Annual General Meeting of the Irish Thoracic Society - IJMS | Irish ...
Annual General Meeting of the Irish Thoracic Society - IJMS | Irish ...
Annual General Meeting of the Irish Thoracic Society - IJMS | Irish ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
51<br />
1<br />
SESSION FIVE ONE<br />
ANNUAL MEETING OF THE IRISH THORACIC SOCIETY • 11 - 12 November 2005 • WESTWOOD HOUSE HOTEL, GALWAY<br />
Session 5: Smoking / Lung Cancer<br />
ANNUAL MEETING OF THE IRISH THORACIC SOCIETY • 11 - 12 November 2005 • WESTWOOD HOUSE HOTEL, GALWAY<br />
5<br />
SESSION<br />
SESSION FIVE ONE<br />
5.1<br />
A study to compare <strong>the</strong> efficiency <strong>of</strong> sterile talc, tetracycline<br />
and bleomycin as sclerosing agents for medical pluerodesis<br />
in <strong>the</strong> treatment <strong>of</strong> malignant pleural effusions<br />
Background<br />
Malignant pleural effusion is a common<br />
complication <strong>of</strong> metastatic disease.Particularly<br />
lung cancer, that is <strong>of</strong>ten managed by drainage<br />
and medical pleurodesis. Sterile talc, tetracycline,<br />
and bleomycin have all been shown to be effective<br />
sclerosants. No randomized clinical trial has<br />
directly compared all three agents in <strong>the</strong> medical<br />
management <strong>of</strong> malignant pleural effusion.<br />
Methods<br />
A prospective, randomised trial was carried out across<br />
multiple sites between September 2001 and August<br />
2005. After complete drainage with symptom relief,<br />
patients with confirmed malignant pleural effusions,<br />
were allocated to receive intrapleural sterile talc (5g),<br />
tetracycline (1500mg) or bleomycin (60mg). Exclusion<br />
criteria included WHO performance status >2, small<br />
cell cancers and leukaemias. Primary outcome was<br />
response rate evaluated by radiographic improvement<br />
at one month after pleurodesis.<br />
Results<br />
Seventy patients were enrolled in <strong>the</strong> study; six<br />
patients were withdrawn before pleurodesis.<br />
Demographics and pleural fluid characteristics were<br />
comparable across all three groups. One patient<br />
randomised to talc experienced adult respiratory<br />
distress syndrome (ARDS).<br />
There was no significant difference in response rates<br />
between sclerosants. While <strong>the</strong>re was a significantly<br />
higher CRP response to pleurodesis in <strong>the</strong> talc group,<br />
this was not associated with an improved response<br />
rate at one month.<br />
Conclusion<br />
There was no difference in <strong>the</strong> efficacy <strong>of</strong> sterile talc,<br />
tetracycline and bleomycin as sclerosant agents<br />
in <strong>the</strong> medical management <strong>of</strong> malignant pleural<br />
effusions.<br />
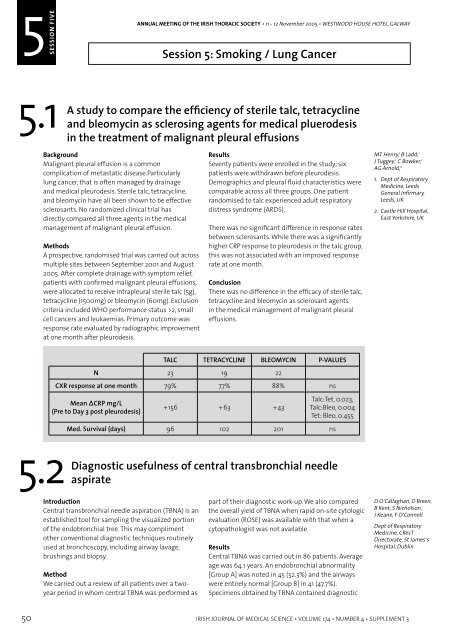
TALC TETRACYCLINE BLEOMYCIN P-VALUES<br />
N 23 19 22<br />
CXR response at one month 79% 77% 88% ns<br />
Mean ΔCRP mg/L<br />
(Pre to Day 3 post pleurodesis)<br />
+156 +63 +43<br />
Talc:Tet, 0.023,<br />
Talc:Bleo, 0.004<br />
Tet: Bleo, 0.455<br />
MT Henry, 1 B Ladd, 1<br />
J Tuggey, 1 C Bowker, 1<br />
AG Arnold, 2<br />
1. Dept <strong>of</strong> Respiratory<br />
Medicine, Leeds<br />
<strong>General</strong> Infirmary,<br />
Leeds, UK<br />
2. Castle Hill Hospital,<br />
East Yorkshire, UK<br />
5.3<br />
material in 58.1% <strong>of</strong> all patients (68.8% <strong>of</strong> Group<br />
A and 46.3% <strong>of</strong> Group B). It was <strong>the</strong> only positive<br />
