You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
Lightwaves News<br />
Featured in a<br />
Special Section<br />
The Official Journal <strong>of</strong> the <strong>Academy</strong> <strong>of</strong> <strong>Laser</strong> <strong>Dentistry</strong> 2011 • Vol. 19 No. 3<br />
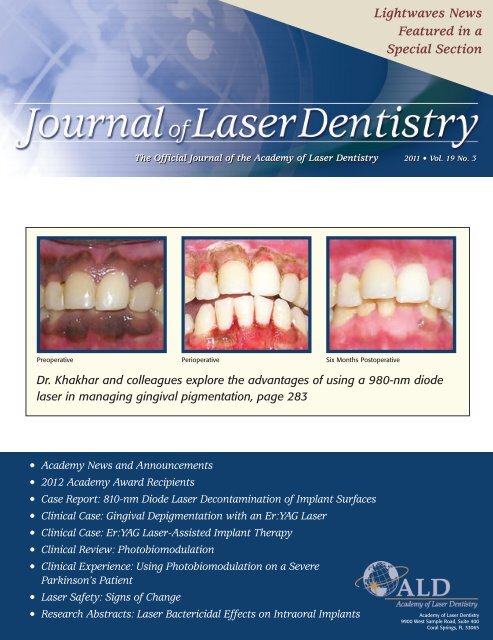
Preoperative Perioperative Six Months Postoperative<br />
Dr. Khakhar and colleagues explore the advantages <strong>of</strong> using a 980-nm diode<br />
laser in managing gingival pigmentation, page 283<br />
• <strong>Academy</strong> News and Announcements<br />
• 2012 <strong>Academy</strong> Award Recipients<br />
• Case Report: 810-nm Diode <strong>Laser</strong> Decontamination <strong>of</strong> Implant Surfaces<br />
• Clinical Case: Gingival Depigmentation with an Er:YAG <strong>Laser</strong><br />
• Clinical Case: Er:YAG <strong>Laser</strong>-Assisted Implant Therapy<br />
• Clinical Review: Photobiomodulation<br />
• Clinical Experience: Using Photobiomodulation on a Severe<br />
Parkinson’s Patient<br />
• <strong>Laser</strong> Safety: Signs <strong>of</strong> Change<br />
• Research Abstracts: <strong>Laser</strong> Bactericidal Effects on Intraoral Implants<br />
<strong>Academy</strong> <strong>of</strong> <strong>Laser</strong> <strong>Dentistry</strong><br />
9900 West Sample Road, Suite 400<br />
Coral Springs, FL 33065
J O U R N A L O F L A S E R D E N T I S T R Y | 2 011 V O L . 19 , N O . 3<br />
250<br />
TA B L E O F C O N T E N T S<br />
EDITOR’S VIEW<br />
New Adventures and Past<br />
Experiences with <strong>Laser</strong>s ................254<br />
Stuart Coleton, DDS<br />
PRESIDENT’S MESSAGE<br />
Approaching ALD Prime ................255<br />
Ana Triliouris, DDS<br />
EXECUTIVE DIRECTOR’S<br />
MESSAGE<br />
ALD – A History <strong>of</strong> Values ............256<br />
Gail Siminovsky, CAE<br />
NOMINATIONS<br />
<strong>Academy</strong> <strong>of</strong> <strong>Laser</strong> <strong>Dentistry</strong>’s 2012<br />
Nominated Slate <strong>of</strong> Officers and<br />
Directors ............................................258<br />
Art Levy, DMD<br />
AWARDS<br />
ALD Award Recipients Announced<br />
for 2012 ..............................................262<br />
Glenda Payas, DMD<br />
2012 CONFERENCE<br />
Elevating Your Practice to New<br />
Peaks! ..................................................264<br />
John J. Graeber, DMD<br />
CERTIFICATION<br />
ALD Certification Program Planned in<br />
Scottsdale March 29-31, 2012 ......266<br />
Mel Burchman, DDS<br />
STUDENT SCHOLARSHIPS<br />
A Helping Hand................................267<br />
Glenda Payas, DMD<br />
CASE REPORT<br />
Treatment <strong>of</strong> Periimplant Infection<br />
in the Posterior Maxilla, with 810nm<br />
Diode <strong>Laser</strong> Decontamination<br />
<strong>of</strong> the Implant Surfaces: A Case<br />
Report..................................................270<br />
Ahmad Kutkut, DDS, MS; Sebastiano<br />
Andreana, DDS, MS; Mohanad<br />
Al-Sabbagh, DDS, MS<br />
CLINICAL REVIEW AND<br />
CASE REPORT<br />
Peri-Implantitis Therapy with an<br />
Er:YAG <strong>Laser</strong> ......................................276<br />
Avi Reyhanian, DDS; Donald J. Coluzzi,<br />
DDS<br />
COVER FEATURE<br />
CASE REPORTS<br />
Advantages <strong>of</strong> 980-nm Diode <strong>Laser</strong><br />
Treatment in the Management <strong>of</strong><br />
Gingival Pigmentation....................283<br />
Mihir Khakhar, BDS; Richa Kapoor,<br />
BDS; N.D. Jayakumar, BDS, MDS; O.<br />
Padmalatha, BDS, MDS; Sheeja S.<br />
Varghese, BDS, MDS; M. Sankari, BDS,<br />
MDS<br />
CLINICAL CASE<br />
Gingival Depigmentation with an<br />
Er:YAG <strong>Laser</strong>: A Clinical Case with<br />
Three-Year Follow-Up ....................286<br />
Grace Sun, DDS<br />
CLINICAL REVIEW AND<br />
CASE REPORTS<br />
Photobiomodulation: An Invaluable<br />
Tool for All Dental Specialties......289<br />
Gerry Ross, DDS<br />
CLINICAL EXPERIENCE<br />
Using Photobiomodulation on a<br />
Severe Parkinson’s Patient to<br />
Enable Extractions, Root Canal<br />
Treatment, and Partial Denture<br />
Fabrication..........................................297<br />
Mel A. Burchman, DDS<br />
LASER SAFETY<br />
Signs <strong>of</strong> Change ..............................301<br />
Raminta Mastis, DDS, FAGD, MALD<br />
RESEARCH ABSTRACTS<br />
<strong>Laser</strong> Bactericidal Effects on<br />
Intraoral Implants ............................303<br />
The Journal <strong>of</strong> <strong>Laser</strong> <strong>Dentistry</strong><br />
The mission <strong>of</strong> the Journal <strong>of</strong> <strong>Laser</strong> <strong>Dentistry</strong><br />
is to provide a pr<strong>of</strong>essional journal that helps<br />
to fulfill the goal <strong>of</strong> information dissemination<br />
by the <strong>Academy</strong> <strong>of</strong> <strong>Laser</strong> <strong>Dentistry</strong>. The purpose<br />
<strong>of</strong> the Journal <strong>of</strong> <strong>Laser</strong> <strong>Dentistry</strong> is to<br />
present information about the use <strong>of</strong> lasers in<br />
dentistry. All articles are peer-reviewed. Issues<br />
include manuscripts on current indications for<br />
uses <strong>of</strong> lasers for dental applications, clinical<br />
case studies, reviews <strong>of</strong> topics relevant to laser<br />
dentistry, research articles, clinical studies,<br />
research abstracts detailing the scientific<br />
basis for the safety and efficacy <strong>of</strong> the devices,<br />
and articles about future and experimental<br />
procedures. In addition, featured columnists<br />
<strong>of</strong>fer clinical insights, and editorials describe<br />
personal viewpoints.<br />
Journal <strong>of</strong> <strong>Laser</strong> <strong>Dentistry</strong><br />
The <strong>of</strong>ficial journal <strong>of</strong> the<br />
<strong>Academy</strong> <strong>of</strong> <strong>Laser</strong> <strong>Dentistry</strong><br />
Editor-in-Chief<br />
Stuart Coleton, DDS<br />
Chappaqua, NY scoleton@aol.com<br />
Managing Editor<br />
Gail S. Siminovsky, CAE, Executive Director<br />
Coral Springs, FL siminovsky@laserdentistry.org<br />
Consulting Editor<br />
John G. Sulewski, MA<br />
Huntington Woods, MI john.sulewski@we-inc.com<br />
Publisher<br />
Max G. Moses<br />
Member Media<br />
1844 N. Larrabee • Chicago, IL 60614<br />
312-296-7864 • Fax: 312-896-9119<br />
max@maxgmoses.com<br />
Design and Layout<br />
Diva Design<br />
2616 Missum Pointe • San Marcos, TX 78666<br />
512-665-0544 • Fax 609-678-0544<br />
kkolstedt@austin.rr.com<br />
Editorial Office<br />
9900 West Sample Road, Suite 400<br />
Coral Springs, FL 33065<br />
Advertising<br />
Nicole Synadinos<br />
Association Services<br />
727-942-4503<br />
sales@fernmanagement.com<br />
954-346-3776<br />
Fax 954-757-2598<br />
www.laserdentistry.org<br />
laserexec@laserdentistry.org<br />
The <strong>Academy</strong> <strong>of</strong> <strong>Laser</strong> <strong>Dentistry</strong> is a not-for-pr<strong>of</strong>it<br />
organization qualifying under Section 501(c)(3) <strong>of</strong><br />
the Internal Revenue Code. The <strong>Academy</strong> <strong>of</strong> <strong>Laser</strong><br />
<strong>Dentistry</strong> is an international pr<strong>of</strong>essional membership<br />
association <strong>of</strong> dental practitioners and supporting<br />
organizations dedicated to improving the<br />
health and well-being <strong>of</strong> patients through the<br />
proper use <strong>of</strong> laser technology. The <strong>Academy</strong> is<br />
dedicated to the advancement <strong>of</strong> knowledge,<br />
research and education and to the exchange <strong>of</strong><br />
information relative to the art and science <strong>of</strong> the<br />
use <strong>of</strong> lasers in dentistry. The <strong>Academy</strong> endorses<br />
the Curriculum Guidelines and Standards for<br />
Dental <strong>Laser</strong> Education.<br />
Copyright 2011 <strong>Academy</strong> <strong>of</strong> <strong>Laser</strong> <strong>Dentistry</strong>
Journal <strong>of</strong> <strong>Laser</strong> <strong>Dentistry</strong>: Guidelines for Authors<br />
The <strong>Academy</strong> <strong>of</strong> <strong>Laser</strong> <strong>Dentistry</strong> Welcomes Your Articles for Submission<br />
The Journal <strong>of</strong> <strong>Laser</strong> <strong>Dentistry</strong> publishes<br />
articles pertaining to the art, science,<br />
and practice <strong>of</strong> laser dentistry. Articles<br />
may be scientific and clinical in nature<br />
discussing new techniques, research,<br />
and programs, or may be applicationsoriented<br />
describing specific problems<br />
and solutions. While lasers are our preferred<br />
orientation, other high-technology<br />
articles, as well as insights into marketing,<br />
practice management, regulation,<br />
and other aspects <strong>of</strong> dentistry that<br />
may be <strong>of</strong> interest to the dental pr<strong>of</strong>ession,<br />
may be appropriate. All articles<br />
are peer-reviewed prior to acceptance,<br />
modification, or rejection.<br />
These guidelines are designed to<br />
help potential authors in writing and<br />
submitting manuscripts to the Journal<br />
<strong>of</strong> <strong>Laser</strong> <strong>Dentistry</strong>, the <strong>of</strong>ficial publication<br />
<strong>of</strong> the <strong>Academy</strong> <strong>of</strong> <strong>Laser</strong> <strong>Dentistry</strong><br />
(ALD). Please follow these instructions<br />
carefully to expedite review and processing<br />
<strong>of</strong> your submission. Manuscripts<br />
that do not adhere to these instructions<br />
will not be accepted for consideration.<br />
The <strong>Academy</strong> <strong>of</strong> <strong>Laser</strong> <strong>Dentistry</strong> and the<br />
editors and publisher <strong>of</strong> the Journal <strong>of</strong><br />
<strong>Laser</strong> <strong>Dentistry</strong> endorse the “Uniform<br />
Requirements <strong>of</strong> Manuscripts Submitted<br />
to Biomedical Journals” (www.icmje.org).<br />
The Journal reserves the right to revise<br />
or rescind these guidelines.<br />
Authors are advised to read the more<br />
comprehensive Guidelines for Authors<br />
and required forms available by mail or<br />
online at www.laserdentistry.org.<br />
Manuscript Eligibility<br />
Submitted manuscripts must be written<br />
clearly and concisely in American<br />
English and appropriate for a scholarly<br />
journal. Write in active voice and use<br />
declarative sentences. Manuscripts will<br />
be considered for publication on the condition<br />
that they have been submitted<br />
exclusively to the Journal, and have not<br />
been published or submitted for publication<br />
in any part or form in another publication<br />
<strong>of</strong> any type, pr<strong>of</strong>essional or lay, or<br />
in any language elsewhere, and with the<br />
understanding that they will not be<br />
reprinted without written consent from<br />
both the managing editor and the author.<br />
Permissions<br />
Direct quotations <strong>of</strong> 100 or more words,<br />
and illustrations, figures, tables, or<br />
other materials (or adaptations there<strong>of</strong>)<br />
that have appeared in copyrighted<br />
material or are in press must be accompanied<br />
by written permission for their<br />
use in the Journal <strong>of</strong> <strong>Laser</strong> <strong>Dentistry</strong><br />
from the copyright owner and original<br />
author along with complete information<br />
regarding source, including (as applicable)<br />
author(s), title <strong>of</strong> article, title <strong>of</strong><br />
journal or book, year, volume number,<br />
issue number, pages. Photographs <strong>of</strong><br />
identifiable persons must be accompanied<br />
by valid signed releases indicating<br />
informed consent. When informed consent<br />
has been obtained from any<br />
patient, identifiable or not, it should be<br />
noted in the manuscript. The appropriate<br />
Permission Letters must be submitted<br />
with the manuscript. Suggested<br />
template letters are available online.<br />
Copyright<br />
All manuscript rights shall be transferred<br />
to the Journal <strong>of</strong> <strong>Laser</strong> <strong>Dentistry</strong><br />
upon submission. Upon submission <strong>of</strong><br />
the manuscript, authors agree to submit<br />
a completed Copyright Transfer<br />
Agreement form, available online. If the<br />
manuscript is rejected for publication,<br />
all copyrights will be retained by the<br />
author(s).<br />
Commercialism<br />
ALD members are interested in learning<br />
about new products and service<br />
<strong>of</strong>ferings, however ALD stresses that<br />
submitted manuscripts should be educational<br />
in nature. The emphasis is on<br />
scientific research and sound clinical<br />
and practical advice, rather than promotion<br />
<strong>of</strong> a specific product or service.<br />
Disclosure <strong>of</strong> Commercial Relationships<br />
According to the <strong>Academy</strong>’s Conflict <strong>of</strong><br />
Interest and Disclosure policy, manuscript<br />
authors and their institutions are<br />
expected to disclose any economic or<br />
financial support, as well as any personal,<br />
commercial, technological, academic,<br />
intellectual, pr<strong>of</strong>essional, philosophical,<br />
political, or religious interests<br />
or potential bias that may be perceived<br />
as creating a conflict related to the<br />
material being published. Such conditions<br />
may include employment, consultancies,<br />
stock ownership or other equity<br />
interests, honoraria, stipends, paid<br />
expert testimony, patent ownership,<br />
patent licensing arrangements, royalties,<br />
or serving as an <strong>of</strong>ficer, director, or<br />
owner <strong>of</strong> a company whose products, or<br />
products <strong>of</strong> a competitor, are identified.<br />
Sources <strong>of</strong> support in the form <strong>of</strong> contracts,<br />
grants, equipment, drugs, material<br />
donations, clinical materials, special<br />
discounts or gifts, or other forms <strong>of</strong> support<br />
should be specified. The roles <strong>of</strong> the<br />
study or manuscript sponsor(s), if any,<br />
are to be described. Disclosure statements<br />
are printed at the end <strong>of</strong> the article<br />
following the author’s biography.<br />
This policy is intended to alert the audience<br />
to any potential bias or conflict so<br />
that readers may form their own judgments<br />
about the material being presented.<br />
Disclosure forms are to be<br />
signed by each author. Manuscripts will<br />
not be reviewed without the Journal<br />
having this form on file.<br />
The <strong>Academy</strong> <strong>of</strong> <strong>Laser</strong> <strong>Dentistry</strong> also<br />
requires that authors disclose whether<br />
any product discussed in their manuscript<br />
is unlabeled for the use discussed<br />
or is investigational.<br />
The Disclosure Statement form is<br />
available online and must be submitted<br />
with the manuscript.<br />
Manuscript Types<br />
Submissions to the Journal should be<br />
limited to one <strong>of</strong> the types indicated<br />
below.<br />
• Scientific / Technology / Clinical<br />
Review<br />
• Case Reports and Clinical Case<br />
Studies<br />
• Scientific / Clinical Research<br />
• Randomized Clinical Trials<br />
• Advances in Dental Products<br />
• Trends<br />
• Practice Management<br />
• Guest Editorials and Essays<br />
• Letters to the Editor<br />
• Book Reviews<br />
Manuscript Preparation and<br />
Submission<br />
Format<br />
All submitted manuscripts should be<br />
double-spaced, using 12 pt. font size<br />
with at least 6 mm between lines.<br />
Submit manuscripts in Micros<strong>of</strong>t Word<br />
(.doc), using either the Windows or<br />
Macintosh platform. Manuscripts must<br />
be submitted electronically in this format.<br />
Hard copy-only submissions will<br />
not be accepted.<br />
Unacceptable Formats<br />
The following submission formats are<br />
unacceptable and will be returned:<br />
• Manuscripts submitted in desktop<br />
publishing s<strong>of</strong>tware<br />
• PowerPoint presentations<br />
• Any text files with embedded images<br />
• Images in lower than the minimum<br />
prescribed resolution.<br />
Manuscript Components<br />
Title Page<br />
The title page <strong>of</strong> the manuscript should<br />
include a concise and informative title<br />
<strong>of</strong> the article; the first name, middle initial(s),<br />
and last name <strong>of</strong> each author,<br />
along with the academic degree(s), pr<strong>of</strong>essional<br />
title(s), and the name and<br />
location (city, state, zip code) <strong>of</strong> current<br />
institutional affiliation(s) and department(s).<br />
Authors who are private practitioners<br />
should identify their location<br />
(city, state, and country). Include all<br />
information in the title that will make<br />
electronic retrieval <strong>of</strong> the article sensi-
tive and specific. Titles <strong>of</strong> case studies<br />
should include the laser wavelength(s)<br />
and type(s) utilized for treatment (for<br />
example, “810-nm GaAlAs diode”).<br />
Identify the complete address, business<br />
and home telephone numbers, fax<br />
number, e-mail address, and Web site<br />
address (if any) for all authors. Identify<br />
one author as the corresponding author.<br />
Unless requested otherwise, the e-mail<br />
address is published in the Journal.<br />
Abstract<br />
A self-standing summary <strong>of</strong> the text <strong>of</strong><br />
up to 250 words should precede the<br />
introduction. It should provide an accurate<br />
summary <strong>of</strong> the most significant<br />
points and be representative <strong>of</strong> the<br />
entire article’s content. Provide the context<br />
or background for the article, basic<br />
procedures, main findings and conclusions.<br />
Emphasize new or important<br />
aspects. Do not use abbreviations (other<br />
than standard units <strong>of</strong> measurement) or<br />
references in the abstract.<br />
Author(s) Biography<br />
Provide a brief, current biographical<br />
sketch <strong>of</strong> each author that includes pr<strong>of</strong>essional<br />
education and pr<strong>of</strong>essional<br />
affiliations. For authors who hold teaching<br />
positions, include the title, department,<br />
and school. For authors who are<br />
in federal service, include rank or title<br />
and station.<br />
References<br />
References are to be cited in the text by<br />
number in order <strong>of</strong> appearance, with<br />
the number appearing either as a<br />
superscript or in brackets. The reference<br />
list should appear at the end <strong>of</strong> the<br />
manuscript with references in order <strong>of</strong><br />
first appearance in the text <strong>of</strong> the manuscript.<br />
The reference list must be<br />
typed double-spaced on a separate page<br />
and numbered in the same sequence as<br />
the reference citations appear in the<br />
text. Prior to submission, all references<br />
are to be properly prepared in the correct<br />
format, checked for completeness,<br />
carefully verified against their original<br />
documents, and checked for accurate<br />
correspondence between references<br />
cited in the text and listed in the<br />
References section.<br />
• For journal citations, include surnames<br />
and all initials <strong>of</strong> all authors,<br />
complete title <strong>of</strong> article, name <strong>of</strong> journal<br />
(abbreviated according to the U.S.<br />
National Library <strong>of</strong> Medicine<br />
(www.nlm.nih.gov/services/<br />
lpabbrev.html), year <strong>of</strong> publication,<br />
volume, issue number, and complete<br />
inclusive page numbers. If abstracts<br />
are cited, add the abstract number<br />
after the page number.<br />
• For book citations, specify surnames<br />
and initials <strong>of</strong> all authors, chapter<br />
number and title (if applicable), editors’<br />
surnames and initials, book<br />
title, volume number (if applicable),<br />
edition number (if applicable), city<br />
and full name <strong>of</strong> publisher, year <strong>of</strong><br />
publication, and inclusive page numbers<br />
<strong>of</strong> citation.<br />
• For government publications or bulletins,<br />
identify the author(s) (if given);<br />
title; department, bureau, agency, or<br />
<strong>of</strong>fice; the publication series, report,<br />
or monograph number; location <strong>of</strong><br />
publisher; publisher; year <strong>of</strong> publication;<br />
and inclusive page numbers.<br />
• For articles published online but not<br />
yet in print, cite with the paper’s<br />
Digital Object Identifier (DOI) added<br />
to the end <strong>of</strong> the reference.<br />
• For Web citations, list the authors<br />
and titles if known, then the URL<br />
and date it was accessed.<br />
• For presentations, list the authors,<br />
title <strong>of</strong> presentation, indication that<br />
the reference is a lecture, name <strong>of</strong><br />
conference or presentation venue,<br />
date, and location.<br />
Illustration Captions and Legends<br />
All illustrations must be accompanied by<br />
individual explanatory captions which<br />
should be typed double-spaced on a separate<br />
page with Arabic numerals corresponding<br />
to their respective illustration.<br />
Tables<br />
Tables must be typewritten doublespaced,<br />
including column heads, data,<br />
and footnotes, and submitted on separate<br />
pages. The tables are to be cited in<br />
the text and numbered consecutively in<br />
Arabic numerals in the order <strong>of</strong> their<br />
appearance in the text. Provide a concise<br />
title for each table that highlights<br />
the key result.<br />
Illustrations<br />
Illustrations include photographs, radiographs,<br />
micrographs, charts, graphs,<br />
and maps. Each should be numbered and<br />
cited in the text in the order <strong>of</strong> appearance<br />
and be accompanied by explanatory<br />
captions. Do not embed figures within<br />
the manuscript text. Each figure and<br />
table should be no larger than 8-1/2 x 11<br />
inches. Digital files must measure at<br />
least 5 inches (127 mm) in width. The<br />
Illustration<br />
Type<br />
image must be submitted in the size it<br />
will be printed, or larger. Illustrations<br />
are to augment, not repeat, material in<br />
the text. Graphs must not repeat data<br />
presented in tables. Clinical photographs<br />
must comply with ALD’s Guidelines for<br />
Clinical Photography, available online.<br />
Authors are to certify in a cover letter<br />
that digitized illustrations accurately<br />
represent the original data, condition, or<br />
image and are not electronically edited.<br />
Publisher and Copyright Holder<br />
The Journal <strong>of</strong> <strong>Laser</strong> <strong>Dentistry</strong> is published<br />
by Max G. Moses, Member<br />
Media, 1844 N. Larrabee, Chicago, IL<br />
60614, Telephone: (312) 296-7864; Fax:<br />
(312) 896-9119. The Journal <strong>of</strong> <strong>Laser</strong><br />
<strong>Dentistry</strong> is copyrighted by The<br />
<strong>Academy</strong> <strong>of</strong> <strong>Laser</strong> <strong>Dentistry</strong>, 9900 W.<br />
Sample Road, Suite 400, Coral Springs,<br />
FL 33065, Telephone: (954) 346-3776;<br />
Fax: (954) 757-2598.<br />
Articles, Questions, Ideas<br />
Questions about clinical cases, scientific<br />
research, or ideas for other articles may<br />
be directed to Stuart Coleton, Editor-in-<br />
Chief, by e-mail: scoleton@aol.com.<br />
Submission <strong>of</strong> Files<br />
by E-mail:<br />
Send your completed files by e-mail<br />
(files up to 10 MB are acceptable). If<br />
files are larger than 10 MB, they may<br />
be compressed or sent as more than one<br />
file, with appropriate labels. Files<br />
should be submitted to: Stuart Coleton,<br />
Editor-in-Chief, by e-mail:<br />
scoleton@aol.com.<br />
By Federal Express or Other<br />
Insured Courier:<br />
If using a courier, please send the files<br />
on a flash drive, include a hard copy <strong>of</strong><br />
your manuscript and also send a verification<br />
by e-mail to Gail Siminovsky<br />
(laserexec@laserdentistry.org).<br />
Gail Siminovsky<br />
<strong>Academy</strong> <strong>of</strong> <strong>Laser</strong> <strong>Dentistry</strong><br />
9900 W. Sample Road, Suite 400<br />
Coral Springs, FL 33065<br />
Phone: (954) 346-3776.<br />
Summary <strong>of</strong> Illustration Types and Specifications<br />
Definition and Examples<br />
Preferred<br />
Format<br />
Required<br />
Resolution<br />
Line Art and Black and white graphic with no<br />
EPS or JPG 1200 DPI<br />
Vector Graphics shading (e.g., graphs, charts, maps)<br />
Halftone Art<br />
Combination<br />
Art<br />
Photographs, drawings, or painting<br />
with fine shading (e.g., radiographs,<br />
micrographs with scale<br />
bars, intraoral photographs)<br />
Combination <strong>of</strong> halftone and line<br />
art (e.g., halftones containing<br />
line drawing, extensive lettering,<br />
color diagrams)<br />
TIFF or<br />
JPG<br />
300 DPI (black &<br />
white)<br />
600 DPI (color)<br />
EPS or JPG 1200 DPI
Editorial Policy<br />
The Journal <strong>of</strong> <strong>Laser</strong> <strong>Dentistry</strong> is devoted to providing the <strong>Academy</strong> and its members with comprehensive clinical, didactic and<br />
research information about the safe and effective uses <strong>of</strong> lasers in dentistry. All statements <strong>of</strong> opinions and/or fact are published<br />
under the authority <strong>of</strong> the authors, including editorials and articles. The <strong>Academy</strong> is not responsible for the opinions expressed<br />
by the writers, editors or advertisers. The views are not to be accepted as the views <strong>of</strong> the <strong>Academy</strong> <strong>of</strong> <strong>Laser</strong> <strong>Dentistry</strong> unless<br />
such statements have been expressly adopted by the organization. Information on any research, clinical procedures or products<br />
may be obtained from the author. Comments concerning content may be directed to the <strong>Academy</strong>’s main <strong>of</strong>fice by e-mail to<br />
laserexec@laserdentistry.org.<br />
Submissions<br />
We encourage prospective authors to follow JLD’s “Instructions to Authors” before submitting manuscripts. To obtain a copy,<br />
please go to our Web site www.laserdentistry.org/index.cfm/pr<strong>of</strong>essionals/Media%20and%20Press. Please send manuscripts by email<br />
to the Editor at<br />
scoleton@aol.com.<br />
Disclosure Policy <strong>of</strong> Contributing Authors’ Commercial Relationships<br />
According to the <strong>Academy</strong>’s Conflict <strong>of</strong> Interest and Disclosure policy, authors <strong>of</strong> manuscripts for JLD are expected to disclose<br />
any economic support, personal interests, or potential bias that may be perceived as creating a conflict related to the material<br />
being published. Disclosure statements are printed at the end <strong>of</strong> the article following the author’s biography. This policy is<br />
intended to alert the audience to any potential bias or conflict so that readers may form their own judgments about the material<br />
being presented.<br />
Disclosure Statement for the <strong>Academy</strong> <strong>of</strong> <strong>Laser</strong> <strong>Dentistry</strong><br />
The <strong>Academy</strong> <strong>of</strong> <strong>Laser</strong> <strong>Dentistry</strong> has no financial interest in any manufacturers or vendors <strong>of</strong> dental supplies.<br />
Reprint Permission Policy<br />
Written permission must be obtained to duplicate and/or distribute any portion <strong>of</strong> the Journal <strong>of</strong> <strong>Laser</strong> <strong>Dentistry</strong>. Reprints may<br />
be obtained directly from the <strong>Academy</strong> <strong>of</strong> <strong>Laser</strong> <strong>Dentistry</strong> provided that any appropriate fee is paid.<br />
Copyright 2011 <strong>Academy</strong> <strong>of</strong> <strong>Laser</strong> <strong>Dentistry</strong>. All rights reserved unless other ownership is indicated. If any omission or infringement<br />
<strong>of</strong> copyright has occurred through oversight, upon notification amendment will be made in a future issue. No part <strong>of</strong> this publication<br />
may be reproduced or transmitted in any form or by any means, individually or by any means, without permission from the<br />
copyright holder.<br />
The Journal <strong>of</strong> <strong>Laser</strong> <strong>Dentistry</strong> ISSN# 1935-2557.<br />
JLD is published quarterly and mailed nonpr<strong>of</strong>it standard mail to all ALD members. Issues are also mailed to new member<br />
prospects and dentists requesting information on lasers in dentistry.<br />
Advertising Information and Rates<br />
Display rates are available at www.laserdentistry.org and/or supplied upon request. Insertion orders and materials should be sent to<br />
Association Services, e-mail sales@fernmanagement.com, telephone 727-942-4503. The cost for a classified ad in one issue is $50 for<br />
the first 25 words and $2.00 for each additional word beyond 25. ALD members receive a 20% discount. Payment must accompany ad<br />
copy and is payable to the <strong>Academy</strong> <strong>of</strong> <strong>Laser</strong> <strong>Dentistry</strong> in U.S. funds only. Classified advertising is not open to commercial enterprises.<br />
Companies are encouraged to contact Association Services for information on display advertising specifications and rates. The<br />
<strong>Academy</strong> reserves the right to edit or refuse ads.<br />
Editor’s Note on Advertising:<br />
The Journal <strong>of</strong> <strong>Laser</strong> <strong>Dentistry</strong> currently accepts advertisements for different dental laser educational programs. Not all dental laser educational<br />
courses are recognized by the <strong>Academy</strong> <strong>of</strong> <strong>Laser</strong> <strong>Dentistry</strong>. ALD as an independent pr<strong>of</strong>essional dental organization is concerned that courses<br />
meet the stringent guidelines following pr<strong>of</strong>essional standards <strong>of</strong> education. Readers are advised to verify with ALD whether or not specific<br />
courses are recognized by the <strong>Academy</strong> <strong>of</strong> <strong>Laser</strong> <strong>Dentistry</strong> in their use <strong>of</strong> the Curriculum Guidelines and Standards for Dental <strong>Laser</strong> Education.
