Golniški simpozij 2011 Zbornik povzetkov
Golniški simpozij 2011 Zbornik povzetkov
Golniški simpozij 2011 Zbornik povzetkov
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
Golnik<br />
Symposium<br />
<strong>2011</strong><br />
Congress<br />
Bled, Slovenia, October 7-8, <strong>2011</strong><br />
Book of abstracts
Publisher<br />
University Clinic of Respiratory<br />
and Allergic Diseases Golnik<br />
Editor<br />
Izidor Kern, Urøka Bidovec Stojkoviœ<br />
Prepress<br />
Trajanus d.o.o., Kranj<br />
Printing<br />
Pro Grafika d.o.o., Æabnica<br />
Printed<br />
200 copies<br />
Bled, Slovenia, October 7-8, 2008<br />
CIP - Kataloæni zapis o publikaciji<br />
Narodna in univerzitetna knjiænica, Ljubljana<br />
616.2(082)<br />
GOLNIK Symposium (<strong>2011</strong> ; Bled)<br />
Book of abstracts / Golnik Symposium, <strong>2011</strong>, Bled, Slovenia,<br />
October 7-8, <strong>2011</strong> ; [editor Izidor Kern, Urøka Bidovec Stojkoviœ].<br />
- Golnik : University Clinic of Respiratory and Allergic Diseases,<br />
<strong>2011</strong><br />
ISBN 978-961-6633-30-7<br />
1. Kern, Izidor<br />
257761536<br />
BOLNIØNICA GOLNIK - KLINIŒNI ODDELEK ZA PLJUŒNE BOLEZNI IN ALERGIJO<br />
UNIVERSITY CLINIC OF RESPIRATORY AND ALLERGIC DISEASES GOLNIK<br />
Golnik 36, 4204 Golnik, Slovenija T: +386 (0)4 25 69 100 F: +386 (0)4 25 69 117<br />
E: kopa.tajnistvo@klinika-golnik.si W: www.klinika-golnik.si
Content<br />
Oral presentations<br />
Kadivec S Coordination of discharge in COPD 9<br />
Joøt M, Morgan T Improving medication management on a hospital level - 10<br />
our experience<br />
Meøko Brguljan P Patient safety – the preanalytical impact on quality 12<br />
of laboratory reports<br />
Muøiœ E Current concept on pathomechanism of Idiopathic 14<br />
pulmonary fibrosis<br />
Poster presentations<br />
Meøko Brguljan P, Benedik B Quality indicators of the preanalytical phase 20<br />
in blood gas analysis<br />
Meøko Brguljan P, Bratoæ S Licensing of medical laboratories in Slovenia 21<br />
Œebron Lipovec N, Mrhar A, Knez L, Impact of pharmacists interventions on the frequency 22<br />
Farinha H, Amaral J,<br />
of medication errors in patients<br />
Parola A, Falcão F<br />
with enteral feeding tubes<br />
Knez L, Reæonja R, Øuøkoviœ S, Comprehensive medication history: the need for the 24<br />
Koønik M, Mrhar A<br />
implementation of medication reconciliation processes<br />
Knez L, Øuøkoviœ S, Primoæiœ A, Implementation of a medication reconciliation service 25<br />
Laaksonen R, Joøt M,<br />
at hospital admission: results<br />
Koønik M, Mrhar A<br />
from a randomised control study<br />
Lunder U, Furlan M Communication in palliative care: challenge 27<br />
for healthcare providers<br />
Ziherl K, Øarc I, Gabrijelœiœ J Patients referred to Laboratory for sleep related 28<br />
breathing disorders: our 5 year experience<br />
Hafner T, Øorli J Pulmonary rehabilitation program – our results 30<br />
Adamiœ K, Lalek N, Øtupnik T Videothoracoscopic resection of giant 31<br />
emphysema bullae<br />
Zabret M, Boneø U, Øarc I, Koønik M, Electrocardiogram analysis of patients with chronic 33<br />
Øuøkoviœ S, Lainøœak M<br />
obstructive pulmonary disease<br />
Øarc I, Tomiœ V, Lainøœak M, Implications of sputum bacteriology in acute 34<br />
Ziherl K, Jeriœ T,<br />
exacerbations of chronic obstructive<br />
Koønik M, Øuøkoviœ S<br />
pulmonary disease<br />
Boneø U, Øarc I, Ziherl K, Zabret M, Antibiotic treatment during hospitalization due 36<br />
Jeriœ T, Tomiœ V, Koønik M,<br />
to acute exacerbation of chronic<br />
Øuøkoviœ S, Lainøœak M<br />
obstructive pulmonary disease<br />
3
Nastasijeviå Borovac D, Pejœiå T, Examination of resistance of bacteria isolated 37<br />
Radjenoviå Petkoviå T,<br />
from sputum and partial broncoalveolar<br />
Djordjeviå I, Ranœiå M<br />
lavage in Clinic for lung disease, Knez Selo<br />
Adamiœ K, Polajnar M, Pneumococcal bacteriemia in adults with 39<br />
Øifrer F, Tomiœ V<br />
community-acquired pneumonia<br />
Jeriœ T, Kern I, Svetina Øorli P Aspergillosis 41<br />
Luænik D, Stokiå J, Tomiœ V, Øifrer F Use of multiplex PCR for detection of bacterial 42<br />
respiratory tract pathogens<br />
Øinkovec K, Luænik D, Carriage rate of extended-spectrum b-lactamase 43<br />
Œernivec J, Tomiœ V<br />
producing Enterobacteriaceae and methicillinresistant<br />
Staphylococcus aureus in elderly<br />
on admission to the nursing home<br />
Øinkovec K, Luænik D, Methicillin-resistant Staphylococcus aureus 44<br />
Œop Z, Tomiœ V<br />
and extended-spectrum b-lactamase producing<br />
Enterobacteriaceae in house pets<br />
Svetina Øorli P, Pivk K, Jakelj A Screening of persons after contact with a TB patient 45<br />
in the Shelter for the homeless<br />
Koren Pucelj N, Hudoklin I Occurrence of tuberculosis in largest Slovenian 46<br />
correctional facility ZPKZ Dob in the period<br />
from 2000 to 2008<br />
Toni J, Œebron Lipovec N, Pharmacist’s role in the treatment of patients 48<br />
Svetina Øorli P<br />
with tuberculosis – our positive experience<br />
Æolnir Dovœ M, Fajfar N, Plesec I, A nation-wide study of nontuberculous mycobacteria 50<br />
Petroviœ Æ, Øorli Peranoviœ N in Slovenia<br />
Bidovec Stojkoviœ U, Æolnir Dovœ M The importance of pre-analytic factors 52<br />
in Quantiferon-TB Gold test<br />
Fajfar N, Bidovec Stojkoviœ U, Evaluation of GeneXpert MTB/RIF assay for detection 54<br />
Æolnir Dovœ M<br />
of Mycobacterium tuberculosis and rifampicin<br />
resistance in a routine laboratory setting in Slovenia<br />
Bidovec Stojkoviœ U, Fajfar N, Nation-wide evaluation of three molecular genotyping 55<br />
Æolnir Dovœ M<br />
methods in Slovenia<br />
Unk M, Kern I, Œufer T Primitive neuro-ectodermal tumour of the lung- 56<br />
a case report<br />
Zukiå E, Keser D, Premalignant lesions among coal miners 58<br />
Jusufoviå E, Sejdinoviå R<br />
Lalek N, Adamiœ K, Øtupnik T Videothoracoscopic lung lobectomy in patients 59<br />
over 75 years of age<br />
Sodja E, Knez L, Ovœariœek T, Clinical impact of ERCC1 protein expression 60<br />
Kern I, Koønik M, Sadikov A, Œufer T in small-cell lung cancer patients treated<br />
with platinum-based chemotherapy<br />
Kontiå M, Stojøiå J, Jovanoviå D, Quantitative Methylation Profiles of Multiple Genes 61<br />
Bunjevacki V, Puumala S,<br />
in Patients with Non-Small Cell Lung Cancer And its<br />
Nelson HH<br />
Association with Clinicopathological Correlations<br />
Jusufoviå E, Rijavec M, Keser D, Anti-angiogenic miRNAs let-7b and miR-126 63<br />
Sodja E, Koønik M, Koroøec P are down-regulated in tumour and tumour surrounding<br />
in NSCLC lung tissue<br />
Knez L, Ovœariœek T, Sadikov A, MDR1 polymorphisms G2677T/A and C3435T 65<br />
Sodja E, Kern I, Koønik M, Œufer T are independent predictive markers in small-cell<br />
lung cancer patients treated with chemotherapy<br />
Øumer TT, Œufer T Changing to another TKI in treatment 66<br />
of metastatic NSCLC<br />
Kern I, Kovaœeviå M, Sodja E, Œufer T Topoisomerase II in small cell lung carcinoma 67<br />
4
Turnøek N, Mohorœiœ K, Neutropenia in lung cancer patients treated 68<br />
Sadikov A, Œufer T with chemotherapy in a routine clinical practice –<br />
an institutional experience<br />
Mlakar J, Œufer T, Triller N, Safety and efficiency of treatment of advanced 70<br />
Sadikov A, Øumer TT<br />
NSCLC with non-squamous histology with pemetrexed<br />
and platinum derivate combination in routine clinical<br />
practice; experience at University Clinic Golnik<br />
Ivaniøeviå J, Kotur Stevuljeviå J, Blood oxidative stress markers and lipid status 72<br />
Stefanoviå A, Jeliå Ivanoviå Z, in sarcoidosis<br />
Spasiå S, Videnoviå Ivanov J,<br />
Vuœiniå Mihailoviå V, Iliå J<br />
Videnoviå Ivanov J, Results of 18 F FDG PET scan in patients 74<br />
Sobiå Øaranoviå D,<br />
with chronic sarcoidosis<br />
Vuœiniå Mihailoviå V, Zugiå V,<br />
Filipoviå S<br />
Øumer TT, Æagar I, Gaøperøiœ N The significance of PET CT in diagnosis 75<br />
of Takayasu arteritis – a case study<br />
Osolnik K, Rijavec M, Koroøec P Diagnostic value of pulmonary 76<br />
NKT CD3 + CD16/56 + cells<br />
Rijavec M, Osolnik K, Peripheral invariant NKT cells and factors involved 77<br />
Koønik M, Koroøec P<br />
in the development of iNKT cells in sarcoidosis patients<br />
Dimitrijeviå J, Vegnuti M, Adamiœ K, Side-effects of specific immunotherapy: 78<br />
Bajroviå N, Eræen R, Koønik M, our experience – KOPA Golnik<br />
Muøiœ E, Zidarn M<br />
Mumoviå G, Hoœevar Bolteæar I, Allergy in patients with vocal fold nodules 79<br />
Popov Dragin O<br />
Balantiœ M, Rijavec M, Kavalar M, ORMDL3 gene polymorphism is associated 81<br />
Øilar M, Koønik M, Koroøec P with asthma risk and severity in Slovenian children<br />
Øilar M, Pevec B, Rijavec M, Expression profiles of regulatory genes after venom 82<br />
Eræen R, Koønik M,<br />
immunotherapy<br />
Stipiå Markoviå A, Koroøec P<br />
Œelesnik N, Kopaœ P, Eræen R, Baseline serum tryptase is not associated 83<br />
Øilar M, Koønik M, Koroøec P with the risk for severe anaphylactic reactions<br />
in honey bee venom allergy<br />
Œelesnik N, Eræen R, Øilar M, Diagnosis of double sensitized Hymenoptera venom 84<br />
Mittermann I, Valenta R,<br />
allergic patients with recombinant species-specific<br />
Zidarn M, Koønik M, Koroøec P major allergens used in basophil activation test<br />
Zidarn M, Koønik M, Øilar M, Rhinitis symptoms caused by grass pollen 85<br />
Grahek A, Koroøec P<br />
are associated with elevated basophil allergen<br />
sensitivity and a larger grass-specific IgE fraction<br />
Kopaœ P, Gentinetta T, Rudin M, Continuous apple consumption induces oral tolerance 86<br />
Gerber R, Pichler C, Hausmann O, in birch-pollen associated apple allergy<br />
Schnyder B, Pichler WJ<br />
Eræen R, Øilar M, Comparison of basophil activation test and inhibition tests 88<br />
Koroøec P, Koønik M<br />
in double positive Hymenoptera venom allergic patients<br />
Perin P, Berce V, Potoœnik U Association analysis of polymorphisms in selected 89<br />
candidate genes in slovenian children with astma<br />
Workshop / Delavnica – organizirajoœa pljuœnica<br />
Kern I Organizirajoœa pljuœnica – histopatoloøka entiteta 92<br />
Poæek I Organizirajoœa pljuœnica – spekter radioloøkih vzorcev 94<br />
Osolnik K Organizirajoœa pljuœnica – kliniœni problem 96<br />
5
ORAL PRESENTATIONS<br />
7
Coordination<br />
of discharge in COPD<br />
Saøa Kadivec<br />
University Clinic of Respiratory and Allergic Diseases Golnik<br />
Healthcare is facing a number of factors that are reducing the inpatient length of stay and have influence<br />
on the intensity of the treatment of hospitalized patients. The average age of patients is increasing,<br />
and so is the complexity of their problems and needs due to the chronic nature of their<br />
illnesses. Many patients are discharged from the hospital while still receiving treatment. These results<br />
in a greater amount and diversity of their needs after discharge, and also in the amount of pressure<br />
that is put on health care services and providers as well as other services that help patients perform<br />
daily and other life activities.<br />
The importance of discharge is still underestimated in daily practice, because discharge is still perceived<br />
as a conclusion of medical treatment and not as a part of integrated treatment. Timely recognition<br />
of patients’ needs after discharge during their hospital stay is often lacking and insufficient<br />
due to short hospitalization, staff work overload due to acute treatment and insufficient and/or ineffective<br />
communication.<br />
In order to solve the problem with the discharge process, the University Clinic of Respiratory and Allergic<br />
Diseases Golnik has implemented a case manager who is a missing link between the integrated<br />
patient treatment and patients’ needs for further treatment at home or in institutional care. A case manager<br />
enables not only the continuity of treatment but also those patients, their families and providers of<br />
health and social care on all levels of treatment get more information. He/she coordinates work, communicates<br />
with the patient the first week after hospital discharge and informs them about the activities<br />
related to discharge, consults them and is in regular contact with their GP and community nurse.<br />
A case manager is included in the treatment of patients that meet the following criteria:<br />
• They have a chronic disease (COPD, TB, asthma, chronic heart conditions, neoplasm) and<br />
• They have been admitted or discharged as at least category II according to demands of hospital<br />
nursing care.<br />
How to develop the role of a case manager in the future?<br />
We believe that case managers could work in nurse-led outpatient units, as heads of registers and<br />
in telemedicine.<br />
In 2009, we started a project of work evaluation of case managers. The purpose of the study was to evaluate<br />
the influence of the case manager’s work on the treatment of patients with chronic obstructive pulmonary<br />
disease (COPD) with a prospective randomized clinical study. Patients are divided into two<br />
equally large groups: an intervention group and a control group. The case manager only works with the<br />
intervention group. Patients from the intervention group are treated according to the principle of good<br />
clinical practice. Data collection was made using a number of tools (different questionnaires).<br />
9
Improving medication management<br />
on a hospital level - our experience<br />
Maja Joøt, Tina Morgan<br />
University Clinic of Respiratory and Allergic Diseases Golnik<br />
The rough beginnings<br />
The story of a comprehensive medicine management on a hospital level began with the decision of<br />
top hospital management to implement clinical pharmacy. Before that the major task of hospital pharmacists<br />
was to provide wards with medicines, at a reasonable time and price. The first step towards<br />
better medicine management was made by the identification of drawbacks in the existing process.<br />
Present state<br />
Quality, effective and safe medicines are the base for successful treatment. Therefore it was essential<br />
to assure proper storage conditions and to establish suitable transport within our hospital (e.g.<br />
cold chain). Stability of diluted solutions and compatibility of admixtures was revised according to the<br />
literature. Special focus was put on safe, centralized preparation of high risk medications (e.g. cytostatics).<br />
A progress was made in the perspective of medicines reaching the patient. Accessibility was upgraded<br />
by ensuring a continuous and controlled access to medicine stocks in the hospital pharmacy.<br />
Rare and expensive medicines are now dispensed per patient for pre-defined medical<br />
indications. Drug administration was unified among wards.<br />
Further on, recommendations and protocols for the treatment of certain diseases or with certain drugs<br />
(e.g. LMWH, chemotherapy) were prepared and implemented in routine clinical practice. This was<br />
upgraded with new pharmacy services: chemotherapy prescription screening and provision of a<br />
medication history for each patient, starting cancer drug therapy.<br />
Substantial improvements in the continuity of care of patients with certain diseases (e.g. TB) was<br />
made: pharmacists perform medication reconciliation at admission, medication review during hospitalization,<br />
patient counselling before discharge and provide patients with medicines for home treatment.<br />
For all other patients, these services are offered to a various extent on some of the wards or<br />
for selected patients.<br />
The definition, identification and monitoring of high risk medications and patients at a high risk for adverse<br />
drug events are objectives of a high priority, on-going process, led by a pharmacist.<br />
Where to?<br />
Medicine management is now being improved in a systematic way to ensure continuity of care for<br />
all patients. The emphasis should be given on the safety, efficacy and quality of drug treatment. A<br />
logistic reorganization of drug dispensing, guaranteeing efficient, safe and recordable unit dose dis-<br />
10
pensing should be undertaken in order to allow pharmacist to focus on more clinically oriented activities<br />
and make the best use of their expertise.<br />
References<br />
1. Knez L, Joøt M, Toni J, Triller N, Œufer T. Implementing new clinical pharmacy services parallel to the introduction<br />
of centralized preparation of anti-cancer drugs. Zdravstveno varstvo <strong>2011</strong>; 50:12-23.<br />
2. Guchelaar H-J, Colen HBB, Kalmeijer MD, et al. Medication Errors Hospital Pharmacist perspective. Drugs<br />
2005; 65:1735-46.<br />
11
Patient safety – the preanalytical<br />
impact on quality of laboratory reports<br />
Pika Meøko Brguljan<br />
University Clinic for Respiratory Diseases and Allergy Golnik, Clinical Chemistry Department, Golnik,<br />
Slovenia<br />
Patient safety, the freedom from accidental or unnecessary harm due to adverse events occurring in<br />
any healthcare setting, directly affects the quality of care. The Institute of Medicine (IOM) report, To err<br />
is human, dramatically increased level of concern about adverse events and patient safety in healthcare,<br />
including errors in laboratory medicine (1). Even a low incidence of laboratory mistakes among<br />
the billions of tests performed every day worldwide could have important public health and patient<br />
safety implications. While the IOM report presented few data on errors in laboratory medicine, it has<br />
wide-reaching implications for all disciplines. The IOM report, Crossing the quality chasm (2), stressed<br />
the concept of patient-centered care and the fact that complex systems are characterized by specialization<br />
and interdependency. The evidence reported can be translated into a better understanding of<br />
the importance of the total testing process (TTP) – preanalytical, analytical and postanalytical, as the<br />
right framework for patient safety in laboratory medicine. The TTP consists of a series on interrelated<br />
processes, each involving a series of a process step, every one of which can result in an error (3).<br />
In the last years, in our laboratory many strategies are used to reduce errors, such as improved laboratory<br />
technology, internal quality control procedures, external quality assurance programs, educational<br />
programs, licensing of laboratory professionals, certification of laboratory (as the part of our<br />
clinic’s ISO 9001:2000 and DNV accreditation certificates). Laboratory also fulfil the Slovenian regulatory<br />
requirements in laboratory medicine and gain the working license in the year 2009. In the<br />
past, the preanalytical phase has been often overlooked as a source of errors, evidence from recent<br />
studies shows that a large percentage of laboratory errors occur in the preanalytical steps (4). In the<br />
laboratory several steps have already been taken to increase awareness and establish a governance<br />
of the preanalytical aspect of laboratory processes. Standardization and monitoring of the most common<br />
preanalytical errors have been implemented in the every-day work in the laboratory. Quality indicators<br />
and the error monitoring system of the preanalytical phase are tools that can be used to<br />
supervise the activity carried out in the laboratory and activities in relation to the clinical laboratory.<br />
Till the data are collected and corrective actions, such as education of staff on preanalytical issues,<br />
have been taken, a big improvement in fulfilment of the quality specifications have been detected.<br />
The interdisciplinary approach to manage the quality of the preanalytical phase is a good approach<br />
to avoid and reduce laboratory errors in TTP. In the future our aim is to integrate more effective error<br />
tracking and quality indicator reporting system to our laboratory informaton system (LIS). Continuous<br />
actions for all involved in the processes and move from error reporting to risk managament is of extreme<br />
importance for patient safety.<br />
12
References<br />
1. Plebani M. Errors in laboratory medicine and patient safety: the road ahead. Clin Chem Lab Med 2007;45:700-<br />
707.<br />
2. Institute of Medicine. Crossing the quality chasm: a new health care system for the 21st century. Washington,<br />
DC: National Academy Press, 2001.<br />
3. Boone DJ. Is it safe to have a laboratory test? Accred Qual Assur 2004; 10:5-9.<br />
4. Lippi e tal.:Preanalytical quality improvement: from dream to reality. Clin Chem Lab Med <strong>2011</strong>;49(7):1113-<br />
1126.<br />
13
Current concept on pathomechanism<br />
of Idiopathic pulmonary fibrosis<br />
Ema Muøiœ<br />
Previously it was anticipated that idiopathic pulmonary fibrosis (IPF) reflects an inflammatory driven<br />
alveolitis form of lung fibrosis. But the frustrated experience in IPF is that steroids and immunosuppressants<br />
are of little help. A more recent hypothesis puts the alveolar type II cell (P II) at the centre<br />
of the concept, according to which chronic epithelial damage is the underlying trigger mechanism<br />
in IPF. Proliferation of pneumocyte type II cells (P II) is induced to overcome the loss of epithelium<br />
and the factor released may largely induce the uncontrolled proliferation of fibroblasts and the excessive<br />
deposition of extracellular matrix, mostly collagen. IPF patients experience a progressive<br />
dyspnoea due to loss of regularly structured alveolar units and concomitant scarring of the lung.<br />
Quality of life gradually decreases and patients usually die within 3-5 years after diagnosis. No approved<br />
treatment was available, but newly some studies are bringing hope with new approach<br />
against the fibroproliferation.<br />
Figure1. From fibroblast foci with collagen production to honey combing of the lung seen on HRCT.<br />
(courtesy of Izidor Kern and Rok Cesar)<br />
The pathomechanism of IPF is yet not totally understood. Previously, it was anticipated that the disease<br />
reflects another inflammatory driven form of lung fibrosis. However, the frustrating experience<br />
in IPF is that steroids and immunosuppressants are of little help, if at all. A more recent and increasingly<br />
favoured hypothesis puts the alveolar type II cell at the centre of a unifying concept, according<br />
to which chronic epithelial damage is the underlying trigger mechanism for the development<br />
14
of lung fibrosis. In more detail, misfolding or defective processing of proteins (e.g. surfactant protein<br />
C), altered lysosomal transport or processing or chronic DNA damage have already been proven to<br />
induce alveolar epithelial apoptosis. Proliferation of P II are induced to overcome the loss of epithelium<br />
and the factors released may in a paracrine fashion largely induce the uncontrolled proliferation<br />
of fibroblasts and the excessive deposition of extracellular matrix, mostly collagen.<br />
What is the triggering event in IPF?<br />
The P II are thought to be at the centre of a pathomechanistic concept for sporadic or familial IPF, but<br />
also for other diffuse interstitial lung diseases (DILD), such as the Hermansky-Pudlack syndrome, amiodarone-induced<br />
pneumonitis, or irradiation-induced lung fibrosis. Both, enhanced PII cell apoptosis<br />
and hyperplasia ultimately induce distorted epithelial-mesenchymal cross-talk, resulting in enhanced<br />
fibroblast activation and extracellular matrix (ECM) synthesis. Ultrastructural studies have revealed the<br />
existence of proliferative alveolar epithelial cells immediately adjacent to injured epithelial cells, suggesting<br />
that epithelial apoptosis, proliferation and hyperplasia occur simultaneously during the process<br />
of fibrosis. In detail, chronic endoplasmic reticulum (ER) or lysosomal stress has been reported to induce<br />
PII apoptosis and thus set the stage for the development of lung fibrosis. In detail, mutations in<br />
the surfactant protein C (SFTPC) and telomerase genes (TR/TERT) in familial forms IPF provided initial<br />
evidence that apoptosis of PII cells may represent an important pathogenetic trigger event.<br />
In parallel, activation of endoplasmatic reticulum (ER) stress pathway components and activating<br />
transcription factor 6 (ATF) was observed in IPF and NSIP, and found to result in a persistent and overwhelming<br />
ER stress response and induction of epithelial apoptosis via DNA damage inducible transcript<br />
(DDIT) 3. Also, respiratory infections represent a common phenomenon in IPF, which not only<br />
seem to frequently antecede the clinical appearance of the disease, but also to accelerate its clinical<br />
course. Consistent with these observations, bacterial, and – even more compelling – viral infections<br />
can induce severe ER-stress. Thus, an intriguing and unifying concept for sporadic and familial<br />
IPF would consist of a genetic predisposition to an epithelial injury, a modifying environmental stimulus<br />
and a common downstream pathway resulting in fibrosis based on ER stress (or DNA damage)<br />
induced PII cell apoptosis. Other diseases resulting in chronic APII cell injury, such as Hermansky<br />
Pudlak Syndrome, amiodarone- or irradiation-induced lung fibrosis, might similarly result in epithelial<br />
apoptosis and subsequent fibrosis, and could thus be integrated into this concept.<br />
What are the mediators of distorted epithelial-mesenchymal interactions (cross-talk) in lung<br />
fibrosis?<br />
Balanced epithelial-mesenchymal interactions are of the utmost importance for proper lung development,<br />
in particular for regular definition of a proximal-distal axis and dichotomous branching. In the<br />
adult lung, mesenchymal-epithelial interactions warrant proper lung function and are a prerequisite<br />
for the maintenance of the trophic alveolar unit, but impaired epithelial-mesenchymal crosstalk between<br />
PII cells and subepithelial fibroblasts, as well as dysregulated precursor cell recruitment, have<br />
recently been shown to contribute to the pathobiology of IPF.<br />
It has been proposed that the PII cell, by action of cyclooxygenase 2, releases PGE2, which then binds<br />
to the EP-2 receptor on fibroblasts, increases cAMP levels in the fibroblast and thereby inhibits the proliferation<br />
and transactivation of this cell. In addition, several growth factors are released by the PII cell<br />
that controls the fibroblast phenotype, such as members of the Wnt, BMP, or TGF-b superfamilies. In<br />
particular, enhanced secretion and/or activity of Wnt and TGF-b superfamily members have been documented<br />
in IPF. The fibroblast itself is a rich source of factors like FGF-7, FGF-10, and HGF. HGF will<br />
be released by fibroblasts in dependency of cAMP levels and must be activated by extracellular serine<br />
proteases such as the HGF activator. FGF-7, FGF-10, as well as HGF are known to exert a marked<br />
influence on PII cell proliferation, migration and survival, and at least HGF has been shown to be released<br />
to a much weaker extent from IPF fibroblasts as compared to fibroblasts from healthy lungs.<br />
What is the origin of activated (myo-) fibroblasts in IPF?<br />
While the initial injury in IPF is most likely affecting the PII cell (see above), it is well accepted that the<br />
interstitial fibroblast / activated myofibroblast represents the key effector cell responsible for the in-<br />
15
creased ECM deposition that is characteristic for this disease. The number of smooth muscle actinpositive,<br />
activated (myo-) fibroblasts is significantly increased in multiple forms of pulmonary fibrosis<br />
including IPF, but their origin remains to be elucidated.<br />
Currently, three major theories attempt to explain this hallmark of maladaptive cell activation:<br />
1. It has been demonstrated that resident pulmonary fibroblasts proliferate in response to fibrogenic<br />
cytokines and growth factors (see below), thereby increasing the local fibroblast pool via local fibroproliferation.<br />
2. In addition, several recent studies have shown that bone marrow-derived circulating fibrocytes<br />
traffic to the lung during experimental lung fibrosis, and serve as progenitors for interstitial fibroblasts.<br />
In particular, collagen I-positive fibrocytes have been shown to traffic to injured lungs in a<br />
chemokine-dependent fashion, integrate into the lung ECM, and contribute to enhanced collagen<br />
synthesis in fibrosis.<br />
3. It was recently proposed that PII cells are capable of undergoing the process of epithelial-to-mesenchymal<br />
transition (EMT), the phenotypic, reversible switching of epithelial to fibroblast-like cells,<br />
which is initiated by an alteration of the transcriptional and proteomic profile of P2 cells. The orchestrated<br />
series of events initiating EMT include remodelling of epithelial cell-cell and cell-matrix<br />
adhesion contacts, reorganization of the actin cytoskeleton, and induction of mesenchymal gene<br />
expression.<br />
EMT is a highly controlled process initially discovered and described in embryonic development and<br />
morphogenesis. In addition, EMT has gained wide recognition as a mechanism that facilitates cancer<br />
progression and metastasis, as well as the development of chronic degenerative fibrotic disorders<br />
of the kidney, liver, and lung. Transforming growth factor (TGF)-b is a main inducer and regulator<br />
of EMT in multiple organ systems.<br />
What are the major signalling pathways for matrix remodelling in the lung?<br />
As a kind of primary wound healing response, activation of the coagulation cascade and suppression<br />
of the fibrinolysis system has been observed in patients with IPF, and the cellular origin of these<br />
coagulation factors (alveolar macrophages and P II cells) has been disclosed. Analysis of bronchoalveolar<br />
lavage fluids (BALF) revealed substantial activation of the extrinsic coagulation pathway<br />
(tissue factor VII), alongside with pronounced suppression of antithrombotic (activated protein C) or<br />
fibrinolytic (plasminogen activator inhibitor 1) activities. These changes promote alveolar and interstitial<br />
fibrin deposition, forming a provisional matrix and thereby contributing to lung fibrosis. Moreover,<br />
several procoagulant serine proteases such as TF/FVII, factor X and thrombin induce fibrotic<br />
events via the Protease activated receptors PAR-1 and PAR-2. In response to the activation of this<br />
G-protein coupled receptor, increased ECM production, secretion and induction of profibrotic growth<br />
factors such as TGF-b and PDGF can be observed. Vice versa, the urokinase system has repeatedly<br />
been shown to exert strong antifibrotic activity, most likely due to the activation of HGF and the removal<br />
of fibrin and ECM.<br />
With respect to scar formation as aberrant alveolar/interstitial wound healing response, there is currently<br />
no doubt that the Transforming Growth Factor (TGF)-b family represents the pivotal mediator<br />
