Guidelines on the Management of Stable Angina Pectoris ... - Cardio
Guidelines on the Management of Stable Angina Pectoris ... - Cardio
Guidelines on the Management of Stable Angina Pectoris ... - Cardio
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
ESC <str<strong>on</strong>g>Guidelines</str<strong>on</strong>g> 3societies and translated into <strong>the</strong> local language, whennecessary.All in all, <strong>the</strong> task <strong>of</strong> writing <str<strong>on</strong>g>Guidelines</str<strong>on</strong>g> or ExpertC<strong>on</strong>sensus Document covers not <strong>on</strong>ly <strong>the</strong> integrati<strong>on</strong> <strong>of</strong> <strong>the</strong>most recent research but also <strong>the</strong> creati<strong>on</strong> <strong>of</strong> educati<strong>on</strong>altools and implementati<strong>on</strong> programmes for <strong>the</strong> recommendati<strong>on</strong>s.The loop between clinical research, writing <strong>of</strong>guidelines, and implementing <strong>the</strong>m into clinical practicecan <strong>the</strong>n <strong>on</strong>ly be completed if surveys and registries areorganized to verify that actual clinical practice is inkeeping with what is recommended in <strong>the</strong> guidelines. Suchsurveys and registries also make it possible to check <strong>the</strong>impact <strong>of</strong> strict implementati<strong>on</strong> <strong>of</strong> <strong>the</strong> guidelines <strong>on</strong>patient outcome.Classes <strong>of</strong> Recommendati<strong>on</strong>sClass IClass IIClass IIaClass IIbClass IIIEvidence and/or general agreement that a givendiagnostic procedure/treatment is beneficial,useful, and effectiveC<strong>on</strong>flicting evidence and/or a divergence <strong>of</strong> opini<strong>on</strong>about <strong>the</strong> usefulness/efficacy <strong>of</strong> <strong>the</strong> treatmentor procedureWeight <strong>of</strong> evidence/opini<strong>on</strong> is in favour <strong>of</strong>usefulness/efficacyUsefulness/efficacy is less well established byevidence/opini<strong>on</strong>Evidence or general agreement that <strong>the</strong> treatmentor procedure is not useful/effective and, in somecases, may be harmfulLevel <strong>of</strong> evidence A Data derived from multiple randomizedclinical trials or meta-analysesLevel <strong>of</strong> evidence B Data derived from a single randomizedclinical trial or large n<strong>on</strong>-randomizedstudiesLevel <strong>of</strong> evidence C C<strong>on</strong>sensus <strong>of</strong> opini<strong>on</strong> <strong>of</strong> <strong>the</strong> experts and/orsmall studies, retrospective studies, andregistriesIntroducti<strong>on</strong><strong>Stable</strong> angina pectoris is a comm<strong>on</strong> and disabling disorder.However, <strong>the</strong> management <strong>of</strong> stable angina has not beensubjected to <strong>the</strong> same scrutiny by large randomized trialsas has, for example, that <strong>of</strong> acute cor<strong>on</strong>ary syndromes(ACS) including unstable angina and myocardial infarcti<strong>on</strong>(MI). The optimal strategy <strong>of</strong> investigati<strong>on</strong> and treatmentis difficult to define, and <strong>the</strong> development <strong>of</strong> new tools for<strong>the</strong> diagnostic and prognostic assessment <strong>of</strong> patients,al<strong>on</strong>g with <strong>the</strong> c<strong>on</strong>tinually evolving evidence base forvarious treatment strategies, mandates that <strong>the</strong> existingguidelines be revised and updated. The Task Force has<strong>the</strong>refore obtained opini<strong>on</strong>s from a wide variety <strong>of</strong> expertsand has tried to achieve agreement <strong>on</strong> <strong>the</strong> best c<strong>on</strong>temporaryapproaches to <strong>the</strong> care <strong>of</strong> stable angina pectoris, bearingin mind not <strong>on</strong>ly <strong>the</strong> efficacy and safety <strong>of</strong> treatments butalso <strong>the</strong> cost and <strong>the</strong> availability <strong>of</strong> resources. The TaskForce has taken <strong>the</strong> view that <strong>the</strong>se guidelines shouldreflect <strong>the</strong> pathophysiology and management <strong>of</strong> angina pectoris,namely myocardial ischaemia due to cor<strong>on</strong>ary arterydisease (CAD), usually macrovascular, i.e. involving largecor<strong>on</strong>ary arteries, but also microvascular in some <strong>of</strong> <strong>the</strong>patients. Fur<strong>the</strong>rmore, this Task Force does not deal withprimary preventi<strong>on</strong>, which has already been covered ino<strong>the</strong>r recently published guidelines 1 and has limited its discussi<strong>on</strong><strong>on</strong> sec<strong>on</strong>dary preventi<strong>on</strong>. Recently published guidelinesand c<strong>on</strong>sensus statements that overlap to ac<strong>on</strong>siderable extent with <strong>the</strong> remit <strong>of</strong> this document arelisted in Table 1.Definiti<strong>on</strong> and pathophysiology<strong>Stable</strong> angina is a clinical syndrome characterized bydiscomfort in <strong>the</strong> chest, jaw, shoulder, back, or arms, typicallyelicited by exerti<strong>on</strong> or emoti<strong>on</strong>al stress and relievedby rest or nitroglycerin. Less typically, discomfort mayoccur in <strong>the</strong> epigastric area. William Heberden first introduced<strong>the</strong> term ‘angina pectoris’ in 1772 2 to characterizea syndrome in which <strong>the</strong>re was ‘a sense <strong>of</strong> strangling andanxiety’ in <strong>the</strong> chest, especially associated with exercise,although its pathological aetiology was not recognizeduntil some years later. 3 It is now usual to c<strong>on</strong>fine <strong>the</strong>term to cases in which <strong>the</strong> syndrome can be attributed tomyocardial ischaemia, although essentially similar symptomscan be caused by disorders <strong>of</strong> <strong>the</strong> oesophagus,lungs, or chest wall. Although <strong>the</strong> most comm<strong>on</strong> cause <strong>of</strong>myocardial ischaemia is a<strong>the</strong>rosclerotic CAD, dem<strong>on</strong>strablemyocardial ischaemia may be induced in <strong>the</strong> abscence byhypertrophic or dilated cardiomyopathy, aortic stenosis,or o<strong>the</strong>r rare cardiac c<strong>on</strong>diti<strong>on</strong>s in <strong>the</strong> absence <strong>of</strong> obstructivea<strong>the</strong>romatous cor<strong>on</strong>ary disease, which are notc<strong>on</strong>sidered in this document.Myocardial ischaemia is caused by an imbalance betweenmyocardial oxygen supply and myocardial oxygen c<strong>on</strong>sumpti<strong>on</strong>.Myocardial oxygen supply is determined by arterialoxygen saturati<strong>on</strong> and myocardial oxygen extracti<strong>on</strong>,which are relatively fixed under normal circumstances,and cor<strong>on</strong>ary flow, which is dependent <strong>on</strong> <strong>the</strong> luminal crosssecti<strong>on</strong>alarea <strong>of</strong> <strong>the</strong> cor<strong>on</strong>ary artery and cor<strong>on</strong>ary arteriolart<strong>on</strong>e. Both cross-secti<strong>on</strong>al area and arterioloar t<strong>on</strong>e may bedramatically altered by <strong>the</strong> presence <strong>of</strong> a<strong>the</strong>roscleroticplaque within <strong>the</strong> vessel wall, leading to imbalancebetween supply and demand when myocardial oxygendemands increase, as during exerti<strong>on</strong>, related to increasesin heart rate, myocardial c<strong>on</strong>tractility, and wall stress.Ischaemia-induced sympa<strong>the</strong>tic activati<strong>on</strong> can fur<strong>the</strong>rincrease <strong>the</strong> severity <strong>of</strong> ischaemia through a variety <strong>of</strong>mechanisms including a fur<strong>the</strong>r increase <strong>of</strong> myocardialoxygen c<strong>on</strong>sumpti<strong>on</strong> and cor<strong>on</strong>ary vasoc<strong>on</strong>stricti<strong>on</strong>. Theischaemic cascade is characterized by a sequence <strong>of</strong>events, resulting in metabolic abnormalities, perfusi<strong>on</strong> mismatch,regi<strong>on</strong>al and <strong>the</strong>n global diastolic and systolic dysfuncti<strong>on</strong>,electrocardiographic (ECG) changes, and angina.Adenosine released by ischaemic myocardium appears tobe <strong>the</strong> main mediator <strong>of</strong> angina (chest pain) through stimulati<strong>on</strong><strong>of</strong> A1 receptors located <strong>on</strong> cardiac nerve endings. 4Ischaemia is followed by reversible c<strong>on</strong>tractile dysfuncti<strong>on</strong>known as ‘stunning’. Recurrent episodes <strong>of</strong> ischaemia and
ESC <str<strong>on</strong>g>Guidelines</str<strong>on</strong>g> 5or at rest. 11 MI is characterized by prol<strong>on</strong>ged angina(.30 min) associated with myocardial necrosis. 12 Bothn<strong>on</strong>-ST-elevati<strong>on</strong> and ST-elevati<strong>on</strong> MI are frequently precededby a period <strong>of</strong> days, or even weeks, <strong>of</strong> unstable symptoms.The comm<strong>on</strong> pathological background <strong>of</strong> ACS is erosi<strong>on</strong>,fissure, or rupture <strong>of</strong> an a<strong>the</strong>rosclerotic cor<strong>on</strong>ary plaqueassociated with platelet aggregati<strong>on</strong>, leading to subtotal ortotal thrombotic cor<strong>on</strong>ary occlusi<strong>on</strong>. Activated plateletsrelease a number <strong>of</strong> vasoc<strong>on</strong>strictors, which may fur<strong>the</strong>rimpair cor<strong>on</strong>ary flow through <strong>the</strong> stimulati<strong>on</strong> <strong>of</strong> vascularsmooth muscle cells both locally and distally. The haemodynamicseverity <strong>of</strong> <strong>the</strong> a<strong>the</strong>rosclerotic plaque prior to destabilizati<strong>on</strong>is frequently mild and <strong>the</strong> plaques are lipid filledwith foam cells. Intravascular ultrasound studies haveshown that so-called vulnerable plaques (i.e. at risk <strong>of</strong> caprupture) that are ,50% in diameter both precede andpredict future acute syndromes occurring precisely in <strong>the</strong>irneighbourhood. 13 Activati<strong>on</strong> <strong>of</strong> inflammatory cells within<strong>the</strong> a<strong>the</strong>rosclerotic plaque appears to play an importantrole in <strong>the</strong> destabilizati<strong>on</strong> process, 14 leading to plaqueerosi<strong>on</strong>, fissure, or rupture. More recently, <strong>the</strong> c<strong>on</strong>cept <strong>of</strong> asingle vulnerable plaque causing an ACS has been challengedin favour <strong>of</strong> a more generalized inflammatory resp<strong>on</strong>se. 15EpidemiologyAs angina is essentially a diagnosis based <strong>on</strong> history, and<strong>the</strong>refore subjective, it is understandable that its prevalenceand incidence have been difficult to assess and mayvary between studies dependent <strong>on</strong> <strong>the</strong> definiti<strong>on</strong> that hasbeen used.For epidemiological purposes, <strong>the</strong> L<strong>on</strong>d<strong>on</strong> School <strong>of</strong>Hygiene and Tropical Medicine cardiovascular questi<strong>on</strong>naire,devised by Rose and Blackburn 16 and adopted by <strong>the</strong> WHO,has been widely used. It defines angina as chest pain,pressure, or heaviness that limits exerti<strong>on</strong>, is situated over<strong>the</strong> sternum or in <strong>the</strong> left chest and left arm, and is relievedwithin 10 min <strong>of</strong> rest. The questi<strong>on</strong>naire allows a subdivisi<strong>on</strong><strong>of</strong> symptoms into definite and possible angina, which can befur<strong>the</strong>r subdivided into grade 1 and grade 2. 17 It should berecognized that this questi<strong>on</strong>naire is a screening tool andnot a diagnostic test.Rose angina questi<strong>on</strong>naire predicts cardiovascular morbidityand mortality in European 18,19 and American populati<strong>on</strong>s, 20independent <strong>of</strong> o<strong>the</strong>r risk factors. Therefore, it has beenindirectly validated. It has been compared with o<strong>the</strong>rstandards including a clinical diagnosis, 21 ECG findings, 22radi<strong>on</strong>uclide tests, 23 and cor<strong>on</strong>ary arteriography. 24 On <strong>the</strong>basis <strong>of</strong> such comparis<strong>on</strong>s, its specificity is 80–95% but itssensitivity varies greatly from 20 to 80%. The exerti<strong>on</strong>alcomp<strong>on</strong>ent <strong>of</strong> <strong>the</strong> symptoms is crucial to <strong>the</strong> diagnosticaccuracy <strong>of</strong> <strong>the</strong> questi<strong>on</strong>aire, 18 and its performance seemsto be less accurate in women. 25The prevalence <strong>of</strong> angina in community studies increasessharply with age in both sexes from 0.1–1% in women aged45–54 to 10–15% in women aged 65–74 and from 2–5% inmen aged 45–54 to 10–20% in men aged 65–74. 26–33Therefore, it can be estimated that in most Europeancountries, 20 000–40 000 individuals <strong>of</strong> <strong>the</strong> populati<strong>on</strong> permilli<strong>on</strong> suffer from angina.Community-based informati<strong>on</strong> <strong>on</strong> <strong>the</strong> incidence <strong>of</strong> anginapectoris is derived from prospective, epidemiologic studieswith repeated examinati<strong>on</strong>s <strong>of</strong> <strong>the</strong> cohort. Such studieshave been scarce over recent years. Available data, from<strong>the</strong> Seven Countries study, 34 studies in <strong>the</strong> UK, 35,36 <strong>the</strong>Israel Ischaemic Heart Disease study, 37 <strong>the</strong> H<strong>on</strong>olulu Heartstudy, 38 <strong>the</strong> Framingham study 39,40 and o<strong>the</strong>rs, 41 suggestan annual incidence <strong>of</strong> uncomplicated angina pectoris<strong>of</strong> 0.5% in western populati<strong>on</strong>s aged .40, but withgeographic variati<strong>on</strong>s evident.A more recent study, using a different definiti<strong>on</strong> <strong>of</strong> anginabased <strong>on</strong> case descripti<strong>on</strong> by clinicians, which definedangina pectoris as <strong>the</strong> associati<strong>on</strong> <strong>of</strong> chest pain at rest or<strong>on</strong> exerti<strong>on</strong> with <strong>on</strong>e positive finding from a cardiovascularexaminati<strong>on</strong> such as arteriography, scintigraphy, exercisetesting, or resting ECG, 42 c<strong>on</strong>firm geographical variati<strong>on</strong>sin <strong>the</strong> incidence <strong>of</strong> angina which occur in parallel withobserved internati<strong>on</strong>al differences in cor<strong>on</strong>ary heartdisease (CHD) mortality. The incidence <strong>of</strong> angina pectorisas a first cor<strong>on</strong>ary event was approximately twice high inBelfast compared with France (5.4 per 1000 pers<strong>on</strong>-yearscompared with 2.6).Temporal trends suggest a decrease in <strong>the</strong> prevalence <strong>of</strong>angina pectoris in recent decades 35,43 in line with falling cardiovascularmortality rates observed in <strong>the</strong> MONICA 44 study.However, <strong>the</strong> prevalence <strong>of</strong> a history <strong>of</strong> diagnosed CHD doesnot appear to have decreased, suggesting that althoughfewer people are developing angina due to changes in lifestyleand risk factors, those who have cor<strong>on</strong>ary disease areliving l<strong>on</strong>ger with <strong>the</strong> disease. Improved sensitivity <strong>of</strong> diagnostictools may additi<strong>on</strong>ally c<strong>on</strong>tribute to <strong>the</strong> c<strong>on</strong>temporaryhigh prevalence <strong>of</strong> diagnosed CHD.Natural history and prognosisInformati<strong>on</strong> <strong>on</strong> <strong>the</strong> prognosis associated with chr<strong>on</strong>ic stableangina is derived from l<strong>on</strong>g-term prospective, populati<strong>on</strong>basedstudies, clinical trials <strong>of</strong> antianginal <strong>the</strong>rapy, andobservati<strong>on</strong>al registries, with selecti<strong>on</strong> bias an importantfactor to c<strong>on</strong>sider when evaluating and comparing <strong>the</strong> availabledata. European data estimate <strong>the</strong> cardiovasculardisease (CVD) mortality rate and CHD mortality rates formen with Rose questi<strong>on</strong>naire angina to be between 2.6and 17.6 per 1000 patient-years between <strong>the</strong> 1970s and1990s. 35,45 Data from <strong>the</strong> Framingham Heart Study 40,46showed that for men and women with an initial clinical presentati<strong>on</strong><strong>of</strong> stable angina, <strong>the</strong> 2-year incidence rates <strong>of</strong> n<strong>on</strong>fatalMI and CHD death were 14.3 and 5.5% in men and 6.2and 3.8% in women, respectively. More c<strong>on</strong>temporary dataregarding prognosis can be gleaned from clinical trials <strong>of</strong>antianginal <strong>the</strong>rapy and/or revascularizati<strong>on</strong>, although<strong>the</strong>se data are biased by <strong>the</strong> selected nature <strong>of</strong> <strong>the</strong> populati<strong>on</strong>sstudied. From <strong>the</strong>se, estimates for annual mortalityrates range from 0.9–1.4% per annum, 47–51 with an annualincidence <strong>of</strong> n<strong>on</strong>-fatal MI between 0.5% (INVEST) 50 and2.6% (TIBET). 48 These estimates are c<strong>on</strong>sistent with observati<strong>on</strong>alregistry data. 52However, within <strong>the</strong> populati<strong>on</strong> with stable angina, anindividual’s prognosis can vary c<strong>on</strong>siderably, by up to10-fold, dependent <strong>on</strong> baseline clinical, functi<strong>on</strong>al, and anatomicalfactors. Therefore, prognostic assessment is animportant part <strong>of</strong> <strong>the</strong> management <strong>of</strong> patients with stableangina. On <strong>the</strong> <strong>on</strong>e hand, it is important to carefullyselect those patients with more severe forms <strong>of</strong> diseaseand candidates for revascularizati<strong>on</strong> and potential
6 ESC <str<strong>on</strong>g>Guidelines</str<strong>on</strong>g>improvement in outcome with more aggressive investigati<strong>on</strong>and treatment. On <strong>the</strong> o<strong>the</strong>r hand, it is also important toselect those patients with a less severe form <strong>of</strong> disease,with a good outcome, <strong>the</strong>reby avoiding unnecessary invasiveand n<strong>on</strong>-invasive tests and procedures.C<strong>on</strong>venti<strong>on</strong>al risk factors for <strong>the</strong> development <strong>of</strong>CAD, 26,53–55,56 hypertensi<strong>on</strong>, hypercholesterolaemia 56–59diabetes, 60–65 and smoking 26 have an adverse influence <strong>on</strong>prognosis in those with established disease, presumablythrough <strong>the</strong>ir effect <strong>on</strong> disease progressi<strong>on</strong>. However, appropriatetreatment can reduce or abolish <strong>the</strong>se risks. O<strong>the</strong>rfactors predictive <strong>of</strong> l<strong>on</strong>g-term prognosis <strong>of</strong> patients withstable angina have been determined from <strong>the</strong> follow-up <strong>of</strong><strong>the</strong> large c<strong>on</strong>trol groups <strong>of</strong> randomized trials aimed at evaluating<strong>the</strong> effectiveness <strong>of</strong> revascularizati<strong>on</strong> 66,67 and o<strong>the</strong>robservati<strong>on</strong>al data. In general, <strong>the</strong> outcome is worse inpatients with reduced LV functi<strong>on</strong>, a greater number <strong>of</strong>diseased vessels, more proximal locati<strong>on</strong>s <strong>of</strong> cor<strong>on</strong>arystenosis, greater severity <strong>of</strong> lesi<strong>on</strong>s, more severe angina,more extensive ischaemia, and greater age.LV functi<strong>on</strong> is <strong>the</strong> str<strong>on</strong>gest predictor <strong>of</strong> survival inpatients with chr<strong>on</strong>ic stable cor<strong>on</strong>ary disease; <strong>the</strong> nextmost important factor is <strong>the</strong> distributi<strong>on</strong> and severity <strong>of</strong>cor<strong>on</strong>ary stenosis. Left main (LM) disease, three-vesseldisease, and <strong>the</strong> proximal involvement <strong>of</strong> <strong>the</strong> left anteriordescending are comm<strong>on</strong> characteristics predicting a pooroutcome and increase <strong>the</strong> risk <strong>of</strong> ischaemic events. 68Myocardial revascularizati<strong>on</strong> can reduce <strong>the</strong> risk <strong>of</strong> deathin selected anatomical subgroups, 69 reduce <strong>the</strong> number <strong>of</strong>ischaemic episodes (ACIP), 70 and in some instances mayimprove <strong>the</strong> LV functi<strong>on</strong> in high-risk patients. 71,72 However,disease progressi<strong>on</strong> and <strong>the</strong> occurrence <strong>of</strong> acute eventsmay not necessarily be related to <strong>the</strong> severity <strong>of</strong> stenosisat cor<strong>on</strong>ary arteriography. In all patients, smaller lipidfilled plaques are present in additi<strong>on</strong> to those that causesevere stenoses. As discussed earlier, <strong>the</strong>se ‘vulnerableplaques’ have a greater likelihood to rupture. 14 Thus,<strong>the</strong> risk <strong>of</strong> acute events is related to <strong>the</strong> overall plaqueburden and to plaque vulnerability. Although an area<strong>of</strong> great research interest, our capabilities to identifyvulnerable plaque remain limited.Diagnosis and assessmentDiagnosis and assessment <strong>of</strong> angina involves clinical assessment,laboratory tests, and specific cardiac investigati<strong>on</strong>s.Clinical assessment related to diagnosis and basic laboratoryinvestigati<strong>on</strong>s are dealt with in this secti<strong>on</strong>. Cardiac specificinvestigati<strong>on</strong>s may be n<strong>on</strong>-invasive or invasive and may beused to c<strong>on</strong>firm <strong>the</strong> diagnosis <strong>of</strong> ischaemia in patients withsuspected stable angina, to identify or exclude associatedc<strong>on</strong>diti<strong>on</strong>s or precipitating factors, for risk stratificati<strong>on</strong>,and to evaluate <strong>the</strong> efficacy <strong>of</strong> treatment. Some should beused routinely in all patients; o<strong>the</strong>rs provide redundantinformati<strong>on</strong> except in particular circumstances; someshould be easily available to cardiologists and generalphysicians, yet o<strong>the</strong>rs may be c<strong>on</strong>sidered as tools forresearch. In practice, diagnostic and prognostic assessmentsare c<strong>on</strong>ducted in tandem ra<strong>the</strong>r than separately, and many<strong>of</strong> <strong>the</strong> investigati<strong>on</strong>s used for diagnosis also <strong>of</strong>fer prognosticinformati<strong>on</strong>. For <strong>the</strong> purposes <strong>of</strong> descripti<strong>on</strong> and presentati<strong>on</strong><strong>of</strong> <strong>the</strong> evidence, <strong>the</strong> individual investigative techniquesare discussed subsequently with recommendati<strong>on</strong>sfor diagnosis. Specific cardiac investigati<strong>on</strong>s routinely usedfor risk stratificati<strong>on</strong> purposes are discussed separately in<strong>the</strong> following secti<strong>on</strong>.Symptoms and signsA careful history remains <strong>the</strong> cornerst<strong>on</strong>e <strong>of</strong> <strong>the</strong> diagnosis <strong>of</strong>angina pectoris. In <strong>the</strong> majority <strong>of</strong> cases, it is possible tomake a c<strong>on</strong>fident diagnosis <strong>on</strong> <strong>the</strong> basis <strong>of</strong> <strong>the</strong> historyal<strong>on</strong>e, although physical examinati<strong>on</strong> and objective testsare necessary to c<strong>on</strong>firm <strong>the</strong> diagnosis and assess <strong>the</strong>severity <strong>of</strong> underlying disease.The characteristics <strong>of</strong> discomfort related to myocardialischaemia (angina pectoris) have been extensively describedand may be divided into four categories, locati<strong>on</strong>, character,durati<strong>on</strong>, and relati<strong>on</strong> to exerti<strong>on</strong> and o<strong>the</strong>r exacerbating orrelieving factors. The discomfort caused by myocardialischaemia is usually located in <strong>the</strong> chest, near <strong>the</strong>sternum, but may be felt anywhere from <strong>the</strong> epigastriumto <strong>the</strong> lower jaw or teeth, between <strong>the</strong> shoulder blades orin ei<strong>the</strong>r arm to <strong>the</strong> wrist and fingers. The discomfort isusually described as pressure, tightness, or heaviness, sometimesstrangling, c<strong>on</strong>stricting, or burning. The severity <strong>of</strong><strong>the</strong> discomfort varies greatly and is not related to <strong>the</strong> severity<strong>of</strong> <strong>the</strong> underlying cor<strong>on</strong>ary disease. Shortness <strong>of</strong> breathmay accompany angina, and chest discomfort may be alsobe accompanied by less specific symptoms such as fatigueor faintness, nausea, burping, restlessness, or a sense <strong>of</strong>impending doom.The durati<strong>on</strong> <strong>of</strong> <strong>the</strong> discomfort is brief, no more than 10 minin <strong>the</strong> majority <strong>of</strong> cases, and more comm<strong>on</strong>ly even minutesless. An important characteristic is <strong>the</strong> relati<strong>on</strong> to exercise,specific activities, or emoti<strong>on</strong>al stress. Symptoms classicallydeteriorate with increased levels <strong>of</strong> exerti<strong>on</strong>, such aswalking up an incline, or against a breeze and rapidly disappearwithin a few minutes, when <strong>the</strong>se causal factors abate.Exacerbati<strong>on</strong>s <strong>of</strong> symptoms after a heavy meal or first thingin <strong>the</strong> morning are classical features <strong>of</strong> angina. Buccal or sublingualnitrates rapidly relieve angina, and a similar rapidresp<strong>on</strong>se may be observed with chewing nifedipine capsules.N<strong>on</strong>-anginal pain lacks <strong>the</strong> characteristic qualitiesdescribed, may involve <strong>on</strong>ly a small porti<strong>on</strong> <strong>of</strong> <strong>the</strong> left hemithorax,and last for several hours or even days. It is usuallynot relieved by nitroglycerin (although it may be in <strong>the</strong> case<strong>of</strong> oesophageal spasm) and may be provoked by palpati<strong>on</strong>.N<strong>on</strong>cardiac causes <strong>of</strong> pain should be evaluated in such cases.Definiti<strong>on</strong>s <strong>of</strong> typical and atypical angina have beenpreviously published, 73 summarized <strong>on</strong> Table 2. It isTable 2Clinical classificati<strong>on</strong> <strong>of</strong> chest painTypical angina (definite)Atypical angina (probable)N<strong>on</strong>-cardiac chest painMeets three <strong>of</strong> <strong>the</strong> followingcharacteristics† Substernal chest discomfort <strong>of</strong>characteristic qualityand durati<strong>on</strong>† Provoked by exerti<strong>on</strong> oremoti<strong>on</strong>al stress† Relieved by rest and/or GTNMeets two <strong>of</strong> <strong>the</strong>se characteristicsMeets <strong>on</strong>e or n<strong>on</strong>e <strong>of</strong><strong>the</strong> characteristics
ESC <str<strong>on</strong>g>Guidelines</str<strong>on</strong>g> 7important when taking <strong>the</strong> history to identify those patientswith unstable angina, which may be associated with plaquerupture, who are at significantly higher risk <strong>of</strong> an acutecor<strong>on</strong>ary event in <strong>the</strong> short-term. Unstable angina maypresent in <strong>on</strong>e <strong>of</strong> <strong>the</strong> three ways: (i) as rest angina, i.e.pain <strong>of</strong> characteristic nature and locati<strong>on</strong>, but occurring atrest and for prol<strong>on</strong>ged periods, up to 20 min; (ii) rapidlyincreasing or crescendo angina, i.e. previously stableangina, which progressively increases in severity and intensityand at lower threshold over a short period, 4 weeks orless; or (iii) new <strong>on</strong>set angina, i.e. recent <strong>on</strong>set <strong>of</strong> severeangina, such that <strong>the</strong> patient experiences marked limitati<strong>on</strong><strong>of</strong> ordinary activity within 2 m<strong>on</strong>ths <strong>of</strong> initial presentati<strong>on</strong>.The investigati<strong>on</strong> and management <strong>of</strong> suspected unstableangina is dealt with in guidelines for <strong>the</strong> management <strong>of</strong> ACS.For patients with stable angina, it is also useful to classify<strong>the</strong> severity <strong>of</strong> symptoms using a grading system such as that<strong>of</strong> <strong>the</strong> Canadian <strong>Cardio</strong>vascular Society Classificati<strong>on</strong>(Table 3). This is useful in determining <strong>the</strong> functi<strong>on</strong>al impairment<strong>of</strong> <strong>the</strong> patient and quantifying resp<strong>on</strong>se to <strong>the</strong>rapy.The Canadian <strong>Cardio</strong>vascular Society Classificati<strong>on</strong> 74 iswidely used as a grading system for angina to quantify <strong>the</strong>threshold at which symptoms occur in relati<strong>on</strong> to physicalactivities. Alternative classificati<strong>on</strong> systems such as DukeSpecific Activity Index 75 and Seattle angina questi<strong>on</strong>naire 76may also be used in determining <strong>the</strong> functi<strong>on</strong>al impairment<strong>of</strong> <strong>the</strong> patient and quantifying resp<strong>on</strong>se to <strong>the</strong>rapy and may<strong>of</strong>fer superior prognostic capability. 77Physical examinati<strong>on</strong> <strong>of</strong> a patient with (suspected) anginapectoris is important to assess <strong>the</strong> presence <strong>of</strong> hypertensi<strong>on</strong>,valvular heart disease, or hypertrophic obstructive cardiomyopathy.Physical examinati<strong>on</strong> should include assessment<strong>of</strong> body-mass index (BMI) and waist circumference to assistevaluati<strong>on</strong> <strong>of</strong> <strong>the</strong> metabolic syndrome, 78,79 evidence <strong>of</strong>n<strong>on</strong>-cor<strong>on</strong>ary vascular disease which may be asymptomatic,and o<strong>the</strong>r signs <strong>of</strong> comorbid c<strong>on</strong>diti<strong>on</strong>s. However, <strong>the</strong>re areno specific signs in angina pectoris. During or immediatelyafter an episode <strong>of</strong> myocardial ischaemia, a third or fourthheart sound may be heard and mitral insufficiency mayalso be apparent during ischaemia. Such signs are,however, elusive and n<strong>on</strong>-specific.Table 3 Classificati<strong>on</strong> <strong>of</strong> angina severity according to <strong>the</strong>Canadian <strong>Cardio</strong>vascular SocietyClassClass IClass IIClass IIIClass IVLevel <strong>of</strong> symptoms‘Ordinary activity does not cause angina’<strong>Angina</strong> with strenuous or rapidor prol<strong>on</strong>ged exerti<strong>on</strong> <strong>on</strong>ly‘Slight limitati<strong>on</strong> <strong>of</strong> ordinary activity’<strong>Angina</strong> <strong>on</strong> walking or climbing stairs rapidly,walking uphill or exerti<strong>on</strong> after meals, incold wea<strong>the</strong>r, when under emoti<strong>on</strong>al stress,or <strong>on</strong>ly during <strong>the</strong> first few hours after awakening‘Marked limitati<strong>on</strong> <strong>of</strong> ordinary physical activity’<strong>Angina</strong> <strong>on</strong> walking <strong>on</strong>e or two blocks a <strong>on</strong> <strong>the</strong> levelor <strong>on</strong>e flight <strong>of</strong> stairs at a normal pace undernormal c<strong>on</strong>diti<strong>on</strong>s‘Inability to carry out any physical activitywithout discomfort’ or ‘angina at rest’a Equivalent to 100–200 m.Laboratory testsLaboratory investigati<strong>on</strong>s may be loosely grouped into thosethat provide informati<strong>on</strong> related to possible causes <strong>of</strong>ischaemia, those that may be used to establish cardiovascularrisk factors and associated c<strong>on</strong>diti<strong>on</strong>s, and those thatmay be used to determine prognosis. Some laboratory investigati<strong>on</strong>sare used for more than <strong>on</strong>e <strong>of</strong> <strong>the</strong>se purposes andmay be applied routinely in all patients, whereas o<strong>the</strong>rinvestigati<strong>on</strong>s should be reserved for use where clinicalhistory and/or examinati<strong>on</strong> indicates a particular need for<strong>the</strong>ir applicati<strong>on</strong>.Haemoglobin and, where <strong>the</strong>re is clinical suspici<strong>on</strong> <strong>of</strong> athyroid disorder, thyroid horm<strong>on</strong>es provide informati<strong>on</strong>related to possible causes <strong>of</strong> ischaemia. The full bloodcount incorporating total white cell count as well as haemoglobinmay also add prognostic informati<strong>on</strong>. 80 If <strong>the</strong>re isclinical suspici<strong>on</strong> <strong>of</strong> instability, biochemical markers <strong>of</strong> myocardialdamage such as trop<strong>on</strong>in or CKMB (creatine kinasemyocardial band), measured by mass assay, should beemployed to exclude myocardial injury. If <strong>the</strong>se markersare elevated, management should c<strong>on</strong>tinue as for an ACSra<strong>the</strong>r than stable angina. After initial assessment, <strong>the</strong>setests are not recommended as routine investigati<strong>on</strong>sduring each subsequent evaluati<strong>on</strong>.Fasting plasma glucose 60,61,63,64,81,82,83,84 and fasting lipidpr<strong>of</strong>ile including total cholesterol (TC), high density lipoprotein(HDL) cholesterol, and low density lipoprotein(LDL) cholesterol, 55–58 and triglycerides 54,85 should be evaluatedin all patients with suspected ischaemic disease,including stable angina, to establish <strong>the</strong> patient’s riskpr<strong>of</strong>ile and ascertain <strong>the</strong> need for treatment. Lipid pr<strong>of</strong>ileand glycaemic status should be re-assessed periodically todetermine efficacy <strong>of</strong> treatment and in n<strong>on</strong>-diabeticpatients to detect new development <strong>of</strong> diabetes. There isno evidence to support recommendati<strong>on</strong>s for how regularlyreassessment should take place. C<strong>on</strong>sensus suggests annualmeasurement. Patients with very high levels <strong>of</strong> lipids, inwhom <strong>the</strong> progress <strong>of</strong> any interventi<strong>on</strong> needs to be m<strong>on</strong>itored,should have measurements more frequently.Patients with diabetes should be managed accordingly.Serum creatinine is a simple but crude method to evaluaterenal functi<strong>on</strong>. Renal dysfuncti<strong>on</strong> may occur due to associatedcomorbidity 86–91 such as hypertensi<strong>on</strong>, diabetes orrenovascular disease and has a negative impact <strong>on</strong> prognosisin patients with CVD, 92,93 giving good grounds for measurementat initial evaluati<strong>on</strong> in all patients with suspectedangina. The Cockcr<strong>of</strong>t–Gault formula 94 may be used toestimate creatinine clearance based <strong>on</strong> age, sex, weight,and serum creatinine. The comm<strong>on</strong>ly used formula is asfollows: ((140—age (years)) (actual weight (kg)))/(72 serum creatinine (mg/dL)), with multiplicati<strong>on</strong> by a factor<strong>of</strong> 0.85 if female.In additi<strong>on</strong> to <strong>the</strong> well-recognized associati<strong>on</strong> betweenadverse cardiovascular outcome and diabetes, elevati<strong>on</strong>s<strong>of</strong> fasting or post-glucose challenge glycaemia have alsobeen shown to predict adverse outcome in stable cor<strong>on</strong>arydisease independently <strong>of</strong> c<strong>on</strong>venti<strong>on</strong>al risk factors. 95–101Although HbAIc predicts outcome in <strong>the</strong> general populati<strong>on</strong>,<strong>the</strong>re is less data in those with CAD. 101,102 Obesity, and inparticular evidence <strong>of</strong> <strong>the</strong> metabolic syndrome, is predictive<strong>of</strong> adverse cardiovascular outcome in patients with establisheddisease as well as asymptomatic populati<strong>on</strong>s. 78,79,103The presence <strong>of</strong> <strong>the</strong> metabolic syndrome can be determined
8 ESC <str<strong>on</strong>g>Guidelines</str<strong>on</strong>g>from assessment <strong>of</strong> waist circumference (or BMI), bloodpressure, HDL, triglycerides, and fasting glucose levelsand <strong>of</strong>fers additi<strong>on</strong>al prognostic informati<strong>on</strong> to thatobtained from c<strong>on</strong>venti<strong>on</strong>al Framingham risk scores 104without major additi<strong>on</strong>al cost in terms <strong>of</strong> laboratoryinvestigati<strong>on</strong>.Fur<strong>the</strong>r laboratory testing, including cholesterol subfracti<strong>on</strong>s(ApoA and ApoB) 105,106 homocysteine, 107,108 lipoprotein(a) (Lpa), haemostatic abnormalities, 109–112 and markers <strong>of</strong>inflammati<strong>on</strong> such as hs-C-reactive protein, 56,113,114 havebeen <strong>the</strong> subject <strong>of</strong> much interest as methods to improvecurrent risk predicti<strong>on</strong>. 113,115 However, markers <strong>of</strong> inflammati<strong>on</strong>fluctuate over time and may not be a reliable estimator<strong>of</strong> risk in <strong>the</strong> l<strong>on</strong>ger term. 116 More recently, NT-BNPhas been shown to be an important predictor <strong>of</strong> l<strong>on</strong>g-termmortality independent <strong>of</strong> age, ventricular ejecti<strong>on</strong> fracti<strong>on</strong>(EF), and c<strong>on</strong>venti<strong>on</strong>al risk factors. 117 As yet, <strong>the</strong>re isinadequate informati<strong>on</strong> regarding how modificati<strong>on</strong> <strong>of</strong><strong>the</strong>se biochemical indices can significantly improve <strong>on</strong>current treatment strategies to recommend <strong>the</strong>ir use in allpatients, particularly given <strong>the</strong> c<strong>on</strong>straints <strong>of</strong> cost and availability.Never<strong>the</strong>less, <strong>the</strong>se measurements have a role inselected patients, for example, testing for haemostaticabnormalities in those with prior MI without c<strong>on</strong>venti<strong>on</strong>alrisk factors, 118 or a str<strong>on</strong>g family history <strong>of</strong> cor<strong>on</strong>arydisease, or where resources are not limited. Fur<strong>the</strong>rresearch into <strong>the</strong>ir use is welcomed. The use <strong>of</strong> glycatedhaemoglobin or resp<strong>on</strong>se to oral glucose load in additi<strong>on</strong>to a single measurement <strong>of</strong> fasting plasma glucose havealso been shown to improve detecti<strong>on</strong> <strong>of</strong> glycaemic abnormalities,but as yet <strong>the</strong>re is insufficient evidence to recommendthis strategy in all patients with chest pain. 119,120This may be a useful method <strong>of</strong> detecting glycaemicabnormalities in selected patients particularly at high riskfor <strong>the</strong>ir development.Recommendati<strong>on</strong>s for laboratory investigati<strong>on</strong> in initialassessment <strong>of</strong> stable anginaClass I (in all patients)(1) Fasting lipid pr<strong>of</strong>ile, including TC, LDL, HDL, andtriglycerides (level <strong>of</strong> evidence B)(2) Fasting glucose (level <strong>of</strong> evidence B)(3) Full blood count including Hb and white cell count(level <strong>of</strong> evidence B)(4) Creatinine (level <strong>of</strong> evidence C)Class I (if specifically indicated <strong>on</strong> <strong>the</strong> basis <strong>of</strong> clinicalevaluati<strong>on</strong>)(1) Markers <strong>of</strong> myocardial damage if evaluati<strong>on</strong> suggestsclinical instability or ACS (level <strong>of</strong> evidence A)(2) Thyroid functi<strong>on</strong> if clinically indicated (level <strong>of</strong>evidence C)Class IIa(1) Oral glucose tolerance test (level <strong>of</strong> evidence B)Class IIb(1) Hs-C-reactive protein (level <strong>of</strong> evidence B)(2) Lipoprotein a, ApoA, and ApoB (level <strong>of</strong> evidence B)(3) Homocysteine (level <strong>of</strong> evidence B)(4) HbA1c (level <strong>of</strong> evidence B)(5) NT-BNP (level <strong>of</strong> evidence B)Recommendati<strong>on</strong>s for blood tests for routinereassessment in patients with chr<strong>on</strong>ic stable anginaClass IIa(1) Fasting lipid pr<strong>of</strong>ile and fasting glucose <strong>on</strong> an annualbasis (level <strong>of</strong> evidence C)Chest X-rayA chest X-ray (CXR) is frequently used in <strong>the</strong> assessment<strong>of</strong> patients with suspected heart disease. However, instable angina, <strong>the</strong> CXR does not provide specific informati<strong>on</strong>for diagnosis or risk stratificati<strong>on</strong>. The test should berequested <strong>on</strong>ly in patients with suspected heartfailure, 121,122 valvular disease, or pulm<strong>on</strong>ary disease.Thepresence <strong>of</strong> cardiomegaly, pulm<strong>on</strong>ary c<strong>on</strong>gesti<strong>on</strong>, atrialenlargement, and cardiac calcificati<strong>on</strong>s has been relatedto impaired prognosis. 123–128Recommendati<strong>on</strong>s for CXR for initial diagnosticassessment <strong>of</strong> anginaClass I(1) CXR in patients with suspected heart failure (level <strong>of</strong>evidence C)(2) CXR in patients with clinical evidence <strong>of</strong> significantpulm<strong>on</strong>ary disease (level <strong>of</strong> evidence B)N<strong>on</strong>-invasive cardiac investigati<strong>on</strong>sThis secti<strong>on</strong> will describe investigati<strong>on</strong>s used in <strong>the</strong> assessment<strong>of</strong> angina and c<strong>on</strong>centrate <strong>on</strong> recommendati<strong>on</strong>s for<strong>the</strong>ir use in diagnosis and evaluati<strong>on</strong> <strong>of</strong> efficacy <strong>of</strong>treatment, and recommendati<strong>on</strong>s for risk stratificati<strong>on</strong> willbe dealt with in <strong>the</strong> following secti<strong>on</strong>. As <strong>the</strong>re are few randomizedtrials assessing health outcomes for diagnostictests, <strong>the</strong> available evidence has been ranked according toevidence from n<strong>on</strong>-randomized studies or meta-analyses <strong>of</strong><strong>the</strong>se studies.Resting ECGAll patients with suspected angina pectoris based <strong>on</strong> symptomsshould have a resting 12-lead ECG recorded. It shouldbe emphasized that a normal resting ECG is not uncomm<strong>on</strong>even in patients with severe angina and does not exclude<strong>the</strong> diagnosis <strong>of</strong> ischaemia. However, <strong>the</strong> resting ECG mayshow signs <strong>of</strong> CAD such as previous MI or an abnormalrepolarizati<strong>on</strong> pattern. The ECG may assist in clarifying<strong>the</strong> differential diagnosis if taken in <strong>the</strong> presence <strong>of</strong> pain,allowing detecti<strong>on</strong> <strong>of</strong> dynamic ST-segment changes in<strong>the</strong> presence <strong>of</strong> ischaemia, 129,130 or by identifying features<strong>of</strong> pericardial disease. An ECG during pain may beparticularly useful if vasospasm is suspected. The ECG mayalso show o<strong>the</strong>r abnormalities such as left ventricularhypertrophy (LVH), left bundle branch block (LBBB),pre-excitati<strong>on</strong>, arrhythmias, or c<strong>on</strong>ducti<strong>on</strong> defects.Such informati<strong>on</strong> may be helpful in defining <strong>the</strong>mechanisms resp<strong>on</strong>sible for chest pain, in selectingappropriate fur<strong>the</strong>r investigati<strong>on</strong>, or in tailoring individualpatient treatment. The resting ECG also has an importantrole in risk stratificati<strong>on</strong>, as outlined in <strong>the</strong> RiskStratificati<strong>on</strong> secti<strong>on</strong>. 131–133There is little direct evidence to support routinely repeating<strong>the</strong> resting ECG at frequent intervals unless to obtain anECG during pain or if <strong>the</strong>re has been a change in functi<strong>on</strong>alclass.
ESC <str<strong>on</strong>g>Guidelines</str<strong>on</strong>g> 9Recommendati<strong>on</strong>s for resting ECG for initial diagnosticassessment <strong>of</strong> anginaClass I (in all patients)(1) Resting ECG while pain free (level <strong>of</strong> evidence C)(2) Resting ECG during episode <strong>of</strong> pain (if possible) (level <strong>of</strong>evidence B)Recommendati<strong>on</strong>s for resting ECG for routine reassessmentin patients with chr<strong>on</strong>ic stable anginaClass IIb(1) Routine periodic ECG in <strong>the</strong> absence <strong>of</strong> clinical change(level <strong>of</strong> evidence C)ECG stress testingExercise ECG is more sensitive and specific than <strong>the</strong> restingECG for detecting myocardial ischaemia 134,135 and forreas<strong>on</strong>s <strong>of</strong> availability and cost is <strong>the</strong> test <strong>of</strong> choice to identifyinducible ischaemia in <strong>the</strong> majority <strong>of</strong> patients withsuspected stable angina. There are numerous reportsand meta-analyses <strong>of</strong> <strong>the</strong> performance <strong>of</strong> exercise ECGfor <strong>the</strong> diagnosis <strong>of</strong> cor<strong>on</strong>ary disease. 136–139 Using exerciseST-depressi<strong>on</strong> ,0.1 mV or 1 mm to define a positive test,<strong>the</strong> reported sensitivity and specificity for <strong>the</strong> detecti<strong>on</strong> <strong>of</strong>significant cor<strong>on</strong>ary disease range between 23–100% (mean68%) and 17–100% (mean 77%), respectively. Excludingpatients with prior MI, <strong>the</strong> mean sensitivity was 67% andspecificity 72%, and restricting analysis to those studiesdesigned to avoid work-up bias, sensitivity was 50% and specificity90%. 140 The majority <strong>of</strong> reports are <strong>of</strong> studies where <strong>the</strong>populati<strong>on</strong> tested did not have significant ECG abnormalitiesat baseline and were not <strong>on</strong> antianginal <strong>the</strong>rapy or were withdrawnfrom antianginal <strong>the</strong>rapy for <strong>the</strong> purposes <strong>of</strong> <strong>the</strong> test.Exercise ECG testing is not <strong>of</strong> diagnostic value in <strong>the</strong> presence<strong>of</strong> LBBB, paced rhythm, and Wolff–Parkins<strong>on</strong>–White (WPW)syndrome, in which cases, <strong>the</strong> ECG changes cannot be evaluated.Additi<strong>on</strong>ally, false-positive results are more frequent inpatients with abnormal resting ECG in <strong>the</strong> presence <strong>of</strong> LVH,electrolyte imbalance, intraventricular c<strong>on</strong>ducti<strong>on</strong> abnormalities,and use <strong>of</strong> digitalis. Exercise ECG testing is also less sensitiveand specific in women. 141Interpretati<strong>on</strong> <strong>of</strong> exercise ECG findings requires a Bayesianapproach to diagnosis. This approach uses clinicians’pre-test estimates <strong>of</strong> disease al<strong>on</strong>g with <strong>the</strong> results <strong>of</strong> diagnostictests to generate individualized post-test diseaseprobabilities for a given patient. The pre-test probabilityis influenced by <strong>the</strong> prevalence <strong>of</strong> <strong>the</strong> disease in <strong>the</strong> populati<strong>on</strong>studied, as well as clinical features in an individual. 142Therefore, for <strong>the</strong> detecti<strong>on</strong> <strong>of</strong> cor<strong>on</strong>ary disease, <strong>the</strong>pre-test probability is influenced by age and gender andfur<strong>the</strong>r modified by <strong>the</strong> nature <strong>of</strong> symptoms at an individualpatient level before <strong>the</strong> results <strong>of</strong> exercise testing are usedto determine <strong>the</strong> posterior or post-test probability, asoutlined in Table 4.In populati<strong>on</strong>s with a low prevalence <strong>of</strong> ischaemic heartdisease <strong>the</strong> proporti<strong>on</strong> <strong>of</strong> false-positive tests will be highwhen compared with a populati<strong>on</strong> with a high pre test probability<strong>of</strong> disease. C<strong>on</strong>versely, in male patients with severeeffort angina, with clear ECG changes during pain, <strong>the</strong>pretest probability <strong>of</strong> significant cor<strong>on</strong>ary disease is high(.90%), and in such cases, <strong>the</strong> exercise test will not <strong>of</strong>feradditi<strong>on</strong>al informati<strong>on</strong> for <strong>the</strong> diagnosis, although it mayadd prognostic informati<strong>on</strong>.A fur<strong>the</strong>r factor that may influence <strong>the</strong> performance <strong>of</strong><strong>the</strong> exercise ECG as a diagnostic tool is <strong>the</strong> definiti<strong>on</strong> <strong>of</strong> apositive test. ECG changes associated with myocardialischaemia include horiz<strong>on</strong>tal or down-sloping ST-segmentdepressi<strong>on</strong> or elevati<strong>on</strong> [1 mm (0.1 mV) for 60–80 msafter <strong>the</strong> end <strong>of</strong> <strong>the</strong> QRS complex], especially when <strong>the</strong>sechanges are accompanied by chest pain suggestive <strong>of</strong>angina, occur at a low workload during <strong>the</strong> early stages <strong>of</strong>exercise and persist for more than 3 min after exercise.Increasing <strong>the</strong> threshold for a positive test, for example,to 2 mm (0.2 mV) ST-depressi<strong>on</strong>, will increase specificityat <strong>the</strong> expense <strong>of</strong> sensitivity. A fall in systolic pressure orlack <strong>of</strong> increase <strong>of</strong> blood pressure during exercise and <strong>the</strong>appearance <strong>of</strong> a systolic murmur <strong>of</strong> mitral regurgitati<strong>on</strong> orventricular arrhythmias during exercise reflect impaired LVfuncti<strong>on</strong> and increase <strong>the</strong> probability <strong>of</strong> severe myocardialischaemia and severe CAD. In assessing <strong>the</strong> significance <strong>of</strong><strong>the</strong> test, not <strong>on</strong>ly <strong>the</strong> ECG changes but also <strong>the</strong> workload,heart rate increase and blood pressure resp<strong>on</strong>se, heartrate recovery after exercise, and <strong>the</strong> clinical c<strong>on</strong>textshould be c<strong>on</strong>sidered. 143 It has been suggested that evaluatingST changes in relati<strong>on</strong> to heart rate improves reliability<strong>of</strong> diagnosis 144 but this may not be so in symptomaticpopulati<strong>on</strong>s. 145–147An exercise test should be carried out <strong>on</strong>ly after carefulclinical evaluati<strong>on</strong> <strong>of</strong> symptoms and a physical examinati<strong>on</strong>including resting ECG. 135,140 Complicati<strong>on</strong>s during exercisetesting are few but severe arrhythmias and even suddendeath can occur. Death and MI occur at a rate <strong>of</strong> less thanor equal to <strong>on</strong>e per 2500 tests. 148 Accordingly, exercisetesting should <strong>on</strong>ly be performed under careful m<strong>on</strong>itoringin <strong>the</strong> appropriate setting. A physician should be presentor immediately available to m<strong>on</strong>itor <strong>the</strong> test. The ECGshould be c<strong>on</strong>tinuously recorded with a printout at preselectedintervals, mostly at each minute during exercise,and 2–10 min <strong>of</strong> recovery after exercise. Exercise ECGshould not be carried out routinely in patients with knownsevere aortic stenosis or hypertrophic cardiomyopathy,although carefully supervised exercise testing may be usedto assess functi<strong>on</strong>al capacity in selected individuals with<strong>the</strong>se c<strong>on</strong>diti<strong>on</strong>s.Ei<strong>the</strong>r <strong>the</strong> Bruce protocol or <strong>on</strong>e <strong>of</strong> its modificati<strong>on</strong>s <strong>on</strong> atreadmill or a bicycle ergometer can be employed. Mostc<strong>on</strong>sist <strong>of</strong> several stages <strong>of</strong> exercise, increasing in intensity,ei<strong>the</strong>r speed, slope, or resistance or a combinati<strong>on</strong> <strong>of</strong> <strong>the</strong>sefactors, at fixed intervals, to test functi<strong>on</strong>al capacity. It isc<strong>on</strong>venient to express oxygen uptake in multiples <strong>of</strong>resting requirements. One metabolic equivalent (MET) is aunit <strong>of</strong> sitting/resting oxygen uptake [3.5 mL <strong>of</strong> O 2 per kilogram<strong>of</strong> body weight per minute (mL/kg/min)]. 149 Bicycleworkload is frequently described in terms <strong>of</strong> watts (W).Increments are <strong>of</strong> 20 W per 1 min stage starting from 20 to50 W, but increments may be reduced to 10 W per stage inpatients with heart failure or severe angina. Correlati<strong>on</strong>between METs achieved and workload in watts varies withnumerous patient-specific and envir<strong>on</strong>mental factors. 135,150The reas<strong>on</strong> for stopping <strong>the</strong> test and <strong>the</strong> symptoms at thattime, including <strong>the</strong>ir severity, should be recorded. Time to<strong>the</strong> <strong>on</strong>set <strong>of</strong> ECG changes and/or symptoms, <strong>the</strong> overallexercise time, <strong>the</strong> blood pressure and heart rate resp<strong>on</strong>se,<strong>the</strong> extent and severity <strong>of</strong> ECG changes, and <strong>the</strong> postexerciserecovery rate <strong>of</strong> ECG changes and heart rateshould also be assessed. For repeated exercise tests, <strong>the</strong>
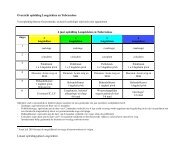
10 ESC <str<strong>on</strong>g>Guidelines</str<strong>on</strong>g>Table 4 Probability <strong>of</strong> cor<strong>on</strong>ary disease in symptomatic patients based <strong>on</strong> (a) age, gender, and symptom classificati<strong>on</strong> and (b) modified byexercise test results(a) Pretest likelihood <strong>of</strong> CAD in symptomatic patients according to age and sexAge (years) Typical angina Atypical angina N<strong>on</strong>-anginal chest painMale Female Male Female Male Female30–39 69.7 + 3.2 25.8 + 6.6 21.8 + 2.4 4.2 + 1.3 5.2 + 0.8 0.8 + 0.340–49 87.3 + 1.0 55.2 + 6.5 46.1 + 1.8 13.3 + 2.9 14.1 + 1.3 2.8 + 0.750–59 92.0 + 0.6 79.4 + 2.4 58.9 + 1.5 32.4 + 3.0 21.5 + 1.7 8.4 + 1.260–69 94.3 + 0.4 90.1 + 1.0 67.1 + 1.3 54.4 + 2.4 28.1 + 1.9 18.6 + 1.9(b) CAD post-test likelihood (%) based <strong>on</strong> age, sex, symptom classificati<strong>on</strong> and exercise-induced electrocardiographicST-segment depressi<strong>on</strong>Age (years) ST-depressi<strong>on</strong> (mV) Typical angina Atypical angina N<strong>on</strong>-anginal chest pain AsymptomaticMale Female Male Female Male Female Male Female30–39 0.00–0.04 25 7 6 1 1 ,1 ,1 ,10.05–0.09 68 24 21 4 5 1 2 40.00–0.14 83 42 38 9 10 2 4 ,10.00–0.19 91 59 55 15 19 3 7 10.00–0.24 96 79 76 33 39 8 18 3.0.25 99 93 92 63 68 24 43 1140–49 0.00–0.04 61 22 16 3 4 1 1 ,10.00–0.09 86 53 44 12 13 3 5 10.00–0.14 94 72 64 25 26 6 11 20.00–0.19 97 84 78 39 41 11 20 40.00–0.24 99 93 91 63 65 24 39 10.0.25 .99 98 97 86 87 53 69 2850–59 0.00–0.04 73 47 25 10 6 2 2 10.00–0.09 91 78 57 31 20 8 9 30.00–0.14 96 89 75 50 37 16 19 70.00–0.19 98 94 86 67 53 28 31 120.00–0.24 99 98 94 84 75 50 54 27.0.25 .99 99 98 95 91 78 81 5660–69 0.00–0.04 79 69 32 21 8 5 3 20.00–0.09 94 90 65 52 26 17 11 70.00–0.14 97 95 81 72 45 33 23 150.00–0.19 99 98 89 83 62 49 37 250.00–0.24 99 99 96 93 81 72 61 47.0.25 .99 99 99 98 94 90 85 76use <strong>of</strong> <strong>the</strong> Borg scale or similar method <strong>of</strong> quantifyingsymptoms may be used to allow comparis<strong>on</strong>s. 151 Reas<strong>on</strong>sto terminate an exercise test are listed in Table 5.In some patients, <strong>the</strong> exercise ECG may be n<strong>on</strong>c<strong>on</strong>clusive,for example, if at least 85% <strong>of</strong> maximum heartrate is not achieved in <strong>the</strong> absence <strong>of</strong> symptoms or ischaemia,if exercise is limited by orthopaedic or o<strong>the</strong>r n<strong>on</strong>cardiacproblems, or if ECG changes are equivocal. Unless<strong>the</strong> patient has a very low pre-test probability (,10% probability)<strong>of</strong> disease, an inc<strong>on</strong>clusive exercise test should befollowed by an alternative n<strong>on</strong>-invasive diagnostic test.Fur<strong>the</strong>rmore, a ’normal’ test in patients taking antiischaemicdrugs does not rule out significant cor<strong>on</strong>arydisease. 135 For diagnostic purposes, <strong>the</strong> test should be c<strong>on</strong>ductedin patients not taking anti-ischaemic drugs, althoughthis may not always be possible or c<strong>on</strong>sidered safe.Exercise stress testing can also be useful for prognosticstratificati<strong>on</strong>, 152 to evaluate <strong>the</strong> efficacy <strong>of</strong> treatmentafter c<strong>on</strong>trol <strong>of</strong> angina with medical treatment or revascularizati<strong>on</strong>or to assist prescripti<strong>on</strong> <strong>of</strong> exercise afterc<strong>on</strong>trol <strong>of</strong> symptoms, but <strong>the</strong> effect <strong>of</strong> routine periodicalexercise testing <strong>on</strong> patient outcomes has not been formallyevaluated.Recommendati<strong>on</strong>s for exercise ECG for initialdiagnostic assessment <strong>of</strong> anginaClass I(1) Patients with symptoms <strong>of</strong> angina and intermediatepre-test probability <strong>of</strong> cor<strong>on</strong>ary disease based <strong>on</strong> age,gender, and symptoms, unless unable to exercise or displaysECG changes which make ECG n<strong>on</strong>-evaluable(level <strong>of</strong> evidence B)Class IIb(1) Patients with 1 mm ST-depressi<strong>on</strong> <strong>on</strong> resting ECG ortaking digoxin (level <strong>of</strong> evidence B)(2) In patients with low pre-test probability (,10% probability)<strong>of</strong> cor<strong>on</strong>ary disease based <strong>on</strong> age, gender, andsymptoms (level <strong>of</strong> evidence B)
ESC <str<strong>on</strong>g>Guidelines</str<strong>on</strong>g> 11Table 5Reas<strong>on</strong>s to terminate <strong>the</strong> exercise stress testThe exercise stress test is terminated for <strong>on</strong>e <strong>of</strong> <strong>the</strong> followingreas<strong>on</strong>s† Symptom limitati<strong>on</strong>, e.g. pain, fatigue, dyspnoea, andclaudicati<strong>on</strong>† Combinati<strong>on</strong> <strong>of</strong> symptoms such as pain with significantST-changes† Safety reas<strong>on</strong>s such as <strong>the</strong> followingMarked ST-depressi<strong>on</strong> (.2 mm ST-depressi<strong>on</strong> can betaken as a relative indicati<strong>on</strong> for terminati<strong>on</strong> and4 mm as an absolute indicati<strong>on</strong> to stop <strong>the</strong> test)ST-elevati<strong>on</strong> 1 mmSignificant arrhythmiaSustained fall in systolic blood pressure .10 mmHgMarked hypertensi<strong>on</strong> (.250 mmHg systolic or .115 mmHgdiastolic)† Achievement <strong>of</strong> maximum predicted heart rate may also bea reas<strong>on</strong> to terminate <strong>the</strong> test in patients with excellentexercise tolerance who are not tired and at <strong>the</strong> discreti<strong>on</strong><strong>of</strong> <strong>the</strong> supervising physicianRecommendati<strong>on</strong>s for exercise ECG for routinere-assessment in patients with chr<strong>on</strong>ic stable anginaClass IIb(1) Routine periodic exercise ECG in <strong>the</strong> absence <strong>of</strong> clinicalchange (level <strong>of</strong> evidence C)Stress testing in combinati<strong>on</strong> with imagingThe most well established stress imaging techniques areechocardiography and perfusi<strong>on</strong> scintigraphy. Both may beused in combinati<strong>on</strong> with ei<strong>the</strong>r exercise stress or pharmacologicalstress, and many studies have been c<strong>on</strong>ductedevaluating <strong>the</strong>ir use in both prognostic and diagnosticassessment over <strong>the</strong> past two decades or more. Novelstress imaging techniques also include stress MRI, which,for logistical reas<strong>on</strong>s, is most frequently performed usingpharmacological ra<strong>the</strong>r than exercise stress.Stress imaging techniques have several advantages overc<strong>on</strong>venti<strong>on</strong>al exercise ECG testing including superior diagnosticperformance (Table 6) for <strong>the</strong> detecti<strong>on</strong> <strong>of</strong> obstructivecor<strong>on</strong>ary disease, <strong>the</strong> ability to quantify and localizeareas <strong>of</strong> ischaemia, and <strong>the</strong> ability to provide diagnosticinformati<strong>on</strong> in <strong>the</strong> presence <strong>of</strong> resting ECG abnormalitiesor inability <strong>of</strong> <strong>the</strong> patient to exercise. Stress imaging techniquesare <strong>of</strong>ten preferred in patients with previous PCI orcor<strong>on</strong>ary artery bypass grafting (CABG) because <strong>of</strong> itssuperior ability to localize ischaemia. In patients withangiographically c<strong>on</strong>firmed intermediate cor<strong>on</strong>ary lesi<strong>on</strong>s,evidence <strong>of</strong> anatomically appropriate ischaemia is predictive<strong>of</strong> future events, whereas a negative stress imagingtest can be used to define patients with a low cardiac riskwho can be reassured. 153Exercise testing with echocardiography. Exercise stressechocardiography has been developed as an alternative to‘classical’ exercise testing with ECG and as an additi<strong>on</strong>alinvestigati<strong>on</strong> to establish <strong>the</strong> presence or locati<strong>on</strong> andextent <strong>of</strong> myocardial ischaemia during stress. A restingechocardiogram is acquired before a symptom-limitedexercise test is performed, most frequently using a bicycleergometer, with fur<strong>the</strong>r images acquired where possibleTable 6 Summary <strong>of</strong> test characteristics for investigati<strong>on</strong>s usedin <strong>the</strong> diagnosis <strong>of</strong> stable anginaDiagnosis <strong>of</strong> CADSensitivity(%)Specificity(%)Exercise ECG 68 77Exercise echo 80–85 84–86Exercise myocardial perfusi<strong>on</strong> 85–90 70–75Dobutamine stress echo 40–100 62–100Vasodilator stress echo 56–92 87–100Vasodilator stress myocardial perfusi<strong>on</strong> 83–94 64–90during each stage <strong>of</strong> exercise and at peak exercise. Thismay be technically challenging. 154 Reported sensitivitiesand specificities for <strong>the</strong> detecti<strong>on</strong> <strong>of</strong> significant cor<strong>on</strong>arydisease are within a similar range to those described forexercise stress perfusi<strong>on</strong> scintigraphy, sensitivity 53–93%specificity 70–100%, although stress echo tends to be lesssensitive and more specific than stress perfusi<strong>on</strong> scintigraphy.Depending <strong>on</strong> <strong>the</strong> meta-analysis, overall sensitivityand specificity <strong>of</strong> exercise echocardiography are reportedas 80–85 and 84–86%. 155–158 Recent improvements intechnology include improvements in endocardial borderdefiniti<strong>on</strong> with <strong>the</strong> use <strong>of</strong> c<strong>on</strong>trast agents to facilitateidentificati<strong>on</strong> <strong>of</strong> regi<strong>on</strong>al wall moti<strong>on</strong> abnormalities, and<strong>the</strong> use <strong>of</strong> injectable agents to image myocardialperfusi<strong>on</strong>. 159–161 Advances in tissue Doppler and strain rateimaging are even more promising.Tissue Doppler imaging allows regi<strong>on</strong>al quantificati<strong>on</strong> <strong>of</strong>myocardial moti<strong>on</strong> (velocity), and strain and strain rateimaging allow determinati<strong>on</strong> <strong>of</strong> regi<strong>on</strong>al deformati<strong>on</strong>,strain being <strong>the</strong> difference in velocity between adjacentregi<strong>on</strong>s and strain rate being <strong>the</strong> difference per unitlength. Tissue Doppler imaging 162,163 and strain rateimaging 164,165 have improved <strong>the</strong> diagnostic performance<strong>of</strong> stress echocardiography 166 improving <strong>the</strong> capability <strong>of</strong>echocardiography to detect ischaemia earlier in <strong>the</strong> ischaemiccascade. 166,167 Because <strong>of</strong> <strong>the</strong> quantitative nature <strong>of</strong><strong>the</strong> techniques, inter-operator variability and subjectivityin interpretati<strong>on</strong> <strong>of</strong> <strong>the</strong> results are also reduced. Hence,tissue Doppler and strain rate imaging are expected tocomplement current echocardiographic techniques forischaemia detecti<strong>on</strong> and improve <strong>the</strong> accuracy and reproducibility<strong>of</strong> stress echocardiography in <strong>the</strong> broader clinicalsetting. There is also some evidence that tissue Dopplerimaging may improve <strong>the</strong> prognostic utility <strong>of</strong> stressechocardiography. 168Exercise testing with myocardial perfusi<strong>on</strong> scintigraphy.201 Th and 99m Tc radiopharmaceuticals are <strong>the</strong> most comm<strong>on</strong>lyused tracers, employed with single phot<strong>on</strong> emissi<strong>on</strong>computed tomography (SPECT) in associati<strong>on</strong> with asymptom-limited exercise test <strong>on</strong> ei<strong>the</strong>r a bicycle ergometeror a treadmill. Although multiple-view planar images werefirst employed for myocardial perfusi<strong>on</strong> scintigraphy, <strong>the</strong>yhave been largely replaced by SPECT, which is superiorfrom <strong>the</strong> standpoint <strong>of</strong> localizati<strong>on</strong>, quantificati<strong>on</strong>, andimage quality. Regardless <strong>of</strong> <strong>the</strong> radiopharmaceutical used,SPECT perfusi<strong>on</strong> scintigraphy is performed to produce
12 ESC <str<strong>on</strong>g>Guidelines</str<strong>on</strong>g>images <strong>of</strong> regi<strong>on</strong>al tracer uptake that reflect relativeregi<strong>on</strong>al myocardial blood flow. With this technique, myocardialhypoperfusi<strong>on</strong> is characterized by reduced traceruptake during stress in comparis<strong>on</strong> with <strong>the</strong> uptake atrest. Increased uptake <strong>of</strong> myocardial perfusi<strong>on</strong> agent in<strong>the</strong> lung field identifies patients with severe and extensivecor<strong>on</strong>ary artery disease (CAD) 169–172 and stress-induced ventriculardysfuncti<strong>on</strong>. 173 SPECT perfusi<strong>on</strong> provides a moresensitive and specific predicti<strong>on</strong> <strong>of</strong> <strong>the</strong> presence <strong>of</strong> CADthan exercise ECG. Without correcti<strong>on</strong> for referral bias,<strong>the</strong> reported sensitivity <strong>of</strong> exercise scintigraphy has generallyranged from 70–98%, and specificity from 40–90%,with mean values in <strong>the</strong> range <strong>of</strong> 85–90% and 70–75%depending <strong>on</strong> <strong>the</strong> meta-analysis. 157,158,171,174Pharmacological stress testing with imaging techniques.Although <strong>the</strong> use <strong>of</strong> exercise imaging is preferable wherepossible, as it allows for more physiological reproducti<strong>on</strong> <strong>of</strong>ischaemia and assessment <strong>of</strong> symptoms, pharmacologicalstress may also be employed. Pharmacological stress testingwith ei<strong>the</strong>r perfusi<strong>on</strong> scintigraphy or echocardiography isindicated in patients who are unable to exercise adequatelyor may be used as an alternative to exercise stress. Twoapproaches may be used to achieve this: Ei<strong>the</strong>r (i) infusi<strong>on</strong><strong>of</strong> short-acting sympatho-mimetic drugs such as dobutamine,in an incremental dose protocol which increases myocardialoxygen c<strong>on</strong>sumpti<strong>on</strong> and mimics <strong>the</strong> effect <strong>of</strong> physical exercise;or (ii) infusi<strong>on</strong> <strong>of</strong> cor<strong>on</strong>ary vasodilators (e.g. adenosineand dipyridamole) which provide a c<strong>on</strong>trast between regi<strong>on</strong>ssupplied by n<strong>on</strong>-diseased cor<strong>on</strong>ary arteries where perfusi<strong>on</strong>increases, and regi<strong>on</strong>s supplied by haemodynamically significantstenotic cor<strong>on</strong>ary arteries where perfusi<strong>on</strong> will increaseless or even decrease (steal phenomen<strong>on</strong>).In general, pharmacological stress is safe and well toleratedby patients, with major cardiac complicati<strong>on</strong>s (includingsustained VT) occuring every 1500 tests with dipyridamole, or<strong>on</strong>e in every 300 with dobutamine. 156,175–177 Particular caremust be taken to ensure that patients receiving vasodilators(adenosine or dipyridamole) are not already receiving dipyridamolefor antiplatelet or o<strong>the</strong>r purposes, and that caffeineis avoided in <strong>the</strong> 12–24 h preceding <strong>the</strong> study, as it interfereswith <strong>the</strong>ir metabolism. Adenosine may precipitate br<strong>on</strong>chospasmin asthmatic individuals, but in such cases dobutaminemay be used as an alternative stressor. Dobutamine does notprovoke as great an increase in cor<strong>on</strong>ary blood flow asvasodilator stress, which is a limitati<strong>on</strong> for perfusi<strong>on</strong> scintigraphy.Thus, for this technique dobutamine is mostlyreserved for patients who cannot exercise and have ac<strong>on</strong>traindicati<strong>on</strong> to vasodilator stress. 178 The diagnosticperformance <strong>of</strong> pharmacological stress perfusi<strong>on</strong> andpharmacological stress echo are also similar to that <strong>of</strong> exerciseimaging techniques. Reported sensitivity and specificityfor dobutamine stress echo range from 40–100% and62–100%, respectively, and 56–92% and 87–100% for vasodilatorstress. 156,157 Sensitivity and specificity for <strong>the</strong> detecti<strong>on</strong><strong>of</strong> cor<strong>on</strong>ary disease with adenosine SPECT range from83–94% and 64–90%. 157On <strong>the</strong> whole stress echo and stress perfusi<strong>on</strong> scintigraphy,whe<strong>the</strong>r using exercise or pharmacological stress,have very similar applicati<strong>on</strong>s. The choice as to which isemployed depends largely <strong>on</strong> local facilities and expertise.Advantages <strong>of</strong> stress echocardiography over stress perfusi<strong>on</strong>scintigraphy include a higher specificity, <strong>the</strong> possibility <strong>of</strong> amore extensive evaluati<strong>on</strong> <strong>of</strong> <strong>the</strong> cardiac anatomy and functi<strong>on</strong>,and <strong>the</strong> greater availability and lower cost, in additi<strong>on</strong>to being free <strong>of</strong> radiati<strong>on</strong>. However, at least 5–10% <strong>of</strong>patients have an inadequate echo window, and specialtraining in additi<strong>on</strong> to standard echocardiographic trainingis required to correctly perform and interpret stress echocardiograms.Nuclear scintigraphy also requires specialtraining for performance and interpretati<strong>on</strong> <strong>of</strong> <strong>the</strong> tests.The development <strong>of</strong> quantitative echocardiographic techniquessuch as tissue Doppler imaging is a step towardsincreasing <strong>the</strong> inter-observer agreement and reliability <strong>of</strong>stress echo.N<strong>on</strong>-invasive diagnosis <strong>of</strong> CAD in patients with LBBB orwith permanent pacemaker in situ remains challenging forboth stress echocardiography and stress scintigraphic techniques,179,180 although stress perfusi<strong>on</strong> imaging is markedlyless specific in this setting. 181–184 Very poor accuracy isreported for both stress perfusi<strong>on</strong> and stress echocardiographyin patients with ventricular dysfuncti<strong>on</strong> associated withLBBB. 185 Stress echo has also been shown to have prognosticvalue even in <strong>the</strong> setting <strong>of</strong> LBBB. 186Although <strong>the</strong>re is evidence to support superiority <strong>of</strong> stressimaging techniques over exercise ECG in terms <strong>of</strong> diagnosticperformance, <strong>the</strong> costs <strong>of</strong> using a stress imaging test as firstline investigati<strong>on</strong> in all-comers are c<strong>on</strong>siderable. These arenot limited to <strong>the</strong> immediate financial costs <strong>of</strong> <strong>the</strong> individualtest, where some <strong>of</strong> <strong>the</strong> cost effectiveness analyses havebeen favourable in certain settings. 187,188 But o<strong>the</strong>r factorssuch as limited availability <strong>of</strong> testing facilities and expertise,with c<strong>on</strong>sequently increased waiting times for testing <strong>the</strong>majority <strong>of</strong> patients attending <strong>the</strong> evaluati<strong>on</strong> <strong>of</strong> anginamust also be c<strong>on</strong>sidered. The resource redistributi<strong>on</strong> andtraining implicati<strong>on</strong>s <strong>of</strong> ensuring adequate access for allpatients are c<strong>on</strong>siderable, and <strong>the</strong> benefits to be obtainedby a change from exercise ECG to stress imaging in allpatients are not sufficiently great to warrant recommendati<strong>on</strong><strong>of</strong> stress imaging as a universal first line investigati<strong>on</strong>.However, stress imaging has an important role to play inevaluating patients with a low pre-test probability <strong>of</strong>disease, particularly women, 189–192 when exercise testingis inc<strong>on</strong>clusive, in selecting lesi<strong>on</strong>s for revascularizati<strong>on</strong>,and in assessing ischaemia after revascularizati<strong>on</strong>. 193–196Pharmacologic stress imaging may also be used in <strong>the</strong> identificati<strong>on</strong><strong>of</strong> viable myocardium in selected patients with cor<strong>on</strong>arydisease and ventricular dysfuncti<strong>on</strong> in whom a decisi<strong>on</strong>for revascularizati<strong>on</strong> will be based <strong>on</strong> <strong>the</strong> presence <strong>of</strong> viablemyocardium. 197,198 A full descripti<strong>on</strong> <strong>of</strong> <strong>the</strong> methods <strong>of</strong>detecti<strong>on</strong> <strong>of</strong> viability is bey<strong>on</strong>d <strong>the</strong> scope <strong>of</strong> <strong>the</strong>se guidelinesbut a report <strong>on</strong> <strong>the</strong> imaging techniques for <strong>the</strong> detecti<strong>on</strong> <strong>of</strong>hibernating myocardium has been previously published byan ESC working group. 199 Finally, although stress imagingtechniques may allow for accurate evaluati<strong>on</strong> <strong>of</strong> changes in<strong>the</strong> localizati<strong>on</strong> and extent <strong>of</strong> ischaemia over time and inresp<strong>on</strong>se to treatment, periodic stress imaging in <strong>the</strong>absence <strong>of</strong> any change in clinical status is not recommendedas routine.Recommendati<strong>on</strong>s for <strong>the</strong> use <strong>of</strong> exercise stress withimaging techniques (ei<strong>the</strong>r echocardiography or perfusi<strong>on</strong>)in <strong>the</strong> initial diagnostic assessment <strong>of</strong> anginaClass I(1) Patients with resting ECG abnormalities, LBBB, .1 mmST-depressi<strong>on</strong>, paced rhythm, or WPW which prevent
