primary prevention of coeliac disease - Associazione Italiana ...
primary prevention of coeliac disease - Associazione Italiana ...
primary prevention of coeliac disease - Associazione Italiana ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
Perspectives on Coeliac Disease<br />
Volume I<br />
PRIMARY PREVENTION<br />
OF COELIAC DISEASE<br />
THE UTOPIA<br />
OF THE NEW MILLENNIUM?<br />
EDITED BY<br />
CARLO CATASSI<br />
ALESSIO FASANO<br />
GINO ROBERTO CORAZZA<br />
AIC Press
PRIMARY PREVENTION<br />
OF COELIAC DISEASE<br />
THE UTOPIA OF THE NEW MILLENNIUM ?
The AIC Meeting was held in the Aula Scarpa <strong>of</strong> the University <strong>of</strong> Pavia, Italy, October 12,<br />
2001.<br />
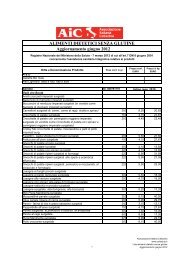
Meeting participants (left to right, from back to front): P. Ciclitira, F. Koning, L. Sollid, R.<br />
Anderson, R. Troncone, M. Mäki, A. Fasano, G. Gasbarrini, F. Cucca, M. Stern, C. Feighery,<br />
G.R. Corazza, C. Catassi, P. Howdle, G. Holmes.
Perspectives on Coeliac Disease<br />
Volume 1<br />
PRIMARY PREVENTION<br />
OF COELIAC DISEASE<br />
THE UTOPIA OF THE NEW MILLENNIUM?<br />
Editors<br />
Carlo Catassi<br />
Department <strong>of</strong> Pediatrics<br />
University <strong>of</strong> Ancona<br />
Ancona, Italy<br />
Center for Celiac Research,<br />
Baltimore, MD, USA<br />
Alessio Fasano<br />
Division <strong>of</strong> Pediatric<br />
Gastroenterology,<br />
Center for Celiac Research,<br />
University <strong>of</strong> Maryland<br />
Baltimore, MD, USA<br />
Gino Roberto Corazza<br />
Department <strong>of</strong><br />
Gastroenterology,<br />
University <strong>of</strong> Pavia,<br />
Pavia, Italy<br />
AIC Press
Italian Coeliac Society, Via Picotti, 22 - 56124 Pisa, Italy<br />
ã2003 Italian Coeliac Society. All rights reserved. This book is protected by copyright.<br />
No part <strong>of</strong> it may be reproduced, stored in a retrieval system, or transmitted, in any form or by<br />
any means, electronic, mechanical, photocopying, or recording, or otherwise, without the<br />
written permission <strong>of</strong> the publisher.<br />
Made in Italy<br />
The material contained in this volume was submitted as previously unpublished material,<br />
except in the instances in which credit has been given to the source from which some <strong>of</strong> the<br />
illustrative material was derived.<br />
Great care has been taken to maintain the accuracy <strong>of</strong> the information contained in the<br />
volume. However, neither the AIC nor the Editors can be held responsible for errors or for<br />
any consequences arising from the use <strong>of</strong> the information contained herein.
Foreward<br />
It is a great honour for me to introduce the Proceedings <strong>of</strong> the Meeting on Coeliac<br />
Disease that was held in Pavia on October 12, 2001.<br />
First <strong>of</strong> all, I would like to thank and to remind the memory <strong>of</strong> Mr. Sergio Spinelli, a<br />
man who strongly wanted and appreciated this meeting during its organization, who<br />
unfortunately passed just a few months before the event took place.<br />
I would also like to thank Pr<strong>of</strong>. Corazza and Dr. Catassi for their hard work and<br />
collaboration during the organization <strong>of</strong> the scientific programme and for selecting the<br />
most important scientists who participated as speakers and chairmen.<br />
Finally, I cannot forget Mrs. Marina Marengo, Mrs. Katia Pilo and the whole<br />
editorial staff, especially Mr. Franco Lucchesi and Mrs. Giusy Cappellotto, for<br />
pr<strong>of</strong>essionally organizing the whole meeting and preparing all the informative material,<br />
including this book.<br />
The Meeting held in Pavia was one <strong>of</strong> the most important scientific events on<br />
<strong>coeliac</strong> <strong>disease</strong> that have ever been organized, not only in Italy but also in Europe.<br />
The Italian Coeliac Society (AIC) has always given a strong support to research and<br />
felt it was time to organize a meeting for giving an up to date on the most important<br />
recent findings on <strong>coeliac</strong> <strong>disease</strong>, both in Italy and other countries.<br />
The aim <strong>of</strong> doing this was tw<strong>of</strong>old: (a) to evaluate the level <strong>of</strong> the current knowledge<br />
on the main aspects <strong>of</strong> <strong>coeliac</strong> <strong>disease</strong> by comparing different scientific working groups<br />
and (b) to identify the possible topics on which the research should be focused on in the<br />
next future. Should these goals be reached, the life <strong>of</strong> the <strong>coeliac</strong>s will be easier<br />
wherever.<br />
I think that the quality level <strong>of</strong> both the speakers and the audience allowed to entirely<br />
achieve these aims.<br />
Adriano Pucci<br />
President <strong>of</strong> the AIC<br />
viii
Preface<br />
Coeliac <strong>disease</strong> (CD) is a unique example in medicine <strong>of</strong> a genetically-based,<br />
immune-mediated condition entirely curable. Treatment with the gluten-free diet<br />
(GFD) is indeed followed by a full clinical and histological recovery (the true restitutio<br />
ad integrum), with the patient shifting from a <strong>disease</strong>d state to a normal condition <strong>of</strong><br />
life. In typical cases, the response to treatment is sometimes prodigious, so that a<br />
severely malnourished and miserable patient is rapidly transformed into a sturdy and<br />
healthy subject. Even in atypical cases, such as those presenting with anaemia,<br />
behavioural changes, or infertility, the diet treatment may miraculously be effective.<br />
However, there is a price to pay for this success. For many populations glutencontaining<br />
foods make a substantial contribution to daily energy intake and are<br />
enjoyable to eat. Bread had, and still has, such a basic role in human nutrition to rise to a<br />
symbolic value in the Holy Communion. The changes needed to begin and maintain a<br />
GFD are substantial and have a major impact on daily life. It is therefore not surprising<br />
that patients ask if a cure is on the horizon, wondering whether they will ever be able to<br />
tolerate a normal diet.<br />
Recently, some gliadin peptides that seem to have a <strong>primary</strong> role in activating the<br />
cascade <strong>of</strong> immune responses leading to the celiac enteropathy were characterized by<br />
different groups worldwide. These findings echoed in the lay media and were<br />
enthusiastically interpreted as a clear-cut step toward the development <strong>of</strong> a <strong>coeliac</strong><br />
“vaccine”. Is this science fiction or a realistic hope? In the year 2000 the Board <strong>of</strong> the<br />
Italian Coeliac Society (AIC) ripened the concept that it was time to give members a<br />
correct information on this hot topic. Therefore, the AIC Scientific Committee<br />
organized an innovative conference on <strong>primary</strong> <strong>prevention</strong> <strong>of</strong> CD, having two basic<br />
ideas in mind: (1) invite all the experts working in the field (in order to hear the different<br />
opinions); (2) translate the scientific language <strong>of</strong> the researchers into plain information<br />
that could be understood by the lay members <strong>of</strong> the Society. On October 12, 2001 a<br />
high-level scientific conference took place in Pavia, Italy, in the extraordinary scenario<br />
<strong>of</strong> the old Aula Scarpa <strong>of</strong> the University. On October 13, 2001 the technical concepts<br />
were summarized to a large lay audience in a meeting in Milan and society members<br />
had plenty <strong>of</strong> time for asking questions to the international experts.<br />
This book contains all the lectures presented at the Pavia meeting in order to give an<br />
up-to-date scenario on the recent developments on treatment strategies alternative to<br />
the GFD. In the first part <strong>of</strong> the book leading experts in the field report their results on<br />
the identification <strong>of</strong> toxic gluten peptides. In the second part, the role <strong>of</strong> environmental<br />
xi
xii<br />
risk factors that can trigger the onset <strong>of</strong> CD, particularly infant feeding, is discussed in<br />
detail. Finally, new strategies <strong>of</strong> treatment, based on either the introduction <strong>of</strong><br />
genetically detoxified grains or induction <strong>of</strong> oral tolerance to gluten, are presented. The<br />
reader will appreciate that the “holy grail” for a possible <strong>coeliac</strong> cure is still far away.<br />
Biochemically speaking, the complexity <strong>of</strong> gluten toxicity is disarming. Furthermore,<br />
the lack <strong>of</strong> an animal model <strong>of</strong> <strong>disease</strong> greatly hampers the investigations on the CD<br />
pathophysiology at the mucosal level. In spite <strong>of</strong> these problems, the route has been<br />
traced and <strong>primary</strong> <strong>prevention</strong> <strong>of</strong> CD should not be considered an utopia anymore at the<br />
beginning <strong>of</strong> the third millennium. We hope that this volume will stimulate researchers<br />
and clinicians alike to pursue this goal.<br />
We express our gratitude to all speakers and chairmen at the Pavia meeting, and to<br />
the academic authorities <strong>of</strong> the University <strong>of</strong> Pavia. We gratefully acknowledge the<br />
support <strong>of</strong> the AIC National Board, particularly <strong>of</strong> Ing. Spinelli, who was one <strong>of</strong> the<br />
promoters <strong>of</strong> this meeting that unfortunately passed away. The publication <strong>of</strong> this<br />
volume would not have been possible without the expertise <strong>of</strong> the AIC Editorial Board,<br />
particularly <strong>of</strong> Dr. Franco Lucchesi and Ms. Giusy Cappellotto. We also thank Dr.<br />
Elisabetta Fabiani for her valuable help with several aspects <strong>of</strong> this book.<br />
C. Catassi A. Fasano G.R. Corazza
Contents<br />
Current understanding <strong>of</strong> the basis for <strong>coeliac</strong> <strong>disease</strong> ............................................<br />
1<br />
Ludvig M Sollid<br />
The identification <strong>of</strong> toxic T cell stimulatory gluten response peptides early<br />
in <strong>coeliac</strong> <strong>disease</strong> ...................................................................................................<br />
13<br />
Frits Koning<br />
Toxic gluten peptides in <strong>coeliac</strong> <strong>disease</strong> identified by in vivo gluten challenge:<br />
a single dominant T cell epitope ? .........................................................................<br />
17<br />
Robert P Anderson<br />
Role <strong>of</strong> A-gliadin 31-49 peptide ........................................................................... 27 27<br />
Paul J Ciclitira<br />
The association <strong>of</strong> the HLA-DQ molecules with <strong>coeliac</strong> <strong>disease</strong> in the<br />
Saharawi: an evolutionary perspective on <strong>coeliac</strong> <strong>disease</strong> ....................................<br />
31<br />
Francesco Cucca, Carlo Catassi<br />
Primary <strong>prevention</strong> <strong>of</strong> <strong>coeliac</strong> <strong>disease</strong> by favourable infant feeding practices .....<br />
43<br />
Anneli Ivarsson, Lars Åke Persson, Olle Hernell<br />
Mechanisms <strong>of</strong> oral tolerance: lessons for <strong>coeliac</strong> <strong>disease</strong> ? ................................<br />
61<br />
Conleth Feighery<br />
Genetically detoxified grains in <strong>coeliac</strong> <strong>disease</strong> ....................................................<br />
75<br />
Federico Biagi, Antonio Di Sabatino, Jonia Campanella, Gino Roberto Corazza<br />
Immunotherapy <strong>of</strong> <strong>coeliac</strong> <strong>disease</strong>: where do we stand? .......................................<br />
83<br />
Carmen Gianfrani, Mauro Rossi, Giuseppe Mazzarella, Francesco Maurano,<br />
VirginiaSalvati, Delia Zanzi, Salvatore Auricchio, Riccardo Troncone<br />
The most recent advances on gluten toxicity in <strong>coeliac</strong> <strong>disease</strong> ............................<br />
89<br />
Gino Roberto Corazza, Carlo Catassi, Alessio Fasano<br />
xiii
Catassi C, Fasano A, Corazza GR (eds):<br />
Primary <strong>prevention</strong> <strong>of</strong> <strong>coeliac</strong> <strong>disease</strong>. The<br />
utopia <strong>of</strong> the new millennium? Perspectives<br />
on Coeliac Disease, vol. 1, AIC Press, pp 1-11<br />
Current understanding <strong>of</strong> the basis for <strong>coeliac</strong> <strong>disease</strong><br />
Ludvig M. Sollid<br />
Institute <strong>of</strong> Immunology, University <strong>of</strong> Oslo, Rikshospitalet, N-0027 Oslo, Norway<br />
lmsollid@labmed.uio.no<br />
Introduction<br />
Coeliac <strong>disease</strong> (CD) has received increased attention in recent years. The <strong>disease</strong> is<br />
more common than previously thought with a prevalence <strong>of</strong> about 1:130-1:300 in<br />
1<br />
Western societies . It is an acquired disorder; it may be diagnosed in early childhood<br />
with classical symptoms like diarrhoea and malabsorption, but it may also be diagnosed<br />
1<br />
later in life <strong>of</strong>ten with symptoms that do not directly allude to a gut <strong>disease</strong> .<br />
CD develops because <strong>of</strong> intolerance to ingested wheat gluten (consisting <strong>of</strong> the<br />
subcomponents gliadin and glutenin) or related proteins from rye and barley. There is a<br />
2<br />
chronic inflammation in the small intestine with resultant flattening <strong>of</strong> the mucosa .<br />
The current treatment is a life-long gluten exclusion diet which <strong>of</strong>ten impairs the quality<br />
<strong>of</strong> life <strong>of</strong> those who are affected. For this reason many <strong>coeliac</strong>s ask for novel treatment<br />
modalities and methods to prevent the <strong>disease</strong>.<br />
CD belongs to the group <strong>of</strong> chronic inflammatory <strong>disease</strong>s with multifactorial<br />
aetiology where genetic and environmental components are involved. Among these<br />
disorders CD stands out as a particularly good model. This paper will briefly cover<br />
some <strong>of</strong> the recent advances in the understanding <strong>of</strong> this disorder.<br />
Genetic factors<br />
3<br />
A high prevalence (10%) among first degree relatives <strong>of</strong> CD patients and a high<br />
4<br />
concordance rate <strong>of</strong> 70-100% in monozygotic twins indicate that susceptibility to<br />
develop CD is strongly influenced by inherited (genetic) factors. Both HLA and non-<br />
HLA genes contribute to the genetic predisposition, and assuming a multiplicative<br />
model <strong>of</strong> <strong>disease</strong> genetics it has been estimated that the overall importance <strong>of</strong> non-HLA<br />
5-6<br />
genes is greater than that <strong>of</strong> HLA genes . These figures should be interpreted with<br />
caution, however, as increased sharing <strong>of</strong> environmental factors by the sibs would tend<br />
to overestimate the role <strong>of</strong> the non-HLA genes.<br />
The majority <strong>of</strong> CD patients carry the DRB1*0301-DQA1*0501-DQB1*0201<br />
1
2<br />
THE BASIS OF COELIAC DISEASE<br />
haplotype (the DR3, DQ2 haplotype) or are DRB1*11/12-DQA1*0505-<br />
DQB1*0301/DRB1*07-DQA1*0201-DQB1*0202 heterozygotes (carry the DR5-<br />
7-11<br />
DQ7/DR7-DQ2 haplotypes) . The chains encoded by DQA1*0501 and DQA1*0505<br />
differ by one residue in the leader peptide, and the DQbchains encoded by DQB1*0201<br />
and DQB1*0202 differ by one residue in the membrane proximal domain. These<br />
substitutions are highly unlikely to have any functional consequence. CD patients with<br />
the above mentioned DR-DQ combinations share the same functional DQ molecule on<br />
the cell surface, encoded by genes carried in cis (e.g. DQA1*05 and DQB1*02 carried<br />
on the same haplotype) or trans position (e.g. DQA1*05 carried on a different<br />
12<br />
haplotype to DQB1*02) . Accumulating evidence suggests that the DR3-DQ2, the<br />
DR7-DQ2 and the DR5-DQ7 haplotypes have a close evolutionary relationship.<br />
Fragments <strong>of</strong> DNA flanking the DQA1 gene <strong>of</strong> the DR3-DQ2 haplotype have been<br />
identified on the DR5-DQ7 haplotype, and fragments <strong>of</strong> DNA flanking the DQB1 gene<br />
13-14<br />
<strong>of</strong> the DR3-DQ2 haplotype have been identified on the DR7-DQ2 haplotype . The<br />
genetic information in the DQ subregion <strong>of</strong> the DR3-DQ2 haplotype is thus reestablished<br />
in DR5-DQ7/DR7-DQ2 heterozygotes, although the sequence information<br />
is split between two chromosomes. Susceptibility to CD therefore likely depends on an<br />
interaction between at least two genes on the DR3-DQ2 haplotype that are reunited in<br />
DR5-DQ7 / DR7-DQ2 heterozygous individuals. The DQA1 and DQB1 genes are the<br />
primordial candidates since their products interact to form an HLA class II heterodimer<br />
and since they are situated close to a putative recombination site.<br />
Almost all the CD patients who are DQA1*05 and DQB1*02 negative bear the<br />
DRB1*04, DQA1*03, DQB1*0302 haplotype (i.e. DR4-DQ8 haplotype) and it is likely<br />
that these patients have an HLA association which is different to those who are DQ2<br />
positive. Although it is less clear what the <strong>primary</strong> <strong>disease</strong> susceptibility determinant <strong>of</strong><br />
15<br />
the DR4-DQ8 haplotype is, most data favour DQ8 .<br />
Overall the existing data suggest that the susceptibility to develop CD is primarily<br />
associated with two conventional DQ molecules DQ(a1*05,b1*02) (=DQ2) and to a<br />
lesser extent DQ(a1*03,b1*0302) (=DQ8). DQ molecules bind peptides and present<br />
these to CD4+ T helper cells carrying the abT cell receptor (TCR). The genetic<br />
evidence thus points towards a central role <strong>of</strong> CD4+ T cells in controlling the <strong>disease</strong><br />
development in CD.<br />
Genome wide linkage studies in CD have indicated numerous susceptibility regions<br />
with weak genetic effects, and the indications are strongest for susceptibility genes<br />
16-17<br />
located at 5qter and 11qter . However, no <strong>disease</strong> associations have been established<br />
so far for any gene <strong>of</strong> these regions. The only gene for which there are relatively<br />
18-20<br />
consistent reports on <strong>disease</strong> association is the CTLA4 gene on chromosome 2q33 .<br />
CTLA4 is involved in down regulating T-cell responses, and the A allele <strong>of</strong> the +49<br />
dimorphism is associated with increased CTLA4 expression and enhanced control <strong>of</strong> T<br />
21-22<br />
cell proliferation . Thus the +49 dimorphism is a prime suspect for the observed<br />
genetic effect, although other polymorphisms in linkage disequilibrium cannot be ruled<br />
out. In this respect it is worth noting that the CD28 and ICOS genes whose gene<br />
products are central players in T and B cell activation, are located very close to the<br />
CTLA4 gene.
THE BASIS OF COELIAC DISEASE<br />
3<br />
Environmental factors<br />
Gluten is obviously a critical environmental factor in CD. Whether other<br />
environmental factors are also involved is still an open question. Gut infections may<br />
well be involved. Adenovirus 12 has been in the forefront among the candidate<br />
microorganisms. This virus was originally proposed as a candidate because <strong>of</strong> partial<br />
23<br />
linear homology over 12 amino acids in a virus protein and a-gliadin . Based on our<br />
current understanding <strong>of</strong> the pathogenesis <strong>of</strong> <strong>coeliac</strong> <strong>disease</strong>, the rationale for the<br />
candidacy <strong>of</strong> this virus is weak, and there is in fact very little epidemiological data<br />
24<br />
supporting a role for this virus .<br />
Peptide binding to the CD associated DQ2 and DQ8 molecules<br />
Both HLA class I and class II molecules bind peptides in a groove located in their<br />
25<br />
membrane distal part . Stable binding is achieved by multiple hydrogen bonds<br />
between amino acids <strong>of</strong> HLA and peptide main chain atoms. Many polymorphic<br />
variants <strong>of</strong> HLA molecules exist. Amino acid residues which differ between the<br />
polymorphic variants are clustered around the peptide binding site where they<br />
contribute to the formation <strong>of</strong> specific binding pockets. Side chains <strong>of</strong> amino acids <strong>of</strong><br />
the peptide (so-called anchor residues) fit into these pockets and their interaction with<br />
HLA contribute to the binding <strong>of</strong> the peptide. The binding site <strong>of</strong> HLA class II<br />
molecules, in contrast to HLA class I molecules, is open at both ends allowing the<br />
bound peptides to protrude. The class II peptide ligands thus vary in length. The<br />
interactions with HLA mainly take place in a core region <strong>of</strong> nine residues. Within this<br />
region side chains <strong>of</strong> amino acids in positions P1, P4, P6, P7 and P9 dock into pockets <strong>of</strong><br />
the class II binding site. The chemistry and size <strong>of</strong> the various pockets vary between the<br />
different class II alleles so that some amino acids are preferred and some are not<br />
preferred. DQ2 has a unique preference for binding peptides with negatively charged<br />
26-28<br />
side chains at the three middle anchor positions . The binding motif <strong>of</strong> DQ8 is<br />
different from that <strong>of</strong> DQ2, but DQ8 also displays a preference for binding negatively<br />
29-31<br />
charged residues at several positions (i.e. P1, P4 and P9) . Hence, both the DQ2 and<br />
DQ8 molecules share a preference for negatively charged residues at some <strong>of</strong> their<br />
anchor positions.<br />
Preferential T cell recognition <strong>of</strong> gluten peptides presented by DQ2 and Dq8<br />
The observation that gluten reactive CD4+ TCRabT cells can be isolated and<br />
propagated from intestinal biopsies <strong>of</strong> CD patients has been instrumental for recent<br />
32<br />
achievements . Strikingly, such T cells <strong>of</strong> patients carrying the DR3-DQ2 haplotype<br />
were found to recognise gluten fragments presented by the DQ2 molecule rather than<br />
32-33<br />
by other HLA molecules <strong>of</strong> the patients . Both DR3-DQ2 positive and DR5-<br />
DQ7/DR7-DQ2 positive antigen presenting cells (i.e. carrying the DQA1*05 and<br />
DQB1*02 genes in cis or in trans configuration) are able to present the gluten antigen to<br />
these patient T cells. Likewise, T cells isolated from small intestinal biopsies <strong>of</strong> DQ2<br />
negative, DR4-DQ8 positive patients predominantly recognise gluten-derived peptides<br />
32-33<br />
when presented by the DQ8 molecule . Taken together, these results allude to
4 THE BASIS OF COELIAC DISEASE<br />
1<br />
presentation <strong>of</strong> gluten peptides in the small intestine as the mechanism by which DQ2<br />
1<br />
and DQ8 confer susceptibility to CD. HLA molecules are also important for<br />
determining the repertoire <strong>of</strong> peripheral T cells during maturation in the thymus. A<br />
thymic effect <strong>of</strong> the same DQ molecules on the TCR repertoire selection is, however,<br />
not excluded by these results.<br />
Importance <strong>of</strong> gluten deamidation for T cell recognition<br />
Wheat gluten is a mixture <strong>of</strong> a large number <strong>of</strong> gliadin and glutenin polypeptides.<br />
Generally, gluten proteins are rich in proline and glutamine residues while many other<br />
amino acids, including glutamic and aspartic acid, are unusually rare. Proteins <strong>of</strong> the<br />
gliadin fraction can be subdivided according to their sequence into the a-, g-, and w-<br />
34<br />
gliadins . Initially it was difficult to reconcile the DQ2 (and DQ8) binding motifs with<br />
presentation <strong>of</strong> gluten peptides, as gluten proteins have an unusual scarcity <strong>of</strong><br />
negatively charged residues. A clue to help explain this paradox came from the<br />
observation that the stimulatory capacity <strong>of</strong> gliadin preparations for gliadin specific<br />
intestinal T cells was significantly enhanced following treatment at high temperatures<br />
35<br />
and low pH . These conditions are known to cause non-specific deamidation <strong>of</strong><br />
glutamines to glutamic acid and may thus convert gliadin from a protein with very few<br />
peptides with the potential to bind to DQ2/DQ8 into one with many. An important and<br />
general role for deamidation <strong>of</strong> gluten for T cell recognition was sustained by analysis<br />
<strong>of</strong> the response pattern <strong>of</strong> a panel <strong>of</strong> polyclonal, gliadin specific T cell lines derived<br />
36<br />
from biopsies . All the cell lines responded poorly to a gliadin antigen prepared under<br />
conditions <strong>of</strong> minimal deamidation (chymotrypsin-digestion), when compared to the<br />
same antigen that had been further heat-treated in an acidic environment.<br />
The characterisation <strong>of</strong> gluten epitopes recognised by intestinal T cells has extended<br />
the knowledge about the importance <strong>of</strong> deamidation for their T cell recognition. Of the<br />
epitopes characterised until now, most <strong>of</strong> them (DQ2-g-gliadin-I, DQ2-a-gliadin-I and<br />
DQ2-a-gliadin-II) fail to stimulate T cells in their native form, but are potent antigens<br />
when a single glutamine residue is exchanged with glutamic acid in certain positions.<br />
For one DQ8 restricted epitope (DQ8-a-gliadin-I), the T cell recognition is augmented<br />
37<br />
by introduction <strong>of</strong> negatively charged residues whereas this is not seen for another<br />
38<br />
DQ8 restricted epitope (DQ8-glutenin-I) . These data demonstrate that most, but not<br />
all gluten specific intestinal T cells from CD patients recognise gluten proteins only<br />
after they have undergone deamidation.<br />
Tissue transglutaminase deamidates gluten peptides in vivo<br />
There is accumulating evidence that the deamidation in vivo is mediated by the<br />
39-40<br />
enzyme tissue transglutaminase (tTG) . tTG is expressed in many different tissues<br />
and organs; in the small intestine it is mainly expressed just beneath the epithelium in<br />
39<br />
the gut wall . The activity <strong>of</strong> tTG in the small intestinal mucosa in CD patients with<br />
41<br />
untreated <strong>disease</strong> is elevated compared to controls . The enzyme is present both<br />
intracellularly and extracellularly, and in the extracellular environment tTG has been<br />
demonstrated to play a role in extracellular matrix assembly, cell adhesion and wound
THE BASIS OF COELIAC DISEASE<br />
5<br />
42<br />
healing . The calcium dependent transglutaminase activity <strong>of</strong> tTG catalyses selective<br />
43<br />
crosslinking or deamidation <strong>of</strong> protein-bound glutamine residues . In contrast to the<br />
non-enzymatically mediated deamidation that results in a near random deamidation <strong>of</strong><br />
the <strong>of</strong>ten numerous glutamine residues in gliadin peptides, tTG appears to carry out an<br />
ordered deamidation <strong>of</strong> some few specific glutamines. In all <strong>of</strong> the known major DQ2<br />
and DQ8 restricted gluten epitopes recognised by gut T cell <strong>of</strong> adult patients, there are<br />
36-37-44<br />
glutamic acid residues modified by tTG which is important for T cell recognition .<br />
Interestingly, the deamidation <strong>of</strong> glutamine residues that are not targeted by tTG (e.g.<br />
40-45<br />
by acid treatment) can be deleterious for T cell recognition . This suggests that<br />
deamidation in vivo is mediated by tTG. This idea is further supported by the results <strong>of</strong><br />
experiments where T cell lines have been established from biopsies challenged with a<br />
minimally deamidated gliadin antigen (chymotrypsin-digested). In all but one <strong>of</strong> 18<br />
adult patients, the established T cell lines only barely responded to the chymotrypsindigested<br />
gliadins, but efficiently recognized the in vitro tTG-treated variants <strong>of</strong> the<br />
46<br />
same gliadins .<br />
Normally we do not mount immune responses to edible proteins. Moreover,<br />
experimental animal models have demonstrated that oral administration <strong>of</strong> antigen<br />
47<br />
usually results in systemic hyporesponsiveness to the same antigen . This<br />
phenomenon, which is termed oral tolerance, is believed to occur because <strong>of</strong> active<br />
tolerization towards edible proteins. In keeping with this thinking, oral tolerance to<br />
gluten in CD patients may not have been established properly or is broken. Given the<br />
preferential intestinal T cell response to deamidated gluten fragments in CD patients, it<br />
may be that deamidation is involved in the perturbation <strong>of</strong> the oral gluten tolerance.<br />
Deamidation increases the binding affinity <strong>of</strong> gliadin peptides for DQ2 from poor but<br />
36-<br />
significant binders, to epitopes with reasonable, but by no means exceptional affinity<br />
44<br />
. The moderate binding affinity <strong>of</strong> these epitopes concurs with the finding that they do<br />
not carry optimal anchors in all the anchor positions. Interestingly, T cell clones specific<br />
for the DQ2-g-gliadin-I, DQ2-a-gliadin-I and DQ2-a-gliadin-II epitopes generally fail<br />
to recognise native peptides at higher concentrations that should compensate for their<br />
lower binding affinity for DQ2. Thus, concurrent with the increase in the binding<br />
affinity for DQ2 caused by deamidation <strong>of</strong> the gliadin peptide, there likely is a change in<br />
the conformation1<strong>of</strong> the gliadin/DQ2 complexes. Oral tolerance to antigens ingested in<br />
47<br />
high doses is usually established by T cell anergy or deletion . It is possible that T cells<br />
specific for native gluten sequences are usually anergised or deleted, and that phlogistic<br />
T cell responses are effectively mounted to novel gluten epitopes being created in an<br />
inflamed environment by the help <strong>of</strong> tTG.<br />
How many gluten T cell epitopes?<br />
There exist several epitopes in gluten that are recognized by small intestinal T cells<br />
35<br />
<strong>of</strong> CD patients . Recent results <strong>of</strong> the author's laboratory and the laboratory <strong>of</strong> Frits<br />
Koning in Leiden indicate that there may be more than ten distinct DQ2 restricted<br />
epitopes. The existence <strong>of</strong> multiple epitopes raises several interesting questions: are<br />
only some <strong>of</strong> the epitopes pathogenic and thereby relevant to explain the HLA<br />
association? Are responses towards some <strong>of</strong> the epitopes generated during the early<br />
phases <strong>of</strong> <strong>disease</strong> development, while the responses to others are a result <strong>of</strong> epitope
6 THE BASIS OF COELIAC DISEASE<br />
spreading? Are different epitopes recognized by distinct groups <strong>of</strong> patients (e.g.<br />
children vs. adults)? Are some epitopes more relevant to <strong>disease</strong> as responses to them<br />
are found in the majority <strong>of</strong> the patients or because there is a higher precursor frequency<br />
<strong>of</strong> T cells in the lesion specific for these epitopes? The answers to most <strong>of</strong> these<br />
questions must await further investigations. At present we know that for the DQ2-agliadin-I<br />
and DQ2-a-gliadin-II epitopes, intestinal T cell reactivity is found in most if<br />
44<br />
not all adult DQ2+ patients , whereas for the DQ2-g-gliadin-I epitope intestinal T cell<br />
36<br />
reactivity is found in fewer DQ2+ patients . Less is known about the DQ8 restricted<br />
epitopes because few DQ8 positive patients have been tested so far. However, the DQ8-<br />
37<br />
a-gliadin-I appears to be frequently recognized . What causes the variance in<br />
responsiveness to the different epitopes and whether this reflects qualitative or<br />
quantitative differences between the patients are presently unclear.<br />
Formation <strong>of</strong> the <strong>coeliac</strong> lesion<br />
The evidence discussed above provides strong evidence that CD4+ TCRab+ T cells<br />
in the lamina propria are central for controlling the immune response to gluten that<br />
produces the immunopathology <strong>of</strong> CD. The knowledge <strong>of</strong> the events down-stream <strong>of</strong> T<br />
cell activation is, however, still incomplete. Knowing how the immune system usually<br />
utilizes a multitude <strong>of</strong> effector mechanisms for fighting its opponents, it is reasonable to<br />
believe that there may well be multiple effector mechanisms involved in the creation <strong>of</strong><br />
the <strong>coeliac</strong> lesion. Adding to the complexity, recent in vitro organ culture studies have<br />
indicated that gluten exerts additional immune relevant effects that are independent <strong>of</strong> T<br />
48-49<br />
cell activation . Some <strong>of</strong> these effects have rapid kinetics and conceivably the direct<br />
effects <strong>of</strong> gluten may facilitate subsequent T cell responses.<br />
Cytokines produced by lamina propria Cd4+ T cells may be involved in the<br />
increased crypt cell proliferation and the increased loss <strong>of</strong> epithelial cells. IFN-g<br />
induces macrophages to produce TNF-a. TNF- activates stromal cells to produce<br />
50<br />
KGF, and KGF causes epithelial proliferation and crypt cell hyperplasia . IFN-gand<br />
51<br />
TNF-acan jointly have a direct cytotoxic effect on intestinal epithelial cells . It is also<br />
conceivable that IELs and in particular gdT cells play a role in the epithelial cell<br />
52<br />
destruction by recognizing MIC molecules induced by stress .<br />
Alterations <strong>of</strong> the extracellular matrix can also distort the epithelial arrangement as<br />
the extracellular matrix provides the scaffold on which the epithelium lies. Enterocytes<br />
adhere to basement membrane through extracellular matrix receptors so that<br />
modification or loss <strong>of</strong> the basement membrane can result in enterocyte shedding.<br />
There is evidence for increased extracellular matrix degeneration in CD, and this may<br />
53<br />
be an important mechanism for the mucosal transformation found in CD . The<br />
increased production <strong>of</strong> metalloproteinases by subepithelial fibroblasts and<br />
macrophages is likely to be directly or indirectly induced by cytokines that are released<br />
from activated T cells.<br />
Coeliac patients on a gluten containing diet have increased levels <strong>of</strong> serum<br />
54-55<br />
antibodies to a variety <strong>of</strong> antigens including gluten and to tTG . We do not as yet<br />
know whether the autoantibodies play a role in the pathogenesis <strong>of</strong> CD. The tTG<br />
antibodies can inhibit the activity <strong>of</strong> tTG. This can cause villous atrophy by blocking
THE BASIS OF COELIAC DISEASE<br />
7<br />
interactions between mesenchymal cells and epithelial cells during the migration <strong>of</strong><br />
56<br />
epithelial cells and fibroblasts from the crypts to the tips <strong>of</strong> the villi . Moreover, the<br />
tTG antibodies may modulate the deamidating activity <strong>of</strong> tTG either in an inhibiting or<br />
57<br />
promoting fashion . Further research will tell us what role these antibodies play.<br />
Translation <strong>of</strong> the new knowledge into therapy<br />
The increasing insight into the molecular and cellular basis <strong>of</strong> CD should give<br />
benefits to the patients. The knowledge on which gluten epitopes are recognized by gut<br />
T cells should allow the methods by which gluten free foods are assessed to be<br />
improved. Moreover, the new knowledge should uncover novel targets for therapy.<br />
There are already some attractive possibilities. Activation <strong>of</strong> CD4+ gluten specific T<br />
cells appears to be a critical checkpoint in the development <strong>of</strong> CD, and interference with<br />
this step in the pathogenesis should be an effective way to control the <strong>disease</strong>. One<br />
possibility, which is basically an extension <strong>of</strong> today's treatment with a gluten free diet, is<br />
to produce wheat that is devoid <strong>of</strong> T cell epitopes, either by breeding programs or<br />
transgenic technology. Success by use <strong>of</strong> classical breeding already seems unlikely as<br />
epitopes are found in both a-gliadins and g-gliadins which are encoded by the Gli-1 and<br />
Gli-2 loci located on chromosomes 1 and 6, respectively. The classical breeding<br />
approach is further complicated by the hexaploid nature <strong>of</strong> wheat. tTG is a target for<br />
intervention because <strong>of</strong> its critical role in generating gluten T cell epitopes. Inhibitors <strong>of</strong><br />
tTG activity exist and likely inhibitors suitable as drugs can be developed. The biggest<br />
problem with this approach is that tTG inhibitors may have unacceptable side effects.<br />
tTG is involved in many different physiological processes including programmed cell<br />
42<br />
death . Another strategy would be to aim at the gluten specific T cells. If <strong>coeliac</strong>s have a<br />
normal oral tolerance to native gluten proteins, but a broken tolerance to deamidated<br />
gluten peptides, exposing the gut immune system to already deamidated peptides may<br />
establish oral tolerance to these deamidated gluten peptides as well. This approach will<br />
utilize the body's own mechanism to silence T cells. Alternatively, one could try to<br />
directly silence gluten specific T cell by using soluble dimers <strong>of</strong> HLA/ peptide<br />
complexes, which have been demonstrated to induce antigen specific apoptosis<br />
58<br />
because <strong>of</strong> inappropriate T cell stimulation . The central role <strong>of</strong> DQ2 and DQ8 in<br />
presenting gluten peptides <strong>of</strong>fers yet another target for intervention. Blocking the<br />
binding-sites <strong>of</strong> these HLA molecules would prevent presentation <strong>of</strong> <strong>disease</strong> inducing<br />
gluten peptides. The challenge with this approach will be to find an efficient way to<br />
target and block the binding sites <strong>of</strong> DQ molecules, which are continuously synthesized<br />
by antigen presenting cells. This approach, blocking <strong>of</strong> peptide presentation, has also<br />
been suggested as therapy for other HLA associated <strong>disease</strong>s. CD should be better<br />
suited to this approach than many other HLA associated <strong>disease</strong>s because drug delivery<br />
in the gut is easy compared for example to joints in rheumatoid arthritis or islet cells in<br />
type 1 diabetes.<br />
Whatever new therapeutic modality is introduced in CD, it will have to prove better<br />
than the current gluten free diet regime, also when coming to its long-term safety. This<br />
fact must be taken into consideration when devising new treatments. Although there are<br />
already interesting therapeutic principles with a good, rational basis that can be tested, it<br />
may for this reason take some years before a new treatment becomes reality.
