Optimizing visualization and ergonomics. - Academy of Laser Dentistry
Optimizing visualization and ergonomics. - Academy of Laser Dentistry
Optimizing visualization and ergonomics. - Academy of Laser Dentistry
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
The Official Journal <strong>of</strong> the <strong>Academy</strong> <strong>of</strong> <strong>Laser</strong> <strong>Dentistry</strong> 2007 • Vol. 15 No. 3<br />
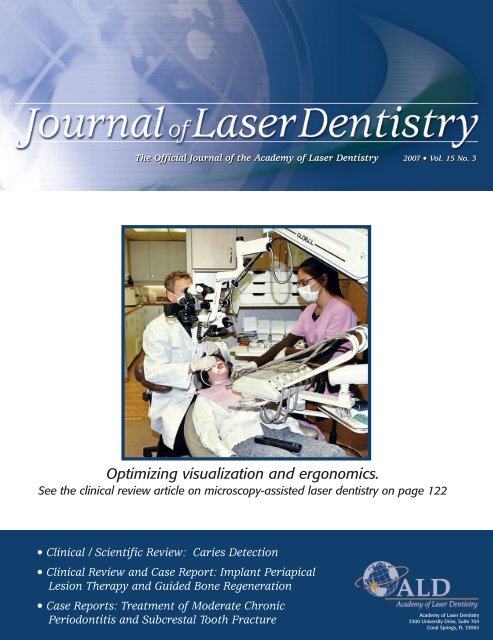
<strong>Optimizing</strong> <strong>visualization</strong> <strong>and</strong> <strong>ergonomics</strong>.<br />
See the clinical review article on microscopy-assisted laser dentistry on page 122<br />
• Clinical / Scientific Review: Caries Detection<br />
• Clinical Review <strong>and</strong> Case Report: Implant Periapical<br />
Lesion Therapy <strong>and</strong> Guided Bone Regeneration<br />
• Case Reports: Treatment <strong>of</strong> Moderate Chronic<br />
Periodontitis <strong>and</strong> Subcrestal Tooth Fracture<br />
<strong>Academy</strong> <strong>of</strong> <strong>Laser</strong> <strong>Dentistry</strong><br />
3300 University Drive, Suite 704<br />
Coral Springs, FL 33065
Journal <strong>of</strong> <strong>Laser</strong> <strong>Dentistry</strong><br />
The <strong>of</strong>ficial journal <strong>of</strong> the<br />
<strong>Academy</strong> <strong>of</strong> <strong>Laser</strong> <strong>Dentistry</strong><br />
Editor in Chief<br />
John D.B. Featherstone, MSc, PhD<br />
San Francisco, CA jdbf@ucsf.edu<br />
Managing Editor<br />
Gail S. Siminovsky, CAE, Executive Director<br />
Coral Springs, FL siminovsky@laserdentistry.org<br />
Consulting Editor<br />
John G. Sulewski, MA<br />
Huntington Woods, MI john.sulewski@we-inc.com<br />
Associate Editors<br />
Donald J. Coluzzi, DDS<br />
Portola Valley, CA don@laser-dentistry.com<br />
Steven P.A. Parker, BDS, LDS RCS, MFGDP<br />
Harrogate, Great Britain<br />
thewholetooth@easynet.co.uk<br />
Editorial Board<br />
John D.B. Featherstone, MSc, PhD<br />
Gail S. Siminovsky, CAE<br />
John G. Sulewski, MA<br />
Donald J. Coluzzi, DDS<br />
Steven P.A. Parker, BDS, LDS RCS, MFGDP<br />
Alan J. Goldstein, DMD<br />
Donald E. Patth<strong>of</strong>f, DDS<br />
Peter Rechmann, Pr<strong>of</strong>. Dr. med. dent.<br />
Publisher<br />
Max G. Moses<br />
Member Media<br />
1844 N. Larrabee<br />
Chicago, IL 60614<br />
312-296-7864<br />
Fax: 312-896-9119<br />
max@maxgmoses.com<br />
Design <strong>and</strong> Layout<br />
Diva Design<br />
2616 Missum Point<br />
San Marcos, TX 78666<br />
512-665-0544<br />
Fax: 512-392-2967<br />
kkolstedt@austin.rr.com<br />
Editorial Office<br />
3300 University Drive, Suite 704<br />
Coral Springs, FL 33065<br />
954-346-3776<br />
Fax 954-757-2598<br />
www.laserdentistry.org<br />
laserexec@laserdentistry.org<br />
The <strong>Academy</strong> <strong>of</strong> <strong>Laser</strong> <strong>Dentistry</strong> is a not-for-pr<strong>of</strong>it<br />
organization qualifying under Section 501(c)(3) <strong>of</strong><br />
the Internal Revenue Code. The <strong>Academy</strong> <strong>of</strong> <strong>Laser</strong><br />
<strong>Dentistry</strong> is an international pr<strong>of</strong>essional membership<br />
association <strong>of</strong> dental practitioners <strong>and</strong> supporting<br />
organizations dedicated to improving the<br />
health <strong>and</strong> well-being <strong>of</strong> patients through the<br />
proper use <strong>of</strong> laser technology. The <strong>Academy</strong> is<br />
dedicated to the advancement <strong>of</strong> knowledge,<br />
research <strong>and</strong> education <strong>and</strong> to the exchange <strong>of</strong><br />
information relative to the art <strong>and</strong> science <strong>of</strong> the<br />
use <strong>of</strong> lasers in dentistry. The <strong>Academy</strong> endorses<br />
the Curriculum Guidelines <strong>and</strong> St<strong>and</strong>ards for<br />
Dental <strong>Laser</strong> Education.<br />
Member American Association <strong>of</strong> Dental Editors<br />
TABLE OF CONTENTS<br />
EDITOR’S VIEW<br />
Optical Methods for the Enhancement <strong>of</strong> Dental Practice ..................116<br />
John D.B. Featherstone, MSc, PhD<br />
GUEST EDITORIAL<br />
The Transformative Dental Experience ........................................................118<br />
Alan J. Goldstein, DMD<br />
COVER FEATURE<br />
CLINICAL REVIEW<br />
Use <strong>of</strong> the Dental Operating Microscope<br />
in <strong>Laser</strong> <strong>Dentistry</strong>: Seeing the Light ..............................................................122<br />
Glenn A. van As, DMD<br />
CLINICAL/SCIENTIFIC REVIEW<br />
Detection <strong>of</strong> Caries by DIAGNOdent:<br />
Scientific Background <strong>and</strong> Performance ....................................................130<br />
Raimund Hibst, PhD<br />
Er:YAG <strong>Laser</strong>-Assisted Implant Periapical Lesion Therapy<br />
(IPL) <strong>and</strong> Guided Bone Regeneration (GBR) Technique:<br />
New Challenges <strong>and</strong> New Instrumentation ..............................................135<br />
Avi Reyhanian, DDS; Donald J. Coluzzi, DDS<br />
ADVANCED PROFICIENCY CASE STUDIES<br />
Introduction ..........................................................................................................142<br />
Nd:YAG <strong>Laser</strong> Use in Treatment <strong>of</strong><br />
Moderate Chronic Periodontitis ....................................................................144<br />
Mary Lynn Smith, RDH<br />
Treatment <strong>of</strong> a Subcrestal Tooth Fracture with the Er:YAG <strong>Laser</strong> ........151<br />
Charles R. Hoopingarner, DDS<br />
R ESEARCH ABS TRA CTS<br />
<strong>Laser</strong> Bactericidal Effects on Intraoral Implants ........................................156<br />
The Journal <strong>of</strong> <strong>Laser</strong> <strong>Dentistry</strong><br />
The mission <strong>of</strong> the Journal <strong>of</strong> <strong>Laser</strong> <strong>Dentistry</strong> is to provide a pr<strong>of</strong>essional quarterly journal<br />
that helps to fulfill the goal <strong>of</strong> information dissemination by the <strong>Academy</strong> <strong>of</strong> <strong>Laser</strong> <strong>Dentistry</strong>.<br />
The purpose <strong>of</strong> the Journal <strong>of</strong> <strong>Laser</strong> <strong>Dentistry</strong> is to present information about the use <strong>of</strong> lasers<br />
in dentistry. All articles are peer-reviewed. Issues include manuscripts on current indications<br />
for uses <strong>of</strong> lasers for dental applications, clinical case studies, reviews <strong>of</strong> topics relevant to<br />
laser dentistry, research articles, clinical studies, research abstracts detailing the scientific<br />
basis for the safety <strong>and</strong> efficacy <strong>of</strong> the devices, <strong>and</strong> articles about future <strong>and</strong> experimental<br />
procedures. In addition, featured columnists <strong>of</strong>fer clinical insights, <strong>and</strong> editorials describe<br />
personal viewpoints.<br />
JOUR NAL OF LASER DENTIS TRY | 2007 VOL 15, NO. 3<br />
115
JOUR NAL OF LASER DENTIS TRY | 2007 VOL 15, NO. 3<br />
116<br />
EDITOR’S VIEW<br />
Optical Methods for the Enhancement <strong>of</strong><br />
Dental Practice<br />
John D.B. Featherstone, MSc, PhD, San Francisco, California<br />
J <strong>Laser</strong> Dent 2007;15(3):116-117<br />
SYNOPSIS<br />
John Featherstone, editor-in-chief, describes some <strong>of</strong> the highlights <strong>of</strong><br />
this issue <strong>of</strong> the Journal <strong>of</strong> <strong>Laser</strong> <strong>Dentistry</strong>, emphasizing the broad<br />
applications <strong>of</strong> optical technology in daily practice.<br />
The use <strong>of</strong> light technology in the<br />
practice <strong>of</strong> everyday clinical<br />
dentistry is not restricted simply to<br />
lasers. Clinicians have examined<br />
the tissues <strong>of</strong> the mouth by eye<br />
forever. The human eye is one <strong>of</strong><br />
the best optical tools that we have.<br />
New optical tools are now available<br />
for the practitioner <strong>and</strong> additional<br />
new ones are on the horizon. These<br />
will be highlighted in future issues.<br />
What remains is to underst<strong>and</strong><br />
what these tools have to <strong>of</strong>fer <strong>and</strong><br />
to make the best use <strong>of</strong> them for<br />
the benefit <strong>of</strong> the patient.<br />
Microscopes have been used in<br />
laboratory settings <strong>and</strong> in clinical<br />
medicine for a long time. More<br />
recently the dental pr<strong>of</strong>ession has<br />
started to embrace the use <strong>of</strong><br />
microscopes on a routine basis,<br />
especially in endodontics. So why<br />
not for dentistry with lasers? In<br />
this issue the <strong>Academy</strong> <strong>of</strong> <strong>Laser</strong><br />
<strong>Dentistry</strong> 2006 Leon Goldman<br />
awardee, Dr. Glenn van As, reviews<br />
the background <strong>and</strong> how the use <strong>of</strong><br />
microscopes has revolutionized his<br />
daily practice.<br />
Until recently caries detection<br />
has been largely visual, tactile, <strong>and</strong><br />
has relied on the use <strong>of</strong> radiography<br />
where the eye could not see.<br />
New tools are coming on the<br />
market to aid the clinician in the<br />
detection <strong>of</strong> carious lesions. <strong>Laser</strong><br />
fluorescence is the science behind<br />
one such tool. Dr. Raimund Hibst,<br />
one <strong>of</strong> the scientists involved in the<br />
research that led to the practical<br />
use <strong>of</strong> this methodology, provides a<br />
review in this issue <strong>of</strong> the science,<br />
laboratory assessment, <strong>and</strong> clinical<br />
evaluation <strong>of</strong> one <strong>of</strong> these tools.<br />
Periodontal therapy can be<br />
enhanced by the use <strong>of</strong> lasers. As<br />
time goes on we are achieving a<br />
better underst<strong>and</strong>ing not only <strong>of</strong><br />
the science behind the use <strong>of</strong> lasers<br />
for periodontal uses but also<br />
learning how better to use lasers in<br />
everyday practice. Several articles<br />
in this issue provide practical illustrations<br />
<strong>of</strong> the benefits <strong>of</strong> laser<br />
technology in this area <strong>of</strong> dentistry.<br />
The dentist <strong>and</strong> the hygienist can<br />
work closely together for the<br />
benefit <strong>of</strong> the patient.<br />
So what does all this mean? The<br />
st<strong>and</strong>ard <strong>of</strong> care in dental practice<br />
is evolving. Judicious use <strong>of</strong> optical<br />
technology in clinical practice<br />
requires ongoing education, sharing<br />
<strong>of</strong> science, practice, clinical studies,<br />
case reports, <strong>and</strong> most importantly<br />
the engaging <strong>of</strong> the brain before<br />
embarking on laser-assisted procedures.<br />
The Journal <strong>of</strong> <strong>Laser</strong><br />
<strong>Dentistry</strong> <strong>of</strong>fers a mix <strong>of</strong> science<br />
<strong>and</strong> practice, including clinical <strong>and</strong><br />
laboratory studies, reviews, <strong>and</strong><br />
case studies. It is over to the reader<br />
to make the best use <strong>of</strong> the information<br />
for their education <strong>and</strong><br />
most importantly the better health<br />
<strong>of</strong> the patient.<br />
Finally, then, let us put this in<br />
perspective. In the guest editorial<br />
in this issue, Dr. Alan Goldstein<br />
addresses the philosophical issue<br />
that is generated by my statements<br />
in the preceding paragraph. He<br />
states “In my <strong>of</strong>fice, I take the position<br />
that our task is to make every<br />
patient experience transformative.”<br />
In order to do that we must truly<br />
underst<strong>and</strong> what we are doing,<br />
what the likely outcomes are, <strong>and</strong><br />
combine science, training, <strong>and</strong><br />
experience together to this end. We<br />
must all be continual learners <strong>and</strong><br />
work out how to apply our learning<br />
to whatever we do each day.<br />
Please enjoy this issue <strong>of</strong> the<br />
Journal. Feel free to e-mail me<br />
with suggestions, criticisms, or<br />
compliments at jdbf@ucsf.edu.<br />
AUTHOR BIOGRAPHY<br />
Dr. John D.B. Featherstone is<br />
Pr<strong>of</strong>essor <strong>of</strong> Preventive <strong>and</strong><br />
Restorative Dental Sciences <strong>and</strong><br />
Interim Dean in the School <strong>of</strong><br />
<strong>Dentistry</strong> at the University <strong>of</strong><br />
California, San Francisco (UCSF).<br />
He has a Ph.D. in chemistry from<br />
the University <strong>of</strong> Wellington (New<br />
Zeal<strong>and</strong>). His research over the<br />
past 33 years has covered several<br />
aspects <strong>of</strong> cariology (study <strong>of</strong> tooth<br />
decay) including fluoride mechanisms<br />
<strong>of</strong> action, de- <strong>and</strong><br />
remineralization <strong>of</strong> the teeth,<br />
apatite chemistry, salivary dysfunction,<br />
caries (tooth decay)<br />
prevention, caries risk assessment,<br />
<strong>and</strong> laser effects on dental hard<br />
tissues with emphasis on caries<br />
prevention <strong>and</strong> early caries<br />
removal. He has won numerous<br />
national <strong>and</strong> international awards<br />
including the T.H. Maiman award<br />
for research in laser dentistry from<br />
the <strong>Academy</strong> <strong>of</strong> <strong>Laser</strong> <strong>Dentistry</strong> in<br />
2002, <strong>and</strong> the Norton Ross Award<br />
for Clinical Research from the<br />
American Dental Association in<br />
2007. In 2005 he was honored as<br />
the first lifetime honorary member<br />
<strong>of</strong> the <strong>Academy</strong> <strong>of</strong> <strong>Laser</strong> <strong>Dentistry</strong>.<br />
Dr. Featherstone has published<br />
Featherstone
Featherstone<br />
EDITOR’S VIEW<br />
more than 200 papers. He is the<br />
editor-in-chief <strong>of</strong> the Journal <strong>of</strong><br />
<strong>Laser</strong> <strong>Dentistry</strong>.<br />
Disclosure: Dr. Featherstone has no<br />
personal financial interest in any<br />
company relevant to the <strong>Academy</strong> <strong>of</strong><br />
<strong>Laser</strong> <strong>Dentistry</strong>. He consults for, has<br />
consulted for, or has done research<br />
funded or supported by Arm &<br />
Hammer, Beecham, Cadbury, GSK,<br />
KaVo, NovaMin, Philips Oralcare,<br />
Procter & Gamble, OMNII Oral<br />
Pharmaceuticals, Oral-B, Wrigley, <strong>and</strong><br />
the National Institutes <strong>of</strong> Health. ■■<br />
Editorial Policy<br />
The Journal <strong>of</strong> <strong>Laser</strong> <strong>Dentistry</strong> is devoted to providing the <strong>Academy</strong> <strong>and</strong> its members with<br />
comprehensive clinical, didactic <strong>and</strong> research information about the safe <strong>and</strong> effective uses <strong>of</strong><br />
lasers in dentistry. All statements <strong>of</strong> opinions <strong>and</strong>/or fact are published under the authority <strong>of</strong><br />
the authors, including editorials <strong>and</strong> articles. The <strong>Academy</strong> is not responsible for the opinions<br />
expressed by the writers, editors or advertisers. The views are not to be accepted as the views<br />
<strong>of</strong> the <strong>Academy</strong> <strong>of</strong> <strong>Laser</strong> <strong>Dentistry</strong> unless such statements have been expressly adopted by the<br />
organization. Information on any research, clinical procedures or products may be obtained<br />
from the author. Comments concerning content may be directed to the <strong>Academy</strong>’s main <strong>of</strong>fice<br />
by e-mail to laserexec@laserdentistry.org<br />
Submissions<br />
We encourage prospective authors to follow JLD’s “Instructions to Authors” before submitting<br />
manuscripts. To obtain a copy, please go to our Web site www.laserdentistry.org/press.cfm.<br />
Please send manuscripts by e-mail to the Editor at jdbf@ucsf.edu.<br />
Disclosure Policy <strong>of</strong> Contributing Authors’ Commercial Relationships<br />
According to the <strong>Academy</strong>’s Conflict <strong>of</strong> Interest <strong>and</strong> Disclosure policy, authors <strong>of</strong> manuscripts<br />
for JLD are expected to disclose any economic support, personal interests, or potential bias<br />
that may be perceived as creating a conflict related to the material being published.<br />
Disclosure statements are printed at the end <strong>of</strong> the article following the author’s biography.<br />
This policy is intended to alert the audience to any potential bias or conflict so that readers<br />
may form their own judgments about the material being presented.<br />
Disclosure Statement for the <strong>Academy</strong> <strong>of</strong> <strong>Laser</strong> <strong>Dentistry</strong><br />
The <strong>Academy</strong> <strong>of</strong> <strong>Laser</strong> <strong>Dentistry</strong> has no financial interest in any manufacturers or vendors <strong>of</strong><br />
dental supplies.<br />
Reprint Permission Policy<br />
Written permission must be obtained to duplicate <strong>and</strong>/or distribute any portion <strong>of</strong> the Journal<br />
<strong>of</strong> <strong>Laser</strong> <strong>Dentistry</strong>. Reprints may be obtained directly from the <strong>Academy</strong> <strong>of</strong> <strong>Laser</strong> <strong>Dentistry</strong><br />
provided that any appropriate fee is paid.<br />
Copyright 2007 <strong>Academy</strong> <strong>of</strong> <strong>Laser</strong> <strong>Dentistry</strong>. All rights reserved unless other ownership is indicated. If<br />
any omission or infringement <strong>of</strong> copyright has occurred through oversight, upon notification amendment<br />
will be made in a future issue. No part <strong>of</strong> this publication may be reproduced or transmitted in<br />
any fom or by any means, individually or by any means, without permission from the copyright holder.<br />
The Journal <strong>of</strong> the <strong>Academy</strong> <strong>of</strong> <strong>Laser</strong> <strong>Dentistry</strong> ISSN# 1935-2557.<br />
JLD is published quarterly <strong>and</strong> mailed nonpr<strong>of</strong>it st<strong>and</strong>ard mail to all ALD members. Issues are<br />
also mailed to new member prospects <strong>and</strong> dentists requesting information on lasers in dentistry.<br />
Advertising Information <strong>and</strong> Rates<br />
Display rates are available at www.laserdentistry.org/press.cfm <strong>and</strong>/or supplied upon<br />
request. Insertion orders <strong>and</strong> materials should be sent to Bill Spilman, Innovative Media<br />
Solutions, P.O. Box 399, Oneida, IL 61467, 877-878-3260, fax: 309-483-2371, e-mail<br />
bill@innovativemediasolutions.com. For a copy <strong>of</strong> JLD Advertising Guidelines go to<br />
www.laserdentistry.org/press_advguide_policy.cfm. The cost for a classified ad in one issue is<br />
$50 for the first 25 words <strong>and</strong> $2.00 for each additional word beyond 25. ALD members<br />
receive a 20% discount. Payment must accompany ad copy <strong>and</strong> is payable to the <strong>Academy</strong> <strong>of</strong><br />
<strong>Laser</strong> <strong>Dentistry</strong> in U.S. funds only. Classified advertising is not open to commercial enterprises.<br />
Companies are encouraged to contact Bill Spilman for information on display advertising<br />
specifications <strong>and</strong> rates. The <strong>Academy</strong> reserves the right to edit or refuse ads.<br />
Editor’s Note on Advertising:<br />
The Journal <strong>of</strong> <strong>Laser</strong> <strong>Dentistry</strong> currently accepts advertisements for different dental laser educational<br />
programs. Not all dental laser educational courses are recognized by the <strong>Academy</strong> <strong>of</strong> <strong>Laser</strong> <strong>Dentistry</strong>.<br />
ALD as an independent pr<strong>of</strong>essional dental organization is concerned that courses meet the stringent<br />
guidelines following pr<strong>of</strong>essional st<strong>and</strong>ards <strong>of</strong> education. Readers are advised to verify with ALD whether<br />
or not specific courses are recognized by the <strong>Academy</strong> <strong>of</strong> <strong>Laser</strong> <strong>Dentistry</strong> in their use <strong>of</strong> the Curriculum<br />
Guidelines <strong>and</strong> St<strong>and</strong>ards for Dental <strong>Laser</strong> Education.