system. In vitro, TGF-b induces fibroblast chemotaxis, proliferation and transdifferentiation into myofibroblasts,<br />
and it largely promotes the production and secretion of extracellular matrix compounds,<br />
mainly collagen. Application of TGF-b encoding adenoviral vectors to the distal lung induces a progressive<br />
and severe lung fibrosis. Likewise, application of these vectors to the pleural space induces<br />
pleural fibrosis and subpleural lung fibrosis as seen in IPF. Increased TGF-b signalling is also observed<br />
in other animal models of lung fibrosis, such as the bleomycin model, where collagen deposition<br />
is reduced by TGF-b antibodies and soluble TGF-b receptors. In lungs of IPF patients, increased<br />
expression of TGF-b has been observed in close proximity to areas of increased ECM deposition.<br />
Apart from TGF-b, there are also other growth factors such as PDGF (platelet-derived growth factor),<br />
CTGF (connective tissue growth factor), members of the Wnt pathway, or IGF-I (insulin-like growth<br />
factor I) and endothelin, which may significantly<br />
contribute to the pathogenetic sequelae of IPF.<br />
16
Apart from the proliferation of fibroblasts, the excessive deposition of matrix is a key feature of IPF<br />
and, most likely, is the result of excessive production of ECM compounds and a local imbalance between<br />
the matrix metalloproteinases (MMP) and their inhibitors (TIMP).<br />
In general, increased TIMP expression and virtual absence of the collagen I specific MMP-1 has<br />
been observed in the lungs of IPF patients, thus contributing to collagen deposition. In view of the<br />
coexistence of fibrotic scars and honeycomb cysts in the lungs of IPF subjects, it is yet not settled,<br />
if a spatial disarrangement of the collagenases (largely MMP-1) and the TIMPs may be the primary<br />
reason for the development of this structural heterogeneity. In contrast, the two gelatinases MMP 2<br />
und 9, known for their ability to destruct the basement membrane and thus to impair epithelial regeneration,<br />
were found to be increased in lung fibrosis. Finally, matrilysin (MMP-7) was also found<br />
to be highly upregulated in IPF and MMP-7 knock out mice were protected from the bleomycin induced<br />
lung fibrosis, thus supporting an important role of this MMP.<br />
Treatment of lung fibrosis - translational approaches<br />
The therapeutic approach to patients with IPF has not changed dramatically over the last 10 years.<br />
But in <strong>2011</strong> Pirfenidone (targeting the TGF-b pathway), as well as bosentan (targeting the endothelin<br />
pathway), have provided initial hope. Pirfenidon was registered in Europa in februar <strong>2011</strong> as the<br />
first medicament for the treatment of IPF. Also N-acetyl cysteine was tested against placebo and<br />
was found out to attenuate the loss of lung function. In the meantime, an encouraging increase in clinical<br />
trials in the field of IPF can be observed. Most of these studies are addressing secondary<br />
processes forwarding fibrosis per se. An overview is given in the figure 2 outlined below.<br />
Figure 2. The cytokine oriented targets of promising drugs for IPF<br />
Conclusions<br />
We are at the entrance to a new time with knowledge, that inflammation is not needed to precede lung<br />
fibrosing but there are multiple, microepithelial injuries, followed by activatoin and formation of fibroblast-myofibroblast<br />
foci, which evolve to fibrosis. The genetic background for abnormal repair of<br />
epithelial damage is of importance. IPF is an epithelial-fibroblastic disease and not a postinflammatory<br />
fibrosing process.<br />
It is the answer why the antiinflammatory, including steroid therapy was not successful in IPF. And<br />
now antifibrotic oriented drugs are already evidence based promising.<br />
17
References<br />
1. Moises Selman, King T.E.,Pardo A: idioppathic pulmonary fibrosis: Prevailing and Evolving Hypotheses about<br />
its Pathogenesis and Implications for therapy. Ann Intern Med 2001;134.136-151<br />
2. Moises Selman, Pardo A:The epithelial/fibroblasic pathway in the pathogenesis of Idiopathic Pulmonary fibrosis.<br />
American Journal of respiartory Cell and Molecular Biology 2003;29: S93-S97<br />
3. 52. Kongress der DGP in Dresden-Symposium 8.4.<strong>2011</strong>: Idiopathische Lungenfibrose (IPF): Neue Erkenntnisse,<br />
neue Hoffnung für den Patienten.<br />
18
POSTER PRESENTATIONS<br />
19
Quality indicators of the preanalytical<br />
phase in blood gas analysis<br />
Pika Meøko Brguljan, Barbara Benedik<br />
University Clinic of Respiratory Diseases and Allergy Golnik<br />
Background<br />
The preanalytical phase is often overlooked as a major source of errors in whole-blood analysis, especially<br />
in blood gasses. Arterial blood samples are very sensitive because of the physiological properties<br />
of blood and the changes after the sampling. Quality indicators of the preanalytical phase are<br />
tools that can be used to supervise the activity carried out in the laboratory and activities in relation<br />
to the clinical laboratory.<br />
Methods<br />
Sampling of the arterial blood for whole blood analysis is performed by nursing staff on the wards,<br />
the analysis are performed by laboratory staff in the clinical laboratory. The standard procedure for<br />
sampling and the importance of the preanalytical phase with the aim to avoid errors in laboratory reports,<br />
has been prepared by both, the laboratory and the nursing staff. Six quality indicators, based<br />
on most common preanalytical errors, have been defined. These were sample volume, mixing of<br />
samples, air bubbles in samples, transportation time, identification of the sample and electronic request<br />
form, transfer of electronic request form from hospital information system to laboratory information<br />
system,. The data are collected 14 days per year for all samples, received by the laboratory.<br />
Results<br />
Till the year 2007 the data were collected and corrective actions, such as education of nursing staff<br />
on preanalytical issues, have been taken. A big improvement in fulfilment of the quality specifications<br />
goals have been detected. By the end of the 2010 99,6% fullfil the criteria on sample volume, 98,2%<br />
on mixing of samples, 97,8% on air bubbles in the samples, 93,8% on transportation time, 98,9% on<br />
identification issues, and 98,9% on appropriate electronic request procedure.<br />
Conclusions<br />
The interdisciplinary approach to manage the quality of the preanalytical phase is a good approach<br />
to avoid laboratory errors in whole-blood testing. Process has already proved benefits. Continuous<br />
actions for all involved in the processes, including new staff, are needed to further improve the quality<br />
of the preanalytical phase.<br />
20
Licensing of medical laboratories<br />
in Slovenia<br />
Pika Meøko Brguljan 1 , Saøa Bratoæ 2<br />
1<br />
University Clinic for Respiratory Diseases and Allergy, Golnik<br />
2<br />
University Medical Centre Ljubljana<br />
Background<br />
Accreditation of medical laboratories in Slovenia is not yet implemented. Nevertheless the concept<br />
of laboratory accreditation defined by ISO/IEC as formal recognition that the testing laboratory is<br />
competent to carry out specific tests was implemented by a different model of licensing. In order to<br />
assure quality and competence in laboratory medicine the National Bylaw for medical laboratories<br />
based on ISO 15189 was adopted.<br />
Methods<br />
Laboratory applies for certification of its professional activity (clinical chemistry, microbiology, transfusiology<br />
or pathology /cytopatholgy) at Ministry of Health. The complyment to the requirements is verified<br />
by commissions appointed by the Ministry. Members of commissions are professionals of the<br />
scientific fields trained for auditing. In principle a commission consists of three members but in case<br />
those laboratories carry out analyses from diffrent fields, a specialist of the relevant field joins the<br />
audit. The special fields often overlap and that as a rule provokes disagreement over professional<br />
competences.<br />
Results<br />
By the end of the 2010 55 out of 102 registered medical biochemistry laboratories were audited, 49<br />
laboratories complied with the requirements and gained the license, 6 laboratories got a suspense<br />
of 6 months due to minor nonconformities.<br />
At microbiology 15 laboratories were audited 3 out of these have to correct deficiencies. Transfusiologists<br />
audited all 16 centers and ordered suspense for two, while at pathology/cytopatholgy one<br />
out of 19 got suspense and two were found not complying.<br />
Conclusions<br />
Process has already proved benefits; laboratories have their quality systems set up, are committed<br />
to continuous quality improvement which will eventually result in accreditation.<br />
21
Impact of pharmacists interventions<br />
on the frequency of medication errors<br />
in patients with enteral feeding tubes<br />
Nanœa Œebron Lipovec 1 , Aleø Mrhar 2 , Lea Knez 1 , H Farinha 3 , J Amaral 3 , A Parola 3 , F Falcão 3<br />
1<br />
University Clinic of Respiratory and Allergic Diseases, Golnik, Slovenia<br />
2<br />
Faculty of Pharmacy, University of Ljubljana, Slovenia<br />
3<br />
Hospital de Egas Moniz – CHLO EPE, Lisbon, Portugal<br />
Background<br />
In the last decade, the use of enteral feeding has expanded due to its advantages over parenteral<br />
nutrition. The choice and administration of medications through enteral feeding tubes (EFT) represents<br />
a challenge since it often requires crushing tablets and off-label use which can cause adverse<br />
drug events (ADE). Purpose of our study was evaluation of prescription, dispensing and administration<br />
of medications to patients with EFT and assessment of the impact of pharmacist interventions<br />
on the frequency of medication errors (ME) and preventable ADE.<br />
Methods<br />
A prospective randomised control trial including 60 patients with EFT was performed in July and August<br />
2010 in a general hospital in Lisbon. In the intervention group, the appropriateness of drug therapy<br />
was assessed daily by the researcher according to selected literature on medication<br />
administration via EFT and specific interventions were suggested by pharmacists. Patients in the observation<br />
group were subjected to usual drug therapy check. For both groups, identified medication<br />
errors were recorded and compared ans potential ADEs assessed.<br />
Results<br />
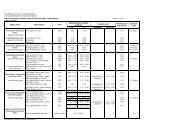
Figure 1. Comparison of main clinical outcomes between control and intervention group<br />
Incorrect doses administrated<br />
(N, mean per patient per day)<br />
151 (0.6) 19 (0.1) p < 0.01<br />
Non-doubtful ADEs<br />
(N, per 100 patients)<br />
8 (27) 1 (3) p < 0.01<br />
ADEs of at least moderate severity<br />
(N, per 100 patients)<br />
8 (27) 0 (0) p < 0.01<br />
* The results are based on 100 % interventions acceptance rate. In practice, acceptance rate was 77 %.<br />
22<br />
Control group Intervention group* Statistical analysis<br />
Prescribing errors (N, %) 20/183 (11 %) 15/190 (8 %) p = 0.49<br />
Dispensing errors (N, %) 13/183 (8 %) 1/190 (0.5 %) p < 0.01
The intervention group had a significantly lower number of dispensing errors (t-test, p
Comprehensive medication history:<br />
the need for the implementation<br />
of medication reconciliation processes<br />
Lea Knez 1 , Renata Reæonja 1,2 , Stanislav Øuøkoviœ 1 , Mitja Koønik 1 , Aleø Mrhar 2<br />
1<br />
Faculty of Pharmacy, University of Ljubljana<br />
2<br />
University Clinic of Respiratory and Allergic Diseases, Golnik<br />
Background<br />
Comprehensive medication history (CMH) is of outmost importance for patient evaluation and prescription<br />
of drug treatment upon hospital admission. The aim of this study was to assess the need<br />
for the implementation of medication reconciliation processes into clinical practice.<br />
Method<br />
Patients admitted to a teaching hospital in Slovenia were randomly selected and included in the<br />
study. For every patient a CMH was obtained by a research pharmacist using different sources of information.<br />
Next, medication history in the hospital medical record was reviewed. Prescription of medicines<br />
was assessed for completeness of information and discrepancies between both medication<br />
histories were recorded and classified.<br />
Results<br />
Overall, 108 patients with a median age of 73 years were included. The research pharmacist recorded<br />
the use of 651 medicines, of which 94.9% provided all relevant details for drug identification and administration.<br />
Less medicines (464) were recorded in the hospital medical record as compared to the<br />
CMH (paired t-test, p>0.001) and only 42.0% of these medicines were evaluated as complete. When<br />
comparing the medication history in the medical record with the CMH, at least one discrepancy was<br />
detected in 72.4% of medicines and was often present in the medication order on the drug chart<br />
(76.2%) and in the discharge letter (69.9%). Discrepancies often arose due to medicine’s omission<br />
(20.9%) and medicine’s commission (6.5%).<br />
Conclusions<br />
The high rate of discrepancies between the recorded drug history and CMH reported in our study<br />
shows the need for implementation of medication reconciliation practices. Pharmacists’ participation<br />
in admission reconciliation, as described in this study, led to more complete and accurate drug<br />
histories. In the study hospital, pharmacist-led CMH have been introduced in a research framework<br />
within which the benefits of this service for the reduction of medication errors and adverse drug<br />
events are being studied against routine practice in a randomised trial.<br />
24
Implementation of a medication<br />
reconciliation service at hospital<br />
admission: results from<br />
a randomised control study<br />
Lea Knez 1 , Stanislav Øuøkoviœ 1 , Anja Primoæiœ 2 ,<br />
Raisa Laaksonen 3 , Maja Joøt 1 , Mitja Koønik 1 , Aleø Mrhar 2<br />
1<br />
University Clinic of Respiratory and Allergic Diseases, Golnik<br />
2<br />
Faculty of Pharmacy, University of Ljubljana<br />
3<br />
Faculty of Pharmacy, University of Helsinki<br />
Background<br />
Medication errors (ME) resulting from poor communication when patients are transferred across the<br />
healthcare interface are a frequent cause of adverse drug events (ADE). Medication reconciliation: the<br />
process of verifying medication use, identifying variances, and preventing errors, has been introduced<br />
as a measure to improve patient safety. This randomised controlled study was undertaken to assess the<br />
effects of a medication reconciliation service at hospital admission on the reduction of MEs and ADEs.<br />
Methods<br />
Patients admitted to an internal medical ward were randomly selected and randomised to the intervention<br />
group, offered a medication reconciliation service within the first four days of hospital admission, or<br />
to the control group, offered routine clinical practice. A comprehensive medication history (CMH) was obtained<br />
for every patient, and the number of ME, defined as any unintentional discrepancies between the<br />
CMH and the prescribed drug therapy, the resulting ADE and their severity was determined as a consensus<br />
of a medical doctor and a clinical pharmacist, blinded for patient’s group allocation.<br />
Results<br />
A total of 120 patients (60 per group), of higher age (72 years) and with a median of seven medicines<br />
in their CMH were included in the study. In both groups, a discrepancy with a patient’s CMH was<br />
recorded for over 60% of drugs, prescribed on the second day of hospitalisation, and around 30%<br />
of these discrepancies represented a ME. For patients in the intervention group, the treating clinician<br />
was notified of all identified ME and reconciliation of prescribed therapy was proposed; however, this<br />
did not result in a significant reduction in the number of ME present on the fourth day of hospitalisation<br />
(in both groups around 65% of prescribed drugs presented a discrepancy, of which around 25%<br />
represented a ME), nor in the number and severity of ADE, experienced by patients. In both groups,<br />
around 20% of recorded ME resulted in an actual ADE that required temporary treatment.<br />
Conclusions<br />
The high number of MEs and ADEs resulting from poor CMH highlights the prosperity of this problem<br />
for patient safety. The implementation of medication reconciliation at hospital admission within<br />
25
a study setting did not reduce the number of ME nor ADE: the sole provision of the service cannot<br />
succeed in tackling this problem without its recognition and commitment by all the members of the<br />
healthcare team.<br />
26
Communication in palliative care:<br />
challenge for healthcare providers<br />
Urøka Lunder 1 , Maja Furlan 2<br />
1<br />
University Clinic of Respiratory and Allergic Diseases Golnik<br />
2<br />
Faculty of Arts, University of Ljubljana<br />
Background<br />
Effective communication is essential component of end-of-life care. The role of health care providers<br />
is considered to be as experts in their professional field and effecitve communicators who should explain,<br />
most often in layman’s terms, the situation to patients and their relatives. Open communication<br />
has gained increasing importance in recent years and sharing of prognostic information is now common<br />
place. Good communication skills are therefore of vital importance. In this study different health<br />
care professionals were surveyed about their communication skills. We examined whether health<br />
care providers are trained to break bad news and what are the challenges they face in their current<br />
practice of breaking bad news.<br />
Methods<br />
56 health care providers filled out a survey before the effective communication workshop.<br />
Results<br />
Majority of participants were physicians and nurses, with average age of 38 years. 57% had 15 years<br />
or less of work experience. More than half of the participants break bad news at least once a week,<br />
yet 79% of them have never received any training. Management of patients’ emotional reactions and<br />
answering difficult questions were two most common areas of difficulty, with hurting the patient and<br />
getting emotionally attached to the patient being two most common fears while communicating bad<br />
news.<br />
Conclusions<br />
Results suggest knowledge (practical as well as theoretical), organizational resources and personal<br />
growth and development are required to be competent in breaking bad news. Besides the challenges<br />
covered in our survey, participants highlited the burdensome residuals of open communication<br />
with patients, e. g. feelings of guilt and emotional attachement to the patient.<br />
27
Patients referred to Laboratory<br />
for sleep related breathing disorders:<br />
our 5 year experience<br />
Kristina Ziherl, Irena Øarc, Jasmina Gabrijelœiœ<br />
University Clinic of Respiratory and Allergic Diseases Golnik<br />
Background<br />
Sleep-disordered breathing (SDB) is a common medical condition affecting at least 5% of population<br />
and by some studies up to 20%. SDB is associated with much co-morbidity, especially with cardiovascular<br />
disease (CVD) and metabolic syndrome. There are no epidemiological studies of SDB<br />
in Slovenia. Aim of study was to describe basic characteristics of patients referred to laboratory for<br />
SDB and comparison of characteristics between patients without SDB and patients with obstructive<br />
sleep apnea syndrome (OSAS) and obesity hypoventilation syndrome (OHS).<br />
Methods<br />
We screened all initial diagnostic hospitalizations in laboratory for SDB, University Clinic Golnik, between<br />
October 2005 and October 2010. Medical records were reviewed for clinical characteristics<br />
and laboratory results. Statistical analysis was performed by SPSS 17.0.<br />
Results<br />
During five years of the study we performed diagnostic polisomnography in 1102 patients (age 53+/-<br />
11 years, 22% women). ESS score was significant (>10 points) in 51% of patients. 91% patients had<br />
BMI ≥25 kg/m 2 and 62% ≥ 30 kg/m 2 . Men were younger, had lower BMI, higher ESS and AHI and<br />
women more often had hypothyrosis, depression and asthma (p
tients with OHS were treated with CPAP (69%), BiPAP (14%) and LTOT (12% alone and 8% in combination<br />
with CPAP). Average CPAP pressure in patients with OSAS was 10.24 +/- 2.8 cmH2O and<br />
in patients with OHS 11.62 +/- 2.7 cmH2O (p
Pulmonary rehabilitation program –<br />
our results<br />
Tomaæ Hafner, Jurij Øorli<br />
University Clinic of Respiratory and Allergic Diseases Golnik<br />
Background<br />
Chronic obstructive pulmonary disease (COPD) is a chronic disease which through systemic inflammation<br />
and physical inactivity because of dyspnea leads to muscle wasting and atrophy. Rehabilitation<br />
improves patients’ physical performance and consequently their ability to perform everyday<br />
tasks and their quality of life. That is why physical rehabilitation of COPD patients is very important<br />
in long term management of COPD. In our hospital we have four week long pulmonary rehabilitation<br />
program (PRP) for COPD patients.<br />
Methods<br />
We retrospectively searched through medical records of patients who underwent our PRP from years<br />
2006-2010 for results of maximal inspiratory and expiratory pressure (MIP & MEP), distance walked<br />
on shuttle and 6 minute walk tests (SWT & 6MWT) before and after PRP. Not all patients performed<br />
all tests. Data are presented as mean, standard deviation and p value from paired-samples T test.<br />
We wondered how efficient our PRP was and how much patients physically improved.<br />
Results<br />
71 patients (46 man and 25 women) with average age of 65,8 +/- 9,0 years were included in this<br />
study. They were mostly COPD stage 3 and 4 according to GOLD with average FEV1 33,8% +/-<br />
14,1%. Average MIP before PRP was 62,8 +/- 22,2 cm H2O. After PRP increased to 73,9 +/- 22,4 cm<br />
H2O which reached statistical significance with p 0,024. Average MEP before PRP was 107,4 +/-<br />
47,4 cm H2O. After PRP increased to 126,0 +/- 46,5 cm H2O with p 0,009. Achieved walking distance<br />
on SWT before PRP was 224,3 +/ -120,3 m. After PRP increased to 263,5 +/- 139,0 m with p 0,000.<br />
Achieved walking distance on 6MWT before PRP was 287,6+/-124,8m. After PRP increased to 353,3<br />
+/- 133,6 m with p 0,000.<br />
Conclusions<br />
Physical rehabilitation of COPD patients importantly increases their measurable physical performance<br />
which consequently improves their everyday functionality and quality of life.<br />
30
Videothoracoscopic resection<br />
of giant emphysema bullae<br />
Katja Adamiœ 1 , Nika Lalek 1 , Tomaæ Øtupnik 2<br />
1<br />
University Clinic of Respiratory and Allergic Diseases Golnik<br />
2<br />
Clinical Department of Thoracic Surgery, University Medical Centre Ljubljana<br />
Background<br />
The most common indications for resection of giant emphysema bullae (GEB - large bulla occupying<br />
at least 30 percent of the hemithorax) are severe dyspnoea, compression of the surrounding normal<br />
lung and secondary spontaneous pneumothorax. Excision of a GEB reduces airway resistance,<br />
functional residual capacity and physiologic dead space. Physiologic outcome after surgery is determined<br />
mostly by the size of the bulla (preferably > 50% of the hemithorax) and the severity of the<br />
underlying emphysema as the patients with severe generalized emphysema tend to have a worse<br />
outcome. The surgical risk is increased when forced expiratory volume in first second (FEV1) is less<br />
than 40% of the predicted (FEV1 < 20% is an absolute contraindication for surgery) (1, 2).<br />
GEB can be removed using open or videothoracoscopic technique (VATS). VATS is technically more<br />
complex, but provides the best preservation of lung function in early postoperative period, thus it is<br />
most beneficial for patients with reduced pulmonary reserve (3).<br />
Methods<br />
In 2010, we have used the three-incision VATS technique on two patients with GEB. All bullae were<br />
opened longitudinally and resected at their base using a 60 mm long endoscopic stapler.<br />
Clinical case 1. A 57-year old male with a non-small cell lung cancer in the left upper lobe<br />
(cT2bN1M0) and a GEB in the apex of the right upper lobe (FEV1 61%, forced vital capacity (FVC)<br />
101%) had undergone an uncomplicated VATS left upper lobectomy Several months later the GEB<br />
grew to almost 50% of the hemithorax and the patient became severely dyspnoeic (Medical Research<br />
Council dyspnea score (MRC) 4, FEV1 46%, FVC 61%). The bulla was resected eight months<br />
after the lobectomy without any further complications. Two weeks after surgery, the patient was capable<br />
of normal efforts (MRC 1, FEV1 65%, FVC 79%).<br />
Clinical case 2. A 53-year old female presented with the first spontaneous pneumothorax and was<br />
initially treated with a chest tube. Computed tomography revealed severe centrilobular emphysema<br />
and two GEBs in the left upper and lower lobe. Two weeks after discharge the pneumothorax recurred.<br />
Chest tube was inserted to relieve severe dyspnoea and she was scheduled for surgery two<br />
days later. Both GEBs were resected using the VATS technique and a mechanical pleurodesis was<br />
performed. Postoperative recovery was uneventful. A month after surgery, she is capable of normal<br />
efforts (MRC 1) with improved pulmonary function: FEV1 from 25% to 50% and FVC from 51% to<br />
60%.<br />
31
Conclusions<br />
VATS resection of GEB using modern 60 mm staplers is a relatively easy and very effective technique.<br />
In our patient with synchronous lung cancer and a GEB, reverse order of the interventions would<br />
have been more appropriate: removal of the GEB on the right side followed by a lobectomy on the<br />
left side a month later. The patient with secondary spontaneous pneumothorax should have been<br />
scheduled for surgery at her first occurrence of pneumothorax.<br />
References<br />
1. Nickoladze GD. Functional results of surgery for bullous emphysema. Chest 1992; 101:119.<br />
2. FitzGerald MX, Keelan PJ, Cugell DW, Gaensler EA. Long– term results of surgery for bullous emphysema. J<br />
Thorac Cardiovasc Surg 1974; 68:566.<br />
3. Wakabayashi A. Thoracoscopic technique for management of giant bullous lung disease. Ann Thorac Surg<br />
1993; 56:708.<br />
32
Electrocardiogram analysis<br />
of patients with chronic obstructive<br />
pulmonary disease<br />
Miha Zabret, Urøa Boneø, Irena Øarc, Mitja Koønik, Stanislav Øuøkoviœ, Mitja Lainøœak<br />
University Clinic of Respiratory and Allergic Diseases, Golnik<br />
Background<br />
Morbidity and mortality from chronic obstructive pulmonary disease (COPD) is increasing worldwide<br />
and cardiovascular disease contributes significantly. Standard electrocardiogram (ECG) provides<br />
wealth of general and COPD specific information which can serve for patient risk stratification. We<br />
aimed to assess the presence of ECG changes and to analyze potential associations with long-term<br />
mortality.<br />
Methods<br />
This retrospective cohort study included 1001 patients with COPD, hospitalized in University clinic<br />
Golnik between years 2002-2007. ECGs were analyzed by three independent investigators. Next to<br />
standard assessment and measurements, particular attention was given to COPD associated<br />
changes (e.g. P-pulmonale, right heart axis, right ventricular hypertrophy and right bundled branch<br />
block) and parameters associated with prognosis (prolonged QTc interval - 120ms). The survival was ascertained with Central population registry and the database was<br />
censored on November 1st, 2008.<br />
Results<br />
Most of our patients had severe or very severe COPD (63%). They were mostly male (72%), aged 70<br />
± 9 years on average. At least one COPD typical ECG change was present in 33% of patients (P-pulmonale<br />
9%, right heart axis 11%, right ventricular hypertrophy 17%, right bundle branch block 8%)<br />
and correlated with GOLD stage (p
Implications of sputum bacteriology<br />
in acute exacerbations of chronic<br />
obstructive pulmonary disease<br />
Irena Øarc, Viktorija Tomiœ, Mitja Lainøœak,<br />
Kristina Ziherl, Tina Jeriœ, Mitja Koønik, Stanislav Øuøkoviœ<br />
University Clinic of Respiratory and Allergic Diseases, Golnik<br />
Background<br />
Pathogenic bacteria have been implicated as a causative agent in majority of episodes of acute exacerbation<br />
of COPD (AECOPD). We aimed to investigate sputum bacteriology and prognostic implications<br />
of sputum results in AECOPD.<br />
Methods<br />
We conducted a retrospective study of consecutive patients admitted to University Clinic Golnik with<br />
AECOPD from 2002 to 2007. The diagnosis of COPD, sputum bacteriology and clinical characteristics<br />
of patients were confirmed with detailed review of complete medical records. Only the initial hospitalization<br />
of patients with quality sputum was included in the study. Vital status was obtained from<br />
Central Population Registry.<br />
Results<br />
Final sample consisted of 697 patients (age 70 ±9 years, 75% men, 65% GOLD III/IV). Most frequently<br />
isolated pathogens were H.influenzae (19.4%), P. aeroginosa (14.9%) and S. pneumoniae (11.8%). The<br />
isolation of S. pneumoniae (p=0.009), P. aeroginosa (p=0.01), non-fermenting Gram negative bacilli<br />
(p
of COPD but not in the severity of exacerbation. Isolation of multiple pathogens was associated with<br />
negative outcomes at 6 months.<br />
35
Antibiotic treatment during<br />
hospitalization due to acute<br />
exacerbation of chronic obstructive<br />
pulmonary disease<br />
Urøa Boneø, Irena Øarc, Kristina Ziherl, Miha Zabret, Tina Jeriœ,<br />
Viktorija Tomiœ, Mitja Koønik, Stanislav Øuøkoviœ, Mitja Lainøœak<br />
University Clinic of Respiratory and Allergic Diseases, Golnik<br />
Background<br />
Antibiotic treatment during acute exacerbation of chronic obstructive pulmonary disease (AECOPD)<br />
remains controversial. Due to lack of information about antibiotic use in clinical practice, this study<br />
investigated therapeutic pattern and association with prognosis.<br />
Methods<br />
In our retrospective cohort study, we screened all consecutive discharges between 2002 and 2007.<br />
We reviewed medical charts for presence of AECOPD, sputum sample and in-hospital management.<br />
The survival was ascertained with Central population registry.<br />
Results<br />
We included 679 patients (age 70 ±9 years, 75% men, 65% GOLD III/IV). Antibiotics were prescribed<br />
to 560 (80%) patients, who had more advanced COPD stage (GOLD III/IV 69% vs. 57%, p