8 THE BASIS OF COELIAC DISEASE<br />
Acknowledgements<br />
Studies in the author's laboratory are funded by grants from the Research Council<br />
<strong>of</strong> Norway, the European Commission (BMH4-CT98-3087, QLRT-1999-00037, QLRT-<br />
2000-00657), Medinnova, the Jahre Foundation and EXTRA funds from the Norwegian<br />
Foundation for Health and Rehabilitation.<br />
References<br />
1. Fasano A, Catassi C. Current approaches to diagnosis and treatment <strong>of</strong> celiac<br />
<strong>disease</strong>: an evolving spectrum. Gastroenterology 2001; 120: 636-51.<br />
2. Sollid LM. The molecular basis <strong>of</strong> celiac <strong>disease</strong>. Annu Rev Immunol 2000; 18: 53-<br />
81.<br />
3. Ellis A. Coeliac <strong>disease</strong>: previous family studies. In: McConnell RB, editor. The<br />
genetics <strong>of</strong> <strong>coeliac</strong> <strong>disease</strong>. Lancaster: MTP press, 1981: 197-9.<br />
4. Polanco I, Biemond I, van Leeuwen A, Schreuder I, Meera Khan P, Guerrero J et al.<br />
Gluten sensitive enteropathy in Spain: Genetic and environmental factors. In:<br />
McConnell RB, editor. The genetics <strong>of</strong> <strong>coeliac</strong> <strong>disease</strong>. Lancaster: MTP Press,<br />
1981: 211-31.<br />
5. Risch N. Assessing the role <strong>of</strong> HLA-linked and unlinked determinants <strong>of</strong> <strong>disease</strong>. Am<br />
J Hum Genet 1987; 40: 1-14.<br />
6. Petronzelli F, Bonamico M, Ferrante P, Grillo R, Mora B, Mariani P et al. Genetic<br />
contribution <strong>of</strong> the HLA region to the familial clustering <strong>of</strong> <strong>coeliac</strong> <strong>disease</strong>. Ann<br />
Hum Genet 1997; 61: 307-17.<br />
7. Keuning JJ, Pena AS, van Leeuwen A, van Ho<strong>of</strong>f JP, van Rood JJ. HLA-DW3<br />
associated with <strong>coeliac</strong> <strong>disease</strong>. Lancet 1976; i: 506-8.<br />
8. Ek J, Albrechtsen D, Solheim BG, Thorsby E. Strong association between the HLA-<br />
Dw3-related B cell alloantigen -DRw3 and <strong>coeliac</strong> <strong>disease</strong>. Scand J Gastroenterol<br />
1978; 13: 229-33.<br />
9. Mearin ML, Biemond I, Pena AS, Polanco I, Vazquez C, Schreuder GT et al. HLA-<br />
DR phenotypes in Spanish <strong>coeliac</strong> children: their contribution to the understanding<br />
<strong>of</strong> the genetics <strong>of</strong> the <strong>disease</strong>. Gut 1983; 24: 532-7.<br />
10. Trabace S, Giunta A, Rosso M, Marzorati D, Cascino I, Tettamanti A et al. HLA-<br />
ABC and DR antigens in celiac <strong>disease</strong>. A study in a pediatric Italian population.<br />
Vox Sang 1984; 46:102-6.<br />
11. Tosi R, Vismara D, Tanigaki N, Ferrara GB, Cicimarra F, Buffolano W et al.<br />
Evidence that celiac <strong>disease</strong> is primarily associated with a DC locus allelic<br />
specificity. Clin Immunol Immunopathol 1983; 28: 395-404.<br />
12. Sollid LM, Markussen G, Ek J, Gjerde H, Vartdal F, Thorsby E. Evidence for a<br />
<strong>primary</strong> association <strong>of</strong> celiac <strong>disease</strong> to a particular HLA-DQ a/bheterodimer. J<br />
Exp Med 1989; 169: 345-50.<br />
13. Lin L, Jin L, Kimura A, Carrington M, Mignot E. DQ microsatellite association<br />
studies in three ethnic groups. Tissue Antigens 1997; 50: 507-20.<br />
14. Lin L, Jin L, Lin X, Voros A, Underhill P, Mignot E. Microsatellite single nucleotide<br />
polymorphisms in the HLA-DQ region. Tissue Antigens 1998; 52: 9-18.<br />
15. Sollid LM, Thorsby E. HLA susceptibility genes in celiac <strong>disease</strong>: genetic mapping
THE BASIS OF COELIAC DISEASE<br />
9<br />
and role in pathogenesis. Gastroenterology 1993; 105: 910-22.<br />
16. Greco L, Corazza G, Babron MC, Clot F, Fulchignoni-Lataud MC, Percopo S et al.<br />
Genome search in celiac <strong>disease</strong>. Am J Hum Genet 1998; 62: 669-75.<br />
17. Greco L, Babron MC, Corazza GR, Percopo S, Sica R, Clot F et al. Existence <strong>of</strong> a<br />
genetic risk factor on chromosome 5q in Italian <strong>coeliac</strong> <strong>disease</strong> families. Ann Hum<br />
Genet 2001; 65: 35-41.<br />
18. Djilali-Saiah I, Schmitz J, Harfouch-Hammoud E, Mougenot JF, Bach JF, Caillat-<br />
Zucman S. CTLA-4 gene polymorphism is associated with predisposition to <strong>coeliac</strong><br />
<strong>disease</strong>. Gut 1998; 43: 187-9.<br />
19. Naluai AT, Nilsson S, Samuelsson L, Gudjonsdottir AH, Ascher H, Ek J et al. The<br />
CTLA4/CD28 gene region on chromosome 2q33 confers susceptibility to celiac<br />
<strong>disease</strong> in a way possibly distinct from that <strong>of</strong> type 1 diabetes and other chronic<br />
inflammatory disorders. Tissue Antigens 2000; 56: 350-5.<br />
20. Holopainen P, Arvas M, Sistonen P, Mustalahti K, Collin P, Maki M et al.<br />
CD28/CTLA4 gene region on chromosome 2q33 confers genetic susceptibility to<br />
celiac <strong>disease</strong>. A linkage and family-based association study. Tissue Antigens 1999;<br />
53: 470-5.<br />
21. Kouki T, Sawai Y, Gardine CA, Fisfalen ME, Alegre ML, DeGroot LJ. CTLA-4 gene<br />
polymorphism at position 49 in exon 1 reduces the inhibitory function <strong>of</strong> CTLA-4<br />
and contributes to the pathogenesis <strong>of</strong> Graves' <strong>disease</strong>. J Immunol 2000; 165: 6606-<br />
11.<br />
22. Ligers A, Teleshova N, Masterman T, Huang WX, Hillert J. CTLA-4 gene expression<br />
is influenced by promoter and exon 1 polymorphisms. Genes Immun 2001; 2: 145-<br />
52.<br />
23. Kagn<strong>of</strong>f MF, Austin RK, Hubert JJ, Bernardin JE, Kasarda DD. Possible role for a<br />
human adenovirus in the pathogenesis <strong>of</strong> celiac <strong>disease</strong>. J Exp Med 1984; 160:<br />
1544-57.<br />
24. Mahon J, Blair GE, Wood GM, Scott BB, Losowsky MS, Howdle PD. Is persistent<br />
adenovirus 12 infection involved in <strong>coeliac</strong> <strong>disease</strong>? A search for viral DNA using<br />
the polymerase chain reaction. Gut 1991; 32:1114-6.<br />
25. Madden DR. The three-dimensional structure <strong>of</strong> peptide-MHC complexes. Annu<br />
Rev Immunol 1995; 13: 587-622.<br />
26. Johansen BH, Vartdal F, Eriksen JA, Thorsby E, Sollid LM. Identification <strong>of</strong> a<br />
putative motif for binding <strong>of</strong> peptides to HLA-DQ2. Int Immunol 1996; 8: 177-82.<br />
27. van de Wal Y, Kooy YMC, Drijfhout JW, Amons R, Koning F. Peptide binding<br />
characteristics <strong>of</strong> the <strong>coeliac</strong> <strong>disease</strong>-associated DQa1*0501, b1*0201. molecule.<br />
Immunogenetics 1996; 44: 246-53.<br />
28. Vartdal F, Johansen BH, Friede T, Thorpe C, Stevanovic S, Eriksen JA et al. The<br />
peptide binding motif <strong>of</strong> the <strong>disease</strong> associated HLA-DQa1*0501, b1*0201.<br />
molecule. Eur J Immunol 1996; 26: 2764-72.<br />
29. Godkin A, Friede T, Davenport M, Stevanovic S, Willis A, Jewell D et al. Use <strong>of</strong><br />
eluted peptide sequence data to identify the binding characteristics <strong>of</strong> peptides to<br />
the insulin-dependent diabetes susceptibility allele HLA-DQ8 (DQ 3.2). Int<br />
Immunol 1997; 9: 905-11.<br />
30. Kwok WW, Domeier ML, Raymond FC, Byers P, Nepom GT. Allele-specific motifs<br />
characterize HLA-DQ interactions with a diabetes-associated peptide derived from
10 THE BASIS OF COELIAC DISEASE<br />
glutamic acid decarboxylase. J Immunol 1996; 156: 2171-7.<br />
31. Lee KH, Wucherpfennig KW, Wiley DC. Structure <strong>of</strong> a human insulin peptide-HLA-<br />
DQ8 complex and susceptibility to type 1 diabetes. Nat Immunol 2001; 2: 501-7.<br />
32. Lundin KEA, Scott H, Hansen T, Paulsen G, Halstensen TS, Fausa O et al. Gliadinspecific,<br />
HLA-DQa1*0501,b1*0201. restricted T cells isolated from the small<br />
intestinal mucosa <strong>of</strong> celiac <strong>disease</strong> patients. J Exp Med 1993; 178: 187-96.<br />
33. Lundin KEA, Gjertsen HA, Scott H, Sollid LM, Thorsby E. Function <strong>of</strong> DQ2 and<br />
DQ8 as HLA susceptibility molecules in celiac <strong>disease</strong>. Hum Immunol 1994; 41:<br />
24-7.<br />
34. Shewry PR, Tatham AS, Kasarda DD. Cereal proteins and <strong>coeliac</strong> <strong>disease</strong>. In:<br />
Marsh M, editor. Coeliac <strong>disease</strong>. Oxford: Blackwell Scientific Publications, 1992:<br />
305-48.<br />
35. Lundin KEA, Sollid LM, Norén O, Anthonsen D, Molberg Ø, Thorsby E et al.<br />
Heterogenous reactivity patterns <strong>of</strong> HLA-DQ-restricted small intestinal T-cell<br />
clones from patients with celiac <strong>disease</strong>. Gastroenterology 1997; 112: 752-9.<br />
36. Sjöström H, Lundin KEA, Molberg Ø, Körner R, McAdam SN, Anthonsen D et al.<br />
Identification <strong>of</strong> a gliadin T-cell epitope in <strong>coeliac</strong> <strong>disease</strong>: general importance <strong>of</strong><br />
gliadin deamidation for intestinal T-cell recognition. Scand J Immunol 1998; 48:<br />
111-5.<br />
37. van de Wal Y, Kooy YM, van Veelen PA, Peña SA, Mearin LM, Molberg Ø et al. Small<br />
intestinal T cells <strong>of</strong> celiac <strong>disease</strong> patients recognize a natural pepsin fragment <strong>of</strong><br />
gliadin. Proc Natl Acad Sci U S A 1998; 95: 10050-4.<br />
38. van de Wal Y, Kooy YM, van Veelen P, Vader W, August SA, Drijfhout JW et al.<br />
Glutenin is involved in the gluten-driven mucosal T cell response. Eur J Immunol<br />
1999; 29: 3133-9.<br />
39. Molberg Ø, McAdam SN, Körner R, Quarsten H, Kristiansen C, Madsen L et al.<br />
Tissue transglutaminase selectively modifies gliadin peptides that are recognized<br />
by gut-derived T cells. Nat Med 1998; 4: 713-7.<br />
40. van de Wal Y, Kooy Y, van Veelen P, Peña S, Mearin L, Papadopoulos G et al.<br />
Selective deamidation by tissue transglutaminase strongly enhances gliadinspecific<br />
T cell reactivity. J Immunol 1998; 161: 1585-8.<br />
41. Bruce SE, Bjarnason I, Peters TJ. Human jejunal transglutaminase: demonstration<br />
<strong>of</strong> activity, enzyme kinetics and substrate specificity with special relation to gliadin<br />
and <strong>coeliac</strong> <strong>disease</strong>. Clin Sci 1985; 68: 573-9.<br />
42. Aeschlimann D, Paulsson M. Transglutaminases: protein cross-linking enzymes in<br />
tissues and body fluids. Thromb Haemost 1994; 71: 402-15.<br />
43. Folk JE. Mechanism and basis for specificity <strong>of</strong> transglutaminase-catalyzed e-g-<br />
(glutamyl) lysine bond formation. Adv Enzymol Relat Areas Mol Biol 1983; 54:1-<br />
56.<br />
44. Arentz-Hansen H, Korner R, Molberg O, Quarsten H, Vader W, Kooy YM et al. The<br />
intestinal T cell response to a-gliadin in adult celiac <strong>disease</strong> is focused on a single<br />
deamidated glutamine targeted by tissue transglutaminase. J Exp Med 2000; 191:<br />
603-12.<br />
45. Quarsten H, Molberg Ø, Fugger L, McAdam SN, Sollid LM. HLA binding and T cell<br />
recognition <strong>of</strong> a tissue transglutaminase - modified gliadin epitope. Eur J Immunol<br />
1999; 29: 2506-14.
THE BASIS OF COELIAC DISEASE<br />
11<br />
46. Molberg Ø, McAdam S, Lundin KEA, Kristiansen C, Arentz-Hansen H, Kett K et al.<br />
T cells from celiac <strong>disease</strong> lesions recognize gliadin epitopes deamidated in situ by<br />
endogenous tissue transglutaminase. Eur J Immunol 2001; 31: 1317-23.<br />
47. Komagata Y, Weiner HL. Oral tolerance. Rev Immunogenet 2000; 2: 61-73.<br />
48. Maiuri L, Picarelli A, Boirivant M, Coletta S, Mazzilli MC, De Vincenzi M et al.<br />
Definition <strong>of</strong> the initial immunologic modifications upon in vitro gliadin challenge<br />
in the small intestine <strong>of</strong> celiac patients. Gastroenterology 1996; 110: 1368-78.<br />
49. Maiuri L, Auricchio S, Coletta S, De Marco G, Picarelli A, Di Tola M et al. Blockage<br />
<strong>of</strong> T-cell costimulation inhibits T-cell action in celiac <strong>disease</strong>. Gastroenterology<br />
1998; 115: 564-72.<br />
50. Bajaj-Elliott M, Poulsom R, Pender SL, Wathen NC, MacDonald TT. Interactions<br />
between stromal cell--derived keratinocyte growth factor and epithelial<br />
transforming growth factor in immune-mediated crypt cell hyperplasia. J Clin<br />
Invest 1998; 102: 1473-80.<br />
51. Deem RL, Shanahan F, Targan SR. Triggered human mucosal T cells release tumour<br />
necrosis factor - alpha and interferon-gamma which kill human colonic epithelial<br />
cells. Clin Exp Immunol 1991; 83: 79-84.<br />
52. Groh V, Steinle A, Bauer S, Spies T. Recognition <strong>of</strong> stress-induced MHC molecules<br />
by intestinal epithelial gdT cells. Science 1998; 279: 1737-40.<br />
53. Daum S, Bauer U, Foss HD, Schuppan D, Stein H, Riecken EO et al. Increased<br />
expression <strong>of</strong> mRNA for matrix metalloproteinases-1 and -3 and tissue inhibitor <strong>of</strong><br />
metalloproteinases-1 in intestinal biopsy specimens from patients with <strong>coeliac</strong><br />
<strong>disease</strong>. Gut 1999; 44: 17-25.<br />
54. Mäki M. The humoral immune system in <strong>coeliac</strong> <strong>disease</strong>. In: Howdle PD, editor.<br />
Coeliac <strong>disease</strong>. London: Bailliére Tindall, 1995: 231-49.<br />
55. Dieterich W, Ehnis T, Bauer M, Donner P, Volta U, Riecken EO et al. Identification<br />
<strong>of</strong> tissue transglutaminase as the autoantigen <strong>of</strong> celiac <strong>disease</strong>. Nat Med 1997; 3:<br />
797-801.<br />
56. Halttunen T, Mäki M. Serum immunoglobulin A from patients with celiac <strong>disease</strong><br />
inhibits human T84 intestinal crypt epithelial cell differentiation. Gastroenterology<br />
1999; 116: 566-72.<br />
57. Sollid LM, Scott H. New tool to predict celiac <strong>disease</strong> on its way to the clinics.<br />
Gastroenterology 1998; 115: 1584-6.<br />
58. Appel H, Seth NP, Gauthier L, Wucherpfennig KW. Anergy induction by dimeric<br />
TCR ligands. J Immunol 2001; 166: 5279-85.
Catassi C, Fasano A, Corazza GR (eds):<br />
Primary <strong>prevention</strong> <strong>of</strong> <strong>coeliac</strong> <strong>disease</strong>. The<br />
utopia <strong>of</strong> the new millennium? Perspectives on<br />
Coeliac Disease, vol. 1, AIC Press, pp 13-16<br />
The identification <strong>of</strong> toxic T cell stimulatory gluten<br />
response peptides early in <strong>coeliac</strong> <strong>disease</strong><br />
Frits Koning<br />
On behalf <strong>of</strong>: Willemijn Vader*, Yvonne Kooy*, Peter van Veelen*, Arnoud de Ru*,<br />
#<br />
Diana Harris*, Willemien Benckhuijsen*, Luisa Mearin , and Jan Wouter Drijfhout*<br />
#<br />
Departments <strong>of</strong> *Immunohematology and Blood Transfusion and Paediatrics,<br />
Leiden University Medical Centre, Leiden, The Netherlands<br />
It is generally accepted that <strong>coeliac</strong> <strong>disease</strong> (CD) is caused by uncontrolled T cell<br />
responses to gluten peptides that are presented by HLA-DQ2 and/or -DQ8 molecules.<br />
In recent years five gluten peptides have been identified that stimulate T cell clones<br />
1-5<br />
derived from small intestinal biopsies <strong>of</strong> CD patients . An important breakthrough has<br />
been the demonstration that deamidation <strong>of</strong> the gluten peptides by the enzyme tissue<br />
transglutaminase (tTG) is either required for, or enhances, T cell recognition <strong>of</strong> four <strong>of</strong><br />
1-8<br />
these peptides . The conversion <strong>of</strong> glutamine into glutamic acid by deamidation<br />
generates negative charges in gluten peptides that facilitate binding to HLA-DQ2 and -<br />
9-11<br />
DQ8 molecules , thus providing a molecular basis for the well established association<br />
between CD and HLA-DQ2/8.<br />
Two major issues, however, remain unsolved. First, all the studies so far have<br />
investigated the gluten specific T cell response in adult patients. It is unclear, therefore,<br />
whether the identified gluten peptides are also involved in T cell activation earlier in the<br />
<strong>disease</strong> process. Second, it is not known whether deamidation <strong>of</strong> gluten peptides is<br />
required for the breaking <strong>of</strong> oral tolerance or that it merely enhances T cell reactivity<br />
towards gluten.<br />
To investigate these matters we have now carried out an extensive investigation <strong>of</strong><br />
the gluten specific response in children with recent onset CD. Twenty-two Caucasian<br />
DQ2-(DQA1*0501/DQB1*02) positive patients with a confirmed diagnosis <strong>of</strong> CD<br />
were included in the present study. Their age at diagnosis (first small bowel biopsy) was<br />
between 1 and 9 years (average age 3.6 years ± 1.8). Biopsies were collected from these<br />
patients and used to generate gluten reactive T cell lines. Subsequently, gluten specific<br />
T cell clones were generated from T cell lines <strong>of</strong> nine patients. The T cell lines and<br />
clones were tested for reactivity against gluten and gluten that has been treated with tTG<br />
(tTG-gluten hereafter). Three patterns <strong>of</strong> reactivity were observed:<br />
1) T cells that did not respond to gluten but did respond to tTG-gluten;<br />
2) T cells that responded to both gluten and tTG-gluten;<br />
3) T cells that did respond to gluten but not to tTG-gluten. In 8 out <strong>of</strong> 9 patients tTGdependent<br />
clonal T cell responses were found while in 7 patients specific responses to<br />
13
14<br />
T CELL RESPONSES TO GLUTEN PEPTIDES<br />
non-deamidated gluten were also observed. These results indicate that a large<br />
proportion <strong>of</strong> the gluten specific responses are directed to deamidated gluten but that<br />
responses to non-deamidated gluten are also common.<br />
Extensive testing <strong>of</strong> the T cell clones against the 3 known HLA-DQ2 restricted T<br />
cell stimulatory gliadin derived peptides indicated that the large majority <strong>of</strong> the T cell<br />
clones did not respond to these peptides, and were thus likely reactive towards yet<br />
unidentified gluten peptides. To characterize these novel peptides we have used two<br />
different methods. First, we purified and characterized T cell stimulatory gluten<br />
epitopes from pepsin/trypsin digests <strong>of</strong> (tTG-) gluten by rpHPLC and mass<br />
1-2<br />
spectrometry as described . This method led to the characterization <strong>of</strong> 3 novel T cell<br />
stimulatory peptides. Second, we tested the T cell clones against a set <strong>of</strong> 250 synthetic<br />
gluten peptides, representing gliadin and glutenin sequences. This method led to the<br />
identification <strong>of</strong> 3 additional novel T cell stimulatory peptides.<br />
Subsequently we tested the response <strong>of</strong> the T cell clones to the identified peptides in<br />
deamidated and non-deamidated form. The T cell response towards 3 peptides required<br />
prior deamidation. In contrast, the response to 2 peptides was found to be largely<br />
indifferent to deamidation. Finally, deamidation abolished the response to the sixth<br />
peptide. Thus, the effect <strong>of</strong> deamidation by tTG on gluten specific T cell stimulation is<br />
heterogeneous and can be positive, neutral and negative.<br />
Subsequently the gluten specific T cell clones <strong>of</strong> all patients were tested against the<br />
3-5<br />
previously characterized HLA-DQ2 restricted gluten peptides as well as against the<br />
peptides reported in the present study. While responses to some peptides were found in<br />
one patient only, responses to other peptides were found in various patients and these<br />
may thus represent more immunodominant peptides. T cell responses towards the a-<br />
gliadin peptides which have been reported to be immunodominant in adult patients<br />
were found in three paediatric patients, among whom the identical twins. In these 9<br />
patients we observed 8 distinct reactivity patterns towards the gluten peptides (Table).<br />
Altogether, these results indicate a highly diverse response against the gluten peptides.<br />
These results indicate a discrepancy between the specificity <strong>of</strong> adult and paediatric<br />
gluten specific T cell responses. While immunodominant responses to a particular a-<br />
gliadin peptide are found in adult patients, the response in paediatric patients appears<br />
more diverse. Our results also indicate that T cell responses to peptides other than the<br />
immunodominant a-gliadin peptide can lead to <strong>disease</strong>. Moreover, our results<br />
demonstrate that responses to non-deamidated peptides are frequently found,<br />
suggesting that native gluten peptides are immunogenic in celiac <strong>disease</strong> patients.<br />
The discrepancy between the specificity <strong>of</strong> the adult and paediatric gluten specific T<br />
cell response could be explained by a deamidation driven narrowing <strong>of</strong> the gluten<br />
response towards immunodominant T cell stimulatory peptides after initiation <strong>of</strong><br />
<strong>disease</strong> by responses towards a diverse repertoire <strong>of</strong> gluten peptides.<br />
Acknowledgements<br />
This study was financially supported by the European Community project no. BMH<br />
CT-98, a grant from the Dutch Digestive Disease Foundation and the University <strong>of</strong><br />
Leiden.
T CELL RESPONSES TO GLUTEN PEPTIDES<br />
15<br />
DB<br />
JB<br />
NB<br />
SB<br />
JP<br />
NP<br />
MS<br />
NV<br />
SV<br />
Glia- Glia- Glia- Glia-<br />
2a 20a 9a 1g<br />
Glia-<br />
30g<br />
Glt-<br />
17<br />
Glt-<br />
156<br />
Glu-<br />
5<br />
Glu-<br />
21<br />
Table. Overview <strong>of</strong> paediatric T cell responses to gluten peptides.<br />
References<br />
1. Van de Wal Y, Kooy YM, Van Veelen PA, Pena AS, Mearin LM, Molberg O, et al. Small<br />
intestinal T cells <strong>of</strong> celiac <strong>disease</strong> patients recognize a natural pepsin fragment <strong>of</strong> gliadin.<br />
Proc Natl Acad Sci U.S.A 1998; 95: 10050-4.<br />
2. Van de Wal Y. Kooy YM, Van Veelen P, Vader W, August SA, Drijfhout JW, et al. Glutenin<br />
is involved in the gluten-driven mucosal T cell response. Eur J Immunol 1999; 29: 3133-<br />
9.<br />
3. Sjostrom H, Lundin KE, Molberg O, Korner R, McAdam SN, Anthonsen D, et al.<br />
Identification <strong>of</strong> a gliadin T-cell epitope in <strong>coeliac</strong> <strong>disease</strong>: general importance <strong>of</strong> gliadin<br />
deamidation for intestinal T-cell recognition. Scand J Immunol. 1998; 48: 111-5.<br />
4. Arentz-Hansen H, Korner R, Molberg O, Quarsten H, Vader W, Kooy YM, et al. The<br />
intestinal T cell response to alpha-gliadin in adult celiac <strong>disease</strong> is focused on a single<br />
deamidated glutamine targeted by tissue transglutaminase. J Exp Med 2000; 191: 603-12.<br />
5. Anderson RP, Degano P, Godkin AJ, Jewell DP, Hill AV. In vivo antigen challenge in<br />
celiac <strong>disease</strong> identifies a single transglutaminase-modified peptide as the dominant A-<br />
gliadin T-cell epitope. Nat Med 2000; 6: 337-42.<br />
6. Molberg O, McAdam SN, Korner R, Quarsten H, Kristiansen C, Madsen L, et al. Tissue<br />
transglutaminase selectively modifies gliadin peptides that are recognized by gut-derived<br />
T cells in celiac <strong>disease</strong>. Nat Med 1998; 4: 713-7.<br />
7. Van de Wal Y, Kooy Y, van Veelen P, Pena S, Mearin L, Papadopoulos G, et al. Selective<br />
deamidation by tissue transglutaminase strongly enhances gliadin-specific T cell<br />
reactivity. J Immunol 1998; 161: 1585-8.<br />
8. Quarsten H, Molberg O, Fugger L, McAdam SN, Sollid LM. HLA binding and T cell<br />
recognition <strong>of</strong> a tissue transglutaminase - modified gliadin epitope. Eur J Immunol 1999;<br />
29: 2506-14.<br />
9. Van de Wal Y, Kooy YMC, Drijfhout JW, Amons R, Koning F. Peptide binding<br />
characteristics <strong>of</strong> the <strong>coeliac</strong> <strong>disease</strong>-associated DQ(alpha1*0501, beta1*0201)<br />
molecule. Immunogenetics 1996; 44: 246-53.<br />
10. Vartdal F, Johansen B.H., Friede T, Thorpe CJ, Stevanovic S, Eriksen JE, et al. The<br />
peptide binding motif <strong>of</strong> the <strong>disease</strong> associated HLA-DQ (alpha 1* 0501, beta 1* 0201)<br />
molecule. Eur J Immunol 1996; 26: 2764-72.<br />
11. Kwok WW. Domeier ML, Raymond FC, Byers P, Nepom GT. Allele-specific motifs<br />
characterize HLA-DQ interactions with a diabetes - associated peptide derived from<br />
glutamic acid decarboxylase. J Immunol. 1996; 156: 2171-7.
Catassi C, Fasano A, Corazza GR (eds):<br />
Primary <strong>prevention</strong> <strong>of</strong> <strong>coeliac</strong> <strong>disease</strong>. The<br />
utopia <strong>of</strong> the new millennium? Perspectives on<br />
Coeliac Disease, vol. 1, AIC Press, pp 17-26<br />
Toxic gluten peptides in <strong>coeliac</strong> <strong>disease</strong> identified by<br />
in vivo gluten challenge: A single dominant T<br />
cell epitope?<br />
Robert P. Anderson<br />
The Royal Melbourne Hospital Autoimmunity and Transplantation Division, Walter and Eliza<br />
Hall Institute c/o Post Office RMH, Victoria, Australia 3050<br />
b.anderson@wehi.edu.au<br />
The realization that as many as 1% <strong>of</strong> Europeans and North Americans are affected<br />
by <strong>coeliac</strong> <strong>disease</strong> adds urgency to understanding the immunopathogenesis <strong>of</strong> <strong>coeliac</strong><br />
<strong>disease</strong> and developing a rational therapy without the inconvenience <strong>of</strong> a gluten free<br />
diet.<br />
Antigen-specific immunotherapy is highly effective in animal models <strong>of</strong> antigendriven<br />
immune-mediated <strong>disease</strong>. Because human immune-mediated <strong>disease</strong>s are<br />
usually only available for study when the immune response is well established, it has<br />
been impossible to be sure what the initiating antigens are, or whether there are critical<br />
dominant T cells epitopes that trigger <strong>disease</strong>.<br />
Coeliac <strong>disease</strong> is unique among human immune-mediated <strong>disease</strong> since gluten is<br />
known to maintain <strong>disease</strong>, and treatment is successful when dietary gluten is excluded.<br />
If <strong>coeliac</strong> <strong>disease</strong> is triggered by one critical gluten component it may be possible to<br />
develop antigen-specific therapies or preventive “vaccines”. This chapter discusses the<br />
rationale for in vivo strategies that have allowed the identification <strong>of</strong> a critical gliadin<br />
peptide that is the dominant <strong>coeliac</strong>-specific T cell epitope in a model alpha-gliadin<br />
protein. A molecular model for the interaction <strong>of</strong> HLA-DQ2, dominant gliadin epitope<br />
and T cell receptor is presented, and preliminary data indicating the potential <strong>of</strong> altered<br />
peptide ligands to antagonize this interaction is discussed.<br />
CD4 T cells have the potential to initiate immunopathology<br />
Gluten and HLA-DQ2 are definitively implicated in the aetiopathogenesis <strong>of</strong><br />
1<br />
<strong>coeliac</strong> <strong>disease</strong> . Since HLA-DQ2 presents peptides to CD4 T cells, there has been<br />
intense interest in defining the specificity and phenotype <strong>of</strong> T cells in <strong>coeliac</strong> <strong>disease</strong><br />
that recognize gluten peptides restricted by HLA-DQ2.<br />
CD4 T cells play a pivotal role in coordinating immune responses. CD8 T cell and<br />
many B cell responses require CD4 T cell “help” provided directly or through CD4 T<br />
cell activation <strong>of</strong> antigen presenting cells (particularly dendritic cells). In <strong>coeliac</strong><br />
<strong>disease</strong>, CD4 T cells predominantly secreting Th1-like cytokines appear in the small<br />
17
18<br />
A DOMINANT EPITOPE IN GLUTEN PEPTIDES ?<br />
intestinal lamina propria within hours <strong>of</strong> gluten challenge in subjects on gluten free diet.<br />
Initial damage to the intestine following gluten challenge in treated <strong>coeliac</strong> <strong>disease</strong> is<br />
likely to be due to cytokines (for example interferon gamma [IFNg] and tumour<br />
necrosis factor [TNF]) secreted by CD4 T cells that activate macrophages causing<br />
2<br />
release <strong>of</strong> inflammatory mediators and other cytokines that activate other cell types . In<br />
addition to immunopathology induced by gluten-specific CD4 T cells, increasing<br />
3<br />
evidence suggests that gluten may also directly activate macrophages , possibly<br />
facilitating induction <strong>of</strong> T cell responses to dietary antigen.<br />
Disease chronicity and epitope spreading: relevance to T cell epitope mapping in<br />
<strong>coeliac</strong> <strong>disease</strong><br />
Experimental autoimmune <strong>disease</strong>s, such as experimental allergic encepahalitis<br />
(EAE), can be initiated by immunization <strong>of</strong> susceptible mice with adjuvant together<br />
with myelin basic protein (MBP) or a specific peptide derived from this protein. This<br />
4<br />
peptide corresponds to the “dominant” T cell epitope <strong>of</strong> MBP . Exactly what qualities,<br />
in addition to affinity for HLA and resistance to proteolysis during processing, that lead<br />
5<br />
to one peptide in an antigenic protein to be dominant are not fully understood . As EAE<br />
progresses, a variety <strong>of</strong> other peptides (sub-dominant epitopes) derived from MBP and<br />
other myelin-associated proteins are recognized by specific T cells in a process termed<br />
4, 6<br />
epitope spreading (also seen in human multiple sclerosis ). Specificity <strong>of</strong> T cell<br />
responses can also be shaped by preferential presentation <strong>of</strong> peptides by B cells<br />
following antigen uptake via B cell receptor or Fc receptor-mediated uptake <strong>of</strong><br />
7<br />
antibody-antigen complexes . Post-uptake processing <strong>of</strong> antigen may also be altered by<br />
the cytokine milieu in established immune responses giving rise to a different repertoire<br />
8<br />
<strong>of</strong> peptides being presented by antigen-presenting cells .<br />
Interestingly, when MBP-specific T cells are transferred to a healthy recipient,<br />
MBP-specific T cells are initially abundant in spleen and blood. Just before onset <strong>of</strong><br />
EAE, MBP-specific T cells disappear from spleen and blood, and become abundant at<br />
9<br />
the site <strong>of</strong> antigen (central nervous system) . Consistent with this, oral administration<br />
<strong>of</strong> antigen is initially followed by proliferation <strong>of</strong> antigen specific T cells in gut-<br />
10<br />
associated as well as systemic lymphoid tissue . Furthermore, T cells with identical<br />
11<br />
specificity are found in murine gut epithelium, lamina propria and the thoracic duct .<br />
Taken together, these studies in mice indicate that T cells specific for dominant or<br />
subdominant epitopes appear at different time points, and may be located in different<br />
anatomical sites according to the chronicity <strong>of</strong> the immune response. Contrary to the<br />
12<br />
widely held view in <strong>coeliac</strong> <strong>disease</strong> research , T cells with identical specificities are<br />
present in gut and extra-intestinal sites such as blood in the early phase <strong>of</strong> immune<br />
responses caused by gut antigen.<br />
Multiple toxic peptides in <strong>coeliac</strong> <strong>disease</strong> identified by multiple methodologies<br />
In <strong>coeliac</strong> <strong>disease</strong>, a variety <strong>of</strong> in vivo, ex vivo and in vitro methods have been
A DOMINANT EPITOPE IN GLUTEN PEPTIDES ?<br />
19<br />
1, 13<br />
exploited to search for “toxic” gluten peptides . A-gliadin, the first fully sequenced<br />
14<br />
wheat gliadin protein , has been used as the archetypal “toxic gluten” protein source<br />
for most <strong>of</strong> these peptides (see Fig. 1). More recently, recombinant gliadins and<br />
peptides corresponding to parts <strong>of</strong> cDNA-derived gliadin sequences have been studied<br />
15<br />
. In view <strong>of</strong> the diversity <strong>of</strong> model systems, some with no relationship to <strong>coeliac</strong><br />
<strong>disease</strong> (for example fetal intestinal explants), it is not surprising that a variety <strong>of</strong><br />
different peptides have been defined as toxic. In other studies, non-specific markers <strong>of</strong><br />
toxicity (for example epithelial cell height) have been used as surrogates for<br />
immunological toxicity. If the <strong>primary</strong> hypothesis is that <strong>coeliac</strong> <strong>disease</strong> is a T cell<br />
mediated <strong>disease</strong>, rational identification <strong>of</strong> “toxic” gluten peptides in <strong>coeliac</strong> <strong>disease</strong><br />
should ideally begin with assays designed to detect HLA-DQ2 restricted CD4 T cells<br />
that secrete Th1-associated cytokines (for example interferon gamma).<br />
Intestinal T cell clones for identification <strong>of</strong> toxic gluten peptides<br />
More recently, intestinal T cell clones from duodenal biopsies <strong>of</strong> <strong>coeliac</strong> patients on<br />
gluten free diet pulsed with protease-digested gliadin have been used to search for<br />
15-17<br />
gliadin-specific T cell epitopes . These studies have revealed that intestinal T cell<br />
clones raised from gliadin-pulsed <strong>coeliac</strong> intestinal biopsies predominantly recognise<br />
12<br />
deamidated gliadin epitopes . T cell epitopes generally correspond to gliadin peptides<br />
deamidated by tissue transglutaminase (tTG). tTG is induced with inflammation and<br />
apoptosis, and irreversibly cross links proteins and peptides via glu-lys isopeptide<br />
18<br />
bonds, or directly deamidates glutamine residues to glutamate . Intestinal tissue,<br />
particularly if inflamed, is rich in tTG. Introduction <strong>of</strong> glutamate in gliadin T cell<br />
12, 15<br />
epitopes by tTG greatly enhances their binding to HLA-DQ2 .<br />
T cell epitope mapping in immune-mediated <strong>disease</strong>s<br />
In human immune-mediated <strong>disease</strong>s, T cell epitopes have been mapped using<br />
synthetic 15-20mers overlapping by 10 residues spanning known antigenic proteins in<br />
assays <strong>of</strong> peripheral blood T cells. In <strong>coeliac</strong> <strong>disease</strong>, it has been contended that gliadin-<br />
1<br />
specific peripheral blood T cells are qualitatively different from intestinal T cells .<br />
Gliadin-specific intestinal T cell clones are generally HLA-DQ2 restricted while<br />
19<br />
peripheral blood T cell clones are HLA-DR, -DQ or -DP restricted . However, these<br />
studies were performed before the realization that deamidation <strong>of</strong> gliadin was<br />
important for T cell recognition. Hence, contemporary understanding <strong>of</strong> toxic gluten<br />
peptides in the context <strong>of</strong> <strong>coeliac</strong> <strong>disease</strong> as an HLA-DQ2 associated CD4 T cellmediated<br />
<strong>disease</strong> has relied upon identification <strong>of</strong> epitopes <strong>of</strong> intestinal T cell clones<br />
using protease-digested gliadin with or without deamidation by tTG.<br />
Unfortunately, it is impossible to know whether epitopes <strong>of</strong> T cell clones are<br />
dominant or subdominant, or whether a clone is specific for only a part <strong>of</strong> a polyclonal T<br />
cell response in vivo. Furthermore, recent studies to identify epitopes <strong>of</strong> gliadin T cell<br />
15<br />
clones have used chymotrypsin-digested gliadins even though chymotrysin<br />
selectively cleaves peptide bonds following bulky hydrophobic aminoacids (the same<br />
aminoacids known to be anchor residues at the N - and C-terminal end <strong>of</strong> the HLA-DQ2<br />
1<br />
binding motif ), raising the possibility that bioactive peptides may be artefactually
20 A DOMINANT EPITOPE IN GLUTEN PEPTIDES ?<br />
truncated or destroyed.<br />
Hence, a variety <strong>of</strong> data support the hypothesis that <strong>coeliac</strong> <strong>disease</strong> could be<br />
initiated by a Th1-like HLA-DQ2 restricted CD4 T cell response focused on particular<br />
(probably deamidated) gluten peptide/s. However, current methods relying upon T cell<br />
clones, or challenge <strong>of</strong> <strong>coeliac</strong> tissue in vivo or ex vivo are incapable <strong>of</strong> defining<br />
whether peptides are dominant or subdominant in the immunopathogenesis <strong>of</strong> <strong>coeliac</strong><br />
<strong>disease</strong>.<br />
In vivo gluten challenge and peripheral blood epitope mapping to define T cell<br />
20<br />
epitope hierarchies<br />
Antigen challenge <strong>of</strong> sensitized subjects results in activation <strong>of</strong> cognate memory T<br />
cells. Memory T cells tend to reside at anatomical sites where their cognate antigen was<br />
previously encountered. Recently, memory T cells have been divided into “effector”<br />
- + 21<br />
(cytokine-secreting, CCR7 ) and lymph node-homing subtypes (CCR7 ) . We<br />
+<br />
reasoned that gluten challenge in healthy HLA-DQ2 <strong>coeliac</strong> subjects following a strict<br />
gluten free diet would reactivate gluten-specific memory T cells. The initial intestinal<br />
inflammation documented by others may be driven by effector memory T cells, but<br />
subsequent appearance <strong>of</strong> T cells in peripheral blood, perhaps homing back to the gut,<br />
may reflect proliferation <strong>of</strong> gluten-specific T cells in lymphoid tissue during the days<br />
after antigen exposure. Hence, the kinetics and frequency <strong>of</strong> epitope-specific peripheral<br />
blood T cells might reveal dominant versus subdominant gluten epitopes.<br />
Synthetic 15mer peptides overlapping by 10 aminoacids corresponding to the<br />
composite aminoacid sequence (rather than cDNA-derived sequence) <strong>of</strong> A-gliadin<br />
(Fig. 1) with or without in vitro deamidation by tTG were studied in overnight ex vivo<br />
A 1. VRVPVPQLQP QNPSQQQPQE QVPLVQQQQF PGQQQ QFPPQ QPYPQPQPFP SQQPYLQLQP<br />
B<br />
P<br />
A 61. PQ PQLPYPQ PQ SFPPQQPY PQPQPQYSQP QQPISQQQ AQ QQQQQQQQQQ<br />
B [..] P R Q Q[..]<br />
A111. QQQILQQILQ QQLIPC MDVV LQQHNIAHAR SQVLQQSTYQ LLQELCCQHL WQIPEQSQCQ<br />
B R GS Q Q<br />
A171. AIHNVVHAII LHQQQ KQQQQ PSSQVSFQQP L QQYPLGQGS FRPSQQNPQA<br />
B [..] [..] Q S<br />
A221. QGSVQPQQLP QFEEIRNLAL QTLPAMCNVY I APYC TIAPF GIFGTN<br />
B P [..]<br />
14<br />
Fig. 1. Aminoacid sequence <strong>of</strong> A-gliadin used to derive overlapping 15mer peptides in<br />
20<br />
gluten challenge studies (A), and residues that deviate from the consensus sequence derived<br />
from 61 Genbank Triticum aestivum a - and a/b-gliadin cDNAs using ClustalW (B) ([..]<br />
indicates polymorphic insertion).
