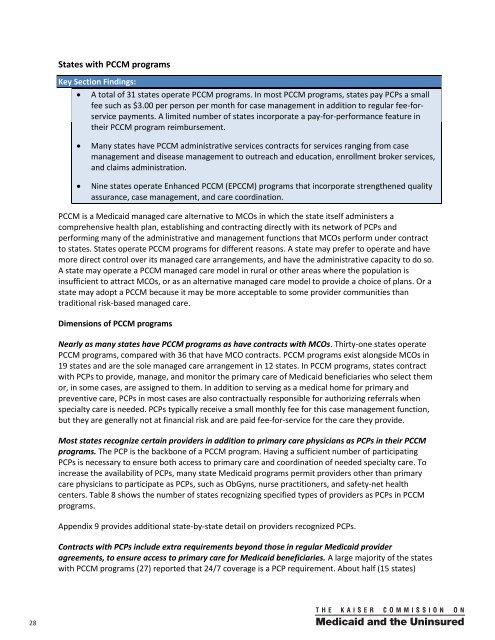
<strong>State</strong>s with PCCM programsKey Secti<strong>on</strong> Findings:A total of 31 states operate PCCM programs. In most PCCM programs, states pay PCPs a smallfee such as $3.00 per pers<strong>on</strong> per m<strong>on</strong>th for case management in additi<strong>on</strong> to regular fee-forservicepayments. A limited number of states incorporate a pay-for-performance feature intheir PCCM program reimbursement.Many states have PCCM administrative services c<strong>on</strong>tracts for services ranging from casemanagement and disease management to outreach and educati<strong>on</strong>, enrollment broker services,and claims administrati<strong>on</strong>.Nine states operate Enhanced PCCM (EPCCM) programs that incorporate strengthened qualityassurance, case management, and care coordinati<strong>on</strong>.PCCM is a <strong>Medicaid</strong> managed care alternative to MCOs in which the state itself administers acomprehensive health plan, establishing and c<strong>on</strong>tracting directly with its network of PCPs andperforming many of the administrative and management functi<strong>on</strong>s that MCOs perform under c<strong>on</strong>tractto states. <strong>State</strong>s operate PCCM programs for different reas<strong>on</strong>s. A state may prefer to operate and havemore direct c<strong>on</strong>trol over its managed care arrangements, and have the administrative capacity to do so.A state may operate a PCCM managed care model in rural or other areas where the populati<strong>on</strong> isinsufficient to attract MCOs, or as an alternative managed care model to provide a choice of plans. Or astate may adopt a PCCM because it may be more acceptable to some provider communities thantraditi<strong>on</strong>al risk-based managed care.Dimensi<strong>on</strong>s of PCCM programsNearly as many states have PCCM programs as have c<strong>on</strong>tracts with MCOs. Thirty-<strong>on</strong>e states operatePCCM programs, compared with 36 that have MCO c<strong>on</strong>tracts. PCCM programs exist al<strong>on</strong>gside MCOs in19 states and are the sole managed care arrangement in 12 states. In PCCM programs, states c<strong>on</strong>tractwith PCPs to provide, manage, and m<strong>on</strong>itor the primary care of <strong>Medicaid</strong> beneficiaries who select themor, in some cases, are assigned to them. In additi<strong>on</strong> to serving as a medical home for primary andpreventive care, PCPs in most cases are also c<strong>on</strong>tractually resp<strong>on</strong>sible for authorizing referrals whenspecialty care is needed. PCPs typically receive a small m<strong>on</strong>thly fee for this case management functi<strong>on</strong>,but they are generally not at financial risk and are paid fee-for-service for the care they provide.Most states recognize certain providers in additi<strong>on</strong> to primary care physicians as PCPs in their PCCMprograms. The PCP is the backb<strong>on</strong>e of a PCCM program. Having a sufficient number of participatingPCPs is necessary to ensure both access to primary care and coordinati<strong>on</strong> of needed specialty care. Toincrease the availability of PCPs, many state <strong>Medicaid</strong> programs permit providers other than primarycare physicians to participate as PCPs, such as ObGyns, nurse practiti<strong>on</strong>ers, and safety-net healthcenters. Table 8 shows the number of states recognizing specified types of providers as PCPs in PCCMprograms.Appendix 9 provides additi<strong>on</strong>al state-by-state detail <strong>on</strong> providers recognized PCPs.C<strong>on</strong>tracts with PCPs include extra requirements bey<strong>on</strong>d those in regular <strong>Medicaid</strong> provideragreements, to ensure access to primary care for <strong>Medicaid</strong> beneficiaries. A large majority of the stateswith PCCM programs (27) reported that 24/7 coverage is a PCP requirement. About half (15 states)28 00