J O U R N A L O F L A S E R D E N T I S T R Y | 2 011 V O L . 19 , N O . 3<br />
254<br />
E D I TO R ’ S V I E W<br />
New Adventures and Past<br />
Experiences with <strong>Laser</strong>s<br />
Stuart Coleton, DDS, New York Medical College, Valhalla, New York,<br />
and Westchester University Medical Center, Valhalla, New York<br />
J <strong>Laser</strong> Dent 2011;19(3):254<br />
As I prepare to take over the position<br />
<strong>of</strong> Editor-in-Chief <strong>of</strong> the<br />
Journal <strong>of</strong> <strong>Laser</strong> <strong>Dentistry</strong> (JLD), I<br />
have this opportunity to say hello<br />
and welcome you to the third issue<br />
<strong>of</strong> volume 19.<br />
Beginning with volume 20, you<br />
will see some significant changes in<br />
the Journal. We will once again<br />
publish a separate Lightwaves<br />
Newsletter so you all will be kept<br />
up to the minute on what is<br />
happening in the <strong>Academy</strong>. I am<br />
establishing new goals for our<br />
Journal which I will discuss with<br />
you in the next issue.<br />
This edition includes three new<br />
case presentations by clinicians<br />
from universities in Kentucky, New<br />
York, and India as well as a private<br />
practitioner from Pennsylvania.<br />
Each article will be complemented<br />
by noteworthy reports from<br />
previous issues <strong>of</strong> the Journal for<br />
added perspective.<br />
• Dr. Ahmad Kutkut and<br />
colleagues from the University <strong>of</strong><br />
Kentucky and the State<br />
University <strong>of</strong> New York at<br />
Buffalo discuss the adjunctive<br />
use <strong>of</strong> a diode laser to disinfect<br />
implant surfaces in the treatment<br />
<strong>of</strong> periimplant infection.<br />
• From volume 15 number 3 <strong>of</strong> the<br />
Journal, we reprise the clinical<br />
case by Dr. Avi Reyhanian and<br />
Donald Coluzzi on treating periimplantitis<br />
with an Er:YAG<br />
<strong>Laser</strong>.<br />
• Continuing with the theme <strong>of</strong><br />
periimplantitis therapy via laser,<br />
the Research Abstracts from<br />
volume 15 number 3 are again<br />
Coleton<br />
presented, and updated in this<br />
issue with recent research in the<br />
area <strong>of</strong> laser bactericidal effects<br />
on intraoral implants.<br />
• Dr. Mihir Khakhar and associates<br />
from the Saveetha Dental<br />
College in Chennai, India,<br />
present a case report outlining<br />
the advantages <strong>of</strong> diode laser<br />
treatment in the management <strong>of</strong><br />
gingival pigmentation.<br />
• Their successful treatment<br />
compares with the favorable<br />
results achieved by Dr. Grace<br />
Sun, who described a clinical case<br />
<strong>of</strong> gingival depigmentation using<br />
an Er:YAG laser, reprinted from<br />
volume 16 number 3 <strong>of</strong> the<br />
Journal.<br />
• The clinical review by Dr. Gerry<br />
Ross on photobiomodulation<br />
taken from volume 17 number 3<br />
sets the stage for Dr. Mel<br />
Burchman’s discussion <strong>of</strong> the use<br />
<strong>of</strong> this technology to enable<br />
dental treatment <strong>of</strong> a patient<br />
with severe Parkinson’s disease.<br />
• Dr. Raminta Mastis provides a<br />
valuable review <strong>of</strong> the proper use<br />
<strong>of</strong> laser safety signs in the dental<br />
environment.<br />
I trust you will find these articles<br />
both informational and a<br />
source <strong>of</strong> reference in the future.<br />
Looking forward to this new adventure,<br />
I remain,<br />
As Always,<br />
Stuart Coleton, DDS<br />
Stuart Coleton, DDS<br />
A U T H O R B I O G R A P H Y<br />
Dr. Stuart Coleton is a Diplomate<br />
<strong>of</strong> the American Board <strong>of</strong><br />
Periodontology and the American<br />
Board <strong>of</strong> Oral Medicine. He is chief<br />
attending periodontist at<br />
Westchester Medical Center<br />
University Hospital, holds the rank<br />
<strong>of</strong> assistant pr<strong>of</strong>essor in dental<br />
medicine at New York Medical<br />
College, and is the chief attending<br />
in periodontics at the Metropolitan<br />
Medical Center in New York City.<br />
He is a past president <strong>of</strong> the<br />
<strong>Academy</strong> <strong>of</strong> <strong>Laser</strong> <strong>Dentistry</strong> and is<br />
a Recognized Course Provider. He<br />
has been certified as having<br />
Advanced Pr<strong>of</strong>iciency, Educator,<br />
and Mastership status in lasers by<br />
the <strong>Academy</strong> <strong>of</strong> <strong>Laser</strong> <strong>Dentistry</strong>.<br />
His areas <strong>of</strong> special expertise are<br />
periodontal diagnosis and treatment<br />
as well as oral medicine. He<br />
has taught didactic and clinical<br />
laser therapy to both dental and<br />
medical general practice residents.<br />
Dr. Coleton may be contacted by<br />
e-mail at Scoleton@aol.com.<br />
Disclosure: Dr. Coleton is a stockholder<br />
in Lantis <strong>Laser</strong>, Inc. nn
Approaching ALD Prime<br />
J <strong>Laser</strong> Dent 2011;19(3):255<br />
As we approach the end <strong>of</strong> our 19th<br />
year as the premier, unbiased<br />
dental laser education entity, I<br />
would like to invite all our<br />
members, as well as all <strong>of</strong> the<br />
nonmember dentists that are just<br />
discovering dental lasers, to join us<br />
in Scottsdale, Arizona for our<br />
Annual Conference and Exhibition.<br />
The dates are March 29 to 31, 2012<br />
and I look forward to meeting all<br />
the attendees and to enjoy learning<br />
from the excellent presentations.<br />
I also want to share with you<br />
our most recent news. We have a<br />
new Editor-in-Chief, Dr. Stuart<br />
Coleton. We welcome him with<br />
open arms and look forward to<br />
working with him for many years<br />
to come. Also, in October the ALD’s<br />
Board <strong>of</strong> Directors met at the<br />
Radisson Fort McDowell, the venue<br />
for our 2012 Annual Conference.<br />
We are excited about the ALD’s<br />
new direction that includes<br />
creating educational materials<br />
more easily accessible to all<br />
members and creating a speakers<br />
bureau and course options to be<br />
<strong>of</strong>fered to dental organizations and<br />
to our members as well. We had a<br />
Leadership Development Day that<br />
was very successful. We worked<br />
very hard and still had time to<br />
have fun. The ADA-ALD <strong>Laser</strong><br />
Pavilion at the ADA Meeting in Las<br />
Vegas last October was a great<br />
success thanks to the hard work <strong>of</strong><br />
our Executive Director and one <strong>of</strong><br />
our past presidents, Dr. Don<br />
Coluzzi, who again presented<br />
dental lasers to all ADA members<br />
that wished to be informed about<br />
this technology. We are planning<br />
even more joint programs for next<br />
year’s ADA meeting. Our Web site<br />
has been revamped and we are<br />
striving to improve it regularly to<br />
make it easier to navigate by all <strong>of</strong><br />
our members. The 2012 Annual<br />
Conference Program is posted on<br />
the Web site for all to see what a<br />
great learning experience we will<br />
have in Scottsdale.<br />
Dr. Vipul Srivastava and a group<br />
<strong>of</strong> very dedicated Indian Dentists<br />
and Academicians from Lucknow,<br />
India had been working with Dr.<br />
Gabi Kessler since March 2011 to<br />
I am happy to preside over a Board <strong>of</strong> Directors that<br />
is working with a great sense <strong>of</strong> teamwork, dedication,<br />
and commitment; this also includes our Committee<br />
Chairs, and it is the best recipe for success.<br />
organize a Standard Pr<strong>of</strong>iciency<br />
Course in India. Dr. Srivastava and<br />
his group also wanted to create an<br />
ALD Affiliate Study Club in India.<br />
They were successful and in<br />
October our Board signed the<br />
agreement to make it <strong>of</strong>ficial. On<br />
December 17 and 18 in New Delhi,<br />
India and on December 19 and 20<br />
in Lucknow, India Dr Gabi Kesler<br />
presented Standard Pr<strong>of</strong>iciency<br />
Courses which were very well<br />
attended and represented the inauguration<br />
<strong>of</strong> the ALD Affiliate India<br />
Study Club. The President <strong>of</strong> the<br />
Dental Council <strong>of</strong> India, Dr.<br />
Dibyendu Mazumder, and other<br />
P R E S I D E N T ’ S M E S S A G E<br />
Ana Triliouris, DDS<br />
Merrick, New York<br />
ALD President 2011-2012<br />
dignitaries <strong>of</strong> the Indian Dental<br />
Community (including Dr. Anil<br />
Chandra, Dr. A.P. Tikku, and Dr.<br />
S.S. Ojha) were present. I was privileged<br />
to have been invited by the<br />
organizing group and enjoyed their<br />
great hospitality as I represented<br />
the <strong>Academy</strong> <strong>of</strong> <strong>Laser</strong> <strong>Dentistry</strong>. We<br />
returned with 25 new members<br />
and 10 registrations to our Annual<br />
Conference in Scottsdale. We look<br />
forward to welcoming the Indian<br />
contingency at the Radisson Resort<br />
this coming March.<br />
I am happy to preside over a<br />
Board <strong>of</strong> Directors that is working<br />
with a great sense <strong>of</strong> teamwork,<br />
dedication, and commitment; this<br />
also includes our Committee<br />
Chairs, and it is the best recipe for<br />
success. I am looking forward to<br />
celebrating our 20th Anniversary<br />
in 2013 with the ALD at its prime.<br />
Let’s continue moving forward and<br />
resolve to be committed and dedicated<br />
to the “ALD Prime.” I thank<br />
all <strong>of</strong> you for your hard work.<br />
Ana Maria Triliouris, DDS<br />
President <strong>of</strong> the <strong>Academy</strong> <strong>of</strong> <strong>Laser</strong><br />
<strong>Dentistry</strong> nn<br />
Triliouris<br />
J O U R N A L O F L A S E R D E N T I S T R Y | 2 011 V O L . 19 , N O . 3<br />
255
J O U R N A L O F L A S E R D E N T I S T R Y | 2 011 V O L . 19 , N O . 3<br />
256<br />
E X E C U T I V E D I R E C TO R ’ S M E S S A G E<br />
ALD – A History <strong>of</strong> Values<br />
Gail S. Siminovsky, CAE, Executive Director<br />
J <strong>Laser</strong> Dent 2011;19(3):256-257<br />
As we begin 2012, my sights are set<br />
12 months from now when we will<br />
be commemorating the <strong>Academy</strong> <strong>of</strong><br />
<strong>Laser</strong> <strong>Dentistry</strong>’s 20th Anniversary<br />
during our 2013 Annual Conference<br />
and Exhibition. As I think about<br />
how we will celebrate, I pause to<br />
reflect upon ALD’s journey as an<br />
organization over the years under<br />
the leadership <strong>of</strong> our past and<br />
current Boards <strong>of</strong> Directors, and<br />
through my own tenure as<br />
Executive Director and the guidance<br />
<strong>of</strong> my predecessors.<br />
Our organizational values firmly<br />
set the role <strong>of</strong> the <strong>Academy</strong> <strong>of</strong><br />
<strong>Laser</strong> <strong>Dentistry</strong> to serve dentistry<br />
as the pr<strong>of</strong>essional standardsetting<br />
society that we are. These<br />
values are the basis <strong>of</strong> our work<br />
with state regulatory agencies,<br />
dental associations, dental schools,<br />
the pr<strong>of</strong>essional community, and<br />
our members.<br />
Back in August 2002, ALD’s core<br />
Siminovsky<br />
values were set to guide our future<br />
direction and policymaking. With<br />
the help <strong>of</strong> the many voices <strong>of</strong> our<br />
constituents, we identified a beginning<br />
set <strong>of</strong> core values:<br />
1. Care<br />
2. Pr<strong>of</strong>essional Happiness<br />
3. Pr<strong>of</strong>essional Community<br />
4. Dental Family<br />
5. Research and Education, and<br />
6. Pr<strong>of</strong>essional Values. 1-2<br />
In 2004 during the development<br />
<strong>of</strong> the <strong>Academy</strong>’s 2005-2010<br />
Strategic Plan, key leaders <strong>of</strong> our<br />
organization summarized those six<br />
values into three general values:<br />
Integrity, Innovation, and<br />
Pr<strong>of</strong>essional Community.<br />
In 2010 our leadership developed<br />
our current 2010-2013<br />
Strategic Plan that we named<br />
‘Governing in Uncertain Times.’ In<br />
it we address the changing needs <strong>of</strong><br />
pr<strong>of</strong>essional environment, changes<br />
within our own leadership, and<br />
THE ACADEMY OF LASER DENTISTRY<br />
Core Values<br />
ALD is committed to the organizational values <strong>of</strong>:<br />
Integrity:<br />
Being trustworthy and reliable; transparent and accountable;<br />
objective and impartial<br />
Innovation:<br />
Being a knowledgeable and competent authority open to<br />
new ideas; actively and courageously leading the evolution<br />
<strong>of</strong> the body <strong>of</strong> knowledge<br />
Pr<strong>of</strong>essional Community:<br />
Being an inclusive forum for dialogue among a variety <strong>of</strong><br />
interests and perspectives; supporting and encouraging<br />
continuous participation in pr<strong>of</strong>essional development<br />
Gail S. Siminovsky, CAE, Executive Director<br />
your needs as members, all the<br />
while upholding our 3 general<br />
values <strong>of</strong> Integrity, Innovation, and<br />
Pr<strong>of</strong>essional Community.<br />
Our <strong>Academy</strong>’s values are essential<br />
to our being. They help us to<br />
achieve our mission and organizational<br />
purpose, provide<br />
fundamental policies, and determine<br />
our future direction. They are<br />
central to developing and fulfilling<br />
our strategic plans. 3 These core<br />
values are an integral part <strong>of</strong> who<br />
we are as an organization and<br />
remain so as we begin planning our<br />
20th Anniversary celebrations.<br />
As any organization evolves and<br />
grows and matures, many changes<br />
occur. Our biggest challenges<br />
include addressing strategies to<br />
fulfill our mission, vision, and goals<br />
while keeping our core values everpresent.<br />
Revisiting programs,<br />
sun-setting what may no longer<br />
work well, and developing new<br />
ways to achieve our mission is challenging,<br />
to say the least. It is part<br />
<strong>of</strong> every organization’s life cycle. As<br />
the economy has changed, ALD’s<br />
financial position has changed, and<br />
the years since 2009 have been<br />
challenging for our small organization.<br />
Our current strengthening<br />
financial standing has not come<br />
without sacrifice. It’s tough to<br />
make tough decisions, especially<br />
under such circumstances. Evolving<br />
and addressing needed change is<br />
courageous and hard to do well.<br />
The real success is in adapting and<br />
navigating through the difficult<br />
times to brighter times. As is the<br />
case with most organizations, not<br />
everyone always agrees. Different<br />
opinions are voiced. Building
consensus is a talent. I’m happy to<br />
report we approach 2012 with<br />
renewed spirit.<br />
Our current leadership has a<br />
strong sense <strong>of</strong> collegiality and we<br />
are devoted to working hard to<br />
become more inclusive, less rigid<br />
and more agile, more welcoming <strong>of</strong><br />
new members, and more appreciative<br />
<strong>of</strong> our volunteers, all at the<br />
same time upholding our core<br />
values and providing more educational<br />
opportunities. We are<br />
expanding our reach by collaborating<br />
with other larger dental<br />
associations like the American<br />
Dental Association (ADA), the<br />
<strong>Academy</strong> <strong>of</strong> General <strong>Dentistry</strong><br />
(AGD), and their various component<br />
societies. We continue our<br />
representation on the American<br />
National Standards Institute<br />
(ANSI) Accredited Standards<br />
Committee (ASC) Z136 for Safe<br />
Use <strong>of</strong> <strong>Laser</strong>s and its standards<br />
subcommittee SSC-3 Safe Use <strong>of</strong><br />
<strong>Laser</strong>s in Health Care. We are<br />
expanding our relationships with<br />
dental schools, state boards <strong>of</strong><br />
dental examiners, and other organizations,<br />
some <strong>of</strong> which are outlined<br />
in the listing <strong>of</strong> 10 ALD Facts. We<br />
have identified areas <strong>of</strong> member<br />
services that can be improved, and<br />
are working diligently to respond to<br />
our member’s needs<br />
We have taken our pulse and we<br />
approach our 20th Anniversary<br />
Year with enthusiasm, courage, and<br />
commitment to our foundational<br />
core values. We are excited for our<br />
future and the future <strong>of</strong> lasers in<br />
dentistry.<br />
See you in Scottsdale in just a<br />
few short weeks!<br />
Sincerely,<br />
Gail S. Siminovsky, CAE<br />
Executive Director<br />
10 ALD Facts<br />
E X E C U T I V E D I R E C TO R ’ S M E S S A G E<br />
1. ALD is a not-for-pr<strong>of</strong>it, independent organization that<br />
determines that pr<strong>of</strong>essional educational standards for<br />
the safe use <strong>of</strong> lasers are met.<br />
2. ALD is internationally recognized as a pr<strong>of</strong>essional standard-setting<br />
leader.<br />
3. ALD has no commercial bias.<br />
4. ALD is recognized by the ADA as an affiliated organization,<br />
is an ADA CERP Continuing Education Recognized<br />
Provider, and is an <strong>Academy</strong> <strong>of</strong> General <strong>Dentistry</strong><br />
approved program provider.<br />
5. ALD is a member <strong>of</strong> the National Coalition <strong>of</strong> General<br />
Dental Organizations.<br />
6. ALD plays an integral role in the ANSI Standards with<br />
the <strong>Laser</strong> Institute <strong>of</strong> America (LIA).<br />
7. ALD is a member <strong>of</strong> the American Dental Editors<br />
Association (ADEA).<br />
8. ALD participates with the Nevada State Board <strong>of</strong> Dental<br />
Examiners in reviewing dental laser educational courses.<br />
9. The American Dental Education Association (ADEA) has<br />
established a Special Interest Group on <strong>Laser</strong>s thanks to<br />
members <strong>of</strong> the ALD.<br />
10. ALD is represented on the ADA Standards Committee<br />
on Dental Products Working Group on Dental <strong>Laser</strong>s<br />
(ADA SCDP) and the ADA Standards Committee on<br />
Dental Informatics (ADA SCDI).<br />
R E F E R E N C E S<br />
1. Siminovsky GS. Core values workshop<br />
determines ALD’s future<br />
direction. Wavelengths 2002;10(4):5.<br />
2. Siminovsky GS. Values. J Acad<br />
<strong>Laser</strong> Dent 2004;12(2):7.<br />
3. Siminovsky GS. Values are the core<br />
<strong>of</strong> ALD policy-making. J Acad <strong>Laser</strong><br />
Dent 2005;13(4):14-15. nn<br />
Siminovsky<br />
J O U R N A L O F L A S E R D E N T I S T R Y | 2 011 V O L . 19 , N O . 3<br />
257
J O U R N A L O F L A S E R D E N T I S T R Y | 2 011 V O L . 19 , N O . 3<br />
258<br />
N O M I N AT I O N S<br />
<strong>Academy</strong> <strong>of</strong> <strong>Laser</strong> <strong>Dentistry</strong>’s 2012 Nominated<br />
Slate <strong>of</strong> Officers and Directors<br />
Arthur B. Levy, DMD, Chester, New Jersey<br />
As the final strains <strong>of</strong> Auld Lang<br />
Syne drift into the distance and the<br />
holidays become a fond memory,<br />
the business <strong>of</strong> the <strong>Academy</strong><br />
returns to its place in the forefront<br />
<strong>of</strong> our minds. The next year is a<br />
busy one preparing for our 20th<br />
Anniversary Year in 2013. Your<br />
Nominating Committee has been<br />
hard at work for the past few<br />
months reviewing questionnaires<br />
and evaluating the candidates<br />
submitted by you, the members, for<br />
positions on the Executive<br />
Committee and Board <strong>of</strong> Directors.<br />
We will be saying good-bye to some<br />
members <strong>of</strong> the Board <strong>of</strong> Directors<br />
and Officers, thanking them for<br />
their tireless and irreplaceable<br />
work for the <strong>Academy</strong> as well as<br />
welcoming new members into new<br />
positions in your <strong>Academy</strong><br />
Leadership. We are fortunate to<br />
have such a dedicated and tireless<br />
group to lead us and have had the<br />
good fortune to be able to select<br />
from a number <strong>of</strong> excellent choices.<br />
Unfortunately, not all members<br />
eligible and submitted can be<br />
chosen due to the limits on the<br />
positions placed in the Constitution<br />
and Bylaws. However, we have<br />
committee chair positions and<br />
committee assignments that will<br />
help us utilize the talent that we<br />
have available.<br />
As set forth in the Constitution<br />
and Bylaws, the Membership<br />
Meeting will take place on Friday,<br />
March 30, 2012 at the Conference<br />
taking place at the Radisson/Fort<br />
McDowell Resort in Scottsdale,<br />
Arizona. At that time the slate <strong>of</strong><br />
<strong>of</strong>ficers, presented below, will be<br />
voted on for the 2012-13 <strong>Academy</strong><br />
Year.<br />
Art Levy, DMD, Nominations<br />
Committee Chairman<br />
Characteristics and Attributes <strong>of</strong> an Ideal <strong>Academy</strong> <strong>of</strong> <strong>Laser</strong> <strong>Dentistry</strong> Board Member<br />
Proven Performance<br />
Leadership requires knowledge, talent, skill, vitality, and the<br />
ability to make a difference. In the association environment,<br />
that translates into a solid track record <strong>of</strong> contributing to the<br />
success <strong>of</strong> programs, events, or projects.<br />
Commitment<br />
Serving as an association leader is both an honor and a<br />
reward, but it requires a demonstrated commitment to the<br />
organization and its mission and goals.<br />
Time to Serve<br />
Participating fully in association activities requires extra time to<br />
prepare for travel and attend meetings.<br />
Understanding <strong>of</strong> Teamwork<br />
Many people contribute their efforts toward the realization <strong>of</strong><br />
an association’s goals and objectives – no one does it alone.<br />
Well-developed interpersonal and communication skills are<br />
essential to effective teamwork.<br />
Sound Judgment and Integrity<br />
In many instances, popularity brings potential leaders into the<br />
The Nominations Committee has<br />
selected the following nominees:<br />
• President-Elect:<br />
Glenda Payas, DMD<br />
• Vice President:<br />
Scott Benjamin, DMD<br />
• Treasurer:<br />
John Graeber, DMD<br />
• Secretary:<br />
Gabi Kesler, DMD.<br />
limelight <strong>of</strong> an association. But popularity must be tempered<br />
with good judgment and integrity. Decisions may need to be<br />
made that are not popular with the members but still serve the<br />
best interests <strong>of</strong> the organization as a whole.<br />
Communication and “Teaching” Skills<br />
By virtue <strong>of</strong> their position, current leaders serve as mentors<br />
and teachers to future leaders. Enthusiasm – a zest for serving<br />
the association – is an important ingredient that leaders must<br />
be able to pass along to their successors.<br />
Ability to Subordinate Special Interests<br />
Leaders <strong>of</strong>ten emerge because <strong>of</strong> their special expertise or<br />
effective representation <strong>of</strong> a specific constituency. Leadership,<br />
however, may require subordinating those interests for the<br />
greater good <strong>of</strong> the association.<br />
Be Strategic Thinkers<br />
Intuitive and interpretive skills enable leaders to understand the<br />
people around them, internalize the data they receive, recognize<br />
the relationships that exist between the systems within their<br />
world, and integrate all these elements into a coherent whole.
P R E S I D E N T- E L E C T :<br />
Dr. Glenda Payas<br />
Dr. Glenda Payas maintains a<br />
general dentistry practice in Tulsa,<br />
Oklahoma. She is a charter<br />
member <strong>of</strong> the <strong>Academy</strong> <strong>of</strong> <strong>Laser</strong><br />
<strong>Dentistry</strong> (ALD), and holds<br />
Advanced Pr<strong>of</strong>iciency in CO 2 and<br />
Er:YAG laser wavelengths. In 2007,<br />
Dr. Payas received her Mastership<br />
from the <strong>Academy</strong> <strong>of</strong> General<br />
<strong>Dentistry</strong> and is a clinical<br />
instructor for the Kois Center, in<br />
Seattle, Washington. She currently<br />
serves as Vice President on the<br />
ALD Executive Committee after<br />
having completed a 3-year term <strong>of</strong><br />
board service in 2009. She has held<br />
the positions <strong>of</strong> Secretary and<br />
Treasurer and is currently the<br />
Chair <strong>of</strong> the ALD Awards and<br />
Student Scholarship Committees as<br />
well as the upcoming Chair <strong>of</strong> the<br />
2013 Annual Conference. She was<br />
awarded the “2011 Top 25 Women<br />
in <strong>Dentistry</strong>” by Dental Products<br />
Report. She was one <strong>of</strong> the first<br />
dentists in the United States to use<br />
a laser, starting in 1991. Dr. Payas<br />
can be contacted at<br />
drglendapayas@msn.com.<br />
V I C E P R E S I D E N T :<br />
Dr. Scott Benjamin<br />
Dr. Scott Benjamin is a graduate<br />
<strong>of</strong> the State University <strong>of</strong> New York<br />
(SUNY) Buffalo, School <strong>of</strong> Dental<br />
Medicine and has been in full-time<br />
private practice in rural upstate<br />
New York for more than 30 years.<br />
Dr. Benjamin is an internationally<br />
recognized authority on oral cancer<br />
and a leader in computerized<br />
dental technology and dental<br />
lasers. He is a visiting pr<strong>of</strong>essor at<br />
the SUNY at Buffalo School <strong>of</strong><br />
Dental Medicine and is a research<br />
associate at the New York<br />
University (NYU) College <strong>of</strong><br />
<strong>Dentistry</strong>. He is an active member<br />
<strong>of</strong> American Dental Association<br />
Standards Committee on Dental<br />
Informatics (ADA-SCDI), the<br />
chairman <strong>of</strong> several separate<br />
Working Groups, and was<br />
appointed to the Task Force on the<br />
National Healthcare Information<br />
Infrastructure (NHII). Dr.<br />
Benjamin is a past president <strong>of</strong> the<br />
Sixth District Dental Society <strong>of</strong> the<br />
New York State Dental Association,<br />
has served on the ALD Board <strong>of</strong><br />
Directors and as the 2010 ALD<br />
Chairman <strong>of</strong> General and Scientific<br />
Sessions Committee for the Miami<br />
Conference. Currently he holds an<br />
Executive Committee position as<br />
Treasurer. Dr. Benjamin may be<br />
reached by e-mail at<br />
sbenjamin@dentalaim.com.<br />
T R E A S U R E R :<br />
Dr. John J. Graeber<br />
N O M I N AT I O N S<br />
Dr. John J. Graeber maintains a<br />
comprehensive, full-time general<br />
practice in East Hanover, New<br />
Jersey. He has been awarded<br />
Mastership in the <strong>Academy</strong> <strong>of</strong><br />
General <strong>Dentistry</strong> and the<br />
<strong>Academy</strong> <strong>of</strong> <strong>Laser</strong> <strong>Dentistry</strong>. He<br />
holds Advanced Pr<strong>of</strong>iciency in the<br />
Nd:YAG laser wavelength as well<br />
as Educator status and is a<br />
Recognized Course Provider. Dr.<br />
Graeber is a visiting lecturer in<br />
lasers at the University <strong>of</strong><br />
Medicine and <strong>Dentistry</strong> <strong>of</strong> New<br />
Jersey, New York University<br />
(NYU), and the University <strong>of</strong><br />
Minnesota Dental Schools. He<br />
utilizes Nd:YAG, diodes, and<br />
erbium laser wavelengths in his<br />
practice. He has been teaching the<br />
Standard Pr<strong>of</strong>iciency course since<br />
1996 and has served two terms on<br />
the ALD Board <strong>of</strong> Directors. In<br />
2011 he holds the position as<br />
Chairman <strong>of</strong> General and Scientific<br />
Sessions for the 2012 Scottsdale<br />
Conference along with the<br />
Executive Committee position as<br />
Secretary. Dr. Graeber may be<br />
reached by e-mail at<br />
hitekdr@mac.com.<br />
J O U R N A L O F L A S E R D E N T I S T R Y | 2 011 V O L . 19 , N O . 3<br />
259
J O U R N A L O F L A S E R D E N T I S T R Y | 2 011 V O L . 19 , N O . 3<br />
260<br />
N O M I N AT I O N S<br />
S E C R E TA RY :<br />
Dr. Gabi Kesler<br />
Dr. Gabi Kesler is in private<br />
general practice in Tel Aviv, Israel.<br />
He is a lecturer in the Department<br />
<strong>of</strong> Oral Rehabilitation at the Tel<br />
Aviv University School <strong>of</strong> Dental<br />
Medicine and is the coordinator <strong>of</strong><br />
the graduate and postgraduate<br />
dental laser program. He has<br />
Advanced Pr<strong>of</strong>iciency in CO 2 and<br />
Er:YAG laser wavelengths, is an<br />
ALD Recognized Course Provider,<br />
and has ALD Educator status. He<br />
received the Leon Goldman Award<br />
for clinical excellence and has<br />
published research papers on bone<br />
healing. He established the Israeli<br />
Chapter <strong>of</strong> the <strong>Academy</strong> <strong>of</strong> <strong>Laser</strong><br />
<strong>Dentistry</strong>, served as its first president<br />
in 2005, and currently serves<br />
as ALD’s Chairman <strong>of</strong><br />
International Relations. Previously<br />
Dr. Kesler completed two 3-year<br />
terms <strong>of</strong> leadership service on the<br />
ALD Board <strong>of</strong> Directors. He is<br />
nominated for the position <strong>of</strong><br />
Secretary 2012-13. Dr. Kesler<br />
may be reached by e-mail at<br />
drkeslerg@-12.net.il.<br />
The <strong>of</strong>fices <strong>of</strong> President, Dr. Art<br />
Levy, and Immediate Past<br />
President, Dr. Ana Triliouris, are<br />
automatically filled, and are not<br />
part <strong>of</strong> the voting process.<br />
Dr. Art Levy automatically<br />
assumes the role <strong>of</strong> President in<br />
2012 and Dr. Ana Triliouris<br />
moves into the position <strong>of</strong><br />
Immediate Past President.<br />
P R E S I D E N T :<br />
Dr. Arthur Levy<br />
Dr. Arthur Levy maintains a<br />
private practice in Chester, New<br />
Jersey, and is a charter member <strong>of</strong><br />
the ALD. He holds Advanced<br />
Pr<strong>of</strong>iciency in the Nd:YAG laser<br />
wavelength. He has served two 3year<br />
terms on the ALD Board <strong>of</strong><br />
Directors and has been active in<br />
numerous committees including<br />
International Relations,<br />
Membership, Finance,<br />
Nominations, and Awards since the<br />
beginning <strong>of</strong> the <strong>Academy</strong> in 1993.<br />
Dr. Levy currently serves as<br />
President-Elect. Dr. Levy may be<br />
contacted by e-mail at<br />
lsrdocl<strong>of</strong>t@embarqmail.com.<br />
I M M E D I AT E PA S T<br />
P R E S I D E N T :<br />
Dr. Ana Maria Triliouris<br />
Dr. Ana Maria Triliouris maintains<br />
a private practice in Merrick,<br />
New York, and is a charter member<br />
<strong>of</strong> the ALD. She is among the very<br />
few dentists that started using<br />
lasers in 1990. She was the first<br />
editor <strong>of</strong> ALD’s initial publication,<br />
Wavelengths. She is an active<br />
member <strong>of</strong> the ADA and its components<br />
as well as the <strong>Academy</strong> <strong>of</strong><br />
General <strong>Dentistry</strong> and the<br />
American Association <strong>of</strong> Women<br />
Dentists. She is past Chair <strong>of</strong> the<br />
Dr. Eugene Seidner Student<br />
Scholarship Committee, past editor<br />
<strong>of</strong> the newsletter Lightwaves, and<br />
has held various other leadership<br />
positions in the ALD. Dr. Triliouris<br />
may be reached by e-mail at<br />
amtdds@gmail.com.<br />
2 012 - 2 015<br />
N O M I N AT E D B OA R D<br />
M E M B E R S<br />
Following a successful election<br />
during the General Membership<br />
Meeting, these nominated members<br />
will join the ALD Board <strong>of</strong><br />
Directors for a 3-year term starting<br />
March 31, 2012.<br />
Dr. Charles Hoopingarner<br />
Dr. Charles Hoopingarner<br />
attended the University <strong>of</strong> Texas<br />
Health Science Center at Houston<br />
(UTHSCH) Dental Branch, graduating<br />
with a DDS in 1973. He has<br />
maintained a private practice in<br />
Houston, Texas since 1973. He was<br />
an adjunct associate pr<strong>of</strong>essor in<br />
anatomical sciences at UTHSCH<br />
Dental Branch for 11 years.<br />
Currently he is adjunct clinical<br />
faculty in the Restorative <strong>Dentistry</strong><br />
Department at UTHSCH and has<br />
been a clinical instructor at the Las<br />
Vegas Institute for Advanced<br />
Dental Studies since 1997, teaching<br />
advanced anterior aesthetics and<br />
comprehensive aesthetic reconstruction<br />
and laser dentistry. Dr.<br />
Hoopingarner is a member <strong>of</strong> the<br />
Board <strong>of</strong> Directors <strong>of</strong> the ALD and<br />
has used dental lasers <strong>of</strong> various<br />
wavelengths as integral parts <strong>of</strong> his<br />
patient care delivery system for the<br />
last 11 years. He is the ALD<br />
Regulatory Affairs Committee<br />
Chair and Vice Chair <strong>of</strong> the
Certification Committee. He holds<br />
Advanced and Standard Pr<strong>of</strong>iciency<br />
certifications in the Er:YAG and<br />
diode laser wavelengths from the<br />
ALD and has lectured internationally<br />
on the safe use <strong>of</strong> laser<br />
technology in the dental practice.<br />
He is nominated for a second 3year<br />
term <strong>of</strong> service on the ALD<br />
Board. Dr. Hoopingarner may be<br />
contacted by e-mail at<br />
choop@swbell.net.<br />
Dr. Edward Kusek<br />
Dr. Edward Kusek is a 1984 graduate<br />
<strong>of</strong> the University <strong>of</strong> Nebraska<br />
School <strong>of</strong> <strong>Dentistry</strong>. He is in private<br />
general practice in Sioux Falls,<br />
South Dakota. He is a Diplomate <strong>of</strong><br />
the American Board <strong>of</strong> Oral<br />
Implantology/Implantology/<br />
Implant <strong>Dentistry</strong>, a Fellow <strong>of</strong> the<br />
American <strong>Academy</strong> <strong>of</strong> Implant<br />
<strong>Dentistry</strong> and <strong>Academy</strong> <strong>of</strong> <strong>Laser</strong><br />
<strong>Dentistry</strong>, has earned Mastership in<br />
the <strong>Academy</strong> <strong>of</strong> General <strong>Dentistry</strong><br />
and World Clinical <strong>Laser</strong> Institute<br />
(WCLI), and Advanced Pr<strong>of</strong>iciency<br />
in the <strong>Academy</strong> <strong>of</strong> <strong>Laser</strong> <strong>Dentistry</strong><br />
in the Er,Cr:YSGG laser wavelength.<br />
Dr. Kusek currently serves<br />
on the Certification Committee. He<br />
is an adjunct pr<strong>of</strong>essor at the<br />
University <strong>of</strong> South Dakota and<br />
lectures nationally and internationally<br />
on the erbium laser and dental<br />
implants. He is nominated for a<br />
3-year term <strong>of</strong> service on the ALD<br />
Board <strong>of</strong> Directors. Dr. Kusek may<br />
be reached by e-mail at<br />
edkusek@me.com<br />
Jeanette Miranda, RDH<br />
Jeanette Miranda, RDH, has<br />
practiced dental hygiene for 31<br />
years and has worked with dental<br />
lasers for 7 years. She currently<br />
practices hygiene with Dr. Ed<br />
Kusek. She has achieved diode<br />
laser Standard Pr<strong>of</strong>iciency with the<br />
WCLI and ALD, and diode laser<br />
Fellowship status with the WCLI.<br />
Ms. Miranda serves on the ALD<br />
<strong>Laser</strong> Safety Committee and as<br />
Vice Chair for the Auxiliary<br />
Committee. In addition to lecturing<br />
on periodontal treatment with<br />
lasers, she teaches diode laser<br />
courses with Dr. Edward Kusek<br />
and Dr. Fred Margolis. Ms.<br />
Miranda is nominated for a 3-year<br />
term as the Auxiliary representative<br />
on the ALD Board <strong>of</strong> Directors.<br />
Jeanette may be reached by e-mail<br />
at jmirand@sio.midco.net.<br />
Dr. Steve Parrett<br />
Dr. Steve Parrett is in the private<br />
practice <strong>of</strong> general dentistry in<br />
Chambersburg, Pennsylvania<br />
where he is currently chairman <strong>of</strong><br />
the Department <strong>of</strong> <strong>Dentistry</strong> at<br />
Chambersburg Hospital. He holds<br />
Standard Pr<strong>of</strong>iciency in Er:YAG,<br />
diode, and CO 2 laser wavelengths.<br />
He is a member <strong>of</strong> the Dean’s<br />
Faculty at the University <strong>of</strong><br />
Maryland Dental School, and has<br />
N O M I N AT I O N S<br />
served on the House <strong>of</strong> Delegates <strong>of</strong><br />
the ADA and Pennsylvania Dental<br />
Association (PDA). He has achieved<br />
Fellowship status in the <strong>Academy</strong><br />
<strong>of</strong> General <strong>Dentistry</strong> and has<br />
served many years as a clinical<br />
evaluator for Dr. Gordon<br />
Christenson’s CRA independent<br />
research organization. He serves on<br />
the ALD’s Membership and<br />
Regulatory Affairs Committees and<br />
has served on the ALD<br />
Communications Committee in the<br />
past. Dr. Parrett currently serves<br />
on the ALD Board <strong>of</strong> Directors and<br />
is nominated for his second 3-year<br />
term. Dr. Parrett may be reached at<br />
drp@embarqmail.com.<br />
2 011- 2 012 A L D<br />
N O M I N AT I O N S<br />
C O M M I T T E E<br />
Art Levy, DMD, President-Elect,<br />
Chester, NJ<br />
Steven Burman, DMD, Immediate<br />
Past President, Manalapan, NJ<br />
Tony Hewlett, DDS, Stanwood, WA<br />
Raminta Mastis, DDS, St. Clair<br />
Shores, MI<br />
Emile Martin, DDS, Syracuse, NY<br />
Gail Siminovsky, CAE, Executive<br />
Director, Coral Springs, FL nn<br />
<strong>Academy</strong> <strong>of</strong> <strong>Laser</strong> <strong>Dentistry</strong><br />
to Hold General<br />
Membership Meeting in<br />
Scottsdale, Arizona on<br />
March 30, 2012<br />
The <strong>Academy</strong> <strong>of</strong> <strong>Laser</strong> <strong>Dentistry</strong><br />
will conduct its general membership<br />
business meeting on March<br />
30, 2012 during the 19th Annual<br />
Conference and Exhibition. Dr. Art<br />
Levy, Nominations Chair and<br />
President-Elect, will explain the<br />
selection process for ALD directors<br />
and <strong>of</strong>ficers as well as the organizational<br />
committee structure.<br />
Eligible voting members present in<br />
Scottsdale will be asked to vote to<br />
accept the nominees to serve in<br />
Board leadership positions for the<br />
<strong>Academy</strong> <strong>of</strong> <strong>Laser</strong> <strong>Dentistry</strong>.<br />
J O U R N A L O F L A S E R D E N T I S T R Y | 2 011 V O L . 19 , N O . 3<br />
261
J O U R N A L O F L A S E R D E N T I S T R Y | 2 011 V O L . 19 , N O . 3<br />
262<br />
A WA R D S<br />
ALD Award Recipients<br />
Announced for 2012<br />
Glenda Payas, DMD, Award Committee Chair<br />
Many <strong>of</strong> the members <strong>of</strong> the<br />
<strong>Academy</strong> <strong>of</strong> <strong>Laser</strong> <strong>Dentistry</strong> (ALD)<br />
submerge themselves in the<br />
dynamics <strong>of</strong> laser dentistry on a<br />
day-by-day basis. They put in long<br />
days at the <strong>of</strong>fice serving their<br />
patients, and in their “free time”<br />
they dedicate themselves in even<br />
deeper ways. They spend time in<br />
research developing new treatment<br />
techniques, write journal articles,<br />
teach at seminars, mentor<br />
colleagues, and spend countless<br />
hours volunteering on <strong>Academy</strong><br />
committees, and they do this<br />
without the thought <strong>of</strong> being given<br />
an award.<br />
The ALD has three awards to<br />
celebrate the hard work <strong>of</strong> its<br />
members: The T.H. Maiman Award<br />
for Excellence in Dental <strong>Laser</strong><br />
Research, The Leon Goldman<br />
Award for Clinical Excellence, and<br />
The Distinguished Service Award<br />
for Outstanding Commitment and<br />
Contributions to the <strong>Academy</strong>.<br />
Because <strong>of</strong> the level <strong>of</strong> sacrifice<br />
our members are committed to,<br />
they understand the criteria it<br />
takes when nominating another<br />
member for one <strong>of</strong> these prestigious<br />
awards. Their nominees are above<br />
the standard and show such dedication<br />
and passion.<br />
As the Awards Committee Chair,<br />
I present to you our 2012 award<br />
recipients. I congratulate each <strong>of</strong><br />
these ALD members that are<br />
honored here.<br />
Our 2012 recipient <strong>of</strong> The Leon<br />
Goldman Award for Clinical<br />
Excellence is Dr. Mel Burchman.<br />
He is an educator, clinician, and<br />
pioneer in the usage <strong>of</strong> low-level<br />
laser therapy (LLLT), particularly<br />
in the treatment <strong>of</strong> the medically<br />
compromised patient.<br />
Dr. Burchman has used lasers in<br />
his private practice since 1999 and<br />
holds both Standard Pr<strong>of</strong>iciency<br />
(SP) and Advanced Pr<strong>of</strong>iciency (AP)<br />
certifications in multiple laser<br />
wavelengths and has achieved<br />
educator status in the <strong>Academy</strong>. He<br />
has used Nd:YAG, diode, and<br />
Er,Cr:YSGG laser wavelengths in<br />
addition to<br />
the work he<br />
has done with<br />
LLLT.<br />
He is a<br />
Master <strong>of</strong> the<br />
<strong>Academy</strong> <strong>of</strong><br />
<strong>Laser</strong><br />
<strong>Dentistry</strong> and<br />
Mel A. Burchman, DDS<br />
has presented<br />
Glenda Payas, DMD,<br />
Awards Committee Chair<br />
multiple times to both our<br />
<strong>Academy</strong> and our Israeli chapter.<br />
He is currently Chairman <strong>of</strong> the<br />
Certification Committee while<br />
being an examiner and a mentor to<br />
our SP and AP candidates. Working<br />
on medically compromised patients<br />
in his private practice in Bucks<br />
County, Pennsylvania, is the area <strong>of</strong><br />
which he is most proud.<br />
Upon learning <strong>of</strong> his honor, Mel<br />
remarked, “Working on medically<br />
compromised patients is absolutely<br />
the most rewarding phase <strong>of</strong> my<br />
practice. Most <strong>of</strong> these patients have<br />
been patients and friends for many<br />
years. To know that you have helped<br />
these people by avoiding another<br />
hospitalization, changes in medications,<br />
and additional expenses is<br />
the best feeling you can have! I am<br />
most grateful to be honored with<br />
this award.”