procedure in 11.6% (11.1% <strong>of</strong> Group A and 12.2%<br />
<strong>of</strong> Group B). A cytopathologist attended 51.2% <strong>of</strong><br />
procedures, resulting in a diagnostic TBNA in 63.6%.<br />
In comparison, TBNA was diagnostic in 42.8% when<br />
ROSE was not performed (p=0.053).<br />
Conclusions<br />
The results suggest that central TBNA compliments<br />
o<strong>the</strong>r diagnostic techniques in evaluation <strong>of</strong> <strong>the</strong><br />
visualized portion <strong>of</strong> <strong>the</strong> endobronchial tree, and may<br />
improve diagnostic yield. This appears to be fur<strong>the</strong>r<br />
enhanced by ROSE.<br />
Diagnostic yield <strong>of</strong> fluoroscopic-guided transbronchial<br />
needle aspiration <strong>of</strong> peripheral pulmonary lesions<br />
Introduction<br />
Peripheral pulmonary lesions which are not visible<br />
within <strong>the</strong> endobronchial tree usually require<br />
radiological or surgical techniques to provide tissue<br />
diagnosis. The role <strong>of</strong> transbronchial needle aspirate<br />
(TBNA) in central lesions is well documented.<br />
However it is not routinely utilized as part <strong>of</strong> <strong>the</strong><br />
evaluation <strong>of</strong> peripheral lesions.<br />
Method<br />
We carried out a retrospective analysis <strong>of</strong> all<br />
patients over a two-year period in whom TBNA<br />
was performed as part <strong>of</strong> <strong>the</strong> diagnostic work-up<br />
<strong>of</strong> peripheral pulmonary lesions. We compared <strong>the</strong><br />
overall yield <strong>of</strong> TBNA when rapid on-site cytologic<br />
evaluation (ROSE) was available with that when a<br />
cytopathologist was not available. We also compared<br />
<strong>the</strong> diagnostic yield <strong>of</strong> TBNA with that <strong>of</strong> BAL and<br />
transbronchial biopsy (TBBx) in those patients who<br />
had all 3 tests performed and had a final diagnosis <strong>of</strong><br />
malignancy.<br />
Results<br />
Of 146 patients in whom TBNA was perfomed, 143<br />
were available for analysis. Mean age was 66 years.<br />
A cytopathologist attended for 60% <strong>of</strong> all procedures<br />
resulting in a diagnositic TBNA in 50.4%. In<br />
comparison, only 25.9% <strong>of</strong> TBNAs yielded a diagnosis<br />
when ROSE was not performed (p=0.003).<br />
Malignancy was confirmed in 56 patients by a<br />
combination <strong>of</strong> TBNA, TBBx and BAL. TBNA was<br />
positive for malignancy in 43 (76.8%) <strong>of</strong> cases, and<br />
was <strong>the</strong> only positive diagnostic procedure in 12<br />
(21.4%). TBBx was positive in 36 (64.3%) and was <strong>the</strong><br />
only positive procedure in 10 (17.9%). BAL was positive<br />
in 19 (33.9%) but was <strong>the</strong> only positive procedure in<br />
only 2 cases (3.6%).<br />
Conclusions<br />
The addition <strong>of</strong> fluoroscopic-guided TBNA to BAL and<br />
TBBx enhances <strong>the</strong> diagnostic yield <strong>of</strong> bronchoscopy<br />
in peripheral lung cancer. This appears to be fur<strong>the</strong>r<br />
enhanced by ROSE.<br />
D Breen, D O’Callaghan,<br />
B Kent, S Nicholson,<br />
J Keane, F O’Connell<br />
Dept <strong>of</strong> Respiratory<br />
Medicine and<br />
Histopathology,<br />
St James’s Hospital,<br />
Dublin<br />
5.2<br />
Med. Survival (days) 96 102 201 ns<br />
Diagnostic usefulness <strong>of</strong> central transbronchial needle<br />
aspirate<br />
Introduction<br />
