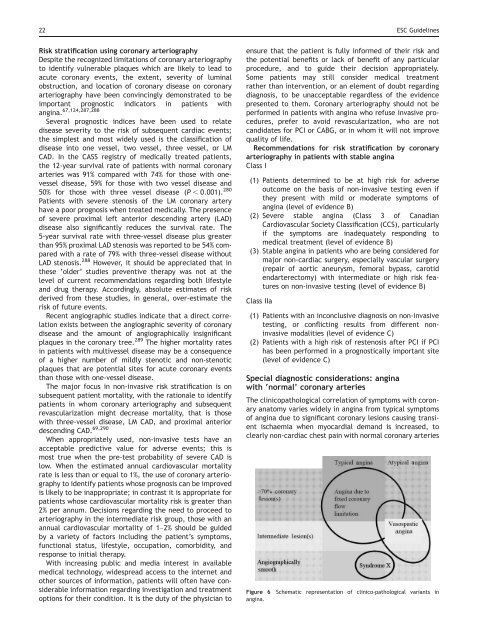
22 ESC <str<strong>on</strong>g>Guidelines</str<strong>on</strong>g>Risk stratificati<strong>on</strong> using cor<strong>on</strong>ary arteriographyDespite <strong>the</strong> recognized limitati<strong>on</strong>s <strong>of</strong> cor<strong>on</strong>ary arteriographyto identify vulnerable plaques which are likely to lead toacute cor<strong>on</strong>ary events, <strong>the</strong> extent, severity <strong>of</strong> luminalobstructi<strong>on</strong>, and locati<strong>on</strong> <strong>of</strong> cor<strong>on</strong>ary disease <strong>on</strong> cor<strong>on</strong>aryarteriography have been c<strong>on</strong>vincingly dem<strong>on</strong>strated to beimportant prognostic indicators in patients withangina. 67,124,287,288Several prognostic indices have been used to relatedisease severity to <strong>the</strong> risk <strong>of</strong> subsequent cardiac events;<strong>the</strong> simplest and most widely used is <strong>the</strong> classificati<strong>on</strong> <strong>of</strong>disease into <strong>on</strong>e vessel, two vessel, three vessel, or LMCAD. In <strong>the</strong> CASS registry <strong>of</strong> medically treated patients,<strong>the</strong> 12-year survival rate <strong>of</strong> patients with normal cor<strong>on</strong>aryarteries was 91% compared with 74% for those with <strong>on</strong>evesseldisease, 59% for those with two vessel disease and50% for those with three vessel disease (P , 0.001). 280Patients with severe stenosis <strong>of</strong> <strong>the</strong> LM cor<strong>on</strong>ary arteryhave a poor prognosis when treated medically. The presence<strong>of</strong> severe proximal left anterior descending artery (LAD)disease also significantly reduces <strong>the</strong> survival rate. The5-year survival rate with three-vessel disease plus greaterthan 95% proximal LAD stenosis was reported to be 54% comparedwith a rate <strong>of</strong> 79% with three-vessel disease withoutLAD stenosis. 288 However, it should be appreciated that in<strong>the</strong>se ‘older’ studies preventive <strong>the</strong>rapy was not at <strong>the</strong>level <strong>of</strong> current recommendati<strong>on</strong>s regarding both lifestyleand drug <strong>the</strong>rapy. Accordingly, absolute estimates <strong>of</strong> riskderived from <strong>the</strong>se studies, in general, over-estimate <strong>the</strong>risk <strong>of</strong> future events.Recent angiographic studies indicate that a direct correlati<strong>on</strong>exists between <strong>the</strong> angiographic severity <strong>of</strong> cor<strong>on</strong>arydisease and <strong>the</strong> amount <strong>of</strong> angiographically insignificantplaques in <strong>the</strong> cor<strong>on</strong>ary tree. 289 The higher mortality ratesin patients with multivessel disease may be a c<strong>on</strong>sequence<strong>of</strong> a higher number <strong>of</strong> mildly stenotic and n<strong>on</strong>-stenoticplaques that are potential sites for acute cor<strong>on</strong>ary eventsthan those with <strong>on</strong>e-vessel disease.The major focus in n<strong>on</strong>-invasive risk stratificati<strong>on</strong> is <strong>on</strong>subsequent patient mortality, with <strong>the</strong> rati<strong>on</strong>ale to identifypatients in whom cor<strong>on</strong>ary arteriography and subsequentrevascularizati<strong>on</strong> might decrease mortality, that is thosewith three-vessel disease, LM CAD, and proximal anteriordescending CAD. 69,290When appropriately