For The T.H. Maiman Award<br />
for Excellence in Dental <strong>Laser</strong><br />
Research our award recipient is<br />
Dr. Sebastiano Andreana. Several<br />
accomplishments must be met for a<br />
person to be considered qualified as<br />
a nominee for this prestigious<br />
award. He or she should be a<br />
researcher, a<br />
pr<strong>of</strong>essional<br />
clinician, and<br />
an academician;<br />
must<br />
have<br />
published<br />
papers; and<br />
Sebastiano Andreana<br />
not only be<br />
involved but<br />
contribute to<br />
the goals and mission <strong>of</strong> ALD.<br />
Dr. Sebastiano Andreana earned<br />
his dental degree at the University<br />
<strong>of</strong> Rome La Sapienza School <strong>of</strong><br />
<strong>Dentistry</strong> in 1990. He earned a<br />
master <strong>of</strong> science degree in oral<br />
sciences from the State University <strong>of</strong><br />
New York at Buffalo School <strong>of</strong> Dental<br />
Medicine in 1995. He has been a<br />
member <strong>of</strong> the International<br />
Association for Dental Research<br />
since 1991; an associate member<br />
American <strong>Academy</strong> <strong>of</strong> Periodontology<br />
since 2003; and is an active member<br />
<strong>of</strong> New York <strong>Academy</strong> <strong>of</strong> Sciences.<br />
He currently is Clinical Assistant<br />
Pr<strong>of</strong>essor in the Department <strong>of</strong><br />
Restorative <strong>Dentistry</strong>, School <strong>of</strong><br />
Dental Medicine, State University <strong>of</strong><br />
New York at Buffalo. He is a<br />
reviewer <strong>of</strong> a several journals,<br />
including the Journal <strong>of</strong><br />
Periodontology, Journal <strong>of</strong> the<br />
American Dental Association, British<br />
Dental Journal, Immunological<br />
Investigations, and Journal <strong>of</strong><br />
Osseointegration. He is presently the<br />
Senior Associate Editor <strong>of</strong> the<br />
Journal Oral Implantology. He<br />
currently serves the <strong>Academy</strong> <strong>of</strong><br />
<strong>Laser</strong> <strong>Dentistry</strong> as University and<br />
Academia Relations Chair and has<br />
served as Vice Chair <strong>of</strong> ALD’s<br />
Science and Research Committee.<br />
When he heard about his nomination,<br />
Dr. Andreana responded by<br />
saying, “I should admit I was very<br />
surprised to hear about my nomination,<br />
definitely unexpected! Within<br />
our organization we have several<br />
researchers that deserve the nomination<br />
and I am surely honored to<br />
be the one this year. Knowing that<br />
my name will be in the same list <strong>of</strong><br />
some outstanding laser researchers<br />
is truly an honor. I will do my best<br />
to continue to work in this field, to<br />
allow more clinicians and therefore<br />
more patients to benefit from using<br />
the laser technology in dentistry.”<br />
And our recipient for The<br />
<strong>Academy</strong> <strong>of</strong> <strong>Laser</strong> <strong>Dentistry</strong><br />
Distinguished Service Award<br />
for Outstanding Commitment and<br />
Contributions to the <strong>Academy</strong> is<br />
Dr. Emile Martin.<br />
A Past President and Board<br />
member <strong>of</strong> the <strong>Academy</strong> <strong>of</strong> <strong>Laser</strong><br />
<strong>Dentistry</strong>, Dr. Martin has maintained a<br />
private dental practice since 1975. He<br />
is a graduate <strong>of</strong> the Temple University<br />
School <strong>of</strong> <strong>Dentistry</strong>, and successfully<br />
completed a 3-year participatory<br />
program in Dental Implantology from<br />
A WA R D S<br />
the University<br />
<strong>of</strong><br />
Pennsylvania.<br />
He has<br />
achieved<br />
Educator and<br />
Mastership<br />
status in the<br />
Dr. Emile Martin<br />
ALD, and is a<br />
Fellow <strong>of</strong> the<br />
American <strong>Academy</strong> <strong>of</strong> Implant<br />
<strong>Dentistry</strong> and a Diplomate <strong>of</strong> the<br />
American Board <strong>of</strong> Oral<br />
Implantology/Implant <strong>Dentistry</strong>. He<br />
has served in various executive positions<br />
with many pr<strong>of</strong>essional dental<br />
organizations, and has made<br />
numerous presentations on laser and<br />
implant dentistry at dental conferences<br />
around the world. He has been<br />
a reviewer for the Journal <strong>of</strong> the<br />
American Dental Association,<br />
Journal <strong>of</strong> Oral Implantology, and<br />
the Journal <strong>of</strong> the <strong>Academy</strong> <strong>of</strong> <strong>Laser</strong><br />
<strong>Dentistry</strong>. He is a recipient <strong>of</strong> the<br />
<strong>Academy</strong> <strong>of</strong> General <strong>Dentistry</strong>’s<br />
Lifetime Learning and Service<br />
Recognition Award.<br />
When he heard about his<br />
Distinguished Service Award, Dr.<br />
Martin stated, “I have been privileged<br />
to work in a leadership capacity in<br />
several national dental organizations.<br />
I have always enjoyed dental organizational<br />
work. It is a way to give back<br />
to the pr<strong>of</strong>ession that I love, meet<br />
people from all parts <strong>of</strong> the United<br />
States and around the globe, and<br />
learn something new at the same<br />
time. I am humbled and grateful to<br />
the Committee that has seen fit to<br />
bestow this honor upon me.” nn<br />
J O U R N A L O F L A S E R D E N T I S T R Y | 2 011 V O L . 19 , N O . 3<br />
263
J O U R N A L O F L A S E R D E N T I S T R Y | 2 011 V O L . 19 , N O . 3<br />
264<br />
2 012 C O N F E R E N C E<br />
Elevating Your Practice<br />
to New Peaks!<br />
John J. Graeber, DMD MAGD MALD FICD,<br />
East Hanover, New Jersey<br />
We have assembled many <strong>of</strong> the<br />
best laser educators in the world to<br />
conduct our Annual Scientific<br />
Meeting!<br />
As part <strong>of</strong> our preconference<br />
certification program on Wednesday,<br />
March 28, Dr. Will Gianni, Dr. Mitch<br />
Lomke, and Angie Mott, RDH will<br />
present this year’s Standard<br />
Pr<strong>of</strong>iciency Course. New this year<br />
will be <strong>Laser</strong>s 101 — a 3-hour introductory<br />
course for nonusers led by<br />
Dr. Chuck Hoopingarner.<br />
World-famous physicist Dr.<br />
Gregory Altschuler will be our<br />
opening session keynote speaker on<br />
Thursday. He will share his experiences<br />
as a laser pioneer in the former<br />
Soviet Union and his new projects in<br />
developing the next generation <strong>of</strong><br />
lasers. The program on chromophores<br />
by Dr. Bryant Cornelius and Dr.<br />
Jeffery Cornelius promises to be very<br />
enlightening. Mary Lynn Smith,<br />
RDH will be sharing insights<br />
comparing the use <strong>of</strong> 980-nm and<br />
10,600-nm laser wavelengths in<br />
nonsurgical perio dontal therapy.<br />
Gloria Monzon, RDH will compare<br />
the effects <strong>of</strong> 3 laser wavelengths on<br />
one patient years apart.<br />
Hands hurt? Cracked? Wonder<br />
about gloves? Leslie Canham, CDA<br />
will poke some fun into these topics.<br />
Endo, anyone? Dr. Ron Porth will<br />
share his ongoing study <strong>of</strong> the efficacy<br />
<strong>of</strong> lasers in the canals. Dr. Roy<br />
George <strong>of</strong> Australia will show us<br />
W E I N V I T E YO U TO S C OT T S DA L E !<br />
Your Conference Committee has devoted itself to making this<br />
year’s ALD Annual Conference what you, the members, want:<br />
You asked for clinically relevant presentations – You’ve got them!<br />
30 CLINICAL PRESENTATIONS<br />
You asked for meaningful hands-on experiences – You’ve got them!<br />
11 WORKSHOPS<br />
You asked for diode laser programs – You’ve got them!<br />
11 PRESENTATIONS AND WORKSHOPS<br />
You asked for some fun in the sun – You’ve got it!<br />
LASER JEOPARDY, HANDS-ON HYGIENE<br />
You asked for low-level science and applications – You’ve got them!<br />
13 PRESENTATIONS<br />
You asked for a dedicated Hygiene Day – You’ve got it!<br />
OUR BEST HYGIENE EDUCATORS<br />
You asked for specialist days – You’ve got them!<br />
ORTHODONTICS AND PEDIATRIC DENTISTRY<br />
Now y’all come to Scottsdale – and bring your friends!<br />
John Graeber, DMD, General and<br />
Scientific Sessions Committee Chairman<br />
how newly modified fiber optics can<br />
enhance our results. Popular<br />
speakers Dr. Giovanni Olivi, Dr.<br />
Felice Marmoro, Dr. Caterina<br />
Faccin, and Dr. Guiseppe Bray (all<br />
from Italy), and Dr. Enrico DiVito<br />
(who is local to Scottsdale now) will<br />
show us the advantages <strong>of</strong> photoacoustic<br />
streaming. Dr. Mel<br />
Burchman will describe an interesting<br />
case <strong>of</strong> endodontic surgery on<br />
a medically compromised patient.<br />
Perio, anyone? Internationally<br />
known periodontist Dr. Larry Nurin<br />
will share his secrets <strong>of</strong> laser use<br />
over the past 21 years <strong>of</strong> practice. We<br />
will see how periodontal surgery is<br />
performed in Japan by the renowned<br />
Dr. Hisamori Hayashihara. Thursday<br />
workshops will include DNA testing<br />
by Dr. Doug Gilio, diode surgery by<br />
Dr. Phil Hudson, and Keynote on<br />
Mac by Dr. Larry Kotlow (bring your<br />
Mac computer!).<br />
Friday will begin with Past<br />
President Dr. Kim Kutch giving a<br />
keynote presentation on minimally<br />
invasive dentistry. Our student<br />
presenter, Jeema Dad, will share her<br />
work in a study <strong>of</strong> bond strengths in<br />
lased tooth structure. Dr. Sebastiano<br />
Andreana and Jeanette Miranda,<br />
RDH will describe the use <strong>of</strong> lasers<br />
in implant dentistry. Dr. Chris<br />
Walinski is going to show us how to<br />
accomplish minimally invasive techniques<br />
with erbium lasers. Dr. Gabi<br />
Kesler from Israel will share bone<br />
healing with erbium lasers. Dr.<br />
Larry Kotlow will have some<br />
provocative thoughts about why we<br />
don’t get the most use out <strong>of</strong> our<br />
lasers. Drs. Peter Pang and Rick<br />
Cordoza will share their cosmetic
estorative cases with us. We finish<br />
Friday with Dr. Paul Silver’s handson<br />
diode laser practical, Dr. Mitch<br />
Lomke’s laser-assisted crown lengthening<br />
workshop, and an interactive<br />
workshop with 20-year laser veteran<br />
Dr. Phil Hudson on practice management<br />
with lasers.<br />
Also on busy Friday will be the<br />
all-day Pediatric <strong>Dentistry</strong> program<br />
with hands-on activities with Drs.<br />
Larry Kotlow, Fred Margolis,<br />
Giovanni Olivi, and Claudia<br />
Caprioglio, and the new all-day<br />
Orthodontists program with Drs.<br />
Lou Chmura, Stephen Tracey, and<br />
J. Courtney Gorman.<br />
We hope your hygienists are<br />
planning to attend our all-day<br />
Hygienist Extravaganza. This will<br />
be a one-day, separate ticketed event<br />
for hygienists, both new and experienced.<br />
The day will be headlined by<br />
Dr. Chris Owens who has trained<br />
thousands <strong>of</strong> practitioners, and ably<br />
complemented by ALD Recognized<br />
Course Providers Gloria Monzon,<br />
RDH and Angie Mott, RDH, along<br />
with Mary Lynn Smith, RDH. Dr.<br />
Gerald Ross will discuss low-level<br />
laser procedures by hygienists.<br />
Saturday will feature an all-day<br />
program on photobiomodulation –<br />
an ALD first-time event! – as well<br />
as programs in oral surgery. For the<br />
photobiomodulation segment, we<br />
will welcome members <strong>of</strong> the North<br />
American Association for <strong>Laser</strong><br />
Therapy (NAALT): Dr. Praveen<br />
Arany, Mr. James Carroll, Dr. John<br />
Hendy, Dr. Mark Dincher, Mr. Steve<br />
Liu, and Dr. Harry Whelan who will<br />
be joined by international presenters<br />
Drs. Juliana Barros and<br />
Shalizeh Patel <strong>of</strong> the University <strong>of</strong><br />
Texas Health Science Center at<br />
Houston, Dr. Masoud Mojahedi<br />
from Germany, Dr. Claudia<br />
Caprioglio from Italy, Dr. Shally<br />
Mahajan from India, and moderator<br />
Dr. Gerry Ross from Canada.<br />
For Saturday’s oral surgery<br />
program, Dr. Ed Kusek will present<br />
on use <strong>of</strong> the erbium laser in s<strong>of</strong>ttissue<br />
grafting. Dr. Nitin Agarwal<br />
will show how to treat oral submu-<br />
cosal fibrosis with diode, Er:YAG,<br />
and Nd:YAG lasers. Dr. Claus<br />
Neckel will present diode laser<br />
cases for treatment <strong>of</strong> impacted<br />
and displaced cuspids; Dr. Jay Sher<br />
on clinical crown lengthening with<br />
the CO 2 laser; Dr. Mike Kelly <strong>of</strong><br />
Scottsdale on depigmentation with<br />
the CO 2 laser; and Dr. Larry<br />
Kotlow on erbium and Nd:YAG<br />
laser-assisted s<strong>of</strong>t tissue surgery.<br />
Last year’s hit program “<strong>Laser</strong><br />
Safety in Jeopardy!” promises us<br />
lots more humor, produced by Dr.<br />
Raminta Mastis and the <strong>Laser</strong><br />
Safety Committee.<br />
2 012 C O N F E R E N C E<br />
Don’t forget the Pioneers Panel<br />
— past presidents Dr. Bob Pick, Dr.<br />
Terry Myers, and Dr. Kim Kutsch<br />
will join Dr. Gregory Altshuler as<br />
they use their perspectives to peer<br />
into the future for the next 20<br />
years <strong>of</strong> lasers in dentistry. That<br />
will lead us into our 20th anniversary<br />
celebration in 2013.<br />
Meet me there!<br />
John Graeber, DMD nn<br />
Final schedule is subject to change.<br />
Join us in Philadelphia this June to enjoy the freedom <strong>of</strong> earning<br />
an entire year’s worth <strong>of</strong> continuing education in one great location!<br />
This year’s educational program includes:<br />
� “Key Implant Position and Implant Number: A Biomechanical Rationale<br />
to Treatment Planning,” Carl E. Misch, BS, DDS, MDS, PhD (hc)<br />
� “Advanced Oral Surgery Techniques for Smoother, Easier, Less Stressful<br />
Procedures,” Karl Koerner, DDS, FAGD, MS<br />
� “What’s Hot and What’s Getting Hotter,” Howard S. Glazer, DDS, FAGD<br />
� “The Occlusal Secrets You Should Have Learned in Kindergarten:<br />
Or, How to Take Your Practice to the Next Level,” Irwin Becker, DDS<br />
REGISTER TODAY!<br />
www.agd.org/philadelphia<br />
You’ll learn tips<br />
and techniques<br />
you can use as soon as you<br />
get back to the <strong>of</strong>fice.<br />
And don’t forget your staff —<br />
we’ve planned a variety <strong>of</strong><br />
practical educational<br />
opportunities<br />
for them, too!<br />
See the latest<br />
dental equipment<br />
and materials in our<br />
Exhibit Hall with<br />
more than<br />
200 exhibitors!<br />
J O U R N A L O F L A S E R D E N T I S T R Y | 2 011 V O L . 19 , N O . 3<br />
265
J O U R N A L O F L A S E R D E N T I S T R Y | 2 011 V O L . 19 , N O . 3<br />
266<br />
C E R T I F I C AT I O N<br />
ALD Certification Program Planned in<br />
Scottsdale, March 29-31, 2012<br />
Mel Burchman, DDS, Langhorne, Pennsylvania<br />
G R E E T I N G S TO A L L M Y<br />
F E L LO W A L D<br />
M E M B E R S !<br />
Our 19th Annual Conference in<br />
Scottsdale, Arizona is approaching<br />
quickly. However, there is still<br />
ample time to sign up for a certification<br />
examination. Last year’s<br />
conference was tremendously<br />
successful. We had 29 candidates<br />
receive their Standard Pr<strong>of</strong>iciency, 3<br />
candidates pass Advanced<br />
Pr<strong>of</strong>iciency (AP) Online Review and<br />
Written Examination and AP<br />
Clinical Simulation Examination,<br />
and one candidate complete AP<br />
Case Study Examination. We’d like<br />
to increase those numbers this year.<br />
This has been a very busy time<br />
Burchman<br />
for the people on the Certification<br />
Committee. We have been hard at<br />
work analyzing the <strong>Academy</strong>’s certification<br />
process and have made<br />
some wonderful enhancements to<br />
the program. We are trying our best<br />
to make the journey to Advanced<br />
Pr<strong>of</strong>iciency as candidate-friendly as<br />
possible. People may now take AP<br />
Online Review and Written Exam<br />
or AP Clinical Simulation Exam at<br />
the same time or in whichever order<br />
they like. The time frame between<br />
completing AP Online Review and<br />
Written Exam and AP Clinical<br />
Simulation Exam and being eligible<br />
to test for the AP Case Study Exam<br />
has been shortened to one year.<br />
We are also in the process <strong>of</strong><br />
You are cordially invited to our<br />
Advanced Pr<strong>of</strong>iciency Review Course<br />
Launch <strong>of</strong> the Class <strong>of</strong> 2014<br />
Wine and Cheese Reception<br />
at<br />
ALD’s 19th Annual Conference<br />
Saturday March 31, 2012<br />
3:00 - 4:30 pm<br />
Radisson Fort McDowell, Room 111<br />
Join us to find out more<br />
about the AP program!<br />
Mel Burchman, DDS, Certification<br />
Committee Chairman<br />
completing a totally new AP Online<br />
Review. This could not have been<br />
accomplished without the diligent<br />
work and long hours <strong>of</strong> a subcommittee<br />
composed <strong>of</strong> Ms. Angie Mott,<br />
RDH, Dr. Ed Kusek, Dr. Charles<br />
Hoopingarner, and myself.<br />
Another subcommittee has been<br />
formed to review and analyze the<br />
<strong>Academy</strong>’s test question library.<br />
Their job is to remove outdated or<br />
ambiguous questions. A third<br />
subcommittee has been formed to<br />
analyze the AP process for specialists.<br />
We want to make the<br />
examination process fair to all. As<br />
you can see, we have been listening!<br />
Now it is up to you to participate.<br />
The Certification Committee<br />
would also like to recruit new<br />
members. We want to keep listening<br />
to new ideas. Also anybody interested<br />
in signing up to be an Examiner or<br />
Mentor please contact me at<br />
mel712a@aol.com. Someone gave <strong>of</strong><br />
their time to help you, so please give<br />
<strong>of</strong> yourselves to help our beginning<br />
learners become the best they can be<br />
and to help our <strong>Academy</strong> grow.<br />
Thank you and hope to see you<br />
in Scottsdale!<br />
Mel Burchman, DDS nn
A Helping Hand<br />
Glenda Payas, DMD, Tulsa, Oklahoma<br />
I didn’t get to where I am without a<br />
lot <strong>of</strong> help from others. When I was<br />
young I had dreams, like most <strong>of</strong><br />
us, but our family lacked the<br />
resources that might have made<br />
those dreams easily come true. I<br />
also grew up in the era in which<br />
one rarely received an encouraging<br />
word for a job well done.<br />
Those factors put me on a path.<br />
They could have put me on a path<br />
where I felt defeated before I<br />
started, but instead they put me on<br />
a path to excel and succeed.<br />
I worked hard, set goals, and<br />
had a vision for where I wanted to<br />
be someday. There were challenges<br />
and disappointments along the way<br />
but as I look back – there was<br />
always someone there that reached<br />
out to assure me that I would get<br />
to my destination.<br />
I still fondly remember those<br />
people. There is no way they could<br />
have known that the tiny seeds<br />
that they were planting; a word, a<br />
smile, a monetary gift, would have<br />
produced such a generous harvest.<br />
These people so impacted my life<br />
that I decided I would, some day,<br />
find others for whom I could do the<br />
same.<br />
As members <strong>of</strong> the ALD, we<br />
have a great opportunity to sow<br />
seeds within students that need<br />
our reinforcement. We can reach<br />
The future <strong>of</strong> lasers in dentistry will be built upon the<br />
commitments we make today. The <strong>Academy</strong> <strong>of</strong> <strong>Laser</strong><br />
<strong>Dentistry</strong>’s goal is to establish a $100,000 endowment<br />
fund. The interest from this fund will be used to support<br />
the study <strong>of</strong> lasers by students and other eligible future<br />
programs, while the principle will remain intact.<br />
For more information visit<br />
www.laserdentistry.org/pr<strong>of</strong>/studentscholarship.cfm<br />
or Email E-mail: laserexec@laserdentistry.org<br />
S T U D E N T S C H O L A R S H I P S<br />
Glenda Payas, DMD,<br />
Awards Committee Chair<br />
out to help them achieve their<br />
goals. Through their education and<br />
practice skills they will in turn<br />
impact those lives that they touch<br />
to have great dental health.<br />
Please join us as we give to the<br />
Eugene Seidner Scholarship Fund.<br />
Glenda Payas, DMD, MAGD nn<br />
Sponsored by Henry Schein Dental<br />
J O U R N A L O F L A S E R D E N T I S T R Y | 2 011 V O L . 19 , N O . 3<br />
267
SSee<br />
ee<br />
MMore<br />
o r re<br />
with<br />
the t h he<br />
BIOLASE BIOL<br />
A ASE<br />
DaVinci Da<br />
Vi Vin<br />
n ci<br />
i IImaging<br />
Imagi<br />
i ing<br />
DD3D<br />
3D<br />
<br />
The TThh<br />
e Total TTo<br />
otal<br />
TTe<br />
TTechnology<br />
echnolo<br />
nolo gy<br />
SSolution<br />
olu olution<br />
ion<br />
© 20 2011 11<br />
BBIOLASE<br />
IOLAS<br />
S E |<br />
wwww.Biolase.com<br />
ww.Biolase.<br />
com<br />
| TToll-free<br />
To oll-frr<br />
ee<br />
8888-424-6527<br />
88-424-652<br />
27<br />
�<br />
�<br />
�<br />
�<br />
�<br />
�<br />
�<br />
�<br />
�<br />
�<br />
�<br />
A DVA<br />
ANCEED<br />
D IMAA<br />
GING<br />
TE ECC<br />
HNOLOGY:<br />
Y:<br />
D3 D DCBCT CT<br />
ultip<br />
le<br />
field<br />
<strong>of</strong><br />
f v<br />
iew<br />
systems<br />
X X-r<br />
r a<br />
y l<br />
o<br />
w<br />
e<br />
r r<br />
a<br />
d i a t i o n d o s a g e<br />
age-blurrin<br />
g p patien<br />
t moveme<br />
nt<br />
by<br />
50%<br />
,<br />
s and<br />
exposu<br />
re<br />
– no<br />
restrai<br />
nt<br />
s o or<br />
“ closed<br />
-in”<br />
feeli<br />
ng<br />
t,<br />
ortho,<br />
ora<br />
l s surger<br />
y,<br />
3rd<br />
molar<br />
extractions,<br />
n one<br />
syste<br />
m<br />
or<br />
high<br />
defini<br />
t tion<br />
with<br />
low<br />
emissi<br />
ons<br />
m a g e s<br />
rienta<br />
tion<br />
<strong>of</strong><br />
f c<br />
ross<br />
sectio<br />
ns<br />
ar nerve<br />
n Hounsfield<br />
u<br />
nits<br />
nal<br />
panoram<br />
ic<br />
project<br />
ions
DDo<br />
o M MMore<br />
ore<br />
wwith<br />
i ith<br />
Wa WWaterLase<br />
at<br />
e erLase<br />
iPlus iPl<br />
l us<br />
AAll<br />
l l TTi<br />
Tissue Tiis<br />
s su sue<br />
<strong>Laser</strong> <strong>Laser</strong>r<br />
SSy<br />
SSystem<br />
ystem<br />
INTUITIVE VEE & INTELLIGENT<br />
GRAPHICAL GRAPHICA<br />
RAPHICAL US USER INTERFACE<br />
Fo For<br />
eex<br />
xa amp<br />
p le,<br />
, p perfo<br />
ormm<br />
in ng g a<br />
Cl Claa ss<br />
I Ca Caviity ty Pr Pre<br />
ep p<br />
th h e iiP<br />
iiP iPl PPl<br />
P l us s iis<br />
iis<br />
s a<br />
a s ea e a as<br />
s y a<br />
s 11,<br />
1,<br />
2,<br />
3 3.<br />
.<br />
Step Stee p 1 Select<br />
“ Re<br />
e storati<br />
ve”<br />
from<br />
the<br />
first<br />
screen<br />
Step Stee<br />
p 2 Choose<br />
“ C<br />
lass<br />
I”<br />
from<br />
the<br />
next<br />
screen<br />
that<br />
appears<br />
s a<br />
utomat<br />
icall<br />
y<br />
Step Stee<br />
p 3 Specif<br />
y ot<br />
t her<br />
option<br />
s such<br />
as<br />
patien<br />
t<br />
sensitivit<br />
y<br />
or bond<br />
strength<br />
Th That’ s it!<br />
! SSt<br />
Steep<br />
p o on<br />
tth<br />
he<br />
fo foot<br />
peda<br />
al,<br />
, a<br />
nd<br />
staa<br />
rt<br />
work<br />
kkii<br />
ng g wwi<br />
wit<br />
th h n<br />
o shot,<br />
, n no<br />
ddr<br />
riilll<br />
l!<br />
BREAKS THE<br />
SP<br />
PEED BARRIER<br />
� � Reduce<br />
chair<br />
r t<br />
ime<br />
by<br />
avoidi<br />
ng<br />
needle<br />
and<br />
drill<br />
�� Patent<br />
ed<br />
lase<br />
e r techno<br />
logy<br />
deliv<br />
ers<br />
10<br />
watts<br />
<strong>of</strong><br />
p o ower<br />
�� Up<br />
to<br />
100<br />
pulses<br />
/ sec.<br />
for<br />
superi<br />
or<br />
s<strong>of</strong>t-t<br />
issue<br />
cut<br />
t ting<br />
�� Enables<br />
multi-<br />
quadra<br />
nt<br />
same-da<br />
y procedu<br />
res<br />
ENA E BBL<br />
BLES PAINLESS<br />
BIOLOGICAL<br />
DENTISTRY D<br />
� � Painl<br />
ess<br />
– no<br />
o s<br />
hot<br />
necessary<br />
in<br />
most<br />
cases<br />
�� No<br />
micro-<br />
frac<br />
c tures<br />
or<br />
thermal<br />
damage<br />
�� Reduce<br />
s the<br />
e r<br />
isk<br />
<strong>of</strong><br />
cross<br />
contam<br />
inatio<br />
n compar<br />
e ed<br />
to<br />
d<br />
�� More<br />
precise<br />
e , minimally<br />
invasive<br />
Call Ca all<br />
8<br />
888-424-6527 88-<br />
- 424-6522<br />
7 now<br />
for<br />
r de<br />
details, tails,<br />
oor<br />
r fifind<br />
nd<br />
yyour<br />
o our<br />
BIOLASE<br />
Territory TTe<br />
er<br />
r ritory<br />
y Manager M<br />
anager<br />
at<br />
BBIOLASE.com<br />
IOLA<br />
A SE.<br />
com<br />
uunder<br />
nder<br />
“<br />
“ “Contact”. Con ontact”<br />
.<br />
R<br />
2011<br />
� � Adds<br />
dual<br />
wavelength<br />
versatil<br />
ity<br />
and<br />
conven<br />
en ience<br />
� � First<br />
totally<br />
y wireles<br />
s dental<br />
laser<br />
� � 5 Watts<br />
p e eak<br />
power<br />
with<br />
<br />
ComfortPu<br />
u lse<br />
� � Battery<br />
op<br />
p erated<br />
with<br />
finger<br />
switch<br />
act<br />
t ivation<br />
� � Exclus<br />
iv<br />
e b bendable<br />
tips<br />
in<br />
many<br />
diameter<br />
s & lengths<br />
� �� S<br />
i<br />
ngl<br />
l e us<br />
e f<br />
o r N O c cross<br />
contamina<br />
na tion<br />
�<br />
�<br />
�<br />
TOP 50<br />
R<br />
Technology<br />
Pr Products oducts<br />
iL i<br />
940nm ASE ASE<br />
DIODE<br />
LASER<br />
DOCKING OCKING STA ATION<br />
PR PROVIDES<br />
GGR<br />
GREAT<br />
RE RET<br />
ETURN ON<br />
INVE INVESTMENT<br />
Increases<br />
tr<br />
r eatment<br />
acceptance<br />
<strong>of</strong><br />
day-to-day<br />
restorat<br />
ive<br />
cases<br />
Attracts<br />
new<br />
w p<br />
atient<br />
s<br />
Increa<br />
ses<br />
produc<br />
tivit<br />
y and<br />
enables<br />
new<br />
procedur<br />
dur es
J O U R N A L O F L A S E R D E N T I S T R Y | 2 011 V O L . 19 , N O . 3<br />
270<br />
C A S E R E P O R T<br />
Treatment <strong>of</strong> Periimplant Infection in the Posterior<br />
Maxilla, with 810-nm Diode <strong>Laser</strong> Decontamination<br />
<strong>of</strong> the Implant Surfaces: A Case Report<br />
Ahmad Kutkut, DDS, MS, 1 Sebastiano Andreana, DDS, MS, 2 Mohanad Al-Sabbagh, DDS, MS 3<br />
1University <strong>of</strong> Kentucky, College <strong>of</strong> <strong>Dentistry</strong>, Division <strong>of</strong> Restorative <strong>Dentistry</strong>, Lexington,<br />
Kentucky, USA; 2State University <strong>of</strong> New York at Buffalo, School <strong>of</strong> Dental Medicine, Department<br />
<strong>of</strong> Restorative <strong>Dentistry</strong>, Buffalo, NY, USA; 3University <strong>of</strong> Kentucky, College <strong>of</strong> <strong>Dentistry</strong>, Division<br />
<strong>of</strong> Periodontology, Lexington, Kentucky, USA<br />
J <strong>Laser</strong> Dent 2011;19(3):270-275<br />
Ahmad Kutkut, DDS, MS<br />
Sebastiano Andreana, DDS, MS<br />
Mohanad Al-Sabbagh, DDS, MS<br />
I N T R O D U C T I O N<br />
The predictability <strong>of</strong> dental<br />
implants has led to widespread<br />
acceptance <strong>of</strong> this treatment<br />
modality as an option for replacement<br />
<strong>of</strong> missing teeth. Success rates<br />
for dental implants are reported to<br />
be 90% or higher. 1-2 However, complications<br />
that may require immediate<br />
Kutkut, Andreana, and Al-Sabbagh<br />
A B S T R A C T<br />
Dental implant therapy is considered a safe and predictable method <strong>of</strong><br />
replacing extracted or missing teeth. However, a number <strong>of</strong> complications may<br />
occur in association with implant dentistry, one <strong>of</strong> which is periimplantitis.<br />
Periimplantitis is defined as an inflammatory process affecting the tissue around<br />
a dental implant; the condition is characterized by s<strong>of</strong>t tissue inflammation and<br />
loss <strong>of</strong> the bone supporting the implant.<br />
The ultimate goal in treating periimplantitis is gaining reosseointegration <strong>of</strong><br />
the infected implant surfaces. Several methods have been used in an attempt<br />
to achieve this goal, including conservative and regenerative treatment in<br />
conjunction with several techniques for decontaminating (i.e., disinfecting) the<br />
infected surfaces. One <strong>of</strong> the most recently reported techniques for achieving<br />
dental implant decontamination and gaining reosseointegration in both animals<br />
and humans is the use <strong>of</strong> a s<strong>of</strong>t tissue surgical laser. The findings <strong>of</strong> several<br />
studies suggest that the s<strong>of</strong>t tissue surgical laser is an effective therapeutic<br />
modality in the treatment <strong>of</strong> periimplantitis.<br />
The aim <strong>of</strong> this paper is to report a case involving implant complications that<br />
were treated with various methods aimed at enhancing the process <strong>of</strong><br />
reosseointegration.<br />
K E Y W O R D S<br />
Dental implant, periimplantitis, bone regeneration, osseointegration, laser<br />
decontamination<br />
intervention do occur. For the clinician,<br />
the consequences <strong>of</strong> implant<br />
retreatment may compromise the<br />
ability to accomplish satisfactory<br />
function and esthetics. For the<br />
patient, this retreatment usually<br />
involves further cost and additional<br />
surgical procedures.<br />
Implant complications may be<br />
caused by several factors, including<br />
early complications, overheating <strong>of</strong><br />
the bone, contamination and trauma<br />
during surgery, poor bone quantity<br />
or quality, lack <strong>of</strong> primary stability,<br />
preexisting infection, and incorrect<br />
immediate loading <strong>of</strong> the implant.<br />
Other complications may appear<br />
later, such as periimplantitis,<br />
occlusal trauma, and overloading.<br />
All <strong>of</strong> these conditions may compromise<br />
the final treatment outcome. 3<br />
Periimplantitis is defined as an<br />
inflammatory process affecting the<br />
supporting tissues around an<br />
osseointegrated implant and<br />
resulting in loss <strong>of</strong> adjacent bone.<br />
Periimplant mucositis is defined as<br />
reversible inflammatory changes <strong>of</strong>
the periimplant s<strong>of</strong>t tissues without<br />
any marginal bone loss. 4 The rate <strong>of</strong><br />
occurrence <strong>of</strong> periimplant mucositis<br />
ranges from 8% to 44%, and the<br />
rate <strong>of</strong> occurrence <strong>of</strong> periimplantitis<br />
ranges from 1% to 19%. 4<br />
However, because <strong>of</strong> the loss <strong>of</strong><br />
osseointegration and the exposure <strong>of</strong><br />
the roughened implant surface structure,<br />
decontaminating the defected<br />
surface with conventional nonsurgical<br />
treatment options is clinically<br />
difficult. 5 Recent clinical studies <strong>of</strong><br />
the use <strong>of</strong> a s<strong>of</strong>t tissue surgical laser<br />
to decontaminate (i.e., disinfect)<br />
rough implant surfaces, combined<br />
with surgical bone augmentation<br />
maintained by resorbable collagen<br />
membrane, have achieved good<br />
results with long-term success <strong>of</strong> the<br />
treated implants. 6<br />
The objective <strong>of</strong> this paper is to<br />
report a case <strong>of</strong> implant complications<br />
that were treated with<br />
various methods aimed at<br />
enhancing reosseointegration. The<br />
main outcome variables were<br />
reduction in probing depth and<br />
filling <strong>of</strong> the defect.<br />
C A S E R E P O R T<br />
A 55-year-old woman presented at<br />
the specialty dental clinics <strong>of</strong> the<br />
School <strong>of</strong> Dental Medicine at the<br />
State University <strong>of</strong> New York at<br />
Buffalo with a history <strong>of</strong> severe<br />
sinusitis in her left maxillary<br />
sinus. Because <strong>of</strong> the severity <strong>of</strong> the<br />
infection, teeth #11 through #15<br />
had been extracted at a private<br />
dental <strong>of</strong>fice. The patient had also<br />
been treated by an otolaryngologist<br />
(ENT). Nine months postoperatively,<br />
this patient presented at our<br />
clinic with an ill-fitting removable<br />
partial denture. The patient stated<br />
that she would like to have the<br />
missing teeth replaced with teeth<br />
that were fixed in the mouth. She<br />
was informed about possible<br />
complications associated with<br />
implants and about the methods <strong>of</strong><br />
treating those complications and<br />
consented to the most appropriate<br />
treatment option.<br />
The treatment plan was initi-<br />
ated with ENT consultation to<br />
verify the elimination <strong>of</strong> the infection<br />
related to the left maxillary<br />
sinus. The ENT report stated that<br />
no signs or symptoms <strong>of</strong> infection<br />
existed. Therefore, the dental treatment<br />
plan proceeded: 3 implants<br />
were placed at sites #11, 12, and<br />
14, and a sinus lift via the crestal<br />
approach was performed concurrently<br />
at site #14.<br />
S U R G I C A L T R E AT M E N T<br />
The patient began taking clindamycin<br />
150 mg (four times a day<br />
for 10 days) one day before the<br />
surgical procedure. On the day <strong>of</strong><br />
the procedure, the patient’s vital<br />
signs were recorded. After the<br />
administration <strong>of</strong> local anesthesia<br />
(injection <strong>of</strong> Xylocaine 2% injection<br />
with 1:100,000 epinephrine), a<br />
papilla-saving crestal incision was<br />
made and a full-thickness flap<br />
C A S E R E P O R T<br />
Figure 1: Hard and s<strong>of</strong>t tissue loss around implants at sites #11, 12, and 14<br />
Figure 1a: Preoperative panoramic view<br />
<strong>of</strong> the planned sites <strong>of</strong> future implant<br />
placements at sites #11, 12, and 14<br />
Figure 1b: Periapical radiograph <strong>of</strong> periimplantitis<br />
and sinus tract associated with<br />
implants at sites #11 and 12 during the<br />
healing period<br />
Figure 1c: Periimplantitis s<strong>of</strong>t tissue loss<br />
and exposure <strong>of</strong> cover screw <strong>of</strong> implant<br />
at site #14<br />
Figure 1d: Periimplantitis bone loss associated<br />
with implants at sites #11 and 12<br />
reflected. Osteotomies for the insertion<br />