A DOMINANT EPITOPE IN GLUTEN PEPTIDES ?<br />
21<br />
interferon gamma (IFNg) ELISpot assays using peripheral blood mononuclear cells<br />
(PBMC). IFNgELISpot assays define the frequency <strong>of</strong> cells secreting IFNg, and are<br />
capable <strong>of</strong> detecting peptide-specific T cell frequencies as low as 5-10 per million<br />
+<br />
PBMC. Blood was collected from HLA-DQ2 healthy non-<strong>coeliac</strong> and <strong>coeliac</strong> subjects<br />
after gluten free diet for at least 4 weeks, and then in the 12 days after commencing<br />
gluten challenge (200 g white bread daily for ½ day [n=1], 3 days [n=10], or 10 days<br />
[n=1]). Short-term gluten challenge was generally well tolerated by <strong>coeliac</strong> subjects,<br />
11/12 subjects were able to consume 200g gluten bread for 3 or more days, and 8/12 had<br />
only mild symptoms. One subject had abdominal cramps and vomited within 3 hours <strong>of</strong><br />
the first 2 slices <strong>of</strong> bread. All symptoms resolved within 1 to 3 days after ceasing gluten<br />
challenge.<br />
Prior to gluten challenge, no A-gliadin peptide elicited responses in the IFNg<br />
ELISpot. However, in 11/12 <strong>coeliac</strong> subjects and 0/4 healthy control subjects there was<br />
induction <strong>of</strong> IFNgELISpot responses on day 4-8 for one pool <strong>of</strong> overlapping peptides<br />
only when treated with tTG. In all cases, IFNginduction was attributed to 2 peptides<br />
overlapping by 10 aminoacids (A-gliadin 56-75). Aminoacid sequencing demonstrated<br />
that only one glutamine residue in A-gliadin 56-75 was susceptible to tTG-mediated<br />
deamidation (Q65). Truncations <strong>of</strong> A-gliadin 56-75 treated with tTG indicated that<br />
residues 64-68 (PQLPY) were critical for bioactivity, and that the 17mer<br />
QLQPFPQPQLPYPQPQS (57-73) was the optimal peptide. Bioactivity <strong>of</strong><br />
QLQPFPQPELPYPQPQS was identical to tTG-treated QLQPFPQPQLPYPQPQS,<br />
demonstrating that bioactivity <strong>of</strong> this peptide was dependent upon a single deamidated<br />
glutamine residue (QE65). Immunomagnetic bead depletion <strong>of</strong> PBMC prior to addition<br />
<strong>of</strong> peptide showed that this peptide specific immune response was due to CD4 T cells<br />
E<br />
expressing the b,<br />
7<br />
but not the aintegrin protein, indicating that A-gliadin 57-73 QE65<br />
specific T cells express the abintegrin<br />
4 7<br />
associated with homing to the intestinal lamina<br />
22<br />
propria . Pre-incubation <strong>of</strong> PBMC from HLA-DQ2 homozygous subjects with<br />
antibody specific for HLA-DQ (but not HLA-DR or HLA-DP) blocks A-gliadin 57-73<br />
QE65 responses, indicating HLA-DQ2 restriction.<br />
In one subject who consumed only 2 slices <strong>of</strong> bread, IFNg-secreting T cells specific<br />
for A-gliadin 57-73 QE65 were induced on day 6 and persisted until day 12. In another<br />
subject who consumed 4 slices <strong>of</strong> bread daily for 10 days, A-gliadin 57-73 QE65-<br />
specific T cells were also present on day 6-8. IFNgsecretion was only induced by A-<br />
gliadin 57-73 QE65 in subjects who consumed bread for 3 days. However, PBMC<br />
collected on day 11 from the subject who consumed bread for 10 days secreted IFNgin<br />
response to 6 out <strong>of</strong> 10 pools <strong>of</strong> tTG-treated A-gliadin peptides (one pool included A-<br />
gliadin 57-73). Hence, T cell epitope spreading occurs as early as 10 days after<br />
commencing antigen challenge.<br />
These studies indicated:<br />
1. In A-gliadin, there is a hierarchy <strong>of</strong> T cell epitopes with only one dominant T cell<br />
epitope.<br />
2. T cells specific for the dominant epitope are present in peripheral blood only
22 A DOMINANT EPITOPE IN GLUTEN PEPTIDES ?<br />
transiently after gluten challenge in vivo, but have predictable kinetics.<br />
3. Gluten challenge induces T cells specific for the same dominant A-gliadin<br />
epitope in all HLA-DQ2 <strong>coeliac</strong> subjects.<br />
Gliadin-specific intestinal T cell clones are focused on two peptides closely related<br />
to A-gliadin 57-73 QE65<br />
15<br />
Arentz-Hansen et al. have shown that two peptides from a panel <strong>of</strong> 11 recombinant<br />
a-gliadins are common epitopes for gliadin-specific intestinal T cell clones. T cell lines<br />
specific for one or both <strong>of</strong> these peptides (QLQPFPQPELPY and<br />
+<br />
PQPELPYPQPELPY) were raised from intestinal biopsies <strong>of</strong> 17/17 HLA-DQ2<br />
<strong>coeliac</strong> subjects on gluten free diet. These peptides closely resemble A-gliadin 57-73<br />
QE65 and contain the core sequence PELPY, supporting the concept that intestinal and<br />
peripheral blood T cell responses induced with gluten challenge are qualitatively<br />
similar. More importantly, if intestinal and peripheral blood T cell responses share the<br />
same specificity it is likely the ex vivo polyclonal peripheral blood T cell response will<br />
be more informative than T cell clones or lines for studies <strong>of</strong> molecular specificity and<br />
definition <strong>of</strong> T cell epitope hierarchies in <strong>coeliac</strong> <strong>disease</strong>.<br />
Comparison <strong>of</strong> HLA-DQ2 restricted epitopes <strong>of</strong> T cell clones with A-gliadin 57-73<br />
QE65<br />
We have studied various HLA-DQ2 restricted gliadin epitopes (Tab. 1) in IFNg<br />
ELISpot assays using PBMC from HLA-DQ2 <strong>coeliac</strong> subjects on day 6 <strong>of</strong> gluten<br />
23<br />
challenge (3 days, 200g gluten-containing bread daily) . A-gliadin 31-49 and GDB2<br />
do not induce IFNgresponses above background levels, while A-gliadin 57-68 QE65 is<br />
generally 25 % and a2 gliadin 62-75 QE65 QE72 60% as bioactive as A-gliadin 57-73<br />
QE65 at optimal concentrations (25 µ g/ml). To determine whether T cells specific for<br />
a2 gliadin 62-75 QE65 QE72 are part <strong>of</strong> the polyclonal T cell response to A-gliadin 57-<br />
73 QE65, IFNgELISpot responses to a2 gliadin 62-75 QE65 QE72 or A-gliadin 57-73<br />
QE65 (25 µ g/ml) alone or mixed together were compared. There was no difference<br />
between A-gliadin 57-73 QE65 alone or mixed with a2 gliadin 62-75 QE65 QE72,<br />
suggesting that in vivo T cells specific for a2 gliadin 62-75 QE65 QE72 and/or A-<br />
gliadin 57-68 QE65 are simply part <strong>of</strong> the polyclonal T cell response targeting A-gliadin<br />
57-73 QE65.<br />
A-gliadin 57-68 (QE65)<br />
QLQPFPQPELPY<br />
a2 gliadin 62-75 (QE65 QE72) PQPELPYPQPELPY<br />
A-gliadin 31-49<br />
LGQQQPFPPQQPYPQPQPF<br />
g-gliadin (GDB2)<br />
QQLPQPEQPQQSFPEQERPF<br />
Tab. 1. HLA-DQ2 restricted epitopes <strong>of</strong> gliadin-specific intestinal T cell clones<br />
A-gliadin 57-73 QE65 is the optimal a-, a/b-gliadin polymorphism<br />
23<br />
A-gliadin 57-73 spans a highly polymorphic region <strong>of</strong> the a-, a/b-gliadins (Tab.2) .
A DOMINANT EPITOPE IN GLUTEN PEPTIDES ?<br />
23<br />
We have compared IFNgELISpot responses <strong>of</strong> all the a-, a/b-gliadin polymorphisms <strong>of</strong><br />
A-gliadin 57-73 found by SwissProt using the search sequence<br />
XXXXXXXPQLPYXXXXX. Amongst these polymorphisms, bioactivity <strong>of</strong><br />
QLQPFPQPQLPYPQPQ[P,L] is identical to QLQPFPQPQLPYPQPQS after<br />
d e a m i d a t i o n b y t T G o r s u b s t i t u t i o n Q E 6 5 . t T G - d e a m i d a t e d<br />
PQLPYPQPQLPYPQPQ[P,L] is generally 80% as bioactive as<br />
QLQPFPQPQLPYPQPQS, but substitution <strong>of</strong> P69 for serine or leucine reduces<br />
bioactivity by 60%. Other polymorphisms are generally less than 20% as bioactive as<br />
A-gliadin 57-73. Hence, tTG-deamidated or QE-substituted at position 9,<br />
QLQPFPQPQLPYPQPQ[P,L,S] is the a-, a/b-gliadin polymorphism <strong>of</strong> A-gliadin 57-<br />
73 with optimal bioactivity.<br />
QLQPFPQ……………… PQLPYPQPQP<br />
QLQPFPQ……………… PQLPYSQPQP<br />
QLQPFPQ……………… PQLPYSQPQQ<br />
QLQPFPQ……………… PQLSYSQPQP<br />
QLQPFPQ……………… PQLPYLQPQP<br />
QLQPFSQ……………… PQLPYSQPQP<br />
QLQPFLQ……………… PQLPYSQPQP<br />
QLQPFLQPQPFP……… PQLPYSQPQP<br />
QLQPFPQPQLPYPQPQLPYPQLPYPQPQP<br />
QLQPFPQPQLPYPQ… PQLPYPQPQP<br />
QLQPFPQPQPFPPQLPYPQPQLPYPQPQP<br />
QLQPFPR……………… PQLPYPQPQP<br />
QLQPFPQPQPFP……… PQLPYPQPPP<br />
QLQPFPQPQPFL……… PQLPYPQPQS<br />
QLQPFPQPQPFP……… PQLPYPQPQS<br />
QPQPFP…………………PQLPYPQTQP<br />
QPQPFPPQ…………… PQLPYPQTQP<br />
Tab. 2. Polymorphisms in the region <strong>of</strong> A-gliadin 57-73 among the 61 Triticum aestivum a-,<br />
a/b-gliadin cDNA-derived protein sequences in Genbank<br />
One reason for the selection <strong>of</strong> QLQPFPQPQLPYPQPQ[L,P,S] and<br />
PQLPYPQPQLPYPQPQ[P,L] as potent epitopes may be that these sequences are<br />
resistant to proteases. Chymotrypsin and pepsin both cleave peptide bonds after<br />
hydrophobic residues. In vitro digestion <strong>of</strong> these peptides and less potent<br />
polymorphisms with tyrosine at position 12 followed by proline, serine or leucine,<br />
indicates that proline at position 13 prevents susceptibility to both chymotrypsin and<br />
pepsin. Hence, it is possible that the specificity <strong>of</strong> the T cell response is shaped by the<br />
susceptibility <strong>of</strong> gliadin peptides to proteases in the gut (and presumably in antigen<br />
presenting cells).<br />
Immune toxicity <strong>of</strong> wheat, rye and barley due to peptides cross-reactive with A-<br />
gliadin 57-73, or epitope spreading initiated by B cells specific for sequences<br />
adjacent to A-gliadin 57-73 QE65<br />
The data we have gathered using PBMC following in vivo gluten challenge in
24 A DOMINANT EPITOPE IN GLUTEN PEPTIDES ?<br />
<strong>coeliac</strong> <strong>disease</strong> are consistent with A-gliadin 57-73 deamidated by tTG being the<br />
dominant a-, a/b-wheat gliadin T cell epitope. Searches for peptides including the core<br />
sequence PQLPY have not revealed other wheat, rye or barley gluten sequences outside<br />
the a-, a/b-gliadins <strong>of</strong> wheat. One possibility is that epitope spreading initiated by the<br />
dominant epitope leads to other epitopes in gluten being recognized. Interestingly, B<br />
cell epitopes have been identified that are immediately adjacent or including the C - and<br />
24-25<br />
N-terminal portions <strong>of</strong> A-gliadin 57-73 . The other HLA-DQ2 restricted epitopes, g-<br />
gliadin GDB2 and A-gliadin 31-49 are also adjacent to or include sequences identical to<br />
or very similar to the same gliadin B cell epitope (QXQPFP). Hence, B cell mediated<br />
epitope spreading may be initiated by B cells given “help” by T cells specific for the<br />
dominant epitope. Alternatively, wheat, rye and barley may contain prolamin<br />
sequences that are cross-reactive with A-gliadin 57-73 but do not include PQLPY, or<br />
there are other unique dominant epitopes.<br />
Fine molecular specificity <strong>of</strong> A-gliadin 57-73 QE65-specific peripheral blood T<br />
cells<br />
Residues in A-gliadin 57-73 QE65 that determine bioactivity were mapped by<br />
comparing bioactivity <strong>of</strong> A-gliadin 57-73 QE65 variants substituted with lysine at each<br />
22<br />
aminoacid . Bioactivity was abolished if lysine was substituted at position 8-11<br />
(PELP), and substantially reduced with lysine at positions 4-7 (PFPQ) and 12-13 (YP).<br />
Single aminoacid substituted variants <strong>of</strong> A-gliadin 57-73 QE65 with all naturally<br />
occurring aminoacids except cysteine at positions 4-13 were synthesized and their<br />
bioactivity compared to the parent peptide. Positions 4-7 were highly sensitive to<br />
substitution, no more than three aminoacids at each position conveyed bioactivity<br />
greater than 50% <strong>of</strong> the parent peptide. Positions 4-7 and 12-13 were less sensitive to<br />
substitution but certain aminoacids such as proline, lysine and arginine tended to<br />
abolish bioactivity. The fine molecular specificity <strong>of</strong> peripheral blood T cells for A-<br />
gliadin 57-73 QE65 was similar amongst all <strong>of</strong> the eight <strong>coeliac</strong> subjects tested.<br />
Antigen-specific therapy using A-gliadin 57-73 Qe65<br />
A-gliadin 57-73 QE65 is clearly “the dominant” or “one <strong>of</strong> the dominant” gliadin T<br />
cell epitopes in HLA-DQ2-associated <strong>coeliac</strong> <strong>disease</strong>. Therefore it is reasonable to<br />
consider peptide therapeutics based on A-gliadin 57-73 QE65. Peptide delivered orally<br />
or nasally would be simple and easy to formulate. Another possibility is design <strong>of</strong><br />
altered peptide ligand (APL) antagonists that differ from the parent peptide by one or<br />
more residues and subtly alter T cell receptor signaling. APL antagonsists have the<br />
26<br />
potential to “switch <strong>of</strong>f” or “skew” TH1 to TH2 responses in vitro . We have shown<br />
that at least 5 single aminoacid-substituted variants <strong>of</strong> A-gliadin 57-73 QE65 with weak<br />
agonist properties also significantly reduce IFNgELISpot responses to A-gliadin 57-73<br />
QE65 when incubated in 5-fold excess with A-gliadin 57-73 QE65 (unpublished<br />
observations). It is likely that multiple substitutions or “cocktails” <strong>of</strong> APL antagonsists<br />
will be required for complete blockade <strong>of</strong> the polyclonal T cell response to A-gliadin<br />
57-73 QE65.
A DOMINANT EPITOPE IN GLUTEN PEPTIDES ?<br />
25<br />
Conclusions<br />
Gluten challenge in <strong>coeliac</strong> <strong>disease</strong> allows gliadin-specific T cell responses to be<br />
measured and epitope hierarchies defined. This method has significant advantages over<br />
T cell clones. One dominant T cell epitope has been defined in A-gliadin and is likely to<br />
be the dominant a-, a/b-wheat gliadin T cell epitope. Whether there are other distinct<br />
dominant T cell epitopes in other classes <strong>of</strong> gliadin in wheat, rye and barley, or whether<br />
toxicity <strong>of</strong> these proteins is due to cross-reactivity with A-gliadin 57-73 QE65 is crucial<br />
to the design <strong>of</strong> antigen-specific therapeutics. In either case, gluten challenge and<br />
testing the bioactivity <strong>of</strong> peptides and proteins using PBMC will allow the importance<br />
<strong>of</strong> particular epitopes to be determined. The efficacy <strong>of</strong> altered peptide ligand<br />
antagonists targeting A-gliadin 57-73 QE65 provides pro<strong>of</strong> <strong>of</strong> principle that peptide<br />
therapeutics may be a practical approach to the treatment <strong>of</strong> <strong>coeliac</strong> <strong>disease</strong> without<br />
resort to gluten free diet.<br />
References<br />
1. Sollid LM. Molecular basis <strong>of</strong> <strong>coeliac</strong> <strong>disease</strong>. Ann Rev Immunol 2000 ; 18: 53-81.<br />
2. Nilsen EM, Jahnsen FL, Lundin KEA, Johansen F-E, Fausa O, Sollid LM, et al.<br />
Gluten induces an intestinal cytokine response strongly dominated by interferon<br />
gamma in patients with celiac <strong>disease</strong>. Gastroenterology 1998; 115: 551-63.<br />
3.Tuckova L, Flegelova Z, Tlaskalova-Hogenova H, Zidek Z. Activation <strong>of</strong><br />
macrophages by food antigens: enhancing effect <strong>of</strong> gluten on nitric oxide and<br />
cytokine production. J Leuk Biol 2000; 67: 312-8.<br />
4.Tuohy VK, Yu M, Ling Y, Kawczak JA, Kinkel RP. Spontaneous regression <strong>of</strong> <strong>primary</strong><br />
autoreactivity during chronic progression <strong>of</strong> experimental autoimmune<br />
encephalitis and multiple sclerosis. J Exp Med 1999; 189: 1033-42.<br />
5. Yewdell JW, Bennink JR. Immunodominance in major histocompatibility complex<br />
class I-restricted T lymphocyte responses. Ann Rev Immunol 1999 ; 17: 51-88.<br />
6. Tuohy VK, Yu M, Weinstock-Guttman B, Kinkel RP. Diversity and plasticity <strong>of</strong> self<br />
recognition during the development <strong>of</strong> multiple sclerosis. J Clin Invest 1997; 99:<br />
1682-90.<br />
7. McCluskey J, Farris AD, Keech CL, Purcell AW, Rischmueller M, Kinoshita G, et<br />
al. Determinant spreading: lessons from animal models and human <strong>disease</strong>.<br />
Immunol Rev 1998; 164: 209-29.<br />
8. Drakesmith H, O'Neill D, Schneider SC, Binks M, Medd P, Sercarz E, et al. In vivo<br />
priming <strong>of</strong> T cells against cryptic determinants by dendritic cells exposed to<br />
interleukin 6 and native antigen. Proc Natl Acad Sci USA 1998; 95: 14903-8.<br />
9. Flugel A, Berkowicz T, Ritter T, Labeur M, Jenne DE, Li Z, et al. Migratory activity<br />
and functional changes <strong>of</strong> green fluorescent effector cells before and during<br />
experimental autoimmune encephalitis. Immunity 2001; 14: 547-60.<br />
10. Gutgeman I, Fahrer AM, Altman JD, Davis MM, Chien Y-h. Induction <strong>of</strong> rapid T cell<br />
activation and tolerance by systemic presentation <strong>of</strong> an orally administered<br />
antigen. Immunity 1998; 8: 667-73.<br />
11. Arstila T, Arstila TP, Calbo S, Selz F, Malassis-Seris M, Vassalli P, et al. Identical T<br />
cell clones are located within the mouse gut epithelium and lamina propria and
26 A DOMINANT EPITOPE IN GLUTEN PEPTIDES ?<br />
circulate in the thoracic duct. J Exp Med 2000; 191: 823-34.<br />
12. Molberg O, McAdam SN, Korner R, Quarsten H, Kristiansen C, Madsen L, et al.<br />
Tissue transglutaminase selectively modifies gliadin peptides that are recognized<br />
by gut-derived T cells in celiac <strong>disease</strong>. Nat Med 1998; 4:713-7.<br />
13. Weiser H. The precipitating factor in <strong>coeliac</strong> <strong>disease</strong>. Balliere's Clin Gastroenterol<br />
1995; 9:191-207.<br />
14. Kasarda DD, Okita TW, Bernardin JE, Baeker PA, Nimmo CC, Lew EJ-L, et al.<br />
Nucleic acid (cDNA) and amino acid sequences <strong>of</strong> type gliadins from wheat<br />
(Triticum aestivum). Proc Natl Acad Sci USA 1984; 81: 4712-6.<br />
15. Arentz-Hansen H, Korner R, Molberg O, Quarsten H, Van der Wal Y, Kooy YMC, et<br />
al. The intestinal T cell response to agliadin in adult celiac <strong>disease</strong> is focused on a<br />
single deamidated glutamine targeted by tissue transglutaminase. J Exp Med 2000;<br />
191: 603-12.<br />
16. Sjostrom H, Lundin KEA, Molberg O, Korner R, McAdam SN, Anthonsen D, et al.<br />
Identification <strong>of</strong> a-gliadin T-cell epitope in <strong>coeliac</strong> <strong>disease</strong>: general importance <strong>of</strong><br />
gliadin deamidation for intestinal T-cell recognition. Scand J Immunol 1998 ; 48 :<br />
111-5.<br />
17. van de Wal Y, Kooy YM, van Veelen P, Vader W, August SA, Drijfhout JW, et al.<br />
Glutenin is involved in the gluten-driven mucosal T cell response. Eur J Immunol<br />
1999 ; 29: 3133-9.<br />
18. Aeschilmann D, Paulsson M. Transglutaminases: protein cross-linking enzymes in<br />
tissues and body fluids. Thromb Haemost 1994; 71: 402-15.<br />
19. Gjertsen HA, Sollid LM, Ek J, Thorsby E, Lundin KEA. T cells from the peripheral<br />
blood <strong>of</strong> <strong>coeliac</strong> <strong>disease</strong> patients recognize gluten antigens when presented by HLA-<br />
DR, -DQ, or DP molecules. Scand J Immunol 1994 ; 39: 567-74.<br />
20. Anderson RP, Degano P, Godkin AJ, Jewell DP, Hill AVS. In vivo antigen challenge<br />
in celiac <strong>disease</strong> identifies a single transglutaminase-modified peptide as the<br />
dominant A-gliadin T-cell epitope. Nat Med 2000; 6: 337-42.<br />
21. Sallusto F, Lenig D, Forster R, Lipp M, Lanzavecchia A. Two subsets <strong>of</strong> memory T<br />
lymphocytes with distinct homing potentials and effector functions T cell memory.<br />
Nature 1999; 401: 708-12.<br />
22. Anderson RP, Jewell DP, Hill AVS. Peripheral blood T cells induced by gluten<br />
challenge in <strong>coeliac</strong> <strong>disease</strong> target a specific molecular motif and express a guthoming<br />
integrin. Gastroenterology 2001; 120: A-684.<br />
23. Anderson RP, Jewell DP, Hill AVS. Bioactivity <strong>of</strong> peptides homologous to the<br />
<strong>coeliac</strong>-specific dominant A-gliadin T cell epitope. Gastroenterology 2011; 120: A-<br />
683.<br />
24. ten Dam M, Van de Wal Y, Mearin ML, Kooy Y, Pena S, Drijfhout JW, et al. Antialpha-gliadin<br />
antibodies (AGA) in the serum <strong>of</strong> <strong>coeliac</strong> children and controls<br />
recognize an identical collection <strong>of</strong> linear epitopes <strong>of</strong> alpha-gliadin. Clin Exp<br />
Immunol 1998; 114: 189-95.<br />
25. Osman AA, Gunnel T, Dietl A, Uhlig HH, Amin B, Fleckenstein B, et al. B cell<br />
epitopes <strong>of</strong> gliadin. Clin Exp Immunol 2000; 121: 248-54.<br />
26. Bielekova B, Martin R. Antigen-specific immunomodulation via altered peptide<br />
ligands. J Mol Med 2001; 79: 552-65.
Catassi C, Fasano A, Corazza GR (eds):<br />
Primary <strong>prevention</strong> <strong>of</strong> <strong>coeliac</strong> <strong>disease</strong>. The<br />
utopia <strong>of</strong> the new millennium? Perspectives on<br />
Coeliac Disease, vol. 1, AIC Press, pp 27-29<br />
Role <strong>of</strong> A-gliadin 31 - 49 peptide<br />
Paul J Ciclitira<br />
The Rayne Institute, St. Thomas’ Hospital, London, UK<br />
Coeliac <strong>disease</strong> was first described in 1888. Samuel Gee who gave a classic<br />
description <strong>of</strong> a wasting <strong>disease</strong> mostly affecting children and causing diarrhoea,<br />
concluded at the end <strong>of</strong> his treaties, "if the patient can be cured at all, it must be by means<br />
<strong>of</strong> the diet". It is unfortunate that his treatment at that time comprised thin gruel which<br />
contained wheat flour. It remained until 1953, for Pr<strong>of</strong>essor Dicke and colleagues to<br />
publish their findings that wheat, rye and barley exacerbated the condition. They also<br />
noted that oats was toxic, which was probably due to contamination <strong>of</strong> flour with wheat.<br />
Dicke's experiment at that time compromised <strong>of</strong> making a slurry <strong>of</strong> the individual flours<br />
in water, pouring them down an eight year old child 's throat and noting that the child<br />
collapsed with vomiting, diarrhoea and near death. They extended this work to show<br />
that the most toxic component <strong>of</strong> wheat resides in the endosperm or flour fraction.<br />
However, the germ and husk were mildly toxic. This was probably due to<br />
contamination <strong>of</strong> these fractions with the gluten proteins.<br />
Flour contains proteins and water soluble starch fractions. Purified wheat starch is<br />
<strong>of</strong>ten used for the production <strong>of</strong> gluten-free products. Wheat flour proteins can be<br />
divided into four groups <strong>of</strong> which gliadins and glutenins together comprise 90% <strong>of</strong> the<br />
protein. The albumins and globulins are minor protein fractions. The glutenins have<br />
molecular weights ranging from 50 kilodaltons to many millions and entrap carbon<br />
dioxide in the dough enabling it to prove and rise. It was in early studies that the alcohol<br />
soluble or gliadin fraction <strong>of</strong> gluten was shown to be toxic in <strong>coeliac</strong> <strong>disease</strong>. The<br />
gliadin proteins were sub-divided into four fractions termed a, b, gand waccording to<br />
their relative electrophoretic mobility. More recently, they were classified as a, g, and w<br />
fractions according to their N-terminal amino acid sequences. We previously purified,<br />
using column chromatography with 20 litres eluent, gliadin into its a,b, g, and w<br />
fractions. The complexity <strong>of</strong> the individual gliadins was shown in further experiments.<br />
Having made polyclonal anti-sera against each gliadin fraction, we looked for<br />
precipitin lines on Ouchterlony gels which revealed four precipitin lines to gliadin, with<br />
an anti-gliadin serum. Precipitin lines were shared between gliadin subfraction<br />
suggesting that they share antigenic determinants. We subsequently used an in vitro<br />
27
28 ROLE OF A-GLIADIN 31-49 PEPTIDE<br />
organ culture model. Small intestinal biopsies were placed on an organ culture grid and<br />
incubated for 16-18 hours in the presence or absence <strong>of</strong> a putatively toxic fraction. We<br />
measured enterocyte surface cell heights on sections <strong>of</strong> the biopsies. Using this<br />
technique, we reported that each <strong>of</strong> the gliadin fractions, that is a, b, gand was<br />
enterotoxic to <strong>coeliac</strong> small intestinal mucosa. Dr Kasarda subsequently went on to<br />
sequence gliadin. The now classic sequence <strong>of</strong> A-gliadin is known to be 266 amino<br />
1<br />
acids long . This is an unusual protein in that it is composed by 10-15% proline and 30-<br />
35% glutamine residues; this is an efficient method <strong>of</strong> storing nitrogen for the growing<br />
plant.<br />
We subsequently went on to develop an in vivo method <strong>of</strong> assessing the toxicity <strong>of</strong><br />
gliadin fractions. This involved passing a Quintron multiple biopsy capsule into the<br />
proximal small intestine to which was taped an infusion tube. This allowed test<br />
fractions to be infused and multiple small intestinal biopsies to be taken over eight<br />
hours. These could then be sectioned and assessed blindly for villous height, crypt<br />
depth ratio, epithelial surface cell height and intraepithelial lymphocyte count. Using<br />
this system, we tested on different days 10 mg, 100 mg followed by 500 mg, and 1g <strong>of</strong><br />
gliadin. We showed that 10 mg produced no histological relapse, 100 mg minimal and<br />
500 mg moderate histological relapse. With 1 g there was gross flattening <strong>of</strong> the mucosa<br />
which commenced between 1-2 hours, was maximal at 4 hours and started to recover by<br />
6 hours. We observed flattening <strong>of</strong> the mucosa, with complete loss <strong>of</strong> the normal villous<br />
2<br />
architecture . We have also used electron microscopy to show increase in the number <strong>of</strong><br />
lysosome-like bodies below the brush border, which occurs 1-2 hours after<br />
commencing gluten challenges, suggesting that these may be relevant to the<br />
pathogenesis <strong>of</strong> the condition. After a matter <strong>of</strong> hours, there is apoptosis and shedding<br />
<strong>of</strong> the surface enterocytes. We hypothesize that there is absorption <strong>of</strong> gluten protein<br />
between and through the enterocytes. Toxic gliadin peptides are presented by antigen<br />
presenting cells to gluten sensitive T cells which exacerbate the condition through the<br />
production <strong>of</strong> TH1 cytokines. We subsequently went on to perform in vivo experiments<br />
assessing the toxicity <strong>of</strong> peptide fractions corresponding to amino acids 31-49, 202-<br />
220, 3-21 <strong>of</strong> A-gliadin. We used, as a positive control, unfractionated gliadin. We tested<br />
four subjects and showed that a fraction corresponding to amino acids 31-49 was<br />
3<br />
enterotoxic and caused flattening <strong>of</strong> the mucosa while the other two peptides did not .<br />
In a variety <strong>of</strong> different experiments we showed that there was an induction <strong>of</strong> TH1<br />
cytokines and inducible nitric oxide, infiltration <strong>of</strong> the mucosa with T cells, a change in<br />
4<br />
the villous morphology and enterocyte surface cell height .<br />
Since gliadin is presented by antigen presenting cells to gluten sensitive T cells by<br />
HLA DQ2 or DQ8, we established a cellular binding assay to study the binding <strong>of</strong><br />
gliadin peptides to DQ2. We demonstrated that the peptide, corresponding to amino<br />
acid residues 31-49 <strong>of</strong> A-gliadin which caused in vivo toxicity, bound to DQ2. The two<br />
other peptides which we tested in vivo, but which did not cause toxicity, did not bind to<br />
5<br />
DQ2 . To date, no group has demonstrated the presence <strong>of</strong> a small intestinal T cell clone<br />
that is sensitive to gliadin 31-49. However, a peripheral blood clone which responds to<br />
6<br />
this peptide has been demonstrated . Interestingly, the peptide has also been shown to<br />
7<br />
induce CD4 T cell infiltration into the buccal mucosa <strong>of</strong> <strong>coeliac</strong> <strong>disease</strong> patients . We<br />
therefore felt that there is good evidence that A-gliadin 31-49 is a <strong>coeliac</strong> toxic epitope,<br />
although it may be a minor one.
ROLE OF A-GLIADIN 31-49 PEPTIDE 29<br />
References<br />
1. Kasarda DD, Okita TW, Bernadin JE, Backer PA, Nimmo C, Lew E, et al. Nucleic acid<br />
(cDNA) and amino acid sequences <strong>of</strong> type gliadins from wheat (Triticum aestivum). Proc Nat<br />
Acad Sci 1984; 81: 4712-6.<br />
2. Ciclitira PJ, Evans DJ, Fagg NLK, Lennox ES, Dowling RH. Clinical testing <strong>of</strong> gliadin<br />
fractions in <strong>coeliac</strong> patients. Clin Sci 1984; 66: 357-64.<br />
3. Sturgess R, Day P, Ellis HJ, Lundin KE, Gjertsen HA, Konakou M, et al. Wheat peptide<br />
challenge in <strong>coeliac</strong> <strong>disease</strong>. Lancet 1994; 343: 758-61.<br />
4. Kontakou M, Przemioslo RT, Sturgess RP, Limb GA, Ellis HJ, Day P, et al. Cytokine mRNA<br />
expression in the mucosa <strong>of</strong> treated <strong>coeliac</strong> patients after wheat peptide challenge. Gut 1995;<br />
37: 52-7.<br />
5. Shidraw RG, Parnell ND, Ciclitira PJ, Travers P, Evan G, Rosen-Bronson S. Binding <strong>of</strong><br />
gluten-derived peptides to the HLA-DQ2 (alpha 1*0501, beta 1*0201) molecule, assessed in<br />
a cellular assay. Clin Exp Immunol 1998; 111: 158-65.<br />
6. Gjertsen HA, Lundin KEA, Sollid L, Eriksen JA, Thorsby E.. T cell recognition <strong>of</strong> gliadin<br />
peptides presented by the <strong>coeliac</strong> <strong>disease</strong> associated HLA-DQ (a1*0501, B1*0201)<br />
heterodimer. Human Immunology 1994; 39:243-52.<br />
7. Lahteenoja H, Mäki M, Viander M, Raiha I, Vilja P, Rantala I, et al. Local challenge on oral<br />
mucosa with an alpha-gliadin related synthetic peptide in patients with <strong>coeliac</strong> <strong>disease</strong>. Am J<br />
Gastroenterol 2000; 95:2880-7.