ESC <str<strong>on</strong>g>Guidelines</str<strong>on</strong>g> 13accurate interpretati<strong>on</strong> <strong>of</strong> ECG changes during stress(level <strong>of</strong> evidence B)(2) Patients with a n<strong>on</strong>-c<strong>on</strong>clusive exercise ECG butreas<strong>on</strong>able exercise tolerance, who do not have ahigh probability <strong>of</strong> significant cor<strong>on</strong>ary disease andin whom <strong>the</strong> diagnosis is still in doubt (level <strong>of</strong>evidence B)Class IIa(1) Patients with prior revascularizati<strong>on</strong> (PCI or CABG) inwhom localizati<strong>on</strong> <strong>of</strong> ischaemia is important (level <strong>of</strong>evidence B)(2) As an alternative to exercise ECG in patients wherefacilities, cost, and pers<strong>on</strong>nel resources allow (level<strong>of</strong> evidence B)(3) As an alternative to exercise ECG in patients with a lowpre-test probability <strong>of</strong> disease such as women withatypical chest pain (level <strong>of</strong> evidence B)(4) To assess functi<strong>on</strong>al severity <strong>of</strong> intermediate lesi<strong>on</strong>s <strong>on</strong>cor<strong>on</strong>ary arteriography (level <strong>of</strong> evidence C)(5) To localize ischaemia when planning revascularizati<strong>on</strong>opti<strong>on</strong>s in patients who have already had arteriography(level <strong>of</strong> evidence B)Recommendati<strong>on</strong>s for <strong>the</strong> use <strong>of</strong> pharmacological stresswith imaging techniques (ei<strong>the</strong>r echocardiography orperfusi<strong>on</strong>) in <strong>the</strong> initial diagnostic assessment <strong>of</strong> anginaClass I, IIa, and IIb indicati<strong>on</strong>s as above if <strong>the</strong> patient isunable to exercise adequately.Stress cardiac magnetic res<strong>on</strong>ance. CMR stress testing inc<strong>on</strong>juncti<strong>on</strong> with a dobutamine infusi<strong>on</strong> can be used todetect wall moti<strong>on</strong> abnormalities induced by ischaemia.The technique has been shown to compare favourably todobutamine stress echocardiography (DSE) because <strong>of</strong>higher quality imaging. 200 Thus, dobutamine stress CMRhas been shown to be very effective in <strong>the</strong> diagnosis <strong>of</strong>CAD in patients who are unsuitable for dobutamine echocardiography.201 Studies <strong>of</strong> outcome following dobutamine CMRshow a low event rate when dobutamine CMR is normal. 202Myocardial perfusi<strong>on</strong> CMR now achieves comprehensiveventricular coverage using multislice imaging. Analysis isei<strong>the</strong>r visual to identify low signal areas <strong>of</strong> reduced perfusi<strong>on</strong>,or with computer assistance with quantificati<strong>on</strong> <strong>of</strong><strong>the</strong> upslope <strong>of</strong> myocardial signal increase during <strong>the</strong> firstpass. Although CMR perfusi<strong>on</strong> is still in development forclinical applicati<strong>on</strong>, <strong>the</strong> results are already very good incomparis<strong>on</strong> with X-ray cor<strong>on</strong>ary angiography, PET, andSPECT. 203,204A recent c<strong>on</strong>sensus panel reviewing <strong>the</strong> currentindicati<strong>on</strong>s for CMR thus gave class II recommendati<strong>on</strong>s forCMR wall moti<strong>on</strong> and CMR perfusi<strong>on</strong> imaging (Class IIprovides clinically relevant informati<strong>on</strong> and is frequentlyuseful; o<strong>the</strong>r techniques may provide similar informati<strong>on</strong>;supported by limited literature). 205Echocardiography at restResting two-dimensi<strong>on</strong>al and doppler echocardiography isuseful to detect or rule out <strong>the</strong> possibility <strong>of</strong> o<strong>the</strong>r disorderssuch as valvular heart disease 206 or hypertrophic cardiomyopathy207 as a cause <strong>of</strong> symptoms, and to evaluate ventricularfuncti<strong>on</strong>. 155 For purely diagnostic purposes, echo isuseful in patients with clinically detected murmurs, 208–211history and ECG changes compatible with hypertrophiccardiomyopathy 207,212 or previous MI, 213,214 and symptomsor signs <strong>of</strong> heart failure. 215–219 Cardiac magnetic res<strong>on</strong>ancemay be also be used to define structural cardiac abnormalitiesand evaluate ventricular functi<strong>on</strong>, but routine use forsuch purposes is limited by availability.The true prevalence <strong>of</strong> isolated diastolic heart failure isdifficult to quantify because <strong>of</strong> heterogeneity in definiti<strong>on</strong>sand variability in populati<strong>on</strong>s studied. 220 Community-basedstudies have an independent associati<strong>on</strong> between diastolicheart failure and a history <strong>of</strong> ischaemic heart disease,including angina, 221 streng<strong>the</strong>ning <strong>the</strong> case for echocardiographyin all patients with angina, and signs or symptoms<strong>of</strong> heart failure. Universal resting echocardiography in astable angina populati<strong>on</strong> without heart failure may alsoidentify previously undetected diastolic dysfuncti<strong>on</strong>.Recent developments in tissue Doppler imaging and strainrate measurement have greatly improved <strong>the</strong> ability tostudy diastolic functi<strong>on</strong> 165,222 but <strong>the</strong> clinical implicati<strong>on</strong>s<strong>of</strong> isolated diastolic dysfuncti<strong>on</strong> in terms <strong>of</strong> treatment orprognosis are less well defined. Diastolic functi<strong>on</strong> mayimprove with anti-ischaemic <strong>the</strong>rapy. 223 However, treatment<strong>of</strong> diastolic dysfuncti<strong>on</strong> as a primary aim <strong>of</strong> <strong>the</strong>rapyin stable angina is not yet warranted. There is no indicati<strong>on</strong>for repeated use <strong>of</strong> resting echocardiography <strong>on</strong> a regularbasis in patients with uncomplicated stable angina in <strong>the</strong>absence <strong>of</strong> a change in clinical c<strong>on</strong>diti<strong>on</strong>.Although <strong>the</strong> diagnostic yield <strong>of</strong> evaluati<strong>on</strong> <strong>of</strong> cardiacstructure and functi<strong>on</strong> in patients with angina is mostlyc<strong>on</strong>centrated in specific subgroups, estimati<strong>on</strong> <strong>of</strong> ventricularfuncti<strong>on</strong> is extremely important in risk stratificati<strong>on</strong>,where echocardiography (or alternative methods <strong>of</strong>assessment <strong>of</strong> ventricular functi<strong>on</strong>) has much widerindicati<strong>on</strong>s.Recommendati<strong>on</strong>s for echocardiography for initialdiagnostic assessment <strong>of</strong> anginaClass I(1) Patients with abnormal auscultati<strong>on</strong> suggesting valvularheart disease or hypertrophic cardiomyopathy(level <strong>of</strong> evidence B)(2) Patients with suspected heart failure (level <strong>of</strong>evidence B)(3) Patients with prior MI (level <strong>of</strong> evidence B)(4) Patients with LBBB, Q-waves, or o<strong>the</strong>r significantpathological changes <strong>on</strong> ECG, including ECG LVH(level <strong>of</strong> evidence C)Ambulatory ECG m<strong>on</strong>itoringAmbulatory ECG (Holter) m<strong>on</strong>itoring may reveal evidence <strong>of</strong>myocardial ischaemia during normal ‘daily’ activities, 224 butrarely adds important diagnostic informati<strong>on</strong> in chr<strong>on</strong>icstable angina pectoris over and above that provided by anexercise test. 6 Ambulatory silent ischaemia 6 has beenreported to predict adverse cor<strong>on</strong>ary events and <strong>the</strong>re isc<strong>on</strong>flicting evidence that <strong>the</strong> suppressi<strong>on</strong> <strong>of</strong> silent ischaemiain stable angina improves cardiac outcome. The significance<strong>of</strong> silent ischaemia in this c<strong>on</strong>text is different from that inunstable angina where it has been shown that recurrentsilent ischaemia predicts an adverse outcome. Prognosticstudies in stable angina seem to identify silent ischaemia<strong>on</strong> ambulatory m<strong>on</strong>itoring as a harbinger <strong>of</strong> hard clinicalevents (fatal and n<strong>on</strong>-fatal MI) <strong>on</strong>ly in highly selectedpatients with ischaemia detectible <strong>on</strong> exercise testing,
14 ESC <str<strong>on</strong>g>Guidelines</str<strong>on</strong>g>and <strong>the</strong>re is little evidence to support its routine deploymentas a prognostic implement in this clinical setting. 225,226Ambulatory m<strong>on</strong>itoring may have a role, however, inpatients in whom vasospastic angina is suspected. Finally,in patients with stable angina and suspected major arrhythmias,Holter m<strong>on</strong>itoring is an important method <strong>of</strong> diagnosingarrhythmias. Repeated ambulatory ECG m<strong>on</strong>itoring asmeans to evaluate patients with chr<strong>on</strong>ic stable angina isnot recommended.Recommendati<strong>on</strong>s for ambulatory ECG for initialdiagnostic assessment <strong>of</strong> anginaClass I(1) <strong>Angina</strong> with suspected arrhythmia (level <strong>of</strong> evidence B)Class IIa(1) Suspected vasospastic angina (level <strong>of</strong> evidence C)N<strong>on</strong>-invasive techniques to assess cor<strong>on</strong>ary calcificati<strong>on</strong>and cor<strong>on</strong>ary anatomyComputed tomography. Although spatial resoluti<strong>on</strong> andmovement artefact have for a l<strong>on</strong>g time been limitingfactors in computed tomography (CT) cardiac imaging, c<strong>on</strong>siderableadvances in technology have been made in recentyears to overcome <strong>the</strong>se issues. Two modalities <strong>of</strong> CTimaging have developed to improve spatial and temporalresoluti<strong>on</strong> in CT, ultra-fast or electr<strong>on</strong> beam CT (EBCT),and multi-detector or multi-slice CT (MDCT). These havebeen accompanied by improvements in processing s<strong>of</strong>twareto facilitate interpretati<strong>on</strong> <strong>of</strong> <strong>the</strong> images acquired. Bothtechniques have been validated as effective in <strong>the</strong> detecti<strong>on</strong><strong>of</strong> cor<strong>on</strong>ary calcium and quantificati<strong>on</strong> <strong>of</strong> <strong>the</strong> extent <strong>of</strong> cor<strong>on</strong>arycalcificati<strong>on</strong>. 227–230 The Agatst<strong>on</strong> score, 231 <strong>the</strong> mostcomm<strong>on</strong>ly used score, is based <strong>on</strong> <strong>the</strong> area and density <strong>of</strong>calcified plaques. It is computed by specific s<strong>of</strong>tware andis used to quantify <strong>the</strong> extent <strong>of</strong> cor<strong>on</strong>ary calcificati<strong>on</strong>.Calcium is deposited in a<strong>the</strong>rosclerotic plaques within <strong>the</strong>cor<strong>on</strong>ary arteries. Cor<strong>on</strong>ary calcificati<strong>on</strong> increases with age,and nomograms have been developed to facilitate interpretati<strong>on</strong><strong>of</strong> calcium scores relative to <strong>the</strong> expected values for agiven age and gender. 232 The extent <strong>of</strong> cor<strong>on</strong>ary calcificati<strong>on</strong>correlates more closely with <strong>the</strong> overall burden <strong>of</strong> plaquethan with <strong>the</strong> locati<strong>on</strong> or severity <strong>of</strong> stenoses. 233 Thus inpopulati<strong>on</strong>-based studies detecti<strong>on</strong> <strong>of</strong> cor<strong>on</strong>ary calciummay identify those at higher risk <strong>of</strong> significant cor<strong>on</strong>arydisease, but assessment <strong>of</strong> cor<strong>on</strong>ary calcificati<strong>on</strong> is not recommendedroutinely for <strong>the</strong> diagnostic evaluati<strong>on</strong> <strong>of</strong>patients with stable angina. 234,235Image acquisiti<strong>on</strong> times and resoluti<strong>on</strong> for EBCT and MDCThave been shortened to <strong>the</strong> extent that CT cor<strong>on</strong>ary arteriographycan be performed by injecti<strong>on</strong> <strong>of</strong> intravenous c<strong>on</strong>trastagents. 236 MDCT or multi-slice CT appears to be <strong>the</strong> mostpromising <strong>of</strong> <strong>the</strong> two techniques in terms <strong>of</strong> n<strong>on</strong>-invasiveimaging <strong>of</strong> <strong>the</strong> cor<strong>on</strong>ary arteries, with preliminary studiessuggesting excellent definiti<strong>on</strong>, and <strong>the</strong> possibility <strong>of</strong> examiningarterial wall and plaque characteristics. Sensitivity andspecificity (segment-specific) <strong>of</strong> CT angiography for <strong>the</strong>detecti<strong>on</strong> <strong>of</strong> cor<strong>on</strong>ary disease has been reported to be 95and 98%, respectively, using 16-slice CT scanners. 237 Studiesusing 64 detector scanning report sensitivities and specificities<strong>of</strong> 90–94% and 95–97%, respectively, and importantly, anegative predictive value <strong>of</strong> 93–99%. 238,239 N<strong>on</strong>-invasive CTarteriography holds c<strong>on</strong>siderable promise for <strong>the</strong> future <strong>of</strong><strong>the</strong> diagnostic assessment <strong>of</strong> cor<strong>on</strong>ary disease. Optimal use<strong>of</strong> this rapidly developing technology will harness <strong>the</strong> skills<strong>of</strong> both radiology and cardiology disciplines, with cardiologynecessarily taking <strong>the</strong> lead in selecti<strong>on</strong> <strong>of</strong> patients for investigati<strong>on</strong>by this method, and appropriate management based<strong>on</strong> <strong>the</strong> results. At present, although <strong>the</strong> diagnostic accuracy<strong>of</strong> this technique has been reported, <strong>the</strong> prognostic utility,and <strong>the</strong> exact place in <strong>the</strong> hierarchy <strong>of</strong> investigati<strong>on</strong>s instable angina has not yet been fully defined. A c<strong>on</strong>servativesuggesti<strong>on</strong> for its use would be in patients with a lowpre-test (,10%) probability <strong>of</strong> disease with an equivocalfuncti<strong>on</strong>al test (exercise ECG or stress imaging).Recommendati<strong>on</strong>s for <strong>the</strong> use <strong>of</strong> CT angiography instable anginaClass IIb(1) Patients with a low pre-test probability <strong>of</strong> disease, witha n<strong>on</strong>-c<strong>on</strong>clusive exercise ECG or stress imaging test(level <strong>of</strong> evidence C)Magnetic res<strong>on</strong>ance arteriography. Similar to <strong>the</strong> case <strong>of</strong> CT,advances in magnetic res<strong>on</strong>ance technology permit n<strong>on</strong>invasiveMR c<strong>on</strong>trast cor<strong>on</strong>ary arteriography, 205 and hold<strong>the</strong> potential for plaque characterizati<strong>on</strong>. 240 Advantages <strong>of</strong><strong>the</strong> technique include <strong>the</strong> c<strong>on</strong>siderable potential for evaluati<strong>on</strong><strong>of</strong> overall cardiac anatomy and functi<strong>on</strong>. However, atpresent this can <strong>on</strong>ly be regarded as a valuable tool forresearch and is not recommended as routine clinicalpractice in <strong>the</strong> diagnostic evaluati<strong>on</strong> <strong>of</strong> stable angina.Invasive techniques to assess cor<strong>on</strong>ary anatomyCor<strong>on</strong>ary arteriographyCor<strong>on</strong>ary arteriography is generally undertaken as part <strong>of</strong> aseries <strong>of</strong> tests to establish a diagnosis and ascertain treatmentopti<strong>on</strong>s. N<strong>on</strong>-invasive testing can establish <strong>the</strong> likelihood<strong>of</strong> <strong>the</strong> presence <strong>of</strong> obstructive cor<strong>on</strong>ary disease withan acceptable degree <strong>of</strong> certainty, and through appropriaterisk stratificati<strong>on</strong> may be used to determine <strong>the</strong> need forcor<strong>on</strong>ary arteriography for fur<strong>the</strong>r risk stratificati<strong>on</strong> purposes.However, it may be c<strong>on</strong>traindicated for reas<strong>on</strong>s <strong>of</strong>disability or serious comorbidity, or <strong>of</strong>fer inc<strong>on</strong>clusiveresults. After a resuscitated cardiac arrest or life threateningventricular arrhythmia, a definitive diagnosis regarding<strong>the</strong> presence or absence <strong>of</strong> cor<strong>on</strong>ary disease is useful inclinical decisi<strong>on</strong>-making. 241,242 In additi<strong>on</strong>, n<strong>on</strong>-invasivetesting does not allow assessment <strong>of</strong> suitability for revascularizati<strong>on</strong>which may be c<strong>on</strong>sidered for symptomatic as wellas prognostic grounds. Cor<strong>on</strong>ary arteriography holds afundamental positi<strong>on</strong> in <strong>the</strong> investigati<strong>on</strong> <strong>of</strong> patients withstable angina, providing reliable anatomical informati<strong>on</strong> toidentify <strong>the</strong> presence or absence <strong>of</strong> cor<strong>on</strong>ary lumen stenosis,define <strong>the</strong>rapeutic opti<strong>on</strong>s (suitability <strong>of</strong> medical treatmentor myocardial revascularizati<strong>on</strong>), and determine prognosis.Methods used to perform cor<strong>on</strong>ary arteriography haveimproved substantially resulting in <strong>the</strong> reducti<strong>on</strong> <strong>of</strong> complicati<strong>on</strong>rates and rapid ambulati<strong>on</strong>. The composite rate <strong>of</strong>major complicati<strong>on</strong>s associated with routine diagnosticca<strong>the</strong>terizati<strong>on</strong> in patients is between 1 and 2%. The compositerate <strong>of</strong> death, MI, or stroke is <strong>of</strong> <strong>the</strong> order <strong>of</strong> 0.1–0.2%. 243Intravascular ultrasoundIntravascular ultrasound is a technique that allows producti<strong>on</strong><strong>of</strong> ultrasound images from within <strong>the</strong> (cor<strong>on</strong>ary)
ESC <str<strong>on</strong>g>Guidelines</str<strong>on</strong>g> 15arteries by passing an ultrasound ca<strong>the</strong>ter into <strong>the</strong> cor<strong>on</strong>aryartery lumen. 244 Intravascular ultrasound allows for accuratemeasurement <strong>of</strong> cor<strong>on</strong>ary luminal diameter, assessment<strong>of</strong> eccentric lesi<strong>on</strong>s and Glagovian remodelling, and quantificati<strong>on</strong><strong>of</strong> a<strong>the</strong>roma and calcium depositi<strong>on</strong>. It also allowsfor detailed assessment <strong>of</strong> interventi<strong>on</strong>al target lesi<strong>on</strong>s,stent placement, appositi<strong>on</strong> and expansi<strong>on</strong>, and transplantvasculopathy. The technique has afforded advantages interms <strong>of</strong> our understanding <strong>of</strong> a<strong>the</strong>rosclerotic plaque depositi<strong>on</strong>and progressi<strong>on</strong>, <strong>of</strong>fering c<strong>on</strong>siderably improvedqualitative and quantitative assessment <strong>of</strong> cor<strong>on</strong>aryanatomy compared with c<strong>on</strong>trast arteriography and doubtless,has an important role in specialized clinical settings,particularly as an adjunct to cor<strong>on</strong>ary interventi<strong>on</strong>.However, it is more appropriately used in highly specificclinical settings and for research purposes than widespreadapplicati<strong>on</strong> as a first line investigati<strong>on</strong> for cor<strong>on</strong>arydisease. 245,246Invasive assessment <strong>of</strong> functi<strong>on</strong>al severity <strong>of</strong> cor<strong>on</strong>arylesi<strong>on</strong>sThe functi<strong>on</strong>al severity <strong>of</strong> cor<strong>on</strong>ary lesi<strong>on</strong>s visualized angiographicallymay be assessed invasively by means <strong>of</strong> measuringei<strong>the</strong>r <strong>the</strong> cor<strong>on</strong>ary flow velocity (cor<strong>on</strong>ary vasodilatoryreserve), or intracor<strong>on</strong>ary artery pressure fracti<strong>on</strong>al flowreserve (FFR). 7,247 Both techniques involve inducing hyperaemiathrough intracor<strong>on</strong>ary injecti<strong>on</strong> <strong>of</strong> vasodilatingagents. The cor<strong>on</strong>ary vasodilatory reserve (CVR) is <strong>the</strong>ratio <strong>of</strong> hyperaemic to basal flow velocity and reflects flowresistance through <strong>the</strong> epicardial artery and <strong>the</strong> corresp<strong>on</strong>dingmyocardial bed. It is dependent <strong>on</strong> microcirculati<strong>on</strong> aswell as severity <strong>of</strong> <strong>the</strong> lesi<strong>on</strong> in <strong>the</strong> epicardial vessel.FFR 248 is calculated as <strong>the</strong> ratio <strong>of</strong> distal cor<strong>on</strong>ary pressureto aortic pressure measured during maximal hyperaemia.A normal value for FFR is 1.0 regardless <strong>of</strong> <strong>the</strong> status <strong>of</strong><strong>the</strong> microcirculati<strong>on</strong>, and an FFR ,0.75 is deemedpathological.Physiological measurements as described may facilitatediagnosis in cases <strong>of</strong> intermediate angiographic stenoses,(visually estimated stenosis 30–70%). FFR measurement hasbeen shown to be useful in differentiating between patientswith favourable l<strong>on</strong>g-term outcome (i.e. patients withFFR .0.75) who do not need revascularizati<strong>on</strong>; and patientswho require revascularizati<strong>on</strong> (i.e. patients withFFR ,0.75) 249 but this investigati<strong>on</strong> is best reserved forspecific clinical circumstances or in deciding suitability forrevascularizati<strong>on</strong> ra<strong>the</strong>r than routine use.Recommendati<strong>on</strong>s for cor<strong>on</strong>ary arteriography for <strong>the</strong>purposes <strong>of</strong> establishing a diagnosis in stable anginaClass I(1) Severe stable angina (Class 3 or greater <strong>of</strong> Canadian<strong>Cardio</strong>vascular Society Classificati<strong>on</strong>), with a highpre-test probability <strong>of</strong> disease, particularly if <strong>the</strong> symptomsare inadequately resp<strong>on</strong>ding to medical treatment(level <strong>of</strong> evidence B)(2) Survivors <strong>of</strong> cardiac arrest (level <strong>of</strong> evidence B)(3) Patients with serious ventricular arrhythmias (level <strong>of</strong>evidence C)(4) Patients previously treated by myocardial revascularizati<strong>on</strong>(PCI, CABG) who develop early recurrence<strong>of</strong> moderate or severe angina pectoris (level <strong>of</strong>evidence C)Class IIa(1) Patients with an inc<strong>on</strong>clusive diagnosis <strong>on</strong> n<strong>on</strong>-invasivetesting, or c<strong>on</strong>flicting results from different n<strong>on</strong>invasivemodalities at intermediate to high risk <strong>of</strong>cor<strong>on</strong>ary disease (level <strong>of</strong> evidence C)(2) Patients with a high risk <strong>of</strong> restenosis after PCI if PCIhas been performed in a prognostically important site(level <strong>of</strong> evidence C)Risk stratificati<strong>on</strong>The l<strong>on</strong>g-term prognosis <strong>of</strong> stable angina is variable, and <strong>the</strong>range <strong>of</strong> treatment opti<strong>on</strong>s has expanded c<strong>on</strong>siderably fromsimple symptomatic c<strong>on</strong>trol to potent and <strong>of</strong>ten expensivestrategies to improve prognosis. When discussing risk stratificati<strong>on</strong>in stable angina, risk refers primarily to <strong>the</strong> risk <strong>of</strong>cardiovascular death, but <strong>the</strong> term is <strong>of</strong>ten more looselyapplied to incorporate cardiovascular death and MI, or insome cases even wider combinati<strong>on</strong>s <strong>of</strong> cardiovascular endpoints.The process <strong>of</strong> risk stratificati<strong>on</strong> serves a dualpurpose, to facilitate an informed resp<strong>on</strong>se to queriesregarding prognosis from patients <strong>the</strong>mselves, employers,insurers, n<strong>on</strong>-cardiology specialists c<strong>on</strong>sidering treatmentopti<strong>on</strong>s for comorbid c<strong>on</strong>diti<strong>on</strong>s and o<strong>the</strong>rs, and sec<strong>on</strong>dlyto assist in choosing appropriate treatment.For certain management opti<strong>on</strong>s, particularly revascularizati<strong>on</strong>and/or intensified pharmacological <strong>the</strong>rapy, prognosticbenefit is <strong>on</strong>ly apparent in high-risk subgroups, withlimited if any benefit in those whose prognosis is alreadygood. This mandates identificati<strong>on</strong> <strong>of</strong> those patients athighest risk, and <strong>the</strong>refore most likely to benefit frommore aggressive treatment, early in <strong>the</strong> assessment <strong>of</strong>stable angina.A 10-year cardiovascular mortality <strong>of</strong> .5% (.0.5% perannum) is determined to be high risk for <strong>the</strong> purpose <strong>of</strong>implementing primary preventi<strong>on</strong> guidelines. 250 However,absolute levels <strong>of</strong> what c<strong>on</strong>stitutes high-risk and low-riskare not clearly defined for those with establishedCVD. 68,251 This problem is linked to difficulties in comparingrisk predicti<strong>on</strong> systems across different populati<strong>on</strong>s, determiningaccuracy <strong>of</strong> individualized predicti<strong>on</strong>s <strong>of</strong> risk, andsyn<strong>the</strong>sis <strong>of</strong> multiple comp<strong>on</strong>ents <strong>of</strong> risk, <strong>of</strong>ten studied separately,into an estimate <strong>of</strong> risk for an individual. Added toc<strong>on</strong>tinuously evolving public and pr<strong>of</strong>essi<strong>on</strong>al percepti<strong>on</strong>s<strong>of</strong> what c<strong>on</strong>stitutes high- and low-risk over <strong>the</strong> past fourto five decades (since many <strong>of</strong> <strong>the</strong> initial risk predictorswere defined), <strong>the</strong> reas<strong>on</strong>s for this lack <strong>of</strong> definiti<strong>on</strong> arenot easily overcome.However, while awaiting development <strong>of</strong> a robust andportable risk predicti<strong>on</strong> model which incorporates all potentialaspects <strong>of</strong> risk stratificati<strong>on</strong>, <strong>the</strong>re is an alternativepragmatic approach, based <strong>on</strong> clinical trial data. Theinherent problems with bias when interpreting and generalizingclinical trial data must be recognized, but such data<strong>of</strong>fer an estimate <strong>of</strong> <strong>the</strong> levels <strong>of</strong> absolute risk achievablewith modern c<strong>on</strong>venti<strong>on</strong>al treatment even in patients withproven vascular disease. This in turn facilitates anestimati<strong>on</strong> <strong>of</strong> what may be accepted as c<strong>on</strong>stituting high,low, and intermediate risk in a c<strong>on</strong>temporary setting for<strong>the</strong> purposes <strong>of</strong> determining <strong>the</strong> threshold for invasiveinvestigati<strong>on</strong> or intensified pharmacological <strong>the</strong>rapy.The cardiovascular mortality and MI rate observed in <strong>the</strong>placebo arms <strong>of</strong> large trials <strong>of</strong> sec<strong>on</strong>dary preventi<strong>on</strong> or
16 ESC <str<strong>on</strong>g>Guidelines</str<strong>on</strong>g>anti-anginal <strong>the</strong>rapy in stable cor<strong>on</strong>ary disease publishedsince 2000 are illustrated in Figure 1. The rate <strong>of</strong> cardiovasculardeath in <strong>the</strong> PEACE 252 study was less than 1% perannum, whereas in ‘high-risk’ populati<strong>on</strong>s such as in diabeticMICRO-HOPE 253 populati<strong>on</strong> and <strong>the</strong> IONA 254 populati<strong>on</strong> <strong>the</strong>annualized cardiovascular mortality rate was .2%. For <strong>the</strong>purposes <strong>of</strong> <strong>the</strong>se guidelines, unless qualified differently in<strong>the</strong> text, if an individual with angina is determined <strong>on</strong> <strong>the</strong>basis <strong>of</strong> a well validated risk predicti<strong>on</strong> model, to haveannual cardiovascular mortality <strong>of</strong> .2% that individual isdeemed high risk, whereas an annual cardiovascular mortality<strong>of</strong> ,1% is c<strong>on</strong>sidered low risk, and 1–2% intermediaterisk.The clinical evaluati<strong>on</strong>, <strong>the</strong> resp<strong>on</strong>se to stress testing,<strong>the</strong> quantificati<strong>on</strong> <strong>of</strong> ventricular functi<strong>on</strong>, and <strong>the</strong> extent<strong>of</strong> CAD are <strong>the</strong> four key pieces <strong>of</strong> informati<strong>on</strong> to stratifypatient’s risk. 66–68,124,255,256 However, not all patients willrequire invasive assessment <strong>of</strong> <strong>the</strong> cor<strong>on</strong>ary anatomy, particularlyif <strong>the</strong>ir clinical evaluati<strong>on</strong> and n<strong>on</strong>-invasivetesting establish that <strong>the</strong>y are in a low-risk group. The riskassessment hierarchy can be described as:(1) Risk stratificati<strong>on</strong> by clinical evaluati<strong>on</strong>(2) Risk stratificati<strong>on</strong> by resp<strong>on</strong>se to stress testing(3) Risk stratificati<strong>on</strong> by ventricular functi<strong>on</strong>(4) Risk stratificati<strong>on</strong> by cor<strong>on</strong>ary anatomyThe route through <strong>the</strong>se successive tests may not alwaysbe directly linear. For example in a patient with a highpre-test probability <strong>of</strong> disease, severe angina, and o<strong>the</strong>rhigh-risk clinical features such as signs <strong>of</strong> heart failure,may proceed directly from clinical evaluati<strong>on</strong> to cor<strong>on</strong>aryarteriography, with perfusi<strong>on</strong> scintigraphy afterwards toevaluate myocardial viability. However, risk stratificati<strong>on</strong>generally follows a pyramidal structure, with all patientsrequiring risk stratificati<strong>on</strong> by clinical evaluati<strong>on</strong> as <strong>the</strong>most basic requirement, proceeding in <strong>the</strong> majority to n<strong>on</strong>invasiveassessment <strong>of</strong> ischaemia and ventricular functi<strong>on</strong>,and finally cor<strong>on</strong>ary arteriography in a selected proporti<strong>on</strong>.A summary <strong>of</strong> <strong>the</strong> recommendati<strong>on</strong>s for <strong>the</strong> routine use <strong>of</strong>investigati<strong>on</strong>s in evaluati<strong>on</strong> <strong>of</strong> stable angina with corresp<strong>on</strong>dinglevels <strong>of</strong> evidence related to diagnosis and prognosis,is presented in Table 7, and an algorithm for <strong>the</strong> initialevaluati<strong>on</strong> <strong>of</strong> patients presenting with clinical symptomssuggestive <strong>of</strong> angina is depicted in Figure 2.Risk stratificati<strong>on</strong> using clinical evaluati<strong>on</strong>The clinical history and physical examinati<strong>on</strong> can providevery important prognostic informati<strong>on</strong>. ECG can be c<strong>on</strong>venientlyincorporated in risk stratificati<strong>on</strong> at this level,and <strong>the</strong> results <strong>of</strong> <strong>the</strong> laboratory tests discussed in <strong>the</strong> previoussecti<strong>on</strong> may modify risk estimati<strong>on</strong> fur<strong>the</strong>r. Diabetes,hypertensi<strong>on</strong>, current smoking, and elevated total cholesterol(untreated or elevated despite treatment) have beenshown to be predictive <strong>of</strong> adverse outcome in patientswith stable angina or o<strong>the</strong>r populati<strong>on</strong>s with established cor<strong>on</strong>arydisease. 56,58,257–259 Increasing age is an importantfactor to c<strong>on</strong>sider, as are prior MI, 66,123 symptoms andsigns <strong>of</strong> heart failure, 66,123,124 and <strong>the</strong> pattern <strong>of</strong> occurrence(recent <strong>on</strong>set or progressive), and severity <strong>of</strong> angina,particularly if unresp<strong>on</strong>sive to <strong>the</strong>rapy. 255,260Pryor et al. 261 studied a total <strong>of</strong> 1030 c<strong>on</strong>secutive outpatientsreferred to n<strong>on</strong>-invasive testing for suspectedCAD; <strong>the</strong> informati<strong>on</strong> from <strong>the</strong> initial history, physical examinati<strong>on</strong>,ECG, and chest radiograph was used to predict cor<strong>on</strong>aryanatomy, i.e. <strong>the</strong> likelihood <strong>of</strong> any significant cor<strong>on</strong>arydisease, severe disease, and significant left main (LM)disease and to estimate 3 years survival. These estimateswere compared with those based <strong>on</strong> treadmill testing.Compared with <strong>the</strong> treadmill exercise test, initialevaluati<strong>on</strong> was slightly better able to distinguish patientswith or without CAD and was similar in <strong>the</strong> ability toidentify patients at increased risk for dying or with anatomicallysevere disease. Although much <strong>of</strong> <strong>the</strong> informati<strong>on</strong>obtained by physicians during <strong>the</strong> initial assessment isFigure 1 <strong>Cardio</strong>vascular mortality and myocardial infarcti<strong>on</strong> in c<strong>on</strong>temporary trials <strong>of</strong> stable cor<strong>on</strong>ary disease or angina: CAMELOT, 467 PEACE, 252 ACTION, 493EUROPA, 461 HOPE, 460 IONA, 254 and MICRO-HOPE. 253
ESC <str<strong>on</strong>g>Guidelines</str<strong>on</strong>g> 17Table 7Summary <strong>of</strong> recommendati<strong>on</strong>s for routine n<strong>on</strong>-invasive investigati<strong>on</strong>s in evaluati<strong>on</strong> <strong>of</strong> stable anginaTest For Diagnosis For PrognosisClass <strong>of</strong>recommendati<strong>on</strong>Level <strong>of</strong>evidenceClass <strong>of</strong>recommendati<strong>on</strong>Level <strong>of</strong>evidenceLaboratory testsFull blood count, creatinine I C I BFasting glucose I B I BFasting lipid pr<strong>of</strong>ile I B I BHs-C-reactive protein, homocysteine, lp(a), apoA,IIb B IIb Band apoBECGInitial evaluati<strong>on</strong> I C I BDuring episode <strong>of</strong> angina I BRoutine periodic ECG <strong>on</strong> successive visits IIb C IIb CAmbulatory ECG m<strong>on</strong>itoringSuspected arrhythmia I BSuspected vasopastic angina IIa CIn suspected angina with normal exercise test IIa CCXRSuspected heart failure or abnormalI B I Bcardiac auscultati<strong>on</strong>Suspected significant pulm<strong>on</strong>ary disease I BEchocardiogramSuspected heart failure, abnormal auscultati<strong>on</strong>,I B I Babnormal ECG, Qwaves, BBB, andmarked ST changesPrevious MI I BHypertensi<strong>on</strong> or diabetes mellitus I C I B/CIntermediate or low-risk patient not due toIIaChave alternative assessment <strong>of</strong> LV functi<strong>on</strong>Exercise ECGFirst line for initial evaluati<strong>on</strong>,I B I Bunless unable to exercise/ECG not evaluablePatients with known CAD andIBsignificant deteriorati<strong>on</strong> in symptomsRoutine periodic testing <strong>on</strong>ce angina c<strong>on</strong>trolled IIb C IIb CExercise imaging technique (echo or radi<strong>on</strong>ucleotide)Initial evaluati<strong>on</strong> in patients with uninterpretable ECG I B I BPatients with n<strong>on</strong>-c<strong>on</strong>clusive exercise testI B I B(but adequate exercise tolerance)<strong>Angina</strong> post-revascularizati<strong>on</strong> IIa B IIa BTo identify locati<strong>on</strong> <strong>of</strong> ischaemiaIIaBin planning revascularizati<strong>on</strong>Assessment <strong>of</strong> functi<strong>on</strong>al severity <strong>of</strong>IIaCintermediate lesi<strong>on</strong>s <strong>on</strong> arteriographyPharmacological stress imaging techniquePatients unable to exercise I B I BPatients with n<strong>on</strong>-c<strong>on</strong>clusive exercise test due toI B I Bpoor exercise toleranceTo evaluate myocardial viability IIa BO<strong>the</strong>r indicati<strong>on</strong>s as for exerciseIIa B IIa Bimaging where local facilities favourpharmacological ra<strong>the</strong>r than exercise stressN<strong>on</strong>-invasive CT arteriographyPatients with low probability <strong>of</strong>disease and n<strong>on</strong>-c<strong>on</strong>clusive or positive stress testIIbCsubjective, <strong>the</strong>ir study c<strong>on</strong>firms <strong>the</strong> importance <strong>of</strong> thatinformati<strong>on</strong> in identifying patients likely to benefit fromfur<strong>the</strong>r testing and supports <strong>the</strong> development <strong>of</strong> strategiesthat use <strong>the</strong> physician’s initial assessment in <strong>the</strong> evaluati<strong>on</strong>process.Typical angina has been shown to be a significant prognosticfactor in patients undergoing cor<strong>on</strong>ary arteriography,however, <strong>the</strong> relati<strong>on</strong> <strong>of</strong> typical angina to prognosis ismediated by its relati<strong>on</strong> to <strong>the</strong> extent <strong>of</strong> cor<strong>on</strong>ary disease.But <strong>the</strong> pattern <strong>of</strong> angina occurrence, angina frequency,and resting ECG abnormalities are independent predictors<strong>of</strong> survival and survival free <strong>of</strong> MI, and may be combinedin a simple weighted score (Figure 3) to predict outcome,particularly in <strong>the</strong> first year after assessment.
18 ESC <str<strong>on</strong>g>Guidelines</str<strong>on</strong>g>Figure 2Algorithm for <strong>the</strong> initial evaluati<strong>on</strong> <strong>of</strong> patients with clinical symptoms <strong>of</strong> angina.The effect <strong>of</strong> angina score <strong>on</strong> prognosis is not apparentafter 3 years and is greatest when ventricular functi<strong>on</strong> ismaintained. 68,255 This is due to <strong>the</strong> pr<strong>of</strong>ound effect <strong>of</strong>impaired ventricular functi<strong>on</strong> <strong>on</strong> prognosis, which whenpresent, greatly outweighs <strong>the</strong> effect <strong>of</strong> symptom severity.The associati<strong>on</strong> between <strong>the</strong> pattern <strong>of</strong> angina occurrence,particularly <strong>the</strong> development <strong>of</strong> new <strong>on</strong>set symptoms,with adverse prognosis may be due to overlap with<strong>the</strong> milder end <strong>of</strong> <strong>the</strong> spectrum <strong>of</strong> unstable angina.Fur<strong>the</strong>rmore, with more severe angina, <strong>the</strong> likelihood <strong>of</strong>cor<strong>on</strong>ary revascularizati<strong>on</strong> for prognostically importantdisease increases, which may also c<strong>on</strong>tribute to <strong>the</strong>time-dependency <strong>of</strong> symptom severity in predicting risk.Physical examinati<strong>on</strong> may also help in determining risk.The presence <strong>of</strong> peripheral vascular disease 262,263 (ei<strong>the</strong>rlower limb or carotid) identifies patients at increased risk<strong>of</strong> subsequent cardiovascular events in stable angina. Inadditi<strong>on</strong>, signs related to heart failure (which reflect LVfuncti<strong>on</strong>) c<strong>on</strong>vey an adverse prognosis.Patients with stable angina who have resting ECG abnormalities:evidence <strong>of</strong> prior MI, LBBB, left anterior hemiblock,LVH, sec<strong>on</strong>d or third degree AV block, or AF are at greater
ESC <str<strong>on</strong>g>Guidelines</str<strong>on</strong>g> 19Figure 3 Prognostic angina score. The pattern <strong>of</strong> angina occurrence can be used to predict prognosis. 80risk <strong>of</strong> future cardiovascular events than those with a normalECG. 45,264–267 It is possible that in an unselected populati<strong>on</strong>with stable angina <strong>the</strong> baseline risk is lower than in many <strong>of</strong><strong>the</strong> studies quoted accepting that many <strong>of</strong> <strong>the</strong>se studieshave been c<strong>on</strong>ducted in patients referred for fur<strong>the</strong>r angiographicevaluati<strong>on</strong>.Recommendati<strong>on</strong>s for risk stratificati<strong>on</strong> by clinical evaluati<strong>on</strong>,including ECG and laboratory tests in stable anginaClass I(1) Detailed clinical history and physical examinati<strong>on</strong>including BMI and/or waist circumference in allpatients, also including a full descripti<strong>on</strong> <strong>of</strong> symptoms,quantificati<strong>on</strong> <strong>of</strong> functi<strong>on</strong>al impairment, past medicalhistory, and cardiovascular risk pr<strong>of</strong>ile (level <strong>of</strong>evidence B)(2) Resting ECG in all patients (level <strong>of</strong> evidence B)Risk stratificati<strong>on</strong> using stress testingStress testing can take <strong>the</strong> form <strong>of</strong> exercise or pharmacologicalstress with or without imaging. Prognostic informati<strong>on</strong>obtained from stress testing relates not just to detecti<strong>on</strong><strong>of</strong> ischaemia as a simple binary resp<strong>on</strong>se, but also <strong>the</strong>ischaemic threshold, <strong>the</strong> extent and severity <strong>of</strong> ischaemia(for imaging techniques), and functi<strong>on</strong>al capacity (for exercisetesting). Stress testing al<strong>on</strong>e is insufficient to assess risk<strong>of</strong> future events. In additi<strong>on</strong> to <strong>the</strong> limitati<strong>on</strong>s <strong>of</strong> <strong>the</strong> differenttechniques in <strong>the</strong> detecti<strong>on</strong> <strong>of</strong> myocardial ischaemia,however small, it must also be recognized that ischaemiaper se is not <strong>the</strong> <strong>on</strong>ly factor which influences <strong>the</strong> likelihood<strong>of</strong> acute events. Several lines <strong>of</strong> evidence have shown that<strong>the</strong> majority <strong>of</strong> vulnerable plaques appear angiographicallyinsignificant before <strong>the</strong>ir rupture, and may not impinge <strong>on</strong>cor<strong>on</strong>ary flow to reveal characteristic changes during exerciseECG or stress imaging. This may explain <strong>the</strong> occasi<strong>on</strong>alacute cor<strong>on</strong>ary event that occurs shortly after a negativestress test result. Risk stratificati<strong>on</strong> with <strong>the</strong> exercise testshould be a part <strong>of</strong> a process that includes readily accessibledata from clinical examinati<strong>on</strong> and should not take place inisolati<strong>on</strong>. Thus <strong>the</strong> stress test is performed to provideadditi<strong>on</strong>al informati<strong>on</strong> regarding <strong>the</strong> patient’s risk status.Symptomatic patients with suspected or known CAD shouldundergo stress testing to assess <strong>the</strong> risk <strong>of</strong> future cardiacevents unless cardiac ca<strong>the</strong>terizati<strong>on</strong> is urgently indicated.However, no randomized trials <strong>of</strong> stress testing have beenpublished, and <strong>the</strong>refore <strong>the</strong> evidence base c<strong>on</strong>sists <strong>of</strong>observati<strong>on</strong>al studies <strong>on</strong>ly. The choice <strong>of</strong> initial stress testshould be based <strong>on</strong> <strong>the</strong> patient’s resting ECG, physicalability to perform exercise, local expertise, and availabletechnologies.Exercise ECG. The exercise ECG has been extensively validatedas an important tool in risk stratificati<strong>on</strong> in symptomaticpatients with known or suspected cor<strong>on</strong>ary disease.The prognosis <strong>of</strong> patients with a normal ECG and a low clinicalrisk for severe CAD is excellent. In <strong>on</strong>e study in which 37%<strong>of</strong> outpatients referred for n<strong>on</strong>-invasive testing met <strong>the</strong>criteria for low risk 261 fewer than 1% had LM stem arterydisease or died within 3 years. Lower-cost opti<strong>on</strong>s such astreadmill testing should <strong>the</strong>refore be used, whenever possible,for initial risk stratificati<strong>on</strong>, and <strong>on</strong>ly those withabnormal results should be referred to arteriography.The prognostic exercise testing markers include exercisecapacity, blood pressure resp<strong>on</strong>se, and exercise-inducedischaemia (clinical and ECG). Maximum exercise capacityis a c<strong>on</strong>sistent prognostic marker, this measure is at leastpartly influenced by <strong>the</strong> extent <strong>of</strong> rest ventricular dysfuncti<strong>on</strong>and <strong>the</strong> amount <strong>of</strong> fur<strong>the</strong>r LV dysfuncti<strong>on</strong> induced byexercise. 139,268 However, exercise capacity is also affectedby age, general physical c<strong>on</strong>diti<strong>on</strong>, comorbidites, andpsychological state. Exercise capacity may be measured bymaximum exercise durati<strong>on</strong>, maximum MET level achieved,maximum workload achieved in Watts, maximum heart rate,and double (rate–pressure) product. The specific variableused to measure exercise capacity is less important than<strong>the</strong> inclusi<strong>on</strong> <strong>of</strong> this marker in <strong>the</strong> assessment. In patientswith known CAD and normal, or mildly impaired LV functi<strong>on</strong>,5-year survival is higher in patients with a better exercisetolerance. 123,139,152,269,270O<strong>the</strong>r prognostic exercise testing markers are related toexercise-induced ischaemia and markers include changesin ST-segment (depressi<strong>on</strong> or elevati<strong>on</strong>), and exerciseinducedangina. McNeer et al. 270 dem<strong>on</strong>strated that anearly positive exercise test (ST-depressi<strong>on</strong> .1 mm in <strong>the</strong>first two stages <strong>of</strong> <strong>the</strong> Bruce protocol) identified a high-riskpopulati<strong>on</strong>, whereas patients who could exercise into stageIV were at low risk regardless <strong>of</strong> <strong>the</strong> ST resp<strong>on</strong>se. ST-segmentelevati<strong>on</strong> is observed most frequently in patients with ahistory <strong>of</strong> MI; in patients without infarcti<strong>on</strong>, ST-elevati<strong>on</strong>during exercise has been associated with severe transmuralmyocardial ischaemia.In <strong>the</strong> CASS Registry, 12% <strong>of</strong> medically treated patientswere identified as high risk <strong>on</strong> <strong>the</strong> basis <strong>of</strong> 0.1 mV <strong>of</strong>exercise-induced ST-segment depressi<strong>on</strong> and inability tocomplete stage I <strong>of</strong> <strong>the</strong> Bruce protocol. These patients hadan average mortality rate <strong>of</strong> 5% per year. Patients whocould exercise to at least stage III <strong>of</strong> <strong>the</strong> Bruce protocolwithout ST changes (34%) c<strong>on</strong>stituted <strong>the</strong> low-risk group(estimated annual mortality, less than 1%). 123Several studies have attempted to incorporate multipleexercise variables into a prognostic score. The clinicalvalue <strong>of</strong> stress testing is improved c<strong>on</strong>siderably by
20 ESC <str<strong>on</strong>g>Guidelines</str<strong>on</strong>g>multivariable analysis including several exercise variables ina given patient such as <strong>the</strong> combinati<strong>on</strong> <strong>of</strong> heart rate atpeak exercise, ST-segment depressi<strong>on</strong>, <strong>the</strong> presence orabsence <strong>of</strong> angina during <strong>the</strong> test, peak workload, andST-segment slope. 152,271–273The Duke treadmill score (DTS) is a well validated scorewhich combines exercise time, ST-deviati<strong>on</strong>, and anginaduring exercise to calculate <strong>the</strong> patient’s risk. 152,272 TheDTS equals <strong>the</strong> exercise time in minutes minus (five times<strong>the</strong> ST-segment deviati<strong>on</strong>, during or after exercise in millimetres)minus (four times <strong>the</strong> angina index, which has avalue <strong>of</strong> ‘0’ if <strong>the</strong>re is no angina, ‘1’ if angina occurs, and‘2’ if <strong>the</strong> angina is <strong>the</strong> reas<strong>on</strong> for stopping <strong>the</strong> test(Figure 4). In <strong>the</strong> original descripti<strong>on</strong> <strong>of</strong> this score in a populati<strong>on</strong>with suspected CAD, two-thirds <strong>of</strong> patients withscores indicating low-risk had a 4-year survival rate <strong>of</strong> 99%(average annual mortality rate 0.25%), and <strong>the</strong> 4% who hadscores indicating high-risk had a 4-year survival rate <strong>of</strong> 79%(average annual mortality rate 5%). The combinati<strong>on</strong> <strong>of</strong>exercise and clinical parameters, with or without <strong>the</strong> use<strong>of</strong> scores such as <strong>the</strong> DTS, has been shown to be an effectivemethod <strong>of</strong> discriminating between high- and low-risk groupswithin a populati<strong>on</strong> presenting with known or suspectedcor<strong>on</strong>ary disease (Figure 5).Stress echocardiography. Stress echocardiography may alsobe used effectively to stratify patients according to <strong>the</strong>irrisk <strong>of</strong> subsequent cardiovascular events 158,274 and similarlyhas an excellent negative predictive value, 275,276 in patientswith a negative test having a hard event rate (death or MI) <strong>of</strong>,0.5%/year. The risk <strong>of</strong> future events is influenced both by<strong>the</strong> number <strong>of</strong> resting regi<strong>on</strong>al wall moti<strong>on</strong> abnormalitiesand inducible wall moti<strong>on</strong> abnormalities <strong>on</strong> stress echocardiography,with more resting abnormalities and a greateramount <strong>of</strong> inducible ischaemia associated with higherrisk. 155 Identificati<strong>on</strong> <strong>of</strong> a high risk cohort allows for appropriatefur<strong>the</strong>r investigati<strong>on</strong> and/or interventi<strong>on</strong>.Stress perfusi<strong>on</strong> scintigraphy. SPECT perfusi<strong>on</strong> scintigraphyis a useful method <strong>of</strong> n<strong>on</strong>-invasive risk stratificati<strong>on</strong>,readily identifying those patients at greatest risk for subsequentdeath and MI. Normal stress myocardial perfusi<strong>on</strong>images are highly predictive <strong>of</strong> a benign prognosis. Severalstudies involving thousands <strong>of</strong> patients have found that anormal stress perfusi<strong>on</strong> study is associated with a subsequentrate <strong>of</strong> cardiac death and MI <strong>of</strong> less than 1% peryear, which is nearly as low as that <strong>of</strong> <strong>the</strong> general populati<strong>on</strong>.169,170,277 The <strong>on</strong>ly excepti<strong>on</strong>s would appear inpatients with normal perfusi<strong>on</strong> images with ei<strong>the</strong>r a highrisktreadmill ECG score or severe resting LV dysfuncti<strong>on</strong>. 278In c<strong>on</strong>trast, abnormal findings <strong>on</strong> stress perfusi<strong>on</strong>scintigraphy have been associated with severe CAD, andFigure 4 Duke treadmill score. 272subsequent cardiac events. Large stress-induced perfusi<strong>on</strong>defects, defects in multiple cor<strong>on</strong>ary artery territories,transient post-stress ischaemic LV dilatati<strong>on</strong>, and in patientsstudied with 201 Th, increased lung uptake 279 <strong>on</strong> postexerciseor pharmacological stress images are all adverseprognostic indicators. 158,174,277,278The results <strong>of</strong> planar and SPECT perfusi<strong>on</strong> scintigraphy canbe used to identify a ‘high-risk’ patient subset. Thesepatients, who have a greater than 3% annual mortalityrate, should be c<strong>on</strong>sidered for early cor<strong>on</strong>ary arteriography,as <strong>the</strong>ir prognosis may be improved by revascularizati<strong>on</strong>.Exercise scintigraphy <strong>of</strong>fers greater prognostic informati<strong>on</strong>than pharmacological stress imaging because <strong>of</strong> <strong>the</strong> informati<strong>on</strong>regarding symptoms, exercise tolerance, andhaemodynamic resp<strong>on</strong>se to exercise which is additive tothat obtained from perfusi<strong>on</strong> data al<strong>on</strong>e.Recommendati<strong>on</strong>s for risk stratificati<strong>on</strong> according toexercise stress ECG in stable angina in patients who canexerciseClass I(1) All patients without significant resting ECG abnormalitiesundergoing initial evaluati<strong>on</strong> (level <strong>of</strong> evidence B)(2) Patients with stable cor<strong>on</strong>ary disease after a significantchange in symptom level (level <strong>of</strong> evidence C)Class IIa(1) Patients post-revascularizati<strong>on</strong> with a significantdeteriorati<strong>on</strong> in symptomatic status (level <strong>of</strong> evidenceB)Recommendati<strong>on</strong>s for risk stratificati<strong>on</strong> according toexercise stress imaging (perfusi<strong>on</strong> or echocardiography)in stable angina in patients who can exerciseClass I(1) Patients with resting ECG abnormalities, LBBB, .1 mmST-depressi<strong>on</strong>, paced rhythm, or WPW which preventaccurate interpretati<strong>on</strong> <strong>of</strong> ECG changes during stress(level <strong>of</strong> evidence C)(2) Patients with a n<strong>on</strong>-c<strong>on</strong>clusive exercise ECG, but intermediateor high probability <strong>of</strong> disease (level <strong>of</strong> evidenceB)Class IIa(1) In patients with a deteriorati<strong>on</strong> in symptoms postrevascularizati<strong>on</strong>(level <strong>of</strong> evidence B)(2) As an alternative to exercise ECG in patients wherefacilities, cost, and pers<strong>on</strong>nel resources allow (level<strong>of</strong> evidence B)Recommendati<strong>on</strong>s for risk stratificati<strong>on</strong> according topharmacological stress imaging (perfusi<strong>on</strong> or echocardiography)in stable anginaClass I(1) Patients who cannot exerciseO<strong>the</strong>r class I and II indicati<strong>on</strong>s as for exercise stressimaging (perfusi<strong>on</strong> or echocardiography) in stable angina inpatients who can exercise, but where local facilities d<strong>on</strong>ot include exercise imaging.Risk stratificati<strong>on</strong> using ventricular functi<strong>on</strong>The str<strong>on</strong>gest predictor <strong>of</strong> l<strong>on</strong>g-term survival is LV functi<strong>on</strong>.In patients with stable angina as LV ejecti<strong>on</strong> fracti<strong>on</strong> (EF)
ESC <str<strong>on</strong>g>Guidelines</str<strong>on</strong>g> 21Figure 5 Prognostic stratificati<strong>on</strong> according to combined clinical and exercise variables. 52,270–273,681–683declines, mortality increases. A resting EF <strong>of</strong> less than 35% isassociated with an annual mortality rate greater than 3% peryear. 67,123,124,280L<strong>on</strong>g-term follow-up data from <strong>the</strong> CASS registry showedthat 72% <strong>of</strong> <strong>the</strong> deaths occurred in <strong>the</strong> 38% <strong>of</strong> <strong>the</strong> populati<strong>on</strong>that had ei<strong>the</strong>r LV dysfuncti<strong>on</strong> or severe cor<strong>on</strong>ary disease.The 12-year survival rate <strong>of</strong> patients with EF .50% was35–49% 280 and ,35% were 73, 54, and 21%, respectively(P , 0.0001). The prognosis <strong>of</strong> patients with a normal ECGand low clinical risk for severe CAD is, <strong>on</strong> <strong>the</strong> o<strong>the</strong>r hand,excellent. 261Ventricular functi<strong>on</strong> affords additi<strong>on</strong>al prognostic informati<strong>on</strong>to cor<strong>on</strong>ary anatomy, with reported 5-year survivalrates <strong>of</strong> a man with stable angina and three-vessel diseaseranging from 93% in those with normal ventricular functi<strong>on</strong>to 58% with reduced ventricular functi<strong>on</strong>. 67 Impaired ventricularfuncti<strong>on</strong> may be inferred from extensive Q-wave <strong>on</strong>ECG, symptoms or signs <strong>of</strong> heart failure, or measured n<strong>on</strong>invasivelyby echocardiography, radi<strong>on</strong>uclide techniques orc<strong>on</strong>trast ventriculography at <strong>the</strong> time <strong>of</strong> cor<strong>on</strong>aryarteriography.Clinical evaluati<strong>on</strong> as outlined earlier may indicate whichpatients have heart failure, and thus at substantiallyincreased risk for future cardiovascular events. However,<strong>the</strong> prevalence <strong>of</strong> asymptomatic ventricular dysfuncti<strong>on</strong> isnot inc<strong>on</strong>siderable, 281–283 and has been reported to be ashigh as twice that <strong>of</strong> clinical heart failure, with <strong>the</strong> presence<strong>of</strong> ischaemic heart disease a major risk factor for itsoccurrence.Ventricular dimensi<strong>on</strong>s have been shown to c<strong>on</strong>tributeuseful prognostic informati<strong>on</strong> which is incremental to <strong>the</strong>results <strong>of</strong> exercise testing in a stable angina populati<strong>on</strong> with2-year follow-up. 284 In a study <strong>of</strong> hypertensive patientswithout angina, <strong>the</strong> use <strong>of</strong> echocardiography to assess ventricularstructure and functi<strong>on</strong> was associated with reclassificati<strong>on</strong>from medium/low risk to high risk in 37% <strong>of</strong> patients, 285and <strong>the</strong> European guidelines for <strong>the</strong> management <strong>of</strong> hypertensi<strong>on</strong>recommend an echocardiogram for patients withhypertensi<strong>on</strong>. 286 Diabetic patients with angina also requireparticular attenti<strong>on</strong>. Echocardiography in diabetic individualswith angina has <strong>the</strong> advantage <strong>of</strong> identifying LVH and diastolicas well as systolic dysfuncti<strong>on</strong>, all <strong>of</strong> which are more prevalentin <strong>the</strong> diabetic populati<strong>on</strong>. Thus, an estimati<strong>on</strong> <strong>of</strong> ventricularfuncti<strong>on</strong> is desirable in risk stratificati<strong>on</strong> <strong>of</strong> patients withstable angina, and an assessment for ventricular hypertrophy(by echocardiography or MRI), as well as assessment <strong>of</strong> ventricularfuncti<strong>on</strong> is particularly pertinent in patients with hypertensi<strong>on</strong>or diabetes. For most o<strong>the</strong>r patients <strong>the</strong> choice <strong>of</strong>investigati<strong>on</strong> to determine ventricular functi<strong>on</strong> will be dependent<strong>on</strong> <strong>the</strong> o<strong>the</strong>r tests which have been performed or areplanned, or <strong>the</strong> level <strong>of</strong> risk estimated by o<strong>the</strong>r methods. Forexample, in a patient who has a stress imaging test it may bepossible to estimate ventricular functi<strong>on</strong> from this testwithout additi<strong>on</strong>al investigati<strong>on</strong>, or a patient scheduled tohave cor<strong>on</strong>ary arteriography <strong>on</strong> <strong>the</strong> basis <strong>of</strong> a str<strong>on</strong>gly positiveexercise test at low workload, in <strong>the</strong> absence <strong>of</strong> prior MI, oro<strong>the</strong>r indicati<strong>on</strong>s for echocardiography, may have ventricularsystolic functi<strong>on</strong> assessed at <strong>the</strong> time <strong>of</strong> arteriography.Recommendati<strong>on</strong>s for risk stratificati<strong>on</strong> by echocardiographicevaluati<strong>on</strong> <strong>of</strong> ventricular functi<strong>on</strong> in stable anginaClass I(1) Resting echocardiography in patients with prior MI,symptoms or signs <strong>of</strong> heart failure, or resting ECGabnormalities (level <strong>of</strong> evidence B)(2) Resting echocardiography in patients with hypertensi<strong>on</strong>(level <strong>of</strong> evidence B)(3) Resting echocardiography in patients with diabetes(level <strong>of</strong> evidence C)Class IIa(1) Resting echocardiography in patients with a normalresting ECG without prior MI who are not o<strong>the</strong>rwise tobe c<strong>on</strong>sidered for cor<strong>on</strong>ary arteriography (level <strong>of</strong>evidence C)
22 ESC <str<strong>on</strong>g>Guidelines</str<strong>on</strong>g>Risk stratificati<strong>on</strong> using cor<strong>on</strong>ary arteriographyDespite <strong>the</strong> recognized limitati<strong>on</strong>s <strong>of</strong> cor<strong>on</strong>ary arteriographyto identify vulnerable plaques which are likely to lead toacute cor<strong>on</strong>ary events, <strong>the</strong> extent, severity <strong>of</strong> luminalobstructi<strong>on</strong>, and locati<strong>on</strong> <strong>of</strong> cor<strong>on</strong>ary disease <strong>on</strong> cor<strong>on</strong>aryarteriography have been c<strong>on</strong>vincingly dem<strong>on</strong>strated to beimportant prognostic indicators in patients withangina. 67,124,287,288Several prognostic indices have been used to relatedisease severity to <strong>the</strong> risk <strong>of</strong> subsequent cardiac events;<strong>the</strong> simplest and most widely used is <strong>the</strong> classificati<strong>on</strong> <strong>of</strong>disease into <strong>on</strong>e vessel, two vessel, three vessel, or LMCAD. In <strong>the</strong> CASS registry <strong>of</strong> medically treated patients,<strong>the</strong> 12-year survival rate <strong>of</strong> patients with normal cor<strong>on</strong>aryarteries was 91% compared with 74% for those with <strong>on</strong>evesseldisease, 59% for those with two vessel disease and50% for those with three vessel disease (P , 0.001). 280Patients with severe stenosis <strong>of</strong> <strong>the</strong> LM cor<strong>on</strong>ary arteryhave a poor prognosis when treated medically. The presence<strong>of</strong> severe proximal left anterior descending artery (LAD)disease also significantly reduces <strong>the</strong> survival rate. The5-year survival rate with three-vessel disease plus greaterthan 95% proximal LAD stenosis was reported to be 54% comparedwith a rate <strong>of</strong> 79% with three-vessel disease withoutLAD stenosis. 288 However, it should be appreciated that in<strong>the</strong>se ‘older’ studies preventive <strong>the</strong>rapy was not at <strong>the</strong>level <strong>of</strong> current recommendati<strong>on</strong>s regarding both lifestyleand drug <strong>the</strong>rapy. Accordingly, absolute estimates <strong>of</strong> riskderived from <strong>the</strong>se studies, in general, over-estimate <strong>the</strong>risk <strong>of</strong> future events.Recent angiographic studies indicate that a direct correlati<strong>on</strong>exists between <strong>the</strong> angiographic severity <strong>of</strong> cor<strong>on</strong>arydisease and <strong>the</strong> amount <strong>of</strong> angiographically insignificantplaques in <strong>the</strong> cor<strong>on</strong>ary tree. 289 The higher mortality ratesin patients with multivessel disease may be a c<strong>on</strong>sequence<strong>of</strong> a higher number <strong>of</strong> mildly stenotic and n<strong>on</strong>-stenoticplaques that are potential sites for acute cor<strong>on</strong>ary eventsthan those with <strong>on</strong>e-vessel disease.The major focus in n<strong>on</strong>-invasive risk stratificati<strong>on</strong> is <strong>on</strong>subsequent patient mortality, with <strong>the</strong> rati<strong>on</strong>ale to identifypatients in whom cor<strong>on</strong>ary arteriography and subsequentrevascularizati<strong>on</strong> might decrease mortality, that is thosewith three-vessel disease, LM CAD, and proximal anteriordescending CAD. 69,290When appropriately used, n<strong>on</strong>-invasive tests have anacceptable predictive value for adverse events; this ismost true when <strong>the</strong> pre-test probability <strong>of</strong> severe CAD islow. When <strong>the</strong> estimated annual cardiovascular mortalityrate is less than or equal to 1%, <strong>the</strong> use <strong>of</strong> cor<strong>on</strong>ary arteriographyto identify patients whose prognosis can be improvedis likely to be inappropriate; in c<strong>on</strong>trast it is appropriate forpatients whose cardiovascular mortality risk is greater than2% per annum. Decisi<strong>on</strong>s regarding <strong>the</strong> need to proceed toarteriography in <strong>the</strong> intermediate risk group, those with anannual cardiovascular mortality <strong>of</strong> 1–2% should be guidedby a variety <strong>of</strong> factors including <strong>the</strong> patient’s symptoms,functi<strong>on</strong>al status, lifestyle, occupati<strong>on</strong>, comorbidity, andresp<strong>on</strong>se to initial <strong>the</strong>rapy.With increasing public and media interest in availablemedical technology, widespread access to <strong>the</strong> internet ando<strong>the</strong>r sources <strong>of</strong> informati<strong>on</strong>, patients will <strong>of</strong>ten have c<strong>on</strong>siderableinformati<strong>on</strong> regarding investigati<strong>on</strong> and treatmentopti<strong>on</strong>s for <strong>the</strong>ir c<strong>on</strong>diti<strong>on</strong>. It is <strong>the</strong> duty <strong>of</strong> <strong>the</strong> physician toensure that <strong>the</strong> patient is fully informed <strong>of</strong> <strong>the</strong>ir risk and<strong>the</strong> potential benefits or lack <strong>of</strong> benefit <strong>of</strong> any particularprocedure, and to guide <strong>the</strong>ir decisi<strong>on</strong> appropriately.Some patients may still c<strong>on</strong>sider medical treatmentra<strong>the</strong>r than interventi<strong>on</strong>, or an element <strong>of</strong> doubt regardingdiagnosis, to be unacceptable regardless <strong>of</strong> <strong>the</strong> evidencepresented to <strong>the</strong>m. Cor<strong>on</strong>ary arteriography should not beperformed in patients with angina who refuse invasive procedures,prefer to avoid revascularizati<strong>on</strong>, who are notcandidates for PCI or CABG, or in whom it will not improvequality <strong>of</strong> life.Recommendati<strong>on</strong>s for risk stratificati<strong>on</strong> by cor<strong>on</strong>aryarteriography in patients with stable anginaClass I(1) Patients determined to be at high risk for adverseoutcome <strong>on</strong> <strong>the</strong> basis <strong>of</strong> n<strong>on</strong>-invasive testing even if<strong>the</strong>y present with mild or moderate symptoms <strong>of</strong>angina (level <strong>of</strong> evidence B)(2) Severe stable angina (Class 3 <strong>of</strong> Canadian<strong>Cardio</strong>vascular Society Classificati<strong>on</strong> (CCS), particularlyif <strong>the</strong> symptoms are inadequately resp<strong>on</strong>ding tomedical treatment (level <strong>of</strong> evidence B)(3) <strong>Stable</strong> angina in patients who are being c<strong>on</strong>sidered formajor n<strong>on</strong>-cardiac surgery, especially vascular surgery(repair <strong>of</strong> aortic aneurysm, femoral bypass, carotidendarterectomy) with intermediate or high risk features<strong>on</strong> n<strong>on</strong>-invasive testing (level <strong>of</strong> evidence B)Class IIa(1) Patients with an inc<strong>on</strong>clusive diagnosis <strong>on</strong> n<strong>on</strong>-invasivetesting, or c<strong>on</strong>flicting results from different n<strong>on</strong>invasivemodalities (level <strong>of</strong> evidence C)(2) Patients with a high risk <strong>of</strong> restenosis after PCI if PCIhas been performed in a prognostically important site(level <strong>of</strong> evidence C)Special diagnostic c<strong>on</strong>siderati<strong>on</strong>s: anginawith ‘normal’ cor<strong>on</strong>ary arteriesThe clinicopathological correlati<strong>on</strong> <strong>of</strong> symptoms with cor<strong>on</strong>aryanatomy varies widely in angina from typical symptoms<strong>of</strong> angina due to significant cor<strong>on</strong>ary lesi<strong>on</strong>s causing transientischaemia when myocardial demand is increased, toclearly n<strong>on</strong>-cardiac chest pain with normal cor<strong>on</strong>ary arteriesFigure 6 Schematic representati<strong>on</strong> <strong>of</strong> clinico-pathological variants inangina.