<strong>of</strong> implants (4.3 x 13 mm,<br />
NobelReplace , Tapered Groovy,<br />
Nobel Biocare ® USA, Yorba Linda,<br />
Calif., USA) were prepared in an<br />
apicocoronal direction according to<br />
the implant recommendations <strong>of</strong><br />
the manufacturer. Three dental<br />
implants were placed in sites #11,<br />
12, and 14. Crestal-approach sinus<br />
elevation was performed at site #14<br />
before the implants were placed.<br />
The prepared site was grafted with<br />
allograft particulate bone substitutes<br />
(alloOss , ACE Surgical<br />
Supply, Brockton, Mass., USA)<br />
mixed with medical-grade calcium<br />
sulfate hemihydrate 7 (DentoGen ® ,<br />
OrthoGen, Springfield, N.J., USA).<br />
Cover screws were placed, and flaps<br />
were secured in a tension-free<br />
manner with 4-0 polytetrafluoro -<br />
ethylene (PTFE) sutures (ACE<br />
Surgical Supply). The patient was<br />
advised to clean the surgical area<br />
gently with a disposable oral swab<br />
(Toothette ® Oral Swab, Sage<br />
Products, Cary, Ill., USA) moistened<br />
with 0.12% chlorhexidine gluconate<br />
four times daily for two weeks.<br />
Kutkut, Andreana, and Al-Sabbagh<br />
J O U R N A L O F L A S E R D E N T I S T R Y | 2 011 V O L . 19 , N O . 3<br />
271
J O U R N A L O F L A S E R D E N T I S T R Y | 2 011 V O L . 19 , N O . 3<br />
272<br />
C A S E R E P O R T<br />
Fourteen days postoperatively,<br />
at the time <strong>of</strong> suture removal, the<br />
patient reported swelling and<br />
tenderness at the surgical site. The<br />
sutures were removed, and the site<br />
was irrigated with saline. The<br />
patient was advised to continue<br />
cleaning the surgical area as<br />
described above for 2 additional<br />
weeks and to continue taking clindamycin<br />
at the same dosage for<br />
another 10 days.<br />
At the 1-month follow-up evaluation,<br />
the patient reported the<br />
presence <strong>of</strong> a fistula related to the<br />
implants at sites #11 and 12.<br />
Severe bone loss was detected<br />
around the implants at sites #11,<br />
12, and 14; the pocket depths<br />
varied from 6 to 8 mm (Figure 1).<br />
Tooth #10 was vital, as confirmed<br />
by a positive response to the electrical<br />
pulp test. This recurrent<br />
infection may have been associated<br />
with the previously existing infection<br />
in the left sinus area or in the<br />
recently extracted infected teeth.<br />
Preoperative radiographs from the<br />
private dental <strong>of</strong>fice were not available<br />
before the implant procedure<br />
was performed. Retreatment at the<br />
surgical site was planned for 2<br />
months after placement <strong>of</strong> the<br />
implants.<br />
S U R G I C A L R E E N T RY<br />
T R E AT M E N T A N D<br />
L A S E R I M P L A N T<br />
D E C O N TA M I N AT I O N<br />
The patient began taking clindamycin<br />
(150 mg four times daily)<br />
one day before the surgery. The<br />
patient’s vital signs were recorded.<br />
After the administration <strong>of</strong> appropriate<br />
local anesthetics, a<br />
crestopalatal incision was made<br />
over the implant area at sites #11<br />
through 14, and a full-thickness<br />
flap was reflected at the buccal side<br />
to access the periimplant defect at<br />
the location <strong>of</strong> the bone loss. All<br />
granulation tissue in the defected<br />
area was removed with hand<br />
instruments. The threads were<br />
carefully cleaned <strong>of</strong> the infected<br />
tissue, and the exposed implant<br />
Kutkut, Andreana, and Al-Sabbagh<br />
Figure 2: Periimplantitis treatment<br />
Figure 2a: Diode laser set in continuous<br />
mode, 1.0 Watt in constant movement,<br />
with a noninitiated tip approximately 5<br />
mm away from the implant to decontaminate<br />
the surfaces<br />
Figure 2b: Tetracycline treatment paste<br />
(250 mg in 2 ml sterile water) applied to<br />
and left on the titanium surfaces for<br />
approximately 2 minutes<br />
surfaces were treated with an 810nm<br />
diode laser (Odyssey ® 2.4G<br />
Diode <strong>Laser</strong>, Ivoclar Vivadent,<br />
Amherst, N.Y., USA), set in continuous<br />
mode at 1.0 Watt, with a<br />
400-micron diameter fiber and a<br />
noninitiated tip used approximately<br />
5 mm away from the<br />
implant surfaces, with constant<br />
movement. The total duration <strong>of</strong><br />
laser decontamination was approximately<br />
4 minutes. Subsequently, a<br />
tetracycline paste (250 mg in 2 ml<br />
sterile water) was applied to the<br />
titanium surfaces and left in place<br />
for approximately 2 minutes; the<br />
surfaces were then rinsed pr<strong>of</strong>usely<br />
with sterile saline solution (Baxter<br />
Healthcare, Deerfield, Ill., USA).<br />
The defected surfaces were further<br />
irrigated with an aqueous solution<br />
Figure 2c: Bone graft. An allograft particulate<br />
bone substitute, mixed with<br />
medical-grade calcium sulfate hemihydrate,<br />
placed in the defected areas<br />
Figure 2d: Tension-free interrupted<br />
nonresorbable sutures placed<br />
<strong>of</strong> iodine and then irrigated with<br />
saline. Tooth #10 was extracted<br />
because <strong>of</strong> periodontal involvement<br />
with grade C mobility. An allograft<br />
<strong>of</strong> particulate bone substitute<br />
(alloOss) was mixed with medicalgrade<br />
calcium sulfate hemihydrate<br />
and placed in the defected areas.<br />
The grafted area was covered by a<br />
resorbable collagen membrane<br />
(conFORM ® , ACE Surgical Supply),<br />
which was trimmed to cover the<br />
defect completely. The flap was<br />
sutured with nonresorbable sutures<br />
(Cytoplast ® PTFE, Osteogenics<br />
Biomedical, Lubbock, Texas, USA).<br />
Submerged healing was allowed for<br />
2 months (Figure 2).<br />
Postoperatively, the patient was<br />
advised to clean the surgical site as<br />
described above twice daily for 2<br />
weeks. For the first 3 days, the<br />
patient took an antiinflammatory<br />
drug (ibupr<strong>of</strong>en, 600 mg every 6<br />
hours). The sutures were removed<br />
after 14 days. Clinically, fixture
exposure, membrane exposure, and<br />
the presence <strong>of</strong> mucosal craters<br />
were recorded. At 4 months, after<br />
radiographic assessment, local<br />
anesthesia was achieved by local<br />
infiltration <strong>of</strong> lidocaine. A minimal<br />
incision was made over the<br />
submerged fixture to expose the<br />
cover screws. The cover screws<br />
were removed, and the area was<br />
cleaned with chlorhexidine<br />
gluconate (1.2%) before the healing<br />
abutments were placed.<br />
C L I N I C A L O U TC O M E<br />
No adverse effects were reported<br />
after reentry treatment. Signs and<br />
symptoms <strong>of</strong> infection were eliminated,<br />
and the patient did not<br />
report any other adverse events.<br />
S<strong>of</strong>t and hard tissues regained<br />
their natural appearance, and<br />
primary stability was confirmed<br />
with a reverse torquing technique.<br />
The pocket depth was reduced to<br />
less than 3 mm around the treated<br />
implants, with a reduction <strong>of</strong> 5 mm<br />
in the pocket. Definitive restoration<br />
was initiated for a fixed partial<br />
denture supported with a milled<br />
bar substructure. After 1 year <strong>of</strong><br />
follow-up, no complications were<br />
reported in the function <strong>of</strong> these<br />
splinted implants (Figure 3).<br />
D I S C U S S I O N<br />
This case <strong>of</strong> periimplantitis was<br />
treated with surgical open-flap<br />
debridement and the placement <strong>of</strong><br />
a bone substitute in combination<br />
with a resorbable membrane and<br />
with a submerged healing situation<br />
during the first few months. The<br />
regenerative bone graft technique<br />
with the use <strong>of</strong> barrier membranes<br />
provided a successful treatment<br />
technique.<br />
After surgical exposure <strong>of</strong> the<br />
contaminated implant surface,<br />
mechanical, chemical, laser therapies<br />
or any combination <strong>of</strong> the three<br />
methodologies can be used to eliminate<br />
infection, resolve<br />
inflammation, and prepare the<br />
implant surface for bone regeneration<br />
and reosseointegration. Various<br />
Figure 3: Clinical and radiographic outcome postoperatively<br />
Figure 3a: Postoperative healing 4<br />
months after treatment<br />
Figure 3b: Postoperative radiograph<br />
before final impression and fabrication <strong>of</strong><br />
the definitive restoration<br />
methods have been advocated, such<br />
as air powder abrasion, saline wash,<br />
citric acid treatment, laser therapy,<br />
peroxide treatment, ultrasonic and<br />
manual debridement, and application<br />
<strong>of</strong> topical medication, but no<br />
definitive gold standard has been<br />
established. These methods must be<br />
used appropriately for cleaning<br />
implant surfaces, and caution must<br />
be exercised so that the implant<br />
surfaces and the surrounding tissue<br />
structures are not damaged. 8-13<br />
A dog study comparing the effectiveness<br />
<strong>of</strong> surgical debridement<br />
using an Er:YAG laser, an ultrasonic<br />
scaler, and plastic curettes plus local<br />
application <strong>of</strong> metronidazole gel<br />
with surgical debridement using<br />
laser and plastic curettes plus<br />
metronidazole gel found that ultrasonic<br />
cleaning results in larger gains<br />
in the clinical attachment level. 14<br />
However, histologic studies demonstrated<br />
that laser therapy resulted<br />
in the greatest degree <strong>of</strong> reosseointegration<br />
(44.8%) compared to<br />
ultrasonic treatment (8.7%) or<br />
debridement with a plastic curette<br />
plus metronidazole gel (14.8%). The<br />
laser produced better regenerative<br />
results than did mechanical cleaning<br />
<strong>of</strong> the implant surface. In addition,<br />
C A S E R E P O R T<br />
Figure 3c: Milled titanium bar substructure<br />
for splinting the implants and<br />
fabricating a fixed partial denture<br />
Figure 3d: Definitive fixed partial denture<br />
in function after 12 months<br />
no signs <strong>of</strong> thermal damage to the<br />
surrounding bone were found within<br />
the laser parameters. 14<br />
In this case report, the diode<br />
laser was used in a noncontact,<br />
noninitiated, continuous mode<br />
fashion. The safe use <strong>of</strong> the diode<br />
laser around implants has been<br />
previously reported. 15-16<br />
Investigation <strong>of</strong> the effect <strong>of</strong><br />
surface treatment, identified as the<br />
machined surface, indicated that<br />
this surface exhibited the lowest<br />
degree <strong>of</strong> reosseointegration but<br />
the greatest amount <strong>of</strong> bone filling<br />
in the defect. It has been speculated<br />
that the rougher surface may<br />
provide support for the developing<br />
coagulum after surgery and thus<br />
facilitate greater bone healing and<br />
maturation in contact with the<br />
implant surface. 11<br />
Collectively, the results <strong>of</strong> the<br />
studies discussed above indicate<br />
that all methods <strong>of</strong> surface debridement<br />
achieve resolution <strong>of</strong> the<br />
inflammatory lesion. However,<br />
Kutkut, Andreana, and Al-Sabbagh<br />
J O U R N A L O F L A S E R D E N T I S T R Y | 2 011 V O L . 19 , N O . 3<br />
273
J O U R N A L O F L A S E R D E N T I S T R Y | 2 011 V O L . 19 , N O . 3<br />
274<br />
C A S E R E P O R T<br />
metal curettes and ultrasonic tips<br />
have been shown to damage the<br />
surface <strong>of</strong> the titanium implant. 17<br />
The optimal results <strong>of</strong> both<br />
reosseointegration and bone fill<br />
tend to occur when a combination<br />
<strong>of</strong> guided bone regeneration (GBR)<br />
and graft material is used along<br />
with laser, chemical, and mechan-<br />
6, 18<br />
ical debridement.<br />
C O N C LU S I O N<br />
Resolution <strong>of</strong> periimplantitis can be<br />
achieved with various treatment<br />
methods <strong>of</strong> surface decontamination<br />
in combination with guided bone<br />
regeneration. However, evidence<br />
indicates that this open debridement,<br />
in combination with surface<br />
decontamination and the use <strong>of</strong> the<br />
s<strong>of</strong>t tissue surgical laser, achieves<br />
substantial reosseointegration with<br />
new bone regeneration <strong>of</strong> the defects.<br />
A U T H O R B I O G R A P H I E S<br />
Dr. Ahmad M. Kutkut is a prosthodontist<br />
and an assistant pr<strong>of</strong>essor<br />
at the University <strong>of</strong> Kentucky,<br />
College <strong>of</strong> <strong>Dentistry</strong>, Department <strong>of</strong><br />
Restorative <strong>Dentistry</strong>, Division <strong>of</strong><br />
Prosthodontics. Presently he is a<br />
reviewer for the Journal <strong>of</strong> Oral<br />
Implantology, the <strong>of</strong>ficial publication<br />
<strong>of</strong> the American <strong>Academy</strong> <strong>of</strong><br />
Implant <strong>Dentistry</strong> and the<br />
American <strong>Academy</strong> <strong>of</strong> Implant<br />
Prosthodontics, and a reviewer for<br />
Smile Dental Journal. Dr. Kutkut<br />
lectures both nationally and internationally<br />
and has published<br />
numerous articles and abstracts. In<br />
addition to his teaching, research,<br />
writing, and lecturing, he has<br />
presented several posters and table<br />
clinics at major dental meetings<br />
such as the <strong>Academy</strong> <strong>of</strong><br />
Osseointegration, Greater New<br />
York Dental Meeting, American<br />
College <strong>of</strong> Prosthodontics, American<br />
<strong>Academy</strong> <strong>of</strong> Fixed Prosthodontics,<br />
Northeast Implant Symposium,<br />
and the Jordanian Dental Implant<br />
Group. Dr. Kutkut may be<br />
contacted by e-mail at<br />
ahmad.kutkut@uky.edu.<br />
Dr. Sebastiano Andreana is<br />
Kutkut, Andreana, and Al-Sabbagh<br />
director <strong>of</strong> implant dentistry and<br />
associate pr<strong>of</strong>essor, Department <strong>of</strong><br />
Restorative <strong>Dentistry</strong> in the School<br />
<strong>of</strong> Dental Medicine at the University<br />
at Buffalo. Currently he is a faculty<br />
member at the Loma Linda<br />
University/American <strong>Academy</strong> <strong>of</strong><br />
Implant <strong>Dentistry</strong> (LLU/AAID)<br />
Loma Linda Maxi Course® and codirector<br />
<strong>of</strong> the University at Buffalo<br />
School <strong>of</strong> Dental Medicine (UBSDM)<br />
Implant Study Club. He has served<br />
as president <strong>of</strong> the American<br />
Association for Dental Research,<br />
Buffalo Chapter, and is a reviewer<br />
for the Journal <strong>of</strong> Periodontology,<br />
Journal <strong>of</strong> the American Dental<br />
Association, Clinical Oral Implant<br />
<strong>Dentistry</strong> and Related Research, and<br />
<strong>Laser</strong>s in Medicine and Surgery. At<br />
present he is senior associate editor<br />
<strong>of</strong> the Journal <strong>of</strong> Oral Implantology,<br />
and chair <strong>of</strong> the <strong>Academy</strong> <strong>of</strong> <strong>Laser</strong><br />
<strong>Dentistry</strong>’s (ALD’s) Science and<br />
Research Committee and the<br />
University and Academia Relations<br />
Committee. He is also a member <strong>of</strong><br />
the ALD Board <strong>of</strong> Directors. Dr.<br />
Andreana may be reached by e-mail<br />
at andrean@buffalo.edu.<br />
Dr. Mohanad Al-Sabbagh is<br />
currently the division chief <strong>of</strong> perio -<br />
dontology and the postdoctoral<br />
program director at the University<br />
<strong>of</strong> Kentucky College <strong>of</strong> <strong>Dentistry</strong>. He<br />
has achieved significant national<br />
and international recognition. He<br />
has received a number <strong>of</strong> prestigious<br />
awards and fellowships,<br />
including the Bud and Linda<br />
Tarrson Fellowship Award<br />
(American <strong>Academy</strong> <strong>of</strong><br />
Periodontology), the FDI/Unilever<br />
Research Award, the American<br />
<strong>Academy</strong> <strong>of</strong> Periodontology<br />
Educator Award (awarded for<br />
outstanding teaching and mentoring<br />
in periodontology), American<br />
<strong>Academy</strong> <strong>of</strong> Periodontology Teaching<br />
Fellowship Award (he was the first<br />
recipient <strong>of</strong> this honor). He has<br />
authored numerous peer-reviewed<br />
articles abstracts. Dr. Al-Sabbagh<br />
may be contacted by e-mail at<br />
malsa2@uky.edu.<br />
Disclosures: Dr. Ahmad-Kutkut and<br />
Dr. Mohanad Al-Sabbagh have no<br />
conflicting financial interests. Dr.<br />
Sebastiano Andreana is a consultant<br />
and trainer for Ivoclar Vivadent, manufacturer<br />
<strong>of</strong> the Odyssey diode laser.<br />
R E F E R E N C E S<br />
1. Chiapasco M, Zaniboni M. Clinical<br />
outcomes <strong>of</strong> GBR procedures to<br />
correct peri-implant dehiscences and<br />
fenestrations: A systematic review.<br />
Clin Oral Implants Res<br />
2009;20(Suppl 4):113-123.<br />
2. Huynh-Ba G, Friedberg JR, Vogiatzi<br />
D, Ioannidou E. Implant failure<br />
predictors in the posterior maxilla:<br />
A retrospective study <strong>of</strong> 273 consecutive<br />
implants. J Periodontol<br />
2008;79(12):2256-2261.<br />
3. Levin L. Dealing with dental<br />
implant failures. J Appl Oral Sci<br />
2008;16(3):171-175.<br />
4. Roos-Jansåker A-M, Renvert S,<br />
Egelberg J. Treatment <strong>of</strong> periimplant<br />
infections: A literature<br />
review. J Clin Periodontol<br />
2003;30(6):467-485.<br />
5. Roos-Jansåker A-M, Renvert H,<br />
Lindahl C, Renvert S. Submerged<br />
healing following surgical treatment<br />
<strong>of</strong> peri-implantitis: A case series. J<br />
Clin Periodontol 2007;34(8):723-727.<br />
6. Romanos GE, Nentwig GH.<br />
Regenerative therapy <strong>of</strong> deep periimplant<br />
infrabony defects after CO2 laser implant surface decontamination.<br />
Int J Periodontics Restorative<br />
Dent 2008;28(3):244-255.<br />
7. Kutkut A, Andreana S. Medicalgrade<br />
calcium sulfate hemihydrate<br />
in clinical implant dentistry: A<br />
review. J Long Term Eff Med<br />
Implants 2010;20(4):295-301.<br />
8. Roos-Jansåker A-M, Renvert H,<br />
Lindahl C, Renvert S. Surgical<br />
treatment <strong>of</strong> peri-implantitis using<br />
a bone substitute with or without a<br />
resorbable membrane: A prospective<br />
cohort study. J Clin Periodontol<br />
2007;34(7):625-632.<br />
9. Claffey N, Clarke E, Polyzois I,<br />
Renvert S. Surgical treatment <strong>of</strong><br />
peri-implantitis. J Clin Periodontol<br />
2008;35(Suppl 8):316-332.<br />
10. Persson GR, Samuelsson E, Lindahl<br />
C, Renvert S. Mechanical non-
surgical treatment <strong>of</strong> peri-implantitis:<br />
A single-blinded randomized<br />
longitudinal clinical study. II.<br />
Microbiological results. J Clin<br />
Periodontol 2010;37(6):563-573.<br />
11. Persson LG, Berglundh T, Sennerby<br />
L, Lindhe J. Re-osseointegration<br />
after treatment <strong>of</strong> peri-implantitis<br />
at different implant surfaces. An<br />
experimental study in the dog. Clin<br />
Oral Implants Res 2001;12(6):595-<br />
603.<br />
12. Renvert S, Polyzois I, Maguire R.<br />
Re-osseointegration on previously<br />
contaminated surfaces: A systematic<br />
review. Clin Oral Implants Res<br />
2009;20(Suppl 4):216-227.<br />
13. Bach G, Neckel C, Mall C, Krekeler<br />
G. Conventional versus laserassisted<br />
therapy <strong>of</strong> periimplantitis:<br />
A five-year comparative study.<br />
Implant Dent 2000;9(3):247-251.<br />
14. Schwarz F, Jepsen S, Herten M,<br />
Sager M, Rothamel D, Becker J.<br />
Influence <strong>of</strong> different treatment<br />
approaches on non-submerged and<br />
submerged healing <strong>of</strong> ligature<br />
induced peri-implantitis lesions: An<br />
experimental study in dogs. J Clin<br />
Periodontol 2006;33(8):584-595.<br />
15. Andreana S, Nihlawi O, Beneduce C.<br />
Temperature propagation on<br />
implant cover-screw after diode<br />
laser irradiation. J Dent Res<br />
2010;89:Abstract 2536.<br />
C A S E R E P O R T<br />
16. Yeh S, Jain K, Andreana S. Using a<br />
diode laser to uncover dental<br />
implants in second-stage surgery.<br />
Gen Dent 2005;53(6):414-417.<br />
17. Schou S, Berglundh T, Lang NP.<br />
Surgical treatment <strong>of</strong> peri-implantitis.<br />
Int J Oral Maxill<strong>of</strong>ac Implants<br />
2004;19(Suppl):140-149.<br />
18. Muller E, González YM, Andreana<br />
S. Treatment <strong>of</strong> peri-implantitis:<br />
Longitudinal clinical and microbiological<br />
findings – A case report.<br />
Implant Dent 1999;8(3):247-254. nn<br />
Kutkut, Andreana, and Al-Sabbagh<br />
J O U R N A L O F L A S E R D E N T I S T R Y | 2 011 V O L . 19 , N O . 3<br />
275
J O U R N A L O F L A S E R D E N T I S T R Y | 2 011 V O L . 19 , N O . 3<br />
276<br />
C A S E R E P O R T<br />
Peri-Implantitis Therapy with<br />
an Er:YAG <strong>Laser</strong><br />
Avi Reyhanian, DDS, Natanya, Israel<br />
Donald J. Coluzzi, DDS, Portola Valley, California<br />
J <strong>Laser</strong> Dent 2011;19(3):276-281<br />
S Y N O P S I S<br />
The etiology <strong>of</strong> peri-implantitis and a treatment protocol using an<br />
Er:YAG laser are described along with a clinical case study with a<br />
successful outcome.<br />
I N T R O D U C T I O N<br />
Osseointegrated dental implants<br />
have become a routinely recommended<br />
procedure in the clinical<br />
practice <strong>of</strong> dentistry. 1-4 Although<br />
they can be highly successful<br />
restorations, implant failure can<br />
and does still occur. 5-8 Among the<br />
many complications possible in the<br />
procedure, one <strong>of</strong> the more common<br />
postoperative ones is peri-implant<br />
disease and, within this category,<br />
peri-implantitis. 9<br />
Three major factors contribute<br />
to the failure and complications <strong>of</strong><br />
implants:<br />
1. Patient-related factors<br />
2. Iatrogenic (doctor/team) factors<br />
3. Surgical equipment / manufacturer<br />
problems.<br />
Patient and iatrogenic factors<br />
are more prevalent than implant<br />
manufacturing problems.<br />
Implant complications are<br />
divided into two main categories:<br />
Intraoperative and postoperative. 9<br />
Peri-implantitis is a postoperative<br />
complication.<br />
Bi<strong>of</strong>ilms form on all hard,<br />
nonshedding surfaces in a fluid<br />
system, i.e., both on teeth and on<br />
oral implants. As a result <strong>of</strong> the<br />
bacterial challenge, the host<br />
responds by mounting a defense<br />
mechanism leading to inflammation<br />
<strong>of</strong> the s<strong>of</strong>t tissue. In the<br />
implantomucosal unit this inflammation<br />
is termed “mucositis” which<br />
Reyhanian and Coluzzi<br />
may develop into “peri-implantitis.”<br />
9<br />
Peri-implantitis is an inflammatory<br />
reaction that is associated<br />
with the presence <strong>of</strong> a submarginal<br />
bi<strong>of</strong>ilm, with advanced breakdown<br />
<strong>of</strong> s<strong>of</strong>t and hard tissue surrounding<br />
the endosseous implant: loss <strong>of</strong> the<br />
bony support <strong>of</strong> the implant. 10<br />
The etiology <strong>of</strong> the disease is<br />
conditioned by the status <strong>of</strong> the<br />
tissue surrounding the implant,<br />
design <strong>of</strong> the implant, degree <strong>of</strong><br />
roughness, poor alignment <strong>of</strong> implant<br />
components, external morphology,<br />
and excessive mechanical load. 10<br />
There are two major factors that,<br />
separately or combined, contribute to<br />
the formation <strong>of</strong> peri-implantitis:<br />
1. Bacterial exposure, especially<br />
gram-negative and anaerobic<br />
species 11-12<br />
2. Overload. 13-14<br />
Clinical signs and diagnosis<br />
include: Bleeding on probing, purulence,<br />
bone loss, pocketing, dull<br />
sound on percussion, peri-implant<br />
radiolucent mobility <strong>of</strong> the implant,<br />
fistula, and changes <strong>of</strong> color in the<br />
gingiva and/or the mucosa. 10<br />
Treatment involves either<br />
implant removal, especially if the<br />
fixture is mobile, or therapy,<br />
usually involving surgery and<br />
debridement techniques.<br />
Conventional approaches include:<br />
• Systemic administration <strong>of</strong><br />
antibiotics<br />
A B S T R A C T<br />
Peri-implantitis is one <strong>of</strong> the<br />
complications possible in osseo -<br />
integrated dental implants.<br />
This article discusses the wisdom<br />
and utility <strong>of</strong> employing an Er:YAG<br />
laser for peri-implantitis therapy. A<br />
clinical case study will demonstrate<br />
how this procedure could replace<br />
the gold standard for peri-implantitis<br />
therapy. This technique using the<br />
Er:YAG laser presents several advantages<br />
vs. conventional treatment<br />
methods, and there are minimal<br />
postoperative complications coupled<br />
with a high rate <strong>of</strong> success.<br />
Key Words: antimicrobial agents;<br />
bone grafting; bone tissue;<br />
debridement; dental implants;<br />
granulation tissue; guided tissue<br />
regeneration; laser ablation<br />
• Removal <strong>of</strong> supragingival bacterial<br />
plaque<br />
• Removal <strong>of</strong> granulation tissue<br />
with plastic curettes<br />
• Debridement <strong>of</strong> the exposed<br />
surface by using mechanical<br />
brushing, air powder abrasives,<br />
citric acid, disinfectants like<br />
chlorhexidine or topical tetracycline,<br />
plaque inhibitor like<br />
delmopinol, or low-intensity<br />
ultraviolet radiation<br />
• Removal <strong>of</strong> the peri-implant pocket<br />
• Regeneration <strong>of</strong> peri-implant<br />
hard tissue by means <strong>of</strong> guided<br />
tissue regeneration<br />
• Plaque control and oral hygiene.<br />
The Use <strong>of</strong> the Er:YAG <strong>Laser</strong> in<br />
Treatment <strong>of</strong> Peri-Implantitis<br />
The Er:YAG laser interacts with<br />
both hard and s<strong>of</strong>t dental tissues,
and thus can be effectively utilized<br />
for both surgery and debridement<br />
<strong>of</strong> the infected implant area.<br />
• The laser can make crestal,<br />
intrasulcular, or vertical release<br />
incisions in raising a flap. The<br />
Er:YAG laser produces a wet<br />
incision (some bleeding) as<br />
opposed to the dry incision (no<br />
bleeding) produced by other s<strong>of</strong>t<br />
tissue lasers. 15<br />
• The laser easily vaporizes any<br />
existing granulation tissue, with<br />
a lower risk <strong>of</strong> overheating the<br />
bone than those posed by the<br />
current diode or CO2 lasers. 16-17<br />
The Er:YAG laser wavelength’s<br />
excellent ability to effectively<br />
ablate s<strong>of</strong>t tissue without<br />
producing major thermal sideeffects<br />
to adjacent tissue has<br />
been demonstrated in numerous<br />
studies. 18-20<br />
• The implant surface can be<br />
debrided by lasing directly on the<br />
implant’s exposed screws with a<br />
low-energy setting. Both the<br />
target tissue and implant surface<br />
are disinfected without damage. 21-25<br />
• Ablating the bone with the<br />
Er:YAG laser also ablates<br />
necrotic bone, as well as contours<br />
and reshapes the surrounding<br />
osseous tissue. 26-28<br />
• The laser is bactericidal. 29-30<br />
C A S E S T U DY<br />
This case describes treatment <strong>of</strong><br />
peri-implantitis with an Er:YAG<br />
laser.<br />
P R E T R E AT M E N T<br />
A. Outline <strong>of</strong> Case<br />
1. Clinical Examination<br />
A 51-year old male presented with<br />
no medical abnormalities. The<br />
patient presented by referral four<br />
months after having implants<br />
inserted in the location <strong>of</strong> the lower<br />
left and right lateral incisors.<br />
2. S<strong>of</strong>t- and Hard-Tissue<br />
Examination<br />
Periodontal probing showed generalized<br />
4 mm pockets with bleeding.<br />
The patient had very ineffective<br />
Figure 1: Patient condition upon presentation.<br />
Note the buccal fistula from the<br />
implant at tooth #25<br />
Figure 2: A periodontal probe inserted<br />
into the fistula<br />
oral hygiene, and does not brush or<br />
floss at all; consequently, all teeth<br />
were covered with plaque. Both <strong>of</strong><br />
the implants were nonsubmerged<br />
with abutments present. The lower<br />
right implant presented a labial<br />
fistula, the probing <strong>of</strong> which led to<br />
the apical end <strong>of</strong> the implant<br />
(Figures 1 and 2). The left implant<br />
presented without complications.<br />
The remaining s<strong>of</strong>t tissue was<br />
within normal limits.<br />
3. Radiographic Examination<br />
Panoramic and periapical X-rays<br />
showed a large radiolucency area<br />
surrounding about 70% <strong>of</strong> the right<br />
implant, implying massive bone<br />
loss (Figure 3).<br />
4. Mobility Tests<br />
The infected implant was stable<br />
with no mobility.<br />
B. Diagnosis and Treatment Plan<br />
1. Provisional and Final Diagnosis<br />
Advanced peri-implantitis with<br />
massive bone loss around the<br />
implant.<br />
C A S E R E P O R T<br />
Figure 3: X-ray image with gutta-percha<br />
inside the fistula, pointing into the defect<br />
Figure 4: The Er:YAG handpiece with the<br />
200-micron sapphire tip ready for the<br />
incision<br />
2. Treatment Plan<br />
An Er:YAG laser will be used for<br />
flap incision, ablation <strong>of</strong> granulation<br />
tissue around the implant,<br />
remodeling, shaping and decortication<br />
<strong>of</strong> the bone, debridement <strong>of</strong><br />
exposed implant screw and guided<br />
bone regeneration (GBR) technique<br />
for the bone loss.<br />
3. Treatments Alternatives<br />
Traditional scalpel, curettes, citric<br />
acid, air flow, air abrasion, and<br />
rotary tools.<br />
T R E AT M E N T<br />
A. <strong>Laser</strong> Operating Parameters<br />
An intrasulcular incision was made<br />
with an Er:YAG laser (OpusDuo<br />
AquaLite, Lumenis Ltd.,<br />
Yokneam, Israel) (2940 nm), using<br />
Reyhanian and Coluzzi<br />
J O U R N A L O F L A S E R D E N T I S T R Y | 2 011 V O L . 19 , N O . 3<br />
277
J O U R N A L O F L A S E R D E N T I S T R Y | 2 011 V O L . 19 , N O . 3<br />
278<br />
C A S E R E P O R T<br />
Figure 5: Intrasulcular and vertical<br />
releasing incisions completed<br />
Figure 6: After the flap is lifted, the defect<br />
is probed<br />
Figure 7: Granulation tissue exposed<br />
a 200-micron sapphire tip in<br />
contact mode with a water spray.<br />
The power setting for the incision<br />
was 450 mJ / 20 PPS (9 Watts)<br />
(Figure 4).<br />
B. Treatment Delivery<br />
Sequence<br />
The intrasulcular incision was<br />
performed from the distal side <strong>of</strong><br />
the right cuspid to the mesial side<br />
<strong>of</strong> the left implant. Then a vertical<br />
incision for release was performed<br />
at the mesial <strong>of</strong> the left implant<br />
and a buccal flap was lifted (Figure<br />
5). The defect was probed to determine<br />
the extent <strong>of</strong> the lesion<br />
(Figure 6). The infection had<br />
Reyhanian and Coluzzi<br />
Figure 8: The Er:YAG handpiece with a<br />
1300-micron sapphire tip for granulation<br />
tissue ablation<br />
Figure 9: <strong>Laser</strong> s<strong>of</strong>t tissue and osseous<br />
ablation completed<br />
Figure 10: Bio-Oss ® material placed for<br />
guided tissue regeneration<br />
engulfed the buccal side and<br />
lingual side toward the apex <strong>of</strong> the<br />
implant, with massive loss <strong>of</strong> bone<br />
and a great deal <strong>of</strong> granulation<br />
tissue, as shown in Figure 7.<br />
The granulation tissue was<br />
ablated with the laser in noncontact<br />
mode using a 1300-micron<br />
sapphire tip and a power setting <strong>of</strong><br />
700 mJ / 12 PPS (8.4 Watts) with a<br />
water spray (Figure 8). Since the<br />
buccal bone had not resorbed,<br />
direct observation was impossible,<br />
making it difficult to ablate the<br />
granulation tissue inside and<br />
around the implant. Therefore a<br />
Figure 11: Bio-Gide ® absorbent bilayer<br />
membrane placed<br />
Figure 12: Immediately postoperative,<br />
sutures in place. Note primary closure<br />
small window <strong>of</strong> the buccal bone<br />
was removed with the same laser<br />
parameters to gain direct access to<br />
the lesion. After removal <strong>of</strong> the<br />
infected s<strong>of</strong>t tissue (Figure 9), the<br />
laser beam was aimed at the<br />
surface <strong>of</strong> the exposed screws in a<br />
low-energy setting <strong>of</strong> 150 mJ / 20<br />
PPS (3 Watts), for debridement.<br />
The next step was to ablate<br />
necrotic bone, and to shape and<br />
recontour the defect. The site was<br />
filled with a xenograft bone substitute<br />
(Bio-Oss ® , (Geistlich Pharma<br />
AG Biomaterials Division,<br />
Wolhusen, Germany) (Figure 10)<br />
and then covered with an<br />
absorbent bilayer membrane (Bio-<br />
Gide ® , Geistlich Pharma AG<br />
Biomaterials Division) (Figure 11).<br />
The flap was sutured (silk 3-0),<br />
with particular attention paid to<br />
primary closure <strong>of</strong> the flap (Figure<br />
12). An immediate postoperative<br />
radiograph is shown in Figure 13.<br />
C. Postoperative Instructions<br />
The patient was prescribed clindamycin<br />
150 mg x 50 tabs to avoid<br />
infection. He was also given<br />
ibupr<strong>of</strong>en 800 mg x 15 tabs for
Figure 13: Immediate postoperative radiograph<br />
pain. He was instructed to rinse<br />
with chlorhexidine 0.2%, starting<br />
the next day, for 2 weeks 3 times a<br />
day and was advised to maintain<br />
good oral hygiene.<br />
F O L LO W- U P C A R E<br />
A. Assessment <strong>of</strong> Treatment<br />
Outcome<br />
The patient was called the next day,<br />
and he reported moderate pain and<br />
moderate swelling. He also said<br />
that there was no tissue bleeding<br />
and the site was closed. At 10 days<br />
postoperative, the patient returned<br />
for inspection and removal <strong>of</strong><br />
sutures (Figure 14). The patient<br />
returned four days later and the<br />
suture points had healed (Figure<br />
15). The swelling had resolved,<br />
there were no signs <strong>of</strong> fistula, and<br />
healing was progressing well. After<br />
six weeks the s<strong>of</strong>t tissue was<br />
completely healed without complications.<br />