Catassi C, Fasano A, Corazza GR (eds):<br />
Primary <strong>prevention</strong> <strong>of</strong> <strong>coeliac</strong> <strong>disease</strong>. The<br />
utopia <strong>of</strong> the new millennium? Perspectives on<br />
Coeliac Disease, vol. 1, AIC Press, pp 31-41<br />
The association <strong>of</strong> the HLA-DQ molecules with<br />
<strong>coeliac</strong> <strong>disease</strong> in the Saharawi: an evolutionary<br />
perspective<br />
1 2<br />
Francesco Cucca and Carlo Catassi<br />
1<br />
Department <strong>of</strong> Biomedical and Biotechnologies Sciences, University <strong>of</strong> Cagliari,<br />
2<br />
Cagliari, Italy. Department <strong>of</strong> Pediatrics , University <strong>of</strong> Ancona, Ancona, Italy.<br />
The familial clustering <strong>of</strong> CD<br />
Coeliac <strong>disease</strong> (CD) is an immune-mediated enteropathy caused by the ingestion<br />
<strong>of</strong> wheat and other gluten-containing cereals (rye, barley) in genetically predisposed<br />
1<br />
individuals . CD is strongly clustered in families as illustrated by the sibling lifetime<br />
2-3<br />
risk/population prevalence ratio, lequal s to 30-60 in different studies . These<br />
epidemiological observations indicate the strong influence <strong>of</strong> genetic factors in the<br />
<strong>disease</strong> predisposition. This is also strongly suggested by the recurrence risk <strong>of</strong> 70-<br />
4<br />
100% observed in monozygotic twins (MZ) . Twin studies are particularly important<br />
for human geneticists because the risk in MZ twins provides a direct estimate <strong>of</strong><br />
penetrance (the effect <strong>of</strong> the genotype on the phenotype) for the whole complement <strong>of</strong><br />
susceptibility alleles at multiple loci. While it is necessary to extend these preliminary<br />
studies in larger cohorts <strong>of</strong> twins, the fact that the recurrence risk might not be 100%,<br />
and thus that the penentrance is incomplete, might indicate that other modifying<br />
epigenetic factors, such as the stochastic rearrangements <strong>of</strong> the T-cell receptor, and/or<br />
other environmental factors (in addition to the gluten in the diet) could also be involved<br />
in CD.<br />
The contribution <strong>of</strong> genes located in the HLA region to CD predisposition<br />
The major histocompatibility complex (MHC) human leukocyte antigen (HLA)<br />
region on chromosome 6p21 contains the major and, so far, the only consistently<br />
confirmed genetic component for CD predisposition. The HLA/MHC contains a<br />
densely packed array <strong>of</strong> at least 150 genes in 3,500 kb <strong>of</strong> DNA. Proteins encoded within<br />
the HLA region determine the way in which antigens are processed, translocated and<br />
presented to T-lymphocytes. During development <strong>of</strong> the T cell repertoire, HLA class I<br />
and class II molecules control positive and negative selection <strong>of</strong> the T-lymphocytes in<br />
the thymus. Not surprisingly, therefore, genes in the HLA region influence<br />
susceptibility to a large number <strong>of</strong> disorders, particularly autoimmune <strong>disease</strong>s.<br />
31
32 COELIAC DISEASE IN THE SAHARAWI<br />
A long series <strong>of</strong> association studies from different Caucasian populations provided a<br />
convincing case that within the HLA region, the combined presence <strong>of</strong> the DQA1*0501<br />
and DQB1*0201 alleles, encoded by genes located in the class II sub-region, is the<br />
5<br />
<strong>primary</strong> predisposing factor for CD . These alleles are found either in phase within the<br />
DR3-DQA1*0501-DQB1*0201 haplotype or in trans in individuals carrying the DR7-<br />
HLA-DQA1*0201-DQB1*0201/DR5-HLA-DQA1*0501-DQB1*0301 genotype.<br />
Additionally, although to a much lesser extent, another molecule, HLA-DQA1*0301-<br />
5<br />
DQB1*0302, found on DR4 haplotypes, is associated with CD . More recently, linkage<br />
analysis in families with multiple cases, in particular tests <strong>of</strong> allele sharing by affected<br />
sibpairs (ASPs), proved that the HLA region encodes the main <strong>disease</strong> locus<br />
predisposing to CD. From these linkage data it was possible to compute that this region<br />
contributes about 40 % <strong>of</strong> the observed familial clustering <strong>of</strong> the <strong>disease</strong> assuming a<br />
2-3.<br />
multiplicative model <strong>of</strong> inheritance<br />
The role <strong>of</strong> these DQ molecules is further substantiated by the observation that<br />
antigen-presenting-cells positive for the DQA1*0501-DQB1*0201 (DQ2) and<br />
DQA1*0301-DQB1*0302 (DQ8) molecules are able to recognize and present gluten<br />
derived peptides to T cells obtained from biopsy specimens from the small intestine <strong>of</strong><br />
6-7<br />
CD patients . The gluten-reactive T cell clones isolated from biopsies were CD4+,<br />
CD8- and inhibition studies with anti-HLA antibodies demonstrated predominant<br />
6<br />
antigen presentation by the dimers encoded by the HLA-DQ loci .<br />
Non-HLA genes and CD<br />
The linkage data from affected sib pair (ASP) families from different populations<br />
indicates that the locus specific ls for the whole HLA region is equal to ~3. This value,<br />
assuming a multiplicative model <strong>of</strong> epistasis (which fits with the rapid fall <strong>of</strong>f in<br />
recurrence risk from first to second to third degree relatives) is equal to 40% <strong>of</strong> the<br />
familial clustering <strong>of</strong> the <strong>disease</strong> (log3/log15). These results imply that 60% <strong>of</strong> the<br />
familial clustering <strong>of</strong> the <strong>disease</strong> must be accounted for by non-HLA genes. To detect<br />
these non-HLA loci , some whole genome scans have been performed but, with the<br />
exception <strong>of</strong> the major <strong>disease</strong> locus in the HLA region on 6p21, they have given weak<br />
8-10<br />
and conflicting results . These results illustrate the difficulties <strong>of</strong> detecting (or<br />
replicating the detection <strong>of</strong>) genes <strong>of</strong> low to moderate effects using ASP-based<br />
methods. Low penetrance, compounded by small individual genetic effects <strong>of</strong> most <strong>of</strong><br />
the non-HLA <strong>disease</strong> loci create major limitations on the power <strong>of</strong> a study (and all the<br />
linkage scans so far performed were severely under-powered). Additionally, locus and<br />
allelic heterogeneity further complicate the search. Nevertheless, the generation <strong>of</strong><br />
<strong>primary</strong> hypotheses deriving from linkage analysis remains an invaluable step when<br />
embarking on an effort to define the genetic risk factors involved in an inherited <strong>disease</strong><br />
especially since whole genome scans <strong>of</strong> association are still technically and<br />
economically impractical and the presence <strong>of</strong> a <strong>disease</strong> model with strong epistasis<br />
between the <strong>disease</strong> loci could severely impair association studies but not linkage<br />
11 -5<br />
analysis . Prior evidence <strong>of</strong> linkage dramatically lowers the threshold (P value to 10 )<br />
required in an association/LD study <strong>of</strong> the linked region to be confident that the result is<br />
12<br />
not a false positive . Some <strong>of</strong> the aforementioned factors, in particular those related to<br />
the statistical power <strong>of</strong> the study, could be alleviated by further increasing the number <strong>of</strong>
COELIAC DISEASE IN THE SAHARAWI<br />
33<br />
ASP families, for instance in a consortium type study addressed to analyse all the CD<br />
ASP collectable worldwide on the order <strong>of</strong> 2,000 or more (ASPs). However, this<br />
strategy based on the analysis <strong>of</strong> very large sample sets <strong>of</strong> ASP families that have to be<br />
necessarily collected from different populations cannot provide a significant benefit<br />
regarding the confounding effects <strong>of</strong> genetic heterogeneity. An alternative approach<br />
could be to concentrate on an isolated population showing an high <strong>disease</strong> prevalence,<br />
to reconstruct all the relationships between the various affected cases and scan with<br />
parametric and non-parametric linkage tests the whole genome to detect non-HLA gene<br />
effects. It is likely that such a study design, already applied in the case <strong>of</strong> type 1<br />
13<br />
diabetes , would provide sufficient statistical power to detect significant results across<br />
the genome.<br />
The high prevalence <strong>of</strong> CD in the Saharawi population<br />
14<br />
CD is typically found in individuals <strong>of</strong> Caucasian origin . In Europe and North<br />
15-16<br />
America the <strong>disease</strong> prevalence is around 0.5-1 % <strong>of</strong> the general population .<br />
Recently a tenfold higher CD frequency (5.6 %) was reported in the Saharawi, a people<br />
<strong>of</strong> Arab and Berber origin with high degree <strong>of</strong> consanguinity, living in the Sahara desert<br />
17<br />
. We analysed the genetic association <strong>of</strong> the main CD locus in a group <strong>of</strong> Saharawi<br />
children affected with CD and their first-degree relatives. The aims <strong>of</strong> this study (which<br />
is described in details below) were:<br />
1) to evaluate whether the degree <strong>of</strong> association at the main <strong>disease</strong> locus was similar to<br />
that observed in other populations;<br />
2) to investigate how the frequency <strong>of</strong> the predisposing HLA molecules in the general<br />
Saharawi population relates to the high prevalence observed in this ethnic group.<br />
Patients and methods<br />
This work was performed on Saharawi refugees living in the camps near Tindouf,<br />
Algeria. Blood samples were collected with the informed consent from a group <strong>of</strong><br />
previously diagnosed subjects with CD and their first-degree relatives. The diagnosis <strong>of</strong><br />
CD was based on the finding <strong>of</strong> serum IgA class antiendomysium antibodies (EMA)<br />
positivity on at least two consecutive blood samples and, in a subgroup <strong>of</strong> patients, the<br />
17<br />
typical enteropathy at the small intestinal biopsy, as previously described . EMA were<br />
detected by indirect immun<strong>of</strong>luorescence on serum diluted both 1:5 and 1:50, using<br />
monkey oesophagus as the antigenic substrate (Antiendomisio Eurospital, Trieste,<br />
Italy). Patients were 79 subjects (33 males and 44 females) deriving from 69<br />
independent families, with a median age <strong>of</strong> 8 years (range: 2-37) and including 69<br />
probands, 8 siblings and 2 mothers. Overall 136 healthy subjects were also investigated<br />
with a median age <strong>of</strong> 30 years, range 2-70 years. These included 29 individuals from 9,<br />
non-CD, unrelated families and 107 first-degree relatives <strong>of</strong> the CD patients (53<br />
mothers, 17 fathers and 37 siblings). Additionally, in 12 parents <strong>of</strong> CD patients for<br />
which DNA samples were not available, the DQ genotypes were unequivocally<br />
deduced based on the available data from the other parent and the <strong>of</strong>fsprings.<br />
DNA was extracted using the chelex method starting from dried blood spots<br />
18<br />
(Guthrie cards) . Amplification <strong>of</strong> the polymorphic second exon <strong>of</strong> the HLA-DRB1,
34<br />
COELIAC DISEASE IN THE SAHARAWI<br />
DQB1 genes and dot blot analysis <strong>of</strong> amplified DNA with sequence specific<br />
19-21<br />
oligonucleotide probes (SSO) were carried out as previously reported . The DQA1<br />
alleles were inferred using the known patterns <strong>of</strong> linkage disequilibrium from the<br />
DRB1-DQB1 haplotypes.<br />
Parental haplotypes were reconstructed using a program written by Frank<br />
Dudbridge available at ftp://ftp-gene.cimr.cam.ac.uk/pub/s<strong>of</strong>tware/.<br />
A possible drawback <strong>of</strong> case-control analyses is their sensitivity to problems related<br />
to genetic stratification. In order to circumvent this problem, 82 affected family-based<br />
control, (AFBAC) DQA1-DQB1 haplotypes have been selected from all the families in<br />
22<br />
which the parents were available, as described for single alleles by Thomson . The<br />
AFBAC frequencies are based on the chromosomes that are never transmitted from the<br />
parents to affected children and provide a source <strong>of</strong> controls which is not sensitive to<br />
population stratification unless very recent. The control frequencies were also enriched<br />
by 18 chromosomes deriving from 9 unaffected and unrelated Saharawi individuals.<br />
The pseudo-controls (AFBAC) and control frequencies were nearly identical and<br />
therefore were merged (total controls equal to 100 chromosomes). Using these control<br />
haplotype frequencies and assuming Hardy-Weinberg equilibrium, we also established<br />
23<br />
the control genotype frequencies as previously described . The frequencies <strong>of</strong> the HLA<br />
class II haplotypes and genotypes obtained in patients and in controls, were then<br />
compared using a 2 x 2 chi-squared Pearson test. The odds ratios ORs) were calculated<br />
using the Wolf formula [a x d)/(b x c)]; when one element <strong>of</strong> this equation was 0 we used<br />
the Haldane formula: RR=[2a + 1) 2d +1)]/[2b +1) 2c +1)], where a is the number <strong>of</strong><br />
patients possessing the HLA antigen; d is the number <strong>of</strong> controls lacking the particular<br />
HLA antigen; b the number <strong>of</strong> patients lacking the particular antigen; c the number <strong>of</strong><br />
controls possessing the particular HLA antigen. In the association analyses performed<br />
in this study, we considered only the probands in the 8 families with more than one<br />
affected sibling. A correction for number <strong>of</strong> tests performed was applied by multiplying<br />
the P values for the tested markers present in more than 1 patient or 1 control<br />
(respectively 10 haplotypes and 8 genotypes).<br />
We also evaluated the evolutionary relationship between the Saharawis and the<br />
24<br />
other human groups. To this aim we performed a multi-dimensional scaling analysis<br />
carried out using the correlation matrix <strong>of</strong> the haplotype frequencies reported in the<br />
various populations and determined with a gene counting procedure.<br />
Who are the Saharawis?<br />
In order to obtain a visual output <strong>of</strong> the DRB1-DQA1-DQB1 haplotype distribution<br />
worldwide and obtain information about the evolutionary relationships between the<br />
various human groups we performed a multi-dimensional scaling analysis. The results<br />
<strong>of</strong> this analysis are shown in Fig.1. The first dimension splits Eastern and Western world<br />
populations. The Asian and the African appear to be the most differentiated human<br />
groups, with the Kogi and Cayapa native American populations as the most<br />
differentiated within the Asian group. The Caucasians are closely grouped and are<br />
located between the African and the Asian range <strong>of</strong> variability. The second dimension<br />
explains the diversity <strong>of</strong> the Caucasian group, which includes the North-African and the<br />
Saharawi samples. More specifically, the Saharawi population appears to be located in
COELIAC DISEASE IN THE SAHARAWI<br />
35<br />
the border between the European and the African range <strong>of</strong> variability. Thus, the genetic<br />
structure <strong>of</strong> this population is consistent with its geographical location.<br />
The association <strong>of</strong> the DQ molecules with CD in the Saharawi population<br />
We first established the sibling lifetime risk/population prevalence ratio, ls in our<br />
Saharawi sample set, that was equal to 3 (16.7%/5.6%). Because <strong>of</strong> the high <strong>disease</strong><br />
prevalence, the degree <strong>of</strong> familial clustering was lower in the Saharawi than in<br />
Caucasian populations ls = ~30).<br />
Next, we established the association <strong>of</strong> the haplotypes and genotypes at the main<br />
<strong>disease</strong> superlocus HLA-DQB1-DQA1 in this population. The distribution <strong>of</strong> the<br />
various haplotypes among the Saharawi CD patients and controls is shown in Tab. 1.<br />
The DQA1*0501-DQB1*0201 haplotype was positively associated with CD (OR:<br />
-6<br />
4.5, Pc = 1.4x10 ) while the DQA1*0102-DQB1*0604, haplotype showed some<br />
-3<br />
degree <strong>of</strong> negative association with the <strong>disease</strong> (OR: 0.4, Pc = 4.7x10 ). To our<br />
knowledge the latter finding has been never reported in other populations and therefore<br />
needs confirmation in independent sample sets.<br />
Tab. 2 shows the distribution <strong>of</strong> the genotypes among patients and controls. The<br />
(DR3)DQA1*0501-DQB1*0201/(DR3)DQA1*0501-DQB1*0201 encoding two<br />
putative a*0501 - b*0201 heterodimers was positively associated with CD (OR: 6.4,<br />
-2<br />
P= 2.4x10 ). The (DR3)DQA1*0501-DQB1*0201/(DR4)DQA1*0301-DQB1*0302<br />
and the (DR3)DQA1*0501-DQB1*0201/(DR7)DQA1*0201-DQB1*0201 genotypes<br />
showed a trend toward a positive association (OR: 8.6 and 2.4 respectively) without<br />
reaching the level <strong>of</strong> significance.<br />
Overall, 91.3% <strong>of</strong> the patients, but only 38.9% <strong>of</strong> the controls were found to be<br />
positive for the combined presence <strong>of</strong> the DQA1*0501 and DQB1*0201 alleles<br />
encoding in cis or in trans at least one putative a*0501 - b*0201 heterodimer. The<br />
patients positive for the DQA1*0501-DQB1*0201 or DQA1*03-0302 heterodimer<br />
HAPLOTYPES Patients Controls<br />
DQA1 DQB1 N N OR 95% C.I. P
36 COELIAC DISEASE IN THE SAHARAWI<br />
were instead 95.6% in comparison with 41.6% <strong>of</strong> the controls. Finally, all but one<br />
patient (98.6%) and 42.5% <strong>of</strong> the controls were found to be positive for the<br />
DQB1*0201 allele.<br />
The CD associations observed in the Saharawi population were then contrasted with<br />
5<br />
those observed in other populations . While the (DR3)DQA1*0501-<br />
DQB1*0201/(DR3) DQA1*0501-DQB1*0201 genotype seems to be strongly and<br />
GENOTYPES<br />
DQA1 DQB1 DQA1 DQB1<br />
Patients Controls<br />
N N OR 95% C.I. P
COELIAC DISEASE IN THE SAHARAWI<br />
37<br />
confirmation <strong>of</strong> the reliability <strong>of</strong> the CD diagnosis (based on both the serum EMA<br />
testing and the small intestinal biopsy) in these North African children. Most<br />
importantly, these results are also clear evidence that CD has a similar HLA association<br />
in distantly related populations. The aetiological mechanism <strong>of</strong> the class II association<br />
involves binding and T cell recognition <strong>of</strong> gluten derived peptides deaminated in the<br />
25<br />
small intestine by the enzyme tissue transglutaminase , and these properties <strong>of</strong> class II<br />
molecules are very likely conserved among different ethnic groups.<br />
In a manner consistent with the high <strong>disease</strong> prevalence, the main CD susceptibility<br />
haplotype DQA1*0501-DQB1*0201, detected nearly always within a DR3 haplotype,<br />
exhibited one <strong>of</strong> the highest frequencies in the world in the general background<br />
Saharawi population. This could partially explain the very high CD prevalence<br />
observed in the Saharawi population. However, it should be noted that a similar<br />
frequency <strong>of</strong> DQA1*0501-DQB1*0201 has been found also in other populations, such<br />
26<br />
as the Sardinians where the <strong>disease</strong> is around 5 times less frequent (1%) . Our results<br />
therefore suggest that other non-DQ genes or environmental factors are also operative<br />
in determining the high CD prevalence observed in the Saharawi.<br />
From an evolutionary perspective, such <strong>disease</strong> frequency might be related to the<br />
high prevalence <strong>of</strong> genes such as the Dq2, that have been selectively neutral or even<br />
beneficial for several hundred generations, that became disadvantageous following<br />
quick and dramatic changes <strong>of</strong> the environmental context in which the Saharawis lived.<br />
In the traditional Saharawi diet, the intake <strong>of</strong> gluten was very low and its introduction<br />
usually occurred after the second or third year <strong>of</strong> life. During the last century, in a span<br />
<strong>of</strong> few generations, wheat-based products, especially bread, have become the staple<br />
food after the Spanish colonization. Nowadays, gluten is introduced early in the<br />
Saharawi infant's diet, occasionally as early as the first month <strong>of</strong> life. Since in CD the<br />
27<br />
degree <strong>of</strong> intestinal mucosal damage is related to the amount <strong>of</strong> ingested gluten , the<br />
enteropathy <strong>of</strong> the “ancestral” CD-prone individuals was presumably milder. As such,<br />
in terms <strong>of</strong> genetic fitness, it did not represent a major selective disadvantage or might<br />
have even exerted some protective effect against intestinal infections because a<br />
moderately atrophic jejunal mucosa partially lacks the membrane receptors required<br />
28<br />
for microorganisms adhesion . Moreover, a mild CD and the accompanying small<br />
degree <strong>of</strong> inflammation <strong>of</strong> the jejunal mucosa, can also provide a source <strong>of</strong> reactive<br />
lymphomonocytes, thus further increasing the protective effect against intestinal<br />
infections. In contrast, the severe celiac enteropathy currently found in Saharawi<br />
children is associated with an early and high gluten intake and it is no longer neutral or<br />
“protective” but instead harmful, as it causes early intestinal malabsorption and<br />
29<br />
malnutrition, potentially leading to death .<br />
From these data a more general theory can be proposed. High <strong>disease</strong> frequency <strong>of</strong> a<br />
complex trait in a given population might be related to the high prevalence <strong>of</strong> genes that<br />
have been selectively neutral or even beneficial for several hundred generations, but<br />
became disadvantageous following quick changes <strong>of</strong> the environment. According to<br />
this interpretation, complex traits can be regarded as “residual traits“ caused by<br />
dramatic transformations <strong>of</strong> the environmental context in which a given population<br />
used to live across evolutionary time periods. Some environmental transformations can<br />
occur too quickly to be accompanied by changes in the genetic structure <strong>of</strong> the human<br />
populations. Indeed, the evolutionary time periods necessary to modify the genetic
38 COELIAC DISEASE IN THE SAHARAWI<br />
Dimension 2<br />
1.4<br />
Sub Saharian Africa<br />
SEN<br />
FIL<br />
Asia<br />
1<br />
+ Europe and N. Africa<br />
+<br />
+<br />
Gre<br />
+<br />
+<br />
0.6<br />
+<br />
Sard<br />
Bulg<br />
+<br />
+<br />
+<br />
HONG KONG<br />
0.2<br />
+<br />
+ + Cre<br />
ETH<br />
+<br />
-0.2<br />
+ ++ ++ +<br />
+ Rom<br />
CHI<br />
JAP<br />
+<br />
+<br />
Ita<br />
+<br />
Tun<br />
-0.6<br />
Tur<br />
POL<br />
+<br />
Mor<br />
+<br />
+<br />
Fra<br />
Spa +<br />
-1<br />
S AFR<br />
+<br />
GAB<br />
+ Cze<br />
Alg+<br />
Nw Rus<br />
Saha<br />
+<br />
+<br />
Nor + Gb<br />
-1.4<br />
+<br />
-2 -1.5 -1 -0.5 0 0.5 1 1.5 2 2.5<br />
Dimension 1<br />
Fig. 1. Multidimentional scaling <strong>of</strong> 26 populations tested for HLA DRB1-DQA1-DQB1<br />
haplotypes. The first dimension splits Eastern and Western world populations. The<br />
Caucasians are closely grouped and located in the African range <strong>of</strong> variability. The second<br />
dimension explains the diversity <strong>of</strong> the Sub-Saharan African and Caucasian groups, which<br />
include the North-African and Saharawi samples.<br />
On the right box, European and North African patterns were enlarged.<br />
30 31 32-33 34<br />
Population samples: ALG, Algerian ; BULG, Bulgarian ; CHI, Chinese ; CRE, Cretan ;<br />
35 36 37<br />
CZE, Czech ; ETH, Ethiopian ; FIL, Filipino ; FRA, French; ITA, Italian; RUM, Rumanian;<br />
38 39 40<br />
S-AFR, South-African; SEN, Senegalese; SPA, Spanish ; GAB, Gabonese ; GB, British ;<br />
41 32 42 43<br />
GRE, Greek ; HONG KONG, Hong-Kong ; JAP, Japanese ; MOR, Moroccan ; NOR,<br />
44 45 46 47<br />
Norwegian ; NW-RUS, North-Western Russian ; POL, Polynesian ; TUN, Tunisian ; TUR,<br />
48 49<br />
Turkish ;SARD, Sardinian and in circle font the Saharawi (current work).<br />
asset <strong>of</strong> a given population are on a much larger scale in comparison to those required to<br />
change environmental factors, i.e. the socalled “gene-environment evolutionary tempo<br />
mismatch”.<br />
Finally there is another important lesson coming from CD to understand the bases <strong>of</strong><br />
other multifactorial traits. CD tells us that some <strong>of</strong> the environmental factors involved<br />
in triggering these complex traits could be nearly ubiquitous (gluten). It might be<br />
extremely difficult to identify them in <strong>disease</strong>s in which the target organ is not able to<br />
regenerate when the trigger factor is removed.<br />
Acknowledgements<br />
We wish to thank Stefano De Virgiliis, M.Doloretta Macis, Mauro Congia, Michael<br />
Whalen , Laura Morelli, Patrizia Zavattari and Antonio Cao for advice and support.<br />
References<br />
1. Mäki M, Collin P. Coeliac <strong>disease</strong>. Lancet 1997; 349: 755-9.<br />
2. Risch N. Assessing the role <strong>of</strong> HLA-linked and unlinked determinants <strong>of</strong> <strong>disease</strong>. Am
COELIAC DISEASE IN THE SAHARAWI<br />
39<br />
J Hum Genet 1987; 401:1-14.<br />
3. Petronzelli F, Bonamico M, Ferrante P, Grillo R, Mora B, Mariani P, et al. Genetic<br />
contribution <strong>of</strong> the HLA region to the familial clustering <strong>of</strong> <strong>coeliac</strong> <strong>disease</strong>. Ann<br />
Hum Genet 1997; 61: 307-17.<br />
4. Polanco I, Biemond I, van Leeuven A, Shreuder I, Meera Khan P, Guerrero J, et al.<br />
In: mcConnel RB, ed. The genetics <strong>of</strong> <strong>coeliac</strong> <strong>disease</strong>. Lancaster 1981: MTP, 211-<br />
31.<br />
5. Sollid LM, Thorsby E. HLA susceptibility genes in celiac <strong>disease</strong>: genetic mapping<br />
and role in pathogenesis. Gastroenterology 1993; 105: 910-22.<br />
6. Lundin KE, Scott H, Hansen T, Paulsen G, Halstensen TS, Fausa O, et al. Gliadinspecific,<br />
HLA-DQ alpha 1*0501,beta 1*0201 restricted T cells isolated from the<br />
small intestinal mucosa <strong>of</strong> celiac <strong>disease</strong> patients. J Exp Med 1993; 178: 187-96.<br />
7. Lundin KE, Scott H, Fausa O, Thorsby E, Sollid LM. T cells from the small intestinal<br />
mucosa <strong>of</strong> a DR4, DQ7/DR4, DQ8 celiac <strong>disease</strong> patient preferentially recognize<br />
gliadin when presented by DQ8. Hum Immunol 1994; 41: 285-91.<br />
8. Greco L, Corazza G, Babron MC, Clot F, Fulchignoni-Lataud MC, Percopo S, et al.<br />
Genome search in celiac <strong>disease</strong>. Am J Hum Genet 1998; 62: 669-75.<br />
9. Zhong F, McCombs CC, Olson JM, Elston RC, Stevens FM, McCarthy CF, et al.An<br />
autosomal screen for genes that predispose to celiac <strong>disease</strong> in the western counties<br />
<strong>of</strong> Ireland. Nat Genet 1996; 14: 329-33.<br />
10. Houlston RS, Tomlinson IP, Ford D, Seal S, Marossy AM, Ferguson A, et al. Linkage<br />
analysis <strong>of</strong> candidate regions for <strong>coeliac</strong> <strong>disease</strong> genes. Hum Mol Genet 1997; 6:<br />
1335-9.<br />
11. Culverhouse R, Suarez BK, Lin J, Reich T. A perspective on epistasis: limits <strong>of</strong><br />
models displaying no main effect. Am J Hum Genet 2002; 70: 461-71.<br />
12. Dahlman I, Eaves IA, Kosoy R, Morrison VA, Heward J, Gough SC, et al.<br />
Parameters for reliable results in genetic association studies in common <strong>disease</strong>.<br />
Nat Genet 2002; 30: 149-50.<br />
13. Verge CF, Vardi P, Babu S, Bao F, Erlich HA, Bugawan T, et al. Evidence for<br />
oligogenic inheritance <strong>of</strong> type 1 diabetes in a large Bedouin Arab family. J Clin<br />
Invest 1998; 15: 1569-75<br />
14. Trier JS. Celiac sprue. N Engl J Med 1991; 325: 1709-19.<br />
15. Catassi C, Fabiani E, Rätsch IM, Coppa GV, Giorgi PL, Pierdomenico R, et al. The<br />
<strong>coeliac</strong> iceberg in Italy. A multicentre antigliadin antibodies screening for <strong>coeliac</strong><br />
<strong>disease</strong> in school-age subjects. Acta Paediatr 1996; Suppl 412: 29-35.<br />
16. Not T, Horvath K, Hill ID, Partanen J, Hammed A, Magazzù G, et al. Celiac <strong>disease</strong><br />
risk in the USA: high prevalence <strong>of</strong> antiendomysium antibodies in healthy blood<br />
donors. Scand J Gastroenterol 1998; 33: 494-8.<br />
17. Catassi C, Rätsch IM, Gandolfi L, Pratesi R, Fabiani E, El Asmar R, et al. Why is<br />
<strong>coeliac</strong> <strong>disease</strong> endemic in the people <strong>of</strong> the Sahara? Lancet 1999; 354: 647-8.<br />
18. Singer S, Tanguay R. Use <strong>of</strong> chelex to improve the PCR signal for a small number <strong>of</strong><br />
cells. Amplifications 1989; 3: 11.<br />
19. Horn GT, Bugawan TL, Long CM, Erlich HA. Allelic sequence variation <strong>of</strong> the<br />
HLA-DQ loci, relationship to serology and to insulin-dependent diabetes<br />
susceptibility. Proc Natl Acad Sci 1988; 85: 6012-6.<br />
20. Wordsworth BP, Allsopp CEM, Youg RP, Bell JI. HLA-DR typing using DNA
40 COELIAC DISEASE IN THE SAHARAWI<br />
amplification by the polymerase chain reaction and sequential hybridization to<br />
sequence-specific oligonucleotide probes. Immunogenetics 1990; 32: 413-8.<br />
21. Bugawan TL, Erlich HA. Rapid typing <strong>of</strong> HLA-DQB1 DNA polymorphism using<br />
nonradiactive oligonucleotide probes and amplified DNA. Immunogenetics 1991;<br />
33: 163-70.<br />
22. Thomson G. Mapping <strong>disease</strong> genes: family-based association studies. Am J Hum<br />
Genet 1995; 57: 487-98.<br />
23. Noble JA, Valdes AM, Cook M, Klitz W, Thomson G, Erlich HA. The role <strong>of</strong> HLA<br />
class II genes in insulin-dependent diabetes mellitus: molecular analysis <strong>of</strong> 180<br />
Caucasian, multiplex families. Am J Hum Genet 1996; 59: 1134-48.<br />
24. Kruscal, J.B. Multidimensional Scaling by Optimizing Goodness <strong>of</strong> fit to a<br />
Nonmetric Hypothesis. Psychometrika 1964; 29: 1-27.<br />
25. Schuppan D. Current concepts <strong>of</strong> celiac <strong>disease</strong> pathogenesis. Gastroenterology<br />
2000; 119: 234-42.<br />
26. Meloni G, Dore A, Fanciulli G, Tanda F, Bottazzo GF. Subclinical <strong>coeliac</strong> <strong>disease</strong> in<br />
schoolchildren from northern Sardinia. Lancet 1999; 353: 37.<br />
27. Marsh MN. Gluten, major histocompatibility complex, and the small intestine: a<br />
molecular and immunobiologic approach to the spectrum <strong>of</strong> gluten-sensitivity<br />
"celiac sprue". Gastroenterology 1992;102: 330-54.<br />
28. Kerneis S, Chauviere G, Darfeuille-Michaud A, et al. Expression <strong>of</strong> receptors for<br />
enterotoxigenic Escherichia coli during enterocytic differentiation <strong>of</strong> human<br />
polarized intestinal epithelial cells in culture. Infect Immun 1992;60: 2572-80.<br />
29. Rätsch IM, Catassi C. Coeliac <strong>disease</strong> is a <strong>primary</strong>, potentially treatable, health<br />
problem <strong>of</strong> Saharawi refugee children. Bulletin <strong>of</strong> the World Health Organization<br />
2001; 79: 541-5.<br />
30. Arnaiz-Villena A, Benmamar D, Alvarez M, Diaz-Campos N, Varela P, Gomez-<br />
Casado, et al. HLA allele and haplotype frequencies in Algerians. Relatedness in<br />
Spaniards and Basques. Hum Immunol 1995; 43: 259-68.<br />
31. Ivanova R, Naoumova E, Lepage V, Djoulah S, Yordanov Y, Loste MN et al. HLA-<br />
DRB1, DQA1, DQB1 DNA polymorphism in the Bulgarian population. Tissue<br />
Antigens 1996; 47: 122-6.<br />
32. Chang YW, Hawkins BR. HLA class I and class II frequencies <strong>of</strong> a Hong Kong<br />
Chinese population based on bone marrow donor registry data. Hum Immunol<br />
2002; 56: 125-35.<br />
33. Fernandez-Viña M, Gao X, Moraes ME, Moraes JR, Salatiel I, Miller et al. Alleles<br />
at four HLA class II loci determined by oligonucleotide hybridization and their<br />
associations in five ethnic groups. Immunogenetics 1991; 34: 299-312.<br />
34. Arnaiz-Villena, A., Iliakis, P., Gonzalez-Hevilla, M., Longas, J., Gomez-Casado, E.,<br />
Sfyridaki, K., et al. The origin <strong>of</strong> Cretan populations as determined by<br />
characterization <strong>of</strong> HLA alleles. Tissue Antigens 1999; 53: 213-26.<br />
35. Cernà,M, Fernandez-Vina M, Ivaskova E. and Stastny P. Comparison <strong>of</strong> HLA class<br />
II alleles in Gypsy and Czech populations by DNA typing with oligonucleotide<br />
probes. Tissue Antigens 1992; 39: 111-6.<br />
36. Fort M, de Stefano, G.F., Cambon-Thomsen, A., Giraldo-Alvarez, P., Dugoujon,<br />
J.M., Ohayon, E., et al. HLA class II allele and haplotype frequencies in Ethiopian<br />
Amhara and Oromo populations. Tissue Antigens 1998; 51: 327-36.
COELIAC DISEASE IN THE SAHARAWI<br />
41<br />
37. Mack SJ, Bugawan TL, Moonsamy PV, Erlich JA, Trachtenberg EA, Paik YK, et al.<br />
Evolution <strong>of</strong> Pacific/Asian populations inferred from HLA class II allele frequency<br />
distributions. Tissue Antigens 2000; 55: 383-400.<br />
38. Imanishi T, Akaza T, Kimura A, Tokunaga K, Gojobori T. Allele and haplotype<br />
frequencies for HLA and complement loci in various ethnic groups. In, Tsuji, K.,<br />
Aizawa, M. and Sasazuki, T. eds.:, HLA 1991. Oxford University Press, Oxford, UK,<br />
Vol. 1, pp. 1065-1220.<br />
39. Migot-Nabias F, Fajardy I, Danze PM, Everaere S, Mayombo Y, Minh TN, et al.<br />
HLA class II polymorphism in a Gabonese Banzabi population. Tissue Antigens<br />
1999; 53: 580-5.<br />
40. Doherty DG, Vaughan RW, Donaldson PT, Mowat AP. HLA DQA, DQB, and DRB<br />
genotyping by oligonucleotide analysis, distribution <strong>of</strong> alleles and haplotypes in<br />
British Caucasoids. Hum Immunol 1992; 34: 53-63.<br />
41 Papassavas EC, Spyropoulou-Vlachou M, Papassavas AC, Schipper RF, Doxiadis<br />
IN, Stavropoulos-Giokas C. MHC Class I and II phenotype, gene, and haplotype<br />
frequencies in Greeks using molecular typing data. Hum Immunol; 61: 615-23.<br />
42. Hashimoto M, Kinoshita T, Yamasaki M, Tanaka H, Imanishi T, Ihara, et al. Gene<br />
frequencies and haplotypic associations within the HLA region in 916 unrelated<br />
Japanese individuals. Tissue Antigens 2000;44: 166-73.<br />
43. Izaabel H, Garchon HJ, Caillat-Zucman S, Beaurain G, Akhayat O, Bach JF et al.<br />
HLA class II DNA polymorphism in a Moroccan population from the Souss, Agadir<br />
area. Tissue Antigens 1998; 51: 106-10.<br />
44. Rønningen KS, Spurkland A, Markussen G, Iwe T, Vartdal F, Thorsby E.<br />
Distribution <strong>of</strong> HLA class II alleles among Norwegian Caucasians. Hum Immunol<br />
1990; 29: 275-281.<br />
45. Kapustin S, Lyshchov A, Alexandrova J, Imyanitov E, Blinov M. HLA class II<br />
molecular polymorphisms in healthy Slavic individuals from North-Western Russia.<br />
Tissue Antigens 1999; 54: 517-520.<br />
46. Gao X, Zimmet P, Serjeantson SW. HLA-DR,DQ sequence polymorphisms in<br />
Polynesians, Micronesians, and Javanese. Hum Immunol 1992; 34: 153-161.<br />
47. Hmida S, Gauthier A, Dridi A, Quillivic F, Genetet B, Boukef K. HLA class II gene<br />
polymorphism in Tunisians. Tissue Antigens 1995; 45: 63-8.<br />
48. Saruhan-Direskeneli G, Esin S, Baykan-Kurt B, Ornek I, Vaughan R. Eraksoy M.<br />
HLA-DR and -DQ associations with multiple sclerosis in Turkey. Hum. Immunol.<br />
1997; 55: 59-65.<br />
49. Lampis R, Morelli L, Congia M, Macis MD, Mulargia A, Loddo M, et al. The interregional<br />
distribution <strong>of</strong> HLA class II haplotypes indicates the suitability <strong>of</strong> the<br />
Sardinian population for case-control association studies in complex <strong>disease</strong>s.<br />
Hum Mol Genet 2000; 9: 2959-65.
Catassi C, Fasano A, Corazza GR (eds):<br />
Primary <strong>prevention</strong> <strong>of</strong> <strong>coeliac</strong> <strong>disease</strong>. The<br />
utopia <strong>of</strong> the new millennium? Perspectives on<br />
Coeliac Disease, vol. 1, AIC Press, pp 43-60<br />
Primary <strong>prevention</strong> <strong>of</strong> <strong>coeliac</strong> <strong>disease</strong><br />
by favourable infant feeding practices<br />
1,2 1,3<br />
Anneli Ivarsson , Lars Åke Persson and Olle Hernell 2<br />
1 2<br />
Department <strong>of</strong> Public Health and Clinical Medicine, Epidemiology and Department<br />
3<br />
<strong>of</strong> Clinical Sciences, Pediatrics, both at Umeå University, Umeå, Sweden, and ICDDR,B:<br />
Centre for Health and Population Research, Dhaka, Bangladesh.<br />
Coeliac <strong>disease</strong> is now recognised as a common health problem throughout a large<br />
1-12<br />
part <strong>of</strong> the world . An effective treatment is available through adherence to a strict<br />
gluten-free diet. Screening studies have revealed that most cases are undiagnosed,<br />
which indicates the need for active case recognition, and possibly also a need for<br />
13-14<br />
screening efforts . However, even when <strong>coeliac</strong> <strong>disease</strong> has been diagnosed, the<br />
widespread use <strong>of</strong> gluten-containing foods makes compliance with the treatment<br />
15<br />
difficult . Clearly, then, it is desirable to explore additional strategies such as <strong>primary</strong><br />
<strong>prevention</strong>.<br />
Family clustering<br />
The risk for <strong>coeliac</strong> <strong>disease</strong> is higher in first degree relatives compared to the general<br />
population. In family members <strong>of</strong> <strong>coeliac</strong> patients, a prevalence <strong>of</strong> 10% is <strong>of</strong>ten<br />
16<br />
mentioned , and in monozygous twins the concordance rate has been estimated at<br />
17-18 19<br />
70% , or even higher .<br />
Family clustering is generally considered as evidence for a strong genetic influence<br />
in <strong>coeliac</strong> <strong>disease</strong> susceptibility. However, the fact that family members share not only<br />
genetics but, in many respects, also the same environment, should be taken into<br />
consideration. This is especially true for monozygous twins, who have a similar<br />
environment not only during childhood, as is the case for most siblings, but also have a<br />
similar environment in utero.<br />
A complex aetiology<br />
The aetiology <strong>of</strong> <strong>coeliac</strong> <strong>disease</strong> is not fully understood, largely as a consequence <strong>of</strong><br />
its complexity, although our understanding <strong>of</strong> different aspects <strong>of</strong> the <strong>disease</strong> process is<br />
rapidly increasing. Based on present knowledge, an immunological pathogenesis for<br />
the <strong>disease</strong> seems most likely. In some genetically susceptible individuals, exposure to<br />
gluten, or related proteins in rye and barley, triggers an errant immune response, which<br />
43
44<br />
INFANT FEEDING PRACTICES AND COELIAC DISEASE<br />
20-23<br />
by means <strong>of</strong> a cascade <strong>of</strong> events results in a chronic enteropathy .<br />
The human leukocyte antigen (HLA)-DQ2 molecule is expressed by more than<br />
90% <strong>of</strong> <strong>coeliac</strong> <strong>disease</strong> patients, compared to 20-30% <strong>of</strong> healthy controls, and the<br />
22<br />
majority <strong>of</strong> the remaining patients express the DQ8 molecule . It has been estimated<br />
that the HLA-complex confers 40% <strong>of</strong> the sibling family risk, and that non-HLA genes<br />
24-25<br />
are the most important . However, efforts to identify these contributing non-HLA<br />
26-27<br />
genes have thus far not resulted in conclusive evidence . In assessing the impact <strong>of</strong><br />
genetics, the ratio lis crucial. This ratio is constructed by the prevalence in relatives <strong>of</strong><br />
28<br />
an affected individual over the prevalence within the general population . Thus, if<br />
causal environmental exposures are aggregated in the family, the impact <strong>of</strong> genetics<br />
29<br />
will be overestimated .<br />
Most common <strong>disease</strong>s have a multifactorial aetiology, and they thus develop<br />
through an interaction between an individual's genetic predisposition and various<br />
30<br />
environmental exposures . This has been shown for insulin dependent diabetes<br />
mellitus (IDDM), which is an autoimmune <strong>disease</strong> with many similarities to <strong>coeliac</strong><br />
<strong>disease</strong>. The immune system has a key function in the pathogenesis <strong>of</strong> both <strong>disease</strong>s,<br />
31<br />
and there is an increased risk for <strong>coeliac</strong> <strong>disease</strong> in persons with IDDM .<br />
It has recently been suggested that each genetic risk factor, taken separately, may<br />
frequently be present in the general population, and it is the combination <strong>of</strong> some <strong>of</strong><br />
26<br />
these and their interaction with environmental factors that induces <strong>coeliac</strong> <strong>disease</strong> .<br />
Thus, in addition to the mere presence <strong>of</strong> gluten in the diet, environmental exposures<br />
may also be expected to be part <strong>of</strong> the causal pattern responsible for <strong>coeliac</strong> <strong>disease</strong>.<br />
Failure <strong>of</strong> oral tolerance<br />
Environmental exposures, including infant feeding, influence the immunological<br />
32-34<br />
process resulting in oral tolerance - or intolerance - to a food constituent .<br />
Considering recent knowledge <strong>of</strong> the aetiology <strong>of</strong> <strong>coeliac</strong> <strong>disease</strong>, this may be viewed at<br />
least hypothetically as a failure in the development <strong>of</strong>, or the later loss <strong>of</strong>, oral<br />
35<br />
tolerance .<br />
In most individuals, oral tolerance towards gluten develops and prevails throughout<br />
life. If oral tolerance fails to develop, however, or is later broken down, then gluten may<br />
act like a “dangerous” foreign antigen, resulting in the development <strong>of</strong> <strong>coeliac</strong> <strong>disease</strong>.<br />
The Swedish epidemic<br />
Sweden has experienced an unusual epidemic <strong>of</strong> symptomatic <strong>coeliac</strong> <strong>disease</strong> in<br />
36-37<br />
children . The incidence reached levels higher than ever reported, and the decline<br />
that followed was amazingly abrupt (Fig. 1). Only children below two years <strong>of</strong> age were<br />
affected, and most <strong>of</strong> the cases had symptoms as severe as those that had been observed<br />
38-39<br />
earlier . These findings are based on our population-based prospective incidence<br />
register established in 1991, covering 40% <strong>of</strong> the Swedish child population, and<br />
36<br />
retrospective data collected back to 1973 from 15% <strong>of</strong> the child population .<br />
Recently it was shown that this was indeed an epidemic <strong>of</strong> <strong>coeliac</strong> <strong>disease</strong><br />
enteropathy, and not only a shift in the proportion <strong>of</strong> cases with symptomatic
INFANT FEEDING PRACTICES AND COELIAC DISEASE<br />
45<br />
Cases per 100 000 person-years<br />
250<br />
200<br />
150<br />
100<br />
50<br />
0-1.9 years<br />
2-4.9 years<br />
5-14.9 years<br />
0<br />
1975 1981 1987 1993 1999<br />
Year <strong>of</strong> diagnosis<br />
Fig. 1. Annual incidence rate <strong>of</strong> <strong>coeliac</strong> <strong>disease</strong> in different age groups <strong>of</strong> children from<br />
37<br />
1973 to 1999. From with permission.<br />
enteropathy that were thus more readily diagnosed. A screening <strong>of</strong> 2½-year-old<br />
Swedish children including birth cohorts both from the epidemic and post-epidemic<br />
years showed this. In the cohort <strong>of</strong> 1992-1993 (epidemic years) with 3004 children,<br />
there were 22 cases diagnosed due to symptomatic <strong>coeliac</strong> <strong>disease</strong>, and out <strong>of</strong> 690<br />
40<br />
screened children, as many as 9 had previously unrecognised <strong>coeliac</strong> <strong>disease</strong> . In the<br />
cohort <strong>of</strong> 1996-1997 (post-epidemic years), only about half as many <strong>coeliac</strong> <strong>disease</strong><br />
cases were identified, and this was true for symptomatic cases as well as cases detected<br />
by screening, with the studies being comparable in all other respects (Carlsson A,<br />
personal communication). Obviously, the epidemic cannot be explained by genetic<br />
changes in the population, as it occurred over such a short time period.<br />
This epidemic <strong>of</strong> <strong>coeliac</strong> <strong>disease</strong> indicates an abrupt increase and decrease,<br />
respectively, <strong>of</strong> one or a few causal factors influencing a large proportion <strong>of</strong> Swedish<br />
infants over the period in question. As only children below two years <strong>of</strong> age were<br />
affected, changes in infant feeding practices were suspected to have contributed. If<br />
these causal exposures could be solidly identified, this might open doors to the<br />
development <strong>of</strong> a <strong>primary</strong> <strong>prevention</strong> strategy.<br />
Infant feeding<br />
The infant feeding pattern is one <strong>of</strong> the few environmental exposures other than<br />
dependence on gluten proteins in the diet that has been approached as possibly<br />
contributing to <strong>coeliac</strong> <strong>disease</strong> aetiology. Taking into consideration established<br />
guidelines for causation (table), some aspects <strong>of</strong> infant feeding will be discussed as<br />
potential risk determinants for development <strong>of</strong> <strong>coeliac</strong> <strong>disease</strong>.
