You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
J O U R N A L O F L A S E R D E N T I S T R Y | 2 011 V O L . 19 , N O . 3<br />
272<br />
C A S E R E P O R T<br />
Fourteen days postoperatively,<br />
at the time <strong>of</strong> suture removal, the<br />
patient reported swelling and<br />
tenderness at the surgical site. The<br />
sutures were removed, and the site<br />
was irrigated with saline. The<br />
patient was advised to continue<br />
cleaning the surgical area as<br />
described above for 2 additional<br />
weeks and to continue taking clindamycin<br />
at the same dosage for<br />
another 10 days.<br />
At the 1-month follow-up evaluation,<br />
the patient reported the<br />
presence <strong>of</strong> a fistula related to the<br />
implants at sites #11 and 12.<br />
Severe bone loss was detected<br />
around the implants at sites #11,<br />
12, and 14; the pocket depths<br />
varied from 6 to 8 mm (Figure 1).<br />
Tooth #10 was vital, as confirmed<br />
by a positive response to the electrical<br />
pulp test. This recurrent<br />
infection may have been associated<br />
with the previously existing infection<br />
in the left sinus area or in the<br />
recently extracted infected teeth.<br />
Preoperative radiographs from the<br />
private dental <strong>of</strong>fice were not available<br />
before the implant procedure<br />
was performed. Retreatment at the<br />
surgical site was planned for 2<br />
months after placement <strong>of</strong> the<br />
implants.<br />
S U R G I C A L R E E N T RY<br />
T R E AT M E N T A N D<br />
L A S E R I M P L A N T<br />
D E C O N TA M I N AT I O N<br />
The patient began taking clindamycin<br />
(150 mg four times daily)<br />
one day before the surgery. The<br />
patient’s vital signs were recorded.<br />
After the administration <strong>of</strong> appropriate<br />
local anesthetics, a<br />
crestopalatal incision was made<br />
over the implant area at sites #11<br />
through 14, and a full-thickness<br />
flap was reflected at the buccal side<br />
to access the periimplant defect at<br />
the location <strong>of</strong> the bone loss. All<br />
granulation tissue in the defected<br />
area was removed with hand<br />
instruments. The threads were<br />
carefully cleaned <strong>of</strong> the infected<br />
tissue, and the exposed implant<br />
Kutkut, Andreana, and Al-Sabbagh<br />
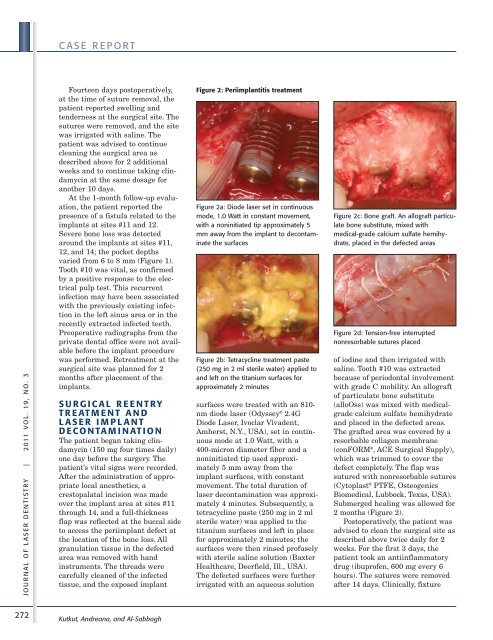
Figure 2: Periimplantitis treatment<br />
Figure 2a: Diode laser set in continuous<br />
mode, 1.0 Watt in constant movement,<br />
with a noninitiated tip approximately 5<br />
mm away from the implant to decontaminate<br />
the surfaces<br />
Figure 2b: Tetracycline treatment paste<br />
(250 mg in 2 ml sterile water) applied to<br />
and left on the titanium surfaces for<br />
approximately 2 minutes<br />
surfaces were treated with an 810nm<br />
diode laser (Odyssey ® 2.4G<br />
Diode <strong>Laser</strong>, Ivoclar Vivadent,<br />
Amherst, N.Y., USA), set in continuous<br />
mode at 1.0 Watt, with a<br />
400-micron diameter fiber and a<br />
noninitiated tip used approximately<br />
5 mm away from the<br />
implant surfaces, with constant<br />
movement. The total duration <strong>of</strong><br />
laser decontamination was approximately<br />
4 minutes. Subsequently, a<br />
tetracycline paste (250 mg in 2 ml<br />
sterile water) was applied to the<br />
titanium surfaces and left in place<br />
for approximately 2 minutes; the<br />
surfaces were then rinsed pr<strong>of</strong>usely<br />
with sterile saline solution (Baxter<br />
Healthcare, Deerfield, Ill., USA).<br />
The defected surfaces were further<br />
irrigated with an aqueous solution<br />
Figure 2c: Bone graft. An allograft particulate<br />
bone substitute, mixed with<br />
medical-grade calcium sulfate hemihydrate,<br />
placed in the defected areas<br />
Figure 2d: Tension-free interrupted<br />
nonresorbable sutures placed<br />
<strong>of</strong> iodine and then irrigated with<br />
saline. Tooth #10 was extracted<br />
because <strong>of</strong> periodontal involvement<br />
with grade C mobility. An allograft<br />
<strong>of</strong> particulate bone substitute<br />
(alloOss) was mixed with medicalgrade<br />
calcium sulfate hemihydrate<br />
and placed in the defected areas.<br />
The grafted area was covered by a<br />
resorbable collagen membrane<br />
(conFORM ® , ACE Surgical Supply),<br />
which was trimmed to cover the<br />
defect completely. The flap was<br />
sutured with nonresorbable sutures<br />
(Cytoplast ® PTFE, Osteogenics<br />
Biomedical, Lubbock, Texas, USA).<br />
Submerged healing was allowed for<br />
2 months (Figure 2).<br />
Postoperatively, the patient was<br />
advised to clean the surgical site as<br />
described above twice daily for 2<br />
weeks. For the first 3 days, the<br />
patient took an antiinflammatory<br />
drug (ibupr<strong>of</strong>en, 600 mg every 6<br />
hours). The sutures were removed<br />
after 14 days. Clinically, fixture