used, n<strong>on</strong>-invasive tests have anacceptable predictive value for adverse events; this ismost true when <strong>the</strong> pre-test probability <strong>of</strong> severe CAD islow. When <strong>the</strong> estimated annual cardiovascular mortalityrate is less than or equal to 1%, <strong>the</strong> use <strong>of</strong> cor<strong>on</strong>ary arteriographyto identify patients whose prognosis can be improvedis likely to be inappropriate; in c<strong>on</strong>trast it is appropriate forpatients whose cardiovascular mortality risk is greater than2% per annum. Decisi<strong>on</strong>s regarding <strong>the</strong> need to proceed toarteriography in <strong>the</strong> intermediate risk group, those with anannual cardiovascular mortality <strong>of</strong> 1–2% should be guidedby a variety <strong>of</strong> factors including <strong>the</strong> patient’s symptoms,functi<strong>on</strong>al status, lifestyle, occupati<strong>on</strong>, comorbidity, andresp<strong>on</strong>se to initial <strong>the</strong>rapy.With increasing public and media interest in availablemedical technology, widespread access to <strong>the</strong> internet ando<strong>the</strong>r sources <strong>of</strong> informati<strong>on</strong>, patients will <strong>of</strong>ten have c<strong>on</strong>siderableinformati<strong>on</strong> regarding investigati<strong>on</strong> and treatmentopti<strong>on</strong>s for <strong>the</strong>ir c<strong>on</strong>diti<strong>on</strong>. It is <strong>the</strong> duty <strong>of</strong> <strong>the</strong> physician toensure that <strong>the</strong> patient is fully informed <strong>of</strong> <strong>the</strong>ir risk and<strong>the</strong> potential benefits or lack <strong>of</strong> benefit <strong>of</strong> any particularprocedure, and to guide <strong>the</strong>ir decisi<strong>on</strong> appropriately.Some patients may still c<strong>on</strong>sider medical treatmentra<strong>the</strong>r than interventi<strong>on</strong>, or an element <strong>of</strong> doubt regardingdiagnosis, to be unacceptable regardless <strong>of</strong> <strong>the</strong> evidencepresented to <strong>the</strong>m. Cor<strong>on</strong>ary arteriography should not beperformed in patients with angina who refuse invasive procedures,prefer to avoid revascularizati<strong>on</strong>, who are notcandidates for PCI or CABG, or in whom it will not improvequality <strong>of</strong> life.Recommendati<strong>on</strong>s for risk stratificati<strong>on</strong> by cor<strong>on</strong>aryarteriography in patients with stable anginaClass I(1) Patients determined to be at high risk for adverseoutcome <strong>on</strong> <strong>the</strong> basis <strong>of</strong> n<strong>on</strong>-invasive testing even if<strong>the</strong>y present with mild or moderate symptoms <strong>of</strong>angina (level <strong>of</strong> evidence B)(2) Severe stable angina (Class 3 <strong>of</strong> Canadian<strong>Cardio</strong>vascular Society Classificati<strong>on</strong> (CCS), particularlyif <strong>the</strong> symptoms are inadequately resp<strong>on</strong>ding tomedical treatment (level <strong>of</strong> evidence B)(3) <strong>Stable</strong> angina in patients who are being c<strong>on</strong>sidered formajor n<strong>on</strong>-cardiac surgery, especially vascular surgery(repair <strong>of</strong> aortic aneurysm, femoral bypass, carotidendarterectomy) with intermediate or high risk features<strong>on</strong> n<strong>on</strong>-invasive testing (level <strong>of</strong> evidence B)Class IIa(1) Patients with an