studies<br />
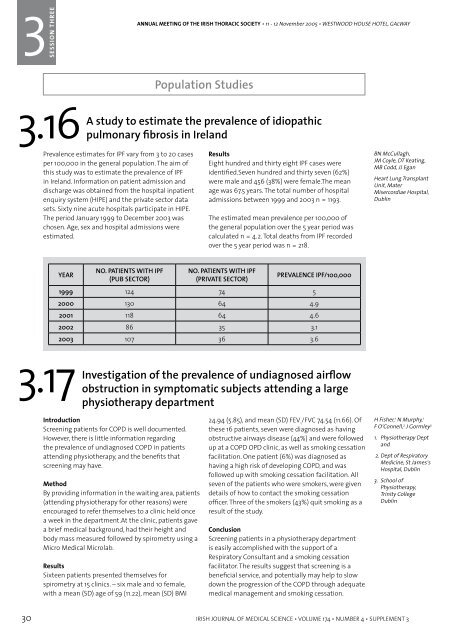
3.16<br />
A study to estimate <strong>the</strong> prevalence <strong>of</strong> idiopathic<br />
pulmonary fibrosis in Ireland<br />
3.18<br />
The effects <strong>of</strong> <strong>the</strong> workplace ban on smoking on <strong>the</strong> lung<br />
function <strong>of</strong> bar workers in Dublin<br />
Prevalence estimates for IPF vary from 3 to 20 cases<br />
per 100,000 in <strong>the</strong> general population. The aim <strong>of</strong><br />
this study was to estimate <strong>the</strong> prevalence <strong>of</strong> IPF<br />
in Ireland. Information on patient admission and<br />
discharge was obtained from <strong>the</strong> hospital inpatient<br />
enquiry system (HIPE) and <strong>the</strong> private sector data<br />
sets. Sixty nine acute hospitals participate in HIPE.<br />
The period January 1999 to December 2003 was<br />
chosen. Age, sex and hospital admissions were<br />
estimated.<br />
YEAR<br />
3.17<br />
NO. PATIENTS WITH IPF<br />
(PUB SECTOR)<br />
Investigation <strong>of</strong> <strong>the</strong> prevalence <strong>of</strong> undiagnosed airflow<br />
obstruction in symptomatic subjects attending a large<br />
physio<strong>the</strong>rapy department<br />
Introduction<br />
Screening patients for COPD is well documented.<br />
However, <strong>the</strong>re is little information regarding<br />
<strong>the</strong> prevalence <strong>of</strong> undiagnosed COPD in patients<br />
attending physio<strong>the</strong>rapy, and <strong>the</strong> benefits that<br />
screening may have.<br />
Method<br />
By providing information in <strong>the</strong> waiting area, patients<br />
(attending physio<strong>the</strong>rapy for o<strong>the</strong>r reasons) were<br />
encouraged to refer <strong>the</strong>mselves to a clinic held once<br />
a week in <strong>the</strong> department.At <strong>the</strong> clinic, patients gave<br />
a brief medical background, had <strong>the</strong>ir height and<br />
body mass measured followed by spirometry using a<br />
Micro Medical Microlab.<br />
Results<br />
Sixteen patients presented <strong>the</strong>mselves for<br />
spirometry at 15 clinics. – six male and 10 female,<br />
with a mean (SD) age <strong>of</strong> 59 (11.22), mean (SD) BMI<br />
Results<br />
Eight hundred and thirty eight IPF cases were<br />
identified.Seven hundred and thirty seven (62%)<br />
were male and 456 (38%) were female.The mean<br />
age was 67.5 years. The total number <strong>of</strong> hospital<br />
admissions between 1999 and 2003 n = 1193.<br />
The estimated mean prevalence per 100,000 <strong>of</strong><br />
<strong>the</strong> general population over <strong>the</strong> 5 year period was<br />
calculated n = 4.2. Total deaths from IPF recorded<br />
over <strong>the</strong> 5 year period was n = 218.<br />
NO. PATIENTS WITH IPF<br />
(PRIVATE SECTOR)<br />
PREVALENCE IPF/100,000<br />
1999 124 74 5<br />
2000 130 64 4.9<br />
2001 118 64 4.6<br />
2002 86 35 3.1<br />
2003 107 36 3.6<br />
24.94 (5.85), and mean (SD) FEV 1<br />
/FVC 74.54 (11.66). Of<br />
<strong>the</strong>se 16 patients, seven were diagnosed as having<br />
obstructive airways disease (44%) and were followed<br />
up at a COPD OPD clinic, as well as smoking cessation<br />
facilitation. One patient (6%) was diagnosed as<br />
having a high risk <strong>of</strong> developing COPD, and was<br />
followed up with smoking cessation facilitation. All<br />
seven <strong>of</strong> <strong>the</strong> patients who were smokers, were given<br />