46 INFANT FEEDING PRACTICES AND COELIAC DISEASE<br />
Temporal relationship<br />
Plausibility<br />
Consistency<br />
Strength<br />
Dose-response relationship<br />
Reversibility<br />
Study design<br />
Coherence <strong>of</strong> evidence<br />
41<br />
Adapted from .<br />
Breast feeding<br />
Table. Guidelines for the evaluation <strong>of</strong> causality.<br />
Does the possible cause precede the effect?<br />
Is the association consistent with other knowledge?<br />
Have similar results been shown in other studies?<br />
What is the strength <strong>of</strong> the association between the<br />
possible cause and the effect?<br />
Is increased exposure to the possible cause associated<br />
with increased effect?<br />
Does the removal <strong>of</strong> a possible cause lead to reduction<br />
<strong>of</strong> <strong>disease</strong> risk?<br />
Is the evidence based on a strong study design?<br />
How many lines <strong>of</strong> evidence support the conclusion?<br />
42-45<br />
Based on increasing knowledge about the immunological impact <strong>of</strong> breast milk ,<br />
it seems plausible that introduction <strong>of</strong> a dietary antigen while the child is still breast-fed<br />
might increase the likelihood <strong>of</strong> developing oral tolerance to that antigen. Whether or<br />
not this relationship holds true for dietary gluten and the risk for development <strong>of</strong> <strong>coeliac</strong><br />
<strong>disease</strong> has not been conclusively established.<br />
Based on observations <strong>of</strong> <strong>coeliac</strong> <strong>disease</strong> patients, it was suggested as early as the<br />
46<br />
1950s that breast-feeding delays onset <strong>of</strong> the <strong>disease</strong> , a view supported by later similar<br />
47-48<br />
studies . Furthermore, an increase in breast-feeding was suggested as a possible<br />
factor contributing to the declining incidence <strong>of</strong> <strong>coeliac</strong> <strong>disease</strong> in the early 1970s in<br />
49-51<br />
England, Scotland and Ireland .<br />
52<br />
In the 1980s, the Italian case-referent studies by Auricchio et al (216 cases/289<br />
53<br />
siblings) and Greco et al (201 cases/1949 referents) demonstrated that <strong>coeliac</strong> <strong>disease</strong><br />
cases were breast-fed for a shorter duration than the referents. This was confirmed in a<br />
54<br />
Swedish case-referent study by Fälth-Magnusson et al (72 cases/288 referents), and<br />
55<br />
recently in a German study by Peters et al (143 cases/137 referents). In contrast, in a<br />
56<br />
family study Ascher et al did not find a difference in breast-feeding duration when<br />
comparing screening-detected cases with their siblings (8 cases/73 siblings). This study<br />
was comparatively small, and the design involved overmatching with respect to dietary<br />
factors, constraints discussed by the authors.<br />
Taken together, the case-referent studies demonstrate that <strong>coeliac</strong> <strong>disease</strong> cases in<br />
general have been breast-fed for a shorter period than other children. However, these<br />
studies could not clarify whether breast-feeding had a direct causal effect, or if the<br />
protective effect was indirect as a consequence <strong>of</strong> the postponed introduction <strong>of</strong> infant<br />
formula (more specifically cow's milk protein), or if it occurred through reduction <strong>of</strong><br />
the amount <strong>of</strong> dietary gluten ingested at an early age.<br />
We have recently reported results from a case-referent study (491 cases/781<br />
57<br />
referents) , which could eliminate some <strong>of</strong> the above-mentioned constraints through a<br />
somewhat different design in comparison with the previously mentioned studies. Our
OR (95%CI)<br />
INFANT FEEDING PRACTICES AND COELIAC DISEASE<br />
47<br />
study was population-based, with a high participation rate, and the results should thus<br />
be representative for Sweden at large. Since our findings are consequences <strong>of</strong><br />
biological phenomena, they should be valid for infants in general. Only incident cases,<br />
i.e. newly diagnosed cases, were included, which reduced the recall period. A<br />
comprehensive questionnaire concerning children's diet and health in general was<br />
mailed to the families; it did not reveal our special interest in <strong>coeliac</strong> <strong>disease</strong>. A semiquantitative<br />
food frequency questionnaire was used to assess both the consumption <strong>of</strong><br />
gluten-containing cereals at the time when these cereals were introduced into the diet<br />
and the total amount consumed by seven months <strong>of</strong> age. The amount <strong>of</strong> glutencontaining<br />
flour in homemade foods was calculated based on standard Swedish recipes<br />
and the amount in industrially produced foods was obtained from the manufacturers.<br />
Multivariate analyses were used to adjust risk estimates for confounding and to suggest<br />
57<br />
causal relationships .<br />
Our main finding was that the risk for <strong>coeliac</strong> <strong>disease</strong> was reduced if the child was<br />
breast-fed during the time period when gluten-containing foods were introduced [Odds<br />
57<br />
Ratio (OR) = 0.59, 95% Confidence Interval (CI) 0.42-0.83] . This protective effect<br />
was even more pronounced if the child was also breast-fed beyond the period <strong>of</strong> gluten<br />
introduction (OR=0.36, 95% CI 0.26-0.51) (Fig. 2). These risk estimates were adjusted<br />
for the age <strong>of</strong> the infant when gluten was introduced into the diet and the amount <strong>of</strong><br />
gluten that was given.<br />
4<br />
2<br />
1<br />
½<br />
¼<br />
Discontinued Continued Continued beyond<br />
Breast feeding status at introduction <strong>of</strong> gluten<br />
Fig. 2. Breast-feeding status (BF) at introduction <strong>of</strong> gluten-containing flour into the diet<br />
and risk (OR, 95% CI) for <strong>coeliac</strong> <strong>disease</strong> before two years <strong>of</strong> age.<br />
A protective effect <strong>of</strong> breast-feeding was supported by our ecological study <strong>of</strong> the<br />
Swedish epidemic, i.e. using aggregated data to explore any temporal relationship<br />
between the changes in incidence rate and changes in infant dietary patterns. Both the<br />
rise and later fall in incidence had a temporal relationship to a change in the proportion<br />
36<br />
<strong>of</strong> infants introduced to gluten while still being breast-fed .<br />
It is important to note that at the time <strong>of</strong> these studies the majority <strong>of</strong> Swedish
48 INFANT FEEDING PRACTICES AND COELIAC DISEASE<br />
infants were breast-fed for six months or longer. As a result, most <strong>of</strong> the infants were<br />
introduced to cow's milk products and other food products while still being breast-fed.<br />
Also, for most infants the termination <strong>of</strong> breast-feeding did not coincide with<br />
introduction <strong>of</strong> infant formula, but rather with increased ingestion <strong>of</strong> other foods.<br />
Moreover, in the case-referent study we could show that a reduced risk for <strong>coeliac</strong><br />
<strong>disease</strong> still remained when the age <strong>of</strong> the infants at introduction <strong>of</strong> gluten into the diet<br />
was considered, along with the amount <strong>of</strong> gluten given at that time (fig. 2). Thus, our<br />
findings strongly supported breast-feeding as directly reducing the risk for <strong>coeliac</strong><br />
<strong>disease</strong>, and not merely influencing the risk indirectly through changes in other<br />
exposures.<br />
It has recently been suggested that the intestinal lesion in <strong>coeliac</strong> <strong>disease</strong> might be<br />
caused by an uncontrolled production <strong>of</strong> pro-inflammatory IFN-gby intraepithelial T<br />
cells that is not sufficiently counteracted by an increased production <strong>of</strong> downregulating<br />
TGF-b1 (Forsberg G, personal communication). It is thus tempting to<br />
35<br />
speculate that the TGF-b1 in breast-milk compensates for this although this is only<br />
42-45<br />
one <strong>of</strong> several possible mechanisms for a protective effect <strong>of</strong> human milk .<br />
Thus, a protective effect <strong>of</strong> being breast-fed when dietary gluten is introduced is<br />
supported by several epidemiological studies <strong>of</strong> different design. Moreover, the<br />
protective effect is biologically plausible when taking into account our present<br />
knowledge <strong>of</strong> breast-milk composition and the impact on immune responses, and the<br />
aetiology <strong>of</strong> <strong>coeliac</strong> <strong>disease</strong>.<br />
Amount <strong>of</strong> dietary gluten<br />
The dose <strong>of</strong> dietary antigen ingested may influence whether or not oral tolerance<br />
32-34<br />
develops . It is not yet clear if this applies to the amount <strong>of</strong> gluten given in relation to<br />
the risk <strong>of</strong> developing <strong>coeliac</strong> <strong>disease</strong>.<br />
Interestingly, a larger consumption <strong>of</strong> wheat gluten was reported for healthy infants<br />
in Sweden and Italy as compared to Finland, Denmark and Estonia, and the former<br />
58-61<br />
countries also reported a higher occurrence <strong>of</strong> <strong>coeliac</strong> <strong>disease</strong> . The study designs,<br />
involving aggregated data, did not, however, allow adjustments for differences in other<br />
exposures.<br />
54<br />
The Swedish case-referent study by Fälth-Magnusson et al indicated that the<br />
<strong>coeliac</strong> <strong>disease</strong> cases, more <strong>of</strong>ten than the referents, were introduced to gluten by means<br />
<strong>of</strong> gluten-containing follow-on formula. In infancy it is clear that bottle-feeding,<br />
compared to feeding by cup and spoon, more readily contributes a larger amount <strong>of</strong><br />
food, and thus also a larger amount <strong>of</strong> gluten. In the Fälth-Magnusson study, however, it<br />
was not possible to estimate the amount <strong>of</strong> gluten given to the infants.<br />
In our case-referent study it was possible, for the first time, to assess the<br />
consumption <strong>of</strong> gluten-containing cereals on an individual basis by use <strong>of</strong> a semi-<br />
57<br />
quantitative food frequency questionnaire . We could show that introduction <strong>of</strong> glutencontaining<br />
foods in larger amounts, as compared to small or medium amounts, was an<br />
independent risk factor for <strong>coeliac</strong> <strong>disease</strong> development (adjusted OR=1.5, 95% CI 1.1-<br />
2.1). Also, at seven months <strong>of</strong> age the cases consumed larger amounts <strong>of</strong> glutencontaining<br />
flour than the referents. It is important to note that through the use <strong>of</strong><br />
multivariate analyses we adjusted for differences in breast-feeding practices and the
INFANT FEEDING PRACTICES AND COELIAC DISEASE<br />
49<br />
age <strong>of</strong> the infant when gluten was introduced into the diet. Thus, our findings clearly<br />
indicate that introduction <strong>of</strong> gluten in larger amounts increases the risk for <strong>coeliac</strong><br />
<strong>disease</strong>. Furthermore, we found that the type <strong>of</strong> food used as the source <strong>of</strong> gluten, i.e.<br />
57<br />
solid foods or follow-on formula, was not important as an independent risk factor . The<br />
relevance <strong>of</strong> our observations is therefore not only applicable to Sweden with its custom<br />
<strong>of</strong> using gluten-containing follow-on formula from the age <strong>of</strong> six months.<br />
The daily amount <strong>of</strong> gluten consumed during infancy as a risk factor for <strong>coeliac</strong><br />
<strong>disease</strong> is further supported by our ecological study <strong>of</strong> the Swedish epidemic, where we<br />
used aggregated data to explore any temporal relationship between changes in<br />
36<br />
incidence rate and changes in infant dietary patterns . The rise in incidence was<br />
preceded by a tw<strong>of</strong>old increase in the average daily consumption <strong>of</strong> gluten through the<br />
use <strong>of</strong> follow-on formula, and later, the fall in incidence coincided with a consumption<br />
36<br />
that was decreased by one-third .<br />
62<br />
Marsh et al concluded that gluten-sensitised individuals respond in a time-related<br />
and dose-dependent fashion to gliadin, which is an observation supported by several<br />
63-66<br />
other studies . These experimental studies do not, however, clarify whether the<br />
amount <strong>of</strong> gluten is also crucial when infants are introduced to this antigen for the first<br />
time.<br />
Taken together, there is evidence to suggest that consumption <strong>of</strong> a large amount <strong>of</strong><br />
gluten-containing flour (increased antigen dose) during infancy increases the risk for<br />
<strong>coeliac</strong> <strong>disease</strong>. It is, however, not clear whether there is a direct dose-response effect or<br />
a threshold effect. Furthermore, it seems likely that the amount <strong>of</strong> gluten tolerated<br />
varies with the genetic predisposition <strong>of</strong> the individual, other environmental exposures,<br />
and the age <strong>of</strong> the individual.<br />
Age at introduction <strong>of</strong> gluten<br />
There might be an age interval during which humans have decreased ability to<br />
develop oral tolerance to a newly introduced dietary antigen. Hypothetically, the age <strong>of</strong><br />
the infant upon introduction <strong>of</strong> gluten into the diet might thus influence the risk for<br />
<strong>coeliac</strong> <strong>disease</strong>.<br />
In a comparison <strong>of</strong> English <strong>coeliac</strong> <strong>disease</strong> patients in the 1950s and 1960s, it was<br />
suggested that earlier introduction <strong>of</strong> dietary gluten resulted in earlier presentation <strong>of</strong><br />
67<br />
the <strong>disease</strong> . Some clinical studies in which differences in breast-feeding duration<br />
47-48<br />
have been taken into account did not show such a relationship . In fact, a delayed<br />
introduction <strong>of</strong> gluten into the diet <strong>of</strong> infants was suggested as contributing to the<br />
49-51<br />
decline in incidence <strong>of</strong> <strong>coeliac</strong> <strong>disease</strong> in England, Scotland and Ireland in the 1970s .<br />
However, at that time comparable dietary changes occurred in Sweden without any<br />
68-69<br />
observed change in incidence . Furthermore, the increased incidence in Swedish<br />
children in the middle <strong>of</strong> the 1980s was preceded by a delayed introduction <strong>of</strong> dietary<br />
36,38-39<br />
gluten from four until six months <strong>of</strong> age . Thus, these ecological observations<br />
resulted in contradictory findings. However, a study design based on aggregated data<br />
cannot by itself provide conclusive evidence.<br />
However, the case-referent design based on individual data allows for adjustments<br />
for differences in other exposures. Such studies in which adjustments have been made<br />
for differences in breast-feeding duration have indicated that the age <strong>of</strong> the infant at
50 INFANT FEEDING PRACTICES AND COELIAC DISEASE<br />
52-54<br />
introduction <strong>of</strong> dietary gluten is <strong>of</strong> no importance with respect to <strong>coeliac</strong> <strong>disease</strong> risk .<br />
In our case-referent study we could move one step further by also adjusting for the<br />
differences in amount <strong>of</strong> gluten-containing foods given at various ages <strong>of</strong> introduction.<br />
Our results also suggested that the age <strong>of</strong> the infant at introduction <strong>of</strong> dietary gluten was<br />
57<br />
<strong>of</strong> no importance for <strong>coeliac</strong> <strong>disease</strong> risk , although with the limitation that only the<br />
first year <strong>of</strong> life was evaluated.<br />
Thus, present evidence does not support age <strong>of</strong> the infant at the time <strong>of</strong> gluten<br />
introduction as an independent risk factor for <strong>coeliac</strong> <strong>disease</strong> development. However,<br />
even when considered together these studies do not encompass all possible ages for<br />
introduction <strong>of</strong> gluten, e.g. after one year <strong>of</strong> age or even later. Thus, this possibility also<br />
needs to be evaluated.<br />
Other possible contributing factors<br />
Infections<br />
70 71<br />
It has been proposed that adenovirus type 12 , and also other adenoviruses , could<br />
initiate <strong>coeliac</strong> <strong>disease</strong> as a consequence <strong>of</strong> sequence similarities between a protein<br />
produced in conjunction with the viral infection and A-gliadin. This has been<br />
72-73<br />
questioned , but not convincingly excluded. Gastrointestinal infections cause a<br />
74<br />
disruption <strong>of</strong> the barrier function <strong>of</strong> the small intestinal mucosa , which theoretically<br />
could result in an increased antigen penetration and unfavourable immune responses.<br />
We found a higher risk for <strong>coeliac</strong> <strong>disease</strong> in children born during summer as<br />
75<br />
compared to winter, but only in children below two years <strong>of</strong> age . These findings<br />
indicate that environmental exposure(s) with a seasonal pattern may have a causal<br />
effect. A temporal relationship suggests that this might be due to a causal effect <strong>of</strong><br />
infections during foetal life and/or an interaction between infections and introduction<br />
<strong>of</strong> gluten into the diet. However, any exposure with a seasonal pattern might be the<br />
explanation, and non-infectious exposures should also be explored.<br />
In our case-referent study we found that children who experienced three or more<br />
infectious episodes before six months <strong>of</strong> age had an increased risk for <strong>coeliac</strong> <strong>disease</strong><br />
76<br />
before two years <strong>of</strong> age (adjusted OR=1.4, 95% CI 1.0-1.9) . This was true even when<br />
episodes <strong>of</strong> gastroenteritis were excluded, and after adjustments were made for<br />
differences in infant feeding patterns and family socio-economic group. Infectious<br />
episodes later in infancy were not included, as these could be secondary to the <strong>disease</strong><br />
itself. The risk for <strong>coeliac</strong> <strong>disease</strong> increased considerably if in addition to having many<br />
infections the child was also introduced to gluten in large amounts, as compared to<br />
76<br />
small and medium amounts .<br />
Socio-economic background<br />
In our case-referent study children in families belonging to the lower as compared to<br />
middle and upper socio-economic strata <strong>of</strong> Swedish society had an increased risk for<br />
76<br />
<strong>coeliac</strong> <strong>disease</strong> (adjusted OR=1.4, 95% CI 1.0-1.8) , but again only in the age group<br />
below two years. Our reported estimate was adjusted for differences in infant feeding<br />
practices and infectious episodes. This indicates that there are also other as yet<br />
unidentified environmental exposures contributing to the causal pattern <strong>of</strong> <strong>coeliac</strong><br />
<strong>disease</strong>.
INFANT FEEDING PRACTICES AND COELIAC DISEASE<br />
51<br />
A multifactorial aetiology<br />
A simplified model <strong>of</strong> the multifactorial aetiology <strong>of</strong> <strong>coeliac</strong> <strong>disease</strong> is outlined<br />
below (Fig. 3). It is based on the results <strong>of</strong> our own studies put into the context <strong>of</strong> present<br />
knowledge <strong>of</strong> <strong>coeliac</strong> <strong>disease</strong> aetiology. The emphasis in the model is on the influence<br />
<strong>of</strong> environmental exposures on <strong>coeliac</strong> <strong>disease</strong> risk.<br />
Throughout life, including foetal life, an individual's genetic makeup interacts with<br />
the continuous and varying exposures <strong>of</strong> the environment. Theoretically, both genes<br />
and the environment, as well as the interaction between them, confer either increased or<br />
reduced <strong>disease</strong> risk. The exposures <strong>of</strong> causal importance most likely vary throughout<br />
life, and the range <strong>of</strong> potential risk determinants is wide. More specifically, with regard<br />
to <strong>coeliac</strong> <strong>disease</strong> the immunological response to dietary gluten is shaped.<br />
Genetic susceptibility and presence <strong>of</strong> dietary gluten are considered necessary<br />
casual factors, i.e. without these factors <strong>coeliac</strong> <strong>disease</strong> will not develop. However,<br />
component causal factors also contribute to whether or not <strong>coeliac</strong> <strong>disease</strong> develops.<br />
Combined, the necessary causes and one or several component causes produce a<br />
77<br />
sufficient cause, i.e. development <strong>of</strong> the <strong>disease</strong> is unavoidable .<br />
As component causal factors in <strong>coeliac</strong> <strong>disease</strong> aetiology we suggest: i) duration <strong>of</strong><br />
breast-feeding, ii) whether breast-feeding is ongoing or not when gluten is introduced<br />
into the diet, iii) amount <strong>of</strong> gluten given to infants when introduced into the diet, and iv)<br />
repeated infectious episodes early in life.<br />
Associated factors are not considered to have a causal effect by themselves, but act<br />
through other directly causal factors. When identified, however, they may be used as<br />
markers for an increased <strong>disease</strong> risk, and thereby focus the search for causal factors.<br />
Such a factor is seasonality in births, with an increased risk for <strong>coeliac</strong> <strong>disease</strong> in<br />
Season<br />
Dietary recommendations<br />
Food contents<br />
Socioeconomic conditions<br />
Structural<br />
factors<br />
Associated<br />
factors<br />
Infections<br />
Breast feeding<br />
?<br />
?<br />
?<br />
Component<br />
causal<br />
factors<br />
Amount<br />
DIETARY GLUTEN<br />
NECESSARY<br />
CAUSAL<br />
FACTORS<br />
GENETICS<br />
sex<br />
Immunopathogenesis<br />
Fetal life Infancy Childhood Adulthood<br />
Fig. 3. Causal model on the multifactorial aetiology <strong>of</strong> <strong>coeliac</strong> <strong>disease</strong>.<br />
37<br />
From , with permission.
Age (years)<br />
52 INFANT FEEDING PRACTICES AND COELIAC DISEASE<br />
children born during summer as compared to winter. It might be that seasonality reflects<br />
a varying exposure to infectious episodes throughout the year, but other possible<br />
explanations should be explored. Another associated factor is the increased risk for<br />
<strong>coeliac</strong> <strong>disease</strong> in Swedish children from the lower as compared to middle and upper<br />
socio-economic strata, suggesting that there are further component causes yet to be<br />
identified.<br />
Structural factors are any change on a societal level influencing the risk for <strong>coeliac</strong><br />
<strong>disease</strong>. However, these must <strong>of</strong> course exhibit their effect through component causes<br />
close to the individual, as illustrated in the depicted model (Fig. 3). These could include<br />
dietary recommendations influencing how gluten is introduced into the infant diet, and<br />
changes in the gluten content in industrially produced infant foods.<br />
What can be learnt from the Swedish epidemic?<br />
What caused the epidemic?<br />
Changes in infant feeding practices have been suspected to contribute to the<br />
Swedish epidemic <strong>of</strong> <strong>coeliac</strong> <strong>disease</strong> in children. To clarify whether or not this was the<br />
case, we used an ecological approach comparing estimated yearly changes in infant<br />
feeding practices with the yearly incidence rate <strong>of</strong> <strong>coeliac</strong> <strong>disease</strong> in children below two<br />
36<br />
years <strong>of</strong> age .<br />
We collected national data for the years 1980 to 1997 on duration <strong>of</strong> breast-feeding<br />
36<br />
and intake <strong>of</strong> gluten-containing cereals in Swedish infants . The latter was estimated<br />
by changes in gluten intake by means <strong>of</strong> industrially produced follow-on formulas as an<br />
estimate <strong>of</strong> changes in total gluten intake. These follow-on formulas, combined with<br />
59<br />
porridge, provide about half <strong>of</strong> the total intake <strong>of</strong> gluten proteins , and <strong>of</strong> that half,<br />
follow-on formulas account for about 90%, according to the manufacturers.<br />
It should be noted that the incidence rate for a particular year in children below two<br />
years <strong>of</strong> age might also be influenced by the exposure pattern <strong>of</strong> the two preceding<br />
years. The reason for this, as illustrated by the Lexis diagram, is that the incidence rate<br />
in children below two years <strong>of</strong> age in 1997, for instance, is based on cases diagnosed<br />
that year, and these children were born during the period 1995 to 1997, which is thus the<br />
period during which they might have been exposed (Fig. 4).<br />
2<br />
Incidence rate in children 0-2 years <strong>of</strong> age in 1997<br />
1<br />
1995 1996 1997 1998 1999<br />
Exposure period<br />
Fig. 4. A Lexis diagram illustrating the population and exposure periods on which the<br />
incidence rate by age is based.
INFANT FEEDING PRACTICES AND COELIAC DISEASE<br />
53<br />
36<br />
Our results showed rapidly increasing incidence rates between 1985 and 1987 .<br />
The period <strong>of</strong> interest with regard to exposure was characterised by i) about half <strong>of</strong> the<br />
infants being breast-fed at six months <strong>of</strong> age, ii) doubling <strong>of</strong> the average daily<br />
consumption <strong>of</strong> flour through use <strong>of</strong> follow-on formula from 1981 to 1983 with regard<br />
to the total amount <strong>of</strong> wheat, rye and barley, while the amount <strong>of</strong> oats decreased, and iii)<br />
a national recommendation at the end <strong>of</strong> 1982 to postpone introduction <strong>of</strong> gluten from<br />
four to six months <strong>of</strong> age (Fig. 5).This latter change was in accordance with European<br />
300<br />
250<br />
Incidence rate<br />
Breastfeeding index<br />
Wheat/Rye/Barley index<br />
200<br />
150<br />
100<br />
50<br />
0<br />
Changed national recommendations<br />
1980 1985 1990 1995<br />
Fig. 5. Annual incidence rate <strong>of</strong> <strong>coeliac</strong> <strong>disease</strong> per 100 000 person years for children 0-1.9<br />
years <strong>of</strong> age from 1980 to 1997, in relation to breast-feeding habits, flour consumption and<br />
c h a n g e d n a t i o n a l re c o m m e n d a t i o n s . T h e a r ro w s i n d i c a t e c h a n g e d<br />
recommendation on introduction <strong>of</strong> gluten to infants. Breast-feeding index based on the<br />
proportion <strong>of</strong> all children breast-fed at six months <strong>of</strong> age (1980; index 100 = 37%).<br />
Wheat/Rye/Barley index based on the estimated average daily consumption <strong>of</strong> these cereals<br />
-1 -1<br />
provided by follow-on formulas (1980; index 100 = 16 gram x child x day ).<br />
36<br />
From with permission.<br />
78<br />
recommendations .<br />
A rapid decline in the incidence rate began in 1995, and was still ongoing through<br />
36<br />
1997 . The period <strong>of</strong> interest with regard to exposure was characterised by i) a<br />
continuous increase (from 54% to 76%) in the proportion <strong>of</strong> infants still breast-fed at six<br />
months <strong>of</strong> age, ii) the average daily consumption <strong>of</strong> flour through the use <strong>of</strong> follow-on<br />
formula decreased by one third starting in 1995 with regard to the total amount <strong>of</strong><br />
wheat, rye and barley, while the amount <strong>of</strong> oats increased, and iii) the national<br />
recommendation was changed in the autumn <strong>of</strong> 1996 to introduction <strong>of</strong> gluten into the<br />
diet in smaller amounts from four months <strong>of</strong> age, and preferably while the child is still<br />
breast-fed (Fig. 5). However, starting at the end <strong>of</strong> the 1980s, and particularly during a<br />
one-year period starting in the autumn <strong>of</strong> 1995, the media focused much attention on the<br />
increased incidence <strong>of</strong> <strong>coeliac</strong> <strong>disease</strong> in relation to the current dietary pattern. This<br />
most likely promoted a change in dietary patterns that was more extensive than revealed
54 INFANT FEEDING PRACTICES AND COELIAC DISEASE<br />
by our study, and that took place before the new national recommendation was<br />
launched.<br />
A certain delay between changes in exposure and <strong>disease</strong> occurrence would be<br />
expected. Indeed, in the 1980s the change in gluten intake with regard to both amounts<br />
consumed during infancy and age at introduction preceded the increase in incidence. In<br />
contrast, the decrease in amounts <strong>of</strong> gluten consumed was first noted in 1995, i.e. the<br />
same year as the decline in incidence started. Further, in 1997 the estimated amount <strong>of</strong><br />
gluten consumed had decreased by one third, while the incidence rate had already<br />
returned to the level <strong>of</strong> the early 1980s. It should also be noted that the proportion <strong>of</strong><br />
infants breast-fed at six months <strong>of</strong> age continuously increased during the 1990s without<br />
any sharp increase before, or coinciding with, the decrease in incidence. Hence, the<br />
changes in exposure caused by each <strong>of</strong> these factors alone cannot explain the entire<br />
epidemic.<br />
Considering the combined effects <strong>of</strong> changes in infant feeding practices over time, it<br />
is clear that both the rise and fall in incidence were accompanied by a change in the<br />
proportion <strong>of</strong> infants introduced to gluten in small amounts while still being breast-fed.<br />
Thus, Swedish infant feeding practices have shifted over time from a favourable to an<br />
unfavourable and then back again to a favourable pattern with respect to <strong>coeliac</strong> <strong>disease</strong><br />
risk.<br />
Public health impact<br />
The public health impact <strong>of</strong> a change in causal exposures can be estimated by the<br />
population attributable fraction (AF), which takes into account the prevalence <strong>of</strong><br />
different exposures among the cases (Pc), and the adjusted odds ratios (OR) <strong>of</strong> these<br />
exposures [AF = Pc (OR-1)/OR]. We used our case-referent study, performed during<br />
the peak <strong>of</strong> the epidemic, for such estimates. Our analysis revealed that about half <strong>of</strong> the<br />
<strong>coeliac</strong> <strong>disease</strong> cases during the epidemic might have been avoided if all infants had<br />
been introduced to gluten in small amounts while still being breast-fed (Fig. 6).<br />
120<br />
100<br />
= Preventable cases<br />
No <strong>of</strong> cases<br />
80<br />
60<br />
40<br />
20<br />
0<br />
A B C D<br />
Continued<br />
Small-medium<br />
Continued<br />
Large<br />
Discontinued<br />
Small-medium<br />
Discontinued<br />
Large<br />
Breast-feeding status at introduction <strong>of</strong> flourand amount <strong>of</strong> flour given<br />
Fig. 6. Preventable <strong>coeliac</strong> <strong>disease</strong> cases below two years <strong>of</strong> age with respect to breastfeeding<br />
status at introduction <strong>of</strong> gluten-containing flour into the diet and the amount <strong>of</strong><br />
flour given. Risk estimates were based on conditional logistic regression with 392 matched<br />
sets <strong>of</strong> cases and referents, and adjusted for age <strong>of</strong> the infant when flour was introduced.<br />
37<br />
Odds ratio (95% CI); A) 1.0, B) 2.0 (1.4, 3.0), C) 2.8 (1.9, 4.0), D) 3.3 (2.3, 4.8). From<br />
with permission.
INFANT FEEDING PRACTICES AND COELIAC DISEASE<br />
55<br />
Thus, other casual exposures changing over time must also have contributed to the<br />
epidemic.<br />
However, it is likely that the proportion <strong>of</strong> <strong>coeliac</strong> <strong>disease</strong> cases that might be<br />
avoided by appropriate measures varies among different populations, being higher in<br />
populations with unusually unfavourable environmental exposures, as was apparently<br />
the situation for Swedish infants during the high incidence years <strong>of</strong> the epidemic.<br />
What will follow after the epidemic?<br />
In a Swedish study based on symptomatic adult <strong>coeliac</strong> <strong>disease</strong> patients, the highest<br />
79<br />
age-specific prevalence was reported for people born between 1927 and 1936 , and<br />
interestingly, the majority <strong>of</strong> cases in our population-based adult screening study were<br />
5<br />
also born during that time period . Thus, these studies indicate a cohort effect, i.e. the<br />
life span <strong>of</strong> certain cohorts coincides with environmental exposures that have resulted<br />
in an excess risk for <strong>coeliac</strong> <strong>disease</strong> throughout life.<br />
Accordingly, it might also be that as a consequence <strong>of</strong> an unfavourable exposure<br />
during their first years <strong>of</strong> life, the birth cohorts <strong>of</strong> the epidemic years will carry an<br />
excess risk for <strong>coeliac</strong> <strong>disease</strong> throughout their lives. If so, the cohorts <strong>of</strong> the postepidemic<br />
period might have a decreased lifetime risk for <strong>coeliac</strong> <strong>disease</strong>. Thus far, at<br />
comparable ages the cohorts <strong>of</strong> this later period actually have a lower cumulative<br />
6<br />
1992<br />
6<br />
Cases per 1000 births<br />
5<br />
4<br />
3<br />
2<br />
1<br />
1989-90<br />
1991<br />
1987-88<br />
1985-86<br />
1983-84<br />
1978-82<br />
1973-77<br />
5<br />
4<br />
3<br />
2<br />
1<br />
1993<br />
1994<br />
1995<br />
1996<br />
1997<br />
0<br />
0 2 4 6 8 10 12 14<br />
Age (years)<br />
0<br />
1998<br />
0 2 4 6<br />
Fig. 7. Cumulative incidence <strong>of</strong> <strong>coeliac</strong> <strong>disease</strong> by age for the birth cohorts from 1973 to<br />
1998. To reduce the graph complexity, the cohorts <strong>of</strong> 1973 to 1982 are aggregated in groups<br />
<strong>of</strong> five, the cohorts <strong>of</strong> 1983 to 1990 in groups <strong>of</strong> two, while the cohorts from 1991 to 1998<br />
are reported separately.
56 INFANT FEEDING PRACTICES AND COELIAC DISEASE<br />
incidence than the cohorts <strong>of</strong> the epidemic period (Fig. 7).<br />
A longer follow-up will reveal to what extent this lower risk continues, and to what<br />
extent new cases develop later in life.<br />
Large screening studies <strong>of</strong> cohorts from both the epidemic and post-epidemic<br />
periods, with repeated screening for a considerable number <strong>of</strong> years, would increase our<br />
understanding <strong>of</strong> the natural history <strong>of</strong> <strong>coeliac</strong> <strong>disease</strong> development in relation to<br />
exposures early in life. These exposures would be complicated, <strong>of</strong> course, by the<br />
addition <strong>of</strong> exposures later in life.<br />
An option for <strong>primary</strong> <strong>prevention</strong><br />
Primary <strong>prevention</strong> <strong>of</strong> <strong>coeliac</strong> <strong>disease</strong> is a clearly desirable option, as it would<br />
contribute substantially to the health <strong>of</strong> the general population. By definition, it aims at<br />
intervening before the <strong>disease</strong> has developed.<br />
Genetic modification <strong>of</strong> the gluten-containing cereals so that they lose their ability<br />
to trigger celiac <strong>disease</strong> might someday become an alternative, although this is<br />
something for the distant future. Another option, at least theoretically, would be<br />
induction <strong>of</strong> immune tolerance to gluten peptides by giving a vaccine. Even today,<br />
<strong>coeliac</strong> <strong>disease</strong> could be effectively prevented if the use <strong>of</strong> gluten-containing cereals<br />
was abandoned, but in most countries such a suggestion would be considered<br />
unacceptable.<br />
However, if <strong>coeliac</strong> <strong>disease</strong> has a multifactorial aetiology, which is likely, then<br />
<strong>primary</strong> <strong>prevention</strong> would be possible, at least in some individuals, without completely<br />
abandoning the use <strong>of</strong> dietary gluten. This might be attained through a change in<br />
component causal exposures, thereby increasing the chance for infants to develop oral<br />
tolerance to gluten, and possibly also promoting the maintenance <strong>of</strong> tolerance<br />
throughout life (Fig. 3).<br />
When knowledge is consolidated from the clinical, epidemiological and basic<br />
sciences, it seems likely that infant feeding practices, in addition to the mere presence <strong>of</strong><br />
gluten in the diet, have an important role in <strong>coeliac</strong> <strong>disease</strong> development. Thus, a<br />
significant contribution to <strong>primary</strong> <strong>prevention</strong> seems possible through a gradual<br />
introduction <strong>of</strong> gluten-containing foods into the infant diet before breast-feeding is<br />
discontinued. The duration <strong>of</strong> breast-feeding in itself seems to reduce the risk even<br />
further, and a long duration should thus be promoted. The risk for <strong>coeliac</strong> <strong>disease</strong> is then<br />
clearly reduced, at least up to two years <strong>of</strong> age. This infant feeding pattern most likely<br />
also contributes to a decreased lifetime risk <strong>of</strong> <strong>coeliac</strong> <strong>disease</strong>, although this remains to<br />
be established.<br />
Only a few <strong>of</strong> all the potential causal environmental exposures have thus far been<br />
explored, and the search for such factors, which exhibit their effect during different<br />
periods in the life span, should be intensified. This approach most likely will lead to the<br />
identification <strong>of</strong> other entry-points for <strong>primary</strong> <strong>prevention</strong>.<br />
Acknowledgements<br />
We thank Don Kasarda, US Department <strong>of</strong> Agriculture, Albany, California, for<br />
valuable comments on the manuscript.
INFANT FEEDING PRACTICES AND COELIAC DISEASE<br />
57<br />
References<br />
1. Grodzinsky E, Franzen L, Hed J, Ström M. High prevalence <strong>of</strong> celiac <strong>disease</strong> in healthy adults<br />
revealed by antigliadin antibodies. Ann Allergy 1992; 69: 66-70.<br />
2. Catassi C, Rätsch I-M, Fabiani E, Rossini M, Bordicchia F, Candela F, et al. Coeliac <strong>disease</strong><br />
in the year 2000: exploring the iceberg. Lancet 1994; 343: 200-3.<br />
3. Not T, Horvath K, Hill ID, Partanen J, Hammed A, Magazzu G, et al. Celiac <strong>disease</strong> risk in the<br />
USA: High prevalence <strong>of</strong> antiendomysium antibodies in healthy blood donors. Scand J<br />
Gastroenterol 1998; 33: 494-8.<br />
4. Johnston SD, Watson RGP, McMillan SA, Sloan J, Love AHG. Coeliac <strong>disease</strong> detected by<br />
screening is not silent--simply unrecognized. QJM 1998; 91: 853-60.<br />
5. Ivarsson A, Persson LÅ, Juto P, Peltonen M, Suhr O, Hernell O. High prevalence <strong>of</strong><br />
undiagnosed <strong>coeliac</strong> <strong>disease</strong> in adults: a Swedish population-based study. J Intern Med<br />
1999; 245: 63-8.<br />
6. Catassi C, Rätsch IM, Gandolfi L, Pratesi R, Fabiani E, El Asmar R, et al. Why is <strong>coeliac</strong><br />
<strong>disease</strong> endemic in the people <strong>of</strong> the Sahara? [letter]. Lancet 1999; 354: 647-8.<br />
7. Csizmadia CGDS, Mearin ML, von Blomberg BME, Brand R, Verloove-Vanhorick SP. An<br />
iceberg <strong>of</strong> childhood <strong>coeliac</strong> <strong>disease</strong> in the Netherlands [letter]. Lancet 1999; 353: 813-4.<br />
8. Gandolfi L, Pratesi R, Cordoba JC, Tauil PL, Gasparin M, Catassi C. Prevalence <strong>of</strong> celiac<br />
<strong>disease</strong> among blood donors in Brazil. Am J Gastroenterol 2000; 95: 689-92.<br />
9. Rabassa EB, Sagaró E, Fragoso T, Castañeda C, Gra B. Coeliac <strong>disease</strong> in Cuban children.<br />
Arch Dis Child 1981; 56: 128-31.<br />
10. Sher KS, Fraser RC, Wicks AC, Mayberry JF. High risk <strong>of</strong> <strong>coeliac</strong> <strong>disease</strong> in Punjabis.<br />
Epidemiological study in the south Asian and European populations <strong>of</strong> Leicestershire.<br />
Digestion 1993; 54: 178-82.<br />
11. Rawashdeh MO, Khalil B, Raweily E. Celiac <strong>disease</strong> in Arabs. J Pediatr Gastroenterol Nutr<br />
1996; 23: 415-8.<br />
12. Demir H, Yuce A, Kocak N, Ozen H, Gurakan F. Celiac <strong>disease</strong> in Turkish children:<br />
presentation <strong>of</strong> 104 cases. Pediatr Int 2000; 42: 483-7.<br />
13. Marsh MN. Screening for latent gluten sensitivity: questions many, but answers few<br />
[editorial; comment]. Eur J Gastroenterolog Hepatol 1996; 8: 3-6.<br />
14. Catassi C, Fabiani E, Ratsch IM, Coppa GV, Giorgi PL. Celiac <strong>disease</strong> in the general<br />
population: should we treat asymptomatic cases? J Pediatr Gastroenterol Nutr 1997; 24:<br />
S10-2.<br />
15. Lohiniemi S. Tricky to find, hard to treat, impossible to cure. Lancet 2001; 358: 14.<br />
16. Ellis A. Coeliac <strong>disease</strong>: Previous family studies. In: McConnell RB, ed. The genetics <strong>of</strong><br />
<strong>coeliac</strong> <strong>disease</strong>: International symposium on the genetics <strong>of</strong> <strong>coeliac</strong> <strong>disease</strong>, 1979,<br />
Liverpool, England. MTP, Lancaster: 1981; 197-9.<br />
17. Polanco I, Biemond I, van Leeuwen A, et al. Gluten sensitive enteropathy in Spain: Genetic<br />
and environmental factors. In: McConnell RB, ed. The genetics <strong>of</strong> <strong>coeliac</strong> <strong>disease</strong>:<br />
International symposium on the genetics <strong>of</strong> <strong>coeliac</strong> <strong>disease</strong>, 1979, Liverpool, England. MTP,<br />
Lancaster: 1981; 211-31.<br />
18. Bardella MT, Fredella C, Prampolini L, Marino R, Conte D, Giunta AM. Gluten sensitivity in<br />
monozygous twins: a long-term follow-up <strong>of</strong> five pairs. Am J Gastroenterol 2000; 95: 1503-5.<br />
19. Hervonen K, Karell K, Holopainen P, Collin P, Partanen J, Reunala T. Concordance <strong>of</strong><br />
Dermatitis Herpetiformis and Celiac Disease in Monozygous Twins. J Invest Dermatol 2000;<br />
115: 990-3.<br />
20. Ferguson A. Coeliac <strong>disease</strong> research and clinical practice: maintaining momentum into the<br />
twenty-first century. Baillieres Clin Gastroenterol 1995; 9: 395-412.<br />
21. Walker-Smith J, Murch S. Coeliac <strong>disease</strong>. Diseases <strong>of</strong> the small intestine in childhood. 4 ed.<br />
Isis Medical Media; Oxford: 1999; 235-77.
58 INFANT FEEDING PRACTICES AND COELIAC DISEASE<br />
22. Sollid LM. Molecular basis <strong>of</strong> celiac <strong>disease</strong>. Annu Rev Immunol 2000; 18: 53-81.<br />
23. Sollid LM, Lundin KEA. An inappropriate immune response. Lancet 2001; 358: s13.<br />
24. Petruzzelli F, Bonamico M, Ferrante P, Grillo R, Mora B, Mariani P, et al. Genetic<br />
contribution <strong>of</strong> the HLA region to the familial clustering <strong>of</strong> <strong>coeliac</strong> <strong>disease</strong>. Ann Hum Genet<br />
1997; 61: 307-17.<br />
25. Bevan S, Popat S, Braegger CP, Busch A, O'Donoghue D, Fälth-Magnusson K, et al.<br />
Contribution <strong>of</strong> the MHC region to the familial risk <strong>of</strong> <strong>coeliac</strong> <strong>disease</strong>. J Med Genet 1999; 36:<br />
687-90.<br />
26. Clot F, Babron MC. Genetics <strong>of</strong> celiac <strong>disease</strong>. Molecular Genetics and Metabolism 2000;<br />
71: 76-80.<br />
27. King AL, Ciclitira PJ. Celiac <strong>disease</strong>: strongly heritable, oligogenic, but genetically complex.<br />
Molecular Genetics and Metabolism 2000; 71: 70-5.<br />
28. Risch N. Assessing the role <strong>of</strong> HLA-linked and unlinked determinants <strong>of</strong> <strong>disease</strong>. Am J Hum<br />
Genet 1987; 40: 1-14.<br />
29. Salvetti M, Ristori G, Bomprezzi R, Pozzilli P, Leslie RDG. Twins: mirrors <strong>of</strong> the immune<br />
system. Immunol Today 2000; 21: 342-7.<br />
30. Sing CF, Haviland MB, Reilly SL. Genetic architecture <strong>of</strong> common multifactorial <strong>disease</strong>s.<br />
Ciba Found Symp 1996; 197: 211-32.<br />
31. Cronin CC, Shanahan F. Insulin-dependent diabetes mellitus and <strong>coeliac</strong> <strong>disease</strong> [see<br />
comments]. Lancet 1997; 349: 1096-7.<br />
32. Strobel S, Mowat AM. Immune responses to dietary antigens: oral tolerance. Immunol Today<br />
1998; 19: 173-81.<br />
33. Constant SL, Bottomly K. Induction <strong>of</strong> Th1 and Th2 CD4+ T cell responses: the alternative<br />
approaches. Annu Rev Immunol 1997; 15: 297-322.<br />
34. Kay AB. Allergy and allergic <strong>disease</strong>s. First <strong>of</strong> two parts. N Engl J Med 2001; 344: 30-7.<br />
35. Hernell O, Forsberg G, Hammarström S, Ivarsson A, Hammarström M-L. Coeliac <strong>disease</strong>: A<br />
model to study oral tolerance. In: Hart AL, Stagg AJ, Graffner H, Glise H, Falk P, Kamm MA,<br />
eds. Gut Ecology. Martin Dunitz, London: 2002; 73-9.<br />
36. Ivarsson A, Persson LÅ, Nyström L, Ascher H, Cavell B, Danielsson L, et al. Epidemic <strong>of</strong><br />
<strong>coeliac</strong> <strong>disease</strong> in Swedish children. Acta Paediatr 2000; 89: 165-71.<br />
37. Ivarsson A. On the multifactorial aetiology <strong>of</strong> <strong>coeliac</strong> <strong>disease</strong>. Scand J Nutr 2001; 45: 184-5.<br />
38. Ascher H, Krantz I, Kristiansson B. Increasing incidence <strong>of</strong> <strong>coeliac</strong> <strong>disease</strong> in Sweden. Arch<br />
Dis Child 1991; 66: 608-11.<br />
39. Cavell B, Stenhammar L, Ascher H, Danielsson L, Dannaeus A, Lindberg T, et al. Increasing<br />
incidence <strong>of</strong> childhood <strong>coeliac</strong> <strong>disease</strong> in Sweden. Results <strong>of</strong> a national study. Acta Paediatr<br />
1992; 81: 589-92.<br />
40. Carlsson AK, Axelsson IEM, Borulf SK, Bredberg ACA, Ivarsson SA. Serological screening<br />
for celiac <strong>disease</strong> in healthy 2. 5-year-old children in Sweden. Pediatrics 2001; 107: 42-5.<br />
41. Beaglehole R, Bonita R, Kjellström T. Basic epidemiology. World Health Organization;<br />
Geneva, 1993; 1-175.<br />
42. Cummins AG, Thompson FM. Postnatal changes in mucosal immune response: A<br />
physiological perspective <strong>of</strong> breast feeding and weaning. Immunol Cell Biol 1997; 75: 419-<br />
29.<br />
43. Hanson LA. Breastfeeding provides passive and likely long-lasting active immunity. Ann<br />
Allergy Asthma Immunol 1998; 81: 523-37.<br />
44. Gar<strong>of</strong>alo RP, Goldman AS. Expression <strong>of</strong> functional immunomodulatory and antiinflammatory<br />
factors in human milk. Clin Perinatol 1999; 26: 361-77.<br />
45. Goldman AS. Modulation <strong>of</strong> the gastrointestinal tract <strong>of</strong> infants by human milk. Interfaces<br />
and interactions. An evolutionary perspective. J Nutr 2000; 426S-31S.<br />
46. Andersen DH, Di Sant'Agnese PA. Idiopathic celiac <strong>disease</strong>: I. Mode <strong>of</strong> onset and diagnosis.<br />
Pediatrics 1953; 11: 207-22.