inc<strong>on</strong>clusive diagnosis <strong>on</strong> n<strong>on</strong>-invasivetesting, or c<strong>on</strong>flicting results from different n<strong>on</strong>invasivemodalities (level <strong>of</strong> evidence C)(2) Patients with a high risk <strong>of</strong> restenosis after PCI if PCIhas been performed in a prognostically important site(level <strong>of</strong> evidence C)Special diagnostic c<strong>on</strong>siderati<strong>on</strong>s: anginawith ‘normal’ cor<strong>on</strong>ary arteriesThe clinicopathological correlati<strong>on</strong> <strong>of</strong> symptoms with cor<strong>on</strong>aryanatomy varies widely in angina from typical symptoms<strong>of</strong> angina due to significant cor<strong>on</strong>ary lesi<strong>on</strong>s causing transientischaemia when myocardial demand is increased, toclearly n<strong>on</strong>-cardiac chest pain with normal cor<strong>on</strong>ary arteriesFigure 6 Schematic representati<strong>on</strong> <strong>of</strong> clinico-pathological variants inangina.
ESC <str<strong>on</strong>g>Guidelines</str<strong>on</strong>g> 23<strong>on</strong> <strong>the</strong> o<strong>the</strong>r end <strong>of</strong> <strong>the</strong> spectrum. Spanning <strong>the</strong> extremes <strong>of</strong>this spectrum are a number <strong>of</strong> clinicopathological correlateswhich may overlap to a greater or lesser extent with eacho<strong>the</strong>r (Figure 6). These range from atypical anginal symptomswith significant cor<strong>on</strong>ary stenoses, which would fallunder <strong>the</strong> umbrella <strong>of</strong> <strong>the</strong> c<strong>on</strong>venti<strong>on</strong>al diagnosis <strong>of</strong> anginapectoris, to typical anginal symptoms with angiographicallynormal cor<strong>on</strong>ary arteries which might be described ascardiac Syndrome X. Vasospastic angina, caused by dynamiccor<strong>on</strong>ary obstructi<strong>on</strong> in cor<strong>on</strong>ary arteries which may beei<strong>the</strong>r angiographically smooth or significantly stenosed, is afur<strong>the</strong>r factor to be c<strong>on</strong>sidered in <strong>the</strong> diagnosis. A c<strong>on</strong>siderableproporti<strong>on</strong> <strong>of</strong> patients, especially women, who undergocor<strong>on</strong>ary arteriography because <strong>of</strong> symptoms <strong>of</strong> chest paindo not have significant CAD. 291 In <strong>the</strong>se patients, <strong>the</strong> features<strong>of</strong> chest pain may suggest <strong>on</strong>e <strong>of</strong> <strong>the</strong> following threepossibilities.. Pain involves a small porti<strong>on</strong> <strong>of</strong> <strong>the</strong> left hemithorax, lastsfor several hours or even days, is not relieved by nitroglycerin,and may be provoked by palpati<strong>on</strong> (n<strong>on</strong>-anginalpain, <strong>of</strong>ten musculoskeletal in origin). Pain has typical features <strong>of</strong> angina in terms <strong>of</strong> locati<strong>on</strong> anddurati<strong>on</strong> but occurs predominantly at rest (atypicalangina, which may be due to cor<strong>on</strong>ary spasm vasospasticangina). <strong>Angina</strong> with mostly typical features (although durati<strong>on</strong>may be prol<strong>on</strong>ged, and relati<strong>on</strong> to exercise somewhatinc<strong>on</strong>sistent) associated with abnormal results <strong>of</strong> stresstests (cardiac Syndrome X)Detailed discussi<strong>on</strong> <strong>of</strong> <strong>the</strong> management <strong>of</strong> <strong>the</strong> first