The s<strong>of</strong>t issue was healing<br />
over the bone and there were no<br />
bony projections observed under the<br />
s<strong>of</strong>t tissue.<br />
B. Prognosis<br />
The prognosis is good. The twomonth<br />
postoperative views and<br />
radiograph show good healing<br />
(Figures 16-18). It will be essential<br />
Figure 14: Ten days postoperative, sutures<br />
just removed<br />
Figure 15: Two weeks postoperative,<br />
suture areas healed<br />
Figure 16: Two-month postoperative view<br />
<strong>of</strong> treated implant<br />
for the patient to maintain good oral<br />
hygiene. It is important to note that<br />
the lack <strong>of</strong> mobility <strong>of</strong> the infected<br />
implant is very important for guided<br />
tissue regeneration to be successful.<br />
Conclusion<br />
The Er:YAG laser can be employed<br />
for debridement <strong>of</strong> implant surfaces<br />
as well as regenerative osseous<br />
surgery, and has been proven to be<br />
effective and safe. The use <strong>of</strong> this<br />
laser wavelength for these procedures<br />
presents many advantages<br />
vs. conventional methods, such as<br />
reducing pathogens and patient<br />
discomfort. This laser has become<br />
an invaluable tool for many proce-<br />
C A S E R E P O R T<br />
Figure 17: Two-month postoperative view<br />
<strong>of</strong> surgical area<br />
Figure 18: Two-month postoperative radiograph<br />
dures by simplifying treatment and<br />
<strong>of</strong>fering patients faster, less<br />
stressful oral therapy with<br />
enhanced outcomes.<br />
A U T H O R B I O G R A P H I E S<br />
Dr. Avi Reyhanian graduated from<br />
the University <strong>of</strong> Bucharest,<br />
Romania in 1988. He then participated<br />
in a fellowship program at<br />
the Oral & Maxill<strong>of</strong>acial<br />
Department, Rambam Hospital in<br />
Israel. He is a member <strong>of</strong> the<br />
academic staff at the Institute <strong>of</strong><br />
Advanced Dental Education in<br />
Haifa, Israel and he currently practices<br />
general dentistry and oral<br />
surgery in Natanya, Israel. Dr.<br />
Reyhanian’s practice has employed<br />
dental lasers since early 2002; he<br />
currently uses Er:YAG (2940 nm),<br />
CO2 (10,600 nm), and diode (830<br />
Reyhanian and Coluzzi<br />
J O U R N A L O F L A S E R D E N T I S T R Y | 2 011 V O L . 19 , N O . 3<br />
279
J O U R N A L O F L A S E R D E N T I S T R Y | 2 011 V O L . 19 , N O . 3<br />
280<br />
C A S E R E P O R T<br />
nm) lasers in his practice. He is a<br />
member <strong>of</strong> the <strong>Academy</strong> <strong>of</strong> <strong>Laser</strong><br />
<strong>Dentistry</strong> and the Israel Society <strong>of</strong><br />
Dental Implantology. Dr.<br />
Reyhanian presents lectures in<br />
Israel, Europe, USA, and Asia on<br />
the topic <strong>of</strong> dental lasers, and has<br />
published several articles. Dr.<br />
Reyhanian may be contacted by email<br />
at avi5000rey@gmail.com.<br />
Disclosure: Dr. Reyhanian is a<br />
member <strong>of</strong> the academic staff at the<br />
Institute <strong>of</strong> Advanced Dental<br />
Education in Haifa, Israel, and is a<br />
consultant to the Lumenis Company.<br />
Dr. Donald Coluzzi, a 1970 graduate<br />
<strong>of</strong> the University <strong>of</strong> Southern<br />
California School <strong>of</strong> <strong>Dentistry</strong>, is an<br />
associate clinical pr<strong>of</strong>essor in the<br />
Department <strong>of</strong> Preventive and<br />
Restorative Dental Sciences at the<br />
University <strong>of</strong> California San<br />
Francisco School <strong>of</strong> <strong>Dentistry</strong>. A<br />
charter member and past President<br />
<strong>of</strong> the <strong>Academy</strong> <strong>of</strong> <strong>Laser</strong> <strong>Dentistry</strong>,<br />
he has used dental lasers since<br />
early 1991. He has Advanced<br />
Pr<strong>of</strong>iciency in Nd:YAG and Er:YAG<br />
laser wavelengths. He is the 1999<br />
recipient <strong>of</strong> the Leon Goldman<br />
Award for Clinical Excellence and<br />
the 2006 Distinguished Service<br />
Award from the <strong>Academy</strong> <strong>of</strong> <strong>Laser</strong><br />
<strong>Dentistry</strong>, and is a Fellow <strong>of</strong> the<br />
American College <strong>of</strong> Dentists. Dr.<br />
Coluzzi has presented about lasers<br />
worldwide, co-authored two books,<br />
and published several peerreviewed<br />
articles.<br />
Disclosure: Dr. Coluzzi is an occasional<br />
presenter and trainer for Hoya<br />
ConBio, and receives an honorarium<br />
for that service.<br />
R E F E R E N C E S<br />
1. Adell R, Lekholm U, Rockler B,<br />
Brånemark P-I. A 15-year study <strong>of</strong><br />
osseointegrated implants in the<br />
treatment <strong>of</strong> the edentulous jaw. Int<br />
J Oral Surg 1981;10(6):387-416.<br />
2. Albrektsson T. A multicenter report<br />
on osseointegrated oral implants. J<br />
Prosthet Dent 1988;60(1):75-84.<br />
Reyhanian and Coluzzi<br />
3. Buser D, Mericske-Stern R, Dula K,<br />
Lang NP. Clinical experience with<br />
one-stage, non-submerged dental<br />
implants. Adv Dent Res1999;13:153-<br />
161.<br />
4. Olsson M, Friberg B, Nilson H,<br />
Kultje C. MkII – A modified selftapping<br />
Brånemark implant: 3-year<br />
results <strong>of</strong> a controlled prospective<br />
pilot study. Int J Oral Maxill<strong>of</strong>ac<br />
Implants 1995;10(1):15-21; Erratum<br />
in: Int J Oral Maxill<strong>of</strong>ac Implants<br />
1995;10(2):243.<br />
5. Jaffin RA, Berman CL. The excessive<br />
loss <strong>of</strong> Branemark fixtures in<br />
type IV bone: A 5-year analysis. J<br />
Periodontol 1991;62(1):2-4.<br />
6. Esposito M, Hirsch J, Lekholm U,<br />
Thomsen P. Differential diagnosis<br />
and treatment strategies for biologic<br />
complications and failing oral<br />
implants: A review <strong>of</strong> the literature.<br />
Int J Oral Maxill<strong>of</strong>ac Implants<br />
1999;14(4):473-490<br />
7. Brisman DL, Brisman AS, Moses<br />
MS. Implant failures associated<br />
with asymptomatic endodontically<br />
treated teeth. J Am Dent Assoc<br />
2001;132(2):191-195.<br />
8. Ayangco L, Sheridan PJ.<br />
Development and treatment <strong>of</strong><br />
retrograde peri-implantitis<br />
involving a site with a history <strong>of</strong><br />
failed endodontic and apicoectomy<br />
procedures: A series <strong>of</strong> reports. Int J<br />
Oral Maxill<strong>of</strong>ac Implants<br />
2001;16(3):412-417.<br />
9. Reyhanian A, Coluzzi DJ. Er:YAG<br />
laser-assisted implant periapical<br />
lesion therapy (IPL) and guided<br />
bone regeneration (GBR) technique:<br />
New challenges and new instrumentation.<br />
J <strong>Laser</strong> Dent<br />
2007;15(3):135-141.<br />
10. Sánchez-Gárces MA, Gay-Escoda C.<br />
Periimplantitis. Med Oral Patol Oral<br />
Cir Bucal 2004;9 Suppl:69-74; 63-69.<br />
11. Albrektsson TO, Johansson CB,<br />
Sennerby L. Biological aspects <strong>of</strong><br />
implant dentistry: Osseointegration.<br />
Periodontol 2000 1994;4:58-73.<br />
12. Meffert RM. Periodontitis and periimplantitis:<br />
One and the same?<br />
Pract Periodontics Aesthet Dent<br />
1993;5(9):79-80, 82.<br />
13. Uribe R, Peñarrocha M, Sanchis JM,<br />
García O. Marginal peri-implantitis<br />
due to occlusal overload. A case<br />
report. Med Oral 2004;9(2):160-162,<br />
159-160.<br />
14. Isidor F. Loss <strong>of</strong> osseointegration<br />
caused by occlusal load <strong>of</strong> oral<br />
implants. A clinical and radiographic<br />
study in monkeys. Clin<br />
Oral Implants Res 1996;7(2):143-<br />
152.<br />
15. Watanabe H, Ishikawa I, Suzuki M,<br />
Hasegawa K. Clinical assessments<br />
<strong>of</strong> the erbium:YAG laser for s<strong>of</strong>t<br />
tissue surgery and scaling. J Clin<br />
<strong>Laser</strong> Med Surg 1996;14(2):67-75.<br />
16. Kreisler M, Al Haj H, d’Hoedt B.<br />
Temperature changes at the<br />
implant-bone interface during simulated<br />
surface decontamination with<br />
an Er:YAG laser. Int J Prosthodont<br />
2002;15(6):582-587.<br />
17. Sasaki KM, Aoki A, Ichinose S,<br />
Yoshino T, Yamada S, Ishikawa I.<br />
Scanning electron microscopy and<br />
Fourier transformed infrared spectroscopy<br />
analysis <strong>of</strong> bone removal<br />
using Er:YAG and CO2 lasers. J<br />
Periodontol 2002;73(6):643-652.<br />
18. Ishikawa I, Aoki A, Takasaki AA.<br />
Potential applications <strong>of</strong><br />
erbium:YAG laser in periodontics. J<br />
Periodontal Res 2004;39(4):275-285.<br />
19. Ishikawa I, Sasaki KM, Aoki A,<br />
Watanabe H. Effects <strong>of</strong> Er:YAG<br />
laser on periodontal therapy. J Int<br />
Acad Periodontol 2003;5(1):23-28.<br />
20. Schwarz F, Bieling K, Sculean A,<br />
Herten M, Becker J. <strong>Laser</strong> und<br />
ultraschall in der therapie periimplantärer<br />
infektionen – Eine<br />
literaturübersicht. [Treatment <strong>of</strong><br />
periimplantitis with laser or ultrasound.<br />
A review <strong>of</strong> the literature.]<br />
Schweiz Monatsschr Zahnmed<br />
2004;114(12):1228-1235. German.<br />
21. Schwarz F, Rothamel D, Becker J.<br />
Einfluss eines Er:YAG-lasers auf die<br />
oberflächen-struktur von Titanimplantaten.<br />
[Influence <strong>of</strong> an<br />
Er:YAG laser on the surface structure<br />
<strong>of</strong> titanium implants.] Schweiz<br />
Monatsschr Zahnmed<br />
2003;113(6):660-671. French,<br />
German.<br />
22. Jovanovic SA. The management <strong>of</strong><br />
peri-implant breakdown around<br />
functioning osseointegrated dental<br />
implants. J Periodontol 1993;64(11<br />
Suppl):1176-1183.
23. Matsuyama T, Aoki A, Oda S,<br />
Yoneyama T, Ishikawa I. Effect <strong>of</strong><br />
the Er:YAG laser irradiation on titanium<br />
implant materials and<br />
contaminated implant abutment<br />
surfaces. J Clin <strong>Laser</strong> Med Surg<br />
2003;21(1):7-17.<br />
24. Schwarz F, Rothamel D, Sculean A,<br />
Georg T, Scherbaum W, Becker J.<br />
Effects <strong>of</strong> an Er:YAG laser and the<br />
Vector ultrasonic system on the<br />
biocompatibility <strong>of</strong> titanium<br />
implants in cultures <strong>of</strong> human<br />
osteoblast-like cells. Clin Oral<br />
Implants Res 2003;14(6):784-792.<br />
25. Kreisler M, Kohnen W, Christ<strong>of</strong>fers<br />
AB, Götz H, Jansen B, Duschner H,<br />
d’Hoedt B. In vitro evaluation <strong>of</strong> the<br />
biocompatibility <strong>of</strong> contaminated<br />
implant surfaces treated with an<br />
Er:YAG laser and an air powder<br />
system. Clin Oral Implants Res<br />
2005;16(1):36-43.<br />
26. Nelson JS, Orenstein A, Liaw LH,<br />
Berns MW. Mid-infrared<br />
erbium:YAG laser ablation <strong>of</strong> bone:<br />
The effect <strong>of</strong> laser osteotomy on<br />
bone healing. <strong>Laser</strong>s Surg Med<br />
1989;9(4):362-374.<br />
27. “Use Of the Dental Erbium <strong>Laser</strong><br />
(2940nm) For Contouring And<br />
Resection Of Osseous Tissue (Bone)<br />
And The Preparation Of Endodontic<br />
Canals,” Copyright 2000 to 2002<br />
Institute for <strong>Laser</strong> <strong>Dentistry</strong>,<br />
www.laserdentistry.ca/erbium.html,<br />
accessed May 24, 2008.<br />
28. Rupprecht S, Tangermann K,<br />
Kessler P, Neukam FW, Wiltfang J.<br />
C A S E R E P O R T<br />
Er:YAG laser osteotomy directed by<br />
sensor controlled systems. J<br />
Craniomaxill<strong>of</strong>ac Surg<br />
2003;31(6):337-342.<br />
29. Folwaczny M, Mehl A, Aggstaller H,<br />
Hickel R. Antimicrobial effects <strong>of</strong><br />
2.94 µm Er:YAG laser radiation on<br />
root surfaces: An in vitro study. J<br />
Clin Periodontol 2002;29(1):73-78.<br />
30. Kreisler M, Kohnen W, Marinello C,<br />
Götz H, Duschner H, Jansen B,<br />
d’Hoedt B. Bactericidal effect <strong>of</strong> the<br />
Er:YAG laser on dental implant<br />
surfaces: An in vitro study. J<br />
Periodontol 2002;73(11):1292-1298. nn<br />
Editor’s Note: This article first<br />
appeared in J <strong>Laser</strong> Dent<br />
2008;16(2):69-74. nn<br />
Reyhanian and Coluzzi<br />
J O U R N A L O F L A S E R D E N T I S T R Y | 2 011 V O L . 19 , N O . 3<br />
281
Unmatched Un<br />
n match<br />
e ed<br />
Ve Versatility Vers<br />
s a ati<br />
ility<br />
to<br />
o MMeet<br />
Meet<br />
Your Yo ou<br />
r DDiode<br />
Diode<br />
<strong>Laser</strong> Las<br />
s er<br />
NNeeds<br />
eeddss<br />
HE E FFIR<br />
FIRS<br />
ST<br />
TO O OTA<br />
ALLL<br />
Y<br />
WIR IRE ELL<br />
ESSS<br />
S D DDE<br />
DENNT<br />
TA AL<br />
LLA<br />
ASEERR<br />
�<br />
�<br />
�<br />
�<br />
The<br />
next<br />
instru<br />
u ment<br />
for<br />
your<br />
tray<br />
Affordable<br />
and<br />
d b<br />
eyond<br />
portable<br />
Call Caa<br />
ll<br />
888-424-6527 888-424-6522<br />
7 now for details, or find your BIOLASE<br />
Territory Te e erritory<br />
y MManager<br />
anageer<br />
r at at BIOLASE. BIOLASE.com .com under r “Contact”. “ Coontact<br />
.<br />
© 20 2011 11<br />
BBIOLASE<br />
IOLAS<br />
S E |<br />
wwww.Biolase.com<br />
ww.Bi<br />
.Biolase.<br />
com<br />
| TTo<br />
Toll-free oll-frr<br />
ee<br />
8888-424-6527<br />
88-424-652<br />
27<br />
�<br />
�<br />
�<br />
�<br />
“ “N NOO<br />
C COMP<br />
PR R ROMI<br />
ISE SE” ”<br />
L DIODE<br />
S O OLUT<br />
UTIO<br />
ION<br />
aximum<br />
performanc<br />
c e for<br />
more<br />
proced<br />
ures<br />
–<br />
ludin<br />
g surgica<br />
l proc<br />
c edures<br />
Watt<br />
peak<br />
powe<br />
r w with<br />
ComfortPuls<br />
e<br />
A c l e a r e d f or t e m p or<br />
a<br />
r<br />
y r<br />
e<br />
l<br />
i<br />
e<br />
f o<br />
f m<br />
i<br />
n<br />
or p<br />
a<br />
i<br />
n<br />
<br />
perior<br />
20-min<br />
ut<br />
e w whitening<br />
solut<br />
ion
C A S E R E P O R T S<br />
Advantages <strong>of</strong> 980-nm Diode <strong>Laser</strong> Treatment<br />
in the Management <strong>of</strong> Gingival Pigmentation<br />
Mihir Khakhar, BDS, Postgraduate Student; Richa Kapoor, BDS, Postgraduate Student; N.D.<br />
Jayakumar, BDS, MDS, Pr<strong>of</strong>essor; O. Padmalatha, BDS, MDS, Pr<strong>of</strong>essor; Sheeja S. Varghese, BDS,<br />
MDS, Pr<strong>of</strong>essor; M. Sankari, BDS, MDS, Assistant Pr<strong>of</strong>essor<br />
Department <strong>of</strong> Periodontics, Saveetha Dental College, Chennai, India<br />
J <strong>Laser</strong> Dent 2011;19(3):283-285<br />
Mihir Khakhar, BDS<br />
I N T R O D U C T I O N<br />
The color <strong>of</strong> the gingiva is determined<br />
by several factors, including the<br />
number and size <strong>of</strong> the blood vessels,<br />
epithelial thickness, quantity <strong>of</strong> keratinization<br />
and pigments within the<br />
epithelium. Melanin, carotene,<br />
reduced hemoglobin, and oxyhemoglobin<br />
are the major pigments that<br />
contribute to the normal color <strong>of</strong> the<br />
oral mucosa. 1 Frequently, gingival<br />
hyperpigmentation is caused by<br />
heavy melanin deposition by<br />
melanocytes located in the basal<br />
layers <strong>of</strong> the epithelium. 2 Demand for<br />
cosmetic therapy <strong>of</strong> gingival melanin<br />
pigmentation is common and various<br />
methods have been used for depigmentation,<br />
each with its own merits<br />
and limitations. With the recent<br />
advances and developments in a wide<br />
range <strong>of</strong> laser wavelengths and<br />
different delivery systems, research<br />
suggests that lasers could be applied<br />
to periodontal, restorative, and<br />
surgical treatments.<br />
<strong>Laser</strong>s have the advantages <strong>of</strong><br />
easy handling, short treatment<br />
time, hemostasis, and bactericidal<br />
effects. They are used extensively<br />
for s<strong>of</strong>t tissue surgical procedures<br />
such as gingivectomy, frenectomy,<br />
sulcular debridement, and exci-<br />
sional and incisional biopsies. In<br />
the present case series an attempt<br />
was made to compare the healing,<br />
pain levels, and patient satisfaction<br />
during the treatment <strong>of</strong> gingival<br />
depigmentation using lasers,<br />
scalpel surgery, and electrocautery.<br />
Figure 1: <strong>Laser</strong> Depigmentation<br />
Figure 1a: Preoperative view showing<br />
diffuse melanin pigmentation<br />
Figure 1b: Intraoperative view showing<br />
de-epithelization performed with the<br />
laser in the maxillary and mandibular<br />
anterior region<br />
Figure 1c: Six-month postoperative view<br />
showing complete re-epithelization has<br />
occurred<br />
A B S T R A C T<br />
Gingival pigmentation is an<br />
aesthetic problem that <strong>of</strong>ten<br />
requires surgical removal. Recently<br />
there has been an increased use<br />
<strong>of</strong> hard and s<strong>of</strong>t tissue lasers in<br />
the field <strong>of</strong> dentistry. In the<br />
present case series, three cases<br />
which have been treated for<br />
gingival depigmentation using<br />
laser, scalpel surgery, and electrocautery<br />
techniques are presented.<br />
Healing, pain levels, and patient<br />
satisfaction in all three techniques<br />
are evaluated and compared.<br />
K E Y W O R D S<br />
Depigmentation, melanin pigmentation,<br />
electrocautery, laser<br />
C A S E 1<br />
A 25-year-old male presented with<br />
melanin pigmentation (Figure 1a).<br />
Topical anesthesia (lignocaine [lidocaine]<br />
hydrochloride, Lox 2% jelly,<br />
Neon Laboratories, India) was<br />
applied in the maxillary and<br />
mandibular anterior region.<br />
Depigmentation was carried out<br />
using a 980-nm diode laser<br />
(SIRO<strong>Laser</strong>, Sirona Dental<br />
Systems, Bensheim, Germany) set<br />
at a power <strong>of</strong> 2 W, in continuous<br />
mode, with a 300-micron fiber. The<br />
fiber tip was moved in a sweeping<br />
motion continuously from one site<br />
to another to avoid heat accumulation<br />
which could cause a<br />
postoperative burning sensation.<br />
Care was taken to maintain the<br />
physiologic contour <strong>of</strong> the gingiva<br />
during the procedure. All<br />
Khakhar, et al.<br />
J O U R N A L O F L A S E R D E N T I S T R Y | 2 011 V O L . 19 , N O . 3<br />
283
J O U R N A L O F L A S E R D E N T I S T R Y | 2 011 V O L . 19 , N O . 3<br />
284<br />
C A S E R E P O R T S<br />
Figure 2: Scalpel Depigmentation Figure 3: Electrocautery Depigmentation<br />
Figure 2a: Preoperative view showing<br />
diffuse melanin pigmentation<br />
Figure 2b: Intraoperative view showing<br />
surface de-epithelization and exposed<br />
underlying connective tissue<br />
Figure 2c: Six-month postoperative view<br />
showing healthy gingival tissues with no<br />
areas <strong>of</strong> repigmentation<br />
pigmented areas were removed; the<br />
area was wiped with gauze soaked<br />
in saline (Figure 1b). The entire<br />
procedure took 30 minutes.<br />
After 24 hours a white fibrin<br />
slough was seen on the surgical<br />
area which lasted for 1 week. Three<br />
months postoperatively gingival<br />
healing was complete with few<br />
areas <strong>of</strong> repigmentation. At the end<br />
<strong>of</strong> 6 months no further increase in<br />
areas <strong>of</strong> repigmentation was<br />
observed (Figure 1c).<br />
Pain levels were evaluated<br />
immediately after the procedure<br />
and 1 week postoperatively using a<br />
Visual Analog Scale (VAS). The<br />
VAS consisted <strong>of</strong> a horizontal line<br />
100 mm long, anchored at the left<br />
by the descriptor “no pain” and at<br />
the other end by “unbearable pain.”<br />
The patient was asked to mark the<br />
Khakhar, et al.<br />
Figure 3a: Preoperative view showing<br />
extensive melanin pigmentation<br />
Figure 3b: Intraoperative view showing<br />
de-epithelization in the maxillary anterior<br />
region<br />
severity <strong>of</strong> the pain. The distance<br />
from the left end to the point<br />
checked was recorded in millimeters<br />
and used as the VAS score.<br />
CASE 2<br />
A 21-year-old female revealed<br />
deeply pigmented gingiva (Figure<br />
2a). Scalpel surgery was planned.<br />
Local anesthesia (lignocaine [lidocaine]<br />
hydrochloride with 1:200,000<br />
adrenaline bitartrate, Lox 2%,<br />
Neon Laboratories; 4 ml total, 2 ml<br />
per arch) was infiltrated in the<br />
maxillary and mandibular anterior<br />
region. A scalpel (Bard-Parker<br />
No. 15 blade) was used to deepithelize<br />
the pigmented<br />
epithelium along with a thin layer<br />
<strong>of</strong> connective tissue. All remnants<br />
<strong>of</strong> pigmented epithelium were<br />
removed; the area was irrigated<br />
with normal saline (Figure 2b). The<br />
surgical area was covered with a<br />
periodontal dressing. The entire<br />
procedure lasted 25 minutes.<br />
After 1 week, the periodontal<br />
dressing was removed; the area<br />
was irrigated with saline and<br />
Figure 3c: Intraoperative view showing<br />
de-epithelization in the mandibular anterior<br />
region<br />
Figure 3d: Three-month postoperative<br />
view showing a few patchy areas <strong>of</strong><br />
repigmentation<br />
repacked for another week. The<br />
healing process was satisfactory<br />
and the patient was asymptomatic.<br />
At the end <strong>of</strong> 1 month, complete<br />
re-epithelization was observed with<br />
no postoperative pain and sensitivity.<br />
At the end <strong>of</strong> 6 months, the<br />
gingiva appeared healthy and no<br />
further repigmentation was seen<br />
(Figure 2c).<br />
Similar to Case 1, pain levels<br />
were evaluated using a Visual<br />
Analog Scale.<br />
CASE 3<br />
A depigmentation procedure using<br />
electrocautery was planned for a<br />
22-year-old female (Figure 3a).<br />
Following administration <strong>of</strong> local<br />
anesthesia (lignocaine [lidocaine]<br />
hydrochloride with 1:200,000 adrenaline<br />
bitartrate, Lox 2%, Neon<br />
Laboratories), a loop electrode was<br />
used to de-epithelize the gingiva<br />
from the right first premolar to the<br />
left first premolar. It was used with<br />
light brushing strokes and the tip
was kept in constant motion. Care<br />
was taken to avoid keeping the tip<br />
in one place as this would lead to<br />
excessive heat buildup and cause<br />
damage to the underlying bone<br />
(Figures 3b-3c). The area was then<br />
irrigated with normal saline to<br />
remove the tissue debris. The entire<br />
procedure was completed in 30<br />
minutes. The 3-month postoperative<br />
examination revealed well-epithelialized,<br />
pink gingiva with few<br />
remnants <strong>of</strong> pigmentation (Figure<br />
3d). Similar to the other cases, pain<br />
measurements were performed.<br />
DISCUSSION<br />
Three cases were treated for<br />
gingival hyperpigmentation using<br />
laser, scalpel surgery, and electrocautery.<br />
Pain levels were evaluated<br />
using a Visual Analog Scale immediately<br />
after the procedure and 1<br />
week postoperatively. As can be<br />
seen in Table 1, immediately after<br />
the procedure, the VAS score for<br />
the patient treated with the laser<br />
was lower compared to patients<br />
treated with scalpel surgery and<br />
electrocautery, indicating the laser<br />
procedure produced less pain and<br />
discomfort. It can be theorized that<br />
this may be due to protein coagulum<br />
that is formed on the wound<br />
surface, which may act as a biological<br />
wound dressing 3 and seal the<br />
ends <strong>of</strong> the sensory nerves. 4<br />
In all three patients, healing<br />
was uneventful. A white fibrin<br />
slough was seen in Case 1 after 24<br />
hours; this is a normal characteristic<br />
<strong>of</strong> a laser wound during the<br />
first several days <strong>of</strong> healing. In this<br />
case, the “hot tip” <strong>of</strong> the diode laser<br />
produced a relatively thick coagulation<br />
layer on the treated surface.<br />
Bleeding that occurred during<br />
scalpel surgery was eliminated<br />
when laser and electrocautery were<br />
used. This can be attributed to the<br />
property <strong>of</strong> lasers and electrocautery<br />
instruments to coagulate<br />
bleeding vessels and thereby assist<br />
in providing a relatively dry<br />
surgical field.<br />
At the end <strong>of</strong> 6 months, all three<br />
treatment modalities provided<br />
satisfactory results in terms <strong>of</strong><br />
healing, repigmentation, and<br />
patient satisfaction. Few patchy<br />
areas <strong>of</strong> repigmentation were<br />
observed in the cases treated with<br />
electrosurgery and laser. This could<br />
be due to deeper pigmentation in<br />
these cases.<br />
CONCLUSION<br />
Within the limitations <strong>of</strong> this study,<br />
the use <strong>of</strong> a diode laser is shown to<br />
be a safe and effective treatment<br />
modality to provide optimal<br />
esthetics and enhanced comfort<br />
with reduced discomfort to the<br />
patients during the treatment for<br />
gingival hyperpigmentation. A<br />
longitudinal investigation <strong>of</strong><br />
similar treatments in a larger<br />
patient population would be helpful<br />
to confirm these findings.<br />
AUTHOR BIOGRAPHY<br />
Dr. Mihir Khakhar received his<br />
BDS from the Maharashtra<br />
University <strong>of</strong> Health Science,<br />
Nashik, India in 2008 and is<br />
currently pursuing his MDS in peri-<br />
C A S E R E P O R T S<br />
Table 1: Visual Analog Scale (VAS) Scores for All Three Cases<br />
VAS Scores<br />
Immediately Postoperative 1-Week Postoperative<br />
Case 1 8 3<br />
Case 2 15 4<br />
Case 3 10 3<br />
odontics at Saveetha University in<br />
Chennai, India. He has been a delegate<br />
at various national conferences<br />
on periodontics, implant dentistry,<br />
and general dentistry and has<br />
received awards for poster and<br />
paper presentations. He is also<br />
working on a research project<br />
related to the molecular pathogenesis<br />
<strong>of</strong> periodontal diseases. He can<br />
be contacted via e-mail at<br />
mihirkhakhar@gmail.com.<br />
Disclosure: Dr. Khakhar has no<br />
commercial affiliations or conflicts <strong>of</strong><br />
interest.<br />
REFERENCES<br />
1. Volker JF, Kenney JA Jr. The physiology<br />
and biochemistry <strong>of</strong><br />
pigmentation. J Periodontol<br />
1960;31(5):346-355.<br />
2. Dummett CO. Overview <strong>of</strong> normal<br />
oral pigmentations. J Indiana Dent<br />
Assoc 1980;59(3):13-18.<br />
3. Fisher SE, Frame JW, Browne RM,<br />
Tranter RMD. A comparative histological<br />
study <strong>of</strong> wound healing<br />
following CO2 laser and conventional<br />
surgical excision <strong>of</strong> canine<br />
buccal mucosa. Arch Oral Biol<br />
1983;28(4):287-291.<br />
4. Schuller DE. Use <strong>of</strong> the laser in the<br />
oral cavity. Otolaryngol Clin North<br />
Am 1990;23(1):31-42. nn<br />
Khakhar, et al.<br />
J O U R N A L O F L A S E R D E N T I S T R Y | 2 011 V O L . 19 , N O . 3<br />
285
J O U R N A L O F L A S E R D E N T I S T R Y | 2 011 V O L . 19 , N O . 3<br />
286<br />
C L I N I C A L C A S E<br />
Gingival Depigmentation with an Er:YAG <strong>Laser</strong>:<br />
A Clinical Case with Three-Year Follow-Up<br />
Grace Sun, DDS, Los Angeles, California<br />
J <strong>Laser</strong> Dent 2011;19(3):286-288<br />
S Y N O P S I S<br />
This clinical case study describes the removal <strong>of</strong> gingival hyperpig-<br />
mentation using an Er:YAG laser. This benign condition was an<br />
esthetic concern for the patient, and the laser procedure produced<br />
good results. While the prognosis is good, the patient’s smoking can<br />
stimulate melanin production and the coloration can reappear.<br />
P R E T R E AT M E N T<br />
A. Case Outline<br />
A 43-year-old African American male<br />
presented with normal medical, oral,<br />
and dental health. The patient<br />
reported that his four upper incisors<br />
had a history <strong>of</strong> trauma, but he<br />
would not supply any details. A clinical<br />
examination revealed that those<br />
four teeth had received endodontic<br />
therapy and were then restored with<br />
porcelain-fused-to-metal crowns. A<br />
panoramic radiograph showed good<br />
dental health (Figure 1). The patient<br />
had been a cigarette smoker for 20<br />
years, but had since quit smoking for<br />
10 years. The patient had recently<br />
finished adult orthodontic therapy<br />
and was happy with the results; but<br />
he expressed concern about the darkened<br />
color <strong>of</strong> his gingival tissue on<br />
both arches, as seen in Figure 2. He<br />
was informed that pigmentation can<br />
Figure 1: Panoramic radiograph<br />
Sun<br />
be a normal benign condition, but he<br />
revealed that he was unhappy with<br />
the esthetics. Furthermore, he<br />
described the coloration to have had<br />
a negative psychological impact on<br />
him for the past 20 years.<br />
B. Diagnosis<br />
The diagnosis is hyperpigmentation<br />
due to excessive melanin in the basal<br />
layer <strong>of</strong> the epithelium. This condition<br />
exists among all races, but is<br />
more prevalent among the African<br />
and South Asian population. It can<br />
be exacerbated by smoking, since<br />
chemicals such as nicotine can activate<br />
melanocytes to produce melanin.<br />
In fact, this benign increase in<br />
melanin has been termed “smoker’s<br />
melanin.” 1 The metal substrate <strong>of</strong> his<br />
crowns appeared to be a precious<br />
alloy, and this finding was important<br />
since some nonprecious metals can<br />
cause marginal gingival discoloration.<br />
It was then determined that<br />
the metal composition was not a<br />
factor in the s<strong>of</strong>t tissue coloration on<br />
the maxilla and had no effect on the<br />
mandibular arch. Periodontal probing<br />
showed adequate biologic width<br />
around all teeth, with normal pocket<br />
depth and healthy tissue.<br />
C. Treatment Options,<br />
Precautions, and Informed<br />
Consent<br />
As per the patient’s request,<br />
removal <strong>of</strong> the excessively<br />
pigmented portion <strong>of</strong> the gingival<br />
tissue will be performed.<br />
The options for this elective<br />
treatment were discussed, including<br />
scalpel surgery, rotary abrasion,<br />
cryotherapy, electrosurgery, and<br />
laser ablation. The patient chose the<br />
laser option. Multiple wavelengths<br />
<strong>of</strong> dental lasers could be utilized to<br />
ablate the basal epithelial layer<br />
containing the melanin. Since prime<br />
absorption <strong>of</strong> melanin and other<br />
pigments occurs in the near-infrared<br />
portion <strong>of</strong> the electromagnetic spectrum,<br />
diode or Nd:YAG laser<br />
wavelengths would be good choices<br />
for efficiency. 2 Erbium and carbon<br />
dioxide lasers could also be used,<br />
since they are also effective for s<strong>of</strong>t<br />
tissue surgery. 3-5<br />
The chief precaution is to control<br />
the energy delivered to the tissue<br />
to avoid potential collateral<br />
damage. Depending on which laser<br />
wavelength is chosen, underlying<br />
connective tissue, periosteum, and<br />
bone could suffer from the heat <strong>of</strong><br />
ablation if it were to extend beyond<br />
the target tissue.<br />
The second precaution is to<br />
preserve as much <strong>of</strong> the thin<br />
marginal tissue as possible, partic-
Figure 2: Preoperative full-smile view <strong>of</strong><br />
excessive pigmentation<br />
ularly on the mandibular arch.<br />
The author chose a fiber-delivered<br />
Er:YAG laser because its<br />
free-running pulse emission mode<br />
provides some degree <strong>of</strong> thermal<br />
relaxation, and it has a relatively<br />
shallow depth <strong>of</strong> penetration. As<br />
with other lasers with flexible<br />
delivery systems, it permits accurate<br />
placement <strong>of</strong> the tip. The<br />
instrument can also be used with a<br />
water spray for s<strong>of</strong>t tissue surgery<br />
to help cool the tissue and flush the<br />
site <strong>of</strong> debris. While the Er:YAG<br />
laser has limited hemostatic ability<br />
on s<strong>of</strong>t tissue, especially when coincidental<br />
water spray is used, it was<br />
felt that whatever bleeding might<br />
occur in this moderately vascular<br />
area could be readily controlled via<br />
conventional means such as<br />
compression. Moreover, efficient<br />
high-volume evacuation and<br />
enhanced visualization with magnification<br />
will aid in the precision <strong>of</strong><br />
the procedure.<br />
The patient gave his consent for<br />
the procedure.<br />
T R E AT M E N T<br />
A. Treatment Objective<br />
The objective was de-epithelization<br />
to remove the melanin principally<br />
located in the basal layer <strong>of</strong> the<br />
epithelium.<br />
B. <strong>Laser</strong> Operating Parameters<br />
An Er:YAG laser (DELight, Hoya<br />
ConBio, Fremont, Calif.), 2940-nm<br />
wavelength with a fiber delivery<br />
system was used with a 600-micrometer<br />
80-degree tip. The parameters<br />
were 30 Hz, 70 mJ, with a water<br />
spray. This is a low power setting<br />
Figure 3: Intraoperative view <strong>of</strong> maxillary<br />
arch<br />
(2.1 W), and some <strong>of</strong> the laser<br />
energy will absorbed by the water<br />
spray. The total treatment time was<br />
2 hours and the laser exposure was<br />
approximately 20 minutes.<br />
C. Treatment<br />
High-volume evacuation was in<br />
place, and all laser safety precautions<br />
were used. Visualization was<br />
enhanced with 3.5x magnification.<br />
Periodontal probing showed adequate<br />
attached gingival width. Only topical<br />
anesthetic (TAC 20% alternate gel –<br />
tetracaine 4%, phenylephrine 2%,<br />
lidocaine 20%) (Pr<strong>of</strong>essional Arts<br />
Pharmacy, Lafayette, La.) was used.<br />
This topical cream is applied for 5<br />
minutes onto an area <strong>of</strong> tissue. After<br />
that time, good anesthesia is<br />
obtained for 20-30 minutes.<br />
The treatment area on the maxillary<br />
arch extended from the right<br />
first bicuspid to the left first<br />
bicuspid and consisted <strong>of</strong> a 5-mmwide<br />
band <strong>of</strong> excessive pigmentation<br />
on thick gingival tissue. On the<br />
mandible, the area extended from<br />
cuspid to cuspid, and the pigmented<br />
width varied from 2 to 7 mm, within<br />
thin marginal tissue.<br />
The first site selected was the<br />
tissue above the upper right cuspid,<br />
where the tissue thickness was<br />
greatest. The laser energy was<br />
directed at the tissue with very light<br />
contact <strong>of</strong> the tip. The epithelium<br />
was gradually ablated in very thin<br />
layers. Ultimately, the basal layer<br />
was exposed and carefully ablated,<br />
and the pigmentation was removed.<br />