Examination of resistance of bacteria<br />
isolated from sputum and partial<br />
broncoalveolar lavage in Clinic<br />
for lung disease, Knez Selo<br />
Nastasijeviå Borovac Desa, Tatjana Pejœiå,<br />
Tatjana Radjenoviå Petkoviå, Djordjeviå Ivanka, Ranœiå Milan<br />
Clinic for lung disease, Knez Selo, Clinical Center Niø, Serbia<br />
Background<br />
Due to irrational antibiotic use, a growing bacterial resistance has been noted worldwide, including<br />
our environment. Resistant and multiresistant bacterial strains pose one of the greatest therapeutic<br />
problems. The aim of this study was to present the sensitivity and resistance of bacteria isolated from<br />
sputum and partial broncholaveolar lavage of patients treated in the Clinic for Lung Diseases, Knez<br />
Selo, Serbia, in the period April 1, 2010 - April 1, <strong>2011</strong>.<br />
Methods<br />
Resistance was examined by disk diffusion method. The results are shown in percents, by groups<br />
including at least 40 isolated bacteria.<br />
Results<br />
From 2012 sputum samples were isolated 403 (20,03%) bacteria, and 49(12,44%) bacteria from 394<br />
partial broncholaveolar lavage. The following bacteria were isolated: Pseudomonas aeruginosa 87<br />
(19,24%), Staphylococcus (aureus, epidermidis) 67 (14,83%), Serratia 60 (13,28%), Streptococcus<br />
(pyogenes, faecalis, and haemoliticus) 45 (9,96%), Streptococcus pneumoniae 42 (9,3%), Escherichia<br />
coli 40 (8,85%). Other bacteria (Providencia, Proteus, Acinetobacter, Citrobacter, Haemophyllus<br />
influencae, Klebsiela, Enterobacter, Moraxella catarralis) were isolated in a number insufficient<br />
for statistical processing. Gram-negative bacteria were isolated in 65,92% of cases. P.aeruginosa<br />
showed high resistance to cefotaksim (94,25%), trimetoprim-sulfametoksazol (86,04%) and sensitivity<br />
to ciprofloxacin (84,9%), ceftazidim (75,8%) and amikacin (74,7%). Staphylococcus showed preserved<br />
sensitivity to cefuroksim (96,6%), trimetoprim-sulfametoksazol (88,7%), ciprofloxacin (83,3%)<br />
and eritromicin (74,6%), but high resistance to penicillin G (88,7%) and sinacillin (82,9%). Serratia<br />
showed high resistance to amikacin (57,8%) and ceftrikson (50,0%), lower resistance to ciprofloksacin<br />
(29,6%), and high sensitivity to carbapenems (93,1%). Streptococcus (pyogenes, faecalis, and<br />
haemoliticus) was sensitive to penicillin G (97,6%), cefuroksim (97,36%), and ciprofloksacin (95,8%)<br />
but highly resistant to trimetoprim-sulfametoksazol (97,22%). Streptococcus pneumoniae was sensitive<br />
to penicillin G (100%), cefuroksim (97,36%), but resistance to eritromicin (51,3%) and trimetoprim-sulfametoksazol<br />
(86,6%). Escherichia coli was sensitive to ciprofloksacin (89,19%),<br />
trimetoprim-sulfametoksazol (89,5%) and ceftazidim (75,0%), but resistance to ceftriakson (32,5%)<br />
and amikacin (61,1%). Gram-negative bacteria dominated among the isolates. A growing resistance<br />
37
of gram-positive bacteria to macrolides was noted, but also the resistance of gram-negative bacteria<br />
to aminoglycosides, penicillins and cephalosporines.<br />
Conclusions<br />
Since Serbia is not an active member of EARSS (European Antibiotic Resistance Surveillance System),<br />
knowing the local resistance can considerably affect a modality of empirical therapy.<br />
38
Pneumococcal bacteriemia in adults<br />
with community-acquired pneumonia<br />
Katja Adamiœ, Mateja Polajnar, Franc Øifrer, Viktorija Tomiœ<br />
University Clinic for Respiratory and Allergic Diseases, Golnik<br />
Background<br />
Streptococcus pneumoniae (SP) is the most common cause of community-acquired pneumonia<br />
(CAP). Complications of CAP are pleural effusion, empyema, lung abscess and metastatic infection<br />
in patients with bacteremia. Appropriate antibiotic therapy should be initiated as soon as possible<br />
after diagnosis. To establish SP as an aetiologic agent of CAP cultivation and isolation of the bacterium<br />
from patients’ blood cultures (BC) and respiratory specimens should be performed. Also detection<br />
of the pneumococcal antigen (Ag-SP) in urine samples can be used.<br />
Methods<br />
We performed a retrospective analysis of hospital records of patients with pneumococcal bacteremia<br />
admitted to University Clinic Golnik between January 1, 2003 and December 31, 2009. We collected<br />
demographic data, signs and symptoms on admission, laboratory results (C-reactive protein (CRP),<br />
white blood count (WBC), urea, creatinine, etc), microbiological testing results, smoking habits, associated<br />
diseases, antibiotic therapy, use of steroids, vaccination status.<br />
Results<br />
Pneumonia with pneumococcal bacteremia was observed in 139 patients (79 men and 60 women),<br />
mean age was 66 years (range 19 to 95 years). Seventy-five percent of patients had at least one associated<br />
chronic disease, mainly hypertension (43%), diabetes type 2 (24%) and COPD (20%). Eighteen<br />
patients had associated malignant diseases and 2 had confirmed HIV infection. Twelve percent<br />
were alcohol dependent, 26% active smokers, 22% former smokers. Fourteen percent of patients<br />
were receiving inhaled or systemic steroids. No patient had documented information on vaccination<br />
against SP, one patient was advised vaccination at discharge. Most commonly reported sings and<br />
symptoms at admission were cough, dispnea, chest pain, fever and chills with 8% of patients having<br />
haemoptysis. Sixty-three percent of patients were hypoxemic and 25% were hypotensive. Average<br />
admission values of laboratory tests were CRP 260mg/L, WBC 14x10 9 /L (less than 4.0x109/L in<br />
12 patients), haemoglobin (Hb) 124g/L, glucose 8.2 mmol/L, urea 11.3 mmol/L, creatinine 125 µmol/L.<br />
In 10% of patients SP was isolated from sputum, in 9% urine Ag-SP was positive. In 14% of patients<br />
pleural effusion was present (empyema in 5 patients). As empirical antibiotic treatment 51% of patients<br />
received amoxicillin with clavulanic acid, 7% received co-amoxiclav and macrolide, 4% penicillin<br />
and 17% respiratory quinolones. In 30% of patients the empiric antibiotic treatment was changed<br />
to penicillin on account of microbiological results. Twenty-three percent of patients needed haemo-<br />
39
dynamic support with dopamine, 12% had to be intubated and mechanically ventilated. Average duration<br />
of hospitalization was 15 days with 31% of patients treated in the intensive care unit (ICU) for<br />
an average of 9 days. From 139 patients 15% died during hospitalization, 7% during the first 3 days.<br />
Conclusions<br />
According to the national recommendations for the treatment of patients with CAP, patients with<br />
pneumococcal bacteremia who meet the criteria for severe CAP 1 should be initially treated in ICU.<br />
In our retrospective analysis 31% of patients were treated in ICU. To curb the development of pneumococcal<br />
resistance replacement of empirically introduced antibiotic with penicillin after receiving<br />
the microbiological test results should be encouraged. Patients with certain associated diseases and<br />
clinical conditions 1 should be advised to receive pneumococcal vaccine after they recover from CAP.<br />
Literature:<br />
1. E. Muøiœ, K.Osolnik, V. Tomiœ, R. Eræen, M. Koønik et al: Recommendations for the Management of Community-acquired<br />
Pneumonia in Adults (Updated and revised Edition, 2010), Zdrav Vestn 2010;79: 245–264<br />
40
Aspergillosis<br />
Tina Jeriœ, Izidor Kern, Petra Svetina Øorli<br />
University Clinic of Respiratory and Allergic Diseases, Golnik<br />
Background<br />
Aspergillus species are ubiquitous in nature and inhalation of infectious conidia is a common event.<br />
Aspergillus causes a spectrum of disease, from colonization to hypersensitivity reactions to chronic<br />
necrotizing infections to rapidly progressive angioinvasion, often resulting in death. Tissue invasion<br />
is uncommon and occurs most frequently in patient with immunosuppression (neutropenia, transplanted<br />
organ). Aspergillus fumigatus is the most common etiological agent of human aspergillosis.<br />
Case report<br />
We present a case of 55 years old male, ex smoker, with asthma and emphysema, who was treated<br />
with inhaled corticosteroids for at least 10 years. On his last admission to our hospital he presented<br />
with shortness of breath, fever, productive cough, and bilateral apical inifiltrates on chest X-ray. Despite<br />
aggressive empiric antibiotic treatment systemic inflammatory response syndrom developed<br />
and the patient died because of cardiorespiratory failure. Post mortem besides pulmonary thrombembolia<br />
chronic necrotizing pulmonary aspergillosis was found.<br />
Conclusions<br />
Aspergillus conidia are frequently inhaled into the airways but in most cases do not cause the disease<br />
because of the effective clearance. Culture isolation of Aspergillus species from the airway<br />
does not necessarily indicate disease. The diagnosis of invasive aspergillosis is based upon both isolating<br />
the organism and the probability that is the cause of disease. Culture of Aspergillus species<br />
in combination with the histopathological demonstration of tissue invasion provides definite evidence<br />
for invasive aspergillosis. So although invasive Aspergillus infection is rare it should be considered<br />
when the disease is resistant to broad-spectrum antibiotics in immunocompromised patient.<br />
41
Use of multiplex PCR for detection of<br />
bacterial respiratory tract pathogens<br />
Dane Luænik, Judit Stokiå, Viktorija Tomiœ, Franc Øifrer<br />
University Clinic of Respiratory and Allergic Diseases, Golnik<br />
Background<br />
To investigate the usefulness of multiplex polymerase chain reaction (mPCR) to detect Mycoplasma<br />
pneumoniae, Legionella pneumophila, and Chlamydophila pneumoniae in patients with suspected<br />
atypical community-acquired pneumonia and to assess the prevalence of Streptococcus pneumoniae<br />
and Haemophilus influenzae detection.<br />
Methods<br />
We evaluated retrospectively the results of mPCR in 210 patients asigned to 3 groups: patients with<br />
suspected atypical pneumonia (n = 110), patients with asthma (n = 27), and patients with diseases<br />
other than infection (heart failure, malignancy, pulmonary embolism, allergic reactions) (n = 73) admitted<br />
to University Clinic of Respiratory and Allergic Diseases Golnik between January 2010 and January<br />
<strong>2011</strong>.<br />
Results<br />
An atypical pathogen was detected only in the 26 patients in suspected atypical pneumonia group<br />
(23.6%). L. pneumophila was detected in 4 patients (3.6%), M. pneumoniae in 21 (19%), and C.<br />
pneumoniae in 1 patient (0.9%). No pathogen could be detected by mPCR in 24 (21.8%), 2 (7.4%),<br />
and 49 (67%) patients in suspected atypical pneumonia group, asthma, and other diseases group,<br />
respectively. In patients with suspected atypical pneumonia S. pneumoniae and H. influenzae were<br />
detected 61.8% and 30% patients, respectively. In asthmatic patients S. pneumoniae and H. influenzae<br />
were detected in 81.5% and 51.8%, respectively. In patients with other diseases S. pneumoniae<br />
and H. influenzae were detected in 31.5% and 23%, respectively.<br />
Conclusions<br />
mPCR can increase the number of microbiological detection of atypical pathogens in patients with<br />
suspected community-acquired pneumonia. Clinical relevance of positive mPCR for S. pneumoniae<br />
and H. influenzae is questionable since it cannot distinguish between colonization and infection and<br />
thus, further studies are needed.<br />
42
Carriage rate of extended-spectrum b-<br />
lactamase producing Enterobacteriaceae<br />
and methicillin-resistant Staphylococcus<br />
aureus in elderly on admission to the<br />
nursing home<br />
Katja Øinkovec 1 , Dane Luænik 2 , Jelka Œernivec 3 , Viktorija Tomiœ 2<br />
1<br />
Faculty for Biotechnology, Ljubljana – Department of Microbiology,<br />
2<br />
University Clinic of Respiratory and Allergic Diseases, Golnik,<br />
3<br />
Nursing Home Danice Vogrinec, Maribor<br />
Background<br />
Resistant bacteria are a major public health concern. With population aging more people are admitted<br />
to nursing homes which are presumed to be reservoirs of resistant bacteria. Reports on prevalence<br />
of extended-spectrum b-lactamase producing Enterobacteriaceae (ESBL-E) and<br />
methicillin-resistant Staphylococcus aureus (MRSA) are few in number. We wanted to determine the<br />
carriage rate of both pathogens in elderly on admission to the largest nursing home in Slovenia.<br />
Methods<br />
A survey was conducted prospectively from January 10 to June 1, <strong>2011</strong> in the Danica Vogrinec nursing<br />
home in Maribor which has 809 beds. All future residents were screened for carriage of ESBL-E<br />
and MRSA on admission. To assess carriage of MRSA nose, throat, rectal, wound (when present)<br />
swabs and for carriage of ESBL-E rectal, wound (when present) swabs and urine samples (when urinary<br />
catheter was inserted) were collected. All swabs were inoculated into brain-heart infusion broth.<br />
After 24 h of incubation, broths were subcultured onto BBL CHROMagar MRSA (BD, USA) and Brilliance<br />
ESBL agar (Oxoid, UK). Urine samples were inoculated directly onto Brilliance ESBL agar plates.<br />
Suspected colonies of MRSA and ESBL-E were identified by standard laboratory procedures.<br />
Results<br />
Screening samples were collected from 87 elderly future residents, 62 females (71.%) and 25 males<br />
(28.7%). Mean age was 79 years (range 35 – 97 years). We detected 14 residents (16%) colonized with<br />
ESBL-E (11 female and 3 male) residents and no resident colonized with MRSA on admission. Mean<br />
age of colonized residents was 79.5 years (range 68 – 89 years). Twenty-seven future residents (31%)<br />
were transfered from hospitals, 15 (17%) were transfered from other nursing homes and 45 (52%) were<br />
admitted from home environment. Of the 14 colonized residents 2 (14.3%) were admitted from home,<br />
9 (64.3%) were transfered from hospital and 3 (21.6%) were transfered from other nursing homes.<br />
Conclusions<br />
Due to implemented infection control program to control the spread of MRSA in hospitals MRSA is<br />
not our primary problem anymore. More efforts should be directed to control the spread of ESBL-E<br />
in hospitals, nursing homes as well as in the community.<br />
43
Methicillin-resistant Staphylococcus<br />
aureus and extended-spectrum b-<br />
lactamase producing<br />
Enterobacteriaceae in house pets<br />
Katja Øinkovec 1 , Dane Luænik 2 , Zlata Œop 3 , Viktorija Tomiœ 2<br />
1<br />
Department of Microbiology, Faculty for Biotechnology, University of Ljubljana<br />
2<br />
University Clinic of Respiratory and Allergic Diseases, Golnik<br />
3<br />
Veterinary Clinic, Lesce<br />
Background<br />
Resistant bacteria are a major public health concern. Methicillin-resistant Staphylococcus aureus<br />
(MRSA) is a major pathogen in human medicine and has become a recognized problem in farm animals<br />
(e.g. pigs). Pet owners as well as veterinary doctors and assistants can be colonized with<br />
MRSA and/or with entended-spectrum b-lactamase producing Enterobacteriaceae (ESBL-E) and<br />
they could transfer the pathogens to their pets through direct contact. We wanted to determine the<br />
carriage rate of both pathogens in house pets attending a busy veterinary clinic in Lesce (NW Slovenia).<br />
Methods<br />
A survey was conducted prospectively from February 1 to May 1, <strong>2011</strong> Veterinary Clinic Lesce.<br />
House pets, mainly cats and dogs were screened for carriage of ESBL-E and MRSA on a visit to the<br />
clinic. To assess carriage of MRSA nose and rectal swabs and for carriage of ESBL-E only rectal<br />
swabs were collected. All swabs were inoculated into brain-heart infusion broth. After 24 h of incubation,<br />
broths were subcultured onto BBL CHROMagar MRSA (BD, USA) and Brilliance ESBL agar<br />
(Oxoid, UK). Suspected colonies of MRSA and ESBL-E were identified by standard laboratory procedures.<br />
Results<br />
Screening samples were collected from 100 house pets, 42 cats (42%), 57 dogs (57%) and 1 guinea<br />
pig. Also nasal screening swabs for MRSA detection were collected from 6 veterinary workers (2 veterinary<br />
doctors and 4 assistants). We detected only 1 cat colonized with ESBL-E and no house pets<br />
colonized with MRSA. All screened employees of the veterinary clinic were free of MRSA.<br />
Conclusions<br />
Carriage of resistant bacteria in screened group of house pets was minimal. Since resistant bacteria<br />
can be easily transferred from owners to pets and vice versa periodic surveillance would seem<br />
reasonable.<br />
44
Screening of persons after contact<br />
with a TB patient in the Shelter<br />
for the homeless<br />
Petra Svetina Øorli, Katja Pivk, Andraæ Jakelj<br />
University Clinic of Respiratory and Allergic Diseases, Golnik<br />
Background<br />
To prevent spreading the infection with tuberculosis (TB) in countries with low incidence of TB it is<br />
very important to screen people who were in contact with a TB patient. A contact person is defined<br />
as a person who was in close contact with a patient during his active phase of TB. 10% of infected<br />
contact persons will develop an active TB. Risk factors for infection are alcoholism, smoking, addiction<br />
to intravenous drugs, cachexia, chronic illnesses, and congenital or acquired imunnodeficiency.<br />
Methods<br />
We analyzed the data obtained from homeless persons who were several weeks in daily contact with<br />
a microscopically positive pulmonary TB patient living in the shelter for the homeless. The goal was<br />
to determine the incidence of both latent TB infection (LTBI) and active disease. This data was compared<br />
to the data from a Slovene retrospective study of contact persons in which the incidence of<br />
LTBI was 15% and of active disease 0.7%. 22 homeless people who were in contact with a TB patient<br />
were invited for an examination. Sputum samples for M. tuberculosis were obtained and physical<br />
exam, chest X-ray and QuantiFERON test (QFT) were done.<br />
Results<br />
18 (82%) out of 22 invited homeless person from the shelter actually came for the examination. They<br />
were all unemployed and had never been treated for TB. Cough was present in 3 persons, other<br />
were symptomless. Only 2 chest X-rays were not normal. From each person sputum was obtained<br />
and they were all microscopically negative for TB. Only one (5.5%) person had culture-positive TB<br />
and standard antituberculosis therapy was initiated. In other 17 persons without TB QFT was done<br />
and in 10 (55.5%) of them latent TB infection was confirmed and 3 months chemoprofilactic therapy<br />
was initiated.<br />
Conclusions<br />
Only one (5.5%) of examined homeless contact person from the shelter had culture-positive pulmonary<br />
TB and was treated with standard regime of anti-TB therapy. In 10 (55.5%) of examined persons<br />
LTBI was confirmed. The number of patients with latent infection and active disease in homeless<br />
contact persons is higher than in general population of contact persons. In order to detect and prevent<br />
spreading the infection with M. tuberculosis examination of persons with history of contact with<br />
a TB patient, especially from high risk groups of the population, is very important.<br />
45
Occurrence of tuberculosis in largest<br />
Slovenian correctional facility ZPKZ<br />
Dob in the period from 2000 to 2008<br />
Nadja Koren Pucelj 1 , Irena Hudoklin 2<br />
1<br />
University Medical Centre, Ljubljana<br />
2<br />
Out-patient Practice for Respiratory Diseases, Trebnje<br />
Background<br />
Inmates are known to be more vulnerable to infection with tuberculosis (TB) compared to general population<br />
(crowded environment, presence of persons of low socioeconomic status, foreign-born individuals,<br />
users of illicit substances, persons with human immunodeficiency virus infection). According<br />
to the Slovenian national central register TB did not occur often in correctional facilities until 2000 (1-<br />
2 cases annually).<br />
Methods<br />
In 2000, after first symptomatic case was found, altogether four cases of pulmonary TB were detected<br />
in epidemiological investigation in largest Slovenian correctional facility ZPKZ Dob (ZPKZ<br />
Dob) with 345 male long term inmates. ZPKZ Dob had been overcrowded for many years (official capacity<br />
is 233 persons). As incidence of TB in general population was 18.9 per 100,000 inhabitants<br />
in the same year, the need for enhanced surveillance for TB in this correctional facility was recognized.<br />
Results<br />
From beginning of 2001 until the end of 2008 all new inmates were screened for symptoms of TB and<br />
had tuberculin skin test and chest x-ray carried out. On average 162 (min 118, max 210, SD 29,1)<br />
new inmates were examined annually (altogether 1251 in 8 years). All were male, on average 36,2<br />
years old (min 19, max 77, SD 10,4). In the period of eight years two cases of pulmonary TB (in 2002<br />
and in 2004) and one person with inactive TB and documented history of adequate treatment for TB<br />
were found. Furthermore 169 cases of latent TB infection, with tuberculin skin test more or equal 10<br />
mm, were detected. Both cases of active and 95,4% cases of latent TB infection (161 of 169) were<br />
treated with standard regimens for active and latent infection respectively.<br />
Conclusions<br />
We believe that the danger of outbreaks of TB in ZPKZ Dob was greatly reduced with treatment of<br />
active and latent TB among new inmates. We also recognize the need to implement the surveillance<br />
protocol for infection with TB among new inmates, already incarcerated inmates and correctional officers<br />
in all correctional facilities in Slovenia because the risk of TB is known to be higher in correctional<br />
facilities compared to general population. This is even more relevant for our country as for<br />
46
many years correctional facilities have been overcrowded and in last ten years 11-16% of inmates<br />
have been foreign-born (including those born in countries with high prevalence of TB and multidrugresistant<br />
TB).<br />
47
Pharmacist’s role in the treatment of<br />
patients with tuberculosis – our<br />
positive experience<br />
Janez Toni, Nanœa Œebron Lipovec, Petra Svetina Øorli<br />
University Clinic of Respiratory and Allergic Diseases, Golnik<br />
Background<br />
Tuberculosis as a disease demands long-term multidrug treatment. These drugs can cause serious<br />
adverse drug reactions, mostly hepatotoxicity, that can affect the course of therapy. Moreover,<br />
antituberculotic drugs interact with a variety of drugs, OTC preparations and food, all of<br />
which can significantly alter the effectiveness of patient’s antituberculotic and/or chronic therapy.<br />
Patient’s compliance and patient-tailored therapy are thus crucial for achieving effective<br />
treatment.<br />
Methods<br />
In the University Clinic Golnik, clinical pharmacists are included in the treatment of patients with tuberculosis.<br />
They teach patients on correct drug use and instruct them on the management of possible<br />
adverse drug events and perform drug therapy reviews. These most frequently include counseling<br />
on clinically important drug-drug interactions as well as recommendations on adjustments of drug<br />
doses according to patient’s renal and hepatic function. In <strong>2011</strong>, the collaboration of clinical pharmacists<br />
in the treatment of tuberculosis in our hospital was supported by the Health Insurance Institute<br />
of Slovenia.<br />
Results<br />
From June to August <strong>2011</strong> clinical pharmacists performed 29 drug therapy reviews on the tuberculosis<br />
department. The most frequent interventions included recommendations on drug-drug interactions.<br />
One of the most clinically important interactions of antituberculotic drugs occurs with<br />
warfarin: its effectiveness can be significantly reduced in concomitant use with rifampicin, requiring<br />
regular INR measurements and possibly a 2 to 5 fold increase in warfarin dose. Oral calcium<br />
preparations reduce the absorption of antituberculotic drugs from the GIT, whereas concomitant use<br />
of rifampicin and levothyroxine reduces the effectiveness of levothyroxine and requires regular<br />
measurement of thyroid hormones levels and possibly dose adjustment. The detected interactions<br />
and adjusted therapy were documented in the hospital electronic clinical files as well as in the patients’<br />
discharge documentation. This allowed the patient’s GP and local pulmonologist to be informed<br />
about the therapy adjustments and the need for readjustments at the end of antituberculotic<br />
treatment. Clinical pharmacists also performed individual patient counseling on correct drug use,<br />
adverse drug reactions, their prevention and treatment. In the selected period 17 individual counselings<br />
were performed.<br />
48
Conclusions<br />
The collaboration of different healthcare professional in the healthcare team at the University Clinic<br />
Golnik aims at ensuring high quality patient care. At the tuberculosis department, clinical pharmacists<br />
counsel to patients and advise on the management of clinically important interactions on a daily<br />
basis and thus constantly improve the high quality of patient care.<br />
49
A nation-wide study of nontuberculous<br />
mycobacteria in Slovenia<br />
Manca Æolnir Dovœ 1 , Nataøa Fajfar 1 , Irena Plesec 1 , Æiva Petroviœ 2 , Nada Øorli Peranoviœ 1<br />
1<br />
University Clinic of Respiratory and Allergic Diseases, Golnik<br />
2<br />
Institute of Public Health, Centre for Microbiology, Maribor<br />
Background<br />
Nontuberculous mycobacteria (NTM) are ubiquitous bacteria and are isolated from many environmental<br />
sources, most often from water and soil. They are capable of infecting and causing disease<br />
(mycobacteriosis) in both immunocompetent and immunocompromised hosts. HIV infection,<br />
previous chronic lung disease, cystic fibrosis, work in mining industry, advanced age, and male<br />
sex are the most frequent risk factors for the disease reported in several studies. Human infections<br />
caused by NTM have four major clinical manifestations: pulmonary disease, lymphadenitis, disseminated<br />
disease, and skin or soft tissue infections. The frequency of NTM diseases differs with<br />
regard to different geographical regions of the world. In general, cases of mycobacteriosis are on<br />
the rise in the last years. The aim of this study was to analyze laboratory diagnostics of NTM and<br />
NTM disease in the last eleven years (2000-2010) and to detect any changes in distribution of<br />
NTM in Slovenia.<br />
Methods<br />
Between 2000 and 2010, there were 3-6 laboratories in Slovenia that were performing laboratory diagnostics<br />
of tuberculosis and NTM in humans. In the majority of laboratories, cultures were grown on<br />
solid and in liquid media. All clinical isolates of mycobacteria were sent for identification to the National<br />
Reference Laboratory for Mycobacteria Golnik. GenoType Mycobaterium CM/AS assays (Hain<br />
Lifescience, Nehren, Germany), AccuProbe tests (GenProbe, San Diego, USA), classical biochemical<br />
tests and/or colony morphology of NTM on transparent medium were used for identification of mycobacteria.<br />
Results<br />
A total of 2238 (1.6%) isolates of NTM were isolated from 140,001 clinical specimens in Slovenia<br />
in the period 2000-2010. Mycobacterium (M.) xenopi (27.5%) was the most frequently isolated<br />
species followed by M. avium complex (22.6%), M. gordonae (16.3%), M. kansasii (8.1%) and M.<br />
fortuitum (6.7%). In contrast, M. kansasii and M. avium complex were found to be the most common<br />
disease-causing mycobacteria in our country in the last 11 years. Mycobacteriosis has been<br />
observed in at least 115 persons in the same period. Eight of them were children aged between<br />
1.5 and 4 years, all had lymphadenitis caused by M. avium complex and all were detected in the<br />
period 2006-2010.<br />
50
Conclusions<br />
NTM are not very often isolated from human specimens in Slovenia. M. xenopi is the most frequently<br />
isolated mycobacteria and M. kansasii the most common disease-causing mycobacteria in our country.<br />
Mycobacterioses are being detected more often in the last years, but are still relatively rare. Lymphadenitis<br />
in children, “an expected novelty”, appeared in 2006, a year and a half after non-selective<br />
BCG vaccination was stopped in our country.<br />
51
The importance of pre-analytic factors<br />
in Quantiferon-TB Gold test<br />
Urøka Bidovec Stojkoviœ, Manca Æolnir Dovœ<br />
University Clinic of Respiratory and Allergic Diseases, Golnik<br />
Background<br />
Addition of a third (mitogen, M) tube to Nil (N) and Antigen (A) tubes in QuantiFERON - TB Gold intube<br />
(QFT-IT) test represented an important step as the test gained a new value; the result of M tube<br />
can give information about immune status of a person or incorrect transport of blood to the laboratory.<br />
QFT-IT is used in our laboratory since 2004. Mitogen tube was introduced into daily routine in<br />
2008. The aim of our study was to evaluate the influence of pre-analytic factors on the percentage of<br />
indeterminate results.<br />
Methods<br />
A total of 4185 samples obtained between 2008 and 2010 were analyzed in this study. Only data obtained<br />
with all three tubes (N, A and M) were used. In 2009 and 2010, all (100%) samples were collected<br />
into all three tubes while in 2008, 822 samples (73.4%) included all three tubes. Approximately<br />
1.4% of blood samples were rejected by the laboratory due to errors in transport (time of transport<br />
exceeding 16 hours, incorrect transport at 4°C, blood collected in wrong type of tubes). In 256 cases<br />
(6.1%), the result was indeterminate while in 709 (17.0%) cases the result was positive. Negative result<br />
was found in 75.8%.<br />
Results<br />
Detailed insight into indeterminate results per year revealed 93 (11.3%), 82 (5.9%) and 81 (4.1%) indeterminate<br />
results in 2008, 2009 and 2010, respectively. The samples collected in one hospital<br />
showed a particularly high number of indeterminate results, 17% in the first half of 2009. The hospital<br />
has a large number of immunocompromised patients; nevertheless, the percentage was still very<br />
high. The communication with the head nurse responsible for the samples led to improved results<br />
(11% of indeterminate samples; unchanged until present).<br />
Conclusions<br />
Pre-analytical steps of QFT-IT importantly affect the result of QFT-IT test. In our case, the implementation<br />
of QFT-IT into daily laboratory routine started with large number of activities to assure good<br />