JOUR NAL OF LASER DENTIS TRY | 2007 VOL 15, NO. 3<br />
118<br />
GUEST EDITORIAL<br />
The Transformative Dental Experience<br />
Alan J. Goldstein, DMD, New York, New York<br />
J <strong>Laser</strong> Dent 2007;15(3):118-119<br />
SYNOPSIS<br />
Dr. Goldstein, past president <strong>of</strong> the <strong>Academy</strong> <strong>of</strong> <strong>Laser</strong> <strong>Dentistry</strong>, high-<br />
lights how we can <strong>and</strong> should pr<strong>of</strong>oundly <strong>and</strong> beneficially affect our<br />
patients during our interactions with them.<br />
In times <strong>of</strong> change, learners inherit<br />
the Earth, while the learned find<br />
themselves beautifully equipped to<br />
deal with a world that no longer<br />
exists.<br />
— Eric H<strong>of</strong>fer<br />
The skills <strong>and</strong> knowledge that<br />
created the problem will be insufficient<br />
in the development <strong>of</strong> its<br />
solution.<br />
— Albert Einstein<br />
The spring 2007 issue <strong>of</strong> the<br />
Journal <strong>of</strong> the New York State<br />
<strong>Academy</strong> <strong>of</strong> General <strong>Dentistry</strong><br />
published an article by Dr. Robert<br />
Willis 1 that emphasized the role <strong>of</strong><br />
emotions over logic as patients<br />
made decisions about proposed<br />
treatment plans. It is a perspective<br />
that has its roots all the way back<br />
to Dale Carnegie’s decades-long<br />
bestseller first published in 1936,<br />
How to Win Friends <strong>and</strong> Influence<br />
People. 2 But is Dr. Willis right? Is<br />
this emotional component valid or<br />
over-hyped? What are we, as scientists,<br />
researchers, <strong>and</strong> clinicians to<br />
believe in our statistically laden<br />
<strong>and</strong> evidence-based world?<br />
As well we might inquire<br />
whether this logic/emotion<br />
dichotomy is valid. I don’t think so.<br />
I believe it is only when we synthesize<br />
emotion <strong>and</strong> logic that we have<br />
the capacity to move people, to<br />
transform them. This is a perspective<br />
that is different from the<br />
teacher whose goal is to teach<br />
laser-tissue interaction to her<br />
students or from the practitioner<br />
whose goal is to fix teeth <strong>and</strong> eradicate<br />
periodontal disease. While<br />
these are all good things to achieve,<br />
essential things if you will, I want<br />
to achieve more.<br />
In my <strong>of</strong>fice, I take the position<br />
that our task is to make every<br />
patient experience transformative.<br />
I want our patients to be changed<br />
by their interaction with us. Some<br />
might consider it preposterous <strong>and</strong><br />
gr<strong>and</strong>iose, but I would happily<br />
extend this challenge to all <strong>of</strong> us in<br />
every activity we undertake, either<br />
as a scientist or clinician. I maintain<br />
that it is the only attitude to<br />
take if leadership is embodied in<br />
our work. If we are alive <strong>and</strong> open<br />
to the ever-exp<strong>and</strong>ing world before<br />
us, every interaction that has its<br />
beginning in the world <strong>of</strong> test<br />
tubes, microscopes, or humans has<br />
the capacity to be transformative.<br />
As scientists <strong>and</strong> clinicians we<br />
are both practitioners <strong>and</strong> learners.<br />
In the former sense we dispense<br />
knowledge <strong>and</strong> craft; in the latter<br />
we take it in. It is very difficult,<br />
probably impossible, to make the<br />
distinction between the learner <strong>and</strong><br />
what it is that is learned – the<br />
scientist from the science or the<br />
clinician from clinical outcomes<br />
achieved. Sure, there is a great deal<br />
to be employed, integrated, <strong>and</strong><br />
dispensed in our scientific community<br />
— skills, content, updating, <strong>and</strong><br />
information-gathering strategies —<br />
<strong>and</strong> we are obligated to do the best<br />
we can. But I’d like to focus on the<br />
side that I think is most important<br />
in the transformational experience:<br />
learning.<br />
Learning has a vibrant <strong>and</strong><br />
exploratory quality. Its root is<br />
education, a word that comes from<br />
the Latin verb educare, which<br />
means to lead. Truly learning is<br />
leading – not only leading others,<br />
but leading ourselves to new ways<br />
<strong>and</strong> seeing, knowing, <strong>and</strong> doing.<br />
Learning means going into<br />
uncharted territory, opening <strong>and</strong><br />
reshaping knowledge. This <strong>of</strong><br />
course requires both a questioning<br />
mind <strong>and</strong> a courageous spirit. What<br />
does this involve for us in the world<br />
<strong>of</strong> dentistry <strong>and</strong> laser technology?<br />
How do we use our learning to<br />
open new horizons in the care we<br />
provide, to explore new clinical<br />
applications while still appreciating<br />
the science that supports them, <strong>and</strong><br />
to bridge new practice <strong>and</strong> established<br />
theory? In short, how do we<br />
create the transformative experience?<br />
Albert Einstein, whose life is<br />
explored in the revealing new biography<br />
by Walter Isaacson, 3 <strong>and</strong> to<br />
whose inquisitiveness <strong>and</strong> genius<br />
we owe the foundations <strong>of</strong> laser<br />
science <strong>and</strong> laser dentistry said,<br />
“The value <strong>of</strong> a college education<br />
[we might add pr<strong>of</strong>essional education]<br />
is not the learning <strong>of</strong> many<br />
facts but the training <strong>of</strong> the mind<br />
to think.” Thinking is far more<br />
challenging <strong>and</strong> rewarding than<br />
simply performing.<br />
In our world <strong>of</strong> laser technology,<br />
we begin with valid scientific principles,<br />
ground them in sound<br />
clinical practice, apply our inquisitiveness<br />
to new techniques, <strong>and</strong> at<br />
the end <strong>of</strong> this process wind up<br />
with potential breakthroughs in<br />
patient care. Of course, one has to<br />
Goldstein
e radical to take the risks that our<br />
conservative pr<strong>of</strong>ession says are<br />
beyond the bounds <strong>of</strong> our do-noharm<br />
charge. But risk-free <strong>and</strong><br />
do-no-harm are not equivalents. No<br />
care is risk-free, <strong>and</strong> neither is life.<br />
We run risks when we invade teeth<br />
with a h<strong>and</strong>piece, we run risks<br />
when do a simple a procedure like<br />
a prophylaxis. Certainly even the<br />
most prudent in our pr<strong>of</strong>ession<br />
would acknowledge that risks<br />
increase in direct proportion to our<br />
zeal to do good <strong>and</strong> the scope <strong>of</strong> our<br />
efforts. And yes, we can mitigate<br />
these risks with education,<br />
training, <strong>and</strong> experience. But risk<br />
cannot be eliminated, ever. Do<br />
nothing <strong>and</strong> the risk <strong>of</strong> malpractice<br />
looms large.<br />
There is irony here. Many<br />
colleagues, <strong>of</strong>ten those least<br />
familiar with the principles <strong>of</strong> laser<br />
technology, see our unique armamentarium<br />
through their own<br />
conservative, do-no-harm prism. A<br />
drill that creates micro (<strong>and</strong> not-somicro)<br />
fractures is seen as proper;<br />
while laser energy that creates<br />
small, easily restorable, virtually<br />
sterile cavities without fractures is<br />
seen as radical. It is language that<br />
has turned dentistry on its head.<br />
Goldstein<br />
This inversion <strong>of</strong> science extends to<br />
the discussion <strong>of</strong> laser technology<br />
for s<strong>of</strong>t-tissue care. Excisional<br />
treatment is deemed conservative<br />
<strong>and</strong> appropriate, while care <strong>of</strong>fered<br />
at the multiple-cell layer level —<br />
which has the added benefit <strong>of</strong><br />
being bactericidal — is deemed<br />
radical <strong>and</strong> without value. Am I<br />
missing something?<br />
My point is that I sometimes see<br />
our pr<strong>of</strong>ession as learned, in the<br />
sense described by Eric H<strong>of</strong>fer<br />
above — <strong>and</strong> yet it <strong>of</strong>ten refuses to<br />
acknowledge that learning is the<br />
activity most urgently required.<br />
Confucius identified the first <strong>and</strong><br />
essential virtue as courage. I have<br />
a feeling I know where he would<br />
come down on this question <strong>of</strong><br />
whether every interaction is potentially,<br />
<strong>and</strong> optimally, transformative<br />
— <strong>and</strong> what it takes to achieve it.<br />
AUTHOR BIOGRAPHY<br />
Born <strong>and</strong> raised in the Bronx, Dr.<br />
Alan Goldstein graduated from the<br />
City College <strong>of</strong> New York before<br />
receiving his dental degree from<br />
the University <strong>of</strong> Pennsylvania<br />
School <strong>of</strong> Dental Medicine in 1968.<br />
He is a frequent contributor to the<br />
dental literature as well as a<br />
GUEST EDITORIAL<br />
lecturer in a variety <strong>of</strong> venues. He<br />
was certified as a Pr<strong>of</strong>essional<br />
Coach in 2001 <strong>and</strong> <strong>of</strong>ten addresses<br />
audiences on topics <strong>of</strong> personal<br />
effectiveness, fulfillment, <strong>and</strong> leadership<br />
as well as dental practice<br />
management <strong>and</strong> use <strong>of</strong> lasers. He<br />
is a past president <strong>of</strong> the <strong>Academy</strong><br />
<strong>of</strong> <strong>Laser</strong> <strong>Dentistry</strong> <strong>and</strong> a former<br />
editor <strong>of</strong> Wavelengths. He serves on<br />
the Dental Advisory Board <strong>of</strong><br />
<strong>Dentistry</strong> Today <strong>and</strong> the Journal <strong>of</strong><br />
<strong>Laser</strong> <strong>Dentistry</strong>. Dr. Goldstein may<br />
be contacted by e-mail at:<br />
llaama1@mindspring.com.<br />
Disclosure: Dr. Goldstein has<br />
provided educational services for a<br />
number <strong>of</strong> laser manufacturers <strong>and</strong><br />
received honoraria for these services.<br />
Presently he has no commercial financial<br />
relationships.<br />
REFERENCES<br />
1. Willis R. What it takes to boost case<br />
acceptance. J N Y State Acad Gen<br />
Dent 2007 Spring:16-17.<br />
2. Carnegie D. How to win friends <strong>and</strong><br />
influence people. New York: Simon &<br />
Schuster, Inc., 1936.<br />
3. Isaacson W. Einstein: His life <strong>and</strong><br />
universe. New York: Simon &<br />
Schuster, Inc., 2007. ■■<br />
JOUR NAL OF LASER DENTIS TRY | 2007 VOL 15, NO. 3<br />
119
Journal <strong>of</strong> <strong>Laser</strong> <strong>Dentistry</strong>: Guidelines for Authors<br />
The <strong>Academy</strong> <strong>of</strong> <strong>Laser</strong> <strong>Dentistry</strong> Welcomes Your Articles for Submission<br />
The Journal <strong>of</strong> <strong>Laser</strong> <strong>Dentistry</strong> publishes<br />
articles pertaining to the art, science,<br />
<strong>and</strong> practice <strong>of</strong> laser dentistry <strong>and</strong><br />
other relevant light-based technologies.<br />
Articles may be scientific <strong>and</strong> clinical in<br />
nature discussing new techniques,<br />
research, <strong>and</strong> programs, or may be<br />
applications-oriented describing specific<br />
problems <strong>and</strong> solutions. While lasers<br />
are our preferred orientation, other<br />
high-technology articles, as well as<br />
insights into marketing, practice management,<br />
regulation, <strong>and</strong> other aspects<br />
<strong>of</strong> dentistry that may be <strong>of</strong> interest to<br />
the dental pr<strong>of</strong>ession, may be appropriate.<br />
All articles are peer-reviewed prior<br />
to acceptance, modification, or rejection.<br />
These guidelines are designed to<br />
help potential authors in writing <strong>and</strong><br />
submitting manuscripts to the Journal<br />
<strong>of</strong> <strong>Laser</strong> <strong>Dentistry</strong>, the <strong>of</strong>ficial publication<br />
<strong>of</strong> the <strong>Academy</strong> <strong>of</strong> <strong>Laser</strong> <strong>Dentistry</strong><br />
(ALD). Please follow these instructions<br />
carefully to expedite review <strong>and</strong> processing<br />
<strong>of</strong> your submission. Manuscripts<br />
that do not adhere to these instructions<br />
will not be accepted for consideration.<br />
The <strong>Academy</strong> <strong>of</strong> <strong>Laser</strong> <strong>Dentistry</strong> <strong>and</strong> the<br />
editors <strong>and</strong> publisher <strong>of</strong> the Journal <strong>of</strong><br />
<strong>Laser</strong> <strong>Dentistry</strong> endorse the “Uniform<br />
Requirements <strong>of</strong> Manuscripts Submitted<br />
to Biomedical Journals” (www.icmje.org).<br />
The Journal reserves the right to revise<br />
or rescind these guidelines.<br />
Authors are advised to read the more<br />
comprehensive Guidelines for Authors<br />
<strong>and</strong> required forms available by mail or<br />
online at www.laserdentistry.org.<br />
Manuscript Eligibility<br />
Submitted manuscripts must be written<br />
clearly <strong>and</strong> concisely in American<br />
English <strong>and</strong> appropriate for a scholarly<br />
journal. Write in active voice <strong>and</strong> use<br />
declarative sentences. Manuscripts will<br />
be considered for publication on the condition<br />
that they have been submitted<br />
exclusively to the Journal, <strong>and</strong> have not<br />
been published or submitted for publication<br />
in any part or form in another publication<br />
<strong>of</strong> any type, pr<strong>of</strong>essional or lay, or<br />
in any language elsewhere, <strong>and</strong> with the<br />
underst<strong>and</strong>ing that they will not be<br />
reprinted without written consent from<br />
both the managing editor <strong>and</strong> the author.<br />
Permissions<br />
Direct quotations <strong>of</strong> 100 or more words,<br />
<strong>and</strong> illustrations, figures, tables, or<br />
other materials (or adaptations there<strong>of</strong>)<br />
that have appeared in copyrighted<br />
material or are in press must be accompanied<br />
by written permission for their<br />
use in the Journal <strong>of</strong> <strong>Laser</strong> <strong>Dentistry</strong><br />
from the copyright owner <strong>and</strong> original<br />
author along with complete information<br />
regarding source, including (as applica-<br />
ble) author(s), title <strong>of</strong> article, title <strong>of</strong><br />
journal or book, year, volume number,<br />
issue number, pages. Photographs <strong>of</strong><br />
identifiable persons must be accompanied<br />
by valid signed releases indicating<br />
informed consent. When informed consent<br />
has been obtained from any<br />
patient, identifiable or not, it should be<br />
noted in the manuscript. The appropriate<br />
Permission Letters must be submitted<br />
with the manuscript. Suggested<br />
template letters are available online.<br />
Copyright<br />
All manuscript rights shall be transferred<br />
to the Journal <strong>of</strong> <strong>Laser</strong> <strong>Dentistry</strong><br />
upon submission. Upon submission <strong>of</strong><br />
the manuscript, authors agree to submit<br />
a completed Copyright Transfer<br />
Agreement form, available online. If the<br />
manuscript is rejected for publication,<br />
all copyrights will be retained by the<br />
author(s).<br />
Commercialism<br />
ALD members are interested in learning<br />
about new products <strong>and</strong> service<br />
<strong>of</strong>ferings, however ALD stresses that<br />
submitted manuscripts should be educational<br />
in nature. The emphasis is on<br />
scientific research <strong>and</strong> sound clinical<br />
<strong>and</strong> practical advice, rather than promotion<br />
<strong>of</strong> a specific product or service.<br />
Disclosure <strong>of</strong> Commercial Relationships<br />
According to the <strong>Academy</strong>’s Conflict <strong>of</strong><br />
Interest <strong>and</strong> Disclosure policy, manuscript<br />
authors <strong>and</strong> their institutions are<br />
expected to disclose any economic or<br />
financial support, as well as any personal,<br />
commercial, technological, academic,<br />
intellectual, pr<strong>of</strong>essional, philosophical,<br />
political, or religious interests<br />
or potential bias that may be perceived<br />
as creating a conflict related to the<br />
material being published. Such conditions<br />
may include employment, consultancies,<br />
stock ownership or other equity<br />
interests, honoraria, stipends, paid<br />
expert testimony, patent ownership,<br />
patent licensing arrangements, royalties,<br />
or serving as an <strong>of</strong>ficer, director, or<br />
owner <strong>of</strong> a company whose products, or<br />
products <strong>of</strong> a competitor, are identified.<br />
Sources <strong>of</strong> support in the form <strong>of</strong> contracts,<br />
grants, equipment, drugs, material<br />
donations, clinical materials, special<br />
discounts or gifts, or other forms <strong>of</strong> support<br />
should be specified. The role <strong>of</strong> the<br />
study or manuscript sponsor(s), if any,<br />
are to be described. Disclosure statements<br />
are printed at the end <strong>of</strong> the article<br />
following the author’s biography.<br />
This policy is intended to alert the audience<br />
to any potential bias or conflict so<br />
that readers may form their own judgments<br />
about the material being pre-<br />
sented. Disclosure forms are to be<br />
signed by each author. Manuscripts will<br />
not be reviewed without the Journal<br />
having this form on file.<br />
The <strong>Academy</strong> <strong>of</strong> <strong>Laser</strong> <strong>Dentistry</strong> also<br />
requires that authors disclose whether<br />
any product discussed in their manuscript<br />
is unlabeled for the use discussed<br />
or is investigational.<br />
The Disclosure Statement form is<br />
available online <strong>and</strong> must be submitted<br />
with the manuscript.<br />
Manuscript Types<br />
Submissions to the Journal should be<br />
limited to one <strong>of</strong> the types indicated<br />
below.<br />
• Scientific / Technology / Clinical<br />
Review<br />
• Case Reports <strong>and</strong> Clinical Case<br />
Studies<br />
• Scientific / Clinical Research<br />
• R<strong>and</strong>omized Clinical Trials<br />
• Advances in Dental Products<br />
• Trends<br />
• Practice Management<br />
• Guest Editorials <strong>and</strong> Essays<br />
• Letters to the Editor<br />
• Book Reviews<br />
Manuscript Preparation <strong>and</strong><br />
Submission<br />
Format<br />
All submitted manuscripts should be<br />
double-spaced, using 12 pt. font size<br />
with at least 6 mm between lines.<br />
Submit manuscripts in Micros<strong>of</strong>t Word<br />
(.doc), using either the Windows or<br />
Macintosh platform. Manuscripts must<br />
be submitted electronically in this format.<br />
Hard copy-only submissions will<br />
not be accepted.<br />
Unacceptable Formats<br />
The following submission formats are<br />
unacceptable <strong>and</strong> will be returned:<br />
• Manuscripts submitted in desktop<br />
publishing s<strong>of</strong>tware<br />
• PowerPoint presentations<br />
• Any text files with embedded images<br />
• Images in lower than the minimum<br />
prescribed resolution.<br />
Manuscript Components<br />
Title Page<br />
The title page <strong>of</strong> the manuscript should<br />
include a concise <strong>and</strong> informative title<br />
<strong>of</strong> the article; the first name, middle initial(s),<br />
<strong>and</strong> last name <strong>of</strong> each author,<br />
along with the academic degree(s), pr<strong>of</strong>essional<br />
title(s), <strong>and</strong> the name <strong>and</strong><br />
location (city, state, zip code) <strong>of</strong> current<br />
institutional affiliation(s) <strong>and</strong> department(s).<br />
Authors who are private practitioners<br />
should identify their location<br />
(city, state, <strong>and</strong> country). Include all<br />
information in the title that will make
electronic retrieval <strong>of</strong> the article sensitive<br />
<strong>and</strong> specific. Titles <strong>of</strong> case studies<br />
should include the laser wavelength(s)<br />
<strong>and</strong> type(s) utilized for treatment (for<br />
example, “810-nm GaAlAs diode”).<br />
Identify the complete address, business<br />
<strong>and</strong> home telephone numbers, fax<br />
number, e-mail address, <strong>and</strong> Web site<br />
address (if any) for all authors. Identify<br />
one author as the corresponding author.<br />
Unless requested otherwise, the e-mail<br />
address is published in the Journal.<br />
Abstract<br />
A self-st<strong>and</strong>ing summary <strong>of</strong> the text <strong>of</strong><br />
up to 250 words should precede the<br />
introduction. It should provide an accurate<br />
summary <strong>of</strong> the most significant<br />
points <strong>and</strong> be representative <strong>of</strong> the<br />
entire article’s content. Provide the context<br />
or background for the article, basic<br />
procedures, main findings <strong>and</strong> conclusions.<br />
Emphasize new or important<br />
aspects. Do not use abbreviations (other<br />
than st<strong>and</strong>ard units <strong>of</strong> measurement) or<br />
references in the abstract.<br />
Author(s) Biography<br />
Provide a brief, current biographical<br />
sketch <strong>of</strong> each author that includes pr<strong>of</strong>essional<br />
education <strong>and</strong> pr<strong>of</strong>essional<br />
affiliations. For authors who hold teaching<br />
positions, include the title, department,<br />
<strong>and</strong> school. For authors who are<br />
in federal service, include rank or title<br />
<strong>and</strong> station.<br />
References<br />
References are to be cited in the text by<br />
number in order <strong>of</strong> appearance, with<br />
the number appearing either as a<br />
superscript or in brackets. The reference<br />
list should appear at the end <strong>of</strong> the<br />
manuscript with references in order <strong>of</strong><br />
first appearance in the text <strong>of</strong> the manuscript.<br />
The reference list must be<br />
typed double-spaced on a separate page<br />
<strong>and</strong> numbered in the same sequence as<br />
the reference citations appear in the<br />
text. Prior to submission, all references<br />
are to be properly prepared in the correct<br />
format, checked for completeness,<br />
carefully verified against their original<br />
documents, <strong>and</strong> checked for accurate<br />
correspondence between references<br />
cited in the text <strong>and</strong> listed in the<br />
References section.<br />
• For journal citations, include surnames<br />
<strong>and</strong> all initials <strong>of</strong> all authors,<br />
complete title <strong>of</strong> article, name <strong>of</strong> journal<br />
(abbreviated according to the U.S.<br />
National Library <strong>of</strong> Medicine<br />
(www.nlm.nih.gov/services/<br />
lpabbrev.html), year <strong>of</strong> publication,<br />
volume, issue number, <strong>and</strong> complete<br />
inclusive page numbers. If abstracts<br />
are cited, add the abstract number<br />
after the page number.<br />
• For book citations, specify surnames<br />
<strong>and</strong> initials <strong>of</strong> all authors, chapter<br />
number <strong>and</strong> title (if applicable), edi-<br />
tors’ surnames <strong>and</strong> initials, book<br />
title, volume number (if applicable),<br />
edition number (if applicable), city<br />
<strong>and</strong> full name <strong>of</strong> publisher, year <strong>of</strong><br />
publication, <strong>and</strong> inclusive page numbers<br />
<strong>of</strong> citation.<br />
• For government publications or bulletins,<br />
identify the author(s) (if given);<br />
title; department, bureau, agency, or<br />
<strong>of</strong>fice; the publication series, report,<br />
or monograph number; location <strong>of</strong><br />
publisher; publisher; year <strong>of</strong> publication;<br />
<strong>and</strong> inclusive page numbers.<br />
• For articles published online but not<br />
yet in print, cite with the paper’s<br />
Digital Object Identifier (DOI) added<br />
to the end <strong>of</strong> the reference.<br />
• For Web citations, list the authors<br />
<strong>and</strong> titles if known, then the URL<br />
<strong>and</strong> date it was accessed.<br />
• For presentations, list the authors,<br />
title <strong>of</strong> presentation, indication that<br />
the reference is a lecture, name <strong>of</strong><br />
conference or presentation venue,<br />
date, <strong>and</strong> location.<br />
Illustration Captions <strong>and</strong> Legends<br />
All illustrations must be accompanied by<br />
individual explanatory captions which<br />
should be typed double-spaced on a separate<br />
page with Arabic numerals corresponding<br />
to their respective illustration.<br />
Tables<br />
Tables must be typewritten doublespaced,<br />
including column heads, data,<br />
<strong>and</strong> footnotes, <strong>and</strong> submitted on separate<br />
pages. The tables are to be cited in<br />
the text <strong>and</strong> numbered consecutively in<br />
Arabic numerals in the order <strong>of</strong> their<br />
appearance in the text. Provide a concise<br />
title for each table that highlights<br />
the key result.<br />
Illustrations<br />
Illustrations include photographs, radiographs,<br />
micrographs, charts, graphs,<br />
<strong>and</strong> maps. Each should be numbered <strong>and</strong><br />
cited in the text in the order <strong>of</strong> appearance<br />
<strong>and</strong> be accompanied by explanatory<br />
captions. Do not embed figures within<br />
the manuscript text. Each figure <strong>and</strong><br />
table should be no larger than 8-1/2 x 11<br />
inches. Digital files must measure at<br />
Illustration<br />
Type<br />
least 5 inches (127 mm) in width. The<br />
image must be submitted in the size it<br />
will be printed, or larger. Illustrations<br />
are to augment, not repeat, material in<br />
the text. Graphs must not repeat data<br />
presented in tables. Clinical photographs<br />
must comply with ALD’s Guidelines for<br />
Clinical Photography, available online.<br />
Authors are to certify in a cover letter<br />
that digitized illustrations accurately<br />
represent the original data, condition, or<br />
image <strong>and</strong> are not electronically edited.<br />
Publisher <strong>and</strong> Copyright Holder<br />
The Journal <strong>of</strong> <strong>Laser</strong> <strong>Dentistry</strong> is published<br />
by Max G. Moses, Member<br />
Media, 1844 N. Larrabee, Chicago, IL<br />
60614, Telephone: (312) 296-7864; Fax:<br />
(312) 896-9119. The Journal <strong>of</strong> <strong>Laser</strong><br />
<strong>Dentistry</strong> is copyrighted by The<br />
<strong>Academy</strong> <strong>of</strong> <strong>Laser</strong> <strong>Dentistry</strong>, 3300<br />
University Drive, Suite 704, Coral<br />
Springs, FL 33065, Telephone: (954)<br />
346-3776; Fax: (954) 757-2598.<br />
Articles, Questions, Ideas<br />
Questions about clinical cases, scientific<br />
research, or ideas for other articles may<br />
be directed to John D.B. Featherstone,<br />
Editor-in-Chief, by e-mail: jdbf@ucsf.edu.<br />
Submission <strong>of</strong> Files<br />
by E-mail:<br />
Send your completed files by e-mail<br />
(files up to 10 MB are acceptable). If<br />
files are larger than 10 MB, they may<br />
be compressed or sent as more than one<br />
file, with appropriate labels. Files<br />
should be submitted to:<br />
John D.B. Featherstone, Editor-in-Chief<br />
by e-mail: jdbf@ucsf.edu.<br />
By Federal Express or Other<br />
Insured Courier:<br />
If using a courier, please send the file as<br />
a CD-ROM, include a hard copy <strong>of</strong> your<br />
manuscript <strong>and</strong> also send a verification<br />
by e-mail to Gail Siminovsky<br />
(laserexec@laserdentistry.org).<br />
Gail Siminovsky<br />
<strong>Academy</strong> <strong>of</strong> <strong>Laser</strong> <strong>Dentistry</strong><br />
3300 University Drive, Suite 704<br />
Coral Springs, FL 33065<br />
Phone: (954) 346-3776.<br />
Summary <strong>of</strong> Illustration Types <strong>and</strong> Specifications<br />
Definition <strong>and</strong> Examples<br />
Preferred<br />
Format<br />
Required<br />
Resolution<br />
Line Art <strong>and</strong> Black <strong>and</strong> white graphic with no<br />
EPS or JPG 1200 DPI<br />
Vector Graphics shading (e.g., graphs, charts, maps)<br />
Halftone Art<br />
Combination<br />
Art<br />
Photographs, drawings, or painting<br />
with fine shading (e.g., radiographs,<br />
micrographs with scale<br />
bars, intraoral photographs)<br />
Combination <strong>of</strong> halftone <strong>and</strong> line<br />
art (e.g., halftones containing<br />
line drawing, extensive lettering,<br />
color diagrams)<br />
TIFF or<br />
JPG<br />
300 DPI (black &<br />
white)<br />
600 DPI (color)<br />
EPS or JPG 1200 DPI
JOUR NAL OF LASER DENTIS TRY | 2007 VOL 15, NO. 3<br />
122<br />
COVER FEATURE<br />
Use <strong>of</strong> the Dental Operating Microscope<br />
in <strong>Laser</strong> <strong>Dentistry</strong>: Seeing the Light<br />
Glenn A. van As, DMD, North Vancouver, British Columbia, Canada<br />
J <strong>Laser</strong> Dent 2007;15(3):122-129<br />
SYNOPSIS<br />
Dr Van As was the recipient <strong>of</strong> the Leon Goldman Award for clinical<br />
excellence in laser dentistry in 2006. This article reviews his<br />
pioneering work using microscopy-assisted laser dentistry.<br />
INTRODUCTION<br />
The virtue <strong>of</strong> high levels <strong>of</strong> magnification<br />
in the medical field had been<br />
understood for many decades. 1-7 In<br />
1981, Apotheker introduced an<br />
operating microscope into dentistry,<br />
although it <strong>of</strong>fered only a single<br />
level <strong>of</strong> magnification <strong>and</strong> could be<br />
used only in a st<strong>and</strong>ing position. 8<br />
In the late 1980s <strong>and</strong> early<br />
1990s, endodontists began to<br />
promote the dental operating<br />
microscope (D.O.M.) for its value in<br />
st<strong>and</strong>ard endodontic therapy <strong>and</strong><br />
for the improvements in outcome <strong>of</strong><br />
both nonsurgical retreatments <strong>and</strong><br />
for surgical cases. 9-24<br />
At the same time, periodontists<br />
utilized the D.O.M. along with their<br />
microsurgical armamentarium,<br />
realizing reductions in postoperative<br />
pain <strong>and</strong> quicker healing. 25-31<br />
The use <strong>of</strong> lower-power telescopic<br />
loupes became more <strong>of</strong> the<br />
norm for all <strong>of</strong> dentistry during<br />
the mid-to-late 1990s. 32-33 With<br />
better underst<strong>and</strong>ing <strong>of</strong> the role<br />
<strong>and</strong> value <strong>of</strong> magnification, many<br />
practitioners purchased a higherpower<br />
set <strong>of</strong> loupes along with an<br />
illuminating headlight. As the<br />
present decade has progressed,<br />
the greatest increase in new users<br />
<strong>of</strong> the D.O.M. has been from those<br />
clinicians who routinely used<br />
loupes. In fact, in 2001, the<br />
author coined the term “magnification<br />
continuum” to describe the<br />
Figure 1: View <strong>of</strong> a microscope-centered<br />
dental operatory<br />
Figure 2: Neutral <strong>and</strong> balanced <strong>ergonomics</strong><br />
<strong>of</strong> the author at the microscope<br />
ever-increasing powers <strong>of</strong> magnification<br />
being used in dentistry. 34<br />
The use <strong>of</strong> the operating microscope<br />
for both diagnosis (new<br />
patient examinations, earlier<br />
<strong>visualization</strong> <strong>of</strong> decay <strong>and</strong><br />
ABSTRACT<br />
This article discusses the history<br />
<strong>and</strong> role <strong>of</strong> the dental operating<br />
microscope in dentistry. The<br />
microscope has become a st<strong>and</strong>ard<br />
part <strong>of</strong> the endodontic<br />
armamentarium since the 1980s<br />
as practitioners recognized the<br />
value <strong>of</strong> improved visual acuity<br />
through enhanced magnification<br />
<strong>and</strong> illumination. Benefits <strong>of</strong> the<br />
dental operating microscope<br />
including improvements in treatment<br />
outcomes, <strong>ergonomics</strong>,<br />
documentation, <strong>and</strong> communication<br />
are described. The<br />
importance <strong>of</strong> high levels <strong>of</strong><br />
magnification for hard tissue laser<br />
dentistry are emphasized <strong>and</strong><br />
detailed as this discipline, like<br />
endodontics, is also largely reliant<br />
on nontactile information for clinical<br />
success.<br />
cracks 35 ) <strong>and</strong> treatment (including<br />
laser dentistry) has become more<br />
accepted (Figure 1). 36-51<br />
This article examines the ability<br />
<strong>of</strong> the microscope to provide<br />
improvement in visual acuity <strong>and</strong><br />
the effect that high levels <strong>of</strong><br />
enhanced magnification <strong>and</strong> illumination<br />
can have on improving the<br />
quality <strong>of</strong> laser dentistry that is<br />
provided.<br />
BENEFITS OF MICRO-<br />
SCOPE-CENTERED<br />
P R A CTICES<br />
When used routinely for all aspects<br />
<strong>of</strong> dentistry, the microscope has<br />
four basic advantages:<br />
1. Improved precision <strong>of</strong> treatment<br />
2. Enhanced <strong>ergonomics</strong> (Figure 2)<br />
3. Ability to capture digital documentation<br />
(Figure 3)<br />
4. Enhanced communication<br />
through integrated video.<br />
van As
Figure 3: Illustration <strong>of</strong> the convenient<br />
arrangement <strong>of</strong> video camera on the left<br />