ESC <str<strong>on</strong>g>Guidelines</str<strong>on</strong>g> 23<strong>on</strong> <strong>the</strong> o<strong>the</strong>r end <strong>of</strong> <strong>the</strong> spectrum. Spanning <strong>the</strong> extremes <strong>of</strong>this spectrum are a number <strong>of</strong> clinicopathological correlateswhich may overlap to a greater or lesser extent with eacho<strong>the</strong>r (Figure 6). These range from atypical anginal symptomswith significant cor<strong>on</strong>ary stenoses, which would fallunder <strong>the</strong> umbrella <strong>of</strong> <strong>the</strong> c<strong>on</strong>venti<strong>on</strong>al diagnosis <strong>of</strong> anginapectoris, to typical anginal symptoms with angiographicallynormal cor<strong>on</strong>ary arteries which might be described ascardiac Syndrome X. Vasospastic angina, caused by dynamiccor<strong>on</strong>ary obstructi<strong>on</strong> in cor<strong>on</strong>ary arteries which may beei<strong>the</strong>r angiographically smooth or significantly stenosed, is afur<strong>the</strong>r factor to be c<strong>on</strong>sidered in <strong>the</strong> diagnosis. A c<strong>on</strong>siderableproporti<strong>on</strong> <strong>of</strong> patients, especially women, who undergocor<strong>on</strong>ary arteriography because <strong>of</strong> symptoms <strong>of</strong> chest paindo not have significant CAD. 291 In <strong>the</strong>se patients, <strong>the</strong> features<strong>of</strong> chest pain may suggest <strong>on</strong>e <strong>of</strong> <strong>the</strong> following threepossibilities.. Pain involves a small porti<strong>on</strong> <strong>of</strong> <strong>the</strong> left hemithorax, lastsfor several hours or even days, is not relieved by nitroglycerin,and may be provoked by palpati<strong>on</strong> (n<strong>on</strong>-anginalpain, <strong>of</strong>ten musculoskeletal in origin). Pain has typical features <strong>of</strong> angina in terms <strong>of</strong> locati<strong>on</strong> anddurati<strong>on</strong> but occurs predominantly at rest (atypicalangina, which may be due to cor<strong>on</strong>ary spasm vasospasticangina). <strong>Angina</strong> with mostly typical features (although durati<strong>on</strong>may be prol<strong>on</strong>ged, and relati<strong>on</strong> to exercise somewhatinc<strong>on</strong>sistent) associated with abnormal results <strong>of</strong> stresstests (cardiac Syndrome X)Detailed discussi<strong>on</strong> <strong>of</strong> <strong>the</strong> management <strong>of</strong> <strong>the</strong> first groupis bey<strong>on</strong>d <strong>the</strong> scope <strong>of</strong> <strong>the</strong>se guidelines. With regard to<strong>the</strong> ‘atypical angina’ group, in general this term refers tosymptoms with any two <strong>of</strong> <strong>the</strong> three main features <strong>of</strong>typical angina pectoris as outlined in Table 2, and <strong>the</strong>term may be used interchangeably with ‘probable angina’.Suspected vasospastic angina is a specific subgroup <strong>of</strong> atypicalangina which is atypical <strong>on</strong>ly in that it lacks a c<strong>on</strong>sistentassociati<strong>on</strong> with exercise. O<strong>the</strong>r forms <strong>of</strong> atypical angina arenot discussed separately, but a brief descripti<strong>on</strong> <strong>of</strong> <strong>the</strong> diagnosticevaluati<strong>on</strong> <strong>of</strong> cardiac Syndrome X and vasospasticangina are outlined below.Syndrome XClinical picture. Although <strong>the</strong>re is no universally accepteddefiniti<strong>on</strong> <strong>of</strong> Syndrome X, to fulfil <strong>the</strong> classical descripti<strong>on</strong><strong>of</strong> ‘Syndrome X’ 292 requires <strong>the</strong> presence <strong>of</strong> <strong>the</strong> triad <strong>of</strong>:(1) Typical exercise-induced angina (with or withoutadditi<strong>on</strong>al resting angina and dyspnoea)(2) Positive exercise stress ECG or o<strong>the</strong>r stress imagingmodality(3) Normal cor<strong>on</strong>ary arteriesChest pain occurs frequently and anginal attacks areusually encountered several times per week, but with astable pattern. Therefore, Syndrome X resembles chr<strong>on</strong>icstable angina. However, <strong>the</strong> clinical presentati<strong>on</strong> <strong>of</strong> patientsincluded in ‘Syndrome X’ studies is highly variable and anginaat rest is <strong>of</strong>ten encountered in additi<strong>on</strong> to exercise-provokedchest pain. 293 Severe attacks <strong>of</strong> resting angina may promptrecurrent emergency presentati<strong>on</strong>s, and hospital admissi<strong>on</strong>swith an inaccurate diagnosis <strong>of</strong> unstable angina leading toinappropriate diagnostic and <strong>the</strong>rapeutic procedures.In a subset <strong>of</strong> patients with Syndrome X, microvasculardysfuncti<strong>on</strong> can be dem<strong>on</strong>strated and this entity is comm<strong>on</strong>lyreferred to as ‘microvascular angina’. 294Arterial hypertensi<strong>on</strong>, ei<strong>the</strong>r with or without associatedventricular hypertrophy, is frequently encountered in <strong>the</strong>populati<strong>on</strong> with chest pain and ‘normal cor<strong>on</strong>ary arteries’.Hypertensive heart disease is characterized by endo<strong>the</strong>lialdysfuncti<strong>on</strong>, 295 LVH, interstitial and perivascular fibrosis withdiastolic dysfuncti<strong>on</strong> 296 changes in myocardial and cor<strong>on</strong>aryultrastructure. 297 and reduced cor<strong>on</strong>ary flow reserve. 298Toge<strong>the</strong>r or separately <strong>the</strong>se changes may compromisecor<strong>on</strong>ary blood flow relative to myocardial oxygen demand,causing angina. For <strong>the</strong> most part, treatment in such casesshould focus <strong>on</strong> c<strong>on</strong>trol <strong>of</strong> hypertensi<strong>on</strong> to restore functi<strong>on</strong>aland structural integrity <strong>of</strong> <strong>the</strong> cardiovascular system. 299Pathogenesis. The mechanism <strong>of</strong> chest pain in patients withangina despite a normal cor<strong>on</strong>ary angiogram c<strong>on</strong>tinues to bec<strong>on</strong>troversial. Functi<strong>on</strong>al abnormalities <strong>of</strong> <strong>the</strong> cor<strong>on</strong>arymicrocirculati<strong>on</strong> during stress, including abnormal dilatorresp<strong>on</strong>ses and a heightened resp<strong>on</strong>se to vasoc<strong>on</strong>strictors,have been c<strong>on</strong>sidered potential mechanisms <strong>of</strong> chest painand ischaemic-appearing ST-segment depressi<strong>on</strong> duringexercise. 300 However, o<strong>the</strong>rs failed to find haemodynamicor metabolic evidence <strong>of</strong> ischaemia in many patients withSyndrome X 301 but propose abnormal cardiac sensitivity(coupled with some impairment in cor<strong>on</strong>ary flow reserve)in <strong>the</strong>se patients that may lead to chest pain <strong>on</strong> a n<strong>on</strong>ischaemicbasis. 302Prognosis. Although <strong>the</strong> prognosis in terms <strong>of</strong> mortality <strong>of</strong>patients with Syndrome X appears to be favourable, 303 <strong>the</strong>morbidity <strong>of</strong> patients with Syndrome X is high 304,305 and<strong>the</strong> c<strong>on</strong>diti<strong>on</strong> is frequently associated with c<strong>on</strong>tinuing episodes<strong>of</strong> chest pain and hospital readmissi<strong>on</strong>. 306 There isemerging evidence that identificati<strong>on</strong> <strong>of</strong> impaired endo<strong>the</strong>lialdysfuncti<strong>on</strong> in this patient populati<strong>on</strong> may identifya subgroup at risk for <strong>the</strong> future development <strong>of</strong> a<strong>the</strong>roscleroticcor<strong>on</strong>ary disease 307 and with a less benign prognosisthan previously thought. 305,308–310Diagnosis <strong>of</strong> Syndrome X. Diagnosis and management <strong>of</strong>patients with chest pain and normal cor<strong>on</strong>ary arteries representa complex challenge. The diagnosis <strong>of</strong> Syndrome Xmay be made if a patient with exercise-induced angina hasnormal or n<strong>on</strong>-obstructed cor<strong>on</strong>ary arteries by arteriographybut objective signs <strong>of</strong> exercise-induced ischaemia(ST-depressi<strong>on</strong> in exercise ECG, ischaemic changes by scintigraphy).It is necessary to differentiate this pain from n<strong>on</strong>cardiacchest pain caused by oesophageal dysmotility, fibromyalgia,or costoch<strong>on</strong>dritis. Cor<strong>on</strong>ary artery spasm shouldbe excluded by appropriate provocati<strong>on</strong> tests. Endo<strong>the</strong>lialdysfuncti<strong>on</strong> may be identified by epicardial cor<strong>on</strong>aryartery diameter resp<strong>on</strong>se to acetylcholine. Invasive testingusing acetylcholine provocati<strong>on</strong> can serve a dual purposeby excluding vasospasm and unmasking endo<strong>the</strong>lial dysfuncti<strong>on</strong>,which may be associated with a worse prognosis. Incertain circumstances, for example in <strong>the</strong> presence <strong>of</strong> anextensive radi<strong>on</strong>uclide perfusi<strong>on</strong> defect or wall moti<strong>on</strong>abnormality during stress testing and an angiographicallyirregular artery, intracor<strong>on</strong>ary ultrasound may be c<strong>on</strong>sideredto exclude missed obstructive lesi<strong>on</strong>s. The excellent prognosiswhen endo<strong>the</strong>lial dysfuncti<strong>on</strong> is not present needs to be
24 ESC <str<strong>on</strong>g>Guidelines</str<strong>on</strong>g>emphasized and <strong>the</strong> patient should be informed and reassuredabout <strong>the</strong> benign course <strong>of</strong> <strong>the</strong> c<strong>on</strong>diti<strong>on</strong>.Recommendati<strong>on</strong>s for investigati<strong>on</strong> in patients withclassical triad <strong>of</strong> Syndrome XClass I(1) Resting echocardiogram in patients with angina andnormal or n<strong>on</strong>-obstructed cor<strong>on</strong>ary arteries to assessfor presence <strong>of</strong> ventricular hypertrophy and/or diastolicdysfuncti<strong>on</strong> (level <strong>of</strong> evidence C)Class IIb(1) Intracor<strong>on</strong>ary acetylcholine during cor<strong>on</strong>ary arteriography,if <strong>the</strong> arteriogram is visually normal, to assessendo<strong>the</strong>lium-dependent cor<strong>on</strong>ary flow reserve, andexclude vasospasm (level <strong>of</strong> evidence C)(2) Intracor<strong>on</strong>ary ultrasound, cor<strong>on</strong>ary flow reserve, or FFRmeasurement to exclude missed obstructive lesi<strong>on</strong>s, ifangiographic appearances are suggestive <strong>of</strong> a n<strong>on</strong>obstructivelesi<strong>on</strong> ra<strong>the</strong>r than completely normal, andstress imaging techniques identify an extensive area<strong>of</strong> ischaemia (level <strong>of</strong> evidence C)Vasospastic/variant anginaClinical picture. Patients with variant or vasospastic anginapresent with typically located pain, which occurs at rest,but does not, or <strong>on</strong>ly occasi<strong>on</strong>ally, occurs with exerti<strong>on</strong>.Such pain characteristics are <strong>of</strong>ten caused by cor<strong>on</strong>aryartery spasm, especially when <strong>the</strong> pain occurs at night andin <strong>the</strong> early morning hours. 311 If <strong>the</strong> chest pain is severe,this may lead to hospital admissi<strong>on</strong>. Nitrates usually relieve<strong>the</strong> pain within minutes. The terms vasospastic or variantangina may be used to describe such symptoms, although‘Prinzmetal angina’ 312 has also been used. This term wasinitially used to describe patients with clearly documentedST-elevati<strong>on</strong> during chest pain due to cor<strong>on</strong>ary spasm.<strong>Angina</strong> at rest with preserved exercise tolerance may alsobe associated with significant obstructive cor<strong>on</strong>ary diseasewithout dem<strong>on</strong>strable vasospasm, and management is as outlinedfor typical symptoms. In <strong>the</strong> case <strong>of</strong> chest pain withoutsignificant cor<strong>on</strong>ary disease or cor<strong>on</strong>ary spasm, and no dem<strong>on</strong>strableischaemia, n<strong>on</strong>-cardiac causes <strong>of</strong> pain should be c<strong>on</strong>sideredand c<strong>on</strong>venti<strong>on</strong>al primary preventi<strong>on</strong> adhered to.Asubstantialproporti<strong>on</strong> <strong>of</strong>patients withahistorysuggestive<strong>of</strong> vasospastic angina have obstructive cor<strong>on</strong>ary disease 313 andin such patients vasospastic angina may co-exist with typicalexerti<strong>on</strong>al angina due to fixed cor<strong>on</strong>ary lesi<strong>on</strong>s. N<strong>on</strong>exerti<strong>on</strong>alsymptoms due to vasospasm may also occur inpatients with minimal or no angiographically evident cor<strong>on</strong>arydisease, and typical exerti<strong>on</strong>al angina and dyspnoeamay also occur in patients with vasospasm but entirelynormal cor<strong>on</strong>ary arteries. This indicates some overlap withpatients suffering from Syndrome X (Figure 6). 314 The prevalence<strong>of</strong> vasospastic angina is difficult to assess, not leastbecause <strong>of</strong> its overlap with typical angina and Syndrome X.Vasospasm may occur in resp<strong>on</strong>se to smoking, electrolytedisturbances (potassium, magnesium), cocaine use, coldstimulati<strong>on</strong>, autoimmune diseases, hyperventilati<strong>on</strong> orinsulin resistance. There is also an ethnic pre-dispositi<strong>on</strong>,with a higher prevalence in Japanese populati<strong>on</strong>s.Pathogenesis. The mechanisms leading to vasospastic anginaare not entirely clear, but hyperreactivity <strong>of</strong> smooth musclecells <strong>of</strong> <strong>the</strong> involved cor<strong>on</strong>ary segment 315 mayplayarole,and endo<strong>the</strong>lial dysfuncti<strong>on</strong> may also be involved. 316,317 Thecauses <strong>of</strong> smooth muscle cell hyperreactivity are unknown,but several possible c<strong>on</strong>tributing factors have beensuggested, including increased cellular rho-kinase activity, 318abnormalities in ATP-sensitive potassium channels, 319 andmembrane Na þ -H þ countertransport. 320 O<strong>the</strong>r c<strong>on</strong>tributingfactors may be imbalances in <strong>the</strong> aut<strong>on</strong>omic nervoussystem, 321,322 enhanced intracor<strong>on</strong>ary c<strong>on</strong>centrati<strong>on</strong>s <strong>of</strong>vasoc<strong>on</strong>stricting substances, such as endo<strong>the</strong>lin, 323 andhorm<strong>on</strong>al changes, such as post-oopherectomy. 324,325Natural history and prognosis. The prognosis <strong>of</strong> vasospasticangina depends <strong>on</strong> <strong>the</strong> extent <strong>of</strong> underlying CAD. Deathand MI are not frequent in patients without angiographicallysignificant obstructive disease, but do occur. 326 Cor<strong>on</strong>arydeath in <strong>the</strong> populati<strong>on</strong> with n<strong>on</strong>-obstructive lesi<strong>on</strong>s hasbeen reported as 0.5% per annum, 327,328 but those withspasm superimposed <strong>on</strong> stenotic lesi<strong>on</strong>s do significantlyless well. 327,329–332Diagnosis <strong>of</strong> vasospastic anginaElectrocardiography. The ECG during vasospasm is classicallydescribed as showing ST-elevati<strong>on</strong>. 312 In o<strong>the</strong>rs, ST-depressi<strong>on</strong>can be documented, 333 whereas o<strong>the</strong>rs may show noST-segment shift at all. 334,335 However, as attacks tend toresolve quickly, 12-lead ECG documentati<strong>on</strong> tends to be difficult.Repeated 24 h ECG m<strong>on</strong>itoring may be able to captureST-segment shifts associated with anginal symptoms in<strong>the</strong>se patients. 336Cor<strong>on</strong>ary arteriography. Although <strong>the</strong> dem<strong>on</strong>strati<strong>on</strong> <strong>of</strong>ST-elevati<strong>on</strong> at <strong>the</strong> time <strong>of</strong> angina and a normal cor<strong>on</strong>aryarteriogram make <strong>the</strong> diagnosis <strong>of</strong> variant angina highlylikely, <strong>the</strong>re is <strong>of</strong>ten uncertainty about <strong>the</strong> diagnosis inless well-documented or clinically less straight forwardcases. Moreover, <strong>the</strong>re is no unanimously accepted definiti<strong>on</strong><strong>of</strong> what c<strong>on</strong>stitutes cor<strong>on</strong>ary vasospasm.Sp<strong>on</strong>taneous spasm during cor<strong>on</strong>ary arteriography is <strong>on</strong>lyoccasi<strong>on</strong>ally observed in patients with symptoms suggestive<strong>of</strong> vasospastic angina. Hence, provocati<strong>on</strong> tests are comm<strong>on</strong>lyused to dem<strong>on</strong>strate <strong>the</strong> presence <strong>of</strong> cor<strong>on</strong>ary vasospasm.337 Hyperventilati<strong>on</strong> and <strong>the</strong> cold pressor test have<strong>on</strong>ly a ra<strong>the</strong>r limited sensitivity for <strong>the</strong> detecti<strong>on</strong> <strong>of</strong>cor<strong>on</strong>ary spasm. 338 Thus, acetylcholine injecti<strong>on</strong>s into <strong>the</strong>cor<strong>on</strong>ary artery 339 are used in most centres today, but intracor<strong>on</strong>aryerg<strong>on</strong>ovine provocati<strong>on</strong> gives similar results. 340,341Acetylcholine is injected in incremental doses <strong>of</strong> 10, 25, 50and 100 mg separated by 5 min intervals. Intravenous erg<strong>on</strong>ovinemay also be used but may be associated with morediffuse spasm, which is not desirable.Cor<strong>on</strong>ary spasm may be focal or diffuse. 335 Lumenreducti<strong>on</strong>s between 75 and 99% when compared with <strong>the</strong>diameter following nitroglycerin injecti<strong>on</strong> are defined asspasm in <strong>the</strong> literature, 342,343 whereas lumen reducti<strong>on</strong>s,30% are comm<strong>on</strong>ly seen in n<strong>on</strong>-spastic cor<strong>on</strong>ary segments344 and may represent <strong>the</strong> ‘physiological’ c<strong>on</strong>strictorresp<strong>on</strong>se to acetylcholine provocati<strong>on</strong>. 342Acetylcholine or erg<strong>on</strong>ovine provocati<strong>on</strong> <strong>of</strong> cor<strong>on</strong>aryspasm is a safe test, 341,345 if <strong>the</strong> agent is infused selectivelyinto each <strong>of</strong> <strong>the</strong> three major cor<strong>on</strong>ary arteries. N<strong>on</strong>-invasiveintravenous erg<strong>on</strong>ovine provocative testing has also beendescribed with <strong>the</strong> additi<strong>on</strong> <strong>of</strong> echocardiographic or perfusi<strong>on</strong>scintigraphy to electrocardiographic m<strong>on</strong>itoringincreasing <strong>the</strong> sensitivity and specificity <strong>of</strong> <strong>the</strong>se
ESC <str<strong>on</strong>g>Guidelines</str<strong>on</strong>g> 25tests. 346,347 However, invasive documentati<strong>on</strong> <strong>of</strong> vasospasmremains <strong>the</strong> gold standard against which diagnostic testsare evaluated, and as fatal complicati<strong>on</strong>s due to prol<strong>on</strong>gedspasm involving multiple vessels may occur with intravenousinjecti<strong>on</strong> <strong>of</strong> erg<strong>on</strong>ovine, 348 <strong>the</strong> intracor<strong>on</strong>ary route is preferred.Provocative testing without cor<strong>on</strong>ary arteriographyor provocative testing in patients with high-gradeobstructive lesi<strong>on</strong>s <strong>on</strong> cor<strong>on</strong>ary arteriography are notrecommended.Recommendati<strong>on</strong>s for diagnostic tests in suspectedvasospastic anginaClass I(1) ECG during angina if possible (level <strong>of</strong> evidence B)(2) Cor<strong>on</strong>ary arteriography in patients with characteristicepisodic chest pain and ST-segment changes thatresolve with nitrates and/or calcium antag<strong>on</strong>ists todetermine <strong>the</strong> extent <strong>of</strong> underlying cor<strong>on</strong>ary disease(level <strong>of</strong> evidence B)Class IIa(1) Intracor<strong>on</strong>ary provocative testing to identify cor<strong>on</strong>aryspasm in patients with normal findings or n<strong>on</strong>obstructivelesi<strong>on</strong>s <strong>on</strong> cor<strong>on</strong>ary arteriography and <strong>the</strong>clinical picture <strong>of</strong> cor<strong>on</strong>ary spasm (level <strong>of</strong> evidence B)(2) Ambulatory ST-segment m<strong>on</strong>itoring to identifyST-deviati<strong>on</strong> (level <strong>of</strong> evidence C)TreatmentAims <strong>of</strong> treatmentTo improve prognosis by preventing MI and death. Efforts toprevent MI and death in cor<strong>on</strong>ary disease focus primarily <strong>on</strong>reducing <strong>the</strong> incidence <strong>of</strong> acute thrombotic events and <strong>the</strong>development <strong>of</strong> ventricular dysfuncti<strong>on</strong>. These aims areachieved by lifestyle or pharmacological interventi<strong>on</strong>swhich (i) reduce plaque progessi<strong>on</strong>, (ii) stabilize plaque,by reducing inflammati<strong>on</strong> and preserving endo<strong>the</strong>lial functi<strong>on</strong>,and finally (iii) by preventing thrombosis if endo<strong>the</strong>lialdysfuncti<strong>on</strong> or plaque rupture occur. In certain circumstances,such as in patients with severe lesi<strong>on</strong>s in cor<strong>on</strong>aryarteries supplying a large area <strong>of</strong> jeopardized myocardium,revascularizati<strong>on</strong> <strong>of</strong>fers additi<strong>on</strong>al opportunities toimprove prognosis by improving existing perfusi<strong>on</strong> or providingalternative routes <strong>of</strong> perfusi<strong>on</strong>.To minimize or abolish symptoms. Lifestyle changes, drugs,and revascularizati<strong>on</strong> all have a role to play in minimizing oreradicating symptoms <strong>of</strong> angina, although not necessarily allin <strong>the</strong> same patient.General managementPatients and <strong>the</strong>ir close associates should be informed <strong>of</strong> <strong>the</strong>nature <strong>of</strong> angina pectoris, and <strong>the</strong> implicati<strong>on</strong>s <strong>of</strong> <strong>the</strong> diagnosisand <strong>the</strong> treatments that may be recommended. Thepatient can be reassured that, in most cases, both <strong>the</strong> symptoms<strong>of</strong> angina and prognosis can be improved with propermanagement. Comprehensive risk stratificati<strong>on</strong> should bec<strong>on</strong>ducted as outlined above, and particular attenti<strong>on</strong>should be paid to <strong>the</strong> elements <strong>of</strong> lifestyle that could havec<strong>on</strong>tributed to <strong>the</strong> c<strong>on</strong>diti<strong>on</strong> and which may influence prognosis,including physical activity, smoking, and dietaryhabits. The recommendati<strong>on</strong>s <strong>of</strong> <strong>the</strong> Third Joint EuropeanSocieties’ Task Force 250 <strong>on</strong> <strong>Cardio</strong>vascular DiseasePreventi<strong>on</strong> in Clinical Practice should be followed.Treatment <strong>of</strong> <strong>the</strong> acute attackPatients should be advised to rest, at least briefly, from <strong>the</strong>activity which provoked <strong>the</strong> angina and advised regarding<strong>the</strong> use <strong>of</strong> sublingual nitrate for acute relief <strong>of</strong> symptoms.It is also useful to warn <strong>the</strong> patient <strong>of</strong> <strong>the</strong> need to protectagainst potential hypotensi<strong>on</strong> by sitting <strong>on</strong> <strong>the</strong> firstnumber <strong>of</strong> occasi<strong>on</strong>s when taking sublingual nitrate andalso o<strong>the</strong>r possible side-effects, particularly headache. Theuse <strong>of</strong> prophylactic nitrate to prevent predictable episodes<strong>of</strong> angina in resp<strong>on</strong>se to exerti<strong>on</strong> can be encouraged.Patients should be informed <strong>of</strong> <strong>the</strong> need to seek medicaladvice if angina persists for .10–20 min after resting and/or is not relieved by sublingual nitrate.All preventive measures, pharmacological and n<strong>on</strong>pharmacological,described in this document apply similarlyto men and women, 349 even if <strong>the</strong>re is less documentati<strong>on</strong> <strong>of</strong>health benefits am<strong>on</strong>g female compared with male patientswith stable angina pectoris and <strong>the</strong> clinical presentati<strong>on</strong> <strong>of</strong><strong>the</strong> disease may differ between genders. Risk factors, clinicalpresentati<strong>on</strong>, and <strong>the</strong> level <strong>of</strong> risk for serious cardiovascularcomplicati<strong>on</strong>s should determine <strong>the</strong> need forpreventive and <strong>the</strong>rapeutic interventi<strong>on</strong>s, ra<strong>the</strong>r than <strong>the</strong>gender <strong>of</strong> <strong>the</strong> patient. Recommendati<strong>on</strong>s c<strong>on</strong>cerninghorm<strong>on</strong>e replacement <strong>the</strong>rapy have changed and are commentedup<strong>on</strong> subsequently.SmokingCigarette smoking should be str<strong>on</strong>gly discouraged, as <strong>the</strong>reis abundant evidence that it is <strong>the</strong> most important reversiblerisk factor in <strong>the</strong> genesis <strong>of</strong> cor<strong>on</strong>ary disease in manypatients. 350,351 Cessati<strong>on</strong> <strong>of</strong> smoking greatly improves bothsymptoms and prognosis. Patients <strong>of</strong>ten require specialhelp in aband<strong>on</strong>ing <strong>the</strong>ir addicti<strong>on</strong>, and nicotine replacement<strong>the</strong>rapy has proved effective and safe in helpingpatients with CAD to quit smoking. 352–355Diet and alcoholDietary interventi<strong>on</strong>s are effective in <strong>the</strong> preventi<strong>on</strong> <strong>of</strong>events in patients with established CAD, when properlyimplemented. 1 Certain food types are to be encouragedsuch as fruit, vegetables, cereal, and grain products as wellas skimmed dairy products, fish, and lean meat, many <strong>of</strong>which are major comp<strong>on</strong>ents <strong>of</strong> <strong>the</strong> Mediterranean diet.Patients should thus be encouraged to adopt a ‘Mediterranean’diet, with vegetables, fruit, fish, and poultry being<strong>the</strong> mainstays. The intensity <strong>of</strong> change needed in <strong>the</strong> dietmay be guided by <strong>the</strong> total and LDL cholesterol levels ando<strong>the</strong>r lipid abnormalities. 356 Those who are overweightshould be put <strong>on</strong> a weight reducing diet.Alcohol in moderati<strong>on</strong> may be beneficial, 357 but excessivec<strong>on</strong>sumpti<strong>on</strong> is harmful, especially in patients with hypertensi<strong>on</strong>or heart failure. It has been difficult to developpublic health recommendati<strong>on</strong>s <strong>on</strong> safe limits <strong>of</strong> alcoholuse, but moderate alcohol c<strong>on</strong>sumpti<strong>on</strong> should not bediscouraged. 1,358–360Omega-3 fatty acidsFish oils rich in omega-3 fatty acids (n-3 polyunsaturatedfatty acids) are useful in <strong>the</strong> reducti<strong>on</strong> <strong>of</strong> hypertriglyceridaemia,and in <strong>the</strong> GISSI-Prevenzi<strong>on</strong>e trial, supplementati<strong>on</strong>
26 ESC <str<strong>on</strong>g>Guidelines</str<strong>on</strong>g>with <strong>on</strong>e fish oil capsule (Omacor) daily was shown to reduce<strong>the</strong> risk <strong>of</strong> sudden death in patients (85% men) with a recentMI. 361 A detailed fur<strong>the</strong>r analysis <strong>of</strong> <strong>the</strong> GISSI-Prevenzi<strong>on</strong>etrial 362 showed an early reducti<strong>on</strong> <strong>of</strong> cardiovascular deathwhich was dependent <strong>on</strong> fewer sudden deaths. The effectwas attributed to antiarrhythmic effects <strong>of</strong> omega-3 fattyacid supplementati<strong>on</strong>, in agreement with previous experimentaldata. 362 A meta-analysis <strong>of</strong> omega-3 fatty acid supplementati<strong>on</strong>363 c<strong>on</strong>firmed <strong>the</strong> effect <strong>on</strong> sudden death and showed areducti<strong>on</strong> <strong>of</strong> mortality, but c<strong>on</strong>cluded that reas<strong>on</strong>ably largerisk reducti<strong>on</strong> with such <strong>the</strong>rapy can <strong>on</strong>ly be expectedam<strong>on</strong>g high-risk patients, such as patients with a recent MI.A more recent meta-analysis <strong>of</strong> <strong>the</strong> effects <strong>of</strong> lipid-lowering<strong>the</strong>rapies <strong>on</strong> mortality also c<strong>on</strong>firmed <strong>the</strong> beneficial effect<strong>of</strong> n-3 fatty acids in sec<strong>on</strong>dary preventi<strong>on</strong>. 364 Patients withstable angina without high risk features should rarely bec<strong>on</strong>sidered for omega-3 fatty acid supplementati<strong>on</strong>. Dietaryinterventi<strong>on</strong> to achieve fish c<strong>on</strong>sumpti<strong>on</strong> at least <strong>on</strong>ceweekly can, however, be more widely recommended. 365,366Vitamins and antioxidantsVitamin supplementati<strong>on</strong> has not been shown to reducecardiovascular risk in patients with CAD. In c<strong>on</strong>trast to <strong>the</strong>above-menti<strong>on</strong>ed findings with dietary interventi<strong>on</strong>,several large studies have failed to find benefits frompharmacological supplementati<strong>on</strong> with antioxidantvitamins. 367–369Hypertensi<strong>on</strong>, diabetes, and o<strong>the</strong>r disordersC<strong>on</strong>comitant disorders should be managed appropriately.Particular attenti<strong>on</strong> should be given to c<strong>on</strong>trol <strong>of</strong> elevatedblood pressure, diabetes mellitus, and o<strong>the</strong>r features <strong>of</strong><strong>the</strong> metabolic syndrome which increase <strong>the</strong> risk <strong>of</strong> progressi<strong>on</strong><strong>of</strong> cor<strong>on</strong>ary disease. Of particular note, <strong>the</strong> TaskForce report <strong>on</strong> CVD preventi<strong>on</strong> 250 suggests c<strong>on</strong>sidering alower threshold for instituti<strong>on</strong> <strong>of</strong> pharmacological <strong>the</strong>rapyfor hypertensi<strong>on</strong> (130/85) for patients with establishedCHD (which would include patients with angina and n<strong>on</strong>invasiveor invasive c<strong>on</strong>firmati<strong>on</strong> <strong>of</strong> cor<strong>on</strong>ary disease).Patients with c<strong>on</strong>comitant diabetes and/or renal diseaseshould be treated with a blood pressure goal <strong>of</strong> ,130/80 mm Hg. 286 Diabetes is a str<strong>on</strong>g risk factor for cardiovascularcomplicati<strong>on</strong>s and should be managed carefully withgood glycaemic c<strong>on</strong>trol and attenti<strong>on</strong> to o<strong>the</strong>r riskfactors. 286,370,371Multifactorial interventi<strong>on</strong> in diabetic patients mayindeed reduce both cardiovascular and o<strong>the</strong>r diabetic complicati<strong>on</strong>smarkedly. 372 Recently, <strong>the</strong> additi<strong>on</strong> <strong>of</strong> pioglitiz<strong>on</strong>eto o<strong>the</strong>r hypoglycaemic medicati<strong>on</strong> has been shown toreduce <strong>the</strong> incidence <strong>of</strong> death, n<strong>on</strong>-fatal MI, or stroke (asec<strong>on</strong>dary endpoint) in patients with type 2 diabetes andvascular disease by 16%; <strong>the</strong> primary composite endpoint,which included a number <strong>of</strong> vascular endpoints, was notsignificantly reduced. 373 Anaemia or hyperthyroidism, ifpresent, should be corrected.Physical activityPhysical activity within <strong>the</strong> patient’s limitati<strong>on</strong>s should beencouraged, as it may increase exercise tolerance, reducesymptoms, and has favourable effects <strong>on</strong> weight, bloodlipids, blood pressure, glucose tolerance, and insulin sensitivity.Advice <strong>on</strong> exercise must take into account <strong>the</strong>individual’s overall fitness and <strong>the</strong> severity <strong>of</strong> symptoms.An exercise test can act as a guide to <strong>the</strong> level at whichan exercise programme can be initiated. Detailed recommendati<strong>on</strong>s<strong>on</strong> exercise prescripti<strong>on</strong> and <strong>on</strong> recreati<strong>on</strong>aland vocati<strong>on</strong>al activities are provided by <strong>the</strong> ESC WorkingGroup <strong>on</strong> Cardiac Rehabilitati<strong>on</strong>. 150Psychological factorsAlthough <strong>the</strong> role <strong>of</strong> stress in <strong>the</strong> genesis <strong>of</strong> CAD is c<strong>on</strong>troversial,<strong>the</strong>re is no doubt that psychological factors are importantin provoking attacks <strong>of</strong> angina. Fur<strong>the</strong>rmore, <strong>the</strong>diagnosis <strong>of</strong> angina <strong>of</strong>ten leads to excessive anxiety.Reas<strong>on</strong>able reassurance is essential, and patients maybenefit from relaxati<strong>on</strong> techniques and o<strong>the</strong>r methods <strong>of</strong>stress c<strong>on</strong>trol. Appropriate programmes may reduce <strong>the</strong>need for drugs and surgery. 374 A randomized c<strong>on</strong>trolledtrial 375 <strong>of</strong> a self-management plan showed an apparentimprovement in <strong>the</strong> psychological, symptomatic, andfuncti<strong>on</strong>al status <strong>of</strong> patients with newly diagnosed angina.Car drivingIn most countries, patients with stable angina are permittedto drive except for commercial public transport or heavyvehicles. Stressful driving c<strong>on</strong>diti<strong>on</strong>s should be avoided.Sexual intercourseSexual intercourse may trigger angina. Comm<strong>on</strong> sense willdictate that this should not be too physically or emoti<strong>on</strong>allydemanding. Nitroglycerin prior to intercourse may behelpful. Phosphodiesterase (PGE5) inhibitors such as sildenafil,tadafil, and vardenafil, used in <strong>the</strong> treatment <strong>of</strong> erectiledysfuncti<strong>on</strong>, may bestow benefits in terms <strong>of</strong> exercise durati<strong>on</strong>and can be safely prescribed to men with CAD butshould not be used in those receiving l<strong>on</strong>g-acting nitrates. 376The patient must be informed about <strong>the</strong> potentially harmfulinteracti<strong>on</strong>s between PGE5 inhibitors and nitrates or NO(nitric oxide) d<strong>on</strong>ors. 377,378EmploymentAn assessment should always be made <strong>of</strong> <strong>the</strong> physical andpsychological factors involved in an affected subject’swork (including housework). Patients should, if possible,be encouraged to c<strong>on</strong>tinue in <strong>the</strong>ir occupati<strong>on</strong>, with appropriatemodificati<strong>on</strong>s, if necessary.Pharmacological treatment <strong>of</strong> stableangina pectorisThe goals <strong>of</strong> pharmacological treatment <strong>of</strong> stable anginapectoris are to improve quality <strong>of</strong> life by reducing <strong>the</strong> severityand/or frequency <strong>of</strong> symptoms and to improve <strong>the</strong> prognosis<strong>of</strong> <strong>the</strong> patient. Measures <strong>of</strong> quality <strong>of</strong> life reflectdisease severity and carry prognostic informati<strong>on</strong> if properlyassessed. 379 When selecting evidence-based strategies forpharmacological preventi<strong>on</strong> <strong>of</strong> cardiac complicati<strong>on</strong>s anddeath, <strong>on</strong>e should c<strong>on</strong>sider <strong>the</strong> <strong>of</strong>ten benign prognosis <strong>of</strong><strong>the</strong> patient with stable angina pectoris. Pharmaco<strong>the</strong>rapyis a viable alternative to invasive strategies for <strong>the</strong> treatment<strong>of</strong> most patients with stable angina pectoris51,290,380,381 and was actually associated with fewercomplicati<strong>on</strong>s than surgery or PCI during a 1-year follow-up<strong>of</strong> <strong>the</strong> MASS-II study. 382 An invasive treatment strategy may
ESC <str<strong>on</strong>g>Guidelines</str<strong>on</strong>g> 27be reserved for patients at high risk or patients with symptomsthat are poorly c<strong>on</strong>trolled by medical treatment. 290The intensity <strong>of</strong> preventive pharmaco<strong>the</strong>rapy should be tailoredto <strong>the</strong> individual risk <strong>of</strong> <strong>the</strong> patient, keeping in mind<strong>the</strong> relatively low risk <strong>of</strong> many patients with stable anginapectoris.Pharmacological <strong>the</strong>rapy to improve prognosisCo-existing disorders such as diabetes and/or hypertensi<strong>on</strong>in patients with stable angina should be well c<strong>on</strong>trolled, dyslipidaemiashould be corrected, and smoking cessati<strong>on</strong>attempted (without or with pharmacological support).Statin and angiotensin-c<strong>on</strong>verting enzyme (ACE)-inhibitortreatment may provide protecti<strong>on</strong> above that which canbe ascribed to <strong>the</strong>ir lipid and blood pressure loweringeffects, respectively, and are discussed separately. Inadditi<strong>on</strong>, antiplatelet treatment should always bec<strong>on</strong>sidered for patients with ischaemic heart disease.Levels <strong>of</strong> evidence based <strong>on</strong> prognosis and symptom reliefare provided for <strong>the</strong> recommended treatments for anginain <strong>the</strong> treatment algorithm illustrated in Figure 7.Antithrombotic drugs. Antiplatelet <strong>the</strong>rapy to preventcor<strong>on</strong>ary thrombosis is indicated, due to a favourable ratiobetween benefit and risk in patients with stable CAD.Low-dose aspirin is <strong>the</strong> drug <strong>of</strong> choice in most cases,whereas clopidogrel may be c<strong>on</strong>sidered for some patients.Because <strong>of</strong> <strong>the</strong> evolving story <strong>of</strong> increased cardiovascularrisks with cyclooxygenase (COX)-2 inhibitor or NSAIDtreatment, as well as interacti<strong>on</strong>s between NSAIDs andaspirin, <strong>the</strong>se drugs will also be commented up<strong>on</strong> from <strong>the</strong>cardiovascular perspective.Low-dose aspirin. Aspirin remains <strong>the</strong> cornerst<strong>on</strong>e <strong>of</strong>pharmacological preventi<strong>on</strong> <strong>of</strong> arterial thrombosis and isvery well studied. 383–387 Aspirin acts via irreversible inhibiti<strong>on</strong><strong>of</strong> platelet COX-1 and thus thromboxane producti<strong>on</strong>,which is normally complete with chr<strong>on</strong>ic dosing 75 mg/day. 385 The optimal antithrombotic dosage <strong>of</strong> aspirinappears to be 75–150 mg/day, as <strong>the</strong> relative risk reducti<strong>on</strong>afforded by aspirin may decrease both below and above thisdose range. 387 In agreement with this interpretati<strong>on</strong>, anobservati<strong>on</strong>al post hoc analysis <strong>of</strong> <strong>the</strong> CURE study found anincreased risk <strong>of</strong> cardiovascular events with an aspirindosage 200 vs. 100 mg per day (HR 1.23; 95% CI1.08–1.39) in patients with acute cor<strong>on</strong>ary syndromes. 388Randomized studies comparing different dosages <strong>of</strong> aspirinare, however, few.C<strong>on</strong>trary to <strong>the</strong> antiplatelet effects, <strong>the</strong> gastrointestinalside-effects <strong>of</strong> aspirin increase at higher doses. 385 In a wellc<strong>on</strong>ductedobservati<strong>on</strong>al study, a doubling <strong>of</strong> peptic ulcerbleeding was observed when <strong>the</strong> aspirin dose increasedfrom 75 to 160 mg, and ano<strong>the</strong>r doubling when it increasedto 325 mg/day. 389 However, in a meta-analysis <strong>of</strong> l<strong>on</strong>g-termstudies, 390 <strong>the</strong>re was no clear dose–resp<strong>on</strong>se relati<strong>on</strong>shipbetween studies regarding <strong>the</strong> risk <strong>of</strong> gastrointestinal haemorrhage.The incidence <strong>of</strong> gastrointestinal haemorrhage was2.30% with aspirin at a dosage below 162.5 mg/day vs.1.45% with placebo, relative risk 1.59 (95% CI 1.40–1.81).The relative risk in trials using higher doses (.162.5 mg)was 1.96 (95% CI 1.58–2.43). In this meta-analysis, <strong>the</strong>large US Physicians Health Study (USPHS) with 325 mg <strong>on</strong>alternate days dominated <strong>the</strong> low-dose aspirin group,whereas <strong>the</strong> The Swedish <strong>Angina</strong> <strong>Pectoris</strong> Aspirin Trial(SAPAT) study (75 mg daily) was not included. Variable definiti<strong>on</strong>sand reporting <strong>of</strong> gastrointestinal bleeds mayc<strong>on</strong>found between-study comparis<strong>on</strong>s <strong>of</strong> different dosages<strong>of</strong> aspirin. Antiplatelet <strong>the</strong>rapy in patients with upper gastrointestinalbleeding problems is commented up<strong>on</strong> afterclopidogrel.Intracranial bleeds may increase with all antithromboticdrugs. The relative risk <strong>of</strong> suffering an intracranial haemorrhageincreases by 30%, 391 but <strong>the</strong> absolute risk <strong>of</strong> suchcomplicati<strong>on</strong>s attributable to antiplatelet drug <strong>the</strong>rapy isless than 1 per 1000 patient-years <strong>of</strong> treatment with aspirinat doses 75 mg/day. 383,385 There is no evidence for a dosedependence<strong>of</strong> <strong>the</strong> risk <strong>of</strong> intracranial bleeding with aspirin in<strong>the</strong> <strong>the</strong>rapeutically effective dose range. In patients witha<strong>the</strong>rosclerotic vascular disease, where <strong>the</strong> main aetiology<strong>of</strong> stroke is ischaemic, <strong>the</strong> net effect <strong>of</strong> aspirin treatmentregarding stroke is clearly beneficial. 383,385 Thus, <strong>the</strong>dosage <strong>of</strong> aspirin should be <strong>the</strong> lowest effective <strong>on</strong>e inorder to optimize <strong>the</strong> balance between <strong>the</strong>rapeutic gainsand gastrointestinal side effects during chr<strong>on</strong>ic <strong>the</strong>rapy.SAPAT showed a 34% reducti<strong>on</strong> <strong>of</strong> MI or cardiac death, corresp<strong>on</strong>dingto an absolute risk reducti<strong>on</strong> (ARR) <strong>of</strong> 1% peryear, with aspirin 75 mg/day compared with placebo insotalol-treated patients with stable angina pectoris. 47Low-dose aspirin treatment slightly increased <strong>the</strong> risk <strong>of</strong>major gastrointestinal haemorrhage (11 vs. 6 cases duringmore than 4000 patient-years <strong>of</strong> treatment in each group).Treatment was disc<strong>on</strong>tinued due to adverse effects in 109aspirin vs. 100 placebo-treated patients. 47 Thus, aspirin75 mg/day is both effective and well tolerated in stableangina pectoris. Treatment <strong>of</strong> a small subgroup <strong>of</strong> doctorswith angina pectoris with 325 mg aspirin every o<strong>the</strong>r day(compared with placebo) resulted in a significant reducti<strong>on</strong><strong>of</strong> n<strong>on</strong>-fatal MI in <strong>the</strong> USPHS. 392 Low daily dosing <strong>of</strong> aspirin(75 mg) is thus well documented in stable angina pectorisand is preferred in order to increase compliance (with aregular daily medicati<strong>on</strong> routine) and to reduce risks <strong>of</strong>side-effects and interacti<strong>on</strong>s.COX-2 inhibitors and NSAIDs. COX-2 inhibiti<strong>on</strong> reduces <strong>the</strong>producti<strong>on</strong> <strong>of</strong> prostacyclin, which has vasodilatory andplatelet-inhibiting effects. Attenuati<strong>on</strong> <strong>of</strong> prostacyclin formati<strong>on</strong>may predispose to elevated blood pressure, accelerateda<strong>the</strong>rogenesis, and thrombosis up<strong>on</strong> plaque rupture. 393The recent withdrawal <strong>of</strong> r<strong>of</strong>ecoxib (Vioxx), a highly selectiveCOX-2 inhibitor, was caused by findings <strong>of</strong> an increasedrisk <strong>of</strong> serious cor<strong>on</strong>ary events in a placebo-c<strong>on</strong>trolled trial<strong>of</strong> cancer preventi<strong>on</strong>. 394 An increased risk <strong>of</strong> sufferingfatal or n<strong>on</strong>-fatal MI was also found in a meta-analysis <strong>of</strong>o<strong>the</strong>r randomized trials with r<strong>of</strong>ecoxib. 395 There is also supportingevidence for harmful effects <strong>of</strong> COX-2 inhibiti<strong>on</strong>from several observati<strong>on</strong>al studies. 396 A cancer preventi<strong>on</strong>trial with celecoxib showed a dose-related increase in <strong>the</strong>risk <strong>of</strong> suffering cardiovascular complicati<strong>on</strong>s, with HRs <strong>of</strong>2.3 (95% CI 0.9–5.5) and 3.4 (1.4–7.8) for 200 and 400 mgcelecoxib bid, respectively. 397 A placebo-c<strong>on</strong>trolled study<strong>of</strong> parecoxib/valdecoxib (iv þ oral <strong>the</strong>rapy) for <strong>the</strong> treatment<strong>of</strong> post-operative pain after CABG showed an increasedrisk <strong>of</strong> suffering cardiovascular events with <strong>on</strong>ly 10 days <strong>of</strong>treatment with COX-2 inhibiti<strong>on</strong>. 398 Thus, <strong>the</strong>re are indicati<strong>on</strong>sfrom studies with several COX-2 inhibitors that<strong>the</strong>y may increase <strong>the</strong> risk <strong>of</strong> cor<strong>on</strong>ary thrombotic eventsin patient populati<strong>on</strong>s with different levels <strong>of</strong> cardiovascular
Figure 7 Algorithm for medical management <strong>of</strong> stable angina. High-risk candidates for revascularizati<strong>on</strong> <strong>on</strong> prognostic grounds al<strong>on</strong>e should be identified and referred appropriately. (Asterisk) Relative c<strong>on</strong>traindicati<strong>on</strong>s tobeta-blockade include asthma, symptomatic peripheral vascular disease, and first-degree heart block. (Double dagger) Avoid short-acting dihydropyridine formulati<strong>on</strong>s when not combined with beta-blocker. Evidence forprognosis refers to evidence <strong>of</strong> reducti<strong>on</strong> in CV death or CV death/MI. Evidence for symptoms includes reducti<strong>on</strong> in need for revascularizati<strong>on</strong> and hospitalizati<strong>on</strong> for chest pain.28 ESC <str<strong>on</strong>g>Guidelines</str<strong>on</strong>g>
ESC <str<strong>on</strong>g>Guidelines</str<strong>on</strong>g> 29risk. In additi<strong>on</strong>, COX-2 inhibiti<strong>on</strong> increases <strong>the</strong> risk <strong>of</strong> sufferingstroke, heart failure, and hypertensi<strong>on</strong>. 399 The use<strong>of</strong> unopposed COX-2 inhibiti<strong>on</strong> (i.e. without effective simultaneousplatelet COX-1 inhibiti<strong>on</strong>) should thus be avoided inpatients with stable angina pectoris.N<strong>on</strong>-selective, reversible COX inhibitors (NSAIDs) caninhibit thromboxane producti<strong>on</strong> and platelet aggregati<strong>on</strong>,400,401 as dem<strong>on</strong>strated for naproxen. 402 However, <strong>the</strong>reversible NSAIDs rarely inhibit thromboxane producti<strong>on</strong> aseffectively as aspirin, 385 and it has been shown that ,5%residual COX-1 activity in platelets is sufficient to sustainfull platelet aggregati<strong>on</strong>. 403 <strong>Cardio</strong>protective effects <strong>of</strong>naproxen treatment have been discussed, 404–407 but <strong>the</strong>balance <strong>of</strong> evidence indicates that also n<strong>on</strong>-selectiveNSAIDs may increase <strong>the</strong> risk <strong>of</strong> cardiovascular complicati<strong>on</strong>s.396 It is recommended to primarily use paracetamol.If NSAIDs are needed, <strong>the</strong>y should be used in <strong>the</strong> lowesteffective doses and for <strong>the</strong> shortest possible durati<strong>on</strong>. Awarning has also recently been issued by <strong>the</strong> FDA fornaproxen. 408 NSAID treatment should, when this is indicatedfor o<strong>the</strong>r reas<strong>on</strong>s, be combined with low-dose aspirin toassure effective platelet inhibiti<strong>on</strong> in patients with stableangina pectoris. In such circumstances, ibupr<strong>of</strong>en shouldbe avoided, as this NSAID prevents aspirin from irreversiblyacetylating <strong>the</strong> COX-1 enzyme <strong>of</strong> platelets, as maynaproxen. 409,410 Dicl<strong>of</strong>enac is a relatively COX2-selectiveNSAID and, <strong>the</strong>refore, a poor platelet inhibitor, but doesnot interfere with <strong>the</strong> antiplatelet effects <strong>of</strong> aspirin andmay be used in combinati<strong>on</strong> with aspirin. 411Clopidogrel. Clopidogrel and ticlopidine are thienopyridineswhich act as n<strong>on</strong>-competitive ADP receptor antag<strong>on</strong>ists andwhich have antithrombotic effects similar to aspirin. 385Ticlopidine efficacy has mainly been documented in strokeand PCI 385,387 and has been replaced by clopidogrel due to<strong>the</strong> risk <strong>of</strong> neutropenia and thrombocytopenia and moresymptomatic side-effects with ticlopidine. The main studydocumenting clopidogrel use in stable CAD is CAPRIE, 412which included three equally large groups <strong>of</strong> patients withprevious MI, previous stroke, or peripheral vascular disease(PVD). 412 When compared with aspirin 325 mg/day, whichmay be less effective than 75 mg/day (see Figure 7 inCollaborative Meta-analysis <strong>of</strong> Randomized Trials 387 ), clopidogrel75 mg/day was slightly more effective (ARR 0.51%per year; P ¼ 0.043) in preventing cardiovascular complicati<strong>on</strong>sin high-risk patients. 412 When comparing outcomesin <strong>the</strong> three subgroups <strong>of</strong> patients enrolled in CAPRIE, <strong>the</strong>benefit with clopidogrel appeared in <strong>the</strong> PVD subgroup<strong>on</strong>ly. 412 Gastrointestinal haemorrhage was <strong>on</strong>ly slightly lesscomm<strong>on</strong> with clopidogrel compared with aspirin treatment(1.99 vs. 2.66% during 1.9 years <strong>of</strong> treatment), despite <strong>the</strong>relatively high aspirin dose. 412 The benefit <strong>of</strong> clopidogrelmay have been over-estimated because <strong>the</strong> dose <strong>of</strong> aspirinwith which it was compared (325 mg) may not be <strong>the</strong> mosteffective dose. The CAPRIE study did not include patientswith aspirin intolerance, and we do not know <strong>the</strong> risk <strong>of</strong> gastrointestinalbleeding during clopidogrel compared withplacebo treatment. Clopidogrel is more expensive thanaspirin, but may be c<strong>on</strong>sidered in aspirin-intolerant patientswith significant risks <strong>of</strong> arterial thrombosis. Gastrointestinalintolerance may, however, be handled differently (discussedsubsequently). After cor<strong>on</strong>ary stenting, an acute cor<strong>on</strong>arysyndrome, or an ST-elevati<strong>on</strong> MI, clopidogrel may becombined with aspirin during a finite period <strong>of</strong> time, butcombinati<strong>on</strong> <strong>the</strong>rapy is currently not warranted in stableangina pectoris. Clopidogrel treatment increases <strong>the</strong> risk<strong>of</strong> severe bleeding in c<strong>on</strong>necti<strong>on</strong> with CABG surgery. 413One much discussed reas<strong>on</strong> for variability <strong>of</strong> antiplateletresp<strong>on</strong>ses to clopidogrel is drug–drug interacti<strong>on</strong>s, as clopidogrelforms its active metabolite(s) via CYP3A4-mediatedmetabolism. A study by Lau et al. 414 showed that atorvastatin,but not pravastatin, dose-dependently inhibited <strong>the</strong>effect <strong>of</strong> clopidogrel <strong>on</strong> ADP-mediated platelet activati<strong>on</strong>.The study also showed <strong>the</strong> expected interacti<strong>on</strong>s betweenclopidogrel and antibiotics that inhibit (erythromycin andtroleandomycin) or induce (rifampicin) CYP3A4. 414 Ano<strong>the</strong>rstudy with clopidogrel maintenance treatment found nointeracti<strong>on</strong> with low-dose atorvastatin (10 mg daily) treatment.415 The short-term effects <strong>of</strong> a 300 mg loading dose<strong>of</strong> clopidogrel in c<strong>on</strong>necti<strong>on</strong> with PCI may 416 or may not 417be attenuated by co-treatment with lipophilic statins (atorvastatin,simvastatin, and lovastatin). The effects <strong>of</strong> a600 mg loading dose appear to be unaffected by treatmentwith atorvastatin or simvastatin. 418,419 Observati<strong>on</strong>al posthoc analyses <strong>of</strong> outcomes am<strong>on</strong>g patients receiving maintenanceco-treatment with clopidogrel and interacting statinhave not shown differences in outcome, but <strong>the</strong>re are noproperly designed prospective studies that address <strong>the</strong>issue. Data from <strong>the</strong> large GRACE registry indicate thatstatin treatment has additi<strong>on</strong>al benefit to those <strong>of</strong> clopidogreltreatment, as might be expected. 420 Thus, <strong>the</strong> literature <strong>on</strong>statin–clopidogrel interacti<strong>on</strong>s is inc<strong>on</strong>sistent, and <strong>the</strong>importance <strong>of</strong> interacti<strong>on</strong>s between maintenance <strong>the</strong>rapywith lipophilic statins and clopidogrel is at present not known.Antiplatelet <strong>the</strong>rapy in patients with gastrointestinalintolerance to aspirin. Gastrointestinal haemorrhages mayincrease with any antiplatelet treatment, but <strong>the</strong> size <strong>of</strong>this effect with clopidogrel is not known in <strong>the</strong> absence <strong>of</strong>data from placebo-c<strong>on</strong>trolled trials. It has been speculatedthat antiplatelet treatment interferes with <strong>the</strong> normalwound healing process which limits <strong>the</strong> progressi<strong>on</strong> <strong>of</strong> subclinicaland ra<strong>the</strong>r comm<strong>on</strong> (2% per m<strong>on</strong>th without anytreatment) gastric erosi<strong>on</strong>s, due to reduced release <strong>of</strong> plateletstored growth factors such as VEGF. 421 In additi<strong>on</strong>, aspirincauses dose-related gastric mucosal damage which mayincrease <strong>the</strong> incidence and severity <strong>of</strong> erosi<strong>on</strong>s. Upper gastrointestinalbleeding due to aspirin or NSAID <strong>the</strong>rapy maybe alleviated by inhibiting gastric acid secreti<strong>on</strong>.Eradicati<strong>on</strong> <strong>of</strong> Helicobacter pylori infecti<strong>on</strong>, if present,also reduces <strong>the</strong> risk <strong>of</strong> aspirin-related gastorintestinalbleeding. 422Am<strong>on</strong>g <strong>the</strong> different acid reducing <strong>the</strong>rapies available,prot<strong>on</strong> pump inibitor (PPI) treatment has been best documented.Thus, 30 mg/day <strong>of</strong> lansoprazole reduced <strong>the</strong>recurrence <strong>of</strong> ulcer complicati<strong>on</strong>s from 14.8% in <strong>the</strong>placebo group to 1.6% (P ¼ 0.008) during a 12-m<strong>on</strong>thfollow-up <strong>of</strong> gastroduodenal ulcer patients treated with100 mg aspirin after H. pylori eradicati<strong>on</strong>. 423 A recentstudy showed that <strong>the</strong> additi<strong>on</strong> <strong>of</strong> a PPI (esomeprazole40 mg/day) to aspirin (80 mg/day) was better than switchingto clopidogrel for <strong>the</strong> preventi<strong>on</strong> <strong>of</strong> recurrent ulcer bleedingin patients with ulcers and vascular disease. 424Dipyridamole and anticoagulants. Dipyridamole is not recommendedfor antithrombotic treatment in stable anginadue to poor antithrombotic efficacy 387 and <strong>the</strong> risk <strong>of</strong>
30 ESC <str<strong>on</strong>g>Guidelines</str<strong>on</strong>g>worsening anginal symptoms due to cor<strong>on</strong>ary steal phenomena.425 Anticoagulant drugs (warfarin or thrombin inhibitors),which are an alternative or combined with aspirin in certainhigh-risk patients, such as post-MI, are not indicated in<strong>the</strong> general stable angina populati<strong>on</strong> without a separateindicati<strong>on</strong> such as AF.Aspirin resistance. Possible problems related to ‘aspirinresistance’ are <strong>of</strong> c<strong>on</strong>siderable interest 386,426 and havebeen much discussed. However, <strong>the</strong> phenomen<strong>on</strong> is illdefinedand may be characterized by <strong>the</strong> occurence <strong>of</strong> cardiovascularevents despite <strong>the</strong>rapy (i.e. <strong>the</strong>rapeutic failure)or by resistance to <strong>the</strong> pharmacological effects <strong>of</strong> aspirin, asdetermined by various laboratory methods. There iscurrently no ‘gold standard’ with which to evaluate aspirinresistance, and fur<strong>the</strong>r research is needed beforec<strong>on</strong>clusi<strong>on</strong>s can be drawn and management schemes canbe implemented. 385 Thus, aspirin resistance is still amatter for research <strong>on</strong> how to m<strong>on</strong>itor and manage patientswith insufficient resp<strong>on</strong>ses to aspirin. 427 A similar issue with‘clopidogrel resistance’ is emerging, and it is similarlyunclear how this should be handled. 428–430Lipid-lowering drugs. Statin treatment reduces <strong>the</strong> risk <strong>of</strong>a<strong>the</strong>rosclerotic cardiovascular complicati<strong>on</strong>s in bothprimary and sec<strong>on</strong>dary preventi<strong>on</strong> settings. 431 In patientswith a<strong>the</strong>rosclerotic vascular disease, simvastatin 432 andpravastatin 433,434 reduce <strong>the</strong> incidence <strong>of</strong> serious cardiovascularcomplicati<strong>on</strong>s by some 30%. The Heart Protecti<strong>on</strong>Study (HPS) 435 and <strong>the</strong> Prospective Pravastatin PoolingProject (PPPP), which included primary preventi<strong>on</strong>, 433were large enough to show reduced mortality. Subgroup analysesindicate beneficial effects also in diabetic patientswith vascular disease 436,437 and benefits <strong>of</strong> statin <strong>the</strong>rapyhave also been dem<strong>on</strong>strated in <strong>the</strong> elderly (.70years). 435,438 In diabetic patients without manifest vasculardisease, simvastatin 40 mg/day 437 and atorvastatin 10 mg/day 439 provided similar primary protecti<strong>on</strong> against majorcardiovascular events. Reducti<strong>on</strong>s in major cardiovascularevents were also observed in <strong>the</strong> placebo-c<strong>on</strong>trolled Anglo-Scandinavian Cardiac Outcomes Trial-Lipid Lowering Arm(ASCOT-LLA) 440 which evaluated atorvastatin treatment in<strong>the</strong> primary preventi<strong>on</strong> <strong>of</strong> CHD in hypertensive patientswith total cholesterol levels 6.5 mmol/L. In additi<strong>on</strong> to<strong>the</strong> relatively low cholesterol levels, blood pressurec<strong>on</strong>trol in <strong>the</strong> study was excellent, resulting in a lowabsolute risk <strong>of</strong> cardiac death and MI in this patient populati<strong>on</strong>.Hence, although <strong>the</strong> relative risk reducti<strong>on</strong> in totalcor<strong>on</strong>ary events was 36%, <strong>the</strong> ARR with statin treatmentwas <strong>on</strong>ly 0.34% per year regarding cardiac death or MI. 440No trial has been performed specifically in patients withstable angina pectoris, but such patients c<strong>on</strong>stitutedsignificant proporti<strong>on</strong>s <strong>of</strong> <strong>the</strong> trials menti<strong>on</strong>ed. In HPS,for example, 41% <strong>of</strong> patients were post-MI and 24% hado<strong>the</strong>r CAD.Statins lower cholesterol effectively, 431 but mechanismso<strong>the</strong>r than cholesterol syn<strong>the</strong>sis inhibiti<strong>on</strong>, such as antiinflammatoryand antithrombotic effects, 441–444 may c<strong>on</strong>tributeto <strong>the</strong> cardiovascular risk reducti<strong>on</strong>. In patientswith stable angina, it has been shown that 7 days pretreatmentwith atorvastatin 40 mg/day compared withplacebo before PCI reduced procedural myocardial injury,as assessed by biochemical markers. 445 Such myocardialprotecti<strong>on</strong> by short-term, high-dose atorvastatintreatment may be related to n<strong>on</strong>-lipid effects <strong>of</strong> <strong>the</strong> statintreatment. Similar relative benefits <strong>of</strong> l<strong>on</strong>g-term statin<strong>the</strong>rapy have been observed in patients with different pretreatmentlevels <strong>of</strong> serum cholesterol, even in <strong>the</strong> ‘normal’range. 433,435,439 Thus, recommendati<strong>on</strong>s to treat withstatins may be guided as much by <strong>the</strong> patients level <strong>of</strong>cardiovascular risk as by <strong>the</strong> cholesterol level (within <strong>the</strong>normal to moderately elevated range). As for blood pressure(discussed subsequently), <strong>the</strong> risk associated with cholesterolincreases log-linearly from low normal levels, 431 andit is <strong>the</strong>refore difficult to evaluate <strong>the</strong> relative importances<strong>of</strong> cholesterol lowering and o<strong>the</strong>r effects <strong>of</strong> statin treatmentfor <strong>the</strong> treatment benefits observed. A recent meta-analysis<strong>of</strong> <strong>the</strong> effects <strong>of</strong> different lipid-lowering <strong>the</strong>rapies <strong>on</strong> mortalityc<strong>on</strong>cluded that statins and n-3 fatty acids reducedmortality, whereas fibrates, resins, niacin, and dietaryinterventi<strong>on</strong>s failed to do so; a tendancy towards reducedcardiac mortality was counterbalanced by an increase inn<strong>on</strong>-cardiac mortality in <strong>the</strong> fibrate trials. 364Current European Preventi<strong>on</strong> guidelines suggest a targetvalue <strong>of</strong> ,4.5 mmol/L (175 mg/dL) for total cholesteroland 2.5 mmol/L (96 mg/dL) for LDL cholesterol in patientswith established CHD or even those who remain at persistentlyhigh multifactorial risk (.5% risk <strong>of</strong> fatal cardiovascularevents over 10 years). However, several studies haveshown that C-reactive protein levels predict beneficial outcomesduring statin <strong>the</strong>rapy as well do cholesterol levels andthat <strong>the</strong>se two markers <strong>of</strong> statin resp<strong>on</strong>siveness are additive.444 Such analyses <strong>of</strong> clinical trial data suggest thatcholesterol-independent effects <strong>of</strong> statin <strong>the</strong>rapy may be<strong>of</strong> clinical importance. Thus, patient selecti<strong>on</strong> based <strong>on</strong>cholesterol levels and <strong>the</strong>rapy solely directed at cholesterolgoals may not fully exploit <strong>the</strong> benefit <strong>of</strong> statin <strong>the</strong>rapy.Statin <strong>the</strong>rapy should always be c<strong>on</strong>sidered for patientswith stable CAD and stable angina, based <strong>on</strong> <strong>the</strong>ir elevatedlevel <strong>of</strong> risk and evidence <strong>of</strong> benefit <strong>of</strong> cholesterol loweringwithin <strong>the</strong> normal range. 446 Therapy should aim at statindosages documented to reduce morbidity/mortality in clinicaltrials. If this dose is not sufficient to achieve <strong>the</strong> targettotal cholesterol and LDL levels as menti<strong>on</strong>ed above, <strong>the</strong>dose <strong>of</strong> statin <strong>the</strong>rapy may be increased as tolerated toachieve <strong>the</strong> targets. The daily statin dosages with soliddocumentati<strong>on</strong> in <strong>the</strong> above-menti<strong>on</strong>ed studies are simvastatin40 mg, pravastatin 40 mg, and atorvastatin 10 mg.Recently, high-dose atorvastatin treatment (80 mg daily)has been shown to reduce <strong>the</strong> risk <strong>of</strong> cardiovascular eventswhen compared with 10 mg atorvastatin or simvastatin24 mg in patients with stable CAD. 447,448 The increasedefficacy <strong>of</strong> high-dose atorvastatin treatment wasaccompanied by six-fold increase (from 0.2 to 1.2%;P , 0.001) in enzymatic signs <strong>of</strong> liver damage, but no discernibleincrease in myalgia. 447 High-dose atorvastatin<strong>the</strong>rapy should be reserved for high-risk patients.Statin treatment is associated with few side effects, butskeletal muscle damage (symptoms, CK elevati<strong>on</strong>s, and,rarely, rhabdomyolysis) may occur, and liver enzymesshould be also m<strong>on</strong>itored after initiati<strong>on</strong> <strong>of</strong> <strong>the</strong>rapy.Gastrointestinal disturbances may limit <strong>the</strong> dosage. Ifstatins are poorly tolerated at high doses, or lipid c<strong>on</strong>trolis not achieved with <strong>the</strong> highest statin dose, reducti<strong>on</strong> <strong>of</strong><strong>the</strong> statin dose and <strong>the</strong> additi<strong>on</strong> <strong>of</strong> <strong>the</strong> cholesterol absorpti<strong>on</strong>inhibitor, ezetimibe, may afford adequate reducti<strong>on</strong><strong>of</strong> cholesterol. 449 Effects <strong>on</strong> morbidity and mortality <strong>of</strong>
ESC <str<strong>on</strong>g>Guidelines</str<strong>on</strong>g> 31such combinati<strong>on</strong> treatment have, however, not yet beendocumented.Lipid-modifying drugs o<strong>the</strong>r than statins, e.g. fibrates,resins, or prol<strong>on</strong>ged release nicotinic acid, and <strong>the</strong>ir combinati<strong>on</strong>swith statins and o<strong>the</strong>r hypolipidaemics may beneeded to c<strong>on</strong>trol <strong>the</strong> lipid levels am<strong>on</strong>g patients withsevere dyslipidaemia. This is especially true <strong>of</strong> those withlow levels <strong>of</strong> HDL cholesterol and high triglycerides.431,450,451 However, benefits <strong>of</strong> gemfibrozil treatmentin <strong>the</strong> VA-HIT study were primarily found am<strong>on</strong>g men withinsulin resistance. 452 The combinati<strong>on</strong> <strong>of</strong> fibrates withstatin <strong>the</strong>rapy increases <strong>the</strong> risk <strong>of</strong> associated myopathy,but fen<strong>of</strong>ibrate has been recently shown not to interferewith <strong>the</strong> catabolism <strong>of</strong> statins and is <strong>the</strong>refore less likelyto increase <strong>the</strong> risk <strong>of</strong> myopathy when combined with moderatedoses <strong>of</strong> statins. 453,454 Fibrate <strong>the</strong>rapy was not associatedwith reduced total deaths in <strong>the</strong> meta-analysis <strong>of</strong>Studer et al. 364 Similarly, <strong>the</strong> recently published FIELDtrial, comparing fen<strong>of</strong>ibrate and placebo in 9795 patientswith type 2 diabetes, found no mortality benefit and no significantreducti<strong>on</strong> <strong>of</strong> <strong>the</strong> primary combined endpoint <strong>of</strong> cor<strong>on</strong>arydeath and n<strong>on</strong>-fatal MI. 455 Thus, gemfibizol treatmentmay be c<strong>on</strong>sidered in high-risk patients with low HDL cholesterol,but <strong>the</strong>re is little support for a more widespread use<strong>of</strong> fibrates. Torcetrapib is a new agent which has beenshown to raise HDL effectively, 456 but as yet <strong>the</strong>re is insufficientevidence to make universal recommendati<strong>on</strong>s regardingtarget HDL or triglyceride levels to be achieved bypharmaco<strong>the</strong>rapy in <strong>the</strong> general populati<strong>on</strong> with angina.However, adjunctive <strong>the</strong>rapy to statin <strong>the</strong>rapy may bec<strong>on</strong>sidered <strong>on</strong> an individualized basis in patients who havesevere dyslipidaemia and remain at high risk after c<strong>on</strong>venti<strong>on</strong>almeasures (estimated cardiovascular mortality .2%per annum).ACE-inhibitors. ACE-inhibitors are well established for <strong>the</strong>treatment <strong>of</strong> hypertensi<strong>on</strong> and heart failure, but have notbeen shown to c<strong>on</strong>fer better overall protecti<strong>on</strong> against <strong>the</strong>cardiovascular complicati<strong>on</strong>s in hypertensi<strong>on</strong>, comparedwith that afforded by o<strong>the</strong>r antihypertensive drugs. 457–459ACE-inhibitors or angiotensin receptor blockers (ARBs) arerecommended for <strong>the</strong> treatment <strong>of</strong> diabetic patients withmicroalbuminuria to prevent progressi<strong>on</strong> <strong>of</strong> renal dysfuncti<strong>on</strong>,and as first-line agents to treat blood pressure indiabetic patients. 286,370Because <strong>of</strong> observed reducti<strong>on</strong>s in MI and cardiac mortalityin trials <strong>of</strong> ACE-inhibitors for heart failure andpost-MI, ACE-inhibitors have also been investigated as sec<strong>on</strong>darypreventive <strong>the</strong>rapy for patients with cor<strong>on</strong>arydisease without heart failure. 252,460,461 The HOPE studyincluded high-risk patients with established CVD (cor<strong>on</strong>aryor n<strong>on</strong>-cor<strong>on</strong>ary) or diabetes, and at least <strong>on</strong>e o<strong>the</strong>r riskfactor, and randomized <strong>the</strong>m to treatment with ramipril orplacebo for 5 years. 460 The EUROPA study included patientswith stable CAD, with a broad range <strong>of</strong> risk but without clinicalheart failure, who were randomized to treatment withperindopril or placebo for 4.2 years. 461 The PEACE studyincluded patients with stable CAD without heart failurewho were treated with trandolapril or placebo for 4.8years. 252 As shown in Figure 1, <strong>the</strong> annual cardiovascularmortality rates in <strong>the</strong> placebo groups ranged from 0.8%(PEACE) to 1.6% (HOPE). The differences in cardiovascularrisk were associated with differences in <strong>the</strong>rapy at baseline.The relative risk reducti<strong>on</strong>s for composite primary endpointswere in <strong>the</strong> order <strong>of</strong> 20% in <strong>the</strong> HOPE and EUROPAstudies, whereas <strong>the</strong> PEACE study found no significant riskreducti<strong>on</strong> with ACE-inhibiti<strong>on</strong>. The results <strong>of</strong> <strong>the</strong> threestudies are unfortunately not directly comparable due todifferent selecti<strong>on</strong>s <strong>of</strong> endpoints. Regarding reducti<strong>on</strong> <strong>of</strong><strong>the</strong> risk for cardiovascular death, HOPE reported a relativerisk reducti<strong>on</strong> <strong>of</strong> 26% (95% CI 13–36), EUROPA 14% (95% CI23 to 28), and PEACE 5% (95% CI 219 to 24). The greatestrelative risk reducti<strong>on</strong> in HOPE was seen for stroke (RR0.68; 95% CI 0.56–0.84), which was not reported in EUROPAbut tended to be reduced in PEACE (HR 0.76; 95% CI0.56–1.04). The PEACE investigators also reported norisk reducti<strong>on</strong> when using <strong>the</strong> combined endpoints <strong>of</strong>HOPE (RR 0.93; 95% CI 0.81–1.07) and EUROPA (RR 0.96;95% CI 0.83–1.12), respectively. 252 All three studies reportedsignificant reducti<strong>on</strong>s <strong>of</strong> heart failure with ACE-inhibitortreatment.Treatment benefits with ACE-inhibiti<strong>on</strong> were thus smallerin PEACE than in HOPE or EUROPA. One possible explanati<strong>on</strong>for this difference in outcomes might be differencesbetween <strong>the</strong> three ACE-inhibitors and/or <strong>the</strong> relativedosages used. However, <strong>the</strong> dosage <strong>of</strong> trandolapril used inPEACE was associated with a significant 25% reducti<strong>on</strong> <strong>of</strong>cardiovascular death and a 29% reducti<strong>on</strong> <strong>of</strong> severe heartfailure, but a lesser decrease in n<strong>on</strong>-fatal MI (214%, NS) inc<strong>on</strong>secutively enrolled post-MI patients with LV dysfuncti<strong>on</strong>in <strong>the</strong> TRACE study. 462 Baseline blood pressure was lower(133/78 mmHg) in <strong>the</strong> PEACE populati<strong>on</strong> than in ei<strong>the</strong>r <strong>of</strong><strong>the</strong> o<strong>the</strong>r two studies. The rates <strong>of</strong> previous revascularizati<strong>on</strong>ranged from 44% (HOPE) to 72% (PEACE), and drug<strong>the</strong>rapy at baseline differed between <strong>the</strong> studies.Lipid-lowering <strong>the</strong>rapy was received by <strong>on</strong>ly 29% <strong>of</strong> patientsin HOPE compared with 70% in PEACE; <strong>the</strong> corresp<strong>on</strong>dingfigures were 76 vs. 96% for antithrombotic drug treatmentand 40 vs. 60% for beta-blocker use. C<strong>on</strong>versely, calciumchannel blocker (CCB) use at baseline was more comm<strong>on</strong>in <strong>the</strong> HOPE study. Overall, PEACE patients were at lowerabsolute risk <strong>of</strong> cardiovascular death than <strong>the</strong> HOPE orEUROPA patients. These differences in baseline risk andn<strong>on</strong>-study-related <strong>the</strong>rapy may have c<strong>on</strong>tributed importantlyto <strong>the</strong> differences in cardiovascular outcome withACE-inhibitor <strong>the</strong>rapy.The relative effects <strong>of</strong> ramipril and perindopril <strong>on</strong> cardiovascularoutcome were similar in a high-risk populati<strong>on</strong> andan intermediate populati<strong>on</strong>, respectively, although forobvious reas<strong>on</strong>s, <strong>the</strong> ARR was greater in <strong>the</strong> populati<strong>on</strong> athighest absolute risk (MICRO-HOPE). 463 Pre-defined subgroupanalysis <strong>of</strong> EUROPA and HOPE according to individual factorsknown to affect risk, such as age, diabetes, prior MI, n<strong>on</strong>cor<strong>on</strong>ary vascular disease, and microalbuminuria, showedrelative benefit <strong>of</strong> similar magnitude from <strong>the</strong>rapy withACE-inhibitor in almost all subgroups.The blood pressure lowering effects <strong>of</strong> ACE-inhibiti<strong>on</strong> mayhave c<strong>on</strong>tributed to <strong>the</strong> beneficial results observed in HOPEand EUROPA. In HOPE, unc<strong>on</strong>trolled hypertensi<strong>on</strong> was anexclusi<strong>on</strong> criteri<strong>on</strong> and mean BP at entry was 139/79 mmHg. 460 The overall 3/2 mmHg blood pressure differencebetween ramipril and placebo treatment 460 may havebeen underestimated because <strong>of</strong> evening dosing <strong>of</strong> ramipriland <strong>of</strong>fice blood pressure measurements <strong>the</strong> next day. AHOPE substudy with 24 h ambulatory measurementsreported a 10/4 mmHg blood pressure difference during