quality of the results, including practical and theoretical education of nurses responsible for the collection<br />
of blood, reducing the number of places where blood is collected, well organized transport,<br />
written instructions and providing information and instructions over the phone. As a consequence of<br />
using the third (M) tube and occurrence of indeterminate results, the laboratory has introduced even<br />
52
more serious measures in pre-analytical steps, e.g. more strict control over transport, recommendation<br />
on shorter transport time (4 hours if possible) and communication with people responsible for<br />
the transport of samples. These measures helped to improve the results of QFT-IT test and the number<br />
of indeterminate results significantly decreased.<br />
53
Evaluation of GeneXpert MTB/RIF<br />
assay for detection of Mycobacterium<br />
tuberculosis and rifampicin resistance<br />
in a routine laboratory setting in<br />
Slovenia<br />
Nataøa Fajfar, Urøka Bidovec Stojkoviœ, Manca Æolnir Dovœ<br />
University Clinic of Respiratory and Allergic Diseases, Golnik<br />
Background<br />
Nucleic acid amplification tests have improved tuberculosis diagnostics considerably. The latest development<br />
in the field of molecular diagnosis of tuberculosis is a quick fully automated real-time PCR<br />
diagnostic test, the Cepheid GeneXpert MTB/RIF assay (GX), for the detection of Mycobacterium tuberculosis<br />
and the detection of rifampicin resistance. The aim of our prospective study was to evaluate<br />
the performance of GX in comparison to the Gen-Probe Amplified M. tuberculosis Direct test<br />
(MTD), using culture as a reference method.<br />
Methods<br />
A total of 63 specimens (56 pulmonary and 7 extra-pulmonary) from 55 untreated patients for whom<br />
there was high clinical suspicion of tuberculosis were included in our study.<br />
Results<br />
42 of 63 specimens were culture positive and 21 culture negative. 35 specimens were positive and<br />
22 negative by GX and MTD. 6 specimens were positive by GX only. From 42 culture positive specimens<br />
MTD did not detect M. tuberculosis in 7 specimens but GX did not detect M. tuberculosis in<br />
only one culture positive specimen with only 1 colony grown on Loewenstein-Jensen medium which<br />
indicates really high sensitivity of the GX test. In comparison to culture, the sensitivity, specificity,<br />
positive predictive value and negative predictive value were 97.7%, 100%, 100% and 95.5%, respectively,<br />
for the GX; the corresponding values were 85.7%, 100%, 100% and 75.0%, respectively,<br />
for the MTD. From 41 GX M. tuberculosis positive specimens all of them were rifampicin sensitive by<br />
phenotypic drug susceptibility testing method, but GX test showed 39 rifampicin sensitive specimens<br />
and detected 1 rifampicin resistance and 1 result was indeterminate. After repeat testing GX<br />
test did not detect rifampicin resistance.<br />
Conclusions<br />
The GX test is rapid and has produced better results than MTD; it is more sensitive with significantly<br />
higher sensitivity and negative predictive value. It is suitable for routine detection of M. tuberculosis<br />
in specimens from untreated patients in small laboratories. Thus it can be easily included in our clinical<br />
laboratory in Slovenia. Further studies are needed to evaluate the performance of the GX test for<br />
the detection of rifampicin resistance since no rifampicin resistant specimens were included in this<br />
study.<br />
54
Nation-wide evaluation of three<br />
molecular genotyping methods<br />
in Slovenia<br />
Urøka Bidovec Stojkoviœ, Nataøa Fajfar, Manca Æolnir Dovœ<br />
University Clinic of Respiratory and Allergic Diseases, Golnik<br />
Background<br />
High discriminatory power of genotyping method is of great importance however some other requirements<br />
such as low cost and timeliness are also relevant. The aim of our one year nation-wide<br />
study was to evaluate three different methods for genotyping Mycobacterium (M.) tuberculosis on all<br />
culture positive isolates in Slovenia in year 2008. All MDR strains in the period 1996 and 2009 were<br />
also evaluated in this study. We tried to determine discriminatory power of different genotyping methods.<br />
Methods<br />
A total of 212 Slovenian M. tuberculosis isolates were typed by three different genotyping methods:<br />
IS6110-RFLP (RFLP), 24 loci MIRU-VNTR (MIRU-VNTR) and spoligotyping. Analysis of typing results<br />
was performed with BioNumerics program ver. 5.1 (Applied Maths, Belgium) and Hunter-Gaston discriminatory<br />
index (HGDI) was calculated as well. 190 isolates were obtained from 190 TB patients registered<br />
in 2008 at Slovenian Central Registry for TB Golnik. Additional 22 MDR strains were included<br />
in the study and they represent all (100%) MDR cases in the period 1996-2009.<br />
Results<br />
Among 212 M. tuberculosis isolates 160, 157, 63 distinct patterns; 135 (63.7%), 126 (59.4%), 36<br />
(17.0%) unique isolates; 77 (36.3%), 86 (40.6%), 176 (83%) clustered isolates; 25, 31, 27 clusters<br />
were found with RFLP, MIRU-VNTR and spoligotyping method, respectively. Number of isolates per<br />
cluster was 2-8, 2-7, 2-46 for RFLP, MIRU-VNTR and spoligotyping, respectively. HGDI showed even<br />
more surprising results since we obtained discriminatory index 0.9947, 0.9953, 0.9183 for RFLP,<br />
MIRU-VNTR and spoligotyping, respectively. Evaluation of MDR strains gave us some interesting information.<br />
Among 22 M. tuberculosis MDR isolates 9, 11 and 8 distinct patterns were found in RFLP,<br />
MIRU-VNTR and spoligotyping, respectively.<br />
Conclusions<br />
Our one year nation-wide study showed that the highest discriminatory power has RFLP method.<br />
Nevertheless MIRU-VNTR has shown very high discriminatory power as well, in some cases even<br />
higher than RFLP (MDR isolates). Spoligotyping method showed very low discriminatory power but<br />
has its advantage in recognizing some important strains lineage (Beijing, Haarlem, LAM type…).<br />
55
Primitive neuro-ectodermal tumour<br />
of the lung- a case report<br />
Mojca Unk, Izidor Kern, Tanja Œufer<br />
University Clinic of Respiratory and Allergic Diseases, Golnik<br />
Background<br />
A rare case of a pulmonary primitive neuro-ectodermal (PNET) tumour in an adult is presented here.<br />
In this case due to the rapid aggressive progression of the tumour, which is the characteristic of disease,<br />
the patient died within few days after the diagnosis.<br />
Case report<br />
A 36-years old male, hypertonic, non smoker was admitted to hospital with febrile state, cough and<br />
haemoptysis. CT scan of the thorax confirmed several bilateral nodular masses in the lung with pleural<br />
involvement, enlarged lymph nodes in the mediastinum and right hilus. Bronchoscopy with transbronchial<br />
biopsy was performed and the samples were suspicious for lymphoproliferative disease.<br />
Biopsy of the bone marrow revealed extensive (20%) lymphoid bone marrow infiltration, without infiltrates<br />
or pools of malignant cells, cells were scattered and TIA-1 positive. There was a diagnostic<br />
dilemma of possible NK cell lymphoma. Sixth day after admission to hospital the patient became<br />
febrile, dyspnoeic, tachycardic, anaemia worsened and chest x-ray revealed massive pleural effusion<br />
right. Pleural thoracocentesis revealed haematothorax. He died 13 days after admission due to<br />
unknown malignant disease. Post-mortem examination showed tumour masses in both lungs and on<br />
the parietal pleura, some homogenous, some haemorrhagic and necrotic, haematothorax bilaterally,<br />
enlarged subcarinal lymph node. The rest of the examination showed no pathological changes. Histological<br />
examination showed highly cellular discohesive necrotic tumour growth, tumour cells were<br />
of medium size, with high mitotic index and blastic morphology. They stained positive for vimentin,<br />
CD99, CD68 (not strongly, but CD163 negative), synaptophysin (focally positive, less than 10%),<br />
actin (nuclear positivity, collagen IV (focal positivity around each cell). All the epithelial, mesenchymal,<br />
lymphoma and other markers (desmin, NSE, CD56, EBV, MPO) were negative. Based on morphology<br />
and immunohistochemistry several diagnoses were proposed: high grade undifferentiated<br />
round cell malignant tumour, granulocytic sarcoma. Second opinion obtained from abroad suggested<br />
PNET/Ewing sarcoma. Cytogenetic analysis for reciprocal translocation of the long arms of chromosomes<br />
11 and 22 was negative.<br />
Conclusions<br />
PNETs are exceedingly rare in the adult population, with very few documented cases of primary lung<br />
PNET in the literature, first reported from Askin. Over the last decade, diagnosis has greatly improved<br />
with the introduction of an array immunohistochemical markers, PNETs stain positive for CD99 and<br />
56
NSE and negative for cytokeratins and desmin. In cases where morphology is inconclusive, cytogenetic<br />
analysis has rapidly become the standard for confirming the diagnosis. PNET lesions are aggressive<br />
and usually lethal; they should be considered in the differential diagnosis of thoracic tumours<br />
regardless of the age of the patient. Once a diagnosis of PNET has been made, early wide excision<br />
of the tumour, if possible, along with multimodality chemo- and radiotherapy, should be undertaken<br />
to offer any hope of a long-term cure.<br />
57
Premalignant lesions<br />
among coal miners<br />
Edin Zukiå 1 , Dragan Keser 1 , Edin Jusufoviå 1 , Rifat Sejdinoviå 2<br />
1<br />
Polyclinic for lung diseases, Healthcare Center Tuzla, Bosnia and Herzegovina<br />
2<br />
General Hospital Teøanj, Bosnia Hercegovina<br />
Background<br />
Similar to other malignant disease the lung cancer in some cases develops after a sequence of premalignant<br />
lesions. Sequential changes of the bronchial epithelia include hyperplasia, metaplasia,<br />
dysplasia, carcinoma in situ, which eventually turn to invasive cancer. In previous studies coal miners<br />
have been confirmed to have increased incidence of lung cancer. Goal of this research was to<br />
determine the frequency of preneoplastic lung lesions among coal miners.<br />
Methods<br />
We examined a total of 89 coal miners, 51 employed in surface mining, and 38 in underground mining.<br />
The control group consisted of 33 patients without serious lung conditions that could lead to<br />
preneoplastic lesions. Videobronhoscopy with NBI light source, followed by cytological analysis was<br />
used to detect preneoplastic lesions.<br />
Results<br />
Metaplasia was detected in 42 of the 89 coal miners (47,19%), and in 8 of the 33 patients in the control<br />
group (24,24%). Significantly higher incidence of metaplasia was detected among coal miners<br />
compared to the control group (p=0,037), taking into account the smoking habits.<br />
Conclusions<br />
Preneoplastic lesions represent an important factor in the development of invasive lung cancer among<br />
coal miners.<br />
58
Videothoracoscopic lung lobectomy<br />
in patients over 75 years of age<br />
Nika Lalek 1 , Katja Adamiœ 1 , Tomaæ Øtupnik 2<br />
1<br />
University Clinic of Respiratory and Allergic Diseases Golnik<br />
2<br />
Clinical Department of Thoracic Surgery, University Medical Centre Ljubljana<br />
Background<br />
Videothoracoscopic (VATS) lobectomies are now routinely performed to treat patients with earlystage<br />
lung cancer. In comparison to open lobectomies, VATS lobectomies are associated with less<br />
postoperative pain, lower rate of postoperative complications, shorter length of hospital stay and<br />
faster return to full activity. Age is a known independent risk factor for minor and major postoperative<br />
complications after open and VATS lung lobectomy (1,2).<br />
Methods<br />
We have made a retrospective study of all lung lobectomies done over a 3 year period (2008-2010)<br />
in patients older than 75 years. Propensity score matching with genetic search algorithm was used<br />
to balance groups for known independent risk factors such as: tumor size, comorbidities, age and<br />
location of the tumor.<br />
Results<br />
A total of 39 lobectomies were performed in patients over 75-years of age (9.9% of all lobectomies<br />
performed at our department): 28 open lobectomies (OL) and 11 VATS lobectomies (VL).<br />
The rate of minor complications (air leak > 5 days, arrhythmia) was 45% in VL and 63% in OL group<br />
(p = 0.05). The rate of major complications (pneumonia, empyema, death) was 9% in VL and 17%<br />
in OL group (p = 0.23). The mean length of hospital stay was 7.1 days in VL and 10.7 days in the OL<br />
group (p = 0.01).<br />
Conclusions<br />
VL are associated with a significantly lower rate of postoperative complications and significantly<br />
shorter hospital stay than OL and are thus a highly recommended way to treat early-stage lung cancer<br />
in a subset of older patients.<br />
References<br />
1. Flores RM, Park BJ, Dycoco J, Aronova A et al. Lobectomy by video-assisted thoracic surgery (VATS) versus<br />
thoracotomy for lung cancer. J Thorac Cardiovasc Surg. 2009 Jul;138(1):11-8.<br />
2. Cattaneo SM, Park BJ, Wilton AS, Seshan VE et al. Use of video-assisted thoracic surgery for lobectomy in the<br />
elderly results in fewer complications. Ann Thorac Surg. 2008 Jan;85(1):231-5.<br />
59
Clinical impact of ERCC1 protein<br />
expression in small-cell lung cancer<br />
patients treated with platinum-based<br />
chemotherapy<br />
Eva Sodja 1 , Lea Knez 1 , Tanja Ovœariœek 2 , Izidor Kern 1 ,<br />
Mitja Koønik 1 , Aleksander Sadikov 3 , Tanja Œufer 1<br />
1<br />
University Clinic of Respiratory and Allergic Diseases Golnik, Golnik<br />
2<br />
University Clinic Maribor, Maribor<br />
3<br />
Faculty of Computer and Information Science, University of Ljubljana<br />
Background<br />
The protein excision repair cross complementing 1 (ERCC1) may decrease the sensitivity to platinum<br />
agents. The relationship between low ERCC1 expression and better response to platinum<br />
agents has already been confirmed in non-small-cell lung cancer (NSCLC), while the data on possible<br />
predictive value of ERCC1 in small-cell lung cancer (SCLC) is still very limited.<br />
Methods<br />
This retrospective study evaluated the impact of ERCC1 levels in primary tumour on response to<br />
platinum-based chemotherapy and on survival of SCLC patients treated in a routine clinical practice<br />
at the University Clinic Golnik, between years 2001 and 2007. ERCC1 expression was determined<br />
immunohistochemically in FFPE tumour tissue. The criteria for ERCC1 IHC evaluation was based on<br />
the percentage of cells with positive nuclear staining (0=none, 1=1-9%, 2=10-49%, 3= 50%) and intensity<br />
of staining (0=none, 1=weak staining, 2=strong staining). FFPE tumour tissue samples presenting<br />
with 50% of strongly stained tumour cells were considered as ERCC1 positive. Medical<br />
charts were reviewed for classical clinico-pathological characteristics and for treatment outcome.<br />
Results<br />
269 SCLC patients were enrolled in this study, but only 86 patients had sufficient amount and well preserved<br />
tumour tissue corresponding to SCLC histology for IHC staining. Of those, 64 patients received platinumbased<br />
chemotherapy and were included in further analysis. ERCC1 protein was positive in 38/64 (59%) of<br />
the SCLC patients. No significant difference in overall survival between ERCC1 positive and negative patients<br />
was observed (median survival 12.1 vs. 11.7 months, respectively). There was no significant difference<br />
between ERCC1 positive and negative patients in response to platinum-based chemotherapy (the<br />
percent of patients who obtained either complete or partial response was 80.8% vs. 76.3%, respectively).<br />
Conclusions<br />
In our limited group of 64 SCLC patients ERCC1 protein expression was not found to correlate with<br />
either overall survival or response to platinum-based chemotherapy. To get a definitive answer on the<br />
predictive value of ERCC1 in SCLC a larger prospective trial is mandatory.<br />
60
Quantitative Methylation Profiles<br />
of Multiple Genes in Patients<br />
with Non-Small Cell Lung Cancer<br />
And its Association<br />
with Clinicopathological Correlations<br />
Milica Kontiå 1 , Jelena Stojøiå 1 , Dragana Jovanoviå 1 ,<br />
Vera Bunjevacki 2 , Susan Puumala 3 , Heather H Nelson 4<br />
1<br />
Pulmonology Clinic, Clinical Centre of Serbia, Medical Faculty, University in Belgrade, Serbia<br />
2<br />
Institute for Human Genetics, Oncogenetics Department, Medical Faculty, University in Belgrade, Serbia<br />
3<br />
Sanford Research/ Sanford School of Medicine of the University of South Dakota, USA<br />
4<br />
CancerCentre, Minneapolis, University of Minnesota, USA<br />
Background<br />
Systemic methylation changes may be a diagnostic marker for tumor development or prognosis.<br />
Many genes have been reported as epigenetically aberrant in non-small cell lung cancer. Further, it<br />
has been suggested that DNA methylation changes that occur in lung tumors may be detectable in<br />
circulating blood leading to a clinical tool for screening or relapse. Here, we investigate the relationship<br />
between gene methylation in lung tumors relative to normal lung tissue, and whether DNA<br />
methylation changes can be detected in paired blood samples.<br />
Methods<br />
Sixty five patients were enrolled in a surgical case series of non-small cell lung cancer (NSCLC) at<br />
a single institution. Using bisulfite pyrosequencing, CpG methylation was quantified at five genes<br />
(RASSF1A, CDH13, MGMT, ESR1 and DAPK) in lung tumor, pathologically normal lung tissue, and<br />
circulating blood from enrolled cases.<br />
Results<br />
Three genes had significantly higher methylation in tumors compared to normal lung tissue (CDH13,<br />
RASSF1A and DAPK), and two of the tested genes were not significantly different (ESR1 and MGMT).<br />
To determine whether the aberrantly methylated genes could be detected in circulating blood, we<br />
stratified cases according to their tumor status for CDH13, RASSF1A and DAPK. However, average<br />
DNA methylation in circulating blood was similar among the tumors positive for methylation and those<br />
that were negative, indicating a low feasibility of detecting lung cancer using these genes in a bloodbased<br />
test. Lastly we probed whether tumor methylation was associatied with clinical and demographic<br />
traits of the cases. Histology and gender were associated with methylation at the CDH13<br />
gene, while stage was associated with methylation at MGMT.<br />
Conclusions<br />
Our results demonstrate that elevated methylation at the RASSF1A, CDH13, and DAPK genes are<br />
specific to lung tumors relative to pathologically normal lung. However, we did not observe these<br />
61
same see methylation changes in blood samples from patients with NSCLC indicating they are poorly<br />
suited to a screening test.<br />
62
Anti-angiogenic miRNAs let-7b<br />
and miR-126 are down-regulated<br />
in tumour and tumour surrounding<br />
in NSCLC lung tissue<br />
Edin Jusufoviå 1, 2 , Matija Rijavec 3 , Dragan Keser 1, 2 , Eva Sodja 3 , Mitja Koønik 2, 3 , Peter Koroøec 3<br />
1<br />
Polyclinic for Pulmonary Diseases, Health Medical Centre Tuzla, Bosnia and Herzegovina<br />
2<br />
Medical Faculty, University in Tuzla, Bosnia and Herzegovina<br />
3<br />
University Clinic of Respiratory and Allergic Diseases Golnik<br />
Background<br />
Lung cancer development represents complex molecular events. Angiogenic processes seem to be<br />
crucial for tumor invasiveness and metastatic potential. Micro RNAs (miRNA) might be important in<br />
regulating tumor angiogenesis.<br />
Methods<br />
A total of 50 patients with pathologically proven non small cell lung cancer (NSCLC) (32 squamous<br />
cell lung carcinoma and 18 lung adenocarcinoma) and a control group of 45 healthy individuals were<br />
included in this study. The expression of four angiogenic miRNAs (let-7b, miR-9, miR-19a and miR-<br />
126) was detected by quantitative real-time RT-PCR in formalin fixes and paraffin embedded tissue<br />
samples. Three different tissue samples of NSCLC patients (tumor tissue, tumor surroundings and<br />
healthy lung tissue) as well as lung tissue of healthy individuals were compared.<br />
Results<br />
Expression of anti-angiogenic let-7b and miR-126 were significantly lower (p
Conclusions<br />
In NSCLC patients we observed down-regulation of let-7b and miR-126 in tumor tissue as well as in<br />
tumor surroundings. The level of expression of anti-angiogenic let-7b and miR-126 was similar in<br />
tumor and tumor surrounding. Our results confirm the possible role of those two miRNas in lung cancer<br />
angiogenesis and suggest the potential new target cancer therapy in controlling tumor angiogenesis.<br />
64
MDR1 polymorphisms G2677T/A<br />
and C3435T are independent predictive<br />
markers in small-cell lung cancer<br />
patients treated with chemotherapy<br />
Lea Knez 1 , Tanja Ovœariœek 2 , Aleksander Sadikov 3 ,<br />
Eva Sodja 1 , Izidor Kern 1 , Mitja Koønik 1 , Tanja Œufer 1<br />
1<br />
University Clinic of Respiratory and Allergic Diseases, Golnik<br />
2<br />
University Clinic Maribor<br />
3<br />
Faculty of Computer and Information Sciences, University of Ljubljana<br />
Background<br />
Multiple drug resistance limits the efficacy of chemotherapy treatment and, consequently, survival of<br />
patients with small-cell lung cancer (SCLC). The protein multiple drug resistance 1 (MDR1) has an<br />
important role in this process and variability in its gene may affect treatment outcomes.<br />
Methods<br />
This study evaluated the associations between MDR1 polymorphisms G2677T/A and C3435T with<br />
progression free survival (PFS) and overall survival (OS) in 177 SCLC patients, treated with cisplatinetoposide<br />
or cyclophosphamide-epirubicin-vincristine chemotherapy in a routine clinical practice at<br />
a teaching hospital in Slovenia, between the years 2002 and 2007. To determine the MDR1 genotype,<br />
allelic specific TaqMan® probes were used in a RT-PCR reaction.<br />
Results<br />
Patients, homozygotes for the G2677T/A variant allele (42/174; 24,1%) or harbouring at least one<br />
C3435T variant allele (127/177; 71,8%) had a longer PFS (Log-rank, p=0,050 and p=0,036, respectively)<br />
which persisted also when adjusted for age, sex, stage and PS in multivariate analysis (Coxregression,<br />
p=0,028 and p=0,037, respectively). Moreover, patients with at least one C3435T variant<br />
allele had a longer OS (Log-rank, p=0,021), the association being significant also in multivariate<br />
analysis (Cox-regression, p=0,028).<br />
Conclusions<br />
Our study indicates that MDR1 polymorphisms G2677T/A and C3435T are independent predictive<br />
markers for longer PFS (both polymorphisms) and OS (only C3435T) in Caucasian patients with<br />
SCLC. However, their use to support decisions on chemotherapy treatment in routine clinical practice<br />
requires further validation.<br />
65
Changing to another TKI<br />
in treatment of metastatic NSCLC<br />
Tijana Taja Øumer, Tanja Œufer<br />
University Clinic of Respiratory and Allergic Diseases, Golnik<br />
Background<br />
Epidermal growth factor receptor (EGFR) gene mutations predict for a good response to EGFR directed<br />
therapy with TKIs (gefitinib, erlotinib) in lung adenocarcinoma. There are available data pointing<br />
out that treatment with erlotinib can be effective in patients with prior exposure to gefitinib. Hereby,<br />
we report on three female patients (age 56-79 yr, median age 67 yr) with activating EGFR mutations<br />
in primary tumor those received two subsequent lines of TKI therapy in a routine clinical practice.<br />
Patients<br />
The youngest patient was smoker, the other two never smoked. In the first patient maintenance treatment<br />
with erlotinib resulted in 25 moths of partial response (PR). Gefitinib was initiated as second line<br />
TKI therapy and resulted in PR that still lasts after 17 months. In another case PR of 31 months was<br />
achieved by first line erlotinib therapy. After 5 months without therapy CT scan showed progression<br />
and gefitinib was introduced. After 15 months of follow up she has a stable disease. In the third patient<br />
(ex smoker) stagnation of the disease lasting for 6 months was achieved by first line gefitinib<br />
treatment. Erlotinib was introduced as second line therapy and she is now in observation period for<br />
5 months without signs of progression.<br />
Conclusions<br />
These limited data from our cases suggest that patients with EGFR gene mutations may benefit from<br />
second line TKI after progression instead of immediate chemotherapy introduction.<br />
66
Topoisomerase IIa in small cell lung<br />
carcinoma<br />
Izidor Kern, Mile Kovaœeviå, Eva Sodja, Tanja Œufer<br />
University Clinic of Respiratory and Allergic Diseases, Golnik<br />
Background<br />
Small cell lung carcinoma (SCLC) is very sensitive to chemotherapy. Topoisomerase IIa (TOP2A)<br />
has important role in DNA replication. Cytostatic drugs used to treat SCLC work by blocking the enzyme.<br />
The aim of this study was to determine the TOP2A gene and protein expression and gene amplification<br />
in SCLC.<br />
Methods<br />
We performed analysis of 29 archived bronchial biopsies samples diagnosed as SCLC. Immunohistochemical<br />
staining (monoclonal antibody clone 3F6) was evaluated semi quantitatively by determing<br />
the intensity of reaction in tumor nuclei (negative, weak, marked). Dual silver in situ<br />
hybridization was performed for gene amplification analysis. Signals were counted in 40 preserved<br />
nuclei to detect a ratio between TOP2A gene copy numbers and CEP 17, while polisomy was considered<br />
when at least 40% cells with at least 4 copies of TOP2A gene were observed. Total RNA<br />
was extracted from sections of formalin-fixed and paraffin-embedded tumor tissue. Relative quantification<br />
was performed by real-time polymerase chain reaction using intron-spanning primer-probe<br />
sets.<br />
Results<br />
All 29 samples showed positive immunohistochemical nuclear reaction for TOP2A (16 weak, 13<br />
marked). Four samples showed polisomy, while ratio TOP2A /CEP 17 value was 1,08 - 1,56. Most<br />
samples showed trisomy (22 of 29), while normosomy was detected in 3 samples. Only 11 out of 13<br />
samples were successfully amplified. Median relative gene expression value was 0,901 (0,277-2,902,<br />
SD=0,73).<br />
Conclusions<br />
This study revealed that, although the majority of the samples expressed TOP2A positive immunohistochemical<br />
nuclear staining, it is not possible to correlate it with neither TOP2A gene expression<br />
nor amplification.<br />
67
Neutropenia in lung cancer patients<br />
treated with chemotherapy in a routine<br />
clinical practice – an institutional<br />
experience<br />
Nina Turnøek 1 , Katja Mohorœiœ 1 , Aleksander Sadikov 2 , Tanja Œufer 1<br />
1<br />
University Clinic of Respiratory and Allergic Diseases, Golnik<br />
2<br />
Faculty of Computer and Information Sciences, University of Ljubljana<br />
Background<br />
Chemotherapy is the standard treatment for advanced small-cell (SCLC) and non-small cell lung<br />
cancer (NSCLC). Mielosuppression is a very common side-effect, compromising clinical outcome and<br />
efficacy of the treatment with chemotherapy (ChT), and predisposes patients to serious infections.<br />
Febrile neutropenia (FN) as the most serious side-effect is associated with dose reductions and delays<br />
and serious complications, sometimes even with death. The use of antibiotics, G-CSF and need<br />
for hospitalization are associated with substantial escalation of costs.<br />
Methods<br />
We performed a retrospective analysis of 190 patients with advanced lung cancer (SCLC and<br />
NSCLC), treated with ChT in a routine clinical practice at University Clinic Golnik from January 2009<br />
until March <strong>2011</strong>. The rate and severity of neutropenia, the rate of febrile neutropenia, treatment<br />
strategies and the impact of neutropenia and its treatment on patient’s outcome were evaluated. Majority<br />
of patients received platinum based ChT schemes (cisplatin 64.7%, carboplatin 20.0%), smaller<br />
amount of patients received schemes containing other cytotoxics in combination or monotherapy<br />
(15.3%). The frequency of SCLC and NSCLC was in concordance with their incidence (71.1% of patients<br />
had NSCLC, 28.9% had SCLC). Majority of patients received 6 cycles of ChT (46.3%, range<br />
2-6 cycles). Most of our patients received first line ChT (86.8%), only 13.2% received ChT in second<br />
or third line.<br />
Results<br />
Neutropenia was recorded in 100/190 (52.6%) of all patients, and 60/190 (31.6%) patients suffered<br />
severe neutropenia grade 3 or 4. No correlation was found between occurence of neutropenia and<br />
histological type of the tumor or line of ChT. Neither there was a correlation between occurence of<br />
neutropenia and cisplatin- vs carboplatin- based ChT. In majority of the patients neutropenia developed<br />
after the first three cycles of ChT (76.0%), FN also developed mostly after first three cycles of<br />
ChT (81.3%). FN was recorded in 16/190 (8.4%) of patients. No correlation between FN and other<br />
tumor or treatment characteristics was done due to the small number of patients. Prophylactic G-CSF<br />
was used in 14/190 (7.4%) of all our patients, 8 of them received G-CSF after the episode of FN, and<br />
6 of them due to higher grade neutropenia without FN. One patient received primary prophylaxis<br />
with G-CSF, all the others secondary prophylaxis. Therapeutic G-CSF received 6 patients. All pa-<br />
68
tients with FN received antibiotic treatment; however no one of our patients received prophylactic antiobiotic<br />
treatment. One patient died due to FN.<br />
Conclusions<br />
The rate of neutropenia observed in our patients was expected, though the rate of FN was quite low.<br />
The reported rate of FN in lung cancer patients treated with comparable cytotoxic schemes is 10-<br />
20%. The number of patients that received G-CSF is relatively high, especially because G-CSF was<br />
mostly used as secondary prophylaxis. The reason for low rate of FN can be due to relatively high<br />
amount of G-CSF used as secondary prophylaxis. On the other hand, we must be aware of the fact,<br />
that this is a retrospective analysis, where there was no clinical examination and blood analysis during<br />
ChT cycles while our patients were at home. Nevertheless, such a result can also be due to well<br />
chosen indication and well conducted ChT. There is a need to conduct prospective analysis to closely<br />
define this situation.<br />
69
Safety and efficiency of treatment of<br />
advanced NSCLC with non-squamous<br />
histology with pemetrexed<br />
and platinum derivate combination<br />