INFANT FEEDING PRACTICES AND COELIAC DISEASE<br />
59<br />
47. Greco L, Mayer M, Grimaldi M, Follo D, De Ritis G, Auricchio S. The effect <strong>of</strong> early feeding<br />
on the onset <strong>of</strong> symptoms in celiac <strong>disease</strong>. J Pediatr Gastroenterol Nutr 1985; 4: 52-5.<br />
48. Mäki M, Kallonen K, Lähdeaho ML, Visakorpi JK. Changing pattern <strong>of</strong> childhood <strong>coeliac</strong><br />
<strong>disease</strong> in Finland. Acta Paediatr Scand 1988; 77: 408-12.<br />
49. Kelly DA, Phillips AD, Elliott EJ, Dias JA, Walker-Smith JA. Rise and fall <strong>of</strong> <strong>coeliac</strong> <strong>disease</strong><br />
1960-85. Arch Dis Child 1989; 64: 1157-60.<br />
50. Logan RFA, Rifkind EA, Busuttil A, Gilmour HM, Ferguson A. Prevalence and "incidence" <strong>of</strong><br />
celiac <strong>disease</strong> in Edinburgh and the Lothian region <strong>of</strong> Scotland. Gastroenterology 1986; 90:<br />
334-42.<br />
51. Stevens FM, Egan-Mitchell B, Cryan E, McCarthy CF, McNicholl B. Decreasing incidence <strong>of</strong><br />
<strong>coeliac</strong> <strong>disease</strong>. Arch Dis Child 1987; 62: 465-8.<br />
52. Auricchio S, Follo D, De Ritis G, Giunta A, Marzorati D, Prampolini L, et al. Does breast<br />
feeding protect against the development <strong>of</strong> clinical symptoms <strong>of</strong> celiac <strong>disease</strong> in children? J<br />
Pediatr Gastroenterol Nutr 1983; 2: 428-33.<br />
53. Greco L, Auricchio S, Mayer M, Grimaldi M. Case control study on nutritional risk factors in<br />
celiac <strong>disease</strong>. J Pediatr Gastroenterol Nutr 1988; 7: 395-9.<br />
54. Fälth-Magnusson K, Franzén L, Jansson G, Laurin P, Stenhammar L. Infant feeding history<br />
shows distinct differences between Swedish celiac and reference children. Pediatr Allergy<br />
Immunol 1996; 7: 1-5.<br />
55. Peters U, Schneeweiss S, Trautwein EA, Erbersdobler HF. A case-control study <strong>of</strong> the effect <strong>of</strong><br />
infant feeding on celiac <strong>disease</strong>. Ann Nutr Metab 2001; 45: 135-42.<br />
56. Ascher H, Krantz I, Rydberg L, Nordin P, Kristiansson B. Influence <strong>of</strong> infant feeding and<br />
gluten intake on <strong>coeliac</strong> <strong>disease</strong>. Arch Dis Child 1997; 76: 113-7.<br />
57. Ivarsson A, Hernell O, Stenlund H, Persson LÅ. Breast-feeding protects against celiac<br />
<strong>disease</strong>. Am J Clin Nutr 2002; 75: 914-21.<br />
58. Mäki M, Holm K, Ascher H, Greco L. Factors affecting clinical presentation <strong>of</strong> <strong>coeliac</strong><br />
<strong>disease</strong>: Role <strong>of</strong> type and amount <strong>of</strong> gluten-containing cereals in the diet. In: Auricchio S,<br />
Visakorpi JK, eds. Common food intolerances 1: Epidemiology <strong>of</strong> <strong>coeliac</strong> <strong>disease</strong>. Karger,<br />
Basel: 1992; 76-82.<br />
59. Ascher H, Holm K, Kristiansson B, Mäki M. Different features <strong>of</strong> <strong>coeliac</strong> <strong>disease</strong> in two<br />
neighbouring countries. Arch Dis Child 1993; 69: 375-80.<br />
60. Weile B, Cavell B, Nivenius K, Krasilnik<strong>of</strong>f PA. Striking differences in the incidence <strong>of</strong><br />
childhood celiac <strong>disease</strong> between Denmark and Sweden: A plausible explanation. J Pediatr<br />
Gastroenterol Nutr 1995; 21: 64-8.<br />
61. Mitt K, Uibo O. Low cereal intake in Estonian infants: the possible explanation for the low<br />
frequency <strong>of</strong> <strong>coeliac</strong> <strong>disease</strong> in Estonia. Eur J Clin Nutr 1998; 52: 85-8.<br />
62. Marsh MN. Gluten, major histocompatibility complex, and the small intestine. A molecular<br />
and immunobiologic approach to the spectrum <strong>of</strong> gluten sensitivity ('celiac sprue').<br />
Gastroenterology 1992; 102: 330-54.<br />
63. Doherty M, Barry RE. Gluten-induced mucosal changes in subjects without overt smallbowel<br />
<strong>disease</strong>. Lancet 1981; i: 517-20.<br />
64. Leigh RJ, Marsh MN, Crowe P, Kelly C, Garner V, Gordon D. Studies <strong>of</strong> intestinal lymphoid<br />
tissue. IX. Dose-dependent, gluten-induced lymphoid infiltration <strong>of</strong> <strong>coeliac</strong> jejunal<br />
epithelium. Scand J Gastroenterol 1985; 20: 715-9.<br />
65. Ferguson A, Blackwell JN, Barnetson RS. Effects <strong>of</strong> additional dietary gluten on the small<br />
intestinal mucosa <strong>of</strong> volunteers and <strong>of</strong> patients with dermatitis herpetiformis. Scand J<br />
Gastroenterol 1987; 22: 543-9.<br />
66. Catassi C, Rossini M, Ratsch IM, Bearzi I, Santinelli A, Castagnani R, et al. Dose dependent<br />
effects <strong>of</strong> protracted ingestion <strong>of</strong> small amounts <strong>of</strong> gliadin in <strong>coeliac</strong> <strong>disease</strong> children: a<br />
clinical and jejunal morphometric study. Gut 1993; 34: 1515-9.<br />
67. Anderson CM, Gracey M, Burke V. Coeliac <strong>disease</strong>. Some still controversial aspects. Arch
60 INFANT FEEDING PRACTICES AND COELIAC DISEASE<br />
Dis Child 1972; 47: 292-8.<br />
68. Lindberg T. Coeliac <strong>disease</strong> and infant feeding practices [letter]. Lancet 1981; i: 449<br />
69. Stenhammar L, Ansved P, Jansson G, Jansson U. The incidence <strong>of</strong> childhood celiac <strong>disease</strong> in<br />
Sweden. J Pediatr Gastroenterol Nutr 1987; 6: 707-9.<br />
70. Kagn<strong>of</strong>f MF, Paterson YJ, Kumar PJ, Kasarda DD, Carbone FR, Unsworth DJ, et al.<br />
Evidence for the role <strong>of</strong> a human intestinal adenovirus in the pathogenesis <strong>of</strong> <strong>coeliac</strong> <strong>disease</strong>.<br />
Gut 1987; 28: 995-1001.<br />
71. Lähdeaho ML, Parkkonen P, Reunala T, Mäki M, Lehtinen M. Antibodies to E1b proteinderived<br />
peptides <strong>of</strong> enteric adenovirus type 40 are associated with celiac <strong>disease</strong> and<br />
dermatitis herpetiformis. Clin Immunol Immunopathol 1993; 69: 300-5.<br />
72. Howdle PD, Blair Zajdel ME, Smart CJ, Trejdosiewicz LK, Blair GE, Losowky MS. Lack <strong>of</strong> a<br />
serologic response to an E1B protein <strong>of</strong> adenovirus 12 in <strong>coeliac</strong> <strong>disease</strong>. Scand J<br />
Gastroenterol 1989; 24: 282-6.<br />
73. Vesy CJ, Greenson JK, Papp AC, Snyder PJ, Qualman SJ, Prior TW. Evaluation <strong>of</strong> celiac<br />
<strong>disease</strong> biopsies for adenovirus 12 DNA using a multiplex polymerase chain reaction. Mod<br />
Pathol 1993; 6: 61-4.<br />
74. Holm S, Andersson Y, Gothefors L, Lindberg T. Increased protein absorption after acute<br />
gastroenteritis in children. Acta Paediatr 1992; 81: 585-8.<br />
75. Ivarsson A, Hernell O, Nyström L, Persson LÅ. Children born in the summer have increased<br />
risk for <strong>coeliac</strong> <strong>disease</strong>. J Epidemiol Community Health [in press].<br />
76. Ivarsson A. On the multifactorial etiology <strong>of</strong> celiac <strong>disease</strong>: An epidemiological approach to<br />
the Swedish epidemic. Department <strong>of</strong> Clinical Sciences, Pedatrics, Umeå University,<br />
Sweden. [Dissertation] 2001.<br />
77. Rothman KJ, Greenland S. Causation and causal inference. In: Rothman KJ, Greenland S,<br />
eds. Modern epidemiology: 2nd ed. Lippincott - Raven, Philadelphia: 1998; 7-28.<br />
78. ESPGAN committee on nutrition. Guidelines on infant nutrition III. Recommendations for<br />
infant feeding. Acta Paediatr Scand Suppl 1982; 302: 16-20.<br />
79. Hallert C, Gotthard R, Jansson G, Norrby K, Walan A. Similar prevalence <strong>of</strong> <strong>coeliac</strong> <strong>disease</strong><br />
in children and middle-aged adults in a district <strong>of</strong> Sweden. Gut 1983; 24: 389-91.
Catassi C, Fasano A, Corazza GR (eds):<br />
Primary <strong>prevention</strong> <strong>of</strong> <strong>coeliac</strong> <strong>disease</strong>. The<br />
utopia <strong>of</strong> the new millennium? Perspectives on<br />
Coeliac Disease, vol. 1, AIC Press, pp 61-73<br />
Mechanisms <strong>of</strong> oral tolerance - lessons<br />
for <strong>coeliac</strong> <strong>disease</strong>?<br />
Conleth Feighery<br />
Department <strong>of</strong> Immunology, Trinity College Dublin and St. James's Hospital, Dublin, Ireland<br />
Introduction<br />
Coeliac <strong>disease</strong> (CD) is an inflammatory <strong>disease</strong> <strong>of</strong> the upper small intestine and<br />
1<br />
results from gluten ingestion in genetically susceptible individuals . Gluten is the<br />
essential environmental factor in the development <strong>of</strong> CD: this is demonstrated by the<br />
clinical and mucosal recovery which follows the institution <strong>of</strong> a gluten-free diet.<br />
Genetic factors also play a critical role in the development <strong>of</strong> CD and a strong<br />
association with certain Major Histocompatibility Complex (MHC) class II genes<br />
2<br />
(HLA-DQ2 and HLA-DQ8) is well established . However, CD is a polygenic disorder<br />
and many additional genes, yet to be identified, also contribute to the pathogenesis <strong>of</strong><br />
CD. There is no evidence to suggest that these genes are in any sense “abnormal” and<br />
similar genetic polymorphisms are well represented in the normal population.<br />
Since gluten is part <strong>of</strong> the normal stable diet, and the genes which permit the<br />
development <strong>of</strong> CD are present in the normal population, the question can be<br />
reasonably posed - what makes a particular individual susceptible to gluten induced<br />
damage? It is speculated that additional factors, for example infectious agents and sex<br />
hormones, may be involved. Other environmental factors may also contribute but<br />
currently there are few clues as to what these are. This leads to the broader issue how<br />
does the gut immune system “view” foods? Foods <strong>of</strong> their essence are foreign proteins<br />
and as such might be targeted for elimination, as is the case with any other foreign<br />
antigen.<br />
CD is a common disorder. According to current evidence, it may affect 0.5 to 1% <strong>of</strong><br />
3-4<br />
the population . This suggests that gluten has unique, but ill-understood, properties<br />
which frequently results in a T cell, delayed-type hypersensitivity response to this food<br />
antigen. There is little evidence that other food proteins cause a similar reaction. In<br />
contrast, many foods stimulate food allergy, a type I hypersensitivity reaction with<br />
5<br />
specific IgE production to the <strong>of</strong>fending antigen . In food allergy, a systemic reaction to<br />
61
62<br />
MECHANISMS OF ORAL TOLERANCE<br />
the food is quite common and the reaction remits promptly after the food has been<br />
eliminated from the diet. Food allergy <strong>of</strong>ten develops in early childhood but may no<br />
6<br />
longer be clinically problematic in later years .<br />
Concept <strong>of</strong> immune tolerance<br />
The absent or low immune reactivity <strong>of</strong> the gut to food antigens raises the concept <strong>of</strong><br />
7<br />
immune tolerance . Essentially, it would appear that a limited, local reaction develops<br />
to ingested foods and this response is confined to the bowel mucosa. This permits the<br />
antigenicity <strong>of</strong> food to be recognised but does not allow a damaging immune response<br />
to develop. In this situation, immune tolerance <strong>of</strong> the food is said to have taken place.<br />
From the viewpoint <strong>of</strong> an immunologist, tolerance is defined as the inability or<br />
failure <strong>of</strong> lymphocytes to respond to an antigen. The importance <strong>of</strong> tolerance is best<br />
observed in the concept <strong>of</strong> self-tolerance: in this, an individual's lymphocytes fail to<br />
react with self-antigen and as a consequence the development <strong>of</strong> autoimmune <strong>disease</strong> is<br />
prevented. Self-tolerance is a central paradigm in immunology, first proposed some<br />
8<br />
100 years ago by Paul Erlich who predicted that “horror autotoxicus” might develop if<br />
such a control system was not in place.<br />
Central and peripheral tolerance<br />
7<br />
Immune tolerance can be divided into central and peripheral forms . Central<br />
tolerance relates to events which take place in organs such as the thymus and bone<br />
marrow. In this, it is envisaged that as T cells mature in the thymus, those cells which<br />
might be capable <strong>of</strong> self reactivity (by binding strongly to self-antigens presented by<br />
self-MHC molecules) undergo apoptosis and are thereby deleted. These events prevent<br />
the development <strong>of</strong> T cell mediated autoimmunity. There is considerable experimental<br />
evidence in support <strong>of</strong> such thymic events. It is also proposed that a similar mechanism<br />
9<br />
may cause deletion <strong>of</strong> B cells in the bone marrow .<br />
Despite the evidence for lymphocyte deletion in the thymus, it is not precisely<br />
known how universal this process is. Indeed, it is increasingly being accepted that a low<br />
level <strong>of</strong> autoreactivity is physiological and may even be important for normal immune<br />
10<br />
function . Since it is improbable that all T lymphocytes capable <strong>of</strong> self-reactivity are<br />
removed by this process, a second mechanism has been invoked: this is referred to as<br />
peripheral tolerance (Fig. 1). In this, the potential self-reactivity <strong>of</strong> circulating<br />
lymphocytes is curbed and these cells are rendered tolerant in the periphery. The<br />
mechanisms involved in peripheral tolerance are not well understood.<br />
7-9<br />
There is evidence that some lymphocytes are deleted in the periphery . A more popular<br />
concept is that lymphocyte anergy develops.<br />
One suggested basis for the development <strong>of</strong> anergy is that when lymphocytes encounter<br />
self-antigen, they do so in the absence <strong>of</strong> the appropriate additional signals provided by<br />
co-stimulatory molecules. These molecules include in particular the B7/CD28<br />
interaction, which markedly enhances interleukin (IL)-2 production and hence full T<br />
9<br />
cell activation . If such co-stimulation is absent, the lymphocyte enters a dormant state,
MECHANISMS OF ORAL TOLERANCE<br />
63<br />
Peripheral tolerance<br />
•Clonal deletion<br />
T cell<br />
apoptosis<br />
•Clonal “anergy”<br />
T cell<br />
Inactive / asleep?<br />
•Regulatory clone<br />
T reg<br />
T reg<br />
cytokines<br />
Fig. 1. Mechanisms <strong>of</strong> peripheral tolerance. T reg = regulatory T cell<br />
incapable <strong>of</strong> reacting with a specific antigen. It is possible that anergic T cells can be<br />
rescued from this state, thereby permitting such a cell to display auto-reactivity.<br />
The presence <strong>of</strong> circulating, regulatory T cells is a further mechanism that has been<br />
proposed to explain the phenomenon <strong>of</strong> peripheral tolerance. Following appropriate<br />
activation, these cells release cytokines which inhibit the auto-reactivity <strong>of</strong> the immune<br />
system. In the 1970s, considerable interest surrounded the concept <strong>of</strong> T suppressor cells<br />
performing this task. However, since no specific cell markers or specific suppressor<br />
factors could be reliably identified, the concept became disreputable and it was<br />
damaging to a research grant application or publication to mention the “S” word!<br />
However, fashions change and there is a saying that “what goes around, comes around”<br />
and there is now a growing belief that regulatory T cells play a central role in the<br />
11<br />
<strong>prevention</strong> <strong>of</strong> auto-immunity . According to this concept, regulatory T cells can be<br />
12<br />
considered to conduct the orchestra <strong>of</strong> the immune response .<br />
Finally, a fourth mechanism whereby peripheral tolerance may operate is the<br />
7<br />
concept <strong>of</strong> antigen “ignorance” . According to this concept, antigen internalised within<br />
a tissue or present in only very small quantities, is unable to interact productively with<br />
lymphocytes. The immune control mechanisms described above do not develop for<br />
such antigens. If tissue damage develops, antigen is released and a potentially<br />
damaging immune response may develop.<br />
Mucosal immune system<br />
Exposure to external antigens in humans commonly takes place at two different<br />
sites: the skin and the mucosal surfaces. Although antigen can enter via the skin, the
64 MECHANISMS OF ORAL TOLERANCE<br />
potential for antigen interaction at mucosal surfaces is even greater. The nature <strong>of</strong> skin,<br />
a multi-layered relatively impermeable structure, inhibits the penetration <strong>of</strong> harmful<br />
antigenic structures such as bacteria. In contrast, mucosal surfaces are typically<br />
protected by a single layer <strong>of</strong> epithelial cells. This makes the task <strong>of</strong> antigen access all<br />
the easier. Furthermore, in sites such as the small intestine which have a major role in<br />
absorption <strong>of</strong> nutrients, constant sampling <strong>of</strong> luminal material takes place. Thus, the<br />
mucosal immune system needs to differentiate between harmful antigens (such as<br />
pathogenic bacteria) and innocuous antigens (such as food).<br />
The organisation <strong>of</strong> the mucosal immune response is structured to permit a local<br />
response to the majority <strong>of</strong> antigens which penetrate to the lamina propria cells <strong>of</strong> the<br />
mucosa. However, this immune response is typically <strong>of</strong> low intensity and remains local.<br />
Systemic reaction to such antigen is either minimal or totally absent. Precisely how this<br />
type <strong>of</strong> response is achieved is not fully understood. Secretory IgA produced in the<br />
mucosa may play an important role but other immune components are doubtless also<br />
13<br />
involved . This controlled mucosal immune response could be considered as a form <strong>of</strong><br />
peripheral tolerance and the term “oral tolerance” is frequently used.<br />
Oral tolerance<br />
The phenomenon <strong>of</strong> oral tolerance has been extensively investigated in various<br />
14-16<br />
animal model systems over the past 30 years . As with all experimental models, they<br />
may not precisely replicate the normal in vivo situation but may nonetheless be<br />
informative about how local mucosal immune responses are regulated. The essential<br />
feature <strong>of</strong> experimental oral tolerance is that by feeding an antigen orally, the induction<br />
<strong>of</strong> a systemic immune response to that antigen is prevented.<br />
A typical experiment examining oral tolerance is to study what happens to an animal<br />
after oral administration <strong>of</strong> ovalbumin: when the animal is later exposed to ovalbumin<br />
systemically (by injection), circulating lymphocyte responsiveness to that antigen is<br />
16<br />
either absent or significantly diminished . Animals not pre-fed ovalbumin have a<br />
normal systemic response to the antigen. This effect <strong>of</strong> oral feeding causing systemic<br />
tolerance could be regarded as a form <strong>of</strong> induced peripheral tolerance. In oral tolerance,<br />
although hyporesponsiveness <strong>of</strong> both specific T and B lymphocytes is noted, T cells<br />
seem to be more pr<strong>of</strong>oundly affected. There is no well validated equivalent experiment<br />
confirming the induction <strong>of</strong> oral tolerance in man.<br />
Relevance <strong>of</strong> oral tolerance to <strong>coeliac</strong> and other gastrointestinal <strong>disease</strong>s<br />
The essence <strong>of</strong> the concept <strong>of</strong> oral tolerance is that local gut mucosal immune<br />
responses are regulated and prevent systemic reactions to orally ingested antigens. If,<br />
for whatever reason, a breakdown in oral tolerance develops, an excessive<br />
inflammatory mucosal reaction may take place. Thus, such a breakdown may be<br />
regarded as central to the development <strong>of</strong> inflammatory gastrointestinal disorders.<br />
Examples <strong>of</strong> these include <strong>coeliac</strong> <strong>disease</strong>, Crohn's <strong>disease</strong> and ulcerative colitis. In the<br />
latter two <strong>disease</strong>s the responsible gut antigens are not known, although bacterial<br />
antigens are suspected. In the case <strong>of</strong> CD, it is well established since the 1950s that<br />
17<br />
gluten is the causative agent . It is postulated that immune tolerance <strong>of</strong> gluten, found in<br />
normal subjects, is lost in CD patients and the consequence is inflammation at the major
MECHANISMS OF ORAL TOLERANCE<br />
65<br />
site <strong>of</strong> gluten exposure, the small intestine.<br />
Experimental models <strong>of</strong> oral tolerance differ from CD in certain respects. In CD, the<br />
most prominent evidence <strong>of</strong> inflammation occurs locally, where antigen exposure takes<br />
place. This is not the case in animals in which the effect <strong>of</strong> abrogation <strong>of</strong> oral tolerance<br />
predominantly affects systemic immune responses. However, in some animal models,<br />
18<br />
oral challenge with the antigen was shown to cause a mild mucosal lesion . Of interest,<br />
there is also evidence that gluten intolerance is associated with systemic damage in<br />
some individuals, as represented by <strong>disease</strong>s such as dermatitis herpetiformis, epilepsy<br />
19-21<br />
and cerebellar ataxia . Moreover, there is some evidence that CD is also associated<br />
with inflammation in the distal intestine and rectal histological changes have been<br />
22<br />
reported . Finally, it is worth noting that systemic antibody responses to gluten are<br />
found in a range <strong>of</strong> disorders, in the absence <strong>of</strong> local gut damage or evidence that these<br />
23<br />
antibodies have a systemic pathogenic significance .<br />
Interest in oral tolerance<br />
Over the decades, an interest in the topic <strong>of</strong> oral tolerance has persisted, in the belief<br />
that its study could lead to a more fundamental understanding <strong>of</strong> homeostasis <strong>of</strong> the<br />
immune system. Furthermore, it is postulated that systemic inflammatory <strong>disease</strong>s<br />
14<br />
might be controlled by inducing oral tolerance to the stimulating antigen . According<br />
to this concept, the administration <strong>of</strong> oral antigen (such as the autoantigenic target <strong>of</strong><br />
systemic <strong>disease</strong>) could lead to a reduced or aborted systemic response to this antigen.<br />
Thus various feeding studies with myelin basic protein (in patients with multiple<br />
24 25<br />
sclerosis ) and collagen (in patients with rheumatoid arthritis ) have been described.<br />
Little therapeutic benefit has been noted in these studies to-date.<br />
Finally, an understanding <strong>of</strong> oral tolerance mechanisms is pertinent to the<br />
development <strong>of</strong> oral vaccines, since this route <strong>of</strong> vaccination is designed to give not<br />
only a local protective immune response, but also systemic protection.<br />
Factors involved in control <strong>of</strong> the mucosal immune response<br />
A clear understanding <strong>of</strong> the homeostatic mechanisms responsible for controlling<br />
the mucosal immune response has yet to be reached. Undoubtedly, many interrelated<br />
factors play a role (Fig. 2) and these will be considered briefly here.<br />
The epithelial lining layer “outpost” <strong>of</strong> mucosal immunity<br />
The epithelial cell sitting on its basement membrane, in a sense guards the mucosal<br />
tissue from full, free exposure to antigen. However, the epithelial cell is not an absolute<br />
barrier and it permits rapid absorption <strong>of</strong> soluble antigen. Thus, epithelial cells, like<br />
many other cells in the body, constantly sample the external milieu. We know that food<br />
antigens can rapidly penetrate this epithelial layer, since these antigens are found in the<br />
26<br />
circulation even within minutes <strong>of</strong> food ingestion .<br />
In addition to antigen absorption, epithelial cells have also been shown to process<br />
and load antigen into MHC II molecules. This was demonstrated in the case <strong>of</strong> gliadin,<br />
27<br />
using immuno-electron microscopy . Furthermore, it is known that MHC class II<br />
28<br />
molecules are expressed or can be induced on intestinal epithelial cells . These<br />
findings raise the possibility that epithelial cells might function as antigen presenting
66 MECHANISMS OF ORAL TOLERANCE<br />
Epithelial<br />
cells<br />
IELs<br />
Anatomical<br />
structure<br />
Antigen<br />
structure<br />
Lamina<br />
propria<br />
T cells<br />
Environment<br />
(cytokines)<br />
Antigen<br />
presenting<br />
cells<br />
Fig. 2. Components involved in control <strong>of</strong> mucosal immune response. IELs =intraepithelial<br />
lymphocytes.<br />
cells. However, there is little evidence that conventional antigen stimulation takes<br />
29<br />
place and it may be that epithelial cells interact with T lymphocytes using non-<br />
30<br />
classical MHC molecules such as CD1d . Since epithelial cells do not express the costimulatory<br />
molecules CD80 and CD86, it might be expected that these cells play a role<br />
31-32<br />
in inducing anergy <strong>of</strong> T cells rather than an active T cell response .<br />
The importance <strong>of</strong> the epithelial cell barrier is emphasised by what happens when<br />
barrier function is disrupted. This may occur during the course <strong>of</strong> local inflammation in<br />
33<br />
which tight junction function is impeded . This in turn would allow ready access <strong>of</strong><br />
antigens to immunocompetent cells in the lamina propria. This may explain the<br />
presence <strong>of</strong> high levels <strong>of</strong> antibodies to dietary antigens (including gliadin) in Crohn's<br />
34<br />
and peptic ulcer <strong>disease</strong> . A further demonstration <strong>of</strong> the importance <strong>of</strong> the epithelial<br />
cell barrier is found in certain gene knockout mouse models in which epithelial cell<br />
adherence or their cytoskeletal structure is disrupted: in these models, genes for either<br />
E-cadherin or keratin 8 (respectively) are knocked out, with the spontaneous<br />
35-36<br />
development <strong>of</strong> inflammatory bowel <strong>disease</strong> as a consequence .<br />
Antigen factors<br />
The size, structure and nature <strong>of</strong> antigens affects the response <strong>of</strong> the mucosal<br />
immune system. Thus in health, soluble dietary antigens induce a limited, local immune<br />
response and <strong>of</strong>ten a barely discernible response in the systemic circulation. Likewise,<br />
the gut flora induces a local immune response only. In contrast, particulate antigen is<br />
37<br />
absorbed by specialised epithelial cells called micr<strong>of</strong>old or M cells . M cells are found
MECHANISMS OF ORAL TOLERANCE<br />
67<br />
interposed between the lining epithelial cells and following uptake <strong>of</strong> antigen,<br />
particulate antigen is processed and presented to local T helper cells. This in turn results<br />
in a systemic immune response to the antigen.<br />
As discussed earlier, in contrast to other food antigens, gluten appears to have an<br />
unique capacity to stimulate a local T cell mediated immune response in CD patients,<br />
leading to damage <strong>of</strong> the local mucosa. The chemical properties <strong>of</strong> gluten involved in<br />
eliciting such a response are unknown, since no essential structural difference is<br />
10<br />
thought to exist between self-antigens and foreign antigens .<br />
Intraepithelial lymphocytes<br />
Intraepithelial lymphocytes (IELs) are T cells located within the surface epithelium<br />
<strong>of</strong> the mucosa. Despite intense research <strong>of</strong> these cells over the past two decades, their<br />
38<br />
principal function remains enigmatic . The majority <strong>of</strong> IELs express the CD8<br />
molecule and employ the abT cell receptor (TCR). It is well established that increased<br />
numbers <strong>of</strong> IELs are found in certain intestinal inflammatory states such as <strong>coeliac</strong><br />
<strong>disease</strong>. Moreover, in <strong>coeliac</strong> <strong>disease</strong> the number <strong>of</strong> IELs expressing the gdTCR<br />
39<br />
increases, with as many as 30% belonging to this phenotype . According to recent<br />
evidence, IELs may include heterogeneous populations <strong>of</strong> T cells, natural killer T cells<br />
40<br />
and also natural killer cells . It has been speculated that IELs play a role in oral<br />
tolerance and there is some experimental evidence to support a role for gdT cells in<br />
41<br />
tolerance induction .<br />
Lamina propria T cells<br />
The major population <strong>of</strong> lamina propria T cells express the CD4 molecule and<br />
employ the abTCR. These T helper cells are thought to have initially encountered<br />
mucosal antigen in organised lymphoid structures such as Peyer's patches and after<br />
passage through the systemic circulation have specifically homed back to the intestine.<br />
In this location, lamina propria T cells play a major role in orchestrating other cells <strong>of</strong><br />
12<br />
the immune system and act as conductors <strong>of</strong> this orchestra . These T cells possess a full<br />
range <strong>of</strong> surface molecules to allow productive interaction with many other cell types.<br />
Moreover, individual populations manufacture the variety <strong>of</strong> cytokines required to<br />
influence B cell production <strong>of</strong> specific antibody isotypes, to induce specific populations<br />
13<br />
<strong>of</strong> antigen presenting cells and to activate other populations <strong>of</strong> T cells . Thus,<br />
regulation <strong>of</strong> immune events in the intestine is largely a function <strong>of</strong> these cells, and<br />
hence maintenance <strong>of</strong> “oral tolerance” or mucosal immune homeostasis is likely to be<br />
achieved by these cells.<br />
Dendritic and other antigen presenting cells<br />
The activation <strong>of</strong> intestinal T cells requires the presentation <strong>of</strong> antigen by local<br />
populations <strong>of</strong> antigen presenting cells (APCs). This task may be performed by a<br />
variety <strong>of</strong> APCs including dendritic cells, macrophages, B cells and, as discussed<br />
12-13<br />
earlier, possibly by enterocytes . Populations <strong>of</strong> all these cell types have been<br />
identified in the mucosal tissue. In individual situations, it is likely that the presentation<br />
<strong>of</strong> antigen is principally performed by specific cell types. Dendritic cells, in particular,<br />
may play a central role in presenting antigen and influencing the evolution <strong>of</strong> specific
68 MECHANISMS OF ORAL TOLERANCE<br />
types <strong>of</strong> T cell populations in the intestine.<br />
Much has been learned about dendritic cells in recent years: some types particularly<br />
42-43<br />
influence the development <strong>of</strong> Th1 cells and others Th2 cells . These dendritic<br />
populations can be identified on the basis <strong>of</strong> expression or absence <strong>of</strong> the adhesion<br />
molecule CD11c and also by the type <strong>of</strong> cytokines (such as IL-12) which they produce.<br />
The heterogeneity <strong>of</strong> dendritic cells is increasingly being recognised and it is now<br />
appreciated that the major function <strong>of</strong> some populations is to induce T cell tolerance,<br />
44<br />
rather than a productive immune response .<br />
As with all events in the immune system, a circular feedback system (so-called<br />
inter-cellular cross-talk) operates between dendritic cells and the T cells which they<br />
help stimulate (fig. 3). Thus, the cytokine products <strong>of</strong> dendritic cells influence the T cell<br />
populations which they generate and in turn, the cytokines produced by T cells<br />
42<br />
influence the type <strong>of</strong> dendritic cells which occupy that locale .<br />
A further population <strong>of</strong> cells, likely to be involved in antigen presentation, which<br />
express the macrophage scavenger receptor (CD163) has been identified by<br />
45<br />
immunohistochemistry in the central core <strong>of</strong> individual villi . The cytokine products <strong>of</strong><br />
this population <strong>of</strong> macrophage-like cells, including secreted CD163, may play a role in<br />
46<br />
down-regulation <strong>of</strong> the local immune response .<br />
Cytokine environment <strong>of</strong> the mucosa<br />
Virtually all cells in the mucosa, including enterocytes, produce a wide range <strong>of</strong><br />
cytokines and the pr<strong>of</strong>ile <strong>of</strong> cytokines determines the net effect on the type <strong>of</strong> immune<br />
response elicited. It is presumed that a major, final determining influence is the type <strong>of</strong><br />
cytokines produced by the local T helper populations. Since the principal default setting<br />
<strong>of</strong> the mucosal immune response is towards tolerance <strong>of</strong> encountered antigen, the<br />
cytokines which could determine tolerance have been investigated. The three cytokines<br />
which have received most interest for their potential involvement are IL-4, IL-10 and<br />
TGF-b.<br />
For some time it was considered that T cell tolerance in the mucosa was achieved by<br />
a predominant Th2 response to local antigens. Major products <strong>of</strong> Th2 cells include the<br />
cytokines IL-4 and IL-10. However, in some animal model experiments, it was shown<br />
that these cytokines are not required for tolerance induction. Moreover, in experimental<br />
oral tolerance, inhibition <strong>of</strong> IgE production is a characteristic feature: the reverse would<br />
14<br />
be predicted in an IL-4 dominant environment . Hence, it is now proposed that<br />
tolerance in the intestine may be achieved by a further T cell population, referred to as T<br />
47<br />
regulatory cells . The major cytokine products <strong>of</strong> these cells are IL-10 and<br />
transforming growth factor-beta (TGF-b).<br />
Although IL-10 is not essential in some models <strong>of</strong> oral tolerance, the importance <strong>of</strong><br />
this cytokine in maintaining tolerance is emphasized by the spontaneous development<br />
48<br />
<strong>of</strong> colitis in mice when the gene for this cytokine is “knocked out” . Of great interest,<br />
49<br />
TGF-bcan reverse the colitis . It is also known that IL-10 may be required for the<br />
production <strong>of</strong> TGF-band that the latter cytokine inhibits the IL-12/interferon-gamma<br />
50<br />
(IFN-g) pathway, likely to play a central role in many inflammatory <strong>disease</strong>s .<br />
It is currently hypothesised that control <strong>of</strong> the mucosal immune system is<br />
maintained by regulatory T cells, but at present, other than studying their cytokine
MECHANISMS OF ORAL TOLERANCE<br />
69<br />
IEL<br />
Lamina propria<br />
M cell<br />
CD4<br />
DC<br />
Cytokines <strong>of</strong> each cell type<br />
influence each other<br />
Epithelial<br />
lining<br />
Fig. 3. Interaction between CD4 + T cells and dendritic cells in lamina propria <strong>of</strong> the<br />
mucosa. DC = dendritic cell; IEL = intraepithelial lymphocyte.<br />
products, we do not have reliable, specific markers for these cells. It is probable that<br />
TGF-band IL-10 are major products <strong>of</strong> these cells. However, it should be emphasised,<br />
that even when a cytokine is shown not to be essential for experimental oral tolerance,<br />
this does not mean that in vivo, this cytokine has no role to play, since a level <strong>of</strong><br />
redundancy is a common feature <strong>of</strong> the immune system.<br />
Mucosal immune tolerance and <strong>coeliac</strong> <strong>disease</strong><br />
The preceding discussion <strong>of</strong> mucosal immune tolerance raises issues which may be<br />
pertinent to the pathogenesis <strong>of</strong> <strong>coeliac</strong> <strong>disease</strong>. Is the essential defect in <strong>coeliac</strong> <strong>disease</strong><br />
a failure <strong>of</strong> the normal tolerance mechanisms, which allow gluten exposure but no<br />
mucosal damage in normal individuals? If so, might tolerance <strong>of</strong> gluten be restored and<br />
thereby permit CD patients to eat a normal diet? If this were possible, how might we go<br />
about achieving it? Obviously, these are major issues and it could be argued that<br />
restoring tolerance to gluten is a fanciful solution, perhaps unlikely ever to be achieved.<br />
Nonetheless, with the gathering pace <strong>of</strong> modern knowledge and technology, it is a goal<br />
which should at least be examined.<br />
Adolescent <strong>coeliac</strong> <strong>disease</strong><br />
Some 30 years ago, one <strong>of</strong> the most frequent inquiries about the nature <strong>of</strong> CD, was<br />
whether gluten intolerance was permanent. Of course, the dogma now is that permanent
70 MECHANISMS OF ORAL TOLERANCE<br />
51<br />
intolerance is a central feature <strong>of</strong> the disorder . However, in the past, cases <strong>of</strong> possible<br />
52<br />
transient gluten sensitivity were described . Is it possible that this phenomenon <strong>of</strong><br />
53-54<br />
transiency is more common than currently appreciated? .<br />
The events that happen to pediatric cases <strong>of</strong> CD, when they reach adolescence, may<br />
be informative concerning the permanency <strong>of</strong> gluten intolerance. Detailed information<br />
about these events is absent. Nonetheless, it is recognized that many children adhere<br />
less well to a strict gluten free diet when they reach adolescence. This may represent the<br />
general “rebellion” <strong>of</strong> teenagers! Despite eating gluten containing foods, few<br />
symptoms may develop. This in turn may lead to increasing carelessness about their<br />
diets. Some <strong>of</strong> these patients eventually have intestinal biopsies performed and the<br />
mucosa can appear surprisingly normal or even completely normal. Doubts about the<br />
accuracy <strong>of</strong> the initial diagnosis <strong>of</strong> CD may then be raised. Some <strong>of</strong> these patients are<br />
then given a gluten challenge and it is reported that it can take many months or even<br />
55-56<br />
years for histological evidence <strong>of</strong> CD to return . This contrasts with gluten challenge<br />
in patients with an adult diagnosis <strong>of</strong> CD when symptomatic and histological evidence<br />
56<br />
<strong>of</strong> <strong>disease</strong> relapse <strong>of</strong>ten only requires one or two months <strong>of</strong> gluten intake .<br />
Although categorical data about adolescent remission <strong>of</strong> CD is lacking, the<br />
information available strongly suggests that this really does occur. If this is the case, it<br />
may indicate that restoration <strong>of</strong> tolerance to gluten is possible. The majority, if not all <strong>of</strong><br />
these patients, eventually develop symptomatic gluten intolerance in adulthood,<br />
demonstrating the essential permanency <strong>of</strong> CD. However, it is possible that<br />
investigation <strong>of</strong> adolescent CD patients, during their period <strong>of</strong> remission, may give<br />
insight to T cell tolerance mechanisms towards gluten.<br />
Conclusions<br />
The gut mucosal immune response to the majority <strong>of</strong> food and other antigens is<br />
typically <strong>of</strong> low intensity and remains confined to the local environment. The term ²oral<br />
tolerance²may be applied to this controlled immune response. However, in the case <strong>of</strong> a<br />
single food type, gluten, an enhanced T cell immune response develops in a substantial<br />
number <strong>of</strong> individuals and features <strong>of</strong> <strong>coeliac</strong> <strong>disease</strong> develop. In this disorder, immune<br />
tolerance <strong>of</strong> gluten is apparently lost. With an improved understanding <strong>of</strong> the<br />
mechanisms <strong>of</strong> oral tolerance, it is possible that manipulation <strong>of</strong> the immune response<br />
to gluten in <strong>coeliac</strong> patients could restore the normal physiological state <strong>of</strong> low<br />
reactivity to this food antigen. This would remove the requirement <strong>of</strong> gluten-free diet<br />
treatment <strong>of</strong> <strong>coeliac</strong> <strong>disease</strong>.<br />
References<br />
1. Feighery C. Coeliac <strong>disease</strong> Fortnightly review. BMJ 1999; 319: 236-9.<br />
2. Kagn<strong>of</strong>f MF. Genetic basis <strong>of</strong> Coeliac Disease: role <strong>of</strong> HLA genes. In: MN Marsh<br />
(Ed) Coeliac Disease, Oxford, Blackwell Scientific Publications, 1992; pp215-38.<br />
3. Catassi C, Fabiani E, Rätsch IM, Coppa GV, Giorgi PL, Pierdomenico R, et al. The<br />
<strong>coeliac</strong> iceberg in Italy. A multicentre antigliadin antibodies screening for <strong>coeliac</strong><br />
<strong>disease</strong> in school-age subjects. Acta Paediatr Suppl 1996; 412: 29-35.<br />
4. McMillan SA, Watson RPG, McCrum EE, Evans AE. Factors associated with serum
MECHANISMS OF ORAL TOLERANCE<br />
71<br />
antibodies to reticulin, endomysium, and gliadin in an adult population. Gut 1996;<br />
39: 43-7.<br />
5. Furukawa CT. Adverse Reactions to Food. In: Allergy in Primary Care. Eds. LC.<br />
Altman, JW. Becker, PV Williams. Publishers. W.B. Saunders Company 2000; 18:<br />
259-64.<br />
6. Sampson HA. What should we be doing for children with peanut allergy? J Pediatr<br />
2000; 137: 741-3.<br />
7. Kamradt T, Mitchison NA. Tolerance and Autoimmunity. N Engl J Med 2001; 344:<br />
655-64.<br />
8. Bibel DJ. Milestones in Immunology: a historical exploration. Science Tech<br />
Publishers, Wisconsin, USA. 1988.<br />
9. Janeway CA, Travers P, Walport M, Capra JD. Immunobiology: the immune system<br />
in health and <strong>disease</strong>. Churchill Livingstone, 1999.<br />
10. Davidson A, Diamond B. Advances in Immunology: Autoimmune Diseases. N Engl<br />
J Med 2001; 345: 340-50.<br />
11. Shevach EM. Certified Pr<strong>of</strong>essionals: CD4+ CD25+ Suppressor T Cells. J Exp Med<br />
2001; 193: F41-5.<br />
12. Feighery C. Intestinal Immune System - A Hidden Symphony. In: Gastrointestinal<br />
Immunology and Gluten-Sensitive Disease. Proceedings <strong>of</strong> the Sixth International<br />
Symposium on Coeliac Disease held at Trinity College, Dublin in July 1992. Eds. C.<br />
Feighery, C. O'Farrelly, Publishers Oak Tree Press, Dublin.<br />
13. Brandtzaeg P, Baekkevold ES, Farstad IN, Jahnsen FL, Johansen FE, Nilsen EM, et<br />
al. Regional specialization in the mucosal immune system: what happens in the<br />
microcompartments? Immunol Today 1999; 3: 141-51.<br />
14. Garside P, Mowat AM, Khoruts A. Oral tolerance in <strong>disease</strong>. Gut 1999; 44: 137-42.<br />
15. Weiner HL. Induction and mechanism <strong>of</strong> action <strong>of</strong> transforming growth factor-betasecreting<br />
Th3 regulatory cells. Immunol Rev 2001; 182: 207-14.<br />
16. Mowat McI A. The regulation <strong>of</strong> immune responses to dietary protein antigens.<br />
Immunology Today 1987; 8: 93-8.<br />
17. Dicke WK. Coeliakie. PhD thesis. University <strong>of</strong> Utreacht, Utreacht, The<br />
Netherlands, 1950.<br />
18. Lamont AG, Mowat AM, Parrott DM. Priming <strong>of</strong> systemic and local delayed-type<br />
hypersensitivity responses by feeding low doses <strong>of</strong> ovalbumin to mice. Immunology<br />
1989; 66: 595-9.<br />
19. Fry L. Dermatitis herpetiformis: from gut to skin, contributions to the nature <strong>of</strong><br />
<strong>coeliac</strong> <strong>disease</strong>. In: Coeliac Disease, Mäki M, Collin P, Visakorpi JK (eds).<br />
Proceedings <strong>of</strong> the Seventh International Symposium on Coeliac Disease, Finland.<br />
Publishers. Coeliac Disease Study Group, Tampere, Finland,1996; pp67-74.<br />
20. Cronin CC, Jackson LM, Feighery C, Shanahan F, Abuzakouk M, Ryder DQ, et al.<br />
Coeliac <strong>disease</strong> and epilepsy. Q J Med 1998; 91: 303-8.<br />
21. Hadjivassiliou M, Grunewald RA, Chattopadhyay AK, Davies-Jones GA, Gibson A,<br />
Jarratt JA et al. Clinical, radiological, neurophysiological, and neuropathological<br />
characteristics <strong>of</strong> gluten ataxia. Lancet 1998; 352: 1582-5.<br />
22. Ensari A, Marsh MN, L<strong>of</strong>t DE, Morgan S, Moriarty K. Morphometric analysis <strong>of</strong><br />
intestinal mucosa. V. Quantitative histological and immunocytochemical studies <strong>of</strong><br />
rectal mucosae in gluten sensitivity. Gut 1993; 34: 1225-9.