32 ESC <str<strong>on</strong>g>Guidelines</str<strong>on</strong>g>24 h and a 17/8 mmHg difference during <strong>the</strong> night, comparedwith 8/2 mmHg with <strong>of</strong>fice measurements in <strong>the</strong>same study. 464 In EUROPA, patients with unc<strong>on</strong>trolled hypertensi<strong>on</strong>(.180/100 mmHg) were also excluded, and <strong>the</strong>mean blood pressure at baseline was 137/82 mmHg. Theoverall blood pressure difference between perindopril andplacebo treatment was 5/2 mmHg, 461 but larger differencesmay have occurred in subgroups <strong>of</strong> patients. However, analysis<strong>of</strong> <strong>the</strong> effect <strong>of</strong> treatment according to tertiles or quartiles<strong>of</strong> baseline blood pressure or fall in blood pressure <strong>on</strong>treatment shows significant benefit in all groups, eventhose in <strong>the</strong> lowest baseline blood pressure or smallestreducti<strong>on</strong> in blood pressure with treatment. 465 Benefits <strong>of</strong>blood pressure reducti<strong>on</strong>s may be expected in subgroups<strong>of</strong> patients with clearly elevated blood pressure, but loweringblood pressure is associated with a lowering <strong>of</strong> cardiovascularrisk also in <strong>the</strong> ‘normal’ range. 466 Thus, it is difficult toseparate blood pressure-related effects from bloodpressure-independent protecti<strong>on</strong> afforded by ACE-inhibiti<strong>on</strong>in stable angina pectoris.Fur<strong>the</strong>r clues regarding <strong>the</strong> effect <strong>of</strong> blood pressure loweringand ACE-inhibiti<strong>on</strong> in stable cor<strong>on</strong>ary disease may beobtained from <strong>the</strong> CAMELOT trial. 467 In this study, patientswith angiographic evidence <strong>of</strong> cor<strong>on</strong>ary disease, althoughnot necessarily obstructive, and normal blood pressure(mean BP 129/78 mmHg) were randomized to amlodipine,enalapril, or placebo and followed-up for 2 years. Sixtypercent <strong>of</strong> <strong>the</strong> patients had hypertensi<strong>on</strong> and <strong>the</strong>y werewell treated in o<strong>the</strong>r respects (83% <strong>on</strong> statins, 75% <strong>on</strong> a betablocker,and 95% <strong>on</strong> aspirin). Blood pressure reducti<strong>on</strong>s(5 mm/2 mm) were almost identical in <strong>the</strong> two active treatmentgroups. The study was not powered to show effects <strong>on</strong>‘hard’ endpoints (670 patients per group), but a ‘post hoc’analysis <strong>of</strong> <strong>the</strong> combined endpoint <strong>of</strong> cardiovascular death,stroke, and MI showed similar n<strong>on</strong>-significant relative riskreducti<strong>on</strong>s with enalapril (29%) and amlodipine (30%).Fur<strong>the</strong>rmore, an IVUS substudy in 274 patients showed a significantcorrelati<strong>on</strong> between <strong>the</strong> progressi<strong>on</strong> <strong>of</strong> a<strong>the</strong>romaand <strong>the</strong> reducti<strong>on</strong> in blood pressure even at this ‘normal’range <strong>of</strong> blood pressure. The recently presented VALUEstudy, which compared antihypertensive treatment withamlodipine or valsartan in 15 245 patients (46% <strong>of</strong> whomhad CAD) during 4.2 years, found that blood pressure loweringwas more important than <strong>the</strong> type <strong>of</strong> drug used. 468 Thesestudies support <strong>the</strong> c<strong>on</strong>tenti<strong>on</strong> that <strong>the</strong> benefits <strong>of</strong> loweringblood pressure extend into <strong>the</strong> ‘normal’ blood pressurerange, as suggested by epidemiological data, 466 and thateffects <strong>on</strong> outcome <strong>of</strong> blood pressure lowering are similarwith ACE-inhibitors or ARBs when compared with calciumantag<strong>on</strong>ists. 457,458 A report from <strong>the</strong> ASCOT study claimsthat blood pressure al<strong>on</strong>e does not account for differencesin outcome between different blood pressure treatmentregimens, with <strong>the</strong> combinati<strong>on</strong> <strong>of</strong> CCBs and ACE-inhibitor<strong>the</strong>rapy achieving greater reducti<strong>on</strong> in clinical events than<strong>the</strong> combinati<strong>on</strong> <strong>of</strong> beta-blocker and diuretic. 469 However,<strong>the</strong> accompanying editorial points out that blood pressuredifferences may fully explain <strong>the</strong> differences in outcomebetween <strong>the</strong> two groups. 470 The benefits <strong>of</strong> blood pressurelowering in <strong>the</strong> normal range, are likely to be greatest inthose at highest absolute risk, 471 particularly those wi<strong>the</strong>stablished vascular disease, but <strong>the</strong> level <strong>of</strong> blood pressurebelow which clinically appreciable benefit may be observedhas not been established.The blood pressure lowering effects <strong>of</strong> ramipril and perindoprilcompared with placebo, thus probably c<strong>on</strong>tributedto <strong>the</strong> risk reducti<strong>on</strong> in <strong>the</strong> HOPE and EUROPA studies, butadditi<strong>on</strong>al cardioprotecti<strong>on</strong> may also be afforded byACE-inhibitors. 441 Fur<strong>the</strong>rmore, ACE-inhibiti<strong>on</strong> is well establishedin <strong>the</strong> treatment <strong>of</strong> heart failure or LV dysfuncti<strong>on</strong>, 472and in <strong>the</strong> treatment <strong>of</strong> diabetic patients with renal involvement.370 Thus, it is appropriate to c<strong>on</strong>sider ACE-inhibitorsfor <strong>the</strong> treatment <strong>of</strong> patients with stable angina pectorisand co-existing hypertensi<strong>on</strong>, diabetes, heart failure,asymptomatic LV dysfuncti<strong>on</strong>, or post-MI. In angina patients,without co-existing indicati<strong>on</strong>s for ACE-inhibitor treatment<strong>the</strong> anticipated benefit <strong>of</strong> treatment (possible ARR)should be weighed against costs and risks for side-effects,and <strong>the</strong> dose and agent used <strong>of</strong> proven efficacy for thisindicati<strong>on</strong>.Effects <strong>of</strong> ARB treatment <strong>on</strong> prognosis in ischaemic heartdisease are less well studied, but <strong>the</strong> VALIANT studyshowed similar effects <strong>of</strong> valsartan and captopril treatmentin post-MI patients with heart failure. 473 However, <strong>the</strong>CHARM-preserved study 474 showed no significant benefit <strong>of</strong>candesartan compared with placebo in patients with preservedventricular functi<strong>on</strong>. Thus, ARB treatment may beappropriate <strong>the</strong>rapy for <strong>the</strong> treatment <strong>of</strong> heart failure,hypertensi<strong>on</strong>, or diabetic renal dysfuncti<strong>on</strong> in patientswith angina when ACE-inhibiti<strong>on</strong> is indicated but not tolerated,but <strong>the</strong>re is no indicati<strong>on</strong> for ARB <strong>the</strong>rapy in patientswith preserved ventricular functi<strong>on</strong> without diabetes as asec<strong>on</strong>dary preventive agent.Horm<strong>on</strong>e replacement <strong>the</strong>rapy. Epidemiological evidencesuggested substantial cardiovascular benefits <strong>of</strong> postmenopausaluse <strong>of</strong> horm<strong>on</strong>e replacement <strong>the</strong>rapy (HRT).More recently, however, properly designed prospective,double-blind, placebo-c<strong>on</strong>trolled trials have shown thatHRT with a combinati<strong>on</strong> <strong>of</strong> oral oestrogen/progestin<strong>of</strong>fered no cardiovascular benefit am<strong>on</strong>g women wi<strong>the</strong>stablished disease 475,476 and that <strong>the</strong>re is an increasedrisk <strong>of</strong> developing CVD in primary preventi<strong>on</strong>, and also anincreased risk <strong>of</strong> suffering breast cancer. 477 Primarypreventi<strong>on</strong> with unopposed oestrogen <strong>the</strong>rapy in hysterectomizedwomen <strong>of</strong>fered no cardiovascular protecti<strong>on</strong>. 478New guidelines <strong>the</strong>refore recommend against routine use<strong>of</strong> HRT for chr<strong>on</strong>ic c<strong>on</strong>diti<strong>on</strong>s 349 and current users havebeen advised to taper doses downwards towardsdisc<strong>on</strong>tinuati<strong>on</strong>. 479Beta-blockers. The risk <strong>of</strong> suffering cardiovascular death orMI was reduced by beta-blockers by some 30% in post-MItrials. 480 A recent meta-regressi<strong>on</strong> analysis <strong>of</strong> <strong>the</strong> effects<strong>of</strong> different beta-blockers <strong>on</strong> mortality found n<strong>on</strong>-significantbenefits <strong>of</strong> acute treatment, but a significant 24% relativerisk reducti<strong>on</strong> in mortality with l<strong>on</strong>g-term sec<strong>on</strong>dary preventivetreatment. 481 Beta-blockers with intrinsic sympathomimeticactivity appeared to provide less protecti<strong>on</strong>, and itwas pointed out that <strong>the</strong> most frequently prescribedagent, atenolol, had poor documentati<strong>on</strong> regarding mortalityafter MI. 481 Also, a recent meta-analysis <strong>of</strong> atenololtrials in hypertensi<strong>on</strong> questi<strong>on</strong>ed <strong>the</strong> prognostic benefitafforded by this drug 482 even though beta-blockers as agroup provided similar protecti<strong>on</strong> as o<strong>the</strong>r antihypertensivedrugs in previous meta-analyses. 457,458 It has beenextrapolated from <strong>the</strong> post-MI trials that beta-blockersmay be cardioprotective also in patients with stable
ESC <str<strong>on</strong>g>Guidelines</str<strong>on</strong>g> 33cor<strong>on</strong>ary disease. However, this has not been proven in aplacebo-c<strong>on</strong>trolled trial. The beta-blocker trials post-MIwere performed before <strong>the</strong> implementati<strong>on</strong> <strong>of</strong> o<strong>the</strong>r sec<strong>on</strong>darypreventive <strong>the</strong>rapy, such as treatment withstatins and ACE-inhibitors, which leaves some uncertaintyregarding <strong>the</strong>ir efficacy <strong>on</strong> top <strong>of</strong> a ‘modern’ treatmentstrategy.Large beta-blocker studies in stable angina, <strong>the</strong> APSIS 49and TIBET 48 studies, did not include placebo groups due toc<strong>on</strong>cerns about withholding symptomatic treatment duringl<strong>on</strong>g periods <strong>of</strong> time. In <strong>the</strong> APSIS trial, which comprised809 patients with clinically diagnosed stable anginapectoris, and a median follow-up <strong>of</strong> 3.4 years (.1400patient-years <strong>of</strong> treatment in each group) 49 treatmentwith verapamil SR (240–480 mg/day) was associated with asimilar cardiovascular event rate as treatment with metoprololCR (100–200 mg/day). An extended follow-up <strong>of</strong><strong>the</strong> APSIS study (to a median <strong>of</strong> 9.1 years) did not alter<strong>the</strong>se findings, and showed an excellent prognosis <strong>of</strong> <strong>the</strong>stable angina patients, especially female patients withoutdiabetes, compared with <strong>the</strong>ir background populati<strong>on</strong>. 483In <strong>the</strong> TIBET trial, which comprised 682 patients wi<strong>the</strong>xercise-induced angina pectoris followed during a median<strong>of</strong> 2 years (450 patient-years in each group), 48 <strong>the</strong>effects <strong>of</strong> nifedipine SR (20–40 mg bid) did not differ significantlyfrom those <strong>of</strong> atenolol (50 mg bid), but combinati<strong>on</strong><strong>of</strong> <strong>the</strong> two drugs tended to be advantageous.A smaller study (300 patient-years) in patients with CADand minimal or no symptoms <strong>of</strong> angina compared atenololand placebo treatment (<strong>the</strong> ASIST trial), and showed ahigher incidence <strong>of</strong> a combined endpoint which includedsymptoms requiring treatment in <strong>the</strong> placebo group. 484This c<strong>on</strong>firmed <strong>the</strong> beneficial anti-anginal effects <strong>of</strong> a betablocker,but does not show if treatment alters <strong>the</strong> prognosis<strong>of</strong> patients with stable angina pectoris.Beta-1 blockade by metoprolol or bisoprolol have beenshown to effectively reduce cardiac events in patientswith c<strong>on</strong>gestive heart failure. 485,486 Carvedilol, a n<strong>on</strong>selectivebeta-blocker that also blocks alpha-1 receptors,also reduces risk <strong>of</strong> death and hospitalizati<strong>on</strong>s for cardiovascularcauses in patients with heart failure. 487Calcium channel blockers. Heart rate lowering CCBs mayimprove <strong>the</strong> prognosis <strong>of</strong> post-MI patients, as shown in <strong>the</strong>DAVIT II study for verapamil 488 and in a subgroup analysis<strong>of</strong> patients without signs <strong>of</strong> heart failure in <strong>the</strong> MDPITstudy for diltiazem. 489 Also, in <strong>the</strong> INTERCEPT trial <strong>the</strong>rewas a trend towards a reducti<strong>on</strong> in <strong>the</strong> primary endpoint<strong>of</strong> cardiac death, n<strong>on</strong>-fatal re-infarcti<strong>on</strong> and refractoryischaemia, and a significant reducti<strong>on</strong> <strong>of</strong> <strong>the</strong> need for revascularizati<strong>on</strong>am<strong>on</strong>g post-MI patients treated with diltiazemcompared with placebo. 490 CCBs are also effective antihypertensiveagents without advantages over o<strong>the</strong>r bloodpressure lowering drugs regarding clinical outcomesoverall, but CCB treatment is associated with an increasedrisk <strong>of</strong> heart failure. 457–459Prognostic documentati<strong>on</strong> in stable CAD has not beenavailable for dihydropyridine CCBs until recently. Oldertrials <strong>of</strong> short-acting nifedipine showed no benefit regardinghard endpoints am<strong>on</strong>g patients with CAD, and even anincreased risk <strong>of</strong> dying with high doses <strong>of</strong> <strong>the</strong> drug. 491 Thissparked an intense ‘calcium antag<strong>on</strong>ist debate’ whichpointed out <strong>the</strong> inappropriateness <strong>of</strong> treatment with shortactingvasodilator drugs such as dihydropyridine CCBs. Ameta-analysis <strong>of</strong> <strong>the</strong> safety <strong>of</strong> nifedipine in stable anginapectoris suggested that <strong>the</strong> drug was safe. 492The recently published ACTION trial 493 (Table 5), whichcompared treatment with l<strong>on</strong>g-acting nifedipine andplacebo during 4.9 years <strong>of</strong> follow-up in 7665 patients withstable angina pectoris, is adequately powered for assessments<strong>of</strong> morbidity and mortality. The ACTION trialshowed no benefit <strong>of</strong> treatment with l<strong>on</strong>g-acting nifedipinecompared with placebo with regard to composite endpointsincluding death, MI, refractory angina, debilitating stroke,and heart failure. Nifedipine treatment tended to increase<strong>the</strong> need for peripheral revascularizati<strong>on</strong> (HR 1.25;P ¼ 0.073), but reduced <strong>the</strong> need for cor<strong>on</strong>ary bypasssurgery (HR 0.79; P ¼ 0.0021). The authors c<strong>on</strong>cludedthat nifedipine treatment is safe and reduces <strong>the</strong> needfor cor<strong>on</strong>ary interventi<strong>on</strong>s, 493 but has not been shown tohave beneficial effects <strong>on</strong> hard endpoints such as deathand MI.A major drawback with <strong>the</strong> ACTION trial is <strong>the</strong> liberalinclusi<strong>on</strong> <strong>of</strong> patients with high blood pressure, as <strong>the</strong> bloodpressure lowering effects <strong>of</strong> nifedipine compared withplacebo would be expected to provide health benefits unrelated(or in additi<strong>on</strong>) to those possibly afforded by <strong>the</strong> antiischaemicor o<strong>the</strong>r effects <strong>of</strong> calcium antag<strong>on</strong>ism. Thus,ACTION included patients with blood pressures ,200/105 mmHg, and 52% <strong>of</strong> <strong>the</strong> patients had blood pressures140/90 mmHg at baseline, even though <strong>the</strong> averageblood pressure was 137/80 mmHg. The proporti<strong>on</strong> withblood pressure 140/90 mmHg was reduced to 35% in <strong>the</strong>nifedipine group and 47% in <strong>the</strong> placebo group, 493 indicatingthat attempts to achieve similar blood pressure c<strong>on</strong>trolam<strong>on</strong>g all participants in <strong>the</strong> study were insufficient. Onaverage, nifedipine treatment caused a slight, but significantand sustained elevati<strong>on</strong> <strong>of</strong> heart rate by approximately1 bpm, and reduced blood pressure by 6/3 mmHg.Subgroup analysis <strong>of</strong> <strong>the</strong> ACTION study showed significantbenefit <strong>of</strong> nifedipine treatment am<strong>on</strong>g patients with elevatedblood pressure at baseline but a tendency towardsunfavourable results am<strong>on</strong>g those who had blood pressuresbelow 140/90 mmHg. A 6 mmHg reducti<strong>on</strong> <strong>of</strong> systolic bloodpressure would be expected to reduce major cardiovascularevents by some 25% according to <strong>the</strong> meta-regressi<strong>on</strong>analysis <strong>of</strong> Staessen et al., 458 and this effect should notbe restricted to clearly hypertensive patients. 466 Thus,<strong>the</strong> findings <strong>of</strong> ACTION may not be compatible with <strong>the</strong>benefits <strong>on</strong>e might expect due to <strong>the</strong> reducti<strong>on</strong> <strong>of</strong> bloodpressure.The CAMELOT study 467 compared treatment with amlodipine,enalapril, or placebo in 1991 patients with stableCAD and normal blood pressure during 2 years <strong>of</strong> follow-up.As discussed earlier, amlodipine and enalapril treatmentlowered blood pressure equally and seemed to reduce <strong>the</strong>incidence <strong>of</strong> ‘hard’ endpoints similarly, although <strong>the</strong>seresults were not significant.The abovementi<strong>on</strong>ed APSIS 49 and TIBET 48 studies were notplacebo-c<strong>on</strong>trolled or ‘powered’ to determine effects <strong>on</strong>mortality, but show no major differences between betablockersand CCBs with regard to cardiovascular morbidityand mortality during l<strong>on</strong>g-term treatment <strong>of</strong> stable anginapectoris. A meta-analysis <strong>of</strong> 72 trials comparing calciumantag<strong>on</strong>ists and beta-blockers in stable angina pectoris indicatedsimilar outcomes with <strong>the</strong> two drug classes. 494
34 ESC <str<strong>on</strong>g>Guidelines</str<strong>on</strong>g>However, <strong>the</strong> mean durati<strong>on</strong> <strong>of</strong> <strong>the</strong> studies in thismeta-analysis was <strong>on</strong>ly 8 weeks. A meta-analysis restrictedto six larger trials reached a similar c<strong>on</strong>clusi<strong>on</strong>. 157To c<strong>on</strong>clude, <strong>the</strong>re is no evidence to support <strong>the</strong> use <strong>of</strong>CCBs for prognostic reas<strong>on</strong>s in uncomplicated stableangina, although heart rate lowering CCBs may be used asan alternative to beta-blockers post-MI in patients withou<strong>the</strong>art failure who do not tolerate beta-blockers.Recommendati<strong>on</strong>s for pharmacological <strong>the</strong>rapy toimprove prognosis in patients with stable anginaClass I(1) Aspirin 75 mg daily in all patients without specific c<strong>on</strong>traindicati<strong>on</strong>s(i.e. active GI bleeding, aspirin allergy,or previous aspirin intolerance) (level <strong>of</strong> evidence A)(2) Statin <strong>the</strong>rapy for all patients with cor<strong>on</strong>ary disease(level <strong>of</strong> evidence A)(3) ACE-inhibitor <strong>the</strong>rapy in patients with coincident indicati<strong>on</strong>sfor ACE-inhibiti<strong>on</strong>, such as hypertensi<strong>on</strong>,heart failure, LV dysfuncti<strong>on</strong>, prior MI with LV dysfuncti<strong>on</strong>,or diabetes (level <strong>of</strong> evidence A)(4) Oral beta-blocker <strong>the</strong>rapy in patients post-MI or withheart failure (level <strong>of</strong> evidence A)Class IIa(1) ACE-inhibitor <strong>the</strong>rapy in all patients with angina andproven cor<strong>on</strong>ary disease (level <strong>of</strong> evidence B)(2) Clopidogrel as an alternative antiplatelet agent inpatients with stable angina who cannot take aspirin(e.g. aspirin allergic) (level <strong>of</strong> evidence B)(3) High dose statin <strong>the</strong>rapy in high-risk (.2% annual CVmortality) patients with proven cor<strong>on</strong>ary disease(level <strong>of</strong> evidence B)Class IIb(1) Fibrate <strong>the</strong>rapy in patients with low HDL and hightriglycerides who have diabetes or <strong>the</strong> metabolicsyndrome (level <strong>of</strong> evidence B)(2) Fibrate or nicotinic acid as adjunctive <strong>the</strong>rapy to statinin patients with low HDL and high triglycerides at highrisk (.2% annual CV mortality) (level <strong>of</strong> evidence C)Pharmacological treatment <strong>of</strong> symptoms and ischaemiaSymptoms <strong>of</strong> angina pectoris and signs <strong>of</strong> ischaemia (alsosilent ischaemia) may be reduced by drugs that reducemyocardial oxygen demand and/or increase blood flow to<strong>the</strong> ischaemic area. Comm<strong>on</strong>ly used anti-anginal drugs arebeta-blockers, calcium antag<strong>on</strong>ists, and organic nitrates.Short-acting nitrates. Rapidly acting formulati<strong>on</strong>s <strong>of</strong> nitroglycerinprovide effective symptom relief in c<strong>on</strong>necti<strong>on</strong>with attacks <strong>of</strong> angina pectoris, and may be used for ‘situati<strong>on</strong>alprophylaxis’. 157,377,495,496 The pain relieving and antiischaemiceffects are related to venodilatati<strong>on</strong> and reduceddiastolic filling <strong>of</strong> <strong>the</strong> heart (reduced intracardiac pressure),which promotes subendocardial perfusi<strong>on</strong>. Cor<strong>on</strong>aryvasodilatati<strong>on</strong> and antag<strong>on</strong>ism <strong>of</strong> cor<strong>on</strong>ary vasospasm mayc<strong>on</strong>tribute. Nitrate tolerance (see below) blunts resp<strong>on</strong>sesto short-acting nitroglycerin, and should be avoided.There is marked first-pass metabolism <strong>of</strong> orally administerednitroglycerin. Absorpti<strong>on</strong> via <strong>the</strong> oral mucosa is rapidand by-passes <strong>the</strong> liver, leading to increased bioavailability.Thus, rapid and efficient symptom relief by nitroglycerinmay be achieved with sublingual or buccal tablets, oran oral spray. Buccal tablets have a l<strong>on</strong>ger durati<strong>on</strong> <strong>of</strong>acti<strong>on</strong> and may be useful for situati<strong>on</strong>al prophylaxis.Nitroglycerin tablets decay when exposed to air, andopened c<strong>on</strong>tainers should be discarded within 3 m<strong>on</strong>ths;spray formulati<strong>on</strong>s are stable.Nitroglycerin causes dose-dependent vasodilator sideeffects,such as headache and flushing. Overdosing maycause postural hypotensi<strong>on</strong> and reflexogenic cardiac sympa<strong>the</strong>ticactivati<strong>on</strong> with tachycardia, leading to ‘paradoxical’angina. An attack <strong>of</strong> angina that does not resp<strong>on</strong>d toshort-acting nitroglycerin should be regarded as a possibleMI. Thus, patients should be carefully instructed abouthow to use short-acting nitroglycerin. Short-acting nitratec<strong>on</strong>sumpti<strong>on</strong> is a simple and good measure <strong>of</strong> treatmenteffects with o<strong>the</strong>r anti-anginal drugs.L<strong>on</strong>g-acting nitrates. Treatment with l<strong>on</strong>g-acting nitratesreduces <strong>the</strong> frequency and severity <strong>of</strong> anginal attacks, andmay increase exercise tolerance. 157,377,495,496 L<strong>on</strong>g-actingnitrate treatment is <strong>on</strong>ly symptomatic, as studies after MIhave failed to show prognostic benefit <strong>of</strong> such treatment.497,498 Side effects are mainly related to vasodilatati<strong>on</strong>,i.e. headaches and flushing, as described earlier.Several l<strong>on</strong>g-acting nitrates are available. Isosobidedinitrate (ISDN) has an intermediate durati<strong>on</strong> <strong>of</strong> acti<strong>on</strong>,and requires more than <strong>on</strong>ce daily dosing. Isosorbide-5-m<strong>on</strong><strong>on</strong>itrate (ISMN) is supplied in various formulati<strong>on</strong>sthat provide extended acti<strong>on</strong> <strong>of</strong> a suitable durati<strong>on</strong> (seebelow). Nitroglycerin patches for transdermal treatmentallow full c<strong>on</strong>trol <strong>of</strong> <strong>the</strong> durati<strong>on</strong> <strong>of</strong> acti<strong>on</strong>, but are moreexpensive than ISDN or ISMN.Nitrate tolerance may develop when nitrate levels arec<strong>on</strong>tinuously maintained above a certain threshold level,and results in poorer protecti<strong>on</strong> against angina attacks andresistance to <strong>the</strong> pain relieving effects <strong>of</strong> short-acting nitroglycerin.Thus, patients treated with l<strong>on</strong>g-acting nitratesshould have a ‘nitrate-free’ interval each day to preserve<strong>the</strong> <strong>the</strong>rapeutic effects. This may be achieved with appropriatetiming <strong>of</strong> doses <strong>of</strong> intermediate acting ISDN or withformulati<strong>on</strong>s <strong>of</strong> ISMN that provide a suitable plasma c<strong>on</strong>centrati<strong>on</strong>pr<strong>of</strong>ile. C<strong>on</strong>tinuous transdermal nitroglycerin<strong>the</strong>rapy is not effective and patients should remove <strong>the</strong>patches during part <strong>of</strong> <strong>the</strong> day or at night to achieve <strong>the</strong>nitrate-free interval; a decreased anginal threshold andrebound angina may, however, occur when patches areremoved. 499–501 Transdermal nitroglycerin has been moreclearly associated with rebound ischaemia than oral l<strong>on</strong>gactingnitrate treatment. 495Beta-blockers. Beta-blockers are well documented for <strong>the</strong>preventi<strong>on</strong> <strong>of</strong> anginal symptoms and ischaemia. 157,377,502,503They reduce oxygen demand by reducing heart rate andc<strong>on</strong>tractility, and by reducing blood pressure. Resting andexercise heart rate will be reduced by most beta-blockersexcept those with partial ag<strong>on</strong>ist activity where <strong>on</strong>ly <strong>the</strong> exerciseheart rate is reduced. Perfusi<strong>on</strong> <strong>of</strong> ischaemic areas maybe improved by prol<strong>on</strong>ging diastole (i.e. <strong>the</strong> perfusi<strong>on</strong>time), and by ‘reverse cor<strong>on</strong>ary steal’ due to increased vascularresistance in n<strong>on</strong>-ischaemic areas. 425 Beta-blockers arealso well established in <strong>the</strong> treatment <strong>of</strong> hypertensi<strong>on</strong>. 286Beta-1 selective antag<strong>on</strong>ists are as effective as n<strong>on</strong>selectiveantag<strong>on</strong>ists, 157 indicating that <strong>the</strong> beta-1 selectivesympa<strong>the</strong>tic neurotransmitter, noradrenaline, is <strong>the</strong> primarybeta-adrenergic target for inhibiti<strong>on</strong>. Beta-1 selective
ESC <str<strong>on</strong>g>Guidelines</str<strong>on</strong>g> 35agents are preferred due to advantages c<strong>on</strong>cerningside-effects and precauti<strong>on</strong>s compared with n<strong>on</strong>-selectivebeta-blockers. 157,377 Comm<strong>on</strong>ly used beta-1 blockers withgood documentati<strong>on</strong> as anti-anginal drugs are metoprolol,atenolol, and bisoprolol. The anti-anginal and anti-ischaemiceffects are related to <strong>the</strong> degree <strong>of</strong> cardiac beta-1 adrenoceptorblockade, i.e. to <strong>the</strong> plasma c<strong>on</strong>centrati<strong>on</strong> <strong>of</strong> <strong>the</strong>drug, whereas <strong>the</strong> blood pressure lowering effect in hypertensi<strong>on</strong>is not. To achieve 24 h efficacy a beta-1 blockerwith a l<strong>on</strong>g half-life (e.g. bisoprolol) or a formulati<strong>on</strong> providingan extended plasma c<strong>on</strong>centrati<strong>on</strong> pr<strong>of</strong>ile (e.g. metoprololCR) may be used. For atenolol (with a plasma half-life <strong>of</strong>6–9 h), twice daily dosing may be better, but increasing <strong>the</strong>dose also extends <strong>the</strong> durati<strong>on</strong> <strong>of</strong> acti<strong>on</strong>. Target doses forfull anti-anginal effects are: bisoprolol 10 mg od, metoprololCR 200 mg od, atenolol 100 mg/day od (or 50 mg bid). Thedegree <strong>of</strong> beta-blockade may be assessed by exercisetesting. Beta-blockers are effective anti-anginal drugs whichincrease exercise tolerance, and decrease symptoms andshort-acting nitrate c<strong>on</strong>sumpti<strong>on</strong>. 157,377,502,503 However,symptoms may increase <strong>on</strong> beta-blockade in patients withvasospastic angina.Side-effects <strong>of</strong> beta-blockade include cold extremitiesand symptomatic bradycardia, both <strong>of</strong> which are relatedto cardiac inhibiti<strong>on</strong>, and increased respiratory symptomsin asthma/COPD (less comm<strong>on</strong> with beta-1 selectiveagents). Beta-blockers may cause fatigue, but <strong>on</strong>ly 0.4% <strong>of</strong>patients in trials disc<strong>on</strong>tinued treatment for this reas<strong>on</strong>. 504Similarly, depressi<strong>on</strong> was not increased am<strong>on</strong>g beta-blockertreated patients, and sexual dysfuncti<strong>on</strong> was <strong>on</strong>ly found in5/1000 patient-years <strong>of</strong> treatment (leading to disc<strong>on</strong>tinuati<strong>on</strong>in 2/1000). 505 Quality <strong>of</strong> life, which has been extensivelystudied in <strong>the</strong> treatment <strong>of</strong> hypertensi<strong>on</strong>, is wellpreserved with beta-blocker treatment <strong>of</strong> hypertensivepatients, 505,506 but this has not been systematicallystudied in patients with stable angina. 379 Psychosocial variablesreflecting quality <strong>of</strong> life were similarly influenced bymetoprolol and verapamil treatment in <strong>the</strong> APSIS study. 49Thus, <strong>the</strong> side-effect pr<strong>of</strong>ile <strong>of</strong> beta-blockade may not beas unpalatable to patients as comm<strong>on</strong>ly perceived.Calcium channel blockers. CCBs are also well establishedanti-anginal agents. 157,377,467,502,503 This is a heterogeneousclass <strong>of</strong> drugs which dilatate cor<strong>on</strong>ary and o<strong>the</strong>r arteries byinhibiting calcium influx via L-type channels. N<strong>on</strong>-selectiveor heart rate lowering CCBs (verapamil and diltiazem) alsoto some degree reduce myocardial c<strong>on</strong>tractility, heartrate, and A-V nodal c<strong>on</strong>ducti<strong>on</strong>. 157,377 Even vasoselectivedihydropyridine CCBs (e.g. nifedipine, amlodipine, and felodipine)may cause some cardiodepressi<strong>on</strong>, but this is counteractedby reflexogenic cardiac sympa<strong>the</strong>tic activati<strong>on</strong>with slight increases in heart rate which subside over time.However, signs <strong>of</strong> sympa<strong>the</strong>tic activati<strong>on</strong> may be seen evenafter m<strong>on</strong>ths <strong>of</strong> treatment with a dihydropyridine CCB. 507L<strong>on</strong>g-acting CCBs (e.g. amlodipine) or sustained releaseformulati<strong>on</strong>s <strong>of</strong> short-acting CCBs (e.g. nifedipine, felodipine,verapamil, and diltiazem) are preferred, to minimizefluctuati<strong>on</strong>s <strong>of</strong> plasma c<strong>on</strong>centrati<strong>on</strong>s and cardiovasculareffects. 508 Side effects are also c<strong>on</strong>centrati<strong>on</strong>-dependent,and mainly related to <strong>the</strong> arterial vasodilator resp<strong>on</strong>ses(headache, flushing, and ankle oedema). These effects aremore pr<strong>on</strong>ounced with dihydropyridine CCBs. Verapamilmay cause c<strong>on</strong>stipati<strong>on</strong>.The anti-anginal effects <strong>of</strong> CCBs are related to decreasedcardiac work due to systemic vasodilatati<strong>on</strong>, as well as cor<strong>on</strong>aryvasodilatati<strong>on</strong> and counteracti<strong>on</strong> <strong>of</strong> vasospasm. 157,377CCBs are especially effective in patients with vasospastic(prinzmetal) angina, but in some patients CCBs may,however, increase ischaemia. 509The CAMELOT study 467 showed that <strong>the</strong> anti-anginaleffects <strong>of</strong> amlodipine compared with placebo treatment significantlyreduced hospitalizati<strong>on</strong> for angina, as well as <strong>the</strong>need for revascularizati<strong>on</strong> during a 2-year follow-up.Enalapril treatment was not associated with similar effects<strong>on</strong> ischaemia-related outcomes. In <strong>the</strong> CAPE study, 510 treatmentwith amlodipine compared with placebo resulted in amodest, but significant fur<strong>the</strong>r reducti<strong>on</strong> <strong>of</strong> ischaemia <strong>on</strong>Holter m<strong>on</strong>itoring (placebo effects were ra<strong>the</strong>r pr<strong>on</strong>ounced)after 7 weeks <strong>of</strong> treatment. The patients reported greaterreducti<strong>on</strong>s <strong>of</strong> anginal attacks (70 vs. 44%) and a more pr<strong>on</strong>ouncedreducti<strong>on</strong> <strong>of</strong> nitroglycerin c<strong>on</strong>sumpti<strong>on</strong> (67 vs.22%) during week 10 <strong>of</strong> amlodipine compared with placebotreatment. The side-effect pr<strong>of</strong>ile <strong>of</strong> amlodipine was favourablein both CAMELOT and CAPE. In <strong>the</strong> ACTION study,although not associated with a reducti<strong>on</strong> in <strong>the</strong> primary endpoint(death, acute MI, refractory angina, new overt heartfailure, debilitating stroke, and peripheral revascularizati<strong>on</strong>),nifedipine <strong>the</strong>rapy was associated with reducedneed for cor<strong>on</strong>ary bypass surgery (HR 0.79, P ¼ 0.002). 493The anti-anginal and anti-ischaemic effects <strong>of</strong> CCBs areadditive to those <strong>of</strong> beta-blockers in many, but not allpatients. Dihydropyridine CCBs are suitable for combinati<strong>on</strong>with beta-blockers, which counteract <strong>the</strong> reflexogeniccardiac sympa<strong>the</strong>tic activati<strong>on</strong>. Heart rate lowering CCBsmay cause c<strong>on</strong>ducti<strong>on</strong> disturbances in predisposed patientstreated with beta-blockers. All CCBs may precipitate heartfailure in predisposed patients. Attempts to use dihydropyridineCCBs for vasodilator treatment <strong>of</strong> heart failurehave not been successful. However, amlodipine may beused for <strong>the</strong> treatment <strong>of</strong> angina in patients with compensatedheart failure if not c<strong>on</strong>trolled by o<strong>the</strong>r <strong>the</strong>rapy (i.e.nitrates, beta-blockers). 511Comparis<strong>on</strong> <strong>of</strong> beta-blocker and calcium antag<strong>on</strong>ist (CCB)treatment in stable angina. The IMAGE study 512 comparedpatients with stable angina treated with metoprolol CR200 mg od or nifedipine SR 20 mg bid during 6 weeks (140patients in each group). Both metoprolol and nifedipine prol<strong>on</strong>gedexercise tolerance over baseline levels, with greaterimprovement in patients receiving metoprolol (P , 0.05).Resp<strong>on</strong>ses to <strong>the</strong> two drugs were variable, and were difficultto predict. In <strong>the</strong> APSIS study, treatment with verapamil SRfor 1 m<strong>on</strong>th was slightly more effective than metoprolol CRin increasing exercise tolerance. 513 However, althoughexercise-induced ischaemia was predictive <strong>of</strong> cardiovascularevents in <strong>the</strong> study, 513 short-term treatment effects <strong>on</strong>exercise-induced ischaemia did not independently predictimprovement in l<strong>on</strong>g-term outcome. This highlights <strong>the</strong>important difference between treatment <strong>of</strong> symptomsand ischaemia and treatment aimed prognosis. Severity <strong>of</strong>ischaemia <strong>on</strong> baseline assessment acts as a marker <strong>of</strong> <strong>the</strong>underlying severity <strong>of</strong> cor<strong>on</strong>ary disease. But it is <strong>the</strong> severity<strong>of</strong> disease which influences <strong>the</strong> likelihood <strong>of</strong> plaque destabilizati<strong>on</strong>,and <strong>the</strong> propensity to and severity <strong>of</strong> thromboticcomplicati<strong>on</strong>s if and when plaque becomes unstable,
36 ESC <str<strong>on</strong>g>Guidelines</str<strong>on</strong>g>factors which are not modified by traditi<strong>on</strong>al anti-ischaemicagents.The TIBBS study 514 showed anti-ischaemic and anti-anginaleffects <strong>of</strong> both bisoprolol and nifedipine, but bisoprolol wasclearly more effective. The TIBET study compared <strong>the</strong>effects <strong>of</strong> atenolol, nifedipine, or <strong>the</strong>ir combinati<strong>on</strong> <strong>on</strong>exercise-induced ischaemia and <strong>the</strong> total ischaemic burdenin a double-blind, parallel group design. Both medicati<strong>on</strong>s,al<strong>on</strong>e and in combinati<strong>on</strong>, caused significant improvementsin exercise parameters and significant reducti<strong>on</strong>s in ischaemicactivity during daily activities when compared with placebobut <strong>the</strong>re were no significant differences between groupsfor any <strong>of</strong> <strong>the</strong> measured ischaemic parameters. There weresignificantly more withdrawals because <strong>of</strong> side-effects in<strong>the</strong> nifedipine group compared with <strong>the</strong> atenolol and <strong>the</strong>combinati<strong>on</strong> groups. 48,515 Meta-analyses comparing effects<strong>of</strong> beta-blockers and CCBs in stable angina pectoris indicatethat beta-blockers are more effective than CCBs in reducinganginal episodes, 494 but that effects <strong>on</strong> exercise toleranceand ischaemia <strong>of</strong> <strong>the</strong> two drug classes are similar. 157,494Thus, in <strong>the</strong> absence <strong>of</strong> prior MI, <strong>the</strong> available datasuggest that <strong>the</strong> choice between a beta-blocker and a CCBfor anti-anginal treatment may be guided by individualtolerance and <strong>the</strong> presence <strong>of</strong> o<strong>the</strong>r disease andco-treatment. If <strong>the</strong>se factors are equally weighted, abeta-blocker is recommended as <strong>the</strong> first choice.Comparis<strong>on</strong> <strong>of</strong> nitrates with beta-blockers or CCBs. Thereare relatively few studies comparing anti-anginal and antiischaemiceffects <strong>of</strong> l<strong>on</strong>g-acting nitrates with beta-blockersor CCBs, and <strong>the</strong>re is no documentati<strong>on</strong> c<strong>on</strong>cerning possibleeffects <strong>of</strong> nitrates <strong>on</strong> morbidity in stable angina pectoris. 494There were n<strong>on</strong>-significant trend towards less nitroglycerinuse with beta-blockers, and fewer angina episodes perweek with CCBs compared with l<strong>on</strong>g-acting nitrates in <strong>the</strong>meta-analysis by Heidenreich et al. 494 Thus l<strong>on</strong>g-actingnitrates have no overall <strong>the</strong>rapeutic advantages over betablockersor CCBs.Potassium channel openers. The principal agent in this class,nicorandil, has a dual mechanism <strong>of</strong> acti<strong>on</strong>, and is a potassiumchannel activator with a nitrate moiety and nitrate likeeffects. 516 Nicorandil is administered at a usual dose <strong>of</strong>20 mg bid for <strong>the</strong> preventi<strong>on</strong> <strong>of</strong> angina. Tolerance to <strong>the</strong>anti-anginal effect may develop with chr<strong>on</strong>ic dosing, 517but cross-tolerance with nitrates does not seem to be aproblem. 516 In additi<strong>on</strong> to its anti-anginal properties,nicorandil is thought to have cardioprotective properties.516,518 The Impact Of Nicorandil in <strong>Angina</strong> (IONA) trialshowed a significant reducti<strong>on</strong> <strong>of</strong> major cor<strong>on</strong>ary events instable angina patients treated with nicorandil comparedwith placebo as add-<strong>on</strong> to c<strong>on</strong>venti<strong>on</strong>al <strong>the</strong>rapy. 254However, <strong>the</strong> result was driven by effects <strong>of</strong> nicorandil <strong>on</strong>‘hospital admissi<strong>on</strong> for cardiac chest pain’, and <strong>the</strong> riskreducti<strong>on</strong> regarding cardiac death or n<strong>on</strong>-fatal MI during1.6 years <strong>of</strong> treatment was n<strong>on</strong>-significant; 254 thus <strong>the</strong>value <strong>of</strong> <strong>the</strong> treatment effect has been argued. 518Nicorandil is not available in all countries.O<strong>the</strong>r agents. Sinus node inhibitors, such as ivabradine, actby selectivity inhibiting <strong>the</strong> cardiac pacemaker current I f,and have negative chr<strong>on</strong>otropic effects both at rest andduring exercise. I f inhibiti<strong>on</strong> has proven anti-anginal efficacy461,519,520 and ivabradine may be used as an alternativeagent in patients who do not tolerate beta-blockade. It hasbeen licenced by <strong>the</strong> EMEA for this purpose.Metabolically acting agents protect from ischaemia byincreasing glucose metabolism relative to that <strong>of</strong> fattyacids. Trimetazidine and ranolazine are both c<strong>on</strong>sidered asmetabolic anti-anginal drugs. However, ranolazine has alsomore recently been shown to be an inhibitor <strong>of</strong> <strong>the</strong> latesodium current, 521 which is activated in case <strong>of</strong> ischaemia,leading to calcium overload <strong>of</strong> <strong>the</strong> ischaemic myocardium,decreased compliance, increased LV stiffness, and compressi<strong>on</strong><strong>of</strong> <strong>the</strong> capillaries. The inhibiti<strong>on</strong> <strong>of</strong> <strong>the</strong> latesodium current by ranolazine reverses <strong>the</strong>se effects, andprevents calcium overload, and <strong>the</strong> subsequent c<strong>on</strong>sequences<strong>the</strong>re<strong>of</strong>. 522,523Both trimetazidine 524–526 and ranolazine 527,528 have beenshown to have anti-anginal efficacy. They may be used incombinati<strong>on</strong> <strong>the</strong>rapy with haemodynamically actingagents, as <strong>the</strong>ir primary effect is not through reducti<strong>on</strong> inheart rate or blood pressure. Trimetazidine has been availablefor several years, but not in all countries. Ranolazine,although under intensive investigati<strong>on</strong> is not yet licencedfor use by <strong>the</strong> EMEA. Whe<strong>the</strong>r <strong>the</strong>se drugs influence <strong>the</strong>prognosis <strong>of</strong> patients with stable angina has not beendetermined.Molsidomine is a vasodilator with an acti<strong>on</strong> similar to that<strong>of</strong> organic nitrates and in <strong>the</strong> appropriate dosage is aneffective anti-ischaemic and anti-anginal agent. 529 It is notavailable in all countries.Recommendati<strong>on</strong>s for pharmacological <strong>the</strong>rapy. Antianginaldrug treatment should be tailored to <strong>the</strong> needs <strong>of</strong><strong>the</strong> individual patient, and should be m<strong>on</strong>itored individually.Short-acting nitrate <strong>the</strong>rapy should be prescribed for allpatients for immediate relief <strong>of</strong> acute symptoms as tolerated.Although different types <strong>of</strong> drugs have been shownto have additive anti-anginal effects in clinical trials, thismay not necessarily be so in <strong>the</strong> individual patient. Moreintense anti-anginal treatment may also cause problems,as it has been shown that three anti-anginal drugs mayprovide less symptomatic protecti<strong>on</strong> than two drugs. 530,531Thus, <strong>the</strong> dosing <strong>of</strong> <strong>on</strong>e drug should be optimized beforeadding ano<strong>the</strong>r <strong>on</strong>e, and it is advisable to switch drug combinati<strong>on</strong>sbefore attempting a three drug regimen. Pooradherence is always a factor to c<strong>on</strong>sider when drug<strong>the</strong>rapy is unsuccessful.An algorithm depicting <strong>the</strong> strategy for medical management<strong>of</strong> stable angina, if revascularizati<strong>on</strong> is not c<strong>on</strong>siderednecessary after initial evaluati<strong>on</strong> and risk stratificati<strong>on</strong>,includes treatments aimed at improving prognosis and symptomsand is shown in Figure 7. The following recommendati<strong>on</strong>spertain to anti-anginal <strong>the</strong>rapy and <strong>the</strong> level <strong>of</strong>evidence refers to anti-anginal or anti-ischaemic efficacyunless stated o<strong>the</strong>rwise.Recommendati<strong>on</strong>s for pharmacological <strong>the</strong>rapy toimprove symptoms and/or reduce ischaemia in patientswith stable anginaClass I(1) Provide short-acting nitroglycerin for acute symptomrelief and situati<strong>on</strong>al prophylaxis, with appropriateinstructi<strong>on</strong>s <strong>on</strong> how to use <strong>the</strong> treatment (level <strong>of</strong>evidence B)
ESC <str<strong>on</strong>g>Guidelines</str<strong>on</strong>g> 37(2) Test <strong>the</strong> effects <strong>of</strong> a beta-1 blocker, and titrate to fulldose; c<strong>on</strong>sider <strong>the</strong> need for 24 h protecti<strong>on</strong> againstischaemia (level <strong>of</strong> evidence A)(3) In case <strong>of</strong> beta-blocker intolerance or poor efficacyattempt m<strong>on</strong>o<strong>the</strong>rapy with a CCB (level <strong>of</strong> evidence A),l<strong>on</strong>g-acting nitrate (level <strong>of</strong> evidence C), or nicorandil(level <strong>of</strong> evidence C)(4) If <strong>the</strong> effects <strong>of</strong> beta-blocker m<strong>on</strong>o<strong>the</strong>rapy are insufficient,add a dihydropyridine CCB (level <strong>of</strong> evidence B)Class IIa(1) In case <strong>of</strong> beta-blocker intolerance try sinus nodeinhibitor (level <strong>of</strong> evidence B)(2) If CCB m<strong>on</strong>o<strong>the</strong>rapy or combinati<strong>on</strong> <strong>the</strong>rapy (CCB withbeta-blocker) is unsuccessful, substitute <strong>the</strong> CCB with al<strong>on</strong>g-acting nitrate or nicorandil. Be careful to avoidnitrate tolerance (level <strong>of</strong> evidence C)Class IIb(1) Metabolic agents may be used, where available, asadd-<strong>on</strong> <strong>the</strong>rapy, or as substituti<strong>on</strong> <strong>the</strong>rapy when c<strong>on</strong>venti<strong>on</strong>aldrugs are not tolerated (level <strong>of</strong> evidence B)C<strong>on</strong>sider triple <strong>the</strong>rapy <strong>on</strong>ly if optimal two drug regimensare insufficient, and evaluate <strong>the</strong> effects <strong>of</strong> additi<strong>on</strong>al drugscarefully. Patients whose symptoms are poorly c<strong>on</strong>trolled <strong>on</strong>double <strong>the</strong>rapy should be assessed for suitability for revascularizati<strong>on</strong>,as should those who express a str<strong>on</strong>g preferencefor revascularizati<strong>on</strong> ra<strong>the</strong>r than pharmacological<strong>the</strong>rapy. The <strong>on</strong>going need for medicati<strong>on</strong> to improve prognosisirrespective <strong>of</strong> revascularizati<strong>on</strong> status, and <strong>the</strong>balance <strong>of</strong> risk and benefit <strong>on</strong> an individual basis, shouldbe explained in detail. Despite <strong>the</strong> array <strong>of</strong> <strong>the</strong>rapeuticopti<strong>on</strong>s outlined, <strong>the</strong> management <strong>of</strong> refractory angina c<strong>on</strong>tinuesto pose a challenge, and management opti<strong>on</strong>s in suchcases are outlined in a separate secti<strong>on</strong> below.Special <strong>the</strong>rapeutic c<strong>on</strong>siderati<strong>on</strong>s: cardiac Syndrome Xand vasospastic anginaTreatment <strong>of</strong> Syndrome X. Treatment should focus <strong>on</strong> symptomaticrelief. 532 As nitrates are effective in about half <strong>of</strong> <strong>the</strong>patients, 303,532 it is reas<strong>on</strong>able to start treatment withl<strong>on</strong>g-acting nitrates. If symptoms persist, calcium antag<strong>on</strong>ists533 and b-blockers, 534 which are beneficial in Syndrome Xpatients, may be added. Although a-adrenergic blockadeincreases vasodilator reserve in patients with Syndrome X, 535a-adrenergic blocking agents are clinically inefficient. 536,537There are reports that o<strong>the</strong>r drugs such as nicorandil 538 andtrimetazidine 539 might be helpful in some patients.ACE-inhibitors 540 and statins 541 are helpful to reverseunderlying endo<strong>the</strong>lial dysfuncti<strong>on</strong>. Thus, <strong>the</strong>se drugsshould be actively c<strong>on</strong>sidered for patients with Syndrome Xas part <strong>of</strong> <strong>the</strong>ir risk factor management, 542 and <strong>the</strong>re aresome data to suggest that ACE-inhibitors and statins mayalso be beneficial in reducing exercise-induced ischaemia inthis populati<strong>on</strong>. 541,543,544The challenge <strong>of</strong> achieving l<strong>on</strong>g-lasting <strong>the</strong>rapeutic effectsin patients with Syndrome X requires a multidisciplinaryapproach. 545 This might include analgesic interventi<strong>on</strong>using imipramine 546 or aminophylline, 547 psychological interventi<strong>on</strong>,545 electrostimulati<strong>on</strong> techniques, 548 and physicaltraining. 549 Some studies <strong>of</strong> transdermal horm<strong>on</strong>e replacement<strong>the</strong>rapy 550,551 in post-menopausal patients haveshown an improvement in endo<strong>the</strong>lial functi<strong>on</strong> and symptoms,but in <strong>the</strong> light <strong>of</strong> recent trials documenting adversecardiovascular outcomes with <strong>the</strong> use <strong>of</strong> HRT, cauti<strong>on</strong> isadvised in prescripti<strong>on</strong> <strong>of</strong> HRT for this purpose.Recommendati<strong>on</strong>s for pharmacological <strong>the</strong>rapy toimprove symptoms in patients with Syndrome XClass I(1) Therapy with nitrates, b-blockers, and calcium antag<strong>on</strong>istsal<strong>on</strong>e or in combinati<strong>on</strong> (level <strong>of</strong> evidence B)(2) Statin <strong>the</strong>rapy in patients with hyperlipidaemia (level<strong>of</strong> evidence B)(3) ACE inhibiti<strong>on</strong> in patients with hypertensi<strong>on</strong> (level <strong>of</strong>evidence C)Class IIa(1) Trial <strong>of</strong> <strong>the</strong>rapy with o<strong>the</strong>r anti-anginals includingnicorandil and metabolic agents (level <strong>of</strong> evidence C)Class IIb(1) Aminophylline for c<strong>on</strong>tinued pain, despite Class Imeasures (level <strong>of</strong> evidence C)(2) Imipramine for c<strong>on</strong>tinued pain, despite Class Imeasures (level <strong>of</strong> evidence C)Treatment <strong>of</strong> vasospastic angina. Removal <strong>of</strong> precipitatingfactors such as cessati<strong>on</strong> <strong>of</strong> smoking is essential. 552 Themain elements <strong>of</strong> drug <strong>the</strong>rapy are nitrates and calciumantag<strong>on</strong>ists. Although nitrates are highly effective in abolishingacute vasospasm, <strong>the</strong>y are not as successful in preventingattacks <strong>of</strong> resting angina. 340 CCBs are moreeffective in alleviating <strong>the</strong> signs and symptoms <strong>of</strong> cor<strong>on</strong>aryspasm and treatment should be aimed at using high doses(up to 480 mg/d verapamil, up to 260 mg/d diltiazem, upto 120 mg/d nifedipine). However, calcium antag<strong>on</strong>istsachieve a complete resoluti<strong>on</strong> <strong>of</strong> symptoms in <strong>on</strong>ly 38% <strong>of</strong>patients. 340 In most patients, a combinati<strong>on</strong> <strong>the</strong>rapy withl<strong>on</strong>g-acting nitrates and high doses <strong>of</strong> calcium antag<strong>on</strong>istswill result in an improvement <strong>of</strong> symptoms. In patientswith resistant symptoms, additi<strong>on</strong> <strong>of</strong> a sec<strong>on</strong>d calciumantag<strong>on</strong>ist <strong>of</strong> ano<strong>the</strong>r class may be successful. Medical treatmentseems to be more effective in women and in patientswith ST-elevati<strong>on</strong> during provocati<strong>on</strong> testing. 340The role <strong>of</strong> a-blockers is c<strong>on</strong>troversial but occasi<strong>on</strong>al<strong>the</strong>rapeutic benefit has been reported. 553 Nicorandil, a potassiumchannel activator, may also be useful in occasi<strong>on</strong>alpatients with refractory vasospastic angina. 554 Reports <strong>of</strong>success in treating drug-resistant focal vasospasm by cor<strong>on</strong>aryartery stenting exist, 555,556 but this approach is notadvocated for widespread applicati<strong>on</strong>. CABG is not indicatedbecause spasm distal to <strong>the</strong> anastomosis may occur.Sp<strong>on</strong>taneous remissi<strong>on</strong> <strong>of</strong> spasmodicity occurs in abouthalf <strong>of</strong> western people following medical treatment for atleast 1 year. 557 Thus, it is acceptable to taper and disc<strong>on</strong>tinuetreatment 6–12 m<strong>on</strong>ths after angina has disappeared<strong>on</strong> drug treatment. If vasospasm occurs in associati<strong>on</strong> withsignificant cor<strong>on</strong>ary disease, guideline recommendati<strong>on</strong>sfor treatments to improve prognosis and sec<strong>on</strong>dary preventi<strong>on</strong>should also be adhered to.Recommendati<strong>on</strong>s for pharmacological <strong>the</strong>rapy <strong>of</strong>vasospastic anginaClass I
38 ESC <str<strong>on</strong>g>Guidelines</str<strong>on</strong>g>(1) Treatment with calcium antag<strong>on</strong>ists and if necessarynitrates in patients whose cor<strong>on</strong>ary arteriogram isnormal or shows <strong>on</strong>ly n<strong>on</strong>-obstructive lesi<strong>on</strong>s (level <strong>of</strong>evidence B)Myocardial revascularizati<strong>on</strong>There are two well-established approaches to revascularizati<strong>on</strong>for treatment <strong>of</strong> chr<strong>on</strong>ic stable angina caused bycor<strong>on</strong>ary a<strong>the</strong>rosclerosis: surgical revascularizati<strong>on</strong>, cor<strong>on</strong>aryartery bypass graft (CABG), and percutaneous cor<strong>on</strong>aryinterventi<strong>on</strong> (PCI). Currently, both methods are facingrapid development with <strong>the</strong> introducti<strong>on</strong> <strong>of</strong> minimally invasiveand <strong>of</strong>f-pump surgery and drug-eluting stents. As in <strong>the</strong>case <strong>of</strong> pharmacological <strong>the</strong>rapy, <strong>the</strong> potential objectives <strong>of</strong>revascularizati<strong>on</strong> are two-fold, to improve survival or survivalfree <strong>of</strong> infarcti<strong>on</strong> or to diminish, or eradicate symptoms.The individual risk <strong>of</strong> <strong>the</strong> patient as well as symptomaticstatus must be a major factor in <strong>the</strong> decisi<strong>on</strong>-makingprocess.Cor<strong>on</strong>ary artery bypass surgeryFavorolo first described <strong>the</strong> use <strong>of</strong> saphenous vein to bypassa diseased cor<strong>on</strong>ary artery in 1969. Since <strong>the</strong>n CABG hasbecome <strong>the</strong> most comm<strong>on</strong> operati<strong>on</strong> for CAD and <strong>on</strong>e <strong>of</strong><strong>the</strong> most comm<strong>on</strong>ly performed surgical operati<strong>on</strong>s worldwide.There are two main indicati<strong>on</strong>s for CABG: prognosticand symptomatic. Prognostic benefit <strong>of</strong> CABG is mainly dueto a reducti<strong>on</strong> in cardiac mortality, as <strong>the</strong>re is less evidencefor reducti<strong>on</strong> in MI. 69,290 Evidence <strong>of</strong> prognostic benefit <strong>of</strong>CABG compared with medical <strong>the</strong>rapy has not been dem<strong>on</strong>stratedin low-risk patients (annual mortality ,1%). 69 In ameta-analysis <strong>of</strong> surgical trials comparing CABG withmedical <strong>the</strong>rapy, CABG was shown to improve prognosis inthose at medium to high risk, but even those in <strong>the</strong>medium risk had a 5-year mortality rate with medical<strong>the</strong>rapy <strong>of</strong> 13.9%, annual mortality 2.8%, which by c<strong>on</strong>temporarystandards appears high. Fur<strong>the</strong>r observati<strong>on</strong>al datafrom <strong>the</strong> Duke registry c<strong>on</strong>firmed that l<strong>on</strong>g-term mortalitybenefit associated with surgery was limited to high-riskgroups. 558 Analyses <strong>of</strong> observati<strong>on</strong>al and randomized c<strong>on</strong>trolledtrial data have revealed that <strong>the</strong> presence <strong>of</strong> specificcor<strong>on</strong>ary artery anatomy is associated with a better prognosiswith surgery than with medical treatment. 69,288 Suchdisease includes <strong>the</strong> following:(1) significant stenosis <strong>of</strong> <strong>the</strong> left main (LM) stem(2) significant proximal stenosis <strong>of</strong> <strong>the</strong> three major cor<strong>on</strong>aryarteries(3) significant stenosis <strong>of</strong> two major cor<strong>on</strong>ary arteries,including high grade stenosis <strong>of</strong> <strong>the</strong> proximal leftanterior descending cor<strong>on</strong>ary arterySignificant stenosis was defined for <strong>the</strong>se studies as 70%<strong>of</strong> major cor<strong>on</strong>ary arteries or 50% <strong>of</strong> <strong>the</strong> LM stem. The presence<strong>of</strong> impaired LV functi<strong>on</strong> increases <strong>the</strong> absolute prognosticadvantage <strong>of</strong> surgery over medical treatment in allcategories. This informati<strong>on</strong> comes from two major randomizedstudies: <strong>the</strong> European Cor<strong>on</strong>ary Artery study and <strong>the</strong>North American CASS study. 287,559Surgery has been c<strong>on</strong>vincingly shown to reduce symptomsand ischaemia and to improve quality <strong>of</strong> life in patients withchr<strong>on</strong>ic angina. These effects are evident in a much widerrange <strong>of</strong> subgroups than in which it has been shown toimprove survival. 290 However, despite improvements overtime, operative morbidity and mortality remain importantc<strong>on</strong>siderati<strong>on</strong>s. Thus individual risks and benefits should bediscussed as thoroughly in low-risk patients, in whomsurgery is undertaken <strong>on</strong> symptomatic grounds al<strong>on</strong>e, as inhigh-risk patients.The overall operative mortality for CABG is between 1 and4% 51,560–563 depending <strong>on</strong> <strong>the</strong> populati<strong>on</strong> studied, and <strong>the</strong>reare well-developed risk stratificati<strong>on</strong> models available for<strong>the</strong> assessment <strong>of</strong> risk in individual patients. 564,565 There is<strong>the</strong> paradox that <strong>the</strong> higher <strong>the</strong> risk <strong>of</strong> operati<strong>on</strong>, <strong>the</strong>greater is <strong>the</strong> benefit <strong>of</strong> surgical over medical treatment.Most patients are angina-free following CABG, but recurrentangina may occur in <strong>the</strong> years after surgery. Although <strong>the</strong>l<strong>on</strong>g-term patency rates for <strong>the</strong> left internal thoracicartery (LITA) graft are extremely good, saphenous veingrafts have a significant rate <strong>of</strong> attriti<strong>on</strong>. Thrombotic occlusi<strong>on</strong>can occur in <strong>the</strong> early post-operative period, 10% by<strong>the</strong> end <strong>of</strong> <strong>the</strong> first year, and after 5 years, <strong>the</strong> vein itselfcan develop a<strong>the</strong>romatous disease. The patency rate <strong>of</strong>vein grafts is 50–60% at 10 years. 566,567Over <strong>the</strong> last 20 years, <strong>the</strong> standard procedure has been tograft <strong>the</strong> LAD with <strong>the</strong> LITA and use saphenous vein for <strong>the</strong>o<strong>the</strong>r bypass grafts. Because at least 70% <strong>of</strong> patients arealive 10 years following surgery, <strong>the</strong> recurrence <strong>of</strong> symptomsfrom vein graft disease remains a clinical problem. Largeobservati<strong>on</strong>al studies have shown that <strong>the</strong> use <strong>of</strong> <strong>the</strong> LITAgraft improves survival and reduces <strong>the</strong> incidence <strong>of</strong> <strong>the</strong>late MI, recurrent angina, and <strong>the</strong> need for fur<strong>the</strong>r cardiacinterventi<strong>on</strong>s. 568 Recent observati<strong>on</strong>al studies havesuggested benefit for bilateral internal thoracic artery(BITA) grafting. 569 There appears to be significant survivalbenefit when using BITA grafts irrespective <strong>of</strong> age, ventricularfuncti<strong>on</strong>, and <strong>the</strong> presence <strong>of</strong> diabetes. Fur<strong>the</strong>rmore,<strong>the</strong> benefit <strong>of</strong> using BITA increased with <strong>the</strong> durati<strong>on</strong> <strong>of</strong>follow-up, particularly in terms <strong>of</strong> <strong>the</strong> need for redosurgery, which at 10 years was 40% for single ITA and 8%for BITA grafting in well-matched patients. Ten years afterCABG 90% <strong>of</strong> ITA grafts c<strong>on</strong>tinue to functi<strong>on</strong> well.With experience, including <strong>the</strong> use <strong>of</strong> skelet<strong>on</strong>ized ITApedicles, <strong>the</strong> risk <strong>of</strong> sternal devascularizati<strong>on</strong> and subsequentdehiscence is much reduced, even in diabetics.O<strong>the</strong>r arterial grafts which have been used include <strong>the</strong>radial artery and <strong>the</strong> right gastroepiploic artery. The greatestexperience has been with <strong>the</strong> radial artery where reportshave indicated patency rates <strong>of</strong> .90% in <strong>the</strong> first 3 years <strong>of</strong>surgery. 570,571The use <strong>of</strong> extra-corporeal circulati<strong>on</strong> (cardiopulm<strong>on</strong>arybypass) to perform cor<strong>on</strong>ary artery surgery remains <strong>the</strong>most comm<strong>on</strong>ly used approach. But <strong>the</strong>re are risks attached,including a whole-body inflammatory resp<strong>on</strong>se and <strong>the</strong> producti<strong>on</strong><strong>of</strong> micro-emboli. The need for aortic cannulati<strong>on</strong>and manipulati<strong>on</strong> <strong>of</strong> <strong>the</strong> ascending aorta may lead torelease <strong>of</strong> emboli, especially in elderly, a<strong>the</strong>romatouspatients. The so-called ‘<strong>of</strong>f-pump’ surgery may lead to areducti<strong>on</strong> in peri-operative mortality and morbidity. Therecent introducti<strong>on</strong> <strong>of</strong> stabilizati<strong>on</strong> devices, which allow isolati<strong>on</strong>and c<strong>on</strong>trol <strong>of</strong> epicardial arteries, facilitates attachment<strong>of</strong> <strong>the</strong> bypass graft without stopping <strong>the</strong> heart andhas enabled surge<strong>on</strong>s to perform surgery without <strong>the</strong> use<strong>of</strong> cardiopulm<strong>on</strong>ary bypass. Randomized trials comparing<strong>of</strong>f-pump with <strong>the</strong> standard procedure are now available.Although <strong>the</strong> use <strong>of</strong> blood products was reduced in <strong>the</strong>
ESC <str<strong>on</strong>g>Guidelines</str<strong>on</strong>g> 39<strong>of</strong>f-pump group (3 vs. 13%) and <strong>the</strong> release <strong>of</strong> CK-MB isoenzynmewas 41% less in <strong>the</strong> <strong>of</strong>f-pump group, <strong>the</strong>re were nodifferences in <strong>the</strong> peri-operative complicati<strong>on</strong> rates. Therewas no difference in outcome in <strong>the</strong> first 1–3 years aftersurgery between <strong>of</strong>f-pump and standard groups. 572,573More recently, Khan et al., 574 in a fur<strong>the</strong>r randomized trialwith angiographic follow-up <strong>of</strong> 3–6 m<strong>on</strong>ths, showed a significantreducti<strong>on</strong> in graft patency (90 vs. 98%) in <strong>the</strong> <strong>of</strong>f-pumpgroup. These studies suggest that <strong>the</strong> use <strong>of</strong> <strong>of</strong>f-pumpsurgery is not a panacea but should be applied cautiouslyand selectively to patients with good target vessels andsignificant co-morbidity.Percutaneous cor<strong>on</strong>ary interventi<strong>on</strong>Although percutaneous transluminal angioplasty was initially<strong>on</strong>ly used for <strong>the</strong> treatment <strong>of</strong> <strong>on</strong>e-vessel disease, advancesin experience, equipment, particularly stents, and adjuvant<strong>the</strong>rapy, have lead to a c<strong>on</strong>siderably expanded role for thismodality <strong>of</strong> treatment in recent years. In patients withstable angina and suitable cor<strong>on</strong>ary anatomy, <strong>the</strong> use <strong>of</strong>stents and adequate adjuvant <strong>the</strong>rapy allows a competentpractiti<strong>on</strong>er to perform ei<strong>the</strong>r <strong>on</strong>e- or multi-vessel PCIwith a high likelihood <strong>of</strong> initial procedural success andacceptable risk. 575 The risk <strong>of</strong> death associated with <strong>the</strong> procedurein routine angioplasty is 0.3–1%, although this canvary quite c<strong>on</strong>siderably. C<strong>on</strong>trary to <strong>the</strong> case <strong>of</strong> bypasssurgery, <strong>on</strong> available evidence, PCI compared with medical<strong>the</strong>rapy does not seem to provide substantial survivalbenefit in stable angina. 576Trial-based evidence indicates, however, that PCI is more<strong>of</strong>ten effective than medical treatment in reducing eventsthat impair quality <strong>of</strong> life (angina pectoris, dyspnoea, and<strong>the</strong> need for re-hospitalisati<strong>on</strong> or limitati<strong>on</strong> <strong>of</strong> exercisecapacity). The ACME investigators 577 dem<strong>on</strong>strated superiorc<strong>on</strong>trol <strong>of</strong> symptoms and better exercise capacity in patientsmanaged with PCI when compared with medical <strong>the</strong>rapy.Death and MI were similar in both groups. However,mid-term results in patients with two-vessel disease didnot dem<strong>on</strong>strate superior c<strong>on</strong>trol <strong>of</strong> symptoms comparedwith medical <strong>the</strong>rapy (similar improvement in exercise durati<strong>on</strong>,freedom from angina, and improvement in quality <strong>of</strong>life at <strong>the</strong> time <strong>of</strong> 6-m<strong>on</strong>th follow-up) as was experienced bypatients with <strong>on</strong>e-vessel disease. 578 This small study(n ¼ 328) suggests that PCI may be less effective in c<strong>on</strong>trollingsymptoms in patients with two-vessel and stable anginawhen compared with <strong>on</strong>e-vessel disease.The RITA-2 trial 579 showed that PCI results in better c<strong>on</strong>trol<strong>of</strong> symptoms <strong>of</strong> ischaemia and improves exercise capacitycompared with medical <strong>the</strong>rapy, but is associated with ahigher combined endpoint <strong>of</strong> death and peri-procedural MI.In this trial, 1018 patients (62% with multi-vessel CAD and34% with significant disease in <strong>the</strong> proximal segment <strong>of</strong> <strong>the</strong>left anterior descending cor<strong>on</strong>ary artery) with stable anginawere randomized to PCI or medical <strong>the</strong>rapy and followedfor a mean <strong>of</strong> 2.7 years. Patients who had inadequatec<strong>on</strong>trol <strong>of</strong> <strong>the</strong>ir symptoms with optimal medical <strong>the</strong>rapywere allowed to cross-over to myocardial revascularizati<strong>on</strong>.Death and definite MI occurred in 6.3% <strong>of</strong> <strong>the</strong> PCI patientsand 3.3% <strong>of</strong> <strong>the</strong> medical patients (P ¼ 0.02). Of <strong>the</strong> 18deaths (11 PCI and seven medical), <strong>on</strong>ly eight were due toheart disease. Twenty-three per cent <strong>of</strong> <strong>the</strong> medical patientsrequired a revascularizati<strong>on</strong> procedure during follow-up.<strong>Angina</strong> improved in both groups, but <strong>the</strong>re was a 16.5%absolute excess <strong>of</strong> worse angina in <strong>the</strong> medical group at 3m<strong>on</strong>ths following randomizati<strong>on</strong> (P , 0.001). Duringfollow-up, 7.9% <strong>of</strong> <strong>the</strong> patients randomized to PCI requiredCABG surgery when compared with 5.8% <strong>of</strong> <strong>the</strong> medicalpatients. AVERT 580 randomly assigned 341 patients withstable CAD, normal LV functi<strong>on</strong>, and Class I and/or II anginato PCI or medical <strong>the</strong>rapy with 80 mg daily atorvastatin. At18 m<strong>on</strong>ths follow-up, 13% <strong>of</strong> <strong>the</strong> medically treated grouphad ischaemic events when compared with 21% <strong>of</strong> <strong>the</strong> PCIgroup (P ¼ 0.048). <strong>Angina</strong> relief was greater in thosetreated with PCI. These data suggest that in low-risk patientswith stable CAD, medical treatment including aggressivelipid-lowering <strong>the</strong>rapy may be as effective as PCI in reducingischaemic events. Greater improvement in anginal symptomsoccurred with PCI.Elective stent inserti<strong>on</strong> and drug-eluting stents (DES). Inameta analysis <strong>of</strong> 29 trials involving 9918 patients, <strong>the</strong>rewas no evidence for a difference between routine cor<strong>on</strong>arystenting and standard ballo<strong>on</strong> angioplasty in terms <strong>of</strong> deathor MI or <strong>the</strong> need for CABG surgery. However, cor<strong>on</strong>ary stentingreduces <strong>the</strong> rate <strong>of</strong> restenosis and <strong>the</strong> need for repeatPCI, 581 findings c<strong>on</strong>firmed in a fur<strong>the</strong>r more recentmeta-analysis. 582 However in-stent restenosis remains alimitati<strong>on</strong> in <strong>the</strong> efficacy <strong>of</strong> PCI for patients with stablecor<strong>on</strong>ary disease, with a need for target lesi<strong>on</strong> revascularizati<strong>on</strong>between 5 and 25%.Drug-eluting stents have been <strong>the</strong> focus <strong>of</strong> attenti<strong>on</strong> <strong>of</strong>interventi<strong>on</strong>al cor<strong>on</strong>ary <strong>the</strong>rapy after <strong>the</strong> RAVEL study. 583The frequently interchangeable use <strong>of</strong> <strong>the</strong> term ‘coatedstent’ and ‘drug-eluting stent’ is misleading becausecoated stent also includes <strong>the</strong> so-called passive coatings,which have failed to prove <strong>the</strong>ir benefit and, in someseries, have even showed harmful effect. Hence, <strong>the</strong> termdrug-eluting stent is recommended instead <strong>of</strong> coatedstent. Presently, three drugs have shown significantly positiveeffects in prospective randomized studies (paclitaxel,sirolimus, and its derivative everolimus). To date, randomizedtrials include <strong>on</strong>ly patients with <strong>on</strong>e-vessel diseaseand with stable or unstable angina. The use <strong>of</strong> drugelutingstents shows a c<strong>on</strong>sistently better treatment effectcompared to bare metal stents, reducing <strong>the</strong> risk <strong>of</strong> restenosisand major adverse cardiac events including target vesselrevascularizati<strong>on</strong>. Reported incidence <strong>of</strong> major adversecardiac events over 9 m<strong>on</strong>ths range between 7.1 and10.3% with drug-eluting stents compared with between13.3 and 18.9. 584–586 More specific guidelines <strong>on</strong> <strong>the</strong> use <strong>of</strong>DES are available in <strong>the</strong> ESC guidelines <strong>on</strong> PCI. 587Revascularizati<strong>on</strong> vs. medical <strong>the</strong>rapyAside from studies dealing exclusively with <strong>the</strong> effects <strong>of</strong>ei<strong>the</strong>r PCI vs. medical <strong>the</strong>rapy or surgery vs. medical<strong>the</strong>rapy, several hybrid studies have investigated <strong>the</strong>effects <strong>of</strong> revascularizati<strong>on</strong>, (ei<strong>the</strong>r PCI or surgery) comparedwith medical <strong>the</strong>rapy. The Asymptomatic CardiacIschaemia Pilot 70 study provides additi<strong>on</strong>al informati<strong>on</strong> comparingmedical <strong>the</strong>rapy with PCI or CABG revascularizati<strong>on</strong>in patients with documented CAD and asymptomatic ischaemiaby both stress testing and ambulatory ECG m<strong>on</strong>itoring.This small study (n ¼ 558) randomized patients withminimal symptoms but evidence <strong>of</strong> ischaemia <strong>on</strong> testing,who were suitable for revascularizati<strong>on</strong> by PCI or CABG to<strong>on</strong>e <strong>of</strong> three treatment strategies: angina-guided drug
