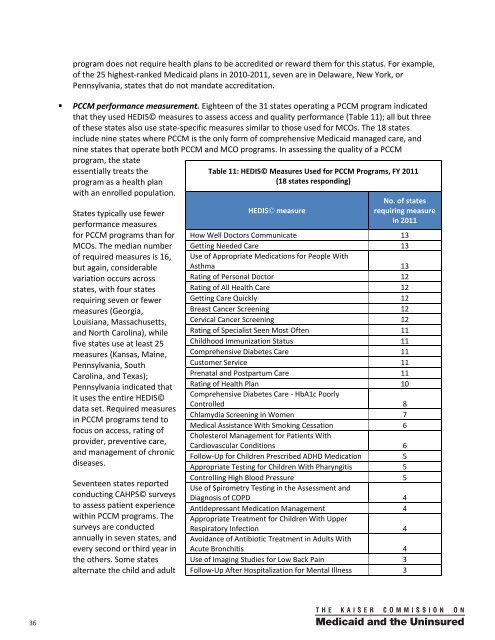
program does not require health plans to be accredited or reward them for this status. For example,of the 25 highest-ranked <strong>Medicaid</strong> plans in 2010-2011, seven are in Delaware, New York, orPennsylvania, states that do not mandate accreditati<strong>on</strong>.• PCCM performance measurement. Eighteen of the 31 states operating a PCCM program indicatedthat they used HEDIS© measures to assess access and quality performance (Table 11); all but threeof these states also use state-specific measures similar to those used for MCOs. The 18 statesinclude nine states where PCCM is the <strong>on</strong>ly form of comprehensive <strong>Medicaid</strong> managed care, andnine states that operate both PCCM and MCO programs. In assessing the quality of a PCCMprogram, the stateessentially treats theprogram as a health planwith an enrolled populati<strong>on</strong>.<strong>State</strong>s typically use fewerperformance measuresfor PCCM programs than forMCOs. The median numberof required measures is 16,but again, c<strong>on</strong>siderablevariati<strong>on</strong> occurs acrossstates, with four statesrequiring seven or fewermeasures (Georgia,Louisiana, Massachusetts,and North Carolina), whilefive states use at least 25measures (Kansas, Maine,Pennsylvania, SouthCarolina, and Texas);Pennsylvania indicated thatit uses the entire HEDIS©data set. Required measuresin PCCM programs tend tofocus <strong>on</strong> access, rating ofprovider, preventive care,and management of chr<strong>on</strong>icdiseases.Seventeen states reportedc<strong>on</strong>ducting CAHPS© surveysto assess patient experiencewithin PCCM programs. Thesurveys are c<strong>on</strong>ductedannually in seven states, andevery sec<strong>on</strong>d or third year inthe others. Some statesalternate the child and adultTable 11: HEDIS© Measures Used for PCCM Programs, FY 2011(18 states resp<strong>on</strong>ding)HEDIS© measureNo. of statesrequiring measurein 2011How Well Doctors Communicate 13Getting Needed <strong>Care</strong> 13Use of Appropriate Medicati<strong>on</strong>s for People WithAsthma 13Rating of Pers<strong>on</strong>al Doctor 12Rating of All Health <strong>Care</strong> 12Getting <strong>Care</strong> Quickly 12Breast Cancer Screening 12Cervical Cancer Screening 12Rating of Specialist Seen Most Often 11Childhood Immunizati<strong>on</strong> Status 11Comprehensive Diabetes <strong>Care</strong> 11Customer Service 11Prenatal and Postpartum <strong>Care</strong> 11Rating of Health Plan 10Comprehensive Diabetes <strong>Care</strong> - HbA1c PoorlyC<strong>on</strong>trolled 8Chlamydia Screening in Women 7Medical Assistance With Smoking Cessati<strong>on</strong> 6Cholesterol Management for Patients WithCardiovascular C<strong>on</strong>diti<strong>on</strong>s 6Follow-Up for Children Prescribed ADHD Medicati<strong>on</strong> 5Appropriate Testing for Children With Pharyngitis 5C<strong>on</strong>trolling High Blood Pressure 5Use of Spirometry Testing in the Assessment andDiagnosis of COPD 4Antidepressant Medicati<strong>on</strong> Management 4Appropriate Treatment for Children With UpperRespiratory Infecti<strong>on</strong> 4Avoidance of Antibiotic Treatment in Adults WithAcute Br<strong>on</strong>chitis 4Use of Imaging Studies for Low Back Pain 3Follow-Up After Hospitalizati<strong>on</strong> for Mental Illness 336 00