Central transbronchial needle aspiration (TBNA) is an<br />
established tool for sampling <strong>the</strong> visualized portion<br />
<strong>of</strong> <strong>the</strong> endobronchial tree. This may compliment<br />
o<strong>the</strong>r conventional diagnostic techniques routinely<br />
used at bronchoscopy, including airway lavage,<br />
brushings and biopsy.<br />
Method<br />
We carried out a review <strong>of</strong> all patients over a twoyear<br />
period in whom central TBNA was performed as<br />
part <strong>of</strong> <strong>the</strong>ir diagnostic work-up. We also compared<br />
<strong>the</strong> overall yield <strong>of</strong> TBNA when rapid on-site cytologic<br />
evaluation (ROSE) was available with that when a<br />
cytopathologist was not available.<br />
Results<br />
Central TBNA was carried out in 86 patients. Average<br />
age was 64.1 years. An endobronchial abnormality<br />
[Group A] was noted in 45 (52.3%) and <strong>the</strong> airways<br />
were entirely normal [Group B] in 41 (47.7%).<br />
Specimens obtained by TBNA contained diagnostic<br />
D O’Callaghan, D Breen,<br />
B Kent, S Nicholson,<br />
J Keane, F O’Connell<br />
Dept <strong>of</strong> Respiratory<br />
Medicine, CResT<br />
Directorate, St James’s<br />
Hospital, Dublin<br />
5.4<br />
The <strong>Irish</strong> workplace smoking ban; an analysis <strong>of</strong> <strong>the</strong><br />
exposure levels in Dublin bars<br />
Introduction<br />
On <strong>the</strong> 29 th March 2004, <strong>the</strong> <strong>Irish</strong> Government<br />
introduced legislation prohibiting <strong>the</strong> consumption<br />
<strong>of</strong> tobacco products in most workplaces.<br />
Controversially, <strong>the</strong> ban applied to <strong>the</strong> hospitality<br />
industry, including licensed premises. The time<br />
prior and subsequent to <strong>the</strong> introduction <strong>of</strong> <strong>the</strong> ban<br />
provided an opportunity to assess <strong>the</strong> exposure<br />
levels <strong>of</strong> particulates and benzene in Dublin pubs,<br />
and <strong>the</strong> effectiveness <strong>of</strong> <strong>the</strong> new legislation at<br />
protecting workers and patrons from unnecessary<br />
exposure to Environmental Tobacco Smoke<br />
Method<br />
Particulate levels (PM2.5 and PM10) were measured<br />
in 43 pubs, prior and subsequent to <strong>the</strong> introduction<br />
<strong>of</strong> <strong>the</strong> smoking ban, using a light scattering optical<br />
based instrument (Aerocet 531). For consistency<br />
purposes, repeat measurements were conducted<br />
on <strong>the</strong> same day <strong>of</strong> <strong>the</strong> week, and <strong>the</strong> same month,<br />
one year later from <strong>the</strong> original measurements.<br />
Simultaneously, benzene levels were monitored<br />
using passive benzene badges incorporating an<br />
activated carbon absorption element. In each public<br />
house, <strong>the</strong> benzene sampler was co-located with<br />
<strong>the</strong> AEROCET monitor, as near as possible to <strong>the</strong><br />
breathing zone.<br />
M McCaffrey, 1<br />
PG Goodman, 2<br />
L Clancy 3<br />
1. Dublin City Council<br />
2. Dublin Institute <strong>of</strong><br />
Technology,<br />
3. Research Institute<br />
for a Tobacco Free<br />
<strong>Society</strong><br />
50 IRISH JOURNAL OF MEDICAL SCIENCE • VOLUME 174 • NUMBER 4 • SUPPLEMENT 3<br />
IRISH JOURNAL OF MEDICAL SCIENCE • VOLUME 174 • NUMBER 4 • SUPPLEMENT 3 51