ORIGINAL CONTRIBUTION AND CLINICAL INVESTIGATIONIntroductionThe core values <strong>of</strong> general practiceinclude holism and patientcentredness.Holism, the integration<strong>of</strong> physical, psychological and socialcomponents <strong>of</strong> health problems inmaking diagnoses and planningmanagement, is well established asa central <strong>issue</strong> <strong>of</strong> good consultingpractice,(1) and there is goodevidence that this is promoted bylonger consultations(2-4) and bygreater continuity <strong>of</strong> care.(5-6)‘Patient-centredness’ is harder todefine. It indicates a commitmentby doctors to value the contribution<strong>of</strong> patients to deciding what iswrong with them and how theircare should be managed. Amongother things, patients place greatemphasis on being helped tounderstand the nature <strong>of</strong> theirproblems and made able to managetheir own illnesses.(7) ‘Enablement’,measured by the Patient EnablementInstrument (PEI), is an outcomemeasure which captures these<strong>issue</strong>s. (8)Finding a way <strong>of</strong> assessing whetherthe goals <strong>of</strong> holism and patientcentrednessare achieved atconsultations by doctors has proveddifficult, but it is a necessary part <strong>of</strong>assessing quality <strong>of</strong> general practicecare across its <strong>full</strong> breadth. (9) Withingeneral practice, work on quality andthe development <strong>of</strong> performanceindicators(10-11) is in hand on <strong>issue</strong>s<strong>of</strong> practice organization, (12) care<strong>of</strong> continuing health problems, (13)and achievement <strong>of</strong> public healthtargets. (14) However, the coreactivity <strong>of</strong> general practice remainsthe consultation. Two areas <strong>of</strong> workin this discipline are particularlyrelevant to this paper: the use <strong>of</strong> timein consultations and its relation to“enablement,” an outcome measurethat seems related to, but differentfrom, satisfaction (8-9); and continuity<strong>of</strong> care. (5-6)Aim <strong>of</strong> the WorkThe aim <strong>of</strong> the present work was tostudy the quality <strong>of</strong> consultation thatreflects the core values <strong>of</strong> generalpractice. The Specific objectivesincluded the following:1. Measurement <strong>of</strong> the consultationlength <strong>of</strong> type2 diabetics2. Assessment <strong>of</strong> enablement <strong>of</strong> thediabetic patients3. Determination <strong>of</strong> the principalcorrelates associated withenablement as an outcomemeasure.Subjects and MethodsStudy Area and Study PopulationA cross sectional design was used.The study was conducted in IsmailiaCity, Egypt, from February 2009to October 2010. Ismailia City isapproximately 120 km from Cairo. Itis the capital <strong>of</strong> Ismailia Governoratethat is located along the coast <strong>of</strong>Suez Canal, midway between PortSaid and Suez. The target populationwas type 2 diabetic patients inIsmailia City. The study populationwas type-2 diabetics attending thefamily medicine clinic in IsmailiaUniversity hospital. The followingequation, according to Holland etal., 1985, was used for sample sizecalculation: (15)N> [(1.96)2 x Sd2]/ (0.05 x M) 2N, number <strong>of</strong> cases;S.d, standard deviationM, the true value to be estimated andknown from previous worksA pilot study was conducted todetermine the mean and standarddeviation <strong>of</strong> the PEI <strong>of</strong> type-2diabetics. The pilot included 50patients. The mean <strong>of</strong> the PEI was3.58 1.6 (from the pilot study). So thesample size needs to be:N> [(1.96)2 x 1.62]/ (0.05 x 3.58) 2N> 303The study sample (n=310) wasselected randomly by systematicrandom sampling technique whereevery 3rd patient attending the clinicbetween February 2009 to May 2009was included in the study. The studywas completed in October 2010.Informed consent <strong>of</strong> the patients toparticipate in the study was one <strong>of</strong>the inclusion criteria. Type 1 diabeticswere excluded from the study.Description <strong>of</strong> the experimentalmanoeuvre1. Pre-consultation questionnaire:A pre-consultation questionnairewas completed by all patients,to collect socio-demographic data.Patients were asked how well theyknew the doctor they were goingto see.2. Post-consultation questionnaire:Doctors completed informationon the time the consultationstarted and finished (time in andtime out), whether the consultationwas booked, open, and whethera student was present. After theconsultation, the patient completedthe patient enablement instrumentthat included the followingitems: Able to cope with life, Ableto understand your illness, Ableto cope with your illness, Ableto keep yourself healthy, Confidentabout your health, and Able tohelp yourself. Responses <strong>of</strong> “muchbetter,” “better,” and “same or less”or “not applicable” were