CAHPS© surveys. North Carolina is the <strong>on</strong>ly state that indicated that it plans to submit the results ofits upcoming CAHPS© survey for its PCCM program to NCQA.• PHP performance measurement. Thirteen of the 25 states with n<strong>on</strong>-comprehensive PHPs reportedthat they assess quality and performance in these plans using HEDIS© or similar state-specificmeasures. <strong>State</strong>s tailor the measures they use to corresp<strong>on</strong>d to the limited benefits provided bythese plans. Thus, because the most comm<strong>on</strong> PHPs are plans providing behavioral health services,typical performance measures relate to access to and timeliness of routine appointments forbehavioral health care, coordinati<strong>on</strong> of behavioral and physical health services, and follow-up careafter hospitalizati<strong>on</strong> for mental illness. Not surprisingly, most states use fewer measures for n<strong>on</strong>comprehensivePHPs than for either MCOs or PCCM programs. Only three states reported usingCAHPS© for their PHPs (Ariz<strong>on</strong>a, Colorado, and DC).Close to a third of states also measure quality in the FFS comp<strong>on</strong>ents of their <strong>Medicaid</strong> programs.Sixteen states reported using HEDIS© measures in FFS. The number of measures varies widely, from alow of 10 or fewer in three states (Ohio, Louisiana, and Wyoming), to a high of 25 or more in threestates (Kansas, Maine, and South Carolina). In additi<strong>on</strong> to providing states with informati<strong>on</strong> <strong>on</strong> accessand quality in FFS, FFS data can also provide a useful benchmark for comparis<strong>on</strong> to managed careperformance in states that have MCOs and/or a PCCM program. In additi<strong>on</strong> to HEDIS© measures, sevenstates reported using state-specific measures for FFS, usually the same <strong>on</strong>es added to assess managedcare, or representing areas of high policy priority, such as access to well-child care and dental care. Eightstates reported that they c<strong>on</strong>duct the CAHPS© survey or a similar survey of patient experience in FFS atthe same time they administer the survey am<strong>on</strong>g managed care enrollees (Colorado, Kansas, Maine,Michigan, Oreg<strong>on</strong>, South Carolina, Virginia, and Washingt<strong>on</strong>).Three-fourths of states with MCOs publicly report <strong>on</strong> the quality of their MCOs, and half of states withPCCM programs publish quality reports <strong>on</strong> those programs. The data collected by states and healthplans provide rich informati<strong>on</strong> about how well <strong>Medicaid</strong> systems of care are performing, how providersand plans compare in their effectiveness, whether patients can access care when they need it, and areaswhere there is room for improvement. This informati<strong>on</strong> supports state value-based purchasing effortsand can help states structure payment to advance quality goals. Also, <strong>on</strong> the principle that transparencyregarding performance will drive improvement in quality, states also provide data <strong>on</strong> performance toproviders, plans, beneficiaries, the public, and policymakers.Thirty-five states reported that they publicly release reports <strong>on</strong> MCO and/or PCCM quality performance,most often by posting the report <strong>on</strong> the <strong>Medicaid</strong> program’s website. Most states also provide thereports back to providers and health plans that submitted the data, while others provide the reports totheir legislature. Three states do not publish quality reports, but make the informati<strong>on</strong> available