Breast Discharge: Ultrasound and Doppler Evaluation - NCI
Breast Discharge: Ultrasound and Doppler Evaluation - NCI
Breast Discharge: Ultrasound and Doppler Evaluation - NCI
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
268<br />
Soha T. Hamed, et al.<br />
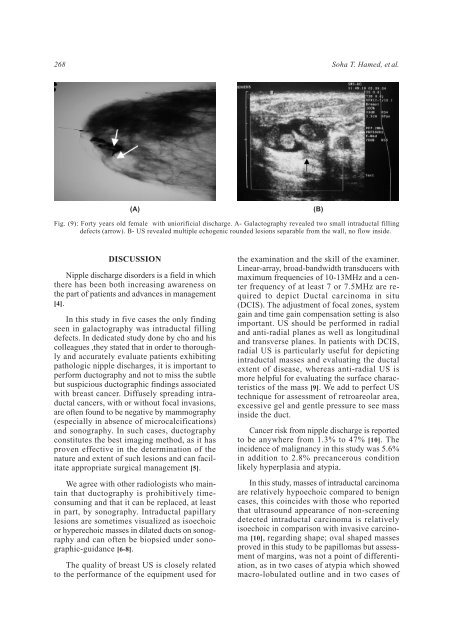
(A)<br />
(B)<br />
Fig. (9): Forty years old female with uniorificial discharge. A- Galactography revealed two small intraductal filling<br />
defects (arrow). B- US revealed multiple echogenic rounded lesions separable from the wall, no flow inside.<br />
DISCUSSION<br />
Nipple discharge disorders is a field in which<br />
there has been both increasing awareness on<br />
the part of patients <strong>and</strong> advances in management<br />
[4].<br />
In this study in five cases the only finding<br />
seen in galactography was intraductal filling<br />
defects. In dedicated study done by cho <strong>and</strong> his<br />
colleagues ,they stated that in order to thoroughly<br />
<strong>and</strong> accurately evaluate patients exhibiting<br />
pathologic nipple discharges, it is important to<br />
perform ductography <strong>and</strong> not to miss the subtle<br />
but suspicious ductographic findings associated<br />
with breast cancer. Diffusely spreading intraductal<br />
cancers, with or without focal invasions,<br />
are often found to be negative by mammography<br />
(especially in absence of microcalcifications)<br />
<strong>and</strong> sonography. In such cases, ductography<br />
constitutes the best imaging method, as it has<br />
proven effective in the determination of the<br />
nature <strong>and</strong> extent of such lesions <strong>and</strong> can facilitate<br />
appropriate surgical management [5].<br />
We agree with other radiologists who maintain<br />
that ductography is prohibitively timeconsuming<br />
<strong>and</strong> that it can be replaced, at least<br />
in part, by sonography. Intraductal papillary<br />
lesions are sometimes visualized as isoechoic<br />
or hyperechoic masses in dilated ducts on sonography<br />
<strong>and</strong> can often be biopsied under sonographic-guidance<br />
[6-8].<br />
The quality of breast US is closely related<br />
to the performance of the equipment used for<br />
the examination <strong>and</strong> the skill of the examiner.<br />
Linear-array, broad-b<strong>and</strong>width transducers with<br />
maximum frequencies of 10-13MHz <strong>and</strong> a center<br />
frequency of at least 7 or 7.5MHz are required<br />
to depict Ductal carcinoma in situ<br />
(DCIS). The adjustment of focal zones, system<br />
gain <strong>and</strong> time gain compensation setting is also<br />
important. US should be performed in radial<br />
<strong>and</strong> anti-radial planes as well as longitudinal<br />
<strong>and</strong> transverse planes. In patients with DCIS,<br />
radial US is particularly useful for depicting<br />
intraductal masses <strong>and</strong> evaluating the ductal<br />
extent of disease, whereas anti-radial US is<br />
more helpful for evaluating the surface characteristics<br />
of the mass [9]. We add to perfect US<br />
technique for assessment of retroareolar area,<br />
excessive gel <strong>and</strong> gentle pressure to see mass<br />
inside the duct.<br />
Cancer risk from nipple discharge is reported<br />
to be anywhere from 1.3% to 47% [10]. The<br />
incidence of malignancy in this study was 5.6%<br />
in addition to 2.8% precancerous condition<br />
likely hyperplasia <strong>and</strong> atypia.<br />
In this study, masses of intraductal carcinoma<br />
are relatively hypoechoic compared to benign<br />
cases, this coincides with those who reported<br />
that ultrasound appearance of non-screening<br />
detected intraductal carcinoma is relatively<br />
isoechoic in comparison with invasive carcinoma<br />
[10], regarding shape; oval shaped masses<br />
proved in this study to be papillomas but assessment<br />
of margins, was not a point of differentiation,<br />
as in two cases of atypia which showed<br />
macro-lobulated outline <strong>and</strong> in two cases of