Optimizing visualization and ergonomics. - Academy of Laser Dentistry
Optimizing visualization and ergonomics. - Academy of Laser Dentistry
Optimizing visualization and ergonomics. - Academy of Laser Dentistry
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
The patient had fair oral hygiene<br />
<strong>and</strong> brushed <strong>and</strong> flossed daily.<br />
Periodontal probing showed 3-mm<br />
pockets with no bleeding. The<br />
implant for tooth #7 was nonsubmerged<br />
<strong>and</strong> a labial fistula was<br />
present; furthermore, insertion <strong>of</strong> a<br />
probe into the fistula led to the end<br />
<strong>of</strong> the implant, <strong>and</strong> revealed loss <strong>of</strong><br />
facial bone on the buccal side <strong>of</strong> the<br />
implant (Figure 3). The s<strong>of</strong>t tissue<br />
around the failed implants in the<br />
area <strong>of</strong> #8 <strong>and</strong> 9 had healed well,<br />
the implant at the location <strong>of</strong> #10<br />
was submerged without s<strong>of</strong>t tissue<br />
complications, <strong>and</strong> all other oral<br />
s<strong>of</strong>t tissue appeared normal.<br />
Panoramic <strong>and</strong> periapical films<br />
showed a radiolucent area around<br />
the apical portion <strong>of</strong> the implant<br />
(Figure 4). The extent <strong>of</strong> buccal<br />
bone resorption could not be determined<br />
from the radiograph.<br />
The implant was stable with no<br />
mobility.<br />
Diagnosis<br />
The provisional <strong>and</strong> final diagnosis<br />
was peri-implantitis <strong>of</strong> the implant<br />
fixture for tooth #7 with an infected<br />
implant periapical lesion exhibiting<br />
severe bone loss on the buccal side<br />
<strong>of</strong> the implant.<br />
Treatment Plan<br />
Treatment would involve the use <strong>of</strong><br />
an Er:YAG laser to perform:<br />
• the incision for a flap<br />
• ablation <strong>of</strong> granulation tissue<br />
around the implant<br />
• remodeling, shaping, <strong>and</strong> decortication<br />
<strong>of</strong> the bone<br />
• decontamination <strong>of</strong> exposed<br />
screw threads <strong>of</strong> the implant, <strong>and</strong><br />
• a GBR procedure.<br />
Since the implant was not<br />
mobile, this technique has a good<br />
prognosis.<br />
Treatment alternatives could<br />
consist <strong>of</strong> traditional scalpel,<br />
curettes, citric acid, air flow, air<br />
abrasion 49 <strong>and</strong> rotary bone burs.<br />
Treatment<br />
An Er:YAG laser (OpusDuo <br />
AquaLite E , Lumenis Ltd.,<br />
Reyhanian et al.<br />
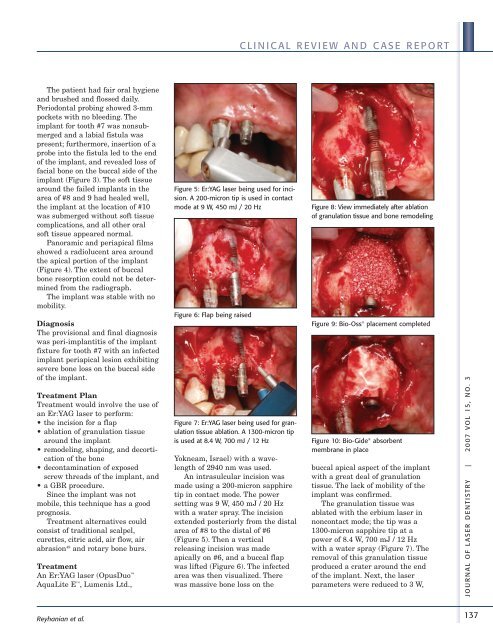
Figure 5: Er:YAG laser being used for incision.<br />
A 200-micron tip is used in contact<br />
mode at 9 W, 450 mJ / 20 Hz<br />
Figure 6: Flap being raised<br />
Figure 7: Er:YAG laser being used for granulation<br />
tissue ablation. A 1300-micron tip<br />
is used at 8.4 W, 700 mJ / 12 Hz<br />
Yokneam, Israel) with a wavelength<br />
<strong>of</strong> 2940 nm was used.<br />
An intrasulcular incision was<br />
made using a 200-micron sapphire<br />
tip in contact mode. The power<br />
setting was 9 W, 450 mJ / 20 Hz<br />
with a water spray. The incision<br />
extended posteriorly from the distal<br />
area <strong>of</strong> #8 to the distal <strong>of</strong> #6<br />
(Figure 5). Then a vertical<br />
releasing incision was made<br />
apically on #6, <strong>and</strong> a buccal flap<br />
was lifted (Figure 6). The infected<br />
area was then visualized. There<br />
was massive bone loss on the<br />
CLINICAL REVIEW AND CASE REPORT<br />
Figure 8: View immediately after ablation<br />
<strong>of</strong> granulation tissue <strong>and</strong> bone remodeling<br />
Figure 9: Bio-Oss ® placement completed<br />
Figure 10: Bio-Gide ® absorbent<br />
membrane in place<br />
buccal apical aspect <strong>of</strong> the implant<br />
with a great deal <strong>of</strong> granulation<br />
tissue. The lack <strong>of</strong> mobility <strong>of</strong> the<br />
implant was confirmed.<br />
The granulation tissue was<br />
ablated with the erbium laser in<br />
noncontact mode; the tip was a<br />
1300-micron sapphire tip at a<br />
power <strong>of</strong> 8.4 W, 700 mJ / 12 Hz<br />
with a water spray (Figure 7). The<br />
removal <strong>of</strong> this granulation tissue<br />
produced a crater around the end<br />
<strong>of</strong> the implant. Next, the laser<br />
parameters were reduced to 3 W,<br />
JOUR NAL OF LASER DENTIS TRY | 2007 VOL 15, NO. 3<br />
137