in routine clinical practice; experience<br />
at University Clinic Golnik<br />
Jernej Mlakar 1 , Tanja Œufer 1 , Nadja Triller 1 , Aleksander Sadikov 2 , Tijana Taja Øumer 1<br />
1<br />
University Clinic of Pulmonary and Allergic Diseases, Golnik<br />
2<br />
Faculty of Computer and Information Science, University of Ljubljana<br />
Background<br />
On the basis of results of a study published in 2008 by Scaggliotti et al, pemetrexed and a platinum<br />
derivate combination has become the standard treatment of advanced non-small cell lung carcinoma<br />
with non-squamous histology. In Slovenia, pemetrexed has become available in the second half<br />
of 2009. We have studied the safety and efficacy of this regimen in our group of patients.<br />
Methods<br />
37 patients with advanced non-small cell lung carcinoma with non-squamous histology, treated with<br />
pemetrexed and platinum derivate from September 2009 to August <strong>2011</strong> were included in a retrospective<br />
study. Previous surgery, radiotherapy or chemotherapy was permitted. At the time of treatment<br />
with pemetrexed and platinum derivate all patients had advanced disease and did not receive<br />
any other treatment modality. Performance status (PS), treatment response and adverse effects were<br />
defined according to the ECOG standards, RECIST 1.1 criteria and CTCAE v4.0, respectively. Time<br />
to disease progression was defined as the time from the start of treatment with pemetrexed and platinum<br />
derivate to disease progression or death and estimated with a Kaplan-Meier method.<br />
Results<br />
31 (83,8%) patients received pemetrexed and cisplatin and 6 (16,2%) patients received pemetrexed<br />
and carboplatin. As a consequence of a small patient number, analysis by chemotherapy regimen<br />
was not possible. Therefore all results represent the entire 37-patient group. Median age was 57<br />
years (range 38-76 years). 7 (18,9%) patients had a PS 0 at the start of treatment with pemetrexed<br />
and a platinum derivate, 26 (70,3%) patients had PS 1, 3 (8,1%) patients had PS 2 and 1 (2,7%) patient<br />
had PS 3. All 37 patients (100%) had adenocarcinoma. The majority of patients (29 or 78,4%)<br />
received pemetrexed and platinum derivate as a first line of treatment, 4 (10,8%) patients received<br />
it as a second line and 4 patients (10,8%) as a third line of treatment. Median number of received<br />
chemotherapy cycles was 5 (range 1-8). Treatment response could be assessed in 35 of 37 patients.<br />
None of the patients achieved complete response, 17 (45,9%) patients achieved partial response<br />
(PR) and 7 (18,9%) patients achieved stable disease. 11 (29,7%) experienced disease progression<br />
during treatment. It was not possible to asses the duration of response due to lack of stringency in<br />
performing regular radiological evaluations. Most of adverse effects (AE) were of grades 1 and 2. Proportions<br />
of patients with individual non-hematologic grade 1 and 2 AE were: nausea 70,2%, vomit-<br />
70
ing 45,9%, elevated liver enzymes 59,5%, stomatitis 5,4%, rash 13,5%, neuropathy 13,5%, elevated<br />
BUN 8,1%, diarrhea 2,7%. Among grade 3 AE neuropathy was present in 2,7% and elevated liver enzymes<br />
in 5,4% of cases. Hematologic AE analysis revealed the following: 29 (24,3%) patients developed<br />
grade 1/2 neutropenia, 5 (13,5%) patients developed grade 3 neutropenia. Grade 1/2<br />
thrombocytopenia developed in 7 (18,9%) patients and grade 1/2 anemia in 24 (64,9%) patients.<br />
Grade 3/4 thrombocytopenia and/or anemia were not detected. Febrile state without neutropenia<br />
(with or without a known localization of infection) occurred in 7 (18,9%) patients. Febrile neutropenia<br />
did not occur. Progression free survival (PFS) of 7,9 months (95%CI, 5,6-10,3 months) was observed<br />
after a median observation time of 11,1 months (95% CI, 4,7 – 17,6 months). Overall survival could<br />
not be estimated due to a short observation time.<br />
Conclusions<br />
According to results of our study we might conclude that pemetrexed and platinum based chemotherapeutic<br />
treatment was safe and active in our group of routinely treated patients. Comparison of results<br />
with the reference study by Scagliotti and colleagues surprisingly showed even better treatment<br />
response (46% vs. 30%), longer PFS (7,9 m vs. 5,3 m) and less AE (especially non-hematologic) in<br />
patients treated in clinical practice than those treated in the trial. Because of the inclusion of patients<br />
with less favorable characteristics, we attribute this discrepancy to a less rigorous response evaluation<br />
and AE assessment in our routine clinical practice. Pemetrexed and a platinum derivate<br />
chemotherapy regimen seem to be safe and effective in clinical practice, however, for a more trustworthy<br />
conclusion to be made, more rigorous evaluation procedures and side effects measurements<br />
need to be performed in routine clinical practice. In addition, a more relevant conclusion on the outcome<br />
of our patients will be possible after a longer follow up period, when overall survival estimation<br />
will be done.<br />
71
Blood oxidative stress markers<br />
and lipid status in sarcoidosis<br />
Jasmina Ivaniøeviå 1 , Jelena Kotur Stevuljeviå 1 , Aleksandra Stefanoviå 1 , Zorana Jeliå Ivanoviå 1 ,<br />
Slavica Spasiå 1 , Jelica Videnoviå Ivanov 2 , Violeta Vuœiniå Mihailoviå 2 , Jasmina Iliå 3<br />
1<br />
Department for Medical Biochemistry, Faculty of Pharmacy, University of Belgrade, Serbia<br />
2<br />
Clinic for Pulmonary Diseases, Clinical Centre of Serbia, Belgrade, Serbia<br />
3<br />
Health Centre „St. Luka“, Smederevo, Serbia<br />
Background<br />
Sarcoidosis is an inflammatory disease with enhanced production of reactive oxygen species (ROS)<br />
and alterations in lipid profile suggested to play a role in its pathogenesis. However, current knowledge<br />
about the significance of blood oxidative stress/antioxidant defense as well as lipid status parameters<br />
measurement in sarcoidosis is very limited. Therefore, the aim of our study was to assess<br />
these parameters and to estimate their value for disease prediction.<br />
Methods<br />
The parameters of oxidative stress [malondialdehyde (MDA), superoxide anion (O 2<br />
.-<br />
), total oxidant status<br />
(TOS), prooxidant-antioxidant balance (PAB)] and antioxidant defense [superoxide dismutase<br />
(SOD), total sulfhydryl (SH) groups, total antioxidant status (TAS)] were determined in serum and<br />
erythrocytes and lipid status parameters [total cholesterol (TC), LDL-cholesterol (LDL-c), HDL-cholesterol<br />
(HDL-c) and triglycerides] were assessed in serum of 213 treated sarcoidosis patients and<br />
90 control subjects. Significant difference was set at P
stress and lipid status showed potential to discriminate sarcoidosis from healthy subjects with pronounced<br />
contribution of oxidative stress status parameters. The joint action of these parameters also<br />
suggests certain risk for the development of atherosclerosis.<br />
Grant support<br />
The authors appreciate the financial support from the Ministry of Science and Technological Development,<br />
Republic of Serbia (Project number 175035).<br />
73
Results of 18 F FDG PET scan<br />
in patients with chronic sarcoidosis<br />
Jelica Videnoviå Ivanov, D Sobiå Øaranoviå, Violeta Vuœiniå Mihailoviå, V Zugiå, S Filipoviå<br />
Clinic for lung diseases and tuberculosis, CC Serbia, Belgrade<br />
Background<br />
Sarcoidosis is rare disorder with non-caseating granulomas as main findings. A systemic disease with<br />
predominantly chronic course is another caracteristics. Relapses occur. Aim of work was to analyze<br />
the potential role of 18 F FDG PET scan as marker of activity.<br />
Methods<br />
Results<br />
Among 40 patients with chronic course of sarcoidosis, only one was not treated with corticosteroid<br />
therapy. Positive scan (hypermetabolism) was obtained in 32 patients. The main findings were enlarged<br />
lymph nodes predominantly in mediastinum but higher uptake were also obtained in lung<br />
parenchyma and accidently findings were in non-pulmonary organs.<br />
Conclusions<br />
According to obtained results 18 F FDG-PET scan can represent as the potential diseases activity<br />
marker.<br />
74
The significance of PET CT in diagnosis<br />
of Takayasu arteritis – a case study<br />
Taja Tijana Øumer 1 , Ivana Æagar 2 , Nataøa Gaøperøiœ 3<br />
1<br />
University Clinic of Respiratory and Allergic diseases, Golnik<br />
2<br />
Department of Nuclear Medicine, Institute of Oncology, Ljubljana<br />
3<br />
Department of Rheumatology, University Medical Centre Ljubljana<br />
Background<br />
PET/CT (positron emission tomography with computer tomography) has been shown to be useful for<br />
assessing the location and extent of cancer. It has also been suggested that PET/CT is useful in evaluating<br />
the presence and extent of vasculitis.<br />
Case<br />
A 59-year old female underwent a long diagnostic procedure in another hospital because of undefined<br />
high inflammatory markers (sedimentation rate over 120mm/h, C-reactive protein 131 mg/l),<br />
microcytic anemia (hemoglobin 82 g/l , ferritin 2420 mcg/l). Her leading symptoms were muscle pain,<br />
weight loss and generally very bad state of health. In 1990 she was treated for of pulmonary embolism<br />
of unknown origin. Acute inflammatory or autoimmune disease, malignant disease or other probable<br />
reasons for her health condition were excluded by extensive diagnostic workout. The only important<br />
finding was a small nodule in left thyroid lobe, which was cytologically proven to be benign, without<br />
evidence of inflammation. As she did not meet criteria for any of rheumatologic diseases, the exact<br />
diagnosis remained unclear.<br />
Results<br />
The patient was referred for PET/CT to exclude occult malignant disease. The examination revealed<br />
diffuse and slightly irregular pathologic 18-F-FDG (fluordeoksyglucose) uptake in the aortic wall along<br />
the entire aorta from its arch to bifurcation, with SUV max<br />
3.6. Pathologic accumulation has also been<br />
detected in the wall of both subclavian and carotid arteries and was suggestive of large vessel vasculitis.<br />
The patient was treated with glucocorticoids according to the scheme for Takayasu arteritis.<br />
During a 1,5 year follow-up she is now without any symptoms and signs of the disease .<br />
Conclusions<br />
18<br />
F-FDG-PET is proving to be a sensitive and specific tool for detection of active vascular wall inflammation<br />
and should be taken into account in diagnosis of Takayasu arteritis. Clinical criteria for<br />
Takayasu arteritis are probably not sufficient. New diagnostic technologies should be evaluated in<br />
such unusual cases.<br />
75
Diagnostic value of pulmonary NKT<br />
CD3 + CD16/56 + cells<br />
Katarina Osolnik, Matija Rijavec, Peter Koroøec<br />
University Clinic of Respiratory and Allergic Diseases, Golnik<br />
Background<br />
Natural killer T (NKT) cells, a unique subgroup of T cells, may be implicated in the pathogenesis of<br />
interstitial lung diseases (ILDs).<br />
Methods<br />
We used multi-parameter flow cytometry with antibodies to CD3, CD4, CD8, CD14, CD45 and<br />
CD16/56 in BAL fluid (BALF) to examine the diagnostic relevance of pulmonary CD3 + CD16/56 + NKT<br />
cells and to compare them with NK cell frequencies and CD4/CD8 index. We selected and analysed<br />
only BALF of patients with initial increased (> 8%) frequency of CD3 + CD16/56 + NKT cells.<br />
Results<br />
Of 88 selected patients with increased frequencies, 25 patients were diagnosed as hypersensitivity<br />
pneumonitis (HP) and 35 as sarcoidosis (SA), 14 patients demonstrated diffuse ILDs, 7 had malignant<br />
diseases and 7 patients had bacterial infection. The uppermost frequencies of BALF<br />
CD3 + CD16/56 + NKT cells were demonstrated in patients with HP (median of 16%, range 8% to 52%),<br />
and those values were significantly higher as CD3 + CD16/56 + frequencies observed in patients with<br />
SA (10%, range 8% to 19%) or diffuse ILDs (10.5%, range 8% to 17%; P
Peripheral invariant NKT cells and<br />
factors involved in the development<br />
of iNKT cells in sarcoidosis patients<br />
Matija Rijavec, Katarina Osolnik, Mitja Koønik, Peter Koroøec<br />
University Clinic of Respiratory and Allergic Diseases, Golnik<br />
Background<br />
Invariant natural killer T (iNKT) cells, with restricted Va24-Ja18-Vb11 T cell receptor, might contribute<br />
to the amplified and prolonged T-cell immune response that characterizes sarcoidosis. Their exact<br />
role as well as factors involved in regulating the development and recruitment of iNKT cells is still to<br />
be determined. SAP-dependent signalling as well as specific miRNAs might be involved in iNKT cell<br />
development. The aim of the study was to analyze the numbers of invariant NKT cells, mRNA and<br />
miRNA expression profiles of factors that might be involved in SAP-dependent signalling in the whole<br />
blood of corticosteroid-naïve patients in comparison with healthy individuals.<br />
Methods<br />
We used multi-parameter flow cytometry, with antibodies to CD3, Vb11 and 6B11 in combination with<br />
beads, to examine the absolute counts of iNKT cells. Total RNA and miRNA was extracted from peripheral<br />
blood, it was reverse transcribed to cDNA and Real time PCR for the mRNA/miRNA of interest,<br />
was performed. We included 31 newly diagnosed sarcoidosis patients and 28 healthy subjects.<br />
Results<br />
We have found striking reduction in absolute numbers of CD3+CD4+ but not CD3+CD4– Va24-Ja18-<br />
Vb11 iNKT cells as well as significantly decreased expression of SAP, SLAMF1, SLAMF6 and Fyn and<br />
increased expression of miR-21 in patients with sarcoidosis in comparison to healthy subjects.<br />
Conclusions<br />
These results suggest that the deficiency of iNKT cells might be crucial for the development and<br />
course of sarcoidosis. Furthermore, we imply on the involvement of SAP-dependent signalling pathway<br />
as well as specific miRNAs in the development of iNKT cells.<br />
77
Side-effects of specific<br />
immunotherapy: our experience –<br />
KOPA Golnik<br />
Jasmina Dimitrijeviå, Miljana Vegnuti, Katja Adamiœ,<br />
Nissera Bajroviå, Renato Eræen, Mitja Koønik, Ema Muøiœ, Mihaela Zidarn<br />
University Clinic of Respiratory and Allergic Diseases Golnik<br />
Background<br />
Immunotherapy celebrated 100 years of efficiency in management of allergic asthma, Allergic rhinitis/conjunctivitis<br />
and stinging insect hypersensitivity. In our Clinic, we perform specific immunotherapy<br />
(SIT) for such group of patients for almost 40 years.<br />
Methods<br />
We performed a retrospective study to compare side effects of immunotherapy to different allergens.<br />
We included 1774 patients that were treated with SIT (2 day ultra-rush protocol for venom immunotherapy<br />
(VIT) and 6 week dose-increase protocol with modified aeroallergen extracts). The aim<br />
of our retrospective study was to show the frequency and degree as well as the type of allergic reaction<br />
during the course of Immunotherapy.<br />
Results<br />
In our study 1449 patients received venom immunotherapy and 465 patients received inhaled allergen<br />
immunotherapy. The overall prevalence of side effects was 29,2%. In venom immunotherapy<br />
prevalence was 30% and for the aero-allergen group 25%. In group of patients receiving VIT, side<br />
effects appeared more frequently in the dose-increase phase and in the other group patients showed<br />
more side effects in the maintenance phase. The majority of systemic reactions were mild. Only eight<br />
patients in both groups had a life-threatening reaction after immunotherapy followed by fall of blood<br />
pressure and/or loss of consciousness which was treated with adrenalin. We had no fatal outcomes<br />
due to immunotherapy during all years of clinical experience. Large local reactions were present in<br />
20.4% in both groups in dose-increase phase and 24.8% in maintenance phase with no significant<br />
difference between the allergens.<br />
Conclusions<br />
In our study we came to conclusion that even though systemic reactions are not rare during the<br />
course of Immunotherapy, they are mild in the most cases and well tolerated. Like in foreign literature,<br />
the group with highest risk for having side effects was the group of patients receiving venom<br />
immunotherapy, first of all – honeybee extract.<br />
78
Allergy in patients<br />
with vocal fold nodules<br />
Gordana Mumoviå 1 , Irena Hoœevar Bolteæar 2 , Olga Popov-Dragin 1<br />
1<br />
University Department of Otorhinolaryngology, Novi Sad, Serbia<br />
2<br />
Department of Otorhinolaryngology and Head & Neck Surgery, University Medical Center, Ljubljana,<br />
Slovenia<br />
Background<br />
Vocal fold nodules (VFN) are results of voice misuse and abuse. The incidence of allergy in patients<br />
with benign vocal fold lesions was found to be higher than in the general population. It is possible<br />
that allergy makes the mucosa of vocal folds more susceptible for mechanical trauma during vocal<br />
fold vibration in aggressive phonation. The aim of the study was to find out whether there are some<br />
differences in the voice quality in patients with VFN with allergy versus those without allergy.<br />
Methods<br />
Fifty consecutive patients with VFN and allergy and 20 patients with VFN and without allergy were included<br />
in the study. The allergy was proven by history and skin prick tests. In all patients acoustic<br />
analysis of voice samples (vowel /a/ at habitual pitch and loudness) was performed. The following parameters<br />
were analyzed: fundamental frequency (F0), jitter, shimmer, minimal and maximal voice intensity,<br />
normalized noise energy (NNE) and harmonic-to-noise ratio (HNR) with the use of Dr. Speech<br />
(TIGER DRS) software. The voice characteristics hoarse, harsh and breathy were also determined in<br />
comparison with the software’s database. A comparison of voice characteristics between the patients<br />
with allergy and without it was done using SPSS statistical package, Version 18.<br />
Results<br />
There were 20 men and 30 women in the allergy group and 9 men and 11 women in the control group<br />
(p=0.791). Their age range was 12-65 years, mean 32.26 years. Thirty-four patients had allergy on<br />
house dust and 33 patients on different pollens. Allergy on other allergens (fungi, animal fur) was<br />
found in less than 10 patients. The patients with allergy had significantly louder minimal (p=0.043)<br />
and maximal voice intensity (p=0.021) and less favorable NNE (p=0.017) than the patients without<br />
allergy. There were no significant differences regarding voice characteristics hoarse, harsh and<br />
breathy.<br />
Conclusions<br />
The results of the study showed that patients with VFN and allergy were louder and had less favorable<br />
noise presence in their voices than the patients without allergy. We suppose that hyperplastic<br />
rhinitis and Eustachian tube dysfunction were the reasons for greater loudness in allergic patients.<br />
79
Anyhow, allergy appears to be one of the important factors which must be considered in the treatment<br />
of patients with VFN.<br />
References<br />
1. Curr Opin Otolaryngol Head Neck Surg. 2009; 17(6):420-3.<br />
2. Curr Opin Otolaryngol Head Neck Surg. 2003; 11(6):456-61.<br />
3. J Voice. 2007; 21(2):151-6.<br />
80
ORMDL3 gene polymorphism is<br />
associated with asthma risk and<br />
severity in Slovenian children<br />
Mateja Balantiœ 1 , Matija Rijavec 1 , Maja Kavalar 2 , Mira Øilar 1 , Mitja Koønik 1 , Peter Koroøec 1<br />
1<br />
University Clinic of Pulmonary and Allergic Diseases, Golnik<br />
2<br />
University Clinical Centre Maribor<br />
Background<br />
Genome-wide association study identified ORM1-like 3 (ORMDL3) as an asthma candidate gene.<br />
ORMDL3 encodes a 4-transmembrane domain-containing protein that is localized to the endoplasmic<br />
reticulum membrane. Although current knowledge of ORMDL3 function is limited, it was associated<br />
with asthma in different population samples. Rs7216389 was one of the most studied SNPs in<br />
ORMDL3 and it was associated with asthma in numerous studies. There is much less data about<br />
rs4795405 C>T, which was missing in majority of above mentioned studies. Therefore we evaluate<br />
rs4795405 allele frequencies in Slovenian children with different severity (severe, moderate, mild)<br />
and healthy controls.<br />
Methods<br />
All subjects came from the East-North region and were genotyped with Real Time TaqMan allelic<br />
discrimination assay, using DNA isolated from blood specimens.<br />
Results<br />
We clearly showed that SNP rs4795405 was significantly associated with asthma risk and severity in<br />
our study groups. The frequency of risk allele C was significantly higher in asthmatic patients than in<br />
healthy controls. Patients with severe asthma had higher C allele frequency, compared to moderate<br />
and mild. Groups of patients with severe and moderate asthma had significantly different allele C frequency.<br />
Conclusions<br />
Finally we can summarize that SNP rs4795405 might be an important asthma genetic marker. It is not<br />
only associated with asthma development, but also with asthma severity in Slovenian children. Therefore<br />
it is necessary to replicate our study on bigger population samples, to additionally confirm its involvement<br />
in asthma.<br />
81
Expression profiles of regulatory<br />
genes after venom immunotherapy<br />
Mira Øilar 1 , Branko Pevec 2 , Matija Rijavec 1 , Renato Eræen 1 ,<br />
Mitja Koønik 1 , Asja Stipiå Markoviå 2 , Peter Koroøec 1<br />
1<br />
University Clinic of Respiratory and Allergic Diseases, Golnik<br />
2<br />
Clinical Hospital Sveti Duh, Department of Clinical Immunology, Pulmonology and Rheumatology,<br />
Zagreb, Croatia<br />
Background<br />
The aim of our study was to investigate the ex vivo gene expression profiles of transcription factors<br />
involved in the regulation of Treg, Th1 and Th2 cells, namely FOXP3, T-BET and GATA-3, and the efficacy<br />
of venom immunotherapy (VIT).<br />
Methods<br />
For the purpose of the study we have included 5 groups of subjects. First group included 24 Hymenoptera<br />
sting allergic patients, whose samples were taken before starting VIT. In second group<br />
28 patients were on VIT for 1 year and sampling was done just before the next maintenance dose.<br />
The third group represents 22 patients after completed VIT, which lasted from 3 to 5.5 years. The sampling<br />
was done just before sting challenge. Sting challenge was performed with the insects implicated<br />
by the VIT. The fourth group consisted of 25 healthy control subjects and the last study group consisted<br />
of 20 atopic patients with mite allergy and allergic rhinitis. Total RNA was isolated from peripheral<br />
blood, reverse transcribed to cDNA and the expression was analyzed with Real time PCR<br />
using the DDCt method.<br />
Results<br />
Expression levels of FOXP3, T-BET and GATA-3 were significantly higher in patients with successfully<br />
completed VIT (negative sting challenge) compared to Hymenoptera venom allergic patients before<br />
VIT, after 1 year of VIT and also to healthy controls. Expression level of T-BET was also<br />
significantly higher in comparison to atopic subjects, but that was not the case for FOXP3 and GATA-<br />
3. Levels of all those markers were also higher compared to the patient who has positive sting challenge<br />
after completed VIT.<br />
Conclusions<br />
Our results suggest that increased expression of FOXP3 might be significantly associated with successfulness<br />
of VIT and long term allergen tolerance.<br />
There was no change of transcription factor expression after one year of immunotherapy. This finding<br />
could explain why short lasting immunotherapy has no long term effect.<br />
82
Baseline serum tryptase is not<br />
associated with the risk for severe<br />
anaphylactic reactions in honey bee<br />
venom allergy<br />
Nina Œelesnik, Peter Kopaœ, Renato Eræen, Mira Øilar, Mitja Koønik, Peter Koroøec<br />
University Clinic of Respiratory and Allergic Diseases, Golnik<br />
Background<br />
An elevated level of tryptase outside anaphylaxis in Hymenoptera allergy has not yet been fully elucidated.<br />
The aim of our study was to evaluate whether a baseline tryptase level predicts the severity<br />
of anaphylactic reaction in honey bee venom allergy.<br />
Methods<br />
We included 184 Hymenoptera venom allergic patients with established honey bee venom allergy.<br />
The study group consisted of patients with large local reaction - LLR (11%), Mueller grade I (8%), II<br />
(18%), III (40%) and IV (23%) after a honey bee field sting. Furthermore all recruited patients had positive<br />
sIgE for honey bee venom and negative for wasp venom. Diagnostic evaluations occurred at<br />
least 14 days after the field sting by ImmunoCAP (Phadia). The value of 11.4 µg/L was considered<br />
to be elevated.<br />
Results<br />
Baseline serum tryptase values were highly comparable between different subgroups of patients.<br />
The comparison between the subgroups clearly did not show any significant differences in elevated<br />
baseline serum tryptase levels, as 5% of LLR and 0%, 3%, 4% and 7% of Mueller grade I, II, III and<br />
IV subgroups exceeded the value for normal baseline tryptase value.<br />
Conclusions<br />
The results of our study indicate that there is no significant association between an elevated serum<br />
tryptase and severe anaphylaxis in honey bee venom allergy. Previous findings observed an elevated<br />
baseline serum tryptase significantly more often in wasp venom than in honey bee venom allergic<br />
patients, which may elucidate our findings.<br />
83
Diagnosis of double sensitized<br />
Hymenoptera venom allergic patients<br />
with recombinant species-specific<br />
major allergens used in basophil<br />
activation test<br />
Nina Œelesnik 1 , Renato Eræen 1 , Mira Øilar 1 , Irene Mittermann 2 ,<br />
Rudolf Valenta 2 , Mihaela Zidarn 1 , Mitja Koønik 1 , Peter Koroøec 1<br />
1<br />
University Clinic of Respiratory and Allergic Diseases, Golnik<br />
2<br />
Christian Doppler Laboratory for Allergy Research, Center for Physiology and Pathophysiology,<br />
Dept. of Pathophysiology/Division of Immunopathology, Medical University of Vienna, Vienna, Austria<br />
Background<br />
Double positivity to honey bee and wasp venom necessitates supplementary testing to distinguish<br />
genuine double sensitization from cross-reactivity in patients, who are unable to identify the culprit<br />
insect. Our aim was to define their primary sensitization.<br />
Methods<br />
We included 14 Hymenoptera venom allergic patients with double-positive sIgE to both venoms. Furthermore<br />
all recruited patients had double-positive basophile activation test as well. The culprit insect<br />
responsible for their anaphylactic reaction remained unidentified. Additional testing was<br />
performed with recombinant species-specific major allergens rApi m1, rApi m2 and rVes V5.<br />
Results<br />
With the use of recombinant species-specific allergens in basophile activation testing we were able<br />
to identify 4 patients with unambiguous wasp venom sensitization, 5 patients with antibodies to wasp<br />
venom and cross-reactive hyaluronidase and 1 patient with cross-reactive antibodies exclusively to<br />
hyaluronidase. One the other hand the remaining 3 patients were displaying a genuine double sensitization<br />
to both species-specific major allergens. In one patient, who did not react with any of the<br />
species-specific major allergens, additional measurements with OSR and MUX from bromelain, revealed<br />
his true sensitization to cross-reactive carbohydrate determinants.<br />
Conclusions<br />
Our results demonstrate the usefulness of species-specific recombinant allergens in elucidating double-positivity<br />
in Hymenoptera venom allergy. Determining the primary sensitizing insect is crucial for<br />
selection of appropriate venom immunotherapy, as it is unlikely that immunotherapy with the second<br />
venom would be of any additional benefit.<br />
84
Rhinitis symptoms caused by grass<br />
pollen are associated with elevated<br />
basophil allergen sensitivity and a<br />
larger grass-specific IgE fraction<br />
Mihaela Zidarn, Mitja Koønik, Mira Øilar, Andrej Grahek, Peter Koroøec<br />
University Clinic of Respiratory and Allergic Diseases, Golnik<br />
Background<br />
The mechanisms responsible for the difference between clinically irrelevant IgE sensitization and allergic<br />
rhinitis are not fully understood. For that reason, we evaluated the humoral and cellular mechanisms<br />
that may be associated with the presence of allergic rhinitis symptoms.<br />
Methods<br />
We selected 26 of 33 subjects with positive grass pollen skin tests, elevated sIgEs specific for Timothy<br />
(g6) and the major grass allergen r Phl p 1, 5b. Fourteen of those patients reported a history of<br />
allergic rhinitis. During winter, we performed a grass pollen CD63 basophil activation test using four<br />
log allergen concentrations, followed by a grass nasal provocation test (NPT). In the subsequent pollination<br />
season, we obtained symptom scores.<br />
Results<br />
We showed that the subjects with a positive NPT have significantly higher CD63 basophil grass pollen<br />
responsiveness then NPT-negative subjects, preferably at sub-maximal allergen concentrations,<br />
which represent cellular sensitivity. Moreover, basophil sensitivity positively correlated with the size<br />
of the grass-specific IgE fraction in relation to total IgE levels, and it was highly predictive of allergic<br />
rhinitis symptoms in the following pollination season.<br />
Conclusions<br />
Allergic rhinitis symptoms are significantly associated with allergen basophil sensitivity, and this cellular<br />
allergen sensitivity correlates with the percentage of grass pollen-specific IgE antibodies relative<br />
to total IgE antibody levels. In vitro evaluation of basophil sensitivity should prove useful for<br />
distinguishing clinical phenotype of allergic sensitization.<br />
85
Diagnosis of double sensitized<br />
Hymenoptera venom allergic patients<br />
with recombinant species-specific<br />
major allergens used in basophil<br />
activation test<br />
Peter Kopaœ 1,2,3 , T. Gentinetta 1,2 , M. Rudin 2 , R. Gerber 2 ,<br />
C. Pichler 2 , O. Hausmann 2 , B. Schnyder 2 , W.J. Pichler 1,2<br />
1<br />
ADR-AC GmbH, Holligenstrasse 91, CH-3008 Bern<br />
2<br />
Division of Allergology, Clinic for Rheumatology and Clinical Immunology/Allergology, Inselspital,<br />
University of Bern, CH-3010-Bern, Switzerland,<br />
3<br />
University Clinic of Respiratory and Allergic Diseases, Golnik<br />
Background<br />
Patients with birch pollen allergy (major allergen: Bet v1) have often an associated oral allergy syndrome<br />