up<strong>on</strong>request. The total of 38 states that make quality informati<strong>on</strong> public includes 28 of the 36 states withMCOs, and 16 of the 31 states that operate PCCM programs. Two of the states reported that they firstmade quality reports public in FY 2011, an indicati<strong>on</strong> that public reporting of quality data may begrowing. Nine states also publicly report <strong>on</strong> PHPs’ performance, allowing a look at quality across allforms of managed care in those states. Further, six states extend quality performance reporting to then<strong>on</strong>-managed fee-for-service comp<strong>on</strong>ents of their <strong>Medicaid</strong> programs.A number of states prepare quality “report cards.” Fifteen states with MCOs and North Carolina, aPCCM-<strong>on</strong>ly state, reported that they prepare a quality report card, using HEDIS©, CAHPS©, and statespecificdata, that <strong>Medicaid</strong> beneficiaries can use to compare and choose health plans. For example, the37
- Page 1 and 2: kaisercommission onmedicaidand theu
- Page 3 and 4: kaisercommission onmedicaidand theu
- Page 5 and 6: Table of ContentsExecutive Summary
- Page 7 and 8: EXECUTIVE SUMMARYMedicaid, the publ
- Page 9 and 10: party enrollment brokers to provide
- Page 11 and 12: HEDIS©, CAHPS©, and state-specifi
- Page 13: ConclusionFor over 30 years, state
- Page 16 and 17: from the recession and the slow rec
- Page 18 and 19: A note on Medicaid managed care ter
- Page 20 and 21: Managed caremodelTable 1: Medicaid
- Page 23 and 24: States are increasingly mandating m
- Page 25 and 26: States with Medicaid MCOsKey Sectio
- Page 27 and 28: States have “auto-assignment” a
- Page 29 and 30: excess of a specified threshold for
- Page 31 and 32: Dental care and outpatient and inpa
- Page 33 and 34: the second trimester, and within th
- Page 35 and 36: eported that they limit PCP panel s
- Page 37 and 38: States with non-comprehensive PHPsK
- Page 39 and 40: Measuring, monitoring, and improvin
- Page 41: seven states required 10 measures o
- Page 45 and 46: Special initiatives to improve qual
- Page 47 and 48: public health efforts to reduce dis
- Page 49 and 50: Medicaid managed long-term care and
- Page 51 and 52: (e.g., need to credential Adult <st
- Page 53 and 54: In many states, broader efforts foc
- Page 55 and 56: Looking ahead: Medicaid managed car
- Page 57 and 58: ConclusionFor over 30 years, state
- Page 59 and 60: APPENDIX 2: Summary of Medicaid Man
- Page 61 and 62: Program Name(e.g., Popular Name, 19
- Page 63 and 64: APPENDIX 3: MCO Contracts, Plan Cha
- Page 65 and 66: State(No. ofcontracts)NameEnrollmen
- Page 67 and 68: State(No. ofcontracts)NameEnrollmen
- Page 69 and 70: APPENDIX 5: MCO Capitation Rate-Set
- Page 71 and 72: APPENDIX 7: MCO Network Adequacy Re
- Page 73 and 74: State Primary Care Obstetric Care S
- Page 75 and 76: APPENDIX 9: Providers Recognized as
- Page 77 and 78: APPENDIX 11: PCCM Administrative Se
- Page 79 and 80: APPENDIX 13: Initiatives to Improve
- Page 81 and 82: I. MANAGED CARE OVERVIEW1. Total Ma
- Page 83 and 84: 4. Enrollment Requirements.a. We ar
- Page 85 and 86: ii. Please indicate whether the fac
- Page 87 and 88: c. Required Providers: We are inter
- Page 89 and 90: IV. NON-COMPREHENSIVE PREPAID HEALT
- Page 91 and 92: . Does your state use CAHPS© surve
- Page 93 and 94:
VI. SPECIAL INITIATIVESAll states s
- Page 95 and 96:
Appendix I: Managed Care Contracts1
- Page 97:
Appendix II: Clinical Quality Perfo
- Page 100:
1330 G S T R E E T NW, W A S H I N