<strong>and</strong> a digital, single lens reflex camera<br />
(Nikon D70) on the right <strong>of</strong> the scope<br />
1. Improved Precision <strong>of</strong><br />
Treatment<br />
The visual information provided by<br />
the operating microscope is in fact<br />
not indicative <strong>of</strong> the magnification<br />
that is being employed. The actual<br />
amount <strong>of</strong> visual information is the<br />
area <strong>of</strong> view through the scope <strong>and</strong><br />
is therefore the product <strong>of</strong> the horizontal<br />
times the vertical number <strong>of</strong><br />
pixels. Therefore, the clinician<br />
using the 2X magnification power<br />
<strong>of</strong> entry-level loupes sees approximately<br />
4 times the visual<br />
information <strong>of</strong> a dentist not using<br />
any magnification (unaided eye).<br />
Likewise, 3X loupes provide 9 times<br />
the visual information <strong>of</strong> the<br />
unmagnified view <strong>and</strong> more than<br />
double the view <strong>of</strong> the 2X set. Table<br />
1 summarizes the relative advantages<br />
<strong>of</strong> a variety <strong>of</strong> magnifications.<br />
The author uses his microscope<br />
typically at 10X magnification<br />
which provides 100X the amount <strong>of</strong><br />
visual information compared to the<br />
unaided eye view. This is 25 times<br />
the information from 2X loupes <strong>and</strong><br />
more than 10 times as that seen<br />
with 3X.<br />
Carr 52 reported that the unaided<br />
human eye has the inherent ability<br />
to resolve or distinguish two separate<br />
lines or entities that are at<br />
least 200 µm or 0.2 mm apart. If<br />
the lines are closer together, then<br />
even 20/20 unmagnified vision will<br />
van As<br />
not allow the<br />
clinician to<br />
resolve them as<br />
two separate<br />
entities <strong>and</strong> the<br />
objects will<br />
appear as one.<br />
Thus with<br />
magnification<br />
the resolution <strong>of</strong><br />
the human eye<br />
improves<br />
dramatically<br />
(Table 2).<br />
Baldissara et<br />
al. 53 showed that<br />
the experienced<br />
clinician, when<br />
using a sharp,<br />
new explorer,<br />
can feel<br />
marginal gaps <strong>of</strong><br />
around 36 µm.<br />
Thus, when<br />
COVER FEATURE<br />
Table 1: Comparison <strong>of</strong> Unaided Eye, 2X Loupes, <strong>and</strong> Other Levels <strong>of</strong><br />
Magnification<br />
Magnification Visual Information (VI)<br />
VI Compared<br />
to 2X Loupes<br />
Unaided eye 1X 1/4<br />
2X loupes 4X Even = 1<br />
3X loupes 9X 2.25<br />
4X loupes 16X 4<br />
6X microscope 36X 9<br />
10X microscope 100X 25<br />
20X microscope 400X 100<br />
Table 2: Resolution vs. Assessment Method<br />
Assessment Method Magnification Resolution<br />
(µm)<br />
Resolution<br />
(mm)<br />
Unaided eye 1X 200 0.2<br />
Low-power loupes 2X 100 0.1<br />
Medium-power loupes 4X 50 0.05<br />
Sharp explorer NA 36 0.036<br />
Low-magnification microscope 6X 36 0.036<br />
Medium-magnification microscope 10X 20 0.02<br />
High-magnification microscope 20X 10 0.01<br />
Figure 4: Views <strong>of</strong> the same tooth area showing the effect <strong>of</strong> the<br />
magnification range <strong>of</strong> a typical microscope<br />
JOUR NAL OF LASER DENTIS TRY | 2007 VOL 15, NO. 3<br />
123
JOUR NAL OF LASER DENTIS TRY | 2007 VOL 15, NO. 3<br />
124<br />
COVER FEATURE<br />
magnification is beyond 6X power,<br />
the effectiveness <strong>of</strong> tactile means <strong>of</strong><br />
inspection with an explorer significantly<br />
decreases. Many clinicians<br />
using a microscope now rely on<br />
visual rather than tactile means <strong>of</strong><br />
discovery as their motor skills<br />
improve during the learning curve.<br />
The increased amount <strong>of</strong> information<br />
provided by the microscope<br />
<strong>of</strong>fers some challenges. As the<br />
magnification increases, the depth<br />
<strong>and</strong> diameter <strong>of</strong> the field <strong>of</strong> view in<br />
the operating field decreases. At<br />
higher magnification, there is an<br />
increased dem<strong>and</strong> for improved<br />
control <strong>of</strong> the micromotor muscles<br />
<strong>and</strong> joints (fingers <strong>and</strong> wrists) that<br />
can require stabilization <strong>of</strong> the<br />
gross motor joints (elbow <strong>and</strong><br />
shoulder) with micro-surgeon<br />
chairs. Tibbets <strong>and</strong> Shanelec 54<br />
reported the medical literature<br />
showed that the clinician not using<br />
magnification made movements<br />
that were 1-2 mm at a time. At<br />
microscope levels <strong>of</strong> 20X magnification,<br />
the refinement in movements<br />
can be as little as 10-20 µm (10-<br />
20/1000ths <strong>of</strong> a millimeter) at a<br />
time. It is useful therefore to note<br />
that the limitation to precision <strong>of</strong><br />
treatment is not in the h<strong>and</strong>s but<br />
in the eyes.<br />
Impact <strong>of</strong> Improved Visual Acuity<br />
in <strong>Laser</strong> <strong>Dentistry</strong><br />
The ability to carefully evaluate<br />
laser-tissue interaction at high<br />
magnification is important in many<br />
areas <strong>of</strong> laser dentistry. The microscope<br />
<strong>of</strong>fers improved visual acuity<br />
through its enhancements in<br />
magnification (Figure 4) <strong>and</strong> coaxial,<br />
shadow-free illumination,<br />
<strong>and</strong> these properties can be <strong>of</strong><br />
tremendous benefit during both<br />
s<strong>of</strong>t tissue <strong>and</strong> hard tissue ablation<br />
procedures.<br />
S<strong>of</strong>t Tissue <strong>Laser</strong> Procedures <strong>and</strong><br />
the Dental Operating Microscope<br />
The microscope can be especially<br />
effective for clinicians using laser<br />
wavelengths with small-diameter<br />
flexible optic fibers for s<strong>of</strong>t tissue<br />
Figure 5: Sequence showing the benefit <strong>of</strong> using magnification<br />
Figure 5a: Preoperative view <strong>of</strong> maxillary<br />
incisors prior to veneer preps<br />
Figure 5b: Veneer preps done<br />
Figure 5c: Diode laser used to trough<br />
around margin<br />
procedures, such as with potassium<br />
titanyl phosphate (KTP), diode, <strong>and</strong><br />
Nd:YAG lasers. For example, using<br />
a laser to trough around subgingival<br />
crown preparations can be<br />
frustrating because dragging the<br />
glass tip through inflamed tissue<br />
creates more bleeding. A 300micron<br />
fiber, which is close to the<br />
resolution <strong>of</strong> the human eye, must<br />
be accurately placed 1 mm or so<br />
into the sulcus to distend it, not to<br />
deepen it or to remove the papilla.<br />
The ability to closely watch the<br />
laser-tissue interaction is important<br />
to prevent excessive heat,<br />
while accurately aiming the endcutting<br />
fiber at the target tissue.<br />
The magnified view should prevent<br />
tissue charring, <strong>and</strong> thus decrease<br />
any postoperative discomfort for<br />
the patient (Figures 5a-5f).<br />
Excisional or incisional surgical<br />
procedures using small optic<br />
Figure 5d: High magnification <strong>of</strong><br />
completed trough<br />
Figure 5e: Veneer impression<br />
Figure 5f: Tissue health at 2 weeks<br />
Figure 5g: Postoperative result<br />
contact fibers can be performed<br />
with added precision when viewed<br />
through the D.O.M. The clinician<br />
can easily visualize exactly when<br />
all tissue fibers have been ablated,<br />
reducing the need for retreatment<br />
due to relapse.<br />
In microscope-assisted noncon-<br />
van As
Figure 6: Examples <strong>of</strong> procedures that benefit from observation by magnification<br />
Figure 6a: Preoperative view <strong>of</strong> lower<br />
second molar<br />
Figure 6b: Sinus tract on buccal aspect<br />
tact s<strong>of</strong>t tissue ablation, the clinician<br />
can keep the laser power<br />
settings lower <strong>and</strong> avoid iatrogenic<br />
damage to nontarget adjacent<br />
tissues. Magnification provides<br />
another advantage when the practitioner,<br />
using either erbium or<br />
carbon dioxide laser energy, is<br />
trying to avoid accidental interaction<br />
with tooth structure or bone.<br />
Other noncontact procedures,<br />
such as aphthous ulcer desensitization,<br />
hemostasis <strong>of</strong> extraction sites,<br />
<strong>and</strong> treatment <strong>of</strong> hemangiomas,<br />
can benefit from the visual acuity<br />
<strong>of</strong>fered by magnification. Examples<br />
are shown in Figures 6a-6f.<br />
The erbium laser wavelengths<br />
(Er:YAG, Er,Cr:YSGG) may be used<br />
in contact or noncontact mode for<br />
s<strong>of</strong>t tissue procedures. Using the<br />
noncontact mode can help to limit<br />
the inherent weakness <strong>of</strong> the<br />
erbium energy to adequately coagulate.<br />
The noncontact “plasty” or<br />
shaving down <strong>of</strong> tissue that is<br />
possible with the chisel or large<br />
footprint Er:YAG tips, when used<br />
in conjunction with the microscope<br />
van As<br />
Figure 6c: Extraction complete<br />
Figure 6d: Hemostasis by diode laser<br />
treatment<br />
Figure 7a: Noncontact Er:YAG frenectomy.<br />
Note early charring before adjusting<br />
power settings<br />
Figure 7b: High-magnification view <strong>of</strong><br />
frenectomy. Note lack <strong>of</strong> hemorrhage in<br />
noncontact mode<br />
COVER FEATURE<br />
Figure 6e: Hemostatic laser-induced clot<br />
viewed at low magnification<br />
Figure 6f: Clot induced by diode laser<br />
viewed at high magnification<br />
Figure 7: Examples <strong>of</strong> Er:YAG or Er, Cr:YSGG laser procedures that can be better carried<br />
out under magnification<br />
Figure 7c: Noncontact “plasty” <strong>of</strong> epulis on<br />
maxillary lip. Note “flash” at ablation site<br />
Figure 7d: High-magnification view <strong>of</strong><br />
frenectomy after periosteum is “scored”<br />
with an Er:YAG laser<br />
JOUR NAL OF LASER DENTIS TRY | 2007 VOL 15, NO. 3<br />
125
JOUR NAL OF LASER DENTIS TRY | 2007 VOL 15, NO. 3<br />
126<br />
COVER FEATURE<br />
Figure 8: Views relating to cavity preparation <strong>and</strong> restorations illustrating the benefits <strong>of</strong> using magnification<br />
Figure 8a: Preoperative interproximal decay<br />
Figure 8b: Decay visible on distal aspect<br />
<strong>of</strong> first primary molar<br />
at high magnification, is a<br />
wonderful technique for treating<br />
epulis <strong>and</strong> tissue tags, as well as in<br />
the creation <strong>of</strong> ovate pontics for<br />
fixed bridges where the tissue can<br />
be “melted” away (Figures 7a-7d).<br />
Hard Tissue <strong>Laser</strong> Ablation <strong>and</strong> the<br />
Operating Microscope<br />
Leknius <strong>and</strong> Geissberger 55 as well<br />
as Zaugg et al. 56 demonstrated that,<br />
when magnification was incorporated,<br />
procedural errors in<br />
restorative treatment decreased<br />
significantly. In the latter study,<br />
the use <strong>of</strong> a microscope resulted in<br />
fewer errors than loupes. Utilizing<br />
conventional instruments, the clinician<br />
can rely upon tactile means<br />
from burs or h<strong>and</strong> instruments to<br />
determine when the carious lesion<br />
is fully excavated or when old<br />
restorations have been completely<br />
removed. These same tactile<br />
methods become more unreliable in<br />
hard tissue laser dentistry where<br />
so much <strong>of</strong> the evaluation <strong>of</strong> the<br />
laser-tissue interface is based on<br />
visual cues. Caries detection dyes<br />
Figure 8c: High magnification shows<br />
decay still visible on facial wall <strong>of</strong> box<br />
Figure 8d: Preparations completed<br />
are not easy to use <strong>and</strong> can produce<br />
false readings with hard tissue<br />
laser preparations (Figures 8a-8f).<br />
Moreover, erbium lasers can use<br />
both contact tips (where the actual<br />
distance for effective ablation is 0.5<br />
- 1.5 mm from the surface) <strong>and</strong><br />
noncontact delivery systems, <strong>and</strong> it<br />
is difficult to “feel” the ablation<br />
process. Therefore the use <strong>of</strong> high<br />
magnification is essential to determine<br />
when the preparation is<br />
complete.<br />
There are several more reasons<br />
to employ magnification for<br />
restorative procedures. A large<br />
amount <strong>of</strong> water is needed for effective<br />
<strong>and</strong> safe hard tissue ablation,<br />
but that amount <strong>of</strong> water can<br />
obscure good <strong>visualization</strong>. Where<br />
rigid contact tips are used to<br />
deliver laser energy, their clear<br />
color makes them difficult to see.<br />
They must have a nonchipped<br />
surface, <strong>and</strong> be held at the proper<br />
working distance from the target<br />
tissue, without tactile feedback.<br />
This optimum distance can vary<br />
with different instruments, but<br />
Figure 8e: Restorations finished<br />
ablation efficiency will significantly<br />
decrease as the delivery system is<br />
placed farther from the tooth. If the<br />
laser tip is brought into direct<br />
contact with the surface the cutting<br />
efficiency decreases, <strong>and</strong> the water<br />
flow is not able to wash away ablation<br />
byproducts <strong>and</strong> cool the tissue.<br />
Charring <strong>and</strong> patient sensitivity<br />
can occur. Enamel bevels for Class<br />
III, IV, <strong>and</strong> V restorations require<br />
the clinician to “scrape” or alter the<br />
ablated enamel prior to acid<br />
etching. High magnification with<br />
the operating microscope shows<br />
that enamel bevels have many<br />
loose rods which, if not altered with<br />
an instrument (hatchet or spoon,<br />
air abrasion or diamond bur), will<br />
yield significantly lower bond<br />
strength compared to bur-cut<br />
enamel. The fragments <strong>of</strong> enamel<br />
that are scraped <strong>of</strong>f are easily<br />
visible under high magnification.<br />
The operating microscope is also<br />
an instrumental piece <strong>of</strong> the armamentarium<br />
for the ablation <strong>of</strong> bone.<br />
To prevent plucking or iatrogenic<br />
notching, it is best to use lower<br />
settings (1.5 - 3 Watts, for<br />
Figure 9: <strong>Laser</strong> beginning closed flap<br />
osseous contouring<br />
van As
Figure 10: Safety filter for use with<br />
various lasers<br />
Figure 10a: Nd:YAG (1064 nm) <strong>and</strong><br />
erbium (2780-2940 nm) laser filter<br />
Figure 10b: Placing a diode (800-830<br />
nm) laser filter in the microscope<br />
example), a noncontact mode, <strong>and</strong> a<br />
high water flow to prevent charring<br />
<strong>and</strong> necrosis. The amount <strong>of</strong> water<br />
<strong>and</strong> slight bleeding can obscure<br />
visibility, so the ability to increase<br />
the magnification during the procedure<br />
is imperative to success.<br />
Osseous crown lengthening to<br />
gain or re-establish biologic width<br />
can be performed with erbium<br />
lasers. The microscope is especially<br />
useful for closed-flap procedures so<br />
that the clinician can more accurately<br />
direct the laser energy <strong>and</strong><br />
avoid iatrogenic troughing <strong>of</strong> the<br />
bone. Figure 9 shows the laser<br />
beginning closed-flap osseous<br />
contouring.<br />
It is therefore very beneficial for<br />
van As<br />
magnification to be used for many<br />
aspects <strong>of</strong> hard tissue laser<br />
dentistry. The higher the level <strong>of</strong><br />
magnification used, the greater the<br />
ability <strong>of</strong> the dentist to directly<br />
view the laser-tissue interaction<br />
<strong>and</strong> to use the lowest possible<br />
energy <strong>and</strong> power to complete the<br />
procedure. This ultimately<br />
produces less patient sensitivity<br />
<strong>and</strong> better tissue health.<br />
<strong>Laser</strong> Safety<br />
Safety is <strong>of</strong> paramount importance<br />
to laser practitioners whether they<br />
are using no magnification, telescopic<br />
loupes, or higher levels <strong>of</strong><br />
magnification. All dental operating<br />
microscopes have holders that<br />
accept wavelength filters for eye<br />
protection. As usual, the laser<br />
safety <strong>of</strong>ficer must ensure that the<br />
appropriate filter is in place, <strong>and</strong><br />
the user must be sure to make<br />
close eye contact with the oculars<br />
to avoid the possibility <strong>of</strong> irradiation<br />
by accidental stray light.<br />
Assistants <strong>and</strong> patients must wear<br />
appropriate eye protection. Figure<br />
10a shows a typical erbium laser<br />
filter <strong>and</strong> Figure 10b shows a filter<br />
being placed into the microscope.<br />
2. Improved Ergonomics<br />
The operating microscope allows<br />
for the dentist to sit with an<br />
upright, neutral, <strong>and</strong> balanced<br />
posture (Figure 2). This neutral<br />
<strong>and</strong> balanced posture obtainable<br />
with the D.O.M. has been discussed<br />
as being helpful in preventing<br />
ergonomic issues that plague so<br />
many dentists <strong>and</strong> seem to be an<br />
occupational hazard. 57-60<br />
3. Ability to Capture Digital<br />
Documentation<br />
The D.O.M. can be a beneficial<br />
addition in documenting a clinical<br />
case, especially because <strong>of</strong> the<br />
detailed image (Figure 3), whether<br />
still or video. Carr, 61 Behle, 62 <strong>and</strong><br />
van As 63-64 have written articles<br />
discussing the merits <strong>of</strong> digital<br />
documentation with the D.O.M. <strong>and</strong><br />
the advantages <strong>of</strong> doing so.<br />
COVER FEATURE<br />
4. Enhanced Communication<br />
through Integrated Video<br />
Dentists who have added video<br />
capability to the microscope have<br />
found it useful in providing information<br />
to both patients <strong>and</strong> to<br />
auxiliaries since they can observe<br />
treatment in real time. 65 Clinicians<br />
have found that the images from<br />
the operating scopes are a benefit<br />
to educating their patients about<br />
treatment needs <strong>and</strong> help in<br />
persuading patients to accept treatment<br />
plans.<br />
The use <strong>of</strong> video transmitted to<br />
different monitors in the operatory<br />
has initiated the possibility <strong>of</strong><br />
working solely from a monitor, a<br />
method some surgeons now employ.<br />
The next improvement will be the<br />
development <strong>of</strong> three-dimensional<br />
displays. 65<br />
CONCLUSION<br />
The operating microscope used for<br />
laser dentistry provides benefits for<br />
any clinician. The advantages are<br />
improved precision, improved<br />
<strong>ergonomics</strong>, ease <strong>of</strong> documentation,<br />
<strong>and</strong> the ability to more fully<br />
communicate with patients, staff,<br />
<strong>and</strong> colleagues. Practitioners using<br />
the combination <strong>of</strong> the dental operating<br />
microscope <strong>and</strong> lasers have<br />
found that the two technologies<br />
work well in t<strong>and</strong>em <strong>and</strong> improve<br />
not only the treatment outcome but<br />
the enjoyment <strong>of</strong> providing it.<br />
AUTHOR BIOGRAPHY<br />
Dr. Glenn A. van As is a 1987 graduate<br />
<strong>of</strong> the University <strong>of</strong> British<br />
Columbia Faculty <strong>of</strong> <strong>Dentistry</strong> who<br />
maintains a full-time private dental<br />
practice in North Vancouver, British<br />
Columbia, Canada. His areas <strong>of</strong><br />
interest <strong>and</strong> expertise involve the<br />
utilization <strong>of</strong> the dental operating<br />
microscope for all <strong>of</strong> his clinical<br />
dentistry <strong>and</strong> in the use <strong>of</strong> multiple<br />
wavelengths <strong>of</strong> hard <strong>and</strong> s<strong>of</strong>t tissue<br />
lasers for many procedures. Since<br />
1999, he has lectured more than<br />
200 times internationally, provided<br />
h<strong>and</strong>s-on workshops, <strong>and</strong> published<br />
internationally on the value <strong>of</strong><br />
JOUR NAL OF LASER DENTIS TRY | 2007 VOL 15, NO. 3<br />
127
JOUR NAL OF LASER DENTIS TRY | 2007 VOL 15, NO. 3<br />
128<br />
COVER FEATURE<br />
multiple wavelengths <strong>of</strong> lasers <strong>and</strong><br />
practicing with the high magnifications<br />
obtainable with the dental<br />
operating microscope. Dr. van As is<br />
a member <strong>of</strong> the British Columbia<br />
Dental Association, the Canadian<br />
Dental Association, the <strong>Academy</strong> <strong>of</strong><br />
Microscope Enhanced <strong>Dentistry</strong><br />
(AMED), <strong>and</strong> the <strong>Academy</strong> <strong>of</strong> <strong>Laser</strong><br />
<strong>Dentistry</strong> (ALD). He has obtained<br />
both St<strong>and</strong>ard <strong>and</strong> Advanced<br />
Pr<strong>of</strong>iciency in laser usage from the<br />
<strong>Academy</strong> <strong>of</strong> <strong>Laser</strong> <strong>Dentistry</strong>, <strong>and</strong><br />
was distinguished with the Leon<br />
Goldman award for clinical excellence<br />
in the field <strong>of</strong> laser dentistry<br />
in 2006. In addition, Glenn is a<br />
founding member <strong>of</strong> the <strong>Academy</strong> <strong>of</strong><br />
Microscope Enhanced <strong>Dentistry</strong>,<br />
<strong>and</strong> in 2004-2005 served as the<br />
second president <strong>of</strong> the group<br />
(www.microscopedentistry.com). Dr.<br />
van As may be contacted by e-mail<br />
at glennvanas@shaw.ca.<br />
Disclosure: Dr. van As receives honoraria<br />
for lectures from the Global<br />
Surgical Corporation on microscopes,<br />
from HOYA ConBio on lasers, <strong>and</strong><br />
from Ivoclar on lasers.<br />
REFERENCES<br />
1. Nylén CO. The microscope in aural<br />
surgery, its first use <strong>and</strong> later development.<br />
Acta Otolaryngol<br />
1954;Suppl 116:226-240.<br />
2. Jacobsen JH II, Suarez EL.<br />
Microsurgery in anastomosis <strong>of</strong><br />
small vessels. Surg Forum<br />
1960;11:243-245.<br />
3. Harms H, Mackensen G. Ocular<br />
surgery under the microscope.<br />
Chicago: Yearbook Medical<br />
Publishers, Inc., 1967.<br />
4. Dohlman GF. Carl Ol<strong>of</strong> Nylén <strong>and</strong><br />
the birth <strong>of</strong> the otomicroscope <strong>and</strong><br />
microsurgery. Arch Otolaryngol<br />
1969;90(6):813-817.<br />
5. Klopper PJ. Microsurgery <strong>and</strong><br />
wound healing. In: Lie TS, editor.<br />
Microsugery. Proceedings <strong>of</strong> the 5th<br />
International Congress <strong>of</strong> the<br />
International Microsurgical Society,<br />
Bonn, October 4-7, 1978.<br />
Amsterdam: Excerpta Medica,<br />
International Congress Series No.<br />
465, 1979:280-282.<br />
6. Banowsky L. A review <strong>of</strong> optical<br />
magnification in urological surgery.<br />
Chapter 13 in Silber SJ, editor.<br />
Microsurgery. Baltimore: Williams<br />
<strong>and</strong> Wilkins, 1979:443-465.<br />
7. Barraquer JL. The history <strong>of</strong> the<br />
microscope in ocular surgery. J<br />
Microsurg 1980;1(4):288-289.<br />
8. Apotheker H, Jako GJ. A microscope<br />
for use in dentistry. J Micosurg<br />
1981;3(1):7-10.<br />
9. Carr GB. Microscopes in endodontics.<br />
J Calif Dent Assoc<br />
1992;20(11):55-61.<br />
10. Carr GB. Common errors in periradicular<br />
surgery. Endod Rep<br />
1993;8(1):12-18.<br />
11. Pecora G, Andreana S. Use <strong>of</strong> dental<br />
operating microscope in endodontic<br />
surgery. Oral Surg Oral Med Oral<br />
Pathol 1993;75(6):751-758.<br />
12. Ruddle CJ. Endodontic perforation<br />
repair: Using the surgical operating<br />
microscope. Dent Today<br />
1994;13(5):48, 50, 52-53.<br />
13. Feldman M. Microscopic surgical<br />
endodontics. N Y State Dent J<br />
1994;60(8):43-45.<br />
14. Mounce RE. Surgical operating<br />
microscope in endodontics: The<br />
paradigm shift. Gen Dent<br />
1995;43(4):346-349.<br />
15. Ruddle CJ. Nonsurgical endodontic<br />
retreatment. J Calif Dent Assoc<br />
1997;25(11): 769-771, 773-775, 777,<br />
779-786, 788-799.<br />
16. Stropko JJ. Canal morphology <strong>of</strong><br />
maxillary molars: Clinical observations<br />
<strong>of</strong> canal configurations. J<br />
Endod 1999;25(6):446-450.<br />
17. de Carvalho MC, Zuolo ML. Orifice<br />
locating with a microscope. J Endod<br />
2000;26(9):532-534.<br />
18. Sempira HN, Hartwell GR.<br />
Frequency <strong>of</strong> second mesiobuccal<br />
canals in maxillary molars as determined<br />
by use <strong>of</strong> an operating<br />
microscope: A clinical study. J<br />
Endod 2000;26(11):673-674.<br />
19. Görduysus MO, Görduysus M,<br />
Friedman S. Operating microscope<br />
improves negotiation <strong>of</strong> second<br />
mesiobuccal canals in maxillary<br />
molars. J Endod 2001;27(11):683-686.<br />
20. Buhrley LJ, Barrows MJ, BeGole<br />
EA, Wenckus CS. Effect <strong>of</strong> magnification<br />
on locating the MB2 canal in<br />
maxillary molars. J Endod<br />
2002;28(4):324-327.<br />
21. Schwarze T, Baethge C, Stecher T,<br />
Geurtsen W. Identification <strong>of</strong> second<br />
canals in the mesiobuccal root <strong>of</strong><br />
maxillary first <strong>and</strong> second molars<br />
using magnifying loupes or an operating<br />
microscope. Aust Endod J<br />
2002;28(2):57-60.<br />
22. Coutinho Filho T, La Cerda RS,<br />
Gurgel Filho ED, de Deus GA,<br />
Magalhães KM. The influence <strong>of</strong> the<br />
surgical operating microscope in<br />
locating the mesiolingual canal<br />
orifice: A laboratory analysis. Braz<br />
Oral Res 2006;20(1):59-63.<br />
23. Tsesis I, Rosen E, Schwartz-Arad D,<br />
Fuss Z. Retrospective evaluation <strong>of</strong><br />
surgical endodontic treatment:<br />
Traditional versus modern technique.<br />
J Endod 2006;32(5):412-416.<br />
24. Schirrmeister JF, Hermanns P,<br />
Meyer KM, Goetz F, Hellwig E.<br />
Detectability <strong>of</strong> residual Epiphany<br />
<strong>and</strong> gutta-percha after root canal<br />
retreatment using a dental operating<br />
microscope <strong>and</strong> radiographs –<br />
An ex vivo study. Int Endod J<br />
2006;39(7):558-565.<br />
25. Shanelec DA. Current trends in s<strong>of</strong>t<br />
tissue. J Calif Dent Assoc<br />
1991;19(12):57-60.<br />
26. Tibbets LS, Shanelec DA. An<br />
overview <strong>of</strong> periodontal microsurgery.<br />
Current Opin Periodontol<br />
1994:187-193.<br />
27. Shanelec DA, Tibbetts LS.<br />
Periodontal microsurgery.<br />
Periodontal Insights 1994;1(2):4-7.<br />
28. Michaelides PL. Use <strong>of</strong> the operating<br />
microscope in dentistry. J<br />
Calif Dent Assoc 1996;24(6):45-50.<br />
29. Shanelec DA, Tibbetts LS. A<br />
perspective on the future <strong>of</strong> periodontal<br />
microsurgery.<br />
Periodontology 2000 1996;11:58-64.<br />
30. Tibbetts LS, Shanelec D. Current<br />
status <strong>of</strong> periodontal microsurgery.<br />
Curr Opin Periodontol 1996;3:118-<br />
125.<br />
31. Belcher JM. A perspective on periodontal<br />
microsurgery. Int J<br />
Periodontics Restorative Dent<br />
2001;21(2):191-196.<br />
van As
32. Shanelec DA. Optical principles <strong>of</strong><br />
loupes. J Calif Dent Assoc<br />
1992;20(11):25-32.<br />
33. Strassler HE, Syme SE, Serio F,<br />
Kaim JM. Enhanced <strong>visualization</strong><br />
during dental practice using magnification<br />
systems. Compend Contin<br />
Educ Dent 1998;19(6):595-596, 598,<br />
600, 602, 604, 606, 608, 610-611,<br />
quiz 12. Erratum in: Compend<br />
Contin Educ Dent 1998;19(9):894.<br />
34. van As G. Magnification <strong>and</strong> the<br />
alternatives for microdentistry.<br />
Compend Contin Educ Dent<br />
2001;22(11A):1008-1012, 1014-1016.<br />
35. Clark DJ, Sheets CG, Paquette JM.<br />
Definitive diagnosis <strong>of</strong> early<br />
enamel <strong>and</strong> dentin cracks based on<br />
microscopic evaluation. J Esthet<br />
Restor Dent 2003;15(7):391-401,<br />
discussion 401.<br />
36. Martignoni M, Schönenberger A.<br />
Precision fixed prosthodontics:<br />
Clinical <strong>and</strong> laboratory aspects.<br />
Chicago: Quintessence Publishing<br />
Co. Inc., 1990.<br />
37. Friedman MJ, L<strong>and</strong>esman HM.<br />
Microscope-assisted precision<br />
dentistry – Advancing excellence in<br />
restorative dentistry. Contemp<br />
Esthetics Restorative Pract<br />
1997;1(1):45-49.<br />
38. Sheets CG, Paquette JM. Enhancing<br />
precision through magnification.<br />
Dent Today 1998;17(1):44, 46, 48-49.<br />
39. Piontkowski PK. The renaissance <strong>of</strong><br />
dentistry: An introduction to the<br />
surgical microscope. Dent Today<br />
1998;17(6):82-87.<br />
40. Sheets CG, Paquette JM. The magic<br />
<strong>of</strong> magnification. Dent Today<br />
1998;17(12):61-67.<br />
41. Cruci P. An operating microscope in<br />
general dental practice. Dent Pract<br />
1999:37(9):1, 4-5.<br />
42. Friedman M, Mora AF, Schmidt R.<br />
Microscope-assisted precision<br />
dentistry. Compend Contin Educ<br />
Dent 1999;20(8):723-726, 728, 730-<br />
731, 735-736, quiz 737.<br />
van As<br />
43. Paquette JM. The clinical microscope:<br />
Making excellence easier.<br />
Contemp Esthetics Restorative Pract<br />
1999;3(9):12-20.<br />
44. van As GA. Using the surgical operating<br />
microscope in general practice.<br />
Contemp Esthetics Restorative Pract<br />
2000;4(1):34, 36-40.<br />
45. van As GA. The role <strong>of</strong> the dental<br />
operating microscope in fixed<br />
prosthodontics. Oral Health<br />
2002;92(6):11-14, 17-20, 23, 25.<br />
46. van As GA. The use <strong>of</strong> extreme<br />
magnification in fixed prosthodontics.<br />
Dent Today 2003;22(6):93-99.<br />
47. Christensen GJ. Magnification in<br />
dentistry: Useful tool or another<br />
gimmick? J Am Dent Assoc<br />
2003;134(12):1647-1650.<br />
48. Clark DJ. Microscope-enhanced<br />
aesthetic dentistry. Dent Today<br />
2004;23(11):96, 98-101.<br />
49. Garcia A. Dental magnification: A<br />
clear view <strong>of</strong> the present <strong>and</strong> a<br />
close-up view <strong>of</strong> the future.<br />
Compend Contin Educ Dent<br />
2005;26(6A Suppl):459-463.<br />
50. Clark DJ. The big push to clinical<br />
microscopes for esthetic dentistry.<br />
Contemp Esthetics Restor Pract<br />
2005;9(11):30-33.<br />
51. Clark DJ, Kim J. <strong>Optimizing</strong> gingival<br />
esthetics: A microscopic perspective.<br />
Oral Health 2006;96(4):116-118, 121-<br />
122, 124-126.<br />
52. Carr GB. Magnification <strong>and</strong> illumination<br />
in endodontics. In: Hardin<br />
JF, editor. Clark’s Clinical <strong>Dentistry</strong>.<br />
New York: Mosby, 1998;4:1-14.<br />
53. Baldissara P, Baldissara S, Scotti R.<br />
Reliability <strong>of</strong> tactile perception<br />
using sharp <strong>and</strong> dull explorers in<br />
marginal opening identification. Int<br />
J Prosthodont 1998;11(6):591-594.<br />
54. Tibbets LS, Shanelec D. Periodontal<br />
microsurgery. Dent Clin North Am<br />
1998;42(2):339-359.<br />
55. Leknius C, Geissberger M. The<br />
effect <strong>of</strong> magnification on the<br />
COVER FEATURE<br />
performance <strong>of</strong> fixed prosthodontic<br />
procedures. J Calif Dent Assoc<br />
1995;23(12):66-70.<br />
56. Zaugg B, Stassinakis A, Hotz P.<br />
Einfluss von vergrösserungshilfen<br />
auf die erkennung nachgestellter<br />
präparations- und füllungsfehler<br />
[Influence <strong>of</strong> magnification tools on<br />
the recognition <strong>of</strong> simulated preparation<br />
<strong>and</strong> filling errors]. Schweiz<br />
Monatsschr Zahnmed<br />
2004;114(9):890-896.<br />
57. Lunn R, Sunell S. Posture, position<br />
<strong>and</strong> surgical telescopes in dental<br />
hygiene. J Dent Educ<br />
1996;60(2):122.<br />
58. Rucker LM. Surgical magnification:<br />
Posture maker or posture breaker?<br />
Chapter 8 in: Murphy DC, editor.<br />
Ergonomics <strong>and</strong> the dental care<br />
worker. Washington, DC: American<br />
Public Health Association,<br />
1998:191-216.<br />
59. Valachi B, Valachi K. Mechanisms<br />
leading to musculoskeletal disorders<br />
in dentistry. J Am Dent Assoc<br />
2003;134(10):1344-1350.<br />
60. Valachi B, Valachi K. Preventing<br />
musculoskeletal disorders in clinical<br />
dentistry: Strategies to address the<br />
mechanisms leading to musculoskeletal<br />
disorders. J Am Dent<br />
Assoc 2003;134(12):1604-1612.<br />
61. Carr GB. Microscopic photography<br />
for the restorative dentist. J Esthet<br />
Restor Dent 2003;15(7):417-425.<br />
62. Behle C. Photography <strong>and</strong> the operating<br />
microscope in dentistry. J Calif<br />
Dent Assoc 2001;29(10):765-771.<br />
63. van As GA. Digital documentation<br />
<strong>and</strong> the dental operating microscope.<br />
Oral Health<br />
2001;91(12):19-20, 22-25.<br />
64. van As G. Erbium lasers in<br />
dentistry. Dent Clin North Am<br />
2004;48(4):1017-1059.<br />
65. Britto LR, Veazey WS, Manasse GR.<br />
Personal video monitor as an accessory<br />
to dental operating<br />
microscopes. Quintessence Int<br />
2004;35(2):151-154. ■■<br />
JOUR NAL OF LASER DENTIS TRY | 2007 VOL 15, NO. 3<br />
129
JOUR NAL OF LASER DENTIS TRY | 2007 VOL 15, NO. 3<br />
130<br />
SCIENTIFIC REVIEW<br />
Detection <strong>of</strong> Caries by DIAGNOdent:<br />
Scientific Background <strong>and</strong> Performance<br />
Raimund Hibst, PhD, Institut für <strong>Laser</strong>technologien in der Medizin und Meßtechnik (ILM),<br />
Ulm, Germany<br />
J <strong>Laser</strong> Dent 2007;15(3):130-134<br />
SYNOPSIS<br />
Pr<strong>of</strong>essor Hibst was one <strong>of</strong> the inventors <strong>of</strong> the DIAGNOdent laser<br />
fluorescence caries detection device. This article provides a review <strong>of</strong><br />
the history, mechanism <strong>of</strong> action, <strong>and</strong> application <strong>of</strong> the device.<br />
INTRODUCTION<br />
The process <strong>of</strong> dental caries is<br />
accompanied by changes in the<br />
