Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
the periimplant s<strong>of</strong>t tissues without<br />
any marginal bone loss. 4 The rate <strong>of</strong><br />
occurrence <strong>of</strong> periimplant mucositis<br />
ranges from 8% to 44%, and the<br />
rate <strong>of</strong> occurrence <strong>of</strong> periimplantitis<br />
ranges from 1% to 19%. 4<br />
However, because <strong>of</strong> the loss <strong>of</strong><br />
osseointegration and the exposure <strong>of</strong><br />
the roughened implant surface structure,<br />
decontaminating the defected<br />
surface with conventional nonsurgical<br />
treatment options is clinically<br />
difficult. 5 Recent clinical studies <strong>of</strong><br />
the use <strong>of</strong> a s<strong>of</strong>t tissue surgical laser<br />
to decontaminate (i.e., disinfect)<br />
rough implant surfaces, combined<br />
with surgical bone augmentation<br />
maintained by resorbable collagen<br />
membrane, have achieved good<br />
results with long-term success <strong>of</strong> the<br />
treated implants. 6<br />
The objective <strong>of</strong> this paper is to<br />
report a case <strong>of</strong> implant complications<br />
that were treated with<br />
various methods aimed at<br />
enhancing reosseointegration. The<br />
main outcome variables were<br />
reduction in probing depth and<br />
filling <strong>of</strong> the defect.<br />
C A S E R E P O R T<br />
A 55-year-old woman presented at<br />
the specialty dental clinics <strong>of</strong> the<br />
School <strong>of</strong> Dental Medicine at the<br />
State University <strong>of</strong> New York at<br />
Buffalo with a history <strong>of</strong> severe<br />
sinusitis in her left maxillary<br />
sinus. Because <strong>of</strong> the severity <strong>of</strong> the<br />
infection, teeth #11 through #15<br />
had been extracted at a private<br />
dental <strong>of</strong>fice. The patient had also<br />
been treated by an otolaryngologist<br />
(ENT). Nine months postoperatively,<br />
this patient presented at our<br />
clinic with an ill-fitting removable<br />
partial denture. The patient stated<br />
that she would like to have the<br />
missing teeth replaced with teeth<br />
that were fixed in the mouth. She<br />
was informed about possible<br />
complications associated with<br />
implants and about the methods <strong>of</strong><br />
treating those complications and<br />
consented to the most appropriate<br />
treatment option.<br />
The treatment plan was initi-<br />
ated with ENT consultation to<br />
verify the elimination <strong>of</strong> the infection<br />
related to the left maxillary<br />
sinus. The ENT report stated that<br />
no signs or symptoms <strong>of</strong> infection<br />
existed. Therefore, the dental treatment<br />
plan proceeded: 3 implants<br />
were placed at sites #11, 12, and<br />
14, and a sinus lift via the crestal<br />
approach was performed concurrently<br />
at site #14.<br />
S U R G I C A L T R E AT M E N T<br />
The patient began taking clindamycin<br />
150 mg (four times a day<br />
for 10 days) one day before the<br />
surgical procedure. On the day <strong>of</strong><br />
the procedure, the patient’s vital<br />
signs were recorded. After the<br />
administration <strong>of</strong> local anesthesia<br />
(injection <strong>of</strong> Xylocaine 2% injection<br />
with 1:100,000 epinephrine), a<br />
papilla-saving crestal incision was<br />
made and a full-thickness flap<br />
C A S E R E P O R T<br />
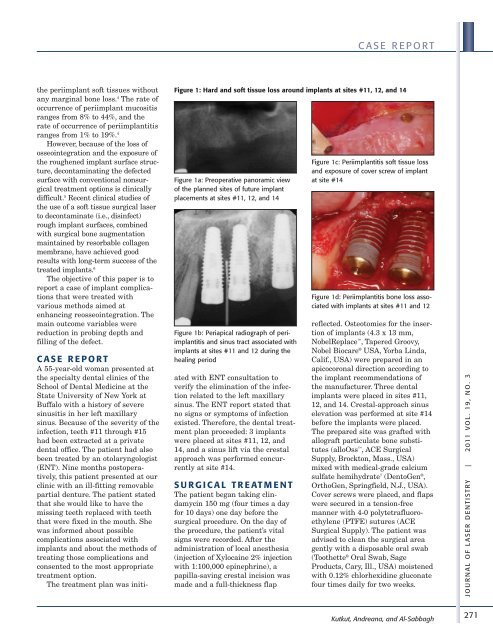
Figure 1: Hard and s<strong>of</strong>t tissue loss around implants at sites #11, 12, and 14<br />
Figure 1a: Preoperative panoramic view<br />
<strong>of</strong> the planned sites <strong>of</strong> future implant<br />
placements at sites #11, 12, and 14<br />
Figure 1b: Periapical radiograph <strong>of</strong> periimplantitis<br />
and sinus tract associated with<br />
implants at sites #11 and 12 during the<br />
healing period<br />
Figure 1c: Periimplantitis s<strong>of</strong>t tissue loss<br />
and exposure <strong>of</strong> cover screw <strong>of</strong> implant<br />
at site #14<br />
Figure 1d: Periimplantitis bone loss associated<br />
with implants at sites #11 and 12<br />
reflected. Osteotomies for the insertion<br />
<strong>of</strong> implants (4.3 x 13 mm,<br />
NobelReplace , Tapered Groovy,<br />
Nobel Biocare ® USA, Yorba Linda,<br />
Calif., USA) were prepared in an<br />
apicocoronal direction according to<br />
the implant recommendations <strong>of</strong><br />
the manufacturer. Three dental<br />
implants were placed in sites #11,<br />
12, and 14. Crestal-approach sinus<br />
elevation was performed at site #14<br />
before the implants were placed.<br />
The prepared site was grafted with<br />
allograft particulate bone substitutes<br />
(alloOss , ACE Surgical<br />
Supply, Brockton, Mass., USA)<br />
mixed with medical-grade calcium<br />
sulfate hemihydrate 7 (DentoGen ® ,<br />
OrthoGen, Springfield, N.J., USA).<br />
Cover screws were placed, and flaps<br />
were secured in a tension-free<br />
manner with 4-0 polytetrafluoro -<br />
ethylene (PTFE) sutures (ACE<br />
Surgical Supply). The patient was<br />
advised to clean the surgical area<br />
gently with a disposable oral swab<br />
(Toothette ® Oral Swab, Sage<br />
Products, Cary, Ill., USA) moistened<br />
with 0.12% chlorhexidine gluconate<br />
four times daily for two weeks.<br />
Kutkut, Andreana, and Al-Sabbagh<br />
J O U R N A L O F L A S E R D E N T I S T R Y | 2 011 V O L . 19 , N O . 3<br />
271