groupis bey<strong>on</strong>d <strong>the</strong> scope <strong>of</strong> <strong>the</strong>se guidelines. With regard to<strong>the</strong> ‘atypical angina’ group, in general this term refers tosymptoms with any two <strong>of</strong> <strong>the</strong> three main features <strong>of</strong>typical angina pectoris as outlined in Table 2, and <strong>the</strong>term may be used interchangeably with ‘probable angina’.Suspected vasospastic angina is a specific subgroup <strong>of</strong> atypicalangina which is atypical <strong>on</strong>ly in that it lacks a c<strong>on</strong>sistentassociati<strong>on</strong> with exercise. O<strong>the</strong>r forms <strong>of</strong> atypical angina arenot discussed separately, but a brief descripti<strong>on</strong> <strong>of</strong> <strong>the</strong> diagnosticevaluati<strong>on</strong> <strong>of</strong> cardiac Syndrome X and vasospasticangina are outlined below.Syndrome XClinical picture. Although <strong>the</strong>re is no universally accepteddefiniti<strong>on</strong> <strong>of</strong> Syndrome X, to fulfil <strong>the</strong> classical descripti<strong>on</strong><strong>of</strong> ‘Syndrome X’ 292 requires <strong>the</strong> presence <strong>of</strong> <strong>the</strong> triad <strong>of</strong>:(1) Typical exercise-induced angina (with or withoutadditi<strong>on</strong>al resting angina and dyspnoea)(2) Positive exercise stress ECG or o<strong>the</strong>r stress imagingmodality(3) Normal cor<strong>on</strong>ary arteriesChest pain occurs frequently and anginal attacks areusually encountered several times per week, but with astable pattern. Therefore, Syndrome X resembles chr<strong>on</strong>icstable angina. However, <strong>the</strong> clinical presentati<strong>on</strong> <strong>of</strong> patientsincluded in ‘Syndrome X’ studies is highly variable and anginaat rest is <strong>of</strong>ten encountered in additi<strong>on</strong> to exercise-provokedchest pain. 293 Severe attacks <strong>of</strong> resting angina may promptrecurrent emergency presentati<strong>on</strong>s, and hospital admissi<strong>on</strong>swith an inaccurate diagnosis <strong>of</strong> unstable angina leading toinappropriate diagnostic and <strong>the</strong>rapeutic procedures.In a subset <strong>of</strong> patients with Syndrome X, microvasculardysfuncti<strong>on</strong> can be dem<strong>on</strong>strated and this entity is comm<strong>on</strong>lyreferred to as ‘microvascular angina’. 294Arterial hypertensi<strong>on</strong>, ei<strong>the</strong>r with or without associatedventricular hypertrophy, is frequently encountered in <strong>the</strong>populati<strong>on</strong> with chest pain and ‘normal cor<strong>on</strong>ary arteries’.Hypertensive heart disease is characterized by endo<strong>the</strong>lialdysfuncti<strong>on</strong>, 295 LVH, interstitial and perivascular fibrosis withdiastolic dysfuncti<strong>on</strong> 296 changes in myocardial and cor<strong>on</strong>aryultrastructure. 297 and reduced cor<strong>on</strong>ary flow reserve. 298Toge<strong>the</strong>r or separately <strong>the</strong>se changes may compromisecor<strong>on</strong>ary blood flow relative to myocardial oxygen demand,causing angina. For <strong>the</strong> most part, treatment in such casesshould focus <strong>on</strong> c<strong>on</strong>trol <strong>of</strong> hypertensi<strong>on</strong> to restore functi<strong>on</strong>aland structural integrity <strong>of</strong> <strong>the</strong> cardiovascular system. 