72 MECHANISMS OF ORAL TOLERANCE<br />
23. McCormick PA, Feighery C, Dolan C, O'Farrelly C, Kelleher P, Graeme-Cook F, et<br />
al. Altered gastrointestinal immune response in sarcoidosis. Gut 1988; 29: 1628-<br />
31.<br />
24. Weiner HL, Mackin GA, Matsui M, Orav EJ, Khoury SJ, Dawson DM, et al. Doubleblind<br />
pilot trial <strong>of</strong> oral tolerization with myelin antigens in multiple sclerosis.<br />
Science 1993; 259: 1321-4.<br />
25. Barnett ML, Combitchi D, Trentham DE. A pilot trial <strong>of</strong> oral type II collagen in the<br />
treatment <strong>of</strong> juvenile rheumatoid arthritis. Arthritis Rheum 1996; 39: 623-8.<br />
26. Husby S, Jensenius JC, Svehag SE. Passage <strong>of</strong> undergraded dietary antigen into the<br />
blood <strong>of</strong> healthy adults. Further characterization <strong>of</strong> the kinetics <strong>of</strong> uptake and the<br />
size distribution <strong>of</strong> the antigen. Scand J Immunol 1986; 24: 447-52.<br />
27. Zimmer KP, Poremba C, Weber P, Ciclitira PJ, Harms E. Translocation <strong>of</strong> gliadin<br />
into HLA-DR antigen containing lysosomes in <strong>coeliac</strong> <strong>disease</strong> enterocytes. Gut<br />
1995; 36: 703-9.<br />
28. Kelly J, Weir DG, Feighery CF. Differential expression <strong>of</strong> HLA-D gene products in<br />
the normal and <strong>coeliac</strong> small bowel. Tissue Antigens 1987; 31: 151-60.<br />
29. Mayer L, Schlien R. Evidence for function <strong>of</strong> Ia molecules on gut epithelial cells in<br />
man. J Exp Med 1987; 166: 1471-83.<br />
30. Canchis PW, Bhan AK, Landau SB, Yang L, Balk SP, Blumberg RS. Tissue<br />
distribution <strong>of</strong> the non-polymorphic major histocompatibility complex class I-like<br />
molecule, CD1d. Immunology 1993 ; 80: 561-5.<br />
31. Byrne B, Madrigal-Estebas L, McEvoy A, Carton J, Doherty DG, O'Donoghue D, et<br />
al. Human duodenal epithelial cells constitutively express molecular components <strong>of</strong><br />
antigen presentation but not costimulatory molecules. (2002, submitted).<br />
32. Mowat AM. Regulation <strong>of</strong> Immune Responses to Dietary Protein Antigens. In:<br />
Gastrointestinal Immunology and Gluten-Sensitive Disease. Proceedings <strong>of</strong> the<br />
Sixth International Symposium on Coeliac Disease held at Trinity College Dublin,<br />
July 1992. Eds. Feighery C, O'Farrelly C. Publishers: Oak Tree Press, Dublin.<br />
33. Madara JL. Regulation <strong>of</strong> the movement <strong>of</strong> solutes across tight junctions. Annu Rev<br />
Physiol 1998; 60: 143-59.<br />
34. Feighery C, Weir DG, Whelan A, Willoughby R, Youngprapakorn S, Lynch S, et al.<br />
Diagnosis <strong>of</strong> gluten-sensitive enteropathy: is exclusive reliance on histology<br />
appropriate? Eur J Gastroenterol Hepatol 1998; 10: 919-25.<br />
35. Hermiston ML, Gordon JI. Inflammatory bowel <strong>disease</strong> and adenomas in mice<br />
expressing a dominant negative N-cadherin. Science 1995; 270: 1203-7.<br />
36. Baribault H, Penner J, Iozzo RV, Wilson-Heiner M. Colorectal hyperplasia and<br />
inflammation in keratin 8-deficient FVB/N mice. Genes Dev 1994; 8: 2964-73.<br />
37. Trier, J. S. Structure and function <strong>of</strong> intestinal M cells. Gastroenterol Clin North Am.<br />
1991; 20: 531-47.<br />
38. Hayday A, Theodoridis E, Ramsburg E, Shires J. Intraepithelial lymphocytes:<br />
exploring the Third Way in immunology. Nat Immunol 2001; 2: 997-1003.<br />
39. Viney J, MacDonald T, Spencer J. Gamma delta T cells in the gut epithelium. Gut<br />
1990: 31: 841-4.<br />
40. Eiras P, Leon F, Camarero C, Lombardia M, Roldan E, Bootello A, et al. Intestinal<br />
intraepithelial lymphocytes contain a CD3 - CD7+ subset expressing natural killer<br />
markers and a singular pattern <strong>of</strong> adhesion molecules. Scand J Immunol 2000; 52:
MECHANISMS OF ORAL TOLERANCE<br />
73<br />
1-6.<br />
41. Ke Y, Kapp JA. Oral antigen inhibits priming <strong>of</strong> CD8+ CTL, CD4+ T cells and<br />
antibody responses which activating CD8+ suppressor T cells. J Immunol 1996;<br />
156: 916-21.<br />
42. Banchereau J, Briére F, Caux C, Davoust J, Lebecque S, Liu Y-J, et al.<br />
Immunobiology <strong>of</strong> dendritic cells. Annu Rev Immunol 2000; 18: 767-811.<br />
43. Lanzavecchia A, Sallusto F. Regulation <strong>of</strong> T cell immunity by dendritic cells. Cell<br />
2001; 106: 263-6.<br />
44. Jonuleit H, Schmitt E, Steinbrink K, Enk AH. Dendritic cells as a tool to induce<br />
anergic and regulatory T cells. Trends in Immunol 2001; 22: 394-400.<br />
45. Whelan CA. (personal communication).<br />
46. Hogger P, Sorg C. Soluble CD163 inhibits phorbol ester-induced lymphocyte<br />
proliferation. Biochem Biophys Res Commun 2001; 288: 841-3.<br />
47. Groux H, O'Garra A, Bigler M, Rouleau M, Antonenko S, de Vries JE, et al. A CD4+<br />
T-cell subset inhibits antigen-specific T-cell responses and prevents colitis. Nature<br />
1997; 389: 737-42.<br />
48. Kuhn R, Lohler J, Rennick D, Rajewsky K, Muller W. Interleukin-10-deficient mice<br />
develop chronic enterocolitis. Cell 1993; 75: 263-79.<br />
50. Neurath MF, Fuss I, Kelsall BL, Presky DH, Waegell W, Strober W. Experimental<br />
granulomatous colitis in mice is abrogated by induction <strong>of</strong> TGF-b-mediated oral<br />
tolerance. J Exp Med 1996; 183: 2605-16.<br />
50. Fishman-Lobell J, Friedman A, Weiner HL. Different kinetic patterns <strong>of</strong> cytokine<br />
gene expression in vivo in orally tolerant mice. Eur J Immunol 1994; 24: 2720-4.<br />
51. Weijers HA, Lindquist B, Anderson CM, et al. Round table discussions. Diagnostic<br />
criteria in celiac <strong>disease</strong>. Acta Paediatr Scand 1970: 59: 461-3.<br />
52. Walker-Smith JA. Transient gluten intolerance. Arch Dis Child 1970; 45: 523-6.<br />
53. Schmitz J. Is celiac <strong>disease</strong> a lifelong disorder? Clin Invest Med 1996; 19: 352-6.<br />
54. Ansaldi N, Tavassoli K, Faussone D, Forni M, Oderda G. Clinical-histological<br />
behavior <strong>of</strong> celiac patients after gluten load following the definitive diagnosis.<br />
Pediatr Med Chir 1988; 10: 3-6.<br />
55. McNicholl B, Egan-Mitchell B, Fottrell PF. Variability <strong>of</strong> gluten intolerance in<br />
treated childhood <strong>coeliac</strong> <strong>disease</strong>. Gut 1979; 20: 126-32.<br />
56. O'Mahony C. Immunological and Clinical Studies in Gluten Sensitive Disease.<br />
University College Dublin. MD Thesis 1986.
Catassi C, Fasano A, Corazza GR (eds):<br />
Primary <strong>prevention</strong> <strong>of</strong> <strong>coeliac</strong> <strong>disease</strong>. The<br />
utopia <strong>of</strong> the new millennium? Perspectives on<br />
Coeliac Disease, vol. 1, AIC Press, pp 75-82<br />
Genetically detoxified grains in <strong>coeliac</strong> <strong>disease</strong><br />
Federico Biagi, Antonio Di Sabatino, Jonia Campanella, Gino Roberto Corazza<br />
Department <strong>of</strong> Gastroenterology, University <strong>of</strong> Pavia, IRCCS Policlinico San Matteo, Pavia, Italy<br />
Coeliac <strong>disease</strong> (CD) is a chronic enteropathy triggered in genetically predisposed<br />
individuals by gluten, the storage proteins <strong>of</strong> wheat, barley, and rye. So, from a<br />
“<strong>coeliac</strong>ologist” point <strong>of</strong> view gluten represents the <strong>coeliac</strong> <strong>of</strong>fending agent. More<br />
precisely, gluten can be defined as the rubbery mass that remains when wheat dough is<br />
1-2<br />
washed to remove starch granules and other soluble constituents .<br />
Classification <strong>of</strong> gluten proteins<br />
According to plant taxonomy, all the species (i.e. wheat, barley, and rye) toxic for<br />
patients affected by CD are members <strong>of</strong> the Gramineae grass family. However, it<br />
should be noted that other Gramineae grass family species, such as rice, sorghum,<br />
maize, and probably oats, are safe for CD patients. Since wheat, barley, and rye all fall<br />
in the tribe Hordae/Triticeae, it is possible that only species found in that tribe have<br />
proteins active in CD. Moreover, Hordae proteins are all rich in proline and glutamine,<br />
which is the reason why they were named prolamins. Although non toxic prolamins,<br />
such as avenins and zeins are also proline - and glutamine-rich, they have a lower<br />
3<br />
proline content compared to Hordae tribe grains .<br />
On the basis <strong>of</strong> their different solubility in a 70% ethanol solution, wheat proteins<br />
1-2<br />
can be divided into gliadins and glutenins . Gliadins are soluble single-chain<br />
polypeptides. On the basis <strong>of</strong> different electrophoretic mobility, gliadins component<br />
were classified into a-, b-, g-, and w-gliadins. Glutenins are insoluble proteins crosslinked<br />
one to another by intrachain disulphide bonds. Components were obtained after<br />
the reduction <strong>of</strong> the disulphide bonds, and grouped into low - (LMW) and highmolecular<br />
weight (HMW) subunits. However, it was shown that the extraction <strong>of</strong> gluten<br />
with aqueous solution does not lead to clear-cut fractions. Very <strong>of</strong>ten, glutenin subunits<br />
can be found in the soluble gliadin fraction and gliadins are also present in the insoluble<br />
glutenin fraction. So, it has recently emerged that the most important criteria to classify<br />
4-5<br />
gluten components is the <strong>primary</strong> structure . Using analysis <strong>of</strong> amino acid sequence<br />
and molecular mass, gluten proteins have been divided into high-, medium - and low-<br />
75
76<br />
GENETICALLY DETOXIFIED GRAINS<br />
molecular weight proteins. High-molecular weight proteins (x - and y-type subunits)<br />
comprise the HMW subunits <strong>of</strong> glutenins; glutamine, glycine, and proline represent<br />
70% <strong>of</strong> total residues. Medium-molecular weight group consists <strong>of</strong> w-gliadins; 80% <strong>of</strong><br />
the amino acids is due to glutamine, proline, and phenylalanine, but cysteine and<br />
methionine, i.e. sulphur containing amino acids, are almost absent. Low-molecular<br />
weight proteins consist <strong>of</strong> a-, b-, g-gliadins and LMW subunits <strong>of</strong> glutenins; they are<br />
rich in sulphur containing amino acids.<br />
Functional properties <strong>of</strong> gluten proteins<br />
Although the only known function <strong>of</strong> these proteins is to act as storage proteins, by<br />
releasing nitrogen for the germinating seed, their biochemistry structure has a crucial<br />
2,6<br />
role in providing the unique baking quality <strong>of</strong> wheat . Both LMW and HMW have not<br />
only intrachain but also interchain disulphide bonds allowing them to crosslink other<br />
glutenin and gliadin peptides, which results in the formation <strong>of</strong> beta-spirals. During the<br />
baking process, CO<br />
2<br />
is produced by yeast fermentation and is trapped in the beta-spiral<br />
three dimensional net. Glutenins spirals become extended but maintain the capacity to<br />
return to the colloid state. So, elasticity and cohesivity <strong>of</strong> the dough system are due to<br />
the cross-linked nature <strong>of</strong> the glutenin subunits, mainly the high molecular weight<br />
glutenins. On the other hand, soluble monomeric gliadins guarantee extensibility and<br />
viscosity to the dough (Fig. 1).<br />
Coeliac toxicity <strong>of</strong> gliadins and glutenins<br />
Since the demolition <strong>of</strong> these proteins to single amino acids results on loss <strong>of</strong> <strong>coeliac</strong><br />
C<br />
C<br />
N<br />
N<br />
N<br />
TECHNOLOGICAL<br />
PROPERTIES<br />
N N C C C<br />
HMWx HMWy LMW g a<br />
Elasticity & Cohesivity<br />
Extensibility & Viscosity<br />
Fig. 1. Schematic representation <strong>of</strong> gluten protein components. Black segments unique<br />
sequence; white segments repeating sequence; ] intrachain disulphide bond; - interchain<br />
disulphide bond; C C-terminal sequence; N N-terminal sequence; HMWx high-molecular<br />
weight glutenins x-type subunit; HMWy high-molecular weight glutenins y-type subunit;<br />
LMW low-molecular weight glutenins; g-gliadins; a-gliadins.
GENETICALLY DETOXIFIED GRAINS<br />
77<br />
toxicity, several studies investigated which one <strong>of</strong> the several gluten components is<br />
responsible for CD intolerance. Briefly, a-, b-, g- and w-gliadins are all toxic for CD<br />
patients. Although glutenins were considered to be non dangerous for <strong>coeliac</strong> patients,<br />
1,7<br />
their safety is at least controversial . First <strong>of</strong> all alcohol extraction does not lead to<br />
clear-cut fractions. So, gliadins have actually been found within the insoluble glutenins,<br />
and that is an obstacle in understanding pure glutenin toxicity. Moreover, it has very<br />
recently been shown that glutenin peptides can induce an in-vitro specific activation<br />
and proliferation <strong>of</strong> T cell from <strong>coeliac</strong> small bowel. Such a response is virtually<br />
identical to that seen with gliadin peptides and is nowadays considered to be an indirect<br />
8-9<br />
evidence <strong>of</strong> <strong>coeliac</strong> toxicity .<br />
Although a major effort needs to be done to understand which gluten components<br />
are toxic in CD, this knowledge would be extremely important in order to develop<br />
genetically detoxified grains (GDG). The development <strong>of</strong> wheat strains lacking those<br />
genes coding for toxic peptides is hopefully regarded as a new and pr<strong>of</strong>itable tool for the<br />
treatment <strong>of</strong> CD. GDG could provide the solution to problems such as the poor<br />
palatability and high costs <strong>of</strong> commercially available gluten-free foods. GDG may be<br />
theoretically achieved with the modern techniques <strong>of</strong> genetic plant engineering which<br />
makes the deleting or silencing <strong>of</strong> one or more genes a possible approach.<br />
Genetics <strong>of</strong> wheat proteins<br />
Bread wheat is a hexaploid species containing three different but related genomas<br />
10-11<br />
(A, B, and D), each consisting <strong>of</strong> seven chromosome pairs (Fig. 2) . Information for<br />
storage proteins is encoded by clustered or dispersed gene families located on<br />
chromosomes 1 and 6 <strong>of</strong> the three different genomes. In particular, genes for a-gliadins<br />
are located on the short arm <strong>of</strong> chromosomes 6A, 6B, and 6D, tightly clustered at the<br />
Gli-A2, Gli-B2, and Gli-D2 loci. Genes coding for gw<br />
-and -gliadins are on the short arm<br />
1A<br />
1B<br />
1D<br />
6A<br />
Glu-1 (HMW)<br />
Glu-B2<br />
Gli-A3<br />
Gli-B3<br />
Glu-3<br />
(LMW) Gli-1 (gw)<br />
Gli-2 (ab)<br />
Gli-A5<br />
Gli-B5<br />
Gli-D5<br />
6B<br />
6D<br />
Long Arm<br />
Short Arm<br />
Fig. 2. Chromosomal position <strong>of</strong> the genes coding for storage proteins <strong>of</strong> bread wheat<br />
endosperm.
78 GENETICALLY DETOXIFIED GRAINS<br />
<strong>of</strong> chromosome 1 at three homologous loci, named Gli-1. However, some w-gliadin<br />
peptides have been found to be encoded by additional dispersed genes located on the<br />
same arm <strong>of</strong> the same set <strong>of</strong> chromosomes. Genes controlling LMW glutenin subunits<br />
are clustered at Glu-A3, B3, and D3 loci and only the genes coding for HMW glutenin<br />
subunits occur on the long arm <strong>of</strong> the group 1 chromosomes, at a major locus named<br />
Glu-1. So, the multigene family nature <strong>of</strong> the wheat genes and the spread <strong>of</strong> these genes<br />
over six different chromosomes entail a very high degree <strong>of</strong> genetic polymorphism.<br />
By applying a Southern analysis to the common cultivar Cheyenne, Anderson et al.<br />
found that up to 150 genes code for a-gliadin, although only half <strong>of</strong> them are expressed<br />
12-13<br />
. An Italian study showed that there is a high degree <strong>of</strong> variability in the genomic<br />
DNA between different cultivars. A genetic polymorphism at the Gli-2 locus encoding<br />
14<br />
for a-gliadin was evident among different subspecies <strong>of</strong> Triticum aestivum .<br />
Naturally occurring detoxified grains<br />
This huge genetic variability let people hope to individuate a “naturally occurring”<br />
GDG. This was the case <strong>of</strong> the nullisomic 6A-tetrasomic 6D variety <strong>of</strong> Chinese Spring<br />
wheat, in which chromosome 6A is missing but compensated for by two extradoses <strong>of</strong><br />
chromosome 6D. Preliminary results were encouraging. The administration for two<br />
weeks <strong>of</strong> 65 grams <strong>of</strong> bread made with this wheat variety did not deteriorate absorptive<br />
15<br />
function . However, it was later proven that these variants do contain a-gliadin, coded<br />
by B and D chromosomes, and that they are toxic, on both histological and clinical<br />
16<br />
ground, for patients affected by CD .<br />
More recently, the toxicity <strong>of</strong> two lines <strong>of</strong> cultivar Raeder, one lacking the Gli-A2<br />
encoded gliadin components and the other lacking both Gli-A2 and Gli-D1 gliadin<br />
components was tested with an organ culture system based on <strong>coeliac</strong> duodenal biopsy<br />
17<br />
specimens . Although the Gli-A2 components were not compensated for by extradoses<br />
<strong>of</strong> chromosomes B and D, those lines were deficient but not devoid <strong>of</strong> gliadins.<br />
Although the toxicity <strong>of</strong> these two mutant lines was reduced compared to the original<br />
cultivar Raeder, yet it was still present. In conclusion, all these studies show that a<br />
naturally-occurring non-toxic line has not been found so far.<br />
Technologies to develop genetically detoxified grains<br />
Technologies allowing genetic plant transformation do exist. For example, a<br />
fragment <strong>of</strong> foreign DNA cut with a restriction enzyme, and plasmid, cut open with the<br />
same enzyme, are mixed together. DNA ligase is added to stitch the complementary<br />
base sequences so that the recombinant plasmid contains foreign DNA that, under<br />
appropriate conditions, is taken up by the Agrobacterium, a naturally occurring plant<br />
pathogen. When host plant cells are exposed to Agrobacterium, plasmid DNA is<br />
transferred into plant chromosomes. At the end <strong>of</strong> the process transgenic plants are<br />
18<br />
regenerated from single transformed cells (Fig. 3A) . An alternative method is the<br />
biolistic “gene gun technique”.<br />
A suspension <strong>of</strong> thousands <strong>of</strong> tiny gold or tungsten particles coated with transgenic<br />
DNA are fired into the target tissue, using compressed helium as propellant. Particles<br />
19<br />
penetrate the nucleus and incorporate into the host genoma (Fig. 3B) .
•<br />
•<br />
GENETICALLY DETOXIFIED GRAINS<br />
79<br />
Foreign DNA<br />
EcoR1<br />
DNA<br />
ligase<br />
Plasmid from<br />
Agrobacterium<br />
EcoR1<br />
Agrobacterium<br />
Recombinant plasmid<br />
containing foreign DNA<br />
•<br />
•<br />
Gene<br />
suspension<br />
Sheath<br />
fluid<br />
•<br />
Carbon<br />
dioxide<br />
3A<br />
Cultured cells<br />
from host plant<br />
Whole plants<br />
regenerated from<br />
single cells<br />
Plasmid DNA<br />
transferred into<br />
plant chromosomes<br />
A) agrobacterium technique B) gene gun technique<br />
Fig. 3. Genetic plant transformation technologies.<br />
Additionally, it may be possible to switch <strong>of</strong>f specific plant genes to eliminate or<br />
reduce natural toxins or allergens. This can take place both at posttranscriptional and<br />
transcriptional level. In the first case, which is the most common, injected doublestranded<br />
RNA is cut into small fragments <strong>of</strong> 20-30 nucleotides, amplified and then<br />
dissociated into single strands complementary, but in reverse to the target messenger<br />
RNA which is thus inactivated. In other words, silenced genes are still active but<br />
20<br />
messenger RNA is degraded before it can be translated into proteins .<br />
It should be kept in mind that these techniques have been applied to wheat only with<br />
the aim <strong>of</strong> improving dough rheological properties by increasing the level <strong>of</strong> high<br />
molecular weight glutenins, resulting in improved functional properties. Moreover,<br />
transformed plants show Mendelian segregation <strong>of</strong> the transgenes and strategies have<br />
21-24<br />
been developed to ensure transgene stability through generations . However, these<br />
techniques have not been directed to the treatment <strong>of</strong> CD so far.<br />
Genetically detoxified grains for <strong>coeliac</strong> <strong>disease</strong><br />
Petri dish with<br />
receiving cells<br />
Power source<br />
Electric<br />
field<br />
A project aiming at the production <strong>of</strong> a genetically detoxified wheat still suitable for<br />
mixing and baking should be set up taking into account a few points:<br />
(a) a minimal amount <strong>of</strong> gluten can be toxic to the <strong>coeliac</strong> small intestine;<br />
(b) all the different classes <strong>of</strong> gliadins have been shown to be harmful for <strong>coeliac</strong><br />
patients;<br />
(c) upwards 150 genes codify for the a-gliadins;<br />
(d) identification <strong>of</strong> all possible toxic sequences is still lacking;<br />
(e) bakery properties are mainly due to HMW glutenins.<br />
Obviously, the first thing to be checked is whether HMW glutenins are really safe<br />
8<br />
for CD patients. Despite the most recent findings on T cell assays , it should be noted<br />
that pure glutenins have not been tested on <strong>coeliac</strong> small bowel mucosa so far. So, once<br />
pure glutenins would be obtained, their safety should be tested first in-vitro and then in-<br />
3B
80 GENETICALLY DETOXIFIED GRAINS<br />
I STEP<br />
Production <strong>of</strong> HMW &<br />
LMW glutenins without any<br />
gliadin contamination<br />
III STEP<br />
Testing the rheologic<br />
functions <strong>of</strong> pure glutenins<br />
(in in vitro experiments) to<br />
confirm that elasticity is mainly<br />
ensured by them<br />
II STEP<br />
Testing HMW<br />
& LMW<br />
glutenin toxicity in in vitro<br />
& in vivo feeding studies<br />
IV STEP<br />
Integrating genes<br />
<strong>of</strong> HMW glutenins and<br />
promoters into maize<br />
by the biolistic method<br />
Fig. 4. A multistep approach to obtain genetically detoxified wheat suitable for baking.<br />
vivo on <strong>coeliac</strong> volunteers (Fig. 4). If the hypothesis <strong>of</strong> safety <strong>of</strong> HMW glutenins is<br />
confirmed, experiments should be planned to confirm the rheologic fractions <strong>of</strong> these<br />
pure fractions and that elasticity is mainly ensured by them. In that case viscous<br />
function could be maintained by proteins other than gliadins. Accordingly, the final step<br />
would be the introduction <strong>of</strong> HMW genes to improve baking quality in grains safe for<br />
CD patients, such as maize, rice and sorghum. This aim is not an easy one. However, it<br />
could be attempted in parallel with targeted inactivation <strong>of</strong> gliadins genes, a procedure<br />
requiring more preliminary information and less likely to lead to the production <strong>of</strong><br />
acceptable baked goods.<br />
Acknowledgements<br />
The authors are in debt with Dr. Donald D Kasarda (US Department <strong>of</strong> Agriculture,<br />
Agricultural Research Service, Albany, CA), Dr. Herbert Wieser (German Research<br />
Institute <strong>of</strong> Food Chemistry, Garching, Germany), Dr. Frederik W Janssen (Insp. <strong>of</strong><br />
Health Protection, Zutphen, The Netherlands), Dr. Rita Redaelli (Istituto Sperimentale<br />
per la Cerealicoltura, Bergamo, Italy) for their helpful suggestions and with<br />
<strong>Associazione</strong> <strong>Italiana</strong> Celiachia for financial support.<br />
References<br />
1. Wieser H. The precipitating factor in <strong>coeliac</strong> <strong>disease</strong>. Bailliere Clin Gastroenterol<br />
1995;9:191-207.<br />
2. Shewry PR, Tatham AS, Kasarda DD. Cereal proteins and <strong>coeliac</strong> <strong>disease</strong>. In: MN<br />
Marsh, ed. Coeliac <strong>disease</strong>. London: Blackwell Scientific 1992;305-48.
GENETICALLY DETOXIFIED GRAINS<br />
81<br />
3. Kasarda DD. Gluten and gliadin: precipitating factors in <strong>coeliac</strong> <strong>disease</strong>. In:<br />
Coeliac <strong>disease</strong>. Mäki M, Collin P, Visakorpi JK (eds). Proceedings <strong>of</strong> the Seventh<br />
International Symposium on Coeliac Disease. September 5-7, 1996, Tampere,<br />
Finland. Tampere: Coeliac Disease Study Group; 1997 pp. 91-9.<br />
4. Shewry PR, Tatham AS, Forde BG et al. The classification and nomenclature <strong>of</strong><br />
wheat gluten proteins: a reassessment. J Cereal Sci 1986;4:97-106.<br />
5. Wieser H, Seimeier W, Belitz H-D. Klassifizierung der Proteinkomponenten des<br />
Weizenklebers. Getreide Mehl Brot 1991;45:35-8.<br />
6. Kasarda DD. Glutenin structure in relation to wheat quality. In: Pomeranz Y, ed.<br />
Wheat is unique. St. Paul: AACC, 1989:277-302.<br />
7. Wieser H, Belitz H-D. Coeliac active peptides from gliadin: large-scale<br />
preparation and characterization. Zeitschrift für Lebensmittel-Untersuchung und-<br />
Forschung 1992;193:428-32.<br />
8. Vader W, Kooy Y, van Veelen P, de Ru A, Harris D, Benckhuijsen W. The gluten<br />
response in children with celiac <strong>disease</strong> is directed towards multiple gliadin and<br />
glutenin peptides. Gastroenterology 2002;122: 1729-37.<br />
9. Martucci S, Corazza GR. Spreading and focusing <strong>of</strong> gluten epitopes in celiac<br />
<strong>disease</strong>. Gastroenterology 2002;122:2072-5.<br />
10. Payne PI. Genetics <strong>of</strong> wheat storage proteins and the effect <strong>of</strong> allelic variation on<br />
bread-making quality. Ann Rev Plant Physiol 1987;38:141-53.<br />
11. Pogna N. Genetic improvement <strong>of</strong> plant for <strong>coeliac</strong> <strong>disease</strong>. Probiotics & Prebiotics<br />
New Foods, Rome: Università Urbaniana, 2001: 155-9.<br />
12. Anderson OD, Litts JC, Greene FC. The a-gliadin gene family. I. Characterization<br />
<strong>of</strong> ten new wheat a-gliadin genomic clones, evidence for limited sequence<br />
conservation <strong>of</strong> flanking DNA, and Southern analysis <strong>of</strong> the gene family. Theor Appl<br />
Genet 1997;95:50-8.<br />
13. Anderson OD, Greene FC. The a-gliadin gene family. II. DNA and protein sequence<br />
variation, subfamily structure, and origins <strong>of</strong> pseudogenes. Theor Appl Genet<br />
1997;95:59-65.<br />
14. D'Ovidio R, Tanzarella OA, Masci S, Lafiandra D, Porceddu E. RFLP and PCR<br />
analyses at Gli-1, Gli-2, Glu-1 and Glu-3 loci in cultivated and wild wheats.<br />
Hereditas 1992;116:79-85.<br />
15. Kasarda DD, Qualset CO, Mecham DK, Goodenberger DM, Strober W. A test <strong>of</strong><br />
toxicity <strong>of</strong> bread made from wheat lacking a-gliadin coded for by the 6A<br />
chromosome. In: Mc Nicholl B, Mc Carthy CF, Fottrell PF, eds. Perspective in<br />
celiac <strong>disease</strong>. Lancaster: MPT Press, 1978:55-61.<br />
16. Ciclitira PJ, Hunter JO, Lennox ES. Clinical testing <strong>of</strong> bread made from nullisomic<br />
6A wheats in <strong>coeliac</strong> patients. Lancet 1980;ii:234-6.<br />
17. Frisoni M, Corazza GR, Lafiandra D, De Ambrogio E, Filipponi C, Bonvicini F, et<br />
al. Wheat deficient in gliadins: promising tool for treatment <strong>of</strong> <strong>coeliac</strong> <strong>disease</strong>. Gut<br />
1995;36:375-8.<br />
18. Jones L. Genetically modified foods. BMJ 1999;318:581-4.<br />
19. Vasil V, Srivastava V, Castillo AM, Fromm ME, Vasil IK. Rapid production <strong>of</strong><br />
transgenic wheat plants by direct bombardment <strong>of</strong> cultured immature embryos. Biol<br />
Technology 1993;11:1553-8.<br />
20. Voinnet O, Pinto YM, Baulcombe DC. Suppression <strong>of</strong> gene silencing: a general
82 GENETICALLY DETOXIFIED GRAINS<br />
strategy used by diverse DNA and RNA viruses <strong>of</strong> plants. Proc Natl Acad Sci<br />
1999;96:14147-52.<br />
21. Blechl AE, Anderson OD. Expression <strong>of</strong> a novel high-molecular-weight glutenin<br />
subunit gene in transgenic wheat. Nat Biotechnol 1996;14:875-9.<br />
22. Barro F, Rooke L, Békés F, Gras P, Tatham AS, Fido R, et al. Transformation <strong>of</strong><br />
wheat with high molecular weight subunit genes results in improved functional<br />
properties. Nat Biotechnol 1997;15:1295-9.<br />
23. Altpeter F, Vasil V, Srivastava V, Vasil IK. Integration and expression <strong>of</strong> the highmolecular-weight<br />
glutenin subunit 1Ax1 gene into wheat. Nat Biotechnol<br />
1996;14:1155-9.<br />
24. Srivastava V, Anderson OD, Ow DW. Single-copy transgenic wheat generated<br />
through the resolution <strong>of</strong> complex integration patterns. Proc Natl Acad Sci. USA.<br />
1999;96:11117-21.