(OAS) to apple, which contain the cross-reactive allergen Mal d1. As successful birch pollen<br />
immunotherapy does not consistently improve apple related OAS symptoms, we evaluated if regular<br />
apple consumption has an effect on apple associated OAS and immune parameters of Mal d1 or<br />
Bet v1 allergy.<br />
Methods<br />
40 patients with a clear history of birch pollen rhino-conjunctivitis and associated OAS to apple were<br />
included into randomized, controlled clinical trial. 13 patients remained untreated (control group),<br />
while 27 patients (active group) consumed daily small amounts of apple (“Golden Delicius” strain with<br />
high content of Mal d1 (6,2 ug/g)). Starting dose was the smallest dose, causing not yet or only very<br />
minor OAS, determined by oral provocation tests (OPT). The dose was increased gradually and was<br />
doubled every 2-3 weeks, always aiming to remain free of symptoms in spite of eating more apples.<br />
In vivo (OPT, intradermal tests (ITD) with Bet v1 and Mal d1, conjunctival provocation test (CPT) with<br />
Bet v1) and in vitro tests (sIgE, sIgG4, basophil activation test (BAT) with both allergens) were performed<br />
at the beginning and after 8 months.<br />
Results<br />
5/27 patients in the active group withdrew (2 experienced local mild gastrointestinal side effects, 3<br />
because personal reasons). After approximately 20 weeks (17-30 weeks) of regular apple consumption,<br />
17/27 patients in the active group could tolerate a whole apple (~ 200g) without OAS. The<br />
dose of apple tolerated at OPT increased from 4g to 128g (p: 0.00001) after 8 months; A few patients<br />
could also tolerate some cross-reactive food. 5/27 patients of the active group could not successfully<br />
reach maintenance dose despite trying eating apple. Stop of apple consumption lead to rapid<br />
reappearance of symptoms. All (13/13) patients in control group had an unchanged reactivity to<br />
apple at the beginning and at the end of the study. In vivo (ITD, CPT) and in vitro (sIgE, sIgG4 levels,<br />
BAT) tests were not significantly altered in the active vs. control group.<br />
86
Conclusions<br />
We provide a protocol of oral desensitization to apple, which was safe and highly successful in clinical<br />
terms, while no clear change of immunological parameters was seen in the 8 months of “apple<br />
therapy”. The procedure proposed seems to induce similar effects as drug desensitization, and may<br />
be transient and only affect the oral mucosa.<br />
87
Comparison of basophil activation test<br />
and inhibition tests in double positive<br />
Hymenoptera venom allergic patients<br />
Renato Eræen, Mira Øilar, Peter Koroøec, Mitja Koønik<br />
University Clinic of Respiratory and Allergic Diseases, Golnik<br />
Background<br />
In Hymenoptera venom allergic patients double positive tests are frequently found. Distinguishing between<br />
double sensitization and cross reactivity is crucial for choosing proper venom for specific immunotherapy.<br />
In diagnostic procedure of double positive patients inhibition tests are helpful. In our<br />
analysis we compared the results of inhibition tests and BAT in evaluating double sensitization and<br />
cross reactivity.<br />
Methods<br />
Patients with a history of anaphylactic reaction after Hymenoptera sting are included into study. Double<br />
positivity was diagnosed with skin prick tests and specific IgE (FEIA, Uppsala, Sweden). FEIA inhibition<br />
tests and BAT were performed in all patients.<br />
Results<br />
26 double positive patients were included into study. 92.3% experienced anaphylactic reaction Muller<br />
grade IV and 7.7% Muller grade III. The culprit insect was honeybee in 38.4% of the patients, wasp<br />
in 30.8% of patients and unknown in 30.8% of patients. In 73.2% of patients the results of inhibition<br />
tests and BAT matched and showed double sensitization. In 15.4% BAT showed double sensitization<br />
while inhibition tests cross reactivity. In 7.6% inhibition tests showed double sensitization while<br />
in BAT only sensitization with one culprit was confirmed.<br />
Conclusions<br />
In distinguishing double sensitization and cross reactivity inhibition tests and BAT are complementary.<br />
Cross-reactive hyaluronidase with proven cross-reactivity in inhibition tests could result in double<br />
positive BAT. Interpretation of results requires careful reassessment and correlation with<br />
anamnestic data.<br />
88
Association analysis of polymorphisms<br />
in selected candidate genes<br />
in slovenian children with astma<br />
Petra Perin 1,2 , Vojko Berce 3 , Uroø Potoœnik 1,2<br />
1<br />
Center for Human Molecular Genetics and Pharmacogenomics, Faculty of Medicine, University of<br />
Maribor, Maribor<br />
2<br />
Laboartory for Biochemistry Molecular Biology and Genomics, Faculty of chemistry and chemical<br />
tehnology, University of Maribor, Maribor<br />
3<br />
Department of Pediatrics, University Medical Centre Maribor<br />
Background<br />
Many candidate genes initially associated with asthma or asthma phenotypes were not confirmed as<br />
asthma genes in the follow up independent studies in different populations. In most association studies,<br />
candidate genes were compared between controls and all asthma patients in one group. The aim<br />
of our study was the association analysis of selected genes in Slovenian asthmatic children.<br />
Methods<br />
We analyzed candidate genes in all asthmatics and separately in the group of atopic asthmatics and the<br />
group of non-atopic asthmatics. In addition, we have analyzed the correlation between selected polymorphisms<br />
(SNPs), clinical parameters and response to therapy with glucocorticoids. Using bioinformatics<br />
tools nine single nucleotide polymorphisms (SNPs) in nine different candidate genes were selected.<br />
We have genotyped 247 children with asthma and 186 healthy controls. Genotyping was performed by<br />
polymerase chain reaction (PCR) and by the restriction fragment length polymorphism (RFLP) analysis.<br />
Results<br />
We have found significant association of genes CCR5, IL13 and RANTES and asthma. In addition, we found<br />
that non-atopic asthmatics with CC or CT genotype for SNP 159C/T in CD14 gene have increased bronchial<br />
hyperreactivity measured by PC20 of methacholine (0.41 mg/ml, compared to 1.50 mg/ml in patients with<br />
TT genotype, p = 0.018). The same SNP is also associated with FEV1/FVC ratio as a measure of bronchial<br />
obstruction in sub-group of non-atopic patients. Carriers of at least one allele T for SNP -159C/T have a<br />
lower FEV1/FVC ratio (87.4%), compared to 91.8% in patients with CC genotype (p=0.017). In atopic asthmatics<br />
we found that IL12B gene influences the bronchial obstruction (p = 0.006). In addition, we are the<br />
first ones who associated CTLA4 and ORMDL3 with response to asthma therapy with glucocorticoids.<br />
Conclusions<br />
Our results contribute to our understanding of the asthma pathogenesis. SNPs which we have identified<br />
as associated with asthma, asthma phenotypes, severity or response to therapy may in future<br />
serve as diagnostic and prognostic biomarkers and lead to better management of asthma patients.<br />
89
WORKSHOP<br />
DELAVNICA – ORGANIZIRAJOŒA PLJUŒNICA<br />
91
Organizirajoœa pljuœnica –<br />
histopatoloøka entiteta<br />
Izidor Kern<br />
Univerzitetna klinika za pljuœne bolezni in alergijo Golnik<br />
Za organizirajoœo pljuœnico (OP) je znaœilna razrast granulacijskega tkiva v svetlini malih dihalnih<br />
poti in okolnih alveolarnih prostorih. Gre za nespecifiœen, pogost odgovor pljuœnega tkiva na razliœne<br />
etioloøke dejavnike z vzorcem intraluminalne fibroplazije z organizacijo vnetnega eksudata. Zaradi<br />
moæne soœasne histoloøko spremenjene strukture stene malih dihalni poti je sinonim za OP tudi obliterantni<br />
bronhiolitis z organizirajoœo pljuœnico (BOOP), kar vnaøa zmedo in ga zato opuøœamo.<br />
Spremembe so v pljuœih razporejene æariøœno (tabela 1). Osnovna arhitektura pljuœnega parenhima<br />
je v celoti ohranjena. Izstopa proliferacija rahlega veziva, granulacijskega tkiva distalno v pljuœih (v<br />
svetlinah malih dihalnih poti, alveolarnih vodov in okolnih alveolov), kar imenjemo tudi Massonovi<br />
poganjki. Gre za œasovno unimorfne bronhiolocentriœne spremembe. Vezivo je bogato z mukopolisaharidi<br />
in ne vsebuje zrelega kolagena, zato ga lahko prikaæemo s specialnimi barvanji (slika 1). V<br />
vezivnih œepih so lahko prisotni fibrin, siderofagi in vnetnice. Blaga do zmerna vnetnoceliœna infiltracija<br />
zajame tudi alveolarne septe. V vnetnem infiltratu so limfociti in plazmatke. Izraæene so reaktivne<br />
spremembe alveolarnega epitela s hiperplazijo pnevmocitov tipa 2. V alveolih se kopiœijo penasti<br />
makrofagi. V intersticiju ni pomembne fibroze. Ni razvitega granulomskega vnetja. Prav tako je pomembna<br />
odsotnost eozinofilcev, nevtrofilcev, oblikovanja abscesov, nekroze, hialinih membran, fibrina.<br />
Tabela 1. Znaœilnosti histoloøkega vzorca OP.<br />
Vedno prisotno Lahko prisotno Odsotno<br />
1. æariøœne spremembe<br />
2. bronhiolocentriœna<br />
razporeditev<br />
3. fibroblastni œepi<br />
4. blaga kroniœna vnetnoceliœna<br />
intersticijska infiltracija<br />
5. arhitektura parenhima<br />
ohranjena<br />
1. Obliterantni bronhiolitis 1. izrazita eozinofilija<br />
2. pomembna intersticijska<br />
fibroza<br />
3. granulomi<br />
Vzorec OP pogosto sreœujemo sekundarno zaradi razliœnih vzrokov (tabela 2). Iz histopatoloøke slike<br />
vzorca OP ne moremo zanesljivo sklepati o moæni etiologiji. V primerih, da so razen vzorca OP izraæene<br />
øe druge histopatoloøke spremembe, se diferencialno diagnostiœne moænosti zelo razøirijo (tabela 3<br />
in 4). Pomembno je, da vzorec OP najdemo tudi pri lokaliziranih, nodularnih spremembah v pljuœih.<br />
Te se lahko kliniœnoradioloøko kaæejo kot pljuœni tumor, zato je bolnik lahko kirurøko zdravljen.<br />
92
Tabela 2. Moæni vzroki vzorca OP<br />
idiopatsko<br />
okuæbe<br />
zdravila<br />
Sistemske vezivnotkivne bolezni<br />
Kriptogena organizirajoœa pljuœnica<br />
bakterije (klamidija, mikoplazma, nokardija, streptokok, stafilokok, …),<br />
virusi (herpes, HIV, gripa, parainfluenca),<br />
glive (kriptokok, pnevmocista)<br />
Amiodaron, bleomicin, busulfan, soli zlata, sulfasalazin,…<br />
Revmatoidni artritis, Sjoegrenov sindrom, sistemski lupus eritemetodes,<br />
sistemska skleroza, idiopatske vnetne miopatije<br />
Tabela 3. Histopatoloøke entitete z vzorcem OP<br />
OP<br />
OP je ena od histopatoloøkih sprememb<br />
OP je nespecifiœna reakcija<br />
Idiopatsko (kriptogena OP)<br />
Sekundarno (glej tabelo 2)<br />
Preobœutljivostni pnevmonitis, Wegenerjeva granulomatoza,<br />
eozinofilna pljuœnica<br />
Perifokalna sprememba ob abscesu, tumorju, infarktu<br />
Aspiracija<br />
Vaskulitis<br />
Tabela 4. Diferencialna diagnoza histopatoloøkega vzorca OP<br />
Difuzna alveolarna okvara v organizaciji<br />
Obiœajna intersticijska pljuœnica (UIP)<br />
Nespecifiœna intersticijska pljuœnica (NSIP)<br />
Preobœutljivostni pnevmonitis<br />
Wegenerjeva granulomatoza<br />
Eozinofilna pljuœnica v organizaciji<br />
Akutna fibrinozna in OP<br />
Konstriktivni bronhiolitis - sekundarno<br />
Organizacija alveolarne krvavitve<br />
Organizacija infekcijske pljuœnice<br />
Organizacija obstrukcijskega pnevmonitisa<br />
Prizadetost pljuœ zaradi zdravil<br />
Prizadetost pljuœ zaradi vdihovanja ali izpostavljenosti toksinom<br />
Prizadetost pljuœ v sklopu sistemskih vezivnotkivnih bolezni<br />
Prizadetost pljuœ pri kroniœnih vnetnih œrevesnih boleznih<br />
Organizacija ob robu drugih procesov (infarkt, absces, tumor,…)<br />
Kriptogena organizirajoœa pljuœnica<br />
Slika 1. Intraluminalna proliferacija mladega veziva (Giemsa)<br />
93
Organizirajoœa pljuœnica –<br />
spekter radioloøkih vzorcev<br />
Igor Poæek<br />
Univerzitetna klinika za pljuœne bolezni in alergijo, Golnik<br />
Organizirajoœa pljuœnica (OP) je histopatoloøki vzorec in predstavlja stopnjo nespecifiœnega odgovora<br />
na poøkodbo pljuœ zaradi razliœnih vzrokov (glej predavanje dr. Kerna – tabela2). OP je tudi kliniœna<br />
entiteta, ki se kaæe z nespecifiœnimi simptomi in razliœnimi radioloøkimi spremembami in je lahko<br />
primarna – kriptogena (COP) ali sekundarna. Radioloøke spremembe pri OP so øtevilne. Opisani<br />
bodo najpogostejøi in øele pred kratkim opisani radioloøki vzorci OP. Pogosto je hkrati prisotnih veœ<br />
vzorcev, nekateri vzorci si œasovno sledijo. Zunaj-pljuœne spremembe so vidne v manjøem odstotku<br />
in zajemajo plevralni izliv ter blago do zmerno poveœane mediastinalne bezgavke.<br />
Klasiœni radioloøki vzorci OP<br />
Migrirajoœe multifokalne periferne konsolidacije. Veœina, pribliæno ¾ pacientov s COP ima v pljuœih<br />
multifokalne infiltrate oz. konsolidacije, ki leæijo najveœkrat periferno in spreminjajo lokacijo v poteku<br />
nekaj tednov. Na CT-ju imajo infiltrati viden zraœni bronhogram, veœkrat jih obdajajo zgostitve mleœnega<br />
stekla. Pogosteje so prizadeti spodnji deli pljuœ, œeprav nekateri avtorji ugotavljajo enakomerno razporeditev<br />
sprememb v vseh pljuœnih poljih. Spontan regres in migracija infiltratov zoæita diferencialno<br />
diagnozo sprememb na pljuœih na COP, eozinofilno pljuœnico, krvavitev in vaskulitis.<br />
Bronhocentriœni vzorec se pojavlja pri cca 1/3 pacientov. Okoli veœjih bronhovaskurarnih snopov so<br />
vidne trakaste konsolidacije, ki so pogostejøe v spodnjih delih pljuœ in lahko segajo do periferije oz.<br />
subplevralno. Pogosto so pridruæene zgostitve mleœnega stekla ali nodularne spremembe.<br />
Neobiœajni vzorci<br />
Solitarna fokalna masa/tumor ali nodul. Gre za fokalno zgostitev, ki ne vsebuje zraœnega bronhograma<br />
in je ne moremo loœiti od pljuœnega tumorja oz. malignoma, œeprav je najveœkrat bolj ovalne<br />
ali romboidne oblike. Pogosteje se nahaja v zgornjih reænjih. Obiœajno kopiœi FDG na PET-u, kar ne<br />
omogoœa razloœevanja od pljuœnega raka.<br />
Nodularen vzorec je lahko viden pri cca 1/3 pacientov, najveœkrat so pridruæeni øe drugi radioloøki<br />
vzorci. Noduli so obiœajno acinarne velikosti (cca 6-10 mm), œeprav so lahko vidni tudi mikronoduli<br />
(< 4 mm). Obiœajno leæijo peribronhovaskularno ali periferno, redko tudi centrilobularno ali v obliki<br />
vejic s popki, kar je znaœilnost eksudativnega bronhiolitisa.<br />
94
Multiple mase ali veœji noduli. Ob prisotnosti veœih tumorskih mas je pomembna izkljuœitev metastaz,<br />
limfoma ali multicentriœnega adenokarcinoma. Pri razloœevanju nam najveœkrat pomaga hkratna<br />
prisotnost drugih vzorcev, pogost o je vsaj mestoma viden zraœni bronhogram. Pri imunokompromitiranem<br />
bolniku ima podobno sliko lahko invazivna aspergiloza.<br />
Progresivno fibrozni vzorec. Na mestu perifernih konsolidacij se postopoma pojavljajo retikularne,<br />
mreæaste spremembe s spremenjeno arhitekturo pljuœ , podroœja mleœnega stekla, noduli in vœasih<br />
satasta pljuœa, kar spominja na fibrozno obliko NSIP.<br />
Perilobularen vzorec je opisan pri veœ kot polovici pacientov s COP, obiœajno je viden skupaj z<br />
drugimi vzorci in ima zato pomembno diagnostiœno vrednost. Predstavlja prizadetost pljuœ na obrobju<br />
sekundarnega pljuœnega lobulusa, ki se kaæe kot neostro omejena poligonalno oblikovana trakasta<br />
podroœja konsolidacij na periferiji pljuœ, obiœajno subplevralno, med katerimi so normalno prezraœena<br />
pljuœa.<br />
Parenhimski traœki predstavljajo trakasta podroœja konsolidacij øirine veœ kot 8 mm, ki potekajo do<br />
plevre, ki ni zadebeljena in vsebujejo enojen zraœni bronhogram, po œemer jih loœimo od trakastih<br />
atelektaz.<br />
Vzorec obrnjenega haloja (reversed halo) ali atolni vzorec. Polkroæna ali obroœasta konsolidacija,<br />
ki obdaja zgostitve mleœnega stekla v sredini je bila najprej opisana pri pacientih z OP in sicer pri cca<br />
20% pacientov. Kasneje je bil vzorec opisan øe pri nekaterih drugih boleznih (sarkoidoza, Wegenerjeva<br />
granulomatoza, ..), kar je nekoliko zmanjøalo njegovo diagnostiœno vrednost.<br />
Crazy paving. Zgostitve mleœnega stekla so vidne pri veœini pacientov z OP, predvsem kot ostanki<br />
prej vidnih konsolidacij pa tudi samostojno. Zadebeljena interlobularna septa so pogosto vidna na<br />
obrobju konsolidacij, vendar obiœajno niso izrazita. Kombinacija mleœnega stekla in zadebeljenih interlobularnih<br />
sept da vzorec »crazy paving«, ki je bil opisan pri OP kot posledica jemanja nekaterih<br />
zdravil.<br />
95
Organizirajoœa pljuœnica –<br />
kliniœni problem<br />
Katarina Osolnik<br />
Univerzitetna klinika za pljuœne bolezni in alergijo, Golnik<br />
S kliniœnega staliøœa o diagnozi organizirajoœe pljuœnice z gotovostjo lahko govorimo øele po prejemu<br />
histoloøkega izvida biopsije pljuœ. Seveda je odloœitev o napotitvi bolnika na invazivno diagnostiko<br />
(bronhoskopija s transbronhialno biopsijo in bronhoalveolarno lavaæo, kirurøka pljuœna biopsija) v<br />
rokah klinika. Le-ta se mora na podlagi anamnestiœnih podatkov, kliniœnih ugotovitev, izvidov radioloøkih<br />
preiskav (rentgenska slika in visokoloœljivostna raœunalniøka tomografija - HRCT), laboratorijskih<br />
preiskav krvi, meritev pljuœne funkcije in upoøtevaje bolnikovo stanje, odloœiti za najprimernejøi<br />
naœin ugotovitve etiologije infiltratov v pljuœih.<br />
Kliniœno obravnavo bolnika z organizirajoœo pljuœnico delimo lahko na dva dela.<br />
Prvi del predstavlja obravnavo bolnika s pljuœnimi infiltrati razliœnih vrst: od bilateralnih intersticijskih<br />
in alveolarnih zgostitev, nesimetriœno razporejenih infiltratov in solitarnih infiltratov v kateremkoli delu<br />
pljuœ pred pridobitvijo histoloøkega izvida – organizirajoœa pljuœnica, ki je nespecifiœna in pogosta<br />
reakcija pljuœnega tkiva na razliœne vzroœne dejavnike. Natanœna anamneza z vsebovanimi demografskimi<br />
podatki, poklicnimi in okoljskimi izpostavitvami, natanœnim popisom jemanja trenutne in<br />
pretekle terapije, epidemioloøkimi podatki, natanœen kliniœni pregled, rentgenska slika, preiskava<br />
pljuœne funkcije vkljuœno z difuzijsko kapaciteto za CO, osnovne laboratorijske preiskave (KKS, CRP,<br />
retenti, urin) in visokoloœljivostni CT so zaœetni in temeljni postopki obravnave.<br />
Vzorec HRCT zoæi diagnostiœno paleto, v veœini primerov pa HRCT ni specifiœen in kliniku v teku diagnostike<br />
obiœajno sugerira vsaj dve, lahko tudi veœ moænosti, ki jih mora z vodenjem nadaljnjega<br />
postopka diagnostike - invazivnimi postopki - razreøiti.<br />
Na podlagi retrogradnih analiz naøih bolnikov ugotavljamo, da so najpogostejøi simptomi in znaki:<br />
kaøelj, dispneja, zviøana temperatura, znojenje, hemoptize, v avskultatornem izvidu nad pljuœi pa inspiratorni<br />
poki. Velika veœina bolnikov prejema kot ustaljeno terapijo veœ razliœnih zdravil, obiœajno<br />
so zdravljeni æe pred zaœetkom pulmoloøke obravnave z vsaj enim antibiotikom. Pri veliki veœini naøih<br />
bolnikov smo histoloøko diagnozo organizirajoœe pljuœnice postavili s transbronhialno biopsijo ob<br />
bronhoskopiji z upogljivim bronhoskopom.<br />
Pred zaœetkom invazivne diagnostike se mora klinik opredeliti do okuæbe kot moænega vzroka radioloøko<br />
vidnih sprememb. Pri bolnikih s kliniœnimi in laboratorijskimi znaki okuæbe je potrebno odvzeti<br />
96
kuænine: hemokulture pri bolnikih s srednje teæko in teæko kliniœno sliko, in sicer pred uvedbo ali menjavo<br />
antibiotiœnega zdravljenja, œe bolnik izkaøljuje, kultiviramo izmeœek na patogene bakterije. Ob<br />
posebnih epidemioloøkih in anamnestiœnih podatkih odvzamemo kuænine za dokazovanje atipiœnih<br />
povzroœiteljev pljuœnic: izmeœek ali bris ærela za dokazovanje atipiœnih in virusnih povzroœiteljev z<br />
metodo veriæne reakcije (PCR) in urin za dokazovanje antigena legionele in pnevmokoka.<br />
Øe pred nadaljevanjem z invazivno diagnostiko je potrebno posebno pozornost posvetiti zdravilom,<br />
ki jih je ali jih trenutno bolnik prejema. V kolikor obstaja po zdruæitvi anamnestiœnih, kliniœnih in radioloøkih<br />
preiskav verjetnost, da gre za preobœutljivostno reakcijo za doloœeno zdravilo, je le-to<br />
potrebno takoj ukiniti.<br />
Podatek o sistemskih vezivno tkivnih boleznih, ki so pri bolniku æe diagnosticirane, mora klinika<br />
nenehno spremljati in usmerjati v iskanje moænih povezav s spremembami na pljuœih.<br />
Drugi del kliniœne obravnave sledi po pridobitvi histoloøkega izvida-organizirajoœa pljuœnica, ki za<br />
klinika pogosto lahko pomeni zaœetek iskanja vzroka. Najpogostejøi vzroki sekundarne organizirajoœe<br />
pljuœnice so bakterijske (veœkrat atipiœne), virusne (influenca) in gliviœne okuæbe, zdravila (amiodaron,<br />
citostatiki, sulfasalazin, soli zlata) in sistemske vezivnotkivne bolezni, pri katerih je lahko pojav<br />
sprememb na pljuœih prva manifestacija do tedaj øe nepoznane sistemske vezivnotkivne bolezni.<br />
Glede na to, je skupino bolezni potrebno pri bolnikih z organizirajoœo pljuœnico aktivno iskati oziroma<br />
s seroloøkimi preiskavami izkljuœevati.<br />
Œe vzroka ne najdemo, govorimo o kriptogeni organizirajoœi pljuœnici.<br />
Za klinika je nujno poznavanje dejstva, da je organizirajoœa pljuœnica lahko samo ena od histopatoloøkih<br />
sprememb pri preobœutljivostnem pnevmonitisu, Wegenerjevi granulomatozi in eozinofilni<br />
pljuœnici in da lahko predstavlja samo nespecifiœno reakcijo ob abscesu, tumorju, pljuœnem infarktu,<br />
vaskulitisih in aspiracijskih pljuœnicah. Iz teh dejstev mora klinik izhajati pri odloœitvi, kdaj se s pridobitvijo<br />
histoloøkega izvida organizirajoœe pljuœnice diagnostiœni postopek zakljuœi, kdaj pa se z diagnostiko<br />
nadaljuje.<br />
Organizirajoœo pljuœnico uspeøno zdravimo s sistemskimi steroidi, ki so terapija izbora. Pri sekundarni<br />
organizirajoœi pljuœnici soœasno zdravimo spremljajoœo vezivnotkivno bolezen, okuæbo, pri z zdravili<br />
povzroœeni, zdravilo za katerega menimo, da je vzroœno povezano s pojavom organizirajoœe<br />
pljuœnice, ukinemo.<br />
Ni ugotovljenih razlik med pogostostjo relapsov in smrtnostjo pri kriptogeni in sekundarni organizirajoœi<br />
pljuœnici. Prognoza kriptogene organizirajoœe pljuœnice je v primerjavi s sekundarno boljøa.<br />
Pri slednji je odvisna od spremljajoœe bolezni-slabøa pri sistemskih vezivnotkivnih boleznih.<br />
97
Notes:<br />
98
Notes:<br />
99
Notes:<br />
100
Notes:<br />
101
Notes:<br />
102
Notes:<br />
103
Notes:<br />
104
Notes:<br />
105
PARTNERS<br />
Congress was supported by Slovenian Research Agency<br />
(Javna agencija za raziskovalno dejavnost Republike Slovenije)<br />
SPONSORS<br />
Astra<br />
Glaxo SmithKline<br />
Medis<br />
Novartis<br />
Boehringer Ingelheim<br />
Bayer HealthCare<br />
Eli Lilly<br />
Ewopharma<br />
IRIS<br />
Johnson &Johnson<br />
Krka<br />
LKB<br />
MEDA Pharma<br />
MSD<br />
Nycomed<br />
Olimpus<br />
Pfizer<br />
Providens<br />
Remas<br />
Roche<br />
Sanofi Aventis<br />
Sapio plini<br />
Torrex Chiesi<br />
106
RAZMISLIMO<br />
Boehringer Ingelheim je predan raziskovanju<br />
novih substanc na področju:<br />
ONC 01/marec <strong>2011</strong> Samo za strokovno javnost<br />
inhibicije angiogeneze tumorja<br />
inhibicije signalne poti<br />
kontrole celičnega cikla<br />
UKREPAJMO<br />
ONKOLOGIJA BOEHRINGER INGELHEIM
Najbolj predpisovano zdravilo za vzdræevalno zdravljenje KOPB 1 ,<br />
ki bolnikom æe 8 let lajπa dihanje in ohranja aktivno æivljenje 3,4<br />
ZGODNEJ©E ZDRAVLJENJE 2 aktivnejπi jutri 3,4<br />
SKRAJ©AN POVZETEK GLAVNIH ZNA»ILNOSTI ZDRAVILA<br />
Samo za strokovno javnost.<br />
SPIRIVA 18 mikrogramov praπek za inhaliranje, trde kapsule<br />
Kakovostna in koliËinska sestava: 1 kapsula vsebuje 22,5 µg tiotropijevega bromida monohidrata, kar ustreza 18 µg tiotropija. Terapevtske indikacije: Vzdræevalno bronhodilatacijsko zdravljenje, ki zmanjπa simptome pri bolnikih<br />
s kroniËno obstruktivno pljuËno boleznijo (KOPB). Odmerjanje in naËin uporabe: Inhalacija vsebine ene kapsule 1-krat na dan ob enakem Ëasu z vdihovalnikom HandiHaler. Bolnikov mlajπih od 18 let ne smemo zdraviti s Spirivo.<br />
Kontraindikacije: preobËutljivost za tiotropijev bromid, atropin ali njune derivate, npr. ipratropij ali oksitropij ter za pomoæno snov laktozo monohidrat. Posebna opozorila in previdnostni ukrepi: Tiotropijev bromid je bronhodilatator<br />
za vzdræevalno zdravljenje z enim odmerkom na dan in ga ne smemo uporabljati za zaËetno zdravljenje akutnih epizod bronhospazma oz. kot reπevalno zdravilo. Po dajanju tiotropijevega bromida v obliki praπka za inhaliranje se lahko<br />
pojavijo takojπnje preobËutljivostne reakcije. Tiotropijev bromid je treba previdno uporabljati pri bolnikih z glavkomom zaprtega kota, hiperplazijo prostate ali zaporo vratu seËnega mehurja. Pri zdravilih za inhaliranje lahko inhalacija<br />
sproæi bronhospazem. Pri bolnikih z zmerno do hudo ledviËno okvaro smemo uporabiti tiotropijev bromid samo, kadar je priËakovana korist zdravljenja veËja od morebitnega tveganja. Pri pojavu znakov in simptomov glavkoma<br />
zaprtega kota morajo bolniki tiotropijev bromid prenehati jemati in se nemudoma posvetovati s specialistom. Suha usta so lahko dolgoroËno povezana z zobnim kariesom. Bolniki z redko dedno intoleranco za galaktozo, laponsko<br />
obliko zmanjπane aktivnosti laktaze ali malabsorbcijo glukoze/galaktoze ne smejo jemati tega zdravila. Interakcije: Pri soËasni uporabi tiotropijevega bromida v obliki praπka za inhaliranje in drugih zdravil niso zasledili kliniËnih znakov<br />
interakcij. Ta zdravila so bila simpatikomimetiËni bronhodilatatorji, metilksantini ter peroralni in inhalacijski steroidi, ki jih pogosto uporabljamo v zdravljenju KOPB. SoËasnega zdravljenja s tiotropijevim bromidom in drugimi zdravili,<br />
ki vsebujejo antiholinergik, niso raziskovali, zato ga ne priporoËamo. NoseËnost in dojenje: ©tudije na æivalih so pokazale vpliv na sposobnost razmnoæevanja, povezano s toksiËnimi uËinki pri samici. Moæno tveganje za ljudi ni znano.<br />
Spirivo smemo med noseËnostjo uporabljati samo, kadar je jasno indicirana. Spirive med dojenjem ne priporoËamo. Tiotropijev bromid je dolgodelujoËa spojina. Pri odloËitvi o nadaljevanju ali prenehanju dojenja oziroma nadaljevanju ali<br />
ukinitvi zdravljenja s Spirivo je treba presoditi med koristjo dojenja za otroka in koristjo zdravljenja matere. Neæeleni uËinki: Pogost neæeleni uËinek so suha usta. ObËasni neæeleni uËinki so: omotica, glavobol, motnje okuπanja, meglen<br />
vid, fibrilacija preddvorov, kaπelj, faringitis, disfonija, stomatitis, slabost, gastroezofagealna refluksna bolezen, zaprtje, izpuπËaj, dizurija, zastoj seËa. Redki neæeleni uËinki so: nespeËnost, poveËan oËesni tlak, glavkom, tahikardija,<br />
palpitacije, supraventrikularna aritmija, epistaksa, bronhospazem, laringitis, sinusitis, zapora Ërevesa, tudi paralitiËni ileus, gingivitis, glositis, orofaringealna kandidoza, disfagija, urtikarija, pruritus, druge oblike preobËutljivosti (tudi<br />
takojπnje reakcije), okuæba seËil. Neæeleni uËinki neznane pogostnosti so: dehidracija, zobni karies, koæna okuæba in koæna razjeda, suha koæa, angionevrotiËni edem, sklepna oteklina. NaËin in reæim izdaje: Rp. Imetnik dovoljenja za<br />
promet: Boehringer Ingelheim International GmbH, Binger Straße 173, D-55216 Ingelheim am Rhein, NemËija.Za podrobnejπe informacije glejte Povzetek glavnih znaËilnosti zdravila, z dne 09.10.2009.<br />
Spirivo je razvilo podjetje Boehringer Ingelheim. Sopromovirata jo podjetji Boehringer Ingelheim in Pfizer.<br />
Literatura<br />
1. IMS podatki 2010. 2. Global Initiative for Chronic Obstructive Lung Disease. Global strategy for the diagnosis, management, and prevention<br />
of chronic obstructive pulmonary disease. Dopolnjeno 2009. http://www.goldcopd.org/Guidelineitem.asp?l1=2&l2=1&intId=2003.<br />
Dostop: april 2010. 3. Tashkin DP, Celli B, Senn S s sod.; on behalf of the UPLIFT ® (Understanding Potential Long-term Impacts on Function<br />
with Tiotropium) study investigators. A 4-year trial of tiotropium in chronic obstructive pulmonary disease. N Engl J Med. 2008;359:1543-<br />
1554. 4. Casaburi R, Kukafka D, Cooper CB, Witek TJ Jr, Kesten S. Improvement in exercise tolerance with the combination of tiotropium and<br />
pulmonary rehabilitation in patients with COPD. Chest. 2005;127:809-817.<br />
@ivljenje. Se nadaljuje.<br />
Pfizer Luxembourg SARL, Podruænica Ljubljana, Letaliπka 3c, Ljubljana<br />
Boehringer Ingelheim RCV, Podruænica Ljubljana, ©landrova 4b, Ljubljana<br />
Spiriva 8/september <strong>2011</strong>
PAH je redka in huda kronina bolezen pljunih krvnih žil, za katero je znailno<br />
progresivno poveanje vaskularne rezistence. e bolezni ne zdravimo, povzroi<br />
popušanje desne strani srca in prezgodnjo smrt. 1 PAH je lahko klasificirana kot idiopatska<br />
(iPAH) ali v povezavi z nekaterimi drugimi boleznimi, kot so bolezni vezivnega<br />
tkiva, prirojene srne napake in pri bolnikih z okužbo z virusom HIV. Povpreno preživetje<br />
nezdravljene napredujoe iPAH je po podatkih iz literature 2,8 let po postavitvi<br />
diagnoze, kar je primerljivo s prognozo napredujoih malignih bolezni. 2, 3<br />
V zgodnjih fazah PAH bolniki obiajno nimajo simptomov ali pa imajo blage netipine<br />
simptome (npr. pomanjkanje zraka), ki so lahko napano diagnosticirani (npr. kot<br />
astma). 4 Dispneja, še posebej ob naporu, je najpogostejši simptom, ki se pojavi<br />
pri skoraj vseh bolnikih in napreduje z napredovanjem bolezni. Od drugih simptomov<br />
navajajo utrujenost in splošno slabotnost, redkeje pa sinkopo ali anginozno<br />
boleino. Simptomi v mirovanju so prisotni le v napredujoi fazi bolezni. 1 Zaradi slabe<br />
prognoze in visoke umrljivosti je izjemno pomembno im prej postaviti diagnozo<br />
in zaeti zdravljenje. Zaradi nespecifinih simptomov je postavljanje tone diagnoze<br />
pogosto oteženo. 5<br />
Ob sumu na PAH ima kljuno vlogo transtorakalni ehokardiografski pregled, saj<br />
omogoa vpogled v stanje desne strani srca in doloanje pljunega arterijskega<br />
tlaka (PAP, pulmonary arterial pressure). Kateterizacija desne strani srca je zlati standard<br />
za potrditev PAH. 6<br />
Pred predpisovanjem zdravila Tracleer ® preberite Povzetek glavnih znailnosti zdravila, ki ga dobite pri naših strokovnih<br />
sodelavcih.<br />
Samo za strokovno javnost<br />
Ni astma.<br />
Ni anemija.<br />
Ni KOPB.<br />
Prepoznajte<br />
pljuno arterijsko<br />
hipertenzijo<br />
(PAH).<br />
www.pah-info.com www.medis.si<br />
(bosentan)<br />
Tracleer® temelj zdravljenja pljune arterijske hipertenzije (PAH)<br />
Srednji pljuni arterijski<br />
tlak 25 mmHg<br />
Pljuni zagozditveni<br />
tlak 15 mmHg<br />
Minutni volumen srca<br />
normalen ali zmanjšan<br />
Prilagojeno po Galiè et al; European Heart Journal (2009)<br />
Reference<br />
1. Galié N, Torbicki A, Barst R et al. Eur Heart J 2004; 25: 2243–2278. 2. D’Alonzo GE, Barst RJ, Ayres SM et al. Ann<br />
Intern Med 1991; 115: 343–9. 3. Kato I, Severson RK, Schwartz AG. Cancer 2001; 92: 2211–2219. 4. Hamilton N, Elliot<br />
C. Hosp Pharm 2006; 13: 7–9. 5. McLaughlin VV, Shillington A, Rich S. Circulation 2002; 106 (12): 1477–1482. 6. Galié<br />
N, Hoeper MM, Humbert M et al. Eur Heart J 2009; 30 (20): 2493–537.
