Guidelines on the Management of Stable Angina Pectoris ... - Cardio
Guidelines on the Management of Stable Angina Pectoris ... - Cardio
Guidelines on the Management of Stable Angina Pectoris ... - Cardio
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
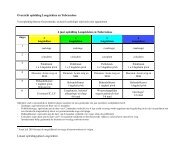
ESC <str<strong>on</strong>g>Guidelines</str<strong>on</strong>g> 3societies and translated into <strong>the</strong> local language, whennecessary.All in all, <strong>the</strong> task <strong>of</strong> writing <str<strong>on</strong>g>Guidelines</str<strong>on</strong>g> or ExpertC<strong>on</strong>sensus Document covers not <strong>on</strong>ly <strong>the</strong> integrati<strong>on</strong> <strong>of</strong> <strong>the</strong>most recent research but also <strong>the</strong> creati<strong>on</strong> <strong>of</strong> educati<strong>on</strong>altools and implementati<strong>on</strong> programmes for <strong>the</strong> recommendati<strong>on</strong>s.The loop between clinical research, writing <strong>of</strong>guidelines, and implementing <strong>the</strong>m into clinical practicecan <strong>the</strong>n <strong>on</strong>ly be completed if surveys and registries areorganized to verify that actual clinical practice is inkeeping with what is recommended in <strong>the</strong> guidelines. Suchsurveys and registries also make it possible to check <strong>the</strong>impact <strong>of</strong> strict implementati<strong>on</strong> <strong>of</strong> <strong>the</strong> guidelines <strong>on</strong>patient outcome.Classes <strong>of</strong> Recommendati<strong>on</strong>sClass IClass IIClass IIaClass IIbClass IIIEvidence and/or general agreement that a givendiagnostic procedure/treatment is beneficial,useful, and effectiveC<strong>on</strong>flicting evidence and/or a divergence <strong>of</strong> opini<strong>on</strong>about <strong>the</strong> usefulness/efficacy <strong>of</strong> <strong>the</strong> treatmentor procedureWeight <strong>of</strong> evidence/opini<strong>on</strong> is in favour <strong>of</strong>usefulness/efficacyUsefulness/efficacy is less well established byevidence/opini<strong>on</strong>Evidence or general agreement that <strong>the</strong> treatmentor procedure is not useful/effective and, in somecases, may be harmfulLevel <strong>of</strong> evidence A Data derived from multiple randomizedclinical trials or meta-analysesLevel <strong>of</strong> evidence B Data derived from a single randomizedclinical trial or large n<strong>on</strong>-randomizedstudiesLevel <strong>of</strong> evidence C C<strong>on</strong>sensus <strong>of</strong> opini<strong>on</strong> <strong>of</strong> <strong>the</strong> experts and/orsmall studies, retrospective studies, andregistriesIntroducti<strong>on</strong><strong>Stable</strong> angina pectoris is a comm<strong>on</strong> and disabling disorder.However, <strong>the</strong> management <strong>of</strong> stable angina has not beensubjected to <strong>the</strong> same scrutiny by large randomized trialsas has, for example, that <strong>of</strong> acute cor<strong>on</strong>ary syndromes(ACS) including unstable angina and myocardial infarcti<strong>on</strong>(MI). The optimal strategy <strong>of</strong> investigati<strong>on</strong> and treatmentis difficult to define, and <strong>the</strong> development <strong>of</strong> new tools for<strong>the</strong> diagnostic and prognostic assessment <strong>of</strong> patients,al<strong>on</strong>g with <strong>the</strong> c<strong>on</strong>tinually evolving evidence base forvarious treatment strategies, mandates that <strong>the</strong> existingguidelines be revised and updated. The Task Force has<strong>the</strong>refore obtained opini<strong>on</strong>s from a wide variety <strong>of</strong> expertsand has tried to achieve agreement <strong>on</strong> <strong>the</strong> best c<strong>on</strong>temporaryapproaches to <strong>the</strong> care <strong>of</strong> stable angina pectoris, bearingin mind not <strong>on</strong>ly <strong>the</strong> efficacy and safety <strong>of</strong> treatments butalso <strong>the</strong> cost and <strong>the</strong> availability <strong>of</strong> resources. The TaskForce has taken <strong>the</strong> view that <strong>the</strong>se guidelines shouldreflect <strong>the</strong> pathophysiology and management <strong>of</strong> angina pectoris,namely myocardial ischaemia due to cor<strong>on</strong>ary arterydisease (CAD), usually