When this area was completed, the<br />
same parameters and procedures<br />
continued toward the left cuspid<br />
C L I N I C A L C A S E<br />
area. Figure 3 shows an intraoperative<br />
photograph, and the ablation<br />
areas are apparent. The mandibular<br />
tissue was treated with the same<br />
parameters and protocol, once again<br />
moving from right to left.<br />
Some bleeding occurred in<br />
various areas after the pigmentation<br />
was removed. Hemostasis was<br />
achieved by compression with wet<br />
gauze and no complications arose.<br />
The immediate postoperative view<br />
is shown in Figure 3.<br />
Upon completion <strong>of</strong> the procedure<br />
in both arches, adequate free<br />
gingival marginal tissue remained,<br />
and bleeding was absent on the<br />
ablated surfaces.<br />
D. Postoperative Assessment<br />
and Instructions<br />
The patient did not experience any<br />
discomfort during or after the<br />
procedure, and there were no<br />
complications. The postoperative<br />
instructions were to eat a s<strong>of</strong>t diet<br />
and take over-the-counter medications<br />
such as Motrin ® , Advil ® , or<br />
Tylenol ® if necessary.<br />
F O L LO W- U P C A R E<br />
A. Treatment Assessment,<br />
Prognosis, and Long-Term<br />
Results<br />
The healing was uneventful and the<br />
early prognosis was good. The patient<br />
returned for follow-up visits at 1<br />
week, 2 weeks, 6 weeks, 3 months, 6<br />
months, 1 year, 2 years, and 3 years.<br />
Figures 4-9 show various postoperative<br />
periods. The gingival tissues have<br />
remained healthy, and the patient<br />
liked the absence <strong>of</strong> the darkened<br />
gingiva. At the 3-year-postoperative<br />
visit, some slight repigmentation<br />
appeared (Figure 9). Comparison <strong>of</strong><br />
photographic records confirmed this<br />
reappearance. The patient reported<br />
that he started smoking cigars, and<br />
he was reminded that smoking can<br />
contribute to excessive pigmentation.<br />
B. Long-Term Prognosis and<br />
Conclusion<br />
The long-term prognosis is good. As<br />
noted above, it is partially<br />
Sun<br />
J O U R N A L O F L A S E R D E N T I S T R Y | 2 011 V O L . 19 , N O . 3<br />
287
J O U R N A L O F L A S E R D E N T I S T R Y | 2 011 V O L . 19 , N O . 3<br />
288<br />
C L I N I C A L C A S E<br />
Figure 4: Two-week postoperative view <strong>of</strong><br />
maxillary arch<br />
Figure 7: Three-month postoperative fullsmile<br />
view<br />
dependent on the patient’s smoking<br />
habits. Moreover, he has a genetic<br />
tendency to produce melanin.<br />
The gingival depigmentation<br />
procedure using the Er:YAG laser<br />
was successful, with good patient<br />
comfort, predictable healing, and<br />
satisfaction.<br />
R E F E R E N C E S<br />
1. Brown FH, Housten GD. Smoker’s<br />
melanosis. A case report. J<br />
Periodontol 1991;62(8):524-527.<br />
2. Coluzzi DJ, Convissar RA. Atlas <strong>of</strong><br />
laser applications in dentistry.<br />
Chicago: Quintessence Publishing<br />
Co., Inc., 2007:1-8.<br />
3. Nakamura Y, Hossain M, Hirayama<br />
K, Matsumoto K. A clinical study on<br />
the removal <strong>of</strong> gingival melanin<br />
pigmentation with the CO2 laser.<br />
Sun<br />
Figure 5: Two-week postoperative view <strong>of</strong><br />
mandibular arch<br />
Figure 8: One-year postoperative fullsmile<br />
view<br />
<strong>Laser</strong>s Surg Med 1999;25(2):140-147.<br />
4. Tal H, Oegiesser D, Tal M. Gingival<br />
depigmentation by erbium:YAG<br />
laser: Clinical observations and<br />
patient responses. J Periodontol<br />
2003;74(11):1660-1667.<br />
5. Rosa DSA, Aranha ACC, Eduardo<br />
Cde P, Aoki A. Esthetic treatment <strong>of</strong><br />
gingival melanin hyperpigmentation<br />
with Er:YAG laser: Short-term clinical<br />
observations and patient<br />
follow-up. J Periodontol<br />
2007;78(10):2018-2025.<br />
A U T H O R B I O G R A P H Y<br />
Dr. Grace Sun routinely utilizes<br />
multiple wavelengths <strong>of</strong> dental<br />
lasers. Her articles on dental lasers<br />
have been published in Dental<br />
Clinics <strong>of</strong> North America. Dr. Sun<br />
is also certified as Advanced<br />
Pr<strong>of</strong>iciency and was awarded<br />
Figure 6: Six-week postoperative fullsmile<br />
view<br />
Figure 9: Three-year postoperative fullsmile<br />
view<br />
Educator status by the <strong>Academy</strong> <strong>of</strong><br />
<strong>Laser</strong> <strong>Dentistry</strong> where she was a<br />
member <strong>of</strong> the Board <strong>of</strong> Directors.<br />
She had lectured internationally on<br />
the subjects <strong>of</strong> laser and cosmetic<br />
dentistry. Dr. Sun is an accredited<br />
Fellow with the American <strong>Academy</strong><br />
<strong>of</strong> Cosmetic <strong>Dentistry</strong>, a Fellow <strong>of</strong><br />
the International Congress <strong>of</strong> Oral<br />
Implantologists, and is a Master <strong>of</strong><br />
the <strong>Academy</strong> <strong>of</strong> General <strong>Dentistry</strong>.<br />
Dr. Sun may be contacted by e-mail<br />
at gracesun@sundds.com.<br />
Disclosure: Dr. Sun has no commercial<br />
relationships relative to this<br />
article.<br />
Editor’s Note: This article first<br />
appeared in J <strong>Laser</strong> Dent<br />
2008;16(3):130-132. nn
C L I N I C A L R E V I E W A N D C A S E R E P O R T S<br />
Photobiomodulation: An Invaluable Tool for All<br />
Dental Specialties<br />
Gerald Ross, DDS, Alana Ross, BScH, Tottenham, Ontario, Canada<br />
J <strong>Laser</strong> Dent 2011;19(3):289-296<br />
I N T R O D U C T I O N<br />
Although low-level lasers are being<br />
used successfully in many dental<br />
clinics, the wide range <strong>of</strong> applications<br />
is still largely unknown to<br />
many practitioners, especially<br />
dental specialists. In these fields,<br />
there is the potential to see the<br />
most definitive results <strong>of</strong> what laser<br />
therapy can do to improve clinical<br />
outcomes and patient satisfaction.<br />
Photobiomodulation (PBM), also<br />
commonly referred to as low-level<br />
laser therapy (LLLT) or cold laser<br />
therapy, uses light energy to elicit<br />
biological responses from the cell<br />
and normalize cell function.<br />
Numerous studies have shown that<br />
PBM affects the mitochondria <strong>of</strong><br />
the cell, primarily cytochrome-c<br />
oxidase in the electron transfer<br />
chain and porphyrins on the cell<br />
membrane. 1-2 It has been proposed<br />
that when light photons are<br />
absorbed by these receptors, three<br />
events occur: stimulation <strong>of</strong> adenosine<br />
triphosphate (ATP) synthesis<br />
by activation <strong>of</strong> the electron transport<br />
chain; transient stimulation <strong>of</strong><br />
reactive oxygen species, which<br />
increases the conversion <strong>of</strong> adenosine<br />
diphosphate (ADP) to ATP;<br />
and a temporary release <strong>of</strong> nitric<br />
oxide from its binding site on<br />
cytochrome-c oxidase. These factors<br />
contribute to the clinical effects<br />
seen with PBM, including tissue<br />
repair, relief <strong>of</strong> inflammation and<br />
pain, and repair <strong>of</strong> nerve damage. 3<br />
Figure 1 depicts a flowchart<br />
showing these interactions.<br />
Studies have documented beneficial<br />
effects <strong>of</strong> PBM, such as<br />
stimulation <strong>of</strong> fibroblasts and<br />
osteoblasts, as well a reduction <strong>of</strong><br />
the depolarization <strong>of</strong> nerve fibers. 4-6<br />
From a clinical perspective, PBM<br />
<strong>of</strong>fers dental practitioners a nonin-<br />
Figure 1: Summary <strong>of</strong> the primary mechanisms <strong>of</strong> photobiomodulation<br />
vasive and nonthermal treatment<br />
modality that can be used as an<br />
adjunct to traditional therapies or<br />
as a therapeutic tool on its own. 7<br />
Examples <strong>of</strong> these clinical applications,<br />
which will be discussed below,<br />
include dental analgesia, treatment<br />
<strong>of</strong> dentin hypersensitivity, healing <strong>of</strong><br />
s<strong>of</strong>t tissue lesions, reduction <strong>of</strong> pain<br />
and swelling after surgical procedures,<br />
better integration <strong>of</strong> implants<br />
into bone, and faster movement <strong>of</strong><br />
teeth during orthodontic procedures.<br />
Determining the Appropriate<br />
Dose<br />
Treatment dose is probably the<br />
most important variable in laser<br />
treatment. Dose is measured in<br />
joules per square centimeter (J/cm 2 )<br />
and is a measure <strong>of</strong> the amount <strong>of</strong><br />
energy that is conducted into the<br />
tissue. Clinical effects <strong>of</strong> the laser,<br />
such as wound healing, pain relief,<br />
or muscle relaxation, are all sensitive<br />
to different irradiances or<br />
doses. An example <strong>of</strong> this is the<br />
stimulation <strong>of</strong> fibroblasts; a dose <strong>of</strong><br />
5 J/cm 2 will stimulate the cellular<br />
activity <strong>of</strong> fibroblasts, whereas<br />
higher doses inhibit cell viability<br />
and proliferation. 8 Thus, for wound<br />
healing, the clinician should ideally<br />
use a dose lower than 5 J/cm 2 .<br />
The biostimulatory and<br />
inhibitory effects <strong>of</strong> lasers are<br />
governed by the Arndt-Schultz<br />
Law, which indicates that weak<br />
stimuli will increase physiological<br />
processes and strong stimuli will<br />
inhibit physiological activity. A<br />
therapeutic window, which includes<br />
both biostimulatory and bioinhibitory<br />
effects, is evident and is<br />
the intended target for PBM treatments.<br />
A depiction <strong>of</strong> the law, based<br />
on Baxter, 9 is shown in Figure 2.<br />
Ross and Ross<br />
J O U R N A L O F L A S E R D E N T I S T R Y | 2 011 V O L . 19 , N O . 3<br />
289
J O U R N A L O F L A S E R D E N T I S T R Y | 2 011 V O L . 19 , N O . 3<br />
290<br />
C L I N I C A L R E V I E W A N D C A S E R E P O R T S<br />
Figure 2: Arndt-Schultz curve. The horizontal axis depicts an increasingly higher dose<br />
from left to right, and indicates that biostimulation occurs with relatively smaller doses<br />
when compared to the higher doses that cause bioinhibition<br />
The importance <strong>of</strong> dose should<br />
always be kept in mind when using<br />
PBM; if the clinician is not<br />
achieving the anticipated response<br />
to laser treatment, the dose should<br />
be re-evaluated to ensure it is<br />
within the optimal range.<br />
Additionally, treatments may need<br />
to be modified over time to ensure<br />
the practitioner is achieving the<br />
ideal effect from the laser dose<br />
(pain relief vs. wound healing).<br />
Acute vs. Chronic Pain<br />
Treatment dose and duration will<br />
largely be governed by the status <strong>of</strong><br />
the injury. PBM can effectively<br />
speed the resolution <strong>of</strong> acute<br />
inflammation and pain, conditions<br />
that should be treated frequently<br />
(daily). The reverse applies to<br />
chronic pain; treatments should be<br />
done using lower doses over a<br />
longer period <strong>of</strong> time (e.g., treat 2 to<br />
3 times per week for 3 to 4 weeks).<br />
CLINICAL APPLICATIONS OF<br />
PHOTOBIOMODULATION IN<br />
DENTAL SPECIALTIES<br />
Oral Surgery<br />
Dental surgeons can utilize PBM in<br />
almost every facet <strong>of</strong> their practice.<br />
Ross and Ross<br />
Many procedures a dental surgeon<br />
performs, especially extraction <strong>of</strong><br />
molars, create an acute inflammatory<br />
response that can result in<br />
edema, bruising, and pain.<br />
Currently, the primary method <strong>of</strong><br />
dealing with the pain and discomfort<br />
<strong>of</strong> the surgical procedures is<br />
prescription <strong>of</strong> pain analgesics,<br />
many <strong>of</strong> which carry side effects or<br />
decreased mental alertness. Studies<br />
have demonstrated that PBM in<br />
acute pain reduction compares well<br />
to standard non steroidal antiinflammatory<br />
drug (NSAID)<br />
treatment, with a better riskbenefit<br />
pr<strong>of</strong>ile. 10 Healing is also<br />
accelerated by stimulation <strong>of</strong> fibroblasts<br />
and osteoblasts, which<br />
produce s<strong>of</strong>t tissue and bone,<br />
respectively, as noted in an animal<br />
study conducted by Gerbi et al. 11<br />
Post-Extraction<br />
Following any surgical extraction,<br />
laser irradiation is applied into the<br />
socket immediately after the<br />
surgery for reduction <strong>of</strong> pain and<br />
inflammation and then after<br />
suturing for s<strong>of</strong>t tissue healing<br />
(Figure 3).<br />
Aras and Güngörmü¸s studied the<br />
effect <strong>of</strong> PBM on trismus and facial<br />
swelling following surgical extraction<br />
<strong>of</strong> the third molar and found<br />
that measurements <strong>of</strong> swelling<br />
were about 5 mm less and measurements<br />
<strong>of</strong> trismus (inter-incisal<br />
opening) were about 5 mm greater<br />
than in the placebo group on days 2<br />
and 7. 12 In a meta-analysis <strong>of</strong><br />
studies investigating pain within 24<br />
hours <strong>of</strong> surgery, Bjordal et al.<br />
found that LLLT with red and<br />
infrared wavelengths is effective in<br />
reducing acute inflammatory pain<br />
after molar extraction. 13<br />
Dry Socket<br />
Tunér and Hode describe the benefits<br />
<strong>of</strong> PBM in helping to prevent<br />
alveolitis after a tooth extraction. 14<br />
The following case study illustrates<br />
PBM treatment for a painful ‘dry<br />
socket.’<br />
Oral Mucositis<br />
Oral mucositis, presenting as an<br />
open sore over the oral s<strong>of</strong>t tissue,<br />
is a life-altering condition that is a<br />
side effect <strong>of</strong> chemotherapy and<br />
radiation therapy. <strong>Laser</strong> therapy<br />
has been investigated as a preventative<br />
application to mucositis and<br />
as a treatment modality for healing<br />
erupted sores, with positive<br />
results. 15 A 2006 study by Corti et<br />
al., using a light-emitting diode<br />
device with an emission <strong>of</strong> 645 ± 15<br />
nm, demonstrated that PBM accelerated<br />
the healing rate <strong>of</strong> oral<br />
mucositis by 117% to 164%. 16<br />
Often, oral mucositis can be so<br />
debilitating for patients that they<br />
cannot continue their cancer treatments,<br />
so a tool that can treat or<br />
Figure 3: Application <strong>of</strong> low-level laser<br />
energy into the socket immediately<br />
following extraction
prevent the sores will have considerable<br />
clinical importance.<br />
Consultation with the oncologist<br />
should always be done prior to<br />
commencing laser treatments.<br />
Fractures and Orthognathic Surgery<br />
PBM accelerates healing <strong>of</strong> bone<br />
after fractures or orthognathic<br />
surgery through the stimulation <strong>of</strong><br />
osteoblasts. A 2005 study in rats<br />
demonstrated that laser irradiation<br />
resulted in an increase in bone<br />
ne<strong>of</strong>ormation, with better quality<br />
bone on the irradiated groups when<br />
compared to the control group, who<br />
received no radiation. 11<br />
S<strong>of</strong>t Tissue Lesions<br />
S<strong>of</strong>t tissue lesions, such as herpes<br />
simplex, denture sores, and angular<br />
cheilitis respond positively to lowlevel<br />
laser irradiation. Schindl and<br />
Neumann investigated the effect <strong>of</strong><br />
LLLT on recurrent herpes simplex<br />
and demonstrated that 10 daily<br />
irradiations significantly lowered<br />
the incidence <strong>of</strong> local recurrence<br />
and is a beneficial treatment alternative<br />
to commonly used drugs<br />
such as acyclovir and famciclovir. 17<br />
Further, the author has clinically<br />
observed that laser irradiation <strong>of</strong><br />
herpes simplex decreases the incidence<br />
<strong>of</strong> lesion recurrence. Marei et<br />
al. examined the effect <strong>of</strong> laser<br />
irradiation on denture sores and<br />
noted that LLLT eased the pain<br />
caused by denture lesions, while at<br />
4 weeks post-treatment the laserirradiated<br />
areas showed clinically<br />
superior healing, and histological<br />
epithelialization and vascularization<br />
<strong>of</strong> the lesion. 18 Tunér and Hode<br />
report successful treatment <strong>of</strong><br />
angular chelitis with PBM, but<br />
warn <strong>of</strong> its recurrence if the fundamental<br />
cause is not dealt with. 19 It<br />
is advantageous to treat any s<strong>of</strong>t<br />
tissue lesion in its most acute<br />
stage. For example, herpetic lesions<br />
are most susceptible to LLLT<br />
during their prodromal stage.<br />
Figure 4 demonstrates the treatment<br />
<strong>of</strong> a lesion on the lip using an<br />
830-nm PBM device.<br />
C L I N I C A L R E V I E W A N D C A S E R E P O R T S<br />
Dental Infections<br />
For infections and edema, PBM has<br />
been reported to dilate lymphatic<br />
vessels and reduce the permeability<br />
<strong>of</strong> blood vessels. 20 Figure 5 demonstrates<br />
the application to the<br />
lymph nodes using a PBM device.<br />
Primary Tooth Restorations<br />
A variety <strong>of</strong> factors contribute to<br />
the analgesic effect produced by<br />
PBM which allows dental practitioners<br />
to perform many primary<br />
tooth restorations without anesthesia.<br />
Small animal studies show<br />
that laser irradiation promotes a<br />
release <strong>of</strong> endorphins and serotonin;<br />
inhibits the conduction <strong>of</strong><br />
C fibers, the fibers that carry<br />
pulpal pain; and increases oxygenation<br />
and lymphatic drainage, which<br />
are responsible for pain relief after<br />
the first minutes <strong>of</strong> tissue irradia-<br />
6, 21-22 tion.<br />
Figure 4: LLLT treatment <strong>of</strong> a s<strong>of</strong>t tissue<br />
lesion<br />
C A S E S T U DY : D RY S O C K E T<br />
Treating Dentist: Dr. Gerald Ross<br />
A 45-year-old male patient had a lower first molar extracted.<br />
During the postoperative instructions, the patient (a smoker) was<br />
advised to avoid smoking cigarettes for a minimum <strong>of</strong> 2 days. The<br />
patient presented the following day with dry socket and admitted to<br />
smoking the previous evening.<br />
An 830-nm PBM device was used. The intraoral light guide was<br />
placed in the socket and the socket was irradiated until pain relief<br />
was felt by patient (in this case 48 J/cm 2 <strong>of</strong> energy was applied before<br />
the patient started to experience a reduction in discomfort). A<br />
dressing was placed into the socket and the patient was sent home<br />
without any pain medications. The patient returned the next day for<br />
a dressing change and the laser was applied into the socket using 4<br />
J/cm 2 before application <strong>of</strong> the new dressing for stimulation <strong>of</strong> the<br />
epithelium in the socket. The patient did not require any additional<br />
treatments and the area healed in 7 days.<br />
C A S E S T U DY : O R A L M U C O S I T I S<br />
Treating Dentist: Dr. Gerald Ross<br />
A 61-year-old female patient undergoing chemotherapy for terminal<br />
cancer presented with numerous sores over the inside <strong>of</strong> her mouth.<br />
The patient could not eat, drink, or swallow without extreme pain.<br />
Treatments (mouth rinses) assigned by the oncologist had no effect<br />
on healing <strong>of</strong> the sores. A visible red laser (660 nm) was applied<br />
intraorally overlapping throughout the mouth for 2 days in a row.<br />
When the patient came in on the second day, the pain was markedly<br />
decreased and she was able to eat soup. By the fourth day, she was<br />
able to eat normally. The patient passed away in the following month<br />
but no sores returned during that time.<br />
NOTE: Prior to laser treatment, the dentist contacted the oncologist<br />
who was willing to try any treatment that could work on the<br />
mucositis.<br />
Ross and Ross<br />
J O U R N A L O F L A S E R D E N T I S T R Y | 2 011 V O L . 19 , N O . 3<br />
291
J O U R N A L O F L A S E R D E N T I S T R Y | 2 011 V O L . 19 , N O . 3<br />
292<br />
C L I N I C A L R E V I E W A N D C A S E R E P O R T S<br />
Figure 5: Application <strong>of</strong> low-level laser to<br />
the submandibular lymph nodes<br />
<strong>Laser</strong> irradiation is applied to<br />
the apex <strong>of</strong> each root for analgesia<br />
and again after the tooth has been<br />
prepared for reduction <strong>of</strong> pain and<br />
inflammation, as shown in Figure<br />
6. Distraction techniques are<br />
recommended to help the patient<br />
deal with the mental fears or<br />
anxiety surrounding the dental<br />
appointment. Dental analgesia does<br />
not seem to be as effective in<br />
permanent teeth because <strong>of</strong> the<br />
increased size and sensitivity <strong>of</strong> the<br />
dental pulp; however, it has been<br />
shown clinically to be effective for<br />
pain relief during crown cementations<br />
and decreased sensitivity<br />
during scaling appointments.<br />
Nausea and Gagging<br />
Application <strong>of</strong> the laser to the P6<br />
(Pericard 6) acupuncture point on<br />
the wrist can decrease or eliminate<br />
the nausea and gagging some<br />
patients feel during impressiontaking<br />
or X-ray procedures. As<br />
shown in Figure 7, the P6 is located<br />
on the underside <strong>of</strong> the wrist,<br />
approximately 1 inch from the<br />
distal palmar crease (approximately<br />
the width <strong>of</strong> the distal<br />
thumb phalanx). 23 For patients who<br />
are extremely nauseous or anxious,<br />
application to three acupuncture<br />
points in the wrist can be effective;<br />
Ross and Ross<br />
Figure 6: Promotion <strong>of</strong> analgesia via LLLT<br />
for primary tooth restorations<br />
H7, LU9, and P6 are the parasympathetic<br />
calming points and<br />
stimulation <strong>of</strong> these points can be<br />
very effective in reducing anxiety.<br />
A 1998 report in the British<br />
Journal <strong>of</strong> Anaesthesia investigated<br />
the effectiveness <strong>of</strong> laser irradiation<br />
to the P6 acupuncture point on postoperative<br />
vomiting. In the laser<br />
stimulation group, the incidence <strong>of</strong><br />
vomiting was significantly lower<br />
(25%) than in the placebo group<br />
(85%), and the patients were quite<br />
receptive to the painless procedure. 24<br />
Uptake and Elimination <strong>of</strong><br />
Anesthesia<br />
Based on the mechanisms <strong>of</strong> PBM<br />
therapy’s ability to increase blood<br />
circulation, 4 the author has found<br />
that there is an increase in uptake<br />
and elimination <strong>of</strong> anesthesia. PBM<br />
is applied to the submandibular<br />
lymph nodes and the site <strong>of</strong> injection<br />
after the injection and upon<br />
completion <strong>of</strong> the dental appointment,<br />
for uptake and elimination,<br />
respectively.<br />
Implant Placement<br />
Three papers indicate that PBM<br />
can reduce inflammation following<br />
implant placement, help speed the<br />
integration <strong>of</strong> the implant into the<br />
bone, and improve the quality <strong>of</strong><br />
the bone around the implant. A<br />
study using rabbits utilized Raman<br />
spectroscopy and electronic<br />
microscopy to investigate the effect<br />
<strong>of</strong> infrared light on the loading<br />
time <strong>of</strong> dental implants, and found<br />
Figure 7: A graphic diagram <strong>of</strong> three<br />
parasympathetic calming acupuncture<br />
points for reduction <strong>of</strong> nausea and<br />
gagging. Courtesy <strong>of</strong> Donald J. Coluzzi, DDS.<br />
Adapted from Atlas <strong>of</strong> acupuncture points. Point<br />
locations [Internet]. Published by<br />
www.AcupunctureProducts.com, 2007. [Cited<br />
2009 Dec 28.] 39 p. Available from:<br />
http://chiro.org/acupuncture/ABSTRACTS/<br />
Acupuncture_Points.pdf.<br />
a significantly greater amount <strong>of</strong><br />
mature bone, a better distribution<br />
<strong>of</strong> bone, and more organization <strong>of</strong><br />
bone after laser irradiation, when<br />
compared to the control group that<br />
received no laser irradiation. 25<br />
Another study used rats to<br />
examine the effect <strong>of</strong> laser therapy<br />
on bone and demonstrated that the<br />
laser group had an abbreviated<br />
initial inflammatory response and<br />
a rapid stimulation <strong>of</strong> bone matrix<br />
formation at 15 and 45 days. 26 An<br />
earlier rabbit study showed that<br />
bone healing is improved and those<br />
authors concluded that it is<br />
possible to reduce the loading time<br />
<strong>of</strong> implants in the mandible <strong>of</strong><br />
humans from 4 months to approximately<br />
2 months and 24 days, and<br />
in the maxilla, from 6 months to 4<br />
months and 6 days. 27<br />
Orthodontics<br />
Orthodontic treatments are lengthy<br />
and <strong>of</strong>ten painful for many patients.<br />
As mentioned previously, Gerbi et<br />
al. have shown that PBM irradiation<br />
on bone increases osteoblastic<br />
proliferation, collagen deposition
and bone ne<strong>of</strong>ormation when<br />
compared to non-irradiated bone. 11<br />
A 2008 study investigating the<br />
effect <strong>of</strong> laser therapy on orthodontic<br />
movement showed that the velocity<br />
<strong>of</strong> canine movement was significantly<br />
higher in the laser-irradiated<br />
teeth compared to teeth that<br />
received no irradiation. In addition,<br />
the pain intensity was also at a<br />
lower level in the lased group<br />
throughout the entire retraction<br />
period. 28 Histological observations<br />
made during another study on<br />
rabbits showed that both osteoblasts<br />
and osteoclasts remained more<br />
active on the lased side which could<br />
account for the accelerated movement.<br />
29 Finally, Turnhani et al.<br />
showed that a single application <strong>of</strong><br />
LLLT reduced the pain at 6 and 30<br />
hours after banding treatment. 30<br />
Periodontics<br />
The use <strong>of</strong> PBM as a treatment<br />
modality in periodontics is effective,<br />
either as a treatment method<br />
on its own or as an adjunct to the<br />
increasingly popular surgical<br />
lasers. A recent study investigated<br />
the gingival inflammatory response<br />
and dental plaque reduction<br />
following scaling and root planing<br />
combined with PBM in 60 patients.<br />
The authors found a significant<br />
decrease in the clinical indices<br />
(plaque, gingival, and sulcular<br />
bleeding), which they thought could<br />
be beneficial in the treatment <strong>of</strong><br />
chronic advanced periodontitis. 31<br />
Periodontal Surgery<br />
Healing after periodontal surgery<br />
is <strong>of</strong>ten a lengthy and painful<br />
process. PBM has been shown to<br />
stimulate fibroblasts for faster<br />
regeneration <strong>of</strong> s<strong>of</strong>t tissue, while<br />
providing analgesia and a modulation<br />
<strong>of</strong> the inflammatory chemicals<br />
that cause pain and discomfort. A<br />
2006 study showed a statistically<br />
significant decrease in pocket depth<br />
at 21 and 28 days post-surgery.<br />
Moreover, the laser-treated wounds<br />
presented with factors suggestive<br />
<strong>of</strong> better healing, including color,<br />
C L I N I C A L R E V I E W A N D C A S E R E P O R T S<br />
contour, and mucosa healing when<br />
compared with non-laser treated<br />
area, which served as a control. 32 To<br />
further exemplify these positive<br />
responses, a study by Ozcelik et al.<br />
demonstrated that LLLT enhanced<br />
epithelialization and improved<br />
wound healing after gingivectomy<br />
and gingivoplasty operations. 33<br />
Figure 8 shows an 830-nm PBM<br />
device being used to irradiate a<br />
closed incision.<br />
Endodontics<br />
PBM is effective for reducing pain<br />
and inflammation after endodontic<br />
treatments, for dentin hypersensitivity,<br />
and as a diagnostic tool for<br />
pulp hyperemia. 34<br />
Figure 8: LLLT irradiation after flap surgery<br />
Figure 9: Flowchart for endodontic diagnosis<br />
<strong>Laser</strong> Therapy as a Diagnostic Tool<br />
Occasionally, a patient will present<br />
to a dental practitioner with excessive<br />
tooth pain, the source <strong>of</strong> which<br />
cannot be accurately identified.<br />
Traditional diagnostic methods<br />
such as thermal or electrical<br />
stimuli <strong>of</strong>ten do not show any indication<br />
<strong>of</strong> the problem, making the<br />
diagnosis and treatment stressful<br />
for both the patient and the doctor.<br />
As stated previously, PBM irradiation<br />
increases circulation, thus a<br />
patient with a hyperemic pulp will<br />
feel a sharp pain when the laser is<br />
applied to a tooth. 35 Figure 9 shows<br />
a diagnostic outline that could be<br />
used in endodontics.<br />
Dentin Hypersensitivity<br />
A study by Marsilio et al. demonstrated<br />
that LLLT treatment <strong>of</strong><br />
dentin hypersensitivity in two<br />
different groups <strong>of</strong> patients was<br />
effective for 86% to 88% <strong>of</strong> all the<br />
participants. 36 Another study<br />
compared LLLT to topical fluoride<br />
varnish application for treatment<br />
<strong>of</strong> dentinal hypersensitivity and<br />
found that 86% <strong>of</strong> the laser irradiation<br />
group achieved absence <strong>of</strong> pain<br />
compared to 27% <strong>of</strong> the fluoride<br />
group. 37<br />
Ross and Ross<br />
J O U R N A L O F L A S E R D E N T I S T R Y | 2 011 V O L . 19 , N O . 3<br />
293
J O U R N A L O F L A S E R D E N T I S T R Y | 2 011 V O L . 19 , N O . 3<br />
294<br />
C L I N I C A L R E V I E W A N D C A S E R E P O R T S<br />
TMJ and Facial Pain<br />
When treating temporomandibular<br />
joint (TMJ) or facial pain, PBM is a<br />
useful tool to add to the therapeutic<br />
arsenal. From simple acute cases<br />
like facial pain after long appointments<br />
to chronic TMJ cases, laser<br />
therapy will help reduce pain and<br />
inflammation, and significantly<br />
resolve muscle trismus. In a systematic<br />
review <strong>of</strong> postoperative pain<br />
relief in patients after undergoing<br />
third molar extraction, a PBM irradiation<br />
was shown to be beneficial in<br />
reducing acute inflammatory pain. 13<br />
In a clinical study <strong>of</strong> 74 patients<br />
complaining <strong>of</strong> TMJ pain, 64% were<br />
pain-free or had improvement in<br />
comfort after 12 PBM sessions over<br />
a six-week period. 38 Pinheiro and<br />
colleagues analyzed the effect <strong>of</strong><br />
PBM on maxill<strong>of</strong>acial disorders by<br />
irradiating 141 female and 24 male<br />
patients twice a week for 6 weeks.<br />
At the end <strong>of</strong> the treatment 72% <strong>of</strong><br />
patients were aymptomatic and 15%<br />
had improved considerably. 39<br />
Neuropathic Pain<br />
Neuropathic facial pain is a debilitating<br />
condition for a patient that<br />
results in their living with excruciating<br />
pain or with a continuous<br />
dose <strong>of</strong> prescription analgesics. As<br />
stated above in the study by<br />
Bjordal et al., 13 PBM permits many<br />
patients to live a life free from<br />
discomfort or with less pain.<br />
C O N C LU S I O N<br />
Although PBM has been available<br />
to health care pr<strong>of</strong>essionals since<br />
the 1960s, low-level laser therapy<br />
did not really begin to gain popularity<br />
until the 1980s when<br />
controlled and randomized studies<br />
began to be published.<br />
In 2007, Karu reported that the<br />
effects <strong>of</strong> PBM are dependent on the<br />
initial redox status <strong>of</strong> a cell. If a cell<br />
is damaged, or in a reduced redox<br />
state, the cellular response to PBM<br />
will be stronger. Conversely, a cell<br />
which is at an optimal redox potential<br />
will have a weak or absent<br />
cellular response to PBM. 2 Thus,<br />
Ross and Ross<br />
cells that are damaged will respond<br />
to PBM better than cells that are<br />
healthy and functioning normally.<br />
However, there are precautions<br />
all laser users should take and areas<br />
to avoid treating when using PBM.<br />
Specifically, those include avoiding<br />
exposure to the thyroid gland, to<br />
pregnant women, and to radiation<br />
therapy patients. 40 Also important to<br />
note is that the laser will be ineffective<br />
if the patient has had a steroid<br />
injection in the last six months. 41 All<br />
laser users should consult their<br />
laser manufacturer for any questions<br />
regarding contraindications<br />
and appropriate treatment doses, as<br />
well as for instructions about safety<br />
eyewear for everyone within the<br />
nominal hazard zone <strong>of</strong> the beam.<br />
Photobiomodulation is an<br />
evolving technology. With every<br />
passing day, more is being discovered<br />
about the mechanisms <strong>of</strong> laser<br />
therapy, doses, treatment locations,<br />
and diseases in which a laser will<br />
have an effect. At our hands is a<br />
tool that can reduce pain, stimulate<br />
wound healing, and modulate the<br />
inflammatory response.<br />
Photobiomodulation can be used<br />
effectively in dental specialties to<br />
better manage treatments that are<br />
<strong>of</strong>ten deemed painful by patients,<br />
without prescribing pharmaceuticals<br />
that <strong>of</strong>ten have a number <strong>of</strong><br />
side effects. All healthcare pr<strong>of</strong>essionals,<br />
including dentists and<br />
dental specialists, should further<br />
investigate photobiomodulation to<br />
enhance their clinical treatments<br />
and outcomes.<br />
C A S E S T U DY : T M J PA I N<br />
Treating Dentist: Dr. Gerald Ross<br />
A 55-year-old patient presented with pain in the left temporomandibular<br />
joint and a limited ability to open the mouth. The<br />
computed tomography (CT) tomogram (R = right, SMV = submental<br />
vertex, L = left) showed degenerative joint disease (osteoarthritis) <strong>of</strong><br />
the left TMJ with no disc present.<br />
Six applications <strong>of</strong> the laser were performed over a three-week period,<br />
with treatment applications to the joint, joint capsule, and the lateral<br />
pterygoid muscle. This treatment resulted in the patient being pain-free<br />
for the last two years and with the ability to open the mouth wider.