40 ESC <str<strong>on</strong>g>Guidelines</str<strong>on</strong>g><strong>the</strong>rapy, angina plus ischaemia-guided drug <strong>the</strong>rapy, andrevascularizati<strong>on</strong> by PCI or CABG surgery. At 2 years <strong>of</strong>follow-up, death or MI had occurred in 4.7% <strong>of</strong> <strong>the</strong> revascularizati<strong>on</strong>patients when compared with 8.8% <strong>of</strong> <strong>the</strong>ischaemia-guided group and 12.1% <strong>of</strong> <strong>the</strong> angina-guidedgroup (P , 0.01 for <strong>the</strong> revascularized group comparedwith ischaemia or angina-guided groups). The results <strong>of</strong><strong>the</strong> ACIP trial indicate that higher-risk patients who areasymptomatic or have minimal symptoms but dem<strong>on</strong>strableischaemia and significant CAD may have a better outcomewith revascularizati<strong>on</strong> with ei<strong>the</strong>r CABG or PCI comparedwith those managed medically.A Swiss study (TIME) 588 in elderly patients (mean age 80years) with severe angina randomized participants toimmediate invasive or c<strong>on</strong>tinued medical <strong>the</strong>rapy. Of thoserandomized to invasive <strong>the</strong>rapy, 52% received PCI and 21%had CABG. Invasive <strong>the</strong>rapy was associated with a statisticallysignificant improvement in symptoms at 6 m<strong>on</strong>ths,but <strong>the</strong> difference was not maintained at 1 year, partlydue to a 48% delayed revascularizati<strong>on</strong> rate in <strong>the</strong> medicallytreated arm. Death and MI were not significantly differentbetween <strong>the</strong> two treatment strategies. Investigators in <strong>the</strong>Medicine, Angioplasty or Surgery Study (MASS) 589 randomizedpatients with stable angina and isolated disease <strong>of</strong><strong>the</strong> left descending cor<strong>on</strong>ary artery to medical treatmentor PCI (including stenting) or CABG using a combined endpoint<strong>of</strong> cardiac death, MI, and refractory angina requiringrepeat revascularizati<strong>on</strong> by surgery. At 3 years <strong>of</strong> follow-up,this combined endpoint occurred in 24% <strong>of</strong> PCI patients, in17% <strong>of</strong> medical patients, and in 3% <strong>of</strong> surgical patients.Importantly, <strong>the</strong>re was no significant difference in overallsurvival in <strong>the</strong> three groups. Death or MI occurred in 1% <strong>of</strong><strong>the</strong> CABG group, 2% <strong>of</strong> <strong>the</strong> PCI group, and 1.4% <strong>of</strong> <strong>the</strong>medically treated group.PCI vs. surgeryA large number <strong>of</strong> clinical trials have compared PCI withsurgery in order to establish <strong>the</strong> choice <strong>of</strong> revascularizati<strong>on</strong>technique, both before and subsequent to <strong>the</strong> introducti<strong>on</strong><strong>of</strong> stenting, 562,597,598 and in multi-vessel as well as <strong>on</strong>evesseldisease. Meta-analysis <strong>of</strong> trials c<strong>on</strong>ducted before1995, 599 when cor<strong>on</strong>ary stenting was rare, revealed no significantdifferences in <strong>the</strong> treatment strategies for ei<strong>the</strong>rdeath and <strong>the</strong> combined endpoint <strong>of</strong> death and MI.Mortality during <strong>the</strong> initial hospitalizati<strong>on</strong> for <strong>the</strong> procedureoccurred in 1.3% <strong>of</strong> <strong>the</strong> CABG group and 1% <strong>of</strong> <strong>the</strong> PCI group.The need for subsequent revascularizati<strong>on</strong> was significantlyhigher in <strong>the</strong> PCI group, and although patients weresignificantly less likely to have angina 1 year after bypasssurgery than after PCI, by 3 years this difference was nol<strong>on</strong>ger statistically significant. Results from <strong>the</strong> BARI study,<strong>the</strong> largest single randomized trial <strong>of</strong> PCI vs. surgery,not included in this meta-analysis, were n<strong>on</strong>e<strong>the</strong>lessc<strong>on</strong>sistent with <strong>the</strong>se findings, although a survival advantagewith bypass surgery was observed in <strong>the</strong> diabeticsubgroup. 590More recent trials, such as <strong>the</strong> ARTS 600 and SOS trials, 597have incorporated <strong>the</strong> use <strong>of</strong> stents as part <strong>of</strong> PCI. TheARTS 1 trial 600 compared <strong>the</strong> strategy <strong>of</strong> multiple-stentimplantati<strong>on</strong> with <strong>the</strong> aim <strong>of</strong> complete revascularizati<strong>on</strong>vs. bypass surgery in patients with multi-vessel disease.However, this trial was not exclusively am<strong>on</strong>g patientswith stable angina; 37 and 35%, respectively, in both armshad unstable angina, 57 and 60%, respectively, had stableangina, and 6 and 5%, respectively, had silent ischaemia.As in previous analyses <strong>of</strong> ballo<strong>on</strong> angioplasty, at 1 year,<strong>the</strong>re was no difference between <strong>the</strong> two groups in terms<strong>of</strong> rate <strong>of</strong> death, stroke, or MI. Am<strong>on</strong>g patients who survivedwithout stroke or MI, 16.8% <strong>of</strong> those in <strong>the</strong> stenting groupunderwent a sec<strong>on</strong>d revascularizati<strong>on</strong>, when comparedwith 3.5% <strong>of</strong> those in <strong>the</strong> surgery group. The rate <strong>of</strong> eventfreesurvival at 1 year was 73.8 percent am<strong>on</strong>g <strong>the</strong> patientswho received stents and 87.8 percent am<strong>on</strong>g those whounderwent bypass surgery. As measured 1 year after <strong>the</strong>procedure, cor<strong>on</strong>ary stenting for multi-vessel disease inselected patients <strong>of</strong>fered a similar outcome in terms <strong>of</strong>death, stroke, and MI as bypass surgery. However, stentingwas associated with a greater need for repeatedrevascularizati<strong>on</strong>.A meta-analysis including trials <strong>of</strong> stents 560 suggests a mortalitybenefit with CABG compared with PCI at 5 years whichc<strong>on</strong>tinued to 8 years in patients with multi-vessel disease, aswell as significantly less angina and less need for repeatrevascularizati<strong>on</strong>. Subgroup analysis <strong>of</strong> trials with andwithout stents indicated significant heterogeneity between<strong>the</strong> two groups, with trials performed pre-stents showing atrend towards reduced mortality favouring CABG which wasnot evident in <strong>the</strong> trials with stents. A more recentmeta-analysis <strong>of</strong> four randomized c<strong>on</strong>trolled trials <strong>of</strong> percutaneousinterventi<strong>on</strong> with stents compared with bypasssurgery (n ¼ 3051) showed no significant differencebetween <strong>the</strong> treatment strategies in <strong>the</strong> primary endpoint<strong>of</strong> death, MI, or stroke at 1 year. 601 However, observati<strong>on</strong>aldata with 3-year follow-up <strong>on</strong> .60 000 patients from <strong>the</strong>New York cardiac registry indicated that for patients withtwo or more diseased cor<strong>on</strong>ary arteries, CABG was associatedwith higher adjusted rates <strong>of</strong> l<strong>on</strong>g-term survival thanstenting. 602To summarize, <strong>the</strong> trial evidence suggests that, outside <strong>of</strong><strong>the</strong> populati<strong>on</strong> with high-risk indicators which have beenproven to benefit prognostically from surgery, ei<strong>the</strong>r PCI orsurgery may be c<strong>on</strong>sidered as an effective opti<strong>on</strong> for <strong>the</strong>treatment <strong>of</strong> symptoms. After an initial pharmacologicalapproach, revascularizati<strong>on</strong> may be recommended forpatients with suitable anatomy who do not resp<strong>on</strong>d adequatelyto medical <strong>the</strong>rapy or for <strong>the</strong> individual patientwho, regardless <strong>of</strong> age, wishes to remain physically active(performing regular physical exercise).In n<strong>on</strong>-diabetic patients with 1–2-vessel disease withouthigh grade stenosis <strong>of</strong> <strong>the</strong> proximal LAD in whom angioplasty<strong>of</strong> <strong>on</strong>e or more lesi<strong>on</strong>s has a high likelihood <strong>of</strong> initial success,PCI is generally <strong>the</strong> preferred initial approach, influenced byfactors such as <strong>the</strong> less invasive nature and lower initial risk<strong>of</strong> <strong>the</strong> initial procedure and <strong>the</strong> absence <strong>of</strong> survivaladvantage <strong>of</strong> CABG in lower risk subgroups. The individualcircumstances and preferences <strong>of</strong> each patient mustbe c<strong>on</strong>sidered carefully when planning <strong>the</strong> treatmentstrategy.In asymptomatic patients, revascularizati<strong>on</strong> cannotimprove symptoms and <strong>the</strong> <strong>on</strong>ly appropriate indicati<strong>on</strong> forrevascularizati<strong>on</strong> with PCI would be to reduce <strong>the</strong> likelihood<strong>of</strong> ischaemic complicati<strong>on</strong>s in <strong>the</strong> future. Evidence tosupport this strategy is limited <strong>on</strong>ly to those patients withobjective evidence <strong>of</strong> extensive ischaemia, in whom revascularizati<strong>on</strong>(ei<strong>the</strong>r PCI or CABG) may reduce <strong>the</strong> likelihood<strong>of</strong> mortality relative to an angina-guided strategy (ACIP). 70
ESC <str<strong>on</strong>g>Guidelines</str<strong>on</strong>g> 41PCI may be c<strong>on</strong>sidered for mildly symptomatic patients in<strong>the</strong> category <strong>of</strong> higher-risk ischaemia and severe anatomicCAD <strong>on</strong>ly if <strong>the</strong>re is a high likelihood <strong>of</strong> success and a lowrisk <strong>of</strong> morbidity or mortality.Specific patient and lesi<strong>on</strong> subsetsPatients with severely depressed LV functi<strong>on</strong> and/or highsurgical risk. Patients in whom surgical risk is prohibitivelyhigh may benefit from revascularizati<strong>on</strong> by PCI, particularlywhen residual viability can be dem<strong>on</strong>strated in <strong>the</strong> dysfuncti<strong>on</strong>ingmyocardium perfused by <strong>the</strong> target vessel(s). Thisissue is currently addressed in two large randomizedstudies, <strong>the</strong> STICH 603 and <strong>the</strong> HEART UK 604 trials.Unprotected LM disease. The LM stem is referred to asunprotected when <strong>the</strong> distal cor<strong>on</strong>ary arteries do notreceive circulati<strong>on</strong> from a bypass graft. Several observati<strong>on</strong>alreports 605,606 indicate <strong>the</strong> feasibility <strong>of</strong> PCI in LMstem disease. More recently, an observati<strong>on</strong>al registry hasshown improved results with drug eluting compared withbare metal stents 607 holding promise for <strong>the</strong> use <strong>of</strong> PCI inLM stem disease in <strong>the</strong> future. However, surgery shouldremain <strong>the</strong> preferred approach until <strong>the</strong> outcome <strong>of</strong>fur<strong>the</strong>r trials are known.Multi-vessel disease in patients with diabetes. Aformaltrialcomparing <strong>the</strong> effect <strong>of</strong> PCI vs. CABG in diabetics is not yetavailable; however, post hoc subgroup analyses <strong>of</strong> randomizedtrials comparing <strong>the</strong>se treatment strategies have shownreduced mortality with bypass surgery compared withPCI. 608,609 The BARI trial was <strong>the</strong> largest <strong>of</strong> <strong>the</strong>se trials and<strong>the</strong> <strong>on</strong>ly in which a statistical difference in mortality wasdetected between <strong>the</strong> treatment groups in <strong>the</strong> diabetics. 590,610Am<strong>on</strong>g treated diabetics (n ¼ 353), <strong>the</strong>re was an absolutesurvival advantage <strong>of</strong> 15% for CABG at 5 years (P ¼ 0.003).The rate <strong>of</strong> repeat revascularizati<strong>on</strong> was also higher with PCIin diabetics in BARI and was evident too even withstent-assisted PCI (41 vs. 8.4%) in <strong>the</strong> ARTS study.A limitati<strong>on</strong> <strong>of</strong> <strong>the</strong>se trials is that <strong>the</strong>y were c<strong>on</strong>ductedbefore <strong>the</strong> widespread use <strong>of</strong> drug-eluting stents or adjuvantperi-procedural antiplatelet <strong>the</strong>rapy. Drug-eluting stentshave reduced <strong>the</strong> rate <strong>of</strong> restenosis in diabetic as in n<strong>on</strong>diabeticpatients 585,586,611 but <strong>the</strong> impact <strong>of</strong> this reducti<strong>on</strong><strong>on</strong> mortality in diabetic patients, particularly in multi-vesselPCI, is unknown. Two major trials are underway to addressthis important issue, BARI 2 Diabetes (BARI 2D) andFREEDOM (Future Revascularisati<strong>on</strong> Evaluati<strong>on</strong> in Patientswith Diabetes Mellitus). However, for <strong>the</strong> present, due c<strong>on</strong>siderati<strong>on</strong>should be given to <strong>the</strong> evidence available and PCIshould be used with reservati<strong>on</strong> in diabetics with multivesseldisease until <strong>the</strong> results <strong>of</strong> fur<strong>the</strong>r trials are known.Patients with previous bypass graft surgery. There are norandomized c<strong>on</strong>trolled trials comparing treatment opti<strong>on</strong>sin patients with previous bypass surgery. Observati<strong>on</strong>aldata suggest that patients with late stenoses <strong>of</strong> vein graftshave a high mortality rate, 612 and re-operati<strong>on</strong> improved<strong>the</strong> outcome <strong>of</strong> <strong>the</strong>se patients in <strong>on</strong>e observati<strong>on</strong>al comparis<strong>on</strong>.613 Redo surgery may be undertaken <strong>on</strong> symptomaticgrounds where <strong>the</strong> anatomy is suitable. However, <strong>the</strong> operativerisk <strong>of</strong> redo bypass surgery is as high as three-foldgreater than initial surgery, 614 and for those with a patentITA graft, <strong>the</strong>re is <strong>the</strong> additi<strong>on</strong>al risk <strong>of</strong> damage to thisgraft during surgery.In c<strong>on</strong>trast, PCI can be performed following previous surgicalrevascularizati<strong>on</strong>, ei<strong>the</strong>r in <strong>the</strong> vein graft or arterialgraft, or <strong>the</strong> native cor<strong>on</strong>ary tree bey<strong>on</strong>d <strong>the</strong> graft whichis not revascularized, and may provide a useful alternativeto redo surgery for symptomatic relief. Protective filterdevices may be employed to reduce particulate debrisfrom embolizing downstream and causing peri-proceduralmyocardial damage (SAFER) 615 when dilating old saphenousvein grafts.Chr<strong>on</strong>ic total occlusi<strong>on</strong>s. Chr<strong>on</strong>ic total occlusi<strong>on</strong>s still represent<strong>the</strong> most frequent mode <strong>of</strong> failure <strong>of</strong> PCI. When <strong>the</strong>occlusi<strong>on</strong> can be crossed with a guide-wire and <strong>the</strong> distallumen has been reached, satisfactory results are obtainablewith stent implantati<strong>on</strong>, as shown by several trials, 616–618albeit at <strong>the</strong> expense <strong>of</strong> high restenosis rate ranging from32 to 55%. The value <strong>of</strong> drug-eluting stents in this respectis currently under evaluati<strong>on</strong>. In patients with multi-vesseldisease, failure to treat chr<strong>on</strong>ic total occlusi<strong>on</strong>s will resultin incomplete revascularizati<strong>on</strong>, which could be avoidedwhen <strong>the</strong> patient is referred for bypass surgery.Indicati<strong>on</strong>s for revascularizati<strong>on</strong>In general, patients who have indicati<strong>on</strong>s for cor<strong>on</strong>ary arteriographyand in whom ca<strong>the</strong>terizati<strong>on</strong> reveals severe cor<strong>on</strong>aryartery stenosis are also potential candidates formyocardial revascularizati<strong>on</strong>. In additi<strong>on</strong>, a patient is potentiallyeligible for revascularizati<strong>on</strong> if:(1) medical <strong>the</strong>rapy is unsuccessful in c<strong>on</strong>trolling symptomsto <strong>the</strong> patient’s satisfacti<strong>on</strong>(2) n<strong>on</strong>-invasive tests reveal a substantial area <strong>of</strong> myocardiumat risk(3) <strong>the</strong>re is a high likelihood <strong>of</strong> success and acceptable risk<strong>of</strong> morbidity and mortality(4) <strong>the</strong> patient prefers an interventi<strong>on</strong>al ra<strong>the</strong>r than amedical approach and is fully informed <strong>of</strong> <strong>the</strong> risks <strong>of</strong>this route <strong>of</strong> <strong>the</strong>rapy in <strong>the</strong>ir individual caseAn adequate resp<strong>on</strong>se to <strong>the</strong>rapy must be judged in c<strong>on</strong>sultati<strong>on</strong>with <strong>the</strong> patient. For some, Class I symptoms(angina <strong>on</strong>ly <strong>on</strong> strenuous exerti<strong>on</strong> but not during ordinaryactivity) are acceptable, but o<strong>the</strong>rs may wish for completeaboliti<strong>on</strong> <strong>of</strong> <strong>the</strong>ir symptoms. Recommendati<strong>on</strong>s for revascularizati<strong>on</strong><strong>on</strong> symptomatic grounds, as summarized in Table 8or below, have taken into account <strong>the</strong> range <strong>of</strong> symptomaticgrades for which evidence is available and should be c<strong>on</strong>struedin this fashi<strong>on</strong> ra<strong>the</strong>r than as a directive to performrevascularizati<strong>on</strong> across <strong>the</strong> entire range <strong>of</strong> symtomatology.What is an acceptable risk <strong>of</strong> morbidity and mortality shouldalso be c<strong>on</strong>sidered <strong>on</strong> an individual basis for each patient.Ideally, patients should not be advised to have a procedurefor which <strong>the</strong> procedural mortality exceeds <strong>the</strong>ir estimatedannual mortality unless <strong>the</strong>re is evidence <strong>of</strong> substantialprognostic benefit in <strong>the</strong> l<strong>on</strong>ger term or symptoms arehaving a serious impact <strong>on</strong> <strong>the</strong>ir quality <strong>of</strong> life, despiteappropriate medical <strong>the</strong>rapy.Selecti<strong>on</strong> <strong>of</strong> <strong>the</strong> method <strong>of</strong> revascularizati<strong>on</strong> should bebased <strong>on</strong>:(1) risk <strong>of</strong> peri-procedural morbidity and morbidity(2) likelihood <strong>of</strong> success, including factors such as technicalsuitability <strong>of</strong> lesi<strong>on</strong>s for angioplasty or surgicalbypass(3) risk <strong>of</strong> restenosis or graft occlusi<strong>on</strong>
42 ESC <str<strong>on</strong>g>Guidelines</str<strong>on</strong>g>Table 8Summary <strong>of</strong> recommendati<strong>on</strong>s for revascularizati<strong>on</strong> in stable anginaIndicati<strong>on</strong> For prognosis a For symptoms b StudiesClass <strong>of</strong>recommendati<strong>on</strong>Level <strong>of</strong>evidenceClass <strong>of</strong>recommendati<strong>on</strong>Level <strong>of</strong>evidencePCI (assuming suitable anatomy for PCI, appropriate risk stratificati<strong>on</strong>, and discussi<strong>on</strong> with <strong>the</strong> patient)<strong>Angina</strong> CCS classes I–IV despite medical <strong>the</strong>rapyI A ACME and MASSwith <strong>on</strong>e-vessel disease<strong>Angina</strong> CCS classes I–IV despite medical <strong>the</strong>rapyI A RITA 2 and VA-ACMEwith multi-vessel disease (n<strong>on</strong>-diabetic)<strong>Stable</strong> angina with minimal (CCS class I) symptoms IIb C ACIP<strong>on</strong> medicati<strong>on</strong> and <strong>on</strong>e-, two-, or three-vesseldisease but objective evidence <strong>of</strong> large ischaemiaCABG (assuming suitable anatomy for surgery, appropriate risk stratificati<strong>on</strong>, and discussi<strong>on</strong> with <strong>the</strong> patient)<strong>Angina</strong> and LM stem disease I A I A CASS, EuropeanCor<strong>on</strong>ary Surgerystudy, VA Study,and Yusefmeta-analysis<strong>Angina</strong> and three-vessel disease with objective I A I Alarge ischaemia<strong>Angina</strong> and three-vessel disease with poorI A I Aventricular functi<strong>on</strong><strong>Angina</strong> with two- or three-vessel disease including I A I Asevere disease <strong>of</strong> <strong>the</strong> proximal LAD<strong>Angina</strong> CCS classes I–IV with multi-vesseldisease (diabetic)IIa B I B BARI, GABI, ERACI-I,SoS, ARTs,Yusef et al.,H<strong>of</strong>fman et al.<strong>Angina</strong> CCS classes I–IV with multi-vesselIAdisease (n<strong>on</strong>-diabetic)<strong>Angina</strong> CCS classes I–IV despite medical <strong>the</strong>rapyI B MASSand <strong>on</strong>e-vessel disease including severedisease <strong>of</strong> <strong>the</strong> proximal LAD<strong>Angina</strong> CCS classes I–IV despite medical <strong>the</strong>rapyIIbBand <strong>on</strong>e-vessel disease not including severedisease <strong>of</strong> <strong>the</strong> proximal LAD<strong>Angina</strong> with minimal (CCS class I) symptoms <strong>on</strong>medicati<strong>on</strong> and <strong>on</strong>e-, two-, or three-vesseldisease but objective evidence <strong>of</strong> large ischaemiaIIb C ACIPRecommendati<strong>on</strong>s for revascularizati<strong>on</strong> <strong>on</strong> symptomatic grounds take into account <strong>the</strong> range <strong>of</strong> symptomatic grades for which evidence is available andshould be c<strong>on</strong>strued in this fashi<strong>on</strong> ra<strong>the</strong>r than as a directive to perform revascularizati<strong>on</strong> across <strong>the</strong> entire range <strong>of</strong> symtomatology.CCS, Canadian <strong>Cardio</strong>vascular Society.a Relates to effects <strong>on</strong> mortality, cardiac or cardiovascular mortality, or mortality combined with MI.b Relates to changes in angina class, exercise durati<strong>on</strong>, time to angina <strong>on</strong> treadmill testing, repeat hospitalizati<strong>on</strong> for angina, or o<strong>the</strong>r parameters <strong>of</strong>functi<strong>on</strong>al capacity or quality <strong>of</strong> life.(4) completeness <strong>of</strong> revascularizati<strong>on</strong>. If c<strong>on</strong>sidering PCIfor multi-vessel disease, is <strong>the</strong>re a high probabilitythat PCI will provide complete revascularizati<strong>on</strong> or atleast in <strong>the</strong> same range as CABG?(5) diabetic status(6) local hospital experience in cardiac surgery and interventi<strong>on</strong>alcardiology(7) patient’s preferenceC<strong>on</strong>traindicati<strong>on</strong>s to myocardial revascularizati<strong>on</strong> comprise<strong>the</strong> following.(1) Patients with <strong>on</strong>e- or two-vessel CAD without significantproximal LAD stenosis who have mild or no symptomsand have not received an adequate trial <strong>of</strong> medical<strong>the</strong>rapy or have no dem<strong>on</strong>strable ischaemia or <strong>on</strong>ly alimited area <strong>of</strong> ischaemia/viability <strong>on</strong> n<strong>on</strong>-invasivetesting(2) Borderline (50–70%) cor<strong>on</strong>ary stenosis in locati<strong>on</strong> o<strong>the</strong>rthan LM and no dem<strong>on</strong>strable ischaemia <strong>on</strong> n<strong>on</strong>invasivetesting(3) N<strong>on</strong>-significant (,50%) cor<strong>on</strong>ary stenosis(4) High risk <strong>of</strong> procedure-related morbidity or mortality(.10–15% mortality risk) unless <strong>the</strong> risk <strong>of</strong> <strong>the</strong> procedureis balanced by an expected significant improvementin survival or <strong>the</strong> patient’s quality <strong>of</strong> life without<strong>the</strong> procedure is extremely poorC<strong>on</strong>stant rapid developments in PCI and CABG, as well assignificant progress in medical treatment and sec<strong>on</strong>dary preventi<strong>on</strong><strong>of</strong> stable angina, have generated <strong>the</strong> need for largerandomizd trials comparing different treatment strategies in
ESC <str<strong>on</strong>g>Guidelines</str<strong>on</strong>g> 43selected groups <strong>of</strong> patients. Many questi<strong>on</strong>s in <strong>the</strong> management<strong>of</strong> stable angina remain incompletely answered, andfur<strong>the</strong>r questi<strong>on</strong>s are generated by <strong>the</strong> development <strong>of</strong>new treatment modalities, necessitating <strong>the</strong> c<strong>on</strong>stant revisi<strong>on</strong>and updating <strong>of</strong> <strong>the</strong>se guidelines and a need for practisingclinicians to remain abreast <strong>of</strong> current literature in <strong>the</strong>area in <strong>the</strong> interim.Recommendati<strong>on</strong>s for revascularizati<strong>on</strong> to improveprognosis in patients with stable anginaClass I(1) CABG for significant LM CAD or its equivalent (i.e.severe stenosis <strong>of</strong> ostial/proximal segment <strong>of</strong> left descendingand circumflex cor<strong>on</strong>ary arteries) (level <strong>of</strong> evidenceA)(2) CABG for significant proximal stenosis <strong>of</strong> three majorvessels, particularly in those patients with abnormalLV functi<strong>on</strong> or with early or extensive reversible ischaemia<strong>on</strong> functi<strong>on</strong>al testing (level <strong>of</strong> evidence A)(3) CABG for <strong>on</strong>e- or two-vessel disease with high-gradestenosis <strong>of</strong> proximal LAD with reversible ischaemia <strong>on</strong>n<strong>on</strong>-invasive testing (level <strong>of</strong> evidence A)(4) CABG for significant disease with impaired LV functi<strong>on</strong>and viability dem<strong>on</strong>strated by n<strong>on</strong>-invasive testing(level <strong>of</strong> evidence B)Class IIa(1) CABG for <strong>on</strong>e- or two-vessel CAD without significantproximal LAD stenosis in patients who have survivedsudden cardiac death or sustained ventricular tachycardia(level <strong>of</strong> evidence B)(2) CABG for significant three-vessel disease in diabeticswith reversible ischaemia <strong>on</strong> functi<strong>on</strong>al testing (level<strong>of</strong> evidence C)(3) PCI or CABG for patients with reversible ischaemia <strong>on</strong>functi<strong>on</strong>al testing and evidence <strong>of</strong> frequent episodes<strong>of</strong> ischaemia during daily activities (level <strong>of</strong> evidence C)Recommendati<strong>on</strong>s for revascularizati<strong>on</strong> to improvesymptoms in patients with stable anginaClass I(1) CABG for multi-vessel disease technically suitable forsurgical revascularizati<strong>on</strong> in patients with moderateto-severesymptoms not c<strong>on</strong>trolled by medical<strong>the</strong>rapy, in whom risks <strong>of</strong> surgery do not outweighpotential benefits (level <strong>of</strong> evidence A)(2) PCI for <strong>on</strong>e-vessel disease technically suitable forpercutaneous revascularizati<strong>on</strong> in patients withmoderate-to-severe symptoms not c<strong>on</strong>trolled bymedical <strong>the</strong>rapy, in whom procedural risks do not outweighpotential benefits (level <strong>of</strong> evidence A)(3) PCI for multi-vessel disease without high-risk cor<strong>on</strong>aryanatomy, technically suitable for percutaneous revascularizati<strong>on</strong>in patients with moderate-to-severe symptomsnot c<strong>on</strong>trolled by medical <strong>the</strong>rapy, in whomprocedural risks do not outweigh potential benefits(level <strong>of</strong> evidence A)Class IIa(1) PCI for <strong>on</strong>e-vessel disease technically suitable forpercutaneous revascularizati<strong>on</strong> in patients with mildto-moderatesymptoms which are n<strong>on</strong>e<strong>the</strong>lessunacceptable to <strong>the</strong> patient, in whom proceduralrisks do not outweigh potential benefits (level <strong>of</strong> evidenceA)(2) CABG for <strong>on</strong>e-vessel disease technically suitable forsurgical revascularizati<strong>on</strong> in patients with moderateto-severesymptoms not c<strong>on</strong>trolled by medical<strong>the</strong>rapy, in whom operative risk does not outweighpotential benefit (level <strong>of</strong> evidence A)(3) CABG for multi-vessel disease technically suitable forsurgical revascularizati<strong>on</strong> in patients with mildto-moderatesymptoms which are n<strong>on</strong>e<strong>the</strong>less unacceptableto <strong>the</strong> patient, in whom operative risk does notoutweigh potential benefit (level <strong>of</strong> evidence A)(4) PCI for multi-vessel disease technically suitable forpercutaneous revascularizati<strong>on</strong> in patients withmild-to-moderate symptoms which are n<strong>on</strong>e<strong>the</strong>lessunacceptable to <strong>the</strong> patient, in whom procedural risksdo not outweigh potential benefits (level <strong>of</strong> evidence A)Class IIb(1) CABG for <strong>on</strong>e-vessel disease technically suitable forsurgical revascularizati<strong>on</strong> in patients with mild-tomoderatesymptoms which are n<strong>on</strong>e<strong>the</strong>less unacceptableto <strong>the</strong> patient, in whom operative risk is notgreater than <strong>the</strong> estimated annual mortality (level <strong>of</strong>evidence B)Treatment <strong>of</strong> stable angina: multi-targeted treatment <strong>of</strong> amulti-faceted diseaseIn his/her lifetime, <strong>the</strong> patient with stable angina may meetepisodes <strong>of</strong> exercise/stress-induced symptomatic myocardialischaemia (angina pectoris), silent ischaemia, progressiveangina, acute cor<strong>on</strong>ary syndromes (unstable angina and MI),acute and chr<strong>on</strong>ic heart failure, and life-threatening arrhythmias.Prol<strong>on</strong>ged periods <strong>of</strong> stability may alternate withperiods <strong>of</strong> instability (sudden progressi<strong>on</strong> and acute cor<strong>on</strong>arysyndromes). According to <strong>the</strong> state <strong>of</strong> <strong>the</strong> disease, a patientwill require treatment aimed at retardati<strong>on</strong> <strong>of</strong> <strong>the</strong> progressi<strong>on</strong><strong>of</strong> disease (preventi<strong>on</strong>), management <strong>of</strong> symptomatic disease(angina pectoris), management <strong>of</strong> acute cor<strong>on</strong>ary syndromes,and management <strong>of</strong> heart failure or life-threatening arrhythmias.The physician should be prepared to <strong>of</strong>fer <strong>the</strong> appropriate<strong>the</strong>rapy at <strong>the</strong> appropriate time. The different modes <strong>of</strong>preventive <strong>the</strong>rapy, symptomatic medical <strong>the</strong>rapy, such aspercutaneous and surgical cor<strong>on</strong>ary revascularizati<strong>on</strong> andmanagement <strong>of</strong> arrhythmias, are all rapidly evolving and soit is recommended that an individual physician operateswithin a team which can <strong>of</strong>fer <strong>the</strong> appropriate <strong>the</strong>rapy at<strong>the</strong> appropriate time with <strong>the</strong> appropriate skills.Special subgroupsWomenThe evaluati<strong>on</strong> <strong>of</strong> chest pain in women is less straightforwardthan in men at multiple levels, because <strong>of</strong> genderdifferences in presentati<strong>on</strong> and disease manifestati<strong>on</strong> 619and also <strong>the</strong> prep<strong>on</strong>derance <strong>of</strong> male-specific data in <strong>the</strong>published literature.There are numerous differences in <strong>the</strong> epidemiology andprimary manifestati<strong>on</strong> <strong>of</strong> CHD in women and men. <strong>Stable</strong>angina is <strong>the</strong> most frequent initial manifestati<strong>on</strong> <strong>of</strong> CHD inwomen, but MI or sudden death <strong>the</strong> most frequent initialmanifestati<strong>on</strong> in men. 40,41,620 Although <strong>the</strong> incidence <strong>of</strong>
44 ESC <str<strong>on</strong>g>Guidelines</str<strong>on</strong>g>CHD death and MI is greater in men than in women at allages, <strong>the</strong> incidence <strong>of</strong> angina in women exceeds that <strong>of</strong>men in post-menopausal age groups. Therefore, it is not surprisingthat at populati<strong>on</strong> level, some studies report an evenhigher prevalence <strong>of</strong> Rose angina questi<strong>on</strong>naire in middleaged and elderly women than in men <strong>of</strong> comparableage. 31–33,621,622 However, in populati<strong>on</strong>-based studies, <strong>the</strong>incidence <strong>of</strong> fatal CHD is higher in men with angina thanwomen with angina, 620 possibly partly due to misclassificati<strong>on</strong><strong>of</strong> angina as CHD in a proporti<strong>on</strong> <strong>of</strong> women.The diagnosis <strong>of</strong> angina in women is more difficult than inmen for several reas<strong>on</strong>s. Atypical symptoms are morecomm<strong>on</strong> in women, but this is ‘atypical ’ compared with<strong>the</strong> typical symptoms described by men. Patient percepti<strong>on</strong><strong>of</strong> pain and <strong>the</strong> language used to report symptoms aredifferent between men and women. 623To compound <strong>the</strong> problem, <strong>the</strong> correlati<strong>on</strong> betweensymptoms and ‘significant’ luminal obstructi<strong>on</strong> at cor<strong>on</strong>aryangiography is weaker in women than in men. In <strong>the</strong>Cor<strong>on</strong>ary Artery Surgery Study, 624 62% <strong>of</strong> women withtypical angina had significant cor<strong>on</strong>ary stenoses, when comparedwith 40% <strong>of</strong> women with atypical angina and 4% <strong>of</strong>women with n<strong>on</strong>-ischaemic pain, illustrating <strong>the</strong> lowerprevalence <strong>of</strong> angiographically verified CHD in women thanin men for all forms <strong>of</strong> chest pain, including typical andatypical angina and n<strong>on</strong>-cardiac chest pain.<strong>Angina</strong>, <strong>the</strong> symptom complex, may still be associatedwith ischaemia even in <strong>the</strong> absence <strong>of</strong> obstructive cor<strong>on</strong>arylesi<strong>on</strong>s, as in Syndrome X, a phenomen<strong>on</strong> which is morecomm<strong>on</strong> in women. Microvascular disease and cor<strong>on</strong>aryvasospasm are also more comm<strong>on</strong> in women. Ischaemia, inthis c<strong>on</strong>text, may be dem<strong>on</strong>strated electrocardiographically,by perfusi<strong>on</strong> scintigraphy, or o<strong>the</strong>r methods and mayresp<strong>on</strong>d appropriately to anti-ischaemic <strong>the</strong>rapy withoutangiographic evidence <strong>of</strong> epicardial stenosis. Although <strong>the</strong>absence <strong>of</strong> obstructive cor<strong>on</strong>ary lesi<strong>on</strong>s remains an indicator<strong>of</strong> better infarct-free survival than <strong>the</strong> presence <strong>of</strong> obstructivedisease, <strong>the</strong>re are some emerging data suggesting that<strong>the</strong> prognosis associated with ‘normal’ cor<strong>on</strong>ary arteries isnot as benign as <strong>on</strong>ce thought. 305When used for <strong>the</strong> detecti<strong>on</strong> <strong>of</strong> significant cor<strong>on</strong>arydisease, exercise ECG testing has a higher false-positiverate in women (38–67%) than in men (7–44%), 140 largelybecause <strong>of</strong> <strong>the</strong> lower pretest likelihood <strong>of</strong> disease, 142 but alower false-negative rate in women. 625 This results in a highnegative predictive value, signifying that a negative result<strong>of</strong> n<strong>on</strong>-invasive testing reliably excludes <strong>the</strong> presence <strong>of</strong>CAD. The difficulties <strong>of</strong> using exercise testing for diagnosingobstructive CAD in women have led to speculati<strong>on</strong> thatstress imaging may be preferred over standard stresstesting. Myocardial perfusi<strong>on</strong> scintigraphy or echocardiographycould be a logical additi<strong>on</strong> to treadmill testing inthis circumstance. However, <strong>the</strong> sensitivity <strong>of</strong> radi<strong>on</strong>uclideperfusi<strong>on</strong> scans may be lower in women than men. 626Artefacts due to breast attenuati<strong>on</strong>, usually manifest in <strong>the</strong>anterior wall, can be an important caveat in <strong>the</strong> interpretati<strong>on</strong><strong>of</strong> women’s perfusi<strong>on</strong> scans, especially when 201 Tl isused as a tracer. More recently, <strong>the</strong> use <strong>of</strong> gated 99 mTc sestamibiSPECT imaging has been associated with an apparentreducti<strong>on</strong> in breast artefacts. 627 Similarly, exercise orpharmacological stress echocardiography may help avoidartefacts specifically due to breast attenuati<strong>on</strong>. Indeed,numerous studies have indicated <strong>the</strong> value <strong>of</strong> stressechocardiography as an independent predictor <strong>of</strong> cardiacevents in women with known or suspected CAD. 171,628,629Despite its limitati<strong>on</strong>s in women, routine exercise ECGtesting has been shown to reduce procedures without loss <strong>of</strong>diagnostic accuracy. Indeed, <strong>on</strong>ly 30% <strong>of</strong> women (in whom areas<strong>on</strong>ably certain diagnosis <strong>of</strong> CAD could not be reached orexcluded) need to be referred for fur<strong>the</strong>r testing. 630Although <strong>the</strong> optimal strategy for diagnosing obstructive CADin women remains to be defined, <strong>the</strong> Task Force believesthat <strong>the</strong>re are currently insufficient data to justify replacingstandard exercise testing with stress imaging in all womenbeing evaluated for CAD. In many women with a low pretestlikelihood <strong>of</strong> disease, a negative exercise test result will be sufficientand imaging procedures will not be required. 630It is important to emphasize that women with objectiveevidence <strong>of</strong> moderate-to-severe ischaemia at n<strong>on</strong>-invasivetesting should have equal access to cor<strong>on</strong>ary arteriographyas men. Fur<strong>the</strong>rmore, limited female representati<strong>on</strong> in clinicaltrials <strong>of</strong> sec<strong>on</strong>dary preventi<strong>on</strong> to date is not a justificati<strong>on</strong>to apply guidelines differently to men and womenafter CAD is diagnosed.It is known that women have a higher morbidity and mortalityafter suffering MI than men, and it has been suggestedby some that less vigorous treatment in women may impact<strong>on</strong> reduced survival in women after MI. 631 A review <strong>of</strong> 27studies c<strong>on</strong>cluded that <strong>the</strong> reas<strong>on</strong>s for increased early mortalityam<strong>on</strong>g women were older age and <strong>the</strong> presence <strong>of</strong>o<strong>the</strong>r unfavourable baseline clinical characteristics. 632Subsequent investigati<strong>on</strong> found an interacti<strong>on</strong> betweengender and age, with a female excess <strong>of</strong> mortality inyounger patients (,50 years <strong>of</strong> age) that diminishes withage. 633Reports <strong>of</strong> <strong>the</strong> impact <strong>of</strong> gender <strong>on</strong> utilizati<strong>on</strong> <strong>of</strong> investigati<strong>on</strong>sand <strong>the</strong>rapies and <strong>on</strong> subsequent clinical outcomein stable settings are similarly divergent. In a recent Dutchstudy, 1894 patients (1526 men and 368 women) with angiographicallydocumented CAD were evaluated over a 16-yearperiod (1981–97). Over time, <strong>the</strong> number <strong>of</strong> angioplasty proceduresincreased significantly from 11.6–23.2% for men andfrom 17.6–28.0% for women, whereas <strong>the</strong> number <strong>of</strong> cor<strong>on</strong>aryartery bypass procedures decreased in men from 34.9%to 29.5% and from 42.6–30.6% in women. 634 However,interpretati<strong>on</strong> <strong>of</strong> this and o<strong>the</strong>r cor<strong>on</strong>ary arteriographyregistries is limited by <strong>the</strong>ir intrinsic referral bias. Datafrom <strong>the</strong> Euro Heart Survey <strong>of</strong> <strong>Stable</strong> <strong>Angina</strong> c<strong>on</strong>ducted in2003 suggest that significant bias exists against <strong>the</strong> use,not just <strong>of</strong> arteriography but also <strong>of</strong> exercise testing inwomen, even after adjustment for factors such as age,comorbidity, severity <strong>of</strong> symptoms, and, in <strong>the</strong> case <strong>of</strong> arteriography,results <strong>of</strong> n<strong>on</strong>-invasive testing. 635 In <strong>the</strong> samestudy, women were less likely to receive revascularizati<strong>on</strong>and were less likely to receive effective sec<strong>on</strong>dary preventivemedical <strong>the</strong>rapy. Such findings suggest that <strong>the</strong> perceiveddifficulties in diagnosis and limited female-specificliterature regarding <strong>the</strong> treatment <strong>of</strong> angina, al<strong>on</strong>gperhaps with more complex social issues, have perpetuated<strong>the</strong> situati<strong>on</strong> where women with stable angina <strong>of</strong>ten remainunder-investigated and under-treated.Diabetes mellitusBoth insulin-dependent diabetes mellitus (type 1) andn<strong>on</strong>-insulin-dependent diabetes mellitus (type 2) are associatedwith an increased risk <strong>of</strong> CVD. Fur<strong>the</strong>rmore, CHD
ESC <str<strong>on</strong>g>Guidelines</str<strong>on</strong>g> 45mortality is increased three-fold in diabetic men and two- t<strong>of</strong>ive-fold in diabetic women, compared with age- and sexmatchedn<strong>on</strong>-diabetic pers<strong>on</strong>s. 81,636–638 Moreover, anumber <strong>of</strong> epidemiological reports indicate that in patientswith diabetes, <strong>the</strong> higher <strong>the</strong> blood glucose, <strong>the</strong> greater <strong>the</strong>incidence <strong>of</strong> CVD. 639,640The clinical manifestati<strong>on</strong>s <strong>of</strong> CHD in diabetic subjects aresimilar to those in n<strong>on</strong>-diabetic patients, with angina, MI,and heart failure being <strong>the</strong> most prominent, but <strong>the</strong> symptomstend to occur at an earlier age in diabetic patients.It is generally accepted that <strong>the</strong> prevalence <strong>of</strong> asymptomaticischaemia is increased in patients with diabetes.However, because <strong>of</strong> c<strong>on</strong>siderable variati<strong>on</strong> in inclusi<strong>on</strong>and exclusi<strong>on</strong> criteria as well as screening tests in studiesto date, it is somewhat difficult to estimate <strong>the</strong> increasedfrequency <strong>of</strong> silent ischaemia accurately. 641There is growing interest in <strong>the</strong> use <strong>of</strong> myocardial perfusi<strong>on</strong>scanning and o<strong>the</strong>r techniques to detect ischaemia in asymptomaticdiabetic individuals 642 and firm evidence <strong>of</strong> <strong>the</strong> prognosticpower <strong>of</strong> perfusi<strong>on</strong> imaging specifically in diabeticpatients. 643 There are also data to suggest that individualswith diabetes may have subclinical ventricular dysfuncti<strong>on</strong>which negatively impacts <strong>on</strong> exercise capacity, 644 an importantendpoint <strong>of</strong> exercise testing, but <strong>the</strong> impact <strong>of</strong> thisfinding <strong>on</strong> <strong>the</strong> diagnostic and prognostic informati<strong>on</strong> yieldedby c<strong>on</strong>venti<strong>on</strong>al testing in a symptomatic populati<strong>on</strong> is notclear. Thus, <strong>the</strong> cardiac assessment <strong>of</strong> symptomatic ischaemiain diabetic patients should, in general, parallel that in n<strong>on</strong>diabeticsubjects, with similar indicati<strong>on</strong>s for exercisetesting, myocardial perfusi<strong>on</strong> testing, and cor<strong>on</strong>ary arteriography.As CVD accounts for 80% <strong>of</strong> mortality in patientswith diabetes mellitus, 645 emphasis should be placed <strong>on</strong>early diagnosis and aggressive treatment in this populati<strong>on</strong>.Current strategies for optimal care <strong>of</strong> patients with diabetesmellitus include vigorous and persistent efforts toachieve physiological c<strong>on</strong>trol <strong>of</strong> blood glucose and c<strong>on</strong>trol<strong>of</strong> o<strong>the</strong>r risk factors such as dyslipidaemia, renal disease,obesity, and smoking. Abundant evidence that l<strong>on</strong>g-termmaintenance <strong>of</strong> near-normal blood glucose levels is protective<strong>of</strong> patients with diabetes and substantially reducescomplicati<strong>on</strong>s and mortality in both diabetes type 1 andtype 2 is now available. 645–648C<strong>on</strong>venti<strong>on</strong>al <strong>the</strong>rapies for CHD with nitrates, betablockers,calcium-channel blockers, statins, antiplateletsagents, and cor<strong>on</strong>ary revascularizati<strong>on</strong> procedures havesimilar indicati<strong>on</strong>s in diabetic and n<strong>on</strong>-diabetic patients.Additi<strong>on</strong>ally, ACE-inhibitors are indicated in diabeticpatients with proven vascular disease. 253 The relativemerits <strong>of</strong> PCI and CABG in diabetic patients are discussedin <strong>the</strong> secti<strong>on</strong> <strong>on</strong> Revascularizati<strong>on</strong>. Unfortunately, owingto <strong>the</strong> chr<strong>on</strong>ic metabolic disturbances <strong>of</strong> diabetes mellitus,<strong>the</strong>se patients usually have a c<strong>on</strong>tinuous progressi<strong>on</strong> <strong>of</strong>native a<strong>the</strong>rosclerotic disease, leading to an extensiveCHD with high rates <strong>of</strong> multi-vessel disease and <strong>of</strong> restenosis.649,650 Thus, even after successful invasive procedures,good management <strong>of</strong> CVD risk factors and a tight glycaemicc<strong>on</strong>trol are essential for good l<strong>on</strong>g-term outcome. 638ElderlyAfter <strong>the</strong> age <strong>of</strong> 75 years <strong>the</strong>re is an equal prevalence <strong>of</strong> CADin men and women. 651 The disease is more likely to bediffuse and severe; LM cor<strong>on</strong>ary artery stenosis and threevesseldisease are more prevalent in older patients, as isimpaired LV functi<strong>on</strong>. The evaluati<strong>on</strong> <strong>of</strong> chest pain syndromesin <strong>the</strong> elderly can be difficult because complaints<strong>of</strong> chest discomfort, weakness, and dyspnoea are comm<strong>on</strong>,and co-morbid c<strong>on</strong>diti<strong>on</strong>s that mimic angina pectoris arefrequently present. Reduced activity levels and bluntedappreciati<strong>on</strong> <strong>of</strong> ischaemic symptoms become <strong>the</strong> norm withadvancing age. 652 In large community studies <strong>of</strong> men andwomen .65-years old, those with atypical symptoms andtypical angina were shown to have similar 3 year cardiacmortality rates. 20 The performance <strong>of</strong> exercise testingposes additi<strong>on</strong>al problems in <strong>the</strong> elderly. Functi<strong>on</strong>al capacity<strong>of</strong>ten is compromised from muscle weakness and dec<strong>on</strong>diti<strong>on</strong>ing.More attenti<strong>on</strong> must be given to <strong>the</strong> mechanicalhazards <strong>of</strong> exercise, and less challenging protocols may bemore appropriate. Arrhythmias occur more frequently withincreasing age, especially at higher workloads. 653 Theinterpretati<strong>on</strong> <strong>of</strong> exercise test results in <strong>the</strong> elderly differsfrom that in <strong>the</strong> young. The higher prevalence <strong>of</strong> diseasemeans that more test results are false negative. 654 Falsepositivetest results also are more frequent because <strong>of</strong> <strong>the</strong>higher prevalence <strong>of</strong> c<strong>on</strong>founders such as prior MI, LV hypertrophyfrom valvular diseases, hypertensi<strong>on</strong> and c<strong>on</strong>ducti<strong>on</strong>disturbances. Despite <strong>the</strong>se differences, exercise testingremains important also in <strong>the</strong> elderly. The Task Forcebelieves that exercise ECG testing should remain <strong>the</strong> initialtest in evaluating elderly patients with suspected <strong>of</strong> CADunless <strong>the</strong> patient cannot exercise, in which case it may bereplaced by pharmacological stress imaging.It is important to emphasize that elderly patients withobjective evidence <strong>of</strong> moderate-to-severe ischaemia at n<strong>on</strong>invasivetesting should have similar access to cor<strong>on</strong>ary arteriographyas younger patients. Notably, diagnostic cor<strong>on</strong>aryarteriography has relatively little increased risk (comparedwith younger patients) in older patients undergoing electiveevaluati<strong>on</strong>. 243 However, age .75 is an important predictor<strong>of</strong> c<strong>on</strong>trast-induced nephropathy. 655Medical treatment is more complex in elderly patients.Indeed, changes in drug bioavailability, eliminati<strong>on</strong>, andsensitivity mean that dose modificati<strong>on</strong> is essential whenprescribing cardiovascular drugs to elderly patients. 656Fur<strong>the</strong>r issues which should be taken into account whenprescribing for <strong>the</strong> elderly include risk <strong>of</strong> drug interacti<strong>on</strong>s,polypharmacy, and compliance problems. Never<strong>the</strong>less, inthis patient populati<strong>on</strong>, anti-anginal medicati<strong>on</strong>s are asefficacious in reducing symptoms and statins in improvingprognosis, 438 as <strong>the</strong>y are in young patients. C<strong>on</strong>sideringsymptoms as well as prognosis, elderly patients have <strong>the</strong>same benefit from medical <strong>the</strong>rapy, angioplasty, andbypass surgery as younger patients. 657–659Chr<strong>on</strong>ic refractory anginaDrugs and revascularizati<strong>on</strong> procedures, i.e. CABG and percutaneoustransluminal angioplasty, can adequatelymanage <strong>the</strong> majority <strong>of</strong> patients suffering from ischaemicheart disease. However, <strong>the</strong>re are patients who remainseverely disabled by angina pectoris in spite <strong>of</strong> differentforms <strong>of</strong> c<strong>on</strong>venti<strong>on</strong>al treatment. It is an unfortunate ir<strong>on</strong>ythat <strong>the</strong> prol<strong>on</strong>gati<strong>on</strong> <strong>of</strong> life due to <strong>the</strong> improvement <strong>of</strong>cardiovascular care and treatment are resp<strong>on</strong>sible for anincrease in <strong>the</strong> number <strong>of</strong> patients with end-stage ischaemiccor<strong>on</strong>ary disease, some who complain from intractable episodes<strong>of</strong> angina. The problem <strong>of</strong> chr<strong>on</strong>ic refractory angina
46 ESC <str<strong>on</strong>g>Guidelines</str<strong>on</strong>g>was addressed in a Report from <strong>the</strong> ESC Joint Study Group <strong>on</strong><strong>the</strong> Treatment <strong>of</strong> Refractory <strong>Angina</strong>, published in 2002. 660Chr<strong>on</strong>ic stable refractory angina can be defined as a clinicaldiagnosis based <strong>on</strong> <strong>the</strong> presence <strong>of</strong> symptoms <strong>of</strong> stableangina, thought to be caused by ischaemia due to advancedcor<strong>on</strong>ary disease and which are not c<strong>on</strong>trollable by a combinati<strong>on</strong><strong>of</strong> maximal medical <strong>the</strong>rapy, bypass surgery and percutaneousinterventi<strong>on</strong>. N<strong>on</strong>-cardiac causes <strong>of</strong> chest painshould be excluded, and where appropriate, cognitive behavioural<strong>the</strong>rapy, psychological assessment, and/or psychiatricc<strong>on</strong>sultati<strong>on</strong> may be c<strong>on</strong>sidered.According to <strong>the</strong> previously menti<strong>on</strong>ed report from <strong>the</strong>Joint Study Group, we have no accurate figures <strong>on</strong> <strong>the</strong>occurrence and frequency <strong>of</strong> refractory angina. A Swedishsurvey <strong>of</strong> patients referred for cor<strong>on</strong>ary arteriographybecause <strong>of</strong> stable angina pectoris performed in 1994–95showed that nearly 10% <strong>of</strong> patients were rejected for revascularizati<strong>on</strong>despite severe symptoms. 661,662The most comm<strong>on</strong> reas<strong>on</strong>s that revascularizati<strong>on</strong> is notc<strong>on</strong>sidered appropriate are:(1) Unsuitable anatomy(2) One or several previous bypass grafting and/or PTCAprocedures(3) Lack <strong>of</strong> available graft c<strong>on</strong>duits(4) Extra-cardiac diseases which increase perioperativemorbidity and mortality(5) Advanced age, <strong>of</strong>ten in combinati<strong>on</strong> with <strong>the</strong>se factorsChr<strong>on</strong>ic refractory angina requires an effective optimizati<strong>on</strong><strong>of</strong> medical treatment assuring <strong>the</strong> use <strong>of</strong> differentdrugs in maximal tolerated doses. This issue is extensivelydeveloped in <strong>the</strong> original document <strong>of</strong> <strong>the</strong> Joint StudyGroup. Within <strong>the</strong> last few years, new modalities exploringnew c<strong>on</strong>cepts <strong>of</strong> <strong>the</strong>rapy are under extensive evaluati<strong>on</strong>,although not all have been successful: neuromodulati<strong>on</strong>techniques (transcutaneous electric nerve stimulati<strong>on</strong> andspinal cord stimulati<strong>on</strong>), thoracic epidural anaes<strong>the</strong>sia,endoscopic thoracic sympa<strong>the</strong>ctomy, stellate gangli<strong>on</strong>blockade, transmyocardial or percutaneous laser revascularizati<strong>on</strong>,angiogenesis, enhanced external counterpulsati<strong>on</strong>,heart transplantati<strong>on</strong>, and drugs that modulate metabolism.Transcutaneous electrical stimulati<strong>on</strong> and spinal cordstimulati<strong>on</strong> are well-established methods used in severalcentres for <strong>the</strong> management <strong>of</strong> refractory angina with positiveeffects <strong>on</strong> symptoms and a favourable side-effectpr<strong>of</strong>ile. 663–665 These techniques have a favourable analgesiceffect even without any improvement in myocardial ischaemia.A significant increase in <strong>the</strong> average exercise time <strong>on</strong>treadmill testing has however been observed. The number<strong>of</strong> published reports and <strong>the</strong> number <strong>of</strong> patients enrolledin clinical trials are small, and <strong>the</strong> l<strong>on</strong>g-term effects <strong>of</strong><strong>the</strong>se techniques are unknown.Enhanced external counterpulsati<strong>on</strong> (EECP) is an interestingn<strong>on</strong>-pharmacological technique, which has also beeninvestigated largely in <strong>the</strong> USA. Two multi-centre registrieshave evaluated <strong>the</strong> safety and effectiveness <strong>of</strong> EECP. 666–668The technique is very well tolerated when used over aperiod <strong>of</strong> 35 hours <strong>of</strong> active counterpulsati<strong>on</strong> during4–7-week period. <strong>Angina</strong>l symptoms were improved in75–80% <strong>of</strong> patients.Transmyocardial revascularizati<strong>on</strong> has been comparedwith medical <strong>the</strong>rapy in several studies. In <strong>on</strong>e study (in275 patients with CCS class IV symptoms), 76% <strong>of</strong> patientswho had underg<strong>on</strong>e transmyocardial revascularizati<strong>on</strong>improved two or more functi<strong>on</strong>al classes after 1 year <strong>of</strong>follow-up, as compared with 32% (P , 0.001) <strong>of</strong> <strong>the</strong> patientswho received medical <strong>the</strong>rapy al<strong>on</strong>e. 669 Mortality did notdiffer significantly between <strong>the</strong> two groups. O<strong>the</strong>r studies<strong>of</strong> transmyocardial revascularizati<strong>on</strong> (ei<strong>the</strong>r surgically or percutaneously)have been unable to c<strong>on</strong>firm this benefit. 670,671In particular, a recent randomized c<strong>on</strong>trolled trial <strong>of</strong> 298patients showed that treatment with percutaneous myocardiallaser provides no benefit bey<strong>on</strong>d that <strong>of</strong> a similar shamprocedure in patients blinded to <strong>the</strong>ir treatment. 672Fur<strong>the</strong>rmore, measurement <strong>of</strong> regi<strong>on</strong>al myocardial bloodflow and cor<strong>on</strong>ary flow reserve by means <strong>of</strong> PET has failedto show imporved perfusi<strong>on</strong> following this procedure. 673Internati<strong>on</strong>al studies and registries are urgently requiredto clarify <strong>the</strong> epidemiology <strong>of</strong> this c<strong>on</strong>diti<strong>on</strong> and fur<strong>the</strong>rresearch is encouraged to definitely establish <strong>the</strong> roles <strong>of</strong>existing and novel alternative techniques to manage <strong>the</strong>sepatients.C<strong>on</strong>clusi<strong>on</strong>s and Recommendati<strong>on</strong>s(1) <strong>Angina</strong> pectoris due to cor<strong>on</strong>ary a<strong>the</strong>rosclerosis is acomm<strong>on</strong> and disabling disorder. Although compatiblewith l<strong>on</strong>gevity, <strong>the</strong>re is an increased risk <strong>of</strong> progressi<strong>on</strong>to MI and/or death. With proper management, <strong>the</strong>symptoms can usually be c<strong>on</strong>trolled and <strong>the</strong> prognosissubstantially improved.(2) Every patient with suspected stable angina requiresprompt and appropriate cardiological investigati<strong>on</strong> toensure that <strong>the</strong> diagnosis is correct and that <strong>the</strong> prognosisis evaluated. As a minimum, each patient shouldhave a carefully taken history and physical examinati<strong>on</strong>,a comprehensive risk factor evaluati<strong>on</strong>, and aresting ECG.(3) To c<strong>on</strong>firm <strong>the</strong> diagnosis and plan fur<strong>the</strong>r management,an initial n<strong>on</strong>-invasive strategy, using exercise ECG,stress echo, or myocardial perfusi<strong>on</strong> scintigraphy ismost appropriate. This allows an assessment <strong>of</strong> <strong>the</strong>likelihood <strong>of</strong> and <strong>the</strong> severity <strong>of</strong> CHD in patients withmild-to-moderate symptoms and effective risk stratificati<strong>on</strong>.In many patients, cor<strong>on</strong>ary arteriography mayfollow, but an initial invasive strategy without priorfuncti<strong>on</strong>al testing is rarely indicated, and may <strong>on</strong>lybe c<strong>on</strong>sidered for patients with new <strong>on</strong>set severe orunc<strong>on</strong>trolled symptoms.(4) The exercise ECG should be interpreted with attenti<strong>on</strong>to haemodynamic resp<strong>on</strong>se, workload achieved, andclinical features <strong>of</strong> <strong>the</strong> individual as well as symptomsand ST-segment resp<strong>on</strong>se. Alternative investigati<strong>on</strong>sare needed when exercise is not possible or <strong>the</strong> ECG isnot interpretable, or in additi<strong>on</strong> to exercise testingwhen <strong>the</strong> diagnosis remains uncertain or functi<strong>on</strong>alassessment is inadequate.(5) In additi<strong>on</strong> to <strong>the</strong>ir role in intial assessment <strong>of</strong> stableangina symptoms, myocardial perfusi<strong>on</strong> scintigraphyand stress echocardiography are <strong>of</strong> particular value indem<strong>on</strong>strating <strong>the</strong> extent and localizati<strong>on</strong> <strong>of</strong> myocardialischaemia.(6) Echocardiography and o<strong>the</strong>r n<strong>on</strong>-invasive imaging modalities,such as magnetic res<strong>on</strong>ance, are helpful in evaluatingventricular functi<strong>on</strong>.
ESC <str<strong>on</strong>g>Guidelines</str<strong>on</strong>g> 47(7) The interpretati<strong>on</strong> <strong>of</strong> chest pain is particularly difficultin young and middle-aged women. The classicalsymptom complex <strong>of</strong> chr<strong>on</strong>ic stable angina, which is areliable indicator <strong>of</strong> obstructive cor<strong>on</strong>ary disease inmen, is not so in younger women. This problem is compoundedby <strong>the</strong> higher prevalence <strong>of</strong> cor<strong>on</strong>ary arteryspasm and ‘Syndrome X’ in women with chest painand by <strong>the</strong> frequency <strong>of</strong> ‘false-positive’ exercisetests. However, <strong>the</strong>se complexities should not preventappropriate investigati<strong>on</strong> and treatment <strong>of</strong> women,particularly <strong>the</strong> use <strong>of</strong> n<strong>on</strong>-invasive investigati<strong>on</strong>s for<strong>the</strong> purposes <strong>of</strong> risk stratificati<strong>on</strong> and use <strong>of</strong> sec<strong>on</strong>darypreventative <strong>the</strong>rapies.(8) After initial risk evaluati<strong>on</strong>, risk-factor correcti<strong>on</strong> bylife-style modificati<strong>on</strong> should be implemented inadditi<strong>on</strong> to pharmacological interventi<strong>on</strong> as necessary.Strict diabetic c<strong>on</strong>trol and weight c<strong>on</strong>trol al<strong>on</strong>gwith smoking cessati<strong>on</strong> strategies are str<strong>on</strong>gly advisedin all patients with cor<strong>on</strong>ary disease, and bloodpressure c<strong>on</strong>trol is extremely important. Successfulrisk-factor management may modify <strong>the</strong> initial riskassessment.(9) In terms <strong>of</strong> specific pharmacological <strong>the</strong>rapy, shortactingnitrates, when tolerated, may be used toprovide acute symtomatic relief. In <strong>the</strong> absence <strong>of</strong> c<strong>on</strong>traindicati<strong>on</strong>sor intolerance, patients with stableangina pectoris should be treated with aspirin(75 mg/day) and statin <strong>the</strong>rapy. A beta-blocker shouldbe used first line or, alternatively, a calcium-channelblocker or l<strong>on</strong>g-acting nitrate may be used to provideanti-anginal effects, as described earlier, withadditi<strong>on</strong>al <strong>the</strong>rapy as necessary. ACE-inhibiti<strong>on</strong> is indicatedin patients with co-existing ventricular dysfuncti<strong>on</strong>,hypertensi<strong>on</strong>, or diabetes and should be str<strong>on</strong>glyc<strong>on</strong>sidered in patients with o<strong>the</strong>r high-risk features.Beta-blockers should be recommended in all post-MIpatients and in patients with LV dysfuncti<strong>on</strong>, unlessc<strong>on</strong>traindicated.(10) Anti-anginal drug treatment should be tailored to <strong>the</strong>needs <strong>of</strong> <strong>the</strong> individual patient and should be m<strong>on</strong>itoredindividually. The dosing <strong>of</strong> <strong>on</strong>e drug should beoptimized before adding ano<strong>the</strong>r <strong>on</strong>e, and it is adviseableto switch drug combinati<strong>on</strong>s before attempting athree drug regimen.(11) If not undertaken for fur<strong>the</strong>r prognostic evaluati<strong>on</strong>,cor<strong>on</strong>ary arteriography should be undertaken whensymptoms are not satisfactorily c<strong>on</strong>trolled by medicalmeans, with a view to revascularizati<strong>on</strong>.(12) PCI is an effective treatment for stable angina pectorisand is indicated for patients with angina not satisfactorilyc<strong>on</strong>trolled by medical treatment when <strong>the</strong>reare anatomically suitable lesi<strong>on</strong>s. Restenosis c<strong>on</strong>tinuesto be a problem, which has been diminished byadvances in stenting technology. There is no evidencethat PCI reduces <strong>the</strong> risk <strong>of</strong> death in patients withstable angina compared with medical or surgical<strong>the</strong>rapy.(13) CABG is highly effective in relieving <strong>the</strong> symptoms <strong>of</strong>stable angina and reduces <strong>the</strong> risk <strong>of</strong> death over l<strong>on</strong>gtermfollow-up in particular subgroups <strong>of</strong> patients,such as those with LM stem stenosis, proximal LADstenosis, and three-vessel disease, especially if LVfuncti<strong>on</strong> is impaired.(14) There is evidence 674,675 that some gaps remainbetween best practice and usual care in <strong>the</strong> management<strong>of</strong> stable angina. Specifically, many individualswith stable angina are not referred for functi<strong>on</strong>altesting to c<strong>on</strong>firm <strong>the</strong> diagnosis and determine prognosis.Fur<strong>the</strong>rmore, <strong>the</strong>re is worrying variability in rates<strong>of</strong> prescripti<strong>on</strong> <strong>of</strong> statins and aspirin. Because <strong>of</strong> <strong>the</strong>wide variati<strong>on</strong>s in <strong>the</strong> quality <strong>of</strong> care afforded to sufferersfrom angina, <strong>the</strong>re is a str<strong>on</strong>g case for auditingseveral comp<strong>on</strong>ents <strong>of</strong> <strong>the</strong> management <strong>of</strong> <strong>the</strong> c<strong>on</strong>diti<strong>on</strong>.As is <strong>the</strong> practice in some countries, local,regi<strong>on</strong>al, or nati<strong>on</strong>al registers <strong>of</strong> <strong>the</strong> outcome <strong>of</strong> PCIand surgery should be created and maintained.References1. De Backer G, Ambrosi<strong>on</strong>i E, Borch-Johnsen K, Brot<strong>on</strong>s C, Cifkova R,Dall<strong>on</strong>geville J et al. European guidelines <strong>on</strong> cardiovascular diseasepreventi<strong>on</strong> in clinical practice: third joint task force <strong>of</strong> European ando<strong>the</strong>r societies <strong>on</strong> cardiovascular disease preventi<strong>on</strong> in clinical practice(c<strong>on</strong>stituted by representatives <strong>of</strong> eight societies and by invitedexperts). Eur J <strong>Cardio</strong>vasc Prev Rehabil 2003;10:S1–S10.2. Heberden. Some account <strong>of</strong> a disorder <strong>of</strong> <strong>the</strong> breast. Med Transact R CollPhys L<strong>on</strong>d 1772;2:59.3. Parry CH. An inquiry into <strong>the</strong> symptoms and causes <strong>of</strong> syncope anginosa,comm<strong>on</strong>ly called angina pectoris. Edinburgh, L<strong>on</strong>d<strong>on</strong>: Bryce, Murray andCallow;1799.4. Crea F, Gaspard<strong>on</strong>e A. New look to an old symptom: angina pectoris.Circulati<strong>on</strong> 1997;96:3766–3773.5. Tomai F, Crea F, Chiariello L, Gi<strong>of</strong>fre PA. Ischemic prec<strong>on</strong>diti<strong>on</strong>ing inhumans: models, mediators, and clinical relevance. Circulati<strong>on</strong>1999;100:559–563.6. Cohn PF, Fox KM, Daly C. Silent myocardial ischemia. Circulati<strong>on</strong>2003;108:1263–1277.7. Gould KL, Kirkeeide RL, Buchi M. Cor<strong>on</strong>ary flow reserve as a physiologicmeasure <strong>of</strong> stenosis severity. J Am Coll <strong>Cardio</strong>l 1990;15:459–474.8. Gould KL. Effects <strong>of</strong> cor<strong>on</strong>ary stenoses <strong>on</strong> cor<strong>on</strong>ary flow reserve andresistance. Am J <strong>Cardio</strong>l 1974;34:48–55.9. Mohlenkamp S, Hort W, Ge J, Erbel R. Update <strong>on</strong> myocardial bridging.Circulati<strong>on</strong> 2002;106:2616–2622.10. Pupita G, Maseri A, Kaski JC, Galassi AR, Gavrielides S, Davies G et al.Myocardial ischemia caused by distal cor<strong>on</strong>ary-artery c<strong>on</strong>stricti<strong>on</strong> instable angina pectoris. N Engl J Med 1990;323:514–520.11. Braunwald E. Unstable angina. A classificati<strong>on</strong>. Circulati<strong>on</strong> 1989;80:410–414.12. Myocardial infarcti<strong>on</strong> redefined–a c<strong>on</strong>sensus document <strong>of</strong> The JointEuropean Society <strong>of</strong> <strong>Cardio</strong>logy/American College <strong>of</strong> <strong>Cardio</strong>logyCommittee for <strong>the</strong> redefiniti<strong>on</strong> <strong>of</strong> myocardial infarcti<strong>on</strong>. Eur Heart J2000;21:1502–1513.13. Yamagishi M, Terashima M, Awano K, Kijima M, Nakatani S, Daikoku Set al. Morphology <strong>of</strong> vulnerable cor<strong>on</strong>ary plaque: insights from follow-up<strong>of</strong> patients examined by intravascular ultrasound before an acute cor<strong>on</strong>arysyndrome. J Am Coll <strong>Cardio</strong>l 2000;35:106–111.14. Libby P. Molecular bases <strong>of</strong> <strong>the</strong> acute cor<strong>on</strong>ary syndromes. Circulati<strong>on</strong>1995;91:2844–2850.15. Buff<strong>on</strong> A, Biasucci LM, Liuzzo G, D’On<strong>of</strong>rio G, Crea F, Maseri A.Widespread cor<strong>on</strong>ary inflammati<strong>on</strong> in unstable angina. N Engl J Med2002;347:5–12.16. Rose GA, Blackburn H. <strong>Cardio</strong>vascular survey methods. M<strong>on</strong>ogr SerWorld Health Organ 1968;56:1–188.17. Cook DG, Shaper AG, MacFarlane PW. Using <strong>the</strong> WHO (Rose) angina questi<strong>on</strong>nairein cardiovascular epidemiology. Int J Epidemiol 1989;18:607–613.18. Lampe FC, Whincup PH, Wanname<strong>the</strong>e SG, Ebrahim S, Walker M, Shaper AG.Chest pain <strong>on</strong> questi<strong>on</strong>naire and predicti<strong>on</strong> <strong>of</strong> major ischaemic heart diseaseevents in men. Eur Heart J 1998;19:63–73.19. Bulpitt CJ, Shipley MJ, Demirovic J, Ebi-Kryst<strong>on</strong> KL, Markowe HL, Rose G.Predicting death from cor<strong>on</strong>ary heart disease using a questi<strong>on</strong>naire. Int JEpidemiol 1990;19:899–904.20. LaCroix AZ, Guralnik JM, Curb JD, Wallace RB, Ostfeld AM, HennekensCH. Chest pain and cor<strong>on</strong>ary heart disease mortality am<strong>on</strong>g older menand women in three communities. Circulati<strong>on</strong> 1990;81:437–446.