macrovascular, i.e. involving largecor<strong>on</strong>ary arteries, but also microvascular in some <strong>of</strong> <strong>the</strong>patients. Fur<strong>the</strong>rmore, this Task Force does not deal withprimary preventi<strong>on</strong>, which has already been covered ino<strong>the</strong>r recently published guidelines 1 and has limited its discussi<strong>on</strong><strong>on</strong> sec<strong>on</strong>dary preventi<strong>on</strong>. Recently published guidelinesand c<strong>on</strong>sensus statements that overlap to ac<strong>on</strong>siderable extent with <strong>the</strong> remit <strong>of</strong> this document arelisted in Table 1.Definiti<strong>on</strong> and pathophysiology<strong>Stable</strong> angina is a clinical syndrome characterized bydiscomfort in <strong>the</strong> chest, jaw, shoulder, back, or arms, typicallyelicited by exerti<strong>on</strong> or emoti<strong>on</strong>al stress and relievedby rest or nitroglycerin. Less typically, discomfort mayoccur in <strong>the</strong> epigastric area. William Heberden first introduced<strong>the</strong> term ‘angina pectoris’ in 1772 2 to characterizea syndrome in which <strong>the</strong>re was ‘a sense <strong>of</strong> strangling andanxiety’ in <strong>the</strong> chest, especially associated with exercise,although its pathological aetiology was not recognizeduntil some years later. 3 It is now usual to c<strong>on</strong>fine <strong>the</strong>term to cases in which <strong>the</strong> syndrome can be attributed tomyocardial ischaemia, although essentially similar symptomscan be caused by disorders <strong>of</strong> <strong>the</strong> oesophagus,lungs, or chest wall. Although <strong>the</strong> most comm<strong>on</strong> cause <strong>of</strong>myocardial ischaemia is a<strong>the</strong>rosclerotic CAD, dem<strong>on</strong>strablemyocardial ischaemia may be induced in <strong>the</strong> abscence byhypertrophic or dilated cardiomyopathy, aortic stenosis,or o<strong>the</strong>r rare cardiac c<strong>on</strong>diti<strong>on</strong>s in <strong>the</strong> absence <strong>of</strong> obstructivea<strong>the</strong>romatous cor<strong>on</strong>ary disease, which are notc<strong>on</strong>sidered in this document.Myocardial ischaemia is caused by an imbalance betweenmyocardial oxygen supply and myocardial oxygen c<strong>on</strong>sumpti<strong>on</strong>.Myocardial oxygen supply is determined by arterialoxygen saturati<strong>on</strong> and myocardial oxygen extracti<strong>on</strong>,which are relatively fixed under normal circumstances,and cor<strong>on</strong>ary flow, which is dependent <strong>on</strong> <strong>the</strong> luminal crosssecti<strong>on</strong>alarea <strong>of</strong> <strong>the</strong> cor<strong>on</strong>ary artery and cor<strong>on</strong>ary arteriolart<strong>on</strong>e. Both cross-secti<strong>on</strong>al area and arterioloar t<strong>on</strong>e may bedramatically altered by <strong>the</strong> presence <strong>of</strong> a<strong>the</strong>roscleroticplaque within <strong>the</strong> vessel wall, leading to imbalancebetween supply and demand when myocardial oxygendemands increase, as during exerti<strong>on</strong>, related to increasesin heart rate, myocardial c<strong>on</strong>tractility, and wall stress.Ischaemia-induced sympa<strong>the</strong>tic activati<strong>on</strong> can fur<strong>the</strong>rincrease <strong>the</strong> severity <strong>of</strong> ischaemia through a variety <strong>of</strong>mechanisms including a fur<strong>the</strong>r increase <strong>of</strong> myocardialoxygen c<strong>on</strong>sumpti<strong>on</strong> and cor<strong>on</strong>ary vasoc<strong>on</strong>stricti<strong>on</strong>. Theischaemic cascade is characterized by a sequence <strong>of</strong>events, resulting in metabolic abnormalities, perfusi<strong>on</strong> mismatch,regi<strong>on</strong>al and <strong>the</strong>n global diastolic and systolic dysfuncti<strong>on</strong>,electrocardiographic (ECG) changes, and angina.Adenosine released by ischaemic myocardium appears tobe <strong>the</strong> main mediator <strong>of</strong> angina (chest pain) through stimulati<strong>on</strong><strong>of</strong> A1 receptors located <strong>on</strong> cardiac nerve endings. 4Ischaemia is followed by reversible c<strong>on</strong>tractile dysfuncti<strong>on</strong>known as ‘stunning’. Recurrent episodes <strong>of</strong> ischaemia and