299Pathogenesis. The mechanism <strong>of</strong> chest pain in patients withangina despite a normal cor<strong>on</strong>ary angiogram c<strong>on</strong>tinues to bec<strong>on</strong>troversial. Functi<strong>on</strong>al abnormalities <strong>of</strong> <strong>the</strong> cor<strong>on</strong>arymicrocirculati<strong>on</strong> during stress, including abnormal dilatorresp<strong>on</strong>ses and a heightened resp<strong>on</strong>se to vasoc<strong>on</strong>strictors,have been c<strong>on</strong>sidered potential mechanisms <strong>of</strong> chest painand ischaemic-appearing ST-segment depressi<strong>on</strong> duringexercise. 300 However, o<strong>the</strong>rs failed to find haemodynamicor metabolic evidence <strong>of</strong> ischaemia in many patients withSyndrome X 301 but propose abnormal cardiac sensitivity(coupled with some impairment in cor<strong>on</strong>ary flow reserve)in <strong>the</strong>se patients that may lead to chest pain <strong>on</strong> a n<strong>on</strong>ischaemicbasis. 302Prognosis. Although <strong>the</strong> prognosis in terms <strong>of</strong> mortality <strong>of</strong>patients with Syndrome X appears to be favourable, 303 <strong>the</strong>morbidity <strong>of</strong> patients with Syndrome X is high 304,305 and<strong>the</strong> c<strong>on</strong>diti<strong>on</strong> is frequently associated with c<strong>on</strong>tinuing episodes<strong>of</strong> chest pain and hospital readmissi<strong>on</strong>. 306 There isemerging evidence that identificati<strong>on</strong> <strong>of</strong> impaired endo<strong>the</strong>lialdysfuncti<strong>on</strong> in this patient populati<strong>on</strong> may identifya subgroup at risk for <strong>the</strong> future development <strong>of</strong> a<strong>the</strong>roscleroticcor<strong>on</strong>ary disease 307 and with a less benign prognosisthan previously thought. 305,308–310Diagnosis <strong>of</strong> Syndrome X. Diagnosis and management <strong>of</strong>patients with chest pain and normal cor<strong>on</strong>ary arteries representa complex challenge. The diagnosis <strong>of</strong> Syndrome Xmay be made if a patient with exercise-induced angina hasnormal or n<strong>on</strong>-obstructed cor<strong>on</strong>ary arteries by arteriographybut objective signs <strong>of</strong> exercise-induced ischaemia(ST-depressi<strong>on</strong> in exercise ECG, ischaemic changes by scintigraphy).It is necessary to differentiate this pain from n<strong>on</strong>cardiacchest pain caused by oesophageal dysmotility, fibromyalgia,or costoch<strong>on</strong>dritis. Cor<strong>on</strong>ary artery spasm shouldbe excluded by appropriate provocati<strong>on</strong> tests. Endo<strong>the</strong>lialdysfuncti<strong>on</strong> may be identified by epicardial cor<strong>on</strong>aryartery diameter resp<strong>on</strong>se to acetylcholine. Invasive testingusing acetylcholine provocati<strong>on</strong> can serve a dual purposeby excluding vasospasm and unmasking endo<strong>the</strong>lial dysfuncti<strong>on</strong>,which may be associated with a worse prognosis. Incertain circumstances, for example in <strong>the</strong> presence <strong>of</strong> anextensive radi<strong>on</strong>uclide perfusi<strong>on</strong> defect or wall moti<strong>on</strong>abnormality during stress testing and an angiographicallyirregular artery, intracor<strong>on</strong>ary ultrasound may be c<strong>on</strong>sideredto exclude missed obstructive lesi<strong>on</strong>s. The excellent prognosiswhen endo<strong>the</strong>lial dysfuncti<strong>on</strong> is not present needs to be