48 ESC <str<strong>on</strong>g>Guidelines</str<strong>on</strong>g>21. Friedman LM, Byingt<strong>on</strong> RP. Assessment <strong>of</strong> angina pectoris after myocardialinfarcti<strong>on</strong>: comparis<strong>on</strong> <strong>of</strong> ‘Rose Questi<strong>on</strong>naire’ with physician judgmentin <strong>the</strong> Beta-Blocker Heart Attack Trial. Am J Epidemiol1985;121:555–562.22. Wilcosky T, Harris R, Weissfeld L. The prevalence and correlates <strong>of</strong> RoseQuesti<strong>on</strong>naire angina am<strong>on</strong>g women and men in <strong>the</strong> Lipid ResearchClinics Program Prevalence Study populati<strong>on</strong>. Am J Epidemiol1987;125:400–409.23. Garber CE, Carlet<strong>on</strong> RA, Heller GV. Comparis<strong>on</strong> <strong>of</strong> ‘Rose Questi<strong>on</strong>naire<strong>Angina</strong>’ to exercise thallium scintigraphy: different findings in malesand females. J Clin Epidemiol 1992;45:715–720.24. Erikssen J, Forfang K, Storstein O. <strong>Angina</strong> pectoris in presumably healthymiddle-aged men. Validati<strong>on</strong> <strong>of</strong> two questi<strong>on</strong>naire methods in making<strong>the</strong> diagnosis <strong>of</strong> angina pectoris. Eur J <strong>Cardio</strong>l 1977;6:285–298.25. Nichols<strong>on</strong> A, White IR, Macfarlane P, Brunner E, Marmot M. Rose questi<strong>on</strong>naireangina in younger men and women: gender differences in<strong>the</strong> relati<strong>on</strong>ship to cardiovascular risk factors and o<strong>the</strong>r reportedsymptoms. J Clin Epidemiol 1999;52:337–346.26. Rose G, Hamilt<strong>on</strong> PS, Keen H, Reid DD, McCartney P, Jarrett RJ.Myocardial ischaemia, risk factors and death from cor<strong>on</strong>ary heartdisease.Lancet 1977;1:105–109.27. Hagman M, J<strong>on</strong>ss<strong>on</strong> D, Wilhelmsen L. Prevalence <strong>of</strong> angina pectoris andmyocardial infarcti<strong>on</strong> in a general populati<strong>on</strong> sample <strong>of</strong> Swedish men.Acta Med Scand 1977;201:571–577.28. Shaper AG, Pocock SJ, Walker M, Cohen NM, Wale CJ, Thoms<strong>on</strong> AG.British Regi<strong>on</strong>al Heart Study: cardiovascular risk factors in middle-agedmen in 24 towns. Br Med J (Clin Res Ed) 1981;283:179–186.29. Baint<strong>on</strong> D, Baker IA, Sweetnam PM, Yarnell JW, Elwood PC. Prevalence<strong>of</strong> ischaemic heart disease: <strong>the</strong> Caerphilly and Speedwell surveys.Br Heart J 1988;59:201–206.30. Krogh V, Trevisan M, Panico S, Farinaro E, Mancini M, Menotti A et al.Prevalence and correlates <strong>of</strong> angina pectoris in <strong>the</strong> Italian nine communitiesstudy. Research Group ATS-RF2 <strong>of</strong> <strong>the</strong> Italian Nati<strong>on</strong>al ResearchCouncil. Epidemiology 1991;2:26–32.31. Ford ES, Giles WH, Cr<strong>of</strong>t JB. Prevalence <strong>of</strong> n<strong>on</strong>fatal cor<strong>on</strong>ary heartdisease am<strong>on</strong>g American adults. Am Heart J 2000;139:371–377.32. Smith WC, Kenicer MB, Tunstall-Pedoe H, Clark EC, Crombie IK.Prevalence <strong>of</strong> cor<strong>on</strong>ary heart disease in Scotland: Scottish HeartHealth Study. Br Heart J 1990;64:295–298.33. Mittelmark MB, Psaty BM, Rautaharju PM, Fried LP, Borhani NO, Tracy RPet al. Prevalence <strong>of</strong> cardiovascular diseases am<strong>on</strong>g older adults. The<strong>Cardio</strong>vascular Health Study. Am J Epidemiol 1993;137:311–317.34. Keys A. Wine, garlic, and CHD in seven countries. Lancet 1980;1:145–146.35. Lampe FC, Morris RW, Whincup PH, Walker M, Ebrahim S, Shaper AG. Is<strong>the</strong> prevalence <strong>of</strong> cor<strong>on</strong>ary heart disease falling in British men? Heart2001;86:499–505.36. Fry J. The natural history <strong>of</strong> angina in a general practice. J R Coll GenPract 1976;26:643–646.37. Medalie JH, Goldbourt U. <strong>Angina</strong> pectoris am<strong>on</strong>g 10,000 men. II.Psychosocial and o<strong>the</strong>r risk factors as evidenced by a multivariate analysis<strong>of</strong> a 5 year incidence study. Am J Med 1976;60:910–921.38. Yano K, Reed DM, McGee DL. 10 year incidence <strong>of</strong> cor<strong>on</strong>ary heart diseasein <strong>the</strong> H<strong>on</strong>olulu Heart Program. Relati<strong>on</strong>ship to biologic and lifestylecharacteristics. Am J Epidemiol 1984;119:653–666.39. Margolis JR, Gillum RF, Feinleib M, Brasch R, Fabsitz R. Community surveillancefor cor<strong>on</strong>ary heart disease: <strong>the</strong> Framingham <strong>Cardio</strong>vascularDisease survey. Comparis<strong>on</strong>s with <strong>the</strong> Framingham Heart Study and previousshort-term studies. Am J <strong>Cardio</strong>l 1976;37:61–67.40. Kannel WB, Feinleib M. Natural history <strong>of</strong> angina pectoris in <strong>the</strong>Framingham study. Prognosis and survival. Am J <strong>Cardio</strong>l1972;29:154–163.41. Reunanen A, Suh<strong>on</strong>en O, Aromaa A, Knekt P, Pyorala K. Incidence <strong>of</strong>different manifestati<strong>on</strong>s <strong>of</strong> cor<strong>on</strong>ary heart disease in middle-agedFinnish men and women. Acta Med Scand 1985;218:19–26.42. Ducimetiere P, Ruidavets JB, M<strong>on</strong>taye M, Haas B, Yarnell J. 5 year incidence<strong>of</strong> angina pectoris and o<strong>the</strong>r forms <strong>of</strong> cor<strong>on</strong>ary heart disease inhealthy men aged 50–59 in France and Nor<strong>the</strong>rn Ireland: <strong>the</strong>Prospective Epidemiological Study <strong>of</strong> Myocardial Infarcti<strong>on</strong> (PRIME)Study. Int J Epidemiol 2001;30:1057–1062.43. Sigurdss<strong>on</strong> E, Thorgeirss<strong>on</strong> G, Sigvaldas<strong>on</strong> H, Sigfuss<strong>on</strong> N. Prevalence <strong>of</strong>cor<strong>on</strong>ary heart disease in Icelandic men 1968–1986. The ReykjavikStudy. Eur Heart J 1993;14:584–591.44. Tunstall-Pedoe H, Kuulasmaa K, Mah<strong>on</strong>en M, Tol<strong>on</strong>en H, Ruokokoski E,Amouyel P. C<strong>on</strong>tributi<strong>on</strong> <strong>of</strong> trends in survival and cor<strong>on</strong>ary-event ratesto changes in cor<strong>on</strong>ary heart disease mortality: 10-year results from37 WHO MONICA project populati<strong>on</strong>s. M<strong>on</strong>itoring trends and determinantsin cardiovascular disease. Lancet 1999;353:1547–1557.45. Rosengren A, Wilhelmsen L, Hagman M, Wedel H. Natural history <strong>of</strong> myocardialinfarcti<strong>on</strong> and angina pectoris in a general populati<strong>on</strong> sample <strong>of</strong>middle-aged men: a 16-year follow-up <strong>of</strong> <strong>the</strong> Primary Preventi<strong>on</strong> Study,Goteborg, Sweden. JInternMed1998;244:495–505.46. Murabito JM, Evans JC, Lars<strong>on</strong> MG, Levy D. Prognosis after <strong>the</strong> <strong>on</strong>set <strong>of</strong>cor<strong>on</strong>ary heart disease. An investigati<strong>on</strong> <strong>of</strong> differences in outcomebetween <strong>the</strong> sexes according to initial cor<strong>on</strong>ary disease presentati<strong>on</strong>.Circulati<strong>on</strong> 1993;88:2548–2555.47. Juul-Moller S, Edvardss<strong>on</strong> N, Jahnmatz B, Rosen A, Sorensen S, OmblusR. Double-blind trial <strong>of</strong> aspirin in primary preventi<strong>on</strong> <strong>of</strong> myocardialinfarcti<strong>on</strong> in patients with stable chr<strong>on</strong>ic angina pectoris. The Swedish<strong>Angina</strong> <strong>Pectoris</strong> Aspirin Trial (SAPAT) Group. Lancet 1992;340:1421–1425.48. Dargie HJ, Ford I, Fox KM. Total Ischaemic Burden European Trial(TIBET). Effects <strong>of</strong> ischaemia and treatment with atenolol, nifedipineSR and <strong>the</strong>ir combinati<strong>on</strong> <strong>on</strong> outcome in patients with chr<strong>on</strong>ic stableangina. The TIBET Study Group. Eur Heart J 1996;17:104–112.49. Rehnqvist N, Hjemdahl P, Billing E, Bjorkander I, Erikss<strong>on</strong> SV, Forslund Let al. Effects <strong>of</strong> metoprolol vs. verapamil in patients with stable anginapectoris. The <strong>Angina</strong> Prognosis Study in Stockholm (APSIS). Eur Heart J1996;17:76–81.50. Pepine CJ, Handberg EM, Cooper-DeH<strong>of</strong>f RM, Marks RG, Kowey P,Messerli FH et al. A calcium antag<strong>on</strong>ist vs. a n<strong>on</strong>-calcium antag<strong>on</strong>isthypertensi<strong>on</strong> treatment strategy for patients with cor<strong>on</strong>ary arterydisease. The Internati<strong>on</strong>al Verapamil-Trandolapril Study (INVEST): a randomizedc<strong>on</strong>trolled trial. JAMA 2003;290:2805–2816.51. Henders<strong>on</strong> RA, Pocock SJ, Clayt<strong>on</strong> TC, Knight R, Fox KA, Julian DG et al.7 year outcome in <strong>the</strong> RITA-2 trial: cor<strong>on</strong>ary angioplasty versus medical<strong>the</strong>rapy. J Am Coll <strong>Cardio</strong>l 2003;42:1161–1170.52. Brunelli C, Crist<strong>of</strong>ani R, L’Abbate A. L<strong>on</strong>g-term survival in medicallytreated patients with ischaemic heart disease and prognostic importance<strong>of</strong> clinical and electrocardiographic data (<strong>the</strong> Italian CNRMulticentre Prospective Study OD1). Eur Heart J 1989;10:292–303.53. Benchimol D, Dubroca B, Bernard V, Lavie J, Paviot B, Benchimol H et al.Short- and l<strong>on</strong>g-term risk factors for sudden death in patients withstable angina. Int J <strong>Cardio</strong>l 2000;76:147–156.54. Stampfer MJ, Krauss RM, Ma J, Blanche PJ, Holl LG, Sacks FM et al.A prospective study <strong>of</strong> triglyceride level, low-density lipoprotein particlediameter, and risk <strong>of</strong> myocardial infarcti<strong>on</strong>. JAMA 1996;276:882–888.55. Rosengren A, Dotevall A, Erikss<strong>on</strong> H, Wilhelmsen L. Optimal risk factorsin <strong>the</strong> populati<strong>on</strong>: prognosis, prevalence, and secular trends; data fromGoteborg populati<strong>on</strong> studies. Eur Heart J 2001;22:136–144.56. Anders<strong>on</strong> JL, Muhlestein JB, Horne BD, Carlquist JF, Bair TL, Madsen TEet al. Plasma homocysteine predicts mortality independently <strong>of</strong> traditi<strong>on</strong>alrisk factors and C-reactive protein in patients with angiographicallydefined cor<strong>on</strong>ary artery disease. Circulati<strong>on</strong> 2000;102:1227–1232.57. Rosengren A, Hagman M, Wedel H, Wilhelmsen L. Serum cholesterol andl<strong>on</strong>g-term prognosis in middle-aged men with myocardial infarcti<strong>on</strong> andangina pectoris. A 16-year follow-up <strong>of</strong> <strong>the</strong> Primary Preventi<strong>on</strong> Study inGoteborg, Sweden. Eur Heart J 1997;18:754–761.58. Pekkanen J, Linn S, Heiss G, Suchindran CM, Le<strong>on</strong> A, Rifkind BM et al.10 year mortality from cardiovascular disease in relati<strong>on</strong> to cholesterollevel am<strong>on</strong>g men with and without preexisting cardiovascular disease.N Engl J Med 1990;322:1700–1707.59. Tervahauta M, Pekkanen J, Nissinen A. Risk factors <strong>of</strong> cor<strong>on</strong>ary heartdisease and total mortality am<strong>on</strong>g elderly men with and without preexistingcor<strong>on</strong>ary heart disease. Finnish cohorts <strong>of</strong> <strong>the</strong> Seven CountriesStudy. J Am Coll <strong>Cardio</strong>l 1995;26:1623–1629.60. Miettinen H, Lehto S, Salomaa V, Mah<strong>on</strong>en M, Niemela M, Haffner SMet al. Impact <strong>of</strong> diabetes <strong>on</strong> mortality after <strong>the</strong> first myocardial infarcti<strong>on</strong>.The FINMONICA Myocardial Infarcti<strong>on</strong> Register Study Group.Diabetes Care 1998;21:69–75.61. Melchior T, Kober L, Madsen CR, Seibaek M, Jensen GV, Hildebrandt Pet al. Accelerating impact <strong>of</strong> diabetes mellitus <strong>on</strong> mortality in <strong>the</strong>years following an acute myocardial infarcti<strong>on</strong>. TRACE Study Group.Trandolapril Cardiac Evaluati<strong>on</strong>. Eur Heart J 1999;20:973–978.62. Luscher TF, Creager MA, Beckman JA, Cosentino F. Diabetes and vasculardisease: pathophysiology, clinical c<strong>on</strong>sequences, and medical <strong>the</strong>rapy:Part II. Circulati<strong>on</strong> 2003;108:1655–1661.63. Herlitz J, Karls<strong>on</strong> BW, Lindqvist J, Sjolin M. Rate and mode <strong>of</strong> deathduring 5 years <strong>of</strong> follow-up am<strong>on</strong>g patients with acute chest pain withand without a history <strong>of</strong> diabetes mellitus. Diabet Med 1998;15:308–314.
ESC <str<strong>on</strong>g>Guidelines</str<strong>on</strong>g> 4964. Kjaergaard SC, Hansen HH, Fog L, Bulow I, Christensen PD. In-hospitaloutcome for diabetic patients with acute myocardial infarcti<strong>on</strong> in <strong>the</strong>thrombolytic era. Scand <strong>Cardio</strong>vasc J 1999;33:166–170.65. Uusitupa MI, Niskanen LK, Siit<strong>on</strong>en O, Voutilainen E, Pyorala K. 5-yearincidence <strong>of</strong> a<strong>the</strong>rosclerotic vascular disease in relati<strong>on</strong> to generalrisk factors, insulin level, and abnormalities in lipoprotein compositi<strong>on</strong>in n<strong>on</strong>-insulin-dependent diabetic and n<strong>on</strong>diabetic subjects.Circulati<strong>on</strong> 1990;82:27–36.66. Harris PJ, Harrell FE Jr, Lee KL, Behar VS, Rosati RA. Survival in medicallytreated cor<strong>on</strong>ary artery disease. Circulati<strong>on</strong> 1979;60:1259–1269.67. Mock MB, Ringqvist I, Fisher LD, Davis KB, Chaitman BR, Kouchoukos NTet al. Survival <strong>of</strong> medically treated patients in <strong>the</strong> cor<strong>on</strong>ary arterysurgery study (CASS) registry. Circulati<strong>on</strong> 1982;66:562–568.68. Califf RM, Armstr<strong>on</strong>g PW, Carver JR, D’Agostino RB, Strauss WE. 27thBe<strong>the</strong>sda C<strong>on</strong>ference: matching <strong>the</strong> intensity <strong>of</strong> risk factor managementwith <strong>the</strong> hazard for cor<strong>on</strong>ary disease events. Task Force 5. Stratificati<strong>on</strong><strong>of</strong> patients into high, medium and low risk subgroups for purposes <strong>of</strong> riskfactor management. J Am Coll <strong>Cardio</strong>l 1996;27:1007–1019.69. Yusuf S, Zucker D, Peduzzi P, Fisher LD, Takaro T, Kennedy JW et al.Effect <strong>of</strong> cor<strong>on</strong>ary artery bypass graft surgery <strong>on</strong> survival: overview <strong>of</strong>10-year results from randomised trials by <strong>the</strong> Cor<strong>on</strong>ary Artery BypassGraft Surgery Trialists Collaborati<strong>on</strong>. Lancet 1994;344:563–570.70. Davies RF, Goldberg AD, Forman S, Pepine CJ, Knatterud GL, Geller Net al. Asymptomatic Cardiac Ischemia Pilot (ACIP) study 2 yearfollow-up: outcomes <strong>of</strong> patients randomized to initial strategies <strong>of</strong>medical <strong>the</strong>rapy versus revascularizati<strong>on</strong>. Circulati<strong>on</strong> 1997;95:2037–2043.71. Bouchart F, Tabley A, Litzler PY, Haas-Hubscher C, Bessou JP, Soyer R.Myocardial revascularizati<strong>on</strong> in patients with severe ischaemic leftventricular dysfuncti<strong>on</strong>. L<strong>on</strong>g term follow-up in 141 patients. Eur J <strong>Cardio</strong>thoracSurg 2001;20:1157–1162.72. Elefteriades JA, Tolis G Jr, Levi E, Mills LK, Zaret BL. Cor<strong>on</strong>ary arterybypass grafting in severe left ventricular dysfuncti<strong>on</strong>: excellent survivalwith improved ejecti<strong>on</strong> fracti<strong>on</strong> and functi<strong>on</strong>al state. J Am Coll <strong>Cardio</strong>l1993;22:1411–1417.73. Diam<strong>on</strong>d GA. A clinically relevant classificati<strong>on</strong> <strong>of</strong> chest discomfort.J Am Coll <strong>Cardio</strong>l 1983;1:574–575.74. Campeau L. Letter: grading <strong>of</strong> angina pectoris. Circulati<strong>on</strong>1976;54:522–523.75. Hlatky MA, Boineau RE, Higginbotham MB, Lee KL, Mark DB, Califf RMet al. A brief self-administered questi<strong>on</strong>naire to determine functi<strong>on</strong>alcapacity (<strong>the</strong> Duke Activity Status Index). Am J <strong>Cardio</strong>l1989;64:651–654.76. Spertus JA, Winder JA, Dewhurst TA, Deyo RA, Prodzinski J, McD<strong>on</strong>ell Met al. Development and evaluati<strong>on</strong> <strong>of</strong> <strong>the</strong> Seattle <strong>Angina</strong> Questi<strong>on</strong>naire:a new functi<strong>on</strong>al status measure for cor<strong>on</strong>ary artery disease. J Am Coll<strong>Cardio</strong>l 1995;25:333–341.77. Spertus JA, J<strong>on</strong>es P, McD<strong>on</strong>ell M, Fan V, Fihn SD. Health status predictsl<strong>on</strong>g-term outcome in outpatients with cor<strong>on</strong>ary disease. Circulati<strong>on</strong>2002;106:43–49.78. Malik S, W<strong>on</strong>g ND, Franklin SS, Kamath TV, L’Italien GJ, Pio JR et al.Impact <strong>of</strong> <strong>the</strong> metabolic syndrome <strong>on</strong> mortality from cor<strong>on</strong>ary heartdisease, cardiovascular disease, and all causes in United States adults.Circulati<strong>on</strong> 2004;110:1245–1250.79. Girman CJ, Rhodes T, Mercuri M, Pyorala K, Kjekshus J, Pedersen TRet al. The metabolic syndrome and risk <strong>of</strong> major cor<strong>on</strong>ary events in<strong>the</strong> Scandinavian Simvastatin Survival Study (4S) and <strong>the</strong> Air Force/Texas Cor<strong>on</strong>ary A<strong>the</strong>rosclerosis Preventi<strong>on</strong> Study (AFCAPS/TexCAPS).Am J <strong>Cardio</strong>l 2004;93:136–141.80. Horne BD, Anders<strong>on</strong> JL, John JM, Weaver A, Bair TL, Jensen KR et al.Which white blood cell subtypes predict increased cardiovascular risk?J Am Coll <strong>Cardio</strong>l 2005;45:1638–1643.81. Haffner SM. Cor<strong>on</strong>ary heart disease in patients with diabetes. NEnglJMed 2000;342:1040–1042.82. Haffner SM, Lehto S, R<strong>on</strong>nemaa T, Pyorala K, Laakso M. Mortality fromcor<strong>on</strong>ary heart disease in subjects with type 2 diabetes and in n<strong>on</strong>diabeticsubjects with and without prior myocardial infarcti<strong>on</strong>. N Engl JMed 1998;339:229–234.83. Gerstein HC, Pais P, Pogue J, Yusuf S. Relati<strong>on</strong>ship <strong>of</strong> glucose and insulinlevels to <strong>the</strong> risk <strong>of</strong> myocardial infarcti<strong>on</strong>: a case-c<strong>on</strong>trol study. JAmColl <strong>Cardio</strong>l 1999;33:612–619.84. Hu FB, Stampfer MJ, Solom<strong>on</strong> CG, Liu S, Willett WC, Speizer FE et al.The impact <strong>of</strong> diabetes mellitus <strong>on</strong> mortality from all causes and cor<strong>on</strong>aryheart disease in women: 20 years <strong>of</strong> follow-up. Arch Intern Med2001;161:1717–1723.85. Hokans<strong>on</strong> JE, Austin MA. Plasma triglyceride level is a risk factor for cardiovasculardisease independent <strong>of</strong> high-density lipoprotein cholesterollevel: a meta-analysis <strong>of</strong> populati<strong>on</strong>-based prospective studies.J <strong>Cardio</strong>vasc Risk 1996;3:213–219.86. Cullet<strong>on</strong> BF, Lars<strong>on</strong> MG, Evans JC, Wils<strong>on</strong> PW, Barrett BJ, Parfrey PSet al. Prevalence and correlates <strong>of</strong> elevated serum creatinine levels:<strong>the</strong> Framingham Heart Study. Arch Intern Med 1999;159:1785–1790.87. Stamler J, Dyer AR, Shekelle RB, Neat<strong>on</strong> J, Stamler R. Relati<strong>on</strong>ship <strong>of</strong>baseline major risk factors to cor<strong>on</strong>ary and all-cause mortality, and tol<strong>on</strong>gevity: findings from l<strong>on</strong>g-term follow-up <strong>of</strong> Chicago cohorts.<strong>Cardio</strong>logy 1993;82:191–222.88. Neat<strong>on</strong> JD, Blackburn H, Jacobs D, Kuller L, Lee DJ, Sherwin R et al.Serum cholesterol level and mortality findings for men screened in <strong>the</strong>Multiple Risk Factor Interventi<strong>on</strong> Trial. Multiple Risk Factor Interventi<strong>on</strong>Trial Research Group. Arch Intern Med 1992;152:1490–1500.89. Goldbourt U, Holtzman E, Neufeld HN. Total and high density lipoproteincholesterol in <strong>the</strong> serum and risk <strong>of</strong> mortality: evidence <strong>of</strong> a thresholdeffect. Br Med J (Clin Res Ed) 1985;290:1239–1243.90. Castelli WP, Garris<strong>on</strong> RJ, Wils<strong>on</strong> PW, Abbott RD, Kalousdian S, Kannel WB.Incidence <strong>of</strong> cor<strong>on</strong>ary heart disease and lipoprotein cholesterol levels.The Framingham Study. JAMA 1986;256:2835–2838.91. Gord<strong>on</strong> DJ, Probstfield JL, Garris<strong>on</strong> RJ, Neat<strong>on</strong> JD, Castelli WP, Knoke JDet al. High-density lipoprotein cholesterol and cardiovascular disease.Four prospective American studies. Circulati<strong>on</strong> 1989;79:8–15.92. Shlipak MG, Stehman-Breen C, Vittingh<strong>of</strong>f E, Lin F, Varosy PD, Wenger NKet al. Creatinine levels and cardiovascular events in women with heartdisease: do small changes matter? Am J Kidney Dis 2004;43:37–44.93. Fried LF, Shlipak MG, Crump C, Bleyer AJ, Gottdiener JS, Kr<strong>on</strong>mal RAet al. Renal insufficiency as a predictor <strong>of</strong> cardiovascular outcomes andmortality in elderly individuals. JAmColl<strong>Cardio</strong>l2003;41:1364–1372.94. Cockr<strong>of</strong>t DW, Gault MH. Predicti<strong>on</strong> <strong>of</strong> creatinine clearance from serumcreatinine. Nephr<strong>on</strong> 1976;16:31–42.95. Arcavi L, Behar S, Caspi A, Reshef N, Boyko V, Knobler H. High fastingglucose levels as a predictor <strong>of</strong> worse clinical outcome in patientswith cor<strong>on</strong>ary artery disease: results from <strong>the</strong> Bezafibrate Infarcti<strong>on</strong>Preventi<strong>on</strong> (BIP) study. Am Heart J 2004;147:239–245.96. Muhlestein JB, Anders<strong>on</strong> JL, Horne BD, Lavasani F, Allen Maycock CA,Bair TL et al. Effect <strong>of</strong> fasting glucose levels <strong>on</strong> mortality rate inpatients with and without diabetes mellitus and cor<strong>on</strong>ary arterydisease undergoing percutaneous cor<strong>on</strong>ary interventi<strong>on</strong>. Am Heart J2003;146:351–358.97. Fisman EZ, Motro M, Tenenbaum A, Boyko V, Mandelzweig L, Behar S.Impaired fasting glucose c<strong>on</strong>centrati<strong>on</strong>s in n<strong>on</strong>diabetic patients withischaemic heart disease: a marker for a worse prognosis. Am Heart J2001;141:485–490.98. Korpilahti K, Syvanne M, Engblom E, Hamalainen H, Puukka P, R<strong>on</strong>nemaa T.Comp<strong>on</strong>ents <strong>of</strong> <strong>the</strong> insulin resistance syndrome are associated with progressi<strong>on</strong><strong>of</strong> a<strong>the</strong>rosclerosis in n<strong>on</strong>-grafted arteries 5 years after cor<strong>on</strong>aryartery bypass surgery. Eur Heart J 1998;19:711–719.99. Wils<strong>on</strong> PW, Cupples LA, Kannel WB. Is hyperglycemia associated withcardiovascular disease? The Framingham Study. Am Heart J 1991;121:586–590.100. Smith NL, Barzilay JI, Shaffer D, Savage PJ, Heckbert SR, Kuller LH et al.Fasting and 2-hour postchallenge serum glucose measures and risk <strong>of</strong>incident cardiovascular events in <strong>the</strong> elderly: <strong>the</strong> <strong>Cardio</strong>vascularHealth Study. Arch Intern Med 2002;162:209–216.101. Park S, Barrett-C<strong>on</strong>nor E, Wingard DL, Shan J, Edelstein S. GHb is abetter predictor <strong>of</strong> cardiovascular disease than fasting or postchallengeplasma glucose in women without diabetes. The Rancho Bernardo Study.Diabetes Care 1996;19:450–456.102. Khaw KT, Wareham N, Luben R, Bingham S, Oakes S, Welch A et al.Glycated haemoglobin, diabetes, and mortality in men in Norfolkcohort <strong>of</strong> european prospective investigati<strong>on</strong> <strong>of</strong> cancer and nutriti<strong>on</strong>(EPIC-Norfolk). BMJ 2001;322:15–18.103. Kip KE, Marroquin OC, Kelley DE, Johns<strong>on</strong> BD, Kelsey SF, Shaw LJ et al.Clinical importance <strong>of</strong> obesity versus <strong>the</strong> metabolic syndrome in cardiovascularrisk in women: a report from <strong>the</strong> Women’s IschemiaSyndrome Evaluati<strong>on</strong> (WISE) study. Circulati<strong>on</strong> 2004;109:706–713.104. Guclu F, Ozmen B, Hekimsoy Z, Kirmaz C. Effects <strong>of</strong> a statin group drug,pravastatin, <strong>on</strong> <strong>the</strong> insulin resistance in patients with metabolicsyndrome. Biomed Pharmaco<strong>the</strong>r 2004;58:614–618.105. Held C, Hjemdahl P, Rehnqvist N, Wallen NH, Bjorkander I, Erikss<strong>on</strong> SVet al. Fibrinolytic variables and cardiovascular prognosis in patientswith stable angina pectoris treated with verapamil or metoprolol.Results from <strong>the</strong> <strong>Angina</strong> Prognosis study in Stockholm. Circulati<strong>on</strong>1997;95:2380–2386.
50 ESC <str<strong>on</strong>g>Guidelines</str<strong>on</strong>g>106. Held C, Hjemdahl P, Rehnqvist N, Bjorkander I, Forslund L, Brodin Uet al. <strong>Cardio</strong>vascular prognosis in relati<strong>on</strong> to apolipoproteins ando<strong>the</strong>r lipid parameters in patients with stable angina pectoris treatedwith verapamil or metoprolol: results from <strong>the</strong> <strong>Angina</strong> Prognosis Studyin Stockholm (APSIS). A<strong>the</strong>rosclerosis 1997;135:109–118.107. Nygard O, Nordrehaug JE, Refsum H, Ueland PM, Farstad M, Vollset SE.Plasma homocysteine levels and mortality in patients with cor<strong>on</strong>aryartery disease. N Engl J Med 1997;337:230–236.108. Boushey CJ, Beresford SA, Omenn GS, Motulsky AG. A quantitativeassessment <strong>of</strong> plasma homocysteine as a risk factor for vasculardisease. Probable benefits <strong>of</strong> increasing folic acid intakes. JAMA1995;274:1049–1057.109. Haverkate F, Thomps<strong>on</strong> SG, Pyke SD, Gallimore JR, Pepys MB. Producti<strong>on</strong><strong>of</strong> C-reactive protein and risk <strong>of</strong> cor<strong>on</strong>ary events in stable and unstableangina. European C<strong>on</strong>certed Acti<strong>on</strong> <strong>on</strong> Thrombosis and Disabilities<strong>Angina</strong> <strong>Pectoris</strong> Study Group. Lancet 1997;349:462–466.110. Thomps<strong>on</strong> SG, Kienast J, Pyke SD, Haverkate F, van de Loo JC.Hemostatic factors and <strong>the</strong> risk <strong>of</strong> myocardial infarcti<strong>on</strong> or suddendeath in patients with angina pectoris. European C<strong>on</strong>certed Acti<strong>on</strong> <strong>on</strong>Thrombosis and Disabilities <strong>Angina</strong> <strong>Pectoris</strong> Study Group. N Engl J Med1995;332:635–641.111. Janss<strong>on</strong> JH, Ol<strong>of</strong>ss<strong>on</strong> BO, Nilss<strong>on</strong> TK. Predictive value <strong>of</strong> tissue plasminogenactivator mass c<strong>on</strong>centrati<strong>on</strong> <strong>on</strong> l<strong>on</strong>g-term mortality in patientswith cor<strong>on</strong>ary artery disease. A 7-year follow-up. Circulati<strong>on</strong>1993;88:2030–2034.112. Held C, Hjemdahl P, Rehnqvist N, Wallen NH, Forslund L, Bjorkander I et al.Haemostatic markers, inflammatory parameters and lipids in male andfemale patients in <strong>the</strong> <strong>Angina</strong> Prognosis Study in Stockholm (APSIS). A comparis<strong>on</strong>with healthy c<strong>on</strong>trols. J Intern Med 1997;241:59–69.113. Blake GJ, Ridker PM. Inflammatory bio-markers and cardiovascular riskpredicti<strong>on</strong>. J Intern Med 2002;252:283–294.114. Zebrack JS, Muhlestein JB, Horne BD, Anders<strong>on</strong> JL. C-reactive protein andangiographic cor<strong>on</strong>ary artery disease: independent and additive predictors<strong>of</strong> risk in subjects with angina. J Am Coll <strong>Cardio</strong>l 2002;39:632–637.115. Pears<strong>on</strong> TA. New tools for cor<strong>on</strong>ary risk assessment: what are <strong>the</strong>iradvantages and limitati<strong>on</strong>s? Circulati<strong>on</strong> 2002;105:886–892.116. Bogaty P BJ, Boyer L, Simard S, Joseph L, Bertrand F, Dagenais GR.Fluctuating inflammatory markers in patients with stable ischaemicheart disease. Arch Intern Med 2005;165:221–226.117. Kragelund C GB, Kober L, Hildebrandt P, Steffensen R. N-terminalpro-B-type natriuretic peptide and l<strong>on</strong>g-term mortality in stable cor<strong>on</strong>aryheart disease. N Engl J Med 2005;352:666–675.118. Andreotti F, Becker FC. A<strong>the</strong>rothrombotic disorders: new insights fromhematology. Circulati<strong>on</strong> 2005;111:1855–1863.119. Norhammar A, Malmberg K, Diderholm E, Lagerqvist B, Lindahl B, Ryden Let al. Diabetes mellitus: <strong>the</strong> major risk factor in unstable cor<strong>on</strong>ary arterydisease even after c<strong>on</strong>siderati<strong>on</strong> <strong>of</strong> <strong>the</strong> extent <strong>of</strong> cor<strong>on</strong>ary artery diseaseand benefits <strong>of</strong> revascularizati<strong>on</strong>. J Am Coll <strong>Cardio</strong>l 2004;43:585–591.120. Bartnik M, Ryden L, Ferrari R, Malmberg K, Pyorala K, Simo<strong>on</strong>s M et al.The prevalence <strong>of</strong> abnormal glucose regulati<strong>on</strong> in patients with cor<strong>on</strong>aryartery disease across Europe. The Euro Heart Survey <strong>on</strong> diabetesand <strong>the</strong> heart. Eur Heart J 2004;25:1880–1890.121. Dash H, Lipt<strong>on</strong> MJ, Chatterjee K, Parmley WW. Estimati<strong>on</strong> <strong>of</strong> pulm<strong>on</strong>aryartery wedge pressure from chest radiograph in patients with chr<strong>on</strong>icc<strong>on</strong>gestive cardiomyopathy and ischaemic cardiomyopathy. Br Heart J1980;44:322–329.122. Chakko S, Woska D, Martinez H, de Marchena E, Futterman L, Kessler KMet al. Clinical, radiographic, and hemodynamic correlati<strong>on</strong>s in chr<strong>on</strong>icc<strong>on</strong>gestive heart failure: c<strong>on</strong>flicting results may lead to inappropriatecare. Am J Med 1991;90:353–359.123. Weiner DA, Ryan TJ, McCabe CH, Chaitman BR, Sheffield LT, Fergus<strong>on</strong> JCet al. Prognostic importance <strong>of</strong> a clinical pr<strong>of</strong>ile and exercise test inmedically treated patients with cor<strong>on</strong>ary artery disease. J Am Coll<strong>Cardio</strong>l 1984;3:772–779.124. Hammermeister KE, DeRouen TA, Dodge HT. Variables predictive <strong>of</strong> survivalin patients with cor<strong>on</strong>ary disease. Selecti<strong>on</strong> by univariate andmultivariate analyses from <strong>the</strong> clinical, electrocardiographic, exercise,arteriographic, and quantitative angiographic evaluati<strong>on</strong>s. Circulati<strong>on</strong>1979;59:421–430.125. Witteman JC, Kok FJ, van Saase JL, Valkenburg HA. Aortic calcificati<strong>on</strong>as a predictor <strong>of</strong> cardiovascular mortality. Lancet 1986;2:1120–1122.126. Hemingway H, Shipley M, Christie D, Marmot M. <strong>Cardio</strong>thoracic ratio andrelative heart volume as predictors <strong>of</strong> cor<strong>on</strong>ary heart disease mortality.The Whitehall study 25 year follow-up. Eur Heart J 1998;19:859–869.127. McCarthy JH, Palmer FJ. Incidence and significance <strong>of</strong> cor<strong>on</strong>ary arterycalcificati<strong>on</strong>. Br Heart J 1974;36:499–506.128. Eggen DA, Str<strong>on</strong>g JP, McGill HC Jr. Cor<strong>on</strong>ary calcificati<strong>on</strong>. Relati<strong>on</strong>ship toclinically significant cor<strong>on</strong>ary lesi<strong>on</strong>s and race, sex, and topographicdistributi<strong>on</strong>. Circulati<strong>on</strong> 1965;32:948–955.129. Kjekshus JK, Maroko PR, Sobel BE. Distributi<strong>on</strong> <strong>of</strong> myocardial injury andits relati<strong>on</strong> to epicardial ST-segment changes after cor<strong>on</strong>ary arteryocclusi<strong>on</strong> in <strong>the</strong> dog. <strong>Cardio</strong>vasc Res 1972;6:490–499.130. Kleber AG. ST-segment elevati<strong>on</strong> in <strong>the</strong> electrocardiogram: a sign <strong>of</strong>myocardial ischemia. <strong>Cardio</strong>vasc Res 2000;45:111–118.131. Proudfit WJ, Bruschke AV, MacMillan JP, Williams GW, S<strong>on</strong>es FM Jr. 15year survival study <strong>of</strong> patients with obstructive cor<strong>on</strong>ary arterydisease. Circulati<strong>on</strong> 1983;68:986–997.132. Frank CW, Weinblatt E, Shapiro S. <strong>Angina</strong> pectoris in men. Prognosticsignificance <strong>of</strong> selected medical factors. Circulati<strong>on</strong> 1973;47:509–517.133. Ruberman W, Weinblatt E, Goldberg JD, Frank CW, Shapiro S, Chaudhary BS.Ventricular premature complexes in prognosis <strong>of</strong> angina. Circulati<strong>on</strong>1980;61:1172–1182.134. Lee TH, Boucher CA. Clinical practice. N<strong>on</strong>invasive tests in patients withstable cor<strong>on</strong>ary artery disease. N Engl J Med 2001;344:1840–1845.135. ESC Working Group <strong>on</strong> Exercise Physiology, Physiopathology andElectrocardiography. <str<strong>on</strong>g>Guidelines</str<strong>on</strong>g> for cardiac exercise testing. Eur Heart J1993;14:969–988.136. Gianrossi R, Detrano R, Mulvihill D, Lehmann K, Dubach P, Colombo Aet al. Exercise-induced ST depressi<strong>on</strong> in <strong>the</strong> diagnosis <strong>of</strong> cor<strong>on</strong>aryartery disease. A meta-analysis. Circulati<strong>on</strong> 1989;80:87–98.137. Kwok Y, Kim C, Grady D, Segal M, Redberg R. Meta-analysis <strong>of</strong> exercisetesting to detect cor<strong>on</strong>ary artery disease in women. Am J <strong>Cardio</strong>l1999;83:660–666.138. Gibs<strong>on</strong> RS. The diagnostic and prognostic value <strong>of</strong> exercise electrocardiographyin asymptomatic subjects and stable symptomatic patients.Curr Opin <strong>Cardio</strong>l 1991;6:536–546.139. Ashley EA, Myers J, Froelicher V. Exercise testing in clinical medicine.Lancet 2000;356:1592–1597.140. Gibb<strong>on</strong>s RJ, Balady GJ, Bricker JT, Chaitman BR, Fletcher GF, Froelicher VFet al. ACC/AHA 2002 guideline update for exercise testing: summaryarticle. A report <strong>of</strong> <strong>the</strong> American College <strong>of</strong> <strong>Cardio</strong>logy/American HeartAssociati<strong>on</strong> Task Force <strong>on</strong> Practice <str<strong>on</strong>g>Guidelines</str<strong>on</strong>g> (Committee to Update <strong>the</strong>1997 Exercise Testing <str<strong>on</strong>g>Guidelines</str<strong>on</strong>g>). J Am Coll <strong>Cardio</strong>l 2002;40:1531–1540.141. Hung J, Chaitman BR, Lam J, Lesperance J, Dupras G, Fines P et al.N<strong>on</strong>invasive diagnostic test choices for <strong>the</strong> evaluati<strong>on</strong> <strong>of</strong> cor<strong>on</strong>aryartery disease in women: a multivariate comparis<strong>on</strong> <strong>of</strong> cardiac fluoroscopy,exercise electrocardiography and exercise thallium myocardialperfusi<strong>on</strong> scintigraphy. J Am Coll <strong>Cardio</strong>l 1984;4:8–16.142. Diam<strong>on</strong>d GA, Forrester JS. Analysis <strong>of</strong> probability as an aid in <strong>the</strong> clinicaldiagnosis <strong>of</strong> cor<strong>on</strong>ary-artery disease. N Engl J Med 1979;300:1350–1358.143. Lauer MS. Exercise electrocardiogram testing and prognosis. Novelmarkers and predictive instruments. <strong>Cardio</strong>l Clin 2001;19:401–414.144. Elamin MS, Boyle R, Kardash MM, Smith DR, Stoker JB, Whitaker W et al.Accurate detecti<strong>on</strong> <strong>of</strong> cor<strong>on</strong>ary heart disease by new exercise test. BrHeart J 1982;48:311–320.145. Okin PM, Grandits G, Rautaharju PM, Prineas RJ, Cohen JD, Crow RSet al. Prognostic value <strong>of</strong> heart rate adjustment <strong>of</strong> exercise-inducedST segment depressi<strong>on</strong> in <strong>the</strong> multiple risk factor interventi<strong>on</strong> trial. JAm Coll <strong>Cardio</strong>l 1996;27:1437–1443.146. Froelicher VF, Lehmann KG, Thomas R, Goldman S, Morris<strong>on</strong> D, Eds<strong>on</strong> Ret al. The electrocardiographic exercise test in a populati<strong>on</strong> withreduced workup bias: diagnostic performance, computerized interpretati<strong>on</strong>,and multivariable predicti<strong>on</strong>. Veterans Affairs Cooperative Studyin Health Services #016 (QUEXTA) Study Group. Quantitative ExerciseTesting and Angiography. Ann Intern Med 1998;128:965–974.147. Yamada H, Do D, Morise A, Atwood JE, Froelicher V. Review <strong>of</strong> studiesusing multivariable analysis <strong>of</strong> clinical and exercise test data topredict angiographic cor<strong>on</strong>ary artery disease. Prog <strong>Cardio</strong>vasc Dis1997;39:457–481.148. Stuart RJ Jr, Ellestad MH. Nati<strong>on</strong>al survey <strong>of</strong> exercise stress testingfacilities. Chest 1980;77:94–97.149. Jette M, Sidney K, Blumchen G. Metabolic equivalents (METS) in exercisetesting, exercise prescripti<strong>on</strong>, and evaluati<strong>on</strong> <strong>of</strong> functi<strong>on</strong>alcapacity. Clin <strong>Cardio</strong>l 1990;13:555–565.150. Recommendati<strong>on</strong>s by <strong>the</strong> Working Group <strong>on</strong> Rehabilitati<strong>on</strong> <strong>of</strong> <strong>the</strong>European Society <strong>of</strong> <strong>Cardio</strong>logy. L<strong>on</strong>g-term comprehensive care <strong>of</strong>cardiac patients. Eur Heart J 1992;13(Suppl. C):1–45.151. Borg G, Holmgren A, Lindblad I. Quantitative evaluati<strong>on</strong> <strong>of</strong> chest pain.Acta Med Scand Suppl 1981;644:43–45.152. Mark DB, Shaw L, Harrell FE Jr, Hlatky MA, Lee KL, Bengts<strong>on</strong> JR et al.Prognostic value <strong>of</strong> a treadmill exercise score in outpatients withsuspected cor<strong>on</strong>ary artery disease. N Engl J Med 1991;325:849–853.
ESC <str<strong>on</strong>g>Guidelines</str<strong>on</strong>g> 51153. Ciar<strong>on</strong>i S, Bloch A, H<strong>of</strong>fmann JL, Bett<strong>on</strong>i M, Fournet D. Prognostic value<strong>of</strong> dobutamine echocardiography in patients with intermediate cor<strong>on</strong>arylesi<strong>on</strong>s at angiography. Echocardiography 2002;19:549–553.154. Davidavicius G, Kowalski M, Williams RI, D’Hooge J, Di Salvo G,Pierre-Justin G et al. Can regi<strong>on</strong>al strain and strain rate measurementbe performed during both dobutamine and exercise echocardiography,and do regi<strong>on</strong>al deformati<strong>on</strong> resp<strong>on</strong>ses differ with different forms <strong>of</strong>stress testing? J Am Soc Echocardiogr 2003;16:299–308.155. Cheitlin MD, Alpert JS, Armstr<strong>on</strong>g WF, Aurigemma GP, Beller GA,Bierman FZ et al. ACC/AHA guidelines for <strong>the</strong> clinical applicati<strong>on</strong> <strong>of</strong>echocardiography: executive summary. A report <strong>of</strong> <strong>the</strong> AmericanCollege <strong>of</strong> <strong>Cardio</strong>logy/American Heart Associati<strong>on</strong> Task Force <strong>on</strong>practice guidelines (Committee <strong>on</strong> Clinical Applicati<strong>on</strong> <strong>of</strong>Echocardiography). Developed in collaborati<strong>on</strong> with <strong>the</strong> AmericanSociety <strong>of</strong> Echocardiography. J Am Coll <strong>Cardio</strong>l 1997;29:862–879.156. Marwick TH. Current status <strong>of</strong> stress echocardiography for diagnosis andprognostic assessment <strong>of</strong> cor<strong>on</strong>ary artery disease. Cor<strong>on</strong> Artery Dis1998;9:411–426.157. Gibb<strong>on</strong>s RJ, Chatterjee K, Daley J, Douglas JS, Fihn SD, Gardin JM et al.ACC/AHA/ACP-ASIM guidelines for <strong>the</strong> management <strong>of</strong> patients withchr<strong>on</strong>ic stable angina: a report <strong>of</strong> <strong>the</strong> American College <strong>of</strong><strong>Cardio</strong>logy/American Heart Associati<strong>on</strong> Task Force <strong>on</strong> Practice<str<strong>on</strong>g>Guidelines</str<strong>on</strong>g> (Committee <strong>on</strong> <strong>Management</strong> <strong>of</strong> Patients With Chr<strong>on</strong>ic<strong>Stable</strong> <strong>Angina</strong>). J Am Coll <strong>Cardio</strong>l 1999;33:2092–2197.158. Schinkel AF, Bax JJ, Geleijnse ML, Boersma E, Elhendy A, Roelandt JRet al. N<strong>on</strong>invasive evaluati<strong>on</strong> <strong>of</strong> ischaemic heart disease: myocardialperfusi<strong>on</strong> imaging or stress echocardiography? Eur Heart J2003;24:789–800.159. Korosoglou G, Labadze N, Hansen A, Selter C, Giannitsis E, Katus H et al.Usefulness <strong>of</strong> real-time myocardial perfusi<strong>on</strong> imaging in <strong>the</strong> evaluati<strong>on</strong><strong>of</strong> patients with first time chest pain. Am J <strong>Cardio</strong>l 2004;94:1225–1231.160. Rocchi G, Fallani F, Bracchetti G, Rapezzi C, Ferlito M, Levorato M et al.N<strong>on</strong>-invasive detecti<strong>on</strong> <strong>of</strong> cor<strong>on</strong>ary artery stenosis: a comparis<strong>on</strong> am<strong>on</strong>gpower-Doppler c<strong>on</strong>trast echo, 99Tc-Sestamibi SPECT and echo wallmoti<strong>on</strong>analysis. Cor<strong>on</strong> Artery Dis 2003;14:239–245.161. Moir S, Marwick TH. Combinati<strong>on</strong> <strong>of</strong> c<strong>on</strong>trast with stress echocardiography:a practical guide to methods and interpretati<strong>on</strong>. <strong>Cardio</strong>vascUltrasound 2004;2:15.162. Cain P, Baglin T, Case C, Spicer D, Short L, Marwick TH. Applicati<strong>on</strong> <strong>of</strong>tissue Doppler to interpretati<strong>on</strong> <strong>of</strong> dobutamine echocardiography andcomparis<strong>on</strong> with quantitative cor<strong>on</strong>ary angiography. Am J <strong>Cardio</strong>l2001;87:525–531.163. Cain P, Marwick TH, Case C, Baglin T, Dart J, Short L et al. Assessment <strong>of</strong>regi<strong>on</strong>al l<strong>on</strong>g-axis functi<strong>on</strong> during dobutamine echocardiography. ClinSci (L<strong>on</strong>d) 2001;100:423–432.164. Voigt JU, Exner B, Schmiedehausen K, Huchzermeyer C, Reulbach U,Nixdorff U et al. Strain-rate imaging during dobutamine stress echocardiographyprovides objective evidence <strong>of</strong> inducible ischemia.Circulati<strong>on</strong> 2003;107:2120–2126.165. Yip G, Abraham T, Belohlavek M, Khandheria BK. Clinical applicati<strong>on</strong>s <strong>of</strong>strain rate imaging. J Am Soc Echocardiogr 2003;16:1334–1342.166. Madler CF, Payne N, Wilkensh<strong>of</strong>f U, Cohen A, Derumeaux GA, Pierard LAet al. N<strong>on</strong>-invasive diagnosis <strong>of</strong> cor<strong>on</strong>ary artery disease by quantitativestress echocardiography: optimal diagnostic models using <strong>of</strong>f-line tissueDoppler in <strong>the</strong> MYDISE study. Eur Heart J 2003;24:1584–1594.167. Yip G, Khandheria B, Belohlavek M, Pislaru C, Seward J, Bailey K et al.Strain echocardiography tracks dobutamine-induced decrease inregi<strong>on</strong>al myocardial perfusi<strong>on</strong> in n<strong>on</strong>occlusive cor<strong>on</strong>ary stenosis. JAmColl <strong>Cardio</strong>l 2004;44:1664–1671.168. Marwick TH, Case C, Leano R, Short L, Baglin T, Cain P et al. Use<strong>of</strong>tissue Doppler imaging to facilitate <strong>the</strong> predicti<strong>on</strong> <strong>of</strong> events in patientswith abnormal left ventricular functi<strong>on</strong> by dobutamine echocardiography.Am J <strong>Cardio</strong>l 2004;93:142–146.169. Zaret BL, Wackers FJ. Nuclear cardiology (1). N Engl J Med 1993;329:775–783.170. Zaret BL, Wackers FJ. Nuclear cardiology (2). N Engl J Med 1993;329:855–863.171. Ritchie JL, Bateman TM, B<strong>on</strong>ow RO, Crawford MH, Gibb<strong>on</strong>s RJ, Hall RJet al. <str<strong>on</strong>g>Guidelines</str<strong>on</strong>g> for clinical use <strong>of</strong> cardiac radi<strong>on</strong>uclide imaging.Report <strong>of</strong> <strong>the</strong> American College <strong>of</strong> <strong>Cardio</strong>logy/American HeartAssociati<strong>on</strong> Task Force <strong>on</strong> Assessment <strong>of</strong> Diagnostic and Therapeutic<strong>Cardio</strong>vascular Procedures (Committee <strong>on</strong> Radi<strong>on</strong>uclide Imaging), developedin collaborati<strong>on</strong> with <strong>the</strong> American Society <strong>of</strong> Nuclear <strong>Cardio</strong>logy. JAm Coll <strong>Cardio</strong>l 1995;25:521–547.172. Daou D, Delahaye N, Lebtahi R, Vilain D, Peker C, Faraggi M et al.Diagnosis <strong>of</strong> extensive cor<strong>on</strong>ary artery disease: intrinsic value <strong>of</strong>increased lung 201 T1 uptake with exercise SPECT. J Nucl Med2000;41:567–574.173. Morel O, Pezard P, Furber A, Le Jeune JJ, Vielle B, Denizot B et al.Thallium-201 right lung/heart ratio during exercise in patients with cor<strong>on</strong>aryartery disease: relati<strong>on</strong> to thallium-201 myocardial single-phot<strong>on</strong>emissi<strong>on</strong> tomography, rest and exercise left ventricular functi<strong>on</strong> andcor<strong>on</strong>ary angiography. Eur J Nucl Med 1999;26:640–646.174. Underwood SR, Anagnostopoulos C, Cerqueira M, Ell PJ, Flint EJ,Harbins<strong>on</strong> M et al. Myocardial perfusi<strong>on</strong> scintigraphy: <strong>the</strong> evidence.Eur J Nucl Med Mol Imaging 2004;31:261–291.175. Lette J, Tatum JL, Fraser S, Miller DD, Waters DD, Heller G et al. Safety<strong>of</strong> dipyridamole testing in 73,806 patients: <strong>the</strong> MulticenterDipyridamole Safety Study. J Nucl <strong>Cardio</strong>l 1995;2:3–17.176. Cortigiani L, Picano E, Coletta C, Chiarella F, Mathias W, Gandolfo Net al. Safety, feasibility, and prognostic implicati<strong>on</strong>s <strong>of</strong> pharmacologicstress echocardiography in 1482 patients evaluated in an ambulatorysetting. Am Heart J 2001;141:621–629.177. Secknus MA, Marwick TH. Evoluti<strong>on</strong> <strong>of</strong> dobutamine echocardiographyprotocols and indicati<strong>on</strong>s: safety and side effects in 3,011 studies over5 years. J Am Coll <strong>Cardio</strong>l 1997;29:1234–1240.178. Wu JC, Yun JJ, Heller EN, Di<strong>on</strong>e DP, DeMan P, Liu YH et al. Limitati<strong>on</strong>s <strong>of</strong>dobutamine for enhancing flow heterogeneity in <strong>the</strong> presence <strong>of</strong> singlecor<strong>on</strong>ary stenosis: implicati<strong>on</strong>s for technetium-99m-sestamibi imaging.J Nucl Med 1998;39:417–425.179. Vigna C, Stanislao M, De Rito V, Russo A, Natali R, Santoro T et al.Dipyridamole stress echocardiography vs. dipyridamole sestamibi scintigraphyfor diagnosing cor<strong>on</strong>ary artery disease in left bundle-branchblock. Chest 2001;120:1534–1539.180. Ciar<strong>on</strong>i S, Bloch A, Albrecht L, Vanautryve B. Diagnosis <strong>of</strong> cor<strong>on</strong>aryartery disease in patients with permanent cardiac pacemaker by dobutaminestress echocardiography or exercise thallium-201 myocardialtomography. Echocardiography 2000;17:675–679.181. Alexanders<strong>on</strong> E, Mannting F, Gomez-Martin D, Ferm<strong>on</strong> S, Meave A.Technetium-99m-Sestamibi SPECT myocardial perfusi<strong>on</strong> imaging inpatients with complete left bundle branch block. Arch Med Res2004;35:150–156.182. Mairesse GH, Marwick TH, Arnese M, Vanoverschelde JL, Cornel JH,Detry JM et al. Improved identificati<strong>on</strong> <strong>of</strong> cor<strong>on</strong>ary artery disease inpatients with left bundle branch block by use <strong>of</strong> dobutamine stressechocardiography and comparis<strong>on</strong> with myocardial perfusi<strong>on</strong> tomography.Am J <strong>Cardio</strong>l 1995;76:321–325.183. Feola M, Biggi A, Ribichini F, Camuzzini G, Uslenghi E. The diagnosis <strong>of</strong>cor<strong>on</strong>ary artery disease in hypertensive patients with chest pain andcomplete left bundle branch block: utility <strong>of</strong> adenosine Tc-99m tetr<strong>of</strong>osminSPECT. Clin Nucl Med 2002;27:510–515.184. Geleijnse ML, Vigna C, Kasprzak JD, Rambaldi R, Salvatori MP, Elhendy Aet al. Usefulness and limitati<strong>on</strong>s <strong>of</strong> dobutamine-atropine stress echocardiographyfor <strong>the</strong> diagnosis <strong>of</strong> cor<strong>on</strong>ary artery disease in patients withleft bundle branch block. A multicentre study. Eur Heart J2000;21:1666–1673.185. Vigna C, Stanislao M, De Rito V, Russo A, Santoro T, Fusilli S et al.Inaccuracy <strong>of</strong> dipyridamole echocardiography or scintigraphy for <strong>the</strong>diagnosis <strong>of</strong> cor<strong>on</strong>ary artery disease in patients with both left bundlebranch block and left ventricular dysfuncti<strong>on</strong>. Int J <strong>Cardio</strong>l 2005;doi:10.1016/j.ijcard.2005.05.068 [Epub ahead <strong>of</strong> print July 4, 2005].186. Cortigiani L, Picano E, Vigna C, Lattanzi F, Coletta C, Mariotti E et al.Prognostic value <strong>of</strong> pharmacologic stress echocardiography in patientswith left bundle branch block. Am J Med 2001;110:361–369.187. Underwood SR, Godman B, Salyani S, Ogle JR, Ell PJ. Ec<strong>on</strong>omics <strong>of</strong> myocardialperfusi<strong>on</strong> imaging in Europe–<strong>the</strong> EMPIRE Study. Eur Heart J1999;20:157–166.188. Maddahi J, Iskandrian AE. Cost-effectiveness <strong>of</strong> nuclear cardiology.J Nucl <strong>Cardio</strong>l 1997;4:S139–S140.189. Cerqueira MD. Diagnostic testing strategies for cor<strong>on</strong>ary artery disease:special issues related to gender. Am J <strong>Cardio</strong>l 1995;75:52D–60D.190. Hachamovitch R, Berman DS, Kiat H, Bairey CN, Cohen I, Cabico A et al.Effective risk stratificati<strong>on</strong> using exercise myocardial perfusi<strong>on</strong> SPECT inwomen: gender-related differences in prognostic nuclear testing. JAmColl <strong>Cardio</strong>l 1996;28:34–44.191. Marwick TH, Shaw LJ, Lauer MS, Kesler K, Hachamovitch R, Heller GVet al. The n<strong>on</strong>invasive predicti<strong>on</strong> <strong>of</strong> cardiac mortality in men andwomen with known or suspected cor<strong>on</strong>ary artery disease. Ec<strong>on</strong>omics <strong>of</strong>N<strong>on</strong>invasive Diagnosis (END) Study Group. Am J Med 1999;106:172–178.
52 ESC <str<strong>on</strong>g>Guidelines</str<strong>on</strong>g>192. Shaw LJ, Hachamovitch R, Redberg RF. Current evidence <strong>on</strong> diagnostictesting in women with suspected cor<strong>on</strong>ary artery disease: choosing<strong>the</strong> appropriate test. <strong>Cardio</strong>l Rev 2000;8:65–74.193. Elhendy A, van Domburg RT, Bax JJ, Nierop PR, Valkema R, Geleijnse MLet al. Dobutamine-atropine stress myocardial perfusi<strong>on</strong> SPECT imagingin <strong>the</strong> diagnosis <strong>of</strong> graft stenosis after cor<strong>on</strong>ary artery bypass grafting.J Nucl <strong>Cardio</strong>l 1998;5:491–497.194. Lakkis NM, Mahmarian JJ, Verani MS. Exercise thallium-201 singlephot<strong>on</strong> emissi<strong>on</strong> computed tomography for evaluati<strong>on</strong> <strong>of</strong> cor<strong>on</strong>aryartery bypass graft patency. Am J <strong>Cardio</strong>l 1995;76:107–111.195. Shapira I, Heller I, Kornizky Y, Topilsky M, Isakov A. The value <strong>of</strong> stressthallium-201 single phot<strong>on</strong> emissi<strong>on</strong> CT imaging as a predictor <strong>of</strong>outcome and l<strong>on</strong>g-term prognosis after CABG. J Med 2001;32:271–282.196. Lauer MS, Lytle B, Pashkow F, Snader CE, Marwick TH. Predicti<strong>on</strong> <strong>of</strong>death and myocardial infarcti<strong>on</strong> by screening with exercise-thalliumtesting after cor<strong>on</strong>ary-artery-bypass grafting. Lancet 1998;351:615–622.197. Marwick TH, Zuchowski C, Lauer MS, Secknus MA, Williams J, Lytle BW.Functi<strong>on</strong>al status and quality <strong>of</strong> life in patients with heart failure undergoingcor<strong>on</strong>ary bypass surgery after assessment <strong>of</strong> myocardial viability.J Am Coll <strong>Cardio</strong>l 1999;33:750–758.198. Di Carli MF, Maddahi J, Rokhsar S, Schelbert HR, Bianco-Batlles D,Brunken RC et al. L<strong>on</strong>g-term survival <strong>of</strong> patients with cor<strong>on</strong>ary arterydisease and left ventricular dysfuncti<strong>on</strong>: implicati<strong>on</strong>s for <strong>the</strong> role <strong>of</strong>myocardial viability assessment in management decisi<strong>on</strong>s. J Thorac<strong>Cardio</strong>vasc Surg 1998;116:997–1004.199. Underwood SR, Bax JJ, vom Dahl J, Henein MY, Knuuti J, van Rossum ACet al. Imaging techniques for <strong>the</strong> assessment <strong>of</strong> myocardial hibernati<strong>on</strong>.Report <strong>of</strong> a Study Group <strong>of</strong> <strong>the</strong> European Society <strong>of</strong> <strong>Cardio</strong>logy. EurHeart J 2004;25:815–836.200. EL Nagel, Bocksch HB, Klein W, Vogel C, Frantz U, Ellmer E, Dreysse A,Fleck ES. N<strong>on</strong>invasive diagnosis <strong>of</strong> ischemia induced wall moti<strong>on</strong>abnormalities with <strong>the</strong> use <strong>of</strong> high dose dobutamine stress MRI.Comparis<strong>on</strong> with dobutamine stress echocardiography. Circulati<strong>on</strong>1999;99:763–770.201. Hundley WG, Hamilt<strong>on</strong> CA, Clarke GD, Hillis LD, Herringt<strong>on</strong> DM, Lange RAet al. Visualizati<strong>on</strong> and functi<strong>on</strong>al assessment <strong>of</strong> proximal and middleleft anterior descending cor<strong>on</strong>ary stenoses in humans with magneticres<strong>on</strong>ance imaging. Circulati<strong>on</strong> 1999;99:3248–3254.202. Hundley WG, Morgan TM, Neagle CM, Hamilt<strong>on</strong> CA, Rerkpattanapipat P,Link KM. Magnetic res<strong>on</strong>ance imaging determinati<strong>on</strong> <strong>of</strong> cardiac prognosis.Circulati<strong>on</strong> 2002;106:2328–2333.203. Schwitter J, Nanz D, Kneifel S, Bertschinger K, Buchi M, Knusel PR et al.Assessment <strong>of</strong> myocardial perfusi<strong>on</strong> in cor<strong>on</strong>ary artery disease by magneticres<strong>on</strong>ance: a comparis<strong>on</strong> with positr<strong>on</strong> emissi<strong>on</strong> tomography andcor<strong>on</strong>ary angiography. Circulati<strong>on</strong> 2001;103:2230–2235.204. Ishida N, Sakuma H, Motoyasu M, Okinaka T, Isaka N, Nakano T et al.N<strong>on</strong>infarcted myocardium: correlati<strong>on</strong> between dynamic first-passc<strong>on</strong>trast-enhanced myocardial MR imaging and quantitative cor<strong>on</strong>aryangiography. Radiology 2003;229:209–216.205. Pennell DJ, Sechtem UP, Higgins CB, Manning WJ, Pohost GM,Rademakers FE et al. Clinical indicati<strong>on</strong>s for cardiovascular magneticres<strong>on</strong>ance (CMR): C<strong>on</strong>sensus Panel report. Eur Heart J 2004;25:1940–1965.206. Xu M, McHaffie DJ. N<strong>on</strong>specific systolic murmurs: an audit <strong>of</strong> <strong>the</strong> clinicalvalue <strong>of</strong> echocardiography. NZMedJ1993;106:54–56.207. Nagueh SF, Bachinski LL, Meyer D, Hill R, Zoghbi WA, Tam JW et al.Tissue Doppler imaging c<strong>on</strong>sistently detects myocardial abnormalitiesin patients with hypertrophic cardiomyopathy and provides a novelmeans for an early diagnosis before and independently <strong>of</strong> hypertrophy.Circulati<strong>on</strong> 2001;104:128–130.208. H<strong>of</strong>fmann A, Burckhardt D. Evaluati<strong>on</strong> <strong>of</strong> systolic murmurs by Dopplerultras<strong>on</strong>ography. Br Heart J 1983;50:337–342.209. Attenh<strong>of</strong>er Jost CH, Turina J, Mayer K, Seifert B, Amann FW, Buechi Met al. Echocardiography in <strong>the</strong> evaluati<strong>on</strong> <strong>of</strong> systolic murmurs <strong>of</strong>unknown cause. Am J Med 2000;108:614–620.210. Fink JC, Schmid CH, Selker HP. A decisi<strong>on</strong> aid for referring patients withsystolic murmurs for echocardiography. J Gen Intern Med 1994;9:479–484.211. McKillop GM, Stewart DA, Burns JM, Ballantyne D. Doppler echocardiographyin elderly patients with ejecti<strong>on</strong> systolic murmurs. PostgradMed J 1991;67:1059–1061.212. Rakowski H, Sass<strong>on</strong> Z, Wigle ED. Echocardiographic and Doppler assessment<strong>of</strong> hypertrophic cardiomyopathy. J Am Soc Echocardiogr1988;1:31–47.213. Shaw LJ, Peters<strong>on</strong> ED, Kesler K, Hasselblad V, Califf RM. A metaanalysis<strong>of</strong> predischarge risk stratificati<strong>on</strong> after acute myocardial infarcti<strong>on</strong> withstress electrocardiographic, myocardial perfusi<strong>on</strong>, and ventricular functi<strong>on</strong>imaging. Am J <strong>Cardio</strong>l 1996;78:1327–1337.214. Marchioli R, Avanzini F, Barzi F, Chieffo C, Di Castelnuovo A, Franzosi MGet al. Assessment <strong>of</strong> absolute risk <strong>of</strong> death after myocardial infarcti<strong>on</strong>by use <strong>of</strong> multiple-risk-factor assessment equati<strong>on</strong>s: GISSI-Prevenzi<strong>on</strong>emortality risk chart. Eur Heart J 2001;22:2085–2103.215. Echeverria HH, Bilsker MS, Myerburg RJ, Kessler KM. C<strong>on</strong>gestive heartfailure: echocardiographic insights. Am J Med 1983;75:750–755.216. Aguirre FV, Pears<strong>on</strong> AC, Lewen MK, McCluskey M, Labovitz AJ. Usefulness<strong>of</strong> Doppler echocardiography in <strong>the</strong> diagnosis <strong>of</strong> c<strong>on</strong>gestive heartfailure. Am J <strong>Cardio</strong>l 1989;63:1098–1102.217. Shah PM. Echocardiography in c<strong>on</strong>gestive or dilated cardiomyopathy.J Am Soc Echocardiogr 1988;1:20–30.218. Rihal CS, Nishimura RA, Hatle LK, Bailey KR, Tajik AJ. Systolic and diastolicdysfuncti<strong>on</strong> in patients with clinical diagnosis <strong>of</strong> dilated cardiomyopathy.Relati<strong>on</strong> to symptoms and prognosis. Circulati<strong>on</strong> 1994;90:2772–2779.219. F<strong>on</strong>seca C, Mota T, Morais H, Matias F, Costa C, Oliveira AG et al. Thevalue <strong>of</strong> <strong>the</strong> electrocardiogram and chest X-ray for c<strong>on</strong>firming or refutinga suspected diagnosis <strong>of</strong> heart failure in <strong>the</strong> community. Eur J HeartFail 2004;6:807–812.220. Vasan RS, Benjamin EJ, Levy D. Prevalence, clinical features and prognosis<strong>of</strong> diastolic heart failure: an epidemiologic perspective. J Am Coll<strong>Cardio</strong>l 1995;26:1565–1574.221. O’Mah<strong>on</strong>y MS, Sim MF, Ho SF, Steward JA, Buchalter M, Burr M. Diastolicheart failure in older people. Age Ageing 2003;32:519–524.222. Mottram PM, Marwick TH. Assessment <strong>of</strong> diastolic functi<strong>on</strong>: what <strong>the</strong>general cardiologist needs to know. Heart 2005;91:681–695.223. Zaliunas R, Jurkevicus R, Zabiela V, Brazdzi<strong>on</strong>yte J. Effect <strong>of</strong> amlodipineand lacidipine <strong>on</strong> left ventricular diastolic and l<strong>on</strong>g axis functi<strong>on</strong>s inarterial hypertensi<strong>on</strong> and stable angina pectoris. Acta <strong>Cardio</strong>l2005;60:239–246.224. Gill JB, Cairns JA, Roberts RS, Costantini L, Sealey BJ, Fallen EF et al.Prognostic importance <strong>of</strong> myocardial ischemia detected by ambulatorym<strong>on</strong>itoring early after acute myocardial infarcti<strong>on</strong>. N Engl J Med1996;334:65–70.225. Ambrose JA, Fuster V. Can we predict future acute cor<strong>on</strong>ary events inpatients with stable cor<strong>on</strong>ary artery disease? JAMA 1997;277:343–344.226. Mulcahy D, Knight C, Patel D, Curzen N, Cunningham D, Wright C et al.Detecti<strong>on</strong> <strong>of</strong> ambulatory ischaemia is not <strong>of</strong> practical clinical value in<strong>the</strong> routine management <strong>of</strong> patients with stable angina. A l<strong>on</strong>g-termfollow-up study. Eur Heart J 1995;16:317–324.227. Knez A, Becker A, Leber A, White C, Becker CR, Reiser MF et al. Relati<strong>on</strong><strong>of</strong> cor<strong>on</strong>ary calcium scores by electr<strong>on</strong> beam tomography to obstructivedisease in 2,115 symptomatic patients. Am J <strong>Cardio</strong>l 2004;93:1150–1152.228. Becker CR. N<strong>on</strong>invasive assessment <strong>of</strong> cor<strong>on</strong>ary a<strong>the</strong>rosclerosis bymultidetector-row computed tomography. Expert Rev <strong>Cardio</strong>vasc Ther2004;2:721–727.229. Stanford W, Thomps<strong>on</strong> BH, Burns TL, Heery SD, Burr MC. Cor<strong>on</strong>ary arterycalcium quantificati<strong>on</strong> at multi-detector row helical CT versuselectr<strong>on</strong>-beam CT. Radiology 2004;230:397–402.230. Nasir K, Bud<strong>of</strong>f MJ, Post WS, Fishman EK, Mahesh M, Lima JA et al.Electr<strong>on</strong> beam CT versus helical CT scans for assessing cor<strong>on</strong>ary calcificati<strong>on</strong>:current utility and future directi<strong>on</strong>s. Am Heart J2003;146:969–977.231. Agatst<strong>on</strong> AS, Janowitz WR, Hildner FJ, Zusmer NR, Viam<strong>on</strong>te M Jr,Detrano R. Quantificati<strong>on</strong> <strong>of</strong> cor<strong>on</strong>ary artery calcium using ultrafastcomputed tomography. J Am Coll <strong>Cardio</strong>l 1990;15:827–832.232. H<strong>of</strong>f JA, Chomka EV, Krainik AJ, Daviglus M, Rich S, K<strong>on</strong>dos GT. Age andgender distributi<strong>on</strong>s <strong>of</strong> cor<strong>on</strong>ary artery calcium detected by electr<strong>on</strong>beam tomography in 35,246 adults. Am J <strong>Cardio</strong>l 2001;87:1335–1339.233. Rumberger JA, Sim<strong>on</strong>s DB, Fitzpatrick LA, Sheedy PF, Schwartz RS.Cor<strong>on</strong>ary artery calcium area by electr<strong>on</strong>-beam computed tomographyand cor<strong>on</strong>ary a<strong>the</strong>rosclerotic plaque area. A histopathologic correlativestudy. Circulati<strong>on</strong> 1995;92:2157–2162.234. O’Rourke RA, Brundage BH, Froelicher VF, Greenland P, Grundy SM,Hachamovitch R et al. American College <strong>of</strong> <strong>Cardio</strong>logy/AmericanHeart Associati<strong>on</strong> Expert C<strong>on</strong>sensus Document <strong>on</strong> electr<strong>on</strong>-beam computedtomography for <strong>the</strong> diagnosis and prognosis <strong>of</strong> cor<strong>on</strong>ary arterydisease. J Am Coll <strong>Cardio</strong>l 2000;36:326–340.235. Daly C, Saravanan P, Fox K. Is calcium <strong>the</strong> clue? Eur Heart J2002;23:1562–1565.