z<br />
b<br />
f<br />
160 µg/4,5 µg/odmerek
SKRAJŠAN POVZETEK GLAVNIH ZNAČILNOSTI ZDRAVIL<br />
SYM 18/11 P<br />
Symbicort Turbuhaler 80 mikrogramov/4,5 mikrograma na odmerek prašek za inhaliranje<br />
Symbicort Turbuhaler 160 mikrogramov/4,5 mikrograma na odmerek prašek za inhaliranje<br />
Symbicort Turbuhaler 320 mikrogramov/9 mikrogramov na odmerek prašek za inhaliranje<br />
SESTAVA: Vsak inhalator Symbicort Turbuhaler 80 µg/4,5 µg na odmerek vsebuje 120 odmerkov. Vsak oddani odmerek (tisti, ki<br />
pride iz ustnika) vsebuje naslednji učinkovini: budezonid, in sicer 80 µg na vdih, in formoterolijev fumarat dihidrat, 4,5 µg na vdih.<br />
Vsak inhalator Symbicort Turbuhaler 160 µg/4,5 µg na odmerek vsebuje 120 odmerkov. Vsak oddani odmerek vsebuje naslednji<br />
učinkovini: budezonid, in sicer 160 µg na vdih, in formoterolijev fumarat dihidrat, 4,5 µg na vdih. Vsak inhalator Symbicort<br />
Turbuhaler 320 µg/9 µg na odmerek vsebuje 60 odmerkov. Vsak oddani odmerek vsebuje naslednji učinkovini: budezonid, in sicer<br />
320 µg na vdih, in formoterolijev fumarat dihidrat, 9 µg na vdih.<br />
INDIKACIJE: Zdravilo Symbicort Turbuhaler 80 µg/4,5 µg na odmerek je indicirano za redno zdravljenje astme, ko je primeren način<br />
zdravljenja kombinacija zdravil (inhalacijski glukokortikoid in dolgodelujoči agonist receptorjev beta2). Zdravilo Symbicort Turbuhaler<br />
80 µg/4,5 µg na odmerek ni primerno za bolnike s hudim astmatičnim obolenjem. Zdravili Symbicort Turbuhaler<br />
160 µg/4,5 µg na odmerek in 320 µg/9 µg na odmerek sta indicirani za redno zdravljenje astme, ko je primeren način zdravljenja<br />
kombinacija zdravil (inhalacijski glukokortikoid in dolgodelujoči agonist receptorjev beta2), in simptomatsko zdravljenje bolnikov s<br />
hudo obliko KOPB (FEV1 < 50 % predvidenega normalnega FEV1) ob ponavljajočih se poslabšanjih v anamnezi, ko se kljub<br />
zdravljenju z dolgodelujočimi bronhodilatatorji pojavljajo izraziti simptomi.<br />
ODMERJANJE IN NAČIN UPORABE: Inhalator Symbicort Turbuhaler se aktivira pri vdihu, kar pomeni, da ob bolnikovem vdihu<br />
skozi ustnik vdihan zrak odnese učinkovini v dihalne poti. Zaradi majhne količine zdravila v posameznem vdihu bolnik pri uporabi<br />
inhalatorja Turbuhaler morda sploh ne bo okusil ali začutil zdravila.<br />
ASTMA: Odmerjanje je individualno. Vzdrževalno zdravljenje (vse jakosti): bolnikom je potrebno svetovati, da imajo hitrodelujoči<br />
bronhodilatator vedno na razpolago. Odrasli (18 let ali več): Symbicort Turbuhaler 80 µg/4,5 µg na odmerek in 160 µg/4,5 µg na<br />
odmerek: 1–2 vdiha dvakrat na dan. Pri nekaterih bolnikih bodo potrebni tudi do največ 4 vdihi dvakrat na dan. Symbicort<br />
Turbuhaler 320 µg/9 µg na odmerek: 1 vdih dvakrat na dan. Pri nekaterih bolnikih bosta potrebna tudi do največ 2 vdiha dvakrat na<br />
dan. Mladostniki (12–17 let): 1–2 vdiha dvakrat na dan oz. 1 vdih dvakrat na dan (Symbicort Turbuhaler 320 µg/9 µg na odmerek).<br />
Otroci (6 let ali več): 2 vdiha dvakrat na dan (samo Symbicort Turbuhaler 80 µg/4,5 µg na odmerek). Zdravila Symbicort ne<br />
priporočamo pri otrocih, mlajših od 6 let. Vzdrževalno in olajševalno zdravljenje (Symbicort Turbuhaler 80 µg/4,5 µg na odmerek in<br />
Symbicort Turbuhaler 160 µg/4,5 µg na odmerek): bolniki redno jemljejo dnevni vzdrževalni odmerek zdravila Symbicort, ob pojavu<br />
simptomov pa po potrebi dodatne odmerke zdravila. Bolnikom je potrebno svetovati, da imajo zdravilo Symbicort kot olajševalec<br />
vedno pri sebi. Priporočeni odmerki: odrasli (18 let in več): priporočen vzdrževalni odmerek je 2 vdiha na dan, bodisi 1 vdih zjutraj<br />
in 1 vdih zvečer bodisi 2 vdiha zjutraj oziroma 2 vdiha zvečer. Za nekatere bolnike je primerno odmerjanje 2 vdiha dvakrat dnevno<br />
(Symbicort Turbuhaler 80 µg/4,5 µg na odmerek ali Symbicort Turbuhaler 160 µg/4,5 µg na odmerek). Ob pojavu simptomov se po<br />
potrebi naredi še 1 dodaten vdih. Če so simptomi po nekaj minutah še vedno prisotni, se doda še 1 vdih. Naenkrat ni dovoljeno<br />
narediti več kot 6 vdihov. Celotni dnevni odmerek, večji od 8 vdihov, v normalnih okoliščinah ni potreben. Kljub temu je lahko v<br />
določenih omejenih časovnih obdobjih celotni dnevni odmerek 12 vdihov. Vzdrževalno in olajševalno zdravljenje za otroke in<br />
mladostnike do 18. leta ni priporočljivo.<br />
KOPB: Priporočeni odmerki za odrasle: Symbicort Turbuhaler 160 µg/4,5 µg na odmerek 2 vdiha dvakrat na dan in Symbicort<br />
Turbuhaler 320 µg/9 µg na odmerek 1 vdih dvakrat na dan.<br />
KONTRAINDIKACIJE: Preobčutljivost za budezonid, formoterol ali laktozo.<br />
POSEBNA OPOZORILA IN PREVIDNOSTNI UKREPI: Priporočamo, da ob prekinitvi zdravljenja odmerek zmanjšujete postopoma in<br />
zdravljenja ne prekinete nenadoma. Če bolnik ugotavlja, da je zdravljenje neučinkovito ali če preseže največji priporočeni<br />
odmerek zdravila Symbicort, mora poiskati zdravniško pomoč. Bolnikom je treba naročiti, naj imajo olajševalec vedno pri sebi. Tako<br />
kot pri drugih inhalacijskih zdravilih se lahko tudi po uporabi tega zdravila pojavi paradoksni bronhospazem. Pri uporabi vseh<br />
inhalacijskih kortikosteroidov se lahko pojavijo sistemski učinki, še posebno če so bili predpisani veliki odmerki za dlje časa. Med<br />
možnimi sistemskimi učinki so Cushingov sindrom, supresija nadledvične žleze, zastoj rasti pri otrocih in mladostnikih, zmanjšanje<br />
mineralne gostote kosti, katarakta in glavkom. Priporočljivo je redno spremljanje višine otrok, ki se dalj časa zdravijo z<br />
inhalacijskimi glukokortikoidi. Da bi čim bolj zmanjšali tveganje orofaringealne kandidoze, je treba bolniku naročiti, da si mora po<br />
inhaliranju vzdrževalnega odmerka usta sprati z vodo. Zdravilo Symbicort predpisujte previdno pri bolnikih s hudimi<br />
kardiovaskularnimi boleznimi, tirotoksikozo, feokromocitomom, sladkorno boleznijo, nezdravljeno hipokaliemijo. Za ostala<br />
posebna opozorila in previdnostne ukrepe glejte celoten povzetek.<br />
INTERAKCIJE: Zaviralci receptorjev beta (vključno s kapljicami za oko) lahko oslabijo ali zavrejo delovanje formoterola. Sočasna<br />
uporaba močnih zaviralcev CYP P450 3A4 lahko poveča plazemski nivo budezonida. Za ostale interakcije glejte celoten povzetek.<br />
NOSEČNOST IN DOJENJE: V času nosečnosti se sme zdravilo Symbicort predpisovati le, če koristi zdravila presegajo morebitna<br />
tveganja. Zdravilo Symbicort se sme doječi ženski predpisati le, če pričakovana korist za mater presega morebitno tveganje za<br />
otroka.<br />
GLAVNI NEŽELENI UČINKI: Pogosti: palpitacije, glavobol, tremor, okužbe s kandido v ustnem delu žrela, blago draženje žrela,<br />
kašelj, hripavost. Občasni: tahikardija, navzeja, mišični krči, omotičnost, agitacija, nemir, razdražljivost, motnje spanja, modrice.<br />
Redki: atrijska fibrilacija, supraventrikularna tahikardija, ekstrasistole, eksantem, urtikarija, pruritus, dermatitis, angioedem,<br />
anafilaktična reakcija, hipokaliemija, bronhospazem.<br />
REŽIM IZDAJE ZDRAVILA: Zdravilo se izdaja le na recept.<br />
IMETNIK DOVOLJENJA ZA PROMET: AstraZeneca AB, Kvarnbergagatan 12, SE-151 85 Södertälje, Švedska<br />
DATUM PRIPRAVE INFORMACIJE: avgust 2010<br />
Pred predpisovanjem, prosimo, preberite celoten povzetek glavnih značilnosti zdravila.<br />
Dodatne informacije so na voljo pri družbi AstraZeneca UK Limited, Podružnica v Sloveniji, Verovškova 55, Ljubljana.<br />
1. Welte T et al. Am J Respir Crit Care Med 2009; 180: 741-750
320 µg/9 µg/odmerek
SKRAJŠAN POVZETEK GLAVNIH ZNAČILNOSTI ZDRAVIL<br />
SYM 07/11 P<br />
Symbicort Turbuhaler 80 mikrogramov/4,5 mikrograma na odmerek prašek za inhaliranje<br />
Symbicort Turbuhaler 160 mikrogramov/4,5 mikrograma na odmerek prašek za inhaliranje<br />
Symbicort Turbuhaler 320 mikrogramov/9 mikrogramov na odmerek prašek za inhaliranje<br />
SESTAVA: Vsak inhalator Symbicort Turbuhaler 80 µg/4,5 µg na odmerek vsebuje 120 odmerkov. Vsak oddani odmerek (tisti, ki pride<br />
iz ustnika) vsebuje naslednji učinkovini: budezonid, in sicer 80 µg na vdih, in formoterolijev fumarat dihidrat, 4,5 µg na vdih. Vsak<br />
inhalator Symbicort Turbuhaler 160 µg/4,5 µg na odmerek vsebuje 120 odmerkov. Vsak oddani odmerek vsebuje naslednji učinkovini:<br />
budezonid, in sicer 160 µg na vdih, in formoterolijev fumarat dihidrat, 4,5 µg na vdih. Vsak inhalator Symbicort Turbuhaler 320 µg/9 µg<br />
na odmerek vsebuje 60 odmerkov. Vsak oddani odmerek vsebuje naslednji učinkovini: budezonid, in sicer 320 µg na vdih, in<br />
olijev fumarat dihidrat, 9 µg na vdih.<br />
INDIKACIJE: Zdravilo Symbicort Turbuhaler 80 µg/4,5 µg na odmerek je indicirano za redno zdravljenje astme, ko je primeren način<br />
zdravljenja kombinacija zdravil (inhalacijski glukokortikoid in dolgodelujoči agonist receptorjev beta2). Zdravilo Symbicort Turbuhaler<br />
80 µg/4,5 µg na odmerek ni primerno za bolnike s hudim astmatičnim obolenjem. Zdravili Symbicort Turbuhaler 160 µg/4,5 µg na<br />
odmerek in 320 µg/9 µg na odmerek sta indicirani za redno zdravljenje astme, ko je primeren način zdravljenja kombinacija zdravil<br />
(inhalacijski glukokortikoid in dolgodelujoči agonist receptorjev beta2), in simptomatsko zdravljenje bolnikov s hudo obliko KOPB<br />
(FEV1 < 50 % predvidenega normalnega FEV1) ob ponavljajočih se poslabšanjih v anamnezi, ko se kljub zdravljenju z dolgodelujočimi<br />
bronhodilatatorji pojavljajo značilni simptomi.<br />
ODMERJANJE IN NAČIN UPORABE: Inhalator Symbicort Turbuhaler se aktivira pri vdihu, kar pomeni, da ob bolnikovem vdihu skozi<br />
ustnik vdihan zrak s sabo potegne učinkovini v dihalne poti. Zaradi majhne količine zdravila v posameznem vdihu bolnik pri uporabi<br />
inhalatorja Turbuhaler morda sploh ne bo okusil ali začutil zdravila.<br />
ASTMA: Odmerjanje je individualno. Vzdrževalno zdravljenje (vse jakosti): bolnikom je potrebno svetovati, da imajo hitrodelujoči<br />
bronhodilatator vedno na razpolago. Odrasli (18 let ali več): Symbicort Turbuhaler 80 µg/4,5 µg na odmerek in 160 µg/4,5 µg na<br />
odmerek: 1–2 vdiha dvakrat na dan. Pri nekaterih bolnikih bodo potrebni tudi do največ 4 vdihi dvakrat na dan. Symbicort Turbuhaler<br />
320 µg/9 µg na odmerek: 1 vdih dvakrat na dan. Pri nekaterih bolnikih bosta potrebna tudi do največ 2 vdiha dvakrat na dan. Mladostniki<br />
(12–17 let): 1–2 vdiha dvakrat na dan oz. 1 vdih dvakrat na dan (Symbicort Turbuhaler 320 µg/9 µg na odmerek). Otroci (6 let ali več):<br />
2 vdiha dvakrat na dan (samo Symbicort Turbuhaler 80 µg/4,5 µg na odmerek). Zdravila Symbicort ne priporočamo pri otrocih, mlajših<br />
od 6 let. Vzdrževalno in olajševalno zdravljenje (Symbicort Turbuhaler 80 µg/4,5 µg na odmerek in Symbicort Turbuhaler 160 µg/4,5 µg<br />
na odmerek): bolniki redno jemljejo dnevni vzdrževalni odmerek zdravila Symbicort, ob pojavu simptomov pa po potrebi dodatne<br />
odmerke zdravila. Bolnikom je potrebno svetovati, da imajo zdravilo Symbicort kot olajševalec vedno pri sebi. Priporočeni odmerki:<br />
odrasli (18 let in več): priporočen vzdrževalni odmerek je 2 vdiha na dan, bodisi 1 vdih zjutraj in 1 vdih zvečer bodisi 2 vdiha zjutraj<br />
oziroma 2 vdiha zvečer. Za nekatere bolnike je primerno odmerjanje 2 vdiha dvakrat dnevno (Symbicort Turbuhaler 160 µg/4,5 µg na<br />
odmerek). Ob pojavu simptomov se po potrebi naredi še 1 dodaten vdih. Če so simptomi po nekaj minutah še vedno prisotni, se doda<br />
še 1 vdih. Naenkrat ni dovoljeno narediti več kot 6 vdihov. Celotni dnevni odmerek, večji od 8 vdihov, v normalnih okoliščinah ni<br />
potreben. Kljub temu je lahko v določenih omejenih časovnih obdobjih celotni dnevni odmerek 12 vdihov.<br />
KOPB: Priporočeni odmerki za odrasle: Symbicort Turbuhaler 160 µg/4,5 µg na odmerek 2 vdiha dvakrat na dan in Symbicort Turbuhaler<br />
320 µg/9 µg na odmerek 1 vdih dvakrat na dan.<br />
KONTRAINDIKACIJE: Preobčutljivost za budezonid, formoterol ali inhalirano laktozo.<br />
POSEBNA OPOZORILA IN PREVIDNOSTNI UKREPI: Priporočamo, da ob prekinitvi zdravljenja odmerek zmanjšujete postopoma in<br />
zdravljenja ne prekinete nenadoma. Če bolnik ugotavlja, da je zdravljenje neučinkovito ali če preseže največji priporočeni odmerek<br />
zdravila Symbicort, mora poiskati zdravniško pomoč. Bolnikom svetujte, naj imajo inhalator kot olajševalec vedno pri sebi, ali Symbicort<br />
(za bolnike, ki uporabljajo Symbicort za vzdrževalno in olajševalno zdravljenje) ali samostojni hitrodelujoči bronhodilatator (za bolnike,<br />
ki uporabljajo Symbicort le za vzdrževalno zdravljenje). Symbicort kot olajševalec se uporablja v primerih, ko se pojavijo simptomi, ne<br />
pa redno v profilakticne namene. Pri uporabi vseh inhalacijskih glukokortikoidov se lahko pojavijo sistemski učinki, še posebno če so<br />
bili predpisani veliki odmerki za dlje časa, vendar pa so sistemski učinki veliko manj verjetni pri inhalacijskem zdravljenju kakor pri<br />
uporabi peroralnih glukokortikoidov. Med možnimi sistemskimi učinki so na primer supresija nadledvične žleze, zastoj rasti pri otrocih<br />
in mladostnikih, zmanjšanje kostne mineralne gostote, katarakta in glavkom. Priporočljivo je redno spremljanje višine otrok, ki se dalj<br />
časa zdravijo z inhalacijskimi glukokortikoidi. Zdravilo Symbicort predpisujte previdno pri bolnikih s hudimi kardiovaskularnimi<br />
boleznimi, tirotoksikozo, feokromocitomom, sladkorno boleznijo, nezdravljeno hipokaliemijo. Za ostala posebna opozorila in<br />
previdnostne ukrepe glejte celoten povzetek.<br />
INTERAKCIJE: Zaviralci receptorjev beta (vključno s kapljicami za oko) lahko oslabijo ali zavrejo delovanje formoterola. Sočasna<br />
uporaba močnih zaviralcev CYP P450 3A4 lahko poveča plazemski nivo budezonida. Za ostale interakcije glejte celoten povzetek.<br />
NOSEČNOST IN DOJENJE: V času nosečnosti se sme zdravilo Symbicort predpisovati le, če koristi zdravila presegajo morebitna<br />
tveganja. Zdravilo Symbicort se sme doječi ženski predpisati le, če pričakovana korist za mater presega vsakršno morebitno tveganje<br />
za otroka.<br />
GLAVNI NEŽELENI UČINKI: Pogosti: palpitacije, glavobol, tremor, okužbe s kandido v ustnem delu žrela, blago draženje grla, kašljanje,<br />
hripavost. Občasni: tahikardija, navzeja, mišični krči, omotičnost, agitacija, nemir, razdražljivost, motnje spanja, modrice. Redki: atrijska<br />
fibrilacija, supraventrikularna tahikardija, ekstrasistole, eksantem, urtikarija, pruritus, dermatitis, angioedem, anafilaktična reakcija,<br />
hipokaliemija, bronhospazem. Zelo redki: angina pektoris, znaki ali simptomi sistemskih učinkov glukokortikoidov, hiperglikemija,<br />
motnje okusa, depresija, vedenjske motnje, spremembe krvnega tlaka.<br />
REŽIM IZDAJE ZDRAVILA: Zdravilo se izdaja le na recept.<br />
IMETNIK DOVOLJENJA ZA PROMET: AstraZeneca UK Limited 15 Stanhope Gate, London, W1K 1LN, Velika Britanija<br />
Pred predpisovanjem, prosimo, preberite celoten povzetek glavnih značilnosti zdravila.<br />
Dodatne informacije so na voljo pri družbi AstraZeneca UK Limited, Podružnica v Sloveniji, Verovškova 55, Ljubljana.<br />
DATUM PRIPRAVE INFORMACIJE: junij 2010<br />
SAMO ZA STROKOVNO JAVNOST<br />
1. Welte T et al. Am J Respir Crit Care Med 2009; 180: 741-750
SAMO ZA STROKOVNO JAVNOST.
SKRAJŠAN POVZETEK GLAVNIH ZNAČILNOSTI<br />
ZDRAVILA<br />
IME ZDRAVILA<br />
SERETIDE DISKUS 50 mikrogramov/100 mikrogramov/odmerek<br />
prašek za inhaliranje, odmerjeni<br />
SERETIDE DISKUS 50 mikrogramov/250 mikrogramov/odmerek<br />
prašek za inhaliranje, odmerjeni<br />
SERETIDE DISKUS 50 mikrogramov/500 mikrogramov/odmerek<br />
prašek za inhaliranje, odmerjeni<br />
KAKOVOSTNA IN KOLIČINSKA SESTAVA<br />
SERETIDE DISKUS 50 mikrogramov/100 mikrogramov/odmerek<br />
prašek za inhaliranje, odmerjeni<br />
En odmerek (en vdih) vsebuje 50 mikrogramov<br />
salmeterola (v obliki 72,5 mikrogramov salmeterolijevega<br />
ksinafoata) in 100 mikrogramov flutikazonpropionata.<br />
SERETIDE DISKUS 50 mikrogramov/250 mikrogramov/odmerek<br />
prašek za inhaliranje, odmerjeni<br />
En odmerek (en vdih) vsebuje 50 mikrogramov<br />
salmeterola (v obliki 72,5 mikrogramov salmeterolijevega<br />
ksinafoata) in 250 mikrogramov flutikazonpropionata.<br />
SERETIDE DISKUS 50 mikrogramov/500 mikrogramov/odmerek<br />
prašek za inhaliranje, odmerjeni<br />
En odmerek (en vdih) vsebuje 50 mikrogramov<br />
salmeterola (v obliki 72,5 mikrogramov salmeterolijevega<br />
ksinafoata) in 500 mikrogramov flutikazonpropionata.<br />
Pomožne snovi:<br />
Laktoza monohidrat<br />
En odmerek zdravila SERETIDE DISKUS (ne glede na<br />
jakost) vsebuje največ do 11,8 mg laktoze.<br />
KLINIČNI PODATKI<br />
Terapevtske indikacije<br />
ASTMA<br />
Če je uporaba kombiniranega zdravila (kombinacije<br />
dolgodelujočega agonista adrenergičnih receptorjev<br />
beta-2 in inhalacijskega kortikosteroida) primerna,<br />
je zdravilo SERETIDE DISKUS indicirano za redno<br />
zdravljenje astme pri:<br />
- bolnikih, katerih simptomi astme z uporabo inhalacijskega<br />
kortikosteroida in občasno uporabo<br />
(po potrebi) kratkodelujočega inhalacijskega<br />
agonista adrenergičnih receptorjev beta-2 niso<br />
zadostno nadzorovani,<br />
ali<br />
- bolnikih, katerih simptomi astme so že zadostno<br />
nadzorovani z uporabo obeh, inhalacijskega<br />
kortikosteroida in dolgodelujočega agonista<br />
adrenergičnih receptorjev beta-2.<br />
KRONIČNA OBSTRUKTIVNA PLJUČNA BOLE-<br />
ZEN (KOPB)<br />
Zdravilo SERETIDE DISKUS je indicirano za simptomatsko<br />
zdravljenje bolnikov s KOPB (forsirani<br />
ekspiracijski volumen v 1. sekundi; FEV1 < 60 %<br />
pričakovane normalne (pre-bronhodilatorne) vrednosti)<br />
in anamnezo ponavljajočih se poslabšanj, ki<br />
imajo signifikantne simptome bolezni kljub rednemu<br />
zdravljenju z bronhodilatatorjem.<br />
Odmerjanje in način uporabe<br />
Zdravilo SERETIDE DISKUS je namenjeno izključno<br />
za inhaliranje.<br />
Bolnikom je treba pojasniti, da bo optimalna korist<br />
zdravila SERETIDE DISKUS dosežena le, če ga bodo<br />
uporabljali vsakodnevno, tudi takrat, ko nimajo simptomov<br />
bolezni.<br />
Bolniki morajo biti pod rednim zdravniškim nadzorom,<br />
da bi tako jakost zdravila SERETIDE DISKUS, ki<br />
ga uporabljajo, ostala optimalna ves čas zdravljenja.<br />
Jakost zdravila SERETIDE DISKUS lahko spremeni le<br />
zdravnik. Odmerek je treba postopno zmanjševati<br />
do najmanjšega odmerka, ki še zagotavlja<br />
učinkovito nadzorovanost simptomov bolezni.<br />
Če se nadzorovanost simptomov vzdržuje z<br />
uporabo najmanjše jakosti kombinacije dvakrat<br />
na dan, se lahko v naslednji fazi zdravljenja<br />
poskusi z uporabo inhalacijskega kortikosteroida<br />
samega. Bolnikom, ki potrebujejo zdravljenje z<br />
dolgodelujočim agonistom adrenergičnih receptorjev<br />
beta-2 se alternativno lahko predpiše uporaba zdravila<br />
SERETIDE DISKUS enkrat na dan, če zdravnik<br />
meni, da bo s takšno uporabo nadzorovanost bolezni<br />
ostala zadovoljiva. V primeru uporabe zdravila enkrat<br />
na dan mora bolnik, ki ima simptome predvsem ponoči,<br />
uporabiti odmerek zdravila zvečer, bolnik, ki pa<br />
ima simptome predvsem podnevi, pa mora odmerek<br />
zdravila uporabiti zjutraj.<br />
Bolnikom je treba predpisati jakost zdravila SERETI-<br />
DE DISKUS, ki vsebuje odmerek flutikazonpropionata,<br />
primeren resnosti bolezni. Zdravniki morajo upoštevati,<br />
da je pri bolnikih z astmo flutikazonpropionat<br />
tako učinkovit kot drugi inhalacijski kortikosteroidi<br />
že v približno polovičnem mikrogramskem dnevnem<br />
odmerku. Na primer, odmerek 100 mikrogramov<br />
flutikazonpropionata je približno enakovreden odmerku<br />
200 mikrogramov beklometazondipropionata<br />
(z vsebnostjo CFC) ali budezonida. Če posamezen<br />
bolnik potrebuje zdravljenje z odmerkom, ki je<br />
izven priporočenega režima odmerjanja, mu je treba<br />
predpisati primeren odmerek agonista adrenergičnih<br />
receptorjev beta in/ali kortikosteroida.<br />
Priporočeni odmerki<br />
ASTMA<br />
• Odrasli in mladostniki, stari 12 let in starejši<br />
- En odmerek (en vdih) 50 mikrogramov salmeterola<br />
in 100 mikrogramov flutikazonpropionata<br />
dvakrat na dan,<br />
ali<br />
- en odmerek (en vdih) 50 mikrogramov salmeterola<br />
in 250 mikrogramov flutikazonpropionata<br />
dvakrat na dan,<br />
ali<br />
- en odmerek (en vdih) 50 mikrogramov salmeterola<br />
in 500 mikrogramov flutikazonpropionata<br />
dvakrat na dan.<br />
Pri odraslih ali mladostnikih z zmerno persistentno<br />
astmo (bolniki z vsakodnevnimi simptomi, vsakodnevno<br />
uporabo olajševalca in zmernim do hudim<br />
zmanjšanjem pretoka zraka), pri katerih je nujno<br />
treba doseči hitro nadzorovanost astme, se lahko<br />
razmisli o kratkotrajni poskusni uporabi zdravila<br />
SERETIDE DISKUS kot začetnega vzdrževalnega<br />
zdravljenja. V takšnih primerih je priporočeni začetni<br />
odmerek ena inhalacija 50 mikrogramov salmeterola<br />
in 100 mikrogramov flutikazonpropionata dvakrat<br />
na dan. Ko je dosežena nadzorovanost astme, je<br />
treba zdravljenje ponovno ovrednotiti in presoditi<br />
o primernosti zmanjšanja odmerka in zdravljenju z<br />
inhalacijskim kortikosteroidom samim. Bolniki, pri<br />
katerih se odmerek zmanjša ali uvede zdravljenje z<br />
inhalacijskim kortikosteroidom samim, morajo biti<br />
pod rednim zdravniškim nadzorom.<br />
V primeru odsotnosti enega ali dveh kriterijev za<br />
opredelitev nadzora bolezni očitna korist pri začetnem<br />
vzdrževalnem zdravljenju, v primerjavi z uporabo<br />
inhalacijskega flutikazonpropionata samega,<br />
ni bila dokazana. Pri večini bolnikov inhalacijski<br />
kortikosteroidi na splošno ostajajo zdravila prvega<br />
izbora. Zdravilo SERETIDE DISKUS ni namenjeno<br />
začetnemu zdravljenju blage astme. Jakost zdravila<br />
SERETIDE DISKUS 50/100 mikrogramov ni primerna<br />
za odrasle in otroke s hudo astmo. Pri bolnikih s hudo<br />
astmo je pred uvedbo katerekoli fiksne kombinacije<br />
priporočljivo določiti ustrezni odmerek inhalacijskega<br />
kortikosteroida.<br />
• Otroci, stari od 4 do 11 let<br />
- En odmerek (en vdih) 50 mikrogramov salmeterola<br />
in 100 mikrogramov flutikazonpropionata<br />
dvakrat na dan.<br />
Največji dovoljeni odmerek flutikazonpropionata, ki<br />
ga lahko prejmejo otroci z zdravilom SERETIDE DIS-<br />
KUS je 100 mikrogramov dvakrat na dan.<br />
• Otroci, mlajši od 4 let<br />
Podatki o uporabi zdravila SERETIDE DISKUS pri otrocih,<br />
mlajših od 4 let, niso na voljo.<br />
KOPB<br />
• Odrasli<br />
- En odmerek (en vdih) 50 mikrogramov salmeterola<br />
in 500 mikrogramov flutikazonpropionata<br />
dvakrat na dan.<br />
Posebne skupine bolnikov<br />
Pri starejših bolnikih in bolnikih z okvaro ledvic<br />
odmerka ni treba prilagajati. Podatki o uporabi<br />
zdravila SERETIDE DISKUS pri bolnikih z okvaro jeter<br />
niso na voljo.<br />
Uporaba zdravila SERETIDE DISKUS<br />
Bolnike je treba natančno poučiti o pravilni uporabi<br />
naprave DISKUS.<br />
Bolnik DISKUS najprej odpre in ga s premikom vzmeti<br />
pripravi za uporabo. Ustnik nato vstavi med ustnici.<br />
Med inhalacijo se iz naprave DISKUS sprosti prašek,<br />
ki ga bolnik skozi usta vdihne v pljuča. Po uporabi<br />
mora bolnik DISKUS ustrezno zapreti. Števec odmerkov<br />
na napravi DISKUS kaže število preostalih<br />
odmerkov.<br />
Kontraindikacije<br />
Preobčutljivost za zdravilni učinkovini ali katerokoli<br />
pomožno snov.<br />
Posebna opozorila in previdnostni ukrepi<br />
Običajno mora zdravljenje astme potekati po stopenjskem<br />
programu. Bolnikov odziv je treba nadzirati<br />
tako klinično kot s testi pljučne funkcije.<br />
Zdravila SERETIDE DISKUS se ne sme uporabljati<br />
za zdravljenje akutnih simptomov astme. V takšnih<br />
primerih morajo bolniki uporabiti kratkodelujoči<br />
bronhodilatator s hitrim začetkom delovanja. Bolnike<br />
je treba poučiti, da morajo imeti svoj medicinski pripomoček<br />
za lajšanje akutnih astmatičnih napadov<br />
(akutnih poslabšanj astme) vedno na razpolago.<br />
Zdravljenja z zdravilom SERETIDE DISKUS se ne sme<br />
uvesti med akutnim poslabšanjem astme oziroma če<br />
bolezen pomembno in hitro napreduje.<br />
Med zdravljenjem z zdravilom SERETIDE DISKUS<br />
se lahko pojavijo resni neželeni učinki, povezani z<br />
astmo, in poslabšanja astme. Bolnikom je treba pojasniti,<br />
da naj v takšnih primerih nadaljujejo z uporabo<br />
zdravila, vendar pa naj poiščejo zdravniško pomoč, če<br />
simptomi astme ostanejo nenadzorovani ali se po začetku<br />
uporabe zdravila SERETIDE DISKUS poslabšajo.<br />
Pogostejša uporaba kratkodelujočih bronhodilatatorjev<br />
za lajšanje simptomov kaže na slabšo nadzorovanost<br />
bolezni. Takšni bolniki potrebujejo ustrezno<br />
zdravniško obravnavo.<br />
Nenadno in progresivno poslabšanje nadzorovanosti<br />
astme je lahko smrtno nevarno. Takšni bolniki potrebujejo<br />
urgentno zdravniško oskrbo. Morda bo potrebno<br />
zdravljenje z večjim odmerkom kortikosteroida.<br />
Bolnik potrebuje zdravniški pregled tudi, če trenutni<br />
odmerek zdravila SERETIDE DISKUS ne zagotavlja zadostne<br />
nadzorovanosti astme. Pri bolnikih z astmo ali<br />
KOPB bo morda potrebno uvesti dodatno zdravljenje<br />
s kortikosteroidi.<br />
Ko je dosežena nadzorovanost simptomov astme je<br />
treba presoditi o primernosti postopnega zmanjšanja<br />
odmerka zdravila SERETIDE DISKUS. Pomembno je,<br />
da so bolniki po zmanjšanju odmerka pod rednim<br />
zdravniškim nadzorom. Uporablja naj se najnižji še<br />
učinkoviti odmerek zdravila SERETIDE DISKUS.<br />
Pri bolnikih z astmo se zaradi nevarnosti poslabšanj<br />
zdravljenje z zdravilom SERETIDE DISKUS ne<br />
sme prekiniti nenadoma. Odmerek zdravila je treba<br />
zmanjševati postopoma, pod zdravniškim nadzorom.<br />
Tudi pri bolnikih s KOPB je opustitev zdravljenja lahko<br />
povezana s simptomatsko dekompenzacijo in mora<br />
zato potekati pod zdravniškim nadzorom.<br />
Tako kot vsa inhalacijska zdravila, ki vsebujejo kortikosteroide,<br />
je treba tudi zdravilo SERETIDE DISKUS<br />
uporabljati previdno pri bolnikih, ki imajo pljučno<br />
tuberkulozo.<br />
Zdravilo SERETIDE DISKUS lahko pri visokih terapevtskih<br />
odmerkih v redkih primerih povzroči aritmije,<br />
npr. supraventrikularno tahikardijo, ekstrasistole in<br />
atrijsko fibrilacijo ter blago prehodno zmanjšanje<br />
serumskega kalija. Zdravilo SERETIDE DISKUS je<br />
treba zato uporabljati previdno pri bolnikih, ki imajo<br />
hujšo kardiovaskularno bolezen, vključno z motnjami<br />
srčnega ritma, sladkorno bolezen, hipertiroidizem<br />
(tirotoksikozo), nezdravljeno hipokaliemijo ali predispozicijo<br />
za nizke vrednosti serumskega kalija.<br />
Zelo redko so poročali o povečanih vrednostih glukoze<br />
v krvi, kar je treba upoštevati pri predpisovanju<br />
zdravila bolnikom, ki imajo v anamnezi sladkorno<br />
bolezen.<br />
Tako kot pri zdravljenju z drugimi inhalacijskimi<br />
zdravili se lahko tudi pri zdravljenju z zdravilom SE-<br />
RETIDE DISKUS pojavi paradoksni bronhospazem, ki<br />
se kaže s pojavom piskajočega dihanja takoj po uporabi<br />
odmerka. Uporabo zdravila SERETIDE DISKUS je<br />
treba nemudoma opustiti, opraviti ponoven pregled<br />
bolnika in po potrebi uvesti alternativno zdravljenje.<br />
Pri prehodu na zdravljenje z zdravilom SERETIDE DI-<br />
SKUS je potrebna previdnost, še posebej pri bolnikih,<br />
pri katerih obstaja kakršenkoli sum na oslabljeno<br />
delovanje nadledvične žleze zaradi predhodnega<br />
zdravljenja s sistemskimi kortikosteroidi.<br />
Sistemski učinki se lahko pojavijo pri zdravljenju s<br />
katerimkoli inhalacijskim kortikosteroidom, še posebej<br />
v primeru velikih odmerkov, predpisanih za daljše<br />
obdobje. Verjetnost pojava sistemskih učinkov pa je<br />
vendarle veliko manjša kot pri zdravljenju s peroralnimi<br />
kortikosteroidi. Možni sistemski učinki vključujejo<br />
Cushingov sindrom in z njim povezane značilnosti,<br />
supresijo nadledvične žleze, zastoj rasti pri otrocih in<br />
mladostnikih, zmanjšanje kostne gostote, katarakto<br />
in glavkom. Pomembno je torej, da so bolniki pod<br />
rednim zdravniškim nadzorom, in da se odmerek<br />
inhalacijskega kortikosteroida zmanjša do<br />
najmanjšega odmerka, ki še zagotavlja učinkovito<br />
nadzorovanost bolezni.<br />
Pri otrocih, ki se dolgotrajno zdravijo z inhalacijskim<br />
kortikosteroidom, je priporočljivo opravljati redne<br />
meritve telesne višine.<br />
Dolgotrajno zdravljenje bolnikov z visokimi odmerki<br />
inhalacijskih kortikosteroidov lahko posledično povzroči<br />
supresijo nadledvične žleze in akutno adrenalno<br />
krizo. Še posebno tveganje lahko obstaja pri otrocih<br />
in mladostnikih, mlajših od 16 let, ki se zdravijo z<br />
visokimi odmerki flutikazonpropionata (običajno<br />
≥ 1.000 mikrogramov/dan). Zelo redko so poročali<br />
tudi o primerih pojava supresije nadledvične žleze in<br />