Catassi C, Fasano A, Corazza GR (eds):<br />
Primary <strong>prevention</strong> <strong>of</strong> <strong>coeliac</strong> <strong>disease</strong>. The<br />
utopia <strong>of</strong> the new millennium? Perspectives on<br />
Coeliac Disease, vol. 1, AIC Press, pp 83-88<br />
Immunotherapy <strong>of</strong> <strong>coeliac</strong> <strong>disease</strong>:<br />
where do we stand?<br />
1 1 1 1<br />
Carmen Gianfrani , Mauro Rossi , Giuseppe Mazzarella , Francesco Maurano ,<br />
2 2 2 2<br />
Virginia Salvati , Delia Zanzi , Salvatore Auricchio and Riccardo Troncone<br />
1 2<br />
Institute <strong>of</strong> Food Sciences and Technology, CNR, Avellino, Italy; Department <strong>of</strong> Pediatrics<br />
and European Laboratory for Food-Induced Disease, University Federico II, Naples, Italy<br />
Introduction<br />
Coeliac Disease (CD) is with little doubt an immune-mediated <strong>disease</strong>, triggered by<br />
the ingestion <strong>of</strong> wheat gliadin and related prolamines from other toxic cereal such as<br />
barley and rye. The hallmark <strong>of</strong> CD is the enteropathy characterized by an altered<br />
morphology <strong>of</strong> villous architecture and severe malabsorption, but it is now very clear<br />
1<br />
that the <strong>disease</strong> affects not only the small intestine .<br />
An important feature <strong>of</strong> CD is its strong genetic association with HLA class II genes:<br />
more than 90% <strong>of</strong> patients carry the HLA-DQA*0501/DQB*0201 (DQ2) alleles,<br />
whereas the majority <strong>of</strong> DQ2-negative patients are DQ8-positive<br />
2<br />
(DQA*0301/DQB*0302) . Among the non HLA genes that have been suggested to<br />
contribute to the CD susceptibility so far, only the CTLA4 gene has been found<br />
associated to <strong>coeliac</strong> <strong>disease</strong> in several populations examined. The strong genetic<br />
association with HLA molecules is strengthened by the finding that gliadin-derived<br />
peptides are recognized by <strong>coeliac</strong> intestinal lymphocytes when presented by the<br />
<strong>disease</strong> predisposing DQ2 or DQ8 molecules. In fact, from the immunological point <strong>of</strong><br />
view, it is now generally accepted that a recognition <strong>of</strong> gliadin peptides in association<br />
with HLA Class II molecules by Th1 T cells secreting proinflammatory cytokine leads<br />
3<br />
to the overt CD lesions at the intestinal level .<br />
CD, in the great majority <strong>of</strong> cases, is efficiently cured by the gluten-free diet;<br />
nevertheless, for some patients the diet is unpalatable and for others the compliance is<br />
quite poor. For these reasons a more acceptable form <strong>of</strong> therapy would be desirable:<br />
many efforts from our laboratory are focused on the development <strong>of</strong> conceptually<br />
amenable therapeutic strategies. In particular, considering that CD is an immune<br />
mediated pathology, any immunomodulatory strategy that could specifically block the<br />
adverse immune reactions triggered by gliadin, represents a valid alternative to the<br />
exclusion diet. Moreover, because the dietetic approach has a proven efficacy and<br />
safety, the immunomodulatory therapy must be strictly antigen-specific, not affecting<br />
the immune response to other antigens, and devoid <strong>of</strong> risks.<br />
83
84<br />
IMMUNOTHERAPY OF COELIAC DISEASE<br />
CD shares several immunological features with other less benign conditions, for<br />
example, insulin dependent diabetes or multiple sclerosis, for which<br />
immunomodulatory strategies have been studied and found to ameliorate the <strong>disease</strong>.<br />
When devising immunomodulatory strategies it is <strong>of</strong> fundamental importance to have<br />
systems where to test the success <strong>of</strong> the strategy implemented. Most <strong>of</strong> the attempts<br />
done so far have been realized using the in vitro organ culture system, which represents<br />
the only available tool since an animal model <strong>of</strong> CD is at moment still lacking.<br />
The organ culture system <strong>of</strong> the treated <strong>coeliac</strong> mucosa is an experimental system to<br />
explore the immunological events triggered by the contact <strong>of</strong> the antigen gliadin with<br />
the jejunal mucosa. Changes suggesting an activation <strong>of</strong> T cell immunity have been<br />
shown at the lamina propria level, including increased density <strong>of</strong> monuclear cells<br />
expressing IL2 receptor or enhanced expression <strong>of</strong> costimulatory molecules or<br />
adhesion molecules. The epithelium is also involved becoming infiltrated by<br />
4-5<br />
lymphocytes and expressing Fas molecules . As far as cytokines are concerned, a<br />
6<br />
strong enhancement <strong>of</strong> mRNA expression for g- interferon and IL2 has been observed .<br />
Block <strong>of</strong> costimulation<br />
B7/CD28 is one <strong>of</strong> major costimulatory pathways for the T cell activation providing<br />
important signals for complete T cell activation; in fact, as in the absence <strong>of</strong><br />
costimulation T cells become unresponsive (anergic), the blockage <strong>of</strong> CD28/B7<br />
7<br />
costimulation represents a potential target for immunotherapeutic strategies . In<br />
addition, the inhibition <strong>of</strong> costimulation has been reported to block specific antibody<br />
response, to prolong transplants survival and to inhibit animal model <strong>of</strong> autoimmune<br />
8<br />
<strong>disease</strong>s .<br />
CTLA4 (CD152) is a CD28 homologue that binds to CD80/CD86 with higher<br />
affinity. CTLA-4 is expressed on activated T cells and down-regulates T cell activation,<br />
9<br />
providing a feedback negative signal . Recently, Maiuri and co-workers observed that a<br />
fusion protein <strong>of</strong> CTLA-4 (CTLA-4-Ig) specifically blocked gliadin-induced immune<br />
10<br />
activation in the treated <strong>coeliac</strong> mucosa challenged with gliadin . They observed that<br />
the addition <strong>of</strong> CTLA4-Ig in the organ culture system <strong>of</strong> treated mucosa, had a clear<br />
effects on T cell activation in terms <strong>of</strong> decreased percentage <strong>of</strong> CD25 positive cells and<br />
reduced expression <strong>of</strong> ICAM-1 on mononuclear cells after 24 hours <strong>of</strong> culture.<br />
Interestingly, they found that almost 10% <strong>of</strong> lamina propria mononuclear cells showed<br />
apoptotic phenomena. Nonetheless, two other features, such as T cell infiltration and<br />
FAS expression by epithelial cells, were not affected. As a whole, these data suggest<br />
that not all phenomena triggered by gliadin in the mucosa are the result <strong>of</strong> T cell<br />
activation, and warn us that probably not everything may be modulated by affecting T<br />
cell activity.<br />
Gliadin peptides as tolerogens<br />
The identification <strong>of</strong> gliadin epitopes has a crucial importance to understand the<br />
mechanism leading to CD mucosal damage, but also to <strong>of</strong>fer an important tool for a<br />
strictly focused immunomodulatory strategy based on the modification <strong>of</strong> the structure<br />
<strong>of</strong> antigenic peptide. In fact, it has been reported that is possible to modulate the specific
IMMUNOTHERAPY OF COELIAC DISEASE<br />
85<br />
11<br />
immune response to antigenic peptide, altering the peptide structure . Peptides could<br />
be enginereed so that they would bind HLA molecules but not TCR, or bind TCR with<br />
the result <strong>of</strong> a switching from a proinflammatory Th1 to a Th2 or protective Th3<br />
12<br />
responses . Of course, the possibility <strong>of</strong> using peptides in immunotherapy and chances<br />
<strong>of</strong> success depend on the identification <strong>of</strong> immunodominat epitopes.<br />
Regarding CD, a number <strong>of</strong> gluten peptides have been implicated in the<br />
pathogenesis <strong>of</strong> the <strong>disease</strong>. At least five different antigenic peptides, three <strong>of</strong> them<br />
13-14 15 16<br />
obtained from a-gliadin , one from g-gliadin , and one from glutenin have been<br />
13-15 14-16<br />
identified so far. Three peptides are DQ2-restricted , two are DQ8-restricted . It is<br />
noteworthy to mention that the complexity <strong>of</strong> the gluten antigens, the variability <strong>of</strong> the<br />
responses <strong>of</strong> CD patients to the identified epitopes and the role <strong>of</strong> each peptide in the CD<br />
3<br />
pathogenesis make the available data difficult to interpret .<br />
Nevertheless, the possible therapeutic use <strong>of</strong> such peptides is hampered by many<br />
unsolved problems, that are not only technical, as the poor bioavailability <strong>of</strong> synthetic<br />
peptides and the choice <strong>of</strong> the administration route. First <strong>of</strong> all, it is still undefined the<br />
number <strong>of</strong> such epitopes: how many they are and which are the immunodominant ones.<br />
Moreover, among the different peptides it is also difficult to identify those which are<br />
primarily <strong>disease</strong> eliciting and those which are created by antigen spreading.<br />
Furthermore, it is possible that different groups <strong>of</strong> patients show different pattern <strong>of</strong><br />
reactivity. To this respect, differences have been hypothesized between adults and<br />
children with CD. Again, Dq8- and DQ2-positive <strong>coeliac</strong> patients may recognize<br />
different sets <strong>of</strong> peptides. We have recently examined in the organ culture system one <strong>of</strong><br />
14<br />
the epitopes characterized in Dr Koning's laboratory as one DQ8-restricted peptides .<br />
It was clearly recognized in vitro only by DQ8 positive <strong>coeliac</strong> patients. Biopsy<br />
fragments from DQ8 positive, but not from DQ2 positive <strong>coeliac</strong> patients, showed a<br />
significant increment <strong>of</strong> CD25 positive cells in the presence <strong>of</strong> such peptide, while both<br />
groups <strong>of</strong> patients reacted to the whole mixture <strong>of</strong> gliadin peptides. As a matter <strong>of</strong> fact,<br />
one <strong>of</strong> the problem with gliadin peptides is the posttranslational modifications they<br />
undergo. Although many evidences have been produced on the importance <strong>of</strong><br />
deamidation <strong>of</strong> some peptides by tissue transglutaminase, it remains to be defined the<br />
13,17<br />
extent <strong>of</strong> such phenomenon . Incidentally, we found that both native and deamidated<br />
18<br />
forms <strong>of</strong> the peptide were equally recognised .<br />
Finally, and this is probably the most important issue, it is still unclear if structures<br />
reacting with T cell receptors are really the ones which trigger the <strong>disease</strong>; in other term,<br />
the relationship between toxicity and immunogenicity is still to be clarified. As already<br />
mentioned, in vitro and in vivo challenge studies have pointed to peptides (e.g. A-<br />
gliadin 31-43 sequence), which instead have shown a scarce if any reactivity with<br />
mucosal T cells.<br />
IL10 and regulatory T cells<br />
Among cytokines with regulatory properties, there is no doubt that IL10 is a<br />
molecule with a strong immunomodulatory activity. IL10 is a potent immunoregulatory<br />
cytokine that has been found to suppress T cell-mediated immune response by either<br />
19<br />
inhibiting the expression <strong>of</strong> costimulatory molecules on antigen presenting cells or<br />
20<br />
directly inducing a long term unresponsiveness <strong>of</strong> specific T cells . Regarding the
86 IMMUNOTHERAPY OF COELIAC DISEASE<br />
hypothetical use <strong>of</strong> IL10 in the treatment <strong>of</strong> intestinal disorders, there are many<br />
evidences both in vitro, in the fetal organ culture system, and in vivo, in a mouse model<br />
<strong>of</strong> inflammatory colitis, that IL10 or cells producing it, such as Tr1 cells, are able to<br />
downregulate T cell activation and to control the pathogenic process. Moreover several<br />
reports showed that IL10 may have a central role in the development and homeostasis<br />
<strong>of</strong> gut associated immune system (GALT). We know that in the mucosa <strong>of</strong> untreated<br />
<strong>coeliac</strong> patients IL10 mRNA levels (and protein level) are higher than in controls, but<br />
they face, and cannot efficiently contrast, enormously higher levels <strong>of</strong> proinflammatory<br />
6<br />
cytokines as gamma interferon . Also the addition <strong>of</strong> further exogenous IL10 to the<br />
organ culture <strong>of</strong> biopsies from untreated <strong>coeliac</strong> patients fail to control the<br />
inflammatory process (Salvati et al, unpublished observations). Nonetheless, the<br />
addition <strong>of</strong> IL10 in the organ culture system <strong>of</strong> treated <strong>coeliac</strong> mucosa challenged with<br />
gliadin is able to downregulate the specific mucosal immune response to gliadin in<br />
terms <strong>of</strong> reduced densities <strong>of</strong> CD25+ cells, reduced expression <strong>of</strong> CD80/CD86<br />
21<br />
costimulatory molecules and <strong>of</strong> mRNA for inflammatory cytokines .<br />
Moreover, preliminary evidences show that the production <strong>of</strong> g-interferon upon<br />
gliadin stimulation is still absent 3 weeks later the isolation <strong>of</strong> T cells from biopsies<br />
cultured with gliadin in presence <strong>of</strong> IL10. Interestingly, the effect is partially reverted<br />
by the addition <strong>of</strong> anti-IL10 receptor and <strong>of</strong> anti-TGF b, this further suggesting the<br />
presence <strong>of</strong> an active suppressive mechanism, maybe mediated by regulatory T cells.<br />
In conclusion, our results showed that immunomodulation by IL10 on gliadin<br />
reactive T cells could be a consequence <strong>of</strong> downregulation <strong>of</strong> costimulatory molecules<br />
but also suggest that IL10 may operate through induction <strong>of</strong> Tr1 cells and inhibits the<br />
migration into the intestine <strong>of</strong> pathogenic Th1 cells. Given that, the induction or the<br />
expansion <strong>of</strong> specific T regulatory cells remains one <strong>of</strong> the possible<br />
immunomodulatory strategies to implement in CD.<br />
Mucosal tolerance<br />
A very efficient route to induce tolerance to a specific antigen is the intravenous<br />
administration, but the induction <strong>of</strong> tolerance via mucosae is a strategy more <strong>of</strong>ten<br />
implemented in the experimental therapy <strong>of</strong> autoimmune <strong>disease</strong>s. Nevertheless, in<br />
CD, being the small intestine the target <strong>of</strong> the <strong>disease</strong>, mucosae other than those <strong>of</strong> the<br />
small intestine are candidate to elicit mucosal tolerance. Despite its peculiar<br />
physicochemical properties, gliadin has been shown to be a good oral tolerogen.<br />
We studied the potential for tolerance induction in gluten-free diet Balb/c mice by<br />
intranasal administration <strong>of</strong> whole antigen, as it has been demonstrated that this<br />
22<br />
strategy is effective in a variety <strong>of</strong> different experimental systems . Our results showed<br />
that intranasal administration <strong>of</strong> native gliadin before immunization abrogated the<br />
specific T cell response. Moreover, a marked decrease in g-interferon and IL-2 levels,<br />
and normal levels <strong>of</strong> IL-4 expression were detected, suggesting that intranasal<br />
23<br />
administration <strong>of</strong> gliadin can induce tolerance in Th1-cells . These data were produced<br />
in mice parenterally immunized with gliadin: it is a model quite far from CD, but yet it<br />
<strong>of</strong>fers a series <strong>of</strong> questions, in particular concerning the ability <strong>of</strong> the nasal<br />
administration <strong>of</strong> antigen to tolerate also gut T responses and to control a Th1 mediated<br />
enteropathy.
IMMUNOTHERAPY OF COELIAC DISEASE<br />
87<br />
In conclusion, CD has a strong T component that renders it susceptible <strong>of</strong><br />
immunomodulation. There are still a number <strong>of</strong> significant theoretical problems to be<br />
solved, first <strong>of</strong> all the relevance <strong>of</strong> the non-T pathogenetic component. In any case the<br />
strategy eventually chosen must be really "competitive" with the safety <strong>of</strong> the glutenfree<br />
diet.<br />
Acknowledgements<br />
Most <strong>of</strong> the studies reported in this paper have been carried out with financial<br />
support from the commission <strong>of</strong> the European Communities, specific RTD programme<br />
"Quality <strong>of</strong> Life and Management <strong>of</strong> Living Resources", QLK1-CT-1999-00037,<br />
Evaluation <strong>of</strong> the prevalence <strong>of</strong> <strong>coeliac</strong> <strong>disease</strong> and its genetic components in the<br />
European population.<br />
References<br />
1. Auricchio S, Troncone R, Maurano F. Coeliac <strong>disease</strong> in the year 2000. Ital J<br />
Gastroenterol Hepatol 1999; 31: 773-80.<br />
2. Kagn<strong>of</strong>f, MF. HLA genes in Coeliac Disease. In: Auricchio S, Greco L, Maiuri<br />
L, Troncone R, eds. Coeliac <strong>disease</strong>. Naples: Jean Gilder Editions, 2000; 5-14.<br />
3. Sollid LM. Molecular basis <strong>of</strong> <strong>coeliac</strong> <strong>disease</strong>. Ann Rev Immunol 2000; 18: 53-<br />
81.<br />
4. Maiuri L, Picarelli A, Boirivant M, Coletta S, Mazzilli MC, De Vincenzi M, et al.<br />
Definition <strong>of</strong> the initial immunologic modification upon in vitro gliadin challenge<br />
in the small intestine <strong>of</strong> celiac patients. Gastroenterology 1996; 110: 1368-78.<br />
5. Maiuri L, Ciacci C, Raia V, Vacca L, Ricciardelli I, Raimondi F, et al. FAS<br />
engagement drives apoptosis <strong>of</strong> enterocytes <strong>of</strong> <strong>coeliac</strong> patients.Gut 2001; 48:<br />
418-24.<br />
6. Salvati VM, Troncone R, Mazzarella G, et al. High levels <strong>of</strong> IFN-gmRNA in<br />
untreated celaics and in treated mucosa in vitro cultured with gliadin. Ital J<br />
Gastroenterol Hepatol 1999; 31: 559.<br />
7. Bluestone JA. New perspective <strong>of</strong> CD28/B7-mediated T cell costimulation.<br />
Immunity 1995; 2: 555.<br />
8. Levisetti MG, Padrid PA, Szot GL, Mittal N, Meehan SM, Wardrip CL, et al.<br />
Immunosuppressive effect <strong>of</strong> human CTLA4Ig in a nonhuman primate model <strong>of</strong><br />
allogeneic pancreatic islet transplantation. J Immunol 1997; 159: 5187.<br />
9. Lenshow DY, Zeng J, Thistlethwaite JR, Montag A, Brady W, Gibson M, et al.<br />
Long term survival <strong>of</strong> xenogeneic pancreatic islet grafts induced by CTLA4Ig.<br />
Science 1992; 257: 789.<br />
10. Maiuri L, Auricchio S, Coletta S, De Marco G, Picarelli S, Di Tola M, et al.<br />
Blockage <strong>of</strong> T cell costimulation inhibits T-cell action in celiac <strong>disease</strong>.<br />
Gastroenterology 1998; 115: 564-72.<br />
11. Whindhagen A, Scholz C, Hollsberg P, Fukaura H, Sette A, DA Hafler.<br />
Modulation <strong>of</strong> cytokine patterns <strong>of</strong> human autoreactive T cell clones by a single<br />
aminoacid substitution <strong>of</strong> their peptide ligand. Immunity 1995; 2: 373.<br />
12. De Magistris MT, Alexander J, Coggeshall M, Altman A, Gaeta F, Grey HM, et
88 IMMUNOTHERAPY OF COELIAC DISEASE<br />
al. Antigen analog-major histocompatibily complexes act as antagonist <strong>of</strong> the T<br />
cell receptor. Cell 1992; 68: 625.<br />
13. Arentz-Hansen H, Korner R, Molberg O, Quarsten H, Vader W, Kooy Y, et al.<br />
The intestinal T cell response to a-gliadin in adult celiac <strong>disease</strong> is focused on a<br />
single deamidated glutamine targeted by tissue transglutaminase. J Exp Med<br />
2000; 191: 603-12.<br />
14. van de Wal Y, Kooy Y, van Veelen PA, Pena SA, Mearin ML, Molberg O, et al.<br />
Small intestinal T cells <strong>of</strong> celiac <strong>disease</strong> patients recognize a natural pepsin<br />
fragment <strong>of</strong> gliadin. Proc Natl Acad Sci U S A 1998; 95: 10050-4.<br />
15. Sjostrom H, Lundin K, Molberg O, Korner R, McAdam S, Anthonsen D, et al.<br />
Identification <strong>of</strong> a gliadin T-cell epitope in <strong>coeliac</strong> <strong>disease</strong>: general importance<br />
<strong>of</strong> gliadin deamidation for intestinal T-cell recognition. Scand J Immunol 1998;<br />
48: 111-5.<br />
16. van de Wal Y. Kooy Y. van Veelen P.A. Vader W. August SA. Drijfhout J. Pena<br />
S.A. Koning F. Glutenin is involved in the gluten-driven mucosal T cell response.<br />
Eur J Immunol 1999; 29: 3133-39.<br />
17. Molberg O, McAdam S, Lundin KEA, Kristiansen C, Arentz-Hansen H, Kett K, et<br />
al. T cell from <strong>coeliac</strong> <strong>disease</strong> lesions recognize gliadin epitopes deamidated in<br />
situ by endogenous tissue transglutaminase. Eur J Immunol 2001; 31: 1317-23.<br />
18. Mazzarella G, Maglio M, Paparo F, Tardone G, Stefanile R, Greco L, et al. An<br />
immunodominant DQ8-restricted gliadin peptide activates small intestinal<br />
immune response in in vitro cultured treated <strong>coeliac</strong> mucosa. J Pediatr<br />
Gastroenterol Nutr 2000; 31: S18.<br />
19. de Waal Malefyt R, Haanen J, Spits H, Roncarlo MG, te Velde A, Figdor C, et al.<br />
Interleukin 10 (IL-10) and viral IL-10 strongly reduce antigen-specific human T<br />
cell proliferation by diminishing the antigen-presenting capacity <strong>of</strong> monocytes<br />
via downregulation <strong>of</strong> class-II major histocompatibilty complex expression. J<br />
Exp Med 1991; 174: 915-24.<br />
20. Groux H, Bigler M, de Vries J, Roncarolo MG. Interleukin-10 induces a longterm<br />
antigen specific anergic state in human CD4+ T cells. J Exp Med 1996;<br />
184: 19-29.<br />
21. Salvati V, Troncone R, Mazzarella G, Stefanile R, Borrelli M, Riccio F, et al.<br />
Recombinant IL-10 down-regulates T-Cell activation and mRNA expression <strong>of</strong><br />
proinflammatory cytokines in treated celiac mucosa in vitro cultured with<br />
gliadin. Scand J Immunol 2000; 4: 438 C25.<br />
22. Myers LK, Seyer JM, Stuart JM, Kang AH. Suppression <strong>of</strong> murine collageninduced<br />
arthritis by nasal administration <strong>of</strong> collagen. Immunology 1997; 90:<br />
161-4.<br />
23. Rossi M, Maurano F, Caputo N, Auricchio S, Sette A, Capparelli R, et al.<br />
Intravenous or intranasal administration <strong>of</strong> gliadin is able to down-regulate the<br />
specific immune response in mice. Scand J Immunol 1999; 50: 177-82.
Catassi C, Fasano A, Corazza GR (eds):<br />
Primary <strong>prevention</strong> <strong>of</strong> <strong>coeliac</strong> <strong>disease</strong>. The<br />
utopia <strong>of</strong> the new millennium? Perspectives on<br />
Coeliac Disease, vol. 1, AIC Press, pp 89-92<br />
The most recent advances on gluten<br />
toxicity in <strong>coeliac</strong> <strong>disease</strong><br />
1 2 3<br />
Gino Roberto Corazza , Carlo Catassi , Alessio Fasano<br />
1<br />
Department <strong>of</strong> Gastroenterology, University <strong>of</strong> Pavia, Italy;<br />
2<br />
Department <strong>of</strong> Pediatrics, University<br />
3<br />
<strong>of</strong> Ancona, Italy; Division <strong>of</strong> Pediatric Gastroenterology, Center for Celiac Research, University<br />
<strong>of</strong> Maryland, Baltimore, MD, USA<br />
After the Pavia meeting held on October 12, 2001, significant advances on the<br />
possibilities <strong>of</strong> a <strong>primary</strong> <strong>prevention</strong> <strong>of</strong> <strong>coeliac</strong> <strong>disease</strong> have been achieved. While a part<br />
<strong>of</strong> these have been recently published, most issues were discussed at the 10th<br />
International Symposium on Coeliac Disease held at the Pasteur Institute in Paris, last<br />
June.<br />
The majority <strong>of</strong> these works deals with a further characterization <strong>of</strong> the gluten<br />
peptides that trigger a T cell response. Although it is worth reminding that T cell<br />
activation does not always mirror gluten toxicity in vitro or in vivo, the reportoire <strong>of</strong><br />
gluten peptides that are able to induce T cell activation seems now wider and more<br />
heterogenous than reported at the Pavia meeting. At that time two different groups<br />
found that a region <strong>of</strong> a-gliadin corresponding to aminoacids 57-75 acted as powerful,<br />
immunodominant epitope if a glutamine residue (Q65) was deamidated by tissue<br />
1-2<br />
transglutaminase (tTG) to glutamic acid . Those findings disclosed new exciting<br />
perspectives on possible alternatives for the treatment <strong>of</strong> <strong>coeliac</strong> <strong>disease</strong>, such as the<br />
achievement <strong>of</strong> a non-toxic wheat by removal or modification <strong>of</strong> the above mentioned<br />
antigenic sequences or specific immune therapy to induce oral tolerance.<br />
Looking at the T cell pr<strong>of</strong>ile in <strong>coeliac</strong> children with recent onset <strong>of</strong> <strong>disease</strong>,<br />
3<br />
Koning's group found that 6 novel additional gliadin and glutenin peptides were able<br />
to induce T cell responses in the early phase <strong>of</strong> the pathogenesis <strong>of</strong> this condition. The<br />
observation that immune activation was at some extent independent <strong>of</strong> deamidation<br />
indicated that T cell responses can also be initiated by native gluten peptides. On the<br />
basis <strong>of</strong> their results they estimated that gluten may contain up to 50 T-cell antigenic<br />
peptide sequences (gliadin plus glutenin). No doubt that these results weakened the<br />
4<br />
expectations for new therapeutic approaches for this condition . In particular, as far as<br />
the production <strong>of</strong> genetically detoxified grains is concerned, to the technical difficulties<br />
listed by Biagi et al (pp 75-82 <strong>of</strong> this volume), the demonstration that glutenin peptides<br />
are able to induce T-cell activation in <strong>coeliac</strong> <strong>disease</strong> makes the suggestion <strong>of</strong><br />
introducing high molecular weight glutenin genes to improve baking quality <strong>of</strong> maize<br />
no longer tenable. On the other side, the observation that the number <strong>of</strong> peptides<br />
89
90<br />
RECENT ADVANCES ON GLUTEN TOXICITY<br />
involved in the pathogenesis <strong>of</strong> <strong>coeliac</strong> <strong>disease</strong> is higher than previously thought further<br />
reduces the technical feasibility <strong>of</strong> targeted inactivation <strong>of</strong> gliadins (and glutenins)<br />
genes.<br />
The most recent results <strong>of</strong> the Sollid's group are on the same line <strong>of</strong> Koning. Even in<br />
adults, DQ2-restricted mucosal T-cells recognize an additional a-gliadin epitope and<br />
several new g-gliadin peptides, confirming also that deamidation is not an absolute<br />
prerequisite for T-cell activation. Interestingly the new and the previously identified<br />
peptides are not randomly scattered accross gliadin molecules but cluster in regions <strong>of</strong><br />
5<br />
the proteins with a high content <strong>of</strong> proline residues .<br />
In apparent contrast with these recent studies indicating a wide array <strong>of</strong> a,/g-gliadin<br />
and glutenin peptides playing a complementary role in <strong>coeliac</strong> <strong>disease</strong> activation, a<br />
6<br />
recent study identified a 33-mer peptide having several characteristics suggesting it is<br />
the <strong>primary</strong> initiator <strong>of</strong> the inflammatory response in this condition. First <strong>of</strong> all, the 33-<br />
mer peptide appeared to be stable toward digestion by gastric, pancreatic and brushborder<br />
proteases. Secondly, it reacted with tTG with substantially greater selectivity<br />
than known natural substrates <strong>of</strong> the enzime. Finally, it turned out to be a potent inducer<br />
<strong>of</strong> gut-derived <strong>coeliac</strong> T-cell lines and its homologs were absent in cereal that are not<br />
toxic for <strong>coeliac</strong> patients. Besides these important features, the aminoacid sequence <strong>of</strong><br />
the peptide included the residues 57-89 <strong>of</strong> a-gliadin, largely overlapping with the 57-68<br />
1 2<br />
and the 62-75 Arentz-Hansen and the Anderson 57-73 peptides. In addition it should<br />
be noted that the 33-mer peptide is particularly rich in proline residues (n=13) and that<br />
its exposure to a bacterial prolyl-endopeptidase catalyzes the breakdown <strong>of</strong> the peptide<br />
diminishing its toxic effect. Should the 33-mer peptide be the dominant epitope in<br />
<strong>coeliac</strong> <strong>disease</strong>, this would <strong>of</strong>fer a possible strategy for oral peptidase supplement<br />
therapy for the treatment <strong>of</strong> this condition.<br />
The apparent discrepancy between multiple and a single toxic peptide in the<br />
7<br />
pathogenesis <strong>of</strong> <strong>coeliac</strong> <strong>disease</strong> has been addressed in a recent editorial . It has been<br />
hypothesized a multi-step sequence in which, in an early phase, T-cell response is<br />
directed to a wide array <strong>of</strong> native gluten (glutenin plus gliadin) epitopes as a<br />
consequence <strong>of</strong> an epitope spreading due to the ubiquitous presence <strong>of</strong> the same highly<br />
repetitive sequence. In a more advanced phase the immune response becomes polarized<br />
to an immunodominant peptide (the 33-mer ?) as a consequence <strong>of</strong> an epitope focusing<br />
catalized by tTG increasingly released from the tissue lesions.<br />
It should be underlined that this view does not preclude a selective immunotherapy.<br />
Several lines <strong>of</strong> evidence suggest that the <strong>primary</strong> problem is understanding the<br />
hierarchy <strong>of</strong> epitope spreading in <strong>coeliac</strong> <strong>disease</strong>, since in other animal and <strong>disease</strong><br />
models it has been shown that immunodominant T-cell epitopes behave as potent<br />
8<br />
tolerogens when ingested by alternative routes and that this process may induce<br />
tolerance to the whole antigenic molecule in a mechanism <strong>of</strong> intramolecular epitope<br />
9<br />
suppression . Alternative strategies may be represented by DNA vaccines based on the<br />
10<br />
construction <strong>of</strong> plasmids containing multiple epitopes and by the use <strong>of</strong> antigen<br />
presenting cells engineered to present both the dominant gluten peptide and the FAS<br />
11<br />
ligand molecule to target and kill FAS positive antigen-specific <strong>coeliac</strong> T-cells .<br />
Toxic peptides must reach the sub-epithelial environment to exert their pathogenic<br />
role. At the Paris meeting new data have been presented on the interaction between
RECENT ADVANCES ON GLUTEN TOXICITY<br />
91<br />
gliadin and the intestinal mucosa leading to functional changes <strong>of</strong> the gut barrier<br />
function. Zonulin represents a novel eukaryotic protein that reversibly opens intestinal<br />
12<br />
tight junctions (tj) . It has been recently demonstrated that zonulin expression is<br />
13<br />
increased during the early stage <strong>of</strong> CD , suggesting that the reported opening <strong>of</strong> tj at the<br />
early stage <strong>of</strong> the <strong>disease</strong> could be mediated by zonulin.<br />
Recent studies indicate that gliadin activates the zonulin-signaling pathway both in<br />
14<br />
normal and celiac <strong>disease</strong>-derived intestinal tissues . In normal intestinal epithelial<br />
cells in vitro, the cellular response to gliadin was observed only a few minutes after<br />
incubation and was characterized by a zonulin-dependent cytoskeleton reorganization<br />
with a redistribution <strong>of</strong> actin filaments mainly in the intracellular subcortical<br />
14<br />
compartment . Spectr<strong>of</strong>luorimetry experiments revealed that such cytoskeleton<br />
reorganization was associated to an increment <strong>of</strong> F-actin amount secondary to an<br />
increased rate <strong>of</strong> intracellular actin polymerization. Experiments performed in Ussing<br />
chambers showed that the addition <strong>of</strong> gliadin peptides to the intestinal mucosa in vitro<br />
causes in a few minutes a significant increased <strong>of</strong> intestinal permeability mediated by<br />
zonulin. Considering the results <strong>of</strong> this study and preliminary data generated by using<br />
15<br />
intestinal tissues from both celiac patients in remission and healthy controls , it is<br />
conceivable to hypothesize a possible gliadin mechanism <strong>of</strong> action leading to zonulinmediated<br />
increase in actin polymerization and intestinal permeability. These new<br />
findings lead to innovative lines <strong>of</strong> research possibly relevant for the <strong>prevention</strong> and<br />
treatment <strong>of</strong> the <strong>disease</strong>.<br />
References<br />
1. Arentz-Hansen H, Korner R, Molberg O, Quarsten H, Vader W, Kooy YMC, et<br />
al. The intestinal T cell response in adult <strong>coeliac</strong> <strong>disease</strong> is focused on a single<br />
deamidated glutamine targeted by tissue transglutaminase. J Exp Med 2000;<br />
191: 603-12.<br />
2. Anderson RP, Degano P, Godkin AJ, Jewell DP, Hill AVS. In vivo antigen<br />
challenge in <strong>coeliac</strong> <strong>disease</strong> identifies a single transglutaminase-modified<br />
peptide as the dominant A-gliadin T cell epitome. Nat Med 2000; 6: 37-42.<br />
3. Vader W, Kooy Y, van Veelen P, de Ru A, Harris D, Benckhuijsen W, et al The<br />
gluten response in children with recent onset celiac <strong>disease</strong>. A highly diverse<br />
response towards multiple gliadin and glutenin peptides. Gastroenterology 2002;<br />
122: 1729-37.<br />
4. Kagn<strong>of</strong>f MF. Coeliac <strong>disease</strong> pathogenesis: the plot thickens. Gastroenterology<br />
2002; 123: 39-43.<br />
5. Arentz-Hansen H, Mcadam SN, Molberg O, Fleckenstein B, Lundin KEA,<br />
Jorgensen TJD, et al. Celiac lesion T cells recognize epitopes that cluster in<br />
regions <strong>of</strong> gliadins rich in proline residues. Gastroenterology 2002;123: 803-9.<br />
6. Shan L, Molberg O, Parrot I, Hausch F, Filiz F, Gray GM, et al. Structural basis<br />
for gluten intolerance in celiac sprue. Science 202; 297: 2275-9.<br />
7. Martucci S, Corazza GR. Spreading and focusing <strong>of</strong> gluten epitopes in celiac<br />
<strong>disease</strong>. Gastroenterology 2002; 122: 2072-5.<br />
8. Hoyne GF, O'Henir, Wraith DC, Thomas WR, Lamb JR. Inhibition <strong>of</strong> T cell and<br />
antibody response s to house dust mite allergen by inhalation <strong>of</strong> the dominant T
92 RECENT ADVANCES ON GLUTEN TOXICITY<br />
cell epitope in naïve and sensitized mice. J Exp Med 1993; 178: 1783-8.<br />
9. Hoyne GF, Jamicki AG, Thomas WR, Lamb JR. Characterization <strong>of</strong> the<br />
specificity and duration <strong>of</strong> T cell tolerance to intranasally administered peptides<br />
in mice: a role for intramolecular epitope suppression. Int Immunol 1997; 9:<br />
1165-73.<br />
10. Steinman L. Despite epitope spreading in the pathogenesis <strong>of</strong> autoimmune<br />
<strong>disease</strong>, highly restricted approaches to immune therapy may still succeed (with<br />
a edge on this bet). J Autoimmun 2000; 14: 278-82.<br />
11. Wu B, Wu J-M, Miagkov A, Adams RN, Levitsky HI, Drachman DB. Specific<br />
immunotherapy by genetically engineered APCs: the "guided missile" strategy. J<br />
Immunol 2001; 166: 4773-9.<br />
12. Wang W, Uzzau S, Goldblum SE, et al. Human zonulin, a potential modulator <strong>of</strong><br />
intestinal tight junctions. J Cell Sci 2000; 113: 24, 4435-44.<br />
13. Fasano A, Not T, Wang W, et al. Zonulin, a newly discovered modulator <strong>of</strong><br />
intestinal permeability, and its expression in <strong>coeliac</strong> <strong>disease</strong>. Lancet 2000;<br />
355:1518-1519.<br />
14. Clemente MG, De Virgiliis S, Kang JS, Macatagney R, Congia M, Fasano A.<br />
New insights on celiac <strong>disease</strong> pathogenesis: gliadin-induced zonulin release,<br />
actin polymerization, and early increased gut permeability. Gut (in press).<br />
15. Drago S, DiPierro M, Giambelluca D, Iacono G, Catassi C, Fasano A. Gliadin<br />
induces occludin down-regulation and tight junctions (tj) disassembly in human<br />
intestine. 10th International Symposium on Coeliac Disease Paris (France),<br />
June 2-5, 2002.
Index<br />
A<br />
Antiendomysium antibodies (EMA), 33-37<br />
Antigen<br />
presenting cells, 3, 17-18, 67<br />
specific T cells, 18, 90<br />
-specific therapies, 17<br />
B<br />
Barley, 1, 23-24, 27, 31, 43, 53, 75, 83<br />
B cell, 17-18, 62<br />
Breast feeding, 46-48<br />
C<br />
Cytokines, 6, 17-19, 68<br />
IL-10, 68, 85-86<br />
interferon gamma (IFNγ), 6, 18, 21, 48,<br />
68, 86<br />
TGF-β1, 48<br />
Th1 associated, 19<br />
Th1-like, 17<br />
tumour necrosis factor (TNF), 6, 18<br />
D<br />
Deamidation, 4-5, 14, 19, 90<br />
Dendritic cells, 17, 67-68<br />
Detoxified grains, 78-79, 89<br />
E<br />
Environmental factors<br />
gut infections, 3<br />
Infant feeding, 45, 52, 54, 56<br />
role <strong>of</strong>, 36-37, 43<br />
Epidemic <strong>of</strong> <strong>coeliac</strong> <strong>disease</strong>, 44-45, 52, 54<br />
Epitope, 4-7, 14, 22, 24, 84, 90<br />
dominant, 90<br />
hierarchies, 20-21, 90<br />
toxic, 28<br />
Extracellular matrix degeneration, 6<br />
F<br />
Familial clustering, 31-32, 35, 43<br />
G<br />
Genetic predisposition, 36, 61<br />
CTLA4, 2, 83-84<br />
DQ2, 2-4, 6-7, 13, 17, 28, 32, 37, 44, 61,<br />
83, 85<br />
DQ7, 2-3<br />
DQ8, 2-4, 6-7, 13, 28, 32, 44, 61, 83, 85<br />
DR3, 2-3, 35-37<br />
DR4, 2-3<br />
DR5, 2-3<br />
DR7, 2-3<br />
5qter, 2<br />
11qter, 2<br />
Gliadin, 1, 4, 75-77, 91<br />
A-gliadin, 19-23, 25, 27-28, 89<br />
31-49, 28<br />
57-73 QE65, 22-24, 90<br />
57-68, 90<br />
57-89, 90<br />
62-75, 90<br />
deamidation <strong>of</strong>, 19<br />
epitopes, 84, 90<br />
HLA-DQ2 restricted, 22, 24<br />
fractions, 27-28<br />
toxicity, 28<br />
genes, 90<br />
intranasal administration, 86<br />
peptides, 28, 91<br />
Gluten, 1, 3-4, 6, 17, 43-44, 48, 51, 54, 61,<br />
64, 67, 75<br />
age at introduction <strong>of</strong>, 49<br />
amount <strong>of</strong>, 47-49, 54, 56<br />
challenge, 18, 21, 25<br />
-containing cereals<br />
consumption <strong>of</strong>, 48<br />
genetic modification <strong>of</strong>, 56<br />
intake, 52<br />
consumption <strong>of</strong>, 48<br />
deamidation, 4<br />
-derived peptides, 3<br />
epitopes, 4-7, 14<br />
free diet, 7, 17-18, 21, 61, 83<br />
immune tolerance <strong>of</strong>, 64<br />
in follow-on formula, 48<br />
in the Saharawi's diet, 37<br />
intolerance, 65<br />
native, 90<br />
peptides, 4, 37, 85, 89<br />
deamidation, 5, 13-14<br />
dominant, 90<br />
immune tolerance to, 56<br />
"toxic", 19<br />
33-mer, 90<br />
proteins, 4<br />
high-molecular weight, 76<br />
medium-molecular weight, 76<br />
93
94<br />
INDEX<br />
low-molecular weight, 76<br />
functional properties <strong>of</strong>, 76<br />
specific response<br />
in children, 13<br />
in adults, 14<br />
toxicity, 89<br />
-specific memory T cells, 20<br />
Glutenin, 1, 4, 27, 75-77, 89-90<br />
Gut barrier, 91<br />
H<br />
HLA genes - see genetic predisposition<br />
I<br />
Immunotherapy, 83-88, 90<br />
Infant feeding, 45, 52-54<br />
Insulin dependent diabetes mellitus (IDDM)<br />
risk, 44<br />
Intestinal mucosa, 91<br />
Intraepithelial lymphocytes (IELs), 6, 67<br />
γδ, 6<br />
M<br />
Mucosal immune<br />
response<br />
control <strong>of</strong>, 65-69<br />
system, 63, 66<br />
tolerance, 69-70<br />
N<br />
Non-HLA genes, 32, 44<br />
O<br />
Oats, 27, 53<br />
Organ culture, 6, 28, 84-85<br />
P<br />
Pathophysiology <strong>of</strong> <strong>coeliac</strong> <strong>disease</strong>, 6, 43,<br />
69, 90<br />
Aetiology, 1, 17, 43<br />
multifactorial, 51<br />
Prevalence <strong>of</strong> <strong>coeliac</strong> <strong>disease</strong>, 1, 33<br />
in the general pediatric population, 1, 36<br />
in the Saharawi, 33, 37<br />
in the Sardinians, 37<br />
in family members, 1, 43<br />
Primary <strong>prevention</strong>, 43, 56, 89<br />
R<br />
Risk factors, 31-32<br />
associated, 51<br />
component causal, 51<br />
necessary causal, 51<br />
contributing, 50<br />
infections, 50<br />
socio-economic background, 50<br />
Rye, 1, 23-24, 27, 43, 53, 75<br />
S<br />
Saharawi population, 33-37<br />
Small intestinal biopsy, 33, 37<br />
Susceptibility haplotype, 37<br />
T<br />
T cell, 2-4, 7, 62, 64. 90<br />
activation, 6, 13, 17, 62, 89-90<br />
antigen specific, 18<br />
CD4, 17-19, 21<br />
CD4+ TCRαβ, 2-3, 6-7<br />
CD8, 17<br />
clones, 5, 14<br />
intestinal, 19, 22<br />
peripheral blood, 19<br />
delayed-type hypersensitivity, 61<br />
DQ2-restricted, 90<br />
epitope, 7, 17, 19<br />
dominant, 24<br />
gliadin-specific, 19<br />
hierarchy, 21<br />
gluten reactive, 3<br />
helper, 67<br />
gliadin-specific, 21<br />
receptor, 17<br />
regulatory, 63, 68, 85<br />
response, 14, 89-90<br />
suppressor, 63<br />
Th1, 83<br />
tolerance, 68<br />
TGF-β, 68<br />
Tissue transglutaminase (tTG), 4, 6-7, 13,<br />
19, 37, 90<br />
activity, 4-5<br />
antibodies, 6-7<br />
Tolerance, 61-63, 90<br />
central, 62<br />
immune, 56, 62<br />
mucosal immune, 69, 86-87<br />
oral, 5, 7, 13, 44, 46, 48, 64-65, 67-68, 70<br />
experimental models <strong>of</strong>, 65<br />
peripheral, 62<br />
Treated <strong>coeliac</strong> <strong>disease</strong>, 18<br />
Twins, 1, 31, 43<br />
V<br />
Vaccine, 17, 56, 65, 90
INDEX 95<br />
W<br />
Wheat, 7, 23, 27, 31, 53, 75, 83<br />
and gluten, 1<br />
flour proteins, 27<br />
gliadin, 83<br />
protein, 75<br />
genetic <strong>of</strong>, 77-78<br />
gliadins, 75, 77<br />
glutenins, 75, 77<br />
starch, 27<br />
Z<br />
Zonulin, 91