optical properties <strong>of</strong> the affected<br />
enamel or dentin. These changes in<br />
scattering, absorption, or fluorescence<br />
are the basis <strong>of</strong> visual/optical<br />
detection <strong>of</strong> carious lesions. First,<br />
demineralization <strong>of</strong> enamel results<br />
in an enlargement <strong>of</strong> intercrystalline<br />
spaces, which makes the tissue less<br />
homogeneous <strong>and</strong> results in an<br />
increase in light scattering (especially<br />
when the tooth is dried). As a<br />
result, decalcified enamel becomes<br />
visible as a highly scattering “white<br />
spot.” Later, the presence <strong>of</strong> chromophores<br />
in the lesion enhances<br />
light absorption so that the carious<br />
lesion appears brownish.<br />
A further tissue property which is<br />
affected by caries is fluorescence.<br />
Fluorescence is the re-emission <strong>of</strong><br />
light by molecules after absorption.<br />
The fluorescence light always has a<br />
longer wavelength than the excitation<br />
light used for illumination. Its<br />
specific spectrum depends on the<br />
excitation wavelength <strong>and</strong> the molecular<br />
species. A variety <strong>of</strong> biological<br />
molecules shows fluorescence, especially<br />
proteins. Fluorescence <strong>of</strong> teeth<br />
on ultraviolet (UV) excitation was<br />
first described nearly one century<br />
ago. 1 When teeth were illuminated<br />
with invisible UV light from a Wood’s<br />
lamp, a bright fluorescence was<br />
observed by the naked eye. As early<br />
as 1927 it was noted that plaque<br />
shows different fluorescence properties<br />
when compared to sound tooth<br />
necks. 2 While all the early studies<br />
were performed with UV-excitation,<br />
the first experiments with visible<br />
light were reported beginning in<br />
1981. 3 In general, the investigations<br />
with UV, blue or green excitation<br />
light revealed a strong fluorescence<br />
<strong>of</strong> enamel, which is slightly altered<br />
when the tissue becomes carious.<br />
This phenomenon allows detection <strong>of</strong><br />
demineralization in the outer surface<br />
regions (sometimes referred to as<br />
quantitative laser / light fluorescence,<br />
or QLF). However, strongly<br />
fluorescing healthy enamel optically<br />
masks changes in deeper layers, as<br />
scattering does, so that deeper<br />
lesions covered by intact tissue are<br />
difficult to detect by direct fluorescence<br />
changes.<br />
R ED EXCITED<br />
FLUORESCENCE<br />
The detection <strong>of</strong> hidden (occlusal)<br />
caries requires a low fluorescence<br />
from the overlying sound enamel,<br />
<strong>and</strong> a stronger emission from the<br />
lesion. Such a situation was found<br />
when excitation by red light was<br />
investigated. 4-6 Experiments showed<br />
that fluorescence yield decreased for<br />
longer excitation wavelengths, as<br />
expected, but this decrease was<br />
much more pronounced for sound<br />
surfaces than for carious lesions.<br />
With red light excitation (e.g., 655<br />
nm) carious lesions fluoresce much<br />
ABSTRACT<br />
Caries covered by macroscopically<br />
intact enamel can be detected by<br />
irradiating the teeth with red light<br />
<strong>and</strong> capturing the re-emitted<br />
infrared fluorescence radiation.<br />
This fluorescence originates from<br />
metabolites produced by caries<br />
bacteria. The optical caries<br />
detector DIAGNOdent ® measures<br />
this fluorescence <strong>and</strong> displays its<br />
intensity as a number. The instrument<br />
can detect hidden caries<br />
better than traditional methods<br />
<strong>and</strong> enables longitudinal monitoring<br />
<strong>of</strong> lesions. In order to avoid<br />
false positive diagnostic decisions,<br />
one should pay attention that<br />
calculus, stains, <strong>and</strong> some filling<br />
materials can also show fluorescence<br />
similar to caries lesions.<br />
more strongly. This is true across<br />
the entire emission wavelength<br />
range. Thus all fluorescence can be<br />
used for differentiation <strong>of</strong> healthy<br />
<strong>and</strong> diseased tissue. The possibility<br />
to utilize the total fluorescence light<br />
is an advantage <strong>of</strong> red excitation,<br />
which compensates in part for the<br />
lower intensities compared to excitation<br />
with shorter wavelengths.<br />
The considerable contrast between<br />
carious <strong>and</strong> sound enamel, or<br />
dentin, respectively, obtained for red<br />
excitation is demonstrated in Figure<br />
1, which shows a hemisectioned<br />
tooth <strong>and</strong> the corresponding fluorescence<br />
image. Both carious sites are<br />
clearly marked on the very low<br />
background fluorescence level. This<br />
<strong>of</strong>fers a very elegant way to detect<br />
caries, because only the bright fluorescence<br />
spots in an otherwise dark<br />
environment are readily observed.<br />
This does not require 2-dimensional<br />
images <strong>and</strong> analysis. Additionally,<br />
Hibst
Figure 1: Hemisectioned tooth with approximal <strong>and</strong> occlusal caries<br />
Normal image with white light<br />
illumination<br />
the detection <strong>of</strong> hidden caries is<br />
possible, since the weaker sound<br />
enamel fluorescence does not<br />
completely mask the signal from a<br />
deeper lesion. Red light, <strong>and</strong> also<br />
infrared fluorescence radiation, is<br />
less absorbed <strong>and</strong> scattered by<br />
enamel than light <strong>of</strong> shorter wavelengths,<br />
so that in general red <strong>and</strong><br />
infrared light penetrates deeper into<br />
the tooth. This also helps to increase<br />
the depth that can be examined.<br />
FLUOROPHORE<br />
I DENTIF ICATION 6<br />
In order to find the origin <strong>of</strong> fluorescence,<br />
one has to consider both<br />
the baseline fluorescence <strong>of</strong> sound<br />
dental tissue <strong>and</strong> its increase<br />
during the carious process.<br />
Sound enamel <strong>and</strong> dentin<br />
exhibit a low, but observable, fluorescence.<br />
The dominant component<br />
<strong>of</strong> enamel <strong>and</strong> dentin is the substituted<br />
hydroxyapatite (HA) calcium<br />
phosphate mineral. Experiments<br />
with pellets pressed out <strong>of</strong><br />
powdered HA <strong>and</strong> various other<br />
calcium phosphates revealed very<br />
low signals. So it seems unlikely<br />
that calcium phosphates are<br />
responsible for the baseline fluorescence<br />
<strong>of</strong> sound teeth. By comparing<br />
teeth with different color one can<br />
Hibst<br />
Fluorescence image in false colors<br />
(655-nm excitation)<br />
observe that whiter teeth exhibit<br />
less fluorescence compared to<br />
darker ones. Presumably the same<br />
stains cause color <strong>and</strong> fluorescence.<br />
Demineralized enamel that was<br />
produced by chemical decalcification<br />
did not significantly enhance<br />
fluorescence. This corresponds to<br />
the finding <strong>of</strong> low calcium phosphate<br />
fluorescence described above.<br />
That is, simply removing mineral<br />
from these hard tissues does not<br />
significantly alter the fluorescence.<br />
Carious lesions show microscopically<br />
a strong correlation between<br />
brownish discoloration <strong>and</strong> fluorescence,<br />
so that brown chromophores<br />
might also act as fluorophores<br />
(substances that fluoresce). Besides<br />
natural carious lesions, calculus <strong>of</strong><br />
various types also fluoresce under<br />
red light, including white calculus.<br />
So besides the brown pigments other<br />
fluorophores can be present. Likely<br />
c<strong>and</strong>idates are bacteria or bacterial<br />
metabolites. To test this hypothesis,<br />
bacteria from carious lesions were<br />
incubated on blood agar <strong>and</strong><br />
analyzed by fluorescence microscopy. 6<br />
Both the bacterial colonies <strong>and</strong> the<br />
surrounding agar showed fluorescence.<br />
Agar fluorescence decreased<br />
with increasing distance from the<br />
colonies, indicating that there are<br />
SCIENTIFIC REVIEW<br />
diffusible bacterial metabolites fluorescing<br />
under red light excitation<br />
(Figure 2). C<strong>and</strong>idates for bacterial<br />
metabolites that fluoresce could be<br />
the so-called porphyrins. Porphyrins<br />
occur as intermediate steps in the<br />
synthesis <strong>of</strong> heme, <strong>and</strong> are also<br />
produced by several types <strong>of</strong> oral<br />
bacteria, such as Prevotella intermedia<br />
or Porphyromonas gingivalis.<br />
In earlier work, porphyrins, especially<br />
Protoporphyrine IX (PPIX),<br />
indeed could be extracted from<br />
carious lesions <strong>and</strong> were demonstrated<br />
to be useful in differentiating<br />
caries from sound tooth structure by<br />
violet (406 nm) excited fluorescence. 7<br />
Although fluorescence yield is<br />
maximal for this short wavelength<br />
excitation, porphyrins were known to<br />
also show some fluorescence when<br />
excited by red light. Solutions <strong>of</strong><br />
these molecules also fluoresce with<br />
655-nm excitation, <strong>and</strong> their emission<br />
spectra are very similar to those<br />
found for caries.<br />
Other substances occurring naturally<br />
in the mouth, like water, saliva,<br />
blood, or s<strong>of</strong>t tissue do not exhibit<br />
fluorescence with red light excitation<br />
<strong>and</strong> thus do not interfere with caries<br />
detection. In contrast, chlorophyll<br />
does fluoresce, so that stains originating<br />
from food (leaves, wine, etc.)<br />
must also be considered as an origin<br />
<strong>of</strong> fluorescence (see below).<br />
DETECTOR SY S TEM<br />
AND APPLICATION<br />
On the basis <strong>of</strong> the investigations<br />
described above the optical caries<br />
detector DIAGNOdent ® (DD) was<br />
developed as a joint project<br />
between the Institut für<br />
<strong>Laser</strong>technologien in der Medizin<br />
und Meßtechnik (ILM, Ulm,<br />
Germany) <strong>and</strong> Kaltenbach <strong>and</strong><br />
Voigt (KaVo, Biberach, Germany).<br />
The set-up <strong>and</strong> function are as<br />
follows. Light from a laser diode<br />
(655 nm) is coupled into an optical<br />
fiber <strong>and</strong> transmitted to the tooth.<br />
The excitation fiber is surrounded<br />
by a bundle <strong>of</strong> fibers which gather<br />
fluorescence as well as backscattered<br />
light <strong>and</strong> guide it to the<br />
JOUR NAL OF LASER DENTIS TRY | 2007 VOL 15, NO. 3<br />
131
JOUR NAL OF LASER DENTIS TRY | 2007 VOL 15, NO. 3<br />
132<br />
SCIENTIFIC REVIEW<br />
Figure 2: Fluorescence microscopic study <strong>of</strong> caries-related bacteria<br />
Figure 2a Figure 2b<br />
detection unit (Figure 3). By the use<br />
<strong>of</strong> a b<strong>and</strong> pass filter in front <strong>of</strong> the<br />
photo diode detector, the backscattered<br />
excitation <strong>and</strong> short<br />
wavelength ambient light is<br />
absorbed. To discriminate the fluorescence<br />
from the ambient light in<br />
the same spectral region, the laser<br />
diode is modulated (i.e., the laser<br />
diode intensity is varied with a<br />
certain frequency). Due to its relatively<br />
short lifetime, fluorescence<br />
follows this modulation. By amplifying<br />
only the modulated portion <strong>of</strong><br />
the signal, the ambient light is<br />
suppressed. The remaining signal is<br />
proportional to the detected fluorescence<br />
intensity <strong>and</strong> displayed as a<br />
number (0 to 99, in arbitrary units).<br />
In order to compensate for potential<br />
variations <strong>of</strong> the system (e.g., laser<br />
diode output power), the device can<br />
be calibrated by a ceramic st<strong>and</strong>ard<br />
<strong>of</strong> known <strong>and</strong> stable fluorescence<br />
yield. This makes the measurement<br />
absolute (although in arbitrary<br />
units) <strong>and</strong> allows comparisons <strong>of</strong><br />
fluorescing tooth spots over time.<br />
Tests on solutions <strong>of</strong> varying PPIX<br />
concentrations demonstrated a<br />
linear response <strong>of</strong> the system (when<br />
the fluorophore concentration is<br />
increased by a factor <strong>of</strong> x, the signal<br />
increases by the same factor).<br />
Sensitivity was tested by applying<br />
small droplets <strong>of</strong> PPIX solution onto<br />
the enamel or dentin area <strong>of</strong> a<br />
hemisectioned tooth. On average 1<br />
picomole <strong>of</strong> PPIX results in a signal<br />
increase <strong>of</strong> 4 DD units. This<br />
compares to the baseline levels <strong>of</strong><br />
sound teeth, <strong>and</strong> would be the<br />
detectable amount <strong>of</strong> porphyrins in<br />
superficial carious lesions. 6<br />
Figure 3: Schematic <strong>of</strong> the optical set-up<br />
<strong>of</strong> the DIAGNOdent caries detector device<br />
Figure 2c<br />
Figure 2a: Light microscopy <strong>of</strong> two<br />
different bacterial colonies on agar<br />
Figure 2b: Corresponding fluorescence<br />
image. Note the fluorescence also from<br />
the agar surrounding the colonies<br />
Figure 2c: Relative fluorescence intensity<br />
along the line marked on the image in<br />
Figure 2b<br />
In practical use the DD should be<br />
calibrated regularly (maybe daily) to<br />
assure comparable readings over<br />
time. After the tooth is cleaned, a<br />
sound spot on the smooth surface is<br />
measured in order to provide a<br />
baseline value. This value is then<br />
subtracted electronically from the<br />
fluorescence <strong>of</strong> the site to be measured.<br />
In order to measure <strong>and</strong><br />
capture the signal from the entire<br />
carious lesion, the instrument has<br />
to be tilted around the measuring<br />
site. This ensures that the tip picks<br />
up fluorescence from the slopes <strong>of</strong><br />
the fissure walls where the caries<br />
process <strong>of</strong>ten begins. A rising<br />
audible tone helps the examiner to<br />
find the maximum fluorescence<br />
value <strong>of</strong> the site under study. 9<br />
P ERFORMANCE<br />
A literature search (with Scopus;<br />
“DIAGNOdent” in title, keywords,<br />
or abstract) yields about 110<br />
published articles on the DD. A<br />
Hibst
large portion <strong>of</strong> these address questions<br />
concerning its:<br />
• reproducibility, reliability (probability<br />
that two measurements by<br />
the same (intraexaminer) or<br />
different (interexaminer)<br />
observers lead to the same result<br />
• sensitivity (ratio: true positive /<br />
(true positive + false negative),<br />
i.e., probability to correctly identify<br />
carious lesions)<br />
• specificity (ratio: true negative /<br />
(true negative + false positive),<br />
i.e., probability to correctly identify<br />
sound teeth).<br />
A systematic review on the DD<br />
performance 8 reveals persistent<br />
high intraexaminer <strong>and</strong> slightly<br />
lower but still good interexaminer<br />
reliability. The results on sensitivity<br />
<strong>and</strong> specificity are variable<br />
among the studies; the data range<br />
for the majority is given in Table 1.<br />
Sensitivity <strong>and</strong> specificity depend<br />
on the cut-<strong>of</strong>f values used as the<br />
threshold to discriminate carious<br />
from sound tissue. As the threshold<br />
is lowered, more lesions are detected<br />
at the price <strong>of</strong> an increasing number<br />
<strong>of</strong> false positives. The few reported<br />
in vivo studies yielded a better<br />
performance than the majority <strong>of</strong> in<br />
vitro investigations. This might be<br />
due to changes in optical properties<br />
after extraction <strong>of</strong> the teeth<br />
(increase <strong>of</strong> scattering, loss <strong>of</strong> fluorescence).<br />
In the in vivo studies, a<br />
threshold <strong>of</strong> 20 DD units was chosen<br />
(in one study, 30). This can serve as<br />
guidance for the user’s (individually<br />
variable) threshold value.<br />
C ONCLUSION<br />
In conclusion, “the DD is clearly<br />
more sensitive than traditional diagnostic<br />
methods.” 8 However, the<br />
increased likelihood <strong>of</strong> false positive<br />
readings compared with that <strong>of</strong><br />
visual methods gives rise to some<br />
concern. The specificity found in the<br />
studies would mathematically<br />
predict numerous unnecessary treatments<br />
for a collective <strong>of</strong> patients<br />
with low caries prevalence. However:<br />
• First, the studies were performed<br />
on samples with very high caries<br />
Hibst<br />
Table 1: Data Ranges for DIAGNOdent Performance *<br />
Condition Sensitivity Specificity<br />
prevalence (typically 20 to 50%)<br />
with numerous suspicious areas.<br />
Specificity with respect to these<br />
samples cannot be extrapolated to<br />
the general situation, since the<br />
DD will never show an increased<br />
signal for completely intact white<br />
teeth. The reason for false positive<br />
readings is always fluorescence,<br />
originating from stains (see<br />
above), calculus, or filing material.<br />
• Secondly, the DD is a detector<br />
<strong>and</strong> not a “diagnostic robot.” Its<br />
readings should be interpreted in<br />
the context <strong>of</strong> the situation. For<br />
example, if fissures <strong>of</strong> a tooth<br />
exhibit increased fluorescence<br />
but the surrounding area does<br />
not, it is more likely that it originates<br />
from superficial stain than<br />
from deeper caries. Even in the<br />
presence <strong>of</strong> fluorescing composites,<br />
information can be gained:<br />
An increase <strong>of</strong> fluorescence from<br />
the center to the periphery would<br />
indicate additional fluorophores<br />
(= caries) at the margin.<br />
In contrast to visual inspection<br />
(<strong>and</strong> also radiography), the DD<br />
provides quantitative data. These are<br />
not directly reflecting to “classical”<br />
lesion parameters like mineral loss<br />
or depth extension, but are related to<br />
the amount <strong>of</strong> fluorescing<br />
porphyrins. Since bacterial<br />
porphyrins accumulate in demineralized<br />
areas <strong>of</strong> increased depth <strong>and</strong><br />
porosity, more severe lesions typically<br />
have higher concentrations <strong>of</strong><br />
porphyrins. Therefore DD readings<br />
may provide quantitative data that<br />
can be related to the severity <strong>of</strong> tooth<br />
decay. DD readings are highly reproducible<br />
<strong>and</strong> this allows longitudinal<br />
SCIENTIFIC REVIEW<br />
Results<br />
Obtained in:<br />
enamel caries in vitro 0.72 - 0.95 0.68 - 0.95 9 <strong>of</strong> 13 studies<br />
dentinal caries in vitro 0.73 - 1.0 0.65 - 1.0 14 <strong>of</strong> 16 studies<br />
dentinal caries in vivo 0.92 - 0.96 0.63 - 0.86 3 <strong>of</strong> 4 studies<br />
*Based on data collected by Bader <strong>and</strong> Shugars from the majority <strong>of</strong> published studies on occlusal<br />
lesions. Bader JD, Shugars DA. A systematic review <strong>of</strong> the performance <strong>of</strong> a laser fluorescence<br />
device for detecting caries. J Am Dent Assoc 2004;135(10):1413-1426.<br />
monitoring <strong>of</strong> lesions. In all questionable<br />
situations with moderate<br />
fluorescence signals, it is reasonable<br />
to follow up the suspicious site at<br />
periodic examinations. Increasing<br />
fluorescence signals would indicate a<br />
progression <strong>of</strong> the lesion <strong>and</strong> thus<br />
indicate enhanced preventive or<br />
operative treatment. However, it is<br />
important to remember that the<br />
increase in fluorescence is a result <strong>of</strong><br />
more absorption <strong>of</strong> external fluorophores<br />
into the more porous tooth<br />
structure, rather than directly<br />
detecting lesion size or extent.<br />
Recently, a miniaturized version<br />
<strong>of</strong> the DD was released<br />
(DIAGNOdent ® pen). First comparisons<br />
show that the new device<br />
performs on occlusal surfaces as well<br />
as the “classic” DIAGNOdent. 10<br />
AUTHOR BIOGRAPHY<br />
Raimund Hibst has been educated in<br />
physics <strong>and</strong> biology. He received a<br />
PhD degree in physics from the<br />
University <strong>of</strong> Bochum, the venia<br />
legendi in biomedical engineering<br />
from the University <strong>of</strong> Ulm in 1995<br />
(medical faculty), <strong>and</strong> in 2000 he<br />
became pr<strong>of</strong>essor for laser <strong>and</strong><br />
dental technologies (Faculty <strong>of</strong><br />
Engineering, University <strong>of</strong> Ulm).<br />
Since 1986 he has been with the<br />
Institut für <strong>Laser</strong>technologien in der<br />
Medizin und Meßtechnik, Ulm,<br />
Germany, where he is actually associate<br />
director <strong>and</strong> the head <strong>of</strong> the<br />
Dental Technology Center. His<br />
special interest is in optical methods<br />
in dentistry. Among his projects has<br />
been the development <strong>of</strong> an Er:YAG<br />
laser system for dental <strong>and</strong> oral therapeutic<br />
applications (KEY <strong>Laser</strong> ® )<br />
JOUR NAL OF LASER DENTIS TRY | 2007 VOL 15, NO. 3<br />
133
JOUR NAL OF LASER DENTIS TRY | 2007 VOL 15, NO. 3<br />
134<br />
SCIENTIFIC REVIEW<br />
<strong>and</strong> caries detection by fluorescence,<br />
which is also now used in clinical<br />
practice (DIAGNOdent ® ). The<br />
Er:YAG laser research was awarded<br />
by the University <strong>of</strong> Ulm in 1990. In<br />
1998 he received the award for best<br />
cooperation with industry. Raimund<br />
Hibst is an editor <strong>of</strong> the journal<br />
Medical <strong>Laser</strong> Application <strong>and</strong> a<br />
board member <strong>of</strong> several journals.<br />
Dr. Hibst may be contacted by e-mail<br />
at raimund.hibst@ilm.uni-ulm.de.<br />
Disclosure: The caries detector<br />
DIAGNOdent has been developed in<br />
cooperation between ILM <strong>and</strong> KaVo. It<br />
is based on an invention made by the<br />
author <strong>and</strong> coworkers. For this, ILM<br />
receives royalties from KaVo which in<br />
part are passed down to the inventors.<br />
REFERENCES<br />
1. Stübel H. Die fluoreszenz tierischer<br />
gewebe in ultraviolettem licht. [The<br />
fluorescence <strong>of</strong> animal tissues by<br />
irradiation with ultraviolet light.]<br />
Pflugers Arch Gesamte Physiol<br />
Menschen Tiere 1911;142:1-14.<br />
2. Bommer S. Hautuntersuchungen im<br />
gefilterten Quarzlicht.<br />
[Investigations on skin with filtered<br />
quartz light.] Klin Wochenschr<br />
1927;6(24):1142-1144.<br />
3. Alfano RR, Yao SS. Human teeth<br />
with <strong>and</strong> without dental caries<br />
studied by visible luminescence<br />
spectroscopy. J Dent Res<br />
1981;60(2):120-122.<br />
4. Hibst R, Gall R. Development <strong>of</strong> a<br />
diode laser-based fluorescence caries<br />
detector. Caries Res 1998;32(4):294,<br />
abstract 80.<br />
5. Hibst R, Paulus, R. A new approach<br />
on fluorescence spectroscopy for<br />
caries detection. In: Featherstone<br />
JDB, Rechmann P, Fried D, editor.<br />
<strong>Laser</strong>s in dentistry V, January 24-<br />
25, 1999, San Jose, California. Proc<br />
SPIE 3593. SPIE – The<br />
International Society for Optical<br />
Engineering, Bellingham,<br />
Washington, 1999:141-147.<br />
6. Hibst R, Paulus R, Lussi A.<br />
Detection <strong>of</strong> occlusal caries by laser<br />
fluorescence: Basic <strong>and</strong> clinical<br />
investigations. Med <strong>Laser</strong> Appl<br />
2001;16(3):205-213.<br />
7. König K, Hibst R, Meyer H,<br />
Flemming G, Schneckenburger H.<br />
<strong>Laser</strong>-induced aut<strong>of</strong>luorescence <strong>of</strong><br />
carious regions <strong>of</strong> human teeth <strong>and</strong><br />
caries-involved bacteria. In: Altshuler<br />
GB, Hibst R, editor. Dental applications<br />
<strong>of</strong> lasers, September 1-2, 1993,<br />
Budapest, Hungary. Proc SPIE 2080.<br />
SPIE – The International Society for<br />
Optical Engineering, Bellingham,<br />
Washington, 1993:170-180.<br />
8. Bader JD, Shugars DA. A systematic<br />
review <strong>of</strong> the performance <strong>of</strong> a<br />
laser fluorescence device for<br />
detecting caries. J Am Dent Assoc<br />
2004;135(10):1413-1426.<br />
9. Lussi A, Hibst R, Paulus R.<br />
DIAGNOdent: An optical method for<br />
caries detection. J Dent Res<br />
2004;83(Spec. Issue C):C80-C83.<br />
10. Lussi A, Hellwig E. Performance <strong>of</strong><br />
a new laser fluorescence device for<br />
the detection <strong>of</strong> occlusal caries in<br />
vitro. J Dent 2006;34(7):467-471.<br />
For additional references, see the works<br />
cited within references 6, 8, <strong>and</strong> 9,<br />
above. ■■<br />
Hibst
Reyhanian et al.<br />
CLINICAL REVIEW AND CASE REPORT<br />
Er:YAG <strong>Laser</strong>-Assisted Implant Periapical<br />
Lesion Therapy (IPL) <strong>and</strong> Guided Bone<br />
Regeneration (GBR) Technique:<br />
New Challenges <strong>and</strong> New Instrumentation<br />
Avi Reyhanian, DDS, Netanya, Israel; Donald J. Coluzzi, DDS, Redwood City, California<br />
J <strong>Laser</strong> Dent 2007;15(3):135-141<br />
SYNOPSIS<br />
The etiology <strong>and</strong> predisposing factors <strong>of</strong> implant periapical lesions<br />
are described <strong>and</strong> a case report <strong>of</strong> treatment using an Er:YAG laser is<br />
presented.<br />
INTRODUCTION<br />
Osseointegrated implants have been<br />
utilized as a successful treatment<br />
modality over three decades, with a<br />
high reported success rate, greater<br />
than 90 percent. 1-4 The predictability<br />
<strong>and</strong> high rate <strong>of</strong> success <strong>of</strong> dental<br />
implants makes them a st<strong>and</strong>ard<br />
treatment modality. Oftentimes in<br />
spite <strong>of</strong> exacting planning <strong>and</strong><br />
precise placement accompanying the<br />
procedure, implant failure can <strong>and</strong><br />
does still occur. 5-8 A small number <strong>of</strong><br />
implants fail because <strong>of</strong> operator<br />
inexperience or clinically recognizable<br />
cause. Their widespread use in<br />
recent years has produced different<br />
types <strong>of</strong> complications which can be<br />
divided into two categories:<br />
1. Intraoperative Complications<br />
• Bleeding<br />
• Nerve injury<br />
• M<strong>and</strong>ibular fractures<br />
• Implant displacements<br />
• Accidental bone perforations<br />
• Incomplete flap closure<br />
2. Postoperative Complications<br />
• Mucositis <strong>and</strong> peri-implantitis<br />
• Implant periapical lesion (IPL)<br />
• Surgical wound dehiscence<br />
• Lesions on adjacent teeth<br />
• Incomplete osseointegration.<br />
Recent case reports introduced<br />
the term retrograde peri-implantitis<br />
as a lesion (radiolucency)<br />
around the most apical part <strong>of</strong> an<br />
osseointegrated implant. 9-11 It<br />
develops within the first month<br />
after insertion <strong>of</strong> the implant.<br />
The Etiology <strong>of</strong> Implant<br />
6, 9-10, 12-15<br />
Periapical Lesion<br />
1. Contamination <strong>of</strong> the implant<br />
surface<br />
10, 16-18<br />
2. Overheating <strong>of</strong> bone<br />
3. Overloading <strong>of</strong> the implant19 4. Presence <strong>of</strong> preexisting bone <strong>and</strong><br />
12, 16, 20<br />
microbial pathology<br />
5. Presence <strong>of</strong> residual root fragments<br />
<strong>and</strong> foreign bodies in bone21 6. Implant placement in an infected<br />
maxillary sinus<br />
7. Implant placement in a poor<br />
bone quality site22-23 8. Lack <strong>of</strong> biocompatibility<br />
9. Excessive tightening <strong>of</strong> the<br />
implant <strong>and</strong> compression <strong>of</strong> the<br />
bone chips inside the apical hole,<br />
16, 24<br />
producing subsequent necrosis<br />
9, 16<br />
10. Contaminated implants.<br />
Predisposing Factors 25<br />
1. Patient characteristics: age,<br />
medical history<br />
ABSTRACT<br />
Osseointegrated implants have<br />
enjoyed a success rate <strong>of</strong> more<br />
than 90 percent. There are several<br />
reasons for failure including challenges<br />
during placement <strong>and</strong><br />
postoperative complications.<br />
This article will discuss one <strong>of</strong><br />
those failures, the implant periapical<br />
lesion (IPL) which is an<br />
accumulation <strong>of</strong> granulation tissue<br />
around the apical area <strong>of</strong> an<br />
implant. It is manifested as a radiographic<br />
radiolucency, <strong>and</strong> results<br />
in compromised osseous health<br />
<strong>and</strong> <strong>of</strong>ten requires the removal <strong>of</strong><br />
the implant fixture.<br />
The etiology <strong>and</strong> predisposing<br />
factors <strong>of</strong> IPL will be enumerated,<br />
<strong>and</strong> descriptions <strong>of</strong> the classification,<br />
prevention, <strong>and</strong> treatment <strong>of</strong><br />
IPL will be elaborated.<br />
A clinical case <strong>of</strong> IPL, treated<br />
with an erbium:YAG laser, will be<br />
presented. The detailed clinical<br />
protocol will be described. The<br />
seven-month postoperative clinical<br />
<strong>and</strong> radiographic findings show<br />
complete reversal <strong>of</strong> the lesion<br />
<strong>and</strong> change the prognosis from<br />
hopeless to good for the implant.<br />
2. Recipient site: local bone quality<br />
<strong>and</strong> quantity, cause <strong>of</strong> tooth loss 22,<br />
26-27<br />
3. Periodontal <strong>and</strong> endodontic<br />
7, 28<br />
conditions <strong>of</strong> neighboring teeth<br />
4. Implant characteristics: length,<br />
22, 29-32<br />
surface characteristics<br />
5. Surgical aspect: guided bone<br />
regeneration, osseous fenestration,<br />
or dehiscence. 10<br />
JOUR NAL OF LASER DENTIS TRY | 2007 VOL 15, NO. 3<br />
135
JOUR NAL OF LASER DENTIS TRY | 2007 VOL 15, NO. 3<br />
136<br />
CLINICAL REVIEW AND CASE REPORT<br />
Figure 1: An example radiograph <strong>of</strong> inactive<br />
implant periapical lesion around two<br />
implants<br />
Classification<br />
A classification <strong>of</strong> implant periapical<br />
lesions has been suggested that<br />
separate them into two categories:<br />
inactive <strong>and</strong> infected. 9 The inactive<br />
form is likely to appear as an apical<br />
scar, resulting from a residual bone<br />
cavity created by placing an implant<br />
that was shorter than the prepared<br />
drill site. An example is shown in<br />
Figure 1. The infected form occurs<br />
when an implant apex is placed in<br />
proximity to an existing infection or<br />
when a contaminated implant is<br />
placed (Figure 2).<br />
Prevention <strong>and</strong> Treatment<br />
Suggested preventions <strong>of</strong> implant<br />
periapical lesion include careful<br />
management <strong>of</strong> contaminants <strong>and</strong><br />
heat generation during implant<br />
surgery.<br />
Treatment would vary according<br />
to the type <strong>of</strong> lesion. The inactive<br />
type is observed <strong>and</strong> monitored.<br />
The infected type requires surgical<br />
intervention, debridement <strong>of</strong> the<br />
infected lesion, systemic antibiotic,<br />
<strong>and</strong>/or guided bone regeneration.<br />
An implant apical resection or<br />
implant removal could be<br />
performed depending on the extent<br />
<strong>of</strong> the infection <strong>and</strong> the stability <strong>of</strong><br />
6, 9, 12, 27, 33<br />
the implant.<br />
The Use <strong>of</strong> Er:YAG <strong>Laser</strong> in IPL<br />
Treatment 34-37<br />
• The erbium laser can make the<br />
initial flap incision, such as a<br />
crestal incision, or an intrasul-<br />
Figure 2: An example radiograph <strong>of</strong> an<br />
infected implant periapical lesion. The<br />
implant was later extracted<br />
cular or vertical releasing incision.<br />
The laser produces a wet<br />
incision (some bleeding) vs. a dry<br />
incision (no bleeding) such as that<br />
34, 36-38<br />
produced by the CO2 laser.<br />
• After the flap is raised, the<br />
erbium laser is also very efficient<br />
at vaporization <strong>of</strong> any granulation<br />
tissue, 34-35 with a lower risk<br />
<strong>of</strong> thermal damage to the bone<br />
than current diode or CO 2<br />
34, 39-40<br />
lasers.<br />
• The erbium laser provides detoxification<br />
<strong>of</strong> implant surfaces. 41<br />
Studies have demonstrated this<br />
laser’s bactericidal potential. 42-43<br />
• Furthermore, implant surface<br />
threads can be disinfected<br />
without damage by lasing<br />
directly on their surfaces with a<br />
low energy. 44-46<br />
• The erbium laser is also efficient<br />
at remodeling, shaping, <strong>and</strong><br />
34, 36, 38, 47-48<br />
ablating necrotic bone.<br />
CASE OVERVIEW<br />
This case describes the use <strong>of</strong> an<br />
Er:YAG laser in treatment <strong>of</strong> periimplantitis<br />
<strong>of</strong> an implant periapical<br />
lesion <strong>and</strong> the advantages <strong>of</strong> this<br />
laser wavelength in performing a<br />
guided bone regeneration (GBR)<br />
technique versus conventional<br />
methods.<br />
Figure 3: Labial fistula on implant at<br />
tooth #7<br />
Examination<br />
A 56-year-old female presented<br />
with a noncontributory medical<br />
history. She was not taking any<br />
medications. She presented two<br />
months after she had 4 implants<br />
placed in the maxillary anterior<br />
area for teeth #7, 8, 9, <strong>and</strong> 10. The<br />
fixtures <strong>of</strong> #8 <strong>and</strong> 9 had failed the<br />
previous month <strong>and</strong> were removed;<br />
the implant for #10 was integrating<br />
normally, but #7 was<br />
compromised.<br />
Figure 4: X-ray image <strong>of</strong> the periapical<br />
lesion<br />
Reyhanian et al.