details <strong>of</strong> how to contact <strong>the</strong> smoking cessation<br />
<strong>of</strong>ficer. Three <strong>of</strong> <strong>the</strong> smokers (43%) quit smoking as a<br />
result <strong>of</strong> <strong>the</strong> study.<br />
Conclusion<br />
Screening patients in a physio<strong>the</strong>rapy department<br />
is easily accomplished with <strong>the</strong> support <strong>of</strong> a<br />
Respiratory Consultant and a smoking cessation<br />
facilitator. The results suggest that screening is a<br />
beneficial service, and potentially may help to slow<br />
down <strong>the</strong> progression <strong>of</strong> <strong>the</strong> COPD through adequate<br />
medical management and smoking cessation.<br />
BN McCullagh,<br />
JM Coyle, DT Keating,<br />
MB Codd, JJ Egan<br />
Heart Lung Transplant<br />
Unit, Mater<br />
Misercordiae Hospital,<br />
Dublin<br />
H Fisher, 1 N Murphy, 1<br />
F O’Connell, 2 J Gormley 3<br />
1. Physio<strong>the</strong>rapy Dept<br />
and<br />
2. Dept <strong>of</strong> Respiratory<br />
Medicine, St James’s<br />
Hospital, Dublin<br />
3. School <strong>of</strong><br />
Physio<strong>the</strong>rapy,<br />
Trinity College<br />
Dublin<br />
Background<br />
It has long been recognised that exposure to<br />
environmental tobacco smoke causes respiratory<br />
and cardio-vascular disease in those exposed to it.<br />
Bar staff are a group <strong>of</strong> workers with long hours <strong>of</strong><br />
exposure at work, and as such, were an ideal group to<br />
study <strong>the</strong> effects <strong>of</strong> <strong>the</strong> government ban on smoking<br />
in <strong>the</strong> workplace.<br />
Methods<br />
Bar workers were recruited through <strong>the</strong>ir Trade<br />
Union, Mandate, and 81 participated in <strong>the</strong> first<br />
phase <strong>of</strong> testing between September 2003 and<br />
March 2004. They attended <strong>the</strong> Respiratory<br />
Laboratory in St. James Hospital for lung function<br />
tests and measurement <strong>of</strong> exhaled carbon monoxide.<br />
They also completed a questionnaire relating to <strong>the</strong>ir<br />
respiratory health, and smoking history. Seventy-five<br />
(93%) returned between September 2004 and March<br />
2005 for repeat testing and again completed <strong>the</strong><br />
questionnaire.<br />
Results<br />
Subject demographics: 75 completed phase 1 and<br />
phase 2, all male. Nine (12%) <strong>of</strong> <strong>the</strong>se had been<br />
diagnosed as asthmatic by a physician. For analysis<br />
two subjects were excluded due to change in<br />
smoking status on return. Thirty-four (47%) had never<br />
smoked. Thirt-one (42%) were ex-smokers. Eight (11%)<br />
were current smokers.<br />
Symptoms<br />
No. complaining<br />
<strong>of</strong> eye, nose and<br />
throat symptoms<br />
No. complaining<br />
<strong>of</strong> respiratory<br />
symptoms<br />
PHASE 1 PHASE 2 CHANGE<br />
65 (89%) 32 (44%) -51%<br />
65 (89%) 47 (64%) -28%<br />
Carbon Monoxide (CO) Measurement<br />
Mean CO levels 5.9ppm 4.2ppm -29%<br />
Lung Function Spirometry, lung volumes and<br />
gas transfer measurement were performed at<br />
both visits and showed changes as follows:<br />
Never<br />
smokers<br />
(34)<br />
Exsmokers<br />
(31)<br />
Smokers<br />
(8)<br />
FEV1 +2% -1% -5%<br />
FVC +5% +3% -3%<br />
PEF +12% +8% -2%<br />
TLC +3% +2% +2%<br />
DLCO +5% -1% -6%<br />
The figures in bold and italics are statistically significant (P