C A S E S T U DY : N E U R O PAT H I C PA I N<br />
Treating Dentist: Dr. Gerald Ross<br />
A 61-year-old male patient presented with pain and felt it was coming<br />
from the lower left molar. The tooth was extracted and the socket healed<br />
uneventfully but the pain got worse. At that point, there were no other<br />
problems with teeth in that quadrant, however the pain was worsening<br />
and the patient was taking Tylenol ® No. 3 (30 mg) approximately 4 times<br />
per day, every day. <strong>Laser</strong> irradiation was applied to the trigeminal nerve,<br />
the molar site, and the trigeminal ganglion. After 1 application, the<br />
patient said he was no longer taking Tylenol No. 3 and took only 2 Advil ®<br />
at bedtime. Three days later a second application was done to the same<br />
site, and the patient reported as pain-free and no longer needing medication.<br />
The pain-free status has lasted for three months.<br />
A U T H O R B I O G R A P H I E S<br />
Dr. Gerald Ross has been practicing<br />
dentistry for more than 30 years in<br />
Tottenham, Ontario. He has been<br />
using surgical and low-level lasers<br />
clinically since 1990 and has<br />
lectured extensively in Canada, the<br />
United States, and internationally.<br />
He holds Advanced Pr<strong>of</strong>iciency<br />
status from the <strong>Academy</strong> <strong>of</strong> <strong>Laser</strong><br />
<strong>Dentistry</strong> and a fellowship from the<br />
American Society <strong>of</strong> <strong>Laser</strong> Medicine<br />
and Surgery. In 2008, Dr. Ross was<br />
asked to present a paper and chair<br />
the dental session at the World<br />
Association for <strong>Laser</strong> Therapy<br />
(WALT) meeting that was held in<br />
South Africa. He is currently a board<br />
member <strong>of</strong> the North American<br />
Association for <strong>Laser</strong> Therapy<br />
(NAALT) and is helping with<br />
numerous studies on photobiomodulation.<br />
Dr. Ross may be contacted by<br />
e-mail at ddsross@rogers.com.<br />
Alana Ross, BScH, graduated<br />
with an honors degree in Biomedical<br />
Science from the University <strong>of</strong><br />
Guelph in Ontario, Canada. In 2004,<br />
Alana c<strong>of</strong>ounded, and is currently<br />
the executive director <strong>of</strong>, <strong>Laser</strong> Light<br />
Canada, a company involved in the<br />
distribution <strong>of</strong> and education<br />
relating to low-level lasers and<br />
phototherapy equipment in North<br />
America. She has published<br />
numerous articles on low-level laser<br />
therapy and is presently overseeing<br />
several clinical studies. Currently,<br />
she is the chair <strong>of</strong> the NAALT 2010<br />
Annual Conference committee,<br />
C L I N I C A L R E V I E W A N D C A S E R E P O R T S<br />
serves on the NAALT Board <strong>of</strong><br />
Directors, and is a member <strong>of</strong> the<br />
NAALT membership committee.<br />
Disclosures: Dr. Ross is the president<br />
<strong>of</strong> <strong>Laser</strong> Light Canada, a company<br />
which is involved in the distribution<br />
and education related to low-level<br />
lasers in dentistry. Ms. Ross is the executive<br />
director <strong>of</strong> that company. None <strong>of</strong><br />
the manufacturers <strong>of</strong> the instruments<br />
sold by <strong>Laser</strong> Light Canada had any<br />
input into this article.<br />
R E F E R E N C E S<br />
1. Tafur J, Mills PJ. Low-intensity<br />
light therapy: Exploring the role <strong>of</strong><br />
redox mechanisms. Photomed <strong>Laser</strong><br />
Surg 2008;26(4):323-328.<br />
2. Karu TI. Low-power laser therapy.<br />
Chapter 48 in: Vo-Dinh T, editor.<br />
Biomedical photonics handbook.<br />
Boca Raton, Fla.: CRC Press,<br />
2003:48-1 – 48-25.<br />
3. Hamblin MR, Demidove TN.<br />
Mechanisms <strong>of</strong> low level light<br />
therapy. In: Hamblin MR, Waynant<br />
RW, Anders J, editors. Mechanisms<br />
for Low-Light Therapy, January 22<br />
and 24, 2006, San Jose, Calif. Proc.<br />
SPIE 6140. Bellingham, Wash.:<br />
SPIE – The International Society for<br />
Optical Engineering, 2006:614001-1<br />
614001-12.<br />
4. Mester E, Mester AF, Mester A. The<br />
biomedical effects <strong>of</strong> laser application.<br />
<strong>Laser</strong>s Surg Med<br />
1985;5(1):31-39.<br />
5. Stein A, Benayahu D, Maltz L, Oron<br />
U. Low-level laser irradiation<br />
promotes proliferation and differen-<br />
tiation <strong>of</strong> human osteoblasts in<br />
vitro. Photomed <strong>Laser</strong> Surg<br />
2005;23(2):161-166.<br />
6. Wakabayashi H, Hamba M,<br />
Mastumoto K, Tachibana H. Effect<br />
<strong>of</strong> irradiation by semiconductor<br />
laser on responses evoked in trigeminal<br />
caudal neurons by tooth pulp<br />
stimulation. <strong>Laser</strong>s Surg Med<br />
1993;13(6):605-610.<br />
7. Tunér J, Hode L. <strong>Laser</strong> therapy:<br />
Clinical practice and scientific background.<br />
Grängesberg, Sweden:<br />
Prima Books AB, 2002: Chapter 11<br />
The mechanisms (pp. 333-364).<br />
8. Hawkins D, Abrahamse H. Effect <strong>of</strong><br />
multiple exposures <strong>of</strong> low-level laser<br />
therapy on the cellular responses <strong>of</strong><br />
wounded human skin fibroblasts.<br />
Photomed <strong>Laser</strong> Surg<br />
2006;24(6):705-714.<br />
9. Baxter GD. Principles and practice <strong>of</strong><br />
laser treatment. Chapter 7 in: Baxter<br />
GD. Therapeutic lasers: Theory and<br />
practice. Edinburgh, UK: Churchhill<br />
Livingstone, 1994:187-220.<br />
10. Bjordal JM, Johnson MI, Iversen V,<br />
Aimbire F, Lopes-Martins RAB.<br />
Low-level laser therapy in acute<br />
pain: A systemic review <strong>of</strong> possible<br />
mechanisms <strong>of</strong> action and clinical<br />
effects in randomized placebocontrolled<br />
trials. Photomed <strong>Laser</strong><br />
Surg 2006;24(2):158-168.<br />
11. Gerbi MEM, Pinheiro ALB, Marzola<br />
C, Limeira Júnior Fde A, Ramalho<br />
LMP, Ponzi EAC, Soares AO,<br />
Carvalho LCB, Lima HV, Gonçalves<br />
TO. Assessment <strong>of</strong> bone repair associated<br />
with the use <strong>of</strong> organic bovine<br />
bone and membrane irradiated at<br />
830nm. Photomed <strong>Laser</strong> Surg<br />
2005;23(4):382-388.<br />
12. Aras MH, Güngörmü¸s M. The effect<br />
<strong>of</strong> low-level laser therapy on trismus<br />
and facial swelling following<br />
surgical extraction <strong>of</strong> a lower third<br />
molar. Photomed <strong>Laser</strong> Surg<br />
2009;27(1):21-24.<br />
13. Bjordal JM, Tuner J, Iversen VV,<br />
Frigo L, Gjerde K, Lopes-Martin<br />
RAB. A systematic review <strong>of</strong> postoperative<br />
pain relief by low level<br />
laser therapy (LLLT) after third<br />
molar extraction. In: The 1st<br />
meeting <strong>of</strong> the European Division <strong>of</strong><br />
the World Federation for <strong>Laser</strong><br />
<strong>Dentistry</strong>, April 26-27, 2007, Nice,<br />
Ross and Ross<br />
J O U R N A L O F L A S E R D E N T I S T R Y | 2 011 V O L . 19 , N O . 3<br />
295
J O U R N A L O F L A S E R D E N T I S T R Y | 2 011 V O L . 19 , N O . 3<br />
296<br />
C L I N I C A L R E V I E W A N D C A S E R E P O R T S<br />
France. <strong>Laser</strong>s Med Sci<br />
2007;22(4):303, abstract O50.<br />
14. Tunér J, Hode L. <strong>Laser</strong> therapy:<br />
Clinical practice and scientific background.<br />
Grängesberg, Sweden:<br />
Prima Books AB, 2002:204.<br />
15. Brugnera Junior A, Zanin FAA,<br />
Zanin T, Bissoli CZ, Carvalhosa AA,<br />
Castro PHS. Prevention and treatment<br />
<strong>of</strong> oral mucositis with diode<br />
laser 660 nm in patients with head<br />
and neck cancer submitted to radiotherapy<br />
and/or chemotherapy.<br />
Photomed <strong>Laser</strong> Surg<br />
2007;25(4):366-367, Abstract 143.<br />
16. Corti L, Chiarion-Sileni V, Aversa S,<br />
Ponzoni A, D’Arcais R, Pagnutti S,<br />
Fiore D, Sotti G. Treatment <strong>of</strong><br />
chemotherapy-induced oral<br />
mucositis with light-emitting diode.<br />
Photomed <strong>Laser</strong> Surg<br />
2006;24(2):207-213.<br />
17. Schindl A, Neumann R. Low-intensity<br />
laser therapy is an effective<br />
treatment for recurrent herpes<br />
simplex infection. Results from a<br />
randomized double-blind placebocontrolled<br />
study. J Invest Dermatol<br />
1999;113(2):221-223.<br />
18. Marei MK, Abdel-Meguid SH,<br />
Mokhtar SA, Rizk SA. Effect <strong>of</strong> lowenergy<br />
laser application in the<br />
treatment <strong>of</strong> denture-induced<br />
mucosal lesions. J Prosthet Dent<br />
1997;77(3):256-264.<br />
19. Tunér J, Hode L. <strong>Laser</strong> therapy:<br />
Clinical practice and scientific background.<br />
Grängesberg, Sweden:<br />
Prima Books AB, 2002:220.<br />
20. Tunér J, Hode L. <strong>Laser</strong> therapy:<br />
Clinical practice and scientific background.<br />
Grängesberg, Sweden:<br />
Prima Books AB, 2002:162.<br />
21. Hagiwara S, Iwasaka H, Hasegawa<br />
A, Noguchi T. Pre-irradiation <strong>of</strong><br />
blood by gallium aluminum arsenide<br />
(830 nm) low-level laser enhances<br />
peripheral endogenous opioid analgesia<br />
in rats. Anesth Analg<br />
2008;107(3):1058-1063.<br />
22. Wakabayashi H, Hamba M,<br />
Matsumoto K, Tachibana H. Effect<br />
<strong>of</strong> irradiation by semiconductor<br />
laser on responses evoked in trigeminal<br />
caudal neurons by tooth pulp<br />
stimulation. <strong>Laser</strong>s Surg Med<br />
1993;13(6):605-610.<br />
23. Kotlow L. <strong>Laser</strong>s and pediatric dental<br />
care. Gen Dent 2008;56(7): 618-627.<br />
Ross and Ross<br />
24. Schlager A, Offer T, Baldissera I.<br />
<strong>Laser</strong> stimulation <strong>of</strong> acupuncture<br />
point P6 reduces postoperative<br />
vomiting in children undergoing<br />
strabismus surgery. Br J Anaesth<br />
1998;81(4):529-532.<br />
25. Lopes CB, Pinheiro ALB, Sathaiah S,<br />
Da Silva NS, Salgado MAC. Infrared<br />
laser photobiomodulation (λ 830 nm)<br />
on bone tissue around dental<br />
implants: A Raman spectroscopy and<br />
scanning electronic microscopy study<br />
in rabbits. Photomed <strong>Laser</strong> Surg<br />
2007;25(2):95-101.<br />
26. Pretel H, Lizarelli RFZ, Ramalho<br />
LTO. Effect <strong>of</strong> low-level laser<br />
therapy on bone repair: Histological<br />
study in rats. <strong>Laser</strong>s Surg Med<br />
2007;39(10):788-796.<br />
27. Lopes CB, Pinheiro ALB, Sathaiah<br />
S, Duarte J, Martins MC. Infrared<br />
laser light reduces loading time <strong>of</strong><br />
dental implants: A Raman spectroscopic<br />
study. Photomed <strong>Laser</strong> Surg<br />
2005;23(1):27-31.<br />
28. Youssef M, Ashkar S, Hamade E,<br />
Gutknecht N, Lampert F, Mir M.<br />
The effect <strong>of</strong> low-level laser therapy<br />
during orthodontic movement: A<br />
preliminary study. <strong>Laser</strong>s Med Sci<br />
2008;23(1):27-33.<br />
29. Sun X, Zhu X, Xu C, Ye N, Zhu H.<br />
[Effects <strong>of</strong> low energy laser on tooth<br />
movement and remodeling <strong>of</strong> alveolar<br />
bone in rabbits.] Hua Xi Kou Qiang Yi<br />
Xue Za Zhi [West China J Stomatol]<br />
2001;19(5):290-293. Chinese.<br />
30. Turhani D, Scheriau M, Kapral D,<br />
Benesch T, Jonke E, Bantleon HP.<br />
Pain relief by single low-level laser<br />
irradiation in orthodontic patients<br />
undergoing fixed appliance therapy.<br />
Am J Orthod Dent<strong>of</strong>acial Orthop<br />
2006;130(3):371-377.<br />
31. Angelov N, Pesevska S, Nakova M,<br />
Gjorgoski I, Ivanovski K, Angelova<br />
D, H<strong>of</strong>fmann O, Andreana S.<br />
Periodontal treatment with lowlevel<br />
diode laser: Clinical findings.<br />
Gen Dent 2009;57(5):510-513.<br />
32. Amorim JCF, de Sousa GR, de<br />
Barros Silveira L, Prates RA, Pinotti<br />
M, Ribeiro MS. Clinical study <strong>of</strong> the<br />
gingiva healing after gingivectomy<br />
and low-level laser therapy.<br />
Photomed <strong>Laser</strong> Surg<br />
2006;24(5):588-594.<br />
33. Ozcelik O, Cenk Haytac M, Kunin A,<br />
Seydaoglu G. Improved wound<br />
healing by low-level laser irradiation<br />
after gingivectomy operations:<br />
A controlled pilot study. J Clin<br />
Periodontol 2008;35(3):250-254.<br />
34. Kert J, Rose L. Clinical laser<br />
therapy: Low level laser therapy.<br />
Reiss E, translator. Veksoe,<br />
Denmark: Scandinavian Medical<br />
<strong>Laser</strong> Technology, 1989:111-119.<br />
35. Kutvolgyi I. Low level laser therapy<br />
as a diagnostic tool in dentistry.<br />
<strong>Laser</strong> Ther 1998;10:79-82.<br />
36. Marsilio AL, Rodrigues JR, Borges<br />
AB. Effect <strong>of</strong> the clinical application<br />
<strong>of</strong> the GaAlAs laser in the treatment<br />
<strong>of</strong> dentine hypersensitivity. J<br />
Clin <strong>Laser</strong> Med Surg<br />
2003;21(5):291-296.<br />
37. Pesevska S, Nakova M, Ivanovski K,<br />
Angelov N, Kesic L, Obradovic R,<br />
Mindova S, Nares S. Dentinal<br />
hypersensitivity following scaling<br />
and root planing: Comparison <strong>of</strong><br />
low-level laser and topical fluoride<br />
treatment. <strong>Laser</strong>s Med Sci. Epub<br />
2009 Jun 1. DOI 10.1007/s10103-<br />
009-0685-0.<br />
38. Carvalho CM, de Lacerda JA, Dos<br />
Santos Neto FP, Cangussu MCT,<br />
Marques AMC, Pinheiro ALB.<br />
Wavelength effect in temporomandibular<br />
joint pain: A clinical<br />
experience. <strong>Laser</strong>s Med Sci. Epub<br />
2009 Jun 30. DOI 10.1007/s10103-<br />
009-0695-y.<br />
39. Pinheiro ALB, Cavalcanti ET,<br />
Pinheiro TITNR, Alves MJPC,<br />
Manzi CTA. Low-level laser therapy<br />
in the management <strong>of</strong> disorders <strong>of</strong><br />
the maxill<strong>of</strong>acial region. J Clin<br />
<strong>Laser</strong> Med Surg 1997;15(4):181-183.<br />
40. Tunér J, Hode L. <strong>Laser</strong> therapy:<br />
Clinical practice and scientific background.<br />
Grängesberg, Sweden:<br />
Prima Books AB, 2002: Chapter 8<br />
Contraindications (pp 285-289).<br />
41. Lopes-Martins RAB, Albertini R,<br />
Lopes-Martins PSL, de Carvalho<br />
FAS, Neto HCCF, Iversen VV,<br />
Bjordal JM. Steroid receptor antagonist<br />
mifepristone inhibits the<br />
anti-inflammatory effects <strong>of</strong><br />
photoradiation. Photomed <strong>Laser</strong><br />
Surg 2006;24(2):197-201.<br />
Editor’s Note: This article first<br />
appeared in J <strong>Laser</strong> Dent<br />
2009;17(3):117-124. nn
C L I N I C A L E X P E R I E N C E<br />
Using Photobiomodulation on a Severe<br />
Parkinson’s Patient to Enable Extractions, Root<br />
Canal Treatment, and Partial Denture Fabrication<br />
Mel A. Burchman, DDS, Langhorne, Pennsylvania<br />
J <strong>Laser</strong> Dent 2011;19(3):297-300<br />
Mel A. Burchman, DDS<br />
I N T R O D U C T I O N<br />
The objective <strong>of</strong> this presentation is<br />
to demonstrate how low-level laser<br />
stimulation <strong>of</strong> acupuncture points<br />
may be used to temporarily relieve<br />
the tremors <strong>of</strong> Parkinsonism,<br />
thereby enabling various dental<br />
treatments.<br />
Acupuncture, as defined by the<br />
American <strong>Academy</strong> <strong>of</strong> Medical<br />
Acupuncture (AAMA), may be<br />
defined as “a method <strong>of</strong> encouraging<br />
the body to promote natural<br />
healing and to improve functioning.<br />
This is done by inserting needles<br />
and applying heat or electrical<br />
stimulation at very precise<br />
acupuncture points.” 1 <strong>Laser</strong>s and<br />
ultrasound are other means <strong>of</strong><br />
stimulating the acupoints.<br />
Dorland’s Illustrated Medical<br />
Dictionary states: “According to<br />
traditional theory, the goal <strong>of</strong><br />
acupuncture is the prevention and<br />
treatment <strong>of</strong> disease by correcting<br />
disturbances in the flow <strong>of</strong> qi (“life<br />
energy”); biologically, the effects <strong>of</strong><br />
acupuncture may result from the<br />
release <strong>of</strong> neurotransmitters such<br />
as endorphins and serotonin.” 2<br />
The AAMA further explains how<br />
acupuncture works: “The classical<br />
Chinese explanation is that chan-<br />
nels <strong>of</strong> energy run in regular<br />
patterns through the body and over<br />
its surface. These energy channels,<br />
called meridians, are like rivers<br />
flowing through the body to irrigate<br />
and nourish the tissues. An<br />
obstruction in the movement <strong>of</strong><br />
these energy rivers is like a dam<br />
that backs up in others. The meridians<br />
can be influenced by<br />
stimulating the acupuncture<br />
points.” 1<br />
How light may be used to stimulate<br />
such points is described by<br />
Vargas, who reported that Russian<br />
researchers from the Institute for<br />
Clinical and Experimental<br />
Medicine showed that “only certain<br />
areas <strong>of</strong> the body were able to<br />
transfer light beneath the surface,<br />
and these areas corresponded to<br />
acupuncture points. Furthermore,<br />
the light was conducted within the<br />
body along the acupuncture meridians.<br />
It appears that the meridians<br />
are a light transferal system within<br />
the body somewhat like optical<br />
fiber.” 3<br />
Instead <strong>of</strong> using needles, heat,<br />
electrical current, or ultrasound to<br />
stimulate certain acupuncture<br />
points, the present case describes a<br />
method <strong>of</strong> photobiomodulation<br />
using a combination <strong>of</strong> low-level<br />
laser and light-emitting diode<br />
instruments to enable dental treatment<br />
<strong>of</strong> a patient with severe<br />
Parkinson’s and positively affect<br />
outcome.<br />
So what do we know about<br />
Parkinson’s disease? It is a degenerative<br />
disorder <strong>of</strong> the central<br />
nervous system that impairs motor<br />
skills, speech, and other functions.<br />
Primary symptoms, including<br />
tremor <strong>of</strong> resting muscles, rigidity,<br />
slowness <strong>of</strong> movement, and<br />
impaired balance, are the result <strong>of</strong><br />
decreased stimulation <strong>of</strong> the motor<br />
cortex by the basal ganglia,<br />
normally caused by the insufficient<br />
formation and action <strong>of</strong> dopamine.<br />
Hence, Parkinson’s disease is<br />
related to low levels <strong>of</strong> dopamine in<br />
certain parts <strong>of</strong> the brain. An<br />
increase in dopamine concentrations<br />
in the brain is thought to<br />
improve nerve conduction and to<br />
assist in lessening the movement<br />
disorders in patients with this<br />
condition.<br />
Dopamine is a neurohormone<br />
released by the hypothalamus. Its<br />
main function is to inhibit the<br />
release <strong>of</strong> prolactin from the anterior<br />
lobe <strong>of</strong> the pituitary gland.<br />
Dopamine is a catecholamine and<br />
an important neurotransmitter<br />
(messenger) in the brain. Begley<br />
states that dopamine is “the precise<br />
chemical that is scarce in the brains<br />
<strong>of</strong> Parkinson’s patients. Dopamine<br />
… calms the chaotic neuronal firing<br />
that causes the spasms and rigidity<br />
<strong>of</strong> Parkinson’s … ” 4-5<br />
The hypothalamus contains a<br />
number <strong>of</strong> small nuclei with a<br />
variety <strong>of</strong> functions. The most<br />
important <strong>of</strong> these is to link the<br />
nervous system to the endocrine<br />
system via the pituitary gland. The<br />
hypothalamus is located below the<br />
thalamus, just above the brain<br />
stem. Important to understanding<br />
this case is the fact that the hypothalamus<br />
is stimulated by light.<br />
Choice <strong>of</strong> which light-emitting<br />
instrument to use is guided by<br />
Burchman<br />
J O U R N A L O F L A S E R D E N T I S T R Y | 2 011 V O L . 19 , N O . 3<br />
297
J O U R N A L O F L A S E R D E N T I S T R Y | 2 011 V O L . 19 , N O . 3<br />
298<br />
C L I N I C A L E X P E R I E N C E<br />
depth <strong>of</strong> penetration <strong>of</strong> wavelength<br />
and site <strong>of</strong> the acupuncture point.<br />
As Naeser points out, the 600-700<br />
nm wavelengths have a shallow<br />
penetration, approximately 0.8<br />
mm, and are used on acupuncture<br />
points on the hand, foot, face, or<br />
sometimes the ear. Deeper-penetrating<br />
(up to 1 inch) wavelengths<br />
<strong>of</strong> 800 to 1000 nm are used to treat<br />
points on the limbs or back. 6<br />
C L I N I C A L C A S E<br />
This presentation represents one <strong>of</strong><br />
the most rewarding experiences I<br />
have had in 35 years <strong>of</strong> dentistry.<br />
Al, age 82 years, is one <strong>of</strong> my<br />
delightful 30-year patients. He<br />
used to be an auto worker, but now<br />
has such severe Parkinson’s that he<br />
can barely sit in the chair and read<br />
a magazine without dropping it. He<br />
walks with a tripod cane. The<br />
extent <strong>of</strong> his condition is evident in<br />
the number and frequency <strong>of</strong> his<br />
Parkinson’s medications: he takes<br />
three oral prescriptions (Requip ,<br />
Sinemet , and Stalevo ® ) for a total<br />
<strong>of</strong> 11 tablets daily. Al is also a<br />
cancer patient, but that is irrelevant<br />
to the case. He wears a full<br />
upper denture that needs a considerable<br />
amount <strong>of</strong> adhesive to stay<br />
in place due to his severe tremors;<br />
it is always coming out.<br />
Al came in several weeks previously<br />
as he had broken two lower<br />
teeth (#20 and #21). I referred him<br />
to an oral surgeon for general anesthesia<br />
for their extraction, because<br />
there was no way I thought I would<br />
be able to extract them due to his<br />
severe tremors. He came back a<br />
couple weeks later complaining <strong>of</strong><br />
something sticking up from the<br />
area and asked me to examine the<br />
site. Unfortunately, part <strong>of</strong> the root<br />
from tooth #20 was still present<br />
and I told him to return to the oral<br />
surgeon to get it taken care <strong>of</strong>, but<br />
he did not want to go back there.<br />
He wanted me to handle it and I<br />
did, but it was really difficult due<br />
to his constant movement. He<br />
needed something done so that he<br />
could eat and in my opinion extrac-<br />
Burchman<br />
Figure 1: Preoperative radiograph<br />
showing the only remaining teeth, #24<br />
through #27<br />
tions and a full lower denture was<br />
equivalent to a death sentence for<br />
him. He could barely function with<br />
a full upper; I couldn’t imagine him<br />
trying to eat with a full lower with<br />
his severe Parkinson’s. We decided<br />
to extract teeth #24 and #26 (due to<br />
his limited finances), provide root<br />
canal treatment for #25 and #27,<br />
and make a partial lower denture.<br />
The preoperative film (Figure 1)<br />
shows his only remaining lower<br />
teeth, #24 through #27.<br />
I decided to work the case at a<br />
pace that Al could handle. At each<br />
visit I would decide what to treat<br />
based on what it appeared he could<br />
handle. On this particular visit Al<br />
was having a horrible day. After my<br />
assistant seated him she came to<br />
get me from another treatment<br />
room. He had already cancelled<br />
several appointments because <strong>of</strong><br />
how poorly he was feeling. He was<br />
kicking his legs, swinging his arms,<br />
and jerking his head. I looked at<br />
him and remembered reading the<br />
section on Parkinson’s in my<br />
manual on low-level laser therapy<br />
(LLLT). 7 It listed three acupuncture<br />
points that were useful in calming<br />
these patients: Gallbladder #20,<br />
Bladder #60, and Bladder #55.<br />
(Editor’s Note: For illustrations <strong>of</strong><br />
meridians and acupuncture points,<br />
readers may consult standard<br />
acupuncture references. One such<br />
source is the Atlas <strong>of</strong> Acupuncture<br />
Points. Point Locations. 2007,<br />
published by<br />
www.AcupunctureProducts.com and<br />
available online as a PDF from<br />
www.archive.org/details/Atlas_<strong>of</strong>_<br />
Acupuncture_Point_Locations.<br />
Accessed February 5, 2012.)<br />
I decided to use a photobiomodulation<br />
device (Q1000, 2035, Inc.,<br />
Rapid City, S.D.) on Gallbladder<br />
#20 because it is located at the<br />
cervical atlas at the base <strong>of</strong> the<br />
skull, the most stable part <strong>of</strong> his<br />
body at the time. The other two<br />
points are on the leg and the way<br />
that Al was kicking it could be<br />
dangerous to hold the instrument<br />
in place. Specifically, the device<br />
consists <strong>of</strong> a light-emitting diode<br />
(LED) cluster with 8 LEDs and 12<br />
diodes that emit wavelengths<br />
between 470 and 940 mm. The unit<br />
also comes with a separate 660-nm<br />
diode laser probe and an 808-nm<br />
diode laser probe. Al’s tremors were<br />
so severe that I used the 660-nm<br />
probe, power output 30 mW, for 3<br />
minutes on both sides <strong>of</strong> his<br />
cervical atlas (Figure 2).<br />
The calming effects after treatment<br />
were striking. Al’s tremors<br />
stopped within 2 to 3 minutes after<br />
laser irradiation <strong>of</strong> the acupuncture<br />
point. He was amazed. Not only<br />
were we able to do dental work, but<br />
Al was able to walk to meet his<br />
wife in the waiting room and to the<br />
parking lot without using his cane.<br />
His wife was similarly amazed.<br />
When I called the next day to see<br />
how Al was doing, she said, “He<br />
was calmer for 2 to 3 hours afterward.”<br />
When Al would come in for<br />
subsequent dental treatment my<br />
assistants would apply LLLT to<br />
Figure 2: Irradiation <strong>of</strong> acupuncture point<br />
Gallbladder #20 at the cervical atlas
Gallbladder #20 as soon as he was<br />
seated. This enabled us to perform<br />
the scheduled treatments (extraction,<br />
endodontics, and partial<br />
denture fabrication) during separate<br />
appointments.<br />
Among LLLT’s reported beneficial<br />
effects are: (1) Stimulating cell<br />
energy production, which aids in<br />
the restoration <strong>of</strong> normal cell<br />
morphology and function; (2)<br />
Increasing lymphatic flow, which<br />
decreases edema and swelling; (3)<br />
Increasing endorphin release,<br />
reducing conduction <strong>of</strong> C-Fibers,<br />
and decreasing release <strong>of</strong> histamine,<br />
bradykinins, and<br />
acetylcholine to reduce the sensation<br />
<strong>of</strong> postoperative pain; (4)<br />
Stimulating osteoblasts, odontoblasts,<br />
and fibroblasts to promote<br />
the growth <strong>of</strong> bone, dentin, and s<strong>of</strong>t<br />
tissue; (5) Stimulating nerve regeneration;<br />
(6) Increasing neutrophil<br />
and macrophage activity. The<br />
regime that I use takes advantage<br />
<strong>of</strong> all <strong>of</strong> these benefits. I predose or<br />
preload the area to be worked on to<br />
stimulate these wanted effects, and<br />
then use photobiomodulation again<br />
postoperatively to enhance these<br />
effects.<br />
The regime I use for extractions<br />
is as follows: For a maxillary tooth<br />
I place the LED instrument (total<br />
maximum power <strong>of</strong> 42 mW) for a<br />
full 3-minute cycle on the outside <strong>of</strong><br />
face by the tooth to be extracted.<br />
For a mandibular tooth I place it<br />
for half a cycle outside the face and<br />
half a cycle submandibular <strong>of</strong> the<br />
tooth to be extracted. I repeat this<br />
application postoperatively,<br />
followed by a full cycle using my<br />
660-nm probe on top <strong>of</strong> the extraction<br />
socket.<br />
The protocol I follow for<br />
endodontic treatment is as follows:<br />
For a tooth without a crown, I<br />
apply the LED device for a full<br />
cycle <strong>of</strong> 3 minutes outside the face,<br />
and then the 660-nm probe for 1<br />
minute on the buccal and lingual<br />
apex and on the occlusal aspect<br />
prior to beginning the endodontic<br />
treatment. I then apply the 660-nm<br />
Figure 3: Postoperative radiograph after<br />
root canal treatment and extraction<br />
probe to the cleaned and shaped<br />
canal for a full cycle just prior to<br />
placing the fillers. If there is a<br />
large radiolucency I will also use<br />
the 808-nm probe, 300 mW power<br />
output, for 1 minute at the apex <strong>of</strong><br />
the tooth after the filler has been<br />
placed. If the tooth has a crown,<br />
after application <strong>of</strong> the LED cycle I<br />
use the 660-nm probe for 1-1/2<br />
minutes at the buccal and lingual<br />
apices. Since I have been using this<br />
regime, I have had to provide fewer<br />
injections due to the analgesia<br />
induced from the LLLT. I do almost<br />
all my endodontics in one visit and<br />
my patients report having no postoperative<br />
pain.<br />
Figure 3 shows the postoperative<br />
results <strong>of</strong> extraction and root<br />
canal treatment. I made Al a 3-unit<br />
bridge from #25-27 (Figure 4) to<br />
increase the stability <strong>of</strong> #25 and<br />
#27, but did not charge him for<br />
#26. Figure 5 depicts the placement<br />
<strong>of</strong> Al’s 3-unit bridge and partial<br />
lower denture.<br />
Al’s dental prognosis is excellent.<br />
He was thrilled that we were<br />
able to complete the procedures,<br />
and that I was able to keep seeing<br />
him as a patient. Prior to this I had<br />
referred him out for extractions to<br />
be performed under general anesthesia,<br />
and he did not like that<br />
experience.<br />
I don’t have a definitive answer<br />
as to why photobiomodulation<br />
C L I N I C A L E X P E R I E N C E<br />
Figure 4: View <strong>of</strong> 3-unit bridge (#25-27)<br />
in place<br />
Figure 5: View <strong>of</strong> 3-unit bridge and<br />
partial lower denture in place<br />
worked so effectively in calming Al’s<br />
tremors. Did it cause the production<br />
<strong>of</strong> dopamine? Did it stimulate mitochondria<br />
to produce more adenosine<br />
triphosphate (ATP)? Did it improve<br />
neurotransmission through the<br />
hypothalamus? Or was it due to<br />
some other reason?<br />
Besides the three acupuncture<br />
points mentioned above, I have also<br />
found that Small Intestine<br />
Meridian #3, located on the<br />
knuckle <strong>of</strong> the little finger (in the<br />
depression proximal to the head <strong>of</strong><br />
the fifth metacarpal bone), is also<br />
very effective for patients with<br />
Parkinson’s experiencing severe<br />
spasms but whose arms are stable.<br />
I place the 660-nm probe on the<br />
side (left or right hand) that corresponds<br />
to the side <strong>of</strong> the upcoming<br />
dental treatment. If I get the<br />
desired calming effect, then I do<br />
not irradiate the other hand, but<br />
occasionally I will apply the probe<br />
on the other hand as needed. The<br />
calming effects after a 3-minute<br />
cycle with the 660-nm probe are<br />
extraordinary.<br />
Burchman<br />
J O U R N A L O F L A S E R D E N T I S T R Y | 2 011 V O L . 19 , N O . 3<br />
299
J O U R N A L O F L A S E R D E N T I S T R Y | 2 011 V O L . 19 , N O . 3<br />
300<br />
C L I N I C A L E X P E R I E N C E<br />
Editor’s Note: This article<br />
describes <strong>of</strong>f-label use <strong>of</strong> the Q1000<br />
device, which has received U.S. FDA<br />
marketing clearance for providing<br />
temporary relief <strong>of</strong> pain associated<br />
with osteoarthritis <strong>of</strong> the hand<br />
which has been diagnosed by a<br />
physician or other licensed medical<br />
pr<strong>of</strong>essional.<br />
A U T H O R B I O G R A P H Y<br />
Dr. Mel Burchman has maintained<br />
a private practice in Bucks County,<br />
Pennsylvania for 35 years. He has<br />
received ALD Standard Pr<strong>of</strong>iciency<br />
certification in Nd:YAG, diode, and<br />
Er:YAG laser wavelengths. He has<br />
received Associate Fellowship from<br />
the World Clinical <strong>Laser</strong> Institute<br />
(WCLI) in Er,Cr:YSGG. In addition,<br />
Dr. Burchman received Advanced<br />
Pr<strong>of</strong>iciency in Nd:YAG in 2001 and<br />
Burchman<br />
became an ALD Certified <strong>Laser</strong><br />
Educator in 2005. In 2008, he<br />
received a Master in <strong>Laser</strong><br />
<strong>Dentistry</strong> from ALD. Dr. Burchman<br />
may be contacted by e-mail at<br />
MEL712A@aol.com.<br />
Disclosure: Dr. Burchman has no<br />
commercial or financial interest relative<br />
to this presentation.<br />
R E F E R E N C E S<br />
1. “Doctor, what’s this acupuncture all<br />
about?” A brief explanation.<br />
American <strong>Academy</strong> <strong>of</strong> Medical<br />
Acupuncture website.<br />
www.medicalacupuncture.org/acu_info<br />
/articles/aboutacupuncture.html. No<br />
date. Accessed February 5, 2012.<br />
2. Dorland’s illustrated medical<br />
dictionary. 31st ed. Philadelphia,<br />
PA: Saunders, 2007:25.<br />
3. Vargas JT. Low-level laser acupuncture.<br />
Med Accupunct<br />
2005;16(2):38-41.<br />
4. Begley S. Hooked on a feeling. This<br />
is your brain on a placebo. In<br />
Newsweek magazine. The Daily<br />
Beast website. May 20, 2009.<br />
www.thedailybeast.com/newsweek/<br />
2009/05/20/hooked-on-a-feeling.html.<br />
Accessed February 5, 2012.<br />
5. Begley S. Train your mind, change<br />
your brain: How a new science<br />
reveals our extraordinary potential<br />
to transform ourselves. New York,<br />
NY: Ballantine Books, 2007.<br />
6. Naeser MA. Some general information<br />
on painless, non-invasive,<br />
low-level laser acupuncture.<br />
Acupuncture.com website.<br />
www.acupuncture.com/education/<br />
theory/laseracu.htm. No date.<br />
Accessed February 5, 2012.<br />
7. Lytle L. Low level laser user’s<br />
manual. 1st ed. Portland, OR:<br />
Wowapi, Inc., 2003. nn
Signs <strong>of</strong> Change<br />
Raminta Mastis, DDS, FAGD, MALD, St. Clair Shores, Michigan<br />
J <strong>Laser</strong> Dent 2011;19(3):301-302<br />
Raminta Mastis, DDS, <strong>Laser</strong> Safety<br />
Committee Chairwoman<br />
The proper display <strong>of</strong> signs is an<br />
essential element in implementing<br />
a successful laser safety program in<br />
the workplace. Since many lasers,<br />
when active, are invisible, they<br />
pose a potentially hazardous environment.<br />
Even small amounts <strong>of</strong><br />
laser light can cause permanent<br />
eye injuries or skin burns. Signs<br />
serve an important function in<br />
identifying hazards, and in giving<br />
directions for appropriate precautions,<br />
warnings, and protection. The<br />
purpose <strong>of</strong> this article is to provide<br />
guidelines specified in ANSI<br />
Z136.1-2007 American National<br />
Standard for Safe Use <strong>of</strong> <strong>Laser</strong>s for<br />
signs in order to properly warn<br />
people <strong>of</strong> the potential laser-related<br />
health hazards in your workplace.<br />
In a dental laser treatment<br />
setting there are two main types <strong>of</strong><br />
signs: equipment labels and area<br />
warning signs. Equipment labeling<br />
is primarily the responsibility <strong>of</strong><br />
the manufacturer. Dental lasers<br />
sold in the USA must achieve U.S.<br />
Food and Drug Administration<br />
(FDA) marketing clearance, which<br />