The patient had fair oral hygiene<br />
<strong>and</strong> brushed <strong>and</strong> flossed daily.<br />
Periodontal probing showed 3-mm<br />
pockets with no bleeding. The<br />
implant for tooth #7 was nonsubmerged<br />
<strong>and</strong> a labial fistula was<br />
present; furthermore, insertion <strong>of</strong> a<br />
probe into the fistula led to the end<br />
<strong>of</strong> the implant, <strong>and</strong> revealed loss <strong>of</strong><br />
facial bone on the buccal side <strong>of</strong> the<br />
implant (Figure 3). The s<strong>of</strong>t tissue<br />
around the failed implants in the<br />
area <strong>of</strong> #8 <strong>and</strong> 9 had healed well,<br />
the implant at the location <strong>of</strong> #10<br />
was submerged without s<strong>of</strong>t tissue<br />
complications, <strong>and</strong> all other oral<br />
s<strong>of</strong>t tissue appeared normal.<br />
Panoramic <strong>and</strong> periapical films<br />
showed a radiolucent area around<br />
the apical portion <strong>of</strong> the implant<br />
(Figure 4). The extent <strong>of</strong> buccal<br />
bone resorption could not be determined<br />
from the radiograph.<br />
The implant was stable with no<br />
mobility.<br />
Diagnosis<br />
The provisional <strong>and</strong> final diagnosis<br />
was peri-implantitis <strong>of</strong> the implant<br />
fixture for tooth #7 with an infected<br />
implant periapical lesion exhibiting<br />
severe bone loss on the buccal side<br />
<strong>of</strong> the implant.<br />
Treatment Plan<br />
Treatment would involve the use <strong>of</strong><br />
an Er:YAG laser to perform:<br />
• the incision for a flap<br />
• ablation <strong>of</strong> granulation tissue<br />
around the implant<br />
• remodeling, shaping, <strong>and</strong> decortication<br />
<strong>of</strong> the bone<br />
• decontamination <strong>of</strong> exposed<br />
screw threads <strong>of</strong> the implant, <strong>and</strong><br />
• a GBR procedure.<br />
Since the implant was not<br />
mobile, this technique has a good<br />
prognosis.<br />
Treatment alternatives could<br />
consist <strong>of</strong> traditional scalpel,<br />
curettes, citric acid, air flow, air<br />
abrasion 49 <strong>and</strong> rotary bone burs.<br />
Treatment<br />
An Er:YAG laser (OpusDuo <br />
AquaLite E , Lumenis Ltd.,<br />
Reyhanian et al.<br />
Figure 5: Er:YAG laser being used for incision.<br />
A 200-micron tip is used in contact<br />
mode at 9 W, 450 mJ / 20 Hz<br />
Figure 6: Flap being raised<br />
Figure 7: Er:YAG laser being used for granulation<br />
tissue ablation. A 1300-micron tip<br />
is used at 8.4 W, 700 mJ / 12 Hz<br />
Yokneam, Israel) with a wavelength<br />
<strong>of</strong> 2940 nm was used.<br />
An intrasulcular incision was<br />
made using a 200-micron sapphire<br />
tip in contact mode. The power<br />
setting was 9 W, 450 mJ / 20 Hz<br />
with a water spray. The incision<br />
extended posteriorly from the distal<br />
area <strong>of</strong> #8 to the distal <strong>of</strong> #6<br />
(Figure 5). Then a vertical<br />
releasing incision was made<br />
apically on #6, <strong>and</strong> a buccal flap<br />
was lifted (Figure 6). The infected<br />
area was then visualized. There<br />
was massive bone loss on the<br />
CLINICAL REVIEW AND CASE REPORT<br />
Figure 8: View immediately after ablation<br />
<strong>of</strong> granulation tissue <strong>and</strong> bone remodeling<br />
Figure 9: Bio-Oss ® placement completed<br />
Figure 10: Bio-Gide ® absorbent<br />
membrane in place<br />
buccal apical aspect <strong>of</strong> the implant<br />
with a great deal <strong>of</strong> granulation<br />
tissue. The lack <strong>of</strong> mobility <strong>of</strong> the<br />
implant was confirmed.<br />
The granulation tissue was<br />
ablated with the erbium laser in<br />
noncontact mode; the tip was a<br />
1300-micron sapphire tip at a<br />
power <strong>of</strong> 8.4 W, 700 mJ / 12 Hz<br />
with a water spray (Figure 7). The<br />
removal <strong>of</strong> this granulation tissue<br />
produced a crater around the end<br />
<strong>of</strong> the implant. Next, the laser<br />
parameters were reduced to 3 W,<br />
JOUR NAL OF LASER DENTIS TRY | 2007 VOL 15, NO. 3<br />
137
JOUR NAL OF LASER DENTIS TRY | 2007 VOL 15, NO. 3<br />
138<br />
CLINICAL REVIEW AND CASE REPORT<br />
Figure 11: Primary closure with sutures<br />
Figure 12: Ten-day postoperative view<br />
Figure 13: One-<strong>and</strong>-a-half-month postoperative<br />
view<br />
150 mJ / 20Hz <strong>and</strong>, with the same<br />
tip <strong>and</strong> water spray, the laser<br />
energy was aimed at the surface <strong>of</strong><br />
the screw thread to obtain decontamination.<br />
Lastly, the laser was<br />
used to ablate the necrotic bone<br />
<strong>and</strong> to shape <strong>and</strong> remodel the site<br />
for GBR. A 1300-micron tip was<br />
used in noncontact with a power <strong>of</strong><br />
9 W, 450 mJ / 20 Hz <strong>and</strong> water<br />
spray (Figure 8). After lasing, the<br />
defect was filled with Bio-Oss ®<br />
(Geistlich Pharma AG, Wolhusen,<br />
Switzerl<strong>and</strong>), a bone substitute<br />
xenograft material, <strong>and</strong> covered<br />
Bio-Gide ® (Geistlich Pharma AG),<br />
an absorbent bilayer membrane<br />
Figure 14: One-<strong>and</strong>-a-half-month postoperative<br />
radiograph<br />
Figure 15: Seven-month postoperative<br />
view<br />
(Figures 9-10). The flap was<br />
sutured with 3-0 silk with careful<br />
attention paid to good primary<br />
closure (Figure 11).<br />
There are four important principles<br />
to keep in mind when<br />
performing GBR. 50-56<br />
• Fixation <strong>of</strong> the implant (the<br />
implant must be stable)<br />
• There must be complete <strong>and</strong><br />
passive s<strong>of</strong>t tissue coverage<br />
• There must be cortical stimulation<br />
by the material, <strong>and</strong><br />
• The vertical releasing incision<br />
should be as far as possible from<br />
the GBR site to enable good<br />
primary closure.<br />
The purpose <strong>of</strong> GBR is to enable<br />
new bone formation, treat the<br />
anatomical defect, <strong>and</strong> improve the<br />
implant’s prognosis. The<br />
morphology <strong>of</strong> the defect is important<br />
for healing: the more walls <strong>of</strong><br />
Figure 16: Seven-month postoperative<br />
radiograph<br />
bone left, the better the implant<br />
reacts. Deficiency <strong>of</strong> blood supply<br />
causes failure; to improve the blood<br />
supply to the bone graft, decortications<br />
<strong>of</strong> the bone are performed.<br />
Postoperative Instructions<br />
Clindamycin (150 mg x 50 tabs)<br />
was prescribed to prevent infection,<br />
<strong>and</strong> Motrin (800 mg x 15 tabs) for<br />
pain control. The patient was<br />
instructed to rinse with chlorhexidine<br />
0.2% starting the next day for<br />
2 weeks, three times a day, <strong>and</strong> was<br />
advised to maintain good oral<br />
hygiene.<br />
Management <strong>of</strong> Complications<br />
<strong>and</strong> Follow-Up Care<br />
The patient was examined the next<br />
day. She reported a moderate pain<br />
<strong>and</strong> moderate swelling <strong>of</strong> the cheek<br />
on the right side; but there was no<br />
tissue bleeding, the site was closed,<br />
<strong>and</strong> the flap was attaching with<br />
normal healing. Figure 12 depicts<br />
the 10-day postoperative view<br />
when the patient returned for<br />
inspection <strong>and</strong> suture removal. The<br />
swelling had resolved, there were<br />
no signs <strong>of</strong> fistula, <strong>and</strong> healing was<br />
progressing well. At six weeks, the<br />
s<strong>of</strong>t tissue had healed over the<br />
bone <strong>and</strong> there were no bony<br />
projections (Figure 13), <strong>and</strong> the<br />
Reyhanian et al.
adiograph showed good integration<br />
(Figure 14). The seven-month<br />
intraoral view (Figure 15) <strong>and</strong> the<br />
radiograph (Figure 16) show full<br />
healing. The prognosis is very good.<br />
CONCLUSION<br />
The Er:YAG laser can be used for<br />
decontamination <strong>of</strong> infected<br />
implant surfaces <strong>and</strong> has been<br />
shown to be effective <strong>and</strong> safe. The<br />
use <strong>of</strong> this laser wavelength for<br />
those procedures presents advantages<br />
over conventional methods<br />
such as reducing the patient’s<br />
discomfort, <strong>and</strong> allowing better<br />
<strong>visualization</strong> in the surgical site. In<br />
addition, postoperative effects, such<br />
as pain <strong>and</strong> swelling, are less<br />
pronounced. This laser is an invaluable<br />
tool for those procedures by<br />
simplifying treatment <strong>and</strong> <strong>of</strong>fering<br />
patients faster <strong>and</strong> less stressful<br />
oral therapy.<br />
AUTHOR BIOGRAPHIES<br />
Dr. Avi Reyhanian graduated from<br />
the University <strong>of</strong> Bucharest,<br />
Romania in 1988. He then participated<br />
in a fellowship program at<br />
the Oral <strong>and</strong> Maxill<strong>of</strong>acial<br />
Department, Rambam Hospital, in<br />
Haifa, Israel. He currently practices<br />
general dentistry <strong>and</strong> oral<br />
surgery in Netanya, Israel. Dr.<br />
Reyhanian first incorporated<br />
dental lasers in his practice in<br />
early 2002, <strong>and</strong> currently uses<br />
Er:YAG, CO 2 , <strong>and</strong> diode (830 nm)<br />
lasers. He has been performing<br />
periodontal surgery for the past 17<br />
years (the last four with lasers)<br />
<strong>and</strong> has completed more than 100<br />
cases <strong>of</strong> periodontal laser surgery.<br />
He is a member <strong>of</strong> the <strong>Academy</strong> <strong>of</strong><br />
<strong>Laser</strong> <strong>Dentistry</strong> <strong>and</strong> the Israel<br />
Society <strong>of</strong> Dental Implantology. Dr.<br />
Reyhanian may be contacted by<br />
e-mail at: avi5000rey@gmail.com.<br />
Disclosure: Dr. Reyhanian has no<br />
commercial affiliations.<br />
Donald J. Coluzzi, DDS is a 1970<br />
graduate <strong>of</strong> the University <strong>of</strong><br />
Southern California School <strong>of</strong><br />
Reyhanian et al.<br />
<strong>Dentistry</strong>. He recently retired after 35<br />
years from his general dental practice<br />
in Redwood City, California. He<br />
is an Associate Pr<strong>of</strong>essor at the<br />
University <strong>of</strong> California San<br />
Francisco School <strong>of</strong> <strong>Dentistry</strong><br />
Department <strong>of</strong> Preventive <strong>and</strong><br />
Restorative Dental Sciences. He is<br />
past president <strong>of</strong> the <strong>Academy</strong> <strong>of</strong><br />
<strong>Laser</strong> <strong>Dentistry</strong> <strong>and</strong> holds Advanced<br />
Pr<strong>of</strong>iciency certificates in Nd:YAG<br />
<strong>and</strong> Er:YAG laser wavelengths. He is<br />
a fellow <strong>of</strong> the American College <strong>of</strong><br />
Dentists, <strong>and</strong> has received the Leon<br />
Goldman Award for Clinical<br />
Excellence <strong>and</strong> the Distinguished<br />
Service Award from the <strong>Academy</strong> <strong>of</strong><br />
<strong>Laser</strong> <strong>Dentistry</strong>. He has published<br />
peer-reviewed manuscripts about<br />
lasers in dentistry, <strong>and</strong> along with<br />
Robert A. Convissar has co-authored<br />
the Atlas <strong>of</strong> <strong>Laser</strong> Applications in<br />
<strong>Dentistry</strong>, published by Quintessence<br />
Publishing Company in 2006. Dr.<br />
Coluzzi may be contacted by e-mail at<br />
don@laser-dentistry.com.<br />
Disclosure: Dr. Coluzzi is a lecturer<br />
for HOYA ConBio. He receives honoraria<br />
for those services.<br />
REFERENCES<br />
1. Adell R, Lekholm U, Rockler B,<br />
Brånemark PI. A 15-year study <strong>of</strong><br />
osseointegrated implants in the<br />
treatment <strong>of</strong> the edentulous jaw. Int<br />
J Oral Surg 1981;10(6):387-416.<br />
2 Albrektsson T. A multicenter report<br />
on osseointegrated oral implants. J<br />
Prosthet Dent 1988;60(1):75-84.<br />
3. Buser D, Mericske-Stern R, Dula K,<br />
Lang NP. Clinical experience with<br />
one-stage, non-submerged dental<br />
implants. Adv Dent Res<br />
1999;13:153-161.<br />
4. Olsson M, Friberg B, Nilson H,<br />
Kultje C. MkII – A modified selftapping<br />
Brånemark implant: 3-year<br />
results <strong>of</strong> a controlled prospective<br />
pilot study. Int J Oral Maxill<strong>of</strong>ac<br />
Implants 1995;10(1):15-21.<br />
5. Jaffin RA, Berman CL. The excessive<br />
loss <strong>of</strong> Branemark fixtures in<br />
type lV bone: A 5-year analysis. J<br />
Periodontol 1991;62(1):2-4.<br />
6. Esposito M, Hirsch J, Lekholm U,<br />
CLINICAL REVIEW AND CASE REPORT<br />
Thomsen P. Differential diagnosis<br />
<strong>and</strong> treatment strategies for biologic<br />
complications <strong>and</strong> failing oral<br />
implants: A review <strong>of</strong> the literature.<br />
Int J Oral Maxill<strong>of</strong>ac Implants<br />
1999;14(4):473-490.<br />
7. Brisman DL, Brisman AS, Moses<br />
MS. Implant failures associated<br />
with asymptomatic endodontically<br />
treated teeth. J Am Dent Assoc<br />
2001;132(2):191-195.<br />
8. Ayangco L, Sheridan PJ.<br />
Development <strong>and</strong> treatment <strong>of</strong><br />
retrograde peri-implantitis<br />
involving a site with history <strong>of</strong><br />
failed endodontic <strong>and</strong> apicoectomy<br />
procedures: A series <strong>of</strong> reports. Int J<br />
Oral Maxill<strong>of</strong>ac Implants<br />
2001;16(3):412-417.<br />
9. Reiser GM, Nevins M. The implant<br />
periapical lesion: Etiology, prevention,<br />
<strong>and</strong> treatment. Compend<br />
Contin Educ Dent 1995;16(8):768,<br />
770, 772, 774-777.<br />
10. Piattelli A, Scarano A, Piattelli M,<br />
Podda G. Implant periapical lesions:<br />
Clinical, histologic, <strong>and</strong> histochemical<br />
aspects. A case report. Int J<br />
Periodontics Restorative Dent<br />
1998;18(2):181-187.<br />
11. Yoon J, Oh T-J, Wang H-L. Implant<br />
periapical lesion: Potential etiology<br />
<strong>and</strong> treatment. J Korean Dent Assoc<br />
2002;40(5):388-397.<br />
12. McAllister BS, Master D, Meffer<br />
RM. Treatment <strong>of</strong> implants demonstrating<br />
periapical radiolucencies.<br />
Pract Periodontics Aesthet Dent<br />
1992;4(9):37-41.<br />
13. Scarano A, Di Domizio P, Petrone G,<br />
Iezzi G, Piattelli A. Implant periapical<br />
lesion: A clinical <strong>and</strong><br />
histologic case report. J Oral<br />
Implantol 2000;26(2):109-113.<br />
14. Oh TJ, Yoon J, Wang HL.<br />
Management <strong>of</strong> the implant periapical<br />
lesion: A case report. Implant<br />
Dent 2003;12(1):41-46.<br />
15. Jalbout ZN, Tarnow DP. The implant<br />
periapical lesion: Four case reports<br />
<strong>and</strong> review <strong>of</strong> the literature. Pract<br />
Proced Aesthet Dent 2001;13(2):107-<br />
112, quiz 114.<br />
16. El Askary AS, Meffert RM, Griffin T.<br />
Why do dental implants fail? Part I.<br />
Implant Dent 1999;8(2):173-185.<br />
17. Eriksson A, Albrektsson T, Grane B,<br />
JOUR NAL OF LASER DENTIS TRY | 2007 VOL 15, NO. 3<br />
139
JOUR NAL OF LASER DENTIS TRY | 2007 VOL 15, NO. 3<br />
140<br />
CLINICAL REVIEW AND CASE REPORT<br />
McQueen D. Thermal injury to bone:<br />
A vital-microscopic description <strong>of</strong><br />
heat effects. Int J Oral Surg<br />
1982;11(2):115-121.<br />
18. Yacker MJ, Klein M. The effect <strong>of</strong><br />
irrigation on osteotomy depth <strong>and</strong><br />
bur diameter. Int J Oral Maxill<strong>of</strong>ac<br />
Implants 1996;11(5):634-638.<br />
19. Isidor F. Loss <strong>of</strong> osseointegration<br />
caused by occlusal load <strong>of</strong> oral<br />
implants. A clinical <strong>and</strong> radiographic<br />
study in monkeys. Clin<br />
Oral Implants Res 1996;7(2):143-<br />
152.<br />
20. Sussman HI, Moss SS. Localized<br />
osteomyelitis secondary to<br />
endodontic-implant pathosis. A case<br />
report. J Periodontol 1993;64(4):306-<br />
310.<br />
21. Park SH, Sorensen WP, Wang HL.<br />
Management <strong>and</strong> prevention <strong>of</strong><br />
retrograde peri-implant infection<br />
from retained root tips: Two case<br />
reports. Int J Periodontics<br />
Restorative Dent 2004;24(5):422-433.<br />
22. Saadoun AP, Le Gall MG. An 8-year<br />
compilation <strong>of</strong> clinical results<br />
obtained with Steri-Oss endosseous<br />
implants. Compend Contin Educ<br />
Dent 1996;17(7):669-672, 674, 676,<br />
678, 680, 682-684, 686, 688, quiz<br />
688.<br />
23. Hutton J, Heath MR, Chai JY,<br />
Harnett J, Jemt T, Johns RB,<br />
McKenna S, McNamara DC, van<br />
Steenberghe D, Taylor R, Watson<br />
RM, Hermann T. Factors related to<br />
success <strong>and</strong> failure rates at 3-year<br />
follow-up in a multicenter study <strong>of</strong><br />
overdentures supported by<br />
Brånemark implants. Int J Oral<br />
Maxill<strong>of</strong>ac Implants 1995;10(1):33-<br />
42.<br />
24. Piattelli A, Scarano A, Balleri P,<br />
Favero GA. Clinical <strong>and</strong> histological<br />
evaluation <strong>of</strong> an active “implant<br />
periapical lesion”: A case report. Int<br />
J Oral Maxill<strong>of</strong>ac Implants<br />
1998;13(5):713-716.<br />
25. Quirynen M, Vogels R, Alsaadi G,<br />
Naert I, Jacobs R, van Steenberghe<br />
D. Predisposing conditions for retrograde<br />
peri-implantitis, <strong>and</strong><br />
treatment suggestions. Clin Oral<br />
Implants Res 2005;16(5):559-608.<br />
26. Albrektsson T, Dahl E, Enbom L,<br />
Engevall S, Engquist B, Eriksson<br />
AR, Feldmann G, Freiberg N, Glantz<br />
P-O, Kjellman O, Kristersson L,<br />
Kvint S, Köndell P-Å, Palmquist J,<br />
Werndahl L, Åstr<strong>and</strong> P.<br />
Osseointegrated oral implants. A<br />
Swedish multicenter study <strong>of</strong> 8139<br />
consecutively inserted Nobelpharma<br />
implants. J Periodontol<br />
1988;59(5):287-296.<br />
27. Sussman HI. Periapical implant<br />
pathology. J Oral Implantol<br />
1998;24(3):133-138.<br />
28. Shaffer M, Juruaz D, Haggerty PC.<br />
The effect <strong>of</strong> periradicular<br />
endodontic pathosis on the apical<br />
region <strong>of</strong> adjacent implants. Oral<br />
Surg Oral Med Oral Pathol Oral<br />
Radiol Endod 1998;86(5):578-581.<br />
29. Quirynen M, Naert I, van<br />
Steenberghe D, Dekeyser C, Callens<br />
A. Periodontal aspects <strong>of</strong> osseointegrated<br />
fixtures supporting a partial<br />
bridge. An up to 6-years retrospective<br />
study. J Clin Periodontol<br />
1992;19(2):118-126.<br />
30. Lekholm U, van Steenberghe D,<br />
Herrmann I, Bolender C, Folmer T,<br />
Gunne J, Henry P, Higuchi K, Laney<br />
WR, Linden U. Osseointegrated<br />
implants in the treatment <strong>of</strong><br />
partially edentulous jaws: A<br />
prospective 5-year multicenter<br />
study. Int J Oral Maxill<strong>of</strong>ac<br />
Implants 1994;9(6):627-635.<br />
31. Wheeler SL. Eight-year clinical<br />
retrospective study <strong>of</strong> titanium<br />
plasma-sprayed <strong>and</strong> hydroxyapatitecoated<br />
cylinder implants. Int J Oral<br />
Maxill<strong>of</strong>ac Implants 1996;11(3):340-<br />
350.<br />
32. Grunder U, Polizzi G, Goené R,<br />
Hatano N, Henry P, Jackson WJ,<br />
Kawamura K, Kohler S, Renouard F,<br />
Rosenberg R, Triplett G, Werbitt M,<br />
Lithner B. A 3-year prospective<br />
multicenter follow-up report on the<br />
immediate <strong>and</strong> delayed-immediate<br />
placement <strong>of</strong> implants. Int J Oral<br />
Maxill<strong>of</strong>ac Implants 1999;14(2):210-<br />
216.<br />
33. Balshi TJ, Pappas CE, Wolfinger GJ,<br />
Hern<strong>and</strong>ez RE. Management <strong>of</strong> an<br />
abscess around the apex <strong>of</strong> a<br />
m<strong>and</strong>ibular root form implant:<br />
Clinical report. Implant Dent<br />
1994;3(2):81-85.<br />
34. Sasaki KM, Aoki A, Ichinose S,<br />
Yoshino T, Yamada S, Ishikawa I.<br />
Scanning electron microscopy <strong>and</strong><br />
Fourier transformed infrared spectroscopy<br />
analysis <strong>of</strong> bone removal<br />
using Er:YAG <strong>and</strong> CO2 lasers. J<br />
Periodontol 2002;73(6):643-652.<br />
35. Nelson JS, Orenstein A, Liaw LH,<br />
Berns MW. Mid-infrared<br />
erbium:YAG laser ablation <strong>of</strong> bone:<br />
The effect <strong>of</strong> laser osteotomy on<br />
bone healing. <strong>Laser</strong>s Surg Med<br />
1989;9(4):362-374.<br />
36. Ishikawa I, Aoki A, Takasaki AA.<br />
Potential applications <strong>of</strong><br />
erbium:YAG laser in periodontics. J<br />
Periodontal Res 2004;39(4):275-285.<br />
37. Watanabe H, Ishikawa I, Suzuki M,<br />
Hasegawa K. Clinical assessments<br />
<strong>of</strong> the erbium:YAG laser for s<strong>of</strong>t<br />
tissue surgery <strong>and</strong> scaling. J Clin<br />
<strong>Laser</strong> Med Surg 1996;14(2):67-75.<br />
38. Ishikawa I, Sasaki KM, Aoki A,<br />
Watanabe H. Effects <strong>of</strong> Er:YAG<br />
laser on periodontal therapy. J Int<br />
Acad Periodontol 2003;5(1):23-28.<br />
39. Schwarz F, Bieling K, Sculean A,<br />
Herten M, Becker J. <strong>Laser</strong> und<br />
ultraschall in der therapie periimplantärer<br />
infektionen – Eine<br />
literaturübersicht. [Treatment <strong>of</strong><br />
periimplantitis with laser or ultrasound.<br />
A review <strong>of</strong> the literature.]<br />
Schweiz Monatsschr Zahnmed<br />
2004;114(12):1228-1235.<br />
40. Kreisler M, Al Haj H, d’Hoedt B.<br />
Temperature changes at the<br />
implant-bone interface during simulated<br />
surface decontamination with<br />
an Er:YAG laser. Int J Prosthodont<br />
2002;15(6):582-587.<br />
41. Schwarz F, Rothamel D, Becker J.<br />
Einfluss eines Er:YAG-lasers auf die<br />
oberflächen-struktur von titanimplantaten.<br />
[Influence <strong>of</strong> an<br />
Er:YAG laser on the surface structure<br />
<strong>of</strong> titanium implants.] Schweiz<br />
Monatsschr Zahnmed<br />
2003;113(6):660-671.<br />
42. Folwaczny M, Mehl A, Aggstaller H,<br />
Hickel R. Antimicrobial effects <strong>of</strong><br />
2.94 microm Er:YAG laser radiation<br />
on root surfaces: An in vitro study. J<br />
Clin Periodontol 2002;29(1):73-78.<br />
43. Kreisler M, Kohnen W, Marinello C,<br />
Götz H, Duschner H, Jansen B,<br />
d’Hoedt B. Bactericidal effect <strong>of</strong> the<br />
Er:YAG laser on dental implant<br />
surfaces: An in vitro study. J<br />
Periodontol 2002;73(11):1292-1298.<br />
Reyhanian et al.