scored 2,1, and 0 respectively, givinga score range <strong>of</strong> 0-12. (16-17)Patients also indicated whether theconsultation was interrupted.Some help for patients who haddifficulty completing thequestionnaire was available in thewaiting room.Statistical methodsAll statistical analyses wereperformed by using the SPSSs<strong>of</strong>tware package (SPSS, 1996) (18).Measures <strong>of</strong> central tendency anddispersion, as well as, appropriatesignificance tests were appliedaccording to the types <strong>of</strong> variables.Group t-test was computed todetect the significance <strong>of</strong> differencein the age, enablement scores,and duration <strong>of</strong> the consultationbetween males and females.Multiple regression analysis wascomputed to detect the significantlinear associations between theenablement scores <strong>of</strong> type 2diabetics as dependent variableand other independent variablesthat were included in the study. Thefollowing variables were convertedto dummy variables (coded 0.0 and1.0) sex (male and female), knowthe doctor well, interruption <strong>of</strong> theconsultation, consultation type (open20 MIDDLE EAST JOURNAL OF FAMILY MEDICINE VOLUME 10 ISSUE 7MIDDLE EAST JOURNAL OF FAMILY MEDICINE • VOLUME 7, ISSUE 10
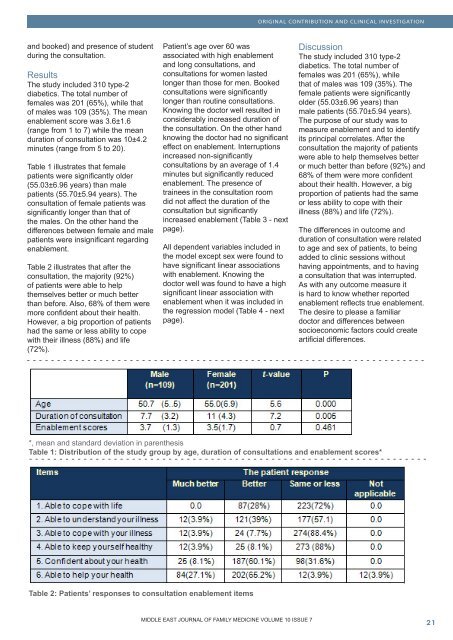
ORIGINAL CONTRIBUTION AND CLINICAL INVESTIGATIONand booked) and presence <strong>of</strong> studentduring the consultation.ResultsThe study included 310 type-2diabetics. The total number <strong>of</strong>females was 201 (65%), while that<strong>of</strong> males was 109 (35%). The meanenablement score was 3.6±1.6(range from 1 to 7) while the meanduration <strong>of</strong> consultation was 10±4.2minutes (range from 5 to 20).Table 1 illustrates that femalepatients were significantly older(55.03±6.96 years) than malepatients (55.70±5.94 years). Theconsultation <strong>of</strong> female patients wassignificantly longer than that <strong>of</strong>the males. On the other hand thedifferences between female and malepatients were insignificant regardingenablement.Table 2 illustrates that after theconsultation, the majority (92%)<strong>of</strong> patients were able to helpthemselves better or much betterthan before. Also, 68% <strong>of</strong> them weremore confident about their health.However, a big proportion <strong>of</strong> patientshad the same or less ability to copewith their illness (88%) and life(72%).Patient’s age over 60 wasassociated with high enablementand long consultations, andconsultations for women lastedlonger than those for men. Bookedconsultations were significantlylonger than routine consultations.Knowing the doctor well resulted inconsiderably increased duration <strong>of</strong>the consultation. On the other handknowing the doctor had no significanteffect on enablement. Interruptionsincreased non-significantlyconsultations by an average <strong>of</strong> 1.4minutes but significantly reducedenablement. The presence <strong>of</strong>trainees in the consultation roomdid not affect the duration <strong>of</strong> theconsultation but significantlyincreased enablement (Table 3 - nextpage).All dependent variables included inthe model except sex were found tohave significant linear associationswith enablement. Knowing thedoctor well was found to have a highsignificant linear association withenablement when it was included inthe regression model (Table 4 - nextpage).DiscussionThe study included 310 type-2diabetics. The total number <strong>of</strong>females was 201 (65%), whilethat <strong>of</strong> males was 109 (35%). Thefemale patients were significantlyolder (55.03±6.96 years) thanmale patients (55.70±5.94 years).The purpose <strong>of</strong> our study was tomeasure enablement and to identifyits principal correlates. After theconsultation the majority <strong>of</strong> patientswere able to help themselves betteror much better than before (92%) and68% <strong>of</strong> them were more confidentabout their health. However, a bigproportion <strong>of</strong> patients had the sameor less ability to cope with theirillness (88%) and life (72%).The differences in outcome andduration <strong>of</strong> consultation were relatedto age and sex <strong>of</strong> patients, to beingadded to clinic sessions withouthaving appointments, and to havinga consultation that was interrupted.As with any outcome measure itis hard to know whether reportedenablement reflects true enablement.The desire to please a familiardoctor and differences betweensocioeconomic factors could createartificial differences.*, mean and standard deviation in parenthesisTable 1: Distribution <strong>of</strong> the study group by age, duration <strong>of</strong> consultations and enablement scores*Table 2: Patients’ responses to consultation enablement itemsMIDDLE EAST JOURNAL OF FAMILY MEDICINE VOLUME 10 ISSUE 7MIDDLE EAST JOURNAL OF FAMILY MEDICINE • VOLUME 7, ISSUE 10 21