includes the permanent affixing <strong>of</strong><br />
various warning and information<br />
labels on the laser equipment itself.<br />
The operator and <strong>Laser</strong> Safety<br />
Officer (LSO) should be aware <strong>of</strong><br />
these and understand their meanings.<br />
These labels identify<br />
protective features and potential<br />
hazards if the laser is tampered<br />
with. Equipment labels also iden-<br />
tify the class <strong>of</strong> laser and degree <strong>of</strong><br />
hazards. The LSO should inspect<br />
these labels to assure that they are<br />
intact, legible, securely affixed, and<br />
document such inspections in a<br />
logbook or an annual checklist. If a<br />
label becomes illegible or comes <strong>of</strong>f,<br />
the manufacturer should be<br />
contacted for a replacement label.<br />
Since area warning signs are<br />
used to indicate a change <strong>of</strong> environment,<br />
they demand more daily<br />
attention in order to serve the<br />
purpose <strong>of</strong> safety. Area warning<br />
signs are the responsibility <strong>of</strong> the<br />
LSO and/or the delegated team<br />
members. The appropriate uses for<br />
these signs <strong>of</strong> change are addressed<br />
in ANSI 136.1-2007, Section 4.7.<br />
Area warning signs are used to<br />
control areas where lasers are being<br />
used. In general, signs for Class 2<br />
and 2M lasers will have the signal<br />
word “Caution,” and will typically be<br />
yellow. Signs for Class 3R, 3B, and 4<br />
lasers will use the signal word<br />
“Danger,” and will be in red. Most<br />
manufacturers provide a preprinted<br />
warning sign with the pertinent<br />
information (type <strong>of</strong> laser, emitted<br />
wavelength, pulse duration,<br />
maximum output, laser class, and<br />
special precautionary instructions<br />
and protective actions) for use by the<br />
operator. Additional signs can be<br />
requested from the manufacturer,<br />
photocopied, or downloaded from the<br />
Internet (paper copy, which you may<br />
want to laminate), or purchased<br />
from various companies or Web sites<br />
that <strong>of</strong>fer laser safety signs (usually<br />
plastic), such as <strong>Laser</strong> Institute <strong>of</strong><br />
America (www.lia.org).<br />
The regulations require that<br />
these area warning signs be<br />
conspicuously displayed before the<br />
entry into the controlled area,<br />
which is determined by the specific<br />
laser’s Nominal Hazard Zone<br />
(NHZ). The regulations also require<br />
L A S E R S A F E T Y<br />
that these signs be covered or<br />
removed when the laser is effectively<br />
taken out <strong>of</strong> operation (which<br />
should be interpreted as laser shutdown<br />
and not just placed in<br />
standby mode). Most dental lasers<br />
are designed to be portable,<br />
meaning that they can be used in<br />
several treatment areas throughout<br />
the day. If the laser is moved to<br />
different locations (i.e., multiple<br />
treatment areas), the signs should<br />
be changed to clearly indicate<br />
where and when a laser is in use in<br />
order to appropriately warn at all<br />
entries into the NHZ.<br />
Accidents happen, <strong>of</strong>ten when<br />
they are least expected. A trained<br />
and experienced skydiver is more<br />
likely to sprain his ankle by tripping<br />
on a rug or a stair in his own<br />
home than from jumping from a<br />
perfectly good airplane over a mile<br />
<strong>of</strong>f the ground, while being<br />
suspended by a strip <strong>of</strong> fabric (parachute).<br />
The same analogy can be<br />
applied in the dental <strong>of</strong>fice. Be<br />
prepared for the unexpected. Be<br />
alert to your environment. Be aware<br />
<strong>of</strong> the stray traffic near the NHZ.<br />
Traffic control within hazard<br />
zones should be managed with<br />
clear and standard operating procedures.<br />
It is the responsibility <strong>of</strong> the<br />
staff to manage stray traffic (such<br />
as a concerned parent “peeking<br />
in”). The staff should also be<br />
trained to recognize that interruptions<br />
for “just a quick question” are<br />
inappropriate during laser procedures.<br />
It is recommended that<br />
other forms <strong>of</strong> inter-<strong>of</strong>fice communications,<br />
such as text-messaging<br />
systems, be included in the standard<br />
operating procedures.<br />
In addition to the appropriate<br />
display <strong>of</strong> Caution and Danger<br />
signs, there is a third type <strong>of</strong> sign<br />
defined by ANSI to identify a<br />
Temporary <strong>Laser</strong> Controlled Area.<br />
Mastis<br />
J O U R N A L O F L A S E R D E N T I S T R Y | 2 011 V O L . 19 , N O . 3<br />
301
J O U R N A L O F L A S E R D E N T I S T R Y | 2 011 V O L . 19 , N O . 3<br />
302<br />
L A S E R S A F E T Y<br />
This sign is designated with the<br />
signal word “Notice,” and is typically<br />
blue. This sign should be<br />
conspicuously posted whenever<br />
service is being done on a Class 3B<br />
or 4 laser. The appropriate red<br />
Danger Warning sign for the<br />
specific wavelength must also be<br />
displayed. It is more likely that an<br />
equipment-associated hazard will<br />
occur during service or maintenance<br />
procedures, since protective<br />
housings or other features may be<br />
removed or disabled. Thus, particular<br />
attention must be given in the<br />
form <strong>of</strong> these additional signs.<br />
Signs give you important information<br />
about the regulations, warn<br />
you about dangerous conditions,<br />
and help you find your way. Signs<br />
use different symbols, colors, and<br />
shapes for easy identification. It is<br />
important that all personnel are<br />
adequately trained to identify<br />
hazardous zones and understand<br />
the various warning signs. It is also<br />
important to document such<br />
Mastis<br />
training in a logbook or safety<br />
checklist. When the environment<br />
changes, signs should conspicuously<br />
change. Understanding the<br />
significance, meaning, and importance<br />
<strong>of</strong> laser signs will help<br />
improve the safety guidelines for<br />
your workplace and help meet<br />
regulation requirements.<br />
A U T H O R B I O G R A P H Y<br />
Dr. Raminta Mastis graduated from<br />
the University <strong>of</strong> Illinois College <strong>of</strong><br />
<strong>Dentistry</strong> in 1987. She is a Master<br />
<strong>of</strong> the <strong>Academy</strong> <strong>of</strong> <strong>Laser</strong> <strong>Dentistry</strong>.<br />
She has Standard Pr<strong>of</strong>iciency certifications<br />
in Er:YAG, diode,<br />
Er,Cr:YSGG, and CO 2 laser wavelengths,<br />
and has achieved Advanced<br />
Pr<strong>of</strong>iciency in the Er:YAG wavelength.<br />
She currently serves as the<br />
chair <strong>of</strong> ALD’s <strong>Laser</strong> Safety<br />
Committee, serves on the<br />
Certification and Communications<br />
Committees, and serves on the ALD<br />
Board. She maintains a private<br />
dental practice, Michigan Cosmetic<br />
and <strong>Laser</strong> <strong>Dentistry</strong>, in St. Clair<br />
Shores, Michigan. She has been<br />
using lasers since 2000, and now<br />
has 18 lasers <strong>of</strong> various wavelengths<br />
in her practice. Her practice<br />
is highlighted by implant surgery<br />
and restoration, laser dentistry,<br />
esthetic and cosmetic dentistry, and<br />
integration <strong>of</strong> advanced technologies<br />
into practice. Dr. Mastis may<br />
be contacted by e-mail at<br />
Mi<strong>Laser</strong>Dentist@comcast.net.<br />
Disclosure: Dr. Mastis has no<br />
commercial or financial interest relative<br />
to this article.<br />
R E F E R E N C E S<br />
1. American National Standard for<br />
Safe Use <strong>of</strong> <strong>Laser</strong>s, ANSI 136.1 –<br />
2007, Section 4.7:48-51. Orlando, FL:<br />
<strong>Laser</strong> Institute <strong>of</strong> America, 2007.<br />
2. American National Standard for<br />
Safe Use <strong>of</strong> <strong>Laser</strong>s in Health Care,<br />
ANSI Z136.3 – 2011, Section 4.7:28-<br />
29. Orlando, FL: <strong>Laser</strong> Institute <strong>of</strong><br />
America, 2011. nn
In their articles on the adjunctive use <strong>of</strong> lasers in<br />
implantology, Dr. Kutkut et al. (270-275) and Drs. Avi<br />
Reyhanian and Donald Coluzzi (276-281) mention the<br />
bactericidal potential <strong>of</strong> laser irradiation <strong>of</strong> implant<br />
surfaces. The notion <strong>of</strong> utilizing laser energy to reduce<br />
surface bacteria on intraoral implants as a means to<br />
help ensure successful osseointegration and reduce the<br />
incidence <strong>of</strong> periimplantitis has been studied by a<br />
number <strong>of</strong> researchers investigating a variety <strong>of</strong> wavelengths,<br />
including excimer, diode, Nd:YAG, erbium, and<br />
carbon dioxide lasers. Abstracts from a sampling <strong>of</strong><br />
published papers representing various wavelengths<br />
appear below.<br />
Most researchers to date have investigated the<br />
antimicrobial effect, primarily due to heat generated by<br />
various lasers, on implant surfaces in in vitro experiments.<br />
Heinrich and colleagues take a different<br />
approach: use a KrF excimer (248 nm) laser to promote<br />
mucosal adhesion as a biological barrier against bacterial<br />
infection. Another group (Dörtbudak et al.) studied<br />
the effects <strong>of</strong> “s<strong>of</strong>t” diode laser exposure on implants in<br />
patients.<br />
Overall, results are mixed. Certain lasers do appear to<br />
have bactericidal potential on selected microorganisms<br />
on certain types <strong>of</strong> implants under certain conditions.<br />
Questions regarding the relative efficacy <strong>of</strong> laser vs.<br />
conventional treatment remain, as do concerns related to<br />
potential alteration <strong>of</strong> implant surface morphology,<br />
thermal damage to adjacent tissues, and inability to<br />
reestablish the biocompatibility <strong>of</strong> contaminated surfaces.<br />
Nevertheless, the potential for laser application in<br />
promoting long-term implant success via bacterial reduction<br />
exists. Further study is warranted, especially to<br />
determine effectiveness and safety in a clinical environment,<br />
with special emphasis placed on appropriate<br />
parameter settings and duration <strong>of</strong> laser exposure.<br />
R E S E A R C H A B S T R A C T S<br />
Editor’s Note: The following material is excerpted and expanded from the Research Abstracts <strong>of</strong><br />
the J <strong>Laser</strong> Dent 2007;15(3):156-160. These nine abstracts are <strong>of</strong>fered as topics <strong>of</strong> current interest.<br />
Readers are invited to submit to the editor inquiries concerning laser-related scientific topics<br />
for possible inclusion in future issues. We’ll scan the literature and present relevant abstracts.<br />
L A S E R B A C T E R I C I DA L E F F E C T S O N<br />
I N T R A O R A L I M P L A N T S : A N U P DAT E<br />
In order to more closely approximate a clinical situation<br />
in their in vitro investigation, Hauser-Gerspach<br />
and colleagues examined the microbicidal effect <strong>of</strong> 810nm<br />
diode and CO 2 lasers on selected bacterial species<br />
(Streptococcus sanguinis and Porphyromonas gingivalis)<br />
adhering to dental implant materials and in<br />
suspension (planktonic cells), “because a fraction <strong>of</strong><br />
peri-implant bacteria are present as floating cells.”<br />
They point out that a key to success is adequately<br />
controlling the laser energy density and dose, factors<br />
that vary with the manual guidance and experience <strong>of</strong><br />
the operator; that is, having sufficient laser energy<br />
present to promote a bactericidal effect without leading<br />
to undesirable alterations <strong>of</strong> the implant surface can be<br />
difficult to achieve, depending upon the laser wavelength<br />
and how it is used. Even when significant<br />
reductions in bacterial counts are realized through<br />
laser irradiation, they conclude that “the question<br />
remains unanswered whether a short-term drastic<br />
reduction <strong>of</strong> P. gingivalis in the peri-implant pocket<br />
achieved by low laser energy is sufficient for stable<br />
clinical improvements. … In periodontitis therapy, a<br />
statistically significant reduction <strong>of</strong> periodontopathogenic<br />
bacteria does not guarantee clinical success<br />
because reinfection from other oral sites may occur or<br />
bacteria may survive intracellularly at the treated<br />
site.”<br />
For U.S. readers, no laser has been cleared by the<br />
U.S. Food and Drug Administration for “decontaminating”<br />
or inducing bactericidal effects on intraoral<br />
implants.<br />
As always, clinicians are advised to review the<br />
specific indications for use <strong>of</strong> their lasers and to review<br />
their operator manuals for guidance on operating<br />
parameters before attempting similar techniques on<br />
their patients. nn<br />
J O U R N A L O F L A S E R D E N T I S T R Y | 2 011 V O L . 19 , N O . 3<br />
303
J O U R N A L O F L A S E R D E N T I S T R Y | 2 011 V O L . 19 , N O . 3<br />
304<br />
R E S E A R C H A B S T R A C T S<br />
L A S E R - M O D I F I E D T I TA N I U M I M P L A N T S F O R I M P R O V E D C E L L A D H E S I O N<br />
Andreas Heinrich, Katrin Dengler, Timo Koerner,<br />
Cornelia Haczek, Herbert Deppe, and Bernd Stritzker<br />
Concerning dental implant systems, a main problem is<br />
the adhesion <strong>of</strong> peri-implant mucosa in the cervical<br />
region. The aim <strong>of</strong> the present study was to use a laser<br />
for modifying titanium implants to promote mucosal<br />
adhesion, which is indispensable as a biological barrier<br />
against bacterial infection. By the use <strong>of</strong> a KrF excimer<br />
laser, it was possible to induce a holey structure on the<br />
polished area <strong>of</strong> the implant surface, which was<br />
analysed by a scanning electron microscope. In addi-<br />
Peri-implantitis is considered to be a multifactorial<br />
process involving bacterial contamination <strong>of</strong> the<br />
implant surface. A previous study demonstrated that a<br />
combination <strong>of</strong> toluidine blue O (100 microgram/ml)<br />
and irradiation with a diode s<strong>of</strong>t laser with a wavelength<br />
<strong>of</strong> 905 nm results in an elimination <strong>of</strong><br />
Porphyromonas gingivalis (P. gingivalis), Prevotella<br />
intermedia (P. intermedia), and Actinobacillus actinomycetemcomitans<br />
(A. actinomycetemcomitans) on<br />
different implant surfaces (machined, plasma-flamesprayed,<br />
etched, hydroxyapatite-coated). The aim <strong>of</strong> this<br />
study was to examine the laser effect in vivo. In 15<br />
patients with IMZ implants who showed clinical and<br />
radiographic signs <strong>of</strong> peri-implantitis, toluidine blue<br />
Universität Augsburg, Augsburg, Germany<br />
<strong>Laser</strong>s Med Sci 2008;23(1):55-58<br />
tion, the attachment <strong>of</strong> fibroblast cells to the created<br />
structures was investigated with the aid <strong>of</strong> an environmental<br />
scanning electron microscope. It turned out that<br />
the cells preferentially attach to the holey structure.<br />
Thereby, the cells form bridges inside, leading to a<br />
complete covering <strong>of</strong> the hole. In this way, a more effective<br />
biological barrier against bacteria can be created.<br />
Copyright 2008 Springer nn<br />
L E T H A L P H OTO S E N S I T I Z AT I O N F O R D E C O N TA M I N AT I O N O F I M P L A N T<br />
S U R FA C E S I N T H E T R E AT M E N T O F P E R I - I M P L A N T I T I S<br />
Orhun Dörtbudak, Robert Haas, Thomas Bernhart, Georg Mailath-Pokorny<br />
University <strong>of</strong> Vienna, Vienna, Austria<br />
Clin Oral Implants Res 2001;12(2):104-108<br />
O was applied to the implant surface for 1 min and the<br />
surface was then irradiated with a diode s<strong>of</strong>t laser with<br />
a wavelength <strong>of</strong> 690 nm for 60 s. Bacterial samples<br />
were taken before and after application <strong>of</strong> the dye and<br />
after lasing. The cultures were evaluated semiquantitatively<br />
for A. actinomycetemcomitans, P. gingivalis, and<br />
P. intermedia. It was found that the combined treatment<br />
reduced the bacterial counts by 2 log steps on<br />
average. The application <strong>of</strong> TBO and laser resulted in a<br />
significant reduction (P < 0.0001) <strong>of</strong> the initial values<br />
in all 3 groups <strong>of</strong> bacteria. Complete elimination <strong>of</strong><br />
bacteria was not achieved.<br />
Copyright 2001 Blackwell Publishing and the European<br />
Association for Osseointegration nn
A N T I M I C R O B I A L E F F I C A C Y O F S E M I C O N D U C TO R<br />
L A S E R I R R A D I AT I O N O N I M P L A N T S U R FA C E S<br />
Matthias Kreisler, Wolfgang Kohnen, Claudio Marinello,<br />
Jürgen Scho<strong>of</strong>, Ernst Langnau, Bernd Jansen, Bernd d’Hoedt<br />
Purpose: This study was conducted to investigate the<br />
antimicrobial effect <strong>of</strong> an 809-nm semiconductor laser on<br />
common dental implant surfaces. Materials and Methods:<br />
Sandblasted and acid-etched (SA), plasma-sprayed (TPS),<br />
and hydroxyapatite-coated (HA) titanium disks were<br />
incubated with a suspension <strong>of</strong> S. sanguinis (ATCC<br />
10556) and subsequently irradiated with a galliumaluminum-arsenide<br />
(GaAlAs) laser using a 600-microm<br />
optical fiber with a power output <strong>of</strong> 0.5 to 2.5 W, corresponding<br />
to power densities <strong>of</strong> 176.9 to 884.6 W/cm 2 .<br />
Bacterial reduction was calculated by counting colonyforming<br />
units on blood agar plates. Cell numbers were<br />
compared to untreated control samples and to samples<br />
treated with chlorhexidine digluconate (CHX). Heat<br />
development during irradiation <strong>of</strong> the implants placed in<br />
bone blocks was visualized by means <strong>of</strong> shortwave thermography.<br />
Results: In TPS and SA specimens, laser<br />
irradiation led to a significant bacterial reduction at all<br />
power settings. In an energy-dependent manner, the<br />
Johannes Gutenberg University, Mainz, Germany<br />
Int J Maxill<strong>of</strong>ac Implants 2003;18(5):706-711<br />
R E S E A R C H A B S T R A C T S<br />
number <strong>of</strong> viable bacteria was reduced by 45.0% to 99.4%<br />
in TPS specimens and 57.6% to 99.9% in SA specimens.<br />
On HA-coated disks, a significant bacterial kill was<br />
achieved at 2.0 W (98.2%) and 2.5 W (99.3%) only (t test,<br />
P < .05). For specimens treated with CHX, the bacterial<br />
counts were reduced by 99.99% in TPS and HA-coated<br />
samples and by 99.89% in SA samples. Discussion: The<br />
results <strong>of</strong> the study indicate that the 809-nm semiconductor<br />
laser is capable <strong>of</strong> decontaminating implant<br />
surfaces. Surface characteristics determine the necessary<br />
power density to achieve a sufficient bactericidal effect.<br />
The bactericidal effect, however, was lower than that<br />
achieved by a 1-minute treatment with 0.2% CHX. The<br />
rapid heat generation during laser irradiation requires<br />
special consideration <strong>of</strong> thermal damage to adjacent<br />
tissues. Conclusion: No obvious advantage <strong>of</strong> semiconductor<br />
laser treatment over conventional methods <strong>of</strong><br />
disinfection could be detected in vitro.<br />
Copyright 2003 Quintessence Publishing Co., Inc. nn<br />
E L I M I N AT I O N O F B A C T E R I A O N D I F F E R E N T I M P L A N T S U R FA C E S T H R O U G H<br />
P H OTO S E N S I T I Z AT I O N A N D S O F T L A S E R : A N I N V I T R O S T U DY<br />
Robert Haas, Orhun Dörtbudak, Nikoletta Mensdorff-Pouilly, Georg Mailath<br />
Microbiologic examinations <strong>of</strong> implants have shown that<br />
certain microorganisms described as periodontal<br />
pathogens may have an influence on the development<br />
and the progression <strong>of</strong> peri-implant disease. This experimental<br />
study aimed to examine the bactericidal effect <strong>of</strong><br />
irradiation with a s<strong>of</strong>t laser on bacteria associated with<br />
peri-implantitis following exposure to a photosensitizing<br />
substance. Platelets made <strong>of</strong> commercially pure titanium,<br />
either with a machined surface or with a hydroxyapatite<br />
or plasma-flame-sprayed surface or with a corundumblasted<br />
and etched surface, were incubated with a pure<br />
suspension <strong>of</strong> Actinobacillus actinomycetemcomitans or<br />
Porphyromonas gingivalis or Prevotella intermedia. The<br />
surfaces were then treated with a toluidine blue solution<br />
University <strong>of</strong> Vienna, Vienna, Austria<br />
Clin Oral Implants Res 1997;8(4):249-254<br />
and irradiated with a diode s<strong>of</strong>t laser with a wavelength<br />
<strong>of</strong> 905 nm for 1 min. None <strong>of</strong> the smears obtained from<br />
the thus-treated surfaces showed bacterial growth,<br />
whereas the smears obtained from surfaces that had<br />
been subjected to only one type <strong>of</strong> treatment showed<br />
unchanged growth <strong>of</strong> every target organism tested<br />
(P < 0.0006). Electron microscopic inspection <strong>of</strong> the<br />
thus-treated platelets revealed that combined dye/laser<br />
treatment resulted in the destruction <strong>of</strong> bacterial cells.<br />
The present in vitro results indicate that lethal photosensitization<br />
may be <strong>of</strong> use for treatment <strong>of</strong> peri-implantitis.<br />
Copyright 1997 Blackwell Publishing and the European<br />
Association for Osseointegration nn<br />
J O U R N A L O F L A S E R D E N T I S T R Y | 2 011 V O L . 19 , N O . 3<br />
305
J O U R N A L O F L A S E R D E N T I S T R Y | 2 011 V O L . 19 , N O . 3<br />
306<br />
R E S E A R C H A B S T R A C T S<br />
E F F E C T S O F T H E N D : YA G D E N TA L L A S E R O N P L A S M A - S P R AY E D<br />
A N D H Y D R O X YA PAT I T E - C OAT E D T I TA N I U M D E N TA L I M P L A N T S :<br />
S U R FA C E A LT E R AT I O N A N D AT T E M P T E D S T E R I L I Z AT I O N<br />
The Nd:YAG dental laser has been recommended for a<br />
number <strong>of</strong> applications, including the decontamination<br />
or sterilization <strong>of</strong> surfaces <strong>of</strong> dental implants that are<br />
diseased or failing. The effects <strong>of</strong> laser irradiation in<br />
vitro (1) on the surface properties <strong>of</strong> plasma-sprayed<br />
titanium and plasma-sprayed hydroxyapatite-coated<br />
titanium dental implants, and (2) on the potential to<br />
sterilize those surfaces after contamination with spores<br />
<strong>of</strong> Bacillus subtilis have been examined. Surface effects<br />
were examined by scanning electron microscopy, energy<br />
dispersive spectroscopy, and X-ray diffraction after<br />
laser irradiation at 0.3, 2.0, and 3.0 W using either<br />
contact or noncontact handpieces. Controls received no<br />
I N V I T R O E VA LU AT I O N O F T H E B I O C O M PAT I B I L I T Y O F<br />
C O N TA M I N AT E D I M P L A N T S U R FA C E S T R E AT E D W I T H<br />
A N E R : YA G L A S E R A N D A N A I R P O W D E R S Y S T E M<br />
Matthias Kreisler, Wolfgang Kohnen, Ann-Babett Christ<strong>of</strong>fers,<br />
Hermann Götz, Bernd Jansen, Heinz Duschner, Bernd d’Hoedt<br />
Titanium platelets with a sand-blasted and acid-etched<br />
surface were coated with bovine serum albumin and<br />
incubated with a suspension <strong>of</strong> Porphyromonas gingivalis<br />
(ATCC 33277). Four groups with a total <strong>of</strong> 48 specimens<br />
were formed. <strong>Laser</strong> irradiation <strong>of</strong> the specimens (n = 12)<br />
was performed on a computer-controlled XY translation<br />
stage at pulse energy 60 mJ and frequency 10 pps.<br />
Twelve specimens were treated with an air powder<br />
system. After the respective treatment, human gingival<br />
fibroblasts were incubated on the specimens. The proliferation<br />
rate was determined by means <strong>of</strong> fluorescence<br />
activity <strong>of</strong> a redox indicator (Alamar Blue Assay) which is<br />
reduced by metabolic activity related to cellular growth.<br />
Proliferation was determined up to 72 h. Contaminated<br />
and nontreated as well as sterile specimens served as<br />
positive and negative controls. Proliferation activity was<br />
Carl M. Block, John A. Mayo, Gerald H. Evans<br />
Louisiana State University Medical Center, New Orleans, Louisiana<br />
Int J Oral Maxill<strong>of</strong>ac Implants 1992;7(4):441-449<br />
Johannes Gutenberg-University Mainz, Mainz, Germany<br />
Clin Oral Implants Res 2005;16(1):36-43<br />
laser irradiation. Melting, loss <strong>of</strong> porosity, and other<br />
surface alterations were observed on both types <strong>of</strong><br />
implants, even with the lowest power setting. For the<br />
sterilization study, both types <strong>of</strong> implants were first<br />
sterilized by exposure to ethylene oxide and then<br />
contaminated with spores <strong>of</strong> B. subtilis. After laser irradiation,<br />
the implants were transferred to sterile growth<br />
medium and incubated. <strong>Laser</strong> irradiation did not sterilize<br />
either type <strong>of</strong> implant. The spore-contaminated<br />
implants in the control group were successfully sterilized<br />
with ethylene oxide.<br />
Copyright 1992 Quintessence Publishing Co., Inc. nn<br />
significantly (Mann-Whitney U-test, P < 0.05) reduced on<br />
contaminated and nontreated platelets when compared<br />
to sterile specimens. Both on laser as well as air powdertreated<br />
specimens, cell growth was not significantly<br />
different from that on sterile specimens. Air powder<br />
treatment led to microscopically visible alterations <strong>of</strong> the<br />
implant surface whereas laser-treated surfaces remained<br />
unchanged. Both air powder and Er:YAG laser irradiation<br />
have a good potential to remove cytotoxic bacterial<br />
components from implant surfaces. At the irradiation<br />
parameters investigated, the Er:YAG laser ensures a reliable<br />
decontamination <strong>of</strong> implants in vitro without<br />
altering surface morphology.<br />
Copyright 2005 Blackwell Publishing and the European<br />
Association for Osseointegration nn
Background and Objective: The aim <strong>of</strong> this study was to<br />
assess CO 2 laser ability to eliminate bacteria from titanium<br />
implant surfaces. The changes <strong>of</strong> the surface<br />
structure, the rise in temperature, and the damage <strong>of</strong><br />
connective tissue cells after laser irradiation were also<br />
considered. Study Design/Materials and Methods:<br />
Streptococcus sanguis and Porphyromonas gingivalis on<br />
titanium discs were irradiated by an expanded beam <strong>of</strong><br />
CO 2 laser. Surface alteration was observed by a light,<br />
and a scanning electron, microscope. Temperature was<br />
measured with a thermograph. Damage <strong>of</strong> fibroblastic<br />
(L-929) and osteoblastic (MC3T3-E1) cells outside the<br />
R E S E A R C H A B S T R A C T S<br />
I N F LU E N C E O F A N E R B I U M , C H R O M I U M - D O P E D Y T T R I U M ,<br />
S C A N D I U M , G A L L I U M , A N D G A R N E T ( E R , C R : Y S G G ) L A S E R<br />
O N T H E R E E S TA B L I S H M E N T O F T H E B I O C O M PAT I B I L I T Y<br />
O F C O N TA M I N AT E D T I TA N I U M I M P L A N T S U R FA C E S<br />
Frank Schwarz, Enaas Nuesry, Katrin Bieling, Monika Herten, Jürgen Becker<br />
Background: The aim <strong>of</strong> the present study was to evaluate<br />
the influence <strong>of</strong> an erbium, chromium-doped<br />
yttrium, scandium, gallium, and garnet (Er,Cr:YSGG<br />
laser [ERCL]) on (1) the surface structure and biocompatibility<br />
<strong>of</strong> titanium implants and (2) the removal <strong>of</strong><br />
plaque bi<strong>of</strong>ilms and reestablishment <strong>of</strong> the biocompatibility<br />
<strong>of</strong> contaminated titanium surfaces. Methods:<br />
Intraoral splints were used to collect an in vivo<br />
supragingival bi<strong>of</strong>ilm on sand-blasted and acid-etched<br />
titanium disks for 24 hours. ERCL was used at an<br />
energy output <strong>of</strong> 0.5, 1.0, 1.5, 2.0, and 2.5 W for the<br />
irradiation <strong>of</strong> (1) noncontaminated (20 and 25 Hz) and<br />
(2) plaque-contaminated (25 Hz) titanium disks.<br />
Unworn and untreated nonirradiated, sterile titanium<br />
disks served as untreated controls (UC). Specimens<br />
were incubated with SaOs-2 osteoblasts for 6 days.<br />
Treatment time, residual plaque bi<strong>of</strong>ilm (RPB) areas<br />
(%), mitochondrial cell activity (MA) (counts per<br />
Heinrich Heine University, Düsseldorf, Germany<br />
J Periodontol 2006;77(11):1820-1827<br />
B A C T E R I C I DA L E F F I C A C Y O F C A R B O N D I O X I D E L A S E R<br />
A G A I N S T B A C T E R I A - C O N TA M I N AT E D T I TA N I U M I M P L A N T A N D<br />
S U B S E Q U E N T C E L LU L A R A D H E S I O N TO I R R A D I AT E D A R E A<br />
Taku Kato, Haruka Kusakari, Etsuro Hoshino<br />
Niigata University, Niigata, Japan<br />
<strong>Laser</strong>s Surg Med 1998;23(5):299-309<br />
second), and cell morphology/surface changes (scanning<br />
electron microscopy [SEM]) were assessed. Results: (1)<br />
ERCL using either 0.5, 1.0, 1.5, 2.0, or 2.5 W at both 20<br />
and 25 Hz resulted in comparable mean MA values as<br />
measured in the UC group. A monolayer <strong>of</strong> flattened<br />
SaOs-2 cells showing complete cytoplasmatic extensions<br />
and lamellopodia was observed in both ERCL and<br />
UC groups. (2) Mean RPB areas decreased significantly<br />
with increasing energy settings (53.8 +/- 2.2 at 0.5 W to<br />
9.8 +/- 6.2 at 2.5 W). However, mean MA values were<br />
significantly higher in the UC group. Conclusion:<br />
Within the limits <strong>of</strong> the present study, it was concluded<br />
that even though ERCL exhibited a high efficiency to<br />
remove plaque bi<strong>of</strong>ilms in an energy-dependent<br />
manner, it failed to reestablish the biocompatibility <strong>of</strong><br />
contaminated titanium surfaces.<br />
Copyright 2006 The American <strong>Academy</strong> <strong>of</strong> Periodontology nn<br />
irradiation spot and adhesion <strong>of</strong> the cells to the irradiated<br />
area were also estimated. Results: All the<br />
organisms (10 8 ) <strong>of</strong> S. sanguis and P. gingivalis were<br />
killed by the irradiation at 286 J/cm 2 and 245 J/cm 2 ,<br />
respectively. Furthermore, laser irradiation did not<br />
cause surface alteration, rise <strong>of</strong> temperature, serious<br />
damage <strong>of</strong> connective tissue cells located outside the<br />
irradiation spot, or inhibition <strong>of</strong> cell adhesion to the<br />
irradiated area. Conclusion: CO 2 laser irradiation with<br />
expanded beam may be useful in removing bacterial<br />
contaminants from implant surface.<br />
Copyright 1998 Wiley-Liss, Inc. nn<br />
J O U R N A L O F L A S E R D E N T I S T R Y | 2 011 V O L . 19 , N O . 3<br />
307
J O U R N A L O F L A S E R D E N T I S T R Y | 2 011 V O L . 19 , N O . 3<br />
308<br />
R E S E A R C H A B S T R A C T S<br />
B A C T E R I C I DA L E F F E C T S O F D I F F E R E N T L A S E R S Y S T E M S<br />
O N B A C T E R I A A D H E R E D TO D E N TA L I M P L A N T S U R FA C E S :<br />
A N I N V I T R O S T U DY C O M PA R I N G Z I R C O N I A W I T H T I TA N I U M<br />
Irmgard Hauser-Gerspach 1 , Stefan Stübinger 2 , Jürg Meyer 1<br />
1 Institute <strong>of</strong> Preventive <strong>Dentistry</strong> and Oral Microbiology, School <strong>of</strong> Dental Medicine, University <strong>of</strong> Basel, Basel, Switzerland<br />
2 Competence Center for Applied Biotechnology and Molecular Medicine, University <strong>of</strong> Zürich, Zürich, Switzerland<br />
Objectives: The purpose <strong>of</strong> this study was to examine in<br />
vitro the antibacterial efficacy <strong>of</strong> two different laser<br />
systems (CO 2 and diode) applied to Streptococcus<br />
sanguinis or Porphyromonas gingivalis cells in suspensions<br />
or adhered to zirconia or titanium dental implant<br />
materials, with two different surfaces each. Materials<br />
and methods: Bacteria were irradiated at two different<br />
power settings with either a CO 2 (λ = 10,600 nm) or a<br />
diode laser (λ = 810 nm). The lower mode is used clinically<br />
(for CO 2 100 J/cm 2 , diode 50 J/cm 2 ) and the higher<br />
may alter the materials’ surface (for CO 2 1200 J/cm 2 ,<br />
diode 150 J/cm 2 ). After irradiation, the number <strong>of</strong> viable<br />
bacteria was determined by culture. Results: Planktonic<br />
cells <strong>of</strong> both species were more resistant to the laser<br />
irradiations than bacteria that adhered to surfaces.<br />
Adhered P. gingivalis were effectively killed at both<br />
Clin Oral Implants Res 2010;21(3):277-283<br />
wavelengths λ = 10,600 and 810 nm even at the lower<br />
settings, independent <strong>of</strong> the material. S. sanguinis cells<br />
that adhered to either zirconia surface were effectively<br />
killed by the CO 2 laser at the lower setting <strong>of</strong> 100<br />
J/cm 2 . However, the higher settings <strong>of</strong> both lasers were<br />
needed to reduce S. sanguinis that adhered to titanium<br />
surfaces. The CO 2 laser at the lower setting and the<br />
diode laser at the higher setting effectively reduced the<br />
viability <strong>of</strong> S. sanguinis or P. gingivalis that adhered to<br />
zirconia surfaces. Conclusions: Under irradiation conditions<br />
known not to alter zirconia implant surfaces in<br />
vitro, both CO 2 laser (100 J/cm 2 ) and the diode laser<br />
(150 J/cm 2 ) effectively reduced the viability <strong>of</strong> adhered<br />
S. sanguinis or P. gingivalis.<br />
Copyright 2006 The American <strong>Academy</strong> <strong>of</strong> Periodontology nn
®<br />
Dual Wavelength, Er:YAG & Nd:YAG All Tissue <strong>Laser</strong><br />
Optimize your laser investment and get the most for your Practice.<br />
Technology4Medicine is proud to bring you the LightWalker. . . an amazing, hard & so� ALL tissue laser delivering<br />
both Nd:YAG and Er:YAG laser wavelengths. The award-winning LightWalker encompasses the two superior proven<br />
wavelengths in dentistry, at less than the price <strong>of</strong> one. Now you have the most advanced, Fast Cu�ing, Best in Class,<br />
Erbium and ND:YAG, both at your finger tips. Revolutionize your practice with advanced <strong>Laser</strong> Periodontal Treatments,<br />
<strong>Laser</strong> Endodontic Treatments (PIPS), as well as expanded so� and hard tissue applications. Doing more for each<br />
patient while delivering a more gratifying experience for you, the dental pr<strong>of</strong>essional.<br />
CDA Meeting<br />
#2619<br />
#2621<br />
ALD<br />
Sco�sdale<br />
Arizona<br />
#109& #111<br />
Hinman<br />
Dental Meeting<br />
#819& #918<br />
Invest Less, Do More.<br />
email: info@t4med.com<br />
949.276.6650<br />
May 3-5<br />
March 29-31<br />
March 22-24