44. Matsuyama T, Aoki A, Oda S,<br />
Yoneyama T, Ishikawa I. Effect <strong>of</strong><br />
the Er:YAG laser irradiation on titanium<br />
implant materials <strong>and</strong><br />
contaminated implant abutment<br />
surfaces. J Clin <strong>Laser</strong> Med Surg<br />
2003;21(1):7-17.<br />
45. Schwarz F, Rothamel D, Sculean A,<br />
George T, Scherbaum W, Becker J.<br />
Effect <strong>of</strong> an Er:YAG laser <strong>and</strong> the<br />
Vector ultrasonic system on the<br />
biocompatibility <strong>of</strong> titanium<br />
implants in cultures <strong>of</strong> human<br />
osteoblast-like cells. Clin Oral<br />
Implants Res 2003;14(6):784-792.<br />
46. Kreisler M, Kohnen W, Christ<strong>of</strong>fers<br />
AB, Götz H, Jansen B, Duschner H,<br />
d’Hoedt B. In vitro evaluation <strong>of</strong> the<br />
biocompatibility <strong>of</strong> contaminated<br />
implant surfaces treated with an<br />
Er:YAG laser <strong>and</strong> an air powder<br />
system. Clin Oral Implants Res<br />
2005;16(1):36-43.<br />
47. Aoki A, Yoshino T, Akiyama F, Miura<br />
M, Kinoshita A. Oda S, Watanabe H,<br />
Ishikawa I. Comparative study <strong>of</strong><br />
Er:YAG laser <strong>and</strong> rotating bur for<br />
bone ablation. In: Ishikawa I, Frame<br />
Reyhanian et al.<br />
JW, Aoki A, editors. <strong>Laser</strong>s in<br />
dentistry: Revolution <strong>of</strong> dental treatment<br />
in the new millennium.<br />
Proceedings <strong>of</strong> the 8th International<br />
Congress on <strong>Laser</strong>s in <strong>Dentistry</strong>, July<br />
31-August 2, 2002, Yokohama, Japan.<br />
Excerpta Medica International<br />
Congress Series 1248. Amsterdam:<br />
Elsevier Science B.V., 2003:389-391.<br />
48. Rupprecht S, Tangermann K, Kessler<br />
P, Neukam FW, Wiltfang J. Er:YAG<br />
laser osteotomy directed by sensor<br />
controlled systems. J Craniomaxillifac<br />
Surg 2003;31(6):337-342.<br />
49. Jovanovic SA. The management <strong>of</strong><br />
peri-implant breakdown around<br />
functioning osseointegrated dental<br />
implants. J Periodontol 1993;64(11<br />
Suppl):1176-1183.<br />
50. Von Arx T, Kurt B, Hardt N.<br />
Treatment <strong>of</strong> severe peri-implant<br />
bone loss using autogenous bone <strong>and</strong><br />
a resorbable membrane. Case report<br />
<strong>and</strong> literature review. Clin Oral<br />
Implants Res 1997;8(6):517-526.<br />
51. Meffert RM. How to treat ailing <strong>and</strong><br />
failing implants. Implant Dent<br />
1992;1(1):25-33.<br />
CLINICAL REVIEW AND CASE REPORT<br />
52. Artzi Z, Tal H, Chweidan H. Bone<br />
regeneration for reintegration in<br />
peri-implant destruction. Compend<br />
Contin Educ Dent 1998;19(1):17-20,<br />
22-23, 26-28, quiz 30.<br />
53. Mellonig JT, Griffiths G, Mathys E,<br />
Spitznagel J. Treatment <strong>of</strong> the<br />
failing implant: Case reports. Int J<br />
Periodontics Restorative Dent<br />
1995;15(4):384-395.<br />
54. Lehmann B, Bragger U, Hammerle<br />
CH, Fourmousis I, Lang NP.<br />
Treatment <strong>of</strong> an early implant failure<br />
according to the principles <strong>of</strong> guided<br />
tissue regeneration (GTR). Clin Oral<br />
Implant Res 1992;3(1):42-48.<br />
55. Goldman MJ. Bone regeneration<br />
around a failing implant using guided<br />
tissue regeneration. A case report. J<br />
Periodontol 1992;63(5):473-476.<br />
56. Hammerle CH, Fourmousis I, Winkler<br />
JR, Weigel C, Brågger U, Lang NP.<br />
Successful bone fill in late periimplant<br />
defect using guided tissue<br />
regeneration. A short communication.<br />
J Periodontol 1995;66(4):303-308. ■■<br />
The Dental Hygiene <strong>Laser</strong> Course<br />
St<strong>and</strong>ard Pr<strong>of</strong>iciency Certification<br />
<strong>Laser</strong> S<strong>of</strong>t Tissue Management<br />
Patient Chairside Clinic<br />
Course Designed for Hygiene<br />
All Courses Held in Your Office with Your <strong>Laser</strong> • Technique Driven Instruction • Advanced Skills Training<br />
<strong>Academy</strong> <strong>of</strong> <strong>Laser</strong> <strong>Dentistry</strong> Recognized Course Provider<br />
S<strong>of</strong>t Tissue LASER Training<br />
Teri Gutierrez, RDH Certified <strong>Laser</strong> Educator<br />
Phone: 1-831-801-8210 or visit www.lasers4hygiene.com<br />
CALL TODAY FOR COURSE AVAILABILITY<br />
JOUR NAL OF LASER DENTIS TRY | 2007 VOL 15, NO. 3<br />
141
JOUR NAL OF LASER DENTIS TRY | 2007 VOL 15, NO. 3<br />
142<br />
CLINICAL CASE STUDIES<br />
Advanced Pr<strong>of</strong>iciency Case Studies<br />
Upcoming issues <strong>of</strong> the Journal will feature case<br />
studies from the most recent recipients <strong>of</strong> Advanced<br />
Pr<strong>of</strong>iciency. These clinicians completed the two-year<br />
process by successfully presenting one <strong>of</strong> these cases at<br />
the <strong>Academy</strong> <strong>of</strong> <strong>Laser</strong> <strong>Dentistry</strong>’s 2007 Annual<br />
Conference in Nashville, Tennessee. They are: Mary<br />
Lynn Smith, RDH; Charles Hoopingarner, DDS; <strong>and</strong><br />
Steven Parker, BDS, LDS RCS, MFGDP.<br />
In this issue, Mrs. Smith utilizes an Nd:YAG laser<br />
as part <strong>of</strong> the protocol for initial treatment <strong>of</strong> periodontal<br />
disease. She explains how the laser is<br />
integrated into the therapeutic appointment <strong>and</strong><br />
demonstrates the wavelength’s benefits in helping to<br />
control the disease.<br />
Dr. Hoopingarner performs gingival <strong>and</strong> osseous<br />
closed flap crown lengthening with an Er:YAG laser to<br />
help restore a bicuspid with a lingual cusp fracture<br />
that extended subgingivally. This case depicts the<br />
laser’s ability to ablate <strong>and</strong> contour both s<strong>of</strong>t <strong>and</strong> hard<br />
tissue with precision <strong>and</strong> care, <strong>and</strong> ultimately to gain<br />
the necessary biologic width <strong>and</strong> tooth structure for a<br />
successful restoration.<br />
These cases show how different laser wavelengths<br />
can be routinely employed in a variety <strong>of</strong> dental procedures<br />
to produce safe, efficient, <strong>and</strong> excellent clinical<br />
results. ■■<br />
Nd:YAG <strong>Laser</strong> Use in Treatment <strong>of</strong> Moderate<br />
Chronic Periodontitis<br />
Mary Lynn Smith, RDH<br />
McPherson, Kansas<br />
Treatment <strong>of</strong> a Subcrestal Tooth Fracture with<br />
the Er:YAG <strong>Laser</strong><br />
Charles R. Hoopingarner, DDS<br />
Houston, Texas
JOUR NAL OF LASER DENTIS TRY | 2007 VOL 15, NO. 3<br />
144<br />
CLINICAL CASE<br />
Nd:YAG <strong>Laser</strong> Use in Treatment <strong>of</strong><br />
Moderate Chronic Periodontitis<br />
Mary Lynn Smith, RDH, McPherson, Kansas<br />
J <strong>Laser</strong> Dent 2007;15(3):144-150<br />
SYNOPSIS<br />
This case report describes the use <strong>of</strong> an Nd:YAG laser as an integral<br />
component <strong>of</strong> the initial treatment <strong>of</strong> periodontal disease.<br />
PRETREATMENT<br />
A. Diagnostic Tests<br />
1. Full Clinical Description<br />
A healthy 47-year-old Hispanic male<br />
presented for examination. His chief<br />
complaint was the dark spot at the<br />
gingival margin <strong>of</strong> tooth #9 <strong>and</strong><br />
limited chewing efficiency (Figure 1).<br />
His last dental visit was 6 months<br />
prior for an emergency extraction <strong>of</strong><br />
tooth #19. He had never had any<br />
type <strong>of</strong> dental hygiene appointment.<br />
The patient speaks Spanish predominately,<br />
<strong>and</strong> communication was<br />
accomplished by the dentist translating<br />
information at specific times<br />
in each appointment.<br />
During the initial hygiene<br />
appointment, the health history was<br />
reviewed <strong>and</strong> tissues were visually<br />
screened for signs <strong>of</strong> oral cancer.<br />
Comprehensive restorative, periodontal,<br />
<strong>and</strong> radiographic exams<br />
were completed. Micro-ultrasonic<br />
scaling, bi<strong>of</strong>ilm removal, <strong>and</strong> coronal<br />
polishing were performed. The<br />
patient was educated concerning his<br />
oral health <strong>and</strong> probable progression<br />
<strong>of</strong> untreated disease.<br />
The patient was taking no<br />
medications <strong>and</strong> had no known allergies.<br />
He was missing nine teeth: #1,<br />
16, 17, 19, 20, 25, 26, 30, <strong>and</strong> 32.<br />
Decay was noted on teeth #3, 15, <strong>and</strong><br />
18. Significant fractures were noted<br />
on tooth #18 as well. The occlusion<br />
was Angle’s classification I with<br />
normal TMJ function. Supragingival<br />
calculus <strong>and</strong> gingival inflammation<br />
indicated possible periodontal<br />
disease. Complete periodontal<br />
charting revealed periodontal<br />
probing depths <strong>of</strong> 2-7 mm. Areas <strong>of</strong><br />
recession exposing 1 to 4 mm <strong>of</strong> root<br />
surface were<br />
present.<br />
Furcations <strong>and</strong><br />
mobility were<br />
also noted on the<br />
molars.<br />
2. Radiographic<br />
Examination<br />
A full-mouth<br />
series with 4<br />
vertical bitewings<br />
<strong>and</strong> 14<br />
periapical films<br />
was taken to<br />
further evaluate<br />
bone loss <strong>and</strong><br />
carious lesions<br />
(Figure 2).<br />
Decay was<br />
noted on teeth<br />
#3 <strong>and</strong> 18.<br />
Decay on #15<br />
was not detected<br />
radiographically.<br />
There was<br />
moderate gener-<br />
Figure 2: Full-mouth film series taken at<br />
initial visit Figure 3: Initial periodontal probing chart<br />
Figure 1: Preoperative full-smile photograph<br />
<strong>of</strong> patient at presentation<br />
alized horizontal bone loss with areas<br />
<strong>of</strong> severe vertical bone loss on posterior<br />
teeth. Areas <strong>of</strong> particular concern were<br />
teeth #2, 15, 18, <strong>and</strong> 31. These teeth<br />
were diagnosed as hopeless due to the<br />
periodontal involvement <strong>and</strong>/or decay<br />
present <strong>and</strong> were scheduled for extraction.<br />
Generalized moderate-to-heavy<br />
calculus was noted on the radiographs.<br />
Smith
3. S<strong>of</strong>t Tissue Status<br />
Tissues appeared inflamed <strong>and</strong> irritated<br />
with the presence <strong>of</strong> plaque<br />
<strong>and</strong> calculus. A complete six-point<br />
periodontal probing was performed<br />
with 7 mm as the greatest pocket<br />
depth. Generalized bleeding was<br />
evident <strong>and</strong> moderate-to-heavy<br />
subgingival calculus was present in<br />
posterior areas, as well as supragingivally<br />
on the lower anterior teeth.<br />
Gingival recession <strong>of</strong> 1-2 mm was<br />
noted on teeth #2, 3, 4, 5, 12, 13, 14,<br />
<strong>and</strong> 15 buccal surfaces <strong>and</strong> 1-4 mm<br />
on lingual surfaces <strong>of</strong> teeth #2, 3, 4,<br />
14, 15, 18, 23, 24, 27, 28, 29, 31.<br />
Mobility <strong>of</strong> class I was detected on<br />
tooth #14 <strong>and</strong> class II on #2, 15, 18,<br />
<strong>and</strong> 31. Class I furcations were<br />
found on #2, 3, 14, 15, 18, <strong>and</strong> 31,<br />
<strong>and</strong> class II furcations on #2, 15, 18,<br />
<strong>and</strong> 31 (Figure 3). A statistical<br />
summary <strong>of</strong> overall periodontal<br />
health showed 36 hemorrhaging<br />
sites upon probing, 45 periodontal<br />
pockets <strong>of</strong> 4 mm or greater, <strong>and</strong> 19<br />
teeth exhibiting beyond-normal<br />
limits in pocketing. (This summary<br />
excludes teeth #2, 15, 18, <strong>and</strong> 31<br />
which were diagnosed as hopeless.)<br />
The oral cancer screening was<br />
within normal limits.<br />
4. Hard Tissue Status<br />
• Missing teeth were #1, 16, 17, 19,<br />
20, 25, 26, 30, <strong>and</strong> 32<br />
• All other teeth were vital<br />
• Occlusion was Angle’s Class I<br />
• Decay was present on teeth #3<br />
DL, #15 O, <strong>and</strong> #18 DOL with<br />
fractures noted on the mesial,<br />
lingual <strong>and</strong> distal aspects<br />
• Limited mastication was present<br />
due to missing posterior teeth.<br />
5. Other Tests<br />
TMJ was normal.<br />
B. Diagnosis <strong>and</strong> Treatment Plan<br />
1. Diagnoses<br />
• Provisional diagnosis included<br />
chronic periodontitis with poor<br />
prognosis <strong>of</strong> molars.<br />
• The doctor’s final diagnosis was<br />
stated as severe generalized<br />
chronic periodontitis. Carious<br />
Smith<br />
lesions were present on teeth #3<br />
DL, #15 O, #18 DOL, with significant<br />
fractures on #18 MLD.<br />
2. Treatment Plan Outline<br />
a. Restorative treatment to include:<br />
• restoration <strong>of</strong> tooth #3 with a<br />
distolingual composite<br />
• simple extractions <strong>of</strong> teeth<br />
#2, 15, 18, <strong>and</strong> 31<br />
• replacement <strong>of</strong> teeth #19, 20,<br />
25, 26, <strong>and</strong> 30 with a partial<br />
denture or implants.<br />
b. Active phase-I periodontal infection<br />
therapy to include five<br />
periodontal infection therapy<br />
appointments, one hour each<br />
<strong>and</strong> scheduled approximately a<br />
week apart:<br />
• assessment <strong>of</strong> patient’s<br />
plaque management, refining<br />
techniques <strong>and</strong> continuing<br />
motivation for thorough daily<br />
care<br />
• micro-ultrasonic instrumentation<br />
<strong>and</strong> h<strong>and</strong><br />
instrumentation for bi<strong>of</strong>ilm<br />
<strong>and</strong> calculus removal<br />
• laser s<strong>of</strong>t tissue decontamination<br />
<strong>and</strong> superficial<br />
coagulation<br />
• intraoral photographs.<br />
c. Six-week post-therapy re-infection<br />
assessment appointment to<br />
include:<br />
• one appointment for 30<br />
minutes:<br />
• health history review<br />
• visual evaluation <strong>of</strong> tissue<br />
rehabilitation<br />
• assessment <strong>of</strong> patient’s plaque<br />
management, refining techniques<br />
<strong>and</strong> continuing motivation<br />
for thorough daily care<br />
• intraoral photographs<br />
• micro-ultrasonic bi<strong>of</strong>ilm<br />
removal at gingival third <strong>of</strong><br />
tooth<br />
• probing <strong>and</strong> sulcular instrumentation<br />
is avoided in order<br />
to allow undisturbed maturation<br />
<strong>of</strong> connective tissue at<br />
the base <strong>of</strong> the pocket.<br />
d. Twelve-week post-therapy<br />
appointment to include:<br />
• health history review<br />
CLINICAL CASE<br />
• oral cancer screening<br />
• periodontal charting to<br />
assess rehabilitation<br />
• assessment <strong>of</strong> patient’s<br />
plaque management, refining<br />
techniques <strong>and</strong> continuing<br />
motivation for thorough daily<br />
care<br />
• micro-ultrasonic instrumentation<br />
for full-mouth<br />
bacterial decontamination<br />
<strong>and</strong> scaling as needed<br />
• coronal polishing<br />
• laser decontamination <strong>of</strong><br />
unresolved areas<br />
• intraoral photos<br />
• determination <strong>of</strong> recare<br />
interval.<br />
3. Indications for Treatment<br />
Treatment is indicated to halt the<br />
periodontal destruction <strong>and</strong> rehabilitate<br />
the affected tissues. Periodontal<br />
infection therapy must include<br />
removal <strong>of</strong> bi<strong>of</strong>ilm <strong>and</strong> calculus from<br />
the root surfaces through scaling. The<br />
Nd:YAG laser furthers decontamination<br />
<strong>of</strong> the pocket by addressing the<br />
periodontal pocket wall. The 1,064nm<br />
laser wavelength is highly<br />
absorbed in melanin <strong>and</strong> hemoglobin.<br />
Both <strong>of</strong> these chromophores are<br />
present in inflammatory tissue.<br />
<strong>Laser</strong>-tissue interaction reduces<br />
pathogens in the pocket <strong>and</strong> coagulates<br />
hemorrhaging sites, assisting<br />
the body’s healing response. This<br />
laser enhances the body’s healing<br />
process by reducing bacterial counts<br />
<strong>and</strong> achieving superficial coagulation.<br />
4. Contraindications for Therapy<br />
<strong>and</strong> Precautions<br />
Though it could be beneficial to reduce<br />
pathogens prior to extraction, teeth<br />
diagnosed as hopeless were not<br />
considered for therapy. There were no<br />
contraindications for this patient to<br />
receive Nd:YAG laser-assisted treatment<br />
<strong>of</strong> periodontal disease. <strong>Laser</strong><br />
safety precautions were followed for<br />
protection <strong>of</strong> the patient <strong>and</strong> clinician.<br />
The energy from the Nd:YAG<br />
laser must be directed toward the<br />
s<strong>of</strong>t tissue <strong>and</strong> away from the tooth<br />
<strong>and</strong> bone.<br />
JOUR NAL OF LASER DENTIS TRY | 2007 VOL 15, NO. 3<br />
145
JOUR NAL OF LASER DENTIS TRY | 2007 VOL 15, NO. 3<br />
146<br />
CLINICAL CASE<br />
5. Treatment Alternatives<br />
Treatment alternatives included:<br />
• No treatment <strong>and</strong> progression <strong>of</strong><br />
disease, eventual tooth loss <strong>and</strong><br />
systemic impact<br />
• Conventional scaling <strong>and</strong> root<br />
planning<br />
• Placement <strong>of</strong> localized antimicrobials<br />
or antibiotics with possible<br />
reactions<br />
• Periodontal surgery.<br />
6. Informed Consent<br />
After being educated in the<br />
progression <strong>of</strong> untreated periodontal<br />
disease <strong>and</strong> treatment<br />
options, the patient gave verbal<br />
<strong>and</strong> written consent to proceed<br />
with the planned therapy. This is<br />
documented in the patient’s record.<br />
TREATMENT<br />
A. Restorative Treatment<br />
Objective<br />
Teeth #2, 15, 18, <strong>and</strong> 31 were<br />
extracted prior to phase I active<br />
periodontal infection therapy.<br />
Tooth #3 caries removal <strong>and</strong><br />
composite restoration was placed<br />
after completion <strong>of</strong> therapy per the<br />
patient’s request.<br />
B. Periodontal Treatment<br />
Objective<br />
The treatment objectives are to<br />
halt the destruction <strong>of</strong> the periodontium<br />
due to disease processes.<br />
<strong>Laser</strong>-assisted periodontal treatment<br />
will reduce bacterial load in<br />
the periodontal pocket wall, eliminating<br />
the related inflammatory<br />
response by the body. The Nd:YAG<br />
laser wavelength is well absorbed<br />
in pigmented <strong>and</strong> hemoglobin-rich<br />
inflamed tissue. Signs <strong>of</strong> healing,<br />
such as decreased probing depths,<br />
elimination <strong>of</strong> hemorrhaging, <strong>and</strong><br />
normal tissue coloration <strong>and</strong><br />
texture, are desired. The appointments<br />
are designed to allow<br />
patient-customized education in<br />
specific daily plaque management<br />
techniques, ensuring maximum<br />
rehabilitation <strong>of</strong> the tissues.<br />
Beginning with the most infected<br />
teeth, each appointment will<br />
address three to four teeth for<br />
debridement <strong>of</strong> root surfaces<br />
through scaling, followed by tissue<br />
decontamination <strong>and</strong> superficial<br />
coagulation through lasing. At the<br />
subsequent appointment, approximately<br />
7 to 10 days later, a<br />
different group <strong>of</strong> teeth will be<br />
debrided <strong>and</strong> tissues lased. The<br />
previously treated area will be<br />
revisited for ultrasonic bi<strong>of</strong>ilm<br />
removal from tooth surfaces <strong>and</strong><br />
laser decontamination <strong>of</strong> tissues.<br />
Instrumentation with the ultrasonic<br />
is concentrated on the<br />
cervical area <strong>of</strong> tooth structure <strong>and</strong><br />
the fiber is calibrated to 1 mm less<br />
than the previous application. This<br />
continues the reduction <strong>of</strong> bacterial<br />
load <strong>and</strong> enhances the body’s<br />
healing response. It also allows<br />
reinforcement <strong>of</strong> behavior modification<br />
in daily plaque management.<br />
C. <strong>Laser</strong> Operating Parameters<br />
A free-running pulsed Nd:YAG<br />
laser (PulseMaster 600 IQ,<br />
American Dental Technologies,<br />
Corpus Christi, Texas) with a 1064nm<br />
emission wavelength was used<br />
with a 400-micron contact fiber. For<br />
bacterial reduction, the laser<br />
parameters were 30 mJ <strong>and</strong> 60 Hz,<br />
average power <strong>of</strong> 1.8 Watts for<br />
approximately 40 seconds per site;<br />
for superficial coagulation, the<br />
settings were 100 mJ <strong>and</strong> 20 Hz,<br />
with an average power <strong>of</strong> 2.0 Watts<br />
for approximately 20 seconds per<br />
site. The total laser emission time<br />
for the five sessions <strong>of</strong> periodontal<br />
infection therapy was 155 minutes.<br />
D. Treatment Delivery<br />
Sequence<br />
The treatment delivery sequence at<br />
each therapeutic appointment<br />
included:<br />
• review <strong>of</strong> health history<br />
• plaque management assessment<br />
<strong>and</strong> instruction<br />
• anesthetic as needed<br />
• topical anesthetic administered<br />
at the gingival margin <strong>and</strong><br />
subgingivally. A compounded<br />
preparation called TAC (20%<br />
lidocaine, 4% tetracaine, <strong>and</strong> 2%<br />
phenylephrine) was used<br />
• local anesthetic <strong>of</strong> 2% lidocaine<br />
with epinephrine 1:100,000 was<br />
administered for more pr<strong>of</strong>ound<br />
anesthesia<br />
• infiltration with 4% articaine<br />
with epinephrine 1:100,000 was<br />
administered when a full block<br />
was not necessary<br />
• micro-ultrasonic <strong>and</strong> h<strong>and</strong><br />
instrument debridement <strong>of</strong> root<br />
surfaces<br />
• laser decontamination <strong>and</strong> superficial<br />
coagulation<br />
• postoperative care instructions<br />
given.<br />
<strong>Laser</strong> safety measures included:<br />
• use <strong>of</strong> 1,064-nm laser wavelength<br />
protective eyewear by all operatory<br />
personnel<br />
• use <strong>of</strong> 0.1-micron filtration masks<br />
• environment secured to limit<br />
access<br />
• laser-in-use warning sign placed<br />
• reflective surfaces minimized<br />
• high-volume evacuation utilized<br />
for plume control <strong>and</strong> to cool the<br />
tissue.<br />
Chart documentation included<br />
laser <strong>and</strong> wavelength used, fiber<br />
size <strong>and</strong> type, operating parameters,<br />
<strong>and</strong> emission time.<br />
The laser fiber was cleaved <strong>and</strong><br />
the laser test-fired. The fiber was<br />
calibrated to 1 mm less than the<br />
pocket depth (Figure 4). With the<br />
fiber remaining in constant contact<br />
with the internal pocket tissue <strong>and</strong><br />
in constant motion, treatment began<br />
at the top <strong>of</strong> the pocket <strong>and</strong><br />
progressed apically, moving the fiber<br />
vertically <strong>and</strong> horizontally until the<br />
Figure 4: <strong>Laser</strong> fiber is calibrated to 1<br />
mm less than the pocket depth<br />
Smith
Figure 5: Any debris clinging to the fiber<br />
must be wiped <strong>of</strong>f<br />
Figure 6: Intraoperative view showing the<br />
technique used on the upper right molar<br />
Figure 7: Intraoperative view demonstrating<br />
fresh bleeding which indicates<br />
that the laser use for this site is complete<br />
calibrated depth was reached. The<br />
fiber was always directed away from<br />
the root surface <strong>and</strong> toward the<br />
target tissue. Accumulated debris<br />
was wiped from the fiber <strong>and</strong> a<br />
proper cleave maintained (Figure 5).<br />
Figure 6 shows the laser technique<br />
on tooth #3, which is featured in<br />
this case. The amount <strong>of</strong> lasing time<br />
was influenced by tissue interaction,<br />
extent <strong>of</strong> disease, <strong>and</strong> depth <strong>of</strong> the<br />
pocket. When fresh bleeding was<br />
visible, the laser procedure was<br />
Smith<br />
Figure 8: Tooth #14 procedure Figure 9: Tooth #28 procedure<br />
Figure 8a: Initial mesiobuccal pocket on<br />
tooth #14<br />
Figure 8b: <strong>Laser</strong> treatment <strong>of</strong> pocket<br />
Figure 8c: Immediate postoperative view<br />
deemed complete for that site<br />
(Figure 7). High-volume suction was<br />
present to eliminate the plume <strong>and</strong><br />
cool the tissue.<br />
Several figures demonstrate the<br />
typical treatment protocol in two<br />
different areas <strong>of</strong> the mouth.<br />
Figure 8a shows initial mesial<br />
pocket depth <strong>of</strong> tooth #14, 8b shows<br />
the laser treatment, <strong>and</strong> 8c shows<br />
the immediate postoperative coagulation.<br />
CLINICAL CASE<br />
Figure 9a: Initial mesiolingual pocket on<br />
tooth #28<br />
Figure 9b: <strong>Laser</strong> treatment <strong>of</strong> pocket<br />
Figure 9c: Immediate postoperative view<br />
Figure 9a shows the mesiolingual<br />
pocket <strong>of</strong> tooth #28, 9b<br />
shows the laser treatment, <strong>and</strong> 9c<br />
shows the immediate postoperative<br />
coagulation.<br />
E. Postoperative Instructions<br />
Postoperative instructions were<br />
given in verbal <strong>and</strong> written form.<br />
The patient was instructed to avoid<br />
(for the first 24 hours) acidic, rough,<br />
or crunchy foods. Normal eating<br />
JOUR NAL OF LASER DENTIS TRY | 2007 VOL 15, NO. 3<br />
147
JOUR NAL OF LASER DENTIS TRY | 2007 VOL 15, NO. 3<br />
148<br />
CLINICAL CASE<br />
could resume following that period.<br />
Avoidance <strong>of</strong> seeds, husks, <strong>and</strong><br />
other foods that may lodge between<br />
the gingiva <strong>and</strong> tooth was recom-<br />
Figure 10: One-week postoperative views<br />
Figure 10a: One-week postoperative view<br />
<strong>of</strong> tooth #14<br />
Figure 10b: One-week postoperative view<br />
<strong>of</strong> tooth #28<br />
mended for a week. In the areas<br />
lased, subgingival flossing <strong>and</strong> the<br />
small Sulcabrush ® (Sulcabrush Inc.,<br />
Niagara Falls, N.Y.) were to be<br />
avoided for several days. Use <strong>of</strong> an<br />
ultras<strong>of</strong>t toothbrush <strong>and</strong> supragingival<br />
cleaning was recommended.<br />
All other areas were to be cleaned<br />
as usual. If discomfort were to<br />
occur, the patient was instructed to<br />
use warm salt water rinses <strong>and</strong><br />
over-the-counter pain medication.<br />
The patient was informed that the<br />
most important aspect <strong>of</strong> the<br />
therapy was the healing process,<br />
<strong>and</strong> minimizing plaque at the<br />
gingival margin was critical in<br />
preventing re-infection.<br />
F. Complications<br />
The patient experienced cold sensitivity.<br />
He was prescribed 1.1%<br />
neutral sodium fluoride with potassium<br />
nitrate for daily use. It was<br />
effective <strong>and</strong> he had no other<br />
complications during or after the<br />
laser treatments.<br />
G. Prognosis<br />
Prognosis overall is good as long as<br />
the patient<br />
conforms to good<br />
oral hygiene <strong>and</strong><br />
recommended<br />
intervals for<br />
pr<strong>of</strong>essional<br />
supportive maintenance<br />
visits.<br />
Periodontally,<br />
teeth #3 <strong>and</strong> 14<br />
will be monitored<br />
for continued<br />
improvement.<br />
Restorative treatment<br />
is needed to<br />
reduce functional<br />
stresses on<br />
existing teeth.<br />
FOLLOW-UP CARE<br />
A. Assessment <strong>of</strong> Treatment<br />
Outcomes<br />
The patient was assessed at 1<br />
