RAI-MDS 2.0 Nutritional Care Resource Guide April 2011 - CCIM
RAI-MDS 2.0 Nutritional Care Resource Guide April 2011 - CCIM
RAI-MDS 2.0 Nutritional Care Resource Guide April 2011 - CCIM
- No tags were found...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
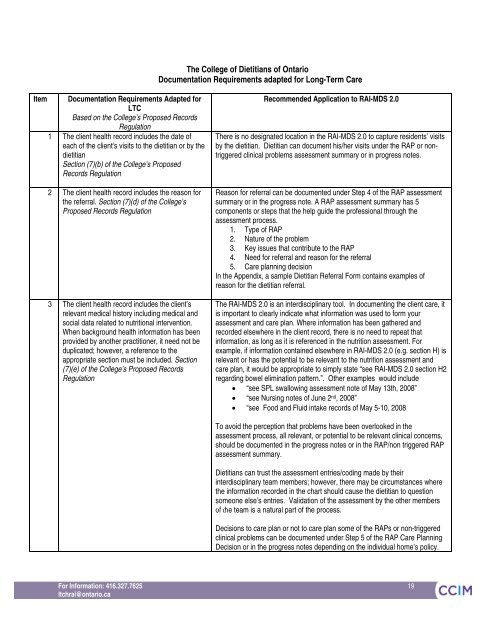
The College of Dietitians of OntarioDocumentation Requirements adapted for Long-Term <strong>Care</strong>ItemDocumentation Requirements Adapted forLTCBased on the College’s Proposed RecordsRegulation1 The client health record includes the date ofeach of the client's visits to the dietitian or by thedietitianSection (7)(b) of the College’s ProposedRecords Regulation2 The client health record includes the reason forthe referral. Section (7)(d) of the College’sProposed Records Regulation3 The client health record includes the client’srelevant medical history including medical andsocial data related to nutritional intervention.When background health information has beenprovided by another practitioner, it need not beduplicated; however, a reference to theappropriate section must be included. Section(7)(e) of the College’s Proposed RecordsRegulationRecommended Application to <strong>RAI</strong>-<strong>MDS</strong> <strong>2.0</strong>There is no designated location in the <strong>RAI</strong>-<strong>MDS</strong> <strong>2.0</strong> to capture residents’ visitsby the dietitian. Dietitian can document his/her visits under the RAP or nontriggeredclinical problems assessment summary or in progress notes.Reason for referral can be documented under Step 4 of the RAP assessmentsummary or in the progress note. A RAP assessment summary has 5components or steps that the help guide the professional through theassessment process.1. Type of RAP2. Nature of the problem3. Key issues that contribute to the RAP4. Need for referral and reason for the referral5. <strong>Care</strong> planning decisionIn the Appendix, a sample Dietitian Referral Form contains examples ofreason for the dietitian referral.The <strong>RAI</strong>-<strong>MDS</strong> <strong>2.0</strong> is an interdisciplinary tool. In documenting the client care, itis important to clearly indicate what information was used to form yourassessment and care plan. Where information has been gathered andrecorded elsewhere in the client record, there is no need to repeat thatinformation, as long as it is referenced in the nutrition assessment. Forexample, if information contained elsewhere in <strong>RAI</strong>-<strong>MDS</strong> <strong>2.0</strong> (e.g. section H) isrelevant or has the potential to be relevant to the nutrition assessment andcare plan, it would be appropriate to simply state “see <strong>RAI</strong>-<strong>MDS</strong> <strong>2.0</strong> section H2regarding bowel elimination pattern.”. Other examples would include “see SPL swallowing assessment note of May 13th, 2008” “see Nursing notes of June 2 nd , 2008” “see Food and Fluid intake records of May 5-10, 2008To avoid the perception that problems have been overlooked in theassessment process, all relevant, or potential to be relevant clinical concerns,should be documented in the progress notes or in the RAP/non triggered RAPassessment summary.Dietitians can trust the assessment entries/coding made by theirinterdisciplinary team members; however, there may be circumstances wherethe information recorded in the chart should cause the dietitian to questionsomeone else’s entries. Validation of the assessment by the other members3-37 of the team is a natural part of the process.Decisions to care plan or not to care plan some of the RAPs or non-triggeredclinical problems can be documented under Step 5 of the RAP <strong>Care</strong> PlanningDecision or in the progress notes depending on the individual home’s policy.For Information: 416.327.7625 19ltchrai@ontario.ca19