ESC <str<strong>on</strong>g>Guidelines</str<strong>on</strong>g> 53236. de Feyter PJ, Nieman K. N<strong>on</strong>invasive multi-slice computed tomographycor<strong>on</strong>ary angiography: an emerging clinical modality. J Am Coll <strong>Cardio</strong>l2004;44:1238–1240.237. H<strong>of</strong>fmann MH, Shi H, Schmitz BL, Schmid FT, Lieberknecht M, Schulze Ret al. N<strong>on</strong>invasive cor<strong>on</strong>ary angiography with multislice computed tomography.JAMA 2005;293:2471–2478.238. Raff GL, Gallagher MJ, O’Neill WW, Goldstein JA. Diagnostic accuracy <strong>of</strong>n<strong>on</strong>invasive cor<strong>on</strong>ary angiography using 64-slice spiral computed tomography.J Am Coll <strong>Cardio</strong>l 2005;46:552–557.239. Leschka S, Alkadhi H, Plass A, Desbiolles L, Grunenfelder J, Marincek Bet al. Accuracy <strong>of</strong> MSCT cor<strong>on</strong>ary angiography with 64-slice technology:first experience. Eur Heart J 2005;26:1482–1487.240. Toussaint JF, LaMuraglia GM, Sou<strong>the</strong>rn JF, Fuster V, Kantor HL. Magneticres<strong>on</strong>ance images lipid, fibrous, calcified, hemorrhagic, and thromboticcomp<strong>on</strong>ents <strong>of</strong> human a<strong>the</strong>rosclerosis in vivo. Circulati<strong>on</strong>1996;94:932–938.241. Spaulding CM, Joly LM, Rosenberg A, M<strong>on</strong>chi M, Weber SN, Dhainaut JFet al. Immediate cor<strong>on</strong>ary angiography in survivors <strong>of</strong> out-<strong>of</strong>-hospitalcardiac arrest. N Engl J Med 1997;336:1629–1633.242. Borger van der Burg AE, Bax JJ, Boersma E, Bootsma M, van Erven L, vander Wall EE et al. Impact <strong>of</strong> percutaneous cor<strong>on</strong>ary interventi<strong>on</strong> or cor<strong>on</strong>aryartery bypass grafting <strong>on</strong> outcome after n<strong>on</strong>fatal cardiac arrestoutside <strong>the</strong> hospital. Am J <strong>Cardio</strong>l 2003;91:785–789.243. Noto TJ Jr, Johns<strong>on</strong> LW, Kr<strong>on</strong>e R, Weaver WF, Clark DA, Kramer JR Jret al. Cardiac ca<strong>the</strong>terizati<strong>on</strong> 1990: a report <strong>of</strong> <strong>the</strong> Registry <strong>of</strong> <strong>the</strong>Society for Cardiac Angiography and Interventi<strong>on</strong>s (SCA&I). Ca<strong>the</strong>ter<strong>Cardio</strong>vasc Diagn 1991;24:75–83.244. Yock PG, Linker DT, Angelsen BA. Two-dimensi<strong>on</strong>al intravascular ultrasound:technical development and initial clinical experience. J AmSoc Echocardiogr 1989;2:296–304.245. Di Mario C, Gorge G, Peters R, Kearney P, Pinto F, Hausmann D et al.Clinical applicati<strong>on</strong> and image interpretati<strong>on</strong> in intracor<strong>on</strong>ary ultrasound.Study Group <strong>on</strong> Intracor<strong>on</strong>ary Imaging <strong>of</strong> <strong>the</strong> Working Group <strong>of</strong>Cor<strong>on</strong>ary Circulati<strong>on</strong> and <strong>of</strong> <strong>the</strong> Subgroup <strong>on</strong> Intravascular Ultrasound<strong>of</strong> <strong>the</strong> Working Group <strong>of</strong> Echocardiography <strong>of</strong> <strong>the</strong> European Society <strong>of</strong><strong>Cardio</strong>logy. Eur Heart J 1998;19:207–229.246. Mintz GS, Nissen SE, Anders<strong>on</strong> WD, Bailey SR, Erbel R, Fitzgerald PJet al. American College <strong>of</strong> <strong>Cardio</strong>logy Clinical Expert C<strong>on</strong>sensusDocument <strong>on</strong> Standards for Acquisiti<strong>on</strong>, Measurement and Reporting <strong>of</strong>Intravascular Ultrasound Studies (IVUS). A report <strong>of</strong> <strong>the</strong> AmericanCollege <strong>of</strong> <strong>Cardio</strong>logy Task Force <strong>on</strong> Clinical Expert C<strong>on</strong>sensusDocuments. J Am Coll <strong>Cardio</strong>l 2001;37:1478–1492.247. Di Carli M, Czernin J, Hoh CK, Gerbaudo VH, Brunken RC, Huang SC et al.Relati<strong>on</strong> am<strong>on</strong>g stenosis severity, myocardial blood flow, and flowreserve in patients with cor<strong>on</strong>ary artery disease. Circulati<strong>on</strong>1995;91:1944–1951.248. Pijls NH, De Bruyne B, Peels K, Van Der Voort PH, B<strong>on</strong>nier HJ,Bartunek JKJJ et al. Measurement <strong>of</strong> fracti<strong>on</strong>al flow reserve to assess<strong>the</strong> functi<strong>on</strong>al severity <strong>of</strong> cor<strong>on</strong>ary-artery stenoses. N Engl J Med1996;334:1703–1708.249. Legalery P, Schiele F, Ser<strong>on</strong>de MF, Meneveau N, Wei H, Didier K et al.1 year outcome <strong>of</strong> patients submitted to routine fracti<strong>on</strong>al flowreserve assessment to determine <strong>the</strong> need for angioplasty. Eur Heart J2005;26:2623–2629.250. De Backer G, Ambrosi<strong>on</strong>i E, Borch-Johnsen K, Brot<strong>on</strong>s C, Cifkova R,Dall<strong>on</strong>geville J et al. European guidelines <strong>on</strong> cardiovascular disease preventi<strong>on</strong>in clinical practice. Third Joint Task Force <strong>of</strong> European andO<strong>the</strong>r Societies <strong>on</strong> <strong>Cardio</strong>vascular Disease Preventi<strong>on</strong> in ClinicalPractice. Eur Heart J 2003;24:1601–1610.251. Hense HW. Risk factor scoring for cor<strong>on</strong>ary heart disease. BMJ2003;327:1238–1239.252. Braunwald E, Domanski MJ, Fowler SE, Geller NL, Gersh BJ, Hsia J et al.Angiotensin-c<strong>on</strong>verting-enzyme inhibiti<strong>on</strong> in stable cor<strong>on</strong>ary arterydisease. N Engl J Med 2004;351:2058–2068.253. Heart Outcomes Preventi<strong>on</strong> Evaluati<strong>on</strong> Study Investigators. Effects <strong>of</strong>ramipril <strong>on</strong> cardiovascular and microvascular outcomes in people withdiabetes mellitus: results <strong>of</strong> <strong>the</strong> HOPE study and MICRO-HOPE substudy.Lancet 2000;355:253–259.254. Effect <strong>of</strong> nicorandil <strong>on</strong> cor<strong>on</strong>ary events in patients with stable angina:<strong>the</strong> Impact Of Nicorandil in <strong>Angina</strong> (IONA) randomised trial. Lancet2002;359:1269–1275.255. Califf RM, Mark DB, Harrell FE Jr, Hlatky MA, Lee KL, Rosati RA et al.Importance <strong>of</strong> clinical measures <strong>of</strong> ischemia in <strong>the</strong> prognosis <strong>of</strong> patientswith documented cor<strong>on</strong>ary artery disease. J Am Coll <strong>Cardio</strong>l1988;11:20–26.256. Proudfit WL, Kramer JR, Bott-Silverman C, Goormastic M. Survival <strong>of</strong>n<strong>on</strong>-surgical patients with mild angina or myocardial infarcti<strong>on</strong>without angina. Br Heart J 1986;56:213–221.257. Schlant RC, Forman S, Stamler J, Canner PL. The natural history <strong>of</strong> cor<strong>on</strong>aryheart disease: prognostic factors after recovery from myocardialinfarcti<strong>on</strong> in 2789 men. The 5-year findings <strong>of</strong> <strong>the</strong> cor<strong>on</strong>ary drug project.Circulati<strong>on</strong> 1982;66:401–414.258. Phillips AN, Shaper AG, Pocock SJ, Walker M, Macfarlane PW. The role <strong>of</strong>risk factors in heart attacks occurring in men with pre-existing ischaemicheart disease. Br Heart J 1988;60:404–410.259. Brewer HB Jr. Hypertriglyceridemia: changes in <strong>the</strong> plasma lipoproteinsassociated with an increased risk <strong>of</strong> cardiovascular disease. Am J <strong>Cardio</strong>l1999;83:3F–12F.260. Hultgren HN, Peduzzi P. Relati<strong>on</strong> <strong>of</strong> severity <strong>of</strong> symptoms to prognosis instable angina pectoris. Am J <strong>Cardio</strong>l 1984;54:988–993.261. Pryor DB, Shaw L, McCants CB, Lee KL, Mark DB, Harrell FE Jr et al.Value <strong>of</strong> <strong>the</strong> history and physical in identifying patients at increasedrisk for cor<strong>on</strong>ary artery disease. Ann Intern Med 1993;118:81–90.262. Papamichael CM, Lekakis JP, Stamatelopoulos KS, Papaioannou TG,Alevizaki MK, Cimp<strong>on</strong>eriu AT et al. Ankle-brachial index as a predictor<strong>of</strong> <strong>the</strong> extent <strong>of</strong> cor<strong>on</strong>ary a<strong>the</strong>rosclerosis and cardiovascular events inpatients with cor<strong>on</strong>ary artery disease. Am J <strong>Cardio</strong>l 2000;86:615–618.263. Eagle KA, Rihal CS, Foster ED, Mickel MC, Gersh BJ. L<strong>on</strong>g-term survivalin patients with cor<strong>on</strong>ary artery disease: importance <strong>of</strong> peripheral vasculardisease. The Cor<strong>on</strong>ary Artery Surgery Study (CASS) Investigators. JAm Coll <strong>Cardio</strong>l 1994;23:1091–1095.264. Kannel WB, Abbott RD. A prognostic comparis<strong>on</strong> <strong>of</strong> asymptomatic leftventricular hypertrophy and unrecognized myocardial infarcti<strong>on</strong>: <strong>the</strong>Framingham Study. Am Heart J 1986;111:391–397.265. Sullivan JM, Vander Zwaag RV, el-Zeky F, Ramanathan KB, Mirvis DM. Leftventricular hypertrophy: effect <strong>on</strong> survival. J Am Coll <strong>Cardio</strong>l1993;22:508–513.266. Block WJ Jr, Crumpacker EL, Dry TJ, Gage RP. Prognosis <strong>of</strong> angina pectoris;observati<strong>on</strong>s in 6,882 cases. J Am Med Assoc 1952;150:259–264.267. Biagini E, Elhendy A, Schinkel AF, Nelwan S, Rizzello V, van Domburg RTet al. Prognostic significance <strong>of</strong> left anterior hemiblock in patients withsuspected cor<strong>on</strong>ary artery disease. J Am Coll <strong>Cardio</strong>l 2005;46:858–863.268. Morris CK, Ueshima K, Kawaguchi T, Hideg A, Froelicher VF. The prognosticvalue <strong>of</strong> exercise capacity: a review <strong>of</strong> <strong>the</strong> literature. Am Heart J1991;122:1423–1431.269. Dagenais GR, Rouleau JR, Christen A, Fabia J. Survival <strong>of</strong> patients with astr<strong>on</strong>gly positive exercise electrocardiogram. Circulati<strong>on</strong> 1982;65:452–456.270. McNeer JF, Margolis JR, Lee KL, Kisslo JA, Peter RH, K<strong>on</strong>g Y et al. Therole <strong>of</strong> <strong>the</strong> exercise test in <strong>the</strong> evaluati<strong>on</strong> <strong>of</strong> patients for ischaemicheart disease. Circulati<strong>on</strong> 1978;57:64–70.271. Morrow K, Morris CK, Froelicher VF, Hideg A, Hunter D, Johns<strong>on</strong> E et al.Predicti<strong>on</strong> <strong>of</strong> cardiovascular death in men undergoing n<strong>on</strong>invasive evaluati<strong>on</strong>for cor<strong>on</strong>ary artery disease. Ann Intern Med 1993;118:689–695.272. Mark DB, Hlatky MA, Harrell FE Jr, Lee KL, Califf RM, Pryor DB. Exercisetreadmill score for predicting prognosis in cor<strong>on</strong>ary artery disease. AnnIntern Med 1987;106:793–800.273. Prakash M, Myers J, Froelicher VF, Marcus R, Do D, Kalisetti D et al.Clinicaland exercise test predictors <strong>of</strong> all-cause mortality: results from .6,000c<strong>on</strong>secutive referred male patients. Chest 2001;120:1003–1013.274. Marwick TH, Mehta R, Arheart K, Lauer MS. Use <strong>of</strong> exercise echocardiographyfor prognostic evaluati<strong>on</strong> <strong>of</strong> patients with known or suspectedcor<strong>on</strong>ary artery disease. J Am Coll <strong>Cardio</strong>l 1997;30:83–90.275. Geleijnse ML, Elhendy A, van Domburg RT, Cornel JH, Rambaldi R, SalustriA et al. Cardiac imaging for risk stratificati<strong>on</strong> with dobutamine-atropinestress testing in patients with chest pain. Echocardiography, perfusi<strong>on</strong>scintigraphy, or both? Circulati<strong>on</strong> 1997;96:137–147.276. Olmos LI, Dakik H, Gord<strong>on</strong> R, Dunn JK, Verani MS, Quin<strong>on</strong>es MA et al.L<strong>on</strong>g-term prognostic value <strong>of</strong> exercise echocardiography comparedwith exercise 201Tl, ECG, and clinical variables in patients evaluatedfor cor<strong>on</strong>ary artery disease. Circulati<strong>on</strong> 1998;98:2679–2686.277. Brown KA. Prognostic value <strong>of</strong> thallium-201 myocardial perfusi<strong>on</strong>imaging. A diagnostic tool comes <strong>of</strong> age. Circulati<strong>on</strong> 1991;83:363–381.278. Hachamovitch R, Berman DS, Shaw LJ, Kiat H, Cohen I, Cabico JA et al.Incremental prognostic value <strong>of</strong> myocardial perfusi<strong>on</strong> single phot<strong>on</strong>emissi<strong>on</strong> computed tomography for <strong>the</strong> predicti<strong>on</strong> <strong>of</strong> cardiac death:differential stratificati<strong>on</strong> for risk <strong>of</strong> cardiac death and myocardialinfarcti<strong>on</strong>. Circulati<strong>on</strong> 1998;97:535–543.279. McClellan JR, Travin MI, Herman SD, Bar<strong>on</strong> JI, Golub RJ, Gallagher JJet al. Prognostic importance <strong>of</strong> scintigraphic left ventricular cavitydilati<strong>on</strong> during intravenous dipyridamole technetium-99m sestamibi
54 ESC <str<strong>on</strong>g>Guidelines</str<strong>on</strong>g>myocardial tomographic imaging in predicting cor<strong>on</strong>ary events. Am J<strong>Cardio</strong>l 1997;79:600–605.280. Em<strong>on</strong>d M, Mock MB, Davis KB, Fisher LD, Holmes DR Jr, Chaitman BRet al. L<strong>on</strong>g-term survival <strong>of</strong> medically treated patients in <strong>the</strong>Cor<strong>on</strong>ary Artery Surgery Study (CASS) Registry. Circulati<strong>on</strong>1994;90:2645–2657.281. McD<strong>on</strong>agh TA, Morris<strong>on</strong> CE, Lawrence A, Ford I, Tunstall-Pedoe H,McMurray JJ et al. Symptomatic and asymptomatic left-ventricular systolicdysfuncti<strong>on</strong> in an urban populati<strong>on</strong>. Lancet 1997;350:829–833.282. Raym<strong>on</strong>d I, Pedersen F, Steensgaard-Hansen F, Green A, Busch-Sorensen M,Tuxen C et al. Prevalence <strong>of</strong> impaired left ventricular systolic functi<strong>on</strong> andheart failure in a middle aged and elderly urban populati<strong>on</strong> segment <strong>of</strong>Copenhagen. Heart 2003;89:1422–1429.283. Mosterd A, Hoes AW, de Bruyne MC, Deckers JW, Linker DT, H<strong>of</strong>man Aet al. Prevalence <strong>of</strong> heart failure and left ventricular dysfuncti<strong>on</strong> in<strong>the</strong> general populati<strong>on</strong>; The Rotterdam Study. Eur Heart J1999;20:447–455.284. Daly C, Norrie J, Murdoch DL, Ford I, Dargie HJ, Fox K. The value <strong>of</strong>routine n<strong>on</strong>-invasive tests to predict clinical outcome in stableangina. Eur Heart J 2003;24:532–540.285. Cuspidi C, Ambrosi<strong>on</strong>i E, Mancia G, Pessina AC, Trimarco B, Zanchetti A.Role <strong>of</strong> echocardiography and carotid ultras<strong>on</strong>ography in stratifying riskin patients with essential hypertensi<strong>on</strong>: <strong>the</strong> Assessment <strong>of</strong> PrognosticRisk Observati<strong>on</strong>al Survey. J Hypertens 2002;20:1307–1314.286. European Society <strong>of</strong> Hypertensi<strong>on</strong> and <strong>the</strong> European Society <strong>of</strong> <strong>Cardio</strong>logy.European Society <strong>of</strong> Hypertensi<strong>on</strong>–European Society <strong>of</strong> <strong>Cardio</strong>logyguidelines for <strong>the</strong> management <strong>of</strong> arterial hypertensi<strong>on</strong>. J Hypertens2003;21:1011–1053.287. European Cor<strong>on</strong>ary Surgery Study Group. L<strong>on</strong>g-term results <strong>of</strong> prospectiverandomised study <strong>of</strong> cor<strong>on</strong>ary artery bypass surgery in stable anginapectoris. Lancet 1982;2:1173–1180.288. Mark DB, Nels<strong>on</strong> CL, Califf RM, Harrell FE Jr, Lee KL, J<strong>on</strong>es RH et al.C<strong>on</strong>tinuing evoluti<strong>on</strong> <strong>of</strong> <strong>the</strong>rapy for cor<strong>on</strong>ary artery disease. Initialresults from <strong>the</strong> era <strong>of</strong> cor<strong>on</strong>ary angioplasty. Circulati<strong>on</strong>1994;89:2015–2025.289. Nakagomi A, Celermajer DS, Lumley T, Freedman SB. Angiographicseverity <strong>of</strong> cor<strong>on</strong>ary narrowing is a surrogate marker for <strong>the</strong> extent <strong>of</strong>cor<strong>on</strong>ary a<strong>the</strong>rosclerosis. Am J <strong>Cardio</strong>l 1996;78:516–519.290. Rihal CS, Raco DL, Gersh BJ, Yusuf S. Indicati<strong>on</strong>s for cor<strong>on</strong>ary arterybypass surgery and percutaneous cor<strong>on</strong>ary interventi<strong>on</strong> in chr<strong>on</strong>icstable angina: review <strong>of</strong> <strong>the</strong> evidence and methodological c<strong>on</strong>siderati<strong>on</strong>s.Circulati<strong>on</strong> 2003;108:2439–2445.291. Kennedy JW, Killip T, Fisher LD, Alderman EL, Gillespie MJ, Mock MB.The clinical spectrum <strong>of</strong> cor<strong>on</strong>ary artery disease and its surgical andmedical management, 1974–1979. The Cor<strong>on</strong>ary Artery Surgery study.Circulati<strong>on</strong> 1982;66:III16–III23.292. Kemp HG Jr. Left ventricular functi<strong>on</strong> in patients with <strong>the</strong> anginal syndromeand normal cor<strong>on</strong>ary arteriograms. Am J <strong>Cardio</strong>l1973;32:375–376.293. Cosin-Sales J, Pizzi C, Brown S, Kaski JC. C-reactive protein, clinicalpresentati<strong>on</strong>, and ischaemic activity in patients with chest pain andnormal cor<strong>on</strong>ary angiograms. J Am Coll <strong>Cardio</strong>l 2003;41:1468–1474.294. Cann<strong>on</strong> RO III, Epstein SE. ‘Microvascular angina’ as a cause <strong>of</strong> chestpain with angiographically normal cor<strong>on</strong>ary arteries. Am J <strong>Cardio</strong>l1988;61:1338–1343.295. Luscher TF. The endo<strong>the</strong>lium and cardiovascular disease–a complexrelati<strong>on</strong>. N Engl J Med 1994;330:1081–1083.296. Oki T, Tabata T, Yamada H, Wakatsuki T, Mishiro Y, Abe M et al. Left ventriculardiastolic properties <strong>of</strong> hypertensive patients measured bypulsed tissue Doppler imaging. J Am Soc Echocardiogr1998;11:1106–1112.297. Diam<strong>on</strong>d JA, Phillips RA. Hypertensive heart disease. Hypertens Res2005;28:191–202.298. Schafer S, Kelm M, Mingers S, Strauer BE. Left ventricular remodelingimpairs cor<strong>on</strong>ary flow reserve in hypertensive patients. J Hypertens2002;20:1431–1437.299. Preik M, Kelm M, Strauer BE. <strong>Management</strong> <strong>of</strong> <strong>the</strong> hypertensive patientwith cor<strong>on</strong>ary insufficiency but without a<strong>the</strong>rosclerosis. Curr Opin<strong>Cardio</strong>l 2003;18:255–259.300. Cann<strong>on</strong> RO III, Camici PG, Epstein SE. Pathophysiological dilemma <strong>of</strong>syndrome X. Circulati<strong>on</strong> 1992;85:883–892.301. Panza JA, Laurienzo JM, Curiel RV, Unger EF, Quyyumi AA, Dilsizian Vet al. Investigati<strong>on</strong> <strong>of</strong> <strong>the</strong> mechanism <strong>of</strong> chest pain in patients withangiographically normal cor<strong>on</strong>ary arteries using transesophageal dobutaminestress echocardiography. J Am Coll <strong>Cardio</strong>l 1997;29:293–301.302. Chauhan A, Mullins PA, Thuraisingham SI, Taylor G, Petch MC, Sch<strong>of</strong>ield PM.Abnormal cardiac pain percepti<strong>on</strong> in syndrome X. J Am Coll <strong>Cardio</strong>l1994;24:329–335.303. Kaski JC, Rosano GM, Collins P, Nihoyannopoulos P, Maseri A, Poole-Wils<strong>on</strong> PA. Cardiac syndrome X: clinical characteristics and left ventricularfuncti<strong>on</strong>. L<strong>on</strong>g-term follow-up study. J Am Coll <strong>Cardio</strong>l1995;25:807–814.304. Atienza F, Velasco JA, Brown S, Ridocci F, Kaski JC. Assessment <strong>of</strong> quality<strong>of</strong> life in patients with chest pain and normal cor<strong>on</strong>ary arteriogram (syndromeX) using a specific questi<strong>on</strong>naire. Clin <strong>Cardio</strong>l 1999;22:283–290.305. Bugiardini R, Bairey Merz CN. <strong>Angina</strong> with ‘normal’ cor<strong>on</strong>ary arteries: achanging philosophy. JAMA 2005;293:477–484.306. Johns<strong>on</strong> BD, Shaw LJ, Buchthal SD, Bairey Merz CN, Kim HW, Scott KNet al. Prognosis in women with myocardial ischemia in <strong>the</strong> absence <strong>of</strong>obstructive cor<strong>on</strong>ary disease: results from <strong>the</strong> Nati<strong>on</strong>al Institutes <strong>of</strong>Health-Nati<strong>on</strong>al Heart, Lung, and Blood Institute-Sp<strong>on</strong>sored Women’sIschemia Syndrome Evaluati<strong>on</strong> (WISE). Circulati<strong>on</strong> 2004;109:2993–2999.307. Bugiardini R, Manfrini O, Pizzi C, F<strong>on</strong>tana F, Morgagni G. Endo<strong>the</strong>lialfuncti<strong>on</strong> predicts future development <strong>of</strong> cor<strong>on</strong>ary artery disease: astudy <strong>of</strong> women with chest pain and normal cor<strong>on</strong>ary angiograms.Circulati<strong>on</strong> 2004;109:2518–2523.308. Halcox JP, Schenke WH, Zalos G, Mincemoyer R, Prasad A, Waclawiw MAet al. Prognostic value <strong>of</strong> cor<strong>on</strong>ary vascular endo<strong>the</strong>lial dysfuncti<strong>on</strong>.Circulati<strong>on</strong> 2002;106:653–658.309. Suwaidi JA, Hamasaki S, Higano ST, Nishimura RA, Holmes DR Jr, LermanA. L<strong>on</strong>g-term follow-up <strong>of</strong> patients with mild cor<strong>on</strong>ary artery diseaseand endo<strong>the</strong>lial dysfuncti<strong>on</strong>. Circulati<strong>on</strong> 2000;101:948–954.310. v<strong>on</strong> Mering GO, Arant CB, Wessel TR, McGorray SP, Bairey Merz CN,Sharaf BL et al. Abnormal cor<strong>on</strong>ary vasomoti<strong>on</strong> as a prognostic indicator<strong>of</strong> cardiovascular events in women: results from <strong>the</strong> Nati<strong>on</strong>al Heart,Lung, and Blood Institute-Sp<strong>on</strong>sored Women’s Ischemia SyndromeEvaluati<strong>on</strong> (WISE). Circulati<strong>on</strong> 2004;109:722–725.311. Hillis LD, Braunwald E. Cor<strong>on</strong>ary-artery spasm. N Engl J Med1978;299:695–702.312. Prinzmetal M, Kennamer R, Merliss R, Wada T, Bor N. <strong>Angina</strong>pectoris. I. A variant form <strong>of</strong> angina pectoris; preliminary report. AmJ Med 1959;27:375–388.313. Maseri A, Severi S, Nes MD, L’Abbate A, Chierchia S, Marzilli M et al.‘Variant’ angina: <strong>on</strong>e aspect <strong>of</strong> a c<strong>on</strong>tinuous spectrum <strong>of</strong> vasospasticmyocardial ischemia. Pathogenetic mechanisms, estimated incidenceand clinical and cor<strong>on</strong>ary arteriographic findings in 138 patients. Am J<strong>Cardio</strong>l 1978;42:1019–1035.314. Bugiardini R, Pozzati A, Ottani F, Morgagni GL, Puddu P. Vasot<strong>on</strong>icangina: a spectrum <strong>of</strong> ischaemic syndromes involving functi<strong>on</strong>alabnormalities <strong>of</strong> <strong>the</strong> epicardial and microvascular cor<strong>on</strong>ary circulati<strong>on</strong>.J Am Coll <strong>Cardio</strong>l 1993;22:417–425.315. Kaski JC, Crea F, Meran D, Rodriguez L, Araujo L, Chierchia S et al. Localcor<strong>on</strong>ary supersensitivity to diverse vasoc<strong>on</strong>strictive stimuli in patientswith variant angina. Circulati<strong>on</strong> 1986;74:1255–1265.316. Nakayama M, Yasue H, Yoshimura M, Shimasaki Y, Kugiyama K, Ogawa Het al. T-786–.C mutati<strong>on</strong> in <strong>the</strong> 5’-flanking regi<strong>on</strong> <strong>of</strong> <strong>the</strong> endo<strong>the</strong>lialnitric oxide synthase gene is associated with cor<strong>on</strong>ary spasm.Circulati<strong>on</strong> 1999;99:2864–2870.317. Kugiyama K, Yasue H, Okumura K, Ogawa H, Fujimoto K, Nakao K et al.Nitric oxide activity is deficient in spasm arteries <strong>of</strong> patients with cor<strong>on</strong>aryspastic angina. Circulati<strong>on</strong> 1996;94:266–271.318. Masumoto A, Mohri M, Shimokawa H, Urakami L, Usui M, Takeshita A.Suppressi<strong>on</strong> <strong>of</strong> cor<strong>on</strong>ary artery spasm by <strong>the</strong> Rho-kinase inhibitorfasudil in patients with vasospastic angina. Circulati<strong>on</strong> 2002;105:1545–1547.319. Chutkow WA, Pu J, Wheeler MT, Wada T, Makielski JC, Burant CF et al.Episodic cor<strong>on</strong>ary artery vasospasm and hypertensi<strong>on</strong> develop in <strong>the</strong>absence <strong>of</strong> Sur2 K(ATP) channels. J Clin Invest 2002;110:203–208.320. Lanza GA, De Candia E, Romagnoli E, Messano L, Sestito A, Landolfi Ret al. Increased platelet sodium-hydrogen exchanger activity in patientswith variant angina. Heart 2003;89:935–936.321. Takusagawa M, Komori S, Umetani K, Ishihara T, Sawanobori T, Kohno Iet al. Alterati<strong>on</strong>s <strong>of</strong> aut<strong>on</strong>omic nervous activity in recurrence <strong>of</strong>variant angina. Heart 1999;82:75–81.322. Lanza GA, Pedrotti P, Pasceri V, Lucente M, Crea F, Maseri A. Aut<strong>on</strong>omicchanges associated with sp<strong>on</strong>taneous cor<strong>on</strong>ary spasm in patients withvariant angina. J Am Coll <strong>Cardio</strong>l 1996;28:1249–1256.323. Luscher TF, Noll G. Is it all in <strong>the</strong> genes? Nitric oxide synthase and cor<strong>on</strong>aryvasospasm. Circulati<strong>on</strong> 1999;99:2855–2857.
ESC <str<strong>on</strong>g>Guidelines</str<strong>on</strong>g> 55324. Hermsmeyer K, Miyagawa K, Kelley ST, Rosch J, Hall AS, Ax<strong>the</strong>lm MKet al. Reactivity-based cor<strong>on</strong>ary vasospasm independent <strong>of</strong> a<strong>the</strong>rosclerosisin rhesus m<strong>on</strong>keys. J Am Coll <strong>Cardio</strong>l 1997;29:671–680.325. Minshall RD, Stanczyk FZ, Miyagawa K, Uchida B, Ax<strong>the</strong>lm M, Novy Met al. Ovarian steroid protecti<strong>on</strong> against cor<strong>on</strong>ary artery hyperreactivityin rhesus m<strong>on</strong>keys. J Clin Endocrinol Metab 1998;83:649–659.326. MacAlpin RN. Cardiac arrest and sudden unexpected death in variantangina: complicati<strong>on</strong>s <strong>of</strong> cor<strong>on</strong>ary spasm that can occur in <strong>the</strong>absence <strong>of</strong> severe organic cor<strong>on</strong>ary stenosis. Am Heart J1993;125:1011–1017.327. Yamagishi M, Ito K, Tsutsui H, Miyazaki S, Goto Y, Nagaya N et al. Lesi<strong>on</strong>severity and hypercholesterolemia determine l<strong>on</strong>g-term prognosis <strong>of</strong>vasospastic angina treated with calcium channel antag<strong>on</strong>ists. Circ J2003;67:1029–1035.328. Bory M, Pierr<strong>on</strong> F, Panagides D, B<strong>on</strong>net JL, Yvorra S, Desfossez L.Cor<strong>on</strong>ary artery spasm in patients with normal or near normal cor<strong>on</strong>aryarteries. L<strong>on</strong>g-term follow-up <strong>of</strong> 277 patients. Eur Heart J1996;17:1015–1021.329. Nakamura M, Takeshita A, Nose Y. Clinical characteristics associatedwith myocardial infarcti<strong>on</strong>, arrhythmias, and sudden death in patientswith vasospastic angina. Circulati<strong>on</strong> 1987;75:1110–1116.330. Walling A, Waters DD, Miller DD, Roy D, Pelletier GB, TherouxP. L<strong>on</strong>g-term prognosis <strong>of</strong> patients with variant angina. Circulati<strong>on</strong>1987;76:990–997.331. Yasue H, Takizawa A, Nagao M, Nishida S, Horie M, Kubota J et al. L<strong>on</strong>gtermprognosis for patients with variant angina and influential factors.Circulati<strong>on</strong> 1988;78:1–9.332. Mark DB, Califf RM, Morris KG, Harrell FE Jr, Pryor DB, Hlatky MA et al.Clinical characteristics and l<strong>on</strong>g-term survival <strong>of</strong> patients with variantangina. Circulati<strong>on</strong> 1984;69:880–888.333. Matsubara T, Tamura Y, Yamazoe M, Hori T, K<strong>on</strong>no T, Ida T et al.Correlati<strong>on</strong> between arteriographic and electrocardiographic featuresduring spasm in <strong>the</strong> left anterior descending cor<strong>on</strong>ary artery. Cor<strong>on</strong>Artery Dis 1997;8:525–535.334. Koh KK, Mo<strong>on</strong> TH, S<strong>on</strong>g JH, Park GS, Lee KH, Cho SK et al. Comparis<strong>on</strong> <strong>of</strong>clinical and laboratory findings between patients with diffuse threevesselcor<strong>on</strong>ary artery spasm and o<strong>the</strong>r types <strong>of</strong> cor<strong>on</strong>ary arteryspasm. Ca<strong>the</strong>ter <strong>Cardio</strong>vasc Diagn 1996;37:132–139.335. Sueda S, Kohno H, Fukuda H, Inoue K, Suzuki J, Watanabe K et al.Clinical and angiographical characteristics <strong>of</strong> acetylcholine- inducedspasm: relati<strong>on</strong>ship to dose <strong>of</strong> intracor<strong>on</strong>ary injecti<strong>on</strong> <strong>of</strong> acetylcholine.Cor<strong>on</strong> Artery Dis 2002;13:231–236.336. Onaka H, Hirota Y, Shimada S, Kita Y, Sakai Y, Kawakami Y et al. Clinicalobservati<strong>on</strong> <strong>of</strong> sp<strong>on</strong>taneous anginal attacks and multivessel spasm invariant angina pectoris with normal cor<strong>on</strong>ary arteries: evaluati<strong>on</strong> by24-hour 12-lead electrocardiography with computer analysis. J AmColl <strong>Cardio</strong>l 1996;27:38–44.337. Bertrand ME, Lablanche JM, Tilmant PY. Use <strong>of</strong> provocative testing inangina pectoris. Herz 1980;5:65–71.338. Sueda S, Saeki H, Otani T, Ochi N, Kukita H, Kawada H et al.Investigati<strong>on</strong> <strong>of</strong> <strong>the</strong> most effective provocati<strong>on</strong> test for patients withcor<strong>on</strong>ary spastic angina: usefulness <strong>of</strong> accelerated exercise followinghyperventilati<strong>on</strong>. Jpn Circ J 1999;63:85–90.339. Yasue H, Horio Y, Nakamura N, Fujii H, Imoto N, S<strong>on</strong>oda R et al.Inducti<strong>on</strong> <strong>of</strong> cor<strong>on</strong>ary artery spasm by acetylcholine in patients withvariant angina: possible role <strong>of</strong> <strong>the</strong> parasympa<strong>the</strong>tic nervous system in<strong>the</strong> pathogenesis <strong>of</strong> cor<strong>on</strong>ary artery spasm. Circulati<strong>on</strong>1986;74:955–963.340. Sueda S, Kohno H, Fukuda H, Watanabe K, Ochi N, Kawada H et al.Limitati<strong>on</strong>s <strong>of</strong> medical <strong>the</strong>rapy in patients with pure cor<strong>on</strong>ary spasticangina. Chest 2003;123:380–386.341. Sueda S, Kohno H, Fukuda H, Ochi N, Kawada H, Hayashi Y et al.Frequency <strong>of</strong> provoked cor<strong>on</strong>ary spasms in patients undergoing cor<strong>on</strong>aryarteriography using a spasm provocati<strong>on</strong> test via intracor<strong>on</strong>ary administrati<strong>on</strong><strong>of</strong> erg<strong>on</strong>ovine. Angiology 2004;55:403–411.342. Maseri A, Davies G, Hackett D, Kaski JC. Cor<strong>on</strong>ary artery spasm andvasoc<strong>on</strong>stricti<strong>on</strong>. The case for a distincti<strong>on</strong>. Circulati<strong>on</strong> 1990;81:1983–1991.343. Mohri M, Koyanagi M, Egashira K, Tagawa H, Ichiki T, Shimokawa H et al.<strong>Angina</strong> pectoris caused by cor<strong>on</strong>ary microvascular spasm. Lancet1998;351:1165–1169.344. Pristipino C, Beltrame JF, Finocchiaro ML, Hattori R, Fujita M, M<strong>on</strong>giardoR et al. Major racial differences in cor<strong>on</strong>ary c<strong>on</strong>strictor resp<strong>on</strong>sebetween japanese and caucasians with recent myocardial infarcti<strong>on</strong>.Circulati<strong>on</strong> 2000;101:1102–1108.345. Sueda S, Saeki H, Otani T, Mineoi K, K<strong>on</strong>dou T, Yano K et al. Majorcomplicati<strong>on</strong>s during spasm provocati<strong>on</strong> tests with an intracor<strong>on</strong>aryinjecti<strong>on</strong> <strong>of</strong> acetylcholine. Am J <strong>Cardio</strong>l 2000;85:391–394. A10.346. S<strong>on</strong>g JK, Park SW, Kim JJ, Doo YC, Kim WH, Park SJ et al. Values <strong>of</strong> intravenouserg<strong>on</strong>ovine test with two-dimensi<strong>on</strong>al echocardiography fordiagnosis <strong>of</strong> cor<strong>on</strong>ary artery spasm. J Am Soc Echocardiogr1994;7:607–615.347. Morales MA, Lombardi M, Distante A, Carpeggiani C, Reisenh<strong>of</strong>er B,L’Abbate A. Erg<strong>on</strong>ovine-echo test to assess <strong>the</strong> significance <strong>of</strong> chestpain at rest without ECG changes. Eur Heart J 1995;16:1361–1366.348. Buxt<strong>on</strong> A, Goldberg S, Hirshfeld JW, Wils<strong>on</strong> J, Mann T, Williams DO et al.Refractory erg<strong>on</strong>ovine-induced cor<strong>on</strong>ary vasospasm: importance <strong>of</strong>intracor<strong>on</strong>ary nitroglycerin. Am J <strong>Cardio</strong>l 1980;46:329–334.349. Mosca L, Appel LJ, Benjamin EJ, Berra K, Chandra-Strobos N, Fabunmi RPet al. Evidence-based guidelines for cardiovascular disease preventi<strong>on</strong> inwomen. Circulati<strong>on</strong> 2004;109:672–693.350. Bartecchi CE, MacKenzie TD, Schrier RW. The human costs <strong>of</strong> tobaccouse (1). N Engl J Med 1994;330:907–912.351. MacKenzie TD, Bartecchi CE, Schrier RW. The human costs <strong>of</strong> tobaccouse (2). N Engl J Med 1994;330:975–980.352. Benowitz NL, Gourlay SG. <strong>Cardio</strong>vascular toxicity <strong>of</strong> nicotine: implicati<strong>on</strong>sfor nicotine replacement <strong>the</strong>rapy. J Am Coll <strong>Cardio</strong>l1997;29:1422–1431.353. Tziv<strong>on</strong>i D, Keren A, Meyler S, Khoury Z, Lerer T, Brunel P. <strong>Cardio</strong>vascularsafety <strong>of</strong> transdermal nicotine patches in patients with cor<strong>on</strong>ary arterydisease who try to quit smoking. <strong>Cardio</strong>vasc Drugs Ther 1998;12:239–244.354. Working Group for <strong>the</strong> Study <strong>of</strong> Transdermal Nicotine in Patients withCor<strong>on</strong>ary artery disease. Nicotine replacement <strong>the</strong>rapy for patientswith cor<strong>on</strong>ary artery disease. Arch Intern Med 1994;154:989–995.355. Critchley J, Capewell S. Smoking cessati<strong>on</strong> for <strong>the</strong> sec<strong>on</strong>dary preventi<strong>on</strong><strong>of</strong> cor<strong>on</strong>ary heart disease. Cochrane Database Syst Rev 2003, Issue 4.Art. No.: CD003041, doi: 10.1002/14651858.CD003041.pub2.356. Smith GD, Shipley MJ, Marmot MG, Rose G. Plasma cholesterol c<strong>on</strong>centrati<strong>on</strong>and mortality. The Whitehall Study. JAMA 1992;267:70–76.357. Doll R, Peto R, Hall E, Wheatley K, Gray R. Alcohol and cor<strong>on</strong>ary heartdisease reducti<strong>on</strong> am<strong>on</strong>g British doctors: c<strong>on</strong>founding or causality?Eur Heart J 1997;18:23–25.358. Di Castelnuovo A, Rot<strong>on</strong>do S, Iacoviello L, D<strong>on</strong>ati MB, De Gaetano G.Meta-analysis <strong>of</strong> wine and beer c<strong>on</strong>sumpti<strong>on</strong> in relati<strong>on</strong> to vascularrisk. Circulati<strong>on</strong> 2002;105:2836–2844.359. Sesso HD, Stampfer MJ, Rosner B, Hennekens CH, Mans<strong>on</strong> JE, Gaziano JM.7 year changes in alcohol c<strong>on</strong>sumpti<strong>on</strong> and subsequent risk <strong>of</strong> cardiovasculardisease in men. Arch Intern Med 2000;160:2605–2612.360. Goldberg IJ, Mosca L, Piano MR, Fisher EA. AHA Science Advisory: Wineand your heart: a science advisory for healthcare pr<strong>of</strong>essi<strong>on</strong>als from <strong>the</strong>Nutriti<strong>on</strong> Committee, Council <strong>on</strong> Epidemiology and Preventi<strong>on</strong>, andCouncil <strong>on</strong> <strong>Cardio</strong>vascular Nursing <strong>of</strong> <strong>the</strong> American Heart Associati<strong>on</strong>.Circulati<strong>on</strong> 2001;103:472–475.361. Gruppo Italiano per lo Studio della Sopravvivenza nell’Infarto miocardico.Dietary supplementati<strong>on</strong> with n-3 polyunsaturated fatty acidsand vitamin E after myocardial infarcti<strong>on</strong>: results <strong>of</strong> <strong>the</strong> GISSI-Prevenzi<strong>on</strong>e trial. Lancet 1999;354:447–455.362. Marchioli R, Barzi F, Bomba E, Chieffo C, Di Gregorio D, Di Mascio R et al.Early protecti<strong>on</strong> against sudden death by n-3 polyunsaturated fattyacids after myocardial infarcti<strong>on</strong>: time-course analysis <strong>of</strong> <strong>the</strong> results<strong>of</strong> <strong>the</strong> Gruppo Italiano per lo Studio della Sopravvivenza nell’InfartoMiocardico (GISSI)-Prevenzi<strong>on</strong>e. Circulati<strong>on</strong> 2002;105:1897–1903.363. Bucher HC, Hengstler P, Schindler C, Meier G. N-3 polyunsaturated fattyacids in cor<strong>on</strong>ary heart disease: a meta-analysis <strong>of</strong> randomized c<strong>on</strong>trolledtrials. Am J Med 2002;112:298–304.364. Studer M, Briel M, Leimenstoll B, Glass TR, Bucher HC. Effect <strong>of</strong> differentantilipidemic agents and diets <strong>on</strong> mortality: a systematic review.Arch Intern Med 2005;165:725–730.365. Kris-E<strong>the</strong>rt<strong>on</strong> PM, Harris WS, Appel LJ. Fish c<strong>on</strong>sumpti<strong>on</strong>, fish oil,omega-3 fatty acids, and cardiovascular disease. Arterioscler ThrombVasc Biol 2003;23:e20–e30.366. He K, S<strong>on</strong>g Y, Daviglus ML, Liu K, Van Horn L, Dyer AR et al. Accumulatedevidence <strong>on</strong> fish c<strong>on</strong>sumpti<strong>on</strong> and cor<strong>on</strong>ary heart disease mortality: ameta-analysis <strong>of</strong> cohort studies. Circulati<strong>on</strong> 2004;109:2705–2711.367. Heart Protecti<strong>on</strong> Study Collaborative Group. MRC/BHF Heart Protecti<strong>on</strong>Study <strong>of</strong> antioxidant vitamin supplementati<strong>on</strong> in 20,536 high-risk individuals:a randomised placebo-c<strong>on</strong>trolled trial. Lancet 2002;360:23–33.368. Yusuf S, Dagenais G, Pogue J, Bosch J, Sleight P. Vitamin E supplementati<strong>on</strong>and cardiovascular events in high-risk patients. The Heart
56 ESC <str<strong>on</strong>g>Guidelines</str<strong>on</strong>g>Outcomes Preventi<strong>on</strong> Evaluati<strong>on</strong> Study Investigators. N Engl J Med2000;342:154–160.369. Kris-E<strong>the</strong>rt<strong>on</strong> PM, Lichtenstein AH, Howard BV, Steinberg D, Witztum JL.Antioxidant vitamin supplements and cardiovascular disease.Circulati<strong>on</strong> 2004;110:637–641.370. American Diabetes Associati<strong>on</strong>. Standards <strong>of</strong> medical care for patientswith diabetes mellitus. Diabetes Care 2003;26(Suppl. 1):s33–s50.371. Inzucchi SE, Amatruda JM. Lipid management in patients with diabetes:translating guidelines into acti<strong>on</strong>. Diabetes Care 2003;26:1309–1311.372. Gaede P, Vedel P, Larsen N, Jensen GV, Parving HH, Pedersen O.Multifactorial interventi<strong>on</strong> and cardiovascular disease in patients withtype 2 diabetes. N Engl J Med 2003;348:383–393.373. Dormandy JA, Charb<strong>on</strong>nel B, Eckland DJ, Erdmann E, Massi-Benedetti M,Moules IK et al. Sec<strong>on</strong>dary preventi<strong>on</strong> <strong>of</strong> macrovascular events inpatients with type 2 diabetes in <strong>the</strong> PROactive Study (PROspectivepioglitAz<strong>on</strong>e Clinical Trial In macroVascular Events): a randomisedc<strong>on</strong>trolled trial. Lancet 2005;366:1279–1289.374. Lewin B, Cay E, Todd I, Goodfield N, Bloomfield P, Elt<strong>on</strong> R. The anginamanagement programme: a rehabiliatati<strong>on</strong> treatment. Br J <strong>Cardio</strong>l1995;2:221–226.375. Lewin RJ, Furze G, Robins<strong>on</strong> J, Griffith K, Wiseman S, Pye M et al. A randomisedc<strong>on</strong>trolled trial <strong>of</strong> a self-management plan for patients withnewly diagnosed angina. Br J Gen Pract 2002;52:194–6–199–201.376. Fox KM, Thadani U, Ma PT, Nash SD, Keating Z, Czorniak MA et al.Sildenafil citrate does not reduce exercise tolerance in men with erectiledysfuncti<strong>on</strong> and chr<strong>on</strong>ic stable angina. Eur Heart J 2003;24:2206–2212.377. Kerins DM. Drugs used for <strong>the</strong> treatment <strong>of</strong> myocardial ischaemia.Goodman & Gilmans The Pharmacological Basis <strong>of</strong> Therapeutics.10th ed. McGraw-Hill; 2001.378. Mittleman MA, Glasser DB, Orazem J. Clinical trials <strong>of</strong> sildenafil citrate(Viagra) dem<strong>on</strong>strate no increase in risk <strong>of</strong> myocardial infarcti<strong>on</strong> andcardiovascular death compared with placebo. Int J Clin Pract2003;57:597–600.379. Gibb<strong>on</strong>s RJ, Abrams J, Chatterjee K, Daley J, Deedwania PC, Douglas JSet al. ACC/AHA 2002 guideline update for <strong>the</strong> management <strong>of</strong> patientswith chr<strong>on</strong>ic stable angina–summary article: a report <strong>of</strong> <strong>the</strong> AmericanCollege <strong>of</strong> <strong>Cardio</strong>logy/American Heart Associati<strong>on</strong> Task Force <strong>on</strong> practiceguidelines (Committee <strong>on</strong> <strong>the</strong> <strong>Management</strong> <strong>of</strong> Patients WithChr<strong>on</strong>ic <strong>Stable</strong> <strong>Angina</strong>). J Am Coll <strong>Cardio</strong>l 2003;41:159–168.380. Luscher TF. Treatment <strong>of</strong> stable angina. Use drugs before percutaneoustransluminal cor<strong>on</strong>ary angioplasty. BMJ 2000;321:62–63.381. Katritsis DG, Ioannidis JP. Percutaneous cor<strong>on</strong>ary interventi<strong>on</strong> versusc<strong>on</strong>servative <strong>the</strong>rapy in n<strong>on</strong>acute cor<strong>on</strong>ary artery disease: ameta-analysis. Circulati<strong>on</strong> 2005;111:2906–2912.382. Hueb W, Soares PR, Gersh BJ, Cesar LA, Luz PL, Puig LB et al. The medicine,angioplasty, or surgery study (MASS-II): a randomized, c<strong>on</strong>trolledclinical trial <strong>of</strong> three <strong>the</strong>rapeutic strategies for multivessel cor<strong>on</strong>aryartery disease: 1 year results. J Am Coll <strong>Cardio</strong>l 2004;43:1743–1751.383. Antiplatelet Trialists’ Collaborati<strong>on</strong>. Collaborative overview <strong>of</strong> randomisedtrials <strong>of</strong> antiplatelet <strong>the</strong>rapy–I: Preventi<strong>on</strong> <strong>of</strong> death, myocardialinfarcti<strong>on</strong>, and stroke by prol<strong>on</strong>ged antiplatelet <strong>the</strong>rapy in variouscategories <strong>of</strong> patients. BMJ 1994;308:81–106.384. Patr<strong>on</strong>o C, Bachmann F, Baigent C, Bode C, De Caterina R, Charb<strong>on</strong>nier Bet al. Expert c<strong>on</strong>sensus document <strong>on</strong> <strong>the</strong> use <strong>of</strong> antiplatelet agents. Thetask force <strong>on</strong> <strong>the</strong> use <strong>of</strong> antiplatelet agents in patients with a<strong>the</strong>roscleroticcardiovascular disease <strong>of</strong> <strong>the</strong> European society <strong>of</strong> cardiology.Eur Heart J 2004;25:166–181.385. Patr<strong>on</strong>o C, Coller B, FitzGerald GA, Hirsh J, Roth G. Platelet-activedrugs: <strong>the</strong> relati<strong>on</strong>ships am<strong>on</strong>g dose, effectiveness, and side effects:<strong>the</strong> Seventh ACCP C<strong>on</strong>ference <strong>on</strong> Antithrombotic and ThrombolyticTherapy. Chest 2004;126(Suppl. 3):234S–264S.386. Patr<strong>on</strong>o C. Aspirin resistance: definiti<strong>on</strong>, mechanisms and clinical readouts.J Thromb Haemost 2003;1:1710–1713.387. Antithrombotic Trialists’ Collaborati<strong>on</strong>. Collaborative meta-analysis <strong>of</strong>randomised trials <strong>of</strong> antiplatelet <strong>the</strong>rapy for preventi<strong>on</strong> <strong>of</strong> death, myocardialinfarcti<strong>on</strong>, and stroke in high risk patients. BMJ 2002;324:71–86.388. Peters RJ, Mehta SR, Fox KA, Zhao F, Lewis BS, Kopecky SL et al. Effects<strong>of</strong> aspirin dose when used al<strong>on</strong>e or in combinati<strong>on</strong> with clopidogrel inpatients with acute cor<strong>on</strong>ary syndromes: observati<strong>on</strong>s from <strong>the</strong>Clopidogrel in Unstable angina to prevent Recurrent Events (CURE)study. Circulati<strong>on</strong> 2003;108:1682–1687.389. Weil J, Colin-J<strong>on</strong>es D, Langman M, Laws<strong>on</strong> D, Logan R, Murphy M et al.Prophylactic aspirin and risk <strong>of</strong> peptic ulcer bleeding. BMJ1995;310:827–830.390. Derry S, Loke YK. Risk <strong>of</strong> gastrointestinal haemorrhage with l<strong>on</strong>g termuse <strong>of</strong> aspirin: meta-analysis. BMJ 2000;321:1183–1187.391. Sudlow C, Baigent C. The adverse effects <strong>of</strong> different doses <strong>of</strong> aspirin:a systematic review <strong>of</strong> randomised trials and observati<strong>on</strong>al studies.(Abstract). Stroke 2000;31:2869.392. Ridker PM, Mans<strong>on</strong> JE, Gaziano JM, Buring JE, Hennekens CH. Low-doseaspirin <strong>the</strong>rapy for chr<strong>on</strong>ic stable angina. A randomized, placeboc<strong>on</strong>trolledclinical trial. Ann Intern Med 1991;114:835–839.393. Fitzgerald GA. Coxibs and cardiovascular disease. N Engl J Med2004;351:1709–1711.394. Bresalier RS, Sandler RS, Quan H, Bolognese JA, Oxenius B, Horgan Ket al. <strong>Cardio</strong>vascular events associated with r<strong>of</strong>ecoxib in a colorectaladenoma chemopreventi<strong>on</strong> trial. N Engl J Med 2005;352:1092–1102.395. Juni P, Nartey L, Reichenbach S, Sterchi R, Dieppe PA, Egger M. Risk <strong>of</strong>cardiovascular events and r<strong>of</strong>ecoxib: cumulative meta-analysis. Lancet2004;364:2021–2029.396. Antman EM, DeMets D, Loscalzo J. Cyclooxygenase inhibiti<strong>on</strong> and cardiovascularrisk. Circulati<strong>on</strong> 2005;112:759–770.397. Solom<strong>on</strong> SD, McMurray JJ, Pfeffer MA, Wittes J, Fowler R, Finn P et al.<strong>Cardio</strong>vascular risk associated with celecoxib in a clinical trial for colorectaladenoma preventi<strong>on</strong>. N Engl J Med 2005;352:1071–1080.398. Nussmeier NA, Whelt<strong>on</strong> AA, Brown MT, Langford RM, Hoeft A, Parlow JLet al. Complicati<strong>on</strong>s <strong>of</strong> <strong>the</strong> COX-2 inhibitors parecoxib and valdecoxibafter cardiac surgery. N Engl J Med 2005;352:1081–1091.399. Bennett JS, Daugherty A, Herringt<strong>on</strong> D, Greenland P, Roberts H, Taubert KA.The use <strong>of</strong> n<strong>on</strong>steroidal anti-inflammatory drugs (NSAIDs): a scienceadvisory from <strong>the</strong> American Heart Associati<strong>on</strong>. Circulati<strong>on</strong> 2005;111:1713–1716.400. Drvota V, Vesterqvist O, Green K. Effects <strong>of</strong> n<strong>on</strong>-steroidal antiinflammatorydrugs <strong>on</strong> <strong>the</strong> in vivo syn<strong>the</strong>sis <strong>of</strong> thromboxane and prostacyclinin humans. Adv Prostaglandin Thromb Leukot Res1991;21A:153–156.401. Cheng JC, Siegel LB, Katari B, Trayn<strong>of</strong>f SA, Ro JO. N<strong>on</strong>steroidal antiinflammatorydrugs and aspirin: a comparis<strong>on</strong> <strong>of</strong> <strong>the</strong> antiplateleteffects. Am J Ther 1997;4:62–65.402. Cap<strong>on</strong>e ML, Tacc<strong>on</strong>elli S, Sciulli MG, Grana M, Ricciotti E, Minuz P et al.Clinical pharmacology <strong>of</strong> platelet, m<strong>on</strong>ocyte, and vascular cyclooxygenaseinhibiti<strong>on</strong> by naproxen and low-dose aspirin in healthy subjects.Circulati<strong>on</strong> 2004;109:1468–1471.403. Reilly IA, FitzGerald GA. Inhibiti<strong>on</strong> <strong>of</strong> thromboxane formati<strong>on</strong> in vivoand ex vivo: implicati<strong>on</strong>s for <strong>the</strong>rapy with platelet inhibitory drugs.Blood 1987;69:180–186.404. Kimmel SE, Berlin JA, Reilly M, Jaskowiak J, Kishel L, Chittams J et al.The effects <strong>of</strong> n<strong>on</strong>selective n<strong>on</strong>-aspirin n<strong>on</strong>-steroidal anti-inflammatorymedicati<strong>on</strong>s <strong>on</strong> <strong>the</strong> risk <strong>of</strong> n<strong>on</strong>fatal myocardial infarcti<strong>on</strong> and <strong>the</strong>irinteracti<strong>on</strong> with aspirin. J Am Coll <strong>Cardio</strong>l 2004;43:985–990.405. Garcia Rodriguez LA, Varas-Lorenzo C, Maguire A, G<strong>on</strong>zalez-Perez A. -N<strong>on</strong>steroidal antiinflammatory drugs and <strong>the</strong> risk <strong>of</strong> myocardial infarcti<strong>on</strong>in <strong>the</strong> general populati<strong>on</strong>. Circulati<strong>on</strong> 2004;109:3000–3006.406. Solom<strong>on</strong> DH, Glynn RJ, Levin R, Avorn J. N<strong>on</strong>steroidal anti-inflammatorydrug use and acute myocardial infarcti<strong>on</strong>. Arch Intern Med2002;162:1099–1104.407. Baigent C, Patr<strong>on</strong>o C. Selective cyclooxygenase 2 inhibitors, aspirin, andcardiovascular disease: a reappraisal. Arthritis Rheum 2003;48:12–20.408. www.fda.gov.medwatch/safety (2005)409. Rao GH, Johns<strong>on</strong> GG, Reddy KR, White JG. Ibupr<strong>of</strong>en protects plateletcyclooxygenase from irreversible inhibiti<strong>on</strong> by aspirin. Arteriosclerosis1983;3:383–388.410. Catella-Laws<strong>on</strong> F, Reilly MP, Kapoor SC, Cucchiara AJ, DeMarco S,Tournier B et al. Cyclooxygenase inhibitors and <strong>the</strong> antiplateleteffects <strong>of</strong> aspirin. N Engl J Med 2001;345:1809–1817.411. Cr<strong>on</strong>berg S, Wallmark E, Soderberg I. Effect <strong>on</strong> platelet aggregati<strong>on</strong> <strong>of</strong>oral administrati<strong>on</strong> <strong>of</strong> 10 n<strong>on</strong>-steroidal analgesics to humans. Scand JHaematol 1984;33:155–159.412. CAPRIE Steering Committee. A randomised, blinded, trial <strong>of</strong> clopidogrelversus aspirin in patients at risk <strong>of</strong> ischaemic events (CAPRIE). Lancet1996;348:1329–1339.413. Kapetanakis EI, Medlam DA, Boyce SW, Haile E, Hill PC, Dullum MK et al.Clopidogrel administrati<strong>on</strong> prior to cor<strong>on</strong>ary artery bypass graftingsurgery: <strong>the</strong> cardiologist’s panacea or <strong>the</strong> surge<strong>on</strong>’s headache? EurHeart J 2005;26:576–583.414. Lau WC, Waskell LA, Watkins PB, Neer CJ, Horowitz K, Hopp AS et al.Atorvastatin reduces <strong>the</strong> ability <strong>of</strong> clopidogrel to inhibit platelet aggregati<strong>on</strong>:a new drug-drug interacti<strong>on</strong>. Circulati<strong>on</strong> 2003;107:32–37.415. Mitsios JV, Papathanasiou AI, Rodis FI, Elisaf M, Goudevenos JA, TselepisAD. Atorvastatin does not affect <strong>the</strong> antiplatelet potency <strong>of</strong> clopidogrel
ESC <str<strong>on</strong>g>Guidelines</str<strong>on</strong>g> 57when it is administered c<strong>on</strong>comitantly for 5 weeks in patients withacute cor<strong>on</strong>ary syndromes. Circulati<strong>on</strong> 2004;109:1335–1338.416. Neubauer H, Gunesdogan B, Hanefeld C, Spiecker M, Mugge A. Lipophilicstatins interfere with <strong>the</strong> inhibitory effects <strong>of</strong> clopidogrel <strong>on</strong> plateletfuncti<strong>on</strong>–a flow cytometry study. Eur Heart J 2003;24:1744–1749.417. Serebruany VL, Midei MG, Malinin AI, Oshrine BR, Lowry DR, Sane DCet al. Absence <strong>of</strong> interacti<strong>on</strong> between atorvastatin or o<strong>the</strong>r statinsand clopidogrel: results from <strong>the</strong> interacti<strong>on</strong> study. Arch Intern Med2004;164:2051–2057.418. Muller I, Besta F, Schulz C, Li Z, Massberg S, Gawaz M. Effects <strong>of</strong> statins<strong>on</strong> platelet inhibiti<strong>on</strong> by a high loading dose <strong>of</strong> clopidogrel. Circulati<strong>on</strong>2003;108:2195–2197.419. Gorchakova O, v<strong>on</strong> Beckerath N, Gawaz M, Mocz A, Joost A, Schomig Aet al. Antiplatelet effects <strong>of</strong> a 600 mg loading dose <strong>of</strong> clopidogrel arenot attenuated in patients receiving atorvastatin or simvastatin for atleast 4 weeks prior to cor<strong>on</strong>ary artery stenting. Eur Heart J2004;25:1898–1902.420. Lim MJ, Spencer FA, Gore JM, Dabbous OH, Agnelli G, Kline-Rogers EMet al. Impact <strong>of</strong> combined pharmacologic treatment with clopidogreland a statin <strong>on</strong> outcomes <strong>of</strong> patients with n<strong>on</strong>-ST-segment elevati<strong>on</strong>acute cor<strong>on</strong>ary syndromes: perspectives from a large multinati<strong>on</strong>alregistry. Eur Heart J 2005;26:1063–1069.421. Cryer B. Reducing <strong>the</strong> risks <strong>of</strong> gastrointestinal bleeding with antiplatelet<strong>the</strong>rapies. N Engl J Med 2005;352:287–289.422. Chan FK. Helicobacter pylori and n<strong>on</strong>steroidal anti-inflammatory drugs.Gastroenterol Clin North Am 2001;30:937–952.423. Lai KC, Lam SK, Chu KM, W<strong>on</strong>g BC, Hui WM, Hu WH et al. Lansoprazolefor <strong>the</strong> preventi<strong>on</strong> <strong>of</strong> recurrences <strong>of</strong> ulcer complicati<strong>on</strong>s from l<strong>on</strong>g-termlow-dose aspirin use. N Engl J Med 2002;346:2033–2038.424. Chan FK, Ching JY, Hung LC, W<strong>on</strong>g VW, Leung VK, Kung NN et al.Clopidogrel versus aspirin and esomeprazole to prevent recurrentulcer bleeding. N Engl J Med 2005;352:238–244.425. Kaufmann PA, Mandinov L, Seiler C, Hess OM. Impact <strong>of</strong>exercise-induced cor<strong>on</strong>ary vasomoti<strong>on</strong> <strong>on</strong> anti-ischaemic <strong>the</strong>rapy.Cor<strong>on</strong> Artery Dis 2000;11:363–369.426. McKee SA, Sane DC, Deliargyris EN. Aspirin resistance in cardiovasculardisease: a review <strong>of</strong> prevalence, mechanisms, and clinical significance.Thromb Haemost 2002;88:711–715.427. Michels<strong>on</strong> AD, Cattaneo M, Eikelboom JW, Gurbel P, Kottke-Marchant K,Kunicki TJ et al. Aspirin resistance: positi<strong>on</strong> paper <strong>of</strong> <strong>the</strong> Working Group<strong>on</strong> Aspirin Resistance. J Thromb Haemost 2005;3:1309–1311.428. Wiviott SD, Antman EM. Clopidogrel resistance: a new chapter in afast-moving story. Circulati<strong>on</strong> 2004;109:3064–3067.429. Cattaneo M. Aspirin and clopidogrel: efficacy, safety, and <strong>the</strong> issue <strong>of</strong>drug resistance. Arterioscler Thromb Vasc Biol 2004;24:1980–1987.430. Nguyen TA, Diodati JG, Pharand C. Resistance to clopidogrel: a review <strong>of</strong><strong>the</strong> evidence. J Am Coll <strong>Cardio</strong>l 2005;45:1157–1164.431. Grundy SM, Cleeman JI, Merz CN, Brewer HB Jr, Clark LT, Hunninghake DBet al. Implicati<strong>on</strong>s <strong>of</strong> recent clinical trials for <strong>the</strong> Nati<strong>on</strong>al CholesterolEducati<strong>on</strong> Program Adult Treatment Panel III <str<strong>on</strong>g>Guidelines</str<strong>on</strong>g>. J Am Coll<strong>Cardio</strong>l 2004;44:720–732.432. The Scandinavian Simvastatin Survival Study (4S). Randomised trial <strong>of</strong>cholesterol lowering in 4444 patients with cor<strong>on</strong>ary heart disease.Lancet 1994;344:1383–1389.433. Sacks FM, T<strong>on</strong>kin AM, Shepherd J, Braunwald E, Cobbe S, Hawkins CMet al. Effect <strong>of</strong> pravastatin <strong>on</strong> cor<strong>on</strong>ary disease events in subgroupsdefined by cor<strong>on</strong>ary risk factors: <strong>the</strong> Prospective Pravastatin PoolingProject. Circulati<strong>on</strong> 2000;102:1893–1900.434. The L<strong>on</strong>g-Term Interventi<strong>on</strong> with Pravastatin in Ischaemic Disease(LIPID) Study Group. Preventi<strong>on</strong> <strong>of</strong> cardiovascular events and deathwith pravastatin in patients with cor<strong>on</strong>ary heart disease and a broadrange <strong>of</strong> initial cholesterol levels. N Engl J Med 1998;339:1349–1357.435. Heart Protecti<strong>on</strong> Study Collaborative Group. MRC/BHF Heart Protecti<strong>on</strong>Study <strong>of</strong> cholesterol lowering with simvastatin in 20,536 high-riskindividuals: a randomised placebo-c<strong>on</strong>trolled trial. Lancet 2002;360(9326):7–22.436. Goldberg RB, Mellies MJ, Sacks FM, Moye LA, Howard BV, Howard WJet al. <strong>Cardio</strong>vascular events and <strong>the</strong>ir reducti<strong>on</strong> with pravastatin in diabeticand glucose-intolerant myocardial infarcti<strong>on</strong> survivors withaverage cholesterol levels: subgroup analyses in <strong>the</strong> cholesterol andrecurrent events (CARE) trial. The Care Investigators. Circulati<strong>on</strong>1998;98:2513–2519.437. Collins R, Armitage J, Parish S, Sleigh P, Peto R. MRC/BHF HeartProtecti<strong>on</strong> Study <strong>of</strong> cholesterol-lowering with simvastatin in 5963people with diabetes: a randomised placebo-c<strong>on</strong>trolled trial. Lancet2003;361:2005–2016.438. Shepherd J, Blauw GJ, Murphy MB, Bollen EL, Buckley BM, Cobbe SMet al. Pravastatin in elderly individuals at risk <strong>of</strong> vascular disease(PROSPER): a randomised c<strong>on</strong>trolled trial. Lancet 2002;360:1623–1630.439. Colhoun HM, Betteridge DJ, Durringt<strong>on</strong> PN, Hitman GA, Neil HA,Livingst<strong>on</strong>e SJ et al. Primary preventi<strong>on</strong> <strong>of</strong> cardiovascular disease withatorvastatin in type 2 diabetes in <strong>the</strong> Collaborative AtorvastatinDiabetes Study (CARDS): multicentre randomised placebo-c<strong>on</strong>trolledtrial. Lancet 2004;364:685–696.440. Sever PS, Dahl<strong>of</strong> B, Poulter NR, Wedel H, Beevers G, Caulfield M et al.Preventi<strong>on</strong> <strong>of</strong> cor<strong>on</strong>ary and stroke events with atorvastatin in hypertensivepatients who have average or lower-than-average cholesterol c<strong>on</strong>centrati<strong>on</strong>s,in <strong>the</strong> Anglo-Scandinavian Cardiac Outcomes Trial–LipidLowering Arm (ASCOT-LLA): a multicentre randomised c<strong>on</strong>trolled trial.Lancet 2003;361:1149–1158.441. Faggiotto A, Paoletti R. State-<strong>of</strong>-<strong>the</strong>-Art lecture. Statins and blockers <strong>of</strong><strong>the</strong> renin-angiotensin system: vascular protecti<strong>on</strong> bey<strong>on</strong>d <strong>the</strong>ir primarymode <strong>of</strong> acti<strong>on</strong>. Hypertensi<strong>on</strong> 1999;34:987–996.442. B<strong>on</strong>etti PO, Lerman LO, Napoli C, Lerman A. Statin effects bey<strong>on</strong>d lipidlowering–are <strong>the</strong>y clinically relevant? Eur Heart J 2003;24:225–248.443. Rosens<strong>on</strong> RS, Tangney CC. Antia<strong>the</strong>rothrombotic properties <strong>of</strong> statins:implicati<strong>on</strong>s for cardiovascular event reducti<strong>on</strong>. JAMA 1998;279:1643–1650.444. Ridker PM, Cann<strong>on</strong> CP, Morrow D, Rifai N, Rose LM, McCabe CH et al. C-reactive protein levels and outcomes after statin <strong>the</strong>rapy. N Engl J Med2005;352:20–28.445. Pasceri V, Patti G, Nusca A, Pristipino C, Richichi G, Di Sciascio G.Randomized trial <strong>of</strong> atorvastatin for reducti<strong>on</strong> <strong>of</strong> myocardial damageduring cor<strong>on</strong>ary interventi<strong>on</strong>: results from <strong>the</strong> ARMYDA (Atorvastatinfor Reducti<strong>on</strong> <strong>of</strong> MYocardial Damage during Angioplasty) study.Circulati<strong>on</strong> 2004;110:674–678.446. Baigent C, Keech A, Kearney PM, Blackwell L, Buck G, Pollicino C et al.Efficacy and safety <strong>of</strong> cholesterol-lowering treatment: prospectivemeta-analysis <strong>of</strong> data from 90,056 participants in 14 randomised trials<strong>of</strong> statins. Lancet 2005;366:1267–1278.447. LaRosa JC, Grundy SM, Waters DD, Shear C, Barter P, Fruchart JC et al.Intensive lipid lowering with atorvastatin in patients with stable cor<strong>on</strong>arydisease. N Engl J Med 2005;352:1425–1435.448. Pedersen TR, Faergeman O, Kastelein JJ, Olss<strong>on</strong> AG, Tikkanen MJ,Holme I et al. High-dose atorvastatin versus usual-dose simvastatin forsec<strong>on</strong>dary preventi<strong>on</strong> after myocardial infarcti<strong>on</strong>: <strong>the</strong> IDEAL study: arandomized c<strong>on</strong>trolled trial. JAMA 2005;294:2437–2445.449. Wierzbicki AS. Ezetimibe: a new additi<strong>on</strong> to lipid-lowering <strong>the</strong>rapy. Int JClin Pract 2003;57:653–655.450. Rubins HB, Robins SJ, Collins D, Fye CL, Anders<strong>on</strong> JW, Elam MB et al.Gemfibrozil for <strong>the</strong> sec<strong>on</strong>dary preventi<strong>on</strong> <strong>of</strong> cor<strong>on</strong>ary heart disease inmen with low levels <strong>of</strong> high-density lipoprotein cholesterol. VeteransAffairs High-Density Lipoprotein Cholesterol Interventi<strong>on</strong> Trial StudyGroup. N Engl J Med 1999;341:410–418.451. Farnier M. Combinati<strong>on</strong> <strong>the</strong>rapy with an HMG-CoA reductase inhibitorand a fibric acid derivative: a critical review <strong>of</strong> potential benefits anddrawbacks. Am J <strong>Cardio</strong>vasc Drugs 2003;3:169–178.452. Robins SJ, Rubins HB, Faas FH, Schaefer EJ, Elam MB, Anders<strong>on</strong> JW et al.Insulin resistance and cardiovascular events with low HDL cholesterol:<strong>the</strong> Veterans Affairs HDL Interventi<strong>on</strong> Trial (VA-HIT). Diabetes Care2003;26:1513–1517.453. Prueksaritan<strong>on</strong>t T, Tang C, Qiu Y, Mu L, Subramanian R, Lin JH. Effects <strong>of</strong>fibrates <strong>on</strong> metabolism <strong>of</strong> statins in human hepatocytes. Drug MetabDispos 2002;30:1280–1287.454. Pan WJ, Gustavs<strong>on</strong> LE, Achari R, Rieser MJ, Ye X, Gutterman C et al.Lack <strong>of</strong> a clinically significant pharmacokinetic interacti<strong>on</strong> betweenfen<strong>of</strong>ibrate and pravastatin in healthy volunteers. J Clin Pharmacol2000;40:316–323.455. Keech A, Simes RJ, Barter P, Best J, Scott R, Takinen MR, Foreder P, Pillai A,Davis T, Glasziou P, Drury P, Kesaniemi YA, Sullivan D, Hunt, Colman D,d’Emden P, M.Whiting M, Ehnholm C, Laakso M, FIELD study investigators.Effects <strong>of</strong> l<strong>on</strong>g-term ffen<strong>of</strong>ibrate <strong>the</strong>rapy <strong>on</strong> cardiovascular events in 9795people with type 2 diabetes mellitus (<strong>the</strong> FIELD study): randomised c<strong>on</strong>trolledtrial. Lancet 2005;366:1829–1831.456. Brousseau ME, Schaefer EJ, Wolfe ML, Blod<strong>on</strong> LT, Digenio AG, Clark RW,Manuscu JP, Rader DJ. Effects <strong>of</strong> an inhibitor <strong>of</strong> cholesteryl ester transferprotein <strong>on</strong> HDL cholesterol. N Engl J Med 2004;350:1491–1494.457. Turnbull F. Effects <strong>of</strong> different blood-pressure-lowering regimens <strong>on</strong>major cardiovascular events: results <strong>of</strong> prospectively-designed overviews<strong>of</strong> randomised trials. Lancet 2003;362:1527–1535.