week, 6 weeks, 12 weeks, <strong>and</strong> 6<br />
months following active phase-I<br />
periodontal infection therapy.<br />
Periodontal charts show comparative<br />
data <strong>of</strong> initial state to 12<br />
weeks post-therapy as well as 6<br />
months post-therapy. Percentage <strong>of</strong><br />
improvement is seen with 92% in<br />
bleeding reduction, 80% in pocket<br />
site reduction, <strong>and</strong> 68% fewer teeth<br />
exhibiting periodontal pocketing.<br />
The one-week examination<br />
revealed that the tissues were<br />
healing <strong>and</strong> the patient’s skill in<br />
plaque management was<br />
improving. For example, Figure 10a<br />
shows the one-week view <strong>of</strong> tooth<br />
#14, <strong>and</strong> Figure 10b shows the oneweek<br />
view <strong>of</strong> tooth #28.<br />
Figure 12: Twelve-week postoperative<br />
probing<br />
Figure 12a: Tooth #14<br />
Figure 11: Twelve-week postoperative periodontal probing chart<br />
H. Documentation<br />
All treatment <strong>and</strong><br />
related information<br />
was recorded<br />
in the patient’s<br />
treatment record. Figure 12b: Tooth #28<br />
Smith
Six-week post-therapy reinfection<br />
assessment<br />
appointment included:<br />
• confirmation that the patient is<br />
maintaining plaque control.<br />
Smith<br />
Tissues are continuing to<br />
improve.<br />
• health history review<br />
• visual evaluation <strong>of</strong> tissue<br />
rehabilitation<br />
• assessment <strong>of</strong> the<br />
patient’s plaque<br />
management,<br />
refining techniques<br />
<strong>and</strong><br />
continuing motivation<br />
for<br />
thorough daily<br />
care<br />
• intraoral photographs<br />
• micro-ultrasonic<br />
bi<strong>of</strong>ilm removal<br />
at gingival third<br />
<strong>of</strong> tooth<br />
• probing <strong>and</strong><br />
sulcular instrumentation<br />
was<br />
avoided in order<br />
to allow undisturbed<br />
maturation <strong>of</strong><br />
connective tissue<br />
at the base <strong>of</strong> the<br />
pocket.<br />
Twelve-week<br />
Figure 13: Six-month postoperative periodontal probing chart post-therapy<br />
appointment:<br />
Figure 14: Six-month postoperative probing Overall, a marked improvement was<br />
seen in periodontal health, such as<br />
decreased probing depths, decreased<br />
bleeding on probing, normal tissue<br />
coloration, firm texture, <strong>and</strong> lack <strong>of</strong><br />
mobility. Teeth #3 <strong>and</strong> 14 need<br />
continued refinement <strong>of</strong> plaque<br />
management <strong>and</strong> further therapy.<br />
This appointment included:<br />
• health history review<br />
• oral cancer screening<br />
Figure 14a: Tooth #14<br />
• six-point pocket <strong>and</strong> hemorrhaging<br />
periodontal charting to<br />
assess rehabilitation (Figure 11)<br />
• assessment <strong>of</strong> the patient’s<br />
plaque management, refining<br />
techniques <strong>and</strong> continuing motivation<br />
for thorough daily care<br />
• micro-ultrasonic instrumentation<br />
for full-mouth bacterial decontamination<br />
<strong>and</strong> h<strong>and</strong><br />
Figure 14b: Tooth #28<br />
instrumentation as needed<br />
Figure 15: Comparison views<br />
CLINICAL CASE<br />
Figure 15a: Preoperative full smile at<br />
presentation<br />
Figure 15b: Six-month postoperative full<br />
smile<br />
• coronal polishing<br />
• laser decontamination <strong>of</strong> appropriate<br />
areas<br />
• determination <strong>of</strong> recare interval<br />
at 12 weeks.<br />
The previously mentioned<br />
Nd:YAG laser was used with a<br />
setting for decontamination <strong>of</strong> 30 mJ<br />
<strong>and</strong> 60 Hz, 1.8 Watts average power,<br />
<strong>and</strong> additional hemostasis application<br />
for teeth #3 <strong>and</strong> 14 at 100 mJ<br />
<strong>and</strong> 20 Hz, 2.0 Watts delivered with<br />
a 400-micron contact fiber for 7<br />
minutes total emission time. Oral<br />
hygiene instructions were reviewed.<br />
Continued use <strong>of</strong> daily fluoride as<br />
caries prevention was recommended.<br />
A 12-week supportive periodontal<br />
therapy appointment was scheduled.<br />
Short-term follow-up for tooth #14 is<br />
shown in Figure 12a <strong>and</strong> for tooth<br />
#28 in Figure 12b.<br />
Six-month post-therapy<br />
appointment:<br />
Tissue health is maintaining very<br />
well. Tooth #3 is continuing to<br />
improve while #14 remains an area<br />
<strong>of</strong> concern. Periodontal chartings<br />
compare the initial, 12-week, <strong>and</strong><br />
JOUR NAL OF LASER DENTIS TRY | 2007 VOL 15, NO. 3<br />
149
JOUR NAL OF LASER DENTIS TRY | 2007 VOL 15, NO. 3<br />
150<br />
CLINICAL CASE<br />
Table 1: Results <strong>of</strong> <strong>Laser</strong>-Assisted Therapy<br />
Treatment<br />
Assessment Interval<br />
Number <strong>of</strong> Sites<br />
with Bleeding<br />
on Probing<br />
6-month periodontal status. The 6month<br />
therapeutic appointment<br />
included:<br />
• health history review<br />
• oral cancer screening<br />
• six-point periodontal charting<br />
(Figure 13)<br />
• assessment <strong>of</strong> the patient’s<br />
plaque management, refining<br />
techniques <strong>and</strong> continuing motivation<br />
for thorough daily care;<br />
instructions to continue daily<br />
fluoride applications<br />
• micro-ultrasonic instrumentation<br />
for full-mouth bacterial decontamination<br />
<strong>and</strong> h<strong>and</strong><br />
instrumentation as needed<br />
• coronal polishing<br />
• laser decontamination <strong>of</strong> appropriate<br />
areas<br />
• instruction to continue 12-week<br />
maintenance interval.<br />
The previously mentioned<br />
Nd:YAG laser was used with a 400micron<br />
fiber <strong>and</strong> parameters <strong>of</strong> 30<br />
Hz, 60 mJ, average power <strong>of</strong> 1.8<br />
Watts for decontamination.<br />
Hemostatic assistance was accomplished<br />
with 100 mJ, 20 Hz,<br />
average power <strong>of</strong> 2.0 Watts applied<br />
to sites <strong>of</strong> tooth #14 due to<br />
increased inflammation. Emission<br />
time totaled 8 minutes. Long-term<br />
follow-up is illustrated: Figure 14a<br />
shows the 6-month probing <strong>of</strong> tooth<br />
#14 <strong>and</strong> 14b shows tooth #28.<br />
Number <strong>of</strong> Sites<br />
with Periodontal<br />
Pockets 4 mm or<br />
Greater<br />
Number <strong>of</strong> Teeth<br />
with Beyond-Normal<br />
Periodontal<br />
Pocketing<br />
Beginning 36 45 19 <strong>of</strong> 19<br />
12 Weeks 3 9 6 <strong>of</strong> 19<br />
6 Months 7 4 2 <strong>of</strong> 19<br />
Rate <strong>of</strong> Improvement<br />
After 6 Months<br />
81% 91% 90%<br />
B. Complications<br />
Continued daily use <strong>of</strong> fluoride was<br />
recommended for caries prevention.<br />
The patient had no s<strong>of</strong>t or hard<br />
tissue damage <strong>and</strong> was pleased<br />
with the results from the laser.<br />
C. Long-Term Results<br />
At 12 weeks post-therapy there<br />
was marked improvement.<br />
Hemorrhaging sites were reduced<br />
by 92%, number <strong>of</strong> perio sites by<br />
80%, <strong>and</strong> number <strong>of</strong> teeth affected<br />
by 68%. At 6 months post-therapy,<br />
the patient had an increase in<br />
hemorrhaging sites but other<br />
improvements continued. The<br />
patient’s health compared to his<br />
initial state showed improvements<br />
<strong>of</strong> 81% in hemorrhaging, 91% in<br />
perio sites, <strong>and</strong> 90% number <strong>of</strong><br />
teeth affected (Table 1). Figures<br />
15a <strong>and</strong> 15b show the comparison<br />
<strong>of</strong> tissues initially <strong>and</strong> at 6 months<br />
post-therapy.<br />
D. Long-Term Prognosis<br />
The patient was compliant with all<br />
treatment aspects <strong>and</strong> a good prognosis<br />
exists. It will require<br />
conformity to good oral hygiene <strong>and</strong><br />
continued pr<strong>of</strong>essional supportive<br />
maintenance visits at 12-week<br />
intervals. Periodontally, teeth #3<br />
<strong>and</strong> 14 will be monitored for<br />
continued improvement.<br />
Adjustment <strong>of</strong> the maintenance<br />
interval <strong>and</strong> adjunctive use <strong>of</strong><br />
Arestin ® (OraPharma Inc.,<br />
Warminster, Pa.) are possible. In<br />
the case <strong>of</strong> acute <strong>and</strong> rapid progression,<br />
surgical intervention or<br />
extraction may be indicated.<br />
Replacement <strong>of</strong> missing<br />
m<strong>and</strong>ibular teeth will be very<br />
important to alleviate excessive<br />
functional stress on existing teeth.<br />
If a partial denture is chosen<br />
rather than implants, caries<br />
prevention <strong>and</strong> periodontal<br />
stability <strong>of</strong> supporting teeth will be<br />
a concern. Caries prevention<br />
strategy includes effective daily<br />
plaque management, daily use <strong>of</strong><br />
fluoride, <strong>and</strong> reduced acid sources<br />
in diet, as well as consistent pr<strong>of</strong>essional<br />
care. An oral irrigator for<br />
daily use would be beneficial for all<br />
teeth present.<br />
AUTHOR BIOGRAPHY<br />
Mary Lynn Smith is a registered<br />
dental hygienist, working clinically<br />
for more than 12 years. She<br />
achieved her St<strong>and</strong>ard Pr<strong>of</strong>iciency<br />
in the Nd:YAG (1,064-nm) <strong>and</strong><br />
diode (810-nm) wavelengths in<br />
2003, <strong>and</strong> completed her<br />
Advanced Pr<strong>of</strong>iciency in the<br />
Nd:YAG in 2007. Mary Lynn has<br />
contributed to the dental community<br />
through articles <strong>and</strong><br />
speaking to fellow hygienists on<br />
care <strong>of</strong> implants, periodontal therapies,<br />
<strong>and</strong> laser-assisted hygiene<br />
techniques <strong>and</strong> principles. She<br />
currently resides in McPherson,<br />
Kansas <strong>and</strong> is employed by Dr.<br />
Jon Julian, DDS. Mrs. Smith may<br />
be contacted by<br />
e-mail at mlsrdh@swbell.net.<br />
Disclosure: Mrs. Smith has no<br />
commercial relationships relative to<br />
this case presentation. ■■<br />
Smith
Treatment <strong>of</strong> a Subcrestal Tooth<br />
Fracture with the Er:YAG <strong>Laser</strong><br />
Charles R. Hoopingarner, DDS, Houston, Texas<br />
J <strong>Laser</strong> Dent 2007;15(3):151-155<br />
SYNOPSIS<br />
This article describes gingival <strong>and</strong> osseous closed flap crown length-<br />
ening with an Er:YAG laser to help restore a bicuspid with a lingual<br />
cusp fracture that extends subgingivally.<br />
PRETREATMENT<br />
A. Outline <strong>of</strong> Case<br />
1. Full Clinical Description<br />
A 62-year-old Caucasian male<br />
presented with severe pain on<br />
chewing in the area <strong>of</strong> tooth #13.<br />
Figure 1 shows a deep vertical fracture<br />
<strong>of</strong> an existing MOD ceramic<br />
onlay <strong>and</strong> the underlying palatal<br />
cusp. He had complained <strong>of</strong> occasional<br />
biting sensitivity at two<br />
previous recare visits. No definitive<br />
findings were made at either visit. At<br />
that time a vital pulp test <strong>and</strong> radiographic<br />
evaluation were performed,<br />
<strong>and</strong> a minor occlusal adjustment was<br />
made. He had been an 11-year<br />
patient in the practice <strong>and</strong> maintained<br />
a very good level <strong>of</strong> dental<br />
health, <strong>and</strong> it was expected he would<br />
continue to be followed in our <strong>of</strong>fice.<br />
A recare evaluation <strong>and</strong> prophylaxis<br />
had been performed 3 months prior<br />
to the onset <strong>of</strong> the obvious fracture<br />
<strong>and</strong> extreme pain with no other<br />
pathologic dental or significant periodontal<br />
findings. He is allergic to<br />
Hoopingarner<br />
penicillin <strong>and</strong> on presentation his<br />
vital signs were within normal limits<br />
(blood pressure 115/68, pulse 64). He<br />
was taking no medications <strong>and</strong> had<br />
no further contributing medical<br />
history. He has a well-restored Class<br />
I dental occlusion <strong>and</strong> has cast<br />
restorations on teeth #4, 15, 29, <strong>and</strong><br />
30. He had existing intracoronal<br />
restorations in teeth #2, 3, 6, 12, 14,<br />
18, 19, 20, 28, <strong>and</strong> 31.<br />
2. Radiographic Examination<br />
Previous panoramic X-ray showed<br />
no significant bone loss or any<br />
lesions present. A periapical X-ray<br />
did not show apical pathology or<br />
vertical bone loss present (Figure 2).<br />
3. S<strong>of</strong>t Tissue Status<br />
An oral cancer screen <strong>and</strong> periodontal<br />
probing had been<br />
CLINICAL CASE<br />
Figure 1: Preoperative view <strong>of</strong> fractured<br />
lingual cusp at presentation<br />
performed within a three-month<br />
period. When done, no s<strong>of</strong>t tissue<br />
lesions were present, <strong>and</strong> no pocket<br />
depth measurements were in<br />
excess <strong>of</strong> 4 mm, as shown in Figure<br />
3. (As is the custom in our <strong>of</strong>fice, no<br />
pocket depths less than 4 mm were<br />
recorded.)<br />
Tooth #13 was probed <strong>and</strong> there<br />
were no readings in excess <strong>of</strong> 3 mm<br />
except along the border <strong>of</strong> the fractured<br />
segment. There was<br />
periodontal attachment present on<br />
the fractured segment <strong>and</strong> a 4-5<br />
mm measurement from the gingival<br />
crest to the remaining attachment.<br />
Figure 2: Periapical radiograph taken at<br />
presentation Figure 3: Periodontal probe chart. Pockets less than 4 mm are not charted<br />
JOUR NAL OF LASER DENTIS TRY | 2007 VOL 15, NO. 3<br />
151
JOUR NAL OF LASER DENTIS TRY | 2007 VOL 15, NO. 3<br />
152<br />
CLINICAL CASE<br />
4. Hard Tissue Status<br />
All bone levels <strong>and</strong> ridge topography<br />
had historically been within<br />
acceptable limits. The area around<br />
tooth #13 showed no vertical bone<br />
loss. The palatal cusp <strong>of</strong> tooth #13<br />
had fractured below the attachment<br />
level <strong>and</strong> after removal would<br />
show a termination at the osseous<br />
crest. There were signs <strong>of</strong> bruxism<br />
present <strong>and</strong> the patient reported<br />
that he was wearing a nighttime<br />
protective appliance that had been<br />
prescribed many years prior to this<br />
presentation. The tooth tested vital<br />
to air spray stimulation <strong>and</strong> it was<br />
necessary to use injected local<br />
anesthesia to fully evaluate the<br />
extent <strong>of</strong> the fracture.<br />
5. Other Tests<br />
TMJ evaluation showed normal<br />
range <strong>of</strong> motion <strong>and</strong> no joint<br />
sounds were present.<br />
B. Diagnosis <strong>and</strong> Treatment<br />
Plan<br />
1. Provisional Diagnosis<br />
A provisional diagnosis <strong>of</strong> vertical<br />
fracture <strong>of</strong> the palatal cusp <strong>of</strong> tooth<br />
#13 was made. It was thought that<br />
the fracture would extend to the<br />
osseous crest in a limited area,<br />
making impression-taking difficult.<br />
The position <strong>of</strong> the osseous crest<br />
obviated a consideration <strong>of</strong> biologic<br />
width issues. There was no pulpal<br />
exposure evident.<br />
2. Final Diagnosis<br />
A final diagnosis <strong>of</strong> vertical fracture<br />
<strong>of</strong> the palatal cusp <strong>of</strong> tooth #13<br />
was made. Figure 4 shows the fragment<br />
being removed. The extent <strong>of</strong><br />
the fracture was limited to areas<br />
coronal to the periodontal attachment<br />
except for an approximate<br />
3-mm linear area in a readily<br />
accessible area <strong>of</strong> the palatal<br />
osseous crest, as seen in Figure 5.<br />
Since the fracture was observed to<br />
terminate at the osseous crest, any<br />
restoration would impinge on the<br />
biologic width necessary to maintain<br />
a healthy tooth support<br />
system.<br />
Figure 4: Removal <strong>of</strong> fractured segment<br />
3. Treatment Plan Outline<br />
The objective was to restore the<br />
patient’s tooth with a bonded<br />
ceramic restoration that would<br />
restore nearly ideal tooth form <strong>and</strong><br />
permit proper attachment levels<br />
without invasion <strong>of</strong> the biologic<br />
width necessary to maintain periodontal<br />
health. Initially the tooth<br />
would be prepared to allow for<br />
coverage <strong>of</strong> the fractured areas. The<br />
preparation would be as conservative<br />
as possible as utilization <strong>of</strong> a<br />
bonded restoration did not require<br />
apical preparation extension for the<br />
purpose <strong>of</strong> retention. This procedure<br />
would be done with<br />
conventional rotary instruments. If<br />
the fractured root structure could<br />
be smoothed to allow placement <strong>of</strong><br />
a margin at a more coronal level,<br />
that would become a part <strong>of</strong> the<br />
procedure.<br />
The 2940-nm Er:YAG laser<br />
would be used for two procedures.<br />
The first would be to contour the<br />
s<strong>of</strong>t tissue in a manner that would<br />
leave the margins <strong>of</strong> the restoration<br />
at the gingival crest. The<br />
second procedure would be to<br />
remove osseous tissue to a level 3<br />
mm below the intended margin <strong>and</strong><br />
bevel the bone to a normal contour.<br />
4. Indications<br />
As the 2940-nm Er:YAG laser<br />
wavelength is highly absorbed by<br />
both water <strong>and</strong> hydroxyapatite, it<br />
can be used to both contour the s<strong>of</strong>t<br />
tissue <strong>and</strong> lower the bone level<br />
where indicated to establish a<br />
healthy attachment. With a closed<br />
Figure 5: Preoperative view <strong>of</strong> existing<br />
sound tooth structure, showing that the<br />
extent <strong>of</strong> the fracture is subgingival<br />
flap technique, the postoperative<br />
recovery is shortened <strong>and</strong> the<br />
patient discomfort level is minimized.<br />
With this approach<br />
impressions could be taken at the<br />
time <strong>of</strong> surgery <strong>and</strong> the restoration<br />
placed within the time frame <strong>of</strong> a<br />
normal delivery.<br />
5. Contraindications<br />
There were no contraindications for<br />
performing this procedure.<br />
6. Precautions<br />
During the initial gingival recontour<br />
it is necessary to carefully<br />
consider the desired outcome after<br />
healing. The s<strong>of</strong>t tissue ablation<br />
should be performed by angling the<br />
tip in a manner to avoid damaging<br />
tooth structure. As the final<br />
contours are approached, care must<br />
be taken to avoid interacting with<br />
the bone prior to the initiation <strong>of</strong><br />
water spray. Rehearsal <strong>of</strong> the bone<br />
ablating stroke is <strong>of</strong>ten necessary<br />
as the water spray can impair<br />
direct <strong>visualization</strong>.<br />
7. Treatment Alternatives<br />
Conventional flap surgery with<br />
gingival sculpting using scalpel<br />
technique <strong>and</strong> bone recontouring<br />
with rotary instruments or chisels<br />
is an alternative. Tooth extraction<br />
is an alternative.<br />
8. Informed Consent<br />
After a description <strong>of</strong> advantages,<br />
possible complications, <strong>and</strong> treatment<br />
alternatives were discussed,<br />
<strong>and</strong> all the patient’s questions were<br />
Hoopingarner
Figure 6: The Er:YAG laser is used first to<br />
contour <strong>and</strong> establish the height <strong>of</strong> the<br />
gingival marginal tissue<br />
answered, the patient’s verbal <strong>and</strong><br />
written informed consent was<br />
obtained.<br />
TREATMENT<br />
A. Treatment Objectives<br />
The objective is to remove the fractured<br />
fragment, prepare the tooth,<br />
smooth the root surface, contour<br />
the gingiva, take an accurate<br />
impression, recontour the osseous<br />
crest to allow for proper biologic<br />
width formation, <strong>and</strong> place a wellformed<br />
provisional restoration so<br />
that bonded cementation could<br />
occur in a timely fashion. The<br />
Er:YAG laser will be used for<br />
recontouring both the gingival<br />
tissues <strong>and</strong> the osseous tissue.<br />
B. <strong>Laser</strong> Operating Parameters<br />
<strong>Laser</strong>: Er:YAG (DELight, HOYA<br />
ConBio, Fremont, Calif.):<br />
• Delivery system: Fiber-optic<br />
system consisting <strong>of</strong> varying<br />
quartz tips: 600-micron for initial<br />
tissue ablation, 400-micron for<br />
osseous recontouring, <strong>and</strong> 1200 x<br />
300-micron chisel tip for tissue<br />
<strong>and</strong> osseous beveling <strong>and</strong><br />
smoothing<br />
• Wavelength: 2940 nm<br />
• Mode: Free-running pulsed<br />
• Pulse width: 300 microseconds<br />
• Power: 1.5 Watts (30 Hz <strong>and</strong> 50<br />
mJ)<br />
• Beam Diameter: Varied, 400 to<br />
600 microns using focused <strong>and</strong><br />
defocused patterns<br />
• Repetition rate: 30 Hz<br />
• Continuous air (reduced volume<br />
<strong>and</strong> water spray for osseous<br />
Hoopingarner<br />
Figure 7: A probe is used to determine<br />
that the osseous crest is less than 1 mm<br />
apical to the gingival margin<br />
procedures, <strong>and</strong> air only for s<strong>of</strong>t<br />
tissue)<br />
<strong>Laser</strong> settings:<br />
• S<strong>of</strong>t tissue ablation: 30 Hz <strong>and</strong><br />
50 mJ, air cooling <strong>and</strong> no water<br />
• Osseous recontouring: 30 Hz <strong>and</strong><br />
50 mJ with air <strong>and</strong> water spray<br />
Tips were used in both light<br />
contact <strong>and</strong> defocused modes.<br />
C. Treatment Delivery<br />
Sequence<br />
Pretreatment: The operatory was<br />
secured <strong>and</strong> the laser warning sign<br />
was posted. The laser unit was<br />
properly placed <strong>and</strong> connected to<br />
an air supply. Safety glasses with<br />
4+ optical density for the 2940-nm<br />
laser wavelength that met ANSI<br />
st<strong>and</strong>ards Z136.1 <strong>and</strong> Z136.3 were<br />
used. All shiny reflective objects<br />
were removed. The operatory was<br />
set up <strong>and</strong> supplied according to<br />
the st<strong>and</strong>ard for a restorative <strong>and</strong> a<br />
surgical procedure. Charting <strong>and</strong><br />
radiographs were visible to the<br />
operator. The procedure was<br />
reviewed with staff in the morning<br />
report meeting. Prior to administration<br />
<strong>of</strong> anesthesia, the treatment<br />
was reviewed with the patient <strong>and</strong><br />
informed consent was confirmed.<br />
The patient was properly draped<br />
<strong>and</strong> approximately 1.5 cc prilocaine<br />
4% 1:200,000 epinephrine was<br />
distributed by infiltration in the<br />
maxillary premolar segment.<br />
Approximately 0.4 cc prilocaine 4%<br />
1:200,000 epinephrine was injected<br />
6 mm below the palatal gingival<br />
crest <strong>of</strong> tooth #13. Eye protection<br />
was placed on the patient as well<br />
CLINICAL CASE<br />
Figure 8: Osseous tissue is removed <strong>and</strong><br />
contoured with the laser, with the tip<br />
sleeve being used as a depth guide<br />
as the operator <strong>and</strong> assistant. The<br />
laser was test-fired in a safe direction<br />
after eye protection was placed<br />
<strong>and</strong> prior to the first s<strong>of</strong>t tissue<br />
procedure. The first laser procedure<br />
was to recontour the s<strong>of</strong>t tissue to<br />
approximate the intended margin<br />
<strong>of</strong> the preparation. This was done<br />
with near but noncontact strokes<br />
with a 600-micron tip <strong>and</strong> energy<br />
settings <strong>of</strong> 30 Hz <strong>and</strong> 50 mJ<br />
(Figure 6). The tissue was beveled<br />
as necessary to produce a physiologic<br />
crestal roll. This entailed an<br />
exposure time <strong>of</strong> less than 3<br />
minutes. No water was used for<br />
this part <strong>of</strong> the procedure <strong>and</strong> the<br />
tip was carefully aligned to avoid<br />
scarring the tooth.<br />
The distance from the fracture<br />
margin to the osseous crest was<br />
determined to be less than 1 mm.<br />
The probing <strong>of</strong> this depth is shown<br />
in Figure 7. It was felt that a<br />
margin could be placed 1 mm<br />
coronal to the extent <strong>of</strong> the fracture<br />
if the root were shaped <strong>and</strong><br />
polished using rotary instruments<br />
<strong>and</strong> curettes. After this procedure<br />
was accomplished, there was still a<br />
distance <strong>of</strong> only 2 mm from the<br />
intended margin to the osseous<br />
crest. With copious water spray, a<br />
400-micron tip, <strong>and</strong> the same<br />
energy settings (30 Hz <strong>and</strong> 50 mJ),<br />
the bone was ablated to allow for a<br />
distance <strong>of</strong> slightly more than 3<br />
mm from the osseous crest to the<br />
intended preparation margin. This<br />
was done with short, noncontact<br />
strokes, with care being taken to<br />
avoid scarring the tooth. The 3-mm<br />
JOUR NAL OF LASER DENTIS TRY | 2007 VOL 15, NO. 3<br />
153
JOUR NAL OF LASER DENTIS TRY | 2007 VOL 15, NO. 3<br />
154<br />
CLINICAL CASE<br />
Figure 9: Initial tooth preparation<br />
showing contouring <strong>of</strong> fractured area<br />
Figure 10: A probe is used to confirm<br />
adequate biologic width<br />
sleeve on the 400-micron tip was<br />
used as a guide, as shown in Figure<br />
8. Had this convenient marking<br />
apparatus not been available, ink<br />
or stopper material could have<br />
been used as a measuring guide.<br />
With the 600-micron tip <strong>and</strong> the<br />
chisel tip, the bone was beveled to<br />
approximate a normal crestal<br />
contour. Total exposure time for the<br />
osseous segment was less than 7<br />
minutes. This gave a total exposure<br />
time <strong>of</strong> less than 10 minutes.<br />
With the depth <strong>of</strong> the fracture<br />
area left untouched where the root<br />
was smoothed, the tooth was<br />
prepared in a conservative manner<br />
to receive a ceramic restoration<br />
(Empress ® , Ivoclar Vivadent Inc.,<br />
Amherst, N.Y.), as shown in Figure<br />
9. Figure 10 shows the confirmation<br />
<strong>of</strong> the new osseous level to be just<br />
over 3 mm from the intended preparation<br />
margin. A deep chamfer/<br />
shoulder margin was then placed in<br />
that area, with care being taken to<br />
maintain the desired crest-to-margin<br />
distance, <strong>and</strong> the preparation was<br />
completed (Figure 11).<br />
With care taken to operate in a<br />
Figure 11: Final tooth preparation<br />
completed<br />
Figure 12: Impression clearly shows<br />
lingual margin <strong>of</strong> preparation<br />
noncontact mode, gingival hemorrhage<br />
was greatly reduced. The final<br />
impression was obtained during the<br />
operative visit. The crisp, clear<br />
impression again confirmed the<br />
osseous crest depth (Figure 12).<br />
A provisional restoration <strong>of</strong><br />
temporary crown <strong>and</strong> bridge material<br />
(Integrity TM , Dentsply, York,<br />
Pa.), shown in Figure 13, was<br />
placed to maintain tissue contour.<br />
The provisional was evaluated at<br />
48 hours <strong>and</strong> no signs <strong>of</strong> infection<br />
or significant inflammation were<br />
present.<br />
Due to patient travel requirements<br />
it was necessary to bond the<br />
final restoration just 10 days after<br />
preparation. There was minimal<br />