akutne adrenalne krize pri bolnikih, ki so se zdravili<br />
s flutikazonpropionatom v odmerkih od 500 do <<br />
1.000 mikrogramov. Okoliščine, v katerih lahko pride<br />
do pojava akutne adrenalne krize, vključujejo travmo,<br />
kirurški poseg, okužbo ali kakršnokoli nenadno<br />
zmanjšanje odmerka. Simptomi so običajno nejasni<br />
in lahko vključujejo anoreksijo, abdominalno bolečino,<br />
hujšanje, utrujenost, glavobol, navzeo, bruhanje,<br />
hipotenzijo, zmanjšano stopnjo zavesti, hipoglikemijo<br />
in epileptične napade. Med obdobjem stresa ali načrtovanega<br />
kirurškega posega bo morda potrebno<br />
dodatno zdravljenje s sistemskimi kortikosteroidi.<br />
Zaradi koristi zdravljenja z inhalacijskim flutikazonpropionatom<br />
se zmanjša potreba po zdravljenju<br />
s peroralnimi kortikosteroidi. Pri bolnikih, ki so se<br />
predhodno zdravili s peroralnimi kortikosteroidi, pa<br />
lahko tveganje za okvarjeno adrenalno rezervo traja<br />
še znaten čas. Tveganje obstaja tudi pri bolnikih, ki so<br />
v preteklosti nujno potrebovali zdravljenje z visokimi<br />
odmerki kortikosteroidov. Takšno možnost rezidualne<br />
okvare je potrebno vedno upoštevati pri urgentnih<br />
in načrtovanih okoliščinah, ki lahko izzovejo stres.<br />
Morda bo potrebno ustrezno kortikosteroidno zdravljenje.<br />
Pred načrtovanimi posegi bo o obsegu okvare<br />
nadledvične žleze morda potrebno pridobiti mnenje<br />
ustreznega specialista.<br />
Ritonavir lahko znatneje poveča koncentracijo flutikazonpropionata<br />
v plazmi. Sočasni uporabi se je torej<br />
potrebno izogibati, razen v primerih, ko morebitna<br />
korist za bolnika prevlada nad tveganjem za pojav<br />
sistemskih kortikosteroidnih neželenih učinkov. Večje<br />
tveganje za pojav sistemskih neželenih učinkov obstaja<br />
tudi pri uporabi flutikazonpropionata v kombinaciji<br />
z drugimi močnimi zaviralci CYP3A4.<br />
V študiji TORCH pri bolnikih s KOPB, ki so prejemali<br />
zdravilo SERETIDE DISKUS 50/500 mikrogramov<br />
dvakrat na dan v primerjavi s placebom, v študijah<br />
SCO40043 in SCO100250 pa pri bolnikih, ki so<br />
prejemali nižji odmerek zdravila SERETIDE DISKUS<br />
50/250 mikrogramov dvakrat na dan v primerjavi<br />
s 50 mikrogramov salmeterola dvakrat na dan, so<br />
pogosteje poročali o infekcijah spodnjih dihal (še<br />
zlasti o pljučnici in bronhitisu). (glejte poglavji 4.8 in<br />
5.1). Podobno incidenco pljučnice so opazili pri vseh<br />
študijah v skupini, ki je prejemala zdravilo SERETIDE<br />
DISKUS. V študiji TORCH so pri starejših bolnikih, pri<br />
bolnikih z nižjim indeksom telesne mase (< 25 kg/m 2 )<br />
in pri bolnikih z zelo resno obliko bolezni (pričakovan<br />
FEV1 < 30 % ) opazili največje tveganje za pojav<br />
pljučnice ne glede na zdravljenje. Pri bolnikih s KOPB<br />
morajo biti zdravniki pozorni na možen pojav pljučnice<br />
in drugih infekcij spodnjih dihal, saj se klinični<br />
znaki takih infekcij in poslabšanja osnovne bolezni<br />
pogosto prekrivajo. V primeru, da je bolnik s hudo<br />
obliko KOPB prebolel pljučnico, je potrebno zdravljenje<br />
z zdravilom SERETIDE DISKUS ponovno oceniti.<br />
Podatki iz obsežnega kliničnega preskušanja (SMART;<br />
“The Salmeterol Multi-Center Asthma Research Trial”)<br />
kažejo, da pri bolnikih afroameriškega porekla<br />
obstaja večje tveganje za pojav resnih respiratornih<br />
dogodkov ali smrtnih izidov pri uporabi salmeterola<br />
v primerjavi s placebom (glejte poglavje 5.1). Povezava<br />
s farmakogenetskimi ali drugimi dejavniki ni<br />
znana. Bolnikom črnega afriškega ali afrokaribskega<br />
izvora je treba pojasniti, da naj nadaljujejo z uporabo<br />
zdravila, vendar pa naj poiščejo zdravniško pomoč,<br />
če simptomi astme ostanejo nenadzorovani ali se<br />
med uporabo zdravila SERETIDE DISKUS poslabšajo.<br />
Sočasna uporaba sistemskega ketokonazola bistveno<br />
poveča sistemsko izpostavljenost salmeterolu.<br />
To lahko poveča incidenco sistemskih učinkov (npr.<br />
podaljšanja intervala QTc in palpitacij). Sočasnemu<br />
zdravljenju s ketokonazolom ali drugimi močnimi<br />
zaviralci CYP3A4 se je zato treba izogibati, razen če<br />
koristi odtehtajo možno povečano tveganje sistemskih<br />
neželenih učinkov zdravljenja s salmeterolom.<br />
Zdravilo SERETIDE DISKUS vsebuje laktozo (do 11,8<br />
miligramov/odmerek). Pri osebah, intolerantnih za<br />
laktozo, takšna količina običajno ne povzroča težav.<br />
Bolniki z redko dedno intoleranco za galaktozo,<br />
laponsko obliko zmanjšane aktivnosti laktaze ali<br />
malabsorpcijo glukoze/galaktoze ne smejo jemati<br />
tega zdravila.<br />
Medsebojno delovanje z drugimi zdravili in<br />
druge oblike interakcij<br />
Izogibati se je treba uporabi tako neselektivnih kot<br />
selektivnih antagonistov adrenergičnih receptorjev<br />
beta, razen v primerih, ko je njihova uporaba utemeljena<br />
in nujno potrebna.<br />
Sočasna uporaba drugih zdravil z beta adrenergičnim<br />
delovanjem ima lahko aditiven učinek.<br />
Flutikazonpropionat<br />
V običajnih okoliščinah so po inhalacijskem odmerjanju<br />
dosežene zelo nizke koncentracije flutikazonpropionata<br />
v plazmi, kar je posledica znatne presnove<br />
prvega prehoda in visokega sistemskega očistka s<br />
citokromom P450 3A4 v črevesju in jetrih. Klinično<br />
pomembne interakcije s flutikazonpropionatom so<br />
zato malo verjetne.<br />
Pri zdravih osebah, ki so v študiji medsebojnega<br />
delovanja z drugimi zdravili prejemale flutikazonpropionat<br />
intranazalno, so ugotovili, da so se zaradi<br />
ritonavirja (zelo močan zaviralec citokroma P450<br />
3A4) v odmerku 100 mg dvakrat na dan plazemske<br />
koncentracije flutikazonpropionata povečale<br />
za več stokrat, serumske koncentracije kortizola pa<br />
posledično znatno zmanjšale. Za inhalacijski flutikazonpropionat<br />
podatki sicer niso na voljo, vendar pa<br />
lahko pričakujemo znatno povečane vrednosti flutikazonpropionata<br />
v plazmi. Poročali so o primerih Cushingovega<br />
sindroma in supresije nadledvične žleze.<br />
Sočasni uporabi flutikazonpropionata in ritonavirja<br />
se je torej potrebno izogibati, razen v primerih, ko<br />
morebitna korist za bolnika prevlada nad povečanim<br />
tveganjem za pojav sistemskih glukokortikoidnih<br />
neželenih učinkov.<br />
Pri zdravih prostovoljcih, ki so bili vključeni v manjšo<br />
študijo, so ugotovili, da se je zaradi ketokonazola (nekoliko<br />
manj močan zaviralec CYP3A4 izpostavljenost<br />
flutikazonpropionatu po eni sami inhalaciji slednjega<br />
povečala za 150 %. To je imelo za posledico močnejše<br />
zmanjšanje kortizola v plazmi kot pa pri uporabi<br />
flutikazonpropionata samega. Pri sočasnem zdravljenju<br />
z drugimi močnimi zaviralci CYP3A4, kot je itrakonazol<br />
se tudi pričakuje, da se bosta sistemska izpostavljenost<br />
flutikazonpropionatu in tveganje za pojav<br />
sistemskih neželenih učinkov povečala. Priporočamo<br />
previdnost. Če je le možno, se je dolgotrajnemu zdravljenju<br />
s tovrstnimi zdravili potrebno izogibati.<br />
Salmeterol<br />
Močni zaviralci CYP3A4<br />
Sočasna 7-dnevna uporaba ketokonazola (400<br />
mg peroralno enkrat na dan) in salmeterola (50<br />
mikrogramov v inhalaciji dvakrat na dan) je pri 15<br />
zdravih preiskovancih bistveno povečala plazemsko<br />
izpostavljenost salmeterolu (1,4-kratno povečanje<br />
Cmax in 15-kratno povečanje AUC). To lahko poveča<br />
incidenco drugih sistemskih učinkov zdravljenja s salmeterolom<br />
(npr. podaljšanja intervala QTc in palpitacij)<br />
v primerjavi z zdravljenjem samo s salmeterolom<br />
ali samo s ketokonazolom.<br />
Klinično pomembnih učinkov na krvni tlak, srčno<br />
frekvenco in koncentracijo glukoze ali kalija v krvi ni<br />
bilo. Sočasna uporaba s ketokonazolom ni podaljšala<br />
eliminacijskega razpolovnega časa salmeterola in<br />
tudi ni povečala kopičenja salmeterola po večkratnem<br />
odmerjanju.<br />
Sočasni uporabi ketokonazola se je treba izogniti,<br />
razen če koristi odtehtajo možno večje tveganje<br />
sistemskih neželenih učinkov zdravljenja s salmeterolom.<br />
Verjetno obstaja podobno tveganje medsebojnega<br />
delovanja z drugimi močnimi zaviralci CYP3A4<br />
(npr. z itrakonazolom, telitromicinom, ritonavirjem).<br />
Zmerni zaviralci CYP3A4<br />
Sočasna 6-dnevna uporaba eritromicina (500 mg<br />
peroralno trikrat na dan) in salmeterola (50 mikrogramov<br />
v inhalaciji dvakrat na dan) je pri 15 zdravih<br />
preiskovancih malenkostno, statistično nepomembno<br />
povečala izpostavljenost salmeterolu (1,4-kratno<br />
povečanje Cmax in 1,2-kratno povečanje AUC). Med<br />
sočasno uporabo z eritromicinom ni bilo nobenih<br />
resnih neželenih učinkov.<br />
Nosečnost in dojenje<br />
Nosečnost<br />
O uporabi salmeterola in flutikazonpropionata pri<br />
nosečnicah in doječih materah je premalo podatkov,<br />
da bi lahko podali oceno o možnih škodljivih učinkih.<br />
Pri študijah na živalih so se po uporabi agonistov<br />
adrenergičnih receptorjev beta-2 in glukokortikosteroidov<br />
pojavile anomalije plodov.<br />
Zdravilo SERETIDE DISKUS se sme nosečnicam predpisati<br />
le, če pričakovana korist za mater prevlada nad<br />
kakršnimkoli možnim tveganjem za plod.<br />
Nosečnicam se sme predpisati le najmanjši še učinkovit<br />
odmerek flutikazonpropionata, ki še zagotavlja<br />
zadovoljivo nadzorovanost astme.<br />
Dojenje<br />
Podatkov o izločanju zdravila z materinim mlekom ni.<br />
Tako salmeterol kot flutikazonpropionat se izločata<br />
z mlekom pri doječih podganah. Zdravilo SERETIDE<br />
DISKUS se sme doječim materam predpisati le, če pričakovana<br />
korist za mater prevlada nad kakršnimkoli<br />
možnim tveganjem za dojenega otroka.<br />
Vpliv na sposobnost vožnje in upravljanja<br />
s stroji<br />
Študij o vplivu na sposobnost vožnje in upravljanja<br />
s stroji niso izvedli.<br />
Neželeni učinki<br />
Zdravilo SERETIDE DISKUS vsebuje salmeterol (v<br />
obliki salmeterolijevega ksinafoata) in flutikazonpropionat,<br />
zato lahko pričakujemo vrsto in resnost<br />
neželenih reakcij, ki so povezane z vsako posamezno<br />
učinkovino. Zaradi sočasne uporabe obeh zdravilnih<br />
učinkovin, se dodatni neželeni učinki niso pojavili.<br />
Neželeni učinki, ki so bili povezani z uporabo salmeterola/flutikazonpropionata<br />
so navedeni v nadaljevanju<br />
glede na organski sistem in pogostnost.<br />
Pogostnost je navedena kot: zelo pogosti (≥ 1/10),<br />
pogosti (≥ 1/100 do < 1/10), občasni (≥ 1/1.000<br />
do < 1/100), redki (≥ 1/10.000 do < 1/1.000), zelo<br />
redki (< 1/10.000) ter neznani (ni mogoče oceniti<br />
iz razpoložljivih podatkov). Podatki o zelo pogostih,<br />
pogostih in občasnih učinkih so bili pridobljeni s kliničnimi<br />
raziskavami, pri čemer pojavnost pri placebu<br />
ni upoštevana. Podatki o zelo redkih učinkih so bili<br />
pridobljeni s pomočjo spontanih poročil med spremljanjem<br />
zdravila po pridobitvi dovoljenja za promet.<br />
Zelo pogosti: glavobol 1 , nazofaringitis 2,3<br />
Pogosti: kandidoza ustne votline in žrela, pljučnica<br />
1,3 , bronhitis 1,3 , hipokalijemija 3 , tremor , palpitacije,<br />
draženje žrela, hripavost/disfonija, sinuzitis 1,3 , kontuzije<br />
1,3 , mišični krči, zlomi kosti zaradi poškodb 1,3<br />
Občasni: preobčutljivostne kožne reakcije, tahikardija<br />
Zelo redki: angioedem (predvsem edem obraza in<br />
orofaringealni edem), respiratorni simptomi (dispneja<br />
in/ali bronhospazem), anafilaksijske reakcije,<br />
vključno z anafilaktičnim šokom, Cushingov sindrom<br />
in z njim povezane značilnosti 4 , supresija nadledvične<br />
žleze 4 , zastoj rasti pri otrocih in mladostnikih 4 , zmanjšanje<br />
mineralne gostote kosti 4 , katarakta 4 , glavkom 4 ,<br />
hiperglikemija 4 , anksioznost, motnje spanja in<br />
vedenjske spremembe, vključno s hiperaktivnostjo<br />
ter razdražljivostjo (predvsem pri otrocih), aritmije<br />
(vključno z atrijsko fibrilacijo, supraventrikularno<br />
tahikardijo in ekstrasistolami), paradoksni bronhospazem<br />
4 , artralgija, mialgija.<br />
1. Pogosta poročila pri placebu, 2. Zelo pogosta poročila<br />
pri placebu, 3. Poročila v 3 letih v študiji pri bolnikih<br />
s KOPB, 4. Glejte poglavje: Posebna opozorila in<br />
previdnostni ukrepi<br />
Opis izbranih neželenih učinkov<br />
Poročali so o farmakoloških neželenih učinkih zdravljenja<br />
z agonisti adrenergičnih receptorjev beta-2,<br />
kot so tremor, palpitacije in glavobol. Običajno so<br />
bili prehodni in so se pri rednem zdravljenju ublažili.<br />
Zaradi flutikazonpropionata se lahko pri posameznih<br />
bolnikih pojavi hripavost in kandidoza (soor) ustne<br />
votline in žrela. Oboje, hripavost in pojavnost kandidoze<br />
se lahko ublaži z izpiranjem ustne votline z<br />
vodo po uporabi zdravila. Simptomatska kandidoza<br />
se lahko, ob sočasnem nadaljevanju zdravljenja z<br />
zdravilom SERETIDE DISKUS, zdravi s topikalnimi<br />
protiglivičnimi zdravili.<br />
Pediatrična populacija<br />
Možni sistemski učinki vključujejo Cushingov<br />
sindrom in z njim povezane značilnosti, supresijo<br />
nadledvične žleze in zastoj rasti pri otrocih in mladostnikih.<br />
Pri otrocih se lahko pojavijo anksioznost,<br />
motnje spanja in vedenjske spremembe vključno s<br />
hiperaktivnostjo ter razdražljivostjo.<br />
Preveliko odmerjanje<br />
Podatkov o primerih prevelikega odmerjanja zdravila<br />
SERETIDE DISKUS med kliničnimi preskušanji ni, vendar<br />
pa so v nadaljevanju podani podatki o prevelikem<br />
odmerjanju posamezne zdravilne učinkovine.<br />
Znaki in simptomi prevelikega odmerjanja salmeterola<br />
so tremor, glavobol in tahikardija. Prednostni<br />
antidot je kardioselektivni antagonist adrenergičnih<br />
receptorjev beta, ki pa ga je pri bolnikih z bronhospazmom<br />
v anamnezi potrebno uporabljati previdno.<br />
Če se mora zdravljenje z zdravilom SERETIDE DISKUS<br />
prekiniti zaradi prevelikega odmerjanja agonista<br />
adrenergičnih receptorjev beta, bo morda potrebno<br />
zagotoviti ustrezno nadomestno zdravljenje s kortikosteroidom.<br />
Lahko se pojavi tudi hipokaliemija, zato<br />
bo morda potrebno nadomeščanje kalija.<br />
Akutno: Akutna uporaba inhalacijskega flutikazonpropionata<br />
v odmerkih, ki so večji od priporočenih,<br />
lahko povzroči začasno supresijo nadledvične žleze.<br />
Nujni ukrepi zaradi tega običajno niso potrebni, saj<br />
se delovanje nadledvične žleze v nekaj dneh povrne,<br />
kar se lahko ugotovi z merjenjem koncentracije<br />
kortizola v plazmi.<br />
Za kronično preveliko odmerjanje inhalacijskega<br />
flutikazonpropionata glejte podatke o tveganju za<br />
supresijo nadledvične žleze v poglavju 4.4. Morda bo<br />
potreben nadzor adrenalne rezerve. V primeru prevelikega<br />
odmerjanja flutikazonpropionata se lahko<br />
zdravljenje z zdravilom SERETIDE DISKUS nadaljuje,<br />
in sicer z odmerki, ki zadoščajo za nadzorovanje<br />
simptomov.<br />
Inkompatibilnosti<br />
Navedba smiselno ni potrebna.<br />
Vrsta ovojnine in vsebina<br />
Škatla vsebuje napravo iz lite plastike (DISKUS), ki<br />
je sestavljena iz zunanjega ohišja, ustnika, vzmeti in<br />
števca preostalih odmerkov. Prašek za inhaliranje se<br />
enakomerno razporejen v odmerke nahaja med dvema<br />
plastema odmernega traku v notranjosti naprave.<br />
Zdravilo SERETIDE DISKUS je na voljo v treh jakostih,<br />
vsaka izmed njih zadošča za 60 odmerkov.<br />
IMETNIK DOVOLJENJA ZA PROMET<br />
GSK d.o.o., Ljubljana, Knezov štradon 90, 1000 Ljubljana,<br />
Slovenija<br />
DATUM ZADNJE REVIZIJE BESEDILA<br />
11. 06. 2010<br />
Pred predpisovanjem, prosimo, preberite celoten<br />
povzetek glavnih značilnosti zdravila.<br />
Predpisovanje in izdaja zdravila je le na recept.<br />
Za vse morebitne neadaljne informacije o tem zdravilu<br />
se lahko obrnete na imetnika dovoljenja za promet<br />
z zdravilom:GSK d.o.o.,Ljubljana, knezov štradon 90,<br />
1000 Ljubljana, Tel:+ 386(0) 1 280 25 00, medical.x.si@<br />
gsk.com.<br />
Seretide ® in Diskus ® sta zaščiteni blagovni znamki skupine<br />
družb GlaxoSmithKline. © 2010 GlaxoSmithKline. Vse<br />
pravice pridržane.<br />
Datum priprave materiala: September <strong>2011</strong>.<br />
Veljavnost 1 leto.<br />
Literatura:<br />
1. Dalal AA in sod., Chest 2009; 136(4): 89s-90s and<br />
poster presented at the meeting of the American<br />
College of Chest Physicians, San Diego 2009 (P428).<br />
2. Povzetek temeljenih značilnosti zdravila Seretide.<br />
SLO/SFC/0002/11
^AS ZA ŽIVLJENJE.<br />
DOKAZANO PODALJŠA PREŽIVETJE PRI BOLNIKIH:<br />
z lokalno napredovalim ali metastatskim<br />
nedrobnoceli~nim rakom plju~ 1<br />
z metastatskim rakom trebu{ne slinavke 1<br />
1<br />
Povzetek glavnih značilnosti zdravila TARCEVA, www.ema.europa.eu
SKRAJ[AN POVZETEK GLAVNIH ZNA^ILNOSTI ZDRAVILA<br />
Samo za strokovno javnost.<br />
Ime zdravila: Tarceva 25 mg/100 mg/150 mg filmsko obložene<br />
tablete<br />
Kakovostna in koli~inska sestava: Ena filmsko obložena tableta<br />
vsebuje 25 mg, 100 mg ali 150 mg erlotiniba (v obliki erlotinibijevega<br />
klorida).<br />
Terapevtske indikacije: Nedrobnoceli~ni rak plju~: Zdravilo Tarceva<br />
je indicirano za samostojno vzdrževalno zdravljenje bolnikov z lokalno<br />
napredovalim ali metastatskim nedrobnoceli~nim rakom plju~ s stabilno<br />
boleznijo po 4 ciklih standardne kemoterapije na osnovi platine v prvi<br />
liniji zdravljenja. Zdravilo Tarceva je indicirano tudi za zdravljenje<br />
bolnikov z lokalno napredovalim ali metastatskim nedrobnoceli~nim<br />
rakom plju~ po neuspehu vsaj ene predhodne kemoterapije. Pri<br />
predpisovanju zdravila Tarceva je treba upo{tevati dejavnike, povezane<br />
s podalj{anim preživetjem. Koristnega vpliva na podalj{anje preživetja<br />
ali drugih klini~no pomembnih u~inkov zdravljenja niso dokazali pri<br />
bolnikih z EGFR-negativnimi tumorji. Rak trebu{ne slinavke: Zdravilo<br />
Tarceva je v kombinaciji z gemcitabinom indicirano za zdravljenje<br />
bolnikov z metastatskim rakom trebu{ne slinavke. Pri predpisovanju<br />
zdravila Tarceva je treba upo{tevati dejavnike, povezane s podalj{anim<br />
preživetjem. Koristnega vpliva na podalj{anje preživetja niso dokazali<br />
za bolnike z lokalno napredovalo boleznijo.<br />
Odmerjanje in na~in uporabe: Zdravljenje z zdravilom Tarceva<br />
mora nadzorovati zdravnik z izku{njami pri zdravljenju raka. Zdravilo<br />
Tarceva vzamemo najmanj eno uro pred zaužitjem hrane ali dve uri po<br />
tem. Kadar je potrebno odmerek prilagoditi, ga je treba zmanj{evati v<br />
korakih po 50 mg. Pri so~asnem jemanju substratov in modulatorjev<br />
CYP3A4 bo morda potrebna prilagoditev odmerka. Pri dajanju zdravila<br />
Tarceva bolnikom z jetrno okvaro je potrebna previdnost. ^e se pojavijo<br />
hudi neželeni u~inki, pride v po{tev zmanj{anje odmerka ali prekinitev<br />
zdravljenja z zdravilom Tarceva. Uporaba zdravila Tarceva pri bolnikih s<br />
hudo jetrno ali ledvi~no okvaro ter pri otrocih ni priporo~ljiva. Bolnikom<br />
kadilcem je treba svetovati, naj prenehajo kaditi, saj so plazemske<br />
koncentracije erlotiniba pri kadilcih manj{e kot pri nekadilcih.<br />
Nedrobnoceli~ni rak plju~: Priporo~eni dnevni odmerek zdravila Tarceva<br />
je 150 mg. Rak trebu{ne slinavke: Priporo~eni dnevni odmerek zdravila<br />
Tarceva je 100 mg, v kombinaciji z gemcitabinom. Pri bolnikih, pri<br />
katerih se kožni izpu{~aj v prvih 4 do 8 tednih zdravljenja ne pojavi,<br />
je treba ponovno pretehtati nadaljnje zdravljenje z zdravilom Tarceva.<br />
Kontraindikacije: Preob~utljivost za erlotinib ali katero koli pomožno<br />
snov.<br />
Posebna opozorila in previdnostni ukrepi: Mo~ni induktorji<br />
CYP3A4 lahko zmanj{ajo u~inkovitost erlotiniba, mo~ni zaviralci<br />
CYP3A4 pa lahko pove~ajo toksi~nost. So~asnemu zdravljenju s temi<br />
zdravili se je treba izogibati. Bolnikom, ki kadijo, je treba svetovati, naj<br />
prenehajo kaditi, saj so plazemske koncentracije erlotiniba pri kadilcih<br />
zmanj{ane v primerjavi s plazemskimi koncentracijami pri nekadilcih.<br />
Verjetno je, da je velikost zmanj{anja klini~no pomembna. Pri bolnikih,<br />
pri katerih se akutno pojavijo novi in/ali poslab{ajo nepojasnjeni<br />
plju~ni simptomi, kot so dispneja, ka{elj in vro~ina, je treba<br />
zdravljenje z zdravilom Tarceva prekiniti, dokler ni znana diagnoza.<br />
Bolnike, ki se so~asno zdravijo z erlotinibom in gemcitabinom, je<br />
treba skrbno spremljati zaradi možnosti pojava toksi~nosti, podobni<br />
intersticijski bolezni plju~. ^e je ugotovljena intersticijska bolezen<br />
plju~, zdravilo Tarceva ukinemo in uvedemo ustrezno zdravljenje. Pri<br />
približno polovici bolnikov, ki so se zdravili z zdravilom Tarceva, se<br />
je pojavila driska (vklju~no z zelo redkimi primeri, ki so se kon~ali s<br />
smrtnim izidom). Zmerno do hudo drisko zdravimo z loperamidom.<br />
V nekaterih primerih bo morda potrebno zmanj{anje odmerka. V<br />
primeru hude ali dolgotrajne driske, navzeje, anoreksije ali bruhanja,<br />
povezanih z dehidracijo, je treba zdravljenje z zdravilom Tarceva<br />
prekiniti in dehidracijo ustrezno zdraviti. O hipokaliemiji in ledvi~ni<br />
odpovedi so poro~ali redko. Posebno pri bolnikih z dejavniki tveganja<br />
(so~asno jemanje drugih zdravil, simptomi, bolezni ali drugi dejavniki,<br />
vklju~no z visoko starostjo) moramo, ~e je driska huda ali dolgotrajna<br />
oziroma vodi v dehidracijo, zdravljenje z zdravilom Tarceva prekiniti<br />
in bolnikom zagotoviti intenzivno intravensko rehidracijo. Dodatno je<br />
treba pri bolnikih s prisotnim tveganjem za razvoj dehidracije spremljati<br />
ledvi~no delovanje in serumske elektrolite, vklju~no s kalijem. Pri<br />
uporabi zdravila Tarceva so poro~ali o redkih primerih jetrne odpovedi.<br />
K njenemu nastanku je lahko pripomogla predhodno obstoje~a jetrna<br />
bolezen ali so~asno jemanje hepatotoksi~nih zdravil. Pri teh bolnikih je<br />
treba zato premisliti o rednem spremljanju jetrnega delovanja. Dajanje<br />
zdravila Tarceva je treba prekiniti, ~e so spremembe jetrnega delovanja<br />
hude. Bolniki, ki prejemajo zdravilo Tarceva, imajo ve~je tveganje za<br />
razvoj perforacij v prebavilih, ki so jih opazili ob~asno (vklju~no z<br />
nekaterimi primeri, ki so se kon~ali s smrtnim izidom). Pri bolnikih, ki<br />
so~asno prejemajo zdravila, ki zavirajo angiogenezo, kortikosteroide,<br />
nesteroidna protivnetna zdravila (NSAID) in/ali kemoterapijo na osnovi<br />
taksanov, ali so v preteklosti imeli pepti~ni ulkus ali divertikularno<br />
bolezen, je tveganje ve~je. ^e pride do tega, je treba zdravljenje z<br />
zdravilom Tarceva dokon~no ukiniti. Poro~ali so o primerih kožnih<br />
bolezni z mehurji in lu{~enjem kože, vklju~no z zelo redkimi primeri,<br />
ki so nakazovali na Stevens-Johnsonov sindrom/toksi~no epidermalno<br />
nekrolizo in so bili v nekaterih primerih smrtni. Zdravljenje z zdravilom<br />
Tarceva je treba prekiniti ali ukiniti, ~e se pri bolniku pojavijo hude<br />
oblike mehurjev ali lu{~enja kože. Zelo redko so poro~ali o primerih<br />
perforacije ali ulceracije roženice; opazili so tudi druge o~esne bolezni.<br />
Zdravljenje z zdravilom Tarceva je treba prekiniti ali ukiniti, ~e se pri<br />
bolnikih pojavijo akutne o~esne bolezni, kot je bole~ina v o~eh, ali se lete<br />
poslab{ajo. Tablete vsebujejo laktozo in jih ne smemo dajati bolnikom<br />
z redkimi dednimi stanji: intoleranco za galaktozo, laponsko obliko<br />
zmanj{ane aktivnosti laktaze ali malabsorpcijo glukoze/galaktoze.<br />
Medsebojno delovanje z drugimi zdravili in druge oblike<br />
interakcij: Erlotinib se pri ljudeh presnavlja v jetrih z jetrnimi<br />
citokromi, primarno s CYP3A4 in v manj{i meri s CYP1A2. Presnova<br />
erlotiniba zunaj jeter poteka s CYP3A4 v ~revesju, CYP1A1 v plju~ih<br />
in CYP1B1 v tumorskih tkivih. Z zdravilnimi u~inkovinami, ki se<br />
presnavljajo s temi encimi, jih zavirajo ali pa so njihovi induktorji,<br />
lahko pride do interakcij. Erlotinib je srednje mo~an zaviralec CYP3A4<br />
in CYP2C8, kot tudi mo~an zaviralec glukuronidacije z UGT1A1 in vitro.<br />
Pri kombinaciji ciprofloksacina ali mo~nega zaviralca CYP1A2 (npr.<br />
fluvoksamina) z erlotinibom je potrebna previdnost. V primeru pojava<br />
neželenih u~inkov, povezanih z erlotinibom, lahko odmerek erlotiniba<br />
zmanj{amo. Predhodno ali so~asno zdravljenje z zdravilom Tarceva<br />
ni spremenilo o~istka prototipov substratov CYP3A4, midazolama in<br />
eritromicina. Inhibicija glukoronidacije lahko povzro~i interakcije z<br />
zdravili, ki so substrati UGT1A1 in se izlo~ajo samo po tej poti. Mo~ni<br />
zaviralci aktivnosti CYP3A4 zmanj{ajo presnovo erlotiniba in zve~ajo<br />
koncentracije erlotiniba v plazmi. Pri so~asnem jemanju erlotiniba in<br />
mo~nih zaviralcev CYP3A4 je zato potrebna previdnost. ^e je treba,<br />
odmerek erlotiniba zmanj{amo, {e posebno pri pojavu toksi~nosti.<br />
Mo~ni spodbujevalci aktivnosti CYP3A4 zve~ajo presnovo erlotiniba in<br />
pomembno zmanj{ajo plazemske koncentracije erlotiniba. So~asnemu<br />
dajanju zdravila Tarceva in induktorjev CYP3A4 se je treba izogibati.<br />
Pri bolnikih, ki potrebujejo so~asno zdravljenje z zdravilom Tarceva in<br />
mo~nim induktorjem CYP3A4, je treba premisliti o pove~anju odmerka<br />
do 300 mg ob skrbnem spremljanju njihove varnosti. Zmanj{ana<br />
izpostavljenost se lahko pojavi tudi z drugimi induktorji, kot so fenitoin,<br />
karbamazepin, barbiturati ali {entjanževka. ^e te zdravilne u~inkovine<br />
kombiniramo z erlotinibom, je potrebna previdnost. Kadar je mogo~e, je<br />
treba razmisliti o drugih na~inih zdravljenja, ki ne vklju~ujejo mo~nega<br />
spodbujanja aktivnosti CYP3A4. Bolnikom, ki jemljejo kumarinske<br />
antikoagulante, je treba redno kontrolirati protrombinski ~as ali INR.<br />
So~asno zdravljenje z zdravilom Tarceva in statinom lahko pove~a<br />
tveganje za miopatijo, povzro~eno s statini, vklju~no z rabdomiolizo;<br />
to so opazili redko. So~asna uporaba zaviralcev P-glikoproteina, kot sta<br />
ciklosporin in verapamil, lahko vodi v spremenjeno porazdelitev in/ali<br />
spremenjeno izlo~anje erlotiniba. Za erlotinib je zna~ilno zmanj{anje<br />
topnosti pri pH nad 5. Zdravila, ki spremenijo pH v zgornjem delu<br />
prebavil, lahko spremenijo topnost erlotiniba in posledi~no njegovo<br />
biolo{ko uporabnost. U~inka antacidov na absorpcijo erlotiniba niso<br />
prou~evali, vendar je ta lahko zmanj{ana, kar vodi v nižje plazemske<br />
koncentracije. Kombinaciji erlotiniba in zaviralca protonske ~rpalke se je<br />
treba izogibati. ^e menimo, da je uporaba antacidov med zdravljenjem<br />
z zdravilom Tarceva potrebna, jih je treba jemati najmanj 4 ure pred ali<br />
2 uri po dnevnem odmerku zdravila Tarceva. ^e razmi{ljamo o uporabi<br />
ranitidina, moramo zdravili jemati lo~eno: zdravilo Tarceva je treba vzeti<br />
najmanj 2 uri pred ali 10 ur po odmerku ranitidina. V {tudiji faze Ib<br />
ni bilo pomembnih u~inkov gemcitabina na farmakokinetiko erlotiniba,<br />
prav tako ni bilo pomembnih u~inkov erlotiniba na farmakokinetiko<br />
gemcitabina. Erlotinib pove~a koncentracijo platine. Pomembnih<br />
u~inkov karboplatina ali paklitaksela na farmakokinetiko erlotiniba ni<br />
bilo. Kapecitabin lahko pove~a koncentracijo erlotiniba. Pomembnih<br />
u~inkov erlotiniba na farmakokinetiko kapecitabina ni bilo.<br />
Neželeni u~inki: Zelo pogosti neželeni u~inki so kožni izpu{~aj<br />
in driska, kot tudi utrujenost, anoreksija, dispneja, ka{elj, okužba,<br />
navzea, bruhanje, stomatitis, bole~ina v trebuhu, pruritus, suha koža,<br />
suhi keratokonjunktivitis, konjunktivitis, zmanj{anje telesne mase,<br />
depresija, glavobol, nevropatija, dispepsija, flatulenca, alopecija,<br />
okorelost, pireksija, nenormalnosti testov jetrne funkcije. Pogosti<br />
neželeni u~inki so krvavitve v prebavilih, epistaksa, keratitis, paronihija,<br />
fisure na koži. Ob~asno so poro~ali o perforacijah v prebavilih,<br />
hirzutizmu, spremembah obrvi, krhkih nohtih, odstopanju nohtov od<br />
kože, blagih reakcijah na koži (npr. hiperpigmentacija), spremembah<br />
trepalnic, hudi intersticijski bolezni plju~ (vklju~no s smrtnimi primeri).<br />
Redko pa so poro~ali o jetrni odpovedi. Zelo redko so poro~ali o Stevens-<br />
Johnsonovem sindromu/toksi~ni epidermalni nekrolizi ter o ulceracijah<br />
in perforacijah roženice.<br />
Režim izdaje zdravila: H/Rp. Imetnik dovoljenja za promet: Roche<br />
Registration Limited, 6 Falcon Way, Shire Park, Welwyn Garden City, AL7<br />
1TW, Velika Britanija. Verzija: 2.0/10. Informacija pripravljena:<br />
avgust <strong>2011</strong>.<br />
DODATNE INFORMACIJE SO NA VOLJO PRI:<br />
Roche farmacevtska družba d.o.o.<br />
Vodovodna cesta 109, 1000 Ljubljana.<br />
Povzetek glavnih zna~ilnosti zdravila je dosegljiv<br />
na www.roche.si ali www.onkologija.si.<br />
025-11-TAR