58 ESC <str<strong>on</strong>g>Guidelines</str<strong>on</strong>g>458. Staessen JA, Wang JG, Thijs L. <strong>Cardio</strong>vascular preventi<strong>on</strong> and bloodpressure reducti<strong>on</strong>: a quantitative overview updated until 1 March2003. J Hypertens 2003;21:1055–1076.459. Psaty BM, Lumley T, Furberg CD, Schellenbaum G, Pahor M, Alderman MHet al. Health outcomes associated with various antihypertensive<strong>the</strong>rapies used as first-line agents: a network meta-analysis. JAMA2003;289:2534–2544.460. Yusuf S, Sleight P, Pogue J, Bosch J, Davies R, Dagenais G. Effects <strong>of</strong> anangiotensin-c<strong>on</strong>verting-enzyme inhibitor, ramipril, <strong>on</strong> cardiovascularevents in high-risk patients. The Heart Outcomes Preventi<strong>on</strong>Evaluati<strong>on</strong> Study Investigators. N Engl J Med 2000;342:145–153.461. Fox KM. Efficacy <strong>of</strong> perindopril in reducti<strong>on</strong> <strong>of</strong> cardiovascular eventsam<strong>on</strong>g patients with stable cor<strong>on</strong>ary artery disease: randomised,double-blind, placebo-c<strong>on</strong>trolled, multicentre trial (<strong>the</strong> EUROPAstudy). Lancet 2003;362:782–788.462. Gustafss<strong>on</strong> I T-PC, Kober L, Gustafss<strong>on</strong> F HP. Effect <strong>of</strong> <strong>the</strong> angiotensinc<strong>on</strong>vertingenzyme inhibitor trandopril <strong>on</strong> mortality and morbidity indiabetic patients with left ventricular dysfuncti<strong>on</strong> after acute myocardialinfarcti<strong>on</strong>. Trace Study Group. 1999;34:83–89.463. Luft FC. Recent clinical trial highlights in hypertensi<strong>on</strong>. Curr HypertensRep 2001;3:133–138.464. Svenss<strong>on</strong> P, de Faire U, Sleight P, Yusuf S, Ostergren J. Comparativeeffects <strong>of</strong> ramipril <strong>on</strong> ambulatory and <strong>of</strong>fice blood pressures: a HOPESubstudy. Hypertensi<strong>on</strong> 2001;38:E28–E32.465. Daly CA, Fox KM, Remme WJ, Bertrand ME, Ferrari R, Simo<strong>on</strong>s ML. Theeffect <strong>of</strong> perindopril <strong>on</strong> cardiovascular morbidity and mortality inpatients with diabetes in <strong>the</strong> EUROPA study: results from <strong>the</strong> PERSUADEsubstudy. Eur Heart J 2005;26:1369–1378.466. Lewingt<strong>on</strong> S, Clarke R, Qizilbash N, Peto R, Collins R. Age-specific relevance<strong>of</strong> usual blood pressure to vascular mortality: a meta-analysis<strong>of</strong> individual data for <strong>on</strong>e milli<strong>on</strong> adults in 61 prospective studies.Lancet 2002;360:1903–1913.467. Nissen SE, Tuzcu EM, Libby P, Thomps<strong>on</strong> PD, Ghali M, Garza D et al.Effect <strong>of</strong> antihypertensive agents <strong>on</strong> cardiovascular events in patientswith cor<strong>on</strong>ary disease and normal blood pressure: <strong>the</strong> CAMELOT study:a randomized c<strong>on</strong>trolled trial. JAMA 2004;292:2217–2225.468. Julius S, Kjeldsen SE, Weber M, Brunner HR, Ekman S, Hanss<strong>on</strong> L et al.Outcomes in hypertensive patients at high cardiovascular risk treatedwith regimens based <strong>on</strong> valsartan or amlodipine: <strong>the</strong> VALUE randomisedtrial. Lancet 2004;363:2022–2031.469. Poulter NR, Wedel H, Dahl<strong>of</strong> B, Sever PS, Beevers DG, Caulfield M et al.Role <strong>of</strong> blood pressure and o<strong>the</strong>r variables in <strong>the</strong> differential cardiovascularevent rates noted in <strong>the</strong> Anglo-Scandinavian CardiacOutcomes Trial-Blood Pressure Lowering Arm (ASCOT-BPLA). Lancet2005;366:907–913.470. Staessen J, Birkenhager WH. Evidence that new antihypertensives aresuperior to older drugs. Lancet 2005;366:869–871.471. Jacks<strong>on</strong> R, Lawes CM, Bennett DA, Milne RJ, Rodgers A. Treatment withdrugs to lower blood pressure and blood cholesterol based <strong>on</strong> an individual’sabsolute cardiovascular risk. Lancet 2005;365:434–441.472. L<strong>on</strong>n EM, Yusuf S, Jha P, M<strong>on</strong>tague TJ, Teo KK, Benedict CR et al.Emerging role <strong>of</strong> angiotensin-c<strong>on</strong>verting enzyme inhibitors in cardiacand vascular protecti<strong>on</strong>. Circulati<strong>on</strong> 1994;90:2056–2069.473. Pfeffer MA, McMurray JJ, Velazquez EJ, Rouleau JL, Kober L, Maggi<strong>on</strong>i APet al. Valsartan, captopril, or both in myocardial infarcti<strong>on</strong> complicatedby heart failure, left ventricular dysfuncti<strong>on</strong>, or both. N Engl J Med2003;349:1893–1906.474. Yusuf S, Pfeffer MA, Swedberg K, Granger CB, Held P, McMurray JJ et al.Effects <strong>of</strong> candesartan in patients with chr<strong>on</strong>ic heart failure and preservedleft-ventricular ejecti<strong>on</strong> fracti<strong>on</strong>: <strong>the</strong> CHARM-Preserved Trial.Lancet 2003;362:777–781.475. Hulley S, Grady D, Bush T, Furberg C, Herringt<strong>on</strong> D, Riggs B et al.Randomized trial <strong>of</strong> estrogen plus progestin for sec<strong>on</strong>dary preventi<strong>on</strong><strong>of</strong> cor<strong>on</strong>ary heart disease in postmenopausal women. Heart andEstrogen/progestin Replacement Study (HERS) Research Group. JAMA1998;280:605–613.476. Grady D, Herringt<strong>on</strong> D, Bittner V, Blumenthal R, Davids<strong>on</strong> M, Hlatky Met al. <strong>Cardio</strong>vascular disease outcomes during 6.8 years <strong>of</strong> horm<strong>on</strong>e<strong>the</strong>rapy: Heart and Estrogen/progestin Replacement Study follow-up(HERS II). JAMA 2002;288:49–57.477. Rossouw JE, Anders<strong>on</strong> GL, Prentice RL, LaCroix AZ, Kooperberg C,Stefanick ML et al. Risks and benefits <strong>of</strong> estrogen plus progestin inhealthy postmenopausal women: principal results From <strong>the</strong> Women’sHealth Initiative randomized c<strong>on</strong>trolled trial. JAMA 2002;288:321–333.478. Mans<strong>on</strong> JE, Hsia J, Johns<strong>on</strong> KC, Rossouw JE, Assaf AR, Lasser NL et al.Estrogen plus progestin and <strong>the</strong> risk <strong>of</strong> cor<strong>on</strong>ary heart disease. NEnglJ Med 2003;349:523–534.479. Hersh AL, Stefanick ML, Stafford RS. Nati<strong>on</strong>al use <strong>of</strong> postmenopausalhorm<strong>on</strong>e <strong>the</strong>rapy: annual trends and resp<strong>on</strong>se to recent evidence.JAMA 2004;291:47–53.480. Yusuf S, Wittes J, Friedman L. Overview <strong>of</strong> results <strong>of</strong> randomized clinicaltrials in heart disease. I. Treatments following myocardial infarcti<strong>on</strong>.JAMA 1988;260:2088–2093.481. Freemantle N, Urdahl H, Eastaugh J, Hobbs FD. What is <strong>the</strong> place <strong>of</strong>beta-blockade in patients who have experienced a myocardial infarcti<strong>on</strong>with preserved left ventricular functi<strong>on</strong>? Evidence and (mis)interpretati<strong>on</strong>.Prog <strong>Cardio</strong>vasc Dis 2002;44:243–250.482. Carlberg B, Samuelss<strong>on</strong> O, Lindholm LH. Atenolol in hypertensi<strong>on</strong>: is it awise choice? Lancet 2004;364:1684–1689.483. Hjemdahl P, Erikss<strong>on</strong> SV, Held C, Forslund L, Nasman P, Rehnqvist N.Favourable l<strong>on</strong>g term prognosis in stable angina pectoris: an extendedfollow up <strong>of</strong> <strong>the</strong> angina prognosis study in Stockholm (APSIS). Heart2006;92(2):177–182. [EPub ahead <strong>of</strong> print June 10, 2005]484. Pepine CJ, Cohn PF, Deedwania PC, Gibs<strong>on</strong> RS, Handberg E, Hill JA et al.Effects <strong>of</strong> treatment <strong>on</strong> outcome in mildly symptomatic patients withischemia during daily life. The Atenolol Silent Ischemia Study (ASIST).Circulati<strong>on</strong> 1994;90:762–768.485. Effect <strong>of</strong> metoprolol CR/XL in chr<strong>on</strong>ic heart failure: Metoprolol CR/XLRandomised Interventi<strong>on</strong> Trial in C<strong>on</strong>gestive Heart Failure (MERIT-HF).Lancet 1999;353:2001–2007.486. The Cardiac Insufficiency Bisoprolol Study II (CIBIS-II): a randomisedtrial. Lancet 1999;353:9–13.487. Packer M, Bristow MR, Cohn JN, Colucci WS, Fowler MB, Gilbert EM et al.The effect <strong>of</strong> carvedilol <strong>on</strong> morbidity and mortality in patients withchr<strong>on</strong>ic heart failure. U.S. Carvedilol Heart Failure Study Group.N 0Engl J Med 1996;334:1349–1355.488. Effect <strong>of</strong> verapamil <strong>on</strong> mortality and major events after acute myocardialinfarcti<strong>on</strong> (<strong>the</strong> Danish Verapamil Infarcti<strong>on</strong> Trial II–DAVIT II). Am J<strong>Cardio</strong>l 1990;66:779–785.489. The Multicenter Diltiazem Postinfarcti<strong>on</strong> Trial Research Group. Theeffect <strong>of</strong> diltiazem <strong>on</strong> mortality and reinfarcti<strong>on</strong> after myocardialinfarcti<strong>on</strong>. N Engl J Med 1988;319:385–392.490. Boden WE, van Gilst WH, Scheldewaert RG, Starkey IR, Carlier MF, JulianDG et al. Diltiazem in acute myocardial infarcti<strong>on</strong> treated with thrombolyticagents: a randomised placebo-c<strong>on</strong>trolled trial. IncompleteInfarcti<strong>on</strong> Trial <strong>of</strong> European Research Collaborators EvaluatingPrognosis post-Thrombolysis (INTERCEPT). Lancet 2000;355:1751–1756.491. Furberg CD, Psaty BM, Meyer JV. Nifedipine. Dose-related increase inmortality in patients with cor<strong>on</strong>ary heart disease. Circulati<strong>on</strong>1995;92:1326–1331.492. Stas<strong>on</strong> WB, Schmid CH, Niedzwiecki D, Whiting GW, Caubet JF, Cory Det al. Safety <strong>of</strong> nifedipine in angina pectoris: a meta-analysis.Hypertensi<strong>on</strong> 1999;33:24–31.493. Poole-Wils<strong>on</strong> PA, Lubsen J, Kirwan BA, van Dalen FJ, Wagener G,Danchin N et al. Effect <strong>of</strong> l<strong>on</strong>g-acting nifedipine <strong>on</strong> mortality and cardiovascularmorbidity in patients with stable angina requiring treatment(ACTION trial): randomised c<strong>on</strong>trolled trial. Lancet 2004;364:849–857.494. Heidenreich PA, McD<strong>on</strong>ald KM, Hastie T, Fadel B, Hagan V, Lee BK et al.Meta-analysis <strong>of</strong> trials comparing beta-blockers, calcium antag<strong>on</strong>ists,and nitrates for stable angina. JAMA 1999;281:1927–1936.495. Parker JD, Parker JO. Nitrate <strong>the</strong>rapy for stable angina pectoris. N EnglJ Med 1998;338:520–531.496. Thadani U, Lipicky RJ. Short and l<strong>on</strong>g-acting oral nitrates for stableangina pectoris. <strong>Cardio</strong>vasc Drugs Ther 1994;8:611–623.497. ISIS-4 (Fourth Internati<strong>on</strong>al Study <strong>of</strong> Infarct Survival) CollaborativeGroup. ISIS-4: a randomised factorial trial assessing early oral captopril,oral m<strong>on</strong><strong>on</strong>itrate, and intravenous magnesium sulphate in 58,050patients with suspected acute myocardial infarcti<strong>on</strong>. Lancet1995;345:669–685.498. Gruppo Italiano per lo Studio della Sopravvivenza nell’infartoMiocardico. GISSI-3: effects <strong>of</strong> lisinopril and transdermal glyceryl trinitratesingly and toge<strong>the</strong>r <strong>on</strong> 6-week mortality and ventricular functi<strong>on</strong>after acute myocardial infarcti<strong>on</strong>. Lancet 1994;343:1115–1122.499. Thadani U, Lipicky RJ. Ointments and transdermal nitroglycerin patchesfor stable angina pectoris. <strong>Cardio</strong>vasc Drugs Ther 1994;8:625–633.500. Parker JD, Parker AB, Farrell B, Parker JO. Intermittent transdermalnitroglycerin <strong>the</strong>rapy. Decreased anginal threshold during <strong>the</strong> nitratefreeinterval. Circulati<strong>on</strong> 1995;91:973–978.501. Pepine CJ, Lopez LM, Bell DM, Handberg-Thurm<strong>on</strong>d EM, Marks RG,McGorray S. Effects <strong>of</strong> intermittent transdermal nitroglycerin <strong>on</strong>
ESC <str<strong>on</strong>g>Guidelines</str<strong>on</strong>g> 59occurrence <strong>of</strong> ischemia after patch removal: results <strong>of</strong> <strong>the</strong> sec<strong>on</strong>d transdermalintermittent dosing evaluati<strong>on</strong> study (TIDES-II). J Am Coll<strong>Cardio</strong>l 1997;30:955–961.502. Sav<strong>on</strong>itto S, Ardissino D. Selecti<strong>on</strong> <strong>of</strong> drug <strong>the</strong>rapy in stable anginapectoris. <strong>Cardio</strong>vasc Drugs Ther 1998;12:197–210.503. Thadani U. Treatment <strong>of</strong> stable angina. Curr Opin <strong>Cardio</strong>l1999;14:349–358.504. Ko DT, Hebert PR, C<strong>of</strong>fey CS, Sedrakyan A, Curtis JP, Krumholz HM.Beta-blocker <strong>the</strong>rapy and symptoms <strong>of</strong> depressi<strong>on</strong>, fatigue, and sexualdysfuncti<strong>on</strong>. JAMA 2002;288:351–357.505. Hjemdahl P, Wiklund IK. Quality <strong>of</strong> life <strong>on</strong> antihypertensive drug<strong>the</strong>rapy: scientific end-point or marketing exercise? J Hypertens1992;10:1437–1446.506. Neat<strong>on</strong> JD, Grimm RH Jr, Prineas RJ, Stamler J, Grandits GA, Elmer PJet al. Treatment <strong>of</strong> Mild Hypertensi<strong>on</strong> Study. Final results. Treatment<strong>of</strong> Mild Hypertensi<strong>on</strong> Study Research Group. JAMA 1993;270:713–724.507. Hjemdahl P, Wallen NH. Calcium antag<strong>on</strong>ist treatment, sympa<strong>the</strong>ticactivity and platelet functi<strong>on</strong>. Eur Heart J 1997;18(Suppl. A):A36–A50.508. Karls<strong>on</strong> BW, Emanuelss<strong>on</strong> H, Herlitz J, Nilss<strong>on</strong> JE, Olss<strong>on</strong> G. Evaluati<strong>on</strong><strong>of</strong> <strong>the</strong> antianginal effect <strong>of</strong> nifedipine: influence <strong>of</strong> formulati<strong>on</strong> dependentpharmacokinetics. Eur J Clin Pharmacol 1991;40:501–506.509. Waters D. Proischemic complicati<strong>on</strong>s <strong>of</strong> dihydropyridine calcium channelblockers. Circulati<strong>on</strong> 1991;84:2598–2600.510. Deanfield JE, Detry JM, Lichtlen PR, Magnani B, Sellier P, Thaulow E.Amlodipine reduces transient myocardial ischemia in patients withcor<strong>on</strong>ary artery disease: double-blind Circadian Anti-Ischemia Programin Europe (CAPE Trial). J Am Coll <strong>Cardio</strong>l 1994;24:1460–1467.511. Packer M, O’C<strong>on</strong>nor CM, Ghali JK, Pressler ML, Cars<strong>on</strong> PE, Belkin RNet al. Effect <strong>of</strong> amlodipine <strong>on</strong> morbidity and mortality in severechr<strong>on</strong>ic heart failure. Prospective Randomized Amlodipine SurvivalEvaluati<strong>on</strong> Study Group. N Engl J Med 1996;335:1107–1114.512. Ardissino D, Sav<strong>on</strong>itto S, Egstrup K, Rasmussen K, Bae EA, Omland Tet al. Selecti<strong>on</strong> <strong>of</strong> medical treatment in stable angina pectoris:results <strong>of</strong> <strong>the</strong> Internati<strong>on</strong>al Multicenter <strong>Angina</strong> Exercise (IMAGE) Study.J Am Coll <strong>Cardio</strong>l 1995;25:1516–1521.513. Forslund L, Hjemdahl P, Held C, Bjorkander I, Erikss<strong>on</strong> SV, Brodin U et al.Prognostic implicati<strong>on</strong>s <strong>of</strong> results from exercise testing in patients withchr<strong>on</strong>ic stable angina pectoris treated with metoprolol or verapamil. Areport from <strong>the</strong> <strong>Angina</strong> Prognosis Study In Stockholm (APSIS). Eur Heart J2000;21:901–910.514. Arnim TV. Medical treatment to reduce total ischaemic burden: totalischaemic burden bisoprolol study (TIBBS), a multicenter trial comparingbisoprolol and nifedipine. The TIBBS Investigators. J Am Coll<strong>Cardio</strong>l 1995;25:231–238.515. Fox KM, Mulcahy D, Findlay I, Ford I, Dargie HJ. The Total IschaemicBurden European Trial (TIBET). Effects <strong>of</strong> atenolol, nifedipine SR and<strong>the</strong>ir combinati<strong>on</strong> <strong>on</strong> <strong>the</strong> exercise test and <strong>the</strong> total ischaemic burdenin 608 patients with stable angina. The TIBET Study Group. Eur HeartJ 1996;17:96–103.516. Markham A, Plosker GL, Goa KL. Nicorandil. An updated review <strong>of</strong> its usein ischaemic heart disease with emphasis <strong>on</strong> its cardioprotectiveeffects. Drugs 2000;60:955–974.517. Rajaratnam R, Brieger DB, Hawkins R, Freedman SB. Attenuati<strong>on</strong> <strong>of</strong>anti-ischaemic efficacy during chr<strong>on</strong>ic <strong>the</strong>rapy with nicorandil inpatients with stable angina pectoris. Am J <strong>Cardio</strong>l 1999;83:1120–1124, A9.518. Nicorandil for angina–an update. Drug Ther Bull. 2003;41:86–88.519. Borer JS, Fox K, Jaill<strong>on</strong> P, Lerebours G. Antianginal and antiischemiceffects <strong>of</strong> ivabradine, an I(f) inhibitor, in stable angina: a randomized,double-blind, multicentered, placebo-c<strong>on</strong>trolled trial. Circulati<strong>on</strong>2003;107:817–823.520. Tardif JC, Ford I, Tendera M, Bourassa MG, Fox K. Efficacy <strong>of</strong> ivabradine,a new selective If inhibitor, compared with atenolol in patients withchr<strong>on</strong>ic stable angina. Eur Heart J 2005;26:2529–2536.521. Antzelevitch C, Belardinelli L, Zygmunt AC, Burashnikov A, Di Diego JM,Fish JM et al. Electrophysiological effects <strong>of</strong> ranolazine, a novel antianginalagent with antiarrhythmic properties. Circulati<strong>on</strong> 2004;110:904–910.522. Haigney MC, Lakatta EG, Stern MD, Silverman HS. Sodium channel blockadereduces hypoxic sodium loading and sodium-dependent calciumloading. Circulati<strong>on</strong> 1994;90:391–399.523. Ver D<strong>on</strong>ck L, Borgers M, Verd<strong>on</strong>ck F. Inhibiti<strong>on</strong> <strong>of</strong> sodium and calciumoverload pathology in <strong>the</strong> myocardium: a new cytoprotective principle.<strong>Cardio</strong>vasc Res 1993;27:349–357.524. Marzilli M, Klein WW. Efficacy and tolerability <strong>of</strong> trimetazidine in stableangina: a meta-analysis <strong>of</strong> randomized, double-blind, c<strong>on</strong>trolled trials.Cor<strong>on</strong> Artery Dis 2003;14:171–179.525. Cross HR. Trimetazidine for stable angina pectoris. Expert OpinPharmaco<strong>the</strong>r 2001;2:857–875.526. Chazov EI, Lepakchin VK, Zharova EA, Fitilev SB, Levin AM, RumiantzevaEG et al. Trimetazidine in <strong>Angina</strong> Combinati<strong>on</strong> Therapy–<strong>the</strong> TACT study:trimetazidine versus c<strong>on</strong>venti<strong>on</strong>al treatment in patients with stableangina pectoris in a randomized, placebo-c<strong>on</strong>trolled, multicenterstudy. Am J Ther 2005;12:35–42.527. Chaitman BR, Skettino SL, Parker JO, Hanley P, Meluzin J, Kuch J et al.Anti-ischaemic effects and l<strong>on</strong>g-term survival during ranolazine m<strong>on</strong>o<strong>the</strong>rapyin patients with chr<strong>on</strong>ic severe angina. J Am Coll <strong>Cardio</strong>l2004;43:1375–1382.528. Chaitman BR, Pepine CJ, Parker JO, Skopal J, Chumakova G, Kuch Jet al. Effects <strong>of</strong> ranolazine with atenolol, amlodipine, or diltiazem <strong>on</strong>exercise tolerance and angina frequency in patients with severechr<strong>on</strong>ic angina: a randomized c<strong>on</strong>trolled trial. JAMA 2004;291:309–316.529. Messin R, Opolski G, Fenyvesi T, Carreer-Bruhwyler F, Dubois C,Famaey JP et al. Efficacy and safety <strong>of</strong> molsidomine <strong>on</strong>ce-a-day inpatients with stable angina pectoris. Int J <strong>Cardio</strong>l 2005;98:79–89.530. Tolins M, Weir EK, Chesler E, Pierp<strong>on</strong>t GL. ‘Maximal’ drug <strong>the</strong>rapy is notnecessarily optimal in chr<strong>on</strong>ic angina pectoris. J Am Coll <strong>Cardio</strong>l1984;3:1051–1057.531. Jacks<strong>on</strong> G. <strong>Stable</strong> angina: maximal medical <strong>the</strong>rapy is not <strong>the</strong> same asoptimal medical <strong>the</strong>rapy. Int J Clin Pract 2000;54:351.532. Kaski JC, Valenzuela Garcia LF. Therapeutic opti<strong>on</strong>s for <strong>the</strong> management<strong>of</strong> patients with cardiac syndrome X. Eur Heart J 2001;22:283–293.533. Cann<strong>on</strong> RO III, Wats<strong>on</strong> RM, Rosing DR, Epstein SE. Efficacy <strong>of</strong> calciumchannel blocker <strong>the</strong>rapy for angina pectoris resulting from small-vesselcor<strong>on</strong>ary artery disease and abnormal vasodilator reserve. Am J <strong>Cardio</strong>l1985;56:242–246.534. Lanza GA, Col<strong>on</strong>na G, Pasceri V, Maseri A. Atenolol versus amlodipineversus isosorbide-5-m<strong>on</strong><strong>on</strong>itrate <strong>on</strong> anginal symptoms in syndrome X.Am J <strong>Cardio</strong>l 1999;84:854–856. A8.535. Camici PG, Marraccini P, Gistri R, Salvadori PA, Sorace O, L’Abbate A.Adrenergically mediated cor<strong>on</strong>ary vasoc<strong>on</strong>stricti<strong>on</strong> in patients withsyndrome X. <strong>Cardio</strong>vasc Drugs Ther 1994;8:221–226.536. Botker HE, S<strong>on</strong>ne HS, Schmitz O, Nielsen TT. Effects <strong>of</strong> doxazosin <strong>on</strong>exercise-induced angina pectoris, ST-segment depressi<strong>on</strong>, and insulinsensitivity in patients with syndrome X. Am J <strong>Cardio</strong>l1998;82:1352–1356.537. Galassi AR, Kaski JC, Pupita G, Vejar M, Crea F, Maseri A. Lack <strong>of</strong>evidence for alpha-adrenergic receptor-mediated mechanisms in <strong>the</strong>genesis <strong>of</strong> ischemia in syndrome X. Am J <strong>Cardio</strong>l 1989;64:264–269.538. Yamabe H, Namura H, Yano T, Fujita H, Kim S, Iwahashi M et al. Effect <strong>of</strong>nicorandil <strong>on</strong> abnormal cor<strong>on</strong>ary flow reserve assessed by exercise 201Tlscintigraphy in patients with angina pectoris and nearly normal cor<strong>on</strong>aryarteriograms. <strong>Cardio</strong>vasc Drugs Ther 1995;9:755–761.539. Rogacka D, Guzik P, Wykretowicz A, Rzezniczak J, Dziarmaga M, Wysocki H.Effects <strong>of</strong> trimetazidine <strong>on</strong> clinical symptoms and tolerance <strong>of</strong> exercise <strong>of</strong>patients with syndrome X: a preliminary study. Cor<strong>on</strong> Artery Dis2000;11:171–177.540. Ozcelik F, Altun A, Ozbay G. Antianginal and anti-ischaemic effects <strong>of</strong>nisoldipine and ramipril in patients with syndrome X. Clin <strong>Cardio</strong>l1999;22:361–365.541. Kayikcioglu M, Payzin S, Yavuzgil O, Kultursay H, Can LH, Soydan I.Benefits <strong>of</strong> statin treatment in cardiac syndrome-X1. Eur Heart J2003;24:1999–2005.542. Pizzi C, Manfrini O, F<strong>on</strong>tana F, Bugiardini R. Angiotensin-c<strong>on</strong>vertingenzyme inhibitors and 3-hydroxy-3-methylglutaryl coenzyme areductase in cardiac Syndrome X: role <strong>of</strong> superoxide dismutase activity.Circulati<strong>on</strong> 2004;109:53–58.543. Kaski JC, Rosano G, Gavrielides S, Chen L. Effects <strong>of</strong> angiotensinc<strong>on</strong>vertingenzyme inhibiti<strong>on</strong> <strong>on</strong> exercise-induced angina and STsegment depressi<strong>on</strong> in patients with microvascular angina. J Am Coll<strong>Cardio</strong>l 1994;23:652–657.544. Nalbantgil I, Onder R, Altintig A, Nalbantgil S, Kiliccioglu B, Boydak Bet al. Therapeutic benefits <strong>of</strong> cilazapril in patients with syndrome X. -<strong>Cardio</strong>logy 1998;89:130–133.545. Kaski JC. Pathophysiology and management <strong>of</strong> patients with chest painand normal cor<strong>on</strong>ary arteriograms (cardiac syndrome X). Circulati<strong>on</strong>2004;109:568–572.546. Cann<strong>on</strong> RO III, Quyyumi AA, Mincemoyer R, Stine AM, Gracely RH,Smith WB et al. Imipramine in patients with chest pain despite normalcor<strong>on</strong>ary angiograms. NEnglJMed1994;330:1411–1417.
60 ESC <str<strong>on</strong>g>Guidelines</str<strong>on</strong>g>547. Yoshio H, Shimizu M, Kita Y, Ino H, Kaku B, Taki J et al. Effects <strong>of</strong> shorttermaminophylline administrati<strong>on</strong> <strong>on</strong> cardiac functi<strong>on</strong>al reserve inpatients with syndrome X. J Am Coll <strong>Cardio</strong>l 1995;25:1547–1551.548. Lanza GA, Sestito A, Sgueglia GA, Infusino F, Papacci F, Visocchi M et al.Effect <strong>of</strong> spinal cord stimulati<strong>on</strong> <strong>on</strong> sp<strong>on</strong>taneous and stress-inducedangina and ‘ischemia-like’ ST-segment depressi<strong>on</strong> in patients withcardiac syndrome X. Eur Heart J 2005;549. Erikss<strong>on</strong> BE, Tyni-Lenne R, Svedenhag J, Hallin R, Jensen-Urstad K,Jensen-Urstad M et al. Physical training in Syndrome X: physicaltraining counteracts dec<strong>on</strong>diti<strong>on</strong>ing and pain in Syndrome X. J AmColl <strong>Cardio</strong>l 2000;36:1619–1625.550. Sitges M, Heras M, Roig E, Duran M, Masotti M, Zurbano MJ et al. Acuteand mid-term combined horm<strong>on</strong>e replacement <strong>the</strong>rapy improves endo<strong>the</strong>lialfuncti<strong>on</strong> in post-menopausal women with angina and angiographicallynormal cor<strong>on</strong>ary arteries. Eur Heart J 2001;22:2116–2124.551. Rosano GM, Peters NS, Lefroy D, Lindsay DC, Sarrel PM, Collins P et al.17-beta-Estradiol <strong>the</strong>rapy lessens angina in postmenopausal womenwith syndrome X. J Am Coll <strong>Cardio</strong>l 1996;28:1500–1505.552. Chevalier P, Dacosta A, Defaye P, Chalvidan T, B<strong>on</strong>nefoy E, Kirkorian Get al. Arrhythmic cardiac arrest due to isolated cor<strong>on</strong>ary arteryspasm: l<strong>on</strong>g-term outcome <strong>of</strong> seven resuscitated patients. J Am Coll<strong>Cardio</strong>l 1998;31:57–61.553. Ricci DR, Orlick AE, Cipriano PR, Guthaner DF, Harris<strong>on</strong> DC. Alteredadrenergic activity in cor<strong>on</strong>ary arterial spasm: insight into mechanismbased <strong>on</strong> study <strong>of</strong> cor<strong>on</strong>ary hemodynamics and <strong>the</strong> electrocardiogram.Am J <strong>Cardio</strong>l 1979;43:1073–1079.554. Lablanche JM, Bauters C, McFadden EP, Quandalle P, Bertrand ME.Potassium channel activators in vasospastic angina. Eur Heart J1993;14(Suppl. B):22–24.555. Khatri S, Webb JG, Carere RG, Dodek A. Stenting for cor<strong>on</strong>ary arteryspasm. Ca<strong>the</strong>ter <strong>Cardio</strong>vasc Interv 2002;56:16–20.556. Gaspard<strong>on</strong>e A, Tomai F, Versaci F, Ghini AS, Polisca P, Crea F et al.Cor<strong>on</strong>ary artery stent placement in patients with variant angina refractoryto medical treatment. Am J <strong>Cardio</strong>l 1999;84:96–98. A8.557. Waters DD, Bouchard A, Theroux P. Sp<strong>on</strong>taneous remissi<strong>on</strong> is a frequentoutcome <strong>of</strong> variant angina. J Am Coll <strong>Cardio</strong>l 1983;2:195–199.558. J<strong>on</strong>es RH, Kesler K, Phillips HR III, Mark DB, Smith PK, Nels<strong>on</strong> CL et al.L<strong>on</strong>g-term survival benefits <strong>of</strong> cor<strong>on</strong>ary artery bypass grafting andpercutaneous transluminal angioplasty in patients with cor<strong>on</strong>aryartery disease. J Thorac <strong>Cardio</strong>vasc Surg 1996;111:1013–1025.559. Myocardial infarcti<strong>on</strong> and mortality in <strong>the</strong> cor<strong>on</strong>ary artery surgery study(CASS) randomized trial. N Engl J Med 1984;310:750–758.560. H<strong>of</strong>fman SN, TenBrook JA, Wolf MP, Pauker SG, Salem DN, W<strong>on</strong>g JB. Ameta-analysis <strong>of</strong> randomized c<strong>on</strong>trolled trials comparing cor<strong>on</strong>aryartery bypass graft with percutaneous transluminal cor<strong>on</strong>aryangioplasty: <strong>on</strong>e- to 8 year outcomes. J Am Coll <strong>Cardio</strong>l 2003;41:1293–1304.561. Hamm CW, Reimers J, Ischinger T, Rupprecht HJ, Berger J, Bleifeld W. Arandomized study <strong>of</strong> cor<strong>on</strong>ary angioplasty compared with bypass surgeryin patients with symptomatic multivessel cor<strong>on</strong>ary disease. GermanAngioplasty Bypass Surgery Investigati<strong>on</strong> (GABI). N Engl J Med1994;331:1037–1043.562. Rodriguez A, Rodriguez Alemparte M, Baldi J, Navia J, Delacasa A,Vogel D et al. Cor<strong>on</strong>ary stenting versus cor<strong>on</strong>ary bypass surgery inpatients with multiple vessel disease and significant proximal LADstenosis: results from <strong>the</strong> ERACI II study. Heart 2003;89:184–188.563. Goy JJ, Eeckhout E, Moret C, Burnand B, Vogt P, Stauffer JC et al.5 year outcome in patients with isolated proximal left anterior descendingcor<strong>on</strong>ary artery stenosis treated by angioplasty or left internalmammary artery grafting. A prospective trial. Circulati<strong>on</strong> 1999;99:3255–3259.564. Nilss<strong>on</strong> J, Algotss<strong>on</strong> L, Hoglund P, Luhrs C, Brandt J. Early mortality incor<strong>on</strong>ary bypass surgery: <strong>the</strong> EuroSCORE versus The Society <strong>of</strong> ThoracicSurge<strong>on</strong>s risk algorithm. Ann Thorac Surg 2004;77:1235–1239; discussi<strong>on</strong>1239–1240.565. Nashef SA, Roques F, Michel P, Gauducheau E, Lemeshow S, Salam<strong>on</strong> R.European system for cardiac operative risk evaluati<strong>on</strong> (EuroSCORE). EurJ <strong>Cardio</strong>thorac Surg 1999;16:9–13.566. Goldman S, Zadina K, Moritz T, Ovitt T, Sethi G, Copeland JG et al. L<strong>on</strong>gtermpatency <strong>of</strong> saphenous vein and left internal mammary artery graftsafter cor<strong>on</strong>ary artery bypass surgery: results from a Department <strong>of</strong>Veterans Affairs Cooperative Study. J Am Coll <strong>Cardio</strong>l 2004;44:2149–2156.567. Lytle BW, Loop FD, Cosgrove DM, Ratliff NB, Easley K, Taylor PC. L<strong>on</strong>gterm(5 to 12 years) serial studies <strong>of</strong> internal mammary artery andsaphenous vein cor<strong>on</strong>ary bypass grafts. J Thorac <strong>Cardio</strong>vasc Surg1985;89:248–258.568. Camer<strong>on</strong> A, Davis KB, Green G, Schaff HV. Cor<strong>on</strong>ary bypass surgery withinternal-thoracic-artery grafts–effects <strong>on</strong> survival over a 15-yearperiod. N Engl J Med 1996;334:216–219.569. Lytle BW, Blackst<strong>on</strong>e EH, Loop FD, Houghtaling PL, Arnold JH, Akhrass Ret al. Two internal thoracic artery grafts are better than <strong>on</strong>e. J Thorac<strong>Cardio</strong>vasc Surg 1999;117:855–872.570. Brodman RF, Frame R, Camacho M, Hu E, Chen A, Hollinger I. Routine use<strong>of</strong> unilateral and bilateral radial arteries for cor<strong>on</strong>ary artery bypassgraft surgery. J Am Coll <strong>Cardio</strong>l 1996;28:959–963.571. Acar C, Ramsheyi A, Pagny JY, Jebara V, Barrier P, Fabiani JN et al.The radial artery for cor<strong>on</strong>ary artery bypass grafting: clinical andangiographic results at 5 years. J Thorac <strong>Cardio</strong>vasc Surg1998;116:981–989.572. van Dijk D, Nierich AP, Jansen EW, Nathoe HM, Suyker WJ, Diephuis JCet al. Early outcome after <strong>of</strong>f-pump versus <strong>on</strong>-pump cor<strong>on</strong>ary bypasssurgery: results from a randomized study. Circulati<strong>on</strong> 2001;104:1761–1766.573. Angelini GD, Taylor FC, Reeves BC, Asci<strong>on</strong>e R. Early and midtermoutcome after <strong>of</strong>f-pump and <strong>on</strong>-pump surgery in Beating Heart Against<strong>Cardio</strong>plegic Arrest Studies (BHACAS 1 and 2): a pooled analysis <strong>of</strong> tworandomised c<strong>on</strong>trolled trials. Lancet 2002;359:1194–1199.574. Khan NE, De Souza A, Mister R, Fla<strong>the</strong>r M, Clague J, Davies S et al. A randomizedcomparis<strong>on</strong> <strong>of</strong> <strong>of</strong>f-pump and <strong>on</strong>-pump multivesselcor<strong>on</strong>ary-artery bypass surgery. N Engl J Med 2004;350:21–28.575. Smith SC Jr, Dove JT, Jacobs AK, Kennedy JW, Kereiakes D, Kern MJ et al.ACC/AHA guidelines <strong>of</strong> percutaneous cor<strong>on</strong>ary interventi<strong>on</strong>s (revisi<strong>on</strong> <strong>of</strong><strong>the</strong> 1993 PTCA guidelines)–executive summary. A report <strong>of</strong> <strong>the</strong>American College <strong>of</strong> <strong>Cardio</strong>logy/American Heart Associati<strong>on</strong> TaskForce <strong>on</strong> Practice <str<strong>on</strong>g>Guidelines</str<strong>on</strong>g> (committee to revise <strong>the</strong> 1993 guidelinesfor percutaneous transluminal cor<strong>on</strong>ary angioplasty). J Am Coll<strong>Cardio</strong>l 2001;37:2215–2239.576. Bucher HC, Hengstler P, Schindler C, Guyatt GH. Percutaneous transluminalcor<strong>on</strong>ary angioplasty versus medical treatment for n<strong>on</strong>-acute cor<strong>on</strong>aryheart disease: meta-analysis <strong>of</strong> randomised c<strong>on</strong>trolled trials. BMJ2000;321:73–77.577. Parisi AF, Folland ED, Hartigan P. A comparis<strong>on</strong> <strong>of</strong> angioplasty withmedical <strong>the</strong>rapy in <strong>the</strong> treatment <strong>of</strong> single-vessel cor<strong>on</strong>ary arterydisease. Veterans Affairs ACME Investigators. N Engl J Med1992;326:10–16.578. Folland ED, Hartigan PM, Parisi AF. Percutaneous transluminal cor<strong>on</strong>aryangioplasty versus medical <strong>the</strong>rapy for stable angina pectoris: outcomesfor patients with double-vessel versus single-vessel cor<strong>on</strong>ary arterydisease in a Veterans Affairs Cooperative randomized trial. VeteransAffairs ACME InvestigatorS. J Am Coll <strong>Cardio</strong>l 1997;29:1505–1511.579. RITA-2 trial participants. Cor<strong>on</strong>ary angioplasty versus medical <strong>the</strong>rapyfor angina: <strong>the</strong> sec<strong>on</strong>d Randomised Interventi<strong>on</strong> Treatment <strong>of</strong> <strong>Angina</strong>(RITA-2) trial participants. Lancet 1997;350:461–468.580. Pitt B, Waters D, Brown WV, van Boven AJ, Schwartz L, Title LM et al.Aggressive lipid-lowering <strong>the</strong>rapy compared with angioplasty in stablecor<strong>on</strong>ary artery disease. Atorvastatin versus Revascularizati<strong>on</strong>Treatment Investigators. N Engl J Med 1999;341:70–76.581. Brophy JM, Belisle P, Joseph L. Evidence for use <strong>of</strong> cor<strong>on</strong>ary stents.A hierarchical bayesian meta-analysis. Ann Intern Med 2003;138:777–786.582. Al Suwaidi J, Holmes DR Jr, Salam AM, Lenn<strong>on</strong> R, Berger PB. Impact <strong>of</strong>cor<strong>on</strong>ary artery stents <strong>on</strong> mortality and n<strong>on</strong>fatal myocardial infarcti<strong>on</strong>:meta-analysis <strong>of</strong> randomized trials comparing a strategy <strong>of</strong> routinestenting with that <strong>of</strong> ballo<strong>on</strong> angioplasty. Am Heart J 2004;147:815–822.583. Morice MC, Serruys PW, Sousa JE, Fajadet J, Ban Hayashi E, Perin Met al. A randomized comparis<strong>on</strong> <strong>of</strong> a sirolimus-eluting stent with a standardstent for cor<strong>on</strong>ary revascularizati<strong>on</strong>. N Engl J Med2002;346:1773–1780.584. Lansky AJ, Costa RA, Mintz GS, Tsuchiya Y, Midei M, Cox DA et al.N<strong>on</strong>-polymer-based paclitaxel-coated cor<strong>on</strong>ary stents for <strong>the</strong> treatment<strong>of</strong> patients with de novo cor<strong>on</strong>ary lesi<strong>on</strong>s: angiographic follow-up <strong>of</strong> <strong>the</strong>DELIVER clinical trial. Circulati<strong>on</strong> 2004;109:1948–1954.585. Moses JW, Le<strong>on</strong> MB, Popma JJ, Fitzgerald PJ, Holmes DR, O’ShaughnessyC et al. Sirolimus-eluting stents versus standard stents in patients withstenosis in a native cor<strong>on</strong>ary artery. N Engl J Med 2003;349:1315–1323.586. St<strong>on</strong>e GW, Ellis SG, Cox DA, Hermiller J, O’Shaughnessy C, Mann JT et al.A polymer-based, paclitaxel-eluting stent in patients with cor<strong>on</strong>aryartery disease. NEnglJMed2004;350:221–231.
ESC <str<strong>on</strong>g>Guidelines</str<strong>on</strong>g> 61587. Silber S, Albertss<strong>on</strong> P, Aviles FF, Camici PG, Colombo A, Hamm C et al.<str<strong>on</strong>g>Guidelines</str<strong>on</strong>g> for percutaneous cor<strong>on</strong>ary interventi<strong>on</strong>s. The Task Forcefor Percutaneous Cor<strong>on</strong>ary Interventi<strong>on</strong>s <strong>of</strong> <strong>the</strong> European Society <strong>of</strong><strong>Cardio</strong>logy. Eur Heart J 2005;26:804–847.588. Pfisterer ME, Kiowski W, Brunner H, Burckhardt D, Burkart F. L<strong>on</strong>g-termbenefit <strong>of</strong> 1-year amiodar<strong>on</strong>e treatment for persistent complex ventriculararrhythmias after myocardial infarcti<strong>on</strong>. Circulati<strong>on</strong> 1993;87:309–311.589. Hueb WA, Bellotti G, de Oliveira SA, Arie S, de Albuquerque CP, JateneAD et al. The Medicine, Angioplasty or Surgery Study (MASS): a prospective,randomized trial <strong>of</strong> medical <strong>the</strong>rapy, ballo<strong>on</strong> angioplasty or bypasssurgery for single proximal left anterior descending artery stenoses. JAm Coll <strong>Cardio</strong>l 1995;26:1600–1605.590. The Bypass Angioplasty Revascularizati<strong>on</strong> Investigati<strong>on</strong> (BARI)Investigators. Comparis<strong>on</strong> <strong>of</strong> cor<strong>on</strong>ary bypass surgery with angioplastyin patients with multivessel disease. N Engl J Med 1996;335:217–225.591. King SB III, Lembo NJ, Weintraub WS, Kosinski AS, Barnhart HX, Kutner MHet al. A randomized trial comparing cor<strong>on</strong>ary angioplasty with cor<strong>on</strong>arybypass surgery. Emory Angioplasty versus Surgery Trial (EAST). NEnglJMed 1994;331:1044–1050.592. Cor<strong>on</strong>ary angioplasty versus cor<strong>on</strong>ary artery bypass surgery: <strong>the</strong>Randomized Interventi<strong>on</strong> Treatment <strong>of</strong> <strong>Angina</strong> (RITA) trial. Lancet1993;341:573–580.593. Henders<strong>on</strong> RA, Pocock SJ, Sharp SJ, Nanchahal K, Sculpher MJ, Buxt<strong>on</strong> MJet al. L<strong>on</strong>g-term results <strong>of</strong> RITA-1 trial: clinical and cost comparis<strong>on</strong>s<strong>of</strong> cor<strong>on</strong>ary angioplasty and cor<strong>on</strong>ary-artery bypass grafting.Randomised Interventi<strong>on</strong> Treatment <strong>of</strong> <strong>Angina</strong>. Lancet 1998;352:1419–1425.594. Rodriguez A, Boull<strong>on</strong> F, Perez-Balino N, Paviotti C, Liprandi MI, PalaciosIF. Argentine randomized trial <strong>of</strong> percutaneous transluminal cor<strong>on</strong>aryangioplasty versus cor<strong>on</strong>ary artery bypass surgery in multivesseldisease (ERACI): in-hospital results and 1-year follow-up. ERACI Group.J Am Coll <strong>Cardio</strong>l 1993;22:1060–1067.595. Rodriguez A, Mele E, Peyregne E, Bull<strong>on</strong> F, Perez-Balino N, Liprandi MIet al. 3 year follow-up <strong>of</strong> <strong>the</strong> Argentine Randomized Trial <strong>of</strong>Percutaneous Transluminal Cor<strong>on</strong>ary Angioplasty versus Cor<strong>on</strong>aryArtery Bypass Surgery in Multivessel Disease (ERACI). J Am Coll<strong>Cardio</strong>l 1996;27:1178–1184.596. CABRI Trial Participants. First-year results <strong>of</strong> CABRI (Cor<strong>on</strong>aryAngioplasty versus Bypass Revascularisati<strong>on</strong> Investigati<strong>on</strong>). Lancet1995;346:1179–1184.597. SoS Investigators. Cor<strong>on</strong>ary artery bypass surgery versus percutaneouscor<strong>on</strong>ary interventi<strong>on</strong> with stent implantati<strong>on</strong> in patients with multivesselcor<strong>on</strong>ary artery disease (<strong>the</strong> Stent or Surgery trial): a randomisedc<strong>on</strong>trolled trial. Lancet 2002;360:965–970.598. Goy JJ, Kaufmann U, Goy-Eggenberger D, Garachemani A, Hurni M,Carrel T et al. A prospective randomized trial comparing stenting tointernal mammary artery grafting for proximal, isolated de novo leftanterior cor<strong>on</strong>ary artery stenosis: <strong>the</strong> SIMA trial. Stenting vs. InternalMammary Artery. Mayo Clin Proc 2000;75:1116–1123.599. Pocock SJ, Henders<strong>on</strong> RA, Rickards AF, Hampt<strong>on</strong> JR, King SB III, HammCW et al. Meta-analysis <strong>of</strong> randomised trials comparing cor<strong>on</strong>ary angioplastywith bypass surgery. Lancet 1995;346:1184–1189.600. Serruys PW, Unger F, Sousa JE, Jatene A, B<strong>on</strong>nier HJ, Sch<strong>on</strong>berger JPet al. Comparis<strong>on</strong> <strong>of</strong> cor<strong>on</strong>ary-artery bypass surgery and stenting for<strong>the</strong> treatment <strong>of</strong> multivessel disease. N Engl J Med2001;344:1117–1124.601. Mercado N, Wijns W, Serruys PW, Sigwart U, Fla<strong>the</strong>r MD, <strong>Stable</strong>s RHet al. 1 year outcomes <strong>of</strong> cor<strong>on</strong>ary artery bypass graft surgery versuspercutaneous cor<strong>on</strong>ary interventi<strong>on</strong> with multiple stenting for multisystemdisease: a meta-analysis <strong>of</strong> individual patient data from randomizedclinical trials. J Thorac <strong>Cardio</strong>vasc Surg 2005;130:512–519.602. Hannan EL, Racz MJ, Walford G, J<strong>on</strong>es RH, Ryan TJ, Bennett E et al.L<strong>on</strong>g-term outcomes <strong>of</strong> cor<strong>on</strong>ary-artery bypass grafting versus stentimplantati<strong>on</strong>. N Engl J Med 2005;352:2174–2183.603. Joyce D, Loebe M, No<strong>on</strong> GP, McRee S, Southard R, Thomps<strong>on</strong> L et al.Revascularizati<strong>on</strong> and ventricular restorati<strong>on</strong> in patients with ischaemicheart failure: <strong>the</strong> STICH trial. Curr Opin <strong>Cardio</strong>l 2003;18:454–457.604. Cleland JG, Freemantle N, Ball SG, B<strong>on</strong>ser RS, Camici P, Chattopadhyay Set al. The heart failure revascularisati<strong>on</strong> trial (HEART): rati<strong>on</strong>ale, designand methodology. Eur J Heart Fail 2003;5:295–303.605. Silvestri M, Barragan P, Sainsous J, Bayet G, Sime<strong>on</strong>i JB, Roquebert POet al. Unprotected left main cor<strong>on</strong>ary artery stenting: immediate andmedium-term outcomes <strong>of</strong> 140 elective procedures. J Am Coll <strong>Cardio</strong>l2000;35:1543–1550.606. Black A, Cortina R, Bossi I, Choussat R, Fajadet J, Marco J. Unprotectedleft main cor<strong>on</strong>ary artery stenting: correlates <strong>of</strong> midterm survival andimpact <strong>of</strong> patient selecti<strong>on</strong>. J Am Coll <strong>Cardio</strong>l 2001;37:832–838.607. Park SJ, Kim YH, Lee BK, Lee SW, Lee CW, H<strong>on</strong>g MK et al.Sirolimus-eluting stent implantati<strong>on</strong> for unprotected left main cor<strong>on</strong>aryartery stenosis: comparis<strong>on</strong> with bare metal stent implantati<strong>on</strong>. JAmColl <strong>Cardio</strong>l 2005;45:351–356.608. Flaherty JD, Davids<strong>on</strong> CJ. Diabetes and cor<strong>on</strong>ary revascularizati<strong>on</strong>.JAMA 2005;293:1501–1508.609. Brooks RC, Detre KM. Clinical trials <strong>of</strong> revascularizati<strong>on</strong> <strong>the</strong>rapy in diabetics.Curr Opin <strong>Cardio</strong>l 2000;15:287–292.610. 7 year outcome in <strong>the</strong> Bypass Angioplasty Revascularizati<strong>on</strong>Investigati<strong>on</strong> (BARI) by treatment and diabetic status. J Am Coll<strong>Cardio</strong>l 2000;35:1122–1129.611. Sch<strong>of</strong>er J, Schluter M, Gershlick AH, Wijns W, Garcia E, Schampaert Eet al. Sirolimus-eluting stents for treatment <strong>of</strong> patients with l<strong>on</strong>g a<strong>the</strong>roscleroticlesi<strong>on</strong>s in small cor<strong>on</strong>ary arteries: double-blind, randomisedc<strong>on</strong>trolled trial (E-SIRIUS). Lancet 2003;362:1093–1099.612. Lytle BW, Loop FD, Taylor PC, Simpfendorfer C, Kramer JR, Ratliff NBet al. Vein graft disease: <strong>the</strong> clinical impact <strong>of</strong> stenoses in saphenousvein bypass grafts to cor<strong>on</strong>ary arteries. J Thorac <strong>Cardio</strong>vasc Surg1992;103:831–840.613. Lytle BW, Loop FD, Taylor PC, Goormastic M, Stewart RW, Novoa R et al.The effect <strong>of</strong> cor<strong>on</strong>ary reoperati<strong>on</strong> <strong>on</strong> <strong>the</strong> survival <strong>of</strong> patients withstenoses in saphenous vein bypass grafts to cor<strong>on</strong>ary arteries. JThorac <strong>Cardio</strong>vasc Surg 1993;105:605–612; discussi<strong>on</strong> 612–614.614. Eagle KA, Guyt<strong>on</strong> RA, David<strong>of</strong>f R, Edwards FH, Ewy GA, Gardner TJ et al.ACC/AHA 2004 guideline update for cor<strong>on</strong>ary artery bypass graftsurgery: summary article. A report <strong>of</strong> <strong>the</strong> American College <strong>of</strong><strong>Cardio</strong>logy/American Heart Associati<strong>on</strong> Task Force <strong>on</strong> Practice<str<strong>on</strong>g>Guidelines</str<strong>on</strong>g> (Committee to Update <strong>the</strong> 1999 <str<strong>on</strong>g>Guidelines</str<strong>on</strong>g> for Cor<strong>on</strong>aryArtery Bypass Graft Surgery). J Am Coll <strong>Cardio</strong>l 2004;44:1146–54–1213–310.615. Baim DS, Wahr D, George B, Le<strong>on</strong> MB, Greenberg J, Cutlip DE et al.Randomized trial <strong>of</strong> a distal embolic protecti<strong>on</strong> device during percutaneousinterventi<strong>on</strong> <strong>of</strong> saphenous vein aorto-cor<strong>on</strong>ary bypass grafts.Circulati<strong>on</strong> 2002;105:1285–1290.616. Sirnes PA, Golf S, Myreng Y, Molstad P, Emanuelss<strong>on</strong> H, Albertss<strong>on</strong> P et al.Stenting in Chr<strong>on</strong>ic Cor<strong>on</strong>ary Occlusi<strong>on</strong> (SICCO): a randomized, c<strong>on</strong>trolledtrial <strong>of</strong> adding stent implantati<strong>on</strong> after successful angioplasty.J Am Coll <strong>Cardio</strong>l 1996;28:1444–1451.617. Rubartelli P, Verna E, Niccoli L, Giachero C, Zimarino M, Bernardi Get al. Cor<strong>on</strong>ary stent implantati<strong>on</strong> is superior to ballo<strong>on</strong> angioplastyfor chr<strong>on</strong>ic cor<strong>on</strong>ary occlusi<strong>on</strong>s: 6 year clinical follow-up <strong>of</strong> <strong>the</strong>GISSOC trial. J Am Coll <strong>Cardio</strong>l 2003;41:1488–1492.618. Dzavik V, Carere RG, Teo KK, Knudts<strong>on</strong> ML, Marquis JF, Buller CE. Anopen design, multicentre, randomized trial <strong>of</strong> percutaneous transluminalcor<strong>on</strong>ary angioplasty versus stenting, with a heparin-coated stent,<strong>of</strong> totally occluded cor<strong>on</strong>ary arteries: rati<strong>on</strong>ale, trial design and baselinepatient characteristics. Total Occlusi<strong>on</strong> Study <strong>of</strong> Canada (TOSCA)Investigators. Can J <strong>Cardio</strong>l 1998;14:825–832.619. Douglas PS, Ginsburg GS. The evaluati<strong>on</strong> <strong>of</strong> chest pain in women. N EnglJ Med 1996;334:1311–1315.620. Lerner DJ, Kannel WB. Patterns <strong>of</strong> cor<strong>on</strong>ary heart disease morbidity andmortality in <strong>the</strong> sexes: a 26-year follow-up <strong>of</strong> <strong>the</strong> Framingham populati<strong>on</strong>.Am Heart J 1986;111:383–390.621. Campbell MJ, Elwood PC, Abbas S, Waters WE. Chest pain in women: astudy <strong>of</strong> prevalence and mortality follow up in south Wales. J EpidemiolCommunity Health 1984;38:17–20.622. Shaper AG, Cook DG, Walker M, Macfarlane PW. Prevalence <strong>of</strong> ischaemicheart disease in middle aged British men. Br Heart J 1984;51:595–605.623. Philpott S, Boynt<strong>on</strong> PM, Feder G, Hemingway H. Gender differences indescripti<strong>on</strong>s <strong>of</strong> angina symptoms and health problems immediatelyprior to angiography: <strong>the</strong> ACRE study. Appropriateness <strong>of</strong> Cor<strong>on</strong>aryRevascularisati<strong>on</strong> study. Soc Sci Med 2001;52:1565–1575.624. Chaitman BR, Bourassa MG, Davis K, Rogers WJ, Tyras DH, Berger R et al.Angiographic prevalence <strong>of</strong> high-risk cor<strong>on</strong>ary artery disease in patientsubsets (CASS). Circulati<strong>on</strong> 1981;64:360–367.625. Villareal RPWJ. N<strong>on</strong>invasive diagnostic testing. In: Wilansky SWJ, ed.Heart Disease in Women. Philadelphia: Churchill Livingst<strong>on</strong>e; 2002.P149–157.626. Osbakken MD, Okada RD, Boucher CA, Strauss HW, Pohost GM.Comparis<strong>on</strong> <strong>of</strong> exercise perfusi<strong>on</strong> and ventricular functi<strong>on</strong> imaging: ananalysis <strong>of</strong> factors affecting <strong>the</strong> diagnostic accuracy <strong>of</strong> each technique.J Am Coll <strong>Cardio</strong>l 1984;3:272–283.
62 ESC <str<strong>on</strong>g>Guidelines</str<strong>on</strong>g>627. DePuey EG, Rozanski A. Using gated technetium-99m-sestamibi SPECTto characterize fixed myocardial defects as infarct or artifact. J NuclMed 1995;36:952–955.628. Dodi C, Cortigiani L, Masini M, Olivotto I, Azzarelli A, Nannini E. Theincremental prognostic value <strong>of</strong> pharmacological stress echo over exerciseelectrocardiography in women with chest pain <strong>of</strong> unknown origin.Eur Heart J 2001;22:145–152.629. Cortigiani L, Dodi C, Paolini EA, Bernardi D, Bruno G, Nannini E.Prognostic value <strong>of</strong> pharmacological stress echocardiography inwomen with chest pain and unknown cor<strong>on</strong>ary artery disease. JAmColl <strong>Cardio</strong>l 1998;32:1975–1981.630. Melin JA, Wijns W, Vanbutsele RJ, Robert A, De Coster P, Brasseur LAet al. Alternative diagnostic strategies for cor<strong>on</strong>ary artery disease inwomen: dem<strong>on</strong>strati<strong>on</strong> <strong>of</strong> <strong>the</strong> usefulness and efficiency <strong>of</strong> probabilityanalysis. Circulati<strong>on</strong> 1985;71:535–542.631. Clarke KW, Gray D, Keating NA, Hampt<strong>on</strong> JR. Do women with acute myocardialinfarcti<strong>on</strong> receive <strong>the</strong> same treatment as men? BMJ1994;309:563–566.632. Vaccarino V, Krumholz HM, Berkman LF, Horwitz RI. Sex differences inmortality after myocardial infarcti<strong>on</strong>. Is <strong>the</strong>re evidence for an increasedrisk for women? Circulati<strong>on</strong> 1995;91:1861–1871.633. Vaccarino V, Krumholz HM, Yarzebski J, Gore JM, Goldberg RJ. Sexdifferences in 2-year mortality after hospital discharge for myocardialinfarcti<strong>on</strong>. Ann Intern Med 2001;134:173–181.634. Roeters van Lennep JE, Zwinderman AH, Roeters van Lennep HW,Westerveld HE, Plokker HW, Voors AA et al. Gender differences in diagnosisand treatment <strong>of</strong> cor<strong>on</strong>ary artery disease from 1981 to 1997. Noevidence for <strong>the</strong> Yentl syndrome. Eur Heart J 2000;21:911–918.635. Daly CA, Clemens F, Send<strong>on</strong> JL, Tavazzi L, Boersma E, Danchin N, DelahayeF, Gitt A, Julian D, Mulcahy D, Ruzyllo W, Thygesen K, Verheugt F,Fox KM; Euro Heart Survey Investigators. Gender differences in<strong>the</strong> management and clinical outcome <strong>of</strong> stable angina. Circulati<strong>on</strong>2006;113:467–469.636. Sowers JR. Diabetes in <strong>the</strong> elderly and in women: cardiovascular risks.<strong>Cardio</strong>l Clin 2004;22:541–551, vi.637. McFarlane SI, Banerji M, Sowers JR. Insulin resistance and cardiovasculardisease. J Clin Endocrinol Metab 2001;86:713–718.638. Blendea MC, McFarlane SI, Isenovic ER, Gick G, Sowers JR. Heart diseasein diabetic patients. Curr Diab Rep 2003;3:223–229.639. Turner RC, Millns H, Neil HA, Stratt<strong>on</strong> IM, Manley SE, Mat<strong>the</strong>ws DR et al.Risk factors for cor<strong>on</strong>ary artery disease in n<strong>on</strong>-insulin dependent diabetesmellitus: United Kingdom Prospective Diabetes Study (UKPDS:23). BMJ 1998;316:823–828.640. Wei M, Gaskill SP, Haffner SM, Stern MP. Effects <strong>of</strong> diabetes and level <strong>of</strong>glycemia <strong>on</strong> all-cause and cardiovascular mortality. The San Ant<strong>on</strong>ioHeart Study. Diabetes Care 1998;21:1167–1172.641. Young LH, Jose P, Chyun D. Diagnosis <strong>of</strong> CAD in patients with diabetes:who to evaluate. Curr Diab Rep 2003;3:19–27.642. Anand DV, Lim E, Lahiri A, Bax JJ. The role <strong>of</strong> n<strong>on</strong>-invasive imaging in<strong>the</strong> risk stratificati<strong>on</strong> <strong>of</strong> asymptomatic diabetic subjects. Eur Heart J.2005.643. Giri S, Shaw LJ, Murthy DR, Travin MI, Miller DD, Hachamovitch R et al.Impact <strong>of</strong> diabetes <strong>on</strong> <strong>the</strong> risk stratificati<strong>on</strong> using stress single-phot<strong>on</strong>emissi<strong>on</strong> computed tomography myocardial perfusi<strong>on</strong> imaging inpatients with symptoms suggestive <strong>of</strong> cor<strong>on</strong>ary artery disease.Circulati<strong>on</strong> 2002;105:32–40.644. Fang ZY, Sharman J, Prins JB, Marwick TH. Determinants <strong>of</strong> exercisecapacity in patients with type 2 diabetes. Diabetes Care 2005;28:1643–1648.645. The AACE System <strong>of</strong> intensive diabetes self-management-2002 update.The American Associati<strong>on</strong> <strong>of</strong> Clinical Endocrinologists Medical<str<strong>on</strong>g>Guidelines</str<strong>on</strong>g> for <strong>the</strong> management <strong>of</strong> diabetes mellitus. Endocr PractSuppl 2002;8(Suppl.):40–82.646. UK Prospective Diabetes Study (UKPDS) Group. Intensive blood-glucosec<strong>on</strong>trol with sulph<strong>on</strong>ylureas or insulin compared with c<strong>on</strong>venti<strong>on</strong>altreatment and risk <strong>of</strong> complicati<strong>on</strong>s in patients with type 2 diabetes(UKPDS 33). Lancet 1998;352:837–853.647. Hellman R, Regan J, Rosen H. Effect <strong>of</strong> intensive treatment <strong>of</strong> diabetes<strong>of</strong> <strong>the</strong> risk <strong>of</strong> death or renal failure in NIDDM and IDDM. Diabetes Care1997;20:258–264.648. The American Associati<strong>on</strong> <strong>of</strong> Clinical Endocrinologists Medical <str<strong>on</strong>g>Guidelines</str<strong>on</strong>g>for <strong>the</strong> <strong>Management</strong> <strong>of</strong> Diabetes Mellitus: <strong>the</strong> AACE system <strong>of</strong> intensivediabetes self-management–2000 update. Endocr Pract 2000;6:43–84.649. Standl E, Schnell O. A new look at <strong>the</strong> heart in diabetes mellitus: fromailing to failing. Diabetologia 2000;43:1455–1469.650. Way KJ, Katai N, King GL. Protein kinase C and <strong>the</strong> development <strong>of</strong>diabetic vascular complicati<strong>on</strong>s. Diabet Med 2001;18:945–959.651. Lernfelt B, Landahl S, Svanborg A. Cor<strong>on</strong>ary heart disease at 70, 75 and79 years <strong>of</strong> age: a l<strong>on</strong>gitudinal study with special reference to sex differencesand mortality. Age Ageing 1990;19:297–303.652. Kurita A, Takase B, Uehata A, Maruyama T, Nishioka T, Sugahara H et al.Painless myocardial ischemia in elderly patients compared withmiddle-aged patients and its relati<strong>on</strong> to treadmill testing and cor<strong>on</strong>aryhemodynamics. Clin <strong>Cardio</strong>l 1991;14:886–890.653. Vasilomanolakis EC. Geriatric cardiology: when exercise stress testing isjustified. Geriatrics 1985;40:47–50–53–4, 57.654. Kasser IS, Bruce RA. Comparative effects <strong>of</strong> aging and cor<strong>on</strong>ary heart disease<strong>on</strong> submaximal and maximal exercise. Circulati<strong>on</strong> 1969;39:759–774.655. Mehran R, Aym<strong>on</strong>g ED, Nikolsky E, Lasic Z, Iakovou I, Fahy M et al. Asimple risk score for predicti<strong>on</strong> <strong>of</strong> c<strong>on</strong>trast-induced nephropathy afterpercutaneous cor<strong>on</strong>ary interventi<strong>on</strong>: development and initial validati<strong>on</strong>.J Am Coll <strong>Cardio</strong>l 2004;44:1393–1399.656. M<strong>on</strong>tamat SC, Cusack BJ, Vestal RE. <strong>Management</strong> <strong>of</strong> drug <strong>the</strong>rapy in <strong>the</strong>elderly. N Engl J Med 1989;321:303–309.657. Gundersen T, Abrahamsen AM, Kjekshus J, R<strong>on</strong>nevik PK. Timolol-relatedreducti<strong>on</strong> in mortality and reinfarcti<strong>on</strong> in patients ages 65-75 yearssurviving acute myocardial infarcti<strong>on</strong>. Prepared for <strong>the</strong> NorwegianMulticentre Study Group. Circulati<strong>on</strong> 1982;66:1179–1184.658. Metzger JP, Tab<strong>on</strong>e X, Georges JL, Gueniche C, Detienne JP, Le Feuvre Cet al. Cor<strong>on</strong>ary angioplasty in patients 75 years and older; comparis<strong>on</strong>with cor<strong>on</strong>ary bypass surgery. Eur Heart J 1994;15:213–217.659. B<strong>on</strong>nier H, de Vries C, Michels R, el Gamal M. Initial and l<strong>on</strong>g-termresults <strong>of</strong> cor<strong>on</strong>ary angioplasty and cor<strong>on</strong>ary bypass surgery in patients<strong>of</strong> 75 or older. Br Heart J 1993;70:122–125.660. Mannheimer C, Camici P, Chester MR, Collins A, DeJ<strong>on</strong>gste M, Eliass<strong>on</strong> Tet al. The problem <strong>of</strong> chr<strong>on</strong>ic refractory angina; report from <strong>the</strong> ESCJoint Study Group <strong>on</strong> <strong>the</strong> Treatment <strong>of</strong> Refractory <strong>Angina</strong>. Eur Heart J2002;23:355–370.661. Brorss<strong>on</strong> B, Bernstein SJ, Brook RH, Werko L. Quality <strong>of</strong> life <strong>of</strong> patientswith chr<strong>on</strong>ic stable angina before and 4 years after cor<strong>on</strong>ary revascularisati<strong>on</strong>compared with a normal populati<strong>on</strong>. Heart 2002;87:140–145.662. Bernstein SJ, Brorss<strong>on</strong> B, Aberg T, Emanuelss<strong>on</strong> H, Brook RH, Werko L.Appropriateness <strong>of</strong> referral <strong>of</strong> cor<strong>on</strong>ary angiography patients inSweden. SECOR/SBU Project Group. Heart 1999;81:470–477.663. Yang EH, Barsness GW, Gersh BJ, Chandrasekaran K, Lerman A. Currentand future treatment strategies for refractory angina. Mayo Clin Proc2004;79:1284–1292.664. Faircloth ME, Redwood SR, Marber MS. Strategies for refractory angina–electricnot eclectic? Int J Clin Pract 2004;58:650–652.665. Kim MC, Kini A, Sharma SK. Refractory angina pectoris: mechanism and<strong>the</strong>rapeutic opti<strong>on</strong>s. J Am Coll <strong>Cardio</strong>l 2002;39:923–934.666. Arora RR, Chou TM, Jain D, Fleishman B, Crawford L, McKiernan T et al.The multicenter study <strong>of</strong> enhanced external counterpulsati<strong>on</strong>(MUST-EECP): effect <strong>of</strong> EECP <strong>on</strong> exercise-induced myocardial ischemiaand anginal episodes. J Am Coll <strong>Cardio</strong>l 1999;33:1833–1840.667. Soran O, Kennard ED, Kelsey SF, Holubkov R, Strobeck J, Feldman AM.Enhanced external counterpulsati<strong>on</strong> as treatment for chr<strong>on</strong>ic anginain patients with left ventricular dysfuncti<strong>on</strong>: a report from <strong>the</strong>Internati<strong>on</strong>al EECP Patient Registry (IEPR). C<strong>on</strong>gest Heart Fail2002;8:297–302.668. Linnemeier G, Rutter MK, Barsness G, Kennard ED, Nesto RW. EnhancedExternal Counterpulsati<strong>on</strong> for <strong>the</strong> relief <strong>of</strong> angina in patients with diabetes:safety, efficacy and 1-year clinical outcomes. Am Heart J2003;146:453–458.669. Allen KB, Dowling RD, Angell WW, Gangahar DM, Fudge TL, Richenbacher Wet al. Transmyocardial revascularizati<strong>on</strong>: 5-year follow-up <strong>of</strong> a prospective,randomized multicenter trial. Ann Thorac Surg 2004;77:1228–1234.670. Schneider J, Diegeler A, Krakor R, Wal<strong>the</strong>r T, Kluge R, Mohr FW.Transmyocardial laser revascularizati<strong>on</strong> with <strong>the</strong> holmium:YAG laser:loss <strong>of</strong> symptomatic improvement after 2 years. Eur J <strong>Cardio</strong>thoracSurg 2001;19:164–169.671. Sch<strong>of</strong>ield PM, Sharples LD, Caine N, Burns S, Tait S, Wistow T et al.Transmyocardial laser revascularisati<strong>on</strong> in patients with refractoryangina: a randomised c<strong>on</strong>trolled trial. Lancet 1999;353:519–524.672. Le<strong>on</strong> MB, Kornowski R, Downey WE, Weisz G, Baim D, B<strong>on</strong>ow R,Hendel RC, Cohen D, Gervino E, Laham R, Lembo NJ, Moses JW, KuntzRE. A blinded, randomized, placebo-c<strong>on</strong>trolled trial <strong>of</strong> percutaneouslaser myocaridla revascularisati<strong>on</strong> to improve angina symptoms inpatients with severe cor<strong>on</strong>ary disease. J Am Coll <strong>Cardio</strong>l 2005;46:1812–1819.
ESC <str<strong>on</strong>g>Guidelines</str<strong>on</strong>g> 63673. Rimoldi O, Burns S, Rosen S, Wistow TE, Sch<strong>of</strong>ield PM, Taylor G, CamiciP. Measurement <strong>of</strong> myocardial blood flow with positorn eissi<strong>on</strong> tomographybefore and after transmyocardial laser revascularizati<strong>on</strong>.Circulati<strong>on</strong> 1999;100(Suppl. II):II134–II138.674. Daly CA, Clemens F, Send<strong>on</strong> JL, Tavazzi L, Boersma E, Danchin N et al.The clinical characteristics and investigati<strong>on</strong>s planned in patients withstable angina presenting to cardiologists in Europe: from <strong>the</strong> EuroHeart Survey <strong>of</strong> <strong>Stable</strong> <strong>Angina</strong>. Eur Heart J 2005;26:996–1010.675. Daly CA, Clemens F, Send<strong>on</strong> JL, Tavazzi L, Boersma E, Danchin N et al.The initial management <strong>of</strong> stable angina in Europe, from <strong>the</strong> EuroHeart Survey: a descripti<strong>on</strong> <strong>of</strong> pharmacological management and revascularizati<strong>on</strong>strategies initiated within <strong>the</strong> first m<strong>on</strong>th <strong>of</strong> presentati<strong>on</strong> toa cardiologist in <strong>the</strong> Euro Heart Survey <strong>of</strong> <strong>Stable</strong> <strong>Angina</strong>. Eur Heart J2005;26:1011–1022.676. Lopez-Send<strong>on</strong> J, Swedberg K, McMurray J, Tamargo J, Maggi<strong>on</strong>i AP,Dargie H et al. Expert c<strong>on</strong>sensus document <strong>on</strong> angiotensin c<strong>on</strong>vertingenzyme inhibitors in cardiovascular disease. The Task Force <strong>on</strong>ACE-inhibitors <strong>of</strong> <strong>the</strong> European Society <strong>of</strong> <strong>Cardio</strong>logy. Eur Heart J2004;25:1454–1470.677. Lopez-Send<strong>on</strong> J, Swedberg K, McMurray J, Tamargo J, Maggi<strong>on</strong>i AP,Dargie H et al. Expert c<strong>on</strong>sensus document <strong>on</strong> beta-adrenergic receptorblockers. Eur Heart J 2004;25:1341–1362.678. Mieres JH, Shaw LJ, Hendel RC, Miller DD, B<strong>on</strong>ow RO, Berman DS et al.American Society <strong>of</strong> Nuclear <strong>Cardio</strong>logy c<strong>on</strong>sensus statement: TaskForce <strong>on</strong> Women and Cor<strong>on</strong>ary Artery Disease–<strong>the</strong> role <strong>of</strong> myocardialperfusi<strong>on</strong> imaging in <strong>the</strong> clinical evaluati<strong>on</strong> <strong>of</strong> cor<strong>on</strong>ary artery diseasein women [correcti<strong>on</strong>]. J Nucl <strong>Cardio</strong>l 2003;10:95–101.679. Scanl<strong>on</strong> PJ, Fax<strong>on</strong> DP, Audet AM, Carabello B, Dehmer GJ, Eagle KAet al. ACC/AHA guidelines for cor<strong>on</strong>ary angiography. A report <strong>of</strong> <strong>the</strong>American College <strong>of</strong> <strong>Cardio</strong>logy/American Heart Associati<strong>on</strong> TaskForce <strong>on</strong> practice guidelines (Committee <strong>on</strong> Cor<strong>on</strong>ary Angiography).Developed in collaborati<strong>on</strong> with <strong>the</strong> Society for Cardiac Angiographyand Interventi<strong>on</strong>s. J Am Coll <strong>Cardio</strong>l 1999;33:1756–1824.680. <strong>Management</strong> <strong>of</strong> stable angina pectoris. Recommendati<strong>on</strong>s <strong>of</strong> <strong>the</strong> TaskForce <strong>of</strong> <strong>the</strong> European Society <strong>of</strong> <strong>Cardio</strong>logy. Eur Heart J1997;18:394–413.681. Weiner DA, Ryan TJ, Pars<strong>on</strong>s L, Fisher LD, Chaitman BR, Sheffield LTet al. L<strong>on</strong>g-term prognostic value <strong>of</strong> exercise testing in men andwomen from <strong>the</strong> Cor<strong>on</strong>ary Artery Surgery Study (CASS) registry. Am J<strong>Cardio</strong>l 1995;75:865–870.682. Alexander KP, Shaw LJ, Shaw LK, Del<strong>on</strong>g ER, Mark DB, Peters<strong>on</strong> ED. Value<strong>of</strong> exercise treadmill testing in women. J Am Coll <strong>Cardio</strong>l1998;32:1657–1664.683. Goraya TY, Jacobsen SJ, Pellikka PA, Miller TD, Khan A, West<strong>on</strong> SA et al.Prognostic value <strong>of</strong> treadmill exercise testing in elderly pers<strong>on</strong>s. AnnIntern Med 2000;132:862–870.The CME Text ‘<str<strong>on</strong>g>Guidelines</str<strong>on</strong>g> <strong>on</strong> <strong>the</strong> <strong>Management</strong> <strong>of</strong> <strong>Stable</strong> <strong>Angina</strong> <strong>Pectoris</strong>’ is accredited by <strong>the</strong> European Board forAccreditati<strong>on</strong> in <strong>Cardio</strong>logy (EBAC) for ‘2’ hours <strong>of</strong> External CME credits. Each participant should claim <strong>on</strong>ly those hours <strong>of</strong>credit that have actually been spent in <strong>the</strong> educati<strong>on</strong>al activity. EBAC works according to <strong>the</strong> quality standards <strong>of</strong> <strong>the</strong>European Accreditati<strong>on</strong> Council for C<strong>on</strong>tinuing Medical Educati<strong>on</strong> (EACCME), which is an instituti<strong>on</strong> <strong>of</strong> <strong>the</strong> European Uni<strong>on</strong><strong>of</strong> Medical Specialists (UEMS).In compliance with EBAC/EACCME guidelines, all authors participating in this programme have disclosed potential c<strong>on</strong>flicts<strong>of</strong> interest that might cause a bias in <strong>the</strong> article. The Organizing Committee is resp<strong>on</strong>sible for ensuring that all potentialc<strong>on</strong>flicts <strong>of</strong> interest relevant to <strong>the</strong> programme are declared to <strong>the</strong> participants prior to <strong>the</strong> CME activities.