s<strong>of</strong>t tissue invasion in the deep<br />
marginal area (Figure 14) which<br />
was easily removed with a 3%<br />
hydrogen peroxide scrub. The<br />
restoration was bonded with a total<br />
etch protocol using a single-component<br />
adhesive (Optibond ® Solo<br />
Plus , Kerr Corporation, Orange,<br />
Calif.) as a bonding agent <strong>and</strong> an<br />
adhesive resin (Nexus II, Kerr<br />
Corporation) as a cement. This was<br />
Figure 13: Provisional restoration in place<br />
Figure 14: Ten-day postoperative view <strong>of</strong><br />
preparation <strong>and</strong> tissue prior to bonding<br />
<strong>of</strong> restoration<br />
Figure 15: Immediate post-bonding<br />
lingual view<br />
performed in light-cure-only mode,<br />
<strong>and</strong> cured for 10 seconds at all four<br />
interproximal corners <strong>and</strong> 20<br />
seconds on the buccal, occlusal, <strong>and</strong><br />
palatal surfaces (Figure 15).<br />
D. Postoperative Instructions<br />
The patient was told to avoid foods<br />
warmer than room temperature for<br />
48 hours <strong>and</strong> then begin hot saline<br />
mouth rinses. The area was to be<br />
cleaned with hydrogen peroxide on<br />
cotton tip applicators for the first<br />
48 hours. After the first postoperative<br />
visit, the patient was cleared<br />
for normal hygiene procedures<br />
Hoopingarner
Figure 16: Three-month postoperative<br />
probing shows healthy sulcular depth <strong>of</strong><br />
2 mm<br />
which included brushing with an<br />
ultras<strong>of</strong>t brush dipped in hot water.<br />
He was told not to floss around the<br />
provisional restoration <strong>and</strong> to avoid<br />
sticky foods in that area.<br />
Emergency care contact numbers<br />
were given. No narcotic analgesics<br />
were prescribed <strong>and</strong> the patient<br />
was instructed to use over-thecounter<br />
ibupr<strong>of</strong>en if necessary.<br />
E. Complications<br />
There was slight s<strong>of</strong>t tissue invasion<br />
under the provisional<br />
restoration. This was removed with<br />
a 3% hydrogen peroxide scrub. The<br />
shade <strong>of</strong> the restoration was a little<br />
opaque but well within the<br />
patient’s acceptable expectation<br />
limits.<br />
F. Prognosis<br />
The prognosis for maintenance <strong>of</strong><br />
the restoration is excellent. The<br />
tissue appeared to be healing<br />
nicely, giving an expectation <strong>of</strong> an<br />
excellent prognosis. The prognosis<br />
for continued pulpal vitality was<br />
still somewhat guarded.<br />
G. Treatment Records<br />
All appropriate details described<br />
Hoopingarner<br />
Figure 17: Three-month postoperative<br />
periapical radiograph<br />
above were entered into the<br />
patient’s record.<br />
FOLLOW-UP CARE<br />
A. Assessment <strong>of</strong> Treatment<br />
Outcome<br />
The patient was very pleased with<br />
the treatment outcome, especially<br />
since he was seen on an emergency<br />
basis <strong>and</strong> treatment was completed<br />
in a short time frame to meet his<br />
travel schedule. He reported no<br />
postoperative pain <strong>and</strong> the tissues<br />
showed no sign <strong>of</strong> inflammation or<br />
inappropriate pocket depth. No<br />
deep probing was indicated for<br />
three months postoperatively.<br />
B. Complications<br />
The patient reported no postoperative<br />
complications.<br />
C. Long-Term Results<br />
At 3 months the restoration<br />
showed no signs <strong>of</strong> failure <strong>and</strong> had<br />
intact margins. The tissues were<br />
maintaining a good level <strong>of</strong> health<br />
with a palatal probing depth <strong>of</strong> 2<br />
mm (Figure 16).The periapical<br />
radiograph (Figure 17) demonstrated<br />
normal tissue.<br />
D. Long-Term Prognosis<br />
Because <strong>of</strong> the biocompatibility <strong>of</strong><br />
CLINICAL CASE<br />
the pressed ceramic restoration <strong>and</strong><br />
the exact treatment planning <strong>of</strong> the<br />
attachment levels, the long-term<br />
tissue prognosis remains excellent.<br />
AUTHOR BIOGRAPHY<br />
Dr. Charles Hoopingarner attended<br />
the University <strong>of</strong> Texas Health<br />
Science Center at Houston<br />
(UTHSCH) Dental Branch, graduating<br />
with a DDS in 1973. He has<br />
maintained a private practice in<br />
Houston, Texas since 1973. He was<br />
an adjunct associate pr<strong>of</strong>essor in<br />
anatomical sciences at UTHSCH<br />
Dental Branch for 11 years.<br />
Currently he is adjunct clinical<br />
faculty in the Restorative <strong>Dentistry</strong><br />
Department at UTHSCH <strong>and</strong> has<br />
been a clinical instructor at the Las<br />
Vegas Institute for Advanced<br />
Dental Studies since 1997, teaching<br />
Advanced Anterior Aesthetics <strong>and</strong><br />
Comprehensive Aesthetic<br />
Reconstruction <strong>and</strong> <strong>Laser</strong><br />
<strong>Dentistry</strong>. Dr. Hoopingarner is a<br />
member <strong>of</strong> the <strong>Academy</strong> <strong>of</strong> <strong>Laser</strong><br />
<strong>Dentistry</strong> (ALD) <strong>and</strong> has used<br />
dental lasers <strong>of</strong> various wavelengths<br />
as integral parts <strong>of</strong> his<br />
patient care delivery system for the<br />
last 10 years. He holds Advanced<br />
<strong>and</strong> St<strong>and</strong>ard Pr<strong>of</strong>iciency certification<br />
from the ALD <strong>and</strong> has lectured<br />
internationally on the safety <strong>and</strong><br />
use <strong>of</strong> laser technology in the<br />
dental practice. He may be<br />
contacted by e-mail at<br />
choop@swbell.net.<br />
Disclosure: Dr. Hoopingarner has no<br />
direct financial or ownership positions<br />
with commercial companies<br />
relative to this case presentation. He<br />
has received honoraria <strong>and</strong> expenses<br />
from HOYA ConBio to present material<br />
on laser dentistry. ■■<br />
JOUR NAL OF LASER DENTIS TRY | 2007 VOL 15, NO. 3<br />
155
JOUR NAL OF LASER DENTIS TRY | 2007 VOL 15, NO. 3<br />
156<br />
RESEARCH ABSTRACTS<br />
Editor’s Note: The following eight abstracts are <strong>of</strong>fered as topics <strong>of</strong> current interest. Readers are<br />
invited to submit to the editor inquiries concerning laser-related scientific topics for possible<br />
inclusion in future issues. We’ll scan the literature <strong>and</strong> present relevant abstracts.<br />
LASER BACTERICIDAL EFFECTS<br />
ON INTRAORAL IMPLANTS<br />
In their article on Er-YAG laser-assisted implant periapical<br />
lesion therapy (135-141), Dr. Avi Reyhanian <strong>and</strong><br />
Dr. Donald Coluzzi mention the bactericidal potential <strong>of</strong><br />
laser irradiation <strong>of</strong> implant surfaces. The notion <strong>of</strong><br />
utilizing laser energy to reduce surface bacteria on<br />
intraoral implants as a means to help ensure successful<br />
osseointegration <strong>and</strong> reduce the incidence <strong>of</strong> periimplantitis<br />
has been studied by a number <strong>of</strong><br />
researchers investigating a variety <strong>of</strong> wavelengths,<br />
including excimer, diode, Nd:YAG, erbium, <strong>and</strong> carbon<br />
dioxide lasers. Abstracts from a sampling <strong>of</strong> published<br />
papers representing various wavelengths appear below.<br />
Most researchers to date have investigated the antimicrobial<br />
effect, primarily due to heat generated by various<br />
lasers, on implant surfaces in in vitro experiments.<br />
Heinrich <strong>and</strong> colleagues take a different approach: use a<br />
KrF excimer (248 nm) laser to promote mucosal adhesion<br />
as a biological barrier against bacterial infection. Another<br />
group (Dörtbudak et al.) studied the effects <strong>of</strong> “s<strong>of</strong>t” diode<br />
laser exposure on implants in patients.<br />
Overall, results are mixed. Certain lasers do appear<br />
to have bactericidal potential on selected microorgan-<br />
isms on certain types <strong>of</strong> implants under certain conditions.<br />
Questions regarding the relative efficacy <strong>of</strong> laser<br />
vs. conventional treatment remain, as do concerns<br />
related to potential alteration <strong>of</strong> implant surface<br />
morphology, thermal damage to adjacent tissues, <strong>and</strong><br />
inability to reestablish the biocompatibility <strong>of</strong> contaminated<br />
surfaces. Nevertheless, the potential for laser<br />
application in promoting long-term implant success via<br />
bacterial reduction exists. Further study is warranted,<br />
especially to determine effectiveness <strong>and</strong> safety in a<br />
clinical environment, with special emphasis placed on<br />
appropriate parameter settings <strong>and</strong> duration <strong>of</strong> laser<br />
exposure.<br />
For U.S. readers, no laser has been cleared by the<br />
U.S. Food <strong>and</strong> Drug Administration for “decontaminating”<br />
or inducing bactericidal effects on intraoral<br />
implants.<br />
As always, clinicians are advised to review the<br />
specific indications for use <strong>of</strong> their lasers <strong>and</strong> to review<br />
their operator manuals for guidance on operating<br />
parameters before attempting similar techniques on<br />
their patients.
RESEARCH ABSTRACTS<br />
LASER-MODIFIED TITANIUM IMPLANTS FOR IMPROVED CELL ADHESION<br />
Andreas Heinrich, Katrin Dengler, Timo Koerner, Cornelia Haczek,<br />
Herbert Deppe, <strong>and</strong> Bernd Stritzker<br />
Concerning dental implant systems, a main problem is<br />
the adhesion <strong>of</strong> peri-implant mucosa in the cervical<br />
region. The aim <strong>of</strong> the present study was to use a laser<br />
for modifying titanium implants to promote mucosal<br />
adhesion, which is indispensable as a biological barrier<br />
against bacterial infection. By the use <strong>of</strong> a KrF excimer<br />
laser, it was possible to induce a holey structure on the<br />
polished area <strong>of</strong> the implant surface, which was<br />
analysed by a scanning electron microscope. In addi-<br />
Universität Augsburg, Augsburg, Germany<br />
<strong>Laser</strong>s Med Sci 2007 Apr 28; [Epub ahead <strong>of</strong> print] 10.1007/s10103-007-0460-z<br />
tion, the attachment <strong>of</strong> fibroblast cells to the created<br />
structures was investigated with the aid <strong>of</strong> an environmental<br />
scanning electron microscope. It turned out that<br />
the cells preferentially attach to the holey structure.<br />
Thereby, the cells form bridges inside, leading to a<br />
complete covering <strong>of</strong> the hole. In this way, a more effective<br />
biological barrier against bacteria can be created.<br />
Copyright 2007 Springer<br />
LETHAL PHOTOSENSITIZATION FOR DECONTAMINATION OF IMPLANT<br />
SUR FA CES IN THE TREATMENT OF PERI-IMPLANTITIS<br />
Orhun Dörtbudak, Robert Haas, Thomas Bernhart, Georg Mailath-Pokorny<br />
Peri-implantitis is considered to be a multifactorial<br />
process involving bacterial contamination <strong>of</strong> the<br />
implant surface. A previous study demonstrated that a<br />
combination <strong>of</strong> toluidine blue O (100 microgram/ml)<br />
<strong>and</strong> irradiation with a diode s<strong>of</strong>t laser with a wavelength<br />
<strong>of</strong> 905 nm results in an elimination <strong>of</strong><br />
Porphyromonas gingivalis (P. gingivalis), Prevotella<br />
intermedia (P. intermedia), <strong>and</strong> Actinobacillus actinomycetemcomitans<br />
(A. actinomycetemcomitans) on<br />
different implant surfaces (machined, plasma-flamesprayed,<br />
etched, hydroxyapatite-coated). The aim <strong>of</strong> this<br />
study was to examine the laser effect in vivo. In 15<br />
patients with IMZ implants who showed clinical <strong>and</strong><br />
radiographic signs <strong>of</strong> peri-implantitis, toluidine blue O<br />
University <strong>of</strong> Vienna, Vienna, Austria<br />
Clin Oral Implants Res 2001;12(2):104-108<br />
was applied to the implant surface for 1 min <strong>and</strong> the<br />
surface was then irradiated with a diode s<strong>of</strong>t laser with<br />
a wavelength <strong>of</strong> 690 nm for 60 s. Bacterial samples<br />
were taken before <strong>and</strong> after application <strong>of</strong> the dye <strong>and</strong><br />
after lasing. The cultures were evaluated semiquantitatively<br />
for A. actinomycetemcomitans, P. gingivalis, <strong>and</strong><br />
P. intermedia. It was found that the combined treatment<br />
reduced the bacterial counts by 2 log steps on<br />
average. The application <strong>of</strong> TBO <strong>and</strong> laser resulted in a<br />
significant reduction (P < 0.0001) <strong>of</strong> the initial values<br />
in all 3 groups <strong>of</strong> bacteria. Complete elimination <strong>of</strong><br />
bacteria was not achieved.<br />
Copyright 2001 Blackwell Publishing <strong>and</strong> the European<br />
Association for Osseointegration<br />
JOUR NAL OF LASER DENTIS TRY | 2007 VOL 15, NO. 3<br />
157
JOUR NAL OF LASER DENTIS TRY | 2007 VOL 15, NO. 3<br />
158<br />
RESEARCH ABSTRACTS<br />
ANTIMICROBIAL EFFICACY OF SEMICONDUCTOR LASER<br />
IRRADIATION ON IMPLANT SURFACES<br />
Matthias Kreisler, Wolfgang Kohnen, Claudio Marinello, Jürgen Scho<strong>of</strong>,<br />
Ernst Langnau, Bernd Jansen, Bernd d’Hoedt<br />
Purpose: This study was conducted to investigate the<br />
antimicrobial effect <strong>of</strong> an 809-nm semiconductor laser on<br />
common dental implant surfaces. Materials <strong>and</strong> Methods:<br />
S<strong>and</strong>blasted <strong>and</strong> acid-etched (SA), plasma-sprayed (TPS),<br />
<strong>and</strong> hydroxyapatite-coated (HA) titanium disks were<br />
incubated with a suspension <strong>of</strong> S. sanguinis (ATCC<br />
10556) <strong>and</strong> subsequently irradiated with a galliumaluminum-arsenide<br />
(GaAlAs) laser using a 600-microm<br />
optical fiber with a power output <strong>of</strong> 0.5 to 2.5 W, corresponding<br />
to power densities <strong>of</strong> 176.9 to 884.6 W/cm 2 .<br />
Bacterial reduction was calculated by counting colonyforming<br />
units on blood agar plates. Cell numbers were<br />
compared to untreated control samples <strong>and</strong> to samples<br />
treated with chlorhexidine digluconate (CHX). Heat<br />
development during irradiation <strong>of</strong> the implants placed in<br />
bone blocks was visualized by means <strong>of</strong> shortwave thermography.<br />
Results: In TPS <strong>and</strong> SA specimens, laser<br />
irradiation led to a significant bacterial reduction at all<br />
power settings. In an energy-dependent manner, the<br />
Microbiologic examinations <strong>of</strong> implants have shown that<br />
certain microorganisms described as periodontal<br />
pathogens may have an influence on the development<br />
<strong>and</strong> the progression <strong>of</strong> peri-implant disease. This experimental<br />
study aimed to examine the bactericidal effect <strong>of</strong><br />
irradiation with a s<strong>of</strong>t laser on bacteria associated with<br />
peri-implantitis following exposure to a photosensitizing<br />
substance. Platelets made <strong>of</strong> commercially pure titanium,<br />
either with a machined surface or with a hydroxyapatite<br />
or plasma-flame-sprayed surface or with a corundumblasted<br />
<strong>and</strong> etched surface, were incubated with a pure<br />
suspension <strong>of</strong> Actinobacillus actinomycetemcomitans or<br />
Porphyromonas gingivalis or Prevotella intermedia. The<br />
surfaces were then treated with a toluidine blue solution<br />
Johannes Gutenberg University, Mainz, Germany<br />
Int J Maxill<strong>of</strong>ac Implants 2003;18(5):706-711<br />
number <strong>of</strong> viable bacteria was reduced by 45.0% to 99.4%<br />
in TPS specimens <strong>and</strong> 57.6% to 99.9% in SA specimens.<br />
On HA-coated disks, a significant bacterial kill was<br />
achieved at 2.0 W (98.2%) <strong>and</strong> 2.5 W (99.3%) only (t test,<br />
P < .05). For specimens treated with CHX, the bacterial<br />
counts were reduced by 99.99% in TPS <strong>and</strong> HA-coated<br />
samples <strong>and</strong> by 99.89% in SA samples. Discussion: The<br />
results <strong>of</strong> the study indicate that the 809-nm semiconductor<br />
laser is capable <strong>of</strong> decontaminating implant<br />
surfaces. Surface characteristics determine the necessary<br />
power density to achieve a sufficient bactericidal effect.<br />
The bactericidal effect, however, was lower than that<br />
achieved by a 1-minute treatment with 0.2% CHX. The<br />
rapid heat generation during laser irradiation requires<br />
special consideration <strong>of</strong> thermal damage to adjacent<br />
tissues. Conclusion: No obvious advantage <strong>of</strong> semiconductor<br />
laser treatment over conventional methods <strong>of</strong><br />
disinfection could be detected in vitro.<br />
Copyright 2003 Quintessence Publishing Co., Inc.<br />
ELIMINATION OF BACTERIA ON DIFFERENT IMPLANT SURFACES THROUGH<br />
PHOTOSENSITIZATION AND SOFT LASER: AN IN VITRO STUDY<br />
Robert Haas, Orhun Dörtbudak, Nikoletta Mensdorff-Pouilly, Georg Mailath<br />
University <strong>of</strong> Vienna, Vienna, Austria<br />
Clin Oral Implants Res 1997;8(4):249-254<br />
<strong>and</strong> irradiated with a diode s<strong>of</strong>t laser with a wavelength<br />
<strong>of</strong> 905 nm for 1 min. None <strong>of</strong> the smears obtained from<br />
the thus-treated surfaces showed bacterial growth,<br />
whereas the smears obtained from surfaces that had<br />
been subjected to only one type <strong>of</strong> treatment showed<br />
unchanged growth <strong>of</strong> every target organism tested (P <<br />
0.0006). Electron microscopic inspection <strong>of</strong> the thustreated<br />
platelets revealed that combined dye/laser<br />
treatment resulted in the destruction <strong>of</strong> bacterial cells.<br />
The present in vitro results indicate that lethal photosensitization<br />
may be <strong>of</strong> use for treatment <strong>of</strong> peri-implantitis.<br />
Copyright 1997 Blackwell Publishing <strong>and</strong> the European<br />
Association for Osseointegration
RESEARCH ABSTRACTS<br />
EFFECTS OF THE ND:YAG DENTAL LASER ON PLASMA-SPRAYED<br />
AND HYDROXYAPATITE-COATED TITANIUM DENTAL IMPLANTS:<br />
SURFACE ALTERATION AND ATTEMPTED STERILIZATION<br />
The Nd:YAG dental laser has been recommended for a<br />
number <strong>of</strong> applications, including the decontamination<br />
or sterilization <strong>of</strong> surfaces <strong>of</strong> dental implants that are<br />
diseased or failing. The effects <strong>of</strong> laser irradiation in<br />
vitro (1) on the surface properties <strong>of</strong> plasma-sprayed<br />
titanium <strong>and</strong> plasma-sprayed hydroxyapatite-coated<br />
titanium dental implants, <strong>and</strong> (2) on the potential to<br />
sterilize those surfaces after contamination with spores<br />
<strong>of</strong> Bacillus subtilis have been examined. Surface effects<br />
were examined by scanning electron microscopy, energy<br />
dispersive spectroscopy, <strong>and</strong> X-ray diffraction after<br />
laser irradiation at 0.3, 2.0, <strong>and</strong> 3.0 W using either<br />
contact or noncontact h<strong>and</strong>pieces. Controls received no<br />
Titanium platelets with a s<strong>and</strong>-blasted <strong>and</strong> acid-etched<br />
surface were coated with bovine serum albumin <strong>and</strong><br />
incubated with a suspension <strong>of</strong> Porphyromonas gingivalis<br />
(ATCC 33277). Four groups with a total <strong>of</strong> 48 specimens<br />
were formed. <strong>Laser</strong> irradiation <strong>of</strong> the specimens (n = 12)<br />
was performed on a computer-controlled XY translation<br />
stage at pulse energy 60 mJ <strong>and</strong> frequency 10 pps.<br />
Twelve specimens were treated with an air powder<br />
system. After the respective treatment, human gingival<br />
fibroblasts were incubated on the specimens. The proliferation<br />
rate was determined by means <strong>of</strong> fluorescence<br />
activity <strong>of</strong> a redox indicator (Alamar Blue Assay) which is<br />
reduced by metabolic activity related to cellular growth.<br />
Proliferation was determined up to 72 h. Contaminated<br />
<strong>and</strong> nontreated as well as sterile specimens served as<br />
positive <strong>and</strong> negative controls. Proliferation activity was<br />
Carl M. Block, John A. Mayo, Gerald H. Evans<br />
Louisiana State University Medical Center, New Orleans, Louisiana<br />
Int J Oral Maxill<strong>of</strong>ac Implants 1992;7(4):441-449<br />
IN VITRO EVALUATION OF THE BIOCOMPATIBILITY OF<br />
CONTAMINATED IMPLANT SURFACES TREATED WITH<br />
AN ER:YA G LA SER AND AN AIR POWDER SY STEM<br />
Matthias Kreisler, Wolfgang Kohnen, Ann-Babett Christ<strong>of</strong>fers, Hermann Götz, Bernd Jansen,<br />
Heinz Duschner, Bernd d’Hoedt<br />
Johannes Gutenberg-University Mainz, Mainz, Germany<br />
Clin Oral Implants Res 2005;16(1):36-43<br />
laser irradiation. Melting, loss <strong>of</strong> porosity, <strong>and</strong> other<br />
surface alterations were observed on both types <strong>of</strong><br />
implants, even with the lowest power setting. For the<br />
sterilization study, both types <strong>of</strong> implants were first<br />
sterilized by exposure to ethylene oxide <strong>and</strong> then<br />
contaminated with spores <strong>of</strong> B. subtilis. After laser irradiation,<br />
the implants were transferred to sterile growth<br />
medium <strong>and</strong> incubated. <strong>Laser</strong> irradiation did not sterilize<br />
either type <strong>of</strong> implant. The spore-contaminated<br />
implants in the control group were successfully sterilized<br />
with ethylene oxide.<br />
Copyright 1992 Quintessence Publishing Co., Inc.<br />
significantly (Mann-Whitney U-test, P < 0.05) reduced on<br />
contaminated <strong>and</strong> nontreated platelets when compared<br />
to sterile specimens. Both on laser as well as air powdertreated<br />
specimens, cell growth was not significantly<br />
different from that on sterile specimens. Air powder<br />
treatment led to microscopically visible alterations <strong>of</strong> the<br />
implant surface whereas laser-treated surfaces remained<br />
unchanged. Both air powder <strong>and</strong> Er:YAG laser irradiation<br />
have a good potential to remove cytotoxic bacterial<br />
components from implant surfaces. At the irradiation<br />
parameters investigated, the Er:YAG laser ensures a reliable<br />
decontamination <strong>of</strong> implants in vitro without<br />
altering surface morphology.<br />
Copyright 2005 Blackwell Publishing <strong>and</strong> the European<br />
Association for Osseointegration<br />
JOUR NAL OF LASER DENTIS TRY | 2007 VOL 15, NO. 3<br />
159
JOUR NAL OF LASER DENTIS TRY | 2007 VOL 15, NO. 3<br />
160<br />
RESEARCH ABSTRACTS<br />
INFLUENCE OF AN ERBIUM, CHROMIUM-DOPED YTTRIUM,<br />
SCANDIUM, GALLIUM, AND GARNET (ER,CR:YSGG) LASER<br />
ON THE REESTABLISHMENT OF THE BIOCOMPATIBILITY<br />
OF CONTAMINATED TITANIUM IMPLANT SURFACES<br />
Frank Schwarz, Enaas Nuesry, Katrin Bieling, Monika Herten, Jürgen Becker<br />
Background: The aim <strong>of</strong> the present study was to evaluate<br />
the influence <strong>of</strong> an erbium, chromium-doped<br />
yttrium, sc<strong>and</strong>ium, gallium, <strong>and</strong> garnet (Er,Cr:YSGG<br />
laser [ERCL]) on (1) the surface structure <strong>and</strong> biocompatibility<br />
<strong>of</strong> titanium implants <strong>and</strong> (2) the removal <strong>of</strong><br />
plaque bi<strong>of</strong>ilms <strong>and</strong> reestablishment <strong>of</strong> the biocompatibility<br />
<strong>of</strong> contaminated titanium surfaces. Methods:<br />
Intraoral splints were used to collect an in vivo<br />
supragingival bi<strong>of</strong>ilm on s<strong>and</strong>-blasted <strong>and</strong> acid-etched<br />
titanium disks for 24 hours. ERCL was used at an<br />
energy output <strong>of</strong> 0.5, 1.0, 1.5, 2.0, <strong>and</strong> 2.5 W for the<br />
irradiation <strong>of</strong> (1) noncontaminated (20 <strong>and</strong> 25 Hz) <strong>and</strong><br />
(2) plaque-contaminated (25 Hz) titanium disks.<br />
Unworn <strong>and</strong> untreated nonirradiated, sterile titanium<br />
disks served as untreated controls (UC). Specimens<br />
were incubated with SaOs-2 osteoblasts for 6 days.<br />
Treatment time, residual plaque bi<strong>of</strong>ilm (RPB) areas<br />
(%), mitochondrial cell activity (MA) (counts per<br />
B ACTERICIDAL EFFICACY OF CARBON DIOXIDE LASER<br />
AGAINST BACTERIA-CONTAMINATED TITANIUM IMPLANT AND<br />
SUBSEQUENT CELLULAR ADHESION TO IRRADIATED AREA<br />
Background <strong>and</strong> Objective: The aim <strong>of</strong> this study was to<br />
assess CO 2 laser ability to eliminate bacteria from titanium<br />
implant surfaces. The changes <strong>of</strong> the surface<br />
structure, the rise in temperature, <strong>and</strong> the damage <strong>of</strong><br />
connective tissue cells after laser irradiation were also<br />
considered. Study Design/Materials <strong>and</strong> Methods:<br />
Streptococcus sanguis <strong>and</strong> Porphyromonas gingivalis on<br />
titanium discs were irradiated by an exp<strong>and</strong>ed beam <strong>of</strong><br />
CO 2 laser. Surface alteration was observed by a light,<br />
<strong>and</strong> a scanning electron, microscope. Temperature was<br />
measured with a thermograph. Damage <strong>of</strong> fibroblastic<br />
(L-929) <strong>and</strong> osteoblastic (MC3T3-E1) cells outside the<br />
Heinrich Heine University, Düsseldorf, Germany<br />
J Periodontol 2006;77(11):1820-1827<br />
Taku Kato, Haruka Kusakari, Etsuro Hoshino<br />
Niigata University, Niigata, Japan<br />
<strong>Laser</strong>s Surg Med 1998;23(5):299-309<br />
second), <strong>and</strong> cell morphology/surface changes (scanning<br />
electron microscopy [SEM]) were assessed. Results: (1)<br />
ERCL using either 0.5, 1.0, 1.5, 2.0, or 2.5 W at both 20<br />
<strong>and</strong> 25 Hz resulted in comparable mean MA values as<br />
measured in the UC group. A monolayer <strong>of</strong> flattened<br />
SaOs-2 cells showing complete cytoplasmatic extensions<br />
<strong>and</strong> lamellopodia was observed in both ERCL <strong>and</strong><br />
UC groups. (2) Mean RPB areas decreased significantly<br />
with increasing energy settings (53.8 +/- 2.2 at 0.5 W to<br />
9.8 +/- 6.2 at 2.5 W). However, mean MA values were<br />
significantly higher in the UC group. Conclusion:<br />
Within the limits <strong>of</strong> the present study, it was concluded<br />
that even though ERCL exhibited a high efficiency to<br />
remove plaque bi<strong>of</strong>ilms in an energy-dependent<br />
manner, it failed to reestablish the biocompatibility <strong>of</strong><br />
contaminated titanium surfaces.<br />
Copyright 2006 The American <strong>Academy</strong> <strong>of</strong> Periodontology<br />
irradiation spot <strong>and</strong> adhesion <strong>of</strong> the cells to the irradiated<br />
area were also estimated. Results: All the<br />
organisms (108) <strong>of</strong> S. sanguis <strong>and</strong> P. gingivalis were<br />
killed by the irradiation at 286 J/cm 2 <strong>and</strong> 245 J/cm 2 ,<br />
respectively. Furthermore, laser irradiation did not<br />
cause surface alteration, rise <strong>of</strong> temperature, serious<br />
damage <strong>of</strong> connective tissue cells located outside the<br />
irradiation spot, or inhibition <strong>of</strong> cell adhesion to the<br />
irradiated area. Conclusion: CO 2 laser irradiation with<br />
exp<strong>and</strong>ed beam may be useful in removing bacterial<br />
contaminants from implant surface.<br />
Copyright 1998 Wiley-Liss, Inc. ■■