eported that they limit PCP panel size, and slightly smaller numbers require PCPs to meet statereporting requirements (14 states) and to participate in state quality initiatives (13 states).Appendix 10 provides state-by-state detail <strong>on</strong> PCPrequirements and <strong>on</strong> PCP payment methods,discussed next.PCCM program payment methods and practicesMost states pay PCPs a small case management fee.<strong>State</strong>s provide some kind of compensati<strong>on</strong> to PCPs inadditi<strong>on</strong> to regular fee-for-service reimbursement. Alarge majority of states (25 of 29 resp<strong>on</strong>ding) payPCPs a per member per m<strong>on</strong>th (PMPM) casemanagement fee. A very small number reported thatthey pay a capitati<strong>on</strong> amount to PCPs withgatekeeper resp<strong>on</strong>sibility for other services, haveshared savings arrangements, or pay enhanced feefor-servicerates.Table 8: Recognized Primary <strong>Care</strong>Provider (PCP) Types* in PCCM ProgramsPCP provider typeNo. of statesrecognizingOb/Gyn 27Nurse practiti<strong>on</strong>er 23FQHC 24Physician group/clinic 22Physician specialist 18Physician assistant 14Nurse midwife 12*In additi<strong>on</strong> to general practiti<strong>on</strong>ers, family andinternal medicine physicians, and pediatricians.<strong>State</strong>s often pay a PMPM case management fee of $2.00 to $4.00, with $3.00 being the most frequentlycited amount. The lowest case management fee reported was $1.00 PMPM in North Carolina, where thestate also pays an additi<strong>on</strong>al PMPM for networks in its Enhanced PCCM program (discussed later). Thehighest PMPM was $175.00 in Georgia, for case managers who coordinate the care of frail elders andindividuals under the state’s “Services Opti<strong>on</strong>s Using Resources in a Community Envir<strong>on</strong>ment” (SOURCE)program, which is classified as an Enhanced PCCM program.One-fourth of states with PCCM programs include a P4P feature in their payment to PCPs. Eight of the31 states with PCCM programs reported a P4P comp<strong>on</strong>ent to their PCCM payments. <strong>State</strong> P4P strategiesfocus <strong>on</strong> a variety of access- and patient care-related objectives. In some states, PCPs can earn extrapayment if, for example, they have extended office hours, reduce emergency room use, or work towardgaining status as a NCQA-recognized Patient-Centered Medical Home. Other P4P policies reward PCPsbased <strong>on</strong> clinical performance – for example, based <strong>on</strong> measures that indicate appropriate managementof diabetes, hypertensi<strong>on</strong>, and other chr<strong>on</strong>ic c<strong>on</strong>diti<strong>on</strong>s, timely prenatal care, cancer screening rates,and EPSDT screening rates.Idaho is piloting management of pers<strong>on</strong>s with diabetes under a P4P arrangement with FQHCs <strong>on</strong>ly.In 2011, Louisiana is paying PCPs <strong>on</strong> a per member per m<strong>on</strong>th basis: $.25 for doing their own EPSDTscreenings; $.75 for having extended hours; $.50 for working to become an NCQA-recognized Patient CenteredMedical Home by the end of CY 2011; and $.75 if the PCP is in the lowest quartile for certain ER visit procedure,$.50 if in sec<strong>on</strong>d lowest quartile, and $.25 if in the third lowest quartile (phasing out after six m<strong>on</strong>ths).Maine reported that 40 percent of its PCCM P4P reimbursement is based <strong>on</strong> performance <strong>on</strong> an accessmeasure, 30 percent <strong>on</strong> performance <strong>on</strong> an ER utilizati<strong>on</strong> measure, and 30 percent <strong>on</strong> performance <strong>on</strong> aquality measure.Many states c<strong>on</strong>tract for PCCM administrative services. Over half the states with PCCM programsreported that they have PCCM administrative services c<strong>on</strong>tracts. Three of these 16 states (Illinois,29
- Page 1 and 2: kaisercommission onmedicaidand theu
- Page 3 and 4: kaisercommission onmedicaidand theu
- Page 5 and 6: Table of ContentsExecutive Summary
- Page 7 and 8: EXECUTIVE SUMMARYMedicaid, the publ
- Page 9 and 10: party enrollment brokers to provide
- Page 11 and 12: HEDIS©, CAHPS©, and state-specifi
- Page 13: ConclusionFor over 30 years, state
- Page 16 and 17: from the recession and the slow rec
- Page 18 and 19: A note on Medicaid managed care ter
- Page 20 and 21: Managed caremodelTable 1: Medicaid
- Page 23 and 24: States are increasingly mandating m
- Page 25 and 26: States with Medicaid MCOsKey Sectio
- Page 27 and 28: States have “auto-assignment” a
- Page 29 and 30: excess of a specified threshold for
- Page 31 and 32: Dental care and outpatient and inpa
- Page 33: the second trimester, and within th
- Page 37 and 38: States with non-comprehensive PHPsK
- Page 39 and 40: Measuring, monitoring, and improvin
- Page 41 and 42: seven states required 10 measures o
- Page 43 and 44: CAHPS© surveys. North Carolina is
- Page 45 and 46: Special initiatives to improve qual
- Page 47 and 48: public health efforts to reduce dis
- Page 49 and 50: Medicaid managed long-term care and
- Page 51 and 52: (e.g., need to credential Adult <st
- Page 53 and 54: In many states, broader efforts foc
- Page 55 and 56: Looking ahead: Medicaid managed car
- Page 57 and 58: ConclusionFor over 30 years, state
- Page 59 and 60: APPENDIX 2: Summary of Medicaid Man
- Page 61 and 62: Program Name(e.g., Popular Name, 19
- Page 63 and 64: APPENDIX 3: MCO Contracts, Plan Cha
- Page 65 and 66: State(No. ofcontracts)NameEnrollmen
- Page 67 and 68: State(No. ofcontracts)NameEnrollmen
- Page 69 and 70: APPENDIX 5: MCO Capitation Rate-Set
- Page 71 and 72: APPENDIX 7: MCO Network Adequacy Re
- Page 73 and 74: State Primary Care Obstetric Care S
- Page 75 and 76: APPENDIX 9: Providers Recognized as
- Page 77 and 78: APPENDIX 11: PCCM Administrative Se
- Page 79 and 80: APPENDIX 13: Initiatives to Improve
- Page 81 and 82: I. MANAGED CARE OVERVIEW1. Total Ma
- Page 83 and 84: 4. Enrollment Requirements.a. We ar
- Page 85 and 86:
ii. Please indicate whether the fac
- Page 87 and 88:
c. Required Providers: We are inter
- Page 89 and 90:
IV. NON-COMPREHENSIVE PREPAID HEALT
- Page 91 and 92:
. Does your state use CAHPS© surve
- Page 93 and 94:
VI. SPECIAL INITIATIVESAll states s
- Page 95 and 96:
Appendix I: Managed Care Contracts1
- Page 97:
Appendix II: Clinical Quality Perfo
- Page 100:
